Psihološke terapije za napadaje panike, sa ili bez agorafobije, u odraslih: mrežna meta‐analiza
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: participants were eligible for the study if they met DSM‐IV diagnostic criteria for panic disorder with or without agoraphobia or were subthreshold for a strict diagnosis of panic disorder but identified panic symptoms as their primary reason for seeking treatment (no subthreshold patient actually entered the study: "seventy‐three percent of participants met criteria for panic disorder with agoraphobia, and 27% met criteria for panic disorder without agoraphobia") Exclusion criteria: participants were excluded if they were seeking treatment for a problem other than panic or anxiety, had an untreated substance‐use problem in the last 6 months, had a diagnosis of psychosis in the past 5 years, were currently judged to be at risk for suicide, or were concurrently involved in other individual psychotherapy. No exclusions were made on the basis of medication use for anxiety or other comorbid psychological or medical problems. Characteristics of the sample:
| |
| Interventions | Participants (n = 80) were randomly assigned to either: 1) Panic control therapy (classified as CBT, n = 38)
2) Treatment as usual (classified as SP, n = 42)
| |
| Outcomes | Time points for assessment: baseline, 5.5 months, 8.5 months, 1 year, 2 years Measures: Panic Disorder Severity Scale (PDSS), Fear Questionnaire (FQ), Beck Depression Inventory (BDI–1), Outcome Questionnaire (OQ–45) The following outcomes were used for quantitative analyses: ST‐Remission: PDSS below a cut‐off score* at 5.5‐month follow‐up ST‐Response: not measured (imputed from continuous scale) ST‐Dropouts: patients who completed fewer than 6 sessions Continuous scale: PDSS at baseline and at 5.5 months LT‐Remission/Response: PDSS below a cut‐off score* at 1 year follow‐up | |
| Notes | * "Cut scores from published norms were obtained for the PDSS (Shear et al., 2001), the OQ–45 (Lambert et al., 1996), the FQ (Gillis, Haaga, & Ford, 1995), and the BDI–1 (Seggar, Lambert, & Hansen, 2002)" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | All randomised patients (n = 80) were assessed at 5.5‐month follow‐up |
| Incomplete outcome data (attrition bias) | Low risk | All randomised patients (n = 80) were assessed at 1‐year follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Low risk | "Ten therapists agreed to participate. None of them identified their primary theoretical orientation as cognitive–behavioral; as a group they were approximately equally distributed between eclectic, family systems, psychodynamic, and humanistic in their self‐described orientation." |
| Treatment fidelity | Low risk | "We rated therapist adherence for 67 of the 80 cases in the study. Data were missing for 11 cases in which the clients did not attend any treatment sessions and 2 cases in which the therapists had audiotaping difficulties. Cases with missing adherence data did not differ from the rest of the sample on any of the primary outcome measures at pre‐ or posttreatment. PCT therapists scored higher than TAU therapists on all of the PCT interventions except for agoraphobic exposure, in which the frequency of use was low with no differences between the treatments." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 60 years, agora‐, social or specific phobic disorder on ICD‐10 criteria for at least a year, mean 4‐phobic‐targets score of greater than 20 on a 0 to 32 scale, written informed consent (patients were told they would be in a research study about the best way to treat their kind of problem) Exclusion criteria: severe organic disease; failed exposure treatment in the last year; more than 2 units of alcohol a day from at least 3 weeks before entering the trial; on medication or on a stable dose of more than the daily equivalent of 5 mg of diazepam, 100 mg imipramine or 10 mg propranolol, taken only at night, for at least 4 months (by when it was unlikely to have any further effect, so this minority was retained to boost cell size) Characteristic of the sample (agoraphobia sub‐sample):
| |
| Interventions | Participants (n = 34) were randomly assigned to either: 1) Daily live self exposure homework + clinician accompanied live exposure (classified as BT, n = 13)
2) Daily live self exposure homework with six negotiation and monitoring sessions (classified as BT, n = 11)
3) Daily self relaxation homework with six negotiation and monitoring sessions (classified as PT, n = 10)
| |
| Outcomes | Time points for assessment: baseline, 8 weeks, 14 weeks, 26 weeks Measures: Fear Questionnaire (FQ), panic frequency, Beck Depression Inventory (BDI), Hamilton Depression (HAM‐D), Global Improvement (CGI‐I), Global Severity (CGI‐S) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured for agoraphobia sub‐sample (imputed from continuous scale) ST‐Dropouts: refusers and dropouts before week 8 Continuous scale: although measured (CGI) detailed data are not reported LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | ST‐Remission not measured: imputed from CGI‐S, which was rated by "an assessor (psychiatrists, psychologists and nurse therapists) kept blind to the treatment condition." |
| Incomplete outcome data (attrition bias) | High risk | 29% of randomised patients (agoraphobia sub‐sample) did not receive/complete the assigned intervention. Dropouts imbalanced in number across the 3 arms. Refusers and dropouts data not reported. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "Both Ee and e patients had the rationale of exposure explained at the 1st session, and were asked to read the self‐help chapter from Living With Fear (Marks IM, 1980) and to follow its guidelines". Marks IM is among the study authors. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Other bias | Unclear risk | Modification of the original sample with replacements. Number and randomisation of replacements not specified. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM–IV diagnosis of one or more anxiety disorders, including panic disorder with or without agoraphobia (PD/A), social anxiety disorder (SAD), specific phobia (SP), obsessive‐compulsive disorder (OCD), or generalised anxiety disorder (GAD) Exclusion criteria: none Characteristic of the sample (agoraphobia sub‐sample):
| |
| Interventions | Participants (n = unclear) were randomly assigned to either: 1) Acceptance and commitment therapy (classified as 3W, n = unclear)
2) Cognitive behaviour therapy (classified as CBT, n = unclear)
| |
| Outcomes | Time points for assessment: pre‐treatment, post‐treatment, 6 months follow‐up, 12 months follow‐up Measures: Anxiety Disorders Interview Schedule–IV (ADIS–IV), Anxiety Sensitivity Index (ASI), Penn State Worry Questionnaire (PSWQ), Fear Questionnaire (FQ), Main Target Phobia Scale (a single‐item avoidance rating for each participant's "main phobia"), Quality of Life Inventory (QOLI), Acceptance and Action Questionnaire–16 (AAQ) The following outcomes were used for quantitative analyses: ST‐Remission: although reported (Clinical Severity Rating on ADIS‐IV lower than 4), ST‐Remission could not be calculated following an ITT principle (number of PD/A patients randomised to each arm not specified) ST‐ Response: not measured ST‐Dropouts: not measured Continuous scale: ASI at pre‐ and post‐treatment LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization sequences were produced by http://www.randomizer.org" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "One hundred and forty‐three participants [...] were randomized to ACT (n=65) or CBT (n=78). All participants who began treatment (n=128) were included in the intent‐to‐treat (ITT) sample (n 57=ACT, n=71 CBT)". Data for randomised patients who did not begin treatment unavailable. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Unclear risk | "CBT for anxiety disorders followed a protocol authored by Craske"; "ACT for anxiety disorders followed a manual authored by Eifert and Forsyth". Both Craske MG and Eifert GH are among the study authors: although possible, the direction of a researcher allegiance bias would be unclear. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "All sessions were videotaped for supervision purposes with a hidden video camera; sessions were also audiotaped for therapy adherence purposes with a discrete digital recorder. Videos were generally played in supervision sessions or watched beforehand by supervisors." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 17 and 70 years, primary DSM‐III‐R diagnosis of panic disorder with no or mild agoraphobic avoidance, panic disorder for at least 3 months, at least one panic attack during the previous 4 weeks, asking for treatment of panic disorder. No use of serotonergic antidepressants or benzodiazepines (for at least 4 weeks; patients using this medication were, if they agreed, taken off medication), or if unwilling to stop medication, keeping this medication at a constant level during treatment or stopping it during treatment. Exclusion criteria: depressive disorder preceding the current episode of panic disorder or requiring immediate treatment; behaviour therapy received for panic disorder; evidence of organic mental disorders, mental retardation, psychotic disorders, alcohol or drug dependence, cardiovascular disease, asthma, epilepsy; medical contraindication for exposure, behavioural experiments or hyperventilation. Characteristic of the sample:
| |
| Interventions | Participants (n = 69) were randomly assigned to either: 1) Cognitive therapy (classified as CT, n = unclear)
2) Interoceptive exposure (classified as BT, n = unclear)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment (16 weeks), 1‐month follow‐up, 6 months follow‐up Measures: panic diary, Fear of Fear Questionnaire, Fear Questionnaire (FQ), State–Trait Anxiety Inventory (STAI), Symptom Check List (SCL‐90) The following outcomes were used for quantitative analyses: ST‐Remission: although measured (panic‐free at post‐treatment), data cannot be used to calculate remission following an ITT principle (n randomised for each arm is unclear) ST‐ Response: not measured ST‐Dropouts: detailed data are not reported Continuous scale: although measured, detailed data are not reported LT‐Remission/Response: although measured (panic‐free at 6 months follow‐up) detailed data are not reported | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | High risk | Study protocol unavailable. Pre‐planned measures are not reported with sufficient details. |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "There were weekly supervisions, during which each case was presented in detail and adherence to the protocol was checked. Care was taken to exclude cognitive techniques from the IE treatment, and exposure techniques from the CT treatment." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM III‐R diagnosis of panic disorder with mild or no agoraphobic avoidance. The interviewers rated the severity of the disturbance on a 0 to 8‐point scale (reflecting co‐jointly distress and disability from the disorder), and only clients whose severity rating was at least 4 were included in the study. Finally, only subjects who reported the presence of at least 1 panic attack in a 2‐week period prior to assessment were included. Subjects on medications or receiving alternative psychotherapies for the requisite time, and who met suitability criteria, were included under the agreement that medication regime and psychotherapy contact were maintained at constant levels throughout. Exclusion criteria: aged below 18 or above 65 years; current alcohol or drug dependency/abuse; primary diagnosis of major depression, and any signs of psychosis or organic brain syndrome. In addition, clients concurrently involved in other psychotherapy programs were assessed for suitability only if the alternative therapy was not focused on anxiety management, and they had been in therapy for at least 6 months. Finally, subjects were excluded if they had begun benzodiazepines within the past 3 months or MAO inhibitors or tricyclic antidepressants within the past 6 months. Characteristic of the sample:
| |
| Interventions | Participants (n = 71) were randomly assigned to either: 1) Wait list (classified as WL, n = 16)
2) Applied progressive muscle relaxation (classified as PT, n = 15)
3) Exposure and cognitive restructuring (classified as CBT, n = 16)
4) Relaxation combined exposure and cognitive restructuring (classified as CBT, n = 24)
| |
| Outcomes | Time points for assessment: assessments were conducted at pre‐treatment and post‐treatment. Active treatment group subjects were also assessed 3 months, 6 months, 12 months and 24 months after treatment completion. Measures: Anxiety Disorder Interview Schedule‐Revised (ADIS‐R), Trait Scale of the State‐Trait Anxiety Inventory (STAI‐T), Cognitive‐Somatic Anxiety Questionnaire, Fear Questionnaire (FQ), Beck Depression Inventory (BDI), Psychosomatic Rating Scale, Subjective Symptom Scale, self monitoring records (regarding daily fluctuations in anxiety and depression and occurrence of panic attacks), composite criteria for treatment responder (20% improvement in at least 3 of the following 4 measures: (1) clinical rating of severity (at least 2 points); (2) client's self rating from the Fear Questionnaire (at least 2 points); (3) number of panic attacks per week, and (4) Subjective Symptom Scale total score (at least 8 points) and End‐State Functioning (applied only to treatment responders. At least three of the following five criteria had to be obtained for high end‐state status: (1) score of 2 or less on the clinician's rating of severity; (2) score of 2 or less for the client's self rating; (3) 0 panic attack per week; (4) score of 2 or less for the mean anxiety rating, and (5) score of 10 or less for the Subjective Symptom Scale total score). The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* at post‐treatment ST‐ Response: treatment responder as defined by composite criteria ST‐Dropouts: subjects who did not complete assigned treatment Continuous scale: Fear Questionnaire (FQ) LT‐Remission/Response: reported data were not included in the analyses because of high level of dropouts (see Secondary outcomes): "data were available for 23 subjects at the 6‐month follow‐up period (R n=9; E&C n=8; COMB n=6)" | |
| Notes | * "At least three of the following five criteria had to be obtained for high end state status: (1) score of 2 or less on the clinician's rating of severity; (2) score of 2 or less for the client's selfrating; (3) zero panic attack per week; (4) score of 2 or less for the mean anxiety rating, and (5) score of 10 or less for the Subjective Symptom Scale total score. End state functioning was determined if data from only three different measures were present but all three reflected positive or negative responding. End state status could not be determined if more than two of the five measures were missing." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | At least 3 out of 5 criteria had to be obtained for high end‐state status. Although assessor was a "blind, independent rater", only one of those 5 criteria was assessor‐rated, so it was possible for a patient to fall into the end‐state category on the basis of self rated measures only. |
| Incomplete outcome data (attrition bias) | High risk | "The percentage of dropouts for each condition were 6%, 33%, 6%, and 17%. For the study completers, data were missing at post‐test for several variables due to non‐compliance. The number of missing data points ranged from 1 to 4 variables within each group. Missing data were not replaced by averages." |
| Incomplete outcome data (attrition bias) | High risk | "data were available for 23 subjects at the 6‐month follow‐up period (R n=9; E&C n=8; COMB n=6)." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Barlow DH and Craske MG are authors of a CBT manual (see Barlow 2000b) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "Treatment delivery was examined by means of ratings of the content of therapy sessions from periodic spot checks of audiotapes (all therapy sessions were audiotaped to avoid the possibility of response bias in the therapists verbal behavior during spot checking). Thirty‐five tapes were randomly selected, with the stipulation that each therapist and each treatment phase of each treatment condition were represented in the sample. Two randomly selected five minute segments (excluding the first and last five minutes of the session and including at least three minutes of therapist talk) were rated from each tape. In all cases, raters identified correctly the treatment condition represented by the sample. Judgments of the treatment phase from which the sample came were correct in 31 of the 35 cases; two misjudgements were from the E & C condition and two from the R condition. There were only two instances of inappropriate material; both of which referred to nontargeted problem areas and not to inappropriate treatment technique." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: not specified, probably DSM‐III diagnosis of panic disorder (as in another previous study by Ottaviani and Beck described in the book) Exclusion criteria: not specified Characteristic of the sample:
| |
| Interventions | Participants (n = 29) were randomly assigned to either: 1) Cognitive therapy (classified as CBT, n = 13)
2) Brief supportive therapy (classified as APP, n = 16)
| |
| Outcomes | Time points for assessment: baseline, 4 weeks, 8 weeks, 12 weeks (only for cognitive therapy group) Measures: panic frequency The following outcomes were used for quantitative analyses: ST‐Remission: not measured (not imputed because of skewed distribution of available continuous scale) ST‐ Response: not measured (not imputed because of skewed distribution of available continuous scale) ST‐Dropouts: non‐completers Continuous scale: although measured (panic frequency), detailed data are not reported LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | "There were no dropouts in either group". |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Beck AT is involved in conceptualisation of cognitive therapy (see Description of the intervention) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial, cross‐over design | |
| Participants | Inclusion criteria: age between 18 and 65 years, DSM‐III diagnosis of panic disorder or agoraphobia with panic disorder Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 33) were randomly assigned to either: 1) Focused cognitive therapy (classified as CT, n = 17)
2) Brief supportive psychotherapy (classified as WL*, n = 16)
| |
| Outcomes | Time points for assessment: baseline, 4 weeks, 8 weeks, 12 weeks (only for focused cognitive therapy group) Measures: panic frequency, Mobility Inventory for Agoraphobia (MI), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Specific Fear Inventory, end‐state functioning (only for focused cognitive therapy group) The following outcomes were used for quantitative analyses: ST‐Remission: absence of panic attacks (clinician rating, before cross‐over) ST‐ Response: not measured (not imputed) ST‐Dropouts: non‐completers (before cross‐over) Continuous scale: not extracted (number of assessed patients unclear: "Ns varied across analyses from 14 to 17 patients in the cognitive therapy group and 15 to 16 patients in the brief supportive psychotherapy group") LT‐Remission/Response: not measured | |
| Notes | *Brief supportive psychotherapy arm was classified as WL (wait list) because: 1) patients received "8 weeks of supportive contact", apparently different from a proper supportive therapy (which therefore cannot be classified as an active treatment, but rather as a comparator intervention); 2) although this study is presented as having a cross‐over design, only patients in supportive psychotherapy group (all of them) actually did cross‐over. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | "At each assessment interval, independent clinical raters reviewed patients’ daily logs of panic frequency to determine whether the recorded panic attacks actually met the DSM‐III criteria for panic". It is unclear whether raters were blind to patients' allocation. |
| Incomplete outcome data (attrition bias) | High risk | "Because of missing values for some variables, Ns varied across analyses from 14 to 17 patients in the cognitive therapy group and 15 to 16 patients in the brief supportive psychotherapy group" |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Beck AT is involved in conceptualisation of cognitive therapy (see Description of the intervention) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age 18 to 65 years, DSM‐III primary diagnosis of panic disorder. Patients who reported use of psychotropic medication were withdrawn from these regimes, with at least a 2‐week drug clearance before taking the ADIS‐R. Exclusion criteria: severe agoraphobia, primary diagnosis of an alternate Axis I diagnosis, current involvement in psychotherapy, alcohol or substance abuse within the previous 6 months, psychotic symptoms, evidence of organic impairment. Characteristic of the sample:
| |
| Interventions | Participants (n = 64) were randomly assigned to either: 1) Cognitive therapy (classified as CT, n = 22)
2) Relaxation training (classified as PT, n = 20)
3) Minimal contact control (classified as NT, n = 22)
| |
| Outcomes | Time points for assessment: baseline, 5 weeks, 10 weeks. Subjects in the 2 intervention groups were asked to return for 1‐, 3‐ and 6‐months follow‐up visits. Measures: panic frequency, Anxiety Disorders Interview Schedule‐Revised (ADIS‐R), Anxiety Sensitivity Index (ASI), Body Sensations Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ), State‐Trait Anxiety Inventory (STAI), Fear Questionnaire (FQ), Hamilton Anxiety and Depression Scales (HAM‐A, HAM‐D), composite index of treatment response (based on 4 variables: global PD severity, number of panic attacks in the previous month, average ACQ and BSQ score, FQ‐Ag score). The following outcomes were used for quantitative analyses: ST‐Remission: panic‐free at post‐test (10 weeks) ST‐ Response: at least mild improvement on composite index of treatment response* ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: panic‐free at 6 months follow‐up | |
| Notes | * "A composite index of treatment response was derived, using guidelines established by Himadi, Boice, and Barlow (1986) and Barlow et al. (1989). This measure quantified treatment response based on four variables: global PD severity, number of panic attacks in the previous month, an average of ACQ and BSQ scores, and FQ‐Ag score". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "Six subjects dropped out, with 5 (23%) from the CT condition, 1 (5%) from the RT condition, and none (0%) from the MCC condition". |
| Incomplete outcome data (attrition bias) | High risk | "Of the 17 subjects who completed CT, 16 (94%) were assessed at all three follow‐up points, with 1 subject not assessed at 3 and 6 months. All 19 RT subjects were evaluated at each follow‐up assessment". |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapies under study (note that first author is Beck JG, not Beck AT). |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "We provided weekly clinical supervision for each session to ensure treatment competence. All sessions were videotaped, with 24% (n=34) selected randomly for treatment integrity monitoring" |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age 18 to 60 years, primary panic disorder with or without agoraphobia according to DSM‐IV criteria, fluency in the German language, living in the proximity of Mainz. Psychotropic medication, if present, had to be held constant. Exclusion criteria: psychosis, bipolar disorder, borderline or antisocial personality disorder, active substance abuse, severe medical or neurological disease precluding exposure therapy and ongoing psychotherapy. Characteristic of the sample:
| |
| Interventions | Participants (n = 54) were randomly assigned to either: 1) Panic focused psychodynamic therapy (classified as PD, n = 36)
2) Cognitive behaviour therapy (classified as CBT, n = 18)
| |
| Outcomes | Time points for assessment: baseline, treatment termination, 6 months follow‐up Measures: Structured Clinical Interview for DSM‐IV (SCID‐I and II), Panic Disorder Severity Scale (PDSS), Clinical Global Impression scale (CGI), Hamilton Depression Rating Scale (HAM‐D), Symptom Checklist (SCL‐90R), Beck Depression Inventory (BDI), Levels of Emotional Awareness Scale (LEAS) The following outcomes were used for quantitative analyses: ST‐Remission: PDSS score < 5 in PD or < 7 in PDA at termination ST‐ Response: at least 40% reduction of PDSS ST‐Dropouts: non‐completers Continuous scale: Panic Disorder Severity Scale (PDSS) LT‐Remission/Response: PDSS score < 5 in PD or < 7 in PDA at 6 months follow‐up | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "subjects were allocated by an a priori computer‐generated list in a 2: 1 randomization ratio either to Panic Focused Psychodynamic Psychotherapy or to manualized cognitive behavioral therapy plus exposure." |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | "Independent, experienced evaluators, blinded to subject condition and therapist orientation, assessed subjects at baseline, at treatment termination and at 6 months follow‐up." |
| Incomplete outcome data (attrition bias) | High risk | Patients analysed at post‐treatment: PFPP n = 28 CBT n = 14 |
| Incomplete outcome data (attrition bias) | High risk | Patients analysed at follow‐up: PFPP n = 25 CBT n = 13 |
| Selective reporting (reporting bias) | High risk | Study protocol available (registered retrospectively). Reported primary outcome is one among other primary outcomes cited in the protocol: "Principal outcome criterion is the reduction of panic‐related symptoms at the follow‐up 6‐months after treatment. Panic‐related symptoms are measured with standardized questionnaires and interviews, e. g. the AKV‐MI/BSQ/ACQ questionnaires, the Hamilton Anxiety Scale, HAMA, and the Panic Disorder Severity scale, PDSS." |
| Researcher allegiance | High risk | Milrod B is co‐author of PFPP manual (see Milrod 1997) |
| Therapist allegiance | Unclear risk | Insufficient information provided |
| Treatment fidelity | Low risk | "All treatments were videotaped as a basis for supervision and for later independent assessment of treatment adherence" |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: 18 years of age or older, met DSM‐IV (American Psychiatric Association, 2000) criteria for the diagnosis of PDA as principal diagnosis and, in the case of taking medication for PDA, did not increase or modify the kind of medication during the study. Exclusion criteria: psychosis, severe organic illness or substance abuse or dependence Characteristic of the sample:
| |
| Interventions | Participants (n = 37) were randomly assigned to either: 1) In vivo exposure (classified as CBT, n = 12)
2) Virtual reality exposure (classified as CBT, n = 12)
3) Wait list (classified as WL, n = 13)
| |
| Outcomes | Time points for assessment: pre‐treatment, post treatment, 12 months follow‐up Measures: Anxiety Diagnostic Interview Schedule IV (ADIS‐IV), Fear and Avoidance Scales, panic attack record, Panic Disorder Severity Scale (PDSS), Anxiety Sensitivity Index (ASI), Agoraphobia Subscale of the Fear Questionnaire (FQ‐Ag), Beck Depression Inventory (BDI), Maladjustment Scale (MS), Clinician Global Impression (CGI) The following outcomes were used for quantitative analyses: ST‐Remission: ASI score < 27 ST‐ Response: panic‐free OR a 50% reduction in panic frequency ST‐Dropouts: non‐completers Continuous scale: Panic Disorder Severity Scale (PDSS) LT‐Remission/Response: not entered in the analyses (reported LT data refer to the 2 treatment arms, both classified as CBT in this review: comparison not feasible) | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table was used (personal communication) |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed by an experimenter who did not participate in the study (personal communication) |
| Blinding of outcome assessment (detection bias) | High risk | Assessors were blind to the conditions (personal communication). However, ASI (used to determine ST‐Remission) is a self administered scale. |
| Incomplete outcome data (attrition bias) | Low risk | "All participants in the treatment conditions were assessed at post treatment 1 week after the treatment completion" |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Authors involved in the developing of virtual reality exposure treatment for panic disorder ("This finding has encouraged us to design a VRE treatment for PDA. Our VR programme for PDA includes several VR scenarios") |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "The therapists were well trained in CBT programmes for PDA. Treatment adherence across the therapists was ensured by a specific training in the treatment programmes. Also, the complete team held weekly meetings to supervise the ongoing treatment of all patients" |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 65 years, DSM‐III‐R diagnosis of panic disorder with or without agoraphobia, at least 1 panic attack in the month preceding the intake evaluation Exclusion criteria: actively psychotic, immediate suicidal or homicidal risk, current abuse of any substance, brain‐damage, in the manic phase of a bipolar disorder without medication Characteristic of the sample:
| |
| Interventions | Participants (n = 48) were randomly assigned to either: 1) Focused cognitive therapy (classified as CBT, n = unclear)
2) Standard cognitive therapy (classified as CT, n = unclear)
| |
| Outcomes | Time points for assessment: baseline, termination, 6 months follow‐up, 12 months follow‐up Measures: panic frequency, Hamilton Anxiety Rating Scale‐Revised (HARS‐R), Hamilton Rating Scale for Depression‐Revised (HRSD‐R), Beck Anxiety Inventory (BAI), Beck Depression Inventory (BDI), Agoraphobic Cognition Questionnaire (ACQ), Panic Belief Questionnaire (PBQ) The following outcomes were used for quantitative analyses: ST‐Remission: although reported (panic‐free at termination), ST‐Remission could not be calculated following an ITT principle (number of patients randomised to each arm not specified) ST‐ Response: not measured (not imputed) ST‐Dropouts: not measured Continuous scale: panic frequency LT‐Remission/Response: although reported (panic‐free at 12 months follow‐up), ST‐Remission could not be calculated following an ITT principle (number of patients randomised to each arm not specified) | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "Forty‐eight subjects initially agreed to participate in the study and 40 patients successfully completed the study through the l‐year follow‐up period. Of eight patients who dropped out of the study, one patient was hospitalized for medical reasons after receiving five SCT sessions, one patient failed to complete a significant portion of the outcome measures at several assessment points, one patient decided to pursue pharmacotherapy exclusively for panic disorder, three patients decided to pursue alternative psychotherapy interventions, and two patients dropped out of the study for unknown reasons." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "Focused cognitive therapy for panic disorder was developed from a theoretical model of panic disorder (Beck, Emery, & Greenberg, 1985; Clark, 1986)." Beck AT is among the study authors. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | High risk | "Results of tape ratings indicated that all therapists addressed catastrophic interpretations according to protocol for the 21 patients in the FCT group. However, protocol violations were noted for 8 of the 19 patients who received SCT." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: females, primary DSM‐III diagnosis of agoraphobia. Patients were instructed not to change their medication during the trial. Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 39) were randomly assigned to either: 1) Exposure (classified as BT, n = 20)
2) Cognitive behaviour therapy (classified as CBT, n = 19)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 6 months follow‐up Measures: Fear Questionnaire (FQ), Agoraphobia Questionnaire, Spielberger Trait Anxiety Inventory (STAI), Beck Depression Inventory (BDI), behavioural test, Agoraphobic Cognitions Questionnaire (ACQ), Anxiety Scale of the Cognitions Checklist (CCLAS), Probability Questionnaire (PQ), Evaluation Questionnaire (EQ) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | ACQ (used to determine ST‐Remission) is a self administered scale |
| Incomplete outcome data (attrition bias) | High risk | "Thirteen participants dropped out of treatment." Reported data refer to treatment completers. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapies under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "CBT session and a tape of an Exp session from each therapist to send to an independent assessor not involved in the trial. The assessor had been trained to teach CT at the Center for Cognitive Therapy, Philadelphia and she teaches a specialist training course in CT in the UK.' A table of random numbers was used to select which of each therapist's CBT and Exp tapes were sent to the assessor. The total sample of tapes came to 18 (10 CBT and eight Exp)." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: African American population, DSM‐IV diagnosis of panic disorder with agoraphobia Exclusion criteria: any psychotic disorder, current substance abuse or dependence, significant suicidal ideation/gestures, any comorbid condition receiving a clinical severity rating equal to or greater than that assigned the panic disorder diagnosis Characteristic of the sample:
| |
| Interventions | Participants (n = 32) were randomly assigned to either: 1) Panic control treatment (classified as CBT, n = 17)
2) Wait‐list control(classified as WL, n = 15)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment Measures: Structured Clinical Interview for DSM‐IV Axis I Disorders (ADIS‐IV), Anxiety Sensitivity Index (ASI), State‐Trait Anxiety Inventory (STAI), Beck Depression Inventory (BDI), Beck Depression Inventory (BDI), The Hyperventilation Questionnaire ‐ Cognitive Subscale (HQC), The Mobility Inventory (MI), African American Acculturation Scale ‐ Short Form (AAAS), Attitude Toward Treatment Questionnaire (ATQ) The following outcomes were used for quantitative analyses: ST‐Remission: recovery (based on ASI)* ST‐ Response: improvement + recovery (based on ASI)* ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: not measured | |
| Notes | * "To assess clinically significant change, the method described by Jacobson and Truax (1991) was employed. For each dependent variable (except the HQC) for which there were established cutoff scores and test–retest reliability statistics, the level of functioning following therapy for each patient was examined and judged whether it was closer to the mean of a functional population than it was to the dysfunctional population. As suggested by Jacobson and Truax (1991), a reliable change (RC) index was computed for each group to assess whether fluctuations were likely the result of imprecise measurement. Each patient was categorized as recovered (score closer to the mean of the functional than dysfunctional group and RC greater than 1.96), improved but not recovered (score closer to the mean of the functional group, but the change noted did not exceed the RC cutoff of 1.96), or unimproved." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | ASI (used to determine ST‐Remission) is a self administered scale |
| Incomplete outcome data (attrition bias) | High risk | "Three of the 17 treatment patients were classified as non‐completers. Of the 15 assigned to the wait‐list condition, 4 did not return for the second evaluation (26.6% attrition). We report the data from the remaining 25 patients who completed either treatment or the wait‐list assessment." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | "The lead therapist for all groups was a licensed clinical psychologist who is an African American male with 15 years experience with cognitive behavioral therapy for anxiety disorders." |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age 18 to 60 years, DSM‐III‐R diagnosis of panic disorder with no, mild or moderate agoraphobic avoidance, current episode duration at least 6 months (this criterion was intended to minimise spontaneous remission, at least 3 panic attacks in the last 3 weeks, consider panic their main problem, willing to accept random allocation. Exclusion criteria: depressive disorder severe enough to require immediate psychiatric treatment; cognitive therapy, applied relaxation or imipramine in the current episode; evidence of organic mental disorder, schizophrenia, alcohol or drug dependence, cardiovascular disease, asthma, epilepsy; pregnancy or intention to become pregnant. Concurrent Axis II personality disorder was not a reason for excluding patients unless personality disorder was clearly the primary problem. Characteristic of the sample:
| |
| Interventions | Participants (n = 72) were randomly assigned to either: 1) Cognitive therapy + in vivo exposure (classified as CBT, n = 17, n = 21 after re‐randomisation of WL patients)
2) Applied relaxation + in vivo exposure (classified as BT, n = 17, n = 21 after re‐randomisation of WL patients)
3) Imipramine + in vivo exposure (not included in this review, n = 22, n = 26 after re‐randomisation of WL patients)
4) Wait list (classified as WL, n = 16; after waiting period, 12 patients were re‐randomised to 1 of the 3 active treatments)
| |
| Outcomes | Time points for assessment: baseline, 3 months follow‐up, 6 months follow‐up, 15 months follow‐up Measures: panic frequency, panic‐related distress/disability, Beck Anxiety Inventory (BAI), Hamilton Anxiety Rating Scale (HARS), Fear Questionnaire (FQ), Bodily Sensations Questionnaire (BSQ), Body Sensations Interpretation Questionnaire (BSIQ), Agoraphobic Cognitions Questionnaire (ACQ), Beck Depression Inventory (BDI) The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* at 3 months (original sample + re‐randomised WL patients) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers (< 3 sessions) at 3 months (original sample) Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ), measured on original sample + re‐randomised WL patients LT‐Remission/Response: high end‐state functioning* at 15 months (original sample + re‐randomised WL patients) | |
| Notes | *High end‐state function was defined as panic‐free and an assessor panic‐related distress/disability rating equal or below 2 ('slight'). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | "Assessments, which included ratings completed by an assessor who was blind to treatment allocation, were at pre‐treatment/waiting‐list, 3, 6, and 15 months." |
| Incomplete outcome data (attrition bias) | Low risk | "Of 72 patients meeting acceptance criteria,3 dropped out (1per treatment). Five who agreed initially to random allocation refused to take imipramine when allocated to that condition. Drop‐outs and refusers after randomisation were replaced and not included in the data analysis.To be classified as a drop‐out, patients had to start treatment but attend no more than two sessions. Patients who attended at least three sessions were considered completers and included in all analyses." For this review we are not considering the imipramine arm, therefore dropouts (CBT n = 1; BT n = 1; WL n = 0) were low in number and evenly distributed. Therefore, the proportion of missing outcomes is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Incomplete outcome data (attrition bias) | Low risk | (See above) |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "Cognitive therapy (CT) was based on the cognitive theory of panic. Several cognitive and behavioural techniques (see Clark, 1989; Salkovskis & Clark, 1991) were used to help patients identify and change misinterpretations of bodily sensations." Both Clark DM and Salkovskis PM are among the study authors. |
| Therapist allegiance | Unclear risk | Insufficient information provided |
| Treatment fidelity | Low risk | "To check therapists' adherence to the treatment protocol ten audiotapes per treatment (each from a different patient) were randomly selected and rated for the presence/absence of features which should be unique to that treatment and for time spent on procedures which should be common to all treatments. There were no protocol violations and the treatments did not differ in times spent on the common procedures." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age 18 to 60 years, DSM‐III‐R diagnosis of panic disorder with no, mild or moderate agoraphobic avoidance, current episode duration at least 6 months (this criterion was intended to minimise spontaneous remission, at least 3 panic attacks in the last 3 weeks, consider panic their main problem, willing to accept random allocation, no use of medication (or, if taking psychotropic medication, on a stable dose for at least 3 months with an agreement not to change dosage), record of at least one panic attack while keeping a daily panic diary during a post‐interview 2‐week baseline period. Exclusion criteria: depressive disorder severe enough to require immediate psychiatric treatment; previous treatment with cognitive therapy or exposure therapy for panic disorder; evidence of organic mental disorder, schizophrenia, alcohol or drug dependence, cardiovascular disease, asthma, epilepsy; pregnancy or intention to become pregnant. Characteristic of the sample:
| |
| Interventions | Participants (n = 43) were randomly assigned to either: 1) Full cognitive therapy (classified as CBT, n = 15)
2) Brief cognitive therapy (classified as CBT, n = 14)
3) Wait list (classified as WL, n = 14)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment/wait list, 3 months post‐treatment follow‐up, 12 months post‐treatment follow‐up Measures: panic‐anxiety composite measure, panic frequency, panic‐related distress/disability, Beck Anxiety Inventory (BAI), Hamilton Anxiety Rating Scale (HARS), Fear Questionnaire (FQ), Body Sensations Interpretation Questionnaire (BSIQ), Agoraphobic Cognitions Questionnaire (ACQ), Beck Depression Inventory (BDI) The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ) LT‐Remission/Response: although measured (high end‐state functioning*), data could not be extracted because the comparison was between the 2 active treatment arms, both classified as CBT (comparison not feasible). | |
| Notes | * "We defined high end‐state functioning as panic free and as an assessor‐scored panic‐related distress—disability rating of 2 or less ('slight')" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | "Assessments, which included ratings completed by an independent assessor who was unaware of treatment allocation, were at pretreatment/wait list, post‐treatment/wait list, 3‐month post‐treatment follow‐up, and 12‐month post‐treatment follow‐up." |
| Incomplete outcome data (attrition bias) | Low risk | "43 patients were randomized. One patient (allocated to FCT) dropped out after one session, having indicated that she was much improved and could not arrange time off work for further sessions. All other patients completed treatment" (and assessments). The proportion of missing outcomes is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "During the 1980s, several effective cognitive—behavioral treatments for panic disorder were developed. The two that have been most extensively evaluated are the panic control treatment (PCT) developed by Barlow, Craske, and colleagues and the cognitive therapy program developed by Clark, Salkovskis, Beck, and colleagues." "To maximize the amount of change achieved in each therapy session, we developed a set of self‐study modules covering the main aspects of therapy and asked patients to complete the modules prior to therapy sessions." |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "Regular individual supervision was provided throughout the trial." Insufficient information provided |
| Methods | Study design: Randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐IV diagnosis of panic disorder with agoraphobia. Eligible patients were not allowed to take any psychotropic medication, with the exception of low doses hypnotics, and could not receive psychotherapy during the study. Exclusion criteria: current major depression, or a score greater than 18 on the Hamilton rating scale for depression; bipolar disorder, schizophrenia or other psychotic disorders; alcoholism, or street drugs use; history of CBT for PDA, or a current psychotherapy; treatment with antidepressants, neuroleptics, anxiolytics or mood stabilisers within the 2 weeks preceding the entry. Characteristic of the sample:
| |
| Interventions | Participants (n = 92) were randomly assigned to either: 1) Virtual reality exposure therapy (classified as BT, n = 29; n = 43 after re‐randomisation of WL patients)
2) Cognitive behaviour treatment (classified as CBT, n = 31; n = 44 after re‐randomisation of WL patients)
3) Wait list (classified as WL, n = 32)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment/WL (3 months), 6 months follow‐up, 12 months follow‐up Measures: Fear Questionnaire (FQ), Panic Disorder Severity Scale (PDSS), Chambless Agoraphobic Cognitions scale (ACQ), Panic, Phobia and Generalized Anxiety Scale (PPGAS), State and Trait Anxiety questionnaire (STAI), Hamilton Anxiety Rating Scale (HARS), 21‐item Beck Depression Inventory (BDI), Sheehan Disability Scale (SDS), Global Assessment of Functioning scale (GAF), Dissociative Experience Scale (DES), Work and Social Adjustment scale (WSA) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: at least 50% reduction of FQ‐Ag score (original sample) at post‐treatment ST‐Dropouts: non‐completers (original sample) Continuous scale: Panic Disorder Severity Scale (PDSS; measured on original + re‐randomised sample) LT‐Remission/Response: although measured (at least 50% reduction of FQ‐Ag score at 12 months follow‐up) data were not entered in the analyses because dropouts exceeded 30% of originally randomised sample (see Secondary outcomes). | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Low risk | "Randomization was kept secret and delivered by the biostatistics department of the CHU of Lyon through a phone call to the secretary of each center" |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | At post‐treatment, 63 patients (on 92 originally randomised) were assessed (see study flow chart). |
| Incomplete outcome data (attrition bias) | High risk | At 12 months follow‐up, 51 patients (on 87 randomised) were assessed (see study flow chart). |
| Selective reporting (reporting bias) | Low risk | Study protocol available. All of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way. |
| Researcher allegiance | Unclear risk | Insufficient information provided |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 65 years, principal diagnosis of panic disorder with or without agoraphobia according to DSM‐III‐R criteria, willingness to random assignment to 17 weeks of either placebo or varying dosage regimes of a psychoactive medication, successful withdrawal from psychotropic medications for at least 7 days prior to initial diagnostic evaluation. Exclusion criteria: hypersensitivity to benzodiazepines; diagnoses of organic disorders, obsessive‐compulsive disorder, psychoses, bipolar disorder, adjustment disorder and current (within the last 6 months) substance abuse/dependence; suicidality; serious medical conditions. Characteristic of the sample:
| |
| Interventions | Participants (n = 30) were randomly assigned to either: 1) Cognitive behaviour therapy (classified as CBT, n = 16)
2) Nondirective supportive therapy (classified as SP, n = 14)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment Measures: panic disorder and agoraphobia sections of the ADIS‐R, Anxiety Sensitivity Index (ASI), Fear Questionnaire (FQ), Four Dimensional Anxiety, Subjective Symptoms Scale The following outcomes were used for quantitative analyses: ST‐Remission: ASI reduced from baseline and < 28 at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | ASI is a self rated measure |
| Incomplete outcome data (attrition bias) | Unclear risk | "Sixteen subjects were assigned randomly to CBT, and 14 to NST. One subject dropped out from NST, none dropped out from CBT." The proportion of missing outcomes is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Craske MG is author of a CBT manual (see Barlow 2000b) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "Treatment integrity was addressed via manualized treatments, and ongoing therapy supervision, with review and feedback of approximately 25% of audiotapes of treatment sessions by the principal author." It is unclear whether all sessions were recorded and selection of audiotapes was randomised. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐IV principal diagnosis of panic disorder with or without agoraphobia. Those who were medicated at the time of the initial diagnostic evaluation were withdrawn from psychotropic medications over a minimum of 4 weeks and washed out for at least 2 weeks prior to a repeat diagnostic evaluation to re‐determine study eligibility. Exclusion criteria: history of bipolar disorder, psychosis, posttraumatic stress disorder or current substance abuse/dependence Characteristic of the sample:
| |
| Interventions | Participants (n = 43) were randomly assigned to either: 1) Cognitive behaviour therapy (classified as CBT, n = 27)
2) Wait list (classified as WL, n = 16)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 12 months (after commencement) follow‐up Measures: panic disorder severity (ADIS‐IV), Anxiety Sensitivity Index (ASI), Fear Questionnaire‐Agoraphobia subscale (FQ‐Ag), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Subjective Symptoms Scale (SSS) The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: not measured | |
| Notes | * "Defined as zero daytime and zero nocturnal panic attacks per week over last 2 weeks, panic disorder severity of 3 or less, and no/mild agoraphobia" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Unclear risk | "Of 43 participants, 27 were assigned to CBT; 3 (11.1%) withdrew during treatment. Sixteen were assigned to WL; none withdrew during WL, but 3 (18.8%) withdrew before (n = 2) or during (n = 1) delayed CBT. Reasons for withdrawal are not known." It is unclear whether non‐completers were assessed at post‐treatment (probably so) |
| Incomplete outcome data (attrition bias) | Unclear risk | Number of assessed patients at 12 months follow‐up is not reported |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Craske MG is author of a CBT manual (see Barlow 2000b) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "Each treatment session was audiotaped and 25% (n = 112) were selected randomly for independent adherence ratings of each content item of each session (1 = none, 7 = complete adherence) 2 and percent of off‐task discussion. [...] Average adherence ratings ranged from 4.95 (SD = 0.77) to 6.01 (SD = 1.00), with a total average of 5.64 (SD ‐‐ 0.96), indicating good adherence overall." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age 18 to 60 years, DSM‐IV diagnosis of panic disorder Exclusion criteria: exhibiting characteristics of, or currently diagnosed with schizophrenia or any personality disorder; evidence of organic brain syndrome or mental retardation; any change in psychotropic or other medications or currently taking a medication for less than 2 weeks; medical conditions that would interfere with the diagnosis and/or treatment of panic disorder not due to a medical condition; report or exhibition of characteristics of present substance abuse that would meet DSM‐IV criteria; unwillingness or inability to give informed consent; experiencing less than 3 panic attacks within a 4‐week period Characteristic of the sample:
| |
| Interventions | Participants (n = unclear) were randomly assigned to either: 1) Breathing retraining (classified as PT, n = unclear)
2) Cognitive therapy (classified as CBT, n = unclear)
| |
| Outcomes | Time points for assessment: pre‐treatment, baseline (first session), termination (last session), 4 weeks after termination Measures: panic diary, Beck Depression Inventory (BDI), Panic Disorder Severity Scale (PDSS), end tidal carbon dioxide level (ETCO₂), respiratory rate The following outcomes were used for quantitative analyses: ST‐Remission: although reported (panic‐free at termination), ST‐Remission could not be calculated following an ITT principle (number of patients randomised to each arm not specified) ST‐ Response: not measured (not imputed) ST‐Dropouts: not reported Continuous scale: Panic Disorder Severity Scale (PDSS) at pre‐treatment and at 4 weeks after termination LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random assignment occurred by using the random number table from a Sharp scientific calculator" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "Of those accepted into the study, one became ineligible after beginning antidepressants after session 3 of the cognitive therapy group, one failed to attend her 6th breathing retraining session and could not be reached by phone, one dropped out of the cognitive behavioral therapy after session 6, five people failed to show up for the first session and could not be reached by phone, three people stated that they were too busy or not interested in beginning the study, and four people did not return phone calls after the initial screening." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "The primary investigator of the study trained each of the therapists and met with each therapist for 2 hours per week during the treatment phase to review the previous session and preview the following session. Additionally, the CBT therapists brought a script into each session with them in order to ensure thorough deliverance of the treatment." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of Panic Disorder with Agoraphobia. Only patients who recognised the symptoms induced by voluntary hyperventilation as similar to their panic attacks were included in the study. Exclusion criteria: psychotic symptoms; substance abuse Characteristic of the sample:
| |
| Interventions | Participants (n = 49) were randomly assigned to either: 1) Breathing retraining/cognitive restructuring (classified as CBT, n = 17)
2) Exposure therapy (classified as BT, n = 17)
3) Breathing retraining/cognitive restructuring + exposure therapy (classified as CBT, n = 15)
| |
| Outcomes | Time points for assessment: baseline (4 weeks prior to treatment), pre‐treatment, post‐treatment Measures: Fear Surrey Schedule‐III (FSS‐IZZ), phobic anxiety and avoidance scales, panic attack diary, Bodily Sensations Questionnaire (BSQ), Symptom CheckIist‐90 (SCL‐90), respiratory rate (RR) and end tidal carbon dioxide pressure (pC0₂). The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Bodily Sensations Questionnaire (BSQ) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | BSQ (used to impute ST‐Remission) is a self rated measure |
| Incomplete outcome data (attrition bias) | High risk | "Of the 49 patients who entered treatment, 40 completed the program. Attrition rates were 4 (24%) for BRCR, 4 (24%) for EXP and 1 (6%) for BRCR + EXP" |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "Supervision by a senior clinical psychologist (the second author) was provided on a weekly basis." Unclear whether all sessions for all patients were supervised. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: between 18 and 60 years of age; DSM‐IV diagnosis of panic disorder, with or without agoraphobia; current episode duration of at least 3 months; consider panic the main problem; willing to accept random allocation, including the wait list condition. All patients taking medication at the time of entry must have been on a stable dose for 3 months and must have been willing and able to remain on a stable regime for 3 months during the course of treatment. Exclusion criteria: depressive disorder severe enough to require urgent treatment; undergoing CBT for the current episode; evidence of organic mental disorder, schizophrenia, alcohol or drug dependence, cardiovascular disease, asthma, epilepsy, or pregnancy or intention to become pregnant during the course of the study. Concurrent Axis II personality disorder was not a reason for exclusion unless the personality disorder was clearly the primary problem. Characteristic of the sample:
| |
| Interventions | Participants (n = 186) were randomly assigned to either: 1) CBT ‐ 12 sessions ‐ therapist delivered (classified as CBT, n = 45)
2) CBT ‐ 6 sessions ‐ therapist delivered (classified as CBT, n = 45)
3) CBT ‐ 6 sessions ‐ computer augmented (classified as CBT, n = 50)
4) Wait list (classified as WL, n = 46)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 6 months follow‐up Measures: panic frequency, panic‐related distress/disability, Fear Questionnaire (FQ), Mobility Inventory for Agoraphobia (MI), Body Sensations Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ), State–Trait Anxiety Inventory, Trait subscale (STAI–T), Beck Depression Inventory (BDI), Medical Outcomes Survey Short Form 36 (SF‐36) The following outcomes were used for quantitative analyses: ST‐Remission: panic‐free at post‐treatment ST‐ Response: not measured (not imputed) ST‐Dropouts: not measured (the number of non‐completers for each arm is not specified) Continuous scale: although measured, data cannot be used because number of assessed patients is not reported LT‐Remission/Response: although measured (panic‐free at follow‐up), data cannot be used because re‐randomisation of WL patients leaves only 3 arms, all classified as CBT (comparison not feasible) | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "In total, 186 patients met entry criteria and were offered and accepted a place in the study. Of these, 163 patients (87.6%) commenced treatment (wait list, n=41; CBT6, n=39; CBT6‐CA, n=41; CBT12, n=42). Twenty‐three patients (14.1%) failed to receive at least three sessions of their respective course of treatment or to provide adequate data and were classified as dropouts." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "All sessions for all treatment conditions were tape‐recorded, and a random selection (20%) of tapes were exchanged between sites and rated by Justin A. Kenardy and Michael G. T. Dow to ensure adherence to treatment protocols and therapeutic competence. There were no significant effects for site, treatment, or Site Treatment on protocol adherence or therapeutic adequacy. Therapists also completed a separate checklist for each therapy session to evaluate adherence to the protocol. The correlation between therapist‐rated and externally rated protocol adherence was 0.92 (p .001). No significant differences were found on therapist‐rated treatment protocol compliance across site or treatment or for Site Treatment. Overall, there was 97.1% protocol adherence." |
| Other bias | Unclear risk | Modification of the original sample with replacements. Number and randomisation of replacements not specified. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 17 and 70 years, primary DSM‐III‐R diagnosis of panic disorder with no or mild agoraphobic avoidance, panic disorder for at least 12 months, at least a mean of 1 panic attack per week during the previous 4 weeks, asking for treatment of panic disorder, no use of serotonergic antidepressants or benzodiazepines (for at least 4 weeks). Exclusion criteria: depressive disorder preceding the current episode of panic disorder or requiring immediate treatment; behaviour therapy received for panic disorder; evidence of organic mental disorders, psychotic disorders, alcohol or drug dependence, cardiovascular disease, asthma, epilepsy; medical contraindication for exposure, behavioural experiments or hyperventilation Characteristic of the sample:
| |
| Interventions | Participants (n = 37) were randomly assigned to either: 1) Cognitive therapy (classified as CT, n = unclear)
2) Applied relaxation (classified as PT, n = unclear)
Note that "after the last patient entered the study, a waiting‐list control group was formed. The first 11 men and 7 women meeting the same criteria as used for the treatment group were drawn from the waiting‐list to form a control group." This control group is not considered for this review because it is not randomised. | |
| Outcomes | Time points for assessment: baseline, post‐treatment (13 weeks), 1‐month follow‐up, 6‐month follow‐up Measures: panic diary, Fear of Fear Questionnaire, Fear Questionnaire (FQ), State–Trait Anxiety Inventory (STAI), Depressive Symptoms Inventory (DSI), Symptom Check List (SCL‐90) The following outcomes were used for quantitative analyses: ST‐Remission: although measured (panic‐free at post‐treatment) detailed data are not reported ST‐ Response: not measured ST‐Dropouts: detailed data are not reported Continuous scale: although measured, detailed data are not reported LT‐Remission/Response: although measured (panic‐free at 6 months follow‐up) detailed data are not reported | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | High risk | Study protocol unavailable. Pre‐planned measures are not reported with sufficient details. |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "Weekly supervision was given by the first author during the whole treatment." It is unclear whether all sessions for all patients were supervised. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III diagnosis of agoraphobia Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | In a first phase of the study, participants (n = 51) were randomly assigned to either: 1) Exposure in vivo (classified as BT, n = unclear)
2) Rational emotive therapy (classified as CT, n = unclear)
3) Self instructional training (classified as CT, n = unclear)
In a second phase of the study, all patents received 6 group sessions (150 minutes each) of exposure in vivo. | |
| Outcomes | Time points for assessment: baseline, post‐test Measures: behavioural walk, phobic anxiety and avoidance scales, Fear Questionnaire (FQ), Irrational Belief Test (IBT), Symptom Check List (SCL‐90) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: not reported Continuous scale: although measured, detailed data are not reported LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | High risk | Study protocol unavailable. Pre‐planned measures are not reported with sufficient details. |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "Therapists received a special training for the research project and extensive manuals were used. Therapists were supervised by the senior author." It is unclear whether all sessions for all patients were supervised. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐IV diagnosis of either panic disorder with or without agoraphobia, OCD, social phobia, generalised anxiety disorder, specific phobia or PTSD. There were no limitations on past or concurrent treatments. Exclusion criteria: active substance abuse or dependence or psychosis Characteristic of the sample (PDA sub‐sample):
| |
| Interventions | Participants (PDA sub‐sample, n = 36) were randomly assigned to either: 1) Cognitive behaviour therapy (classified as CBT, n = unclear)
2) Wait list (classified as WL, n = unclear)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment Measures: Beck Anxiety Inventory (BAI) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: although measured (40% reduction in BAI score), data for the PDA sub‐sample are not reported ST‐Dropouts: not reported for PDA sub‐sample Continuous scale: the only available measure (BAI) is not considered among outcomes of interest for this review (see Secondary outcomes) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "We assessed clinicians’ adherence to the protocol by asking independent raters to listen to audiotapes of a random sample of sessions (33 tapes, or one of every four sessions). Overall, the ratings indicated that group leaders adhered closely to the intended protocol and that quality of implementation was midway between good and very good." |
| Methods | Study design: multicentre randomised controlled trial | |
| Participants | Inclusion criteria: 18 to 65 years old (see protocol), DSM–IV–TR diagnosis of panic disorder with agoraphobia, score of 18 or more on the Hamilton Anxiety Scale (HAM‐A), score of 4 or more on the Clinical Global Impression (CGI). Patients had to agree to discontinue all psychopharmacological medication and were not allowed to have any concomitant psychotherapy. Patients on psychopharmacological medication underwent a washout period prior to baseline. Exclusion criteria: unable to comply with the study schedule or requirements; clinically significant suicidal intent; DSM‐IV‐TR diagnosis of any psychotic or bipolar disorder, borderline personality disorder, or current alcohol dependence; medical condition that could explain symptoms. Other current comorbid diagnoses, including unipolar depression and other anxiety disorders, were allowed unless they were of primary clinical concern. Characteristic of the sample:
| |
| Interventions | Participants (n = 369) were randomly assigned to either: 1) CBT variant with therapist‐guided exposure outside the therapy room (classified as BT, n = 163)
2) CBT variant with non‐therapist‐guided exposure outside the therapy room (classified as BT, n = 138)
3) Wait list (classified as WL, n = 68)
| |
| Outcomes | Time points for assessment: baseline, intermediate (after the 4th session), post‐treatment, 6 months follow‐up Measures: Structured Interview Guide for the Hamilton Anxiety Scale (HAM‐A/SIGH‐A), Clinical Global Impression (CGI), Panic Agoraphobia Scale (PAS), Mobility Inventory ‐ Agoraphobia subscale (MI‐Ag) The following outcomes were used for quantitative analyses: ST‐Remission: PAS score ≤ 8 at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Panic Agoraphobia Scale (PAS) LT‐Remission/Response: although measured (PAS score ≤ 8 at 6 months follow‐up), data cannot be used because re‐randomisation of WL patients leaves only 2 arms, both classified as BT (comparison not feasible) | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Low risk | "The randomization list was generated at the clinical coordination center (Dresden) by personnel not associated with patient care. The study centers were blind to the assignment of subsequent cases and were informed of treatment status only after a fax documenting the included patient was sent to the clinical coordination center. More numbers for each center were drawn than necessary so that treatment condition of final patients in each study center remained unpredictable, thereby ensuring blinding of the randomization throughout the study." |
| Blinding of outcome assessment (detection bias) | High risk | The Panic Agoraphobia Scale (PAS, used to determine ST‐Remission) is a self report questionnaire |
| Incomplete outcome data (attrition bias) | High risk | A total of 63 patients (34 + 25 + 4) were lost at post‐treatment assessment (see study flow chart) |
| Selective reporting (reporting bias) | High risk | Not all of the study's pre‐specified primary outcomes have been reported (Aggregated Panic Disorder Scale and Mobility Inventory: PDS‐MI score). One reported outcome was not pre‐specified (PAS). |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "All treatment sessions were videotaped, and a randomly selected sample of almost 18% was evaluated. All raters were blind to treatment condition and evaluated each tape using the therapist adherence and competence rating scale for PD and AG. Adherence and competence were assessed on the basis of a 9‐point scale from 0 (nonexistent) to 8 (optimal adherence/excellent competence).The mean overall ratings of therapy adherence and competence across all sessions were 5.53 (SD 1.29) and 5.73 (SD 1.26), respectively, indicating that therapists demonstrated good levels of adherence to the manual and implemented it with good levels of competence." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 65 years, DSM‐IV diagnosis of panic disorder with agoraphobia at least 1 year's duration, agoraphobic avoidance at least moderately severe for the prior 6 months. Participants excluded on the basis of recent medication changes were eligible for reconsideration once medications were stabilised in appropriate limits. Exclusion criteria: being in therapy elsewhere if not willing to suspend that treatment until the end of the study; on dosages of alprazolam in excess of 1.5 mg daily (or similar dosages for other benzodiazepines); taking antidepressant or antianxiety medication for less than 6 months or change of medication within the last 12 weeks; comorbid diagnoses of thought disorder, major depression, bipolar disorder, or substance dependence; presence of another anxiety disorder more severe than the PDA; DSM‐IV diagnosis of any of the following Axis II disorders: paranoid, schizoid, schizotypal, antisocial or borderline Characteristic of the sample:
| |
| Interventions | Participants (n = 46) were randomly assigned to either: 1) EMDR (not included in this review, n = 18)
2) Association and relaxation therapy (classified as PT, n = 13)
3) Wait list (classified as WL, n = 15)
| |
| Outcomes | Time points for assessment: baseline, termination, 5 to 6 weeks after termination Measures: Agoraphobic Cognitions Questionnaire (ACQ), Body Sensations Questionnaire (BSQ), Brief Body Sensations Interpretation Questionnaire (BBSIQ), Panic Appraisal Inventory (PAl), Mobility Inventory (MI), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Brief Symptom Inventory (BSI), Social Adjustment Scale‐Self‐Report (SAS‐SR), Distress Questionnaire, Panic Disorder Symptom The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: non‐completers Continuous scale: although measured, data concerning ART group are not reported. EMDR is not an included treatment, therefore only data on WL patients could be extracted (comparison not feasible) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "Of the 46 participants who entered the study, 4 dropped out prior to the completion of treatment. One dropped out during the waiting list period before she provided posttest data or received her treatment condition assignment. Three participants (one of whom had previously been in the waiting list condition) dropped out or were terminated during EMDR: one because of a marital crisis, another because of deterioration, and a third for repeated cancellations of appointments." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable. Data concerning ART group are not reported. |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "To ensure that therapists adhered to the treatment protocol, all sessions were audio‐ Or videotaped and reviewed by Alan J. Goldstein prior to supervision meetings, which were held weekly to discuss clinical issues and proper provision of treatment. Two of the authors, Dianne L. Chambless and Kimberly A. Wilson, and their trained research assistants followed detailed integrity checklists that assessed adherence to treatment protocol, presence of therapist support and reinforcement, and protocol violations, which included introducing other treatments into the session. Adherence checks were conducted on 31% (n = 80) of all sessions. Of these, 33 were independently rated by additional coders to assess reliability. Average percent agreement was 95% for the integrity items identified a priori to be most important. The adherence monitoring team was not otherwise involved in participants' treatment and was unaware of participants' treatment outcome." |
| Other bias | Unclear risk | Modification of the original sample with replacements. Number and randomisation of replacements not specified. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder with or without agoraphobia. Subjects were dissuaded from participating in other therapy or self help procedures during the study. Subjects taking medication for anxiety or depression were allowed to participate if they had been stabilised on the medication for at least 4 weeks and continued to have panic symptoms. Exclusion criteria: seizure disorder, kidney disease, stroke, schizophrenia, organic brain syndrome, emphysema, heart attack, chronic hypertension Characteristic of the sample:
| |
| Interventions | Participants (n = 33) were randomly assigned to either: 1) Bibliotherapy (not included in this review, n = 12)
2) Guided imaginal coping (classified as CBT, n = 9)
3) Wait list (classified as WL, n = 12)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment Measures: Daily Panic Attack Records (DPAR), Panic Cognitions Questionnaire (PACQ), Panic Symptoms Questionnaire (PASQ), Mobility Inventory for Agoraphobia (MI), Anxiety Sensitivity Index (ASI), Beck Depression Inventory (BDI), Likelihood of Having a Panic Attack, Your Thoughts During a Panic Attack, Coping with Panic Attacks, Panic Self‐Efficacy Questionnaire. The following outcomes were used for quantitative analyses: ST‐Remission: panic‐free ST‐ Response: panic‐free OR 50% reduction in number of panic attacks, panic symptoms ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI). Note that reported SDs are uncommonly low, so we considered them as being SEs. LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | Panic frequency (used to determine ST‐Remission) was self rated |
| Incomplete outcome data (attrition bias) | Low risk | "Only 2 subjects dropped out: 1 from the WL group and 1 from the BT group. The subject from the WL group reported that she had to move to a different state to seek employment and could no longer continue in the study. The subject from the BT condition completed all the dependent measures of the study, but was not included in the analyses because she had failed to read the book." For this review we are not considering the bibliotherapy arm, therefore data are missing for only one subject (WL) and reasons for missing outcome data are unlikely to be related to true outcome. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | In bibliotherapy arm, "subjects read the book Coping with Panic (Clum, 1990)." In Guided Imaginal Coping arm, "the protocol for each of the eight treatment sessions was outlined for therapists. These plans were derived primarily from material in Coping with Panic." Clum G is among the study authors. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "The second author supervised the four therapists weekly in order to ensure the uniformity of treatment procedures, and the research team met regularly for discussion. In addition, some treatment sessions were observed directly, or videotaped and later observed by the first and second authors. A random sample of 8 sessions was observed to ensure treatment integrity." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder with or without agoraphobia. Subjects using psychotropic medications were required to maintain a stable dosage for at least 1 month and throughout treatment and evaluation. Exclusion criteria: comorbid DSM‐III‐R diagnosis rated as severe as panic disorder; being in psychotherapy for anxiety (subjects who were in psychotherapy for other psychological difficulties were included if they had been in a stable therapeutic relationship for at least 3 months). Characteristic of the sample:
| |
| Interventions | Participants (n = 37) were randomly assigned to either: 1) Breathing retraining ‐ slow respiration rate (classified as PT, n = 11)
2) Breathing retraining ‐ increase respiration rate (classified as PT, n = 12)
3) Wait list (classified as WL, n = 14)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment. Measures: Anxiety Disorders Interview Schedule–R (ADIS–R), Anxiety Sensitivity Index (ASI), Emotional Control Questionnaire (ECQ), Self‐Efficacy Questionnaire (SEQ), Diagnostic Symptom Questionnaire (DSQ), Interoceptive Exposure Test (IET), respiratory rate The following outcomes were used for quantitative analyses: ST‐Remission: panic‐free ST‐ Response: not measured ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | Panic frequency was rated by assessors. "Assessors who conducted evaluations at pre‐ and post‐assessment were blind to the subjects' experimental condition." |
| Incomplete outcome data (attrition bias) | High risk | "The first 37 subjects agreeing to participate were randomly assigned to one of three groups to enlist the requisite sample size of 10 subjects per cell (7 subjects dropped out of the study before completion of the post‐assessment)." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "All sessions were audiotaped and 25% of these tapes were rated by an assessor blind to the treatment conditions, who was then asked to identify the treatment condition being conducted. Accurate identification of treatment protocol was made 93% of the time (14/15). One tape was inaudible and could not be rated." It is unclear whether the selection of tapes to assess was random. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: 18 years of age or older, primary DSM‐III‐R diagnosis of panic disorder with or without agoraphobia, minimum Grade 8 reading and writing ability, physician agreement regarding participation Exclusion criteria: presence of organic disease which might be related to panic disorder or interfere with participation in the study; presence of other serious psychiatric disorders, specifically psychotic disorders, substance abuse and current major depressive disorder; presence of significant suicidal risk; involvement in other psychological treatment; current pharmacological treatment for panic disorder, with the exception of low doses of benzodiazepines (equivalent of 20 mg diazepam or less) or stable doses of antidepressants (i.e. prescribed for at least 6 months and stable dose for at least 3 months) Characteristic of the sample:
| |
| Interventions | Participants (n = 117) were randomly assigned to either: 1) Individual self administration of the self help manual (not included, n = unclear)
2) Use of the manual in a self help treatment group (not included, n = unclear)
3) Use of the manual in a treatment group led by professional therapists (classified as CBT, n = unclear)
4) Wait list (classified as WL, n = unclear)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment Measures: Anxiety Sensitivity Index (ASI), Fear Questionnaire‐Agoraphobia Subscale (FQ‐Ag), Sheehan Patient‐Rated Anxiety Scale (SPRAS), Clinical Global Improvement (CGI) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (not imputed: number of randomised patients for each arm not specified) ST‐ Response: not measured (not imputed: number of randomised patients for each arm not specified) ST‐Dropouts: not reported by treatment group Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "Of the 117 subjects enrolled in the evaluation study, 106 completed the Anxiety Sensitivity Index at pre‐ and posttreatment. These subjects comprised the sample for the present study." No further detail about these 11 dropouts is reported. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: adults aged over 60 years, principal DSM‐IV diagnosis of panic disorder with or without agoraphobia. Co‐morbidity with other anxiety disorders, depression or dysthymia was allowed as long as PD(A) was the principal diagnosis. Participants using benzodiazepines were asked to adhere to a fixed daily dose for the duration of the study. Exclusion criteria: presence of severe psychiatric disorders (e.g. psychotic disorder, bipolar disorder), severe somatic condition that would hinder appropriate application of CBT (e.g. severe cardiovascular disease), contraindication for paroxetine, current use of an antidepressant in an adequate dose, current and adequate psychological treatment, failure of paroxetine or CBT in the past, abuse of or dependency on alcohol or psychoactive substances, dementia and a score of 23 or less on the Mini‐Mental State Examination Characteristic of the sample:
| |
| Interventions | Participants (n = 49) were randomly assigned to either: 1) Cognitive behaviour therapy (classified as CBT, n = 20)
2) Paroxetine (not included, n = 17)
3) Wait list (classified as WL, n = 12)
| |
| Outcomes | Time points for assessment: baseline, 8 weeks, 14 weeks (termination), 26 weeks (3 months follow‐up) Measures: Agoraphobic Cognitions Questionnaire (ACQ), Mobility Inventory (MI), Symptom Checklist (SCL‐90) The following outcomes were used for quantitative analyses: ST‐Remission: panic‐free (zero panic attacks in the preceding week) at termination ST‐ Response: improvement > 30% on one of the primary outcome scales ST‐Dropouts: non‐completers Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ) LT‐Remission/Response: although measured (panic‐free at 26 weeks), details are not reported and anyway refer to the comparison paroxetine versus CBT | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A sealed envelope was randomly selected from an initial total of 75 envelopes containing the treatment assignments, with 30 being labelled as CBT, 30 as paroxetine and 15 as waiting list." |
| Allocation concealment (selection bias) | Unclear risk | See above. It is unclear whether envelopes were opaque and sequentially numbered |
| Blinding of outcome assessment (detection bias) | High risk | "All assessments were administered by trained, independent psychologists who were blind to the study and treatments delivered." However, panic frequency was rated through MI, which is a self rated measure. |
| Incomplete outcome data (attrition bias) | Low risk | "Five patients (10.2%) failed to complete the 14‐week treatment protocol: three dropped out in the paroxetine condition (side‐effects, n = 1; protocol violation, n = 1; broken hip, n = 1), one in the CBT condition (protocol violation) and one in the WL condition (severe somatic illness." We are not considering the paroxetine group for this review, therefore the proportion of missing outcomes compared with the observed event risk is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Selective reporting (reporting bias) | Low risk | Study protocol available. All primary outcomes coincide (however, note that BDI, a secondary outcome, is not reported). |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "Throughout the study, they were weekly supervised by a registered supervisor (a member of the Dutch Association of Behavioural and Cognitive Therapy). Per session, the therapists recorded which specific CBT component they had applied and any deviations from the treatment manual were discussed." It is unclear whether all sessions for all patients were supervised; no detail is reported about supervisor assessments. |
| Other bias | Unclear risk | This study has been funded by Glaxo Smith Kline, so a sponsorship bias is possible. However, because the Paroxetine arm is not considered for this review, it is unclear whether the comparison CBT versus WL can be affected by this possible source of bias. |
| Methods | Study design: randomised controlled trial, inpatient setting | |
| Participants | Inclusion criteria: age from 20 to 65 years, DSM‐III‐R diagnosis of panic disorder with agoraphobia, DSM‐III‐R agoraphobia severity rated as moderate or severe, patients considered the symptoms of agoraphobia (that is avoidance behaviour and situational panic or symptom attacks and not spontaneous panics or other mental problems) as their main problem. A plan for the reduction or discontinuation of medication before hospital admission was agreed upon and patients were informed that use of psychotropic medication was prohibited during the 6‐week inpatient treatment period. Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 52) were randomly assigned to either: 1) Cognitive therapy (classified as CBT, n = 26)
2) Guided mastery therapy (classified as BT, n = 26)
| |
| Outcomes | Time points for assessment: precare (before hospital admission), pre‐treatment (1 week), post‐intensive period (4 weeks), post‐treatment (6 weeks), 1 year follow‐up Measures: Behavioral Avoidance Tests (BATs), Structured Clinical Interview for the DSM‐III‐R (SCID‐I), Phobic Avoidance Rating Scale (PARS), Body Sensations Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ), Mobility Inventory for Agoraphobia (M), Self‐Efficacy Scales for Agoraphobia (SESA), State‐Trait Anxiety Inventory (STAI), Beck Depression Inventory (BDI), panic diary The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* at post‐treatment ST‐ Response: improvement > 50% on PARS separation avoidance sub‐scale ST‐Dropouts: non‐completers Continuous scale: Body Sensations Questionnaire (BSQ) LT‐Remission/Response: high end‐state functioning* at 1 year follow‐up | |
| Notes | * "It was decided a priori to give a status of high endstate functioning to those who at posttreatment (l) had a score of 1.5 or lower at the PARS separation avoidance subscale, implying that at least half of the six situations of this subscale were approached regularly without use of safety signals (e.g. medication); (2) had a score of 3‐‐"symptoms interfere with work or social activity only in minor ways"‐‐or less in interviewer rated global severity; and (3) were free of spontaneous panic attacks in the two weeks after discharge." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | "A symptom rating interview was performed by a psychiatrist who worked in another institution and was blind to the treatment condition of the patients. The interview included the 0 to 4 point Phobic Avoidance Rating Scale (PARS)." |
| Incomplete outcome data (attrition bias) | Unclear risk | "Six of the 52 patients, 3 in each condition, dropped out from the study. Four patients dropped out before or within the first 24 hours after admission to the hospital: 2 because of problematic family circumstances, 1 was not allowed financial coverage for the hospital stay from her home country, and 1 withdrew as she experienced overwhelming fantasies of being locked in forever in a mental hospital. Two patients, 1 in each condition, withdrew just after the discontinuation of anxiolytics because they could not tolerate being without them." Missing outcome data are balanced in numbers across intervention groups, with similar reasons for missing data across groups. However, it is unclear whether the proportion of missing outcomes is enough to have a clinically relevant impact on the intervention effect estimate. |
| Incomplete outcome data (attrition bias) | Unclear risk | All treatment completers (n = 46, see above) were assessed at 1‐year follow‐up |
| Selective reporting (reporting bias) | High risk | Study protocol unavailable. Results of ACQ measurements are not reported. |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | "The two psychologists alternated between being supervisor and being the primary therapist, responsible for the overall treatment and for conducting the group sessions together with a co‐therapist, in the 6 groups. In the intensive three‐week period, the supervising psychologist conducted two 45 min supervision sessions per week, addressing immediate treatment problems and questions about adherence to the manuals. In addition, the supervisor listened to audiotapes of therapy sessions and gave written feedback to the therapists." It is unclear whether all therapy sessions were assessed. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: primary DSM‐IV diagnosis of panic disorder with or without agoraphobia Exclusion criteria: psychosis, substance abuse, suicidal ideation or intent Characteristic of the sample:
| |
| Interventions | Participants (n = 28) were randomly assigned to either: 1) Panic control treatment (classified as CBT, n = 14)
2) Acceptance‐enhanced panic control treatment (classified as 3W, n = 14)
| |
| Outcomes | Time points for assessment: pre‐treatment, mid‐treatment, post‐treatment, 6 months follow‐up Measures: State‐Trait Anxiety Inventory (STAI), Acceptance and Action Questionnaire (AAQ), Automatic Thoughts Questionnaire (ATQ), Beck Depression Inventory (BDI), Anxiety Sensitivity Index (ASI), Agoraphobic Cognitions Questionnaire (ACQ), Panic and Agoraphobia Scale (PAS), Panic Disorder Severity Scale (PDSS), quality of life (SF‐36), Valued Living Questionnaire (VLQ), White Bear Suppression Inventory (WBSI), Subjective Units of Distress Scale (SUDS), Diagnostic Symptoms Questionnaire (DSQ), Anxiety and Willingness Scale (AWS) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: non‐completers (including early dropouts) Continuous scale: although measured, data cannot be used because number of assessed patients is not reported LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "Twenty‐eight individuals met inclusion criteria and were scheduled for treatment. Of those, 22 attended at least the first session. Fourteen participants completed the full 10 weeks of treatment. The cases of participants who prematurely dropped out of treatment are dropped out from further analyses." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 65 years, DSM‐III‐R primary diagnosis of panic disorder with a clinician's severity rating of at least 4 on a 0 to 8 scale (moderate severity), at least 1 panic attack in the week before starting treatment Exclusion criteria: pharmacotherapy or psychotherapy begun in the past 6 months; either in drug or psychotherapeutic treatment more than 6 months (unless subjects agreed to stop such treatment for the duration of the study); on 4 mg or more of alprazolam for any 3‐week period and were non‐responders; evidence of benzodiazepine hypersensitivity; undergone cognitive behaviour therapy for anxiety at any time; females who were pregnant or lactating or at risk to become pregnant; significant medical problems, as determined by history, medical report and laboratory values; history of psychotic disorder or dementia; history of alcohol or other substance abuse within the last 6 months; current or past bipolar disorder. Subjects with major depression were excluded only if depression predominated over panic disorder at the time of presentation and if depression preceded panic disorder chronologically. Subjects with acute suicidal ideation were excluded. Characteristic of the sample:
| |
| Interventions | Participants (n = 69) were randomly assigned to either: 1) Alprazolam (not included, n = 17)
2) Placebo (not included, n = 18)
3) Behaviour therapy (classified as CBT, n = 18)
4) Wait list (classified as WL, n = 16)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment. Measures: daily self monitoring, Anxiety Disorders Interview Schedule ‐ R (ADIS‐R), Hamilton Anxiety Rating Scale (HAM‐A), Hamilton Rating Scale for Depression (HAM‐D) The following outcomes were used for quantitative analyses: ST‐Remission: ADIS‐IV severity < 4 ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Disorders Interview Schedule ‐ R (ADIS‐R) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | "Posttreatment clinical assessment measures were gathered through administration of a short form of the ADIS‐R. The ADISR administrators were blind to group assignment" |
| Incomplete outcome data (attrition bias) | High risk | "Out of 69 initial subjects, 57 subjects completed the study, and 12 subjects dropped out. A higher rate of dropout was observed in the placebo group compared with the other three groups. One subject out of 17 (5.9%) dropped from the alprazolam group, 7 out of 18 (38.9%) from the placebo group, 3 out of 18 (16.7%) from the PCT group, and 1 out of 16 (6.3%) from the waiting‐list group." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Barlow DH is author of a CBT manual (see Barlow 2000b) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "All therapy sessions were tape‐recorded and checked for treatment integrity." |
| Other bias | High risk | Performance bias: in contrast with patients in the CBT group, patients in the WL were not asked to withdraw medications. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age 18 to 65 years, DSM‐IV‐TR clinical diagnosis of panic disorder with or without agoraphobia, being able to read, speak and understand Dutch well enough to participate in the treatment groups and to fill in all assessments. Use of psychotropic medication was permitted only if the medication dose was stable during the study and had been stable for at least 2 months prior to study inclusion. Patients who changed their medication during treatment were considered to be dropouts, patients who started (a new) medication less than 2 months before inclusion had to wait for participation until they had fulfilled this 2‐month criterion. Exclusion criteria: severe co‐morbid psychopathology, such as psychosis; addiction; being suicidal; mental retardation; concurrent psychological treatments, or cognitive behavioural treatments in the past 6 months Characteristic of the sample:
| |
| Interventions | Participants (n = 143) were randomly assigned to either: 1) Competitive memory training for panic (classified as CBT, n = 70)
2) Applied relaxation (classified as PT, n = 73)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 6 months follow‐up Measures: Panic Appraisal Inventory (PAI), Mobility Inventory (MI) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Mobility Inventory for agoraphobia when alone (MI‐A) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | MI is a self rated scale |
| Incomplete outcome data (attrition bias) | Low risk | "During treatment, a total of 24 patients (17%) dropped out (13 in AR and 11 in COMET). Analyses were on an intention‐to‐treat basis. First, in a binary logistic regression analysis, it was checked whether dropout was predicted by age, diagnosis, gender or any of the outcome measures at M‐pre. Then missing values were imputed with the SPSS 20 multiple imputation algorithm." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | It seems that authors are involved in conceptualisation of COMET‐panic: "Since this COMET‐panic protocol appeared to be effective in two pilot studies in routine clinical settings (Korrelboom et al. 2008; Peeters et al. 2005), it was decided to put the new protocol to the test in a randomized controlled trial versus an evidence‐based anti‐panic procedure, in this case AR." |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "Both panic management techniques were available in written form (a manual) for therapists and patients. In regular meetings therapists and researchers discussed adherence to the treatment protocols. As an additional check on treatment integrity, patients filled in a checklist containing specific questions about the nature of the treatments they had just received. This checklist contained statements about specific differential identifying elements of both therapies. If both treatments had been delivered properly, AR patients should identify more AR ingredients in the treatment they had received and few/none of the COMET elements, and vice versa for the COMET patients. In the AR condition the mean score for ‘AR ingredients’ was 36.7 (SD = 3.1) whereas the highest possible score was 40, while the mean score for ‘COMET ingredients’ in this condition was only 16.6 (SD = 9.5) whereas the lowest possible score was 4. On the other hand, in the COMET condition these figures were 34.0 (SD = 5.7) for ‘COMET ingredients’ (possible maximum of 40) and 15.2 (SD = 7.6) for ‘AR ingredients’ (possible minimum of 4)." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder with or without agoraphobia. Individuals taking medication for anxiety could participate if they were still suffering from panic symptoms after 6 weeks of stabilisation on medication, if they maintained the same dosages throughout treatment, and if they recorded both the type and amount of medication usage throughout the study. Exclusion criteria: seizure disorder, kidney disorder, stroke, myocardial infarction, chronic hypertension, emphysema, organic brain syndrome, chronic use of alcohol, drug dependence, major depressive disorder, psychotic disorders, involvement in any type of therapy focusing on anxiety management Characteristic of the sample:
| |
| Interventions | Participants (n = 36) were randomly assigned to either: 1) Bibliotherapy (not included, n = 12)
2) Group therapy (classified as CBT, n = 12)
3) Wait list (classified as WL, n = 12)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 3 months follow‐up, 6 months follow‐up Measures: panic frequency and severity, Panic Attack Symptom Questionnaire (PASQ), Panic Attack Cognition Questionnaire (PACQ), Mobility Inventory (MI), Panic Self‐Efficacy Questionnaire (PSEQ), Beck Depression Inventory (BDI) The following outcomes were used for quantitative analyses: ST‐Remission: Mobility Inventory (MI) score < 32 at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Mobility Inventory for agoraphobia when alone (MI‐A) LT‐Remission/Response: Mobility Inventory (MI) score < 32 at 6 months follow‐up | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | Mobility Inventory (MI) is a self rated measure |
| Incomplete outcome data (attrition bias) | Low risk | "Attrition rates were zero for all three conditions" |
| Incomplete outcome data (attrition bias) | Low risk | (see above) |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "The BT condition used Clum's (1990) Coping with panic book. Subjects in the GT condition also used Clum's (1990) Coping with panic text." Glum GA is among the study authors. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "We videotaped all sessions, with the faculty member on the research team viewing these tapes for treatment integrity." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐IV diagnosis of panic disorder with agoraphobia Exclusion criteria: epilepsy, dissociative or non‐dissociative chronic psychosis, recent discontinuation of psychotropic drugs, substance dependence Characteristic of the sample:
| |
| Interventions | Participants (n = 17) were randomly assigned to either: 1) Virtual reality exposure only (classified as BT, n = 9)
2) Virtual reality exposure + cognitive therapy (classified as CBT, n = 8)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 3 months follow‐up Measures: Presence Questionnaire (PQ v3.0), Subjective Units of Discomfort (SUD), Depression Anxiety Stress Scales (DASS 21), Anxiety Sensitivity Index (ASI), Agoraphobia Cognitions Questionnaire (ACQ), Mobility Inventory for Agoraphobia (MI), Simulation Sickness Questionnaire (SSQ), Behavioural Avoidance Test (BAT), heart rate (HR) and heart rate variability (HRV) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The allocation to each group was done using a randomisation table generated by a computerised sequence generator." |
| Allocation concealment (selection bias) | Low risk | "It was impossible to foresee the assignment of the next patient entering the study" (personal communication) |
| Blinding of outcome assessment (detection bias) | High risk | ASI is a self rated measure |
| Incomplete outcome data (attrition bias) | Low risk | "One participant (VRO)dropped out at an early stage due to a severe myopia." The proportion of missing outcomes is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Unclear risk | "In the present study we designed all required VEs for the VRET of agoraphobia within a game level editor." Although possible, the extent to which this source of bias may affect the results is unclear, because both arms are administered the same VEs. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III diagnosis of agoraphobia with panic attacks, other inclusion criteria are mentioned but not reported. Exclusion criteria: none reported Characteristic of the sample:
| |
| Interventions | Participants (n = 19) were randomly assigned to either: 1) Cognitive therapy + graduated exposure (classified as CBT, n = unclear)
2) Progressive deep muscle relaxation + graduated exposure (classified as BT, n = unclear)
3) Graduated exposure alone (classified as BT, n = unclear)
| |
| Outcomes | Time points for assessment: baseline, mid‐treatment, post‐treatment Measures: Global Assessment of Severity, Self‐Rating of Severity, Phobic Anxiety and Avoidance Scale, Fear Survey Schedule, Fear Questionnaire (FQ), Taylor Manifest Anxiety Scale, Panic Scale, Beck Depression Inventory (BDI), Hopkins Symptom Checklist, Subjective Symptom Checklist, Standardised Behavioral Avoidance Course (S‐BAC), heart rate The following outcomes were used for quantitative analyses: ST‐Remission: although measured (high end‐state functioning*) detailed data are not reported ST‐ Response: not measured ST‐Dropouts: detailed data are not reported Continuous scale: although measured, detailed data are not reported LT‐Remission/Response: not measured | |
| Notes | * "Five criteria were used to classify subjects’ level of Endstate (low‐medium‐high) functioning. Subjects were assigned 1 point for each of the following scores: (a) ≤2 on the Global Assessment of Severity; (b) ≤2 on the Self‐Rating of Severity; (c) ≤3 on the Phobic Anxiety and Avoidance Scale; (d) Completing the Standardized‐Behavioral Avoidance Course; and, (e) ≤3 SUDS (in vivo anxiety). Subjects with 0‐1 points = low Endstate functioning; 2‐3 points = medium Endstate functioning, and those with 4‐5 points were classified as having high Endstate functioning." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | High risk | Study protocol unavailable. Pre‐planned measures are not reported with sufficient detail. |
| Researcher allegiance | High risk | "The cognitive therapy was developed by Michelson (1984), adapted from Antaki and Brewin (1982), Beck and Emery (1979), Bums (1980), Mckay, Davis and Fanning (1981), and Sank and Shaffer (1984)." Michelson L is among the study authors. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "To ensure the treatment procedures were administered consistently, weekly meetings were held to discuss and review all treatment sessions. Treatment integrity probes were randomly conducted on 25% of the sessions and revealed consistently high (100%) levels of fidelity." |
| Methods | Study design: multicentre randomised controlled trial | |
| Participants | Inclusion criteria: over 18 years of age, subthreshold or mild panic disorder with or without agoraphobia (DSM‐IV), defined as having symptoms of panic disorder falling below the cut‐off of 13 on the Panic Disorder Severity Scale–Self Report (PDSS–SR). If a participant used medication for anxiety or depression (e.g. benzodiazepines or antidepressants) it was agreed to keep medication use stable during the study period. Exclusion criteria: severe panic disorder (PDSS–SR > 12), current psychological treatment for panic disorder‐related complaints, presence of other severe mental or social problems, suicidal intention warranting treatment or likely to interfere with participation in the group course as assessed by an experienced psychologist during intake. Characteristic of the sample:
| |
| Interventions | Participants (clinical sub‐sample, n = 100) were randomly assigned to either: 1) "Don't Panic" intervention (classified as CBT, n = 50)
2) Wait list (classified as WL, n = 50)
| |
| Outcomes | Time points for assessment: baseline, post‐intervention, 6 months follow‐up Measures: Panic Disorder Severity Scale–Self Report (PDSS–SR), Mini International Neuropsychiatric Interview–Plus (MINI–Plus), Mobility Inventory (MI), sub‐scale for anxiety of the Hospital Anxiety and Depression Scale (HADS–Anxiety), Beck Depression Inventory (BDI–II) The following outcomes were used for quantitative analyses: ST‐Remission: PDSS at post‐treatment < 1 SD compared to baseline mean and below 4 (cut‐off value) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: not reported for clinical sub‐sample Continuous scale: Panic Disorder Severity Scale–Self Report (PDSS–SR, data for clinical sub‐sample available on personal communication) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A blocked randomisation scheme was used, stratified by mental health centre, subthreshold panic disorder v. mild panic disorder, and by presence v. absence of co‐occurring agoraphobia." |
| Allocation concealment (selection bias) | Low risk | "The randomisation took place after administration of the Mini International Neuropsychiatric Interview–Plus (MINI–Plus)8 and was carried out centrally by an independent third party." |
| Blinding of outcome assessment (detection bias) | High risk | ST‐Remission is calculated from the Self Report of Panic Disorder Severity Scale |
| Incomplete outcome data (attrition bias) | Low risk | All randomised patients (clinical sub‐sample) were assessed with PDSS‐SR at post‐treatment (personal communication) |
| Selective reporting (reporting bias) | High risk | Study protocol available: declared primary outcome is "incidence of DSM‐IV panic disorder." In published report: "we used the PDSS–SR and the MINI–Plus as the primary outcome measures." |
| Researcher allegiance | High risk | "We developed an early intervention for panic symptoms, called the ‘Don't Panic’ course" |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Other bias | High risk | Performance bias: WL patients are free to make use of other interventions |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 60 years, principal DSM‐IV diagnosis of panic disorder with or without agoraphobia, no additional psychological treatment until after the 2‐month follow‐up. If on psychotropic medications, on stable doses for at least 3 months prior to treatment with an agreement not to change dosage at least until after the 2‐month follow‐up Exclusion criteria: evidence of organic mental disorder, suicidality, schizophrenia, alcohol or drug dependence, cardiovascular disease, pulmonary disease, epilepsy or pregnancy Characteristic of the sample:
| |
| Interventions | Participants (n = 43) were randomly assigned to either: 1) Breathing training therapy (classified as PT, n = 24)
2) Wait list (classified as WL, n = 19)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment (week 4), 2 months follow‐up (week 12), 12 months follow‐up Measures: Panic Disorder Severity Scale (PDSS), Clinical Global Impression Scale (CGI), Anxiety Sensitivity Index (ASI), Sheehan Disability Scale (SDS), Mobility Inventory for Agoraphobia (MI‐AAL), Beck Depression Inventory (BDI), week‐by‐week changes in end‐tidal pCO₂ (mm Hg) and RR (breaths/minute) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Panic Disorder Severity Scale (PDSS) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | "An assessment battery was administered at baseline (week 0), post‐treatment (week 4), 2‐month follow‐up (week 12), and 12‐month follow‐up (week 53). It included the PDSS (Shear et al., 1997), a clinician‐rated scale of PD severity and the Clinical Global Impression Scale (CGI; Guy, 1976) (both assessed by independent raters)." It is unclear whether raters were blind to treatment allocation. |
| Incomplete outcome data (attrition bias) | High risk | 35 patients were analysed at post‐treatment (see study flow chart) |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "We devised a capnometry‐assisted breathing training therapy (BRT) that uses immediate feedback to teach patients how to raise their pCO₂ over a series of training and practice sessions." |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: 2‐site, randomised controlled trial | |
| Participants | Inclusion criteria: minimum age of 18 years, current principal DSM‐IV diagnosis (i.e. the disorder presently associated with the greatest life interference) of panic disorder with agoraphobia, being on a stable dose of psychotropic medication for at least 3 months before study initiation (if applicable) and agreement to continue this dose through the 2‐month follow‐up appointment, agreement not to initiate additional therapy until after the final follow‐up appointment. Exclusion criteria: indication of a history of bipolar disorder, psychotic disorder or suicidal intention, or current substance abuse or dependence, organic mental disorder, serious unstable medical disease, respiratory illness or seizures Characteristic of the sample:
| |
| Interventions | In a first phase of the study, participants (n = 47) were randomly assigned to 5 weekly sessions of either capnometry‐assisted breathing training (n = 24) or cognitive training (n = 23) In a second phase of the study, participants of both groups underwent 3 weekly sessions of in vivo exposure plus a 4th session at 2‐month follow‐up, therefore: 1) Capnometry‐assisted breathing training + in vivo exposure (classified as BT, n = 24)
2) Cognitive training + in vivo exposure (classified as CBT, n = 23)
| |
| Outcomes | Time points for assessment: baseline, pre‐phase 1, post‐phase 1/pre‐exposure (beginning of phase 2), post‐exposure (after the 3 weekly sessions of in vivo exposure), 2 months follow‐up (last exposure session) Measures: Panic Disorder Severity Scale (PDSS), Body Sensations Questionnaire (BSQ), Anxiety Sensitivity Index (ASI), combined measure of symptom appraisal (ASI/BSQ), Mobility Inventory for Agoraphobia (MI), Anxiety Control Questionnaire (ACQ), end‐tidal pCO₂, respiration rate (RR) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: non‐completers at termination (last exposure session) Continuous scale: although measured, detailed data are not reported LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization software was used to assign patients to condition." |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | In the CT + exposure arm, a total of 12 patients (out of 23 randomised) completed all sessions; in the CART + exposure arm, a total of 16 patients (out of 24 randomised) completed all sessions. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "CART is based on the theory that sustained levels of hypocapnia contribute to symptom development and maintenance of PD (Meuret 2008)." |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "All sessions were audio‐ or video‐taped and discussed in the weekly supervision meetings by expert clinicians to ensure that therapists adhered to the treatment protocol. A random sample of 10% of all recorded treatment sessions (10 CART and 10 CT sessions) was evaluated blindly for protocol adherence by two independent, experienced master’s‐level clinicians. In addition, 50% of the rated sessions (5 CART and 5 CT) were randomly selected and rated by another master’s‐level and one doctoral‐level clinician to assess interrater reliability. Adherence to the given model/protocol was rated high for both conditions (CART: M 6.25, SD 0.92; CT: M 5.50, SD 1.20), and ratings were not significantly different between conditions. Interrater agreement was calculated with intraclass correlation coefficients. The results suggest that coders showed high agreement (intraclass correlation [2, 1] 0.85; Shrout & Fleiss, 1979)." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 65 years, DSM‐IV‐TR diagnosis of panic disorder with agoraphobia Exclusion criteria: presence of a medical condition (pregnancy, seizure disorder, pacemaker), current use of tranquillisers or not on a stable dose of antidepressants, current substance dependence, current depression with suicidal ideation, bipolar disorder, borderline or antisocial personality disorder, history of psychosis, severe cognitive impairment Characteristic of the sample:
| |
| Interventions | Participants (n = 55) were randomly assigned to either: 1) CBT + virtual reality exposure (classified as CBT, n = 19)
2) CBT + in vivo exposure (classified as CBT, n = 18)
3) Wait list (classified as WL, n = 18)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment. Measures: Panic Disorder Severity Scale (PDSS), Mobility Inventory (MI), Bodily Sensation Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ), Panic Appraisal Inventory (PAI), Avoidance Scale of Watson and Marks The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: non‐completers Continuous scale: although measured, data cannot be used (n, mean and SD are reported only for the comparison VRET versus IVExp, both classified as CBT: comparison not feasible) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Patients were randomized with randomly permuted blocks" (personal communication) |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | "After randomization, 9 of the 55 patients declined to start the treatment. During treatment 15 patients dropped out for various reasons: medical issues (n = 2), acute crisis 2), could not experience the virtual environment as real (n = 2), had no further complaints (n = 3) and personal circumstances (n = 1). Completer analyses included the remaining sample of 31 patients who completed all treatment sessions (n = 29) or at least 80% of the sessions (n = 2). Intent‐to‐treat analyses were done with multiple imputation on the full sample (n = 46) who started at least 1 treatment session" |
| Selective reporting (reporting bias) | High risk | Study protocol available: declared primary outcomes are PDSS and MI (plus Behavioural Avoidance Test, added subsequently). Primary outcomes are not specified in published report. |
| Researcher allegiance | Low risk | "None of the authors has any conflict of interest" |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: diagnosis with primary DSM‐IV panic disorder with or without agoraphobia, minimum severity score of 5 on the 0‐ to 8‐point Anxiety Disorders Interview Schedule for DSM‐IV (ADIS‐IV‐Lifetime Version), minimum of 1 weekly panic attack. Patients were included whether or not they were taking anti‐panic medication: subjects meeting study entrance criteria while taking stable doses of medication agreed to keep medication type and dose constant throughout the study. Patients discontinued ongoing psychotherapy to gain study entrance. Patients with comorbid major depression, personality disorders and severe agoraphobia were included. Exclusion criteria: psychosis, bipolar disorder and active substance abuse (6 months remission necessary for inclusion) Characteristic of the sample:
| |
| Interventions | Participants (n = 49) were randomly assigned to either: 1) Panic focused psychodynamic psychotherapy (classified as PD, n = 26)
2) Applied relaxation training (classified as PT, n = 23)
| |
| Outcomes | Time points for assessment: baseline, termination, 2 months follow‐up, 4 months follow‐up, 6 months follow‐up, 12 months follow‐up Measures: Panic Disorder Severity Scale (PDSS), Sheehan Disability Scale (SDS), Hamilton Depression Rating Scale (HAM‐D), Hamilton Anxiety Rating Scale (HAM‐A) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: 40% reduction in PDSS at termination ST‐Dropouts: non‐completers Continuous scale: Panic Disorder Severity Scale (PDSS) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were randomly assigned using a computer generated treatment assignment list that was stratified by presence or absence of 1) comorbid current DSM‐IV major depression and 2) stable doses of antipanic medication." |
| Allocation concealment (selection bias) | Low risk | "All study staff was blinded" (personal communication) |
| Blinding of outcome assessment (detection bias) | Low risk | "Independent evaluators, blinded to subject condition and therapist orientation, assessed subjects at baseline, treatment termination, and at 2, 4, 6, and 12 months posttreatment termination" |
| Incomplete outcome data (attrition bias) | High risk | "Rates of dropout from the 12‐week randomized controlled clinical trial differed significantly between the randomly assigned treatment groups: two out of 26 (7%) panic‐focused psychodynamic psychotherapy subjects and eight out of 23 (34%) applied relaxation training subjects dropped out. The analyses described above adhered to the intention‐to‐treat principle using last observation forward to impute missing data for the primary outcome and three continuous secondary outcomes." Although a LOCF method was used, LOCF cases are many and unbalanced between arms. |
| Selective reporting (reporting bias) | Low risk | Study protocol available. All of the study's pre‐specified (primary and secondary) outcomes have been reported in the pre‐specified way. |
| Researcher allegiance | High risk | Milrod B and Busch F are co‐authors of PFPP manual (see Milrod 1997) |
| Therapist allegiance | Unclear risk | Insufficient information provided |
| Treatment fidelity | Unclear risk | "Therapists in both modalities met monthly for group supervision and received individual supervision as needed. Therapists in both modalities were monitored for adherence to treatment protocol by adherence raters in each modality with equal frequency. Three videotapes were rated for adherence per individual treatment. All therapists met predetermined adherence standards." It is unclear whether all sessions for both therapies were recorded and if the 3 videotapes monitored for adherence where chosen randomly. |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder with or without agoraphobia, drug‐free, in reasonably good health, not currently in therapy (or, in this case, able to arrange with the therapist to work within the structure of the project) Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 26) were randomly assigned to either: 1) Rational emotive therapy (classified as CT, n = 7)
2) Rational emotive therapy + biofeedback (classified as CT, n = 8)
3) Imipramine (not included, n = 7)
4) Wait list (classified as WL, n = 4)
| |
| Outcomes | Time points for assessment: baseline, mid‐treatment (3 weeks after commencement), termination (6 weeks after commencement). Measures: Minnesota Multiphasic Personality Inventory (MMPI), Millon Clinical Multiaxial Inventory (MCMI), Beck Depression Inventory (BDI), State‐Trait Anxiety Inventory (STAI) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: non‐completers Continuous scale: not measured (none of the available measures meets our inclusion criteria, see Secondary outcomes) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | "Two subjects from G3 (Imipramine arm)abandoned the study in the first three weeks of the treatment due to their inability to tolerate the side‐effects of imipramine. Thus, the number of observations was reduced to 24 [...]." Since we are not considering the imipramine arm for this review, the number of dropouts is 0 |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 20 and 60 years, DSM‐III‐R diagnosis of panic disorder with agoraphobia, express a willingness to participate in the study for a period of 3 months. If any medication was used the intake was to be held constant during the study; participants had to agree not to receive any other kind of psychiatric or psychological treatment except for any ongoing medication during the treatment. Exclusion criteria: any other psychiatric complaint in need of immediate treatment; psychotic or organic symptoms Characteristic of the sample:
| |
| Interventions | Participants (n = 46) were randomly assigned to either: 1) Applied relaxation (classified as PT, n = 15)
2) Exposure in vivo (classified as BT, n = 16)
3) Cognitive treatment (classified as CBT, n = 15)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 1 year follow‐up Measures: Agoraphobia Scale, Fear Questionnaire (FQ), Mobility Inventory for Agoraphobia (MI), Agoraphobic Cognitions Questionnaire (ACQ), Body Sensations Questionnaire (BSQ), Hamilton Anxiety Scale (HAM‐A), State‐Trait Anxiety Inventory (STAI), Hamilton Depression Scale (HAM‐D), Beck Depression Inventory (BDI), Behavior Test (BAT), Autonomic Perception Questionnaire (APQ) The following outcomes were used for quantitative analyses: ST‐Remission: clinically significant improvement* (Agoraphobia Scale criteria) at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ) LT‐Remission/Response: clinically significant improvement* (Agoraphobia Scale criteria) at 1 year follow‐up | |
| Notes | * "To assess the degree of clinically significant improvement achieved by the patients the method described by Jacobson, Follette and Revenstorf (1984) was used. On any single measure a patient’s post‐treatment or follow‐up score must be outside the range of the patient group’s pre‐treatment scores, or inside a normal group’s range, in the direction of functionality, defined as Mean ±1.96 x SD . Besides, the change must be statistically reliable. For this study we chose to apply two criteria; percentage of situations completed in the BAT, and score on the avoidance part of Agoraphobic Scale. The respective cutoff scores were: BAT: Mean 23.23, SD 14.57, criterion: 22.23 + 1.96(14.57) = 51.79, i.e. 52. Agoraphobia Scale‐Avoidance: Mean 20.56, SD 6.76, criterion 20.56 ‐ 1.96(6.76) = 7.31." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | The Agoraphobia Scale (used to determine ST‐Remission) is a self report measure |
| Incomplete outcome data (attrition bias) | Low risk | "One patient from the Exposure group dropped out after 2 sessions and was replaced. All the AR‐ and CT‐patients completed the study. At follow‐up I patient (in the AR‐group) had died, I refused participation in the assessment (E‐group), and 1 (AR‐group) had moved and was unreachable by mail or telephone. Thus, follow‐up assessment was done on 42 (93.3%) of the original patients." |
| Incomplete outcome data (attrition bias) | Low risk | (See above). Missing outcome data balanced in numbers across intervention groups; the proportion of missing outcomes compared with the observed event risk is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Ost LG is involved in conceptualisation of Applied Relaxation (see Ost 1987) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Other bias | Unclear risk | Modification of the original sample with one replacement |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 60 years, DSM‐III‐R diagnosis of panic disorder with mild or no agoraphobic avoidance, duration of the panic disorder of at least 1 year, at least 3 panic attacks during the 3 weeks baseline, panic disorder seen as the patient's primary problem, agreeing to take part in the study for 18 weeks, including pre‐ and post‐assessment, and 1 year follow‐up, and be willing to accept random allocation. If on prescribed drugs for panic disorder: (a) the dosage had to be constant for 3 months before the start of the treatment; and (b) the patient had to agree to keep the dosage constant throughout the study. Exclusion criteria: primary depression (i.e. onset before the start of the panic disorder), any other psychiatric disorder in immediate need of treatment Characteristic of the sample:
| |
| Interventions | Participants (n = 38) were randomly assigned to either: 1) Applied relaxation (classified as PT, n = 19)
2) Cognitive therapy (classified as CBT, n = 19)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 1 year follow‐up. Measures: Anxiety Disorders Interview Schedule‐Revised (ADIS‐R), Hamilton Anxiety Scale (HAM‐A), Hamilton Depression Scale (HAM‐D), panic diary, Panic Attack Scale (PAS), Beck Anxiety Inventory (BAI), State‐Trait Anxiety Inventory (STAI), Self‐Rating of Anxiety Scale (SAS), Beck Depression Inventory (BDI), Body Sensations Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ), Bodily Sensations Interpretations Questionnaire The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Body Sensations Questionnaire (BSQ) LT‐Remission/Response: high end‐state functioning* at 1 year follow‐up | |
| Notes | * "High end‐state functioning (HEF) was defined as being panic‐free and having an independent assessor rating of severity of the panic disorder of ≤2 (i.e. 'slight') on the (ADIS‐R)0‐8 scale." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information reported |
| Allocation concealment (selection bias) | Unclear risk | No information reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | "High end‐state functioning (HEF) was defined as being panic‐free and having an independent assessor rating of severity of the panic disorder of ≤2 (i.e. 'slight') on the (ADIS‐R)0‐8 scale." It is unclear whether the assessor was blind to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | 2 patients, both in the AR group, dropped out at an early stage of treatment due to scheduling difficulties. All 36 patients that completed the study were followed up 1 year later. The proportion of missing outcomes compared with the observed event risk is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Incomplete outcome data (attrition bias) | Low risk | (see above) |
| Selective reporting (reporting bias) | High risk | Study protocol unavailable. Agoraphobic Cognitions Questionnaire (ACQ) results are not reported, although this should be an administered scale according to the methods section. |
| Researcher allegiance | High risk | Ost LG is involved in conceptualisation of Applied Relaxation (see Ost 1987) |
| Therapist allegiance | Unclear risk | No information reported |
| Treatment fidelity | Unclear risk | No information reported |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 60 years, primary DSM‐IV diagnosis of panic disorder with agoraphobia, severity of at least 4 on the ADIS‐IV 0 to 8 scale, minimum of 1 year duration of the phobia. If on psychotropic medication: have been on a constant dose for at least 4 months and accept to keep the dosage constant throughout therapy. Exclusion criteria: primary major depression (i.e. onset before the PDA), current alcohol or substance abuse, psychotic or organic symptoms, ongoing psychotherapy Characteristic of the sample:
| |
| Interventions | Participants (n = 73) were randomly assigned to either: 1) Exposure in vivo (classified as BT, n = 25; after re‐randomisation of WL n = 35)
2) Cognitive behaviour therapy (classified as CBT, n = 26; after re‐randomisation of WL n = 36)
3) Wait list (classified as WL, n = 22)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 1 year follow‐up. Measures: Anxiety Disorders Interview Schedule‐IV (ADIS‐IV), Hamilton Anxiety Scale (HAM‐A), Hamilton Depression Scale (HAM‐D), Agoraphobia Scale, Mobility Inventory (MI), Fear Questionnaire (FQ), Panic Attack Scale (PAS), Anxiety Sensitivity Index (ASI), Body Sensations Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ), Beck Anxiety Inventory (BAI), State‐Trait Anxiety Inventory (STAI), Beck Depression Inventory (BDI), Quality of Life Inventory panic diary, behavioural approach tests The following outcomes were used for quantitative analyses: ST‐Remission: no longer meet DSM‐IV criteria for PDA at post‐treatment (original sample) ST‐ Response: not measured (imputed from the continuous scale for the original sample) ST‐Dropouts: non‐completers (original sample) Continuous scale: Anxiety Sensitivity Index (ASI) measured on the original sample (SDs are not reported but could be borrowed from other studies using ASI) LT‐Remission/Response: no longer meet DSM‐IV criteria for PDA at 1 year follow‐up (original + re‐randomised sample) | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | "An independent research assistant not involved with the treatment performed all the diagnostic interviews and ratings." It is unclear whether the assessor was blind to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | "Seven patients dropped out of treatment before completion; 3 (13%) in the E‐group, 2 (8%) in the CBT‐group, and 2 (9%) in the WLC‐group, a non‐significant difference." Missing outcome data balanced in numbers across intervention groups. The proportion of missing outcomes compared with the observed event risk is not enough to have a clinically relevant impact on the intervention effect estimate. |
| Incomplete outcome data (attrition bias) | High risk | "After the post‐assessment of the waiting list two patients dropped out and the remaining were randomized to the two treatment conditions with 10 in each. When the former WLC‐patients were treated 3 of the 10 randomized to the E‐group, but none in the CBT‐group, dropped out." Reason for missing outcome data likely to be related to true outcome, with imbalance in numbers for missing data across intervention groups. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "The therapy sessions were audiotaped and upon completion, three sessions were randomly selected for every patient, one from each third of the therapy, for analysis. Three licensed psychotherapists with long experience of CBT and blind to the allocation of the patients listened to the tapes and classified the sessions as either an exposure or a CBT‐session. They also rated the competency of the therapists using a modified version of the Cognitive therapy scale (Young & Beck, 1980), consisting of nine specific items and a general item (rated on a 0–6 scale). Which treatment the patient was receiving was correctly identified in 96.7% of the sessions rated by the experts, indicating a satisfying degree of treatment integrity." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 27*) were randomly assigned to either: 1) Cognitive behaviour treatment (classified as CBT, n = 14?)
2) No treatment (classified as NT, n = 13?)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment Measures: Anxiety Sensitivity Index (ASI), State‐Trait Anxiety Inventory (STAI), Panic Attack Record, physiologic measures (blood pressure, pulse rate, finger temperature) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (not imputed because number of randomised patients is unclear) ST‐ Response: not measured (not imputed because number of randomised patients is unclear) ST‐Dropouts: unclear Continuous scale: Anxiety Sensitivity Index (ASI). SDs are not reported but could be borrowed from other studies using ASI LT‐Remission/Response: not measured | |
| Notes | *It is unclear whether the reported number participants (n = 27) refers to the ITT sample or to treatment completers ("Twenty‐seven adults completed the study. [...] The subjects were randomly assigned to either the Treatment (n = 14) or Control (n = 13) conditions"). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III diagnosis of panic disorder with little or no agoraphobic avoidance Exclusion criteria: secondary diagnosis with an overall severity rating less than 2 points away from the panic disorder severity rating on the clinician's 9‐point rating scale in ADIS; any medical condition such as asthma, angina, emphysema that might have complicated the panic disorder Characteristic of the sample:
| |
| Interventions | Participants (n = 40) were randomly assigned to either: 1) Information giving + self monitoring (classified as PE, n = 20)
2) Self monitoring alone (classified as APP, n = 20)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment. Measures: daily records of panic, anxiety, depression and anticipatory fear of panic The following outcomes were used for quantitative analyses: ST‐Remission: not measured (not imputed because of skewed distribution of available continuous scale) ST‐ Response: not measured (not imputed because of skewed distribution of available continuous scale) ST‐Dropouts: non‐completers Continuous scale: panic frequency LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐IV diagnosis of panic disorder with or without agoraphobia, naive to exposure‐based CBT; at least moderate agoraphobic avoidance, panic‐related safety behaviours (e.g. medication, or standing close to an escape exit to prevent panic attacks) and catastrophic panic cognitions (e.g. "If I stay here my heart will beat even faster, and I will suffer a heart attack"), assessed with a structured panic assessment interview. Occasional medication with benzodiazepines Exclusion criteria: lifetime history of epilepsy, psychotic disorders, bipolar disorder or substance abuse, primary depressive disorder, insufficient English skills, psychopharmacological or psychotherapeutic treatment during the last 6 months Characteristic of the sample:
| |
| Interventions | Participants (n = 28) were randomly assigned to either: 1) Single session exposure‐based CBT (classified as CBT, n = 14)
2) Wait list (classified as WL, n = 14)
| |
| Outcomes | Time points for assessment: baseline (day 1), post‐treatment (day 2), follow‐up (4 weeks) Measures: Hospital Anxiety and Depression Scale, Body Sensations Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ), Mobility Inventory (MI), Faces Dot Probe Task, Stress Test The following outcomes were used for quantitative analyses: ST‐Remission: MI‐Ag score falling within the range reported for healthy control subjects ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | Mobility Inventory (used to determine ST‐Remission) is a self rated measure. |
| Incomplete outcome data (attrition bias) | Low risk | All patients were assessed at 4 weeks follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "Our single‐session treatment was a very condensed version of psychological intervention recommended for delivery in routine clinical care" |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder with moderate or severe avoidance, at least 2 panic attacks occurring in the 4 weeks prior to assessment, a score of 9 or more on the modified Fear Questionnaire, agoraphobic avoidance sub‐scale (FQ‐Ag), being unable to complete the penultimate step of a pre‐determined standardised behavioural avoidance test course conducted prior to the experimental procedure, it was possible to identify both catastrophic thoughts which occurred during panic attacks, and safety‐seeking behaviours which the patients said they carried out during the attacks to prevent the feared catastrophes. In addition, it was required that the patient rated an increase of anxiety from baseline of at least 20 points on a 100 point visual analogue scale when entering the 5‐minute individualised behaviour test. Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 18) were randomly assigned to either: 1) Cognitive behaviour therapy (classified as CBT, n = 9)
2) Habituation‐based exposure therapy (classified as BT, n = 9)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment. Measures: Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), panic frequency, Fear Questionnaire (FQ), Agoraphobic Cognitions Questionnaire (ACQ), standardised behavioural walk (BW), individualised behavioural test (BT). The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was on the basis of sampling without replacement, using sealed envelopes opened on completion of the initial assessments" |
| Allocation concealment (selection bias) | Unclear risk | It is unclear whether envelopes were opaque and sequentially numbered. |
| Blinding of outcome assessment (detection bias) | High risk | Agoraphobic Cognitions Questionnaire (ACQ), used to impute ST‐remission, is a self rated measure. |
| Incomplete outcome data (attrition bias) | Unclear risk | Missing outcome data balanced in numbers across intervention groups (1 dropout from each arm), it is unclear whether the proportion of missing outcomes compared with the observed event risk is enough to have a clinically relevant impact on the intervention effect estimate. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | Both Salkovskis PM and Clark DM are authors of a manual for CBT in panic disorder (see Clark 1986b) |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: principal DSM‐IV diagnosis of panic disorder Exclusion criteria: change in medication type or dose during the 8 weeks preceding entry, evidence of serious suicide intent, current substance abuse, current or past schizophrenia, bipolar disorder, organic mental disorder Characteristic of the sample:
| |
| Interventions | Participants (n = 54) were randomly assigned to either: 1) Cognitive behaviour therapy + respiratory training (classified as CBT, n = 18)
2) Cognitive behaviour therapy (classified as CBT, n = 20)
3) Wait list (classified as WL, n = 16)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment (12 weeks) Measures: Clinical Global Impression ‐ Severity (CGI‐S), panic diary, Shehan Patient‐Rated Scale (SPRAS), Fear Questionnaire (FQ), Anxiety Sensitivity Inde (ASI), Panic Appraisal Inventory (PAI), Beck Depression Inventory (BDI), Shehan Disability Scale (SDS), Acute Panic Inventory (API), physiological measures (vital capacity, CO₂ intake volume), psychophysiological measures (heart rate, systolic blood pressure, diastolic blood pressure) The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Inde (ASI) LT‐Remission/Response: not measured | |
| Notes | * High end‐state functioning: "A patient was classified as recovered when scores on each of three clinical dimensions (i.e. panic frequency, anxiety and phobic avoidance) fell within the normal range. Recovery criteria for the SPRAS and FQ are based on established cutoff scores reported in the literature. The recovery criterion for panic attacks was zero." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | The 3 measures used to assess the high end‐state functioning status (panic frequency, SPRAS score, FQ score) are all self reported. |
| Incomplete outcome data (attrition bias) | High risk | "Of those patients assigned to the treatment conditions (n=54), 34 were assessed at post‐treatment." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "Treatment integrity was maintained by using a structured and manualized treatment protocol (Schmidt 1994) that described specific goals and strategies for each session." Schmidt NB is among the study authors. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | High risk | "Treatment integrity was maintained by using a structured and manualized treatment protocol that described specific goals and strategies for each session." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: principal DSM‐IV diagnosis of panic disorder with or without agoraphobia (active duty military sample) Exclusion criteria: change in medication type or dose during the 8 weeks preceding entry, evidence of serious suicide intent, current substance abuse, current or past schizophrenia, bipolar disorder, organic mental disorder Characteristic of the sample:
| |
| Interventions | Participants (n = 37) were randomly assigned to either: 1) Cognitive behaviour treatment (classified as CBT, n = 25)
2) Wait list (classified as WL, n = 12)
| |
| Outcomes | Time points for assessment: baseline (week 0), post‐treatment (week 9), 3 months follow‐up (week 21) Measures: Texas Panic Attack Record Form, Shehan Patient‐Rated Scale (SPRAS), Fear Questionnaire (FQ), Shehan Disability Scale (SDS), Beck Depression Inventory (BDI) The following outcomes were used for quantitative analyses: ST‐Remission: high end‐state functioning* at post‐treatment ST‐ Response: not measured ST‐Dropouts: non‐completers Continuous scale: not measured LT‐Remission/Response: not measured | |
| Notes | * High end‐state functioning: "A patient was classified as recovered when scores on each of three clinical dimensions (i.e. panic frequency, anxiety and phobic avoidance) fell within the normal range. Recovery criteria for the SPRAS and FQ are based on established cutoff scores reported in the literature. The recovery criterion for panic attacks was set at zero." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | The 3 measures used to assess the high end‐state functioning status (panic frequency, SPRAS score, FQ score) are all self reported. |
| Incomplete outcome data (attrition bias) | High risk | "Of those patients assigned to a treatment condition (n=37), 29 were assessed at post‐treatment. Dropouts were similar across conditions, with 20% of patients in the immediate treatment condition (n=5) and 25% of patients in the delayed treatment condition (n=3) discontinuing their participation." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "Treatment integrity was maintained by utilizing a structured and manualized treatment protocol (Schmidt 1994) that described specific goals and strategies for each session." Schmidt NB is among the study authors. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | High risk | "Treatment integrity was maintained by utilizing a structured and manualized treatment protocol that described specific goals and strategies for each session." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of generalised anxiety disorder, panic disorder with or without agoraphobia and major depression Exclusion criteria: none Characteristic of the sample (panic disorder sub‐sample):
| |
| Interventions | Participants (panic disorder sub‐sample, n = 21) were randomly assigned to either: 1) Cognitive behaviour therapy (classified as CBT, n = 15)
2) Wait list (classified as WL, n = 6)
| |
| Outcomes | Time points for assessment: baseline, start of treatment, termination, 6 weeks follow‐up, 3 months follow‐up, 6 months follow‐up, 12 months follow‐up Measures: Beck Anxiety Inventory (BAI), Beck Depression Inventory (BDI) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: non‐completers Continuous scale: not measured LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 70 years, DSM‐IV diagnosis of panic disorder with or without agoraphobia, score a minimum of 15 on the Hamilton Anxiety Scale, score a maximum of 20 on the Montgomery Asberg Depression Rating Scale, symptoms lasting at least 3 months. Patients taking concurrent psychotropic medications were not excluded from the study, but were required to continue taking these medications as prescribed throughout the study period. Exclusion criteria: having received a psychological treatment for panic disorder and agoraphobia in the past 6 months Characteristic of the sample:
| |
| Interventions | Participants (n = 97) were randomly assigned to either: 1) Group CBT (classified as CBT, n = 38)
2) Individual CBT (classified as CBT, n = 37)
3) Wait list (classified as WL, n = 22)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 3 months follow‐up Measures: Hamilton Anxiety Scale (HAM‐A), Symptom Rating Test (SRT), Montgomery Asberg Depression Rating Scale (MADRS), Fear Questionnaire ‐ agoraphobia sub‐scale (FQ‐Ag), panic diary The following outcomes were used for quantitative analyses: ST‐Remission: FQ‐Ag below 10 at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Fear Questionnaire ‐ agoraphobia sub‐scale (FQ‐Ag) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | Although assessor was blind to treatment allocation, FQ (used to extract ST‐Remission), is a self rated measure |
| Incomplete outcome data (attrition bias) | High risk | "A total of n = 27 patients dropped out of treatment early failing to complete five sessions of study treatment. Group treatment had a significantly higher drop‐out rate (n=18, 47%), than either individual treatment (n=6, 16%), or waiting list (n=3, 14%)." |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Unclear risk | "For the two treatment groups all patients received the same CBT and all received identical treatment instructions with the same written treatment manual being supplied to all patients." It is unclear whether authors were involved in writing the administered manual. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder with or without agoraphobia. All subjects were required to discontinue psychotropic medication for at least 2 weeks before study entry and to refrain from using medication or any other psychotherapeutic treatment during the study. Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 66) were randomly assigned to either: 1) Cognitive behaviour treatment (classified as CBT, n = 37)
2) Non‐prescriptive treatment (classified as SP, n = 29)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 6 months follow‐up Measures: Anxiety Disorders Interview Schedule–R (ADIS‐R), panic diary, Brief Fear Questionnaire, Mobility Inventory (MI), Beck Depression Inventory (BDI), Hopkin's Symptom Checklist (SCL‐90), Sheehan Disability Scale (SDS), Hamilton Rating Scale for Anxiety (HAM‐A), Hamilton Rating Scale for Depression (HAM‐D), State‐Trait Anxiety Inventory (STAI), Anxiety Sensitivity Index (ASI), Body Sensations Questionnaire (BSQ), Agoraphobic Cognitions Questionnaire (ACQ) The following outcomes were used for quantitative analyses: ST‐Remission: panic‐free at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: although measured (panic‐free at 6 months follow‐up) data were not entered in the analyses because dropouts exceeded 30% of the originally randomised sample (see Secondary outcomes). | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | "Most pretreatment and all posttreatment and follow‐up interviews were conducted by an independent evaluator who was "blind" to the treatment condition, study aims, and methods." However, ST‐remission is defined as being panic‐free, a self rated measure. |
| Incomplete outcome data (attrition bias) | High risk | "Pretreatment data were obtained on 45 subjects (CBT=24, NPT=21). Forty‐one subjects completed posttreatment assessments (CBT=20, NPT=21)." |
| Incomplete outcome data (attrition bias) | High risk | "43 subjects completed the follow‐up assessments (CBT=23, NPT=20)." |
| Selective reporting (reporting bias) | High risk | Study protocol unavailable. The results of some measures planned in the methods section are not reported (e.g. ACQ, BSQ). |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "All treatments were supervised by one of us (MKS) in weekly meetings. The CBT sessions were rated for treatment adherence by Michelle Craske, PhD, and Karla Moras, PhD, from the Albany Stress and Anxiety Clinic. The NPT sessions were rated for absence of CBT material. The CBT intervention was rated separately for protocol adherence, general skill, and specific skill on a scale of 0 through 8. The NPT intervention was screened for absence of CBT. Thirty audiotapes were randomly selected from each condition. The mean adherence ratings for CBT sessions was 4.5 on a scale of 0 through 8. [...] There was no indication that NPT sessions 3 through 16 included CBT techniques. The NPT intervention was not rated for adherence or skill in this study." |
| Methods | Study design: randomised controlled trial, cross‐over design | |
| Participants | Inclusion criteria: DSM‐III diagnosis of panic disorder, at least 1 panic attack in the last 3 weeks, agreement to discontinue all psychotropic medications except as prescribed in the study Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | In the first phase of the treatment (before cross‐over), participants (n = unclear) were randomly assigned to either: 1) Relaxation (classified as, n = unclear)
2) Diazepam (not included, n = unclear)
3) Placebo (not included, n = unclear)
4) No treatment (classified as WL, n = unclear)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment Measures: self report diary (anxiety, mood), State‐Trait Anxiety Inventory (STAI), Profile of Mood States, physiological measures (heart rate, skin conductance) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: detailed data are not reported Continuous scale: the only available measure (STAI) is not considered among the outcomes of interest for this review (see Secondary outcomes). Furthermore, detailed data are not reported. LT‐Remission/Response: not measured | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Unclear risk | It is unclear whether the researchers involved have a vested interest for or against the psychological therapy under study (ref. 1 of study report). |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: age between 18 and 65 years, principal DSM‐III‐R diagnosis of panic disorder with or without agoraphobia, at least 1 panic attack during the past 30 days Exclusion criteria: recent change in psychotropic medications; current psychosis, bipolar disorder or substance abuse disorder Characteristic of the sample:
| |
| Interventions | Participants (n = 67) were randomly assigned to either: 1) Panic inoculation training (classified as CBT, n = 34)
2) Wait list (classified as WL, n = 33)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment (week 9), 6 months follow‐up Measures: Sheehan Patient‐Rated Anxiety Scale (SPRAS), Agoraphobia scale of the Fear Questionnaire (FQ‐Ag), Beck Depression Inventory (BDI), Anxiety Sensitivity Index (ASI), panic diary The following outcomes were used for quantitative analyses: ST‐Remission: recovery* at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI) LT‐Remission/Response: not measured | |
| Notes | * "The two groups were compared on a composite index of recovery defined as the proportion of patients attaining normal levels of functioning on all three major facets of the disorder (i.e. panic attacks, anxiety and panic‐related avoidance)." Recovery criterion for panic attack was set at 0, for anxiety it was SPRAS score < 30, for avoidance it was FQ‐Ag < 12. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | The 3 measures used to assess the high end‐state functioning status (panic frequency, SPRAS score, FQ score) are all self reported |
| Incomplete outcome data (attrition bias) | Low risk | No dropout in either group |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "A 65‐page treatment manual (Telch 1990) describes the specific goals and strategies for each session." |
| Therapist allegiance | High risk | "All sessions were conducted by one primary therapist (MJT, JL or NBS) and a graduate student assistant." As noted above, MJ Telch and NB Schmidt may have a vested interested in the success of their active treatment. |
| Treatment fidelity | Low risk | "To help protect the integrity of the treatment, therapists and their assistants followed a procedural outline for each therapy session. In addition, all treatment sessions were videotaped and randomly selected segments were rated for consistency with the written treatment protocol." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III diagnosis of generalised anxiety disorder, panic disorder or dysthymic disorder; currently receiving no psychotropic drugs (and had not been taking benzodiazepines, neuroleptic drugs or antidepressants in regular dosage for at least 4 weeks before entry to the study); willing to enter the study, in which they understood that they would receive either drug or psychological treatments for up to 10 weeks Exclusion criteria: major depressive episode or other psychiatric disorders that take diagnostic precedence over the 3 diagnoses above in the DSM‐III classification Characteristic of the panic disorder sub‐sample:
| |
| Interventions | Participants (panic disorder sub‐sample, n = 74) were randomly assigned to either: 1) Cognitive and behaviour therapy (classified as CT, n = 33)
2) Self help treatment package (classified as APP, n = 17)
3) Diazepam (not included, n = 7)
4) Dothiepin (not included, n = 7)
5) Placebo (not included, n = 10)
| |
| Outcomes | Time points for assessment: baseline, mid‐treatment (2, 4, 6 weeks), post‐treatment (10 weeks), 16 weeks follow‐up, 32 weeks follow‐up, 1 year follow‐up, 2 years follow‐up, 5 years follow‐up, 12 years follow‐up Measures: Comprehensive Psychopathological Rating Scale (CPRS), Montgomery & Asberg Depression Rating Scale (MADRS), Brief Anxiety Scale (BAS), Hospital Anxiety and Depression Scale (HADS), General Neurotic Syndrome Scale (GNSS), Life Events Schedule, Personality Assessment Schedule (PAS) The following outcomes were used for quantitative analyses: ST‐Remission: not measured ST‐ Response: not measured ST‐Dropouts: non‐completers Continuous scale: although measured, none of the available scales is considered for this review (see Secondary outcomes) LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomised treatments were indicated by opening a sealed envelope once patients satisfied the inclusion criteria for the study." |
| Allocation concealment (selection bias) | Unclear risk | It is unclear whether envelopes were opaque and sequentially numbered |
| Incomplete outcome data (attrition bias) | Low risk | Considering only panic disorder patients allocated to either CBT (n = 33) or self help treatment package (n = 17), 3 patients were lost at post‐treatment assessment (personal communication: 2 patients in the CBT arm, 1 patient in the self help arm). Therefore, missing outcome data are low in number and balanced across intervention groups. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐III‐R diagnosis of panic disorder with or without agoraphobia, at least 2 DSM‐III‐R‐defined panic attacks per week over a 2‐week baseline period. Subjects were asked to refrain from receiving any other psychological treatment for panic, phobia or depression during the study until after the 6‐week follow‐up. Subjects taking regularly prescribed medications were asked not to alter their medication regimen during the programme, and all subjects were asked to refrain from taking discretionary medication. Exclusion criteria: none Characteristic of the sample:
| |
| Interventions | Participants (n = 48) were randomly assigned to either: 1) Cognitive treatment (classified as CT, n = 14)
2) Performance treatment (classified as BT, n = 12)
3) Combined treatment (classified as CBT, n = 13)
4) Delayed treatment (classified as WL, n = 9)
| |
| Outcomes | Time points for assessment: baseline, post‐treatment, 6 weeks follow‐up, 1 to 2 years follow‐up Measures: panic diary, Self‐Efficacy Scales for Agoraphobia (SESA), Fear Questionnaire (FQ), panic coping self efficacy, Agoraphobic Cognitions Questionnaire (ACQ), Body Sensations Questionnaire (BSQ), Beck Depression Inventory (BDI) The following outcomes were used for quantitative analyses: ST‐Remission: panic‐free at post‐treatment ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Agoraphobic Cognitions Questionnaire (ACQ) LT‐Remission/Response: panic‐free at 1 to 2 years follow‐up | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | Panic frequency is a self rated measure |
| Incomplete outcome data (attrition bias) | Low risk | "All Ss completed the treatment program; there were no dropouts in any treatment condition." |
| Incomplete outcome data (attrition bias) | Unclear risk | Among the 39 subjects allocated to the 3 active intervention arm, 34 were assessed at 1 to 2‐year follow‐up. Dropouts (n = 5) were 2/14 in cognitive treatment group, 2/12 in the performance treatment group and 1/13 in the combined treatment group. Missing outcome data are balanced across intervention groups. It is unclear whether the proportion of missing outcomes compared with the observed event risk is enough to have a clinically relevant impact on the intervention effect estimate. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable |
| Researcher allegiance | High risk | "The performance‐based treatment was an office‐based adaptation of guided mastery treatment (Williams 1990; Williams, Dooseman & Kleifield 1984; Williams & Zane 1989; Zane & Williams 1993), which emphasizes the importance of performance successes in helping people gain a sense of mastery and self‐efficacy." Williams SL is among the study authors. |
| Therapist allegiance | Unclear risk | Insufficient information provided |
| Treatment fidelity | Low risk | "All treatment sessions were audiotaped, and for each treatment condition, one tape from each therapist was chosen randomly, and all therapist statements on it were transcribed and assembled into sets containing five consecutive statements. Two assistants trained in the coding manual independently, coded the sets of statements, while remaining unaware of Ss' assigned treatment condition and of the hypotheses under investigation. Based on the codes of one randomly chosen coder, in the performance treatment sessions, 72% of the sets of therapist statements contained performance interventions and 0% cognitive interventions. Sets of therapist statements in the cognitive treatment sessions contained 58% cognitive interventions and 0% performance interventions. Combined treatment sessions contained 54% performance interventions and 29% cognitive interventions." |
| Methods | Study design: randomised controlled trial | |
| Participants | Inclusion criteria: DSM‐IV diagnosis of panic disorder with or without agoraphobia, willing to accept an 8‐week treatment delay if assigned to the wait list Exclusion criteria: history of schizophrenia, bipolar disorder, dementia, alcohol or drug abuse, current use of medications with pronounced sympathetic, parasympathetic or respiratory effects, current score on the BDI exceeding 30, current suicidality Characteristic of the sample:
| |
| Interventions | Participants (n = 74) were randomly assigned to either: 1) Lower‐CO₂ breathing retraining (classified as PT, n = 19)
2) Raise‐CO₂ breathing retraining (classified as PT, n = 28)
3) Wait list (classified as WL, n = 27)
| |
| Outcomes | Time points for assessment: baseline, 1‐month follow‐up (coincides with end of wait list), 6‐month follow‐up Measures: Panic Disorder Severity Scale (PDSS), Anxiety Sensitivity Index (ASI), Beck Depression Inventory (BDI), Mobility Inventory for Agoraphobia (MI), Agoraphobic Cognitions Questionnaire (ACQ), Anxiety Control Questionnaire, Beck Anxiety Inventory (BAI), Body Sensations Questionnaire (BSQ) The following outcomes were used for quantitative analyses: ST‐Remission: not measured (imputed from continuous scale) ST‐ Response: not measured (imputed from continuous scale) ST‐Dropouts: non‐completers Continuous scale: Anxiety Sensitivity Index (ASI). Note that reported SDs are uncommonly low, so we considered them as being SEs. LT‐Remission/Response: not measured | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | ASI is a self rated measure |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts at 1‐month follow‐up (see study flow chart) |
| Selective reporting (reporting bias) | High risk | Study protocol available. PDSS scores at 1‐month follow‐up (primary outcome) are not reported. |
| Researcher allegiance | Low risk | To our knowledge, the researchers involved do not have a vested interest for or against the psychological therapy under study. |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Low risk | "All sessions were audiotaped. Of the 50 treatment completers, the session for 20 were randomly selected and rated for therapist competence and adherence. Overall competence ratings of all therapists ranged from 3 (good) to 5 (excellent). The mean adherence rating as measured by application of respiratory behavioral techniques was 5.35 (SD 0.67), with rating of 6 being excellent." |
3W: third‐wave
AAAS: African American Acculturation Scale ‐ Short Form
AAQ: Acceptance and Action Questionnaire
ACQ: Agoraphobic Cognitions Questionnaire
ADIS–IV: Anxiety Disorders Interview Schedule–IV
API: Acute Panic Inventory
APP: attention/psychological placebo
APQ: Autonomic Perception Questionnaire
AR: applied relaxation
ART: applied relaxation training
ASI: Anxiety Sensitivity Index
ATQ: Attitude Toward Treatment Questionnaire/Automatic Thoughts Questionnaire
AWS: Anxiety and Willingness Scale
BAI: Beck Anxiety Inventory
BATs: Behavioral Avoidance Tests
BBSIQ: Brief Body Sensations Interpretation Questionnaire
BDI: Beck Depression Inventory
BSI: Brief Symptom Inventory
BSQ: Body Sensations Questionnaire
BT: behaviour therapy
CART: capnometry‐assisted breathing training
CBT: cognitive behaviour therapy
CCLAS: Anxiety Scale of the Cognitions Checklist
CGI: Clinician Global Impression
CT: cognitive training
DPAR: Daily Panic Attack Records
DSI: Depressive Symptoms Inventory
DSM: Diagnostic and Statistical Manual of Mental Disorders
DSQ: Diagnostic Symptom Questionnaire
ECQ: Emotional Control Questionnaire
EMDR: eye movement desensitisation and reprocessing
FQ: Fear Questionnaire
FQ‐Ag: Fear Questionnaire‐Agoraphobia Subscale
FSS‐IZZ: Fear Surrey Schedule‐III
GNSS: General Neurotic Syndrome Scale
HAM‐D: Hamilton Depression Scale
HARS: Hamilton Anxiety Rating Scale
HARS‐R: Hamilton Anxiety Rating Scale ‐ Revised
HEF: high end‐state functioning
HR: heart rate
HRV: heart rate variability
IBT: Irrational Belief Test
ICD‐10: International Classification of Diseases
IET: Interoceptive Exposure Test
ITT: intention‐to‐treat
IVExp: in vivo exposure
LEAS: Levels of Emotional Awareness Scale
LOCF: last observation carried forward
LT: long‐term
MAO: monoamine oxidase
MCMI: Millon Clinical Multiaxial Inventory
MMPI: Minnesota Multiphasic Personality Inventory
NT: no treatment
OCD: obsessive compulsive disorder
OQ: Outcome Questionnaire
PACQ: Panic Cognitions Questionnaire
PAI: Panic Appraisal Inventory
PARS: Phobic Avoidance Rating Scale
PAS: Panic Agoraphobia Scale/Personality Assessment Schedule
PASQ: Panic Symptoms Questionnaire
PBQ: Panic Belief Questionnaire
PCT: panic control therapy
PD/A: Panic disorder with or without agoraphobia
PDS‐MI: Panic Disorder Scale and Mobility Inventory
PDSS: Panic Disorder Severity Scale
PE: psychoeducation
PFPP: panic focused psychodynamic therapy
PPGAS: Panic, Phobia and Generalized Anxiety Scale
PQ: Presence Questionnaire
PSEQ: Panic Self‐Efficacy Questionnaire
PSWQ: Penn State Worry Questionnaire
PT: physiological therapies
PTSD: post‐traumatic stress disorder
QOLI: Quality of Life Inventory
RR: respiration rate
SAS‐SR: Social Adjustment Scale‐Self‐Report
SCL: Symptom Check List
SD: standard deviation
SE: standard error
SESA: Self‐Efficacy Scales for Agoraphobia
SP: supportive psychotherapy
SPRAS: Sheehan Patient‐Rated Anxiety Scale
SSQ: Simulation Sickness Questionnaire
ST: short‐term
STAI: State–Trait Anxiety Inventory
SUD: Subjective Units of Discomfort
TAU: treatment as usual
VLQ: Valued Living Questionnaire
VRET: virtual reality exposure therapy
WBSI: White Bear Suppression Inventory
WL: wait list
WSA: Work and Social Adjustment scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Mixed sample. More than 20% of patients are under 18 (personal communication) [Ongoing study] | |
| Drug versus placebo versus CBT versus CBT + drug versus CBT + placebo. In the related study exploring EFT versus CBT, not all patients in the EFT arm were randomised. | |
| All participants are required to have a comorbid personality disorder [Ongoing study] | |
| Assignment to WL was not randomised | |
| Quasi‐randomised design (personal communication) | |
| Quasi‐randomised design (personal communication) | |
| The study focuses on refractory patients | |
| The study focuses on refractory patients | |
| Since data for the intervention arms include data from re‐randomised WL patients, data for WL arm cannot be extracted (double‐count): the 3 remaining arms would be BT(I) versus BT(E) versus BT(I+E). Comparison not feasible. Randomisation probably not respected: "twenty patients left the trial before week 4 and were replaced", "the final sample of 80 patients included 10 of the WL who were re‐randomised". Number of patients originally randomised to each arm unclear. Assessment of the original arms (without the re‐randomised and the substitutes) not reported. | |
| Replacements are not evenly distributed and constitute more than 15% of the final sample | |
| Replacements constitute 24.5% of the final sample | |
| The study explicitly focuses on agoraphobia, reporting that only 73% of participants had a comorbid panic disorder. We considered studies focusing on agoraphobia, rather than panic disorder, when it could be safely assumed that at least 80% of the participants were suffering from panic disorder. |
BT: behaviour therapy
CBT: cognitive behaviour therapy
EFT: emotion focused therapy
WL: wait list
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised controlled trial |
| Participants | 35 patients with a diagnosis of panic disorder (DSM IV‐TR) |
| Interventions | CBT versus PD versus NT (usual care) |
| Outcomes |
|
| Notes | Only abstract available. No reply after trying to contact the author at the available email addresses. |
| Methods | Randomised controlled trial |
| Participants | Mixed sample (diagnosis for depressive and/or anxiety related disorders according the Anxiety Disorders Interview Schedule) |
| Interventions | CBT versus 3W (each administered in 8 weekly group therapy sessions) |
| Outcomes |
|
| Notes | Only abstract available. No reply after trying to contact the author at the available email addresses. |
| Methods | Unclear |
| Participants | 56 patients with chronic panic disorder |
| Interventions | BT + SMT (self mastery training) versus BT + APP (imaginal rehearsal) |
| Outcomes |
|
| Notes | Only abstract available. No reply after trying to contact the author at the available email addresses. |
| Methods | Allocation: randomised |
| Participants | 72 patients, age 18 years or older, diagnosis of agoraphobia, score on Mobility Inventory "Alone" of 2.5 or more |
| Interventions | TFT (thought field therapy: not included) versus CBT versus WL |
| Outcomes | Change in agoraphobic situation scores in ADIS. Among secondary outcomes: MI, ACQ, BSQ, BDI, BAI. |
| Notes | (Personal communication) |
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | Full report not retrievable. No reply after trying to contact the author at the available email addresses. |
| Methods | Allocation: randomised |
| Participants | Age 18 to 70 years, DSM‐IV diagnosis criteria for primary PD with or without agoraphobia, history of at least 1 spontaneous panic attack per week within the month prior to study entry |
| Interventions | CBT versus PD versus PT |
| Outcomes | Panic Disorder Severity Scale (PDSS) |
| Notes | Only protocol available. Study completed but not yet published. |
| Methods | Unclear |
| Participants | Unclear |
| Interventions | Unclear |
| Outcomes | Unclear |
| Notes | Full report not retrievable. No reply after trying to contact the author at the available email addresses. |
| Methods | Randomised controlled trial |
| Participants | 30 patients with generalised anxiety or panic disorder |
| Interventions | CBT versus NT |
| Outcomes |
|
| Notes | Only abstract. No reply after trying to contact the author at the available email addresses. |
| Methods | Unclear |
| Participants | 58 patients with the DSM‐III‐R diagnosis of panic disorder with and without agoraphobia |
| Interventions | CBT versus PT versus CBT+Imipramine versus BT + imipramine |
| Outcomes |
|
| Notes | Only abstract. No reply after trying to contact the author at the available email addresses. |
| Methods | Randomised controlled trial |
| Participants | 12 patients with a "DSM‐IV diagnosis of anxiety disorders for a minimum of 6 months as determined by independent clinicians on clinical interviews." |
| Interventions | Experiential‐cognitive therapy (ECT) versus CBT versus WL |
| Outcomes |
|
| Notes | The diagnosis of participants is unclear. No reply after trying to contact the author at the available email addresses. |
| Methods | Randomised controlled trial |
| Participants | 36 patients (age 35 to 53) with a diagnosis of panic disorder with agoraphobia |
| Interventions | CBT (12 sessions) versus CBT plus virtual reality exposure (8 sessions) versus WL |
| Outcomes |
|
| Notes | Only abstract. Maybe continuation of Vincelli 2003a. No reply after trying to contact the author at the available email addresses. |
3W: third‐wave
ACQ: Agoraphobic Cognitions Questionnaire
ADIS: Anxiety Disorders Interview Schedule
APP: attention/psychological placebo
BAI: Beck Anxiety Inventory
BDI: Beck Depression Inventory
BSQ: Body Sensations Questionnaire
BT: behaviour therapy
CBT: cognitive behaviour therapy
DSM: Diagnostic and Statistical Manual of Mental Disorders
FQ: Fear Questionnaire
HAM‐A: Hamilton Anxiety Rating Scale
HAM‐D: Hamilton Depression Scale
PAAAS: Panic and Anticipatory Anxiety Scale
PD: psychodynamic therapies
PDSS: Panic Disorder Severity Scale
PT: physiological therapies
MI: Mobility Inventory
NT: no treatment
SMT: self mastery training
STAI: State‐Trait Anxiety Inventory
WL: wait list
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | NCT01243606 |
| Methods | Allocation: randomised |
| Participants | Age 18 years or older, fluent in the English language, who have a principal DSM‐IV diagnosis of SAD, PD/A, GAD or OCD |
| Interventions | CBT (disorder specific) versus CBT (unified protocol) versus WL |
| Outcomes |
|
| Starting date | December 2010 |
| Contact information | David H Barlow: [email protected] Todd J Farchione: [email protected] |
| Notes | Completion expected by December 2014 |
| Trial name or title | NCT01677429 |
| Methods | Allocation: randomised |
| Participants | Age 18 to 45 years, clinical diagnosis of panic disorder, stable on the same drug and dosage for at least 1 month |
| Interventions | BT (with VR balance challenge) versus BT (without VR balance challenge) versus CBT |
| Outcomes |
|
| Starting date | September 2012 |
| Contact information | Revital Amiaz: [email protected] Efrat Czerniak: [email protected] |
| Notes | Completion expected by September 2013 |
| Trial name or title | DRKS00004386 |
| Methods | Study type: interventional |
| Participants | Age 18 or older, clinical diagnosis of panic disorder with or without agoraphobia (ICD‐10: F.41.0 or F40.01), positive screening questionnaires, sufficient German language skills, private telephone |
| Interventions | CBT versus NT |
| Outcomes | Severity of anxiety, measured by the Beck Anxiety Inventory (BAI) |
| Starting date | October 2012 |
| Contact information | Thomas Hiller: [email protected]‐jena.de |
| Notes | Completion expected by Spring 2015 |
| Trial name or title | NCT01606592 |
| Methods | Allocation: randomised |
| Participants | Age between 18 and 60, DSM‐V diagnosis of panic disorder (with or without agoraphobia), willingness to stop other ongoing psychotherapy treatments and to refrain from non‐study treatments during follow‐up |
| Interventions | Randomised CBT/PD versus chosen CBT/PD versus WL |
| Outcomes |
|
| Starting date | January 2010 |
| Contact information | Not specified |
| Notes | Completion expected by 2017 |
| Trial name or title | NCT01680237 |
| Methods | Allocation: randomised |
| Participants | Age between 18 and 65 years, diagnosis of panic disorder with agoraphobia |
| Interventions | CBT versus BT |
| Outcomes | Change (from baseline) in the Mobility Inventory |
| Starting date | October 2011 |
| Contact information | Tobias Teismann: [email protected] Juergen Margraf: [email protected] |
| Notes | Completion expected by August 2015 |
ADIS: Anxiety Disorders Interview Schedule
BAI: Beck Anxiety Inventory
BT: behaviour therapy
CBT: cognitive behaviour therapy
CGI: Clinical Global Impression
DSM: Diagnostic and Statistical Manual of Mental Disorders
GAD: generalised anxiety disorder
HAM‐A: Hamilton Rating Scale for Anxiety
ICD‐10: International Classification of Diseases
NT: no treatment
OC: obsessive compulsive disorder
PAS: Panic and Agoraphobia Scale
PD: psychodynamic therapies
PD/A panic disorder with/without agoraphobia
PDSS: Panic Disorder Severity Scale
SAD: social anxiety disorder
SIGH‐A/SIGH‐D: Structured Interview Guide for the Hamilton Anxiety and Depression Rating Scale
VR: virtual reality
WL: wait list
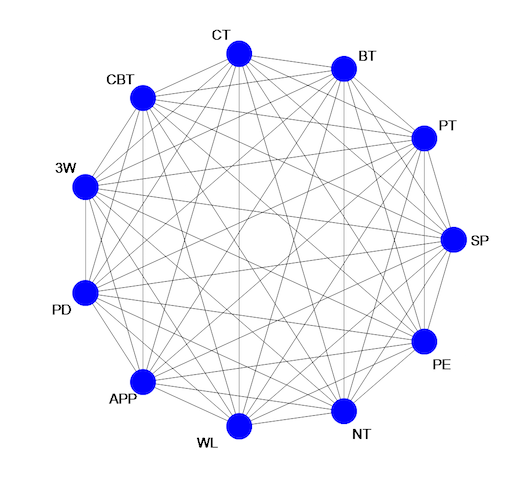
Ideal network of included treatment and control conditions.
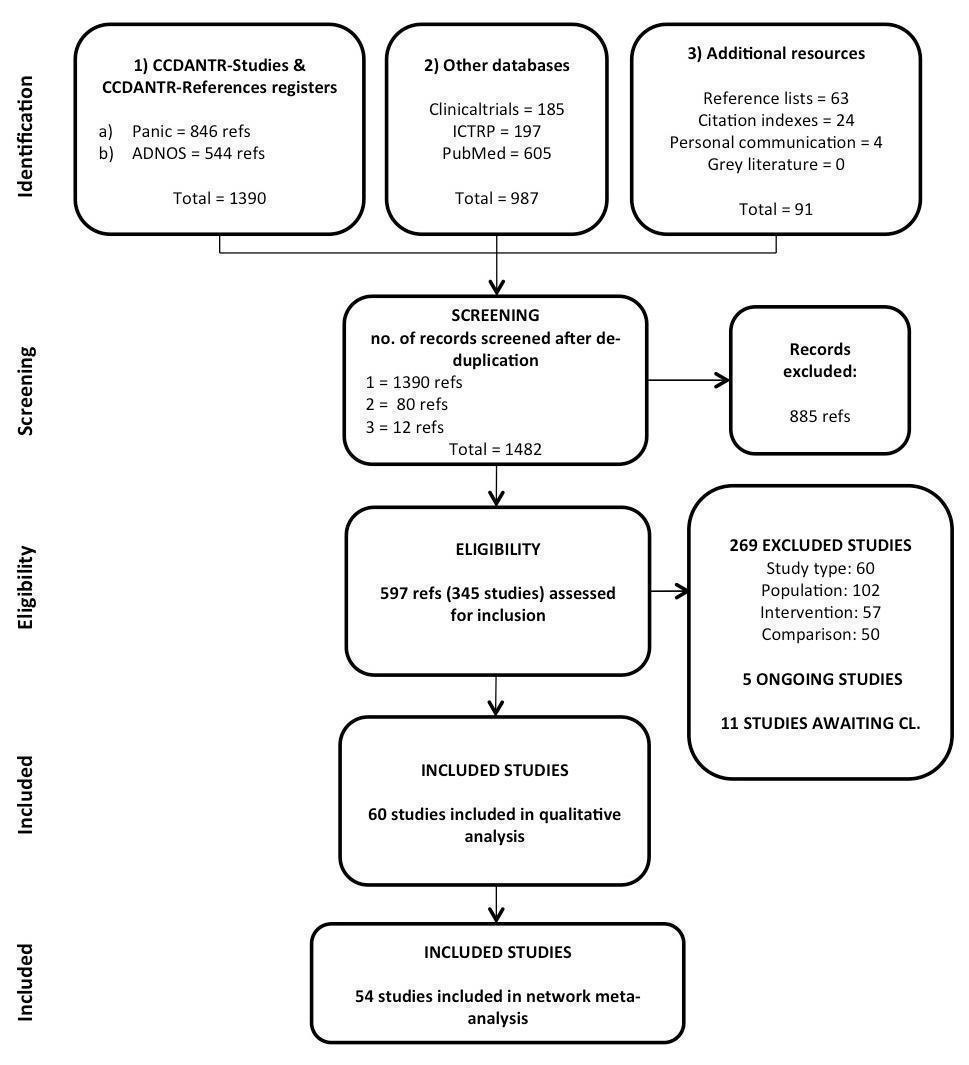
Study selection process: PRISMA flow diagram

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary. Note that we left the boxes empty when the RoB assessment was not applicable (e.g. in the case of incomplete outcome data in the long term when the study did not report any long term measure that could be included in the analyses).

Short‐term remission: network plot

Short‐term remission: forest plot for the comparison WL vs CBT
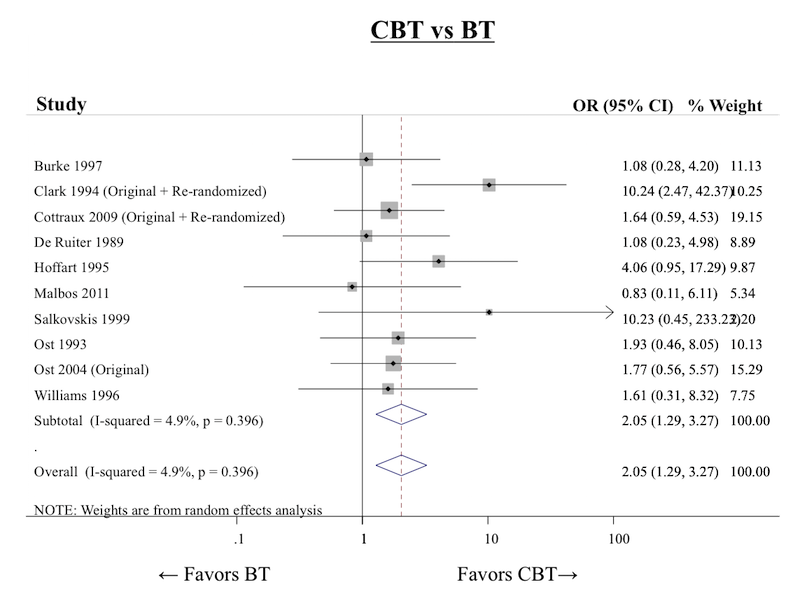
Short‐term remission: forest plot for the comparison CBT vs BT
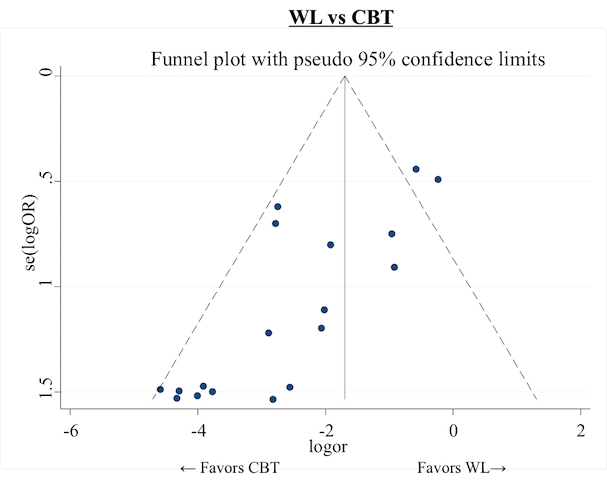
Short‐term remission: funnel plot for the comparison CBT vs WL
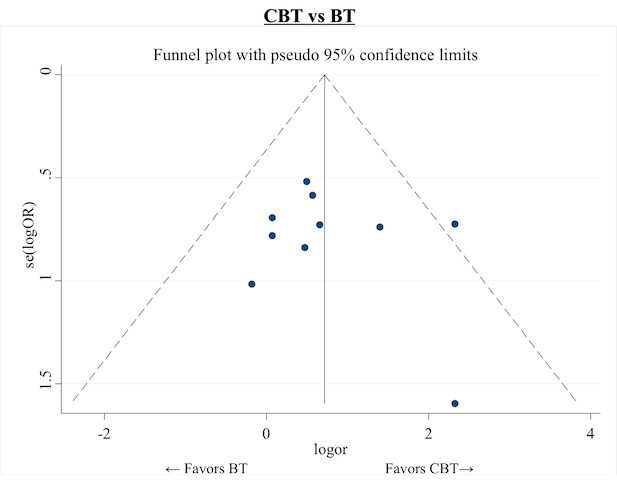
Short‐term remission: funnel plot for the comparison CBT vs BT
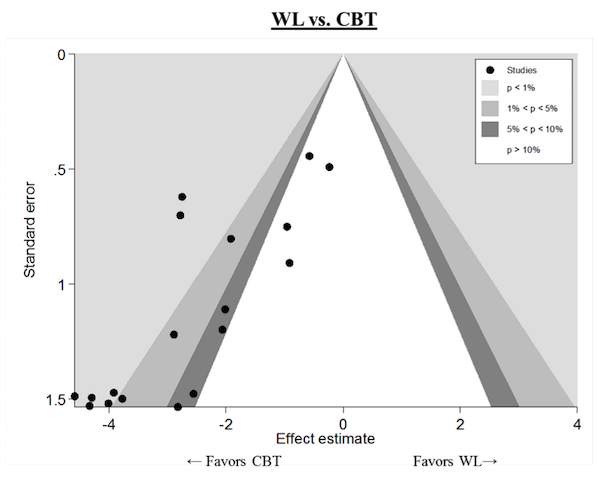
Short‐term remission: contour‐enhanced funnel plot for the comparison CBT vs WL

Short‐term remission: inconsistency factors for the network

Short‐term response: network plot

Short‐term response: forest plot for the comparison WL vs CBT

Short‐term response: forest plot for the comparison CBT vs BT

Short‐term response: funnel plot for the comparison WL vs CBT
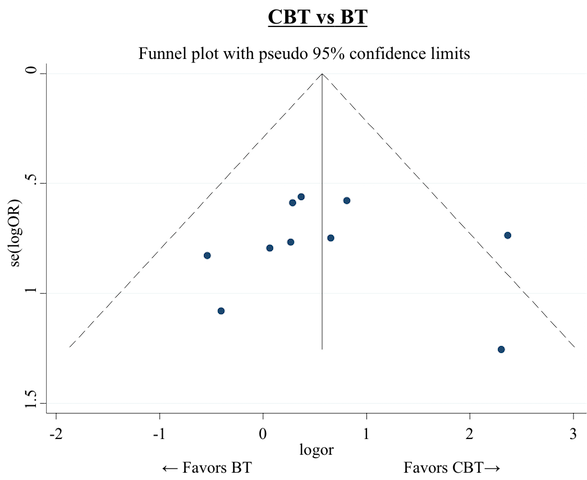
Short‐term response: funnel plot for the comparison CBT vs BT
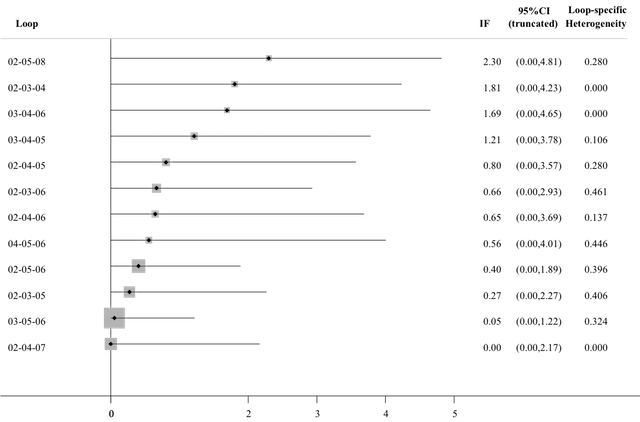
Short‐term response: inconsistency factors for the network

Short‐term dropouts: network plot

Short‐term dropouts: forest plot for the comparison WL vs CBT
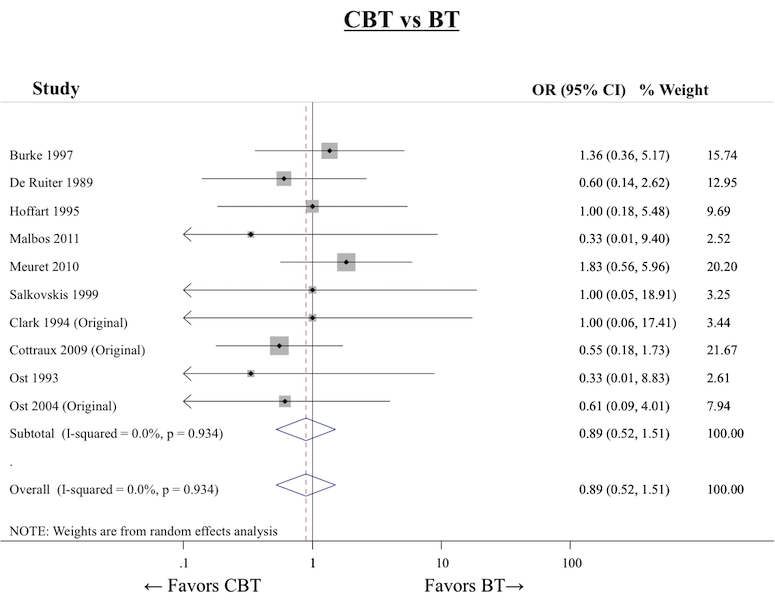
Short‐term dropouts: forest plot for the comparison CBT vs BT
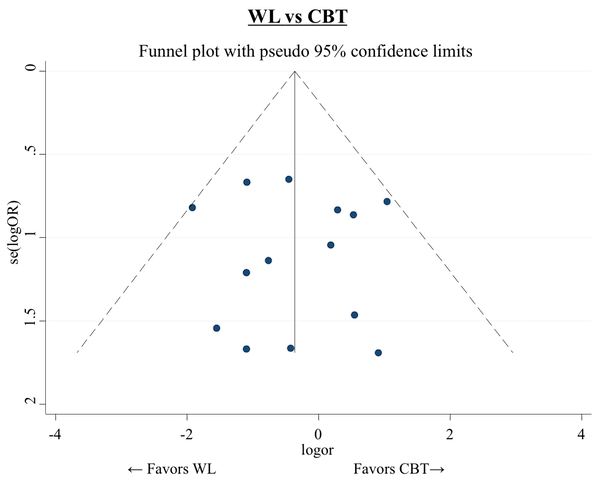
Short‐term dropouts: funnel plot for the comparison WL vs CBT
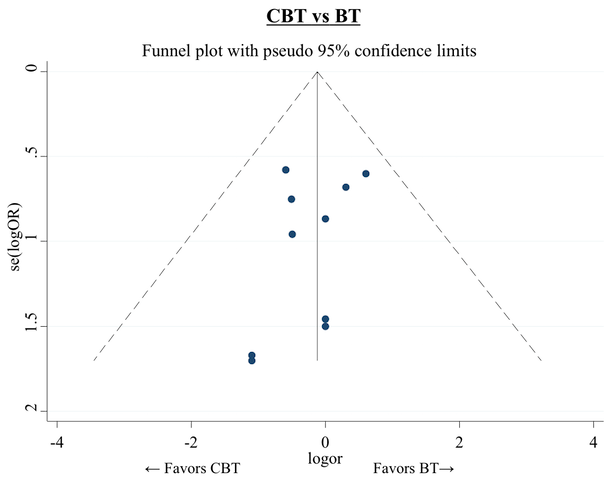
Short‐term dropouts: funnel plot for the comparison CBT vs BT
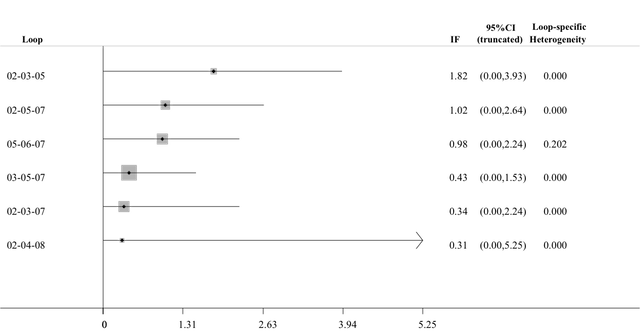
Short‐term dropouts: inconsistency factors for the network

Short‐term improvement: network plot
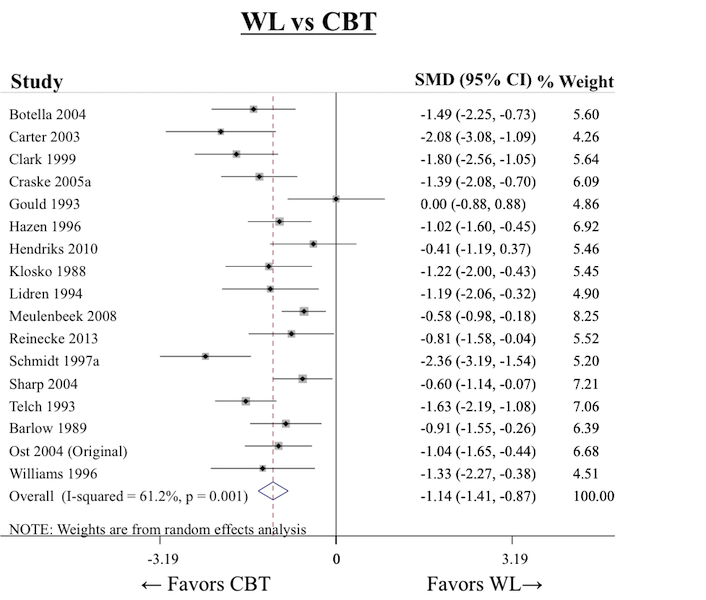
Short‐term improvement: forest plot for the comparison WL vs CBT
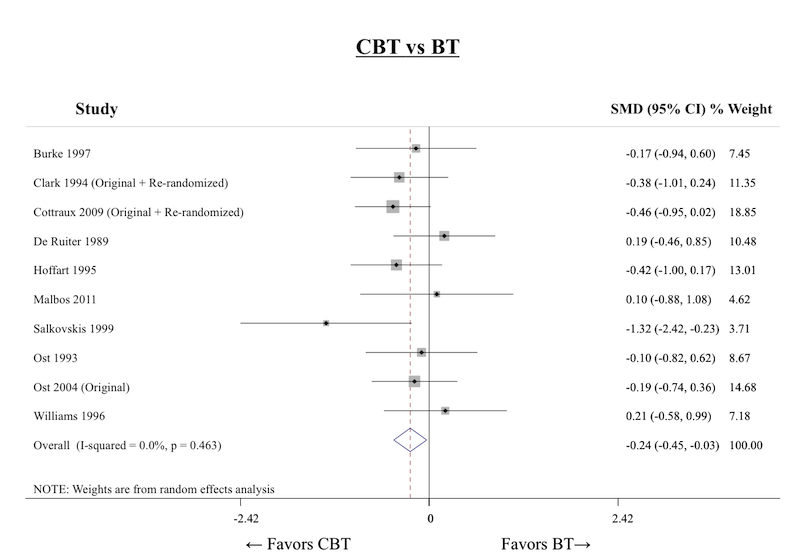
Short‐term improvement: forest plot for the comparison CBT vs BT

Short‐term improvement: funnel plot for the comparison WL vs CBT
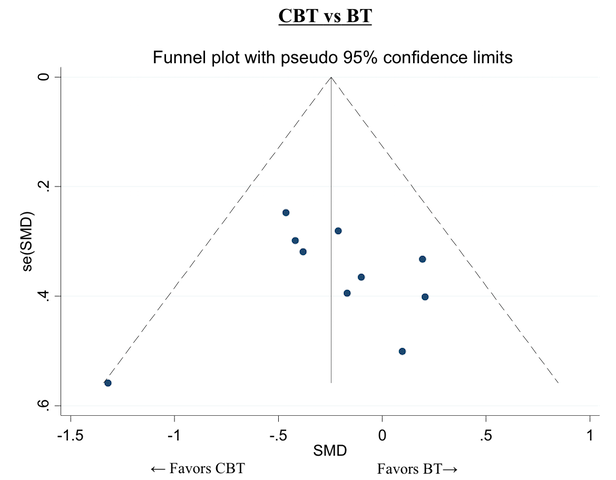
Short‐term improvement: funnel plot for the comparison CBT vs BT

Short‐term improvement: inconsistency factors for the network

Long‐term remission/response: network plot

Long‐term remission/response: inconsistency factors for the network

Subgroup analysis: number of treatment sessions, forest plot for the comparison WL vs CBT
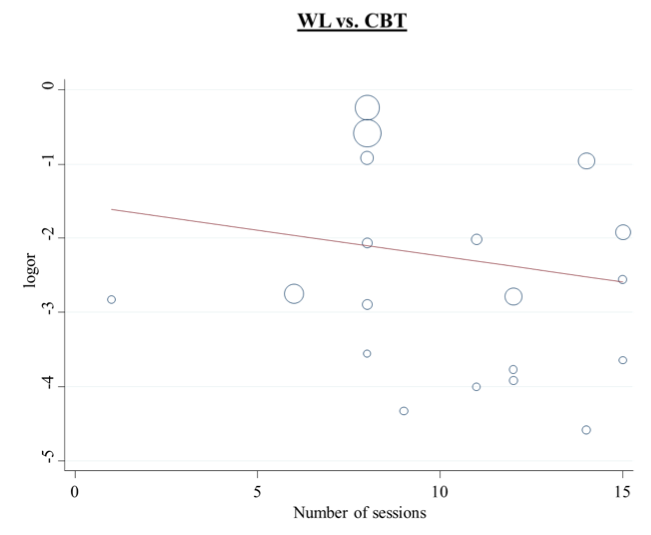
Subgroup analysis: number of treatment sessions, regression line for the comparison WL vs CBT

Subgroup analysis: number of treatment sessions, forest plot for the comparison CBT vs BT

Subgroup analysis: number of treatment sessions, regression line for the comparison CBT vs BT
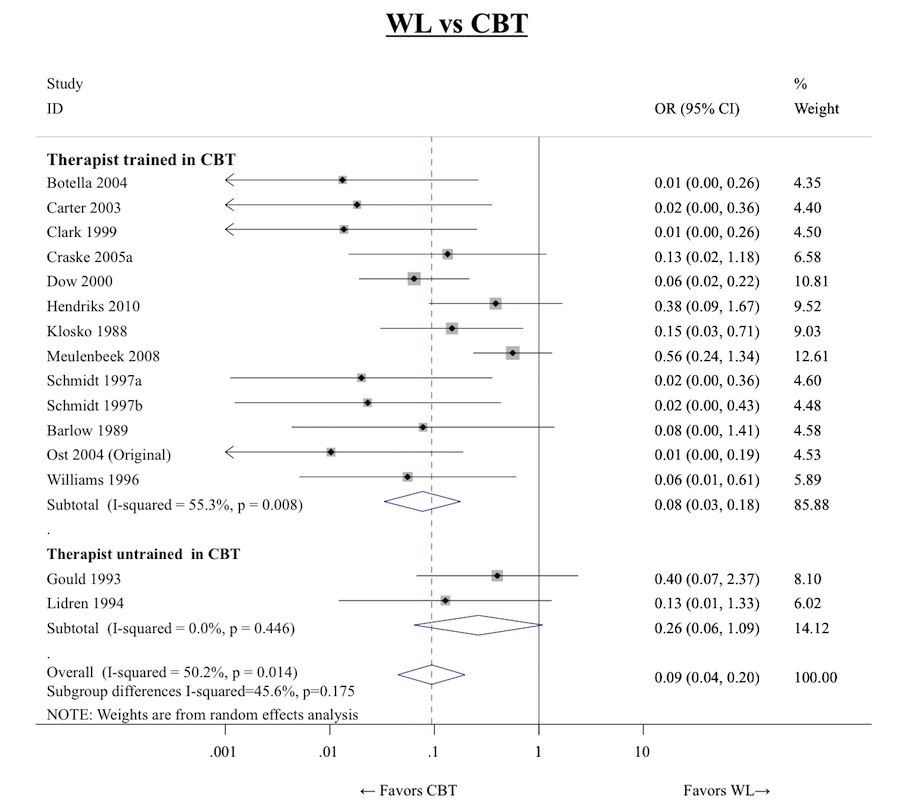
Subgroup analysis: therapist training, forest plots for the comparison WL vs CBT

Subgroup analysis: therapist training, forest plot for the comparison CBT vs BT
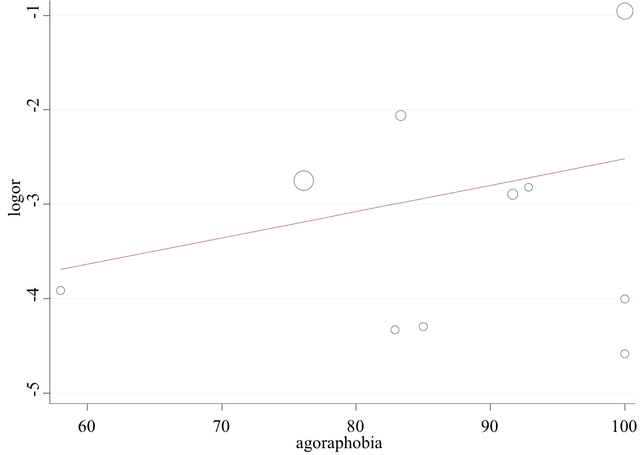
Subgroup analysis: percentage of agoraphobic patients, regression line for the comparison WL vs CBT

Subgroup analysis: percentage of depressed patients, regression line for the comparison WL vs CBT

Subgroup analysis: percentage of drug‐treated patients, regression line for the comparison WL vs CBT

Sensitivity analyses: network plot for short‐term remission excluding from the analyses group therapy trials

Sensitivity analyses: forest plot for the comparison WL vs CBT excluding group therapy trials

Sensitivity analyses: forest plot for the comparison CBT vs BT excluding group therapy trials
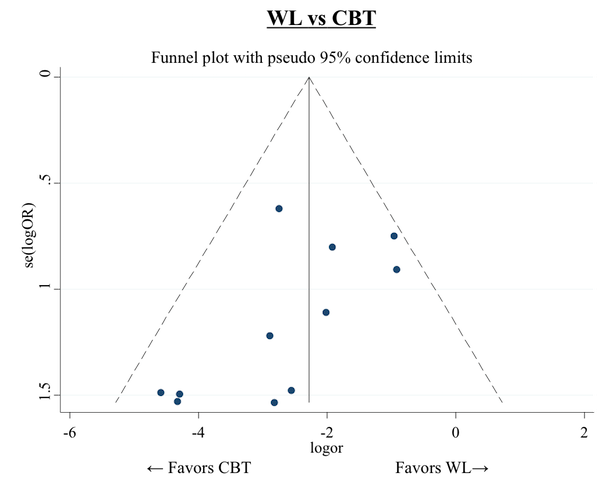
Sensitivity analyses: funnel plot for the comparison WL vs CBT excluding group therapy trials
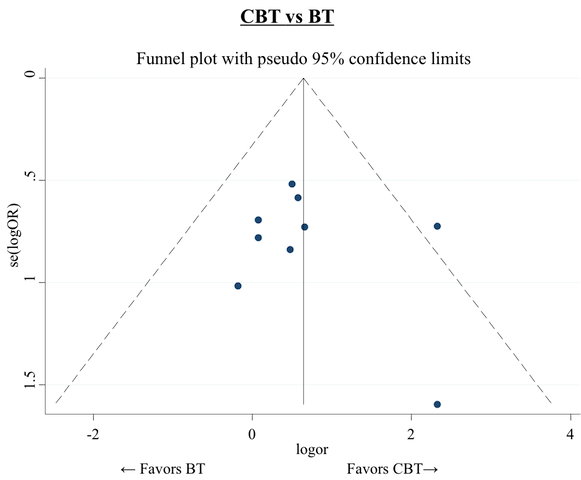
Sensitivity analyses: forest plot for the comparison CBT vs BT excluding group therapy trials

Sensitivity analyses: inconsistency factors for the network of short‐term remission excluding from the analyses group therapy trials

Sensitivity analyses: network plot for short‐term remission excluding from the analyses trials in which a concomitant pharmacotherapy is allowed

Sensitivity analyses: network plot for short‐term remission excluding from the analyses trials in which pharmacotherapy stabilisation was not required
| Cognitive behaviour therapy compared to no treatment for panic disorder with or without agoraphobia in adults | |||||
| Patient or population: adult patients with panic disorder with or without agoraphobia Setting: outpatients | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| No treatment (NT) | Cognitive‐behavioral therapy (CBT) | ||||
| Short‐term remission (follow‐up: mean 3 months) | Study population | OR 2.78 | No direct evidence available: indirect evidence based on 357 participants (2 studies via CT; 5 studies via PT)a | ⊕⊝⊝⊝ | |
| 36 per 100 | 61 per 100 | ||||
| Short‐term response (follow‐up: mean 3 months) | Study population | OR 7.14 | No direct evidence available: indirect evidence based on 357 participants (2 studies via CT; 5 studies via PT)a | ⊕⊝⊝⊝ | |
| 36 per 100 | 80 per 100 | ||||
| Short‐term dropouts (follow‐up: mean 3 months) | Study population | OR 6.25 | No direct evidence available: indirect evidence based on 278 participants (4 studies via PT)a | ⊕⊝⊝⊝ | |
| 1 per 100 (no events were observed in the available direct evidence: this percentage was assumed in order to calculate the corresponding risk) | 6 per 100 | ||||
| Long‐term remission/response (follow‐up: mean 12 months) | No data available for this comparison | ‐ | ‐ | ‐ | ‐ |
| Short‐term improvement as measured on a continuous scale (follow‐up: mean 3 months) | The mean short‐term improvement as measured on a continuous scale in the control group was 0 | The mean short‐term improvement, measured on a continuous scale as SMD (NMA results), was ‐0.83 (95% CI ‐1.5 to ‐0.16), indicating a large effect size in favour of CBT | ‐ | 27 participants | ⊕⊕⊝⊝ |
| Reported ORs are derived (as reciprocal values) from the results of network meta‐analyses presented in Table 1, Table 4 and Table 7 (for ST‐remission and ST‐response we used the results of NMA adjusted for SSE). Reported SMD is derived from the results of network meta‐analysis presented in Table 10. aIndirect comparison is performed using all possible intermediate comparisons in the network. For brevity we report the number of studies contributing indirect evidence only via a single intermediate comparator. *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| We downgraded the quality of the evidence one step at a time when one or more of the following criticisms was present: 1Only indirect evidence is available for this outcome. 2Wide 95% CI. 3The risk of bias of indirect evidence is often unclear. 4The risk of bias in the included study was unclear in almost every domain. 5Only one study, with a small sample size, available for direct comparison. | |||||
| Cognitive behaviour therapy compared to supportive psychotherapy for panic disorder with or without agoraphobia in adults | |||||
| Patient or population: adult patients with panic disorder with or without agoraphobia Setting: outpatients | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Supportive psychotherapy (SP) | Cognitive behaviour therapy (CBT) | ||||
| Short‐term remission (follow‐up: mean 3 months) | Study population | OR 0.67 | 176 | ⊕⊕⊝⊝ | |
| 38 per 100 | 29 per 100 | ||||
| Short‐term response (follow‐up: mean 3 months) | Study population | OR 1.12 | 176 | ⊕⊝⊝⊝ | |
| 32 per 100 | 34 per 100 | ||||
| Short‐term dropouts (follow‐up: mean 3 months) | Study population | OR 0.64 | 176 | ⊕⊝⊝⊝ | |
| 46 per 100 | 35 per 100 | ||||
| Long‐term remission/response (follow‐up: mean 12 months) | Study population | OR 2.09 | 80 | ⊕⊕⊝⊝ | |
| 24 per 100 | 40 per 100 | ||||
| Short‐term improvement as measured on a continuous scale (follow‐up: mean 3 months) | The mean short‐term improvement as measured on a continuous scale in the control group was 0 | The mean short‐term improvement, measured on a continuous scale as SMD (NMA results), was ‐0.05 (95% CI ‐0.56 to 0.47), indicating almost no difference between CBT and SP (the negative value of the point estimate indicates a slight trend in favour of CBT) | ‐ | 152 | ⊕⊕⊝⊝ |
| Reported ORs and SMD are derived from the network meta‐analyses. *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| We downgraded the quality of the evidence one step at a time when one or more of the following criticisms was present: 1Risk of bias for the included studies was in many cases unclear. 2Only a few studies available for direct comparison. 95% CI still wide and non‐significant even after combining direct and indirect evidence. 3Results were inconsistent across studies, although with wide confidence intervals. 4ST‐response data were imputed from the continuous outcome for all the included studies. 5Only one study available for direct comparison. 95% CI still wide and non‐significant even after combining direct and indirect evidence. | |||||
| Cognitive behaviour therapy compared to psychodynamic psychotherapy for panic disorder with or without agoraphobia in adults | |||||
| Patient or population: adult patients with panic disorder with or without agoraphobia Setting: outpatients | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Psychodynamic psychotherapy (PD) | Cognitive behaviour therapy (CBT) | ||||
| Short‐term remission (follow‐up: mean 3 months) | Study population | OR 0.94 | 54 | ⊕⊝⊝⊝ | |
| 44 per 100 | 43 per 100 | ||||
| Short‐term response (follow‐up: mean 3 months) | Study population | OR 1.05 | 54 | ⊕⊝⊝⊝ | |
| 47 per 100 | 48 per 100 | ||||
| Short‐term dropouts (follow‐up: mean 3 months) | Study population | OR 1.92 | 54 | ⊕⊝⊝⊝ | |
| 19 per 100 | 32 per 100 | ||||
| Long‐term remission/response (follow‐up: mean 12 months) | Study population | OR 1.25 | 54 | ⊕⊕⊝⊝ | |
| 50 per 100 | 56 per 100 | ||||
| Short‐term improvement as measured on a continuous scale (follow‐up: mean 3 months) | The mean short‐term improvement as measured on a continuous scale in the control group was 0 | The mean short‐term improvement as measured on a continuous scale in the intervention group was 0.17 standard deviations higher (0.5 lower to 0.83 higher), indicating a small effect size in favour of PDb | ‐ | 54 | ⊕⊝⊝⊝ |
| a Reported ORs are derived (as reciprocal values) from the results of network meta‐analyses presented in Table 1, Table 4, Table 7 and Table 13 (for ST‐remission and ST‐response we used the results of NMA adjusted for SSE). b Reported SMD is derived from the results of network meta‐analysis presented in Table 10. *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| We downgraded the quality of the evidence one step at a time when one or more of the following criticisms was present: 1The available direct evidence was affected by a high risk of bias in various important domains. 2Relevant (although non‐significant) inconsistency was found in the loop PD‐CBT‐PT. 3Indirect evidence importantly influences the NMA results. 4Only one study available for direct comparison. 95% CI still wide and non‐significant even after combining direct and indirect evidence. 5Statistically significant inconsistency was found in the loop PD‐CBT‐PT. | |||||
| NMA Rankings of psychological therapies for panic disorder with or without agoraphobia in adults | |||
| Patient or population: adult patients with panic disorder with or without agoraphobia Setting: outpatients | |||
| Outcomes | Treatment hierarchy (in descending order) | № of participants | Quality of the evidence |
| Short‐term remission | (SP)‐CBT‐PD‐CT‐BT‐PT‐NT‐WL | 2491 | ⊕⊕⊝⊝ |
| Short‐term response | CBT‐PD‐(SP)‐BT‐PT‐WL‐CT‐NT | 2240 | ⊕⊕⊝⊝ |
| Short‐term dropouts | NT‐PD‐WL‐3W‐CBT‐APP‐PE‐PT‐CT‐BT‐SP | 2535 | ⊕⊕⊝⊝ |
| Long‐term remission/response | CBT‐PD‐PT‐BT‐SP‐CT | 464 | ⊕⊕⊝⊝ |
| Short‐term improvement as measured on a continuous scale | (PD)‐CBT‐SP‐CT‐3W‐BT‐PT‐NT‐WL | 2318 | ⊕⊕⊝⊝ |
| Reported rankings are based on absolute SUCRA values, which are derived from network meta‐analyses (NMA). The ranking of treatments reported in parenthesis must be interpreted with caution, because the evidence supporting those rankings is either too scarce or hampered by relevant inconsistency. The assessment of quality of evidence has been made by adapting the GRADE tool, designed for pairwise meta‐analyses, to network meta‐analyses, as suggested in Salanti 2014. | |||
| GRADE Working Group grades of evidence | |||
| 1 Downgraded for study limitations because the risk of bias was unclear or high in more than one important domain for many of the included studies. 2 Downgraded for imprecision because too few comparisons remained clinically important after adjusting the results of NMA for SSE (See additional Table 1 and Table 4) 3 Downgraded for imprecision because too few comparisons showed clinically important results in NMA (See additional Table 7, Table 10 and Table 14) | |||
| Comparison (X vs Y) | Pairwise meta‐analyses (common τ = 0.69) | Standard NMA (τ = 0.64) | ΝΜΑ adjusted for SSE (τ = 0.59) | |||||||
| # of studies | OR | CI (lower) | CI (upper) | OR | CI (lower) | CI (upper) | OR | CrI (lower) | CrI (upper) | |
| PT vs SP | ‐ | ‐ | ‐ | ‐ | 0.36 | 0.11 | 1.18 | 0.35 | 0.10 | 1.11 |
| BT vs SP | ‐ | ‐ | ‐ | ‐ | 0.37 | 0.12 | 1.15 | 0.38 | 0.12 | 1.19 |
| BT vs PT | 2 | 1.11 | 0.21 | 6.00 | 1.03 | 0.42 | 2.28 | 1.10 | 0.51 | 2.50 |
| CT vs SP | ‐ | ‐ | ‐ | ‐ | 0.47 | 0.11 | 2.07 | 0.44 | 0.10 | 1.90 |
| CT vs PT | 1 | 1.22 | 0.20 | 7.48 | 1.33 | 0.44 | 4.05 | 1.27 | 0.41 | 3.91 |
| CT vs BT | 1 | 0.95 | 0.12 | 7.47 | 1.29 | 0.41 | 4.07 | 1.15 | 0.37 | 3.61 |
| CBT vs SP | 3 | 0.68 | 0.24 | 1.91 | 0.68 | 0.25 | 1.83 | 0.67 | 0.25 | 1.82 |
| CBT vs PT | 4 | 1.56 | 0.62 | 3.94 | 1.90 | 0.98 | 3.69 | 1.95 | 1.02 | 3.97 |
| CBT vs BT | 10 | 2.09 | 1.10 | 3.97 | 1.84 | 1.06 | 3.22 | 1.77 | 1.02 | 3.11 |
| CBT vs CT | 1 | 1.69 | 0.21 | 13.47 | 1.43 | 0.48 | 4.23 | 1.53 | 0.52 | 4.68 |
| WL vs SP | ‐ | ‐ | ‐ | ‐ | 0.08 | 0.03 | 0.26 | 0.22 | 0.06 | 0.78 |
| WL vs PT | 4 | 0.21 | 0.06 | 0.70 | 0.23 | 0.12 | 0.48 | 0.64 | 0.27 | 1.65 |
| WL vs BT | 3 | 0.12 | 0.04 | 0.43 | 0.23 | 0.12 | 0.45 | 0.58 | 0.25 | 1.36 |
| WL vs CT | 2 | 0.12 | 0.02 | 0.61 | 0.18 | 0.06 | 0.52 | 0.50 | 0.15 | 1.77 |
| WL vs CBT | 18 | 0.13 | 0.07 | 0.22 | 0.12 | 0.07 | 0.21 | 0.33 | 0.16 | 0.69 |
| NT vs SP | ‐ | ‐ | ‐ | ‐ | 0.26 | 0.04 | 1.82 | 0.24 | 0.03 | 1.67 |
| NT vs PT | 1 | 0.70 | 0.11 | 4.33 | 0.73 | 0.14 | 3.68 | 0.70 | 0.14 | 3.48 |
| NT vs BT | ‐ | ‐ | ‐ | ‐ | 0.71 | 0.13 | 3.96 | 0.64 | 0.11 | 3.51 |
| NT vs CT | 1 | 0.57 | 0.09 | 3.48 | 0.55 | 0.11 | 2.73 | 0.55 | 0.11 | 2.71 |
| NT vs CBT | ‐ | ‐ | ‐ | ‐ | 0.38 | 0.07 | 2.05 | 0.36 | 0.07 | 1.85 |
| NT vs WL | ‐ | ‐ | ‐ | ‐ | 3.11 | 0.58 | 16.78 | 1.10 | 0.18 | 6.26 |
| PD vs SP | ‐ | ‐ | ‐ | ‐ | 0.71 | 0.14 | 3.52 | 0.71 | 0.14 | 3.42 |
| PD vs PT | 1 | 4.21 | 0.70 | 25.49 | 1.99 | 0.57 | 7.02 | 2.05 | 0.60 | 7.38 |
| PD vs BT | ‐ | ‐ | ‐ | ‐ | 1.94 | 0.50 | 7.48 | 1.88 | 0.48 | 7.17 |
| PD vs CT | ‐ | ‐ | ‐ | ‐ | 1.50 | 0.30 | 7.43 | 1.61 | 0.33 | 8.17 |
| PD vs CBT | 1 | 0.51 | 0.09 | 2.99 | 1.05 | 0.30 | 3.68 | 1.06 | 0.29 | 3.66 |
| PD vs WL | ‐ | ‐ | ‐ | ‐ | 8.50 | 2.27 | 31.84 | 3.21 | 0.75 | 12.87 |
| PD vs NT | ‐ | ‐ | ‐ | ‐ | 2.73 | 0.36 | 20.56 | 2.91 | 0.40 | 22.56 |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). For each comparison X vs Y, an OR greater than one favours treatment X, an OR less than one favours treatment Y. Note that in the main text, where necessary, we inverted the values presented in Table 4 for an easier presentation, in which an OR greater than 1 stands for a higher number of events (short‐term remissions) in the intervention group when compared to the control group. Statistically significant results are written in bold. BT: behaviour therapy | ||||||||||
| Comparison | I2(%) | 95% CI |
| CBT vs SP | 0 | 0 to 90 |
| WL vs CBT | 58 | 29 to 75 |
| CBT vs BT | 5 | 0 to 64 |
| WL vs BT | 34 | 0 to 78 |
| WL vs PT | 56 | 0 to 85 |
| CBT vs PT | 0 | 0 to 85 |
| This values refer to standard meta‐analyses, where each comparison has its own heterogeneity variance. BT: behaviour therapy | ||
| Treatment | SUCRA |
| SP | 88 |
| CBT | 76 |
| PD | 73 |
| CT | 50 |
| BT | 41 |
| PT | 35 |
| NT | 25 |
| WL | 13 |
| BT: behaviour therapy | |
| Comparison (X vs Y) | Pairwise meta‐analyses (common τ = 0.55) | Standard NMA (τ = 0.63) | NMA adjusted for SSE (τ = 0.65) | |||||||
| # of studies | OR | CI (lower) | CI (upper) | OR | CI (lower) | CI (upper) | OR | CrI (lower) | CrI (upper) | |
| PT vs SP | ‐ | ‐ | ‐ | ‐ | 0.68 | 0.20 | 2.31 | 0.69 | 0.20 | 2.41 |
| BT vs SP | ‐ | ‐ | ‐ | ‐ | 0.589 | 0.18 | 1.93 | 0.69 | 0.21 | 2.33 |
| BT vs PT | 2 | 0.90 | 0.21 | 3.90 | 0.87 | 0.41 | 1.88 | 1.00 | 0.46 | 2.23 |
| CT vs SP | ‐ | ‐ | ‐ | ‐ | 0.39 | 0.07 | 2.07 | 0.36 | 0.07 | 1.96 |
| CT vs PT | 1 | 0.94 | 0.18 | 4.97 | 0.58 | 0.16 | 2.09 | 0.53 | 0.14 | 2.04 |
| CT vs BT | 1 | 0.20 | 0.03 | 1.46 | 0.66 | 0.18 | 2.51 | 0.53 | 0.13 | 2.07 |
| CBT vs SP | 3 | 1.02 | 0.38 | 2.73 | 1.04 | 0.36 | 2.99 | 1.12 | 0.40 | 3.26 |
| CBT vs PT | 4 | 1.23 | 0.56 | 2.71 | 1.54 | 0.81 | 2.94 | 1.62 | 0.84 | 3.17 |
| CBT vs BT | 10 | 1.78 | 1.00 | 3.18 | 1.77 | 1.02 | 3.04 | 1.61 | 0.92 | 2.86 |
| CBT vs CT | 1 | 2.92 | 0.43 | 19.98 | 2.65 | 0.73 | 9.62 | 3.08 | 0.81 | 12.26 |
| WL vs SP | ‐ | ‐ | ‐ | ‐ | 0.17 | 0.05 | 0.53 | 0.45 | 0.12 | 1.93 |
| WL vs PT | 4 | 0.15 | 0.05 | 0.44 | 0.25 | 0.12 | 0.50 | 0.65 | 0.24 | 1.91 |
| WL vs BT | 4 | 0.32 | 0.14 | 0.73 | 0.29 | 0.15 | 0.54 | 0.65 | 0.28 | 1.68 |
| WL vs CT | 1 | 0.31 | 0.02 | 4.27 | 0.43 | 0.12 | 1.61 | 1.24 | 0.26 | 6.42 |
| WL vs CBT | 17 | 0.19 | 0.05 | 0.31 | 0.16 | 0.10 | 0.26 | 0.40 | 0.18 | 1.00 |
| NT vs SP | ‐ | ‐ | ‐ | ‐ | 0.16 | 0.02 | 1.21 | 0.15 | 0.02 | 1.22 |
| NT vs PT | 1 | 0.31 | 0.06 | 1.62 | 0.24 | 0.05 | 1.25 | 0.22 | 0.04 | 1.25 |
| NT vs BT | ‐ | ‐ | ‐ | ‐ | 0.27 | 0.05 | 1.59 | 0.22 | 0.03 | 1.37 |
| NT vs CT | 1 | 0.33 | 0.06 | 1.68 | 0.41 | 0.08 | 2.13 | 0.42 | 0.07 | 2.31 |
| NT vs CBT | ‐ | ‐ | ‐ | ‐ | 0.16 | 0.03 | 0.87 | 0.14 | 0.02 | 0.80 |
| NT vs WL | ‐ | ‐ | ‐ | ‐ | 0.96 | 0.17 | 5.46 | 0.33 | 0.04 | 2.32 |
| PD vs SP | ‐ | ‐ | ‐ | ‐ | 1.02 | 0.20 | 5.28 | 1.07 | 0.20 | 5.70 |
| PD vs PT | 1 | 4.22 | 0.84 | 21.31 | 1.51 | 0.42 | 5.35 | 1.54 | 0.42 | 5.92 |
| PD vs BT | ‐ | ‐ | ‐ | ‐ | 1.73 | 0.44 | 6.70 | 1.54 | 0.37 | 6.41 |
| PD vs CT | ‐ | ‐ | ‐ | ‐ | 2.59 | 0.45 | 14.82 | 2.94 | 0.47 | 18.59 |
| PD vs CBT | 1 | 0.34 | 0.07 | 1.76 | 0.98 | 0.27 | 3.47 | 0.95 | 0.25 | 3.60 |
| PD vs WL | ‐ | ‐ | ‐ | ‐ | 6.02 | 1.60 | 22.61 | 2.37 | 0.49 | 10.75 |
| PD vs NT | ‐ | ‐ | ‐ | ‐ | 6.28 | 0.80 | 49.20 | 7.03 | 0.84 | 61.98 |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). For each comparison X vs Y, an OR greater than one favours treatment X, an OR less than one favours treatment Y. Note that in the main text, where necessary, we inverted the values presented in Table 4 for an easier presentation, in which an OR greater than 1 stands for a higher number of events (short‐term remissions) in the intervention group when compared to the control group. Statistically significant results are written in bold. BT: behaviour therapy | ||||||||||
| Comparison | I2(%) | 95% CI |
| CBT vs SP | 7 | 0 to 90 |
| WL vs CBT | 39 | 0 to 66 |
| CBT vs BT | 22 | 0 to 62 |
| WL vs BT | 26 | 0 to 72 |
| WL vs PT | 14 | 0 to 87 |
| CBT vs PT | 45 | 0 to 82 |
| This values refer to standard meta‐analyses, where each comparison has its own heterogeneity variance. BT: behaviour therapy | ||
| Treatment | SUCRA |
| CBT | 84 |
| PD | 74 |
| SP | 72 |
| BT | 53 |
| PT | 52 |
| WL | 31 |
| CT | 27 |
| NT | 7 |
| BT: behaviour therapy | |
| Comparison | Pairwise meta‐analysis | Network meta‐analysis (τ = 0.33) | |||||
| # of studies | OR | CI (lower) | CI (upper) | OR | CI (lower) | CI (upper) | |
| PT vs SP | ‐ | ‐ | ‐ | ‐ | 0.76 | 0.28 | 2.08 |
| BT vs SP | ‐ | ‐ | ‐ | ‐ | 0.92 | 0.35 | 2.28 |
| BT vs PT | 2 | 2.19 | 0.46 | 10.38 | 1.20 | 0.60 | 2.40 |
| CT vs SP | ‐ | ‐ | ‐ | ‐ | 1.06 | 0.20 | 5.62 |
| CT vs PT | 1 | 5.59 | 0.59 | 52.73 | 1.38 | 0.33 | 5.86 |
| CT vs BT | ‐ | ‐ | ‐ | ‐ | 1.15 | 0.26 | 5.20 |
| CBT vs SP | 3 | 0.63 | 0.21 | 1.89 | 0.64 | 0.28 | 1.43 |
| CBT vs PT | 3 | 0.56 | 0.24 | 1.28 | 0.83 | 0.46 | 1.50 |
| CBT vs BT | 10 | 0.89 | 0.52 | 1.51 | 0.69 | 0.42 | 1.15 |
| CBT vs CT | ‐ | ‐ | ‐ | ‐ | 0.60 | 0.14 | 2.60 |
| WL vs SP | ‐ | ‐ | ‐ | ‐ | 0.48 | 0.19 | 1.22 |
| WL vs PT | 5 | 0.74 | 0.30 | 1.83 | 0.63 | 0.35 | 1.15 |
| WL vs BT | 4 | 0.34 | 0.16 | 0.69 | 0.52 | 0.30 | 0.93 |
| WL vs CT | ‐ | ‐ | ‐ | ‐ | 0.46 | 0.11 | 1.97 |
| WL vs CBT | 14 | 0.70 | 0.42 | 1.16 | 0.76 | 0.48 | 1.20 |
| NT vs SP | ‐ | ‐ | ‐ | ‐ | 0.10 | 0.00 | 2.18 |
| NT vs PT | 1 | 0.29 | 0.01 | 7.51 | 0.13 | 0.01 | 3.10 |
| NT vs BT | ‐ | ‐ | ‐ | ‐ | 0.11 | 0.00 | 2.69 |
| NT vs CT | 1 | 0.07 | 0.00 | 1.37 | 0.10 | 0.00 | 1.93 |
| NT vs CBT | ‐ | ‐ | ‐ | ‐ | 0.16 | 0.01 | 3.80 |
| NT vs WL | ‐ | ‐ | ‐ | ‐ | 0.21 | 0.09 | 5.01 |
| PD vs SP | ‐ | ‐ | ‐ | ‐ | 0.33 | 0.08 | 1.46 |
| PD vs PT | 1 | 0.16 | 0.03 | 0.84 | 0.44 | 0.12 | 1.52 |
| PD vs BT | ‐ | ‐ | ‐ | ‐ | 0.36 | 0.10 | 1.35 |
| PD vs CT | ‐ | ‐ | ‐ | ‐ | 0.32 | 0.05 | 2.04 |
| PD vs CBT | 1 | 1.21 | 0.27 | 5.35 | 0.52 | 0.15 | 1.80 |
| PD vs WL | ‐ | ‐ | ‐ | ‐ | 0.69 | 0.19 | 2.50 |
| PD vs NT | ‐ | ‐ | ‐ | ‐ | 3.31 | 0.11 | 97.03 |
| APP vs SP | ‐ | ‐ | ‐ | ‐ | 0.84 | 0.07 | 10.61 |
| APP vs PT | ‐ | ‐ | ‐ | ‐ | 1.10 | 0.10 | 12.30 |
| APP vs BT | ‐ | ‐ | ‐ | ‐ | 0.92 | 0.08 | 10.49 |
| APP vs CT | 1 | 0.97 | 0.08 | 11.51 | 0.80 | 0.09 | 7.21 |
| APP vs CBT | ‐ | ‐ | ‐ | ‐ | 1.32 | 0.12 | 14.61 |
| APP vs WL | ‐ | ‐ | ‐ | ‐ | 1.75 | 0.16 | 19.51 |
| APP vs NT | ‐ | ‐ | ‐ | ‐ | 8.37 | 0.21 | 333.81 |
| APP vs PD | ‐ | ‐ | ‐ | ‐ | 2.53 | 0.17 | 36.70 |
| PE vs SP | ‐ | ‐ | ‐ | ‐ | 0.84 | 0.01 | 97.42 |
| PE vs PT | ‐ | ‐ | ‐ | ‐ | 1.10 | 0.01 | 119.64 |
| PE vs BT | ‐ | ‐ | ‐ | ‐ | 0.92 | 0.01 | 100.89 |
| PE vs CT | ‐ | ‐ | ‐ | ‐ | 0.80 | 0.01 | 77.96 |
| PE vs CBT | ‐ | ‐ | ‐ | ‐ | 1.32 | 0.01 | 142.93 |
| PE vs WL | ‐ | ‐ | ‐ | ‐ | 1.75 | 0.02 | 189.75 |
| PE vs NT | ‐ | ‐ | ‐ | ‐ | 8.36 | 0.04 | 1954.05 |
| PE vs PD | ‐ | ‐ | ‐ | ‐ | 2.53 | 0.02 | 316.00 |
| PE vs APP | ‐ | ‐ | ‐ | ‐ | 1.00 | 0.02 | 55.66 |
| 3W vs SP | ‐ | ‐ | ‐ | ‐ | 0.36 | 0.06 | 2.12 |
| 3W vs PT | ‐ | ‐ | ‐ | ‐ | 0.47 | 0.08 | 2.65 |
| 3W vs BT | ‐ | ‐ | ‐ | ‐ | 0.39 | 0.07 | 2.15 |
| 3W vs CT | ‐ | ‐ | ‐ | ‐ | 0.34 | 0.04 | 3.03 |
| 3W vs CBT | 1 | 0.56 | 0.13 | 2.51 | 0.56 | 0.11 | 2.88 |
| 3W vs WL | ‐ | ‐ | ‐ | ‐ | 0.74 | 0.14 | 4.04 |
| 3W vs NT | ‐ | ‐ | ‐ | ‐ | 3.55 | 0.10 | 126.65 |
| 3W vs PD | ‐ | ‐ | ‐ | ‐ | 1.07 | 0.13 | 8.31 |
| 3W vs APP | ‐ | ‐ | ‐ | ‐ | 0.42 | 0.02 | 7.74 |
| 3W vs PE | ‐ | ‐ | ‐ | ‐ | 0.42 | 0.00 | 60.45 |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). Of course, since this is dropout outcome, an OR smaller than one favours treatment X. Statistically significant results are written in bold. 3W: third‐wave | |||||||
| Comparison | I2(%) | 95% CI |
| CBT vs SP | 49 | 0 to 85 |
| WL vs CBT | 0 | 0 to 55 |
| CBT vs BT | 0 | 0 to 62 |
| WL vs BT | 0 | 0 to 85 |
| WL vs PT | 25 | 0 to 70 |
| CBT vs PT | 12 | 0 to 91 |
| This values refer to standard meta‐analyses, where each comparison has its own heterogeneity variance. BT: behaviour therapy | ||
| Treatment | SUCRA |
| NT | 85 |
| PD | 75 |
| WL | 67 |
| 3W | 67 |
| CBT | 51 |
| APP | 42 |
| PE | 42 |
| PT | 38 |
| CT | 29 |
| BT | 28 |
| SP | 26 |
| Note that higher ranking treatments correspond to lower dropout rate. 3W: third‐wave | |
| Comparison (X vs Y) | Pairwise meta‐analysis | Network meta‐analysis (τ = 0.34) | |||||
| # of studies | SMD | CI (lower) | CI (upper) | SMD | CI (lower) | CI (upper) | |
| PT vs SP | ‐ | ‐ | ‐ | ‐ | 0.24 | ‐0.35 | 0.84 |
| BT vs SP | ‐ | ‐ | ‐ | ‐ | 0.16 | ‐0.42 | 0.74 |
| BT vs PT | 1 | ‐0.26 | ‐0.98 | 0.46 | ‐0.08 | ‐0.47 | 0.31 |
| CT vs SP | ‐ | ‐ | ‐ | ‐ | 0.17 | ‐0.56 | 0.90 |
| CT vs PT | 1 | ‐0.02 | ‐0.67 | 0.64 | ‐0.08 | ‐0.63 | 0.48 |
| CT vs BT | 1 | 0.65 | ‐0.16 | 1.46 | 0.00 | ‐0.56 | 0.57 |
| CBT vs SP | 3 | ‐0.08 | ‐0.40 | 0.24 | ‐0.05 | ‐0.56 | 0.47 |
| CBT vs PT | 5 | ‐0.05 | ‐0.30 | 0.19 | ‐0.29 | ‐0.60 | 0.02 |
| CBT vs BT | 10 | ‐0.24 | ‐0.45 | ‐0.03 | ‐0.21 | ‐0.48 | 0.07 |
| CBT vs CT | 2 | 0.03 | ‐0.88 | 0.94 | ‐0.21 | ‐0.73 | 0.31 |
| WL vs SP | ‐ | ‐ | ‐ | ‐ | 1.05 | 0.49 | 1.60 |
| WL vs PT | 4 | 0.87 | 0.09 | 1.65 | 0.80 | 0.47 | 1.13 |
| WL vs BT | 3 | 0.92 | 0.59 | 1.26 | 0.89 | 0.57 | 1.20 |
| WL vs CT | 1 | 0.60 | ‐0.27 | 1.47 | 0.88 | 0.34 | 1.42 |
| WL vs CBT | 17 | 1.14 | 0.87 | 1.41 | 1.09 | 0.88 | 1.31 |
| NT vs SP | ‐ | ‐ | ‐ | ‐ | 0.78 | ‐0.06 | 1.63 |
| NT vs PT | 1 | 0.36 | ‐0.26 | 0.98 | ‐0.46 | ‐1.12 | 0.21 |
| NT vs BT | ‐ | ‐ | ‐ | ‐ | 0.62 | ‐0.09 | 1.33 |
| NT vs CT | 1 | 0.39 | ‐0.25 | 1.03 | 0.61 | ‐0.11 | 1.34 |
| NT vs CBT | 1 | 1.30 | 0.46 | 2.14 | 0.83 | 0.16 | 1.50 |
| NT vs WL | ‐ | ‐ | ‐ | ‐ | ‐0.27 | ‐0.96 | 0.42 |
| PD vs SP | ‐ | ‐ | ‐ | ‐ | ‐0.21 | ‐1.05 | 0.63 |
| PD vs PT | 1 | ‐1.18 | ‐1.79 | ‐0.57 | ‐0.46 | ‐1.12 | 0.21 |
| PD vs BT | ‐ | ‐ | ‐ | ‐ | ‐0.38 | ‐1.09 | 0.34 |
| PD vs CT | ‐ | ‐ | ‐ | ‐ | ‐0.38 | ‐1.21 | 0.45 |
| PD vs CBT | 1 | 0.57 | ‐0.07 | 1.2 | ‐0.17 | ‐0.83 | 0.50 |
| PD vs WL | ‐ | ‐ | ‐ | ‐ | ‐1.26 | ‐1.95 | ‐0.57 |
| PD vs NT | ‐ | ‐ | ‐ | ‐ | ‐1.00 | ‐1.91 | ‐0.07 |
| PE vs APP | 1 | ‐0.25 | ‐0.87 | 0.38 | ‐ | ‐ | ‐ |
| 3W vs SP | ‐ | ‐ | ‐ | ‐ | 0.20 | ‐0.82 | 1.22 |
| 3W vs PT | ‐ | ‐ | ‐ | ‐ | ‐0.04 | ‐0.98 | 0.90 |
| 3W vs BT | ‐ | ‐ | ‐ | ‐ | 0.04 | ‐0.89 | 0.97 |
| 3W vs CT | ‐ | ‐ | ‐ | ‐ | 0.04 | ‐0.99 | 1.07 |
| 3W vs CBT | 1 | 0.26 | ‐0.33 | 0.84 | 0.25 | ‐0.64 | 1.14 |
| 3W vs WL | ‐ | ‐ | ‐ | ‐ | ‐0.84 | ‐1.76 | 0.07 |
| 3W vs NT | ‐ | ‐ | ‐ | ‐ | ‐0.58 | ‐1.69 | 0.53 |
| 3W vs PD | ‐ | ‐ | ‐ | ‐ | 0.42 | ‐0.69 | 1.53 |
| A positive SMD for Χ vs Y means treatment Y is better than X, the opposite for a negative SMD (this is because for the scales used a lower score corresponds to a better treatment). Statistically significant results are written in bold. 3W: third‐wave | |||||||
| Comparison | I2(%) | 95% CI |
| CBT vs SP | 0 | 0 to 90 |
| CBT vs PT | 0 | 0 to 79 |
| WL vs PT | 79 | 45 to 92 |
| CBT vs BT | 0 | 0 to 62 |
| WL vs BT | 23 | 0 to 92 |
| WL vs CBT | 61 | 34 to 77 |
| This values refer to standard meta‐analyses, where each comparison has its own heterogeneity variance. BT: behaviour therapy | ||
| Treatment | SUCRA |
| PD | 83 |
| CBT | 79 |
| SP | 69 |
| CT | 54 |
| 3W | 53 |
| BT | 52 |
| PT | 43 |
| NT | 14 |
| WL | 4 |
| 3W: third‐wave | |
| Comparison (X vs Y) | Pairwise meta‐analyses | Network meta‐analysis | |||||
| # of studies | OR | CI (lower) | CI (upper) | OR | CI (lower) | CI (upper) | |
| PT vs SP | ‐ | ‐ | ‐ | ‐ | 1.31 | 0.33 | 5.25 |
| BT vs SP | ‐ | ‐ | ‐ | ‐ | 1.27 | 0.38 | 4.27 |
| BT vs PT | 1 | 1.17 | 0.28 | 4.87 | 0.97 | 0.37 | 2.57 |
| CT vs SP | ‐ | ‐ | ‐ | ‐ | 0.96 | 0.21 | 4.36 |
| CT vs PT | 1 | 0.83 | 0.25 | 2.80 | 0.74 | 0.26 | 2.06 |
| CT vs BT | 1 | 0.38 | 0.08 | 1.86 | 0.76 | 0.28 | 2.31 |
| CBT vs SP | 1 | 2.09 | 0.80 | 5.47 | 2.09 | 0.73 | 5.98 |
| CBT vs PT | 2 | 1.33 | 0.47 | 3.76 | 1.60 | 0.64 | 3.95 |
| CBT vs BT | 5 | 1.66 | 0.80 | 3.44 | 1.64 | 0.90 | 2.97 |
| CBT vs CT | 1 | 1.56 | 0.34 | 7.11 | 2.16 | 0.73 | 6.37 |
| PD vs SP | ‐ | ‐ | ‐ | ‐ | 1.67 | 0.33 | 8.33 |
| PD vs PT | ‐ | ‐ | ‐ | ‐ | 1.28 | 0.28 | 5.81 |
| PD vs BT | ‐ | ‐ | ‐ | ‐ | 1.31 | 0.34 | 5.07 |
| PD vs CT | ‐ | ‐ | ‐ | ‐ | 1.73 | 0.34 | 8.79 |
| PD vs CBT | 1 | 0.80 | 0.26 | 9.86 | 0.80 | 0.24 | 2.69 |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). For each comparison X vs Y, an OR greater than one favours treatment X, an OR less than one favours treatment Y. Note that in the main text, where necessary, we inverted the values presented in Table 4 for an easier presentation, in which an OR greater than 1 stands for a higher number of events (short‐term remissions) in the intervention group when compared to the control group. BT: behaviour therapy | |||||||
| Treatment | SUCRA |
| CBT | 85 |
| PD | 64 |
| PT | 49 |
| BT | 43 |
| SP | 31 |
| CT | 27 |
| BT: behaviour therapy | |
| Comparison | Pairwise meta‐analyses (common τ 0.05) | Standard NMA (τ ≅ 0) | NMA adjusted for SSE (τ ≅ 0.60) | |||||||
| # of studies | OR | CI (lower) | CI (upper) | OR | CI (lower) | CI (upper) | OR | CrI (lower) | CrI (upper) | |
| PT vs SP | ‐ | ‐ | ‐ | ‐ | 0.27 | 0.11 | 0.64 | 0.34 | 0.10 | 1.08 |
| BT vs SP | ‐ | ‐ | ‐ | ‐ | 0.35 | 0.16 | 0.75 | 0.38 | 0.12 | 1.16 |
| BT vs PT | 2 | 0.98 | 0.26 | 3.74 | 1.29 | 0.69 | 2.42 | 1.10 | 0.51 | 2.52 |
| CT vs SP | ‐ | ‐ | ‐ | ‐ | 0.43 | 0.13 | 1.47 | 0.44 | 0.10 | 1.87 |
| CT vs PT | ‐ | ‐ | ‐ | ‐ | 1.60 | 0.51 | 4.96 | 1.27 | 0.41 | 3.90 |
| CT vs BT | 1 | 0.95 | 0.19 | 4.84 | 1.24 | 0.44 | 3.51 | 1.15 | 0.37 | 3.68 |
| CBT vs SP | 3 | 0.67 | 0.33 | 1.35 | 0.67 | 0.34 | 1.27 | 0.67 | 0.24 | 1.77 |
| CBT vs PT | 3 | 2.02 | 0.85 | 4.76 | 2.46 | 1.39 | 4.33 | 1.94 | 1.02 | 3.97 |
| CBT vs BT | 9 | 1.90 | 1.15 | 3.16 | 1.90 | 1.26 | 2.88 | 1.76 | 1.02 | 3.13 |
| CBT vs CT | 1 | 1.69 | 0.33 | 8.76 | 1.54 | 0.55 | 4.32 | 1.53 | 0.52 | 4.66 |
| WL vs SP | ‐ | ‐ | ‐ | ‐ | 0.07 | 0.03 | 0.15 | 0.22 | 0.06 | 0.76 |
| WL vs PT | 4 | 0.22 | 0.09 | 0.53 | 0.25 | 0.14 | 0.45 | 0.64 | 0.27 | 1.66 |
| WL vs BT | 3 | 0.17 | 0.08 | 0.36 | 0.19 | 0.12 | 0.31 | 0.58 | 0.26 | 1.36 |
| WL vs CT | 2 | 0.12 | 0.03 | 0.46 | 0.16 | 0.06 | 0.43 | 0.51 | 0.15 | 1.82 |
| WL vs CBT | 11 | 0.10 | 0.05 | 0.19 | 0.10 | 0.07 | 0.16 | 0.33 | 0.16 | 0.70 |
| PD vs SP | ‐ | ‐ | ‐ | ‐ | 0.61 | 0.21 | 1.80 | 0.24 | 0.03 | 1.64 |
| PD vs PT | 1 | 4.22 | 1.17 | 15.15 | 2.25 | 0.93 | 5.42 | 0.70 | 0.14 | 3.66 |
| PD vs BT | ‐ | ‐ | ‐ | ‐ | 1.74 | 0.68 | 4.47 | 0.64 | 0.11 | 3.60 |
| PD vs CT | ‐ | ‐ | ‐ | ‐ | 1.41 | 0.37 | 5.34 | 0.55 | 0.11 | 2.74 |
| PD vs CBT | 1 | 0.51 | 0.15 | 1.76 | 0.91 | 0.38 | 2.19 | 0.36 | 0.07 | 1.87 |
| PD vs WL | ‐ | ‐ | ‐ | ‐ | 8.97 | 3.50 | 22.95 | 1.09 | 0.18 | 6.45 |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). For each comparison X vs Y, an OR greater than one favours treatment X, an OR less than one favours treatment Y. Note that in the main text, where necessary, we inverted the values presented in Table 4 for an easier presentation, in which an OR greater than 1 stands for a higher number of events (short‐term remissions) in the intervention group when compared to the control group. Statistically significant results are written in bold. BT: behaviour therapy | ||||||||||
| Comparison | I2(%) | 95% CI |
| WL vs PT | 56 | 0 to 85 |
| WL vs BT | 34 | 0 to 78 |
| WL vs CBT | 21 | 0 to 60 |
| CBT vs BT | 6 | 0 to 67 |
| CBT vs SP | 0 | 0 to 90 |
| CBT vs PT | 0 | 0 to 90 |
| This values refer to standard meta‐analyses, where each comparison has its own heterogeneity variance. BT: behaviour therapy | ||
| Treatment | SUCRA |
| SP | 89 |
| CBT | 76 |
| PD | 73 |
| CT | 50 |
| BT | 40 |
| PT | 35 |
| NT | 26 |
| WL | 13 |
| BT: behaviour therapy | |
| Comparison (X vs Y) | Pairwise meta‐analyses | ||||
| # of studies | OR | CI (lower) | CI (upper) | I2 | |
| WL vs CBT | 3 | 0.07 | 0.01 | 0.30 | 0.0% |
| CBT vs BT | 2 | 2.21 | 0.96 | 5.10 | 0.7% |
| CBT vs SP | 2 | 0.51 | 0.22 | 1.23 | 0.0% |
| WL vs BT | 1 | 0.22 | 0.11 | 0.44 | ‐ |
| NT vs CT | 1 | 0.57 | 0.17 | 1.91 | ‐ |
| CT vs PT | 1 | 1.22 | 0.36 | 4.12 | ‐ |
| NT vs PT | 1 | 0.70 | 0.27 | 1.10 | ‐ |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). For each comparison X vs Y, an OR greater than one favours treatment X, an OR less than one favours treatment Y. Note that in the main text, where necessary, we inverted the values presented in Table 4 for an easier presentation, in which an OR greater than 1 stands for a higher number of events (short‐term remissions) in the intervention group when compared to the control group. Statistically significant results are written in bold. BT: behaviour therapy | |||||
| Comparison (X vs Y) | Pairwise meta‐analyses | Network meta‐analysis (tau = 0.63) | ||||||
| # of studies | OR | CI (lower) | CI (upper) | I2 | OR | CI (lower) | CI (upper) | |
| BT vs PT | ‐ | ‐ | ‐ | ‐ | ‐ | 0.56 | 0.12 | 2.67 |
| CBT vs PT | 3 | 1.56 | 0.69 | 3.55 | 30 | 1.80 | 0.69 | 4.67 |
| CBT vs BT | 2 | 4.04 | 0.73 | 22.52 | 72 | 3.16 | 0.93 | 10.71 |
| WL vs PT | 3 | 0.22 | 0.01 | 4.04 | 69 | 0.11 | 0.03 | 0.36 |
| WL vs BT | 1 | 0.02 | 0.00 | 0.32 | ‐ | 0.19 | 0.04 | 0.87 |
| WL vs CBT | 6 | 0.06 | 0.03 | 0.014 | 0 | 0.06 | 0.02 | 0.16 |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). For each comparison X vs Y, an OR greater than one favours treatment X, an OR less than one favours treatment Y. Note that in the main text, where necessary, we inverted the values presented in Table 4 for an easier presentation, in which an OR greater than 1 stands for a higher number of events (short‐term remissions) in the intervention group when compared to the control group. Statistically significant results are written in bold. BT: behaviour therapy | ||||||||
| Comparison (X vs Y) | # of studies | Random‐effects pairwise meta‐analyses | Fixed‐effect pairwise meta‐analyses | ||||
| OR | CI (lower) | CI (upper) | OR | CI (lower) | CI (upper) | ||
| BT vs PT | 2 | 1.09 | 0.22 | 5.52 | 0.96 | 0.27 | 3.46 |
| CT vs PT | 1 | 1.22 | 0.36 | 4.12 | 1.22 | 0.36 | 4.12 |
| CT vs BT | 1 | 0.95 | 0.20 | 4.54 | 0.95 | 0.20 | 4.54 |
| CBT vs SP | 3 | 0.67 | 0.35 | 1.27 | 0.67 | 0.35 | 1.27 |
| CBT vs PT | 4 | 1.43 | 0.78 | 2.62 | 1.43 | 0.78 | 2.62 |
| CBT vs BT | 10 | 2.05 | 1.29 | 3.27 | 2.05 | 1.30 | 3.22 |
| CBT vs CT | 1 | 1.69 | 0.35 | 8.22 | 1.69 | 0.35 | 8.22 |
| PT vs WL | 4 | 4.55 | 0.89 | 25.00 | 4.55 | 1.96 | 10.00 |
| BT vs WL | 3 | 8.33 | 2.33 | 25.00 | 5.56 | 2.94 | 11.11 |
| CT vs WL | 2 | 8.33 | 2.22 | 33.33 | 8.33 | 2.22 | 33.33 |
| CBT vs WL | 18 | 9.09 | 4.76 | 20.00 | 5.56 | 3.70 | 8.33 |
| PT vs NT | 1 | 1.43 | 0.41 | 5.00 | 1.43 | 0.41 | 5.00 |
| CT vs NT | 1 | 1.75 | 0.52 | 5.88 | 1.75 | 0.52 | 5.88 |
| PD vs PT | 1 | 4.22 | 1.27 | 13.95 | 4.22 | 1.27 | 13.95 |
| PD vs CBT | 1 | 0.51 | 0.16 | 1.613 | 0.51 | 0.16 | 1.613 |
| OR (X vs Y) is defined as (Odds X)/(Odds Y). For each comparison X vs Y, an OR greater than one favours treatment X, an OR less than one favours treatment Y. Statistically significant results are written in bold. BT: behaviour therapy | |||||||

