Colchicina para la prevención de eventos cardiovasculares
Información
- DOI:
- https://doi.org/10.1002/14651858.CD011047.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 27 enero 2016see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Corazón
- Copyright:
-
- Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Design of the study: LGH, MB
Data extraction: LGH, HE, VLG, AA, KKO, DG, AJN, MB
Data analysis: LGH, HE
Interpreation of results:LGH, HE, AJN, MN, MB
Writing the first draft: LGH, HE
Critical revision of the manuscript: All authors
Reading and approval of the final version of the paper: All Authors
Guarantor: LGH
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Heart Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health, UK
Declarations of interest
All authors declare no financial relationships with any organisation that might have an interest in the submitted work in the previous three years.
Mark Nidorf was involved in one of the included studies, which was investigator‐initiated and conducted without external financial support.
All other authors declare no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements
The authors thank Mark A. Berendsen and Nicole Martin for conducting the literature searches, Kübra Özoglu for her excellent administrative support and assistance with literature management, Tiago V. Pereira, Benjamin Kasenda, Cemile Bathelt‐Cicek for assessing studies reported in Portuguese, Chinese, and Turkish. We thank the Cochrane Heart Group for their support in publishing this review. We thank all study investigators for providing helpful information on their studies.
Version history
| Published | Title | Stage | Authors | Version |
| 2016 Jan 27 | Colchicine for prevention of cardiovascular events | Review | Lars G Hemkens, Hannah Ewald, Viktoria L Gloy, Armon Arpagaus, Kelechi K Olu, Mark Nidorf, Dominik Glinz, Alain J Nordmann, Matthias Briel | |
| 2014 Mar 26 | Colchicine for prevention of cardiovascular events | Protocol | Lars G Hemkens, Viktoria L Gloy, Kelechi K. Olu, Alain J Nordmann, Matthias Briel | |
Differences between protocol and review
There were no relevant study protocol deviations.
We prespecified all analyses, with the exception of sensitivity analyses using alternative meta‐analytical models, which we deemed useful when we observed event rates close to 1% (Bradburn 2007). In addition, we analysed the risk of bias in more detail.
Since there were no data specifically for populations without a history of cardiovascular disease events or without established coronary heart disease, but data specifically for participants at high risk for cardiovascular events (secondary prevention of cardiovascular disease events or established coronary heart disease), we focused more specifically on this clinically very relevant population and described the findings for this population in more detail. To be consistent, we also report the subgroup analyses on colchicine dose for all outcomes. The prespecified approach and the analyses remained unchanged.
To reduce the overall number of subanalyses, we dropped the analysis on the type of condition (other than CVD) for which colchicine was given and the analysis including only studies reporting on both a primary outcome indicating potential benefit and adverse events, and we did not evaluate the impact of funding of the primary studies. We conducted sensitivity analyses only when there were at least three studies to be combined.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Anti-Inflammatory Agents [adverse effects, *therapeutic use];
- Cardiovascular Diseases [mortality, *prevention & control];
- Cause of Death;
- Colchicine [adverse effects, *therapeutic use];
- Heart Failure [prevention & control];
- Myocardial Infarction [mortality, prevention & control];
- Randomized Controlled Trials as Topic;
- Risk;
- Stroke [mortality, prevention & control];
Medical Subject Headings Check Words
Humans;
PICO

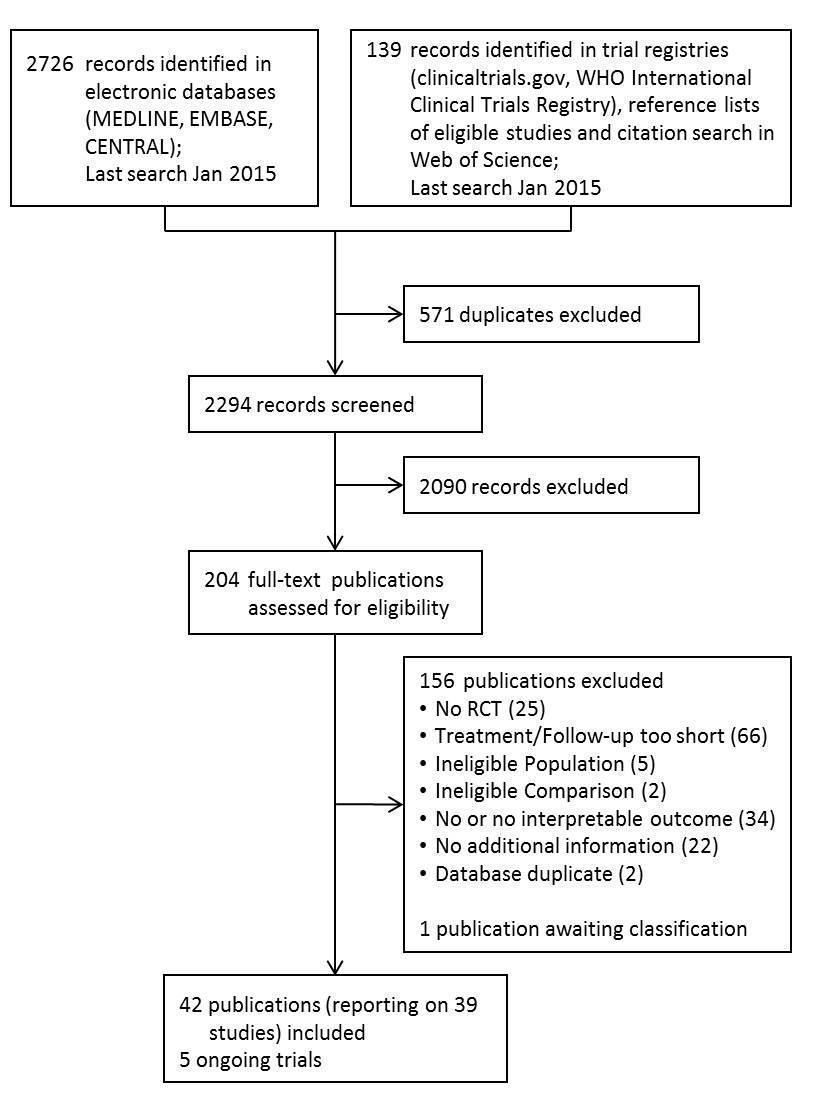
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Funnel plot: Mortality (all‐cause)

Funnel plot: Adverse event (total)

Funnel plot: Adverse event (gastrointestinal)

Overview of results of meta‐analyses for colchicine treatment vs. control
ES: Effect Estimate; OR: Peto Odds Ratio; RR: risk ratio. * including one study without events ** including two studies without events.
Effects for some outcomes were estimated using Peto Odds Ratios because this is a more appropriate method when event rates are very low.

Comparison 1: Colchicine vs control, Outcome 1: Mortality (all‐cause)

Comparison 1: Colchicine vs control, Outcome 2: Myocardial infarction (total)

Comparison 1: Colchicine vs control, Outcome 3: Myocardial infarction (non‐fatal)

Comparison 1: Colchicine vs control, Outcome 4: Myocardial Infarction (fatal)

Comparison 1: Colchicine vs control, Outcome 5: Adverse event (serious)

Comparison 1: Colchicine vs control, Outcome 6: Adverse event (total)

Comparison 1: Colchicine vs control, Outcome 7: Adverse event (gastrointestinal)

Comparison 1: Colchicine vs control, Outcome 8: Mortality (cardiovascular)

Comparison 1: Colchicine vs control, Outcome 9: Stroke (total)

Comparison 1: Colchicine vs control, Outcome 10: Stroke (fatal)

Comparison 1: Colchicine vs control, Outcome 11: Stroke (non‐fatal)

Comparison 1: Colchicine vs control, Outcome 12: Heart failure (total)

Comparison 1: Colchicine vs control, Outcome 13: Heart failure (fatal)

Comparison 1: Colchicine vs control, Outcome 14: Heart failure (non‐fatal)

Comparison 1: Colchicine vs control, Outcome 15: Non‐scheduled hospitalisation (total)

Comparison 1: Colchicine vs control, Outcome 16: Non‐scheduled cardiovascular interventions

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 1: Mortality (all‐cause)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 2: Mortality (cardiovascular)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 3: Myocardial infarction (total)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 4: Myocardial infarction (fatal)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 5: Myocardial infarction (non‐fatal)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 6: Adverse event (total)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 7: Adverse event (gastrointestinal)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 8: Adverse event (serious)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 9: Stroke (total)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 10: Stroke (fatal)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 11: Stroke (non‐fatal)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 12: Heart failure (total)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 13: Heart failure (fatal)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 14: Heart failure (non‐fatal)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 15: Non‐scheduled hospitalisation (total)

Comparison 2: Colchicine vs control: subgroup analysis ‐ colchicine dose fixed ≤ 1 mg/d, Outcome 16: Non‐scheduled cardiovascular interventions

Comparison 3: Colchicine vs control: sensitivity analysis ‐ placebo or other inactive control, Outcome 1: Mortality (all‐cause)

Comparison 3: Colchicine vs control: sensitivity analysis ‐ placebo or other inactive control, Outcome 2: Mortality (cardiovascular)

Comparison 3: Colchicine vs control: sensitivity analysis ‐ placebo or other inactive control, Outcome 3: Myocardial infarction (fatal)

Comparison 3: Colchicine vs control: sensitivity analysis ‐ placebo or other inactive control, Outcome 4: Adverse event (total)

Comparison 3: Colchicine vs control: sensitivity analysis ‐ placebo or other inactive control, Outcome 5: Adverse event (gastrointestinal)

Comparison 4: Colchicine vs control: sensitivity analysis ‐ selection bias (random sequence generation and allocation concealment), Outcome 1: Mortality (all‐cause)

Comparison 4: Colchicine vs control: sensitivity analysis ‐ selection bias (random sequence generation and allocation concealment), Outcome 2: Mortality (cardiovascular)

Comparison 4: Colchicine vs control: sensitivity analysis ‐ selection bias (random sequence generation and allocation concealment), Outcome 3: Myocardial infarction (fatal)

Comparison 4: Colchicine vs control: sensitivity analysis ‐ selection bias (random sequence generation and allocation concealment), Outcome 4: Adverse event (total)

Comparison 4: Colchicine vs control: sensitivity analysis ‐ selection bias (random sequence generation and allocation concealment), Outcome 5: Adverse event (gastrointestinal)

Comparison 5: Colchicine vs control: sensitivity analysis ‐ performance bias (double‐blinded studies), Outcome 1: Mortality (all‐cause)

Comparison 5: Colchicine vs control: sensitivity analysis ‐ performance bias (double‐blinded studies), Outcome 2: Mortality (cardiovascular)

Comparison 5: Colchicine vs control: sensitivity analysis ‐ performance bias (double‐blinded studies), Outcome 3: Myocardial infarction (fatal)

Comparison 5: Colchicine vs control: sensitivity analysis ‐ performance bias (double‐blinded studies), Outcome 4: Adverse event (total)

Comparison 5: Colchicine vs control: sensitivity analysis ‐ performance bias (double‐blinded studies), Outcome 5: Adverse event (gastrointestinal)

Comparison 6: Colchicine vs control: sensitivity analysis ‐ detection bias (blinding of outcome assessment), Outcome 1: Mortality (all‐cause)

Comparison 6: Colchicine vs control: sensitivity analysis ‐ detection bias (blinding of outcome assessment), Outcome 2: Mortality (cardiovascular)

Comparison 6: Colchicine vs control: sensitivity analysis ‐ detection bias (blinding of outcome assessment), Outcome 3: Myocardial infarction (fatal)

Comparison 6: Colchicine vs control: sensitivity analysis ‐ detection bias (blinding of outcome assessment), Outcome 4: Adverse event (total)

Comparison 6: Colchicine vs control: sensitivity analysis ‐ detection bias (blinding of outcome assessment), Outcome 5: Adverse event (gastrointestinal)

Comparison 7: Colchicine vs control: sensitivity analysis ‐ attrition bias (incomplete outcome data), Outcome 1: Mortality (all‐cause)

Comparison 7: Colchicine vs control: sensitivity analysis ‐ attrition bias (incomplete outcome data), Outcome 2: Mortality (cardiovascular)

Comparison 7: Colchicine vs control: sensitivity analysis ‐ attrition bias (incomplete outcome data), Outcome 3: Myocardial infarction (fatal)

Comparison 7: Colchicine vs control: sensitivity analysis ‐ attrition bias (incomplete outcome data), Outcome 4: Adverse event (total)

Comparison 7: Colchicine vs control: sensitivity analysis ‐ attrition bias (incomplete outcome data), Outcome 5: Adverse event (gastrointestinal)

Comparison 8: Colchicine vs control: sensitivity analysis ‐ reporting bias (selective reporting, i.e. abstract publication only), Outcome 1: Mortality (all‐cause)

Comparison 8: Colchicine vs control: sensitivity analysis ‐ reporting bias (selective reporting, i.e. abstract publication only), Outcome 2: Mortality (cardiovascular)

Comparison 8: Colchicine vs control: sensitivity analysis ‐ reporting bias (selective reporting, i.e. abstract publication only), Outcome 3: Myocardial infarction (fatal)

Comparison 8: Colchicine vs control: sensitivity analysis ‐ reporting bias (selective reporting, i.e. abstract publication only), Outcome 4: Adverse event (total)

Comparison 8: Colchicine vs control: sensitivity analysis ‐ reporting bias (selective reporting, i.e. abstract publication only), Outcome 5: Adverse event (gastrointestinal)
| Colchicine compared to any control treatment for prevention of cardiovascular events | ||||||
| Patient or population: any patient population and people with high cardiovascular risk | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Any control treatment | Colchicine | |||||
| Mortality (all‐cause) | 193 per 1000 | 182 per 1000 | RR 0.94 | 4174 | ⊕⊕⊕⊝ | |
| Patients with high cardiovascular risk | ||||||
| 32 per 1000 | 17 per 1000 | RR 0.54 | 1230 | ⊕⊕⊕⊝ | Follow‐up: 0.5 ‐ 3 years | |
| Mortality (cardiovascular) | 27 per 1000 | 9 per 1000 | RR 0.34 | 1132 | ⊕⊕⊕⊝ | |
| Patients with high cardiovascular risk | ||||||
| 31 per 1000 | 8 per 1000 | RR 0.25 | 754 | ⊕⊕⊝⊝ | Follow‐up: 0.5 ‐ 3 years | |
| Myocardial Infarction (total) | 58 per 1000 | 12 per 1000 | RR 0.20 | 652 | ⊕⊕⊕⊝ | Most evidence provided by a single study |
| Patients with high cardiovascular risk | ||||||
| Study population | RR 0.20 | 532 | ⊕⊕⊕⊝ | Evidence provided by a single study. Follow‐up: mean 3 years Please see footnote6 | ||
| 72 per 1000 | 18 per 1000 | |||||
| Assumed 1‐year risk | ||||||
| 25 per 1000 | 6 per 1000 | |||||
| Adverse event (total) | Study population | RR 1.52 | 1313 | ⊕⊝⊝⊝ | No study in participants with high cardiovascular risk reported on total adverse events.9 | |
| 89 per 1000 | 135 per 1000 | |||||
| Assumed 1‐year risk | ||||||
| 89 per 1000 | 135 per 1000 | |||||
| Adverse event (gastrointestinal) | Study population | RR 1.83 | 1258 | ⊕⊕⊝⊝ | Please see footnote9 | |
| 132 per 1000 | 242 per 1000 | |||||
| Assumed 1‐year risk | ||||||
| 132 per 1000 | 242 per 1000 | |||||
| Adverse event (serious) | See comment | See comment | Not estimable | 472 | ⊕⊕⊝⊝ | No illustration of comparative risks due to very uncertain assumed risks10,11 |
| Heart failure (total) | See comment | See comment | RR 0.62 | 426 | ⊕⊕⊝⊝ | No illustration of comparative risks due to very uncertain assumed risks |
| Stroke (total) | See comment | See comment | OR 0.38 | 874 | ⊕⊕⊝⊝ | No illustration of comparative risks due to very uncertain assumed risks |
| *The basis for the assumed risk is the mean control group risk across studies if not otherwise stated in comments/footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Confidence interval is compatible with participant‐relevant benefit and harm. | ||||||
| All Studies | Studies in participants with | |
|---|---|---|
| Total number of studies | 39 (100%) | 4 (100%) |
| No. of participants in all studies | 4992 | 1230 |
| Publication year, median (range) | 1996 (1974 ‐ 2014) | 2013 (1992 ‐ 2014) |
| Publication year < 2000 | 24 (62%) | 1 (25%) |
| Multicentre studies | 9 (23%) | 0 (0%) |
| Study size, median (IQR) | 84 (54 ‐ 129) | 251 (210 ‐ 406) |
| Participant age, median (IQR) | 54 (51 ‐ 61) | 66 (63 ‐ 67) |
| Men, median (IQR) | 62 (25 ‐ 87) | 77 (66 ‐ 88) |
| Follow‐up¹ | ||
| 0.5 to 1 year | 6 (15%) | 3 (75%) |
| 1 to 3 years | 17 (44%) | 0 (0%) |
| > 3 years | 15 (38%) | 1 (25%) |
| Colchicine treatment | ||
| ≤ 1 mg/d | 27 (69%) | 3 (75%) |
| > 1 mg/d | 12 (31%) | 1 (25%) |
| Control treatment, n (%) | ||
| Active treatment | 8 (21%) | 0 (0%) |
| Inactive, placebo | 31 (79%) | 4 (100%) |
| Clinical setting | ||
| CVD, arteriosclerotic | 3 (8%) | 3 (75%) |
| CVD, other | 1 (3%) | 1 (25%) |
| Hepatobiliary disease | 25 (64%) | 0 (0%) |
| Other | 10 (26%) | 0 (0%) |
| Cardiovascular risk profile | ||
| Primary prevention | 0 (0%) | 0 (0%) |
| Secondary prevention | 4 (10%) | 4 (100%) |
| Not specified | 34 (87%) | 0 (0%) |
| Number of studies (% of column total) if not stated otherwise. | ||
| Study | Participants | Centres | Clinical | Age* | Men (%) | Colchicine dose (mg/d) | Control | Follow‐up |
|---|---|---|---|---|---|---|---|---|
| Studies in patients with high cardiovascular risk | ||||||||
| 222 | Single | PCI/CVD | 64 | 65 | 2 x 0.5 | Placebo | 0.5 | |
| 279 | Single | Heart failure | 67 | 67 | 1 ‐ 2 x 0.5² | Placebo | 0.5 | |
| 532 | Single | PCI/CVD | 67 | 89 | 0.5 | Usual care³ | 3 | |
| 197 | Single | PCI/CVD | 61 | 86 | 2 x 0.6 | Placebo | 0.5 | |
| Other studies | ||||||||
| 52 | Single | Liver disease | 54 | 87 | 1⁴ | Placebo | 11 | |
| 90 | Multi | PBC | 55 | 10 | 1 | Placebo⁵ | 3 | |
| 50 | Multi | Other | 68 | 84 | 1 | IFN‐gamma⁶ | 2.1 | |
| 57 | N/R | PBC | 52 | 9 | 2 x 0.6 | Placebo | 2.2 | |
| 180 | N/R. | Liver disease | N/R | N/R | 1 | “Conventional therapy” | 3 | |
| 129 | N/R | Liver disease | N/R | N/R | 1 | Placebo | 3.8 | |
| 555 | N/R | Liver disease | 51 | 70 | 2 x 0.6 | Peg‐IFN‐alpha | 2 | |
| 84 | Single | Other | 54 | 35 | 1 ‐ 2 x 0.5² | Usual care³,⁷ | 1.7 | |
| 120 | Multi | Other | 48 | 46 | 0.5 ‐ 1² | Placebo⁸ | 2 | |
| 240 | Multi | Other | 49 | 50 | 1 ‐ 2 x 0.5² | Placebo | 1.7 | |
| 62 | Single | Liver disease | 54 | 89 | 1⁴ | Placebo | 3.4 | |
| 26 | Single | Other | 68 | 77 | 0.6 ‐ 1.2⁹ | Prednisone | 2.5 | |
| 22 | Single | PBC | 61 | 14 | 1 | Usual care ³,⁵ | 2 | |
| 60 | Single | PBC | N/Rₑ⁰ | 5 | 2 x 0.6 | Placebo | 2 | |
| 87 | Single | PBC | 51 | 6 | 2 x 0.6 | Methotrexateₑₑ | 10 | |
| 28 | N/R | Liver disease | N/R | N/R | 1⁴ | Placebo | 2 | |
| 100 | Single | Liver disease | 51 | 50 | 1⁴ | Placebo | 14 | |
| 101 | Single | Other | 63 | 58 | 2 x 0.6ₑ² | Melphalan/prednisone | 5 | |
| 148 | N/R | Other | 64 | N/R | 2 x 0.6 | Usual care ³,ₑ³ | 9 | |
| 66 | Single | Liver disease | 40 | 88 | 1⁴ | Usual care³ | 4 | |
| 54 | N/R | Other | N/R | N/R | 1 ‐ 2 | Dimethyl sulfoxide | 2 or 7ₑ⁴ | |
| 549 | Multi | Liver disease | 56 | 98 | 2 x 0.6 | Placebo | 6 | |
| 74 | Single | Liver disease | 53 | 62 | 1 | "usual treatment for cirrhosis" | 4 | |
| 38 | Single | Liver disease | 51 | 61 | 1d | Usual care³ | 1 | |
| 84 | Multi | PSC | 42 | 67 | 1 | Placebo | 3 | |
| 41 | Single | Liver disease | 49 | 88 | 1 | Placebo | 1 | |
| 52 | Multi | Other | 53 | 100 | 3 x 0.5 | Placeboₑ⁵ | 0.5 | |
| 74 | Multi | PBC | 54 | 15 | 1⁴ | Placebo⁵ | 2 | |
| 28 | Single | PBC | 54 | 0 | 1 | Placebo⁵ | 2 | |
| 74 | Single | Liver disease | N/R | N/R | 4 x 0.25d | Placebo | 3 | |
| 67 | Single | Liver disease | 52 | 57 | 1 | Placebo | 0.5 | |
| 90 | Multi | Liver disease | 57 | 14 | 2x 0.5 | Placebo | 2 | |
| 100 | Single | Liver disease | 60 | 94 | 1 | Placebo | 2.2 | |
| 64 | Single | PBC | N/R | N/R | 2x 0.5 | Placebo | 1.5 | |
| 116 | Single | Other | 27 | 53 | 2 ‐ 4 x 0.5² | Placebo | 2 | |
| *Age is reported as mean in all studies but three: Antoniou 2006; Kyle 1985; Nikolaidis 2006 reported median age. | ||||||||
| Outcome | Studies (n) | Events (n) | Participants (n) | Summary effect | Heterogeneity (I²), % | Subgroup effect (P value) |
|---|---|---|---|---|---|---|
| Participants with high cardiovascular risk | ||||||
| All‐cause mortality | 4 | 29 | 1230 | RR 0.54 (0.26 to 1.14) | 0% | 0.13 |
| Cardiovascular mortality | 2 | 13 | 754 | RR 0.25 (0.02 to 2.66) | 49% | N/C |
| Myocardial infarction | ||||||
|
| 1 | 22 | 532 | RR 0.20 (0.07 to 0.57) | ‐ | N/C |
|
| 1 | 1 | 532 | RR 0.30 (0.01 to 7.22) | ‐ | N/C |
|
| 1 | 21 | 532 | RR 0.21 (0.07 to 0.61) | ‐ | N/C |
| Stroke | ||||||
|
| 2 | 7 | 754 | OR 0.38 (0.09 to 1.70) | 0% | N/C |
|
| 2 | 1 | 754 | OR 7.26 (0.14 to 365.85) | ‐ | N/C |
|
| 2 | 6 | 754 | OR 0.23 (0.05 to 1.17) | 0% | N/C |
| Heart failure | ||||||
|
| 1 | 3 | 222 | RR 0.14 (0.01 to 2.69) | ‐ | N/C |
|
| 1 | 1 | 222 | RR 0.33 (0.01 to 7.95) | ‐ | N/C |
|
| 1 | 2 | 222 | RR 0.20 (0.01 to 4.05) | ‐ | N/C |
| Hospitalisation | 0 | ‐ | ‐ | ‐ | ‐ | ‐ |
| Cardiovascular intervention | 1 | 9 | 222 | RR 0.79 (0.22 to 2.85) | ‐ | N/C |
| Adverse event, any | 0 | ‐ | ‐ | ‐ | ‐ | N/C |
| Adverse event, gastrointestinal | 2 | 62 | 501 | RR 2.41 (1.43 to 4.06) | 0% | N/C |
| Colchicine dose | ||||||
| All‐cause mortality | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| ≤ 1mg/d | 21 | 268 | 2420 | RR 0.82 (0.67 to 0.99) | 0% | 0.03 |
| > 1mg/d | 9 | 505 | 1754 | RR 1.08 (0.93 to 1.25) | 31% | ‐ |
| Adverse event, any | ||||||
| ≤ 1mg/d | 7 | 60 | 687 | RR 1.75 (0.74 to 4.14) | 40% | 0.75 |
| > 1mg/d | 3 | 87 | 626 | RR 1.47 (0.72 to 2.97) | 73% | ‐ |
| Peto odds ratio for outcomes with event rates between 1% and 5% | ||||||
| All‐cause mortality in participants with high cardiovascular risk | 4 | 29 | 1230 | OR 0.53 (0.25 to 1.11) | 0% | ‐ |
| Cardiovascular mortality | 7 | 17 | 1132 | OR 0.24 (0.09 to 0.64) | 15% | ‐ |
| Mantel‐Haenszel risk ratio without zero correction for outcomes with event rates between 1% and 5% | ||||||
| All‐cause mortality in participants with high cardiovascular risk | 4 | 29 | 1230 | RR 0.54 (0.26 to 1.12) | 0% | ‐ |
| Cardiovascular mortality | 7 | 17 | 1132 | RR 0.20 (0.06 to 0.68) | 0% | ‐ |
| N/C: not calculated | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 1.1.1 Participants with high cardiovascular risk | 4 | 1230 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.26, 1.14] |
| 1.1.2 Other | 26 | 2944 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.84, 1.12] |
| 1.2 Myocardial infarction (total) Show forest plot | 2 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.07, 0.57] |
| 1.2.1 Participants with high cardiovascular risk | 1 | 532 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.07, 0.57] |
| 1.2.2 Other | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.3 Myocardial infarction (non‐fatal) Show forest plot | 2 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.07, 0.61] |
| 1.3.1 Participants with high cardiovascular risk | 1 | 532 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.07, 0.61] |
| 1.3.2 Other | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.4 Myocardial Infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 1.4.1 Participants with high cardiovascular risk | 1 | 532 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.00, 6.04] |
| 1.4.2 Other | 5 | 378 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.35 [0.05, 2.47] |
| 1.5 Adverse event (serious) Show forest plot | 4 | 472 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.5.1 Participants with high cardiovascular risk | 0 | 0 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.5.2 Other | 4 | 472 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.6 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 1.6.1 Participants with high cardiovascular risk | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.6.2 Other | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 1.7 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 1.7.1 Participants with high cardiovascular risk | 2 | 501 | Risk Ratio (M‐H, Random, 95% CI) | 2.41 [1.43, 4.06] |
| 1.7.2 Other | 9 | 757 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [0.82, 3.02] |
| 1.8 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 1.8.1 Participants with high cardiovascular risk | 2 | 754 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.02, 2.66] |
| 1.8.2 Other | 5 | 378 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.09, 3.32] |
| 1.9 Stroke (total) Show forest plot | 3 | 874 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.38 [0.09, 1.70] |
| 1.9.1 Participants with high cardiovascular risk | 2 | 754 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.38 [0.09, 1.70] |
| 1.9.2 Other | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.10 Stroke (fatal) Show forest plot | 4 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.10.1 Participants with high cardiovascular risk | 2 | 754 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.26 [0.14, 365.85] |
| 1.10.2 Other | 2 | 161 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.11 Stroke (non‐fatal) Show forest plot | 3 | 874 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.05, 1.17] |
| 1.11.1 Participants with high cardiovascular risk | 2 | 754 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.05, 1.17] |
| 1.11.2 Other | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.12 Heart failure (total) Show forest plot | 3 | 426 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.10, 3.88] |
| 1.12.1 Participants with high cardiovascular risk | 1 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.69] |
| 1.12.2 Other | 2 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.46, 2.51] |
| 1.13 Heart failure (fatal) Show forest plot | 3 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.13.1 Participants with high cardiovascular risk | 1 | 222 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.00, 6.70] |
| 1.13.2 Other | 2 | 161 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.14 Heart failure (non‐fatal) Show forest plot | 2 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.14.1 Participants with high cardiovascular risk | 1 | 222 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.12] |
| 1.14.2 Other | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 1.15 Non‐scheduled hospitalisation (total) Show forest plot | 2 | 599 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.77, 0.99] |
| 1.15.1 Participants with high cardiovascular risk | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.15.2 Other | 2 | 599 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.77, 0.99] |
| 1.16 Non‐scheduled cardiovascular interventions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.16.1 Participants with high cardiovascular risk | 1 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.22, 2.85] |
| 1.16.2 Other | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 2.1.1 ≤ 1 mg/d | 21 | 2420 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.67, 0.99] |
| 2.1.2 > 1 mg/d | 9 | 1754 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.93, 1.25] |
| 2.2 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 2.2.1 ≤ 1 mg/d | 5 | 955 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.06, 0.82] |
| 2.2.2 > 1 mg/d | 2 | 177 | Risk Ratio (M‐H, Random, 95% CI) | 3.10 [0.13, 73.12] |
| 2.3 Myocardial infarction (total) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.3.1 ≤ 1 mg/d | 1 | 532 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.07, 0.57] |
| 2.3.2 > 1 mg/d | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.4 Myocardial infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 2.4.1 ≤ 1 mg/d | 4 | 733 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.02, 0.87] |
| 2.4.2 > 1 mg/d | 2 | 177 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.66 [0.15, 386.16] |
| 2.5 Myocardial infarction (non‐fatal) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.5.1 ≤ 1 mg/d | 1 | 532 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.07, 0.61] |
| 2.5.2 > 1 mg/d | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.6 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 2.6.1 ≤ 1 mg/d | 8 | 687 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.74, 4.14] |
| 2.6.2 > 1 mg/d | 3 | 626 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [0.72, 2.97] |
| 2.7 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 2.7.1 ≤ 1 mg/d | 9 | 1104 | Risk Ratio (M‐H, Random, 95% CI) | 2.15 [1.26, 3.66] |
| 2.7.2 > 1 mg/d | 2 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.61, 2.19] |
| 2.8 Adverse event (serious) Show forest plot | 4 | 472 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.8.1 ≤ 1 mg/d | 4 | 472 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.8.2 > 1 mg/d | 0 | 0 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.9 Stroke (total) Show forest plot | 3 | 874 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.38 [0.09, 1.70] |
| 2.9.1 ≤ 1 mg/d | 2 | 754 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.38 [0.09, 1.70] |
| 2.9.2 > 1 mg/d | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.10 Stroke (fatal) Show forest plot | 4 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2.10.1 ≤ 1 mg/d | 3 | 795 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.26 [0.14, 365.85] |
| 2.10.2 > 1 mg/d | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.11 Stroke (non‐fatal) Show forest plot | 3 | 874 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.05, 1.17] |
| 2.11.1 ≤ 1 mg/d | 2 | 754 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.23 [0.05, 1.17] |
| 2.11.2 > 1 mg/d | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.12 Heart failure (total) Show forest plot | 3 | 426 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.10, 3.88] |
| 2.12.1 ≤ 1 mg/d | 1 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.01, 2.69] |
| 2.12.2 > 1 mg/d | 2 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.46, 2.51] |
| 2.13 Heart failure (fatal) Show forest plot | 3 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2.13.1 ≤ 1 mg/d | 2 | 263 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.00, 6.70] |
| 2.13.2 > 1 mg/d | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.14 Heart failure (non‐fatal) Show forest plot | 2 | 342 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.12] |
| 2.14.1 ≤ 1 mg/d | 1 | 222 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.12] |
| 2.14.2 > 1 mg/d | 1 | 120 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 2.15 Non‐scheduled hospitalisation (total) Show forest plot | 2 | 599 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.77, 0.99] |
| 2.15.1 ≤ 1 mg/d | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.31, 2.55] |
| 2.15.2 > 1 mg/d | 1 | 549 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.77, 0.99] |
| 2.16 Non‐scheduled cardiovascular interventions Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.16.1 ≤ 1 mg/d | 1 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.22, 2.85] |
| 2.16.2 > 1 mg/d | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 3.1.1 Placebo, inactive control | 26 | 3479 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.84, 1.11] |
| 3.1.2 Active control | 4 | 695 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.41, 1.95] |
| 3.2 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 3.2.1 Placebo, inactive control | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 3.2.2 Active control | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 3.3 Myocardial infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 3.3.1 Placebo, inactive control | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 3.3.2 Active control | 0 | 0 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 3.4 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 3.4.1 Placebo, inactive control | 9 | 725 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [0.90, 2.84] |
| 3.4.2 Active control | 2 | 588 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.41, 4.74] |
| 3.5 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 3.5.1 Placebo, inactive control | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 3.5.2 Active control | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 4.1.1 Low risk | 6 | 1411 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.87, 1.22] |
| 4.1.2 High or unclear risk | 24 | 2763 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.74, 1.11] |
| 4.2 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 4.2.1 Low risk | 2 | 652 | Risk Ratio (M‐H, Random, 95% CI) | 0.09 [0.01, 0.69] |
| 4.2.2 High or unclear risk | 5 | 480 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.15, 2.95] |
| 4.3 Myocardial infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 4.3.1 Low risk | 2 | 652 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.00, 6.04] |
| 4.3.2 High or unclear risk | 4 | 258 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.35 [0.05, 2.47] |
| 4.4 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 4.4.1 Low risk | 3 | 415 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [0.61, 4.04] |
| 4.4.2 High or unclear risk | 8 | 898 | Risk Ratio (M‐H, Random, 95% CI) | 1.54 [0.81, 2.91] |
| 4.5 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 4.5.1 Low risk | 4 | 531 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.59, 2.04] |
| 4.5.2 High or unclear risk | 7 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 2.17 [1.49, 3.17] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 5.1.1 Double‐blind | 22 | 2538 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.07] |
| 5.1.2 Not clearly double‐blind | 8 | 1636 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.82, 1.32] |
| 5.2 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 5.2.1 Double‐blind | 6 | 600 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.15, 2.95] |
| 5.2.2 Not clearly double‐blind | 1 | 532 | Risk Ratio (M‐H, Random, 95% CI) | 0.09 [0.01, 0.69] |
| 5.3 Myocardial infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 5.3.1 Double‐blind | 5 | 378 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.35 [0.05, 2.47] |
| 5.3.2 Not clearly double‐blind | 1 | 532 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.00, 6.04] |
| 5.4 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 5.4.1 Double‐blind | 6 | 581 | Risk Ratio (M‐H, Random, 95% CI) | 1.77 [1.01, 3.12] |
| 5.4.2 Not clearly double‐blind | 5 | 732 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.49, 3.11] |
| 5.5 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 5.5.1 Double‐blind | 9 | 1198 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.98, 3.14] |
| 5.5.2 Not clearly double‐blind | 2 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 5.91 [0.32, 110.47] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 6.1.1 Outcome assessment blinded | 4 | 1582 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.88, 1.25] |
| 6.1.2 Not clearly blinded | 26 | 2592 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.75, 1.09] |
| 6.2 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 6.2.1 Outcome assessment blinded | 3 | 874 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.02, 2.66] |
| 6.2.2 Not clearly blinded | 4 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.09, 3.32] |
| 6.3 Myocardial infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 6.3.1 Outcome assessment blinded | 2 | 652 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.00, 6.04] |
| 6.3.2 Not clearly blinded | 4 | 258 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.35 [0.05, 2.47] |
| 6.4 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 6.4.1 Outcome assessment blinded | 3 | 444 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.58, 1.93] |
| 6.4.2 Not clearly blinded | 8 | 869 | Risk Ratio (M‐H, Random, 95% CI) | 2.07 [1.03, 4.16] |
| 6.5 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 6.5.1 Outcome assessment blinded | 5 | 977 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.77, 2.68] |
| 6.5.2 Not clearly blinded | 6 | 281 | Risk Ratio (M‐H, Random, 95% CI) | 5.06 [0.92, 27.72] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 7.1.1 Low risk | 6 | 1548 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.89, 1.25] |
| 7.1.2 High or unclear risk | 24 | 2626 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.73, 1.09] |
| 7.2 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 7.2.1 Low risk | 3 | 630 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.01, 13.68] |
| 7.2.2 High or unclear risk | 4 | 502 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.07, 2.30] |
| 7.3 Myocardial infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 7.3.1 Low risk | 3 | 630 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.96 [0.06, 15.36] |
| 7.3.2 High or unclear risk | 3 | 280 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.01, 1.18] |
| 7.4 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 7.4.1 Low risk | 2 | 360 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.66, 2.51] |
| 7.4.2 High or unclear risk | 9 | 953 | Risk Ratio (M‐H, Random, 95% CI) | 1.72 [0.89, 3.33] |
| 7.5 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 7.5.1 Low risk | 3 | 639 | Risk Ratio (M‐H, Random, 95% CI) | 1.65 [0.87, 3.16] |
| 7.5.2 High or unclear risk | 8 | 619 | Risk Ratio (M‐H, Random, 95% CI) | 2.18 [0.94, 5.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Mortality (all‐cause) Show forest plot | 30 | 4174 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.82, 1.09] |
| 8.1.1 Full journal publication | 26 | 3303 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.80, 1.09] |
| 8.1.2 Abstract only | 4 | 871 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.58, 1.57] |
| 8.2 Mortality (cardiovascular) Show forest plot | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 8.2.1 Full journal publication | 7 | 1132 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.09, 1.21] |
| 8.2.2 Abstract only | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 8.3 Myocardial infarction (fatal) Show forest plot | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 8.3.1 Full journal publication | 6 | 910 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.05, 1.62] |
| 8.3.2 Abstract only | 0 | 0 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Not estimable |
| 8.4 Adverse event (total) Show forest plot | 11 | 1313 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.93, 2.46] |
| 8.4.1 Full journal publication | 9 | 725 | Risk Ratio (M‐H, Random, 95% CI) | 1.60 [0.90, 2.84] |
| 8.4.2 Abstract only | 2 | 588 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.41, 4.74] |
| 8.5 Adverse event (gastrointestinal) Show forest plot | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 8.5.1 Full journal publication | 11 | 1258 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.03, 3.26] |
| 8.5.2 Abstract only | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |