Калибр иглы и формы наконечников для предотвращения головной боли после дуральной пункции (ГБПДП)
Appendices
Appendix 1. Glossary of terms
| Term | Definition | Source |
| Analgesia, epidural | Relief of pain without loss of consciousness through the introduction of an analgesic agent into the epidural space of the vertebral canal. | |
| Analgesia, obstetric | Elimination of pain, without loss of consciousness, during obstetrical labour; obstetrical delivery; or the postpartum period, usually through the administration of analgesics. | |
| Blood patch, epidural | Injection of autologous blood into the epidural space either as a prophylactic treatment immediately after an epidural puncture or for treatment of headache resulting from an epidural puncture. | |
| Cerebrospinal fluid pressure | Manometric pressure of the cerebrospinal fluid as measured by lumbar, cerebroventricular or cisternal puncture. Within the cranial cavity, it is called intracranial pressure. | |
| Dura mater | The outermost of the three meninges, a fibrous membrane of connective tissue that covers the brain and the spinal cord. | |
| Myelography | X‐ray visualization of the spinal cord after injection of contrast medium into the spinal arachnoid space. | |
| Needle | Sharp instruments used for puncturing or suturing. | |
| Primary prevention | Specific practices for the prevention of disease or mental disorders in susceptible individuals or populations. These include health promotion, including mental health; protective procedures, such as communicable disease control; and monitoring and regulation of environmental pollutants. | |
| Post‐dural puncture headache | A secondary headache disorder attributed to low cerebrospinal fluid pressure caused by spinal puncture, usually after dural or lumbar puncture. | |
| Spinal puncture | Tapping fluid from the subarachnoid space in the lumbar region, usually between the third and fourth lumbar vertebrae. |
Appendix 2. CENTRAL, the Cochrane Library search strategy
#1 MeSH descriptor: [Post‐Dural Puncture Headache] explode all trees
#2 (pdph or plph or pph or post dural or postdural or headach* or cephalea* or cephalalgi*):ti,ab
#3 MeSH descriptor: [Anesthesia, Epidural] explode all trees
#4 MeSH descriptor: [Anesthesia, Spinal] explode all trees
#5 MeSH descriptor: [Injections, Spinal] explode all trees
#6 MeSH descriptor: [Myelography] explode all trees
#7 MeSH descriptor: [Spinal Puncture] explode all trees
#8 (#1 or #2) and (#3 or #4 or #5 or #6 or #7)
#9 ((spinal or intraspinal or dural or intradural or epidural or lumbar* or thecal* or intrathecal or sub?arachnoid*) near (puncture* or inject* or anesth* or anaesth* or needle* or tap)):ti,ab
#10 #8 or #9
#11 (caliber or needle gauge* or needle tip* or needle size* or traumatic tap* or traumatic needle* or atraumatic needle* or pencil point* or diamond tip* or spinal needle* or ((quincke or greene or hingson or lutz or brace or rovenstine or lemmon or whitacre or atraucan or sprotte or cappe or gertie marx or deutsch) and (needle*))):ti,ab
#12 #10 and #11
Appendix 3. MEDLINE (PubMed) search strategy
(Post‐Dural Puncture Headache[Mesh] OR PDPH[tiab] OR PLPH[tiab] OR PPH[tiab] OR Post dural[tiab] OR Postdural[tiab] OR Headache[Mesh] OR Headach*[tiab] OR cephalea*[tiab] OR cephalalgi*[tiab]) AND (Anesthesia, Epidural[Mesh] OR Anesthesia, Spinal[Mesh] OR Injections, Spinal[Mesh] OR Myelography[Mesh] OR Spinal Puncture[Mesh] OR ((spinal[tiab] OR intraspinal[tiab] OR dural[tiab] OR intradural[tiab] OR epidural[tiab] OR lumbar*[tiab] OR thecal*[tiab] OR intrathecal[tiab] OR subarachnoid*[tiab] OR sub arachnoid*[tiab]) AND (Spinal Puncture[Mesh] OR puncture*[tiab] OR inject*[tiab] OR anesth*[tiab] OR anaesth*[tiab] OR needle*[tiab] OR Tap[tiab]))) AND (caliber[tiab] OR Needle Gauge*[tiab] OR Needle Tip*[tiab] OR Needle size*[tiab] OR Traumatic Tap*[tiab] OR Traumatic Needle*[tiab] OR Atraumatic Needle*[tiab] OR Pencil Point*[tiab] OR Diamond Tip*[tiab] OR Spinal Needle*[tiab] OR ((Quincke[tiab] OR Greene[tiab] OR Hingson[tiab] OR Lutz[tiab] OR Brace[tiab] OR Rovenstine[tiab] OR Lemmon[tiab] OR Whitacre[tiab] OR Atraucan[tiab] OR Sprotte[tiab] OR Cappe[tiab] OR Gertie Marx[tiab] OR Deutsch[tiab]) AND (Needle*[tiab])))
Appendix 4. EMBASE (Ovid SP) search strategy
1. (postdural puncture headache/ or pdph.ti,ab. or plph.ti,ab. or pph.ti,ab. or post dural.ti,ab. or postdural.ti,ab. or headache/ or headach*.ti,ab. or cephalea*.ti,ab. or cephalalgi*.ti,ab.) and (epidural anesthesia/ or spinal anesthesia/ or intraspinal drug administration/ or myelography/ or puncture/ or ((spinal or intraspinal or dural or intradural or epidural or lumbar* or thecal* or intrathecal or sub?arachnoid*) and (puncture* or inject* or anesth* or anaesth* or needle* or tap)).ti,ab.) and (caliber or needle gauge* or needle tip* or needle size* or traumatic tap* or traumatic needle* or atraumatic needle* or pencil point* or diamond tip* or spinal needle* or ((quincke or greene or hingson or lutz or brace or rovenstine or lemmon or whitacre or atraucan or sprotte or cappe or gertie marx or deutsch) and needle*)).ti,ab.
Appendix 5. CINAHL (EBSCOhost) search strategy
S1. ( (MM "Anesthesia, Epidural") OR (MM "Analgesia, Epidural") OR (MM "Anesthesia, Spinal") OR (MM "Injections, Intraspinal+") OR (MM "Myelography") OR (MH "Spinal Puncture") ) AND ( (MH "Headache") OR TI ( pdph or plph or pph or post dural or postdural or headach* or cephalea* or cephalalgi* ) OR AB ( pdph or plph or pph or post dural or postdural or headach* or cephalea* or cephalalgi* ) )
S2. TI ( (spinal or intraspinal or dural or intradural or epidural or lumbar* or thecal* or intrathecal or subarachnoid* or sub arachnoid*) and (puncture* or inject* or anesth* or anaesth* or needle* or tap) ) OR AB ( (spinal or intraspinal or dural or intradural or epidural or lumbar* or thecal* or intrathecal or subarachnoid* or sub arachnoid*) and (puncture* or inject* or anesth* or anaesth* or needle* or tap) )
S3. S1 OR S2
S4. TI ( (caliber or needle gauge* or needle tip* or needle size* or traumatic tap* or traumatic needle* or atraumatic needle* or pencil point* or diamond tip* or spinal needle* or ((quincke or greene or hingson or lutz or brace or rovenstine or lemmon or whitacre or atraucan or sprotte or cappe or gertie marx or deutsch) and (needle*))) ) OR AB ( (caliber or needle gauge* or needle tip* or needle size* or traumatic tap* or traumatic needle* or atraumatic needle* or pencil point* or diamond tip* or spinal needle* or ((quincke or greene or hingson or lutz or brace or rovenstine or lemmon or whitacre or atraucan or sprotte or cappe or gertie marx or deutsch) and (needle*))) )
S5. S3 AND S4
Appendix 6. LILACS (BIREME) search strategy
((pdph or plph or pph or post dural or postdural or headach$ or cephalea$ or cephalalgi$) and (epidural or spinal anesthesia or spinal injections or myelography or spinal puncture)) or ((spinal or intraspinal or dural or intradural or epidural or lumbar$ or thecal$ or intrathecal or subarachnoid$ or sub arachnoid$) and (puncture$ or inject$ or anesth$ or anaesth$ or needle$ or tap)) [Words] and (caliber or needle gauge$ or needle tip$ or needle size$ or traumatic tap$ or traumatic needle$ or atraumatic needle$ or pencil point$ or diamond tip$ or spinal needle$ or ((quincke or greene or hingson or lutz or brace or rovenstine or lemmon or whitacre or atraucan or sprotte or cappe or gertie marx or deutsch) and (needle$)))
Appendix 7. Study eligibility screening and data extraction form
Needle Gauge and Tip designs for Preventing PDPH — Intervention Cochrane Review
Study Selection, Quality Assessment & Data Extraction Form
| First Author | Journal/Conference proceedings, etc | Year |
|
|
|
|
1. Study Eligibility
|
| RCT/CCT | Relevant participants | Relevant interventions | Relevant outcomes* |
| Yes |
|
|
|
|
| No |
|
|
|
|
| Unclear |
|
|
|
|
aIssues related to selective reporting when authors may have taken measurements for particular outcomes but did not report these within the paper(s). Review authors should contact trialists for information on possible non‐reported outcomes and reasons for exclusion from publication. Study should be listed in 'Studies awaiting assessment' until clarified. If no clarification is received after three attempts, study should then be excluded.
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
Do not proceed if any of the above answers is "No".
2. References to Trial
Check other references identified in searches. If further references to this trial are identified, link the papers and list below. All references to a trial should be linked under one Study ID in RevMan.
| Author | Journal/Conference proceedings, etc | Year |
|
|
|
|
3. Participant and Trial Characteristics
|
| Further details |
| Age, years (mean, median, range, etc.) |
|
| Gender of participants |
|
| Country |
|
| Reason for puncture (dx, anaesthesia, radiology) |
|
| Surgical procedure (obstetrical, orthopaedic, etc.) |
|
| Type of anaesthesia used |
|
| Trial design (parallel, etc.) |
|
| Single centre/multi‐centre |
|
| Eligibility criteria |
|
| Exclusion criteria |
|
| Follow‐up, years (mean, median, range, etc.) |
|
| Time points reported in the study |
|
| Other |
|
4. Intervention Characteristics
|
| Further details |
| Needle tip |
|
| Needle gauge |
|
| Number of attempts |
|
5. Number of Participants
|
| Enrolled participants | Randomly assigned participants | Participants included in analysis | Lost to follow‐up | Reasons |
| At beginning |
|
|
|
|
|
| A Group |
|
|
|
|
|
| B Group |
|
|
|
|
|
| C Group |
|
|
|
|
|
| D Group |
|
|
|
|
|
6. Methodological Quality
|
| Low risk of bias | Unclear risk of bias | High risk of bias | Details |
| Random sequence generation |
|
|
|
|
| Allocation concealment |
|
|
|
|
| Blinding of participants and personnel |
|
|
|
|
| Blinding of outcome assessment |
|
|
|
|
| Selective reporting bias |
|
|
|
|
| Incomplete outcome data |
|
|
|
|
| Other bias |
|
|
|
|
| Withdrawals |
|
|
|
|
| Other (describe) |
|
|
|
|
7. Results
|
| A Group (define) |
| B Group (define) |
|
|
| # Participants with outcome | # Participants analysed | # Participants with outcome | # Participants analysed |
| PDPH |
|
|
|
|
| Severe PDPH (define) |
|
|
|
|
| Any headache after spinal anaesthesia |
|
|
|
|
| Other (define) |
|
|
|
|

Study flow diagram

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Traumatic needle versus atraumatic needle, outcome: 1.1 PDPH by indication.

Funnel plot of comparison: 1 Traumatic needle versus atraumatic needle, outcome: 1.1 PDPH by indication.

Funnel plot of comparison: 3 Atraumatic needles: different gauges, outcome: 3.1 PDPH major gauge versus minor gauge by number.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 1 PDPH by indication.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 2 PDPH by gauge.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 3 PDPH by gender.
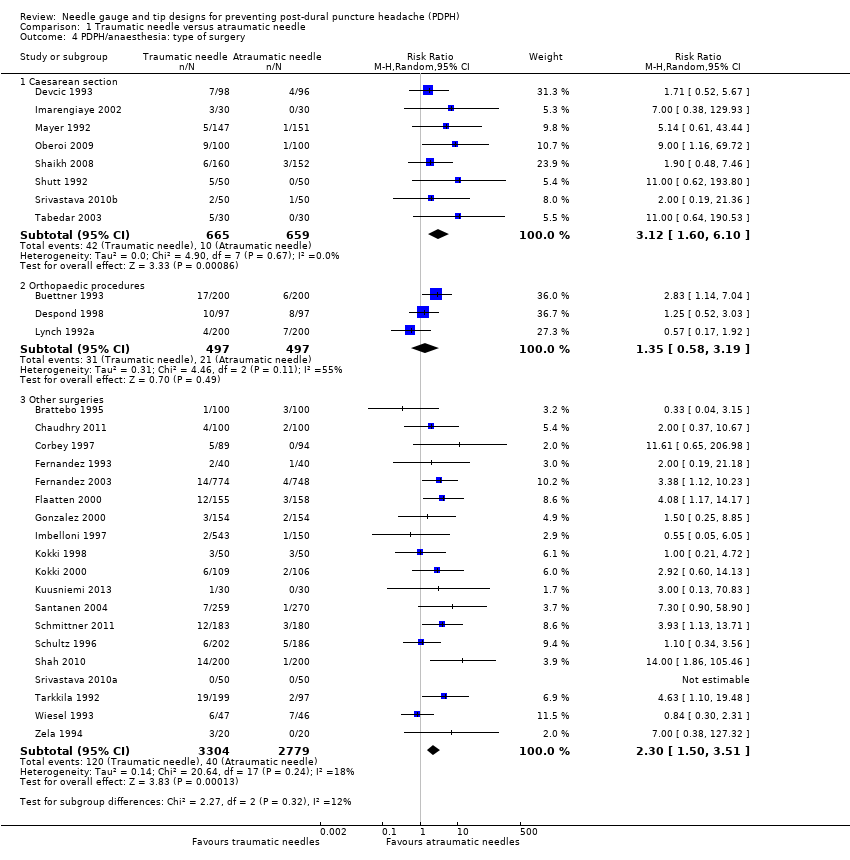
Comparison 1 Traumatic needle versus atraumatic needle, Outcome 4 PDPH/anaesthesia: type of surgery.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 5 PDPH by position.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 6 PDPH by age.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 7 AE: paraesthesia.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 8 AE: backache.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 9 Severe PDPH by indication.
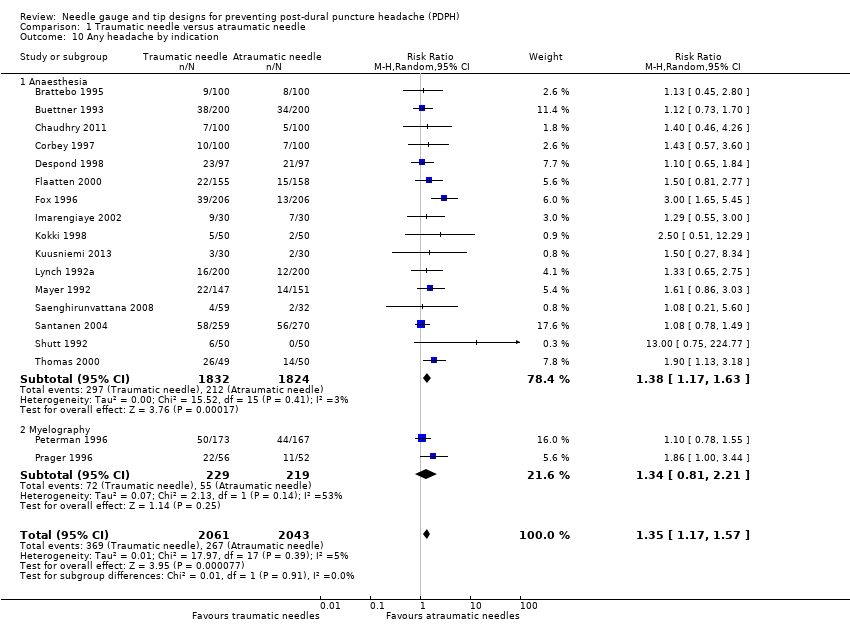
Comparison 1 Traumatic needle versus atraumatic needle, Outcome 10 Any headache by indication.

Comparison 1 Traumatic needle versus atraumatic needle, Outcome 11 PDPH sensitivity analysis.

Comparison 2 Larger gauge traumatic needles versus smaller gauge traumatic needles, Outcome 1 PDPH larger gauge vs smaller gauge.

Comparison 2 Larger gauge traumatic needles versus smaller gauge traumatic needles, Outcome 2 PDPH by type of surgery.

Comparison 2 Larger gauge traumatic needles versus smaller gauge traumatic needles, Outcome 3 PDPH by age.

Comparison 2 Larger gauge traumatic needles versus smaller gauge traumatic needles, Outcome 4 PDPH by position.

Comparison 2 Larger gauge traumatic needles versus smaller gauge traumatic needles, Outcome 5 AE: backache.
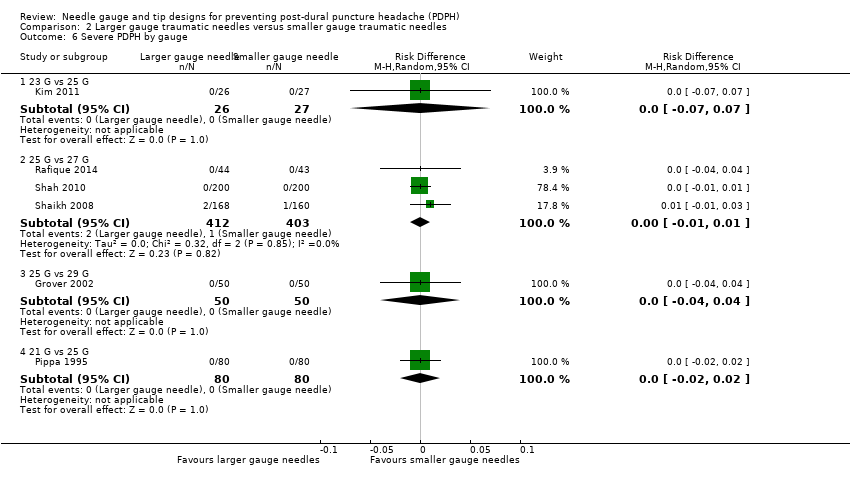
Comparison 2 Larger gauge traumatic needles versus smaller gauge traumatic needles, Outcome 6 Severe PDPH by gauge.

Comparison 2 Larger gauge traumatic needles versus smaller gauge traumatic needles, Outcome 7 Any headache.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 1 PDPH larger gauge vs smaller gauge.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 2 PDPH by type of surgery.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 3 PDPH by gender.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 4 PDPH by position.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 5 AE: paraesthesia.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 6 AE: backache.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 7 Severe PDPH by gauge.

Comparison 3 Larger gauge atraumatic needles versus smaller gauge atraumatic needles, Outcome 8 Any headache by gauge.
| Traumatic needles compared to atraumatic needles for prevention of PDPH | ||||||
| Patient or population: patients undergoing lumbar punctures | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Atraumatic needles | Traumatic needles | |||||
| Onset of PDPH | 30 per 1000 | 64 per 1000 | RR 2.14 | 9378 | ⊕⊕⊕⊝ | — |
| Adverse events: paraesthesia | 52 per 1000 | 50 per 1000 | RR 0.96 | 573 | ⊕⊕⊕⊝ | — |
| Adverse events: backache | 155 per 1000 | 147 per 1000 | RR 0.94 | 3027 | ⊕⊕⊕⊝ | — |
| Severe PDPH | 0 per 1000 | 10 per 1000 | RD 0 | 6420 | ⊕⊕⊝⊝ | — |
| Any headache | 221 per 1000 | 290 per 1000 | RR 1.35 | 4104 | ⊕⊕⊕⊝ | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Risk of bias downgraded by one level due to unclear reporting (especially related to allocation concealment and random sequence generation issues). | ||||||
| Traumatic needle(major gauge) compared to traumatic needle (minor gauge) for prevention of PDPH | ||||||
| Patient or population: patients undergoing lumbar punctures with traumatic needles (Quincke, Greene, Hingson Ferguson, Lutz, Brace, Rovenstine, Lemmon) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Traumatic needle ‐ smaller gauge | Traumatic needle ‐ larger gauge | |||||
| Onset of PDPH | — | — | RR ranged from 0.86 to 6.47 | 2288 | ⊕⊕⊝⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in another. |
| Adverse events: paraesthesia ‐ not reported | See comment | See comment | Not estimable | — | See comment | We did not identify any studies reporting this outcome. |
| Adverse event: backache | — | — | RR ranged | 948 | ⊕⊕⊕⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in another. |
| Severe PDPH | — | — | RD ranged | 1128 | ⊕⊕⊝⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in another. |
| Any headache | — | — | RR ranged | 771 | ⊕⊕⊕⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in another. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Risk of bias downgraded by one level due to unclear reporting (especially related to allocation concealment and random sequence generation issues). 2Imprecision downgraded by one level due to few events reported in each arm. 3Imprecision downgraded by one level due unclear clinical decisions indicated by each confidence interval limit. | ||||||
| Atraumatic needle (major gauge) compared to atraumatic needle (minor gauge) for prevention of PDPH | ||||||
| Patient or population: patients undergoing lumbar punctures with atraumatic needles (Whitacre, Atraucan, Sprotte, Cappe‐Deutsh, Pajunk, Gertie Marx, Durasafe, Cappe, Deutsch and Eldor) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Atraumatic needle ‐ smaller gauge | Atraumatic needle ‐ larger gauge | |||||
| Onset of PDPH | — | — | RR ranged from 0.38 to 9.3 | 3134 | ⊕⊕⊝⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in other. |
| Adverse events: paraesthesia | — | — | RR ranged from 1.03 to 7.61 | 439 | ⊕⊕⊕⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in other. |
| Adverse events: backache | — | — | RR ranged | 526 | ⊕⊕⊕⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in other. |
| Severe PDPH | — | — | RD ranged | 1983 | ⊕⊕⊝⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in other. |
| Any headache | — | — | RR ranged | 1791 | ⊕⊕⊕⊝ | We decided against overall pooling of results because the gauge of a needle could be considered small in one comparison but large in other. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Risk of bias downgraded by one level due to unclear reporting (especially related to allocation concealment and random sequence generation issues). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PDPH by indication Show forest plot | 36 | 9378 | Risk Ratio (M‐H, Random, 95% CI) | 2.14 [1.72, 2.67] |
| 1.1 Anaesthesia only | 30 | 8401 | Risk Ratio (M‐H, Random, 95% CI) | 2.21 [1.60, 3.04] |
| 1.2 Myelography only | 3 | 548 | Risk Ratio (M‐H, Random, 95% CI) | 2.01 [1.34, 3.00] |
| 1.3 Diagnostic lumbar puncture only | 3 | 429 | Risk Ratio (M‐H, Random, 95% CI) | 2.22 [1.38, 3.58] |
| 2 PDPH by gauge Show forest plot | 20 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 22 gauge | 5 | 877 | Risk Ratio (M‐H, Random, 95% CI) | 2.15 [1.56, 2.97] |
| 2.2 25 gauge | 5 | 1260 | Risk Ratio (M‐H, Random, 95% CI) | 2.48 [1.56, 3.95] |
| 2.3 27 gauge | 11 | 4076 | Risk Ratio (M‐H, Random, 95% CI) | 2.87 [1.81, 4.53] |
| 3 PDPH by gender Show forest plot | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Only women | 9 | 1424 | Risk Ratio (M‐H, Random, 95% CI) | 2.60 [1.62, 4.17] |
| 4 PDPH/anaesthesia: type of surgery Show forest plot | 30 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Caesarean section | 8 | 1324 | Risk Ratio (M‐H, Random, 95% CI) | 3.12 [1.60, 6.10] |
| 4.2 Orthopaedic procedures | 3 | 994 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.58, 3.19] |
| 4.3 Other surgeries | 19 | 6083 | Risk Ratio (M‐H, Random, 95% CI) | 2.30 [1.50, 3.51] |
| 5 PDPH by position Show forest plot | 20 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Lateral position | 9 | 3242 | Risk Ratio (M‐H, Random, 95% CI) | 4.70 [2.39, 9.24] |
| 5.2 Sitting position | 11 | 2193 | Risk Ratio (M‐H, Random, 95% CI) | 2.11 [1.52, 2.94] |
| 6 PDPH by age Show forest plot | 36 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 No distinctions by age | 34 | 9063 | Risk Ratio (M‐H, Random, 95% CI) | 2.17 [1.73, 2.73] |
| 6.2 Only < 18 years | 2 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [0.56, 5.12] |
| 7 AE: paraesthesia Show forest plot | 3 | 573 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.47, 1.96] |
| 8 AE: backache Show forest plot | 12 | 3027 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.78, 1.13] |
| 9 Severe PDPH by indication Show forest plot | 24 | 6420 | Risk Ratio (M‐H, Random, 95% CI) | 1.88 [1.20, 2.94] |
| 9.1 Anesthesia | 19 | 5542 | Risk Ratio (M‐H, Random, 95% CI) | 1.77 [0.88, 3.53] |
| 9.2 Myelography | 4 | 778 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [0.68, 4.28] |
| 9.3 Diagnostic lumbar puncture | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [1.18, 7.63] |
| 10 Any headache by indication Show forest plot | 18 | 4104 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [1.17, 1.57] |
| 10.1 Anaesthesia | 16 | 3656 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [1.17, 1.63] |
| 10.2 Myelography | 2 | 448 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.81, 2.21] |
| 11 PDPH sensitivity analysis Show forest plot | 3 | 802 | Risk Ratio (M‐H, Random, 95% CI) | 2.78 [1.26, 6.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PDPH larger gauge vs smaller gauge Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 23 G vs 25 G | 1 | 53 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [0.20, 21.55] |
| 1.2 25 G vs 27 G | 4 | 1041 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.98, 3.39] |
| 1.3 25 G vs 29 G | 3 | 376 | Risk Ratio (M‐H, Random, 95% CI) | 2.13 [0.46, 9.78] |
| 1.4 26 G vs 27 G | 1 | 658 | Risk Ratio (M‐H, Random, 95% CI) | 6.47 [2.55, 16.43] |
| 1.5 21 G vs 25 G | 1 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.30, 2.44] |
| 2 PDPH by type of surgery Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Caesarean section | 2 | 455 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.64, 2.57] |
| 2.2 Orthopaedic surgeries | 2 | 213 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.38, 2.58] |
| 2.3 Other surgeries | 6 | 1620 | Risk Ratio (M‐H, Random, 95% CI) | 2.94 [1.23, 7.03] |
| 3 PDPH by age Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 No distinctions about age | 8 | 2175 | Risk Ratio (M‐H, Random, 95% CI) | 2.09 [1.11, 3.95] |
| 3.2 Only children | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.13, 70.83] |
| 3.3 Only > 60 years | 1 | 53 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [0.20, 21.55] |
| 4 PDPH by position Show forest plot | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Lateral position | 5 | 859 | Risk Ratio (M‐H, Random, 95% CI) | 1.76 [0.98, 3.16] |
| 4.2 Sitting position | 2 | 584 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.64, 1.56] |
| 5 AE: backache Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6 Severe PDPH by gauge Show forest plot | 6 | Risk Difference (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 23 G vs 25 G | 1 | 53 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.07, 0.07] |
| 6.2 25 G vs 27 G | 3 | 815 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.01, 0.01] |
| 6.3 25 G vs 29 G | 1 | 100 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.04, 0.04] |
| 6.4 21 G vs 25 G | 1 | 160 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.02, 0.02] |
| 7 Any headache Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PDPH larger gauge vs smaller gauge Show forest plot | 13 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 22 G vs 24 G | 1 | 375 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.20, 4.81] |
| 1.2 22 G vs 25 G | 2 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.32, 28.50] |
| 1.3 24 G vs 25 G | 2 | 647 | Risk Ratio (M‐H, Random, 95% CI) | 5.62 [1.00, 31.67] |
| 1.4 25 G vs 26 G | 3 | 519 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.30, 1.90] |
| 1.5 25 G vs 27 G | 2 | 612 | Risk Ratio (M‐H, Random, 95% CI) | 3.72 [0.59, 23.64] |
| 1.6 26 G vs 27 G | 2 | 258 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.30, 10.73] |
| 1.7 27 G vs 29 G | 1 | 389 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.58, 4.37] |
| 2 PDPH by type of surgery Show forest plot | 13 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Caesarean section | 6 | 1263 | Risk Ratio (M‐H, Random, 95% CI) | 1.92 [0.64, 5.79] |
| 2.2 Orthopaedic procedures | 2 | 392 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.30, 5.07] |
| 2.3 Other surgeries | 5 | 1479 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.73, 2.83] |
| 3 PDPH by gender Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Only women | 8 | 1853 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.51, 2.20] |
| 4 PDPH by position Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Sitting position | 5 | 1106 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.45, 2.06] |
| 4.2 Lateral position | 5 | 992 | Risk Ratio (M‐H, Random, 95% CI) | 1.88 [0.65, 5.41] |
| 5 AE: paraesthesia Show forest plot | 2 | 439 | Risk Ratio (M‐H, Random, 95% CI) | 2.19 [0.31, 15.30] |
| 6 AE: backache Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7 Severe PDPH by gauge Show forest plot | 8 | Risk Difference (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 22 G vs 24 G | 1 | 375 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.01, 0.01] |
| 7.2 22 G vs 25 G | 1 | 234 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.02, 0.02] |
| 7.3 24 G vs 25 G | 1 | 304 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.02, 0.03] |
| 7.4 25 G vs 26 G | 2 | 311 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.01, 0.03] |
| 7.5 25 G vs 27 G | 1 | 212 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.02, 0.04] |
| 7.6 26 G vs 27 G | 1 | 158 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.02, 0.02] |
| 7.7 27 G vs 29 G | 1 | 389 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [‐0.01, 0.01] |
| 8 Any headache by gauge Show forest plot | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 22 G vs 25 G | 1 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 2.17 [0.85, 5.51] |
| 8.2 24 G vs 25 G | 2 | 645 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.49, 2.77] |
| 8.3 25 G vs 26 G | 2 | 311 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.65, 1.99] |
| 8.4 25 G vs 27 G | 1 | 212 | Risk Ratio (M‐H, Random, 95% CI) | 1.87 [0.65, 5.39] |
| 8.5 27 G vs 29 G | 1 | 389 | Risk Ratio (M‐H, Random, 95% CI) | 1.80 [0.85, 3.83] |

