مداخلات ورزشی و باورهای بیمار برای افراد مبتلا به استئوآرتریت مفصل ران، زانو یا مفصل ران و زانو: یک مرور روشهای ترکیبی
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع اضافی
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: OA of knee meeting ACR radiographic grade II, III or IV criteria; aged 50‐69 years; judged to be engaged in independent in daily activity. Exclusion criteria: use of intra‐articular injections in the last 6 months; involved in regular physical activity and physiotherapy, using assistive equipment, unable to exercise, diagnosed with a chronic condition, or a combination of these. Country: Turkey. Sample number: IG: 16; CG: 9. Mean age: 57 years. 100% women. | |
| Interventions | Provider(s): fitness trainer and health technician. Training: yes. Setting: not stated. Content: multicomponent: strength/resistance + aerobic + patient information. Length/intensity: 3 sessions a week for 12 weeks. Control: waiting list. | |
| Outcomes | At 12 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | Low risk | Managed externally to the project. |
| Blinding of participants and personnel (performance bias) | High risk | Not reported. However, participants and providers unlikely to be blinded to exercise intervention. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessments. |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition: IG: 5.8% (1/17); CG: 35.7% (5/14). Lost to follow‐up: IG: 1 reactive arthritis; CG: 2 change of city; 1 low back pain; 1 intra‐articular injection; 1 no contact. ITT/intervention received not reported. Note that there was a higher rate of attrition in the CG, increasing risk, and that some instances may relate to lack of intervention. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: radiographic evidence of knee OA (defined as the presence of osteophytes in the tibiofemoral compartment or the patellofemoral compartment (or both), as assessed on standing anterior/posterior and lateral views), aged 55+ years, BMI ≤ 40 kg/m2; pain on more than half the days of the past month during at least 1 of the following activities; walking, going up or down stairs, standing upright or in bed at night. Exclusion criteria: medical condition that prohibited people from participating safely in an exercise programme, diagnosed with inflammatory arthritis, experience of an exercise programme in the past 6 months (e.g. strength training or > 20 minutes of aerobic activity twice a week, or both). Country: US. Sample number: IG: 22; CG: 22. Mean age: 68 years. Progress Plus: 83% women. | |
| Interventions | Provider(s): not stated. Training: yes. Setting: home. Content: progressive strength training programme Length/intensity: 3 times a week for 16 weeks. Control: attention control; home visits, nutrition education. | |
| Outcomes | At 16 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment by biostatistician. |
| Allocation concealment (selection bias) | Low risk | Allocation concealed from the technician and physician collecting the data. |
| Blinding of participants and personnel (performance bias) | High risk | Authors reported that participants were blinded to the 'active' intervention. However, no further details provided regarding how this was achieved. |
| Blinding of outcome assessment (detection bias) | High risk | Assessor not blinded to participant's group assignment. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IG: 17% (4/22); CG: 13.6% (3/22). Lost to follow‐up reported: IG: 1 severe neck arthritis; 1 prior back injury; 2 lack of time; CG: 2 severe intercurrent illness; 1 diagnostic of psoriatic arthritis. No differences in baseline characteristics of the 8 participants who withdrew when compared to participants who completed trial. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised, placebo‐controlled, participant‐ and assessor‐blinded trial. | |
| Participants | Inclusion criteria: aged ≥ 50 years, hip OA fulfilling ACR classification criteria, pain in groin/hip for > 3 months, mean pain intensity in past week of ≥ 40 on 100 mm VAS, at least moderate difficulty with daily activities. Exclusion criteria: hip or knee joint replacements or both; planned lower limb surgery, physical therapy, chiropractic treatment or prescribed exercises for hip, lumbar spine or both in the past 6 months; walking continuously > 30 minutes daily; regular structured exercise more than once weekly. Sample size: 102; 96 completed intervention, 83 completed follow‐up. IG (n = 49): mean age 64.5 years; CG (n = 53): mean age 62.7 years. Country: Australia. | |
| Interventions | Providers: 8 physical therapists with ≥ 5 years of clinical experience and postgraduate qualifications. Training: yes. Setting: private clinic. Content: semi‐standardised exercises with core components and exercises depending on assessment. Participants given manual therapy techniques and 4‐6 home exercises to perform 4 times a week including strengthening, flexibility and balance exercises. Length/intensity: 10 individual treatment sessions over 12 weeks: 2 sessions in week 1, then once weekly for 6 weeks, then approximately once per fortnight. First 2 sessions were 45‐60 minutes, subsequent sessions were 30 minutes. Control: sham intervention of inactive ultrasound and inert gel applied to hip. No exercise or manual therapy instructions. During follow‐up phases, participants asked to apply gel for 5 minutes 3 times a week. | |
| Outcomes | Musculoskeletal impairments and functional performance tests at baseline and week 13:
Outcomes at 13 and 36 weeks: Primary:
Secondary:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table, results placed in sealed envelopes by independent person. |
| Allocation concealment (selection bias) | Low risk | Opened by another independent person 1 by 1, shortly before the next participant attended, and allocation result emailed to non‐blinded therapist. |
| Blinding of participants and personnel (performance bias) | High risk | IG delivered by non‐blinded therapist: authors acknowledged non‐blinding of therapists was a weakness. Blinding of participants was low risk: checked with James test. Participants informed that the comparison was between physical intervention and sham physical therapy intervention but not what either consisted of. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessor and biostatistician blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: 6 (5.9%) completed did not complete the intervention in both groups and 19 (18.6%) did not complete follow‐up. |
| Selective reporting (reporting bias) | Low risk | Results reported for all measures. |
| Other bias | Low risk | |
| Methods | Assessor‐blinded, 3‐arm randomised controlled trial. | |
| Participants | Inclusion criteria: aged > 50 years, knee OA fulfilling ACR criteria, and at least moderate difficulty with daily activities (WOMAC). Exclusion criteria: "systemic arthritic conditions such as rheumatoid arthritis; medical condition precluding safe exercise such as uncontrolled hypertension or heart condition; self‐reported history of serious mental illness, such as schizophrenia, or self‐reported diagnosis of current clinical depression; neurological condition such as Parkinson's disease, multiple sclerosis or stroke; knee surgery including arthroscopy within the past 6 months or total joint replacement; awaiting or planning any back or lower limb surgery within the next 12 months; current or past (within 3 months) oral or intra‐articular corticosteroid use; physiotherapy, chiropractic or acupuncture treatment or exercises specifically for the knee within the past 6 months; walking exercise for >30 minutes continuously daily; participating in a regular (more than twice a week) structured or supervised (or both) exercise programme such as attending exercise classes in a gym or use of a personal trainer; participating in or previous participation in a formal PCST programme; inability to walk unaided; inadequate written and spoken English; inability to comply with the study protocol such as inability to attend physical therapy sessions or attend assessment appointments at the University." Sample size: 222. Exercise group: 75; mean age: 62.7 years (SD 7.9); 44 women; median symptom duration 6 years. Education group: 74; mean age: 63.0 years (SD 7.9); 45 women; median symptom duration 5.5 years. Combined intervention: 73; mean age 64.6 years (SD 8.3); 44 women; median symptom duration 5.5 years. Country: Australia. | |
| Interventions | Providers: physical therapists, with 11 therapists delivering education and education/exercise treatments and 11 therapists delivering exercise treatments. Training: yes. Setting: private practice. Content: CG: education only (pain education and cognitive and behavioural pain coping skills; exercise only group: 6 exercises to strengthen quadriceps, hamstrings, and hip abductor muscles; exercise + education group. Length/intensity: 10 treatments over 12 weeks + home programme. | |
| Outcomes | Outcomes at 12, 32 and 52 weeks: Primary outcomes:
Secondary outcomes:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers table used for allocations, which were sealed in an envelope by an independent person. |
| Allocation concealment (selection bias) | Low risk | Envelopes opened by another independent person who emailed the therapist shortly before the next participant attended. |
| Blinding of participants and personnel (performance bias) | High risk | Therapists not blinded. Participants blinded to study hypotheses but not to intervention. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Loss to follow‐up from 222 participants: 21 at 12 weeks (9.5%), 41 (27.9%) at 32 weeks and 36 (44.1%) at 52 weeks. |
| Selective reporting (reporting bias) | Low risk | Results reported for all variables. |
| Other bias | Low risk | |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: symptomatic knee OA for ≥ 6 months, no previous yoga training, no current participation in a supervised exercise programme. Exclusion criteria: score < 8 on Short Portable Mental Status Questionnaire; symptoms of joint locking; use of knee brace, walking stick, walker or wheelchair; corticosteroid injection in symptomatic joint within 3 months or hyaluronic acid injection within 6 months of study entry; knee surgery in previous 2 years; joint replacement; self‐reported hypertension; heart condition or other condition with symptoms overlapping with OA. Sample: 36 community‐dwelling women, mean age 72 years, 18 allocated to IG and 18 to CG, 1 participant withdrew from each group. Country: US. | |
| Interventions | Providers: programme developed by 5 certified/registered yoga teachers specifically for older adults with knee OA. All classes taught by same yoga teacher. Training: no specific training, but teacher had 10 years' experience. Setting: small classes (9 participants per class). Content: Hatha yoga. Length/intensity: 1 × 60‐minute class a week for 8 weeks, and instructed to practice for 30 minutes 4 times a week at home using printed instructions. Control: wait‐list control. | |
| Outcomes | Outcomes at baseline; 4, 8 and 20 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random list of numbers from 1 to 36, allocated in the order of enrolment. An even computer‐generated number denoted allocation to the CG and an odd number to the IG. |
| Allocation concealment (selection bias) | Low risk | Allocation carried out blinded. |
| Blinding of participants and personnel (performance bias) | High risk | Participants in wait list control, so no blinding. Low risk for personnel: research assistant enrolling participants and collecting outcome data blinded to group assignment. |
| Blinding of outcome assessment (detection bias) | Low risk | Research assistant enrolling participants and collecting outcome data blinded to group assignment. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IG: 1 (5.6%); CG: 1 (5.6%). |
| Selective reporting (reporting bias) | Low risk | Results for all variables measured reported. |
| Other bias | Low risk | |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: aged 40‐80 years, with radiographically verified minimum joint space (< 4 mm for participants aged < 70 years and < 3 mm for participants aged > 70 years), and a Harris Hip Score 60‐95 points. Exclusion criteria: total hip replacement in the index joint, diagnosed with knee OA or had knee or lower back pain, rheumatoid arthritis, osteoporosis, cancer, cardiovascular disease, dysfunction in lower extremities due to accident or disease, were pregnant, could not participate in exercise, who could not communicate in Norwegian. Sample number: IG: 54; CG: 54. Country: Norway. Mean age: 58 years. Progress‐plus: 56% women; 78.2% > 12 years; 63.6% employed, 20% retired, 14.5%sick‐leave. | |
| Interventions | Provider(s): physical therapist. Training: yes. Setting: healthcare site. Content: strength/resistance + participant education. Length/intensity: 2‐3 times a week for 12 weeks. Control: attention control: patient education. | |
| Outcomes | At 16 months:
| |
| Notes | Included participant education a 'Hip school' comprising of 3 group‐based sessions and 1 individual physical therapy visit, 2 months after completing the group sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using computer‐generated, blocked schedule, administered through numbered, opaque, sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Unlikely that participants or providers were blind to treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Assessors blinded to group allocation throughout trial and analysis period. |
| Incomplete outcome data (attrition bias) | Low risk | IG=23.6% attrition (13/55) CG=33% attrition (18/54) Lost to follow‐up: IG: 6 'total hip replacement' surgery; 7 did not respond; CG: 1 'total hip replacement' surgery; 7 did not respond. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed randomised controlled trial. | |
| Participants | Inclusion criteria: radiographic evidence of tibiofemoral OA as determined by a single observer on the basis of weight‐bearing anteroposterior radiographs; aged > 60 years,; BMI > 28; engaging in < 20 minutes formal exercise a week; difficulty with ≥ 1 of the following activities due to knee pain: walking 0.25 miles, climbing stairs, bending, stooping, kneeling, shopping, house cleaning, getting in or out of bed, standing up from a chair, lifting and carrying groceries, or getting in or out of a bathtub; willingness to undergo testing and intervention procedures. Exclusion criteria: medical condition that precluded safe participation in an exercise programme, mental score < 28; inability to complete the 18‐month study or unlikely to be compliant; inability to walk without a walking stick or other assistive device; participation in another research study; excessive alcohol consumption; or inability to complete the trial protocol, in the opinion of the clinical staff, because of frailty, illness or other reasons. Country: USA. Sample number: IGa: 76; IGb: 80; CG: 78. Mean age: 69 years Progress Plus: 74% women, 22% non‐white, 88% post 16 or higher education (e.g. vocational/college); Income: 19% < USD15,000; 33% USD15,000‐USD35,000; 23% USD35,000‐USD50,000; 26% > USD50,000. | |
| Interventions | Provider(s): not stated. Training: yes. Setting: facility and home. Length/intensity: 3 times a week for 18 months. Intervention content: IGa: exercise (strength/resistance/aerobic) and diet; IGb: exercise (strength/resistance/aerobic). Control: attention control; healthy lifestyle education. | |
| Outcomes | At 18 months:
| |
| Notes | There are 2 Focht 2005 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated block randomisation stratified by race. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) | High risk | Not clear and unlikely that participants or providers were aware of group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of staff to the treatment assignment of the participants. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IGa: 23.7% (18/76); IGb: 20% (16/80); CG: 14% (11/78). Reasons for withdrawal not specified. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: aged 59‐85 years, diagnosed with hip or knee OA using the ACR criteria and living current and chronic (>1 year) hip or knee pain hip or knee pain. Exclusion criteria: involved in recreational physical activity more than twice a week; inability to walk indoors without a walking aide; unstable cardiac conditions or severe pulmonary disease; incontinence, fear of water or uncontrolled epilepsy; low back pain referred to the lower limbs; joint replacement surgery in previous year; arthroscopic surgery or intra‐articular injections within previous 3 months; and current participation in Tai Chi or hydrotherapy. Country: Australia. Sample number: IG: 56; CG: 41. Mean age: 70 years. Progress Plus: 68% women. | |
| Interventions | Provider(s): qualified Tai Chi Master. Training: yes. Setting: not stated. Content: 24 forms from the Sun style of Tai Chi and 10‐minute warm‐up session. Length/intensity: 1 session a week for 12 weeks. Control: waiting list. | |
| Outcomes | At 12 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule, in blocks of 30. |
| Allocation concealment (selection bias) | Low risk | Concealed in an offsite location. |
| Blinding of participants and personnel (performance bias) | High risk | Authors stated that trial involved a physical intervention, therefore participants were not blinded to treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding of outcome assessments. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IG: 7.1% (4/56); CG: 0% (0/43). Lost to follow‐up: IG: 3 withdrew and 1 had knee surgery. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed randomised controlled trial. | |
| Participants | Inclusion criteria: subjective complaint of hip pain with either 1. (a) hip internal rotation < 15° and hip flexion < 115° or (b) > 15° hip internal rotation and pain on hip internal rotation, morning stiffness ≤ 60 minutes, aged > 50 years. 2. Aged 40‐80 years except in (b) above (aged > 50 years). 3. Radiological evidence of OA (2 of the following 3 criteria): osteophytes, joint space narrowing, ESR < 20 mm/hour (ACR Criteria for the Classification and Reporting of Osteoarthritis of the Hip) (Altman 1991). Exclusion criteria: previous hip arthroplasty, history of congenital/adolescent hip disease; clinical signs of lumbar spine disease; physiotherapy in previous 6 months; pregnancy; hip fracture; contraindications to exercise therapy (unstable angina/blood pressure, myocardial infarction in past 3 months, cardiomyopathy, uncontrolled metabolic disease, recent ECG changes, advanced respiratory disease, third‐degree heart block) (AGS 2001); on waiting list for joint replacement within the next 27 weeks; rheumatic diseases (e.g. rheumatoid arthritis, ankylosing spondylitis); intra‐articular hip corticosteroid injection in previous 30 days; insufficient English language to complete questionnaires. Country: Ireland. Sample number: IGa: 43; IGb: 45; CG: 43. Mean age: 61 years. Progress Plus: 61% women, 24% retired, 30% homemaker, 35% employed, 9% other. | |
| Interventions | Provider(s): senior grade or clinical specialist physiotherapists. Training: yes. Setting: hospital and home. Intervention content: IGa: multicomponent: strength/resistance and manual therapy + patient information; IGb: strength/resistance + patient information no manual therapy. Length/intensity: 8 sessions over 8 weeks. Control: wait list. | |
| Outcomes | At 9 weeks:
| |
| Notes | There are 2 French 2013 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple randomisation number table devised in Microsoft Excel 2003. |
| Allocation concealment (selection bias) | Low risk | Group allocation by external research. |
| Blinding of participants and personnel (performance bias) | High risk | Authors stated that blinding not viable in a non‐pharmacological trial. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding undertaken. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IGa: 7% (3/43); IGb: 7% (3/45); CG: 0% (43/43). Lost to follow‐up: IGa: 2 declined, 1 family reasons; IGb: 1 unable to contact, 1 cardiac symptoms, 2 declined, 1 surgery. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All primary outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: self‐reported OA, aged 50‐75 years. Exclusion criteria: on waiting list for knee/hip replacement. Country: Netherlands. Sample number: IG: 35; CG: 35. Mean age: 65 years. Progress Plus: 80% women; 68% living as married; 29% living alone; primary education 17%, secondary education 54%, college/university 27%. | |
| Interventions | Provider(s): physical therapist. Training: yes. Setting: not stated. Content: stretch/balance + patient information. Length/intensity: 1 session a week for 6 weeks. Control: wait list. | |
| Outcomes | At 12 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Limited information. Participants described as ‘randomised.' |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) | High risk | Likely that participants and providers were aware of treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded outcomes assessment. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IG: 0% (0/35); CG: 2.8% (1/35). ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed cluster‐randomised controlled trial. | |
| Participants | Inclusion criteria: aged ≥ 50 years; mild, moderate or severe knee pain of > 6 months' duration. Exclusion criteria: lower limb arthroplasty, physiotherapy for knee pain in the preceding 12 months, intra‐articular injections in the preceding 6 months, unstable medical conditions, inability/unwillingness to exercise, wheelchair dependence and inability to understand English. Participants were not excluded if they used assistive walking devices; had stable comorbidities common in this age group (e.g. type II diabetes, cardiovascular or respiratory disorders); or had back, lower limb pain or upper limb pain. Country: UK. Sample number: IGa: 132 (108 with no missing data points); IGb: 146 (121 with no missing data points); CG: 140 (113 with no missing data points). Mean age: IGa: 66 years; IGb 68 years; CG 67 years. Progress Plus: women:men: IGa 94:38; IGb: 104:42; CG 96:44. | |
| Interventions | Provider(s): physiotherapists. Training: yes. Setting: clinical setting, hospital. Intervention content: intervention: combined discussion on specific topics regarding self‐management and coping, etc., with a progressive exercise regimen delivered to IGa (small groups of participants) and IGb (individual participants). Length/intensity: twice weekly for 6 weeks. Control: usual primary care. | |
| Outcomes | At 24 weeks:
| |
| Notes | There are 2 Hurley 2007 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Primary care practices randomly allocated in blocks of 3. 2 centres were randomly assigned as intervention sites (usual primary care and individual rehabilitation or group rehabilitation) and 1 clinic assigned as control site. |
| Allocation concealment (selection bias) | Low risk | Central allocation. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and providers not blinded to allocation groups. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors blinded to a participant's allocation. Success of blinding evaluated by asking assessors to identify each participant's allocation at each assessment. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: CG: 27/140 (9%); IGa: 24/132 (18%); IGb: 25/146 (17%). Reasons reported. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Cluster randomised controlled trial. | |
| Participants | Inclusion criteria: adults verbally complaining of knee pain or muscle weakness in lower extremity or when they were confirmed by a clinical examination as having OA affecting their knees. Diagnosis of OA of the knee confirmed by medical history and a physical examination. Consisted of having at least 1 of 3 conditions: aged > 50 years; having morning stiffness lasting for < 30 minutes or existing crepitus when moving the legs; or an X‐ray showing osteophytes. Exclusion criteria: previous knee replacement or surgery, unable to maintain balance while standing independently, comorbidity with any medical conditions that could be exacerbated by the protocol, such as unstable heart disease. Country: Taiwan. Sample number: IG: 114; CG: 91. Mean age: 67 years. Progress Plus: gender: mixed; marital status: single/widow: 34.2%, married: 65.8%; elementary/primary school education: 41.2%, high school education: 28.1%, above college education: 30.7%. | |
| Interventions | Provider(s): physical therapist. Training: yes. Setting: community. Content: education; stretching and strengthening exercises and discussion. Length/intensity: 80‐minute sessions 1 × week for 4 weeks. Control: Normal routine care. | |
| Outcomes | At 8 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Lack of information regarding cluster randomisation process. |
| Allocation concealment (selection bias) | High risk | No information. |
| Blinding of participants and personnel (performance bias) | High risk | Not reported, but unlikely that providers and participants were blind to treatment condition. |
| Blinding of outcome assessment (detection bias) | High risk | Unblinded outcomes assessors. |
| Incomplete outcome data (attrition bias) | High risk | Attrition: IG: 14.9% (20/134); CG: 27.2% (34/125). Details of how missing data were handled not reported. No ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐armed randomised controlled trial. | |
| Participants | Inclusion criteria: married adults with persistent knee pain due to OA and who were diagnosed as having OA of the knees and their respective spouses. Exclusion criteria: comorbid medical conditions that could affect health status over course of trial, abnormal cardiac response to exercise or other known organic disease that would contraindicate safe participation in the study. Country: US. Sample number: IGa: 20; IGb: 16; CG: 18. Mean age: 59 years. Progress Plus: 50% women. | |
| Interventions | Provider(s): exercise physiologist and psychologist. Training: yes. Setting: not stated. Intervention content: IGa: spouse‐assisted coping skills training + exercise training (strength/resistance + aerobic) + patient information; IGb: exercise training (strength/resistance + aerobic) + patient information. Length/intensity: 3 × 60‐minute sessions a week for 12 weeks total 50 hours. Control: usual treatment/care with assignment. | |
| Outcomes | At 12 weeks:
| |
| Notes | There are 2 Keefe 2004 lines in some analyses: first indicated IGa and second indicated IGb. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Limited information. |
| Allocation concealment (selection bias) | High risk | No information given. |
| Blinding of participants and personnel (performance bias) | High risk | No information given. |
| Blinding of outcome assessment (detection bias) | High risk | No information given. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IGa: 5% (1/20); IGb: 0% (0/16); CG: 11% (2/18). Reasons for lost to follow‐up not reported. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: women aged ≥ 60 years with OA capable of understanding the information in the questionnaires and the objectives of the study; gave consent to participate; able to detect and record their pain levels (over 3 points on VAS); able to walk and move. Exclusion criteria: none reported. Country: South Korea. Sample number: IG: 35; CG: 35. Mean age: IG: 55‐59 0 (0.0%); 60‐64 11 (31.4%); 65‐69 15 (42.9%); ≥70 9 (25.7%) CG: 55‐59 2 (5.7%); 60‐64 9 (25.7%); 65‐69 17 (48.6%); ≥70 7 (20.0%) Progress Plus: 100% women; education: none 11.4, elementary 14.3, middle school 42.9, high school 14.3, ≥ college 17.1; marital status: married 62.9, bereavement 31.4, other 5.7; income: yes 11.4, none 88.6. | |
| Interventions | Provider(s): certified exercise instructor. Training: yes. Setting: recreational/leisure facilities. Content: patient education; stretching; strengthening exercises; cardiovascular\range of motion, flexibility, muscle strength and endurance. Length/intensity: 3 sessions a week for 12 weeks. Control: usual care. | |
| Outcomes | At 12 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as "simple randomization" of people recruited from a public health centre located in G city, South Korea. |
| Allocation concealment (selection bias) | High risk | Not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Not reported. |
| Blinding of outcome assessment (detection bias) | High risk | Not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition: IG: 12.5% (5/40); CG: 12.5% (5/40). Lost to follow‐up: IG: 1 accident on the pool deck, 2 domestic problems, 2 physical problems; CG: 2 domestic problems; 3 physical problems. Details of how missing data was handled not reported. No ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: adults aged > 55 years with knee OA, considered to be present if 1 or both knees exhibited grade 2 or higher OA by Kellgren and Lawrence (K/L) criteria. Knee pain was considered to be present if participants reported moderate or greater knee pain in the past month (i.e. a rating of ≥3 on a 5‐point Likert scale) for any of the 5 items of the WOMAC pain scale. Exclusion criteria: inability to walk without assistance; amputation of either lower extremity; knee or hip replacement; history of stroke, myocardial infarction, congestive heart failure, uncontrollable hypertension, fibromyalgia, rheumatoid arthritis or other systemic connective tissue disease; lower‐extremity neuropathy; severe cognitive impairment. Country: US. Sample number: IG: 82; CG: 80. Mean age: 69 years. Progress Plus: 84% women. | |
| Interventions | Provider(s): fitness trainer. Training: yes. Setting: National Institute for Fitness and Sport and home based. Content: strength training. Length/intensity: exercise 3 times a week (twice at a fitness facility, once at home) for 12 weeks, followed by transition to home‐based exercise after 12 months. Comparator: attention placebo/alternative intervention; range of motion exercises. | |
| Outcomes | At 30 months:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation scheme allocated participants into 8 groups on the basis of sex and the presence of radiographic evidence of knee OA and knee pain. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and providers not blind to treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded outcome assessor. |
| Incomplete outcome data (attrition bias) | Unclear risk | Breakdown of attrition by group for each follow‐up period not provided. Attrition: entire sample: 30% (66/221); IG: 36%; CG: 24%. Reasons for dropout not reported in full. However, authors described that primary reason was time and travel involved in participating. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Quasi‐experimental partially randomised controlled trial. | |
| Participants | Inclusion criteria: aged > 65 years; living in the community/non‐institutionalised; self‐reported joint pain attributed to OA and in 1 or more of hip, knee, foot or ankle; chronic pain ≥ 15 days a month for > 3 months, pain level ≥ 4 on a 10‐point scale (1 = no pain, 10 = excruciating pain); inability to participate in standing exercise; ability to speak English. Sample size: 34; IG: 23; CG: 11. Mean age: 79 years (SD 6.42). Country: US. Progress Plus: 26 women (76.5%); 21 non‐Hispanic white (61.8%); 19 widowed (55.8%); 27 (79.4%) reported chronic pain for > 3 years; 11 (73.5%) reported highest pain level ≥ 5; 27 (79.4%) taking medication for pain. | |
| Interventions | Providers: Yoga Alliance certified instructors with cardiopulmonary resuscitation certification and ≥ 1 year of yoga teaching experience. Setting: group sessions at a senior centre. Content: chair yoga. Length/intensity: both groups had 45 minutes twice a week for 8 weeks. Control: general health education information and specific facts related to effects of OA. | |
| Outcomes | Outcomes: at 4 and 8 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sealed envelopes; unclear if these were selected 1 by 1 removed from box: this could have made subsequent participants have an increased chance of picking an envelope for a particular condition. |
| Allocation concealment (selection bias) | High risk | 9 participants with more severe Alzheimer's disease were assigned to the intervention condition as the control condition was not suitable for them. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding apparent, and CG participants appeared to have been aware of what the IG entailed (contamination reported by authors). |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | High risk | Attrition: uneven and some uncertainty in reporting. 1 IG (due to unrelated hospitalisation) and 5 CG withdrew (1 due to scheduling and preference for IG, others unspecified. Some inconsistency in reporting: the final reported sample size is "29 participants after 5 participants withdrew" but other reporting suggested 6 withdrawals. |
| Selective reporting (reporting bias) | Low risk | All measured variables had results reported. |
| Other bias | Low risk | No other bias identified. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: aged > 50 years with knee OA. Exclusion criteria: not expecting to be absent from the city for > 2 weeks; having independent non‐institutional lifestyle, not having intra‐articular steroid or visco‐elastic device injections within 2 months preceding intervention period; stable regimen using analgesics or non‐steroidal anti‐inflammatory drugs ≥ 2 weeks before beginning of intervention. Country: Canada. Sample number: IG: 59; CG: 65. Mean age: 66 years. Progress Plus: 70% women; married or living as married 61%; divorced separated 5%; never married: 15%. | |
| Interventions | Provider(s): not stated. Training: yes. Setting: not stated. Content: aerobic strength, stretching and strengthening exercises. Length/intensity: 3 × 1‐hour session a week for 12 weeks. Control: usual treatment/care, with assignment, continued usual activities and attended 1‐hour education/information session twice a month. | |
| Outcomes | At 12 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Blocked random number tables, stratified according to disease severity. |
| Allocation concealment (selection bias) | High risk | No further information provided. |
| Blinding of participants and personnel (performance bias) | High risk | Unlikely that participants and providers were unaware of treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded outcome assessment. |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition: IG: 14.4% (10/69); CG: 4.4% (3/68). Breakdown of participants lost to follow‐up by group not reported. Authors described medical conditions and lack of time as most common reason for dropout. 1 person withdrew after knee inflammation. Reported difference included dropouts: having a lower educational level, more difficulty performing household tasks, fewer social activities and more joint pain and were more likely to be separated or divorced. No ITT analysis reported. |
| Selective reporting (reporting bias) | Low risk | Selective outcome not apparent. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial, feasibility study. | |
| Participants | Inclusion criteria: aged ≥ 50 years, physician‐confirmed diagnosis of OA of knee, overweight or obese, and written permission to participate from a physician. Exclusion criteria: self‐reported currently doing lower‐extremity exercise ≥ 2 times a week; self‐reported currently fitness walking ≥ 90 minutes a week; unable to read and write English at a level necessary to complete a physical activity diary and questionnaires; did not have, or could not use, a telephone or was unwilling to provide home telephone number; incapable of managing own treatment regimen or scored ≤ 23 on the Mini‐Mental Status Examination (Folstein 1975); self‐reported OA of hip that prohibited participation in fitness walking or inflammatory arthritis; self‐reported current knee conditions such as meniscus tears, knee ligament ruptures or previous unilateral knee replacement surgery; scheduled to undergo major surgical procedure in the next 6 months; currently participating in a drug or psychoeducational trial that may confound, or be confounded by, participation in this study; and contraindications for exercise testing based on American College of Sports Medicine (ACSM 2006) criteria or has resting or exercise responses during baseline maximum‐graded exercise testing that are consistent with the ACSM guidelines suggesting that exercise is contraindicated. Country: US. Sample number: IG: 11; CG: 10. Mean age: 63 years. Progress Plus: 96% women; 54% married; 71% unemployed. | |
| Interventions | Provider(s): physical therapist and nurse. Training: yes. Setting: medical centre and home. Content: multicomponent lower‐extremity flexibility and strengthening exercise and adherence counselling using self‐efficacy strategies. Length/intensity: 15 sessions over 24 weeks; 6 weekly physical activity sessions and 9 biweekly telephone counselling sessions. Control: usual care. | |
| Outcomes | At 12 months:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Limited information provided. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) | High risk | Participants could not be blinded to group assignment. |
| Blinding of outcome assessment (detection bias) | High risk | No information provided. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IG: 15.3% (2/13); CG: 23% (3/13). Reasons for dropout not reported; however, authors report no differences between groups. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | Authors reported no statistically significant baseline differences between intervention and control groups but did not report values. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: aged ≥ 40 years; documented diagnosis of chronic, stable, primary OA of 1 or both knee joints in association with ≥ 4‐month history of symptomatic knee pain occurring during weight‐bearing activities (people with multiple joint involvement, who had undergone major joint surgery, or had a lower joint prosthesis were also eligible); radiographic evidence of primary OA of 1 or both knee joints, as demonstrated by joint‐space narrowing, marginal spur formation or subchondral cyst formation; use of any of the various common, non‐prescription non‐steroidal anti‐inflammatory drugs ≥ 2 days a week; and non‐participation in a regular programme of physical activity at time of enrolment. Exclusion criteria: serious medical conditions for which exercise would be contraindicated, such as unstable angina, significant aortic stenosis, myocardial infarction within the last 3 months or advanced chronic obstructive pulmonary disease; asymptomatic primary OA of 1 or both knees; dementia or inability to give informed consent; non‐ambulation due to amputation, stroke or incapacitating arthritis; or involvement in another treatment programme or study protocol. Country: US. Sample number: IG: 47; CG: 45. Mean age: 72 years. Progress Plus: 75% women; 27% married, 72% unmarried; 96% white American, 3% Hispanic Latino. | |
| Interventions | Provider(s): not stated. Training: yes. Setting: hospital, group based. Content: multicomponent: aerobic + patient education. Length/intensity: 3 sessions a week for 8 weeks. Control: weekly telephone call. | |
| Outcomes | At 12 months:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | High risk | Randomisation conducted by the study co‐ordinator; no mention of concealment. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and providers not blind to treatment allocation. |
| Blinding of outcome assessment (detection bias) | High risk | Unblinded outcomes assessor. |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition: IG: 38.2% (18/47); CG: 48.8% (22/45). Lost to follow‐up: IG: 3 refused to be interviewed, 2 sick in the hospital and unable to complete an interview, 1 death 1, 12 could not be contacted; CG: 3 refused to be interviewed, 2 death, 17 could not be contacted. ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: aged > 55 years, body mass index ≤40 kg/m2, WOMAC pain subscale score (VAS version) >40 (range 0‐500), and fulfilment of the ACR criteria for knee OA with radiographic Kellgren/Lawrence scale knee OA grade ≥ 2. Exclusion criteria: none specified. Country: US. Sample number: IG: 20; CG: 20. Mean age: 72 years. Progress Plus: gender: mixed; high school education: 100%. | |
| Interventions | Provider(s): qualified Tai Chi Master/instructor. Training: yes. Setting: hospital. Content: warm up and review of Tai Chi principles and techniques; Tai Chi exercises; breathing techniques and relaxation methods. Length/intensity: twice weekly for 12 weeks. Control: attention placebo/alternative intervention; wellness education and stretching programme. | |
| Outcomes | At 48 weeks:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment by statistician using computer‐generated numbers to randomise permuted blocks of sizes 2 and 4. |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and providers unblended to treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded outcomes assessment. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition: IG 0% (0/20); CG 0% (0/20). ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | Randomised controlled trial. | |
| Participants | Inclusion criteria: capable of completing questionnaire verbally and either had OA affecting the knee according to self‐report or screening of outpatient medical records. Diagnosis of OA of the knee confirmed by medical history and physical examination based on the clinical criteria of the ACR criteria 1991 (Altman 1986, Altman 1991, Hopkins 2002). Clinical criteria for OA of knee consisted of pain in knee and any 3 of: aged ≥ 50 years; < 30 minutes of morning stiffness; crepitus on active motion; bony tenderness; bony enlargement; or no palpable joint warmth. Exclusion criteria: bed bound, wheelchair bound or loss of balance while standing; knee replacement; currently undergoing active physiotherapy such as hydrotherapy or strengthening exercises; currently receiving acupuncture treatments, since they could over‐exert efforts for exercise compliance and could influence the outcome results masking the results from the intervention itself. Country: Hong Kong. Sample number: IG: 67; CG: 54. Mean age: 64 years. Progress Plus: 88% women; 53% married/living together. | |
| Interventions | Provider(s): nurse. Training: yes. Setting: not stated. Content: multicomponent: stretching/walking/Tai Chi + patient education self‐management programme. Length/intensity: 1 session a week for 16 weeks. Control: usual care. | |
| Outcomes | At 8 months:
| |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table. |
| Allocation concealment (selection bias) | High risk | No information provided. |
| Blinding of participants and personnel (performance bias) | High risk | No information provided. |
| Blinding of outcome assessment (detection bias) | High risk | No information provided. |
| Incomplete outcome data (attrition bias) | High risk | Attrition: IG: 23.9% (21/88); CG: 43.6% (41/94). Missing data between groups not accounted for; no ITT analysis. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias detected. |
ACR: American College of Rheumatology; AIMS: Arthritis Impact Measurement Scale; AQoL‐6D: Assessment of Quality of Life‐6D; BMI: body mass index; CES‐D: Center for Epidemiologic Studies Depression Scale; CG: control group; ECG: electrocardiogram; ESR: erythrocyte sedimentation rate; HADS: Hospital Anxiety and Depression Scale; HRQoL: health‐related quality of life; IG: intervention group; ITT: intention to treat; m: metre; m/s: metres/second; n: number of participants; NRS: numerical rating scale; OA: osteoarthritis; PCST: Pain Coping Skills Training; SD: standard deviation; SF‐12: 12‐item Short Form; SF‐36: 36‐item Short Form; VAS: visual analogue scale; VAP: Visual Analogue Pain Scale; WOMAC: Western Ontario McMaster Universities Osteoarthritis Index.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Intervention: no non‐exercise control group. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: mental health component score. | |
| Intervention: no non‐exercise control group. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only | |
| Intervention: no non‐exercise control group. | |
| Outcome: data not available as mean scores and standard deviations. | |
| Outcome: mental component score given as a total not individual. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: data not available as mean scores and standard deviations. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: data not available as mean scores and standard deviations. | |
| Outcome: data not available as mean scores and standard deviations. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Intervention: no non‐exercise control group. | |
| Outcome: pain only. | |
| Outcome: mental health component score. | |
| Intervention: no non‐exercise control group. | |
| Outcome: pain only. | |
| Intervention: no non‐exercise control group. | |
| Outcome: pain only; additional analysis reported in Focht 2005. | |
| Intervention: no non‐exercise control group. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: mental health component score. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: data not available as mean scores and standard deviations. | |
| Outcome: mental health component score. | |
| Outcome: pain only. | |
| Outcome: pain only. | |
| Outcome: pain only. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 19 | 2144 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.28, ‐0.11] |
| Analysis 1.1  Comparison 1 Exercise versus control, Outcome 1 Pain. | ||||
| 1.1 WOMAC pain | 9 | 1058 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.46, ‐0.21] |
| 1.2 Other pain outcomes | 10 | 1086 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.19, 0.05] |
| 2 Physical function Show forest plot | 13 | 1599 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.37, ‐0.17] |
| Analysis 1.2  Comparison 1 Exercise versus control, Outcome 2 Physical function. | ||||
| 3 Self‐efficacy (SE) Show forest plot | 11 | 1138 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.46 [0.34, 0.58] |
| Analysis 1.3  Comparison 1 Exercise versus control, Outcome 3 Self‐efficacy (SE). | ||||
| 3.1 Six‐minute walk SE | 1 | 115 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.05, 0.83] |
| 3.2 Lorig SE exercise scale | 2 | 168 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.63, 1.27] |
| 3.3 ExBeliefs SE | 1 | 338 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [0.20, 0.66] |
| 3.4 Arthritis SE scale | 1 | 54 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.42, 0.72] |
| 3.5 McAuley SE exercise scale | 1 | 21 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.04, 1.87] |
| 3.6 VAP SE | 1 | 52 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.70, 0.39] |
| 3.7 Arthritis SE scale ‐ pain | 1 | 120 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.04, 0.69] |
| 3.8 SE Score | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.71 [0.07, 1.35] |
| 3.9 ASES pain | 2 | 230 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.11, 0.63] |
| 4 Depression Show forest plot | 7 | 876 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.29, ‐0.02] |
| Analysis 1.4  Comparison 1 Exercise versus control, Outcome 4 Depression. | ||||
| 4.1 Kim | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.88 [‐1.37, ‐0.39] |
| 4.2 Other studies | 6 | 806 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.24, 0.05] |
| 5 Anxiety Show forest plot | 4 | 704 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.26, 0.05] |
| Analysis 1.5  Comparison 1 Exercise versus control, Outcome 5 Anxiety. | ||||
| 6 Stress Show forest plot | 2 | 206 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐7.57, ‐1.95] |
| Analysis 1.6  Comparison 1 Exercise versus control, Outcome 6 Stress. | ||||
| 7 SF‐36 mental health Show forest plot | 5 | 576 | Mean Difference (IV, Fixed, 95% CI) | 5.07 [2.43, 7.72] |
| Analysis 1.7  Comparison 1 Exercise versus control, Outcome 7 SF‐36 mental health. | ||||
| 7.1 Aglamis study | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 32.9 [23.07, 42.73] |
| 7.2 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 2.90 [0.15, 5.65] |
| 8 SF‐36 emotional role Show forest plot | 5 | 576 | Mean Difference (IV, Random, 95% CI) | 11.43 [‐4.06, 26.91] |
| Analysis 1.8  Comparison 1 Exercise versus control, Outcome 8 SF‐36 emotional role. | ||||
| 8.1 Aglamis | 1 | 25 | Mean Difference (IV, Random, 95% CI) | 72.8 [47.14, 98.46] |
| 8.2 Other studies | 4 | 551 | Mean Difference (IV, Random, 95% CI) | 1.76 [‐6.63, 10.14] |
| 9 SF‐36 social function Show forest plot | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| Analysis 1.9  Comparison 1 Exercise versus control, Outcome 9 SF‐36 social function. | ||||
| 9.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| 10 SF‐36 vitality Show forest plot | 5 | 1158 | Mean Difference (IV, Fixed, 95% CI) | 6.06 [3.57, 8.54] |
| Analysis 1.10  Comparison 1 Exercise versus control, Outcome 10 SF‐36 vitality. | ||||
| 10.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 51.9 [34.74, 69.06] |
| 10.2 Other studies | 4 | 582 | Mean Difference (IV, Fixed, 95% CI) | 3.90 [0.55, 7.25] |
| 10.3 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 6.58 [2.78, 10.38] |
| 11 Sleep Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐2.54, 0.34] |
| Analysis 1.11  Comparison 1 Exercise versus control, Outcome 11 Sleep. | ||||

Complex reciprocal inter‐relationship between pain, physical and psychosocial function and exercise (Hurley 2003: permission for reproduction provided by the publishers, Wolters Kluwer).

Effect of erroneous health beliefs (Hurley 2003: permission for reproduction provided by the publishers, Wolters Kluwer).
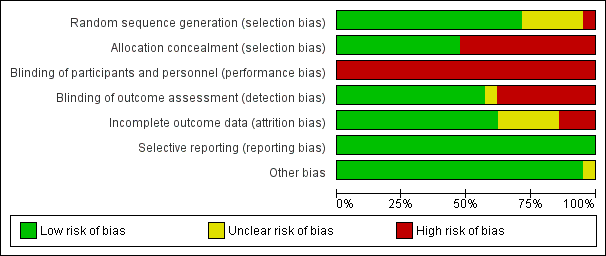
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
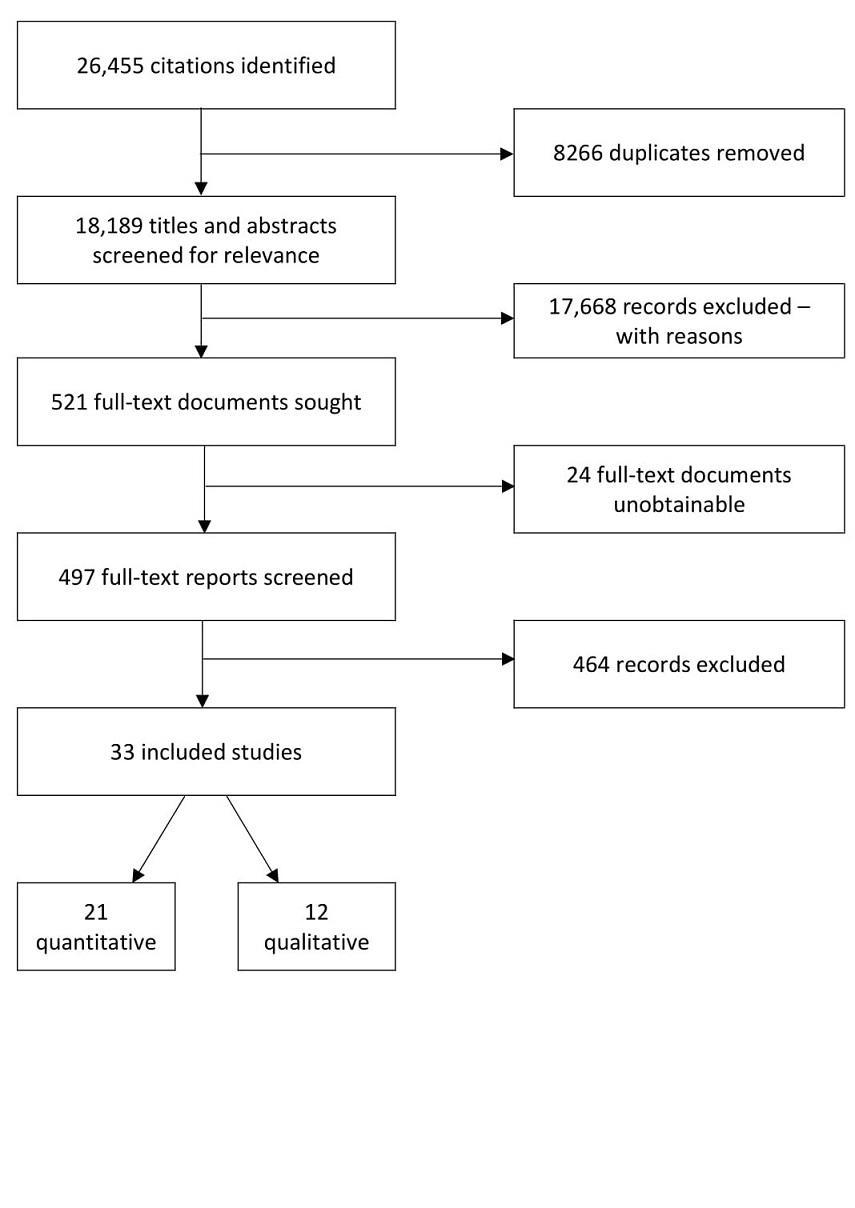
Flow chart of search and screening process.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Emergent themes from qualitative synthesis. OA: osteoarthritis.

Comparison 1 Exercise versus control, Outcome 1 Pain.

Comparison 1 Exercise versus control, Outcome 2 Physical function.

Comparison 1 Exercise versus control, Outcome 3 Self‐efficacy (SE).
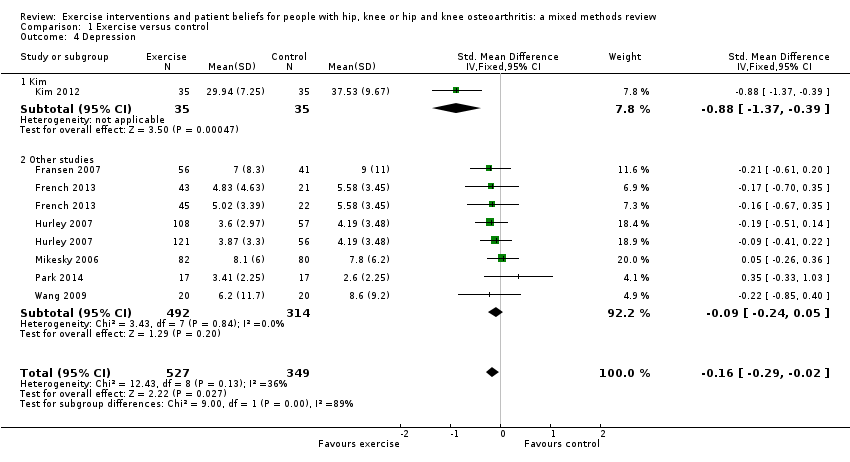
Comparison 1 Exercise versus control, Outcome 4 Depression.
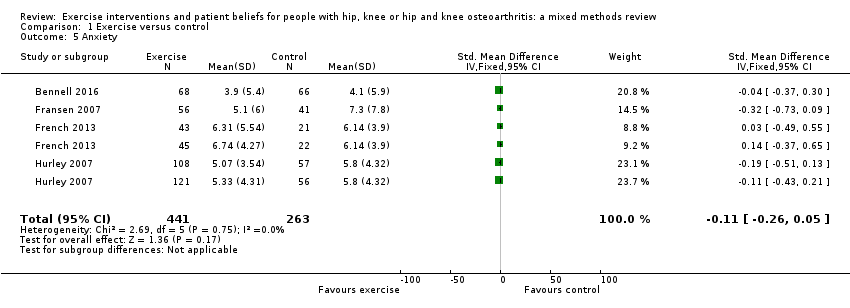
Comparison 1 Exercise versus control, Outcome 5 Anxiety.
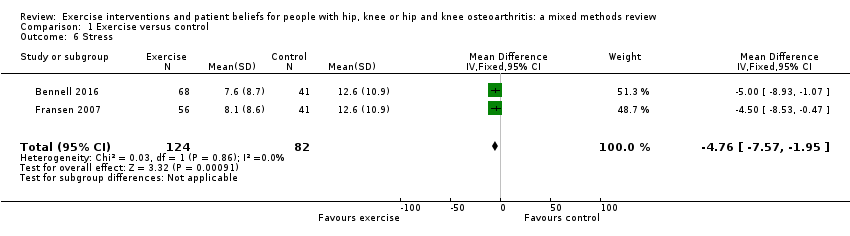
Comparison 1 Exercise versus control, Outcome 6 Stress.
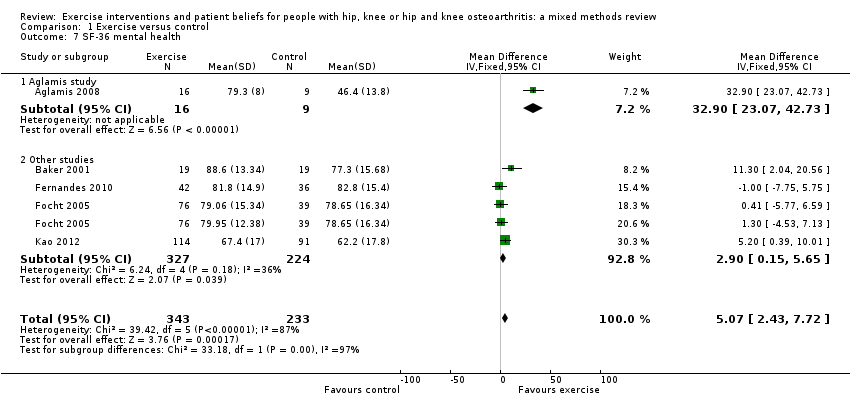
Comparison 1 Exercise versus control, Outcome 7 SF‐36 mental health.
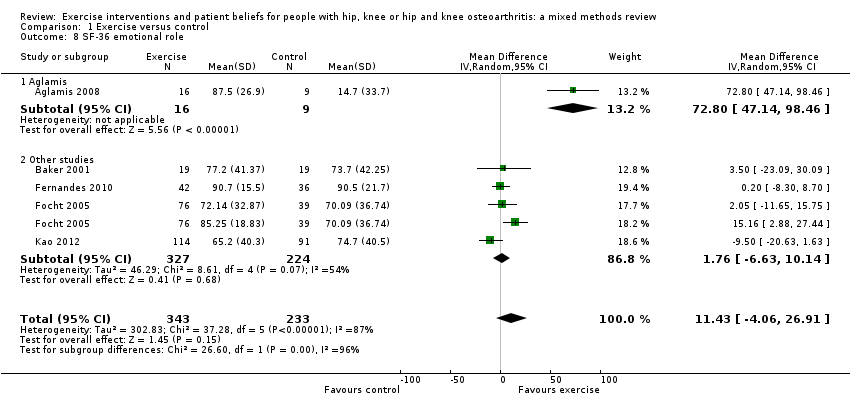
Comparison 1 Exercise versus control, Outcome 8 SF‐36 emotional role.

Comparison 1 Exercise versus control, Outcome 9 SF‐36 social function.

Comparison 1 Exercise versus control, Outcome 10 SF‐36 vitality.

Comparison 1 Exercise versus control, Outcome 11 Sleep.
| Physical and psychosocial outcomes in people with hip, knee or hip and knee osteoarthritis | ||||||
| Patient or population: people with chronic hip, knee or hip and knee osteoarthritis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Exercise | |||||
| Pain. WOMAC normalised to 0‐20 pain scale based on largest study reporting the 0‐20 scale (Hurley 2007). Lower score indicated less pain. Mean duration of follow‐up: 45 weeks (range: 12 weeks to 30 months). | The mean WOMAC pain score was 6.5. | The mean pain in the intervention groups was 1.25 points lower (1.8 to 0.8 lower) | ‐ | 1058 (9 studies) | ⊕⊕⊕⊝ | 6% absolute pain reduction (95% CI ‐9% to ‐4%). 19% relative pain reduction (95% CI ‐27% to ‐11%). SMD ‐0.33 (95% CI ‐0.46 to ‐0.21). |
| Physical function. WOMAC function scales normalised to 0‐100. Lower score indicated improved physical function. Mean duration of follow‐up: 41 weeks (range: 9 weeks to 30 months). | The mean WOMAC function was 49.9. | The mean function in the intervention groups was 5.6 points lower (7.6 to 2.0 lower) | ‐ | 1599 | ⊕⊕⊕⊝ Moderate2 | 5.6% absolute function improvement (95% CI ‐7.6% to 2%). 11.2% relative function improvement (95% CI ‐15.2% to ‐4%). SMD ‐0.27 (95% CI ‐0.37 to ‐0.17). |
| Self‐efficacy. Self‐efficacy scores transformed to exercise beliefs score with score range from 17 to 85. Higher score indicated greater self‐efficacy. Mean duration of follow‐up: 35 weeks (range: 12 weeks to 18 months). | The mean self‐efficacy was 64.3. | The mean self‐efficacy in the intervention groups was 1.13 points higher (0.74 to 1.51 higher) | ‐ | 1138 | ⊕⊕⊝⊝ | 1.66% absolute increase in self‐efficacy (95% CI 1.08% to 2.20%). 1.76% relative increase (95% CI 1.14% to 2.23%). SMD 0.46 (95% CI 0.34 to 0.58). |
| Depression. Depression scores were transformed to the HADS depression scale with score range of 0‐21. Lower score indicated less depression. Mean duration of follow‐up: 35 weeks (range: 8 weeks to 30 months). | The mean depression was 3.5. | The mean depression in the intervention groups was 0.5 points lower (1.0 to 0.1 lower). | ‐ | 919 | ⊕⊕⊕⊝ | 2.4% absolute reduction in depression (95% CI ‐4.7% to ‐0.5%). The relative reduction was 14.3% (95% CI ‐2.8% to ‐28%). SMD ‐0.16 (95% CI‐0.29 to ‐0.02). |
| Anxiety. HADS scale of 0‐21. Lower score indicated lower anxiety levels. Mean duration of follow‐up: 24 weeks (range: 9 weeks to 12 months). | The mean anxiety was 5.8. | The mean anxiety in the intervention groups was 0.4 points lower (1.0 lower to 0.2 higher). | ‐ | 704 | ⊕⊕⊕⊝ | 2% absolute improvement in anxiety (95% CI ‐5% to 1%). The relative change was 6.9% (95% CI ‐17.2% to 3.4%). SMD ‐0.11 (95% CI ‐0.26 to 0.05). |
| SF‐36 social function. Domain of SF‐36 considered representative of quality of life: mental health domain largely covered by depression and anxiety above: scale of 0‐100. Higher score indicated improved social function. Mean duration of follow‐up: 36 weeks (range: 8 weeks to 18 months). | The mean social function was 73.6. | The mean SF‐36 social function in the intervention groups was 7.9 (4.1 to 11.6 higher). | ‐ | 576 | ⊕⊕⊝⊝ | 7.9% absolute improvement in social function (95% CI 4.1% to 11.6%). The relative improvement was 8.8% (95% CI 2.7% to 13.9%). |
| Adverse effects of treatment | ‐ | ‐ | ‐ | ‐ | ‐ | Studies did not provide information on adverse events. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Pain downgraded one level due to high risk of bias for blinding of participants. 2Function downgraded one level due to high risk of bias for blinding of participants. 3Self‐efficacy downgraded two levels; one level due to moderate heterogeneity (I2 = 47%) probably due to different measures of self‐efficacy being used in each study, and one level due to high risk of blinding bias. 4Depression downgraded one level due to high risk of blinding bias. 5Anxiety downgraded one level due to high risk of blinding bias. | ||||||
| No | Study | Quality of evidence | |||||
| Dependabilityof findings | Credibilityof findings | ||||||
| Author | Low | Medium | High | Low | Medium | High | |
| 1 | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ | |
| 2 | ‐ | ✔ | ‐ | ‐ | ✔ | ‐ | |
| 3 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 4 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 5 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 6 | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ | |
| 7 | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ | |
| 8 | ‐ | ‐ | ✔ | ‐ | ✔ | ||
| 9 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 10 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 11 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 12 | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ | |
| Quality appraisal question | Answer options | |||
| Not at all/not stated | Few steps | Several steps | A thorough attempt | |
| 1. Were steps taken to increase rigour in sampling? | 0 studies | 1 study | 7 studies Fisken 2016; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Stone 2015 | 4 studies |
| 2. Were steps taken to increase rigour in data collection? | 0 studies | 0 studies | 7 studies Campbell 2001; Fisken 2016; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Veenhof 2006 | 5 studies Hendry 2006; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006 |
| 3. Were steps taken to increase rigour in data analysis? | 0 studies | 0 studies | 6 studies Campbell 2001; Fisken 2016; Hurley 2010; Larmer 2014b; Moody 2012; Stone 2015 | 6 studies Hendry 2006; Hinman 2016; Morden 2011; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 |
| Quality appraisal question | No grounding | Limited grounding/support | Fairly well grounded | Well grounded/supported |
| 4. Were the findings of the study grounded in/supported by data? | 0 studies | 0 studies | 4 studies | 8 studies Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006 |
| Quality appraisal question | Limited breadth and depth | Good/fair breadth, limited depth | Good/fair depth, limited breadth | Good/fair breadth and depth |
| 5. Breadth and depth of findings? | 0 studies | 3 studies | 3 studies | 6 studies Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Stone 2015; Thorstensson 2006 |
| Quality appraisal question | Not at all | A little | Somewhat | A lot |
| 6. To what extent did the study privilege the perspectives and experiences | 0 studies | 0 studies | 6 studies Fisken 2016; Hurley 2010; Moody 2012; Morden 2011; Thorstensson 2006; Veenhof 2006 | 6 studies Campbell 2001; Hendry 2006; Hinman 2016; Larmer 2014b; Petursdottir 2010; Stone 2015 |
| # | Review finding | Relevant papers | CERQual assessment of confidence in the evidence | Explanation of CERQual assessment |
| I. Symptoms | ||||
| Pain, muscle weakness, physical function: the experience of living with pain and its impact dominated people's narratives because it affected most areas of their daily life and became worse over time. Pain levels varied, and were described as episodic and unpredictable. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Morden 2011; Petursdottir 2010; Stone 2015 | High confidence | Low methodological limitations across all studies, with high coherence and high relevance. 3 countries and 4 geographical regions represented by 6 studies. | |
| Capacity to exercise: pain, joint stiffness, fatigue, comorbidity and people's perceptions of their physical fitness, both before and after exercise, restricted the type and amount of exercise people felt able to engage in. Additional efforts required to shower and change exacerbated the difficulties, and people also reported difficulties with fatigue after exercise sessions. | Campbell 2001; Hendry 2006; Hurley 2010; Moody 2012; Petursdottir 2010; Thorstensson 2006 | High confidence | Low methodological limitations for 5 of the 6 studies, high relevance for 5 of the 6 studies, and high coherence. 4 countries and 2 geographical regions represented. | |
| Impact of exercise on the effects of OA: some participants reported dramatic improvements in symptoms as a result of exercising, while some felt there was little or no benefit. Some people believed other treatment routes were more effective. However, for those who did benefit from exercise, function was improved and pain reduced allowing a return to more normal day‐to‐day activities that had been avoided. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | Findings applied to 9 studies, 8 having low methodological limitations and 6 having high relevance. Moderate coherence across the studies. 6 countries and 2 geographical regions represented. | |
| II Health beliefs and views on the management of OA | ||||
| Aetiology and prognosis of OA: people considered OA to be an inevitable result of placing stress on their joints, the ageing process or a hereditary condition, with limited hope of improvement. Expectations that the condition would worsen over time made it difficult to convince people of the scope for improvement through appropriate treatment. | Low confidence | 4 studies representing 2 countries from 2 different geographical regions. Methodological limitations low across all studies, relevance high in 3 of the 4 but medium coherence. | ||
| Non‐exercise management strategies: some people's understanding of how to manage their OA condition was limited to medication (analgesia) or surgery with little awareness of the role of exercise. Views on pain medication and surgery were mostly negative, with concerns of becoming addicted (to medication) and mixed views and hesitancy regarding surgery, with some people unsure it would work while others considered it a worthwhile option. There was a keenness to delay surgery as long as possible. | Low confidence | Low methodological limitations, but only 3 studies with medium‐to‐high relevance and medium coherence, all from the same country. | ||
| Advice and information from health professionals: participants described their experiences of receiving advice and information from health professionals. This was wide‐ranging in its usefulness and detail for people, and some formed negative beliefs due to limitations of the information they were provided with. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Thorstensson 2006 | Medium confidence | Low methodological limitations, high relevance in 5 of the 6 studies, 3 geographical regions represented by 4 countries. Medium coherence. | |
| Health beliefs and managing OA and exercise: attitudes towards exercise in OA were found to be closely linked to beliefs and perceptions regarding aetiology. Negative beliefs were widely held about the OA prognosis which in turn demotivated them from active management of the condition. Some were concerned about exacerbating the condition, and some felt they were too old for exercise to be of benefit. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Thorstensson 2006 | High confidence | Low methodological limitations across the 6 studies with high relevance for all except 1. Medium‐to‐high coherence. 4 countries and 2 geographical regions represented. | |
| Everyday activities (physical activity) versus structured exercise: this relates to whether people felt that general physical activities that took place in everyday life were sufficient to manage OA, or whether structured exercise sessions had additional benefits. Some people did not perceive a difference between the two, and did not see a need for structured exercise, while others felt normal daily activity was insufficient and needed to be supplemented with formal exercise. Some people worked to increase their general physical activity levels in the belief it would be helpful for their OA. | Hendry 2006; Moody 2012; Petursdottir 2010; Thorstensson 2006 | Low confidence | Low methodological limitations in 3 of only 4 studies, 2 regions and 4 countries represented, with high relevance but only medium coherence. | |
| III Psychological factors | ||||
| Impact of OA on people's sense of "self": the limitations of OA meant that activities that people had previously defined themselves by were now compromised. A new sense of self needed to be constructed to help overcome the negative psychological effects of this, taking on alternative social roles to ensure they maintained a sense of purpose and remained 'useful' despite incapacitation. Those who struggled to do so expressed negative emotions and the feeling of being a burden and frustrated with their limitations. | High confidence | 4 studies with low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | ||
| Individual disposition: high self‐efficacy and a positive outlook was seen as vital in ensuring people did not become defined by their OA. This involved the determination to find new ways to cope. Where self‐efficacy was low, there was an avoidance of physical activity because of the belief it would aggravate pain levels. | Low confidence | 2 studies, from 2 countries/regions with good methodological rigour and high relevance overall. However, medium coherence and lack of confidence in this review finding due to paucity of data. | ||
| Psychological benefits of exercise: people reported favourable psychological benefits of exercise. They also appreciated the peer support and social opportunities that accompanied group forms of exercise. | Fisken 2016; Hendry 2006; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Thorstensson 2006 | High confidence | 8 studies with overall low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Influence of programme supervisors: people who undertook supervised exercise programmes valued programme providers who understood their condition and encouraged and facilitated their engagement in exercise. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | 9 studies with overall low methodological limitations. Highly relevant data from 5 countries and 2 geographical regions. High coherence. | |
| IV Social and environmental factors | ||||
| Impact of OA on people's sense of "self": the limitations of OA meant that activities that people had previously defined themselves by were now compromised. A new sense of self needed to be constructed to help overcome the negative psychological effects of this, taking on alternative social roles to ensure they maintained a sense of purpose and remained 'useful' despite incapacitation. Those who struggled to do so expressed negative emotions and the feeling of being a burden and frustrated with their limitations. | High confidence | 4 studies with low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | ||
| Individual disposition: high self‐efficacy and a positive outlook was seen as vital in ensuring people did not become defined by their OA. This involved the determination to find new ways to cope. Where self‐efficacy was low, there was an avoidance of physical activity because of the belief it would aggravate pain levels. | Low confidence | 2 studies, from 2 countries/regions with good methodological rigour and high relevance overall. However, medium coherence and lack of confidence in this review finding due to paucity of data. | ||
| Psychological benefits of exercise: people reported favourable psychological benefits of exercise. They also appreciated the peer support and social opportunities that accompanied group forms of exercise. | Fisken 2016; Hendry 2006; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Thorstensson 2006 | High confidence | 8 studies with overall low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Influence of programme supervisors: people who undertook supervised exercise programmes valued programme providers who understood their condition and encouraged and facilitated their engagement in exercise. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | 9 studies with overall low methodological limitations. Highly relevant data from 5 countries and 2 geographical regions. High coherence. | |
| CERQual: Confidence in the Evidence from Reviews of Qualitative Research; OA: osteoarthritis. | ||||
| Integrative review | Implications for exercise programmes derived from the qualitative synthesis | Mean and 95% CI | ||||||||||||||
| Information/demonstrate improvement | Individually tailored interventions | Challenge beliefs | Practical support | |||||||||||||
| Trial (meta‐analysis comparison) | Recruitment | Intervention | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Pain | Function | Self‐efficacy | Depression | Anxiety |
| Studies with a low risk of bias | ||||||||||||||||
| Local community. | 10 individual sessions of semi‐standardised exercises over 12 weeks plus exercises to perform 4 times a week at home. | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | √ | 0.21 ‐0.19 to 0.61 | 0.09 ‐0.31 to 0.49 | 0.05 ‐0.35 to 0.45 | ‐ | ‐ | |
| Community participants. | 10 treatments over 12 weeks of exercise or exercise and education. | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.33 ‐0.67 to 0.01 | ‐0.81 ‐1.17 to ‐0.46 | 0.61 0.26 to 0.96 | ‐ | ‐0.04 ‐0.37 to 0.30 | |
| Community through flyers, press releases and mailings via local physician practice. | Hatha yoga, once a week in a class + 4 shorter sessions a week at home. | ‐ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.86 ‐1.55 to ‐0.17 | ‐0.42 ‐1.08 to 0.24 | ‐ | ‐ | ‐ | |
| University hospital, local hospital, rehabilitation centre, general practitioners, and local newspaper advert. | 3 group‐based sessions and 1 individual physical therapy visit, 2 months after completing the group sessions. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.30 ‐0.75 to 0.15 | ‐0.47 ‐0.92 to ‐0.02 | ‐ | ‐ | ||
| Local newspapers & social clubs, general practitioners and rheumatologists. | Tai Chi, twice a week, 12 weeks. | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.52 ‐0.93 to ‐0.11 | ‐0.66 ‐1.07 to ‐0.24 | ‐ | ‐0.21 ‐0.61 to 0.20 | ‐0.32 ‐0.73 to 0.09 | |
| General practitioners, rheumatologists, orthopaedic surgeons, and hospital consultants. | 6‐8 individual 30‐minute physiotherapy sessions over 8 weeks. Strength/resistance training and manual therapy + patient information. | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.43 ‐0.96 to 0.10 | ‐0.40 ‐0.83 to 0.03 | ‐ | ‐0.18 ‐0.61 to 0.24 | 0.04 ‐0.39 to 0.46 | |
| General practitioners, rheumatologists, orthopaedic surgeons, and hospital consultants. | 6‐8 individual 30‐minute physiotherapy sessions over 8 weeks. Strength/resistance training + patient information (no manual therapy). | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.55 ‐1.07 to ‐0.03 | ‐0.49 ‐0.92 to ‐0.07 | ‐ | ‐0.16 ‐0.58 to 0.26 | 0.15 ‐0.27 to 0.56 | |
| Inner‐city primary care practices. | Physiotherapist, twice a week, 6 weeks; individual exercise. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.25 ‐0.56 to 0.07 | ‐0.15 ‐0.41 to 0.10 | 0.44 0.12 to 0.76 | ‐0.19 ‐0.50 to 0.13 | ‐0.19 ‐0.51 to 0.13 | |
| Inner‐city primary care practices. | Physiotherapist, twice a week, 6 weeks; group exercise. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.13 ‐0.45 to 0.19 | 0.06 ‐0.19 to 0.19 | 0.42 0.09 to 0.75 | ‐0.09 ‐0.42 to 0.23 | ‐0.11 ‐0.43 to 0.21 | |
| Studies with a high risk of bias | ||||||||||||||||
| ‐ | ‐ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.54 ‐1.37 to 0.30 | ‐0.64 ‐1.48 to 0.20 | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.56 ‐1.16 to 0.05 | ‐0.48 ‐1.08 to 0.12 | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐0.23 ‐0.62 to 0.16 | ‐0.17 ‐0.22 to 0.56 | 0.44* 0.05 to 0.83 | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐0.05 ‐0.33 to 0.44 | ‐0.3 ‐0.42 to 0.36 | ‐ | ‐ | ‐ | |
| ‐ | ‐ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.15 ‐0.55 to 0.24 | ‐ | 0.89* 0.47 to 1.30 | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.54 0.26 to 0.82 | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.13 ‐0.51 to 0.76 | ‐ | 0.36 ‐0.44 to 1.15 | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.42 ‐1.10 to 0.27 | ‐ | ‐0.07 ‐0.89 to 0.74 | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.60 ‐1.07 to 0.12 | ‐ | 1.04 0.05 to 1.54 | ‐0.88 ‐0.37 to 0.39 | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.56 ‐0.88 to ‐0.25 | 0.10 ‐0.21 to 0.41 | ‐ | 0.05 ‐0.26 to 0.36 | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.35 ‐0.33 to 1.03 | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.04 ‐0.32 to 0.39 | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.22 ‐0.52 to 0.08 | ‐0.95* 0.04 to 1.87 | ‐ | ‐ | |
| ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.40 ‐0.95 to 0.16 | ‐ | ‐0.16 ‐0.70 to 0.39 | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.68 ‐1.32 to ‐0.04 | ‐0.17 ‐0.31 to ‐0.03 | 0.71 0.07 to 1.35 | ‐ | ‐ | |
| ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.17 ‐0.53 to 0.19 | ‐ | 0.32 ‐0.04 to 0.69 | ‐ | ‐ | |
| CI: confidence interval. | ||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 19 | 2144 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.28, ‐0.11] |
| 1.1 WOMAC pain | 9 | 1058 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.46, ‐0.21] |
| 1.2 Other pain outcomes | 10 | 1086 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.19, 0.05] |
| 2 Physical function Show forest plot | 13 | 1599 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.37, ‐0.17] |
| 3 Self‐efficacy (SE) Show forest plot | 11 | 1138 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.46 [0.34, 0.58] |
| 3.1 Six‐minute walk SE | 1 | 115 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.05, 0.83] |
| 3.2 Lorig SE exercise scale | 2 | 168 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.63, 1.27] |
| 3.3 ExBeliefs SE | 1 | 338 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [0.20, 0.66] |
| 3.4 Arthritis SE scale | 1 | 54 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.42, 0.72] |
| 3.5 McAuley SE exercise scale | 1 | 21 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.04, 1.87] |
| 3.6 VAP SE | 1 | 52 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.70, 0.39] |
| 3.7 Arthritis SE scale ‐ pain | 1 | 120 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.04, 0.69] |
| 3.8 SE Score | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.71 [0.07, 1.35] |
| 3.9 ASES pain | 2 | 230 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.11, 0.63] |
| 4 Depression Show forest plot | 7 | 876 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.29, ‐0.02] |
| 4.1 Kim | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.88 [‐1.37, ‐0.39] |
| 4.2 Other studies | 6 | 806 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.24, 0.05] |
| 5 Anxiety Show forest plot | 4 | 704 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.26, 0.05] |
| 6 Stress Show forest plot | 2 | 206 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐7.57, ‐1.95] |
| 7 SF‐36 mental health Show forest plot | 5 | 576 | Mean Difference (IV, Fixed, 95% CI) | 5.07 [2.43, 7.72] |
| 7.1 Aglamis study | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 32.9 [23.07, 42.73] |
| 7.2 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 2.90 [0.15, 5.65] |
| 8 SF‐36 emotional role Show forest plot | 5 | 576 | Mean Difference (IV, Random, 95% CI) | 11.43 [‐4.06, 26.91] |
| 8.1 Aglamis | 1 | 25 | Mean Difference (IV, Random, 95% CI) | 72.8 [47.14, 98.46] |
| 8.2 Other studies | 4 | 551 | Mean Difference (IV, Random, 95% CI) | 1.76 [‐6.63, 10.14] |
| 9 SF‐36 social function Show forest plot | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| 9.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| 10 SF‐36 vitality Show forest plot | 5 | 1158 | Mean Difference (IV, Fixed, 95% CI) | 6.06 [3.57, 8.54] |
| 10.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 51.9 [34.74, 69.06] |
| 10.2 Other studies | 4 | 582 | Mean Difference (IV, Fixed, 95% CI) | 3.90 [0.55, 7.25] |
| 10.3 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 6.58 [2.78, 10.38] |
| 11 Sleep Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐2.54, 0.34] |

