Intervenciones comunitarias y en sistemas sanitarios para mejorar la cobertura de atención prenatal y los desenlaces en salud
Información
- DOI:
- https://doi.org/10.1002/14651858.CD010994.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 01 diciembre 2015see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Embarazo y parto
- Copyright:
-
- Copyright © 2016 The Authors. Cochrane Database of Systematic Reviews published by John Wiley & Sons, Ltd. on behalf of The Cochrane Collaboration.
- This is an open access article under the terms of the Creative Commons Attribution‐Non‐Commercial Licence, which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
LM is the guarantor for this review. He contributed to the background and methods section of the protocol. LM, HG and POZ jointly conceived the idea for the review as a response to policy debates in Cameroon. All authors worked on the protocol and approved the final manuscript.
LM and NM assessed trials for inclusion. LM, AD and NM extracted data. AD contributed to the text describing included studies. MR is the review statistician; she adjusted data from cluster trials and prepared all of the meta‐analyses. LM and NM completed the text of the review.
Sources of support
Internal sources
-
Centre for Development of Best Practices in Health, Cameroon.
-
South African Cochrane Centre, Medical Research Council, South Africa.
External sources
-
Effective Health Care Research Consortium, UK.
-
UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Lawrence Mbuagbaw ‐ none known.
Nancy Medley ‐ none known.
Andrea J Darzi ‐ none known.
Marty Richardson ‐ none known.
Theresa A Lawrie ‐ none known.
Kesso Habiba Garga ‐ none known.
Pierre Ongolo‐Zogo ‐ the Centre for the Development of Best Practices receives funding from UKaid through the Effective Health Care Research Consortium, UK to promote and support evidence based health care.
Acknowledgements
We acknowledge the assistance of the Centre for the Development of Best Practices in Health (CDBPH) and the South African Cochrane Centre (SACC). This review is written within the scope of activities of the Effective Health Care Research Consortium (EHCRC).
Nancy Medley's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors alone are responsible for the views expressed in this publication.
We are grateful to Tess Lawrie for her help in preparing the tables of included studies and conducting 'Risk of bias' assessments; she also contributed text for the descriptions of included studies.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), members of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Dec 01 | Health system and community level interventions for improving antenatal care coverage and health outcomes | Review | Lawrence Mbuagbaw, Nancy Medley, Andrea J Darzi, Marty Richardson, Kesso Habiba Garga, Pierre Ongolo‐Zogo | |
| 2014 Feb 27 | Health system and community level interventions for improving antenatal care coverage and health outcomes | Protocol | Lawrence Mbuagbaw, Kesso Habiba Garga, Pierre Ongolo‐Zogo | |
Differences between protocol and review
The are some differences between our published protocol (Mbuagbaw 2014) and the full review.
-
We have deleted the subgroup of single versus combined interventions because this analysis has been captured at the comparison level.
-
Three new co‐authors have joined the review team: N Medley, A J Darzi, M Richardson and T Lawrie.
-
We have used the GRADE approach as outlined in the GRADE Handbook to assess the quality of the body of evidence and we have included 'Summary of findings' tables.
-
Methods/Assessment of Risk of bias: ‐ due to the inclusion of cluster‐randomised trials in the review, we have added several recommended 'Risk of bias' domains, including recruitment bias and analysis bias
-
Methods/Measures of treatment effect/Dichotomous data ‐ we have presented these results as summary odds ratios not summary risk ratios as stated in our protocol.
-
Methods/Assessment of heterogeneity ‐ we have added the following text: "We have left the overall totals turned off only if the effect estimates of different trials were so disparate that it made little clinical sense to combine the trials (for example, if effect estimates fell on opposite sides of the line of no difference and the trials' confidence intervals do not overlap). Overall, even with high heterogeneity in several outcomes, the effect estimates were reasonably similar, and confidence intervals always overlapped. We have not turned off the totals for any outcome below".
-
Methods/Unit of analysis issues ‐ we have expanded this section. We have provided more details about how we handled cluster‐randomised trials. We have expanded the methods for 'other unit of analysis issues' relating to studies with multiple treatment arms. We have also discussed issues relating to studies involving multiple pregnancies.
-
Methods/subgroup analysis and investigation of heterogeneity ‐ we have removed 'single versus combined interventions' from our list of planned subgroup analyses since this is a comparison rather than a subgroup analysis.
-
We did not measure agreement during the screening and data extraction processes.
-
Methods/types of studies ‐ in our protocol we did not specify whether studies published in abstract form were eligible for inclusion. In the full review we have clarified that "Trials reported in abstract form were eligible for inclusion in the review; however, we did not include any trial based on an abstract report alone."
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Female; Humans; Infant, Newborn; Pregnancy;
PICO

Study flow diagram.
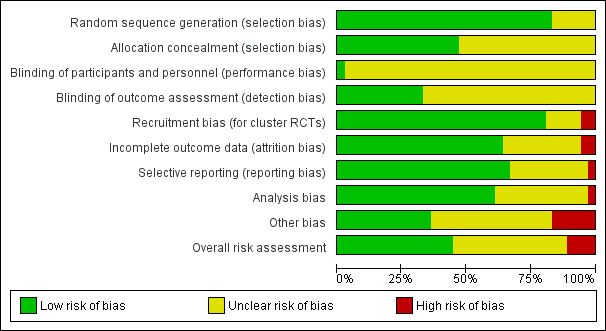
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
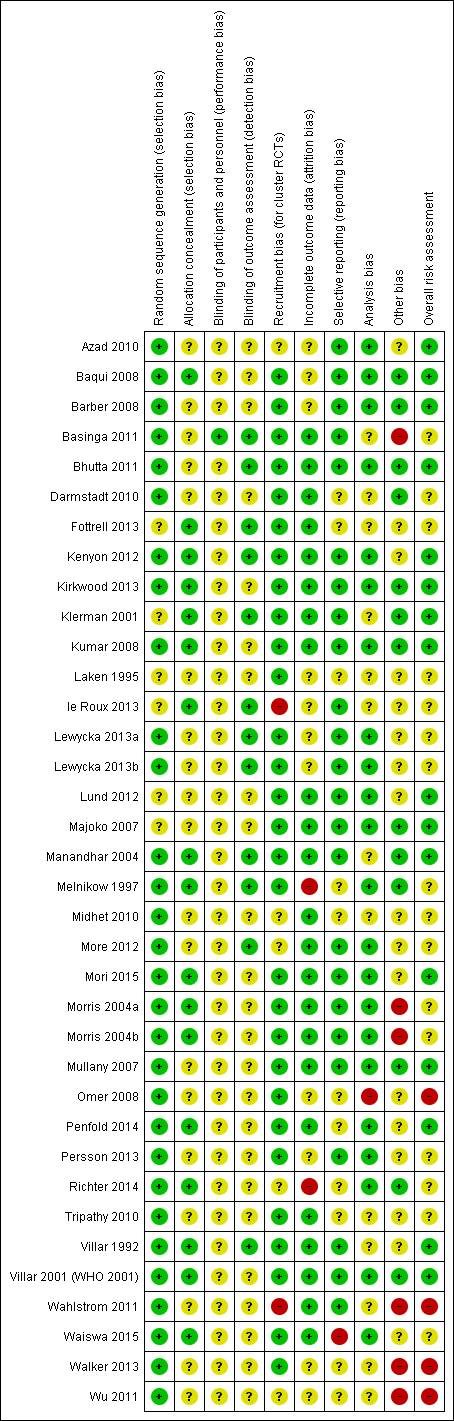
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
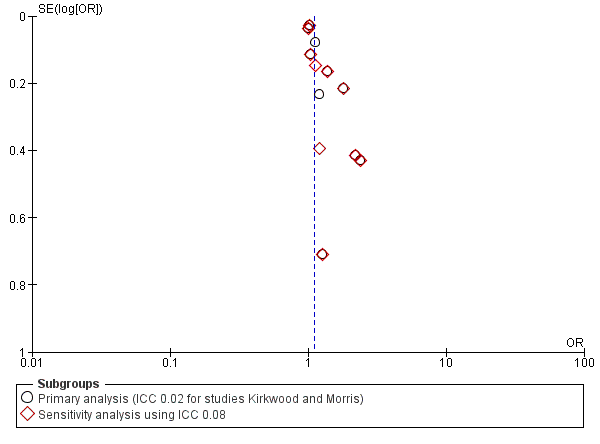
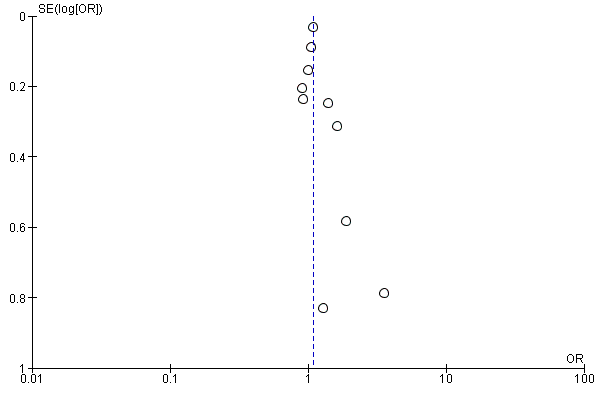
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.1 ANC coverage: four or more visits.
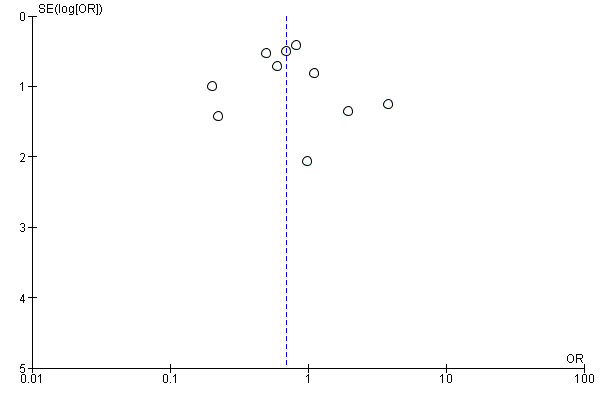
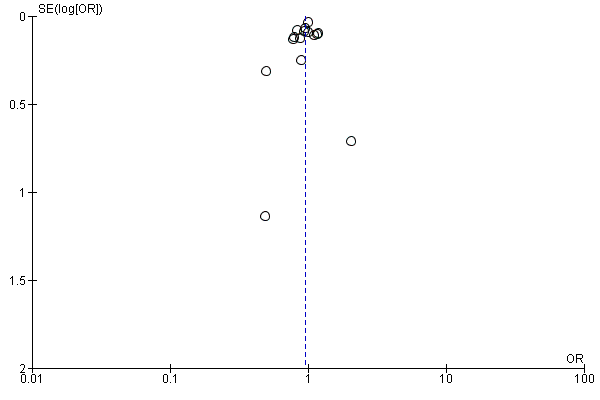
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.2 Pregnancy‐related deaths.
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.6 Deliveries in a health facility.
Funnel plot of comparison: 1 One intervention versus no intervention, outcome: 1.13 Perinatal mortality.
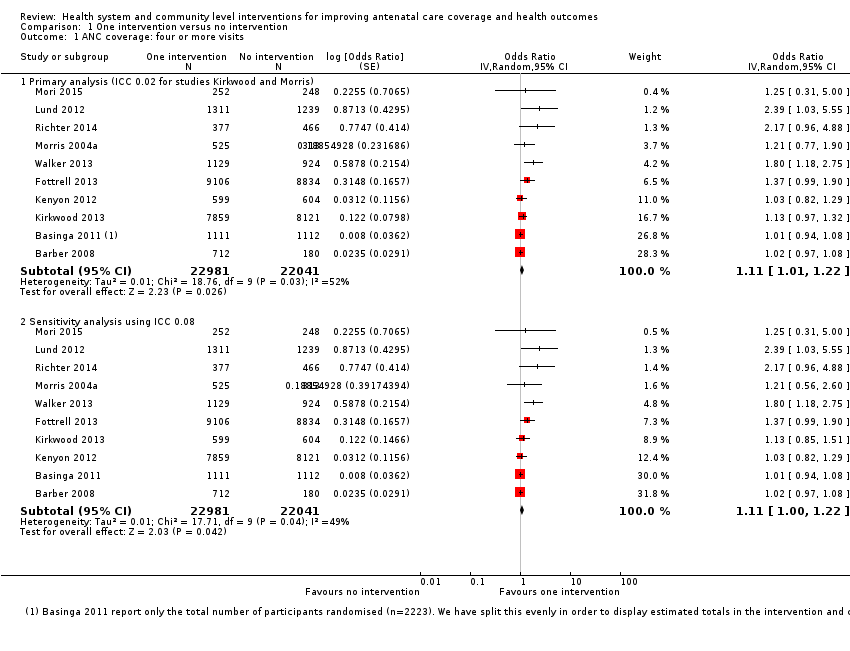
Comparison 1 One intervention versus no intervention, Outcome 1 ANC coverage: four or more visits.

Comparison 1 One intervention versus no intervention, Outcome 2 Pregnancy‐related deaths.
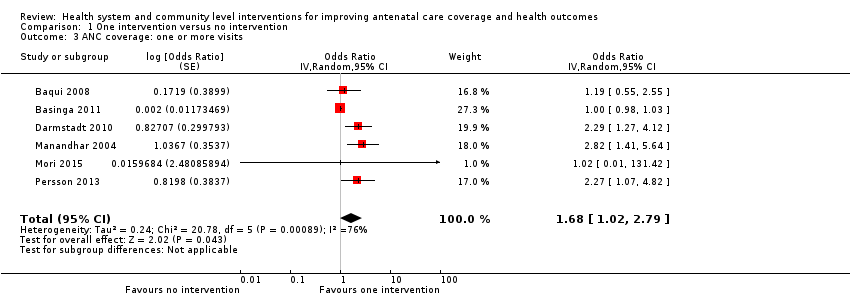
Comparison 1 One intervention versus no intervention, Outcome 3 ANC coverage: one or more visits.
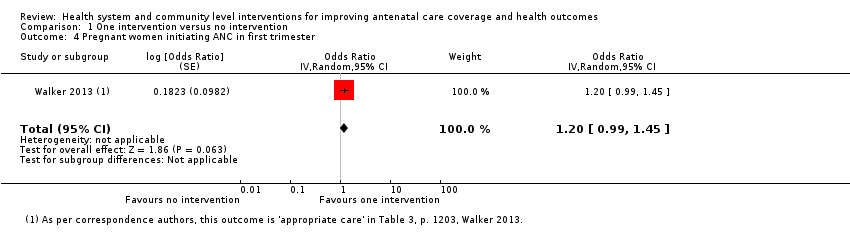
Comparison 1 One intervention versus no intervention, Outcome 4 Pregnant women initiating ANC in first trimester.
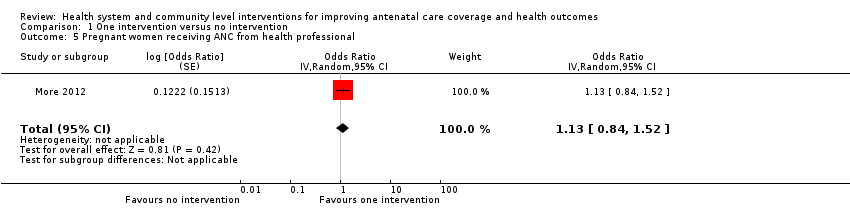
Comparison 1 One intervention versus no intervention, Outcome 5 Pregnant women receiving ANC from health professional.

Comparison 1 One intervention versus no intervention, Outcome 6 Deliveries in a health facility.

Comparison 1 One intervention versus no intervention, Outcome 8 Proportion of women with tetanus protection at birth.
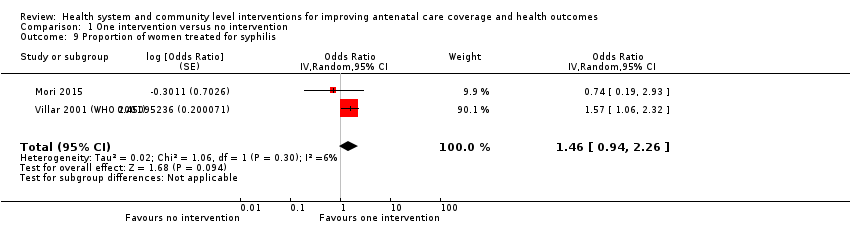
Comparison 1 One intervention versus no intervention, Outcome 9 Proportion of women treated for syphilis.
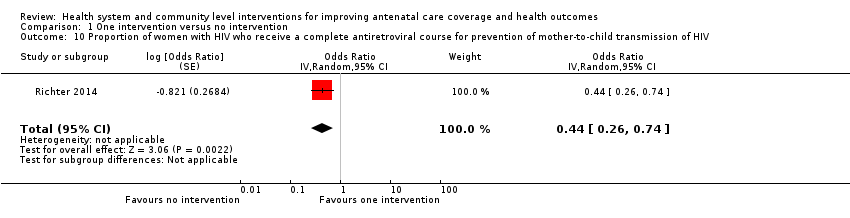
Comparison 1 One intervention versus no intervention, Outcome 10 Proportion of women with HIV who receive a complete antiretroviral course for prevention of mother‐to‐child transmission of HIV.

Comparison 1 One intervention versus no intervention, Outcome 11 Preterm labour.

Comparison 1 One intervention versus no intervention, Outcome 12 Low birthweight.
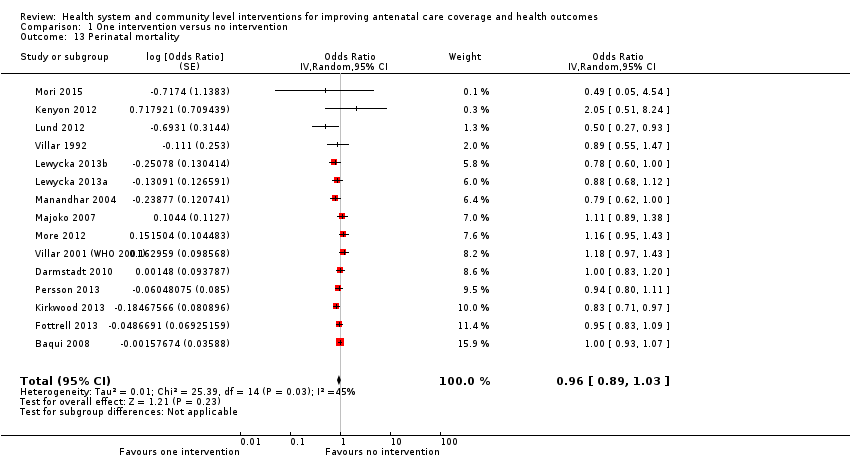
Comparison 1 One intervention versus no intervention, Outcome 13 Perinatal mortality.

Comparison 2 Combination of interventions versus no intervention, Outcome 1 ANC coverage: four or more visits.
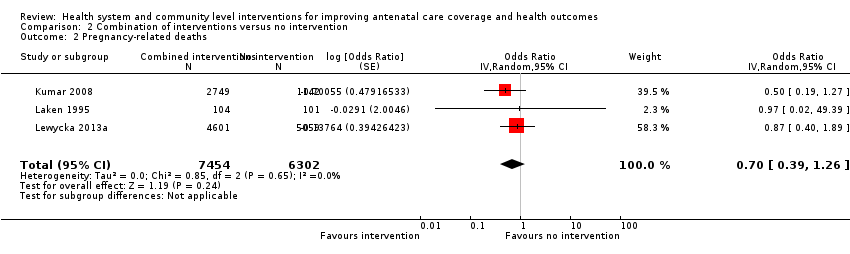
Comparison 2 Combination of interventions versus no intervention, Outcome 2 Pregnancy‐related deaths.
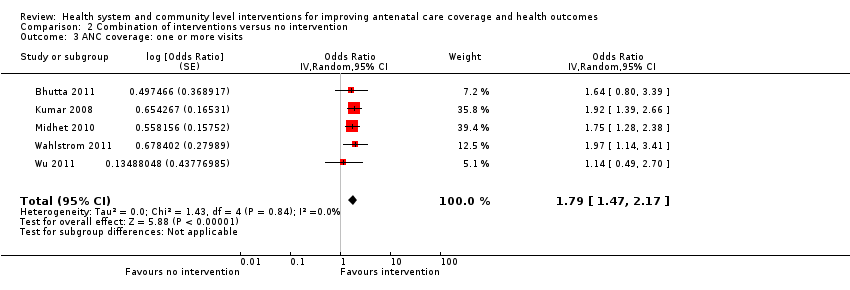
Comparison 2 Combination of interventions versus no intervention, Outcome 3 ANC coverage: one or more visits.

Comparison 2 Combination of interventions versus no intervention, Outcome 4 Pregnant women initiating ANC in first trimester.
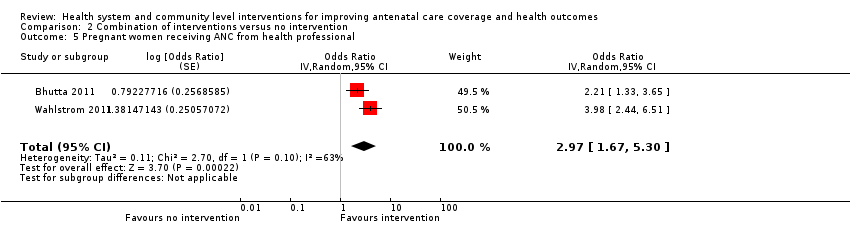
Comparison 2 Combination of interventions versus no intervention, Outcome 5 Pregnant women receiving ANC from health professional.
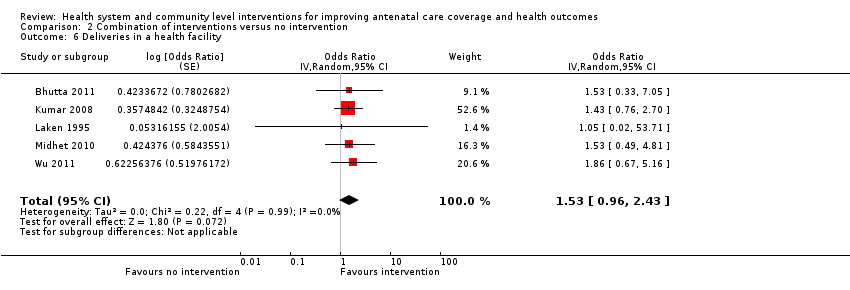
Comparison 2 Combination of interventions versus no intervention, Outcome 6 Deliveries in a health facility.
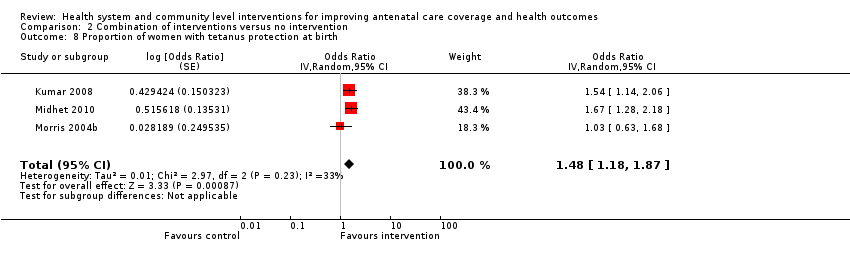
Comparison 2 Combination of interventions versus no intervention, Outcome 8 Proportion of women with tetanus protection at birth.
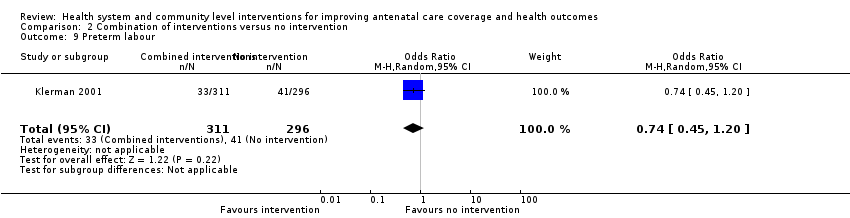
Comparison 2 Combination of interventions versus no intervention, Outcome 9 Preterm labour.

Comparison 2 Combination of interventions versus no intervention, Outcome 10 Low birthweight.
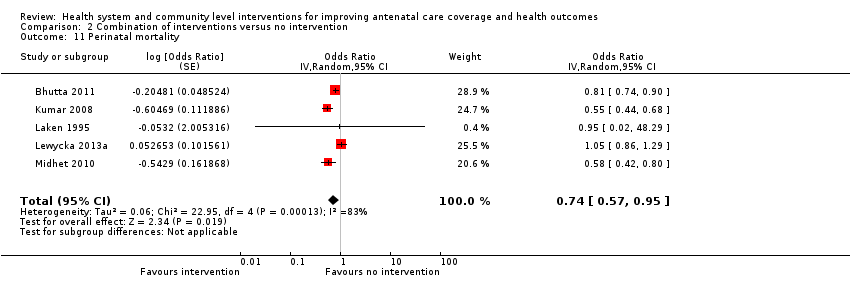
Comparison 2 Combination of interventions versus no intervention, Outcome 11 Perinatal mortality.

Comparison 4 Combination of interventions versus one intervention, Outcome 1 ANC coverage: four or more visits.

Comparison 4 Combination of interventions versus one intervention, Outcome 2 Pregnancy‐related deaths.

Comparison 4 Combination of interventions versus one intervention, Outcome 3 ANC coverage: one or more visits.
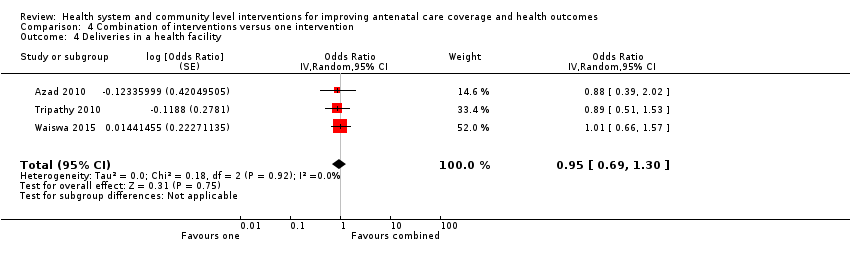
Comparison 4 Combination of interventions versus one intervention, Outcome 4 Deliveries in a health facility.

Comparison 4 Combination of interventions versus one intervention, Outcome 5 Perinatal mortality.
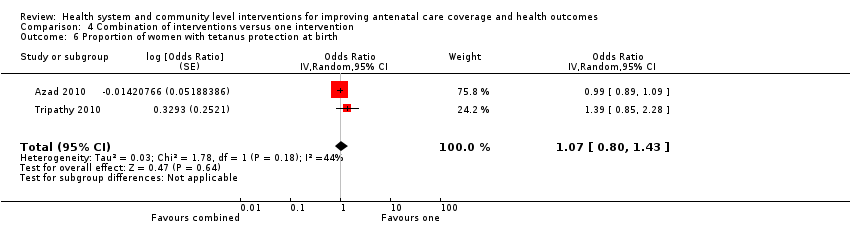
Comparison 4 Combination of interventions versus one intervention, Outcome 6 Proportion of women with tetanus protection at birth.
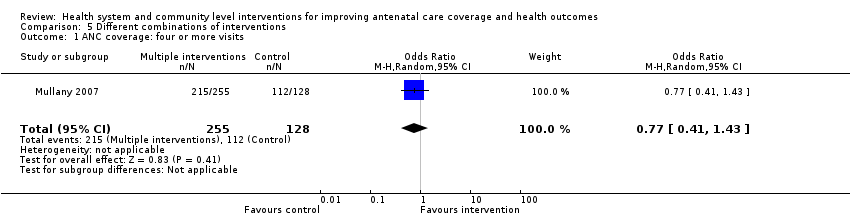
Comparison 5 Different combinations of interventions, Outcome 1 ANC coverage: four or more visits.

Comparison 5 Different combinations of interventions, Outcome 4 Deliveries in a health facility.
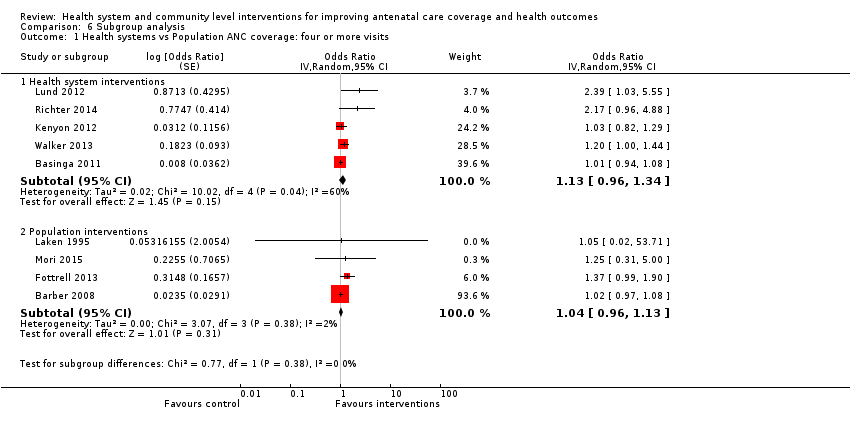
Comparison 6 Subgroup analysis, Outcome 1 Health systems vs Population ANC coverage: four or more visits.
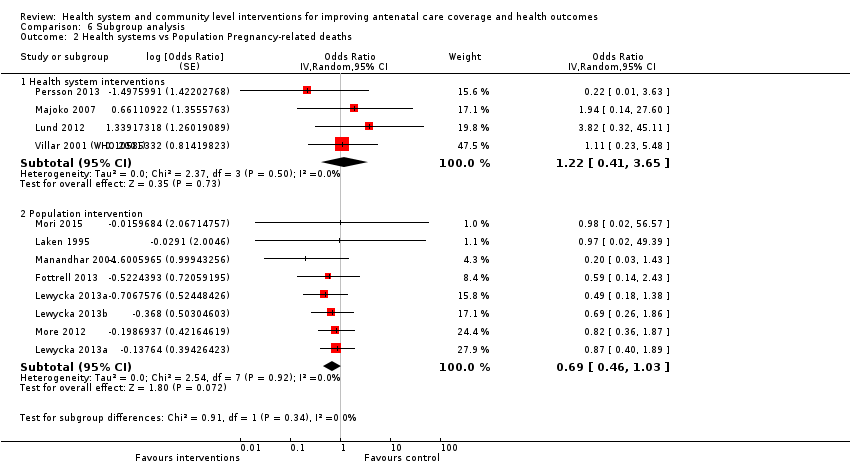
Comparison 6 Subgroup analysis, Outcome 2 Health systems vs Population Pregnancy‐related deaths.

Comparison 6 Subgroup analysis, Outcome 3 Country Income Low vs High ANC at least 4 visits.

Comparison 7 One intervention versus no intervention ‐ Sensitivity analysis by risk of bias, Outcome 1 ANC coverage: four or more visits.
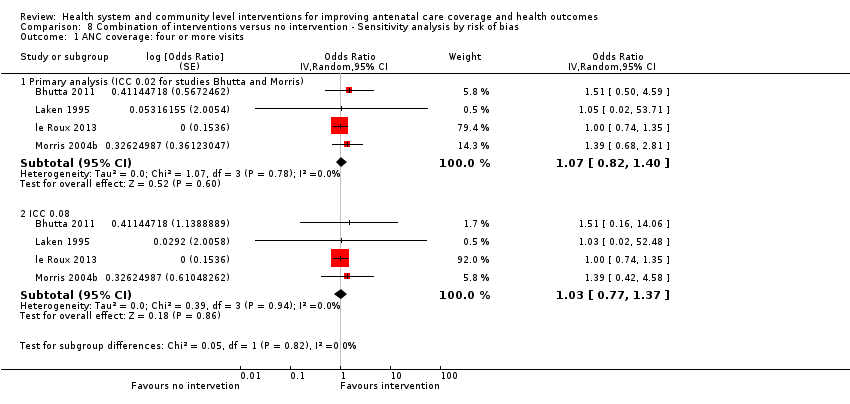
Comparison 8 Combination of interventions versus no intervention ‐ Sensitivity analysis by risk of bias, Outcome 1 ANC coverage: four or more visits.
| Comparison 1: One intervention versus no intervention | ||||||
| Patient or population: improving antenatal care coverage and health outcomes among pregnant women | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with One intervention | |||||
| ANC coverage: four or more visits | Moderate | Average OR 1.11 | 45022 | ⊕⊕⊕⊕ | This is the primary analysis, ICC 0.02. | |
| 529 per 1000 | 555 per 1000 | |||||
| Pregnancy‐related deaths | Moderate | Average OR 0.69 | 114930 | ⊕⊕⊝⊝ | ||
| 700 per 1000000 | 483 per 1000000 | |||||
| ANC coverage: one or more visits | Moderate | Average OR 1.68 | 19281 | ⊕⊕⊕⊝ | ||
| 490 per 1000 | 617 per 1000 | |||||
| Deliveries in a health facility | Moderate | Average OR 1.08 | 74299 | ⊕⊕⊕⊕ | ||
| 645 per 1000 | 662 per 1000 | |||||
| Perinatal mortality | Moderate | Average OR 0.96 | 189164 | ⊕⊕⊕⊝ | ||
| 40 per 1000 | 38 per 1000 | |||||
| Low birthweight | Moderate | Average OR 0.94 | 27154 | ⊕⊕⊕⊕ | ||
| 125 per 1000 | 118 per 1000 | |||||
| Intermittent Prophylactic Treatment for malaria | Study population | not pooled | 00 | No trial included in this review reported this outcome. | ||
| not pooled | not pooled | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio. Denominators for the calculation of the absolute comparative effects have been taken from individual trial reports or from Prost 2013. Where different denominators are stated in different reports, we have taken the larger. The median control group risk has been calculated from event and participant raw data, where this was available. If we found no raw event and participant data in published reports, these trials were not included in the calculation of the median control group risk. Both the participant totals and the median control group risk are for illustrative purposes only. In the majority of the trials in this review, the final odds ratio presented will not correspond with raw event and participant data due to adjustments made for the effects of cluster design. We have designated the control risk as moderate because it is based on the median of a wide range of baseline rates in control groups. | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Statistical heterogeneity, I2 = 52%; we did not downgrade for heterogeneity unless the I2 > 60%. 2 Downgraded one level due to serious risk of bias. Most weight from trials with design limitations (‐1). 3 Downgraded one level due to serious imprecision. Wide confidence interval crossing the line of no effect (‐1). 4 Downgraded one level due to serious inconsistency. Statistical heterogeneity, I2= 76% (‐1). 5 Statistical heterogeneity, I2= 58%; we did not downgrade for heterogeneity unless the I2 > 60%. | ||||||
| Comparison 2: Combination of interventions versus no intervention | ||||||
| Patient or population: improving antenatal care coverage and health outcomes among pregnant women | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with Combination of interventions | |||||
| ANC coverage: four or more visits | Moderate | Average OR 1.48 | 7840 | ⊕⊕⊝⊝ | This is the primary analysis, ICC 0.02. | |
| 430 per 1000 | 528 per 1000 | |||||
| Pregnancy‐related deaths | Moderate | Average OR 0.70 | 13756 | ⊕⊕⊕⊝ | ||
| 600 per 100000 | 421 per 100000 | |||||
| ANC coverage: one or more visits | Moderate | Average OR 1.79 | 12426 | ⊕⊕⊕⊝ | ||
| 580 per 1000 | 712 per 1000 | |||||
| Deliveries in a health facility | Moderate | Average 1.53 | 12314 | ⊕⊕⊕⊝ | ||
| 165 per 1000 | 252 per 1000 | |||||
| Perinatal mortality | Moderate | Average 0.74 | 39130 | ⊕⊕⊕⊝ | ||
| 90 per 1000 | 67 per 1000 | |||||
| Low birthweight | Moderate | Average 0.61 | 2084 | ⊕⊕⊕⊝ | ||
| 165 per 1000 | 101 per 1000 | |||||
| Intermittent Prophylactic Treatment for malaria | Study population | not pooled | 00 | No trial eligible for this comparison reported this outcome | ||
| not pooled | not pooled | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).CI: Confidence interval; RR: Risk ratio; OR: Odds ratio. Denominators for the calculation of the absolute comparative effects have been taken from individual trial reports or from Prost 2013. Where different denominators are stated in different reports, we have taken the larger. The median control group risk has been calculated from event and participant raw data, where this was available. If we found no raw event and participant data in published reports, these trials were not included in the calculation of the median control group risk. Both the participant totals and the median control group risk are for illustrative purposes only. In the majority of the trials in this review, the final odds ratio presented will not correspond with raw event and participant data due to adjustments made for the effects of cluster design. We have designated the control risk as moderate because it is based on the median of a wide range of baseline rates in control groups. | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Most weight from trials with design limitations (‐1). 2 Statistical heterogeneity, I2 = 48% ; we did not downgrade for heterogeneity unless the I2 > 60%. 3 Wide confidence interval crossing the line of no effect (‐1). 4 Statistical heterogeneity, I2 = 83% (‐1). | ||||||
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Barber 2008 | Beta coefficient: 0.0235 (Cash transfer, instrumental variable model; p. 1411, Barber 2008) | Calculate exp(beta) to get OR and CI | 712 | 180 |
| Basinga 2011 | Beta (95% CI): 0.008 (‐0.063 to 0.079) | Calculate exp(beta) to get OR and CI | Reported only the total n, stated as = 2223 | |
| Fottrell 2013 | Adjusted Odds Ratio (95%CI) 1.37 (0.99 to 1.88) | Cluster adjusted, straight into RevMan | 9106 | 8834 |
| Kenyon 2012 | RR = 1.01 (95% CI 0.91 to 1.13) | Non‐cluster trial, calculated OR | 322/599 | 320/604 |
| Kirkwood 2013 | RR 1·02 (0·96 to 1·09) | Adjusted using ICC 0.02 | 5975/7859 | 5988/8121 |
| Lund 2012 | Adjusted OR 2.39 (1.03 to 5.55) adjusted for cluster effect and significant variables | Cluster adjusted, straight into RevMan | 574/1311 | 385/1239 |
| Mori 2015 | Adjusted OR 1.25 (0.31 to 5.00) trial statistician (H Noma) calculated unpublished OR for this systematic review. OR adjusted for cluster effect and significant variables. | Cluster adjusted, straight into RevMan | 243/252 | 237/248 |
| Morris 2004 | Calculated from change scores, Table 2 Program effects p. 2034 of main report. | Adjusted using ICC 0.02 | 166/293 + 112/232 | 151/313 |
| Walker 2013 | Adjusted OR 95% CI 1.8(1.2 to 2.8). OR adjusted various characteristics and cluster ('in accordance with WHO standards' from Table 3, p. 1203 Walker 2013) | Cluster adjusted, straight into RevMan | 78/1129 | 39/924 |
| 1Main analysis with ICC of 0.02. We decided to use the same ICC for this outcome as for Proportion of women with one ANC visit. ICC of 0.02 provided in Manandhar 2004 and Wu 2011. We performed sensitivity analyses with the ICC of 0.08, a midrange of the ICC values in Pagel 2011. | ||||
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Lewycka 20132 women's groups only | Adjusted | 14/4773 | 15/2530 | |
| Lewycka 2013a peer counselling only | Adjusted | 18/4690 | 14/2529 | |
| Lund 2014 | Adjusted | 4/1351 | 1/1286 | |
| Majoko 2007 | OR 1.94 (0.31‐15.2) | Adjusted raw data because the reported OR is asymmetrical. No reply from trial authors regarding our query. | 4/6696 | 2/6483 |
| Manandhar 2004 | Adjusted | 2/2899 | 11/3226 | |
| More 2012 | Adjusted | 20/7656 | 24/7536 | |
| Mori 2015 | Continuity correction for no events in either treatment arm. Unpublished data provided by trial author | 0/252 | 0/248 | |
| Persson 2013 | Adjusted | 1/11,906 | 4/10655 | |
| Fottrell 2013 | Adjusted | 14/8819 | 23/8602 | |
| Villar 2001 | Adjusted | 7/11672 | 6/11121 | |
| 1All data adjusted using an ICC of 0.00247 as suggested by Professor J P Souza by email. 2Mortality data from Trial Profile (Lewycka 2013, p. 1724). Control group (n = 5059) split for this analysis. | ||||
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Basinga 2011 | beta (95% CI): 0.002 (‐0.021 to 0.025); | Calculated ln (OR) and se (ln OR) | Reported only the total n = 2309 | |
| Baqui 2008 | Adjusted | 2297/3421 | 828/1689 | |
| Darmstadt 2010 | Adjusted | 1192/1732 | 864/1759 | |
| Manandhar 2004 | Adjusted OR 2.82 (1.41 to 5.62) | Straight into RevMan. Worked out what ICC they used to adjust for clustering | 1747/3190 | 1051/3524 |
| Mori 2015 | Adjusted OR 1.02 (0.01 to 131.42) trial statistician provided unpublished OR adjusted for clustering and significant variables | Straight into RevMan | 252/252 | 248/248 |
| Persson 2013 | Adjusted OR 2.27 95% CI 1.07 to 4.80. For years 1‐3. | Straight into RevMan | 596/656 | 482/587 |
| 1ICC of 0.02 provided in Manandhar 2004 and Wu 2011. | ||||
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Barber 2008 | Adjusted | 480/776 | 130/203 | |
| Basinga 2011 | beta (95% CI): 0.081 (0.015 to 0.146) | Calculated ln (OR) and se (ln OR) | Reported only total n = 2108 | |
| Darmstadt 2010 | Adjusted | 350/1732 | 290/1759 | |
| Fottrell 2013 | Adjusted Odds Ratio (95%CI) 1.05 (0.88 to 1.25) | Straight into RevMan | ||
| Kirkwood 2013 | Adjusted | 5373/7859 | 5539/8121 | |
| Mojoko 2007 | Adjusted OR for delivery at health centre 1.7 (0.88 to 3.0) ICC used 0.103 | Decided to use delivery at health centre outcome rather than hospital outcome. The OR is asymmetrical so will not go in RevMan ‐ have adjusted the data using the reported ICC 0.103 | Health centre 2660/5261 | 1986/5137 |
| Manandhar 2004 | Adjusted | 201/2945 | 66/3270 | |
| More 2012 | Adjusted OR 0.92 (0.58 to 1.47) | Straight into RevMan | 6602 / 7656 | 6573/ 7536 |
| Penfold 2014 | Adjusted | 187/256 | 166/254 | |
| Persson 2013 | Adjusted OR 1.88 95% CI 0.60 to 5.87. For years 1‐3. | Straight into RevMan | 594/656 | 510/587 |
| 1Data adjusted using ICC 0.103 from Majoko 2007. | ||||
| Trial | Measure of effect | Statistical approach1 | Intervention | Control |
| Kenyon 2012 | RR 0.92 (0.74, 1.14) P = 0.43 | Not cluster trial ‐ calculated OR | 127/605 | 141/613 |
| Mori 2015 | Adjusted OR 0.65 (0.26 to 1.59) trial statistician (H Noma) calculated unpublished OR adjusted for cluster effects and significant variables | Straight into RevMan | 8/251 | 12/247 |
| Richter 2014 | Adjusted | 67/377 | 52/414 | |
| Villar 1992 | OR 0.88 (95% CI 0.67 to 1.16) | Straight into RevMan | 115/1033 | 130/1040 |
| Villar 2001 | Adjusted | 910/11534 | 852/11040 | |
| 1ICC from Piaggio 2001 paper of 0.0004 for ANC trial with average cluster size 426. | ||||
| Trial | Effect Measure | Statistical approach1 | Intervention | Control |
| Baqui 2008 | Adjusted | 2552/32279 | 1260/15914 | |
| Darmstadt 2010 | Adjusted | 224/4800 | 255/5472 | |
| Fottrell 2013 | Risk Ratio (95% CI) adjusted without Tea‐garden residents 0.87 (0.62 to 1.22) | Calculated OR | 474/9106 | 503/8834 |
| Kenyon 2012 | RR 2.04 (0.51 to 8.12) P = 0.30 | Not a cluster trial. Calculated adjusted OR | 6/604 | 3/616 |
| Kirkwood 2013 | Adjusted | 288/8035 | 355/8294 | |
| Lewycka 2013a peer counselling only | Adjusted | 150/4690 | 103/2529 | |
| Lewycka 2013 women's groups only | Adjusted | 173/4773 | 104/2530 | |
| Lund 2012 | Adjusted OR 0.50 (0.27 to 0.93) adjusted for clustering and covariates associated with perinatal mortality | Straight into RevMman | 25/1300 | 44/1236 |
| Majoko 2007 | OR 1.11 (0.89 to 1.39) | 185/6614 | 161/6384 | |
| Manandhar 2004 | Adjusted as below | 123/2972 | 147/3303 | |
| More 2012 | Adjusted | 205/8017 | 173/7844 | |
| Mori 2015 | Unpublished OR 0.49 (0.05 to 4.54) provided by trial statistician (H Noma) adjusted for cluster effect and significant variables | Straight into RevMan | 1/253 | 2/248 |
| Persson 2013 | Adjusted | 283/11906 | 290/10655 | |
| Villar 1992 | OR 0.89 (95% CI 0.55 to 1.47) | Straight into RevMan | 3.6% of 1033 | 4% of 1040 |
| Villar 2001 (WHO 2001) | From Vogel 2013 Adjusted RR 1.18 (1.01 to 1.37). Adjusted for clustering and for risk strata, smoking, education less than primary, hospital admission in last pregnancy, previous surgery on reproductive tract, late booking, vaginal bleeding in the first trimester, age, previous low birth weight, parity. | Calculated adjusted OR | 234/11672 | 190/11121 |
| 1Piaggio 2001 reports ICC for perinatal mortality of 0. | ||||
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Adjusted | 302/2339 | 191/2135 | |
| Laken 1995 | Not cluster trial – two intervention arms added together. calculated ln (OR) and se (Ln OR) | 104/194 | 101/101 | |
| Le Roux 2013 | 1.00 (0.74, 1.34) OR Random effects logistic regression, adjusted for neighbourhood clustering. Models for outcomes among HIV‐positive mothers control for baseline employment. | Straight into RevMan | 474/608 | 439/549 |
| Morris 2004 | Calculated from change scores, Table 2 Program effects p. 2034 of main report. Intervention 38.1% + 18.4% = 56.5% of the final sample size in this group which is 110; 48.9% ‐ 0.7% = 48.2 % in the control group (n = 313). | 62/110 | 151/313 | |
| Manthip 2015 | Adjusted | 62/127 | 53/190 | |
| Wu 2011 | Calculated adjusted SE from P value 0.246 | 376/673 | 253/591 | |
| 1Primary analysis using ICC of 0.02. | ||||
| Study | Measure of effect | Statistical approach | Intervention | Control |
| Kumar 2008 | Adjusted | 12/2749 | 10/1142 | |
| Laken 1995 | 0.9713 (0.0191 to 49.4211) | Straight into RevMan | 0/104 | 0/101 |
| Lewycka 2013 | Adjusted | 23/4601 | 29/5059 | |
| 1All data adjusted using an ICC of 0.00247 as suggested by Professor J P Souza by email. | ||||
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Adjusted | 1616/2339 | 1230/2135 | |
| Kumar 2008 | 24.5% of 2681 intervention and 14.4% of 1129 controls: RR (95%CI); 1.67 (1.47 to 1.91) | Calculated adjusted OR | 657/2681 | 163/1129 |
| Wahlstrom 2011 | Adjusted | 99/127 | 122/190 | |
| Midhet 2010 | Adjusted | Womens group 254/836 | 191/1022 | |
| Wu 2011 | Calculated the ICC that they used to adjust the results using the reported P = 0.758 | 85/88 | 74/77 | |
| 1As for first comparison, ICC of 0.02 used for this outcome. Both Manandhar 2004 and Wu 2011 use ICCS of approximately 0.02 | ||||
| Study | Measure of effect | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Adjusted as below | 1272/2339 | 936/2135 | |
| Kumar 2008 | RR (95%CI); 1.35 (0.88 to 2.07) | Calculated adjusted OR | 507/2681 | 158/1129 |
| Laken 1995 | NOT A CLUSTER TRIAL ‐ calculated OR and confidence interval | 104/104 | 101/101 | |
| Midhet 2010 | Adjusted as below | 46/ 836 in women's group | 39/1022 | |
| Wu 2011 | Calculated what the ICC would have been using the reported adjusted p‐value (P = 0.231) | 625/673 | 517/591 | |
| 1ICC from Wu (0.099). | ||||
| Trial | Statistical approach1 | Intervention | Control |
| Klerman 2001 | Straight into RevMan ‐ not cluster trial | 39/311 | 33/296 |
| Le roux 2013 | Calculated adjusted OR | 88/608 | 123/549 |
| ICC from Piaggio paper of 0.0004 for ANC trial with average cluster size 426 | |||
| Trial | Statistical approach1 | Intervention | Control |
| Bhutta 2011 | Calculated OR | 880/12028 | 972/11005 |
| Laken 1995 | Calculated OR | 0/96 | 0/91 |
| Lewycka 2013 | Calculated OR | 198/4601 | 207/5059 |
| Midhet 2010 | Calculated OR | Women's group 36/836 plus couple's group 42/703 | Control 86/1022 |
| Kumar 2008 | Calculated OR | 219/ 2609 | 155/ 1079 |
| 1Piaggio 2001 reports and ICC of 0 for perinatal deaths. | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ANC coverage: four or more visits Show forest plot | 10 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Kirkwood and Morris) | 10 | 45022 | Odds Ratio (Random, 95% CI) | 1.11 [1.01, 1.22] |
| 1.2 Sensitivity analysis using ICC 0.08 | 10 | 45022 | Odds Ratio (Random, 95% CI) | 1.11 [1.00, 1.22] |
| 2 Pregnancy‐related deaths Show forest plot | 10 | 114930 | Odds Ratio (Random, 95% CI) | 0.69 [0.45, 1.08] |
| 3 ANC coverage: one or more visits Show forest plot | 6 | Odds Ratio (Random, 95% CI) | 1.68 [1.02, 2.79] | |
| 4 Pregnant women initiating ANC in first trimester Show forest plot | 1 | Odds Ratio (Random, 95% CI) | 1.20 [0.99, 1.45] | |
| 5 Pregnant women receiving ANC from health professional Show forest plot | 1 | Odds Ratio (Random, 95% CI) | 1.13 [0.84, 1.52] | |
| 6 Deliveries in a health facility Show forest plot | 10 | Odds Ratio (Random, 95% CI) | 1.08 [1.02, 1.15] | |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Proportion of women with tetanus protection at birth Show forest plot | 8 | Odds Ratio (Random, 95% CI) | 1.03 [0.92, 1.15] | |
| 9 Proportion of women treated for syphilis Show forest plot | 2 | Odds Ratio (Random, 95% CI) | 1.46 [0.94, 2.26] | |
| 10 Proportion of women with HIV who receive a complete antiretroviral course for prevention of mother‐to‐child transmission of HIV Show forest plot | 1 | Odds Ratio (Random, 95% CI) | 0.44 [0.26, 0.74] | |
| 11 Preterm labour Show forest plot | 4 | Odds Ratio (Random, 95% CI) | 1.00 [0.93, 1.09] | |
| 12 Low birthweight Show forest plot | 5 | Odds Ratio (Random, 95% CI) | 0.94 [0.82, 1.06] | |
| 13 Perinatal mortality Show forest plot | 15 | Odds Ratio (Random, 95% CI) | 0.96 [0.89, 1.03] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ANC coverage: four or more visits Show forest plot | 6 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Bhutta and Morris) | 6 | 7840 | Odds Ratio (Random, 95% CI) | 1.48 [0.99, 2.21] |
| 1.2 ICC 0.08 | 6 | 7840 | Odds Ratio (Random, 95% CI) | 1.45 [0.95, 2.23] |
| 2 Pregnancy‐related deaths Show forest plot | 3 | 13756 | Odds Ratio (Random, 95% CI) | 0.70 [0.39, 1.26] |
| 3 ANC coverage: one or more visits Show forest plot | 5 | Odds Ratio (Random, 95% CI) | 1.79 [1.47, 2.17] | |
| 4 Pregnant women initiating ANC in first trimester Show forest plot | 1 | Odds Ratio (Random, 95% CI) | 0.83 [0.47, 1.47] | |
| 5 Pregnant women receiving ANC from health professional Show forest plot | 2 | Odds Ratio (Random, 95% CI) | 2.97 [1.67, 5.30] | |
| 6 Deliveries in a health facility Show forest plot | 5 | Odds Ratio (Random, 95% CI) | 1.53 [0.96, 2.43] | |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Proportion of women with tetanus protection at birth Show forest plot | 3 | Odds Ratio (Random, 95% CI) | 1.48 [1.18, 1.87] | |
| 9 Preterm labour Show forest plot | 1 | 607 | Odds Ratio (M‐H, Random, 95% CI) | 0.74 [0.45, 1.20] |
| 10 Low birthweight Show forest plot | 2 | Odds Ratio (Random, 95% CI) | 0.61 [0.46, 0.80] | |
| 11 Perinatal mortality Show forest plot | 5 | Odds Ratio (Random, 95% CI) | 0.74 [0.57, 0.95] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ANC coverage: four or more visits | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Pregnancy‐related deaths | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 ANC coverage: one or more visits | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Deliveries in a health facility | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Perinatal mortality | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Low birthweight | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ANC coverage: four or more visits Show forest plot | 2 | Odds Ratio (Random, 95% CI) | 0.99 [0.70, 1.40] | |
| 2 Pregnancy‐related deaths Show forest plot | 2 | Odds Ratio (Random, 95% CI) | 1.00 [0.52, 1.96] | |
| 3 ANC coverage: one or more visits Show forest plot | 3 | Odds Ratio (Random, 95% CI) | 0.86 [0.61, 1.20] | |
| 4 Deliveries in a health facility Show forest plot | 3 | Odds Ratio (Random, 95% CI) | 0.95 [0.69, 1.30] | |
| 5 Perinatal mortality Show forest plot | 2 | Odds Ratio (Random, 95% CI) | 0.88 [0.72, 1.07] | |
| 6 Proportion of women with tetanus protection at birth Show forest plot | 2 | Odds Ratio (Random, 95% CI) | 1.07 [0.80, 1.43] | |
| 7 Low birthweight | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ANC coverage: four or more visits Show forest plot | 1 | 383 | Odds Ratio (M‐H, Random, 95% CI) | 0.77 [0.41, 1.43] |
| 2 Pregnancy‐related deaths | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 ANC coverage: one or more visits | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Deliveries in a health facility Show forest plot | 1 | 383 | Odds Ratio (M‐H, Random, 95% CI) | 1.55 [0.71, 3.37] |
| 5 Perinatal mortality | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Low birthweight | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Intermittent Prophylactic Treatment for malaria | 0 | 0 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Health systems vs Population ANC coverage: four or more visits Show forest plot | 9 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Health system interventions | 5 | Odds Ratio (Random, 95% CI) | 1.13 [0.96, 1.34] | |
| 1.2 Population interventions | 4 | Odds Ratio (Random, 95% CI) | 1.04 [0.96, 1.13] | |
| 2 Health systems vs Population Pregnancy‐related deaths Show forest plot | 11 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Health system interventions | 4 | Odds Ratio (Random, 95% CI) | 1.22 [0.41, 3.65] | |
| 2.2 Population intervention | 7 | Odds Ratio (Random, 95% CI) | 0.69 [0.46, 1.03] | |
| 3 Country Income Low vs High ANC at least 4 visits Show forest plot | 18 | Odds Ratio (Random, 95% CI) | 1.14 [1.04, 1.25] | |
| 3.1 Low or lower middle income countries | 11 | Odds Ratio (Random, 95% CI) | 1.21 [1.04, 1.40] | |
| 3.2 High or higher middle income countries | 7 | Odds Ratio (Random, 95% CI) | 1.12 [0.95, 1.32] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ANC coverage: four or more visits Show forest plot | 9 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Kirkwood and Morris) | 9 | Odds Ratio (Random, 95% CI) | 1.07 [0.99, 1.15] | |
| 1.2 Sensitivity analysis using ICC 0.08 | 9 | Odds Ratio (Random, 95% CI) | 1.05 [0.98, 1.14] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ANC coverage: four or more visits Show forest plot | 4 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 Primary analysis (ICC 0.02 for studies Bhutta and Morris) | 4 | Odds Ratio (Random, 95% CI) | 1.07 [0.82, 1.40] | |
| 1.2 ICC 0.08 | 4 | Odds Ratio (Random, 95% CI) | 1.03 [0.77, 1.37] | |

