Intervenções baseadas em exercício físico e crenças dos pacientes em doentes com osteoartrose da anca, do joelho, ou da anca e joelho: uma revisão de métodos mistos
Appendices
Appendix 1. Example of search strategy
CONCEPT 1 OSTEOARTHRITIS TERMS
Controlled vocabulary:
| Arthralgia Osteoarthritis Arthritis Osteoarthritis, Hip Osteoarthritis, Knee Osteoarthritis |
OR
Free text, title and abstract:
| Gonarthros* Coxarthros* Osteoarthr* Arthralgia* Arthrosis "degenerative joint" |
OR
Terms used in conjunction – both columns ANDed:
| Controlled vocabulary · Musculoskeletal Diseases · Chronic Pain · Pain · Joint Diseases OR freetext in title and abstract · "joint pain" · "chronic joint" · arthriti* · "Chronic pain" | Controlled vocabulary · Knee Joint · hip joint · knee · hip OR freetext in title and abstract · Knee · Knees · Hip · hips |
Exclusion of surgery terms.
| Exclude in title: · Arthroplasty · Surgery · Surgical · "hip replacement" · "knee replacement" · osteotomy · arthroscopic · postoperative · "post operative" |
CONCEPT 2 ‐ EXERCISE
Controlled vocabulary
-
Exercise therapy
-
Exercise
-
Muscle Stretching Exercises
-
Physiotherapy
-
Rehabilitation
-
"Tai Ji"
-
Walking
-
Yoga
OR
Free text – title and abstract
Aerobic OR Aerobics OR aquarobics OR balneotherapy OR classes OR exercise OR exercises OR hydrotherapy OR "muscle strength" OR "muscle strengthening" OR "Muscle training" OR "nonpharmacological" OR "non‐pharmacological" OR "nonsurgical" OR "non‐surgical" OR "physical activity" OR "physical therapy" OR "physical training" OR "pool therapy" OR physiotherap* OR pilates OR "resistance training" OR "strength training" OR "T ai Chi" OR "Tai Chi" OR "taichi" OR Walk OR walking OR walks OR yoga OR manipulative therap* OR stretch OR stretches OR stretching
Example of PubMed search
Where mh = MeSH terms, and tiab = title and abstract terms
| #25 | Search #23 AND #24 |
| #24 | Search ("1985"[Date ‐ Publication] : "3000"[Date ‐ Publication]) |
| #23 | Search #19 NOT #22 |
| #22 | Search #21 NOT #20 |
| #21 | Search animals[mh] |
| #20 | Search humans[mh] AND animals[mh] |
| #19 | Search #18 AND #14 |
| #18 | Search #15 OR #16 OR #17 |
| #17 | Search "Exercise therapy"[mh] OR Exercise[mh] OR "Muscle Stretching Exercises"[mh] OR Rehabilitation[mh:noexp] OR "Tai Ji"[mh] OR Walking[mh] OR Yoga[mh] |
| #16 | Search (stretch[tiab] OR stretches[tiab] OR stretching[tiab]) AND (muscle[tiab] OR muscles[tiab] OR physical[tiab] OR physically[tiab]) |
| #15 | Search Aerobic[tiab] OR aerobics[tiab] OR aquarobics[tiab] OR balneotherapy[tiab] OR classes[tiab] OR exercise[tiab] OR exercises[tiab] OR hydrotherapy[tiab] OR "muscle strength"[tiab] OR "muscle strengthening"[tiab] OR "Muscle training"[tiab] OR "nonpharmacological"[tiab] OR "non‐pharmacological"[tiab] OR "nonsurgical"[tiab] OR "non‐surgical"[tiab] OR "physical activity"[tiab] OR "physical activities"[tiab] OR "physical therapy"[tiab] OR "physical therapies"[tiab] OR "physical training"[tiab] OR "pool therapy"[tiab] OR physiotherap*[tiab] OR pilates[tiab] OR "resistance training"[tiab] OR "strength training"[tiab] OR "T ai Chi"[tiab] OR "Tai Chi"[tiab] OR "taichi"[tiab] OR Walk[tiab] OR walking[tiab] OR walks[tiab] OR yoga[tiab] OR "manipulative therapy"[tiab] OR "manipulative therapies"[tiab] OR "water therapy"[tiab] OR "water therapies"[tiab] |
| #14 | Search #13 NOT #12 |
| #13 | Search #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #11 |
| #12 | Search arthroplasty[ti] OR surgery[ti] OR surgical[ti] OR "hip replacement"[ti] OR "knee replacement"[ti] OR osteotomy[ti] OR arthroscopic[ti] OR postoperative[ti] OR "post operative"[ti] |
| #11 | Search #9 AND #10 |
| #10 | Search Knee Joint[mh] OR hip joint[mh] OR knee[mh] OR hip[mh] OR knee[tiab] OR knees[tiab] OR hip[tiab] OR hips[tiab] |
| #9 | Search Musculoskeletal Diseases[mh:noexp] OR "joint pain"[tiab] OR "chronic joint"[tiab] OR arthriti*[tiab] OR "Chronic pain"[tiab] OR "Chronic Pain"[mh] OR Pain[mh:noexp] OR Joint Diseases[mh:noexp] |
| #7 | Search Osteoarthr*[tiab] OR Arthralgia*[tiab] OR Arthrosis[tiab] OR "degenerative joint"[tiab] |
| #6 | Search Arthralgia[mh:noexp] NOT Arthralgia/surgery[mh:noexp] |
| #5 | Search Osteoarthritis[mh:noexp] NOT Osteoarthritis/surgery[mh:noexp] |
| #4 | Search Arthritis[mh:noexp] NOT Arthritis/surgery[mh:noexp] |
| #3 | Search Coxarthros*[tiab] OR Gonarthros*[tiab] |
| #2 | Search Osteoarthritis, Hip[mh] NOT Osteoarthritis, Hip/surgery[mh] |
| #1 | Search Osteoarthritis, Knee[mh] NOT Osteoarthritis, Knee/surgery[mh] |
Appendix 2. Electronic databases and other resources searched
We applied these search strategies for a comprehensive search of the following clinical, public health, psychology, social care databases:
-
Allied and Complementary Medicine (AMED);
-
Applied Social Sciences Index and Abstracts (ASSIA);
-
BiblioMap (EPPI‐Centre database of health promotion research);
-
British Nursing Index (BNI);
-
Cochrane Database of Systematic Reviews (CDSR);
-
Cochrane Central Register of Controlled Trials (CENTRAL);
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL);
-
Database of Abstracts of Reviews of Effects (DARE);
-
Database of Promoting Health Effectiveness Reviews (DoPHER);
-
EMBASE;
-
Health Management Information Consortium (HMIC);
-
Health Technology Assessment (HTA);
-
International Bibliography of the Social Sciences (IBSS);
-
Medline
-
NHS Economic Evaluation Database (NHS EED);
-
Physiotherapy Evidence Database (PEDro) (systematic reviews and appraised randomised trials in physiotherapy);
-
PsycINFO;
-
PubMed;
-
Sociological Abstracts (SOCABS);
-
Social policy and Practice (SPP);
-
Social Services Abstracts;
-
Trials Register of Promoting Health Interventions (TRoPHI);
-
Web of Knowledge.
We handsearched the following resources:
-
Arthritis Australia;
-
Arthritis Foundation (USA);
-
Arthritis New Zealand;
-
Arthritis Society (Canada);
-
Cochrane Collaboration Behavioral Medicine Field Register archive;
-
British library Integrated Catalogue (BLIC);
-
British Index to Theses;
-
Dart Europe;
-
British Library Electronic Theses Online Service (ETHOS);
-
Economic and Social Research Council (ESRC);
-
Evidence Database on Ageing Care;
-
Fade: The North West Grey Literature Service (UK);
-
Google;
-
Google Scholar;
-
New York Academy of Medicine Library Catalogue;
-
Arthritis Care UK;
-
Healthtalkonline.org;
-
NHS Evidence;
-
NHS Health Scotland Library;
-
Opengrey.eu;
-
Rehabdata;
-
Social Science Research Network;
-
Alerts from Rehab database;
-
Northern Ireland Qualitative Archive on Ageism;
-
Arthritis Research Centre of Canada.
Appendix 3. Characteristics of included qualitative studies
Campbell 2001
| Methods | Sampling frame: purposely selected from list of participants in RCT intervention arm of study. Data collection: in depth interviews. Data analysis: constant comparative/thematic analysis. | |
| Stated aim of study | To understand reasons for compliance and non‐compliance with a home‐based exercise regimen by people with osteoarthritis of the knee. | |
| Details of participants | Country: UK. Sample number: 20. Age: ≥ 45 years. Gender: mixed. SES: not stated. Occupation/employment: not stated. | |
| Details of exercise programme | Provider(s): physiotherapists Training: not stated Setting: home‐based Content: strengthening of the vastus medialis component of the quadriceps muscle, medial taping of the patella; advice and information leaflets. Length/intensity: 8 weeks; 9 sessions; 30‐minute duration; and encouraged to continue with the exercises and taping at home. Comparator: general advice about weight reduction and exercise at a single visit. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | A thorough attempt. | |
| Were steps taken to increase rigour in data collection? | Several steps. | |
| Were steps taken to increase rigour in data analysis? | Several steps. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth, but limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | Medium. | |
Fisken 2016
| Methods | Sampling frame: advertising within community to find participants with OA who had discontinued aqua‐based exercise. Data collection: focus groups. Data analysis: general Inductive Thematic Analysis. | |
| Stated aim of study | To provide insight into the factors contributing to older adults with OA ceasing participation in an aqua‐based exercise programme. | |
| Details of participants | Country: New Zealand. Sample number: 11. Age: ≥ 60 years. Gender: female. SES: Not stated Ethnicity: 6 New Zealand European, 2 Maori, 3 others. Occupation/employment: Not stated | |
| Details of exercise programme | Name of programme: Not stated Provider(s): Not stated Training: Not stated Setting: Aqua facilities Content: aqua‐fitness or aqua‐jogging classes attended previously, but no longer attended. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, several attempts. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth, but little depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | Medium. | |
| Credibility of findings | Medium. | |
Hendry 2006
| Methods | Sampling frame: purposely selected from GPs' disease registers and gyms representing geographic and socioeconomic diversity. Data collection: semi‐structured interviews. Data analysis: Framework 'thematic' analysis. | |
| Stated aim of study | To examine the views of primary care patients with OA knee towards exercise, explore factors that determine the acceptability and motivation to exercise, and to identify barriers that limit its use. To examine the views of primary care patients with OA of the knee towards exercise, to explore factors that determine the acceptability and motivation to exercise and to identify barriers that limit its use that could be addressed in primary care consultations. | |
| Details of participants | Country: UK. Sample number: 22. Age: ≥ 50 years. Gender: 16 women. SES: not stated. Ethnicity: not stated. Occupation/employment: not stated. | |
| Details of exercise programme | Not applicable. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, a (fairly) thorough attempt was made. | |
| Were steps taken to increase rigour in data collection? | Yes, a (fairly) thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a (fairly) thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Hinman 2016
| Methods | Sampling frame: sequential purposive sampling to recruit from RCT that recruited from the community. Data collection: semi‐structured individual interviews. Data analysis: thematic analysis guided by grounded theory method: systematic and structured engagement, and interplay and constant comparison. | |
| Stated aim of study | To explore how key stakeholders (physical therapists, telephone coaches and patients) experienced, and made sense of, being involved in delivering or receiving an integrated physical therapy and telephone coaching intervention. | |
| Details of participants | Country: Australia. Sample number: 6 participants (10 physical therapists, 4 telephone coaches). Age: ≥ 50 years. Gender: mixed. SES: Not stated Ethnicity: Not stated Occupation/employment: Not stated | |
| Details of exercise programme | Name of programme: Not stated Provider(s): physiotherapists and telephone coaches. Training: physical therapists: at least 2 years of postgraduate musculoskeletal experience. Coaches completed training programme by HealthChange Australia. Setting: private practice and at home. Content: exercise and physical activity programme with telephone coaching, plus a booklet explaining the benefits of exercise. Coaching component: assistance with behaviour change through effective information exchange, assistance to form behavioural goal intention, and helping to convert intention into action. Exercise component: 4‐6 individualised lower limb exercises performed 3 times a week and advice to increase general physical activity. Coaching component: mean 28 minutes per call, with 6‐12 calls over the 6‐month intervention. Exercise component: 30‐minute consultations in weeks 1, 3, 7, 12 and 20 of a 6‐month period, with exercises carried out 3 times a week. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, fairly thorough attempt. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, fairly thorough attempt. | |
| Were the findings of the study grounded/supported by data? | Well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Hurley 2010
| Methods | Sampling frame: from RCT that recruited from primary care surgery databases. Data collection: semi‐structured interviews. Data analysis: constant comparative/thematic analysis. | |
| Stated aim of study | To explore the health beliefs, experiences, treatment and expectations of people with chronic knee pain, and investigate if, how and why these change after taking part in an integrated exercise‐based rehabilitation programme‐Enabling Self‐management and Coping with Arthritis knee Pain through Exercise. | |
| Details of participants | Country: UK. Sample number: 29 (6 interviewed before the intervention only, 23 interviewed before and after the intervention). Age: ≥ 50 years. Gender: mixed. SES: Not stated Ethnicity: 3 black African, 5 black Caribbean, 1 Indian, 20 Caucasian (White). Occupation/employment: Not stated | |
| Details of exercise programme | Name of programme: ESCAPE. Provider(s): physiotherapists. Training: Not stated Setting: Community, gym of a physiotherapy outpatient department. Content: rehabilitation programme comprising of education component and exercise component. Education component: themed, informal discussion led by a physiotherapist designed to enhance patients understanding of condition, its causes, consequences, prognosis and promote simple self‐management strategies. Exercise component: designed to increase strength, balance and co‐ordination and confidence. Length/intensity: Overall rehabilitation programme: 12 sessions twice weekly for 6 weeks. Education component: 10‐15 minutes. Exercise component: 30‐45 minutes. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Several steps. | |
| Were steps taken to increase rigour in data collection? | Several steps. | |
| Were steps taken to increase rigour in data analysis? | Several steps. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Larmer 2014
| Methods | Sampling frame: via 3 hydrotherapy services in Auckland, with potential participants given information packs by clinicians. Data collection: focus groups, with an option provided for individual interview. Data analysis: content analysis framework with constant comparative methods. | |
| Stated aim of study | To explore the perceived benefits of hydrotherapy from a patient's perspective. | |
| Details of participants | Country: New Zealand. Sample number: 15. Age: ≥ 56 years. Gender: mixed. SES: Not stated Ethnicity: 14 New Zealand European, 1 Samoan. Occupation/employment: Not stated | |
| Details of exercise programme | Name of programme: Not stated Provider(s): Hydrotherapy services. Training: Not stated Setting: hydrotherapy pool. Content: hydrotherapy exercise programme. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, several attempts. | |
| Were the findings of the study grounded/supported by data? | Well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth, but little depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | Medium. | |
Moody 2010
| Methods | Sampling frame: from RCT (no other details reported). Data collection: focus groups. Data analysis: The General Inductive Approach. | |
| Stated aim of study | To investigate the effects of a 12‐week aqua‐aerobics programme on falls risk and physical function in older adults with lower extremity osteoarthritis in New Zealand. | |
| Details of participants | Country: New Zealand. Sample number: 17. Age: ≥ 65 years. Gender: 13 women. SES: not stated. Ethnicity: not stated Occupation/employment: not stated. | |
| Details of exercise programme | Provider(s): water exercise instructor. Training: yes. Setting: community; local municipal swimming pool. Content: group water‐based exercise programme that included warm‐up and warm‐down exercises and a series of progressively more challenging balance exercises. Length/intensity: twice weekly for 12 weeks. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, several steps were taken. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth but limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | Medium. | |
| Credibility of findings | High. | |
Morden 2011
| Methods | Sampling frame: from longitudinal survey of people aged > 50 years. Data collection: indepth interviews, semi‐structured interviews and diary. Data analysis: constant comparative/thematic analysis. | |
| Stated aim of study | To explore the ‘lay' model of self‐management for knee pain within a populace of people with knee pain who have not recently consulted with their GP for their condition. It can be argued that this allows specific exploration of how people manage without professional advice and support, and whether they distinguish between professional and lay approaches to self‐management. | |
| Details of participants | Country: UK. Sample number: 22. Age: > 50 years. Gender: 9 male, 13 female SES: not stated. Ethnicity: not stated. Occupation/employment: 2 professional; 3 unskilled; 15 retired/pensioner; 1 semi‐retired. | |
| Details of exercise programme | Not applicable. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, a fairly thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Petursdottir 2011
| Methods | Sampling frame: advertisements in clinics and newsletter. Data collection: indepth interviews. Data analysis: Phenomenological Analysis. | |
| Stated aim of study | To increase knowledge and understanding of the experience of exercising among people with OA and to determine what they perceive as facilitators and barriers to exercising. | |
| Details of participants | Country: Iceland. Sample number: 12. Age: ≥ 50 years. Gender: 44 men; 72 women. SES: not stated. Ethnicity: not stated. Occupation/employment: 6 retired/pensioner; 1 full‐time; 2 part‐time; 3 disability pension/allowance. | |
| Details of exercise programme | Not applicable | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, a fairly thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/Fair breadth, but limited depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Stone 2015
| Methods | Sampling frame: advertising through posters in physician's surgery, with snowball recruitment used to extend sample beyond initial volunteers. Data collection: demographic survey and semi‐structured individual interviews. Data analysis: interpretational analysis: coding, categorisation and forming themes based on verbal trends. | |
| Stated aim of study | To develop a broader understanding of patients' perspectives and experiences with physician‐recommended treatments and interventions for OA symptoms, with an emphasis on exploring facilitators and barriers toward regular physical activity participation. | |
| Details of participants | Country: Canada. Sample number: 15. Age: 30‐85 years (3 participants under 45 years, whose quotations are excluded). Gender: mixed. SES: Not stated Ethnicity: Not stated Occupation/employment: 3 retired, 12 working. | |
| Details of exercise programme | Study was an exploration of attitudes to exercise and physical activity, and details of exercise participated in are limited. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, several steps taken. | |
| Were steps taken to increase rigour in data collection? | Yes, fairly thorough attempt. | |
| Were steps taken to increase rigour in data analysis? | Yes, several attempts. | |
| Were the findings of the study grounded/supported by data? | Well grounded. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | A lot. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Thorstensson 2006
| Methods | Sampling frame: exercise intervention. Data collection: interviews. Data analysis: Phenomenological Analysis. | |
| Stated aim of study | To describe how middle‐aged people conceive exercise as a treatment for knee osteoarthritis. | |
| Details of participants | Country: Sweden. Sample number: 16. Age: ≥ 45 years. Gender: 10 male, 6 female SES: not stated. Ethnicity: not stated. Occupation/employment: not stated | |
| Details of exercise programme | Part of an intervention; details not provided. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, minimal few steps were taken. | |
| Were steps taken to increase rigour in data collection? | Yes, a fairly thorough attempt was made. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair breadth and depth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | High. | |
| Credibility of findings | High. | |
Veenhof 2006
| Methods | Sampling frame: from RCT investigating behavioural graded activity. Data collection: indepth interviews. Data analysis: grounded theory approach. | |
| Stated aim of study | To investigate which factors explain the difference, after a behavioural graded activity programme, between people who successfully integrate activities in their daily lives and those who do not succeed in integrating activities in their daily lives. | |
| Details of participants | Country: Netherlands. Sample number: 12. Age: ≥ 55 years. Gender: 4 male, 8 female SES: not stated. Ethnicity: not stated. Occupation/employment: Not stated | |
| Details of exercise programme | Provider(s): physiotherapists. Training: yes. Setting: primary care. Content: behavioural graded activity delivered individually according to strict protocols directed at increasing the level of activities in a time‐contingent way, with the goal being to integrate these activities into daily living; included written materials such as education messages, activity diaries, and performance charts. Length/intensity: maximum of 18 sessions delivered over a 12‐week period, followed by 5 preset booster sessions in week 18. | |
| Notes | ||
| Quality appraisal | ||
| Questions used to judge the dependability and credibility of studies | Review authors' judgements | |
| Were steps taken to increase rigour in sampling? | Yes, a (fairly) thorough attempt was made. | |
| Were steps taken to increase rigour in data collection? | Yes, several steps were taken. | |
| Were steps taken to increase rigour in data analysis? | Yes, a fairly thorough attempt was made. | |
| Were the findings of the study grounded/supported by data? | Fairly well grounded/supported. | |
| What was the breadth and depth of findings? | Good/fair depth but limited breadth. | |
| To what extent does the study privilege the perspectives and experiences of older people with osteoarthritis of the knee or hip? | Somewhat. | |
| Overall dependability and credibility of findings | Review authors' judgements | |
| Dependability of findings | Medium. | |
| Credibility of findings | High. | |
GP: general practitioner; OA: oestioarthritis; RCT: randomised controlled trial; SES: socioeconomic status.
Appendix 4. Themes: people's views of living with arthritis and exercise
Themes: people's views of living with arthritis and exercise
Symptoms
| Subtheme | Study | Direct participant data | Author description of data |
| Pain, muscle weakness, physical function | "It [severity of knee symptoms] got worse and worse and I started falling down." p.135. "I was having trouble with my knees every so often it did hurt you know with one thing and another." p.135. "Because when you've got knees like this, you like to do other things, you think I'm gonna go ‐ I'd like to get back to how I was before, but I don't think that's ever going to happen now." p.136. | None reported. | |
| "I can't walk as fast or as far as I used to because my knee hurts." p.560. "My knee is stiff, especially first thing in the morning or after resting." p.560. "Going downhill or downstairs is particularly painful." p.560. "It's absolute agony in spite of painkillers, so any activity is very limited." p.560. | None reported. | ||
| Pain described as: "a niggle", "not too bad", "murder" or "agony." p.3. "…Getting out of bed, getting going, turning over in bed, waking up in the night…getting in and out of the car is a nightmare…" p.5. "…I'm limited now, I can't go out as often as before, you know." p.5. "…It alters your life…it swings your life right round, it restricts you…" p.5. | Typically, people described episodic pain that increased gradually over several years. Pain varied greatly within and between participants, described variously. Often weight‐bearing activities brought on pain, but people with advanced disease also had pain while sitting or in bed. The unpredictability of pain bewildered people. p.3. | ||
| "I mean, I now work at (Supermarket X) shelf filling and I've actually bought a set of knee‐pads. The tilers use them. Yeah, I put them on, it's a source of amusement for most other people, but they are not 'with it' ‐ the kneeling on a cold floor, for eight hours a day. Young people don't realise what they're doing to their knees. I tried it for the first week and I couldn't walk. I've got my kneepads, now. I can do the job with no problem at all, no problem at all. My knees are as good as they were before I went to (Supermarket X)" p.194. | Frequently participants discussed how they make adaptations and adjust routines to enable them to continue in their daily tasks in the face of painful symptoms. This could include bursts of activity followed by rest and using heat rubs, making adaptations to the household such as rearranging the order of kitchen shelving or altering walking routes to avoid hills if they found them problematic. For example, Michael had experienced knee pain for several years. He was a keen keep fit fanatic and engaged in regular exercise. The pain from his knee caused him difficulties when bending and also prevented him from placing his knee on hard surfaces for too long. Michael works as a manual labourer for a large supermarket chain. In his account, he discussed the importance of having to work to help keep the family home, arguably part of a moral need to maintain a sense of competency in his social role which, in turn, was related to his sense of self. He outlined a particular self‐initiated strategy that helped to maintain his role as a contributor to the family home. Michael discovered this particular strategy after going on a tiling course when he was unemployed. This particular knowledge helped him to plan and ensure his knee pain was manageable while working. pp.193‐4. | ||
| "It was like my body was made of lead." p.1020. | A few of the women mentioned "paralyzing fatigue" as a major barrier for getting anything done and felt it might be related more to mental fatigue than to physical fatigue. | ||
| "I'm always in pain and agony, every movement "I can't bend down. I can't get on the floor, if I do, it is a chore for me to get up. Bending my knees hurts all the time. Walking now seems to be hurting me as "If someone called to play ball or something I would say, "I'm busy, I can't, and pretty soon I realized that I couldn't do it, not that I didn't want to, I just couldn't anymore. It wasn't worth the pain." p.9. | Multiple participants expressed being in a constant state of pain, in which any movement, let alone "stressful" exercise, was overwhelming. This statement exemplifies the difficulties many participants expressed when attempting to accomplish functional tasks, such as ascending and descending staircases. Other functional difficulties included pain during walking, showering and bending. These activities of daily living were frequently described as "chores." p.8. In addition to these limitations, participants spoke of fatiguing rapidly, which made considering physical activity as more of a challenge. Some participants elaborated on this "fatigue," explaining how OA pain caused them to feel "broken" or "100 years old," and often motivated them in avoiding social interactions that involved some sort of physical activity. p.9. |
| Subtheme | Study | Direct participant data | Author description of data |
| Capacity to exercise | "When I did the exercises in the beginning, it wasn't painful with the tape on, so I think that was how I was able to get on with them so well…whereas if the tape came off and I didn't put it on it was more painful." p.135. "I see people come in with arthritis and I think oh…god they are in terrible trouble and absolute agony and I think well I've got nothing to complain about." p.135. | The perceived severity of knee symptoms was an important factor in motivation, with those experiencing severe pain or loss of mobility (or both) being most likely to continue to exercise. p.135. The existence of other comorbidities, comparison with other people with more limiting disease or a stoic attitude to knee symptoms all seemed to be associated with an attenuation of the motivation to comply. p.135. | |
| "Anything that would jog or jar my knee would really hurt." p.560. "I can't swim anymore because breaststroke is bad for my knee." p.560. "It's hard to get going on a bike and very painful." p.560. "I've reached an age where exercise doesn't help, I just get tired." p.560 "I'm not fit and agile enough to do exercises." p.560. | Participants' ability to exercise was limited by the pain and stiffness in their knees, which restricted the type and amount of exercise that was possible. Ability was also limited by a perceived general lack of physical fitness, sometimes attributed to old age, as well as comorbidity including angina, lymphoedema, congenitally malformed hip and osteoporosis. p.560. | ||
| "…Well there's hardly a good day you know. I mean I just make the best of it. I don't try to you know, let it get me down. Although I have pain, I'll try and do what I can do you know rather than to just say' I am in pain I can't do that'…" p.5. "…I'm good at going up stairs, it's the coming down I have difficulty with." p.5. "…It's very tiring walking round shops…Some days I just sit here most of the time because it's too painful to move…" p.5. "…my daughter has to be with me to have a bath…I can't move, I can't push my legs down from my knees, they won't function…I can't do shopping…my daughter does it all, yeah. You know, I mean she's ever so good to me…She does things, she does this of a morning before she goes to work…" p.5. "…I don't have a bath. I can't get up and down…I stand in the bath and wash down." p.5. | Pain, muscle weakness and fatigue after common activities of daily living impaired people's physical functioning and mobility. They stoically tried to carry out their normal activities, but often had to adjust or avoid activities (e.g. showering instead of bathing) to cope with their limitations and maximise their independence, and depended on family and friends for help with essential domestic and social activities (e.g. shopping, housework, gardening, transport, bathing). | ||
| "Umm, I suppose the things that sort of do prevent you are if you get ill. One thing, that's probably the only thing would be if I got ill…I probably wouldn't be able to go, but only that would keep me away." p.67. "Well for me, at first that's why I missed some of them. I couldn't go more than one because I was just so tired the next day and would sleep so sound, you know at the night‐time, that I couldn't always wake up early enough to get myself organized to get the bus." p.67. | 1 barrier to ongoing participation was that of illness. For some participants, fatigue was an issue. | ||
| "The effort to get clean afterward is really hard…You just don't have the energy to take a shower." p.1020. | Pain was a crucial issue in the interviews, being a barrier in itself, but the hope of decreasing the pain by exercising turned out to be a major facilitator to encourage regular exercise. The participants described the difficulty of having to constantly adapt their exercise pattern to pain that could vary from day to day and even be too intense to be able to exercise at all. p.1020. 1 woman expressed her deep concern regarding how pain and fatigue led to difficulties with personal hygiene. She believed that people with chronic pain hesitate to exercise because they do not feel up to taking a shower afterward. p.1020. | ||
| "You need to have the will to do it…when you are well you don't do it, and when you need to do it, then it hurts and therefore you don't do it (laughter)." p.55. "And even if it hurts a bit, one should not give in but of course sometimes you can feel sore or aching joints afterwards, if it hurts when doing certain movements…of course it hurts, even when exercising." p.55. | ‐ |
| Subtheme | Study | Direct participant data | Author description of data |
| Impact of exercise on the effects of OA | "Since I started strengthening these muscles it seems I don't fall over so much which is good…" p.135. "I still do [the exercises] and I remember to stand the correct way without even thinking about it now…[The pain] has been a lot better, much better, and I can do things better. Dressing ‐ I don't have to hold on to anything, I can balance now and in fact, you know, I find it a great improvement." p.136. "I was able to do [the exercises] pretty easily but it didn't appear to me to make a lot of difference…I carried them on during the time I was taking part in the programme although I've dropped them since." p.136. | High levels of continued compliance were closely related to the perception that the physiotherapy intervention was effective. Those who noticed an improvement in their knee symptoms were much more likely to comply than those who did not. However, if the benefits of the physiotherapy were not perceived as sufficient, or there was an allergic reaction to the tape, non‐compliance was a rational outcome. p.136. | |
| "Exercise is the best thing for relieving the pain." p.561. "Exercise doesn't help pain but it gets it going, improves stiffness and mobility." p.561. "Exercise doesn't help my knees at all." p.561. | Some people found that exercise was helpful for relieving pain; other people found that pain persisted, but stiffness and mobility improved; other people found no improvement in knee symptoms. p.560. | ||
| "The pain is different pain and I feel that I can do things easier now than I could a while back." p.486. | None reported. | ||
| "…the exercises we did at (centre) were helping. and see I haven't had the pain…it was very helpful." p.7 "…I felt generally strong, you know. Walking up stairs, I mean, at times I used to have to go up one step at a time, but then after the exercise I could just walk up the stairs and I was even beginning to try to walk normal…" p.7. "…I was disappointed, because I hoped, I just hoped…but it didn't sort of do what I wanted it to do for my knees and I don't think anything will…I think your age, as you get older, you know, you get a bit dodgy." p.7. "…If I can get myself back to a little bit of [line dancing] then I kind of umm, my life is kind of coming back to normality, you know, cause it can take over your life a bit as I say, you are scared of what to do and what not to do…" p.7. | Most participants found the programme "interesting" and "informative," bringing "small" to "life‐changing" improvements in pain and function (i.e. walking, domestic and social activities, getting on and off buses, driving). They felt less tired and had a general sense of better physical well‐being. p.6. The physical and psychological improvements returned a degree of normality to people's lives. Some returned to previous activities they had begun to avoid for fear of harm, or take up activities to increase their level of physical activity. p.6. 2 participants were "disappointed" in the programme, experiencing little or no benefit from. This may have been a factor in the participants who withdrew from the study. The small number of people who found the programme ineffective makes it difficult to explore the reasons for ineffectiveness, but the 2 participants believed themselves too old or their symptoms too severe to enable them to benefit from exercise, and were sceptical and pessimistic about all interventions. p.6. | ||
| "It's just a relief to get into the water to get out of pain." p.91. "It takes your mind off, my pain. It's there all the time but when I get into the water, it lifts away from me." p.91. | Pain relief was described as a benefit from hydrotherapy and was ascribed to warmth and buoyancy…Not only did the pain itself ease, but hydrotherapy helped participants shift the focus from the constant pain that they were experiencing. p.91. | ||
| None reported | Participants described the perceived health benefits they received from attending the programme, such as an increase in movement or mobility, an improvement in breathing, a decrease in their pain levels, balance had improved and a reduction in falls. p.66. | ||
| "Exercising has a good effect on everything, including the heart." p.1020 | Many benefits of exercising concerning the OA symptoms were mentioned. Other general effects were also mentioned, such as increased fitness and a better heart condition. p.1020. | ||
| "Sometimes, after a long day, I'll throw some ice on my knees, take a hot bath after. It feels great…Using the heat was my favorite part of my physiotherapy…That is probably the only way I could handle exercising." p.14. "The physiotherapist professionally guided me to feel less pain. It made me want to do exercises on my own." p.14. | Pain relief. When participants were able to moderate their pain effectively, they were motivated toward contemplating physical activity adoption. Participants commonly found heat and hydrotherapy helpful for pain management. p.14. Participants also noted that positive experiences with physiotherapy inspired them toward physical activity. | ||
| "…exercise hurts. The pain was almost unbearable but I still carried on. Yes, it was very strenuous, but that's how it is, the pain becomes increasingly worse, I think…it just becomes more and more painful." p.55. "…for example, walking longer distances, there are limits, but nevertheless longer walks without experiencing pain. It is a huge difference. So it was very positive…it makes it possible to work more and you can do more enjoyable things too…Go fishing and hunting, walking the dog. All those things, like simply going for a walk." p.55. "…when I have been walking for a while, the pain goes away, which makes me happy." p.55. "…exercise can help, I am convinced about that, although it did not work for me…the damage was too great when I started. It had gone too far. If one had started to exercise five or six years earlier, it might have helped." "In my case…the damage became worse, it only led to more pain instead of improvement." p.56. "it [the exercise] was beneficial and it helped in the short term. However, had I not received injections I would never have been able to work for so long. It is thanks to them that I have been able to work for the past five or six years or since I got osteoarthritis. That is a fact." p.56. | To experience symptom relief. This conception contained experiences of the effects of exercise on pain and other symptoms. Statements ranged from total pain relief to a worsening of symptoms. p.55. To deprecate; the belief that exercise could cause harm or be unnecessary in that the informants considered other treatments to be more effective. p.56. | ||
| "I continue with my exercises, they are integrated in my daily living. I really know these exercises have beneficial effects and that motivates me to continue with my exercises. The main motivation to do all this is to prevent an operation to get a new hip." p.275. "Although I experience the same level of pain, I have learned to continue with my activities and I realise that I achieve more because of that." p.275. | First, the initial motivation of the participants played an important role. Some participants were motivated to reach short‐term goals, e.g. to decrease pain, while other people were motivated to reach long‐term goals, e.g. to postpone an operation or to live independently for as long as possible. It appeared that all adherent participants were initially motivated to reach long‐term goals, while all non‐adherent participants reported a short‐term initial goal or had no specific goal. These participants tended to stop performing their activities as soon as the short‐term goal was obtained. Therefore, there seems to be a relationship between the initial motivation in visiting a physiotherapist and exercise adherence. p.275. |
Health beliefs and views on the management of OA
| Subtheme | Study | Direct participant data | Author description of data |
| Aetiology and prognosis of OA | "I was having trouble with my knees every so often it did hurt you know with one thing and another. Working in the construction industry there is a lot of lifting and a lot kneeling you see and I felt well I wonder if that's got anything to do with it…" p.135. | ‐ | |
| "It's caused by heavy work, always being on your feet or doing a lot of sport when young." p.56. "Being overweight has made my knee problem worse." p.56. "It's a vicious circle; you put on weight because you don't want to exercise when your knees hurt and then they hurt more because of the extra weight." p.56. | Some believed that their joint problems were a direct result of excessive sport or heavy manual work when younger. p.561. | ||
| "I think it's just wear and tear. I think it's just accepted that you're going to get these things as you get older." p.5. "…I was very athletic when I was young, and you know yourself with the athletes the injuries they get affects them later in life." p.5. "…My daughters have trouble with their knee now as well, don't know if it's inheritance…my granddad suffered with it, my mother's troubled with it." p.5. "…Well as I say, I need to lose weight…Well I mean there must be a lot of pressure on my knees as well, because I am overweight." p.5 "…I hope not permanent." p.5. "…I think probably it might get worse because it has been getting worse over the years." p.5. "…I think, having to sit in one of those [wheelchairs]…I wouldn't want to do it, I don't want to get to that stage…" p.5. "…nothing will stop it getting worse I'm sure…if you have a replacement thing well alright that'll be alright but I mean otherwise they [his knees] just go on getting older…" p.5. | People were uncertain and bewildered about how, why and when their knee pain started. Most attributed knee pain to mechanical "wear and tear" of occupational, sporting and leisure physical activities, which led them to believe knee pain was an inevitable consequence of normal ageing. Some people tried to identify a specific incident as the start of their pain, but their recollection of the incident was often vague and they struggled to convince even themselves that this was the start of their problems. Frequently a familial predisposition for joint pain was mentioned with reference to a close relative, often female, who had "arthritis" or "rheumatism." p.3. People hoped rather than believed their symptoms would improve. They reasoned that joint damage was irreversible and likely to deteriorate without surgical correction. These beliefs arose from people linking the cause of joint pain to their biography, and the influence of other people's experiences and beliefs. p.6. | ||
| None reported. | A large number of participants described their knee pain as something unremarkable or related to ageing. p.193. |
| Subtheme | Study | Direct participant data | Author description of data |
| Non‐exercise management strategies | "I am not a one for taking a lot of tablets. I get a bit dubious, you know, so I just learnt to live with it for a bit and then I had the chance of [the trial]." p.134. "I'm a great believer in physiotherapy anyway I think. I don't agree with drugs quite as much as, I think, if you can have it naturally." p.134. | A dislike of taking prescription drugs and a positive view or experience of physiotherapy also provided an initial motivation to comply. p.134. | |
| "I'm not keen to take things because they're not going to cure it, and I mean to hide it is not strictly a good idea because you do things and it makes it worse." p.561. | Analgesics were used warily, as there was concern that they might disguise the warning function of pain. p.561. | ||
| "…I don't want too many tablets in me…I can try and bear pain myself." p.5. "…I do really try to keep off drugs because, you know, I mean I think that they all have side effects." p.5. "I'm waiting for a knee replacement, cos I find it very difficult to get around, you know…I'm hoping the operation will correct it." p.5. "…I'd have to be a lot worse than what I am now I think…well I mean if I've gone for thirty years I can go on for a few more." p.5 (about surgery). "…I don't want knee surgery, I've seen it happen; I've seen people have it very successfully and I've seen it be a disaster." p.5. | People used analgesia reluctantly, usually when pain was severe or before/after activities that exacerbated pain (e.g. shopping, gardening). They were concerned about adverse effects, becoming addicted and worried that taking it regularly would reduce its effectiveness. People taking medication for common comorbidities (e.g. diabetes, cardiovascular, respiratory disease) wanted to limit the medications they were taking, preferring to omit analgesia and cope with pain rather than omit medication for comorbidities seen as more serious, over which they had little control. pp.3‐4. People reasoned that while medication might alleviate symptoms, surgery was the only way to correct structural joint damage, eliminate pain and restore mobility, function and independence, but they wanted to delay surgery as long as possible. Other people were more sceptical and frightened of surgery. Whether people held positive or negative expectations of surgery was strongly influenced by the experiences of family, friends, media reports or presence of comorbidities that contraindicated surgery. p.4. Awareness of treatment options other than medication and surgery was poor. Many people were using alternative remedies (e.g. fish oils, glucosamine, herbal remedies, acupuncture, osteopathy, copper bracelets, etc.) on the recommendation of family, friends, media reports and advertisements. Some people found these helpful, other people were sceptical but often continued to use them in the hope they would prevent or delay progression." p.5. |
| Subtheme | Study | Direct participant data | Author description of data |
| Advice and information from health professionals | "So I go to the doctor and all he just simply done was put his hand on my knee, he said "move your leg…you are getting old you've got rheumatism." You see that was it I didn't take any more notice of it [the knee pain]." p.135. "She [the physiotherapist] said the kneecap is out, so she taped it up and pushed it back…So now if it starts aching, that's what I do. I tape it up and push it back to where it should be." p.136. | As the model described in fig 1 of Campbell 2001 suggests, these ideas (about exercise interventions) were sometimes shaped by people's previous experiences of health care. p.135. | |
| "My doctor told me to keep exercising and not to stop." p.561. "…they [hospital doctors] said, 'the walking's agitating you, your joints, so stop it'." "The physiotherapist told me to exercise." p.561. "My doctor showed me how to do quads exercises to strengthen the muscles." "My doctor gave me a referral to the gym." p.561. "I was given advice about exercise at the gym." p.561. "At the hospital they told me I shouldn't overdo exercise, I should look after my knees." p.561. "He told me to take painkillers and keep my knees moving but he didn't advise any particular kind of exercise." p.561. "I haven't had any advice about exercising and what exercises to do." p.561. "Doctors could give you more encouragement to exercise; I had to get the referral form from the gym myself and ask him to sign it." p.561. "I think they would have told me in the clinic if I should be exercising and what exercises to do." p.561. This could be more relevant in/similar to 'influence of program supervisors in terms of individual instruction and the 'knowledge' is a secondary part of this; currently quoted in text for this themes: "…I had to stick rigidly to what he had said, the weights that he had specified…the idea was to stretch it that little bit further than I normally would do in order to support the joint more…but too much would…cause more damage and not enough wouldn't do any good…I was quite impressed actually by his knowledge…and I did exactly what he said and I did notice an improvement, a definite improvement." p.563. | Advice from health professionals was mainly in favour of exercise and consisted of encouragement to exercise, advice about specific exercises and referral to a gym. Sometimes the advice was vague or absent. p.561. Occasionally exercise was discouraged. p.561. The expert advice and supervision available in gyms or from physiotherapists was valued. p.563. | ||
| "I was a bit sceptical at first and when the exercises came I thought 'hang on, this has got nothing to do with the knee as far as I understand' being ignorant, you know. Now I sort of feel that 'hang on, yeah there is a difference' because the work has paid off." p.486. | All 3 groups of participants referred to the importance of giving and receiving information. p.483. | ||
| "…[participants GP] never said anything, that's why I have always thought it's not worth bothering about. He's not bothered so I am not bothered…" p.5. "…I learned so much from [the physiotherapist]…I learnt about pain management…" p.7. "…It helped me understand arthritis much better…" p.7. "…I class it as spring cleaning my mind…" p.7. "…[helped understand] how to cope with pain…that exercise does help ease the pain and helps your mobility…" p.7. | Our inclusion criteria meant all participants had consulted their GP about knee pain. People were often told the problem was due to wear and tear and getting old. Few could remember receiving information or advice, and they perceived knee pain was considered a benign condition that did not have a high priority, which confirmed their own beliefs and attitudes. No‐one had been offered a self‐management programme. Management was seen as ineffectual, and consequently few were regularly consulting their GP despite ongoing problems. p.3. Management usually involved people being offered palliative medication. p.3. Receiving information and practical advice about what (not) to do, and the opportunity to discuss things that concerned and confused them with a healthcare professional, helped people appreciate their problems and what they could do to address these. In particular, they learned about the role of inactivity and excess bodyweight in development of knee pain, and how exercise and losing weight could control symptoms. p.8. | ||
| "He encourages me in every way." p.1021. "They have not done it [encouraged exercising]." p.1021. "They [the physicians] are positive if you ask [for a referral to a physical therapist], but you have to ask." p.1021. "Now I think I handle it more wisely. I know better because I've been fortunate to get good instruction." p.1021. "There are many 60 year‐olds who don't use computers to get information. And these are the people with arthritis! I think it is much easier to get information to the younger people. We use the Internet." p.1020. | The encouragement of physicians to exercise was very important to some of the participants. However, this encouragement (i.e. whether physicians emphasised exercise) varied. Whether physicians referred their patients to physical therapists also varied. p.1021. Participants' knowledge of both general health and OA was of high importance. Most of the participants had experienced being educated by their physical therapists. Some participants wondered how to get such information to the public. p.1020. | ||
| "My doctor told me to go on a [recumbent] bicycle for 20 minutes a day, or "I was never prescribed exercise. My family doctor and rheumatologist have "When I was first diagnosed, I didn't know what to think. I knew it wasn't good, but I didn't know how bad it was going to be. After a couple of years, the pain was too much to bear and I thought, that's it…my life is over. And no one warned me…I didn't even know what to do…exercise was the farthest thing Many participants echoed, "If my doctor tells me to [exercise], then 1 participant noted, "If [my doctor] told me what to do and how to do it, | Participants were knowledgeable of the benefits that physical activity can have for the general population; however, many were unaware of specific OA‐related benefits and unsure of what activities would provide optimal self‐management. Furthermore, participants noted that physicians often provided them with counteradvice or did not offer any recommendations. This created further confusion about physical activity and the potential benefits for OA. p.12. Much like the quotations above, many participants held the perspective of being inadequately educated about exercise by their healthcare providers, and rarely having an open dialogue regarding prescribing exercise or physiotherapies (or both). This lack of communication regarding exercise and physical activity was compounded with a participant perspective of having inadequate knowledge/communication regarding their OA diagnosis in general. All participants spoke about the instrumental role of healthcare providers in influencing and encouraging physical activity. Participants expressed that if their physician advocated exercise, they would be eager to adopt it. p.14. In addition, participants desired more knowledge and specific guidance related to physical activity. p.14. |
| Subtheme | Study | Direct participant data | Author description of data |
| Health beliefs and managing OA and exercise | "[the exercise and taping]might not help me because I'm getting old but it might help somebody else…I just think I'm too old really to improve." p.136. | Ideas about the cause of arthritis also played a part. Those who thought that arthritis was caused by immutable factors such as age, obesity and "wear and tear," tended to have a resigned attitude towards their arthritis. As a consequence, they found it hard to believe that the intervention could be effective and this weakened the resolve to comply. In contrast, those most likely to be continued compliers tended to believe that although there was no cure for arthritis, there were things they could do to minimise its impact, including the physiotherapy. p.136. | |
| "If it's wear and tear on the bone, is it helping to do all this exercising, walking and that?" p.561. "So your movement is important; this is why I want to get back into a regular exercise routine, so I can do more to help myself." p.562. "You should do moderate exercise; overdoing it could make things worse." p.562. You can't do too much exercise; take painkillers, if you need to, and keep going. | Many participants were worried that exercise was wearing out their joints. They reasoned that if OA is caused by wear and tear, then exercise would exacerbate the disease process. p.561. Some participants were determined to take control of their disability and used exercise as a means of actively maintaining or improving their mobility. In some cases, this determination was such that they continued to exercise in spite of a belief that OA was caused by 'wear and tear.' p.562. 1 participant felt that it was impossible to do too much exercise, but people felt that excessive exercise would make the knee problem worse. However, other people had become resigned to their physical limitations. p.563. | ||
| "I know now it's going to be for my benefit. I keep on doing these exercises…if I stop, pain comes on again, and I can't do any activities." p.485. | No direct description. | ||
| (Before intervention): "…I get the pain and there is nothing that can be done about it…" p.5. "…I'm questioning whether exercise might exacerbate or ease it. I really don't know." p.5. "…I got a little bit frightened of doing exercise because I don't know what exercises will be detrimental to the knee or advantageous to it." p.5. (After intervention): "…I thought if I exercise I am going to make the pain worse…they have showed me that I can still exercise even though I have a bad knee…" p.7. "…I feel that I am not thinking about my knee pain anymore as a pain, I think about it more as preventing it by doing the exercises." p.7. "…[arthritis]can ease…but there is no cure for it, so it's learning to live with it…" p.7. "…I'll go on as much as I can doing the exercises…" p.7. "…I thought it was good, very good. To my mind I was helping to do something to help my knee pain…" "…This [exercise] is much better because like I said I found is helpful, because I don't take any medicine…" "…If you don't exercise you're never going to be able to manage the pain…Gentle exercise actually relieves the pain, and it means that you should be able to cut down [analgesia] and that the answer is not necessarily knee replacement…" p.7. "…I mean exercise might stop it from getting worse any sooner that it would have done…before it deteriorates to the point where an operation might be needed…" p.7. | As a result of this confusion, and in the absence of any advice about what they should (not) be doing, few people were exercising and most were refraining from or avoiding activities. p.5. Participation in the exercise regimen allayed people's fears, confusion and anxiety about the safety of exercise and showed them it was beneficial. Its successful completion convinced participants that exercise was an effective self‐management strategy they were capable of implementing and a viable alternative to medication that might slow deterioration and delay or avoid surgery. p.8. | ||
| "There is nothing that can be done about the OA; therefore, I do nothing." p.1021. | Only 1 woman did not exercise. She worked part‐time and believed that was quite enough activity. p.1021. | ||
| "Well, I am worried, I sometimes think that if it hurts when I do something it will cause even more damage." p.56. "…I now know that it is beneficial. I know that simply going for a walk every day is very good for me. In that way I have changed. Previously I was not even aware that it was necessary." p.53. "It can't have improved just like that. It [exercise] must have helped. So that's why I've found it beneficial in all sorts of ways, and it has changed my attitude to this kind of exercise. It must have done it." p.53. "Well, it is different now because, as I've already said, previously you exercised to maintain your level of fitness whereas now you exercise in order to regain your physical condition." p.55. | To hesitate. This conception contained doubts about the benefits of exercise. Experiencing pain while exercising made it difficult to decide whether it was beneficial or counterproductive. p.53. To experience coherence. This conception contained statements about connecting knowledge about OA with knowledge and experiences of exercise. The informants expressed satisfaction and were convinced of the effectiveness of exercise. p.56. |
| Subtheme | Study | Direct participant data | Author description of data |
| Everyday activities versus structured exercise programs | "Day‐to‐day activity isn't enough to keep you mobile." p.562. "There's a basic level of exercise that I have to do to keep the joints flexible, so I can get up and move around." p.562. "I get enough exercise leading an active life." p.562. | There was a broad range of opinion as to the appropriate level of exercise. Some people felt that keeping active was sufficient; other people that this was insufficient. p.563. | |
| "Exercise in water, it's not like walking or running…you're not jarring any limbs or bones…And for old people I'm, I'm not sure (land‐based exercise) is the best sort of exercise that you could do." (p.66). | Participants were of the opinion that exercise in water was superior to other forms of exercise for them. They talked of other types of exercise they had tried and how land‐based exercise caused pain whereas water‐based exercise did not. p.66. | ||
| "And I think that it is important when people choose which exercises to do, that you enjoy it, that you feel it is rewarding…these positive factors have to be present." p.1020. | The participants described the importance of suitable exercise…the importance of finding an enjoyable training mode. p.1020. | ||
| "I really don't think that I need to take some exercise but I just tell myself that I am going shopping and things like that." p.55. "I try to walk more and more, to walk in the correct way and to climb stairs in the correct way and not to wear myself out." p.54. "Well, with respect to time, I try to be out for at least half an hour and then I try to go for a longer walk at the weekend, perhaps for up to an hour." p.55. | The informants described their need to exercise. The statements ranged from conceptions about the importance of exercise in order to maintain physical functioning, to the fact that daily living demands movement. p.55. |
Psychological
| Subtheme | Study | Direct participant data | Author description of data |
| Impact of OA on people's sense of "self" | "…[inability to do gardening] makes me mad at times, cos I feel frustrated about it. I know there's masses of things that want to be done out there, I just haven't got the energy to do them…It makes you feel older." p.5 "…I'm very upset with myself cos, you know, when you're used to being mobile and able to do things for yourself, now you have to depend on people to do it, it's not very nice is it?…It's embarrassing. Like [at a dinner and dance] I sat down and had the dinner, and when I was to get up I couldn't move. I was so embarrassed and people looking at me." p.5. | Limitations in functioning and the need for help made people feel frustrated, angry, depressed, embarrassed, incapacitated and a burden to other people, and increased worries that the ultimate outcome would be severe disability, immobility and dependency. p.3. | |
| "Today I am very tired and in quite a lot of pain, I went fishing with my grandson for the full day yesterday. Even though I enjoy the sport and have warm gear and wet gear, it still knocks me about. With having back pain and knee pain anyway, I can't stand for long. I was given a folding chair for Christmas, and very useful it turned out to be. With being able to adjust the chair to several positions and also the height I can usually find a position that suits me. One of the problems about not being able to walk very far is that if we want to go somewhere that we haven't been before we have to do lots of research into the place. We have to check to see if the terrain is reasonably flat, and if not, how far I will have to walk." p.194. | In James' account, his biography became disrupted due to a combination of back and knee pain. As a result, his physical capacity to work declined forcing him to retire early. His sense of self as male provider and head of the family was challenged. His account highlights the process of changing his role and renegotiating his sense of self as a family man. By taking on more of a carer role in the sense of looking after grandchildren and doing more work around the house, he was able to engage in what Gareth Williams calls 'narrative reconstruction.' As part of this process, James is constantly engaged in activities, strategies and treatments to enable him to carry on in a social role within the context of family life that was important to him. James' position as a 'good grandparent' sees him constantly negotiating ways to maintain physical and psychological well‐being. Spending time with his grandson both aided and threatened. For example, by taking regular shared fishing trips, he not only gained pleasure and psychological well‐being, but also incurred pain and suffering. Embedded in James' account are a number of strategies that he has to utilise to ensure continuity that he can continue valued activities: James, Diary 2 entry 18th January 2009. Here, we can see how James negotiates the negative part of 'being a good grandparent' (pain) to maintain a valued identity. This requires the application of aids (chair) and planning (research into place) p.193. A broader perspective of self‐management is witnessed in the accounts. Examining how people maintain acceptable social roles, remain competent moral actors and preserve a sense of self is central to understanding self‐managing in chronic illness. Taking such an approach acknowledges the essential part that making adaptations in daily life plays, so that people are able to continue valued activities, fulfil obligations and roles. p.194. | ||
| "I was extremely unhappy with myself…I couldn't work as hard as before, and I just could not understand why. It was one of the hardest things, to accept myself as what I had become." "Well, you have to face the fact that you are not young anymore, and you just have to slow down." p.1019. "I worked out new ways to cope, to keep my arthritis from getting in the way too much." "I think that general positivism is part of your health; if you think constantly about pain and aches, then you get really sick." p.1018. | Many of the participants described how they had to fit their OA into their self‐image and adapt their lives to it. Some of the younger participants seemed frustrated. The older participants expressed greater acceptance. The personality traits of adaptability and initiative had a strong influence on the exercise behaviour of the participants. They described the importance of not letting the OA control their lives, although its existence should be recognised and respected. Many participants talked about the importance of mental health and the importance of being positive, cheerful and not lingering on negative circumstances. | ||
| It definitely wears on you, on your mind because it stops you from doing what you want to do. Even if my body wanted to [exercise], my mind won't let me…I feel helpless and worthless." p.5. | Participants expressed depressing thoughts, referring to OA as "mentally agonising." Many participants felt betrayed by their bodies and felt helpless regarding their functional limitations. 1 participant specifically mentioned, "Mentally, it's so depressing. I can't tell you how I just want to sit down and cry sometimes because I can't move." p.13. Other participants echoed this "helplessness," noting the effects of OA‐related psychological |
| Subtheme | Study | Direct participant data | Author description of data |
| Self‐efficacy | "I worked out new ways to cope, to keep my arthritis from getting in the way too much." p.1018. | The personality traits of adaptability and initiative had a strong influence on the exercise behaviour of the participants. They described the importance of not letting the OA control their lives, although its existence should be recognized and respected. p.1018. | |
| "Not only does it hurt when you [move], but it would hurt the next day. The pain | Low exercise self‐efficacy was consistently mentioned by other participants. Low levels of self‐efficacy demotivated participants from physical activity as they did not believe they could successfully perform a task without exacerbating their current pain levels. In addition to fear of pain on a daily basis (pre‐exercise) and fear of exacerbating pain during exercise, participants also expressed fear of experiencing pain after exercise of which they were determined to avoid. This fear avoidance of physical pain seemed to provide participants with a "logical" rationale for avoiding activity. p.9. |
| Subtheme | Study | Direct participant data | Author description of data |
| Psychological benefits of exercise | "Strengthening your muscles…keeping your weight down…keeps you in shape." | ‐ | |
| "You just feel great when you've done it…you know, they say exercise releases happy something in your brain and it certainly does…" p.560. "You feel great when you exercise, it gives you a buzz." p.561. "Exercise is part of a healthy lifestyle, it improves fitness and I feel better for it." p.561. | Some commented on an improvement in general well‐being. p.560. | ||
| "…Overall I have improved…. it's a feeling of general well being really…I feel a lot better in myself, I mean mentally, mostly mentally…" p.7. "…If I can get myself back to a little bit of [line dancing] then I kind of umm, my life is kind of coming back to normality, you know, cause it can take over your life a bit as I say, you are scared of what to do and what not to do…" p.7. "…I didn't do no exercise, I didn't know I should do, I was frightened…but since I knew of the exercise, I have been doing it…" p.7. "…you are all in there with similar problems, and it's the friendliness, like on a, personal level." p.7. "…we formed very tightly knit group…we were all trying to help one another, you know." p.7. | The programme reduced anxiety and fear of activities people previously thought might increase pain, increased confidence in their ability to exercise safely and effectively, and generated a sense of self‐achievement. p.6. The physical and psychological improvements returned a degree of normality to people's lives. Some returned to previous activities they had begun to avoid for fear of harm, or take up activities to increase their level of physical activity. p.6. Participants who received group‐rehabilitation thought meeting, sharing experiences and the support derived from fellow group members was beneficial, and that observing improvements in other people was a source of encouragement. p.8. | ||
| "It's been an awful shock to get sick…It's been really really difficult, so coming and talking to other people, probably has been almost as beneficial as doing the exercise and realising that you're not the only one." p.91. | Participants described psychological benefits from going to hydrotherapy…sharing and comparing their health condition with people who also had OA was also identified as beneficial. The sessions helped participants gain a better perspective on their condition, through comparing to other people and talking with other people in similar situations. p. 91. | ||
| "So, you tended to be concentrating more on the dogs than on what you were doing. So you then noticed that you've been walking and you were getting more comfortable purely because your mind was distracted from the circumstances of the pain in the knee and the hip. So that was what we used the dogs for, but that was an incidental. It just happened that it was when you took the dogs out, you were distracted from the pain. So, you got your Physio." pp.194‐195. "I think swimming is one of the best exercises that you can get and I do feel when I've been swimming, that it does me good. Plus, I just love it. I enjoy it. It's a social thing as well and I just get so much out of it. I pay a fee at the gym and I only swim; I don't do anything else but I just love the place I go to. It's only just over the way and I just go every Monday, Wednesday and Friday morning so it's not just the exercise. The exercise is very important to me but it's everything that goes along with it. I've made new friends since I retired and I just find that completely satisfying; I enjoy it and I don't want to give that up." p. 195. | One participant outlined the unintended beneficial consequence of walking his dogs, in particular, the fact that this was not just physical ('you got your physio') but also psychological in terms of distracting his thoughts away from pain. p.195. Another participant recognised the psychological, social and physical benefits of exercise and the combination of these factors provide the motivation to continue. p.195. Participants had some worries about the potential for damaging the joint, but their main concern was maintaining their social contacts, preferred leisure activities or sense of self as a 'fit and active' person. p.195. | ||
| "the social side of things is really, really good." p.66. "all in the same boat." p.66. "…sometimes being actually on your own to be motivated uh it's harder. It's harder: A lot harder." p.66. | Participants spoke of the good social atmosphere of camaraderie created by the group and the instructor and the friendships that were forged. Exercising with other people made it more fun and enjoyable and participants found they helped one another. As they were "all in the same boat" they felt more comfortable and could empathisse with and relate to each other. Many people stated they would not have gone to water‐based exercise or similar exercise on their own. Some participants expressed frustration that they could not motivate themselves to go alone, but that there was no problem with motivation if they went with the group. Being part of a group contributed to motivation both for getting to the classes and also once they were there. p.66. | ||
| "I am more vivacious, both physically and mentally." | Most of the participants agreed that physical exercise improved their mental well‐being. | ||
| "…it has a beneficial effect on the whole body. It gives you a sense of well‐being, not just because you have done it and feel good about it, but your muscles feel as if they have benefited too." p.53. "…yes, I definitely feel better, apart from my knees that is…I'm more alert…. Perhaps not immediately afterwards but I feel more alert after a shower." | To experience well‐being. In this conception, the informants described experiences of mental and physical relaxation, satisfaction and well‐being connected to the moments immediately following the exercise sessions. p.53. |
| Subtheme | Study | Direct participant data | Author description of data |
| Influence of programme supervisors | "Well I felt because [physiotherapist] took the trouble of explaining it all to me I couldn't turn around and say, "well blow it, why bother sort of thing? you know?" And when I first turned round and said that I would do it, I felt well alright I wasn't obligated to do it but I felt let's do my bit towards it, you know. I didn't want her. p.134. ME: "So would you say that some weeks you do them [the exercises] two or three times?" Eileen: "Some weeks I can't…" ME: "Sometimes you can't make it at all?" Participant: "Yeah. Latterly. I think this is my own fault. I mean when I was going [to see the physiotherapist] every week you make yourself sort of do it don't you…I must admit I am not so good now I am not going." p.135. MT "Since you have stopped seeing [the physiotherapist] have you stopped doing the exercises?" Participant: "Yes I'm sorry I have yes. But as I said I haven't had no pain…I wondered whether it was temperature or dampness or something like that you see. Now there is nothing wrong with them." MT: "So you feel if there is nothing wrong with it you feel there is not much point in a…" Participant: "Well that's it. It's the wrong attitude I know." | The complex reciprocity that surrounds the relationship between therapist and patient and the obligation patients felt towards the physiotherapist, particularly the desire not to let her down, were important reasons for high levels of initial compliance. One participant explained how difficult it was to continue the exercises programme since she stopped seeing the physiotherapist. p.135. | |
| "The gym instructors advise you and give you confidence that you're not going to make things worse." p.562. "I think the physiotherapist or someone with a medical background is the best person to supervise exercise." p.562. "At the gym they give you one‐to‐one attention and an individual programme that's right for your body." "The supervision at the gym is very good; they monitor what you do." p.562. "…I had to stick rigidly to what he had said, the weights that he had specified…the idea was to stretch it that little bit further than I normally would do in order to support the joint more…but too much would…cause more damage and not enough wouldn't do any good…I was quite impressed actually by his knowledge…and I did exactly what he said and I did notice an improvement, a definite improvement." p.563. | The expert advice and supervision available in gyms or from physiotherapists was valued. p.563. | ||
| "The most important thing is listening to the physio and doing the exercises because he motivated me to do the exercises." p.486 | The impact of this feeling of accountability was to increase their motivation to exercise. People with knee OA described feeling accountable to their physical therapists and not wanting to let down the therapist. p.483. | ||
| "…I think it's really a lot, in fact an enormous amount, to do with the facilitator, she's both kind of encouraging and yielding and nurturing and understanding, but also was able to use a bit of steel and get us off our bums, you know, so she's got those kind of qualities naturally…" p.7. "…[Physiotherapist] gave us enormous confidence because she is such a, she is very very confident, obviously highly qualified, so it was good to have some body for an hour giving you good advice, which was sound…" p.7. | The care, support and guidance participants received during the informal discussions helped build a trusting, collaborative partnership between patient and physiotherapist. This increased participant's confidence and trust in the physiotherapist and belief in the rehabilitation programme. The interpersonal qualities and professional skills of the supervising therapist were considered as important to the success of the programme as the content of the programme itself. p.7. However, their greatest concern was losing the ongoing support of the physiotherapist would undermine their motivation to exercise, and they expressed a desire for ongoing support. pp.8‐9. | ||
| "She's so enthusiastic and she's pleased to see us every day, whether she feels like she is or not. She's always very welcoming and um yeah, very encouraging and you can ask her things all the time." p. 91. | The importance of good 'therapist/instructor' interaction was noted. The instructor helped create an enjoyable and supportive atmosphere, which appeared crucial for many participants. p.91. | ||
| "…umm the instructor we had was very, very good and ah I think it was just so good. And I think the motivation was there which is the big thing is to get you motivated you know?" p.66. "jolly you along." p.66. "Yes, I think the instructor was sort of aware of our capabilities and kept the challenge up. And it made it more interesting that way, because if you did the same thing over and over at the same level, it would be boring." p.66. "Yeah, so it's just funny little things that keep you thinking you have a responsibility to attend 'cause someone's gonna miss you." p.66. "No, I'd sooner have a leader." p.66. | The instructor was important and group members considered essential attributes of an instructor were: being understanding, tolerant, friendly and someone who will "jolly you along." The participants valued their relationship with a challenging instructor with whom they could establish a connection. It emerged that accountability was an important factor in motivation. Participants felt if they missed a class the instructor or group would notice, and this helped keep them motivated to go. The fact that there was a record of attendance being kept also contributed towards this. Participants were cognisant of the instructor watching them and noticing if they were doing exercises incorrectly, that he/she would playfully encourage them to challenge themselves and they wanted to do well for the instructor. All these factors contributed to the feeling of accountability, and were strong motivators to attend the classes. A number of questions as to how a water‐based exercise programme could continue to run, especially if funding for it was limited, were discussed. One question was the use of a 'buddy' system, where people would be paired up and go to the pool with their friend to do the exercises together. However, most participants were unenthusiastic about this idea as they would rather attend in a group with an instructor and did not want to rely on one person to go with. It was asked if groups could run with a short‐term instructor for a few weeks to demonstrate the exercises, with the groups then becoming self‐sufficient. Reactions to this idea were mixed. Some felt this would work, as long as it was a structured group with a set time and place to meet. However, most participants felt that an instructor was essential and that a class without an instructor would fall apart; that they were too forgetful to remember the exercises without an instructor there to tell them or that there would not be sufficient motivation. It was considered embarrassing to go without an instructor and some felt it would not be safe exercising without an instructor to guide them. A few participants had continued with the water exercises on their own since the classes had finished, and had found it difficult to maintain. Nominating a leader from the group to be the instructor was suggested and some participants liked this idea but other people felt this would not be fair on the nominated instructor. The instructor was important and group members. | ||
| "I think that physical therapists are the best to help those who have a physical dilemma to start exercising…and start carefully, and under supervision. I think that is very important." p.1020. "Well, I always say that my physical therapist is as good as any psychologist." p.1021. "What keeps me going now is attending physical therapy sessions." p.1021. | The participants described the importance of suitable exercise and their experience of how exercise should progress gradually under the supervision of a qualified person. p.1020. All participants had some experience with physical therapists, most of it positive, and many participants placed emphasis on the fact that the encouragement and understanding they received from their physical therapists were very important. The importance of listening and good communication was highlighted and seemed to play a big role in the perceived benefits of physical therapy. p.1021. 4 participants exercised under the supervision of a physical therapist at the time of the interviews. These participants described how the physical therapists kept them going and that the therapists were sometimes the key to going on. p.1021. | ||
| "It is something you notice when you give it up, since it [the exercise] was very difficult to do on your own…As there was nobody to supervise me it was easy to deteriorate again…Then there was nobody to urge you on." "I think that [an instructor] is good because then you learn what to do so that you do not do it in the wrong way. Otherwise you might do certain movements incorrectly and put too much pressure on your knees." p.55. | To receive guidance: this conception concerned the perceived need for moral support, encouragement and instructions on how to exercise. The statements were about compliance and the anxiety of doing something wrong. | ||
| "The physiotherapist determined the gradual increase of the exercises; he told me, for example, to increase the exercises by five minutes. I liked it that he told me what to do, nevertheless, he was my physiotherapist." p.275. The approach of the physiotherapist was very democratic, which I appreciated. Together, we discussed the activities and the increase of the activities. I could indicate to what extent I wanted to increase the activities, to what extent I could maintain the exercises. p.276. | Some participants reported that they were actively involved in choosing the activities, in gradually increasing these activities, and in using the performance charts. In contrast, other participants reported that the main decisions were taken by the physiotherapist and that they performed the activities as instructed by the physiotherapist. It appeared that all adherent participants reported that they were actively involved in the whole process and that the physiotherapists had a coaching role during intervention. However, most non‐adherent participants reported that the physiotherapist made all decisions (which was sometimes a deliberate choice of the participants). Therefore, it seems that active involvement of the participant facilitates adherence to exercises and activities. p.275. |
Social and environmental
| Subtheme | Study | Direct participant data | Author description of data |
| Prioritising exercise | Alan: "It wasn't so much at home I am able to do it, it's more at work…Perhaps not as often as I would really like to, but I can do it quite freely then, because I'm totally on my own." Kenneth: "So many things happening…The boys used to come in from school or work…people come and see [wife] and ugh…I'm out twice at least a week to band practice and I have two engagements as well." p.134. Eileen: "Weekends I try to do [the exercises] but I am very busy on the weekend really it is the only chance I get to do sort of any cleaning. Then my family usually come up in the afternoon, my sister and her husband, because on the way to Mum's they always come in. Sunday's I have Mum on Sunday see, then I have her two sisters because they are older." p.134. Kenneth: "It's just excuses when it comes down to basics. I mean you know you could get up in the morning and do it between 6 or 7 or something like that." p.134. Geoffrey: "There was a time when I missed one [session with the physiotherapist]. I don't know why…I think it was taking the wife somewhere I don't know and I must honestly admit that her needs come as a priority as far as I am concerned." p.135. | While a positive disposition towards exercise could increase motivation, more important was the willingness and ability to accommodate the exercises into everyday life. People who ceased exercising often cited conflict with regular routines to explain why continuing with exercises was not possible. By giving these explanations, 2 participants could have been trying to portray themselves in a favourable light by indicating that their non‐compliance was due to family commitments and obligations. Nevertheless, later in their interviews, both went on to admit some personal responsibility for their lack of compliance. For example, 1 participant indicated that non‐compliance resulted from a combination of a busy life and a reduced commitment to the physiotherapy. 1 participant, who was only partially compliant even during the time he was seeing the physiotherapist, recalled in his interview that he had missed 1 of the sessions with the physiotherapist because, not unreasonably, he always put the needs of his wife, who had a progressive and debilitating disease, before his own needs. p.135. | |
| "…I try and say, 'OK well I'll go there [gym], have a shower and go shopping'. I also work in a charity shop on a Saturday so I can go before I go there you know…I try to fit it in." p.563. I try to fit exercise into my weekly routine. (25) I'm on a gym referral scheme, so I have a set time to go and that helps. p.562. I do my exercises when I remember but when I'm busy I forget. (15, 11) I don't have enough self‐discipline to make me exercise regularly. (11) Finding the time to go to the gym is a problem. p.562. | Prioritising exercise and making it part of a weekly routine helped some people to maintain their exercise habit. For other people finding time to exercise was a low priority; some because they did not consider exercise to be important or appropriate, while other people freely admitted to being lazy or lacking motivation. | ||
| "It's part of life…I get up in the morning, I have a cup of coffee, I take my blood pressure medication, then I go and do my exercises…and I don't have to leave home!" p.486. | The structured programme enabled people with knee OA to incorporate the prescribed exercises into their daily schedules. p. 483. | ||
| "…I do the exercises upstairs when I get up in the morning…I find I might have a bit more time, because during the day you tend to let things slide." | ‐ | ||
| No data reported. | There was much discussion surrounding all aspects around the timing of the classes (time of day, frequency, regularity, which days of the week, how many days a week, duration of class, duration of programme, continuity, time of year/season) and no consensus was reached. This discussion mostly hinged around tiredness, illness and business. Some people felt they could not manage twice a week as they got tired or were too busy, while other people would prefer the classes to be more frequent, for example, 3 times a week or more to derive more health benefits. p.67. | ||
| "My job's very important, really important at the moment. Not only for the money but for myself as well because when my husband died, I just had to get busy. I just like being busy." p.196. | Some people had ceased to exercise and this was due to differing priorities. In some cases, they worked or had familial obligations like child minding or carer duties to fulfil. The way that participants made priorities in their life was not a linear process. For example, spending a lot of time working was not just related to needing money. Rather, making priorities of how time was spent formed part of the ongoing 'back story' of participant's lives. 1 woman who had talked about her longstanding love of walking and the benefits of it for easing her knee pain outlined how she had chosen to do more hours at work to help her cope with the loss of her husband. The amount of time she spent in work then impacted upon the amount of time available to go walking. Knee pain was not the main priority. Often, the activities that people engaged in are related to psychological and social well‐being. It is not to say that some participants had lost the motivation to exercise in some cases. 1 participant had access to gym facilities as part of his job, but when he left that position he lost that benefit. As a result, he described how he had fallen out of the 'habit.' pp.195‐196. | ||
| "One is so occupied that it is very easy not to find time for exercise. Everything else takes precedence." | To devote time. This conception included different aspects of time as essential for the effectiveness of the exercise. The statements concerned time as the most appropriate time point during disease course when first starting to exercise, and having adequate time to exercise. pp.55‐6. |
| Subtheme | Study | Direct participant data | Author description of data |
| Support of friends and family | Stanley: "If perhaps my wife would work with me and you had a bit of competition, but I feel such a fool standing on one leg and going up and down on my own and I tends to drop it I do. I'm not very strong disciplined on that, no. I know some people can be so, but not me. I suppose if there was a really good reason I would." | 1 participant stopped the exercises because it was difficult to do them alone and, as he had not noticed much improvement in his symptoms, there did not seem to be a strong rationale for continuing. | |
| "You know, you're not stuck at home all the time, it's a way of getting out." "It's nice to be out in a group and not feel so isolated so it was a good, psychological it was, really good." "I think it's important to be with other people, how other people cope and that you're not alone and there are other people you know, in | ‐ | ||
| "Yes, my wife, naturally, she encourages me." "It [the experience of lack of support] was, just, what should I say, totally pathetic…. I guess men are not all equally understanding." p.2020. | The support, caring and encouragement of other people were among important external factors influencing how much the participants exercised. Most of the participants seemed to feel the need for such encouragement. Yet, when talking about the family's attitudes toward the disease and the importance of exercise, some of the women expressed having a hard time justifying to themselves and their families their need to spend time exercising. | ||
| "One of my friends who knows about my arthritis asked me if I ever exercise." "I know [my husband] supports being active, but I never really felt overly | Participants expressed feeling facilitated toward physical activity adoption with high levels of social support stemming from their family and friends. p.15. Other participants contemplated physical activity if they had support from their family members. More specifically, spouses and children were cited as being the most important family members in facilitating physical activity adoption. p.16. |
| Subtheme | Study | Direct participant data | Author description of data |
| Social identity | "They're (gyms) mostly young people that go to those aren't they? I think I'd feel out of place…They don't want to be dragged down by somebody that's not up to their standard I would think." p.563. "I imagined…all these fit people you know, bodies like Adonis…I thought that I would be old, that I would show myself up, but in fact it wasn't like that at all…the people who were sort of totally 100% fit were very few and far between." p.563. "I imagined the people at the gym would all be young and fit and that I would feel out of place but it wasn't like that at all." "The gym is safer for women than going out walking alone." | Data not reported. | |
| "I would love to see something for the elderly people, to be active and keep reasonably fit. There's very little around for the older people. They don't want to know the older people." "It's got to be paced at our age range." "They need to have something for the older people, keep the younger ones different." "Well I think it's important that you go, even if it's on land, that you go with people relative to your own age and that you're all at the same level 'cause I mean if you go with a 30‐year old…we can't keep up with that, as much as we'd like to. Whereas if you go and you're all this age, you encourage each other." p.14. | 1 of the primary reasons given for discontinuing an aqua‐based exercise programme was that participants felt the class they had attended was not suitable for their age…Participants in the study felt strongly that they should be attending classes suitable for their age. p.14. Training with people of a comparable age was also considered important in the study. Similarly, older adults who performed land‐based resistance training identified this as an important facilitator for exercise. Attending age or ability (or both) appropriate classes may have increased adherence to aqua‐based exercise among participants in the study. p.15. |
| Subtheme | Study | Direct participant data | Author description of data |
| Exercise facilities | "I'm happy to go to the gym." "I'd be too embarrassed to go to a gym." "I would go to a gym if my doctor referred me." "The bikes at the gym are easier to use and safer than cycling in traffic." p.562. "I prefer to do outdoor exercise like cycling or walking." p.562. "I would rather do exercises at home." p.562. "I wasn't keen on doing things on the machines 'cause I think that they're so boring." p.562. | The location of exercise was important. Some people preferred exercising at home; other people preferred outdoors. Some people who had tried exercising at a gym did not enjoy it. Gyms were sometimes viewed as inappropriate places. Other people found by experience that this was not the case. pp.563‐4. | |
| "In the break in the summer time, I've gone to the normal pool…and tried to do my exercises there…you're less stiff after you come out, shall we say, than before you went in, but you don't get the same kind of pain relief as from the heated water." p.91. "After about 20 minutes in that temperature of the normal public pools, you tend to get cramp…So the water there, isn't warm enough really for arthritic people." p.91. | Participants also discussed the importance of the warm water to exercise in, helping to relax muscles and easing pain, a benefit they did not gain from public pools…And importantly for some people, being in a normal (cooler) pool gave them extra symptoms. p.91. | ||
| "I suppose one of the reasons why I did stop is because it's coming up to winter and it's outside…and it's cold…I would like to go to a class in a hotter pool." "Very cold, I found that a real downside." "At [the pool I attended] that was the worst…coming out you were freezing cold and you have to get changed back again." "Then I ran out of money basically…it's very expensive, to belong to a gym club." "I mean some of them charge an awful lot to get in. When you go up to the pool it's $2 and then you get charged $5 to go into the aerobics, well that's really, sort of, you know, pay for the guys time, that person's time but when you're on a pension you haven't got that." "The cost, when you're on a limited budget." "When I was in [name of pool] I stopped going because I got chlorine burns on my skin, from here (indicated chest level) right up." "That's right, it was like weeping eczema and the arthritis society was so worried because I was going to one of their classes at the beginning and they said that they wanted to take it further and of course I became allergic to a lot of the minerals that are added to the [name of pool]." p.14. | 2 weaker environmental themes that emerged were cost and skin reaction to the pool water. Several participants in the study felt that cost was a barrier to continued participation in aqua‐based exercise and this applied regardless of whether they had attended a private or public facility. Not surprisingly, socioeconomic status would appear to be a major factor in whether or not cost is perceived as a barrier to activities like aqua‐based exercise. Skin reaction to the pool water was described by 2 participants in the study. p.15. | ||
| "…couldn't probably afford a big amount, twice a week." | The location of the water‐based exercise classes (a large indoor aquatic centre pool) was discussed, as well as other potential locations (the warm therapeutic community pool, local school pools, the community salt water pool and other smaller community pools). Participants weighed up the pros and cons of the various pools and opinion differed on the ideal location for the classes. p.67. The next discussion centred on which community pool to use. While a few people thought that using local smaller community or school pools would increase accessibility and reduce transportation issues, the suitability of these pools, particularly the depth and width, was questioned. Furthermore, these pools did not regularly have lifeguards in attendance and thus there were safety concerns. Most people liked the large, centrally located medium‐depth pool the classes were held in even though it was "very public" and busy. An added bonus to the latter pool was the spa pool which some participants used at the end of each class. p.67. Money (e.g. cost, funding, payment, expense, price, discounts) and who pays or contributes was discussed extensively. While grateful for the free classes, participants were realistic in understanding that this could not continue. The majority of participants said they would not mind contributing a small amount of money towards pool entry or the cost of the classes. Some participants were confident that alternative funding could be sourced, and thought that personal contributions may not be necessary allowing the classes to continue to be run free of charge. Ideas of how the classes could continue were discussed. Alternative sources of funding was discussed, such as from local charitable organisations concerned with assisting older adults or perhaps the pool itself would provide discounted or free entry for these classes. The majority of participants said they would not mind contributing a small amount toward pool entry or to the running of the classes. However, some participants stated they were on their pension and that it was a great motivation to have the classes for free. p.68. | ||
| If I was a boy or a man, I would kick those machines; I hate adjusting them, it takes half the time." "And this costs money. Walking, however, is free. Such things matter when you only have your pension." p.2021. | Sometimes, the accessibility of training facilities was poor and the equipment not user‐friendly. When walking outside, the lack of benches was mentioned as a barrier. The cost of exercising indoors (e.g. using a gym) was a barrier for those participants with low income. p.2021. | ||
| "It has to be close at hand, one should not have to travel long distances. It would never work for me, if I had to travel to a rehabilitation centre every day. I don't think so." p.55. "But it [the exercise] should be done in an appropriate manner." p.55. | To have structure. This conception contained statements about accessibility as a prerequisite for exercise, and the importance of quality of exercise, concerning both purpose with and type of exercise. p.55. | ||
| GP: general practitioner; OA: osteoarthritis. | |||
Appendix 5. Contribution of each study to the themes arising from the qualitative synthesis
| Themes from the qualitative synthesis (number of studies) | ||||||||||||
| Symptoms | ||||||||||||
| Pain and physical function (6) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ‐ | ✔ | ✔ | ✔ | ‐ | ‐ |
| Capacity to exercise (6) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ |
| Impact of exercise on the effects of OA (10) | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ |
| Health beliefs and views on the management of OA | ||||||||||||
| Aetiology and prognosis of OA (4) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Non‐exercise management strategies (3) | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Advice and information from health professionals (6) | ✔ | ‐ | ✔ | ✔ | ✔ | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ |
| Health beliefs and managing OA and exercise (6) | ✔ | ‐ | ✔ | ✔ | ✔ | ‐ | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ |
| Everyday activities (physical activity) versus structured exercise (4) | ‐ | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ |
| Psychological factors | ||||||||||||
| Impact of OA on people's sense of "self" (4) | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ | ‐ |
| Individual disposition (2) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ |
| Psychological benefits of exercise (8) | ‐ | ✔ | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ | ✔ | ‐ | ✔ | ‐ |
| Influence of programme supervisors (9) | ✔ | ‐ | ✔ | ✔ | ✔ | ✔ | ✔ | ‐ | ✔ | ‐ | ✔ | ✔ |
| Social and environmental factors | ||||||||||||
| Prioritising exercise (7) | ✔ | ‐ | ✔ | ✔ | ✔ | ‐ | ✔ | ✔ | ‐ | ‐ | ✔ | ‐ |
| The support of family and friends (4) | ✔ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ✔ | ✔ | ‐ | ‐ |
| Social identity (2) | ‐ | ✔ | ‐ | ‐ | ✔ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Exercise facilities (6) | ‐ | ✔ | ✔ | ‐ | ‐ | ✔ | ✔ | ‐ | ✔ | ‐ | ✔ | ‐ |
| OA: osteoarthritis. | ||||||||||||

Complex reciprocal inter‐relationship between pain, physical and psychosocial function and exercise (Hurley 2003: permission for reproduction provided by the publishers, Wolters Kluwer).

Effect of erroneous health beliefs (Hurley 2003: permission for reproduction provided by the publishers, Wolters Kluwer).
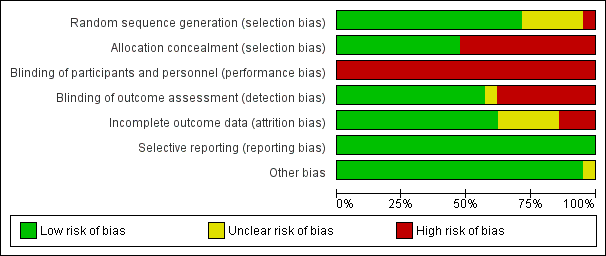
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
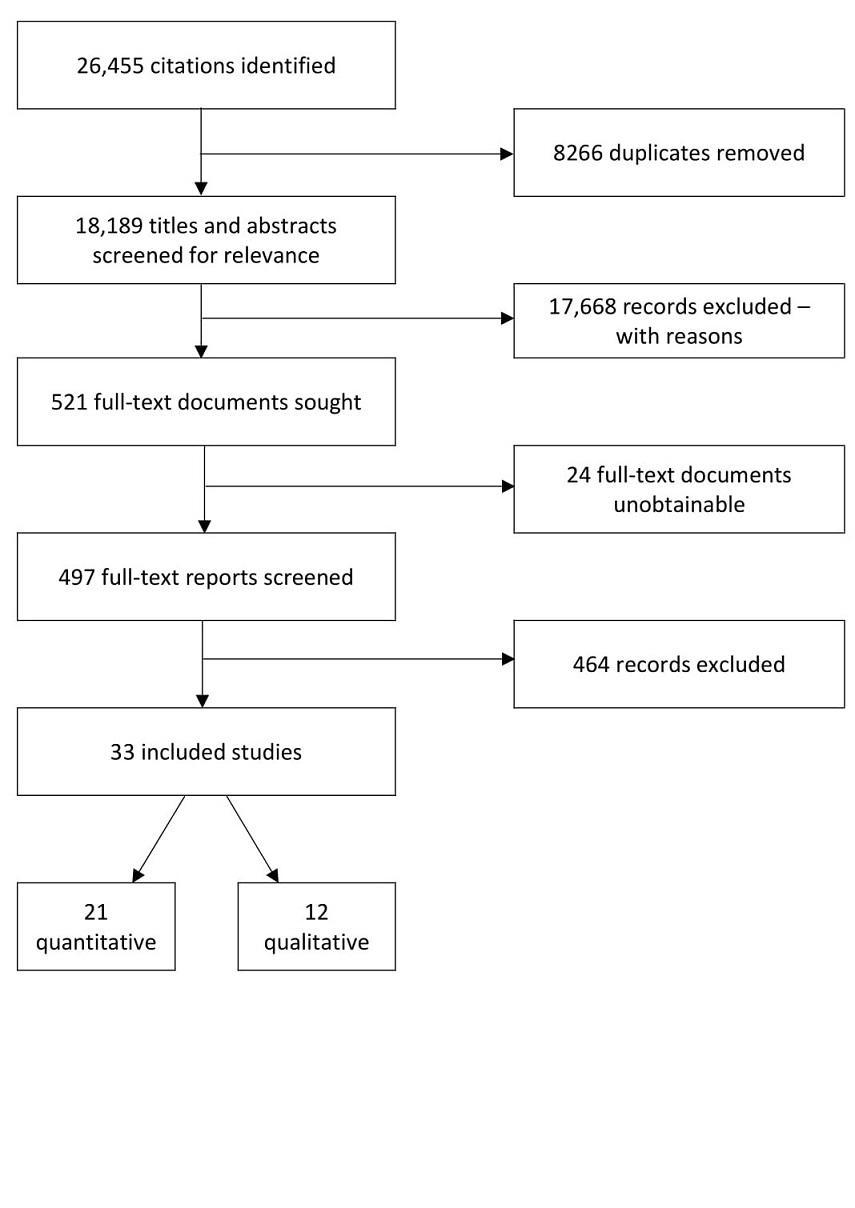
Flow chart of search and screening process.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Emergent themes from qualitative synthesis. OA: osteoarthritis.

Comparison 1 Exercise versus control, Outcome 1 Pain.

Comparison 1 Exercise versus control, Outcome 2 Physical function.

Comparison 1 Exercise versus control, Outcome 3 Self‐efficacy (SE).
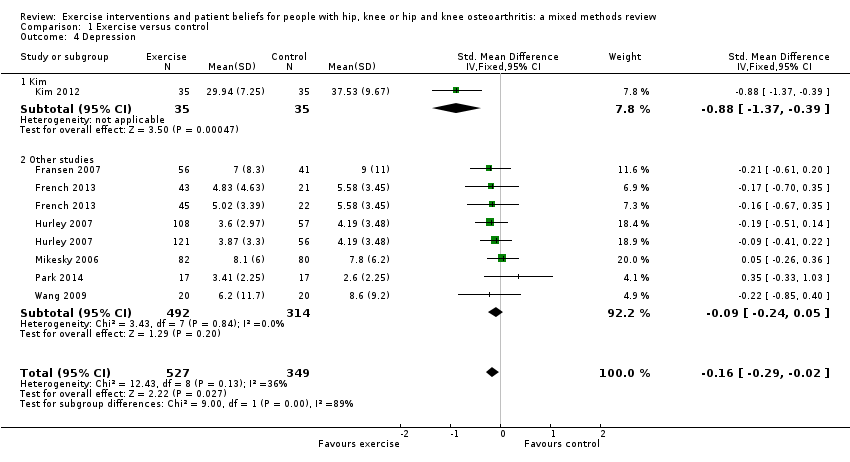
Comparison 1 Exercise versus control, Outcome 4 Depression.
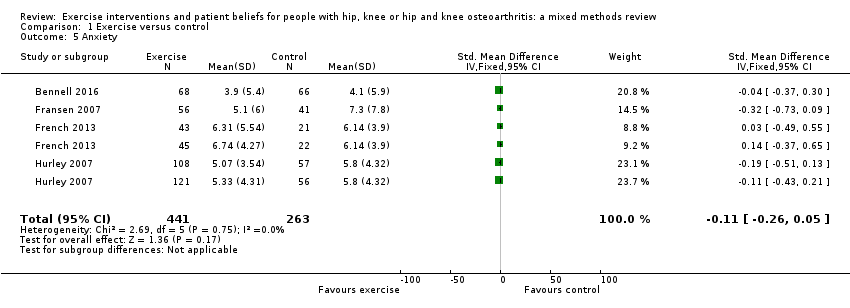
Comparison 1 Exercise versus control, Outcome 5 Anxiety.
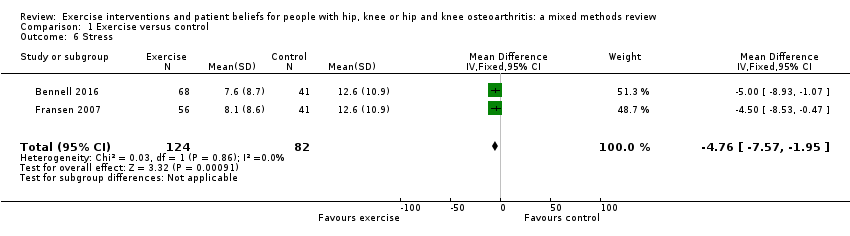
Comparison 1 Exercise versus control, Outcome 6 Stress.
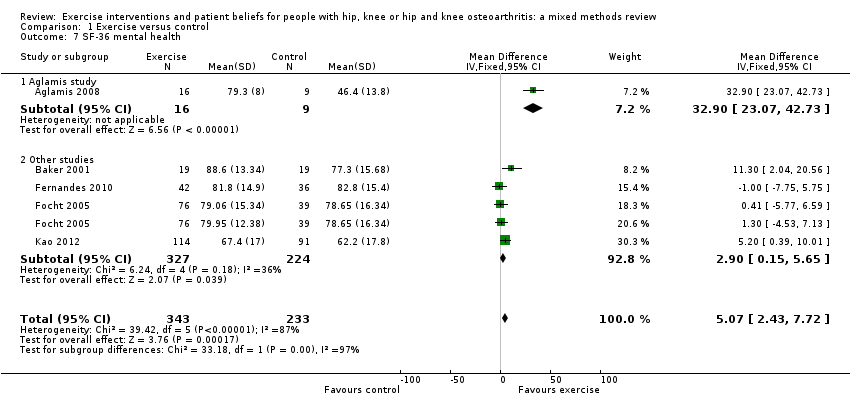
Comparison 1 Exercise versus control, Outcome 7 SF‐36 mental health.
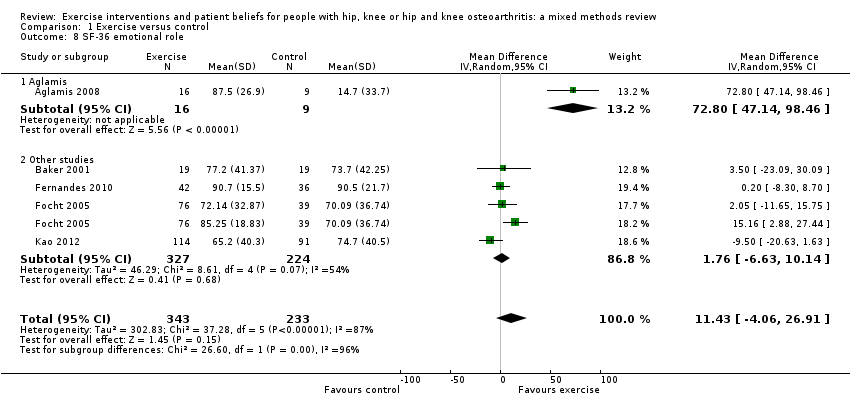
Comparison 1 Exercise versus control, Outcome 8 SF‐36 emotional role.

Comparison 1 Exercise versus control, Outcome 9 SF‐36 social function.

Comparison 1 Exercise versus control, Outcome 10 SF‐36 vitality.

Comparison 1 Exercise versus control, Outcome 11 Sleep.
| Physical and psychosocial outcomes in people with hip, knee or hip and knee osteoarthritis | ||||||
| Patient or population: people with chronic hip, knee or hip and knee osteoarthritis | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Exercise | |||||
| Pain. WOMAC normalised to 0‐20 pain scale based on largest study reporting the 0‐20 scale (Hurley 2007). Lower score indicated less pain. Mean duration of follow‐up: 45 weeks (range: 12 weeks to 30 months). | The mean WOMAC pain score was 6.5. | The mean pain in the intervention groups was 1.25 points lower (1.8 to 0.8 lower) | ‐ | 1058 (9 studies) | ⊕⊕⊕⊝ | 6% absolute pain reduction (95% CI ‐9% to ‐4%). 19% relative pain reduction (95% CI ‐27% to ‐11%). SMD ‐0.33 (95% CI ‐0.46 to ‐0.21). |
| Physical function. WOMAC function scales normalised to 0‐100. Lower score indicated improved physical function. Mean duration of follow‐up: 41 weeks (range: 9 weeks to 30 months). | The mean WOMAC function was 49.9. | The mean function in the intervention groups was 5.6 points lower (7.6 to 2.0 lower) | ‐ | 1599 | ⊕⊕⊕⊝ Moderate2 | 5.6% absolute function improvement (95% CI ‐7.6% to 2%). 11.2% relative function improvement (95% CI ‐15.2% to ‐4%). SMD ‐0.27 (95% CI ‐0.37 to ‐0.17). |
| Self‐efficacy. Self‐efficacy scores transformed to exercise beliefs score with score range from 17 to 85. Higher score indicated greater self‐efficacy. Mean duration of follow‐up: 35 weeks (range: 12 weeks to 18 months). | The mean self‐efficacy was 64.3. | The mean self‐efficacy in the intervention groups was 1.13 points higher (0.74 to 1.51 higher) | ‐ | 1138 | ⊕⊕⊝⊝ | 1.66% absolute increase in self‐efficacy (95% CI 1.08% to 2.20%). 1.76% relative increase (95% CI 1.14% to 2.23%). SMD 0.46 (95% CI 0.34 to 0.58). |
| Depression. Depression scores were transformed to the HADS depression scale with score range of 0‐21. Lower score indicated less depression. Mean duration of follow‐up: 35 weeks (range: 8 weeks to 30 months). | The mean depression was 3.5. | The mean depression in the intervention groups was 0.5 points lower (1.0 to 0.1 lower). | ‐ | 919 | ⊕⊕⊕⊝ | 2.4% absolute reduction in depression (95% CI ‐4.7% to ‐0.5%). The relative reduction was 14.3% (95% CI ‐2.8% to ‐28%). SMD ‐0.16 (95% CI‐0.29 to ‐0.02). |
| Anxiety. HADS scale of 0‐21. Lower score indicated lower anxiety levels. Mean duration of follow‐up: 24 weeks (range: 9 weeks to 12 months). | The mean anxiety was 5.8. | The mean anxiety in the intervention groups was 0.4 points lower (1.0 lower to 0.2 higher). | ‐ | 704 | ⊕⊕⊕⊝ | 2% absolute improvement in anxiety (95% CI ‐5% to 1%). The relative change was 6.9% (95% CI ‐17.2% to 3.4%). SMD ‐0.11 (95% CI ‐0.26 to 0.05). |
| SF‐36 social function. Domain of SF‐36 considered representative of quality of life: mental health domain largely covered by depression and anxiety above: scale of 0‐100. Higher score indicated improved social function. Mean duration of follow‐up: 36 weeks (range: 8 weeks to 18 months). | The mean social function was 73.6. | The mean SF‐36 social function in the intervention groups was 7.9 (4.1 to 11.6 higher). | ‐ | 576 | ⊕⊕⊝⊝ | 7.9% absolute improvement in social function (95% CI 4.1% to 11.6%). The relative improvement was 8.8% (95% CI 2.7% to 13.9%). |
| Adverse effects of treatment | ‐ | ‐ | ‐ | ‐ | ‐ | Studies did not provide information on adverse events. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Pain downgraded one level due to high risk of bias for blinding of participants. 2Function downgraded one level due to high risk of bias for blinding of participants. 3Self‐efficacy downgraded two levels; one level due to moderate heterogeneity (I2 = 47%) probably due to different measures of self‐efficacy being used in each study, and one level due to high risk of blinding bias. 4Depression downgraded one level due to high risk of blinding bias. 5Anxiety downgraded one level due to high risk of blinding bias. | ||||||
| No | Study | Quality of evidence | |||||
| Dependabilityof findings | Credibilityof findings | ||||||
| Author | Low | Medium | High | Low | Medium | High | |
| 1 | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ | |
| 2 | ‐ | ✔ | ‐ | ‐ | ✔ | ‐ | |
| 3 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 4 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 5 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 6 | ‐ | ‐ | ✔ | ‐ | ✔ | ‐ | |
| 7 | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ | |
| 8 | ‐ | ‐ | ✔ | ‐ | ✔ | ||
| 9 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 10 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 11 | ‐ | ‐ | ✔ | ‐ | ‐ | ✔ | |
| 12 | ‐ | ✔ | ‐ | ‐ | ‐ | ✔ | |
| Quality appraisal question | Answer options | |||
| Not at all/not stated | Few steps | Several steps | A thorough attempt | |
| 1. Were steps taken to increase rigour in sampling? | 0 studies | 1 study | 7 studies Fisken 2016; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Stone 2015 | 4 studies |
| 2. Were steps taken to increase rigour in data collection? | 0 studies | 0 studies | 7 studies Campbell 2001; Fisken 2016; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Veenhof 2006 | 5 studies Hendry 2006; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006 |
| 3. Were steps taken to increase rigour in data analysis? | 0 studies | 0 studies | 6 studies Campbell 2001; Fisken 2016; Hurley 2010; Larmer 2014b; Moody 2012; Stone 2015 | 6 studies Hendry 2006; Hinman 2016; Morden 2011; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 |
| Quality appraisal question | No grounding | Limited grounding/support | Fairly well grounded | Well grounded/supported |
| 4. Were the findings of the study grounded in/supported by data? | 0 studies | 0 studies | 4 studies | 8 studies Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Morden 2011; Petursdottir 2010; Stone 2015; Thorstensson 2006 |
| Quality appraisal question | Limited breadth and depth | Good/fair breadth, limited depth | Good/fair depth, limited breadth | Good/fair breadth and depth |
| 5. Breadth and depth of findings? | 0 studies | 3 studies | 3 studies | 6 studies Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Stone 2015; Thorstensson 2006 |
| Quality appraisal question | Not at all | A little | Somewhat | A lot |
| 6. To what extent did the study privilege the perspectives and experiences | 0 studies | 0 studies | 6 studies Fisken 2016; Hurley 2010; Moody 2012; Morden 2011; Thorstensson 2006; Veenhof 2006 | 6 studies Campbell 2001; Hendry 2006; Hinman 2016; Larmer 2014b; Petursdottir 2010; Stone 2015 |
| # | Review finding | Relevant papers | CERQual assessment of confidence in the evidence | Explanation of CERQual assessment |
| I. Symptoms | ||||
| Pain, muscle weakness, physical function: the experience of living with pain and its impact dominated people's narratives because it affected most areas of their daily life and became worse over time. Pain levels varied, and were described as episodic and unpredictable. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Morden 2011; Petursdottir 2010; Stone 2015 | High confidence | Low methodological limitations across all studies, with high coherence and high relevance. 3 countries and 4 geographical regions represented by 6 studies. | |
| Capacity to exercise: pain, joint stiffness, fatigue, comorbidity and people's perceptions of their physical fitness, both before and after exercise, restricted the type and amount of exercise people felt able to engage in. Additional efforts required to shower and change exacerbated the difficulties, and people also reported difficulties with fatigue after exercise sessions. | Campbell 2001; Hendry 2006; Hurley 2010; Moody 2012; Petursdottir 2010; Thorstensson 2006 | High confidence | Low methodological limitations for 5 of the 6 studies, high relevance for 5 of the 6 studies, and high coherence. 4 countries and 2 geographical regions represented. | |
| Impact of exercise on the effects of OA: some participants reported dramatic improvements in symptoms as a result of exercising, while some felt there was little or no benefit. Some people believed other treatment routes were more effective. However, for those who did benefit from exercise, function was improved and pain reduced allowing a return to more normal day‐to‐day activities that had been avoided. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | Findings applied to 9 studies, 8 having low methodological limitations and 6 having high relevance. Moderate coherence across the studies. 6 countries and 2 geographical regions represented. | |
| II Health beliefs and views on the management of OA | ||||
| Aetiology and prognosis of OA: people considered OA to be an inevitable result of placing stress on their joints, the ageing process or a hereditary condition, with limited hope of improvement. Expectations that the condition would worsen over time made it difficult to convince people of the scope for improvement through appropriate treatment. | Low confidence | 4 studies representing 2 countries from 2 different geographical regions. Methodological limitations low across all studies, relevance high in 3 of the 4 but medium coherence. | ||
| Non‐exercise management strategies: some people's understanding of how to manage their OA condition was limited to medication (analgesia) or surgery with little awareness of the role of exercise. Views on pain medication and surgery were mostly negative, with concerns of becoming addicted (to medication) and mixed views and hesitancy regarding surgery, with some people unsure it would work while others considered it a worthwhile option. There was a keenness to delay surgery as long as possible. | Low confidence | Low methodological limitations, but only 3 studies with medium‐to‐high relevance and medium coherence, all from the same country. | ||
| Advice and information from health professionals: participants described their experiences of receiving advice and information from health professionals. This was wide‐ranging in its usefulness and detail for people, and some formed negative beliefs due to limitations of the information they were provided with. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Thorstensson 2006 | Medium confidence | Low methodological limitations, high relevance in 5 of the 6 studies, 3 geographical regions represented by 4 countries. Medium coherence. | |
| Health beliefs and managing OA and exercise: attitudes towards exercise in OA were found to be closely linked to beliefs and perceptions regarding aetiology. Negative beliefs were widely held about the OA prognosis which in turn demotivated them from active management of the condition. Some were concerned about exacerbating the condition, and some felt they were too old for exercise to be of benefit. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Petursdottir 2010; Thorstensson 2006 | High confidence | Low methodological limitations across the 6 studies with high relevance for all except 1. Medium‐to‐high coherence. 4 countries and 2 geographical regions represented. | |
| Everyday activities (physical activity) versus structured exercise: this relates to whether people felt that general physical activities that took place in everyday life were sufficient to manage OA, or whether structured exercise sessions had additional benefits. Some people did not perceive a difference between the two, and did not see a need for structured exercise, while others felt normal daily activity was insufficient and needed to be supplemented with formal exercise. Some people worked to increase their general physical activity levels in the belief it would be helpful for their OA. | Hendry 2006; Moody 2012; Petursdottir 2010; Thorstensson 2006 | Low confidence | Low methodological limitations in 3 of only 4 studies, 2 regions and 4 countries represented, with high relevance but only medium coherence. | |
| III Psychological factors | ||||
| Impact of OA on people's sense of "self": the limitations of OA meant that activities that people had previously defined themselves by were now compromised. A new sense of self needed to be constructed to help overcome the negative psychological effects of this, taking on alternative social roles to ensure they maintained a sense of purpose and remained 'useful' despite incapacitation. Those who struggled to do so expressed negative emotions and the feeling of being a burden and frustrated with their limitations. | High confidence | 4 studies with low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | ||
| Individual disposition: high self‐efficacy and a positive outlook was seen as vital in ensuring people did not become defined by their OA. This involved the determination to find new ways to cope. Where self‐efficacy was low, there was an avoidance of physical activity because of the belief it would aggravate pain levels. | Low confidence | 2 studies, from 2 countries/regions with good methodological rigour and high relevance overall. However, medium coherence and lack of confidence in this review finding due to paucity of data. | ||
| Psychological benefits of exercise: people reported favourable psychological benefits of exercise. They also appreciated the peer support and social opportunities that accompanied group forms of exercise. | Fisken 2016; Hendry 2006; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Thorstensson 2006 | High confidence | 8 studies with overall low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Influence of programme supervisors: people who undertook supervised exercise programmes valued programme providers who understood their condition and encouraged and facilitated their engagement in exercise. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | 9 studies with overall low methodological limitations. Highly relevant data from 5 countries and 2 geographical regions. High coherence. | |
| IV Social and environmental factors | ||||
| Impact of OA on people's sense of "self": the limitations of OA meant that activities that people had previously defined themselves by were now compromised. A new sense of self needed to be constructed to help overcome the negative psychological effects of this, taking on alternative social roles to ensure they maintained a sense of purpose and remained 'useful' despite incapacitation. Those who struggled to do so expressed negative emotions and the feeling of being a burden and frustrated with their limitations. | High confidence | 4 studies with low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | ||
| Individual disposition: high self‐efficacy and a positive outlook was seen as vital in ensuring people did not become defined by their OA. This involved the determination to find new ways to cope. Where self‐efficacy was low, there was an avoidance of physical activity because of the belief it would aggravate pain levels. | Low confidence | 2 studies, from 2 countries/regions with good methodological rigour and high relevance overall. However, medium coherence and lack of confidence in this review finding due to paucity of data. | ||
| Psychological benefits of exercise: people reported favourable psychological benefits of exercise. They also appreciated the peer support and social opportunities that accompanied group forms of exercise. | Fisken 2016; Hendry 2006; Hurley 2010; Larmer 2014b; Moody 2012; Morden 2011; Petursdottir 2010; Thorstensson 2006 | High confidence | 8 studies with overall low methodological limitations. Highly relevant data from 4 countries across 2 geographical regions. High coherence. | |
| Influence of programme supervisors: people who undertook supervised exercise programmes valued programme providers who understood their condition and encouraged and facilitated their engagement in exercise. | Campbell 2001; Hendry 2006; Hinman 2016; Hurley 2010; Larmer 2014b; Moody 2012; Petursdottir 2010; Thorstensson 2006; Veenhof 2006 | High confidence | 9 studies with overall low methodological limitations. Highly relevant data from 5 countries and 2 geographical regions. High coherence. | |
| CERQual: Confidence in the Evidence from Reviews of Qualitative Research; OA: osteoarthritis. | ||||
| Integrative review | Implications for exercise programmes derived from the qualitative synthesis | Mean and 95% CI | ||||||||||||||
| Information/demonstrate improvement | Individually tailored interventions | Challenge beliefs | Practical support | |||||||||||||
| Trial (meta‐analysis comparison) | Recruitment | Intervention | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Pain | Function | Self‐efficacy | Depression | Anxiety |
| Studies with a low risk of bias | ||||||||||||||||
| Local community. | 10 individual sessions of semi‐standardised exercises over 12 weeks plus exercises to perform 4 times a week at home. | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | √ | 0.21 ‐0.19 to 0.61 | 0.09 ‐0.31 to 0.49 | 0.05 ‐0.35 to 0.45 | ‐ | ‐ | |
| Community participants. | 10 treatments over 12 weeks of exercise or exercise and education. | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.33 ‐0.67 to 0.01 | ‐0.81 ‐1.17 to ‐0.46 | 0.61 0.26 to 0.96 | ‐ | ‐0.04 ‐0.37 to 0.30 | |
| Community through flyers, press releases and mailings via local physician practice. | Hatha yoga, once a week in a class + 4 shorter sessions a week at home. | ‐ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.86 ‐1.55 to ‐0.17 | ‐0.42 ‐1.08 to 0.24 | ‐ | ‐ | ‐ | |
| University hospital, local hospital, rehabilitation centre, general practitioners, and local newspaper advert. | 3 group‐based sessions and 1 individual physical therapy visit, 2 months after completing the group sessions. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.30 ‐0.75 to 0.15 | ‐0.47 ‐0.92 to ‐0.02 | ‐ | ‐ | ||
| Local newspapers & social clubs, general practitioners and rheumatologists. | Tai Chi, twice a week, 12 weeks. | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.52 ‐0.93 to ‐0.11 | ‐0.66 ‐1.07 to ‐0.24 | ‐ | ‐0.21 ‐0.61 to 0.20 | ‐0.32 ‐0.73 to 0.09 | |
| General practitioners, rheumatologists, orthopaedic surgeons, and hospital consultants. | 6‐8 individual 30‐minute physiotherapy sessions over 8 weeks. Strength/resistance training and manual therapy + patient information. | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.43 ‐0.96 to 0.10 | ‐0.40 ‐0.83 to 0.03 | ‐ | ‐0.18 ‐0.61 to 0.24 | 0.04 ‐0.39 to 0.46 | |
| General practitioners, rheumatologists, orthopaedic surgeons, and hospital consultants. | 6‐8 individual 30‐minute physiotherapy sessions over 8 weeks. Strength/resistance training + patient information (no manual therapy). | √ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.55 ‐1.07 to ‐0.03 | ‐0.49 ‐0.92 to ‐0.07 | ‐ | ‐0.16 ‐0.58 to 0.26 | 0.15 ‐0.27 to 0.56 | |
| Inner‐city primary care practices. | Physiotherapist, twice a week, 6 weeks; individual exercise. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.25 ‐0.56 to 0.07 | ‐0.15 ‐0.41 to 0.10 | 0.44 0.12 to 0.76 | ‐0.19 ‐0.50 to 0.13 | ‐0.19 ‐0.51 to 0.13 | |
| Inner‐city primary care practices. | Physiotherapist, twice a week, 6 weeks; group exercise. | √ | ‐ | √ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐0.13 ‐0.45 to 0.19 | 0.06 ‐0.19 to 0.19 | 0.42 0.09 to 0.75 | ‐0.09 ‐0.42 to 0.23 | ‐0.11 ‐0.43 to 0.21 | |
| Studies with a high risk of bias | ||||||||||||||||
| ‐ | ‐ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.54 ‐1.37 to 0.30 | ‐0.64 ‐1.48 to 0.20 | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.56 ‐1.16 to 0.05 | ‐0.48 ‐1.08 to 0.12 | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐0.23 ‐0.62 to 0.16 | ‐0.17 ‐0.22 to 0.56 | 0.44* 0.05 to 0.83 | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐0.05 ‐0.33 to 0.44 | ‐0.3 ‐0.42 to 0.36 | ‐ | ‐ | ‐ | |
| ‐ | ‐ | √ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.15 ‐0.55 to 0.24 | ‐ | 0.89* 0.47 to 1.30 | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.54 0.26 to 0.82 | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.13 ‐0.51 to 0.76 | ‐ | 0.36 ‐0.44 to 1.15 | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.42 ‐1.10 to 0.27 | ‐ | ‐0.07 ‐0.89 to 0.74 | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.60 ‐1.07 to 0.12 | ‐ | 1.04 0.05 to 1.54 | ‐0.88 ‐0.37 to 0.39 | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | √ | ‐0.56 ‐0.88 to ‐0.25 | 0.10 ‐0.21 to 0.41 | ‐ | 0.05 ‐0.26 to 0.36 | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.35 ‐0.33 to 1.03 | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.04 ‐0.32 to 0.39 | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | √ | √ | √ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.22 ‐0.52 to 0.08 | ‐0.95* 0.04 to 1.87 | ‐ | ‐ | |
| ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.40 ‐0.95 to 0.16 | ‐ | ‐0.16 ‐0.70 to 0.39 | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.68 ‐1.32 to ‐0.04 | ‐0.17 ‐0.31 to ‐0.03 | 0.71 0.07 to 1.35 | ‐ | ‐ | |
| ‐ | ‐ | √ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.17 ‐0.53 to 0.19 | ‐ | 0.32 ‐0.04 to 0.69 | ‐ | ‐ | |
| CI: confidence interval. | ||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain Show forest plot | 19 | 2144 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.28, ‐0.11] |
| 1.1 WOMAC pain | 9 | 1058 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.46, ‐0.21] |
| 1.2 Other pain outcomes | 10 | 1086 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.19, 0.05] |
| 2 Physical function Show forest plot | 13 | 1599 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐0.37, ‐0.17] |
| 3 Self‐efficacy (SE) Show forest plot | 11 | 1138 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.46 [0.34, 0.58] |
| 3.1 Six‐minute walk SE | 1 | 115 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.44 [0.05, 0.83] |
| 3.2 Lorig SE exercise scale | 2 | 168 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.63, 1.27] |
| 3.3 ExBeliefs SE | 1 | 338 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [0.20, 0.66] |
| 3.4 Arthritis SE scale | 1 | 54 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.42, 0.72] |
| 3.5 McAuley SE exercise scale | 1 | 21 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.95 [0.04, 1.87] |
| 3.6 VAP SE | 1 | 52 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.70, 0.39] |
| 3.7 Arthritis SE scale ‐ pain | 1 | 120 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.04, 0.69] |
| 3.8 SE Score | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.71 [0.07, 1.35] |
| 3.9 ASES pain | 2 | 230 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.11, 0.63] |
| 4 Depression Show forest plot | 7 | 876 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.16 [‐0.29, ‐0.02] |
| 4.1 Kim | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.88 [‐1.37, ‐0.39] |
| 4.2 Other studies | 6 | 806 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.24, 0.05] |
| 5 Anxiety Show forest plot | 4 | 704 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.26, 0.05] |
| 6 Stress Show forest plot | 2 | 206 | Mean Difference (IV, Fixed, 95% CI) | ‐4.76 [‐7.57, ‐1.95] |
| 7 SF‐36 mental health Show forest plot | 5 | 576 | Mean Difference (IV, Fixed, 95% CI) | 5.07 [2.43, 7.72] |
| 7.1 Aglamis study | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 32.9 [23.07, 42.73] |
| 7.2 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 2.90 [0.15, 5.65] |
| 8 SF‐36 emotional role Show forest plot | 5 | 576 | Mean Difference (IV, Random, 95% CI) | 11.43 [‐4.06, 26.91] |
| 8.1 Aglamis | 1 | 25 | Mean Difference (IV, Random, 95% CI) | 72.8 [47.14, 98.46] |
| 8.2 Other studies | 4 | 551 | Mean Difference (IV, Random, 95% CI) | 1.76 [‐6.63, 10.14] |
| 9 SF‐36 social function Show forest plot | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| 9.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 58.30 [34.58, 82.02] |
| 10 SF‐36 vitality Show forest plot | 5 | 1158 | Mean Difference (IV, Fixed, 95% CI) | 6.06 [3.57, 8.54] |
| 10.1 Aglamis | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 51.9 [34.74, 69.06] |
| 10.2 Other studies | 4 | 582 | Mean Difference (IV, Fixed, 95% CI) | 3.90 [0.55, 7.25] |
| 10.3 Other studies | 4 | 551 | Mean Difference (IV, Fixed, 95% CI) | 6.58 [2.78, 10.38] |
| 11 Sleep Show forest plot | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐2.54, 0.34] |

