انجام جراحی با حداقل تهاجم در مقابل رادیوتراپی/شیمیدرمانی در درمان اولیه کارسینوم اوروفارنکس با حجم کم
Referencias
منابع مطالعات خارجشده از این مرور
منابع مطالعات در حال انجام
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| 1) PARTICIPANTS: T1‐4a tumours; all have positive neck disease with extracapsular spread 2) INTERVENTION: all patients have endoscopic head and neck surgery | |
| 1) PARTICIPANTS: advanced (T3‐4) tumours only 2) INTERVENTION: all patients receive endoscopic head and neck surgery/surgical intervention | |
| 1) ALLOCATION: randomisation only after stratification by stage/high‐risk features of excised tumour/neck nodes 2) PARTICIPANTS: T1‐3, N0‐2b 3) INTERVENTION: all patients receive endoscopic head and neck surgery/surgical intervention |
Characteristics of ongoing studies [ordered by study ID]
Ir a:
| Trial name or title | EORTC 1420‐HNCG‐ROG "The best of" trial |
| Methods | Parallel‐group randomised controlled trial |
| Participants | Exact details awaited |
| Interventions | Experimental: Endoscopic head and neck surgery Comparator: Radiotherapy Exact details awaited |
| Outcomes | Primary:
Secondary:
|
| Starting date | Mid 2016 |
| Contact information | Co‐ordinator: Prof Christian Simon |
| Notes | http://www.eortc.org/research‐groups/head‐and‐neck‐cancer‐group/ongoing‐projects/ |
| Trial name or title | A phase II randomised trial for early‐stage squamous cell carcinoma of the oropharynx: radiotherapy vs trans‐oral robotic surgery (ORATOR) |
| Methods | Parallel‐group randomised controlled trial |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Experimental: TORS + neck dissection using Da Vinci Robot. Cautery spatula. 1 cm margins. Frozen sections + proceed until negative margins if feasible. Comparator: Radiotherapy ± chemotherapy Gross tumour and nodes: 70 Gy in 35 fractions over 7 weeks. High‐risk nodal areas: 63 Gy in 35 fractions over 7 weeks. Low‐risk nodal areas: 56 Gy in 35 fractions over 7 weeks |
| Outcomes | Primary:
Secondary:
|
| Starting date | June 2012 |
| Contact information | Primary Investigator: David Palma, MD, PhD; [email protected] London Regional Cancer Program of the Lawson Health Research Institute London, Ontario, Canada, N6A 4L6 Primary Investigator: Anthony Nichols, MD Same address |
| Notes |
ECOG: Eastern Cooperative Oncology Group
MDADI: MD Anderson Dysphagia Inventory
QOL: quality of life
TORS: transoral robotic surgery
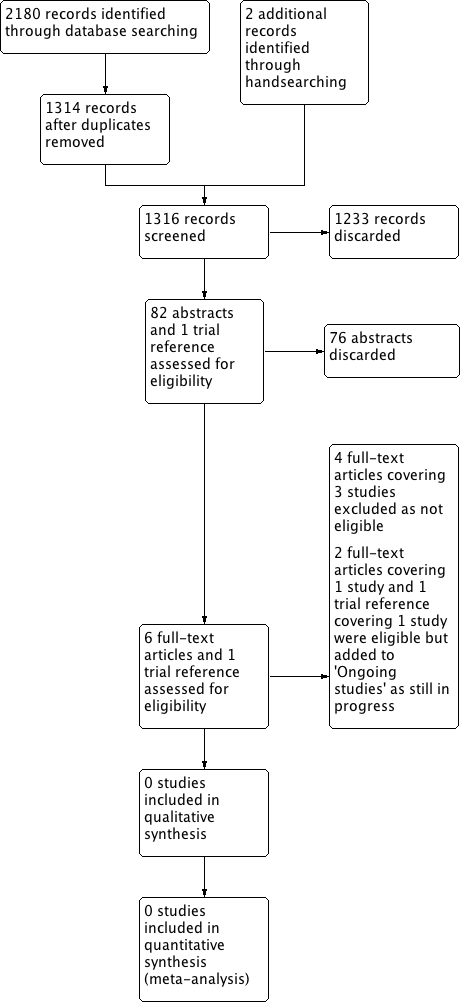
Process for sifting search results and selecting studies for inclusion.
| Minimally invasive surgery versus radiotherapy/chemoradiotherapy for small‐volume primary oropharyngeal carcinoma | ||||||
| Patient or population: patients with small‐volume primary oropharyngeal carcinoma Settings: inpatient Intervention: transoral, minimally invasive surgery (transoral robotic surgery/transoral laser microsurgery) with or without adjuvant radiotherapy or adjuvant chemoradiotherapy Comparison: primary radiotherapy with or without induction or concurrent chemotherapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Primary radiotherapy ± induction or concurrent chemotherapy | Transoral, minimally invasive surgery ± adjuvant radiotherapy or adjuvant chemoradiotherapy | |||||
| Overall survival | No data | No data | No data | No data | — | — |
| Locoregional control | No data | No data | No data | No data | — | — |
| Progression‐free survival | No data | No data | No data | No data | — | — |
| Gastrostomy rate (at 1 year) | No data | No data | No data | No data | — | — |
| Tracheostomy rate | No data | No data | No data | No data | — | — |
| Swallowing function (MDADI) | No data | No data | No data | No data | — | — |
| Quality of life (EORTC QLQ‐C30 and H&N35) | No data | No data | No data | No data | — | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||

