Testy wykrywające zeza u dzieci w wieku od 1 do 6 lat w populacji ogólnej
Appendices
Appendix 1. Prevalence of strabismus
| Study ID | Country/ Region | Definition of strabismus | Population | Strabismus prevalence |
| Friedman 2009 | USA, Baltimore. | Any constant or intermittent heterotropia at near or distance fixation. | Age 6 to 71 months, white. | 3.3% |
|
|
|
| Age 6 to 71 months, African‐American. | 2.1% |
| Preslan 1996 | USA, Baltimore. | Manifest strabismic deviation with or without fixation preference, using alternate cover testing with the child fixating on an accommodative target at 33 cm. | All children attending one school: preschool (125 children), kindergarten (213), first grade (165) and second grade (177); 75% African‐American, 22% white, 3% other. | 3.1% |
| Traboulsi 2008 | USA, Cleveland. | Manifest ocular deviation of any type or magnitude with or without fixation preference; any vertical phoria; any esophoria more than 8 prism dioptres (PD) or exophoria more than 15 PD at near or distance; any restricted eye movement or muscle overaction. | Age 4 to 8 years. | 2.1% |
| Turacli 1995 | Turkey, Ankara. | Not defined, but results report manifest and latent deviations, with manifest in 93% of all those classified as "strabismic". | Children attending randomly selected school in the Ankara urban area, age 5 to 12 years. | 2.5% |
| Wedner 2000 | Tanzania, rural area | Not defined. | Tanzanian children and young people age 7 to 19 years. | 0.5% |
| Matsuo 2007a | Japan, Okyama. | Not defined in abstract; full article not available. | Japanese children age 1.5 years. | 0.01 to 0.12% |
| Japanese children age 3 years. | 0.2 to 0.34% | |||
| Matsuo 2007b | Japan, Okyama | Not defined in abstract; full article not available | Japanese children age 6 to 12 years | 0.99% in 2005, 1.28% in 2003 |
| Graham 1974 | UK | Manifest deviation, or exophoria of 9 PD or more, or esophoria of 7 PD or more, any hyperphoria. | All children born in Cardiff between 1 January and 31 December in one year (not specified), age 5 to 6 years. | manifest or large latent: 7%; manifest only: 5% |
Appendix 2. Index tests
Corneal reflection test (Hirschberg) (Hirschberg 1881)
First described in 1881, the Hirschberg or corneal reflection test (CRT) uses the reflection of a light target by the surface of the cornea, also known as first Purkinje image, to evaluate whether the eye is fixing on a target. The normal position of the corneal light reflection (CR) is 0.5 mm nasal to the centre of the cornea, as the fovea is located temporal to the optical axis, resulting in a small angle between the visual axis and the optical axis of the eye (angle kappa).
In the literature there is some confusion around the terms visual axis, pupillary axis, optical axis, line of sight, angle kappa and angle lambda.
The visual axis is the line connecting the fovea and the nodal point of the eye and continuing anteriorly through the cornea.
The pupillary axis is the line perpendicular to the cornea that intersects the centre of the pupil. It is a clinical approximation of the visual axis.
The optical or anatomical axis of the eye connects the centre of the curvature of the cornea and the centre of the curvature of the posterior pole.
The line of sight is the line that connects the fixation point and the centre of the pupil; it is a clinical approximation of the optical axis.
The angle between visual and optical axis is called angle kappa. Landolt originally defined angle kappa as "the angle between the visual axis and the so‐called central pupillary line (the pupillary axis)" (Emsley 1948). Lancaster then defined angle lambda as the angle between the pupillary axis and the line of sight. LeGrand finally re‐defined angle kappa exactly the way Lancaster had defined angle lambda, stating that the nodal point of the eye is a theoretical concept, and that for all practical purposes the visual axis is identical to the line of sight (LeGrand 1980). In addition, angle lambda and angle kappa are nearly identical when the point of fixation is not very close to the eye.
Angle kappa is the angle between the visual and optical axis, or between the pupillary axis and the line of sight (LeGrand 1980). By convention it is normally positive.
Individuals with exotropia have higher angle kappa values than esotropic and orthotropic individuals (Basmak 2007). A large angle kappa may also give rise to pseudo‐exotropia. When the fovea is situated nasal to the optical axis, such as in high myopia or ectopic fovea, for example after retinopathy of prematurity, the angle kappa is negative, the CR is located temporal to the centre of the cornea, and pseudo‐esotropia may be present.
In ocular misalignment, the CR is displaced – nasally in exotropia, temporally in esotropia (Hirschberg 1881). When the CR is located at the border of the pupil, the deviation is approximately 15 prism dioptres (PD). If it lies midway across the iris, the deviation measures around 30 PD, and when the reflection is near the limbus, around 45 PD. Hirschberg’s original observations indicated a ratio of 12 to 14 PDs per millimetre displacement of the CR from the pupillary axis, the so‐called Hirschberg ratio. Later evaluations of the Hirschberg test using photography to standardise measurements indicated a ratio of 19.5/1 (Wick 1980), 21/1 (Brodie 1987; DeRespinis 1989), 22/1 (Eskridge 1988) or 24/1 (Carter 1978) with little change from birth to adulthood (Hasebe 1998; Riddell 1994; Wick 1980). Photographs acquired whilst fixating with first the preferred eye, then the deviating eye, in primary position and in slightly eccentric fixation may allow a highly accurate measurement of the ocular misalignment (Romano 2006). Based mainly on reasons of photographic technique, some consider the limbus a more accurate landmark than the centre of the pupil (Barry 1997; Romano 2006); however displacement from the centre of the pupil remains the more commonly used value.
Use of the Hirschberg test as a screening test for ocular alignment has been recommended in young preverbal and also in pre‐school children (daSilva 1991; Sansonetti 2004). To allow standardisation, videographic techniques have been proposed (Miller 1993). These can be applied when using video refractors or photoscreeners developed for the automated assessment of refractive errors (Griffin 1989; Hasebe 1995; Moghaddam 2012; Schaeffel 2002; Weinand 1998).
Automated assessment of CR on digital photographs and videographs is currently in development (Almeida 2012; Model 2012; Yang, 2012).
Accuracy of the Hirschberg test may be in the range of ± 9 to 10 PD, which would make it unsuitable to detect or exclude microtropia. In orthoptic practice, Hirschberg and Krimsky tests are reserved for very young, preverbal patients or those with profound visual impairment which prevents fixation with the affected eye(s). The Hirschberg test is useful to demonstrate pseudo‐strabismus in young children with a broad nasal bridge and epicanthal folds or in individuals with wide interpupillary distance.
Coaxial fundus reflex test (Brückner)
The Brückner test (Brückner 1965; Tongue 1981) is based on reflection of light by the fundus/retina at the back of the eye. A bright coaxial light source and observation system is used, usually a direct ophthalmoscope. Both eyes of the patient are simultaneously illuminated from a distance of around one metre. The observer notes any difference in brightness of the fundus reflex seen in the pupil through the ophthalmoscope. In the presence of strabismus the reflex is darker in the fixing eye than in the deviated eye. An additional, dynamic examination of pupil size, pupil reaction to light, and fixation movement of the eyes on alternating illumination can be useful to detect amblyopia (Tongue 1981). Whilst the manual Brückner test appears reliable at detecting strabismus, it may give rise to false positives, and its usefulness in screening for ocular misalignment is unclear (Griffin 1986; Griffin 1989). A recent evaluation of a modified Brückner test, performed using a streak retinoscope, indicated a sensitivity of 0.5, specificity of 0.98, negative predictive value of 0.97 and positive likelihood ratio of 20 to detect strabismus in a cohort of 343 children with a 5% prevalence of strabismus (Amitava 2012). Photographic and videographic versions of the Brückner test may also have high sensitivity and specificity to detect strabismus (Carrera 1993; Cibis 1994; Kaakinen 1979; Miller 1995; VanEenwyk 2008). Some photorefractors use the Brückner principle, as refractive errors cause a white crescent at the pupil border (Arnold 2000; Kothari 2007; Tongue 1987; Weinand 1998). These devices are commonly used in community screening programmes, operated by lay observers (Arnold 2000). Sensitivity and specificity appear higher on analysis of the coaxial fundus reflex on photographs than during manual performance of the test (Paysse 2001). The size of misalignment may affect the accuracy of the Brückner test, with lower sensitivity in small‐angle esotropia (Graf 2012).
Stereovision tests
Stereovision or stereopsis is the perception of depth when viewing a scene with both eyes. As the visual axis of the right and left eye are at a slight angle to each other, the image seen by the right eye slightly differs from that seen by the left eye. This binocular disparity allows the brain to 'calculate' depth in the visual scene. True stereopsis requires perfect alignment and fusion of the foveal images from both eyes, known as central fusion. When assessing stereopsis, it is important to eliminate any monocular cues and to present stimuli whose three‐dimensional qualities can only be perceived when foveal information from both eyes is integrated.
Tests of stereovision may indicate ocular misalignment. As other causes — such as uncorrected refractive errors and reduced visual acuity — also impair stereopsis, specificity for any particular cause may be poor.
Stereopsis is most commonly tested at near. Near stereotests fall into two categories: contour (Titmus fly, Wirt ring test); and random dot tests. Contour tests achieve horizontal image disparity by vectographic techniques and require polarised glasses to view a three‐dimensional (3D) picture embedded in polarised filter sheets made from plastic. By stacking two of these sheets at a perpendicular angle, a separate image is shown to each eye. When viewed without the glasses, the picture can still be seen, but its 3D qualities can only be perceived through the polarising glasses. As contour tests gives some monocular cues to the position of the 3D shapes many clinicians prefer random dot tests for testing stereovision.
Random dot images do not contain any contour lines. Shapes can only be seen and depth can only be perceived when true binocular stereopsis with central (foveal) fusion is present. Random dot tests include the Frisby, Lang, TNO, Randot and Randot‐E stereotests (Broadbent 1990; Lang 1983; Rosner 1984; Simons 1981b).
The Frisby test consists of three Perspex plates of different thickness. On each plate there are four square areas which contain triangular shapes apparently distributed in a random pattern. On one of the squares, some shapes arranged in a geometric pattern, such as a circle, are printed onto the back surface of the Perspex plate, whilst the remaining square is filled with triangles printed onto the front surface. The physical thickness of the Perspex plate and the distance between the shapes printed onto the front and the back of the plate induce horizontal image disparity. This test is simple to perform, does not require 3D viewers and is popular with children. Preverbal children may point onto the 3D shape or may direct their eyes towards it, similar to their response in preferential looking tests.
The Lang stereotest combines two methods of three‐dimensional image perception: random dots and cylindrical gratings. The cylindrical gratings use a prismatic effect to achieve the slight horizontal image displacement required for a 3D effect. The advantage of this method is that it does not require special glasses for viewing. Essentially, the separation of the two images is achieved by a system of fine parallel cylindrical shapes. Beneath each cylinder are two fine strips of picture, one seen by the right, the other seen by the left eye. In the Lang test, random dot images hide simple shapes such as a star, a cat, a car. As it does not require 3D viewers, it is easy to use with children and is commonly used in vision screening programmes. Like the Frisby test, it can be used in preverbal children by observing their behavioural response.
The Randot and Random dot E stereotests require polarising glasses for viewing. Images of animals and geometric shapes are horizontally displaced using vectographic techniques. These tests allow fine grading of stereopsis, but not all children will like wearing the polarising glasses.
The TNO test creates a 3D effect by using red‒green anaglyphs. Red‒green anaglyphs are based on two images showing the same scene from a slightly different angle. One image is processed through a red, and the other image through a green or blue or mixed (cyan) filter. The resulting images are superimposed, but slightly offset. When viewing these pictures through glasses with one red and one green lens, a stereoscopic effect results.
Near stereotests are not sufficiently accurate to be used as standalone vision screening tests (Donahue 2013; Huynh 2005; Ohlsson 2002; Schmidt 2003; VIP 2005; VIP 2007). Testability is affected by age (Pai 2012; Schmidt 2003).
Distance stereopsis can be measured with the distance Frisby stereotest, a cabinet which houses Perspex plates which present random images at slightly different distances from the observer (Adams 2005; Holmes 2005; Kaye 2005), or with a distance Randot test (Fu 2006). Despite reports of high sensitivity to detect vision defects (Rutstein 2000), distance stereopsis has not been evaluated in vision screening programmes. Distance stereoacuity can be reduced in convergence excess esotropia and intermittent distance exotropia (Hatt 2008).
Visual acuity tests
Visual acuity (VA) is a measure of the spatial resolution of the visual system. Manifest strabismus causes a loss of VA in one eye by central suppression of the information from the deviating eye. Uncorrected refractive errors and ocular anomalies also cause a reduction in VA.
In older children and adults, VA is assessed by reading a chart of characters, or optotypes, at a defined distance. In very young children, assessment of visual acuity relies on observation of behavioural responses to visual targets.
Preferential looking cards showing patterns of high‐contrast black and white stripes are used in children under the age of 2 years to determine “grating acuity” (Dobson 1978). In strabismic amblyopia, grating acuity is reduced to a lesser degree than linear letter acuity and results may overestimate the level of vision.
From the age of 2 years, single symbols such as Kay pictures can be used (Kay 1983). From the age of 3 years, crowded linear optotypes such as HOTV, or crowded Kay or Lea pictures can be used. These tests are often used in childhood vision screening programmes (Schmidt 2004; Hered 1997; Anonymous 2004). Crowded optotypes (several characters next to each other) viewed one eye at a time (monocularly), such as on HOTV or logMAR charts, are considered the 'gold standard' for visual acuity testing (Schmidt 2004). The use of crowded optotypes instead of single optotypes is particularly important in amblyopia screening, as single optotype testing can overestimate visual acuity. All visual acuity tests can be performed either by the child calling out the name of the picture or letter, or by the child matching the target optotype with a chart held by a parent/guardian. More detailed letter‒optotype tests include the Keeler logMar and the Sonksen Silver logMar tests.
In order to both increase portability of charts and reduce variation of illumination levels, computer‐based testing applications are available and used in some screening settings (Thomson 1999).
Visual acuity tests can be administered by any suitably trained person. In the UK, screening programmes are delivered by qualified orthoptists, health care technicians or school nurses trained by orthoptists (Hall 2003; UK National Screening Committee) In the USA, paediatric vision screening is usually performed by suitably trained nurses or lay screeners.
Autorefractors/Photorefractors
Autorefractors are instruments that measure the refractive state of the eye. Objective devices contain an optical system which determines the vergence of light reflected from the patient’s retina. To avoid inducing accommodation, modern autorefractors use infrared rather than visible light.
Photorefraction analyses the reflection of light emitted from a small flashlight placed close to the camera lens. Three types of photorefraction have been developed: orthogonal, isotropic and eccentric (also called photoretinoscopy). Refractive errors result in certain patterns of photographic appearances, which vary with the degree to which the eye is defocused with respect to the plane of the camera (Howland 1974; Howland 2009). Photorefractors are mainly used to obtain refractive values. Some devices combine a photographic Brückner test and eccentric photorefraction to detect amblyogenic risk factors (Cibis 1994; VanEenwyk 2008). Several current photorefractors also detect strabismus as asymmetry of corneal light reflections (Arnold 2013; Dahlmann‐Noor 2009a; Dahlmann‐Noor 2009b; Moghaddam 2012; Silbert 2013).
The following table summarises possible test outcomes, pass/fail thresholds and examples of published screening studies that have used these tests. The variation of tests used in different studies for each group of index tests means that many specific tests have only been used in one or a small number of studies.
For the purpose of comparison all visual acuity thresholds have been converted to logMar, though this may not be entirely accurate.
|
| Possible measurements | Threshold for diagnosis of manifest strabismus | Use in studies |
| Type 1 tests: |
|
|
|
| Corneal reflection tests |
|
|
|
| Hirschberg test | Categorical: | Any displacement from centre of pupil. |
|
| Cover test (Gold standard) |
|
|
|
| Cover‒uncover test | Dichotomous: refixation movement present/absent. | Any refixation movement. | Traboulsi 2008: manifest ocular deviation of any type or magnitude with or without fixation preference. |
|
|
|
| Friedman 2009: constant or intermittent tropia of any magnitude at distance (6 m) or near (40 cm) fixation; if only testable at one distance and no strabismus on that test: non‐strabismic. |
|
|
|
| Schmidt 2004: at 3 m and 40 cm: strabismus = any heterotropia in primary gaze. |
| Simultaneous prism and cover test | Categorical: | Any use of prism. |
|
| Alternate cover test | Dichotomous: refixation movement present/absent. | Demonstrates manifest plus latent strabismus. | Traboulsi 2008: any vertical phoria; any esophoria more than 8 PD or exophoria more than 15 PD at near or distance. |
| Prism and alternate cover test | Categorical: | Quantifies manifest plus latent strabismus. | Traboulsi 2008: Any vertical phoria; any esophoria more than 8 PD or exophoria more than 15 PD at near or distance. |
| Type 2 test: Tests of binocular function: control and stereoacuity |
|
|
|
| Contour tests: Titmus | Fly 3,600 sec of arc, animals 400, 200, 100, Wirt circles 800, 400, 200, 140, 100, 80, 60, 50, 40 seconds of arc at 40 cm. | Fly 3,600 sec of arc; animals 400, 200, 100; Wirt rings 800 to 40 seconds of arc. | Traboulsi 2008: less than 400 seconds of arc. |
| Random dot stereotests |
|
|
|
| TNO | 480, 240, 120, 60, 30, 15 seconds of arc. | At age 5 years: greater than 60 seconds of arc. | Manufacturer recommends 240 seconds of arc as “fail” threshold, as 95% of amblyopes are unable to see this figure. |
| Lang II | 600, 400, 200 seconds of arc at 40 cm. |
|
|
| Frisby | At 30 cm viewing distance: 600, 300 150 seconds of arc. |
|
|
| Randot | 500 to 20 seconds of arc. | At age 5 years: greater than 60 seconds of arc. |
|
| Random dot E at 0.5, 1 and 1.5 m | Schmidt 2004: non‐stereocard only; 504; 252; 168 arc seconds |
| Schmidt 2004: non‐stereocard only; 504; 252; 168 seconds of arc |
| Stereo Smile II at 40 cm | Schmidt 2004: non‐stereocard only; 480; 240; 120 arc seconds. |
| Schmidt 2004: non‐stereo card only; 480; 240; 120 seconds of arc. |
| Type 3 tests: |
|
|
|
| Single‐surrounded HOTV |
|
|
|
| HOTV at 3 m |
| Schmidt 2004: 4 years: 10/100; 10/25; 10/20; 10/16. |
|
| LEA symbols at 3 m |
| Schmidt 2004: 4 years: 10/100; 10/25; 10/20; 10/16. |
|
| Snellen letters |
|
| Traboulsi 2008: screen fail if visual acuity difference of 2 Snellen lines between eyes or visual acuity less than 0.30 logMar in either eye. |
| Allen figures |
|
| Traboulsi 2008: screen fail if visual acuity difference of 2 Snellen lines between eyes or visual acuity less than 0.30 logMar in either eye. |
| Keeler (previously Glasgow) crowded logMar | |||
| Sonksen | |||
| Crowded Kay Picture Test | |||
| Type 4 tests: |
|
|
|
| Plusoptix Vision Screener | Assessment of corneal reflections (asymmetry in millimetres or ratio). |
|
|
Other tests used in the diagnosis of strabismus, but not in primary care or community screening settings delivered by lay screeners or primary care professionals
Krimsky test
The prism reflection test is a modification of the Hirschberg test. The patient fixes a spotlight at a near position (33 cm). Prisms are placed in front of the fixing eye, with the apex pointing in the direction of the deviation. This shifts the CR towards the centre of the pupil. The prism which positions the CR in the centre of both pupils indicates the angle of deviation (Krimsky 1951). This test is typically used in children or adults who are not cooperative enough to undertake a Prism Cover Test or in cases when the visual acuity is poor and the patient is unable to move the eye to take up fixation. The 95% limit of agreement of inter‐observer variability for the Krimsky test has been reported as 6.1 PD (Yang, 2012). Neutralisation of the deviation with prisms requires orthoptic expertise, and this test is not used by lay screeners or non‐ophthalmic professionals in community screening programmes.
Prism reflection test
The prism reflection test is similar to the Krimsky test, but the prism is placed in front of the deviating eye. Some authors found the prism reflection test to have low accuracy (Choi 1998).
Controlled binocular acuity (CBA) test of strabismus
Some types of strabismus can be controlled by increased accommodation, i.e. 'over‐focusing'. In intermittent distance exotropia (IDEX), individuals may use accommodative convergence to control the exodeviation; hence over‐accommodating and losing clarity of vision in the distance (Walsh 2000). To measure controlled binocular acuity, the patient reads an optotype chart whilst the examiner observes the patient’s ocular alignment by corneal reflections and noting at which optotype size one eye deviates.
Suppression tests
Visual information from the deviating eye is suppressed at the level of the visual cortex of the brain (Smith 1985). Binocular suppression tests may have high specificity and may be useful for strabismus and amblyopia screening (Pott 1998; Simons 1996b). Tests are based on dissociation of the images seen by each eye, for example by using polarised lenses (Nuzzi 1986; Pott 1998; Pott 2003; Prakash 1996). Worth’s four‐light test, Bagolini striated lenses or the synoptophore are used to detect the presence of suppression. The 4‐prism dioptre (PD) prism test is used to detect central suppression. The area of suppression within the field of vision can be approximated by the synoptophore. Density of suppression can be quantified by using neutral density filters or the Sbisa bar (Bagolini filter bar) (McCormick 2002). Whilst used in orthoptic practice to determine the risk of developing double vision in adult patients undergoing amblyopia treatment, suppression measurement is not used in paediatric screening.
Fusion tests
Orthoptists may test children's ability to overcome a 4, 15 or 20 PD prism to maintain binocular single vision (prism reflex test); failure to overcome the prism can indicate weakness of fusional control. The prism fusion range uses the same principle, but uses a prism bar, allowing a more detailed measurement of prisms that can be overcome. Measurements are typically in steps as dictated by prism bar or loose prism used (2 to 20 PD usually in 2 PD increments, then 20 to 45 PD in 5 PD increments).
Blur test
The blur test aims to detect low hypermetropia, which may be associated with potentially decompensating strabismus.
Appendix 3. The Cochrane Library search strategy
#1 MeSH descriptor: [Vision Tests] explode all trees
#2 MeSH descriptor: [Mass Screening] explode all trees
#3 (test* or screen* or diagnos* or assess*) near/4 (vision or visual*)
#4 (test* or screen* or diagnos* or assess*) near/4 program*
#5 (test* or screen* or diagnos* or assess*) near/4 (communit* or population)
#6 (test* or screen* or diagnos* or assess*) near/4 hospital*
#7 (test* or screen* or diagnos* or assess*) near/4 (nursery or preschool* or school*)
#8 (test* or screen* or diagnos* or assess*) near/4 (referred or referal or monit*)
#9 (test* or screen* or diagnos* or assess*) near/4 (orthoptist* or ophthalmologist* or optometrist*)
#10 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9
#11 MeSH descriptor: [Strabismus] explode all trees
#12 strabism* or squint*
#13 esotrop* or exotrop*
#14 hypertrop* or hypotrop*
#15 microtrop*
#16 MeSH descriptor: [Amblyopia] this term only
#17 amblyop*
#18 lazy near/3 eye*
#19 #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18
#20 MeSH descriptor: [Infant] this term only
#21 MeSH descriptor: [Child, Preschool] this term only
#22 MeSH descriptor: [Child] this term only
#23 infan* or child* or toddler* or boy* or girl* or paediatric* or pediatric* or nursery or nurseries or kindergarten* or pre school* or preschool* or school age or schoolage*
#24 #20 or #21 or #22 or #23
#25 MeSH descriptor: [Photogrammetry] this term only
#26 MeSH descriptor: [Photography] this term only
#27 MeSH descriptor: [Blinking] this term only
#28 corneal light reflection*
#29 corneal reflection*
#30 CLRT
#31 (cover or uncover) near/3 test*
#32 fundus reflection*
#33 (Hirschberg* or Krimsky* or Bruckner*) near/5 test*
#34 MeSH descriptor: [Retinoscopy] this term only
#35 retinoscop*
#36 stereoscopy or stereotest*
#37 Randot
#38 random dot
#39 two pencil test
#40 Frisby* or Titmus*
#41 TNO or FD2
#42 HOTV or LEA
#43 suppression near/3 test*
#44 autorefractor* or photorefractor* or Plusoptix or Retinomax
#45 #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44
#46#10 and #19 and #24 and #45
Appendix 4. MEDLINE (Ovid) search strategy
1. exp vision tests/
2. exp mass screening/
3. ((test$ or screen$ or diagnos$ or assess$) adj4 (vision or visual$)).tw.
4. ((test$ or screen$ or diagnos$ or assess$) adj4 program$).tw.
5. ((test$ or screen$ or diagnos$ or assess$) adj4 (communit$ or population)).tw.
6. ((test$ or screen$ or diagnos$ or assess$) adj4 hospital$).tw.
7. ((test$ or screen$ or diagnos$ or assess$) adj4 (nursery or preschool$ or school$)).tw.
8. ((test$ or screen$ or diagnos$ or assess$) adj4 (referred or referral or monit$)).tw.
9. ((test$ or screen$ or diagnos$ or assess$) adj4 (orthoptist$ or ophthalmologist$ or optometrist$)).tw.
10. or/1‐9
11. exp strabismus/
12. (strabism$ or squint$).tw.
13. (esotrop$ or exotrop$).tw.
14. (hypertrop$ or hypotrop$).tw.
15. microtrop$.tw.
16. amblyopia/
17. amblyop$.tw.
18. (lazy adj3 eye$).tw.
19. or/11‐18
20. Infant/
21. child, preschool/
22. child/
23. (infan$ or child$ or toddler$ or boy$ or girl$ or paediatric$ or paediatric$ or nursery or nurseries or kindergarten$ or pre school$ or preschool$ or schoolage$ or school age$).tw.
24. or/20‐23
25. Photogrammetry/
26. Photography/
27. Blinking/
28. corneal light reflection$.tw.
29. corneal reflection$.tw.
30. CLRT.tw.
31. ((cover or uncover) adj3 test$).tw.
32. fundus reflection$.tw.
33. ((Hirschberg$ or Krimsky$ or Bruckner$) adj5 test$).tw.
34. Retinoscopy/
35. retinoscop$.tw.
36. (stereoscopy or stereotest$).tw.
37. Randot.tw.
38. random dot.tw.
39. two pencil test.tw.
40. (Frisby$ or Titmus$).tw.
41. (TNO or FD2).tw.
42. (HOTV or LEA).tw.
43. (suppression adj3 test$).tw.
44. (autorefractor$ or photorefractor$ or Plusoptix or Retinomax).tw.
45. or/25‐44
46. 10 and 19 and 24 and 45
Appendix 5. Embase (Ovid) search strategy
1. exp vision test/
2. exp mass screening/
3. ((test$ or screen$ or diagnos$ or assess$) adj4 (vision or visual$)).tw.
4. ((test$ or screen$ or diagnos$ or assess$) adj4 program$).tw.
5. ((test$ or screen$ or diagnos$ or assess$) adj4 (communit$ or population)).tw.
6. ((test$ or screen$ or diagnos$ or assess$) adj4 hospital$).tw.
7. ((test$ or screen$ or diagnos$ or assess$) adj4 (nursery or preschool$ or school$)).tw.
8. ((test$ or screen$ or diagnos$ or assess$) adj4 (referred or referral or monit$)).tw.
9. ((test$ or screen$ or diagnos$ or assess$) adj4 (orthoptist$ or ophthalmologist$ or optometrist$)).tw.
10. or/1‐9
11. exp strabismus/
12. (strabism$ or squint$).tw.
13. (esotrop$ or exotrop$).tw.
14. (hypertrop$ or hypotrop$).tw.
15. microtrop$.tw.
16. amblyopia/
17. amblyop$.tw.
18. (lazy adj3 eye$).tw.
19. or/11‐18
20. Infant/
21. preschool child/
22. child/
23. (infan$ or child$ or toddler$ or boy$ or girl$ or paediatric$ or pediatric$ or nursery or nurseries or kindergarten$ or pre school$ or preschool$ or schoolage$ or school age$).tw.
24. or/20‐23
25. Eye photography/
26. Medical photography/
27. Photography/
28. Blinking/
29. Hirschberg cornea light reflection test/
30. corneal light reflection$.tw.
31. corneal reflection$.tw.
32. CLRT.tw.
33. ((cover or uncover) adj3 test$).tw.
34. fundus reflection$.tw.
35. ((Hirschberg$ or Krimsky$ or Bruckner$) adj5 test$).tw.
36. Retinoscopy/
37. retinoscop$.tw.
38. (stereoscopy or stereotest$).tw.
39. Randot.tw.
40. random dot.tw.
41. two pencil test.tw.
42. Frisby test/
43. Revised Frisby Davis Distance test/
44. (Frisby$ or Titmus$).tw.
45. TNO stereotest/
46. (TNO or FD2).tw.
47. (HOTV or LEA).tw.
48. (suppression adj3 test$).tw.
49. (autorefractor$ or photorefractor$ or Plusoptix or Retinomax).tw.
50. or/25‐49
51. 10 and 19 and 24 and 50
Appendix 6. CINAHL (EBSCO) search strategy
S34 S28 and S33
S33 S29 or S30 or S31 or S32
S32 infan* or child* or toddler* or boy* or girl* or paediatric* or pediatric* or nursery or nurseries or kindergarten* or pre school* or preschool* or schoolage* or school age*
S31 (MH "Child+")
S30 (MM "Child, Preschool")
S29 (MH "Infant+")
S28 S18 and S27
S27 S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26
S26 lazy N3 eye
S25 amblyop*
S24 (MM "Amblyopia")
S23 microtrop*
S22 hypertrop* or hypotrop*
S21 esotrop* or exotrop*
S20 strabism* or squint*
S19 (MM "Strabismus")
S18 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17
S17 optometrist* N4 (test* or screen* or diagnos* or assess*)
S16 ophthalmologist* N4 (test* or screen* or diagnos* or assess*)
S15 orthoptist* N4 (test* or screen* or diagnos* or assess*)
S14 monit* N4 (test* or screen* or diagnos* or assess*)
S13 referral N4 (test* or screen* or diagnos* or assess*)
S12 referred N4 (test* or screen* or diagnos* or assess*)
S11 school* N4 (test* or screen* or diagnos* or assess*)
S10 preschool* N4 (test* or screen* or diagnos* or assess*)
S9 nursery N4 (test* or screen* or diagnos* or assess*)
S8 hospital* N4 (test* or screen* or diagnos* or assess*)
S7 population N4 (test* or screen* or diagnos* or assess*)
S6 communit* N4 (test* or screen* or diagnos* or assess*)
S5 program* N4 (test* or screen* or diagnos* or assess*)
S4 visual* N4 (test* or screen* or diagnos* or assess*)
S3 vision N4 (test* or screen* or diagnos* or assess*)
S2 (MM "Vision Screening")
S1 (MH "Vision Tests+")
Appendix 7. Web of Science Conference Proceedings Citation Index – Science (CPCI‐S) search strategy
#20 #15 AND #18 AND #19
#19 TS= (infan* or child* or toddler* or boy* or girl* or paediatric* or pediatric* or nursery or nurseries or kindergarten* or pre school* or preschool* or schoolage* or school age*)
#18 #16 OR #17
#17 TS= (esotrop* or exotrop* or hypertrop* or hypotrop* or microtrop*)
#16 TS= (strabimus or strabismic or squint*)
#15 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14
#14 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 optometrist*)
#13 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 ophthalmologist*)
#12 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 orthoptist*)
#11 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 monitor*)
#10 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 referral*)
#9 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 referred*)
#8 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 hospital*)
#7 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 population*)
#6 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 communit*)
#5 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 program*)
#4 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 visual*)
#3 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 vision)
#2 TS=mass screening
#1 TS= vision test
Appendix 8. BIOSIS Previews search strategy
#20 #15 AND #18 AND #19
#19 TS= (infan* or child* or toddler* or boy* or girl* or paediatric* or pediatric* or nursery or nurseries or kindergarten* or pre school* or preschool* or schoolage* or school age*)
#18 #16 OR #17
#17 TS= (esotrop* or exotrop* or hypertrop* or hypotrop* or microtrop*)
#16 TS= (strabimus or strabismic or squint*)
#15 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14
#14 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 optometrist*)
#13 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 ophthalmologist*)
#12 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 orthoptist*)
#11 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 monitor*)
#10 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 referral*)
#9 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 referred*)
#8 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 hospital*)
#7 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 population*)
#6 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 communit*)
#5 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 program*)
#4 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 visual*)
#3 TS= ((test* or screen* or diagnos* or assess*) NEAR/4 vision)
#2 TS=mass screening
#1 TS= vision test
Appendix 9. MEDION search strategy
Database was searched on ICPC code field. Using code "f" for ophthalmology.
Appendix 10. ARIF search strategy
strabismus OR amblyopia
Appendix 11. ISRCTN search strategy
(strabismus OR amblyopia) AND (test OR screen OR diagnosis OR assess)
Appendix 12. ClinicalTrials.gov search strategy
(strabismus OR amblyopia) AND (test OR screen OR diagnosis OR assess)
Appendix 13. ICTRP search strategy
strabismus OR amblyopia = Condition AND test OR screen OR diagnosis OR assess = Intervention
Appendix 14. Glossary
Accommodation: mechanism by which an eye focuses on a near object; accommodation involves contraction of the ciliary muscle, which relaxes the fibres holding the lens inside the eye; the lens then assumes a more rounded shape.
Binocular: seeing with both eyes.
Convergent: appearance of one or both eyes deviated inwards/towards the nose.
Cornea: the clear window at the front of the eye.
Cycloplegic: using pharmacological agents (eyedrops) to paralyse the ciliary muscle in the eye to prevent accommodation when carrying out a test for glasses.
Dioptre (D): the unit of measurement describing the optical power of a lens.
Divergent: appearance of one or both eyes deviated outwards/towards the temple.
Esotropia: appearance of one or both eyes deviated inwards/towards the nose; same as convergent.
Exotropia: appearance of one or both eyes deviated outwards/towards the temple; same as divergent.
Fundus: the structures at the back of the eye which change the visual information from light to electrical signals and transmit them to the brain.
Horizontal: ocular misalignment in the horizontal plane, i.e. the eyes are at the same level, but one or both eyes are deviated towards one side.
Hypermetropia: far‐sightedness.
Latent: strabismus not present when both eyes are open and fixing on a target, but can be demonstrated by interrupting binocular viewing (seeing with both eyes).
Manifest: strabismus present when both eyes are open.
Myopia: short‐sightedness.
Prism dioptre (PD); unit of measurement describing the power of a prism that aligns the eyes.
Refraction: test for glasses.
Strabismus: ocular misalignment.
Vertical: ocular misalignment in the vertical plane, i.e. one eye appears higher or lower than the other.

Study flow diagram.

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study
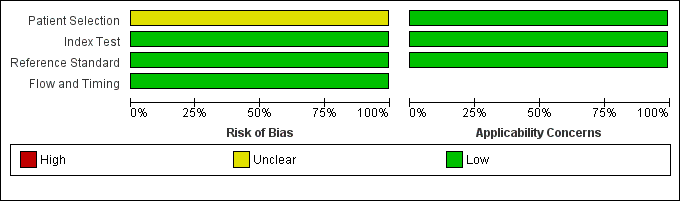
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies

Forest plot of 1 Photoscreener.
| Accuracy of a photoscreener to detect strabismus in the community | ||||||
| Patient/population: children aged 1 to 6 years old Setting: school Index test: plusoptix S04 photoscreener Target condition: constant and intermittent manifest strabismus Reference standard: cover test at distance and near | ||||||
| Number of studies | Number of participants | Number affected by target condition | Sensitivity of test (95% CI) | Specificity of test (95% CI) | Risk of bias based on QUADAS‐2 domains | Comments |
| 271 | 13 | 0.46 (0.19 to 0.75) | 0.97 (0.94 to 0.99) | Unclear risk | Low participation rate of 25% | |
| CI: confidence intervals | ||||||
| Study ID | Arthur 2009 |
| Clinical features and settings | Previous testing and results: unknown. Referral route/selection: all who were screened offered gold standard examination. |
| Participants | Sample size: 306 screened (1343 invited to study (consents sent: this may have introduced selection bias from concerned parents being more likely to return consent forms), 387 returned, 45 excluded as consents too late, 7 excluded for document errors, 28 absent on day of screening, 1 uncooperative), 275 gold standard exam (14 declined, 11 unable to attend within time frame, 6 uncontactable) of which 271 data interpretable for both index and reference (3 photographs unusable, 1 did not complete exam). Socio‐demographic items: 98% 4 to 5 years of age, gender and ethnicity not given, no ocular abnormalities (i.e. media opacities, which would affect test results/technical failure rates). Geographic region: Limestone school district, Ontario, Canada. |
| Study design | Selection: all patients with data available on both index and reference tests as single group. |
| Target condition | Constant and intermittent manifest strabismus (esotropia, exotropia, vertical tropia, microtropia), prevalence of the target condition in the sample: 13 (of 271). |
| Reference standard | Test definition and description: monocular visual acuity with occlusion glasses (crowded Keeler logMAR letter matching test/Crowded Kay pictures/Cardiff cards), cover test at distance and near, ocular movements and convergence, binocular single vision assessment (20D base‐out prism test and/or stereopsis) and red reflex test. Standards: discharged if VA 0.2 logMAR or better, binocular single vision at distance and near and no suspected ocular pathology, 6‐ to 12‐week review and re‐check if borderline, cycloplegic refraction/dilated examination all others. |
| Index tests | plusoptiX S04 photoscreener, co‐axial camera, handheld at 1 m. |
| Follow‐up | How many participants were lost to follow‐up: 31. |
| Notes | Sources of funding: none declared. Anything else of relevance: low participation rate (25%). |
| Study ID | First author, year of publication |
| Clinical features and settings | Previous testing and results. Referral route/selection. |
| Participants | Sample size. Socio‐demographic items: age, gender, ethnicity, frequency of ocular abnormalities (i.e. media opacities, which would affect test results/technical failure rates), geographic region. |
| Study design | Selection: as single group/as separate group with/without target condition. |
| Target condition | Constant and intermittent manifest strabismus (esotropia, exotropia, vertical tropia, microtropia), including the prevalence of the target condition in the sample. |
| Reference standard | Test definition and description, i.e. cover test; 'comprehensive eye examination' (visual acuity, cover test, cycloplegic refraction). |
| Index tests | Test definition and description. |
| Follow‐up | How many participants were lost to follow‐up: unknown. |
| Notes | Sources of funding. Abbreviations. Anything else of relevance. |
| Domain | Yes | No | Unclear |
| PATIENT SELECTION Describe methods of patient selection: Describe included patients (prior testing, presentation, intended use of index test and setting) | |||
| Was a consecutive or random sample of patients enrolled? | Consecutive sampling or random sampling of children according to inclusion criteria. | Non‐random sampling or sampling based on volunteering or referral. | Unclear whether consecutive or random sampling used. |
| Was a case‐control design avoided? | Yes for all studies since case‐control studies are excluded unless nested in cohort studies. | N/A | N/A |
| Did the study avoid inappropriate exclusions? | Exclusions are detailed and felt to be appropriate (systemic disease causing strabismus). Children with known strabismus can be excluded. | Inappropriate exclusions are reported e.g. of children in whom strabismus has been suspected in primary care but not confirmed by trained professionals. | Exclusions are not detailed (pending contact with study authors). |
| Risk of bias: could the selection of patients have introduced bias? | ‐ | ‐ | ‐ |
| Concerns regarding applicability: are there concerns that the included patients do not match the review question? | Inclusion of children in community settings, such as school or screening settings, with no previous diagnosis of any eye disease. | Inclusion of children over the age of 6 years, referred to clinical settings, referred to eye professionals for suspect eye disease, or assessed in commercial settings on a volunteer basis; or previous diagnosis of failed screening test or strabismus. | Unclear inclusion criteria. |
| INDEX TEST Describe the index test and how it was conducted and interpreted | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Test performed "blinded" or "independently and without knowledge of" reference standard results are sufficient and full details of the blinding procedure are not required; or clear temporal pattern to the order of testing that precludes the need for formal blinding. | Reference standard results available to those who conducted or interpreted the index tests. | Unclear whether results are interpreted independently. |
| If a threshold was used, was it pre‐specified? | Many included index tests are based on continuous measures (e.g. eye deviation, stereopsis, refractive error, visual acuity); the study authors declare that the selected cut‐off used to dichotomise data was specified a priori, or a protocol is available with this information. | A study is classified at higher risk of bias if the authors define the optimal cut‐off post hoc based on their own study data. | No information on pre‐selection of index test cut‐off values. |
| Risk of bias: could the conduct or interpretation of the index test have introduced bias? | ‐ | ‐ | ‐ |
| Concerns regarding applicability: are there concerns that the index test, its conduct, or interpretation differ from the review question? | Tests used and testing procedure clearly reported and tests executed by personnel with sufficient training. | Tests used are not validated or study personnel is insufficiently trained. | Unclear tests (e.g. stereopsis‐based tests but does not mention if a validated test is used) or unclear study personnel profile, background and training. |
| REFERENCE STANDARD Describe the reference standard and how it was conducted and interpreted | |||
| Is the reference standard likely to correctly classify the target condition? | Cover‒uncover test performed by trained professionals, e.g. ophthalmologists, optometrists, orthoptists. | Complete eye examination with cover‒uncover test used as reference standard but not only the cover‒uncover test used to judge on strabismus (e.g. visual acuity measure also used). | Complete eye examination used but unclear whether cover‐uncover test used. |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Reference standard performed "blinded" or "independently and without knowledge of" index test results are sufficient and full details of the blinding procedure are not required; or clear temporal pattern to the order of testing that precludes the need for formal blinding. | Index test results available to those who conducted the reference standard; or the index test is part of the reference standard (e.g. visual acuity within a compete ophthalmic examination used as reference standard and visual acuity is also the index test analysed ‒ this will be specific of each analysis). | Unclear whether results are interpreted independently. |
| Risk of bias: could the reference standard, its conduct, or its interpretation have introduced bias? |
|
|
|
| Concerns regarding applicability: are there concerns that the target condition as defined by the reference standard does not match the review question? | Cover‒uncover test used and testing procedure executed by personnel with sufficient training. | Cover‒uncover test used by personnel with inappropriate profile or insufficient training. | Unclear study personnel profile, background and training. |
| FLOW AND TIMING Describe any patients who did not receive the index test(s) and/or reference standard or who were excluded from the 2×2 table (refer to flow diagram): describe the time interval and any interventions between index test(s) and reference standard | |||
| Was there an appropriate interval between index test(s) and reference standard? | No more than three months between index and reference test execution, and no corrective intervention between assessments. | More than three months between index and reference test execution. | Unclear whether test results are executed within three months. |
| Did all patients receive a reference standard? | The verification rate of index test‐positive children is definitely higher than that of negative children (the opposite is unlikely). | All children receiving the index test are verified with the reference standard. | Unclear whether all children receiving the index test are verified with the reference standard. |
| Did all patients receive the same reference standard? | All children are verified with the cover‒uncover test by trained professionals. | Some children, i.e. positive children, are verified with the cover‒uncover test by specialised personnel, while the others are verified by personnel with lower level of training. | Unclear whether all children are verified with the cover‒uncover test by trained professionals. |
| Were all patients included in the analysis? | The number of children included in the study does not match the number in analyses or children with undefined or borderline test results are excluded. However, children in whom one or more index tests are not performed because they are poorly cooperative can be excluded. | The number of children included in the study does not match the number in analyses and children with undefined or borderline test results are excluded from the analyses. | The number of children analysed, but not that included in the study, are reported; or unclear if there were inappropriate exclusions. |
| Risk of bias: could the patient flow have introduced bias? | ‐ | ‐ | ‐ |
| COMPARATIVE STUDIES (MULTIPLE INDEX TESTS) | |||
| Were all tests performed on all patients, or randomly assigned? | All children received all index tests, or tests were randomly assigned. | Not all children received all index tests and the assignment criterion was opportunistic or non‐random (e.g. depending on test availability or type of professional). | Not all children received all index tests and the assignment criterion was unclear. |
| Could the order in which the index tests were used affect the target condition or the interpretation of the alternative tests? | The order of presentation of the index test was random or alternate to avoid fatigue effects; or clear that no fatigue effect can arise. | Several tests are delivered in a fixed order which can cause children to be less compliant with the second or later test. | Unclear order of test presentation. |
| Test type categories | Tests included | Output measure | Threshold to extract data |
| 1) Tests which identify ocular misalignment | 1.1) Corneal reflections tests: Hirschberg, Krimsky (prism reflection test). | Prism dioptres (PD). | 8 PD for horizontal deviations; 1 PD for vertical deviations (no published threshold identified). |
| 2) Test of binocular function: stereopsis | Stereoacuity tests such as contour and random dot stereotests. | Seconds of arc. | 400 seconds of arc. |
| 3) Tests designed to detect reduced ventral vision | 3.1) Visual acuity tests, e.g. HOTV, LEA symbols, Keeler (previously Glasgow) crowded logMAR, Sonksen crowded logMAR, crowded Kay picture test. 3.2) Suppression tests. | LogMAR or logMAR equivalent. | 0.2 logMAR. |
| 4) Automated refraction devices designed to report ocular misalignment | ‐ | Millimetres of asymmetry or corneal reflections. | No published threshold identified. |
| Test | No. of studies | No. of participants |
| 1 Photoscreener Show forest plot | 1 | 271 |


