Intervensi pembedahan untuk pencegahan atau rawatan limfedema selepas rawatan kanser payudara
Abstract
Background
Breast cancer is the most common type of cancer amongst women worldwide, and one distressing complication of breast cancer treatment is breast and upper‐limb lymphoedema. There is uncertainty regarding the effectiveness of surgical interventions in both the prevention and management of lymphoedema affecting the arm after breast cancer treatment.
Objectives
1. To assess and compare the efficacy of surgical interventions for the prevention of the development of lymphoedema (LE) in the arm after breast cancer treatment.
2. To assess and compare the efficacy of surgical interventions for the treatment of established LE in the arm after breast cancer treatment.
Search methods
We searched the Cochrane Breast Cancer Group’s Specialised Register, the Cochrane Central Register of Controlled Trials, MEDLINE, Embase, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the WHO International Clinical Trials Registry Platform (ICTRP) and ClinicalTrials.gov for all prospectively registered and ongoing trials on 2 November 2017. Reference lists of included studies were also handsearched by three review authors for additional eligible trials.
Selection criteria
All randomised controlled trials (RCTs) comparing a surgical intervention for the prevention or treatment of lymphoedema of the arm after breast cancer treatment to either standard intervention, placebo intervention, or another surgical intervention were included. Patients of both sexes and all ages who have had treatment for their breast cancer were considered. No limits were applied to language or study location. Three authors independently determined the eligibility of each study.
Data collection and analysis
Three authors independently extracted data for each included study using a pre‐designed data extraction pro forma and used Cochrane's 'risk of bias' tool for assessing risk of bias. Dichotomous variables were analysed using the Mantel‐Haenszel method to estimate risk ratios (RRs). Differences in continuous variables were expressed as mean differences (MDs). GRADE was used to assess the certainty of the evidence provided by the included studies.
Main results
Two studies involving 95 participants examined surgical interventions for preventing breast cancer‐related lymphoedema. Both studies evaluated the efficacy of the lymphaticovenular anastomosis technique as part of a preventative management protocol. Both studies were deemed to be at unclear risk of bias overall. Statistical variation between the studies was low, which increases the reliability of the evidence. However, the two studies were conducted in the same centre. Lymphaticovenular anastomosis appears to result in a reduction in the incidence of lymphoedema compared to nonoperative management with a risk ratio of 0.20 (95% CI 0.06 to 0.63, P = 0.006; 95 participants; low‐certainty evidence). The RCTs did not evaluate any of the secondary outcomes.
One study involving 36 participants evaluated the effectiveness of vascularised lymph node transfer for treating breast cancer‐related lymphoedema. The trial was deemed to be at unclear risk of bias. For participants suffering from stage 2 lymphoedema, the evidence suggested reductions in limb volume (MD ‐39.00%, 95% CI ‐47.37% to ‐30.63%, very low‐certainty evidence), pain scores (MD ‐4.16, 95% CI ‐5.17 to ‐3.15, very low‐certainty evidence), heaviness sensation (MD ‐4.27, 95% CI ‐5.74 to ‐2.80, very low‐certainty evidence), mean number of infections/year (MD ‐1.22, 95% CI ‐2.00 to ‐0.44, very low‐certainty evidence), and an improvement in overall function scores (MD ‐3.77, 95% CI ‐4.89 to ‐2.65, very low‐certainty evidence) for those who had undergone vascularised lymph node transfer compared to those who had undergone no treatment.
Authors' conclusions
There is low‐certainty evidence that lymphaticovenular anastomosis is effective in preventing the development of lymphoedema after breast cancer treatment based on the findings from two studies. One study providing very low‐certainty evidence found that vascularised lymph node transfer is an efficacious option in the treatment of established stage 2 lymphoedema related to breast cancer. Important secondary outcomes in this review were rarely reported in the included studies. More high‐quality RCTs are required to further elucidate the effectiveness of surgical interventions in the prevention and treatment of lymphoedema after breast cancer treatment. At the time of this review, no ongoing trials on this topic were identified.
PICOs
Ringkasan bahasa mudah
Teknik pembedahan untuk mencegah dan merawat pembengkakan lengan daripada limfedema selepas rawatan kanser payudara
Apakah isunya?
Ramai wanita dalam dunia ini terkena kanser payudara. Radioterapi dan pembedahan yang digunakan sebagai rawatan kanser payudara mensasarkan payudara, dada serta axilla (atau ketiak) pada bahagian yang terkena dan boleh merosakkan limfatik tempatan di kawasan‐kawasan tersebut. Ini menyebabkan aliran cecair yang lemah dari lengan yang terkena, di mana ini boleh mengakibatkan sensasi berat dan kelihatan bengkak. Istilah yang digunakan untuk menggambarkan keadaan ini adalah limfedema. Limfedema amat dikenali oleh pesakit dan profesional penjagaan kesihatan. Ia menyebabkan ketidakselesaan dan boleh mengganggu banyak aspek kehidupan seharian. Di samping itu, sebilangan pesakit menganggap pembengkakan lengan pada satu sisi tidak sedap dipandang. Pembengkakan jangka panjang mungkin akan menurunkan kualiti kulit dan menyebabkan ulangan jangkitan kulit. Langkah‐langkah tradisional untuk mengatasi keadaan yang menyusahkan ini termasuk latihan lengan, urut, dan stoking mampatan. Walaupun langkah‐langkah ini berkesan untuk mengurangkan pembengkakan lengan, ia memerlukan masa, kesabaran dan dedikasi harian daripada pesakit, serta boleh menyebabkan kerugian terhadap pesakit. Langkah‐langkah tradisional perlu diteruskan sepanjang hayat supaya tetap berkesan.
Soalan kajian
Para profesional penjagaan kesihatan telah memeriksa kaedah alternatif untuk menguruskan limfedema selepas rawatan kanser payudara. Laporan ini mengkaji keberkesanan teknik pembedahan yang dijanakan untuk mencegah atau merawat keadaan ini.
Hasil kajian
Sebilangan teknik telah dicadangkan tetapi hanya tiga kajian yang diterbitan sebelum November 2017 yang memenuhi kriteria untuk dimasukkan dalam tinjauan kami. Dua kajian melihat kepada pencegahan limfedema dan satu kajian melihat kepada merawat limfedema. Secara keseluruhan, ketiga‐tiga kajian ini melibatkan 131 individu.
Dua kajian memberi fokus pada teknik pembedahan anastomosis limfaticovenular (prosedur pencegahan) yang menggabungkan saluran limfa ke saluran darah dan menggunakan sistem peredaran darah untuk mengalirkan cecair yang berlebihan dari lengan. Mereka menunjukkan bahawa individu yang menjalani prosedur pembedahan ini mempunyai risiko yang kurang untuk mendapati limfedema (255 kes kurang dalam 1000 wanita untuk mendapati limfedema, di mana nilai sebenarnya mungkin antara 118 hingga 300 kes kurang dalam 1000 wanita untuk mendapati limfedema) berbanding dengan mereka yang tidak menjalani pembedahan. Kedua‐dua kajian ini tidak memberikan data penting untuk hasil sekunder seperti hasil dilaporkan oleh pesakit, kemampuan untuk menghentikan intervensi selanjutnya untuk limfedema, komplikasi pembedahan, atau komplikasi jangka panjang.
Satu kajian menilai teknik pemindahan nod limfa vaskularis, yang memindahkan sekeping tisu mengandungi nod limfa dari pangkal paha atau perut ke ketiak pada anggota badan yang terkena limfedema. Penulis memerhatikan bahawa mereka yang menjalani prosedur ini mengalami penurunan pada:
‐ isi padu anggota badan: secara purata, wanita yang menjalani prosedur mengalami penurunan 39% isi padu anggota badan berbanding dengan mereka yang diberi rawatan standard sahaja;
‐ sakit: secara purata, wanita yang menjalani prosedur mendapat 4.16 mata lebih rendah dalam skala 10‐mata (seperti 1 = tidak sakit, 10 = sangat sakit) berbanding dengan mereka yang diberi rawatan standard sahaja;
‐ sensasi berat: secara purata, wanita yang menjalani prosedur mendapat 4.27 mata lebih rendah dalam skala sensasi berat 10‐mata (seperti 1 = tidak ada sensasi berat, 10 = sensasi berat yang sangat kuat) berbanding dengan mereka yang diberi rawatan standard sahaja; serta
‐ jangkitan: secara purata, wanita yang menjalani prosedur mendapat 1.22 jangkitan yang lebih rendah dalam setahun berbanding dengan mereka yang diberi rawatan standard sahaja.
Teknik pemindahan nod limfa vaskularisasi juga membantu dalam peningkatan fungsi yang bermaksud, secara purata, wanita yang menjalani prosedur mendapat 3.77 mata lebih baik pada skor fungsi keseluruhan (fungsi diukur dengan skala 10‐mata di mana 1 = fungsi yang sangat baik, 10 = fungsi yang tidak baik) berbanding dengan mereka yang diberi rawatan standard sahaja. Kajian ini tidak memberikan data untuk hasil sekunder yang penting seperti kemampuan untuk berhentikan intervensi lebih lanjut untuk limfedema atau komplikasi jangka panjang.
Kepastian bukti
Kepastian bukti yang menyokong penggunaan anastomosis limfedema dalam pencegahan limfedema adalah rendah, yang hanya terdiri daripada dua kajian kecil dari satu pusat. Begitu juga, hanya satu pusat kajian yang menilai penggunaan pemindahan nod limfa vaskularisasi dan memberikan kepastian bukti yang sangat rendah secara keseluruhan untuk menyokong penggunaan prosedur dalam rawatan limfedema bahagian atas anggota badan.
Authors' conclusions
Summary of findings
| Lymphaticovenular anastomosis compared to standard care for prevention of lymphoedema development | ||||||
| Patient or population: prevention of lymphoedema development | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with standard care | Risk with lymphaticovenular anastomosis | |||||
| Development of LE | Study population | RR 0.20 | 95 | ⊕⊕⊝⊝ | ||
| 319 per 1,000 | 64 per 1,000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The surgical intervention groups were small: In Boccardo 2009 the preventive protocol was followed for 25 women of which seven underwent LVA primarily and the number undergoing LVA at a later stage was not reported. In Boccardo 2011, all 23 participants in the intervention group had LVA done at the time of axillary clearance. 2 In Boccardo 2009, the control group received physical therapy and compression garments only after lymphoedema was detected whereas the intervention group received these as a preventive measure already before any lymphoedema was detected. Therefore, the difference detected between the two groups cannot be attributed solely to the LVA done. In Boccardo 2011, neither of the groups received any compression treatments which means that the effect of the intervention was not compared with the standard treatment but no treatment at all. 3 The study group allocation was not concealed and the assessment was not blinded in either of the included studies. Therefore, we downgraded the certainty of the evidence by 1 point for risk of bias 4 Due to the small number of participants in each trial and wide confidence intervals, we downgraded the certainty of evidence by 1 point for imprecision. | ||||||
| Vascularised lymph node transfer compared to standard care for treatment of arm lymphoedema | ||||
| Patient or population: treatment of arm lymphoedema | ||||
| Outcomes | Relative effects* (95% CI) | № of participants | Certainty of the evidence | Comments |
| Vascularised lymph node transfer vs standard care | ||||
| Reduction of LE (%) | MD 39 lower | 36 | ⊕⊝⊝⊝ | |
| Number of infections per year | MD 1.22 lower | 36 | ⊕⊝⊝⊝ | |
| Pain score (1‐10; where 1 = no pain; 10 = extreme pain) | MD 4.16 lower | 36 | ⊕⊝⊝⊝ | |
| Heaviness score (1‐10; where 1 = no heaviness; 10 = extreme heaviness) | MD 4.27 lower | 36 | ⊕⊝⊝⊝ | |
| Function score (1‐10; where 1 = good function; 10 = poor function) | MD 3.77 lower | 36 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||
| GRADE Working Group grades of evidence | ||||
| 1 The control group in Dionyssiu 2016 study received no physical or compression treatments for the 12 months prior to the final assessment and thus did not receive the current golden standard of nonoperative lymphoedema treatment. Therefore we downgraded the evidence by 1 point for indirectness | ||||
Background
Description of the condition
Breast cancer is the most common type of cancer amongst women worldwide (Globocan 2012). Advances in treatment for breast cancer mean that more women are surviving and living with the consequences of the cancer and its treatment. One common and distressing sequelae of breast cancer treatment is lymphoedema (LE) (Hayes 2008). LE describes a condition where an excess of fluid builds up in the subcutaneous tissue of the arms, usually because of impairment to the outflow of lymphatic fluid from an affected area. Lymph or lymphatic fluid contains circulating tissue fluid and infection fighting white blood cells. The aetiology of the imbalance between production and drainage can be either congenital or acquired, so‐called primary or secondary LE, respectively (Rockson 2008). Secondary LE is more common and has a variety of causes, including infection, cancer, radiation therapy, and surgery. Worldwide, the most common cause of LE is filariasis, caused by infection with the parasite Wuchereria bancrofti, whereas in the developed world the most common cause is malignancy and its treatment (Doscher 2012). As breast cancer is very common, its treatment is a major cause of secondary LE.
LE may occur after breast cancer treatment due to damage or destruction of the upper limb lymphatic drainage system, by either surgery or radiotherapy, or both, or owing to the destructive effects of the cancer itself (Brennan 1996). Estimates of the incidence of LE after breast cancer treatment vary widely depending on the type of treatment undergone and the diagnostic criteria for LE. At five years post‐operation, 5% of patients who have had sentinel node biopsy, a surgery in which only a few lymph nodes are removed for analysis, develop measurable LE compared to 16% of patients who have had an axillary dissection and thus removal of all lymph nodes in the area (McLaughlin 2008). Obstruction to lymphatic drainage and accumulation of lymph fluid in the tissues leads to swelling, thickening of skin and the fatty layer of tissue under the skin, fibrosis or scarring and eventually to elephantiasis with chronic enlargement of the limb (Doscher 2012). The International Society of Lymphology staging system is the most universally accepted system for assessing the degree of LE (ISL 2009). In stage 0 disease, LE is subclinical, with no swelling despite evidence of impaired lymphatic transport; in stage 1, disease swelling is evident but goes down with limb elevation; in stage 2, the swelling is persistent and fibrosis of the subcutaneous tissues becomes evident; and in stage 3, there is thickening of the skin with fatty deposits and lymphostatic warts, so called elephantiasis (ISL 2009).
Patients with LE may experience significant morbidity related to their condition including loss of limb function, discomfort, and disfigurement (Brennan 1996). LE may also be complicated by infections of the affected soft tissue and lymph vessels (cellulitis and lymphangitis) (Shih 2009). Although not a life‐threatening condition, LE can cause great distress for breast cancer survivors, both through the physical effects, described above, and its psychological consequences (Bulley 2013). It can act as a constant reminder of previous disease and attract unwanted attention from others (Petrek 1998). Until recently, the effects that LE can have on a patient's quality of life have been underestimated. This is being addressed by the development of condition‐specific quality of life assessment tools (Keeley 2010).
Measurement of limb circumference is the most commonly used method to evaluate LE as it is simple and widely available (Yamamoto 2013). Other tests are also used, including sentinel lymph node mapping with radioactive tracer in lymphoscintigraphy or radiocontrast material in lymphography, indocyanine green (ICG), and volume assessment based on computed tomography (CT), magnetic resonance imaging (MRI), measurement of water displacement and laser scanning (Bulley 2013;Yamamoto 2013). It is widely considered to be important to diagnose LE as early as possible in the natural history described above. This allows early intervention, including the provision of information and psychological support, and may prevent symptomatic LE formation and progression to severe disease (Yamamoto 2011). Objective evaluation of existing LE is important both to evaluate its extent and to assess interventions to reduce it.
Description of the intervention
Various conservative strategies are used for women with breast cancer to decrease the risk of developing LE (Stuiver 2012) and to manage it, once developed (Preston 2008). These include exercise, patient education, monitoring, compression therapy, manual lymph drainage, and lymph taping (kinesiotaping). There is no consensus as to the optimal conservative management.
Surgery is traditionally the option of last resort, when conservative measures have failed (Vignes 2002). Indications for surgery include insufficient LE reduction by well performed medical and physical therapy, recurrent episodes of lymphangitis, intractable pain, decreasing limb function, patient's dissatisfaction with conservative methods, and the patient's wish to proceed to surgery (Campisi 2010). However, patients and surgeons are increasingly undertaking modern surgical interventions early in the disease process in the hope of preventing or reversing the swelling arising from impaired lymph flow changes (Boccardo 2011).
These interventions include liposuction, lymph node transfer, and lymphaticovenular anastomosis (LVA) (Becker 2006; Brorson 1997; Campisi 2004; Nagase 2005). The techniques aim to either directly reduce the volume of the arm by removing fat and fibrous tissue (liposuction), bypass the obstruction to lymphatic outflow by creating a direct route for lymphatic fluid to re‐enter the circulation in the arm (LVA), or improve lymphatic drainage from the arm possibly by the creation of new lymphatic channels (lymph node transfer).
How the intervention might work
Chronic LE causes an increase in swelling of subcutaneous fat tissue, which leads to deformity and limb swelling. This is the rationale behind liposuction for LE where the hypertrophied adipose tissue is removed in a circumferential fashion through cannulae inserted into small incisions, usually under general anaesthesia (Brorson 2002;Damstra 2009). Lifelong compression garments are then needed to prevent postoperative recurrence of the lymphoedema (Brorson 2002; Damstra 2009).
Microsurgical lymphatic reconstruction is another surgical intervention for LE, most often in the form of LVA, though occasionally an unaffected lymphatic channel is used to bypass the area of lymphatic damage, a method known as a lymphatico‐lymphatic bypass (Lee 2011). LVA consists of anastomosing, or connecting, lymphatic vessels to a small vein in the subcutaneous tissue. This returns the lymph fluid to the circulation peripherally, meaning it no longer has to pass through the area of lymphatic damage to return to the circulatory system. Dye is used to find healthy, functioning lymphatics and to confirm that the connection between the vessels is open. Lymphoscintigraphy or ICG lymphography can be used during follow‐up to confirm ongoing anastomosis patency (Campisi 2010).
Lymph node transfers take healthy lymph nodes from an unaffected limb and move them to either the armpit or elbow of the affected arm (Becker 2006). The aim of the technique is for the transplanted lymph nodes to take over lymphatic drainage from local lymph nodes which have been damaged or removed by surgery (Becker 2006). Notably, the precise mechanism of action of lymph node transplant is complex and is not completely understood.
Why it is important to do this review
LE as a consequence of breast cancer treatment causes severe physical and psychosocial morbidity amongst this patient group. There is no consensus as to which of the available surgical options described above provides the best outcome in this patient group, both in terms of prevention and treatment of established disease. We aim to clarify the indications, benefits, and uncertainties in the field.
Objectives
-
To assess and compare the efficacy of surgical interventions for the prevention of the development of lymphoedema (LE) in the arm after breast cancer treatment.
-
To assess and compare the efficacy of surgical interventions for the treatment of established LE in the arm after breast cancer treatment.
Methods
Criteria for considering studies for this review
Types of studies
We considered all types of randomised controlled trials (RCTs) that compared a surgical intervention for the treatment or prevention of LE in the arm after breast cancer treatment to either standard intervention (conservative measures such as compression garments, lymphatic massage, bandaging, and intermittent pneumatic compression), placebo intervention (surgery performed without the critical surgical step), or another surgical intervention that was included in this review (see types of intervention).
All studies that presented predefined, objective criteria for diagnosing or assessing LE, or both, were considered eligible. These criteria (Bulley 2013;Yamamoto 2013) included, but were not limited to:
-
measurements of tissue volume and distribution, such as water displacement, tape measure, and perometry;
-
determination of limb composition, such as tonometry, skinfold thickness, dual energy x‐ray absorptiometry, and bioelectrical impedance analysis;
-
imaging tests, such as lymphoscintigraphy, lymphangiography, MRI, ultrasound, and CT scanning.
Types of participants
We included participants of both sexes and all ages who had treatment for their breast cancer. This included any type of surgery, radiotherapy, chemotherapy, or combination of these.
Types of interventions
We considered any surgical intervention for the treatment or prevention of secondary LE of the arm after breast cancer treatment. Both reductive and reconstructive techniques were considered, including, but not limited to:
-
liposuction;
-
lymphaticovenular anastomoses;
-
lymphatico‐lymphatic bypass;
-
lymph node transfer.
Types of outcome measures
Primary outcomes
All outcome measures were assessed at the latest time point reported in the study.
Prevention
-
The development of LE at the latest time point specified in the study
Treatment
-
The percentage reduction in LE between randomisation and the end of follow‐up, as measured by a validated system for limb volume measurement
Secondary outcomes
Secondary outcome measures were as follows.
-
Patient‐reported outcomes using validated questionnaires, such as the condition‐specific quality of life measure for limb lymphoedema (LYMQOL) which accounts for not only physical symptoms but also social function and psychological effects (Keeley 2010). Other similar validated questionnaires include the Upper Limb Lymphedema 27 (ULL‐27) (Launois 2002) and Freiburg Life Quality Assessment‐Lymphedema (FLQA‐L) (Augustin 2005).
-
Ability to discontinue further interventions for LE; for example, this may be non‐adherence to or the number of dropouts from continued use of compression therapy, manual therapy, or lymph taping.
-
Surgical complications related to LE surgery, such as seroma, lymphorrhoea, wound dehiscence, wound infections.
-
Long‐term complications, such as rate of cellulitis, lymphangitis, lymphadenitis, skin ulcers, and lymphorrhoea.
Search methods for identification of studies
We did not impose any language or publication date restrictions.
Electronic searches
For published trials, we searched the following on 2 November 2017.
-
The Cochrane Breast Cancer Group (CBCG) Specialised Register. Details of the search strategies used by the CBCG for the identification of studies and the procedure used to code references are outlined in the Group's module (www.mrw.interscience.wiley.com/cochrane/clabout/articles/BREASTCA/frame.html). Trials with the key words 'lymphoedema', 'lymphedema', 'breast cancer', 'axillary clearance', 'axillary lymphadenectomy', 'axillary dissection', 'lymphaticovenular anastomosis', 'lymphaticovenous anastomosis', 'LYMPHA', 'lymph node transfer', 'lymph node flap', 'liposuction', 'lymphatic bypass', 'prevention', and 'treatment' were extracted and considered for inclusion in the review.
-
Cochrane Central Register of Controlled Trials (CENTRAL). See Appendix 1.
-
MEDLINE via OvidSP. See Appendix 2.
-
Embase via EMBASE.com (1947 to January 2015) and OvidSP (January 2015 to November 2017). See Appendix 3 for the search strategy.
-
The Cumulative Index to Nursing and Allied Health Literature (CINAHL) through EBSCO (1980 to May 2013). See Appendix 4 for the search strategy.
For prospectively registered and ongoing trials, we searched:
-
the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) search portal (http://apps.who.int/trialsearch/Default.aspx). See Appendix 5 for the search strategy;
-
ClinicalTrials.gov (http://clinicaltrials.gov/).
Searching other resources
Three review authors independently searched the reference lists of included studies for additional eligible studies.
Data collection and analysis
Selection of studies
Three review authors (PM, NL, VA) independently determined the eligibility of each study. Three authors reviewed the titles and abstracts of all citations found through the search strategy previously described. A copy of the full article for each citation reporting a potentially eligible study was obtained, and three review authors (PM, NL, VA) independently applied the eligibility criteria; any discrepancies were resolved by consensus through discussion with a fourth review author (DF). Where necessary and possible, additional information was sought from the principal investigator of the study concerned. Any exclusions from the review of a potentially eligible study were justified in the final report.
Data extraction and management
Three review authors (PM, NL, VA) independently extracted the data for each included study using a pre‐designed data extraction pro forma. Data were extracted on the details of the study (first author, year of publication, journal, publication status, period and country of study, sources of funding, study design, sample size); participants' characteristics (age, sex, type of disease, stage of disease, type of surgery, and prior treatment status); risk of bias assessment; details of the intervention; duration of follow‐up; and the primary and secondary outcomes. A fourth review author (DF) resolved any discrepancies regarding data extraction, and consensus was reached. The most complete data set feasible was assembled. The study authors were contacted with the aim of acquiring additional information on the data presented.
Assessment of risk of bias in included studies
Three review authors (PM, NL, VA) independently assessed each study for risk of bias using the Cochrane Collaboration's 'risk of bias' tool (Higgins 2011). We considered selection bias, performance bias, detection bias, attrition bias, and reporting bias for each individual study. Any discrepancies were resolved by consensus through discussion with a fourth author (DF). We contacted study authors for additional information to enable the assessment of the risk of bias but did not receive any further information. We acknowledge that there is no accepted definition of high risk of bias, so we chose the threshold as those trials with greater than or equal to three of seven domains (random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, other bias) with high risk of bias when analysed with the Cochrane Collaboration's risk of bias tool to represent high risk of bias studies. In addition, if there were some risk of bias concerns on multiple domains, we classified the study to be an unclear risk of bias overall.
Measures of treatment effect
We planned to use hazard ratios (HRs) with 95% confidence intervals (CIs) to evaluate the comparative times to development of LE after preventive LE surgery and also time to the development of complications related to surgery or to LE itself. However, this was not possible in this review version as there was insufficient detail in the reports of included studies, and the authors did not respond to requests for further information. In future updates, this analysis will be considered.
Risk ratios (RR) with 95% CI were used to quantify the risk of developing LE, surgical complications, and LE complications.
Differences in continuous variables, such as those measuring the percentage reduction of LE after treatment or the psychosocial well‐being of participants with LE, were estimated as mean differences (MDs). The amount of LE was calculated as the excess volume in the affected limb compared to the unaffected limb, expressed as a percentage of the volume of the unaffected limb. The patient‐reported measures of LE‐related well‐being assessed on a 10 point scale (where 1 was good; 10 was bad) were reported as means (at baseline and post‐intervention) and change from baseline scores.
Unit of analysis issues
All included studies addressed people with unilateral LE after breast cancer with each participant randomly assigned. Therefore, no unit of analysis issues arose. With the surgical interventions that were done after a period of observation or nonsurgical treatment, we considered only the postoperative intervention period in the analysis.
Dealing with missing data
We based our analysis only on participants who completed the study and made no assumptions about loss to follow‐up. All analyses were done by intention‐to‐treat (Hollis 1999). If participants were allocated to one intervention (for example LVA), but after randomisation underwent a different intervention (for example lymphatico‐lymphatic bypass), they were analysed according to their randomised allocation. In Boccardo 2009, 89% of participants randomised were assessed at two years. In Boccardo 2011 and Dionyssiou 2016, no participants were lost to follow‐up after randomisation. No missing data was identified to necessitate contacting study authors for additional information.
Assessment of heterogeneity
We examined heterogeneity using the Chi2 test with significance set at a P value of 0.10, and measured the quantity of heterogeneity using the I2 statistic (Higgins 2002).
Thresholds for the interpretation of the I2 statistic can be misleading. A rough guide to interpretation is:
-
0% to 40%, might not be important;
-
30% to 60%, may represent moderate heterogeneity;
-
50% to 90%, may represent substantial heterogeneity;
-
75% to 100%, considerable heterogeneity.
We took factors such as clinical and methodological heterogeneity, along with whether the heterogeneity was in the magnitude of effect or in the direction of effect, into account while interpreting the I2 statistic, particularly where there was overlap in the ranges defining levels of heterogeneity.
Assessment of reporting biases
We compared the reported outcomes with those stated in the methods of the studies and also those listed in clinical trials registries as both primary and secondary outcomes (for example http://www.clinicaltrials.gov/). We planned to assess publication bias by creating a funnel plot using software within Review Manager 5.2 (RevMan 2012) if at least 10 studies were identified. Only three studies were included in this review so a funnel plot was not used.
Data synthesis
We presented a narrative overview of the included studies. Where appropriate, we undertook meta‐analyses of outcome data using Review Manager software (RevMan 2012).
For time‐to‐event data, such as time to development of LE in a prevention study, we planned to plot (and, if appropriate, pool) estimates of the HR and 95% CI as presented in the study reports using the generic inverse variance method in the Review Manager software (RevMan 2012). However, this was not possible in this review version because there was insufficient detail on time‐to event data in the reports, and the authors did not respond to requests for further details. Comparison of the primary outcome for prevention was instead reported as a risk ratio at the final time point.
For dichotomous outcomes, such as surgical wound infection, we planned to present the summary estimate as a RR with 95% CI.
For continuous outcomes measured in the same way across studies, for example, measurements of limb volume, we planned to present a MD with 95% CI. We planned to present a standardised mean difference (SMD) for studies measuring the same outcome using different methods. The three studies identified did not enable these meta‐analyses.
To grade the certainty of the evidence, GRADE profiler software (GRADE) was used and 'Summary of findings' tables were produced for the six prespecified outcomes for the prevention and treatment of LE.
Subgroup analysis and investigation of heterogeneity
We planned to conduct subgroup analyses for participants with different types of axillary surgery and adjuvant treatments as well as those with normal or high body mass index. However, all three studies identified enrolled only participants who had axillary clearance and the study samples were too small to allow any subgroup analyses.
In future review updates, if possible, the following will be considered for possible subgroup analysis:
-
patients with sentinel lymph node biopsy and complete lymph node clearance;
-
patients treated with and without radiotherapy to the axilla;
-
patients treated with and without radiotherapy to any area (axilla, breast, chest wall);
-
patients treated with and without chemotherapy;
-
patients with a body mass index above 30 or below 30;
-
patients with different stages of lymphoedema.
Sensitivity analysis
We planned to perform sensitivity analysis, through excluding studies with a high risk of bias from the analysis. We acknowledged that there is no accepted categorisation of high risk of bias and therefore judged a study to be at high risk of bias if greater than or equal to three of seven domains were judged to be at high risk of bias. However, only three studies were identified and a sensitivity analysis was not conducted.
Results
Description of studies
Results of the search
A total of 792 records were retrieved (see Figure 1). Fourteen records were considered potentially relevant, and three of these met our predefined inclusion criteria (Boccardo 2009; Boccardo 2011; Dionyssiou 2016). There were no ongoing studies or studies awaiting classification identified.
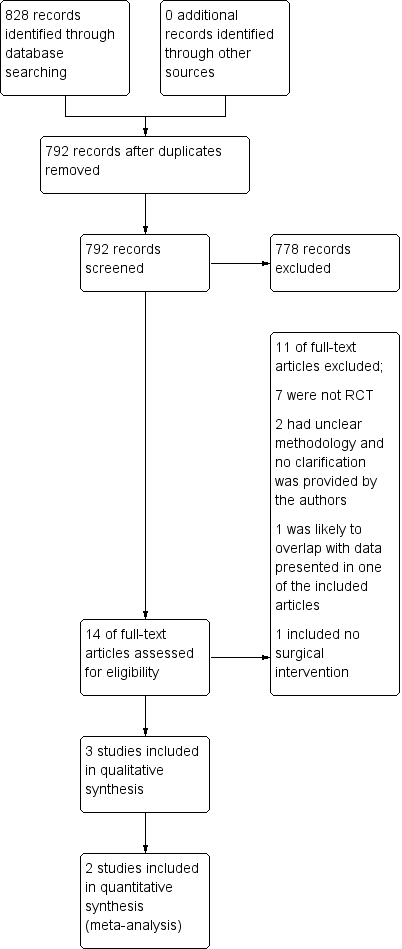
Study flow diagram.
Included studies
Three studies were included: two studies reported on the effectiveness of lymphaticovenular anastomosis as part of preventive management protocols in the prevention of breast cancer‐related lymphoedema (Boccardo 2009; Boccardo 2011) and one study (Dionyssiou 2016) reported on the effectiveness of vascularised lymph node transfer in the treatment of established breast cancer‐related lymphoedema, comparing outcomes at 18 months between two groups of participants ‐ the intervention group ‐ who had lymph node transfer and six months of combination physical and compression therapy, and the comparator group ‐ who had six months of combination physical and compression therapy only. All participants in the three studies were women. Lymphoedema was defined as an arm volume increase of 100 mL (Boccardo 2011) or 200 mL (Boccardo 2009) in comparison with the preoperative volume of that arm or as a percentage difference in volume of the affected arm in comparison with the unaffected arm (Dionyssiou 2016). Refer to the Characteristics of included studies for additional details.
Excluded studies
Of the eleven potentially relevant studies that were eventually excluded, seven studies were determined to not be randomised controlled trials after full‐text review (Brorson 1997; Brorson 1998; Brorson & Svensson 1998; Brorson 2000; Ciudad 2017; Maldonado 2011; Saaristo 2012); two studies had incomplete reporting of the study design making it impossible to determine whether they were randomised trials (Campisi 2006; Youssef 2010); one study was reported as an abstract with results that likely overlapped with another study which had already been assessed in this review (Campisi 2014); and one study was determined to not have evaluated a surgical technique (Hou 2008).
Efforts were made to contact authors to clarify their methods where there were uncertainties, but there was either no response to our efforts or no available contact details (Campisi 2006; Campisi 2014; Youssef 2010). Refer to the Characteristics of excluded studies.
Risk of bias in included studies
See Figure 2 for visual summaries of the 'risk of bias' assessment. All three studies, Boccardo 2009, Boccardo 2011 and Dionyssiou 2016, were judged to be at unclear risk of bias due to multiple domains in each study being at unclear or high risk of bias.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Both Boccardo 2009 and Boccardo 2011 were rated as unclear risk for selection bias. The studies mentioned only that they "randomly assigned" participants to different groups, without describing how the randomisation was achieved. There was also no mention as to when the allocation was revealed and whether steps were taken to ensure strict implementation of the schedule of random assignments by those enrolling participants into the different treatment arms. However, it was notable that, in both studies, no statistically significant, or potentially clinically important, differences in participants' baseline characteristics were noted between the treatment and control groups; comparisons included age, body mass index, the presence of metastatic lymph nodes, baseline lymphoedema volume, radiotherapy, infection, etc (Boccardo 2009; Boccardo 2011).
Dionyssiou 2016 employed both a satisfactory method of random sequence generation using a "random number generator" and a conscious approach to conceal allocation by revealing allocation only after participants had been initially examined, assessed and recruited. These efforts resulted in an overall rating of low risk of selection bias for this study.
Blinding
Two of the studies had a high risk of performance and detection bias as, for each of the studies, the control group did not receive a surgical intervention (Boccardo 2009; Dionyssiou 2016) and it would be practically impossible to blind the surgeons and participants to the surgical treatments provided. Moreover, outcome assessors could not practically be reliably blinded to the intervention received because of the presence of surgical scarring and also participants' knowledge. In the third study (Boccardo 2011), the experimental surgical intervention was done during the same operation as standard care. However, it was not clear whether the participants were blinded to the treatment provided.
Incomplete outcome data
For two studies, there were no concerns regarding attrition bias, and complete outcome data were reported for all participants (Boccardo 2011; Dionyssiou 2016). Boccardo 2009 reported that 6, or 11%, of their 55 participants did not complete follow‐up. Unfortunately, no reasons were specified for failure to complete the follow‐up assessments and partial data were included so it was unclear as to what impact this would have on the results.
Selective reporting
All three studies were rated as low risk for reporting bias (Boccardo 2009; Boccardo 2009; Dionyssiou 2016). Whilst no pre‐trial protocols were available, all results in these studies were reported as per the outcomes specified in the methods (Boccardo 2009; Boccardo 2009; Dionyssiou 2016). Notably, however, neither Boccardo 2009 nor Boccardo 2011 formally looked at surgical complications as an outcome to be assessed, and it was certainly unclear whether their participants suffered any complications as part of the procedure.
Other potential sources of bias
No other potential sources of bias were identified.
Effects of interventions
See: Summary of findings for the main comparison Lymphaticovenular anastomosis compared to standard care for prevention of lymphoedema development; Summary of findings 2 Vascularised lymph node transfer compared to standard care for treatment of arm lymphoedema
Prevention
The development of LE
Both Boccardo 2009 and Boccardo 2011 included the development of LE as an outcome, reporting on a total of 95 participants. The statistical heterogeneity between the trials was low (I2 = 0%, P = 0.68). Analysis using a fixed‐effect model demonstrated that participants who had undergone lymphaticovenular anastomosis as a preventive measure had a reduced risk of developing lymphoedema during the 18‐month (Boccardo 2011) and 24‐month (Boccardo 2009) follow‐up compared to those who had not (RR 0.20, 95% CI 0.06 to 0.63, P = 0.006; low‐certainty evidence ; Analysis 1.1; Figure 3).

Forest plot of comparison: 1 Development of LE, outcome: 1.1 Development of LE.
Patient‐reported outcomes
The two studies did not evaluate patient‐reported outcomes.
Ability to discontinue further interventions for LE
The two studies did not report on this outcome.
Surgical complications (seroma, lymphorrhoea, wound dehiscence, wound infections)
The two studies did not report on these outcomes.
Long‐term complications (cellulitis, lymphangitis, lymphadenitis, skin ulcers, and lymphorrhoea)
The two studies did not report on these outcomes.
Treatment
The percentage reduction of LE
Dionyssiou 2016 reported a statistically significant difference (57% versus 18%) in mean limb volume reductions for participants who had undergone lymph node transfer in addition to standard care (i.e. physical and compression therapy) and those participants who had received standard care alone.This equated to a difference in volume reduction of 39.00% (95% 30.63% to 47.37%; 36 participants; very low‐certainty evidence) between the two groups, favouring lymph node transfer over no treatment (P < 0.00001; Analysis 2.1; Figure 4).
![Forest plot of comparison: 2 Reduction of LE, outcome: 2.1 Reduction of LE [%].](/cdsr/doi/10.1002/14651858.CD011433.pub2/media/CDSR/CD011433/image_n/nCD011433-AFig-FIG04.png)
Forest plot of comparison: 2 Reduction of LE, outcome: 2.1 Reduction of LE [%].
Patient‐reported outcomes
Dionyssiou 2016 studied various patient‐reported outcomes: pain, sensation of heaviness, and overall function, all of which were rated on a 10‐point scale (Dionyssiou 2016). This scale ranged from 1 (e.g. no pain or good function) to 10 (e.g. extreme pain or very poor function). Those in the lymph node transfer group (plus with standard care) experienced a reduction in pain, heaviness sensation, and also improvements function scores compared to baseline, in contrast to effects that were statistically not significant amongst participants in the standard care alone group. The mean difference in pain reduction (MD ‐4.16, 95% CI ‐5.17 to ‐3.15; very low‐certainty evidence; Analysis 2.2), sensation heaviness reduction (MD ‐4.27, 95% CI ‐5.74 to ‐2.80; very low‐certainty evidence; Analysis 2.3), and overall functional improvement (MD ‐3.77, 95% CI ‐4.89 to ‐2.65; very low‐certainty evidence; Analysis 2.4) favoured lymph node transfer over no treatment.
Ability to discontinue further interventions for LE
The study did not report on this outcome.
Surgical complications (seroma, lymphorrhoea, wound dehiscence, wound infections)
Dionyssiou 2016 reported that lymph node transfer reduced the mean number of infections per year that participants experienced in the arm affected by LE, such as erysipelas, cellulitis, or lymphangitis. The reduction in the mean number of infections was greater for the surgical group with an MD ‐1.22 (95% CI ‐2.00 to ‐ 0.44; very low‐certainty evidence; Analysis 2.5).
Long‐term complications (cellulitis, lymphangitis, lymphadenitis, skin ulcers, and lymphorrhoea)
The study did not report on these outcomes.
Discussion
Summary of main results
Performing lymphaticovenular anastomosis as part of a preventive management protocol early during breast cancer treatment appears to reduce the risk of lymphoedema development in the arm on the affected side (based on the results of two studies). However, these two prevention studies did not report on important secondary outcomes. Vascularised lymph node transfer used in the treatment of established breast cancer‐related lymphoedema may reduce limb volume, pain scores, heaviness sensation, and infections per year and improve overall function (based on one study). Important secondary outcomes such as long‐term complications and ability to discontinue further interventions for treating lymphoedema were not collected in the study.
Overall completeness and applicability of evidence
Due to the lack of randomised controlled trials on the topic, our systematic review has been able to answer only one of a number of questions it could have potentially addressed. In particular, there were no eligible studies that compared the effectiveness of one surgical technique against another, and there were no eligible studies that looked at the efficacy of other known surgical techniques, such as liposuction and lymphatico‐lymphatic bypass, in the treatment and/or prevention of breast cancer‐related lymphoedema. Amongst the studies retrieved and included, there was also a lack of uniformity in the way lymphoedema was assessed, outcomes measured, and complications reported.
The two studies examining the use of lymphaticovenular anastomosis in the prevention of breast cancer‐related lymphoedema included women who had undergone or were scheduled to undergo complete axillary dissection as part of their breast cancer treatment (Boccardo 2009; Boccardo 2011). The certainty of the evidence provided by these two studies was low. The studies included a total of only 95 participants, insufficient numbers for effective subgroup analysis, which would have been helpful, for example, in identifying participants' characteristics that may be more predictive of treatment success, informing future management pathways. It is also notable that these two studies only evaluated one outcome ‐ the presence of lymphoedema. The authors did not formally report on patient‐reported outcome measures, postoperative complications, or the ability to discontinue with further interventions; and since the maximum follow‐up time for the studies was only two years, long‐term outcomes were unknown. The data from both studies came from only one surgical team based in Italy, which potentially reduces generalisability of the evidence.
One study evaluated the effectiveness of vascularised lymph node transfer, without the need for continued physical or compression therapy, in the treatment of established breast cancer‐related lymphoedema of stage 2 severity, again potentially reducing generalisability of the evidence. (Dionyssiou 2016). The certainty of the evidence provided in this study was very low. Similar to Boccardo 2009 and Boccardo 2011, Dionyssiou 2016 was limited by both a relatively small number of study participants and a short follow‐up period. Dionyssiou 2016 did look at a wider range of outcomes, however, to include not only the reduction of the number of infections per year, but also patient‐reported outcome measures such as pain, sensation of heaviness, and function. Nevertheless, an important question this trial failed to answer was whether participants who underwent vascularised lymph node transfer experienced outcomes that were comparable to those who underwent complete decongestive physiotherapy, the current gold standard treatment of lymphoedema.The 'control' group in Dionyssiou 2016 had no physical or compression treatment for a total of 12 months prior to their final evaluation.
Quality of the evidence
The number of eligible studies for this review was low, and the conclusions were based on a total of only 131 participants. Whilst all three studies were randomised controlled trials, there were a number of design deficiencies. There was no evidence of random sequence generation or allocation concealment in two of the trials, and because of the surgical nature of the interventions, blinding of participants, personnel, and outcome measurement was, in some cases, impossible. Outcome data for Boccardo 2009 was incomplete because six participants failed to complete follow‐up; no reasons or partial outcomes were reported. Additionally, our final rating of low risk for selective reporting in the Boccardo studies may be incorrect, since the authors did not formally mention patient‐reported outcomes, postoperative complications, or the ability to discontinue with further interventions, which would have been expected for modern studies analysing surgical interventions. Increased follow‐up times would have also made the findings of this systematic review more authoritative.
With respect to the evidence for the use of lymphaticovenular anastomosis in the prevention of lymphoedema, the heterogeneity between Boccardo 2009 and Boccardo 2011 was low and the results for the main outcome were consistent. Whilst the participants' demographic characteristics, interventions, and methods were slightly different, both studies suggested a decreased risk of lymphoedema development when lymphaticovenular anastomosis was performed early as part of or after breast cancer treatment. Overall, the certainty of the evidence supporting the use of lymphaticovenular anastomosis provided in these studies was graded as low.
The Dionyssiou 2016 showed clear, statistically significant differences, for five different outcomes, of the effectiveness of vascularised lymph node transfer for the treatment of established breast cancer‐related stage 2 lymphoedema. Overall, the certainty of the evidence provided in this study was very low. The major shortcoming of the study, however, is arguably whether this trial addressed the correct question. Specifically, it compared participants who had undergone vascularised lymph node transfer against participants who received no treatment for 12 months prior to the final evaluation of their lymphoedema. Indeed, a more appropriate method would have been to compare their surgical outcomes with participants who have been treated with gold standard complex decongestive therapy throughout the duration of follow‐up. This would have provided valuable insight as to whether participants could truly completely do away with time‐consuming physical and compression therapy after surgical treatments for breast cancer‐related lymphoedema. Furthermore, the sensitivity of the 10‐point scale used was not addressed, questioning the clinical significance of the statistically significant changes detected for the various domains.
Potential biases in the review process
The potential for bias in the review process was low to moderate. The literature search was conducted by the Cochrane Breast Cancer Group according to accepted standards. We are therefore confident that studies on this topic have been captured in this review. Additionally, study selection was undertaken independently by three review authors (PM, NL, and VA), working in strict adherence to agreed upon inclusion/exclusion criteria. Disagreements were resolved by a senior reviewer (DF).
However, because non‐English language articles were identified in the search and the four review authors are English language speaking, non‐English language material could have been missed. The authors attempted to prevent this from happening by having any non‐English language material reviewed and assessed by medically‐trained colleagues fluent in the non‐English language in question. Notably, none of the non‐English language articles met the inclusion criteria for this review.
Overall, it is difficult to exclude publication bias secondary to outcomes that have not been published because the results were not significant or because the trials were not accepted for publication by journal editors.
Agreements and disagreements with other studies or reviews
Five earlier systematic reviews reported on the effectiveness of surgical intervention for extremity lymphoedema and were mainly based on case series (Carl 2017; Cormier 2012; Leung 2015; Penha 2013; Scaglioni 2017). Two of these focused specifically on breast cancer‐related lymphoedema (Leung 2015; Penha 2013); one focused specifically on the lymphovenous anastomosis technique (Scaglioni 2017); and the remaining two additionally covered lymphoedema affecting the lower limbs (Carl 2017; Cormier 2012). Between the earliest and latest of the above reviews, it is clear that there has been an explosion of research regarding this topic in recent years; indeed, whilst Cormier 2012's comprehensive search returned only 20 eligible studies in 2010, a similarly comprehensive search done by Carl 2017 returned 69 eligible studies in 2016 (Cormier 2012; Carl 2017). Nevertheless, the major conclusions that could be drawn from all the above studies are the same and concur with the perspective reached by the present Cochrane reviewers: as there is very low‐certainty evidence of the effectiveness of surgical intervention for the treatment of lymphoedema, the conclusions that could be drawn from the evidence are limited overall both by the relatively short follow‐up periods and the small number of randomised controlled trials.
With respect to specific recommendations, Penha 2013 favoured vascularised lymph node transfer, because from their qualitative assessment of the literature at the time, it was the only technique which provided evidence to allow for the discontinuation of postoperative conservative therapy. Furthermore, they reasoned that the technique could theoretically be combined with autologous breast reconstruction, which might make it easier to incorporate into already established breast cancer management programs (Penha 2013). Leung 2015 agreed with the potential benefit of utilising vascularised lymph node transfer as part of planned breast reconstruction, but argued that the risk and potential morbidity associated with the procedure (e.g. donor site lymphoedema, scarring, cosmetic concerns, etc.) make it less preferable to the less invasive lymphovenous approach in the treatment of less severe lymphoedema up to International Society of Lymphology (ISL) stage IIa (Leung 2015). From their systematic review and meta‐analyses, Carl 2017 further clarified the potential treatment algorithm, suggesting lymphovenous anastomosis as the preferred method for Tc‐99m lymphoscintigraphy‐defined partially obstructed lymphoedema up to ISL stage II, but vascularised lymph node transfer, liposuction, or excision for more severe cases with total lymphatic obstruction.
For want of randomised controlled trials, this present review is unable to further clarify the validity of the treatment algorithm proposed by Carl 2017. However, this review does make a case for extending the proposed algorithm to include the use of lymphovenous anastomosis for the prevention of breast cancer‐related lymphoedema. It also lends further evidence to support the use of vascularised lymph node transfer for those with more severe lymphoedema.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Development of LE, outcome: 1.1 Development of LE.
![Forest plot of comparison: 2 Reduction of LE, outcome: 2.1 Reduction of LE [%].](/cdsr/doi/10.1002/14651858.CD011433.pub2/media/CDSR/CD011433/image_n/nCD011433-AFig-FIG04.png)
Forest plot of comparison: 2 Reduction of LE, outcome: 2.1 Reduction of LE [%].

Comparison 1 Prevention of LE, Outcome 1 Development of LE.

Comparison 2 Treatment of LE, Outcome 1 Reduction of LE.

Comparison 2 Treatment of LE, Outcome 2 Pain score (1‐10 scale).

Comparison 2 Treatment of LE, Outcome 3 Heaviness sensation score (1‐10 scale).

Comparison 2 Treatment of LE, Outcome 4 Function score (1‐10 scale).

Comparison 2 Treatment of LE, Outcome 5 Number of infections per year.
| Lymphaticovenular anastomosis compared to standard care for prevention of lymphoedema development | ||||||
| Patient or population: prevention of lymphoedema development | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with standard care | Risk with lymphaticovenular anastomosis | |||||
| Development of LE | Study population | RR 0.20 | 95 | ⊕⊕⊝⊝ | ||
| 319 per 1,000 | 64 per 1,000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 The surgical intervention groups were small: In Boccardo 2009 the preventive protocol was followed for 25 women of which seven underwent LVA primarily and the number undergoing LVA at a later stage was not reported. In Boccardo 2011, all 23 participants in the intervention group had LVA done at the time of axillary clearance. 2 In Boccardo 2009, the control group received physical therapy and compression garments only after lymphoedema was detected whereas the intervention group received these as a preventive measure already before any lymphoedema was detected. Therefore, the difference detected between the two groups cannot be attributed solely to the LVA done. In Boccardo 2011, neither of the groups received any compression treatments which means that the effect of the intervention was not compared with the standard treatment but no treatment at all. 3 The study group allocation was not concealed and the assessment was not blinded in either of the included studies. Therefore, we downgraded the certainty of the evidence by 1 point for risk of bias 4 Due to the small number of participants in each trial and wide confidence intervals, we downgraded the certainty of evidence by 1 point for imprecision. | ||||||
| Vascularised lymph node transfer compared to standard care for treatment of arm lymphoedema | ||||
| Patient or population: treatment of arm lymphoedema | ||||
| Outcomes | Relative effects* (95% CI) | № of participants | Certainty of the evidence | Comments |
| Vascularised lymph node transfer vs standard care | ||||
| Reduction of LE (%) | MD 39 lower | 36 | ⊕⊝⊝⊝ | |
| Number of infections per year | MD 1.22 lower | 36 | ⊕⊝⊝⊝ | |
| Pain score (1‐10; where 1 = no pain; 10 = extreme pain) | MD 4.16 lower | 36 | ⊕⊝⊝⊝ | |
| Heaviness score (1‐10; where 1 = no heaviness; 10 = extreme heaviness) | MD 4.27 lower | 36 | ⊕⊝⊝⊝ | |
| Function score (1‐10; where 1 = good function; 10 = poor function) | MD 3.77 lower | 36 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||
| GRADE Working Group grades of evidence | ||||
| 1 The control group in Dionyssiu 2016 study received no physical or compression treatments for the 12 months prior to the final assessment and thus did not receive the current golden standard of nonoperative lymphoedema treatment. Therefore we downgraded the evidence by 1 point for indirectness | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Development of LE Show forest plot | 2 | 95 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.06, 0.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Reduction of LE Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐39.0 [‐47.37, ‐30.63] |
| 2 Pain score (1‐10 scale) Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐4.16 [‐5.17, ‐3.15] |
| 3 Heaviness sensation score (1‐10 scale) Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐4.27 [‐5.74, ‐2.80] |
| 4 Function score (1‐10 scale) Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐3.77 [‐4.89, ‐2.65] |
| 5 Number of infections per year Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐1.22 [0.00, ‐0.44] |

