Групповые психосоциальные вмешательства для улучшения психологического благополучия у взрослых людей с ВИЧ
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Trial design: 2‐arm randomized controlled trial (RCT) Follow‐up: 3, 9, and 15 months follow up Loss to follow‐up: 22 in treatment group, 23 in control group | |
| Participants | Population: 130 HIV‐positive homosexual men receiving highly active antiretroviral therapy (HAART); intervention = 76, control = 54 Inclusion criteria: 18 to 65 years old, no changes in their HAART regime during past month Exclusion criteria: prescribed medications with immunomodulatory effects, history of chemotherapy or whole‐body radiation for cancer that was not AIDS‐related, history of chronic illness associated with permanent changes in immune system | |
| Interventions | Intervention: N = 76. Cognitive Behavioural Stress Management (CBSM): focused on eliciting participant experiences with adherence and medication side effects using cognitive restructuring exercises, managing stressors related to adherence, using productive coping responses.
Control: N = 54. Medication adherence training (MAT): aimed to increase knowledge about HIV and HAART, including how medications work, why they must be taken on time and at the proper dose, and how to recognize possible side effects
| |
| Outcomes | Included in this review
Not included in this review
| |
| Notes | Used 2 scales to measure depression POMS‐D and BDI; we chose BDI Setting: not reported Country: USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants identification numbers were drawn randomly from a box for assignment to trial conditions." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization procedures were conducted by a master’s level project manager and overseen by the principal investigator. Participants identification numbers were drawn randomly from a box for assignment to trial conditions." No further details. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Loss to follow‐up: 19.7% intervention group versus 25.9% control. Intention‐to‐treat (ITT) analysis done. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 2‐arm RCT Follow‐up: 9‐month follow‐up Loss to follow‐up: Cognitive Behavioral Stess Management (CBSM) group: 47% completed follow‐up; control participants: 69% completed follow‐up | |
| Participants | Population: 39 HIV‐positive African American, Hispanic, or Caribbean women. Intervention = 21, control = 18. Inclusion criteria: HIV‐positive women aged 18 to 60 years old; at least 2 Papanicolaou smears indicating low grade squamous intraepithelial lesions (LSIL) or al least 2 cervical biopsies indication CIN 1 (mild or grade 1 neoplasia) in the 2 years prior to trial entry; fluency in spoken English. Exclusion criteria: no exclusion criteria were listed. | |
| Interventions | Treatment: N = 21. Cognitive behavioural training (CBT) that increased awareness of the effects of stress, identifying and reframing automatic thoughts, improving productive coping skills, anger management, assertiveness training, productive use of one's social network, and safer sex negotiation.
Control: N = 18. 5‐hour 1‐day CBSM workshop with four 20‐minute relaxation modules, four 40‐minute CBSM modules, and two 30‐minute breaks. | |
| Outcomes | Included in this review
Not included in this review
| |
| Notes | Jensen 2013 did secondary analysis on psychological well‐being but only used a subset of Beck Depression Inventory (BDI) Setting: not reported Country: USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned to either the 10‐week CBSM group intervention or the one‐day CBSM workshop at a 2:1 ratio (experimental:control)". No further details. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Participants and assessors were blinded to experimental condition during completion of all study entry procedures". No further details. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Loss to follow‐up: 43.2% intervention group versus 21.7% control. Trial authors conducted an ITT analysis. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 2‐arm RCT Follow‐up: 12 months Loss to follow‐up: intervention loss n = 2; treatment loss n = 4 | |
| Participants | Population: 104 HIV‐positive people taking combination antiretroviral therapy (ART), intervention = 53, control = 51. Inclusion criteria: adults between 18 to 65 years, German speaking, received combination Antiretroviral Therapy (cART) within the 3 months prior to screening, had a CD4 lymphocyte count > 100 cells/µL and no opportunistic infection at baseline. Exclusion criteria: received psychotherapy in past 3 months, intravenous drug users or on stable methadone maintenance, diagnosis of psychiatric disorder as determined by standardized interview. | |
| Interventions | Treatment: N = 53. Psychoeducation, group dynamics exercises, homework, cognitive strategies, and PMR
Control: N = 51. 30‐minute health check by physician. | |
| Outcomes | Included in review
Not included in review
| |
| Notes | Ethics approval. Setting: outpatient clinics Country: Switzerland | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Allocation sequences included randomly permuted block sizes of two and four and were generated using the computer program RANCODE V3.0". |
| Allocation concealment (selection bias) | Low risk | Quote: "Individual assignment codes were properly concealed between black sheets, stored in sequentially numbered envelopes and opened in the presence of study participants". |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 37.7% intervention group versus 25.5% control group.Trial authors conducted an ITT analysis. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: RCT 2 group by 4 time repeated measures design Follow‐up: baseline, 10 weeks, 3 months follow‐up, 22 weeks post follow‐up Loss to follow‐up: 71% completed all trial points | |
| Participants | Population: 93 HIV‐positive adults, intervention = 46, control = 47 Inclusion criteria: HIV‐positive for ≥ 6 months; 18 to 65 years old; no drug or substance abuse for ≥ 6 months; able to read, write, and comprehend English Exclusion criteria: Trial authors did not list any exclusion criteria. | |
| Interventions | Treatment: N = 46. Information on choosing and using a mantram, attention to mindfulness, phone calls to encourage mantram practice.
Control: N = 47. Videotapes on HIV topics including medications, treatment issues, wasting syndrome, and nutrition. Attention control group the same. | |
| Outcomes | Included in review
Not included in review
| |
| Notes | 50% homosexual participants Setting: not reported Country: USA University Institutional Review Board approval | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment was done by the project coordinator using a table of random numbers and stratifying on CD4 count". |
| Allocation concealment (selection bias) | Unclear risk | Trial authors did not describe selection bias. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Trial authors conducted an ITT analysis. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 30.4% intervention group versus 27.7% control group. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Unclear risk | Groups differed on 4 baseline variables; "baseline imbalance". |
| Methods | Trial design: 2‐arm RCT Follow‐up: pre, post, 6 months, and 12 months Loss to follow‐up: 50% followed up in intervention and 47% in control. | |
| Participants | Population: 129 HIV seropositive homosexual men. Intervention = 31, control = 18 Inclusion criteria: have at least 1 non‐AIDS HIV‐related symptom occurring within 3 years of trial entry of laboratory signs of mildly progressed HIV infection, have at least an 8th grade education and ability to read and write in fluent English, CD4 counts > 200 cells/mm³, those on AZT or ART had to have maintained current dosage without change in regimen for at least 2 months before trial entry, those concurrently engaged in psychotherapy or support groups were asked not to change their involvement during the trial Exclusion criteria: individuals with AIDS symptomology, a prior diagnosis of AIDS (CD4 count < 200 cells/mm³), those who had been hospitalized in previous 3 months, those who had a chronic immune system‐related physical condition other than HIV and regular use of medications (other than ARVs) with substantial known effects on the endocrine or immune systems, those with psychiatric or neuropsychological conditions, alcohol or substance abuse dependency, or and major psychiatric and personality disorder, who were cognitively impaired, patients with concurrent clinical levels of depression, individuals who had been bereaved of a significant other within the previous 6 months, risk factors for HIV transmission other than sexual orientation (for example, past or present intravenous drug use, blood transfusion), initiating a new psychotherapy or exercise training programme in past 3 months | |
| Interventions | Treatment: N = 31. CBSM (GET SMART) included increasing awareness of physiological effects of stress, cognitive behavioural theory of stress and emotions, identification of cognitive distortions and automatic thoughts, rational thought replacement, coping skills training, assertiveness training, anger management, and identification and use of social supports. Homework was assigned and participants were taught a variety of relaxation techniques including PMR, autogenic training, meditation and breathing exercises
Control: N = 18. Waitlist, 2 weeks post treatment they were offered a 1 day seminar consisting of condensed CBSM components | |
| Outcomes | Included in review
Not included in review
| |
| Notes | Setting: not reported Country: USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial authors described the trial as "randomized" but did not provide any further details. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe selection biases, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 66.3% intervention group versus 65.2% control group. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 3‐arm RCT Follow‐up: 6 and 12 months Loss to follow‐up: 86% retained | |
| Participants | Population: 149 HIV‐positive men who have sex with men (MSM) and who have depression Inclusion criteria: (1) self‐identified as homosexual or bisexual, (2) 21 to 60 years of age, (3) self‐reported CD4 levels between 200 and 700 cells/mm³ Exclusion criteria: (1) individuals with major depressive or psychotic disorders, (2) history of drug or alcohol dependency in past year, (3) currently in psychotherapy, (4) using psychoactive medication | |
| Interventions | Treatment: N = 54. Coping Effectiveness Training (CET) comprising psychoeducation: appraisal of stressful situations, problem‐focused and emotion‐focused coping, use of social support; skills‐building group activities, relaxation guidance.
Control: N = 51. HIV‐Informational Control comprising Didactic information on HIV‐related topics and resources, workbooks, fact sheets, and reading material. 10 weekly 90‐minute group sessions of 8 to 10 men plus 6 maintenance sessions Waiting list: N = 44. Waiting list control | |
| Outcomes | Included in review
Not included in review
Mediating variables
| |
| Notes | Setting: not reported Country: San Francisco, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial authors described the trial as "randomized" but did not provide any further details. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe selection bias, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Loss to follow‐up: 33.3% intervention versus 33.3% control. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 2‐arm RCT Follow‐up: baseline, 3 month and 6 month follow‐up Loss to follow‐up: 93% 6‐month follow‐up | |
| Participants | Population: 76 participants actively taking ART, intervention = 40, control = 36 Inclusion criteria: (1) documentation of HIV test results, (2) currently taking a recognized ART regimen and (3) reporting a side effect bother in last 30 days of 8 or a bother on the side effect and symptom distress scale. Exclusion criteria: (1) if enrolled in another behavioural coping or HIV adherence intervention research trial or MBSR | |
| Interventions | Treatment: N = 40. Mindfulness‐based stress reduction consisting of daily homework, sitting meditation with mindfulness of breath, thoughts, and emotions, including deliberate awareness of routine activities such as eating and interpersonal communication, and yoga postures
Control: N = 36. Waitlist control group offered the MBSR subsequent to 6 month follow‐up | |
| Outcomes | Included in the review
Not included in the review
| |
| Notes | Setting: not reported Country: USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed in blocks of six using the SAS system’s PLAN procedure". |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe any selection bias. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | Low risk | Losses to follow‐up: 7.5% intervention group versus 5.6% control. |
| Selective reporting (reporting bias) | Low risk | We did not detect any other potential sources of selection reporting bias. |
| Other bias | Low risk | No differences between groups at baseline except for viral load and this was controlled for. |
| Methods | Trial design: 2‐arm follow‐up Follow‐up: baseline, 2 months post, and 6 months follow‐up Loss to follow‐up: 21 participants discontinued the intervention | |
| Participants | Population: 117 homosexual male participants, intervention =78, control = 39 Inclusion criteria: male, aged 18 to 70 years, living within 1 hour of the hospital, and having a diagnosis of HIV Exclusion criteria: (1) subjects with active current major depression, substance abuse, or significant cognitive deficit. | |
| Interventions | Treatment: N = 78. Mindfulness‐Based Stress Reduction (MBSR): participants were taught mindfulness skills geared towards enhancing their awareness of and relation to current experience rather than focusing on the content and reappraisal of thoughts and interpretations of experiences.
Control: N = 39. Treatment as Usual (TAU) group offered at end of intervention | |
| Outcomes | Included in review
Not included in review
| |
| Notes | Homosexual population Ethics reviewed. Setting: hospital Country: Toronto, Canada | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A randomization free‐ware, software program (Network, 1997) was utilized to generate a random allocation sequence 2:1 in favour of the group intervention for each cohort of up to 30 eligible participants". |
| Allocation concealment (selection bias) | Unclear risk | Quote: "study staff were not aware of a potential participant’s group member‐ ship until the whole cohort was assigned at the same time". The trial authors did not provide any further details. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 24.4% intervention group versus 5.1% control. ITT analysis done. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 3‐arm RCT Follow‐up: baseline, post, 4 months, and 8 months follow‐up Loss to follow‐up: 73%; 68%, 82% | |
| Participants | Population: 299 adults, intervention = 84, control = 107 Inclusion: 18 years or older, provision of written consent, a self reported diagnosis of HIV AIDS, and residence in a community of 50,000 people or fewer that was at least 20 miles from a city of 100,000 or more. Exclusion: there were no exclusion related to psychological functioning. | |
| Interventions | Treatment: N = 108. Coping improvement group intervention used cognitive behavioural principles to appraise stressor severity, develop adaptive problem‐ and emotion‐focused coping skills, and optimize coping through the appropriate use of personal and social resources.
Treatment: N = 84. Information Support Group provided information on HIV symptom management, nutrition and HIV, exercise and HIV, and discussions of personal topics.
Control: N = 107. Usual care condition received no intervention but had access to usual services | |
| Outcomes | Included in review
Not included in review
| |
| Notes | Setting: telephone‐delivered Country: USA Groups conducted separately for MSM, heterosexual men, and women 71% reporting moderate to severe depression at baseline. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial authors described the trial as "randomized" but did not provide any further details. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe selection bias, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 18.5 intervention group versus 27.1% control. ITT done. A last‐observation‐carried‐forward (LOCF) approach was used to input missing data. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 3‐arm RCT Follow‐up: baseline, post, 4 months, and 8 months follow‐up Loss to follow‐up: coping group 79% loss, interpersonal support group 69% loss, individual therapy group 86% loss. | |
| Participants | Population: 295 men and women over the age of 50, intervention = 104, control = 105. Inclusion: 50 years or older, a diagnosis of HIV infection or AIDS, a BDI‐II score of 10 or higher, a score of 75 or more on the 3MS, a minimum value of 10 on the BDI‐II. (A minimum value of 10 on the BDI‐II was used to ensure that participants had a minimally elevated number of depressive symptoms that had the potential to be reduced by the interventions). Exclusion: the project did not exclude individuals with alcohol or substance use disorders, active bipolar disorder, psychotic symptoms, or individuals receiving psychotherapy. | |
| Interventions | Treatment: N = 104. Coping improvement group intervention addressed introductions and participants' sharing of personal histories (Session 1 and 2) appraisal and changeability of stressors related to one's HIV infection and stressors related to normal ageing (Sessions 3 and 4); developing and implementing adaptive problem‐ and emotion‐focused coping skills (Sessions 5 through 9); optimizing coping efforts through the use of interpersonal supports (Session 10 and 11); and termination issues and voluntary sharing of personal contact information (Session 12)
Treatment: N = 105. Interpersonal Support Group of 12 x 90‐minute group sessions (5 minutes spent on viewing and discussing videotapes on HIV‐related topics of nutrition, treatment, adherence, sexual risk reduction, 45 minutes spent discussing how the sessions' topic pertained to their personal lives). Facilitators: 2 Masters‐level clinicians Control: N = 86. Individual Therapy Upon Request (ITUR) Group had access to standard psychosocial community‐based services. | |
| Outcomes | Included in review
Not included in the review
| |
| Notes | Setting: community Country: Ohio and New York, USA. Each 90‐minute group conducted separately for MSM, heterosexual men, and women. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial authors described the trial as "randomized" but did not provide any further details. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe selection bias, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 15.4% intervention group versus 31.4% control. |
| Selective reporting (reporting bias) | Low risk | We did not detect any selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 2‐arm RCT Follow‐up: pre, post, 12 months Loss to follow‐up: not reported. | |
| Participants | Population: 451 minority women, intervention = 212, control = 239 Inclusion: 18 years and older, meet the CDC classification for case‐defined AIDS (i.e. CD4+ cell count below 200/mm² and/or one opportunistic infection, CDC 1993), have at least 6th grade education Exclusion: women with psychiatric, neuropsychiatric or medical conditions were temporarily excluded pending treatment. | |
| Interventions | Treatment: N = 212. Cognitive Behavioural Stress Management: sessions included didactic components on the physiological effects of stress, cognitive behavioural interpretation of stress and emotions, identification of cognitive distortions and automatic thoughts, rational thought replacement, coping skills training, assertiveness training, anger management, and identification of social support.
Control: N = 239. Individual 120‐minute information education sessions delivered by videotape covering stress management, relaxation, and coping with HIV. 10 sessions | |
| Outcomes | Included in this review
Not included in this review
| |
| Notes | Setting: medical school setting and community health centres Country: USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial used a table of random numbers to randomize participants to treatment. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe selection bias, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 45.1% intervention group versus 36.9% control. |
| Selective reporting (reporting bias) | Low risk | We did not detect any potential source of selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 3‐arm RCT Follow‐up: pre, post, and 6 months Loss to follow‐up: 69% follow‐up at 6 months | |
| Participants | Population: 148 individuals diagnosed with HIV disease (119 men, 29 women). Intervention = 59, support group = 3, Waitlist = 36 Inclusion: (1) 18 years of age, (2) able to read and speak English, (3) previously aware of their HIV diagnosis, (4) deemed capable of attending intervention sessions and completing 6 months follow‐up. Exclusion: (1) no significant psychiatric illness, (2) no cognitive impairment, (3) not pregnant or taking steroids. | |
| Interventions | Treatment 1: N = 59. CBSM focused on breathing, PMR, yoga‐form stretching, guided imagery, and beginning meditation, along with cognitive restructuring techniques and active coping skills.
Treatment 2: N = 43. SSG focused on facilitating communication related emotional issues, problem‐solving and cognitive‐reframing techniques, and individual and group empowerment
Control: N = 36. Waitlist group | |
| Outcomes | Included in this review
Not included in this review
| |
| Notes | Setting: Trial authors did not describe the setting. Country: USA Separate gender groups, interaction terms included by group by gender | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Quota sampling was used to achieve appropriate sample representation by gender, at a ratio of 4 males:1 female (20%)". The trial authors did not provide any further details. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe selection bias, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 27.1% intervention group versus 27.8% control. |
| Selective reporting (reporting bias) | Low risk | We did not detect any potential source of selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 2‐arm RCT Follow‐up: baseline, immediately post, 6 months follow‐up Loss to follow‐up: 23% in intervention group, 21% lost in control group | |
| Participants | Population: 109 HIV‐positive individuals (peasant farmers) with major depression, intervention = 57, control = 52 Inclusion: 19 years or older, met the MINI International Neuropsychiatric Interview criteria for major depression, from an urban HIV care centre, were antidepressant naive Exclusion: individuals with severe medical disorder such as pneumonia or active tuberculosis, psychotic symptoms, and hearing or visual impairment | |
| Interventions | Treatment: N = 57. Group Support Psychotherapy (GSP) is a culturally sensitive intervention that aims to treat depression by enhancing social support, teaching coping skills and income generating skills
Control: N=52. Active treatment group receives Group HIV education (GHE) immediately post intervention and 6 months later. | |
| Outcomes | Included in the review
Not included in review
| |
| Notes | Setting: HIV care centre, urban Country: Uganda Gender‐specific groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial authors performed randomization by urn with a ratio of 1:1. The trial authors did not provide any further details or properties of this method. |
| Allocation concealment (selection bias) | Unclear risk | Men and women separately picked a paper containing the intervention allocation from a basket, ratio. The trial authors did not provide further details on allocation concealment. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 22.8% intervention group versus 21.2% control. |
| Selective reporting (reporting bias) | Low risk | We did not detect any potential source of selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 2 arm RCT Follow‐up: baseline, 1 month, 4 months Loss to follow‐up: 147 follow‐up (96.7% follow‐up); 3.9% attrition in MAI and 2.6% attrition in SC | |
| Participants | Population: 152 HIV‐positive individuals on ART with an adherence problem, intervention = 76, control = 72 Inclusion: 18 years or older, new ARV medication users (2 to 24 months of ARV use) Exclusion: Trial authors did not describe any exclusion criteria. | |
| Interventions | Treatment: N = 76. Medication adherence intervention (MAI) is medication information combined with problem‐solving skills in an experiential/interactive group format.
Control: N = 76. Practitioner medical directive (standard of care; 20 min) led by medical physician. Patients individually attended monthly 1 visit to review their health status with their medical practitioner. | |
| Outcomes | Included in this review
Not included in this review
| |
| Notes | Setting: hospital Country: South Africa. Short follow‐up of 3 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized into study condition using a table of random numbers following their baseline assessment". |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe any selection bias, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | Low risk | Losses to follow‐up: 3.9% intervention group versus 2.6% control. Trial authors performed an intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | We did not detect any potential source of selective reporting bias. |
| Other bias | Low risk | We did not detect any other sources of bias. |
| Methods | Trial design: 2‐arm RCT Follow‐up: 3 months, 6 months and 12 months Loss to follow‐up: 84% follow‐up to at least one follow‐up assessment | |
| Participants | Population: 89 HIV individuals prescribed ARVS and with a history of injection drug use, intervention = 44, control = 45 Inclusion: aged 18 to 65 years, HIV‐positive, prescribed ARVs, endorsed history of injection drug use, currently enrolled in opoid treatment for at least one month, and met criteria for a diagnosis of current or subsyndromal depressive mood disorder Exclusion: individuals with any active untreated or unstable major mental illness, inability or unwillingness to provide informed consent, or current participation in a CBT for depression. | |
| Interventions | Treatment: N = 44. CBT‐AD included Life Steps, psychoeducation about HIV and depression, motivational interviewing for behaviour change, behavioural activation to increase pleasurable activities, training in adaptive thinking, problem solving, PMR, and diaphragmatic breathing.
Control: N = 45. Enhanced Treatment As Usual (ETAU) with a letter to medical provider documenting participants depression and suggesting continued assessment and treatment. Both treatment conditions received a single‐session intervention on medication adherence (Life Steps) with involved 11 informational, problem‐solving and cognitive‐behavioural steps. | |
| Outcomes | Included in this review
Not included in this review
| |
| Notes | Setting: methadone clinics Country: Boston, USA | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "Random assignment in block of 2 ‐ stratified by sex, depression severity and adherence". The trial authors did not provide any further details. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Assignment to study condition (CBT‐AD or ETAU) was concealed from both study therapists and participants until the conclusion of the first counseling visit (see below)". The trial authors did not provide any further details. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Low risk | An independent assessor who was blinded to the trial conditions assessed depression. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 18.2% intervention group versus 33.3% control. |
| Selective reporting (reporting bias) | Low risk | We did not detect any potential sources of selective reporting bias. |
| Other bias | Unclear risk | Small sample size of 89. CD4 count differed at baseline but controlled for in analysis |
| Methods | Trial design: 3‐arm RCT Follow‐up: baseline, post, 4, 8, 12 months Loss to follow‐up: minimal loss to follow‐up, ITT analysis done | |
| Participants | Population: 247 HIV‐positive men (N = 117) and women (N = 130), intervention = 124, control = 123 Inclusion: sexual abuse as a child (age 12 and under) and/or adolescent (age 13 to 17 years); current age of 18 or older; HIV serostatus Exclusion: acute distress due to sexual revictimization experienced within past month; presence of impaired mental status; extreme distress or depressive symptomatology | |
| Interventions | Treatment 1: N= 124. HIV and Trauma Coping Group Intervention (LIFT) where participants Identify stressors that they perceived to be related to their sexual abuse experiences and those related to their HIV diagnosis, learn adaptive coping and risk reduction skills related to both sexual abuse and HIV infection.
Control: N = 123. HIV standard therapeutic support group. The comparison intervention paralleled a standard therapeutic support group and was led by experienced co‐therapists not trained on the coping intervention model. The purpose of the group was to provide a supportive environment for participants to address issues of HIV and trauma. | |
| Outcomes | Included in this review
Not included in this review
| |
| Notes | Setting: Community Health Centre Country: USA Different populations in each report | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial authors described the trial as 'randomized' but did not provide any further details. |
| Allocation concealment (selection bias) | Unclear risk | The trial authors did not describe the method of allocation concealment, if any. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The trial authors did not describe the method of blinding, if any. |
| Incomplete outcome data (attrition bias) | High risk | Losses to follow‐up: 16.5% Intervention group versus 33.3% control. The trial authors conducted an intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | We did not detect any other sources of selective reporting bias. |
| Other bias | Low risk | We did not detect any other potential sources of bias. |
Abbreviations: HAART: highly active antiretroviral therapy; PMR: progressive muscle relaxation; RCT: randomized controlled trial.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| No 3‐month follow‐up post intervention. | |
| Individual psychoeducational intervention, not a group intervention. | |
| No specified outcomes reported. The study measured salivary cortisol as a biomarker of immune function. | |
| Individual counselling sessions, not a group intervention. | |
| No 3‐month follow‐up postintervention. | |
| Not a group‐based intervention. | |
| No specified outcomes measured. | |
| No 3‐month follow‐up postintervention. | |
| No 3‐month follow‐up postintervention. | |
| Nurse‐patient intervention, not a group intervention. | |
| Overview of intervention, not a randomized controlled trial (RCT). | |
| Only formative qualitative data presented, not a RCT. | |
| We contacted the study author. This was not a group intervention. | |
| Individual therapy for patient‐partner dyads. This was not a group intervention. | |
| No 3‐month follow‐up postintervention, only 3‐month follow‐up after baseline. | |
| Individual, not a group intervention. | |
| No specified outcomes. | |
| No 3‐month postintervention follow‐up. | |
| No specified outcomes included. | |
| No RCT result reported, only baseline data reported. | |
| No post 3‐month follow‐up. | |
| Not a group intervention. | |
| Measured positive affect and positive mood. These are not specified outcomes. | |
| Not a RCT as no control group. | |
| No 3‐month follow‐up postintervention. | |
| Describes intervention development and components, not a RCT. | |
| Nurse‐patient intervention, not a group intervention. | |
| Treatment supporter intervention, not a group intervention. | |
| The study author presented a subgroup analysis only, a subgroup from the larger Jones 2010 study. | |
| Not a HIV‐positive population. | |
| No 3‐month follow‐up postintervention. | |
| Not a RCT and no control group. | |
| Not a group intervention. | |
| Not a group intervention. | |
| No specified outcomes reported. | |
| Interpersonal therapy, not a group intervention. | |
| Not truly randomized. | |
| Not a RCT, quasi‐experimental. | |
| No 3‐month follow‐up postintervention. | |
| No RCT reported. | |
| Individual therapy, not a group intervention. | |
| Not a group intervention. | |
| No specified outcomes reported. | |
| No 3‐month follow‐up postintervention. | |
| Adolescents 12 to 17 years old. | |
| No RCT reported. | |
| Individual art therapy sessions, not a group intervention. | |
| No RCT reported. | |
| No 3‐month follow‐up postintervention, small sample size (N = 30), and unsure whether a group intervention. | |
| Not a group intervention. The intervention was individually administered to each couple. | |
| No 3‐months follow‐up postintervention. | |
| One‐to‐one intervention by lay health workers, not a group intervention. | |
| Study protocol only. No RCT data reported. | |
| No specified outcomes. | |
| Both individual and group formats to intervention. No effects reported for group components of intervention. | |
| Control invited to cross over to intervention at 3‐months postintervention. No postintervention follow‐up of 3 months for control group. | |
| Measured coping using 3 subscales of Coping Scale. | |
| No specified outcomes. Used global score of broad range of psychological symptoms, did not measure depression and anxiety outcomes separately. | |
| No 3‐month follow‐up postintervention. | |
| Not a group‐based intervention. | |
| Content analysis, no RCT reported. | |
| Therapy sessions with family at home. | |
| Individually administered intervention, not a group intervention. | |
| Not a group intervention but home‐based individual intervention. | |
| Inconsistencies in reporting of data. | |
| Individual counselling sessions, not a group intervention. | |
| There was unclear presentation of follow‐up data and it was unclear whether it was 3‐month or 6‐month follow‐up data. We contacted the study author but received no response. | |
| Not a RCT, no control group, HIV‐positive and HIV‐negative mixed sample. | |
| Individual psychotherapy, not a group intervention. | |
| Not a group intervention. |
Abbreviations: RCT: randomized controlled trial.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Group therapy (CBT) versus control, Outcome 1 Depression scores. | ||||
| 1.1 Baseline mean scores | 10 | 1600 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.05, 0.15] |
| 1.2 Mean score at end of group sessions (10 to 12 weeks after randomization) | 9 | 1142 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.29, ‐0.05] |
| 1.3 Mean score at longest follow‐up (6 to 15 months after randomization) | 10 | 1139 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.42, ‐0.10] |
| 2 Depression scores at longest follow‐up; subgrouped by depression score used Show forest plot | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Group therapy (CBT) versus control, Outcome 2 Depression scores at longest follow‐up; subgrouped by depression score used. | ||||
| 2.1 Beck depression inventory (score out of 63) | 6 | 753 | Mean Difference (IV, Random, 95% CI) | ‐1.41 [‐2.61, ‐0.21] |
| 2.2 Hospital Anxiety and Depression score (score out of 21) | 1 | 71 | Mean Difference (IV, Random, 95% CI) | ‐2.12 [‐3.90, ‐0.34] |
| 2.3 Geriatric depression score (score out of 30) | 1 | 160 | Mean Difference (IV, Random, 95% CI) | ‐1.48 [‐2.83, ‐0.13] |
| 2.4 Centre for Epidemiological Studies (score out of 60) | 1 | 70 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐4.03, 4.63] |
| 2.5 Self‐reported questionnaire (score out of 20) | 1 | 85 | Mean Difference (IV, Random, 95% CI) | ‐2.5 [‐3.91, ‐1.09] |
| 2.6 Profile of mood states (depression) (score out of 60) | 1 | 101 | Mean Difference (IV, Random, 95% CI) | ‐4.30 [‐10.47, 1.87] |
| 2.7 Montgomery‐Asberg Depression Rating Scale (score out of 60) | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐4.72 [‐9.67, 0.23] |
| 3 Depression scores (trials with mean scores in the range of depression at baseline) Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.3 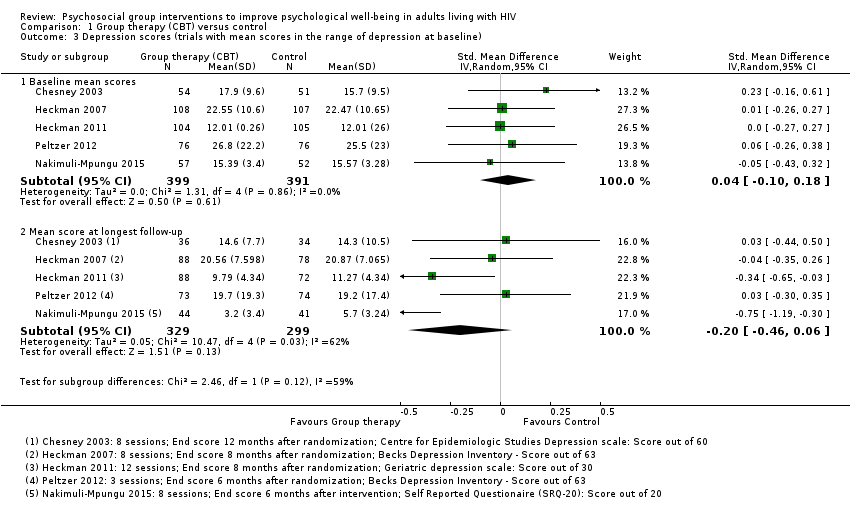 Comparison 1 Group therapy (CBT) versus control, Outcome 3 Depression scores (trials with mean scores in the range of depression at baseline). | ||||
| 3.1 Baseline mean scores | 5 | 790 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.10, 0.18] |
| 3.2 Mean score at longest follow‐up | 5 | 628 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.46, 0.06] |
| 4 Depression scores at longest follow‐up; subgrouped by control Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.4 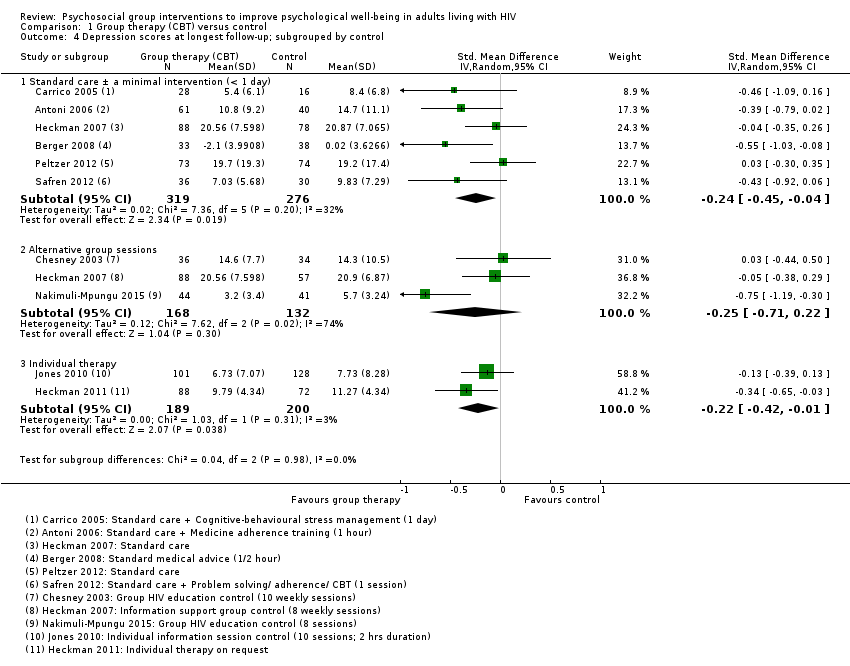 Comparison 1 Group therapy (CBT) versus control, Outcome 4 Depression scores at longest follow‐up; subgrouped by control. | ||||
| 4.1 Standard care ± a minimal intervention (< 1 day) | 6 | 595 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.45, ‐0.04] |
| 4.2 Alternative group sessions | 3 | 300 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.71, 0.22] |
| 4.3 Individual therapy | 2 | 389 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.42, ‐0.01] |
| 5 Depression scores (trials with mean scores in the normal range at baseline) Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Group therapy (CBT) versus control, Outcome 5 Depression scores (trials with mean scores in the normal range at baseline). | ||||
| 5.1 Baseline mean scores | 5 | 810 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.30] |
| 5.2 Mean score at longest follow‐up (6 to 15 months after randomization) | 5 | 511 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.48, ‐0.13] |
| 6 Depression scores at longest follow‐up; subgrouped by primary focus of intervention Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6 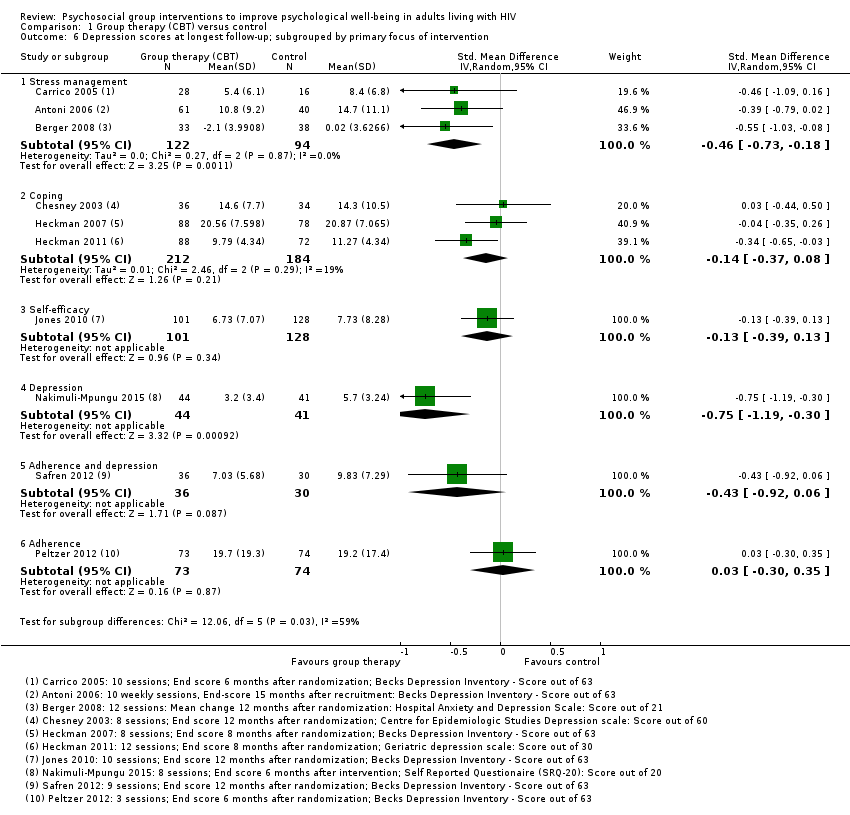 Comparison 1 Group therapy (CBT) versus control, Outcome 6 Depression scores at longest follow‐up; subgrouped by primary focus of intervention. | ||||
| 6.1 Stress management | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.73, ‐0.18] |
| 6.2 Coping | 3 | 396 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.37, 0.08] |
| 6.3 Self‐efficacy | 1 | 229 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.39, 0.13] |
| 6.4 Depression | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.19, ‐0.30] |
| 6.5 Adherence and depression | 1 | 66 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.92, 0.06] |
| 6.6 Adherence | 1 | 147 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.30, 0.35] |
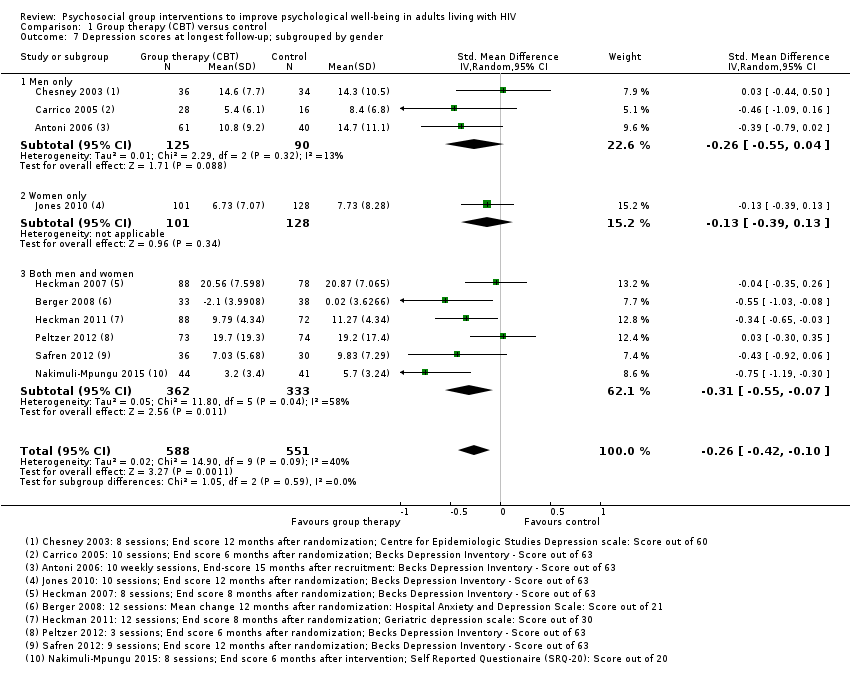
| 7 Depression scores at longest follow‐up; subgrouped by gender Show forest plot | 10 | 1139 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.42, ‐0.10] |
| Analysis 1.7  Comparison 1 Group therapy (CBT) versus control, Outcome 7 Depression scores at longest follow‐up; subgrouped by gender. | ||||
| 7.1 Men only | 3 | 215 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.55, 0.04] |
| 7.2 Women only | 1 | 229 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.39, 0.13] |
| 7.3 Both men and women | 6 | 695 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.55, ‐0.07] |
| 8 Anxiety scores Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 Group therapy (CBT) versus control, Outcome 8 Anxiety scores. | ||||
| 8.1 Baseline mean scores | 4 | 697 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.05, 0.27] |
| 8.2 Mean score at end of group sessions (10 to 12 weeks after randomization) | 3 | 420 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.25, 0.22] |
| 8.3 Mean score at longest follow‐up (12 to 15 months after randomization) | 4 | 471 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.31, 0.06] |
| 9 Anxiety scores: at longest follow‐up; subgrouped by anxiety scale used Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 Group therapy (CBT) versus control, Outcome 9 Anxiety scores: at longest follow‐up; subgrouped by anxiety scale used. | ||||
| 9.1 State trait anxiety inventory (score between 20 and 80) | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐6.06, 4.46] |
| 9.2 Modified State Trait Anxiety Inventory (score between 10 and 40) | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐2.09, 0.87] |
| 9.3 Hospital Anxety and Depression Scale (score out of 21) | 1 | 71 | Mean Difference (IV, Random, 95% CI) | ‐2.4 [‐4.92, 0.12] |
| 9.4 Profile of Mood States (score out of 36) | 1 | 101 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐2.64, 3.04] |
| 10 Anxiety scores: at longest follow‐up; subgrouped by control Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.10 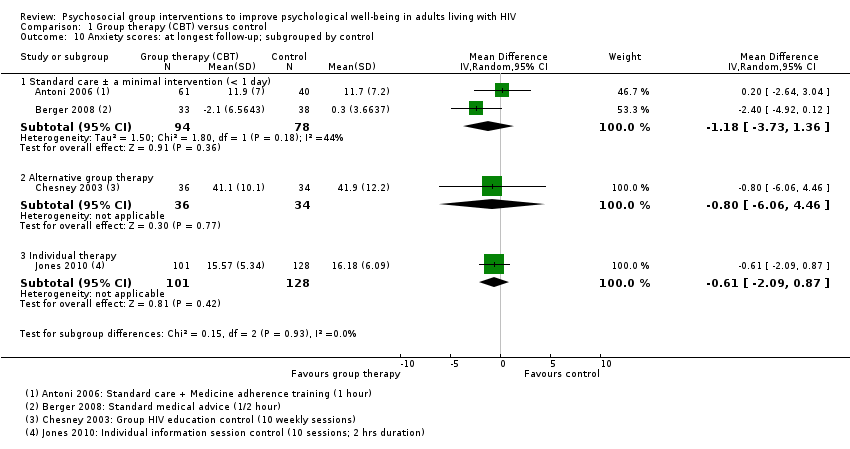 Comparison 1 Group therapy (CBT) versus control, Outcome 10 Anxiety scores: at longest follow‐up; subgrouped by control. | ||||
| 10.1 Standard care ± a minimal intervention (< 1 day) | 2 | 172 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐3.73, 1.36] |
| 10.2 Alternative group therapy | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐6.06, 4.46] |
| 10.3 Individual therapy | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐2.09, 0.87] |
| 11 Stress scores Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.11  Comparison 1 Group therapy (CBT) versus control, Outcome 11 Stress scores. | ||||
| 11.1 Baseline mean scores | 5 | 695 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.03, 0.27] |
| 11.2 Mean score at end of group sessions | 4 | 533 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.23, 0.12] |
| 11.3 Mean score at longest follow‐up | 5 | 507 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.23, 0.15] |
| 12 Stress scores at longest follow‐up; subgrouped by stress score used Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.12  Comparison 1 Group therapy (CBT) versus control, Outcome 12 Stress scores at longest follow‐up; subgrouped by stress score used. | ||||
| 12.1 Perceived stress score (score out of 40) | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐3.77, 2.37] |
| 12.2 Dealing with illness scale | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐7.62, 4.02] |
| 12.3 HIV‐related life‐stressor burden score (score out of 5) | 1 | 166 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.06, 0.22] |
| 12.4 Life experiences survey (score out of 3) | 1 | 39 | Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐3.00, 0.28] |
| 12.5 Impact of event scale (score out of 75) | 2 | 232 | Mean Difference (IV, Random, 95% CI) | ‐1.33 [‐3.60, 0.95] |
| 13 Stress scores at longest follow‐up; subgrouped by control Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.13 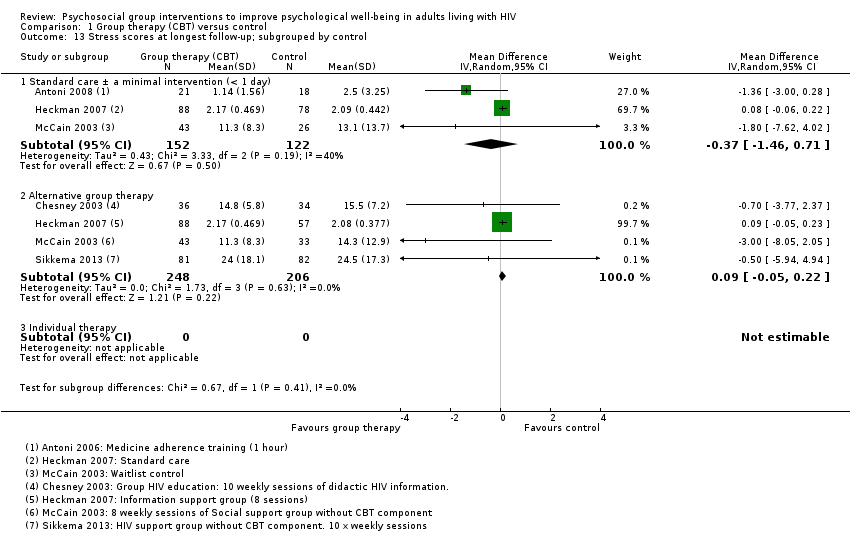 Comparison 1 Group therapy (CBT) versus control, Outcome 13 Stress scores at longest follow‐up; subgrouped by control. | ||||
| 13.1 Standard care ± a minimal intervention (< 1 day) | 3 | 274 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.46, 0.71] |
| 13.2 Alternative group therapy | 4 | 454 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.05, 0.22] |
| 13.3 Individual therapy | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Coping scores Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.14  Comparison 1 Group therapy (CBT) versus control, Outcome 14 Coping scores. | ||||
| 14.1 Baseline mean scores | 5 | 1022 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.11, 0.14] |
| 14.2 Mean score at end of group sessions | 5 | 762 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.16, 0.19] |
| 14.3 Mean score at longest follow‐up (6 months after randomization) | 5 | 697 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.11, 0.19] |
| 15 Coping scores at longest follow‐up; subgrouped by coping score used Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.15  Comparison 1 Group therapy (CBT) versus control, Outcome 15 Coping scores at longest follow‐up; subgrouped by coping score used. | ||||
| 15.1 Dealing with illness: coping subscale (score out of 120) | 1 | 69 | Mean Difference (IV, Random, 95% CI) | 1.90 [‐1.79, 5.59] |
| 15.2 Cognitive behavioural self‐efficacy scale (score out of 28) | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐1.29, 0.97] |
| 15.3 Coping self‐efficacy scale (score out of 260) | 2 | 236 | Mean Difference (IV, Random, 95% CI) | 1.76 [‐6.53, 10.05] |
| 15.4 Avoidant coping scale (score out of 69) | 1 | 163 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐5.26, 1.86] |
| 16 Coping scores at longest follow‐up; subgrouped by control Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.16  Comparison 1 Group therapy (CBT) versus control, Outcome 16 Coping scores at longest follow‐up; subgrouped by control. | ||||
| 16.1 Standard care ± a minimal intervention (< 1 day) | 2 | 235 | Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.21, 0.59] |
| 16.2 Alternative group therapy | 4 | 454 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.67, 0.17] |
| 16.3 Individual therapy | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐1.29, 0.97] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Group therapy (mindfulness) versus control, Outcome 1 Depression scores. | ||||
| 1.1 Baseline mean scores | 3 | 286 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.35, 0.12] |
| 1.2 Mean scores at end of group sessions (8 weeks after randomization) | 3 | 242 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.48, 0.04] |
| 1.3 Mean score at longest follow‐up | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.49, 0.03] |
| 2 Anxiety scores Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Group therapy (mindfulness) versus control, Outcome 2 Anxiety scores. | ||||
| 2.1 Baseline mean scores | 2 | 210 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.29, 0.27] |
| 2.2 Mean scores at end of group sessions (8 weeks after randomization) | 2 | 178 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.53, 0.07] |
| 2.3 Mean score at longest follow‐up | 2 | 162 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.47, 0.15] |
| 3 Stress scores Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2 Group therapy (mindfulness) versus control, Outcome 3 Stress scores. | ||||
| 3.1 Baseline mean scores | 2 | 169 | Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐3.50, 1.46] |
| 3.2 Mean scores at end of treatment | 2 | 139 | Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐4.46, ‐0.11] |
| 3.3 Mean score at longest follow‐up | 2 | 137 | Mean Difference (IV, Random, 95% CI) | ‐2.02 [‐4.23, 0.19] |

Conceptual framework
Study flow diagram
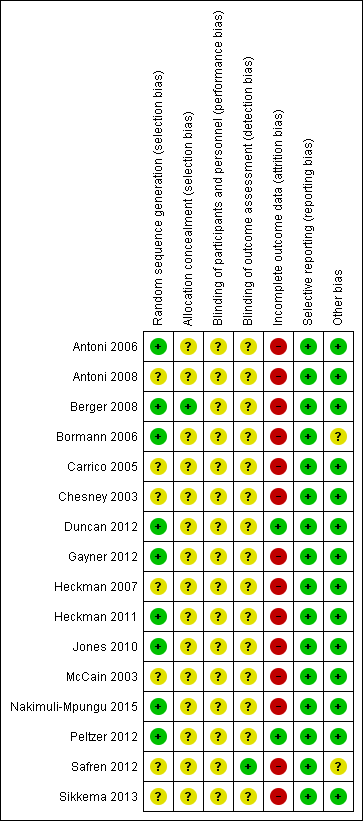
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included trial

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included trials

Comparison 1 Group therapy (CBT) versus control, Outcome 1 Depression scores.

Comparison 1 Group therapy (CBT) versus control, Outcome 2 Depression scores at longest follow‐up; subgrouped by depression score used.

Comparison 1 Group therapy (CBT) versus control, Outcome 3 Depression scores (trials with mean scores in the range of depression at baseline).

Comparison 1 Group therapy (CBT) versus control, Outcome 4 Depression scores at longest follow‐up; subgrouped by control.
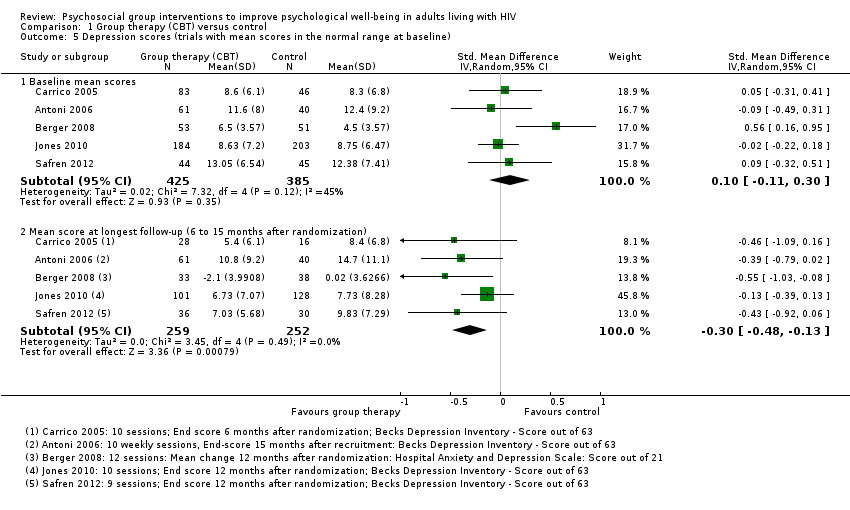
Comparison 1 Group therapy (CBT) versus control, Outcome 5 Depression scores (trials with mean scores in the normal range at baseline).

Comparison 1 Group therapy (CBT) versus control, Outcome 6 Depression scores at longest follow‐up; subgrouped by primary focus of intervention.
Comparison 1 Group therapy (CBT) versus control, Outcome 7 Depression scores at longest follow‐up; subgrouped by gender.

Comparison 1 Group therapy (CBT) versus control, Outcome 8 Anxiety scores.

Comparison 1 Group therapy (CBT) versus control, Outcome 9 Anxiety scores: at longest follow‐up; subgrouped by anxiety scale used.

Comparison 1 Group therapy (CBT) versus control, Outcome 10 Anxiety scores: at longest follow‐up; subgrouped by control.

Comparison 1 Group therapy (CBT) versus control, Outcome 11 Stress scores.

Comparison 1 Group therapy (CBT) versus control, Outcome 12 Stress scores at longest follow‐up; subgrouped by stress score used.

Comparison 1 Group therapy (CBT) versus control, Outcome 13 Stress scores at longest follow‐up; subgrouped by control.

Comparison 1 Group therapy (CBT) versus control, Outcome 14 Coping scores.

Comparison 1 Group therapy (CBT) versus control, Outcome 15 Coping scores at longest follow‐up; subgrouped by coping score used.

Comparison 1 Group therapy (CBT) versus control, Outcome 16 Coping scores at longest follow‐up; subgrouped by control.

Comparison 2 Group therapy (mindfulness) versus control, Outcome 1 Depression scores.

Comparison 2 Group therapy (mindfulness) versus control, Outcome 2 Anxiety scores.

Comparison 2 Group therapy (mindfulness) versus control, Outcome 3 Stress scores.
| Group therapy (cognitive behavioural therapy (CBT)) versus control for improving psychological well‐being in adults living with HIV | |||||
| Patient or population: adults living with HIV | |||||
| Outcomes | Illustrative comparative risks (95% CI)* | Number of participants (trials) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Control | Group therapy (CBT) | ||||
| Depression score | The mean scores in the control groups at the end of follow‐up ranged from normal to moderately depressed | The mean score in the intervention groups was: | 1139 | ⊕⊕⊝⊝ due to indirectness and risk of bias | There may be a small benefit which lasts for up to 15 months |
| Anxiety score Follow‐up: 6 to 15 months | The mean scores in the control groups at the end of follow‐up ranged from normal to clinically anxious | The mean score in the intervention groups was: | 471 | ⊕⊕⊝⊝ due to indirectness and risk of bias | There may be little or no effect on mean anxiety scores |
| Stress score Follow‐up: 6 to 15 months | The mean score in the control groups at the end of follow‐up were variable | The mean score in the intervention groups was | 507 | ⊕⊕⊝⊝ due to indirectness and risk of bias | There may be little or no effect on mean stress scores |
| Coping score Follow‐up: 6 to 15 months | The mean score in the control groups at the end of follow‐up were variable | The mean score in the intervention groups was | 697 | ⊕⊕⊝⊝ due to indirectness and risk of bias | There may be little or no effect on mean coping scores |
| Studies used a variety of different scales to measure depression, anxiety and stress. Consequently, trials were pooled using a standardized mean difference. Examples of how large this effect would be on standardized measurement scales are given in the review main text and abstract. | |||||
| GRADE Working Group grades of evidence | |||||
| 1Downgraded by 1 for serious risk of bias: most of the trials did not adequately described a method of allocation concealment, and so trials are at unclear or high risk of selection bias. Loss of follow‐up was generally more than 20% and attrition bias may be present. | |||||
| Group therapy (mindfulness) compared to control for improving psychological well‐being in adults living with HIV | |||||
| Patient or population: adults living with HIV | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | ||||
| Control | Group therapy (Mindfulness) | ||||
| Depression score Follow‐up: 4 to 6 months | The mean scores in the control groups at the end of follow‐up were in the range of normal to mild depression | The mean score in the intervention groups was | 233 | ⊕⊝⊝⊝ due to risk of bias, indirectness, and imprecision | We don't know if there is a benefit on depression scores |
| Anxiety score Follow‐up: 4 to 6 months | The mean scores in the control group at the end of follow‐up were in the range of normal to mild anxiety | The mean score in the intervention groups was | 162 | ⊕⊝⊝⊝ due to risk of bias, indirectness, and imprecision | We don't know if there is an effect on mean anxiety scores |
| Stress score Follow‐up: 4 to 6 months | The mean scores in the control group at the end of follow‐up were in the range of mild stress | The mean score in the intervention groups was | 137 | ⊕⊝⊝⊝ due to risk of bias, indirectness, and imprecision | We don't know if there is an effect on mean stress scores |
| Coping score Follow‐up: no coping was measured by mindfulness intervention trials | — | — | 0 (0 trials) | — | — |
| Studies used a variety of different scales to measure depression, anxiety and stress. Consequently, trials were pooled using a standardized mean difference. Examples of how large this effect would be on standardized measurement scales are given in the review main text and abstract. | |||||
| GRADE Working Group grades of evidence | |||||
| 1Downgraded by 1 for serious risk of bias: none of the trials adequately described a method of allocation concealment, and so trials are at unclear or high risk of selection bias. Loss of follow‐up was generally more than 20% and attrition bias may be present. | |||||
| Trial | Country | Age (years) | On antiretroviral therapy (ART) | General population or subgroup | Mood disorders | |
| Inclusion criteria | Exclusion criteria | |||||
| USA | 18 to 65 | Yes | Homosexual men | None stated | Current psychosis or panic disorder | |
| USA | 18 to 60 | Not stated | Women with evidence of CIN1 | None stated | Current major psychiatric illness | |
| Switzerland | 18 to 65 | Yes | General population | None stated | Current major psychiatric disorder | |
| USA | Not stated | No (recruited largely during the era prior to highly active antiretroviral therapy (HAART; 1992 to 1997) | Homosexual men | None stated | Current major psychiatric illness | |
| USA | > 18 | Not stated | Minority women | None stated | Untreated major psychiatric illness | |
| USA | > 18 | Yes | General population | None stated | Significant psychiatric illness | |
| USA | 18 to 65 | Yes | Prior intravenous drug users | Current depressive mood disorder | Untreated or unstable major mental illness | |
| USA | Not stated | Not stated | Rural population | No inclusion or exclusion criteria related to psychological functioning were employed | No inclusion or exclusion criteria related to psychological functioning were employed | |
| USA | > 50 | Not stated | Individuals over the age of 50 | BDI‐II score is minimum 10 | Exclude severe depression or cognitive impairment | |
| USA | Not stated | Not stated | History of child sexual abuse | Not stated | Not stated | |
| South Africa | > 18 | Yes | Individuals with ART adherence problem/new antiretroviral (ARV) medication users (6 to 24 months of ARV use) | Not stated | Not stated | |
| USA | 21 to 60 | No | Homosexual men | Reported depressed mood 10 or higher on CES‐D scale | Major depressive disorder or other psychotic disorders | |
| USA | 18 to 65 | Not stated | Adult men and women (50% homosexual) | Not stated | Cognitive impairment of active psychosis | |
| USA | Not specified | Yes | Adult men and women who reported | Reporting a level of side effect‐related bother for the previous 30 days at or above eight (corresponding to the 40th percentile in another sample) on the side effect and symptom distress scale | Severe cognitive impairment, | |
| Canada | Not specified | Not stated | Homosexual men | None stated | Active current major depression, substance abuse, or significant cognitive deficit | |
| Uganda | > 19 | Not stated | Both men and women | People with major depression on Mini Psychiatric Interview Scale | The trial excluded individuals with a severe medical disorder such as pneumonia or active tuberculosis, psychotic symptoms, and hearing or visual impairment. | |
| Abbreviations: ART: antiretroviral therapy; ARV: antiretroviral. | ||||||
| Scale | Number of items | Scale for each item1 | Total score | Interpretation | Description2 | Trials |
| Beck Depression Inventory | 21 | 0 (I do not) to 3 (I do and I can't stand it) | 0 to 63 | 0 to 13: minimal 14 to 19: mild 20 to 28: moderate 29 to 63: severe | Participants rate the intensity of depressive feelings over the preceding 1 or 2 weeks | Carrico 2005; Antoni 2006; Heckman 2007; Jones 2010; Duncan 2012; Peltzer 2012; Safren 2012 |
| Hospital Anxiety and Depression Scale (HADS) (Zigmond 1983) | 7 | 0 (not at all) to 3 (very often) | 0 to 21 | 0 to 7: normal 8 to 10: borderline 11 to 21: depression | Participants rate the frequency of depressive thoughts and behaviours over the preceding 4 weeks | |
| Geriatric Depression Scale (GDS) (Yesavage 1982) | 30 | 0 (no) to 1 (yes) | 0 to 30 | 0 to 9: normal 10 to 19: mild 20 to 30: severe | Participants report the presence or absence of depressive thoughts and behaviours | |
| The Centre for Epidemiological Studies‐Depression Scale (CES‐D) | 20 | 0 (not at all) to 3 (all of the time) | 0 to 60 | 0 to 15: normal 16 to 60: depression Cut off is 16 | Participants rate the frequency of depressive symptoms, feelings, and behaviours over the past week | |
| Self Reported Questionnaire (SRQ‐20) | 20 | 0 (no) to 1 (yes) | 0 to 20 | 0 to 5: normal 6 to 20: depression | Participants report the presence or absence of depressive symptoms, thoughts, and behaviours | |
| Profile of Mood States (POMS) Depression (D) | 15 | 0 (not at all) to 4 (extremely) | 0 to 60 | Higher scores indicate worsening depression | Participants rate adjectives describing their mood states over the past week | |
| Montgomery‐Asberg Depression Rating Scale (MADRS) (Montgomery 1979) | 10 | 0 (normal) to 6 (severe) | 0 to 60 | 0 to 6: normal 7 to 19: mild 20 to 34: moderate > 34: severe | A physician assessment based on a clinical interview covering depression symptoms | |
| 1The exact responses may vary between items. | ||||||
| Scale | Number of items (anxiety) | Score for each item1 | Total score (anxiety) | Interpretation | Description2 | Trials |
| Profile of Mood States | 9 | 0 (not at all) to 4 (extremely) | 0 to 36 | Higher scores indicate worsening anxiety | Participants rate adjectives describing their mood states over the past week | |
| Hospital Anxiety and Depression Scale (HADS) (Zigmond 1983) | 7 | 0 (not at all) to 3 (very often) | 0 to 21 | 0 to 7: normal 8 to 10: borderline 11 to 21: anxiety | Participants rate the frequency of anxiety feelings and behaviours over the preceding 4 weeks | |
| State Trait‐Anxiety Inventory | 20 | 1 (not at all) to 4 (very much so) | 20 to 80 | A cut point of 39 to 40 has been suggested to detect clinically significant symptoms | Participants rate the frequency and intensity of anxiety feelings at this moment (state), and more generally (trait) | |
| 1The exact responses may vary between items. | ||||||
| Scale | Number of items | Score for each item1 | Total score | Interpretation | Description2 | Trials |
| Perceived Stress Scale (PSS) (Cohen 1983) | 10 | 0 (never) to 4 (very often) | 0 to 40 | Higher scores indicate higher perceived stress | Participants rate the frequency of stress related thoughts and feelings in the preceding 4 weeks | |
| Dealing with Illness Scale ‐ Stress subscale (DIS) (McCain 1992) | Unclear | Unclear | Unclear | Higher scores reflect higher stress | Participants rate the desirability or undesirability and personal impact of experienced events | |
| HIV‐Related Life‐Stress Scale (Sikkema 2000) | 19 | 1 (not a problem) to 5 (most serious problem) | 1 to 5 | Higher scores indicate higher stress | Participants rate the severity of each HIV‐related potential stressor | |
| Life Experiences Survey (LES) (Sarason 1978) | 10 | 0 (not at all stressed) to 3 (extremely stressful) | 0 to 3 | 0 = not at all stressed 1 = mildly stressed 2 = moderately stressed 3 = extremely stressed | Participants rate the extent to which an event commonly experienced by HIV‐positive women had been stressful | Antoni 2008 (a 10‐item abbreviated version) |
| Impact of Event Scale (IES) | 15 | 0 (not at all) to 4 (often) | 0 to 75 | Higher scores indicate higher impact | Participants rate the frequency of intrusive or avoidant thoughts and experiences over the preceding 7 to 28 days (the authors describe this scale as measuring 'psychological distress' or 'traumatic stress') | |
| 1The exact responses may vary between items. | ||||||
| Trial | Group size | Session duration (mins) | Session frequency | Intervention | Comparison | |||||
| Underlying theory | Primary focus | Components | ||||||||
| Skills training | Relaxation techniques | Peer support2 | Education2 | |||||||
| 6 to 10 | 90 | Weekly for 8 weeks | Cognitive‐behavioural | Stress management | Cognitive restructuring coping skills | Progressive muscle relaxation (PMR)/meditation/yoga | Not described | Not described | No intervention ‐ waitlist group | |
| 4 to 9 | 135 | Weekly for 10 weeks | Cognitive‐behavioural | Stress management | Cognitive restructuring, coping skills, anger management, use of social network | PMR/meditation | Not described | Not described | No intervention ‐ waitlist group | |
| 4 to 9 | 135 | Weekly for 10 weeks | Cognitive‐behavioural | Stress management | Cognitive restructuring, coping skills | PMR/meditation | Not described | Medication adherence | 1 hour medication adherence training (MAT) | |
| 4 to 6 | 135 | Weekly for 10 weeks | Cognitive‐behavioural | Stress management | Cognitive restructuring, coping skills, assertiveness, anger management, use of social network | PMR/meditation | Not described | Not described | Condensed 1 day CBSM workshop | |
| 4 to 10 | 120 | Weekly for 12 weeks | Cognitive‐behavioural | Stress management | Cognitive strategies | PMR | Group dynamic exercises | HIV related topics | No intervention ‐ 30‐minute health check by physician | |
| 10 | 90 | Weekly for 15 weeks | Cognitive theory of stress and coping | Traumatic stress | Cognitive appraisal, coping skills | 'relaxation strategies' | Not described | Not described | Attention control ‐ HIV standard therapeutic support group | |
| 8 to 10 | 90 | Weekly for 10 weeks | Cognitive theory of stress and coping | Coping/stress | Appraising stressors, coping skills, stress management | 'relaxation guidance' | Skill building group exercises | Psychoeducation around models of coping | No intervention ‐ waitlist group | |
| 6 to 8 | 90 | Weekly for 8 weeks | Transactional model of stress and coping | Coping | Appraising stressors, coping skills, use of personal and social resources | No | Not described | Not described | No intervention ‐ usual care | |
| 6 to 810 | 90 | Weekly for 12 weeks | Transactional model of stress and coping | Coping | Appraising stressors, coping skills, use of personal and social resources | No | Not described | Not described | No intervention ‐ individual therapy upon request (ITUR) | |
| Not stated | 120 | Weekly for 10 weeks | Cognitive‐behavioural | Self‐efficacy | Cognitive restructuring, stress management, coping skills, anger management, use of social network | 'relaxation' | Expressive supportive therapy | HIV/mental health topics | Attention control group | |
| 10 to 12 | 120 to 180 | Weekly for 8 weeks | Cognitive‐behavioural, social learning theory, and the sustainable livelihoods framework | Depression | Coping skills, problem solving skills, dealing with stigma, income‐generation | Not described | Group rituals | Triggers, symptoms, and treatment of depression. | Active control group | |
| Not stated | 50 mins | Weekly for 9 weeks | Cognitive‐behavioural | Adherence/ depression | Cognitive restructuring, problem solving, activity scheduling | PMR/diaphragmatic breathing | Not described | Adherence, depression | Enhanced treatment as usual (ETAU) | |
| 10 | 60 mins | Monthly for 3 months | Cognitive‐behavioural | Adherence | Not specifically described | Not described | Buddy system to increase social support | Knowledge of HIV and HIV‐related medication | No intervention ‐ standard care | |
| Abbreviations: HIV: human immunodeficiency virus; PMR: progressive muscle relaxation. | ||||||||||
| Scale | Number of items | Score for each item1 | Total score | Interpretation | Description2 | Trials |
| Coping Self‐Efficacy Scale (CSES) (Chesney 2006) | 26 | 0 (cannot do at all) to 10 (certain can do) | 0 to 260 | Higher scores indicate better coping skills | Participants rate the extent to which they believe they could perform behaviours important to adaptive coping | |
| Cognitive Behavioral Self Efficacy (CB‐SE) (Ironson 1987) | 7 | 0 (not at all) to 4 (all of the time) | 0 to 28 | Higher scores indicate higher self‐efficacy | Participants rate their certainty that they could perform certain skills related to AIDS, and antiretroviral medication adherence | |
| Dealing with Illness Scale ‐ coping subscale (DIS) (McCain 1992) | 40 | 0 (never used) to 3 (regularly used) | 0 to 120 | Higher scores reflect more frequent use of the various coping strategies. | The DIS is a 40‐item coping subscale modelled on the Revised Ways of Coping Checklist. Participants rate the frequency that thoughts or behaviours have been used to deal with problems and stresses over the past month. | |
| 'Avoidant Coping Scale' Created from 23 items taken from 'The ways of Coping Questionnaire' and 'the Coping with AIDS Scale' (Sikkema 2013) | 23 | 0 (not at all) to 3 (used a great deal) | 0 to 69 | Higher scores reflect more frequent use of coping strategies | Participants rate how often they have used avoidant strategies for coping | |
| 1The exact responses may vary between items. | ||||||
| Trial | Group size | Session duration (mins) | Session frequency | Intervention | Comparison | |||
| Primary focus | Secondary components | |||||||
| Relaxation techniques | Peer support | Education | ||||||
| Not stated | 150 to 180 | Weekly for 8 weeks plus 1 day retreat | Mindfulness‐stress reduction | Mindfulness meditation | Not described | Stress physiology and reactivity | No intervention ‐ waitlist group | |
| 14 to 18 | 180 | Weekly for 8 weeks plus 1 day retreat | Mindfulness‐stress reduction | Mindfulness meditation | Not described | Not described | No intervention ‐ treatment as usual (TAU) group offered at end of intervention | |
| 8 to 15 | 90 | Weekly for 5 weeks, then 4 automated phone calls, then a final session in week 10 | Mindfulness‐stress reduction | Mantram repetition | Not described | Not described | Attention control | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Baseline mean scores | 10 | 1600 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.05, 0.15] |
| 1.2 Mean score at end of group sessions (10 to 12 weeks after randomization) | 9 | 1142 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.29, ‐0.05] |
| 1.3 Mean score at longest follow‐up (6 to 15 months after randomization) | 10 | 1139 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.42, ‐0.10] |
| 2 Depression scores at longest follow‐up; subgrouped by depression score used Show forest plot | 10 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Beck depression inventory (score out of 63) | 6 | 753 | Mean Difference (IV, Random, 95% CI) | ‐1.41 [‐2.61, ‐0.21] |
| 2.2 Hospital Anxiety and Depression score (score out of 21) | 1 | 71 | Mean Difference (IV, Random, 95% CI) | ‐2.12 [‐3.90, ‐0.34] |
| 2.3 Geriatric depression score (score out of 30) | 1 | 160 | Mean Difference (IV, Random, 95% CI) | ‐1.48 [‐2.83, ‐0.13] |
| 2.4 Centre for Epidemiological Studies (score out of 60) | 1 | 70 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐4.03, 4.63] |
| 2.5 Self‐reported questionnaire (score out of 20) | 1 | 85 | Mean Difference (IV, Random, 95% CI) | ‐2.5 [‐3.91, ‐1.09] |
| 2.6 Profile of mood states (depression) (score out of 60) | 1 | 101 | Mean Difference (IV, Random, 95% CI) | ‐4.30 [‐10.47, 1.87] |
| 2.7 Montgomery‐Asberg Depression Rating Scale (score out of 60) | 1 | 66 | Mean Difference (IV, Random, 95% CI) | ‐4.72 [‐9.67, 0.23] |
| 3 Depression scores (trials with mean scores in the range of depression at baseline) Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Baseline mean scores | 5 | 790 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.10, 0.18] |
| 3.2 Mean score at longest follow‐up | 5 | 628 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.46, 0.06] |
| 4 Depression scores at longest follow‐up; subgrouped by control Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Standard care ± a minimal intervention (< 1 day) | 6 | 595 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.45, ‐0.04] |
| 4.2 Alternative group sessions | 3 | 300 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.71, 0.22] |
| 4.3 Individual therapy | 2 | 389 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.42, ‐0.01] |
| 5 Depression scores (trials with mean scores in the normal range at baseline) Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Baseline mean scores | 5 | 810 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.11, 0.30] |
| 5.2 Mean score at longest follow‐up (6 to 15 months after randomization) | 5 | 511 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.48, ‐0.13] |
| 6 Depression scores at longest follow‐up; subgrouped by primary focus of intervention Show forest plot | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Stress management | 3 | 216 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.73, ‐0.18] |
| 6.2 Coping | 3 | 396 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.37, 0.08] |
| 6.3 Self‐efficacy | 1 | 229 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.39, 0.13] |
| 6.4 Depression | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.19, ‐0.30] |
| 6.5 Adherence and depression | 1 | 66 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.92, 0.06] |
| 6.6 Adherence | 1 | 147 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.30, 0.35] |
| 7 Depression scores at longest follow‐up; subgrouped by gender Show forest plot | 10 | 1139 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.42, ‐0.10] |
| 7.1 Men only | 3 | 215 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.55, 0.04] |
| 7.2 Women only | 1 | 229 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.39, 0.13] |
| 7.3 Both men and women | 6 | 695 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.55, ‐0.07] |
| 8 Anxiety scores Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Baseline mean scores | 4 | 697 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.05, 0.27] |
| 8.2 Mean score at end of group sessions (10 to 12 weeks after randomization) | 3 | 420 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.25, 0.22] |
| 8.3 Mean score at longest follow‐up (12 to 15 months after randomization) | 4 | 471 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.31, 0.06] |
| 9 Anxiety scores: at longest follow‐up; subgrouped by anxiety scale used Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 State trait anxiety inventory (score between 20 and 80) | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐6.06, 4.46] |
| 9.2 Modified State Trait Anxiety Inventory (score between 10 and 40) | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐2.09, 0.87] |
| 9.3 Hospital Anxety and Depression Scale (score out of 21) | 1 | 71 | Mean Difference (IV, Random, 95% CI) | ‐2.4 [‐4.92, 0.12] |
| 9.4 Profile of Mood States (score out of 36) | 1 | 101 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐2.64, 3.04] |
| 10 Anxiety scores: at longest follow‐up; subgrouped by control Show forest plot | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Standard care ± a minimal intervention (< 1 day) | 2 | 172 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐3.73, 1.36] |
| 10.2 Alternative group therapy | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐6.06, 4.46] |
| 10.3 Individual therapy | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐2.09, 0.87] |
| 11 Stress scores Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Baseline mean scores | 5 | 695 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.03, 0.27] |
| 11.2 Mean score at end of group sessions | 4 | 533 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.23, 0.12] |
| 11.3 Mean score at longest follow‐up | 5 | 507 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.23, 0.15] |
| 12 Stress scores at longest follow‐up; subgrouped by stress score used Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Perceived stress score (score out of 40) | 1 | 70 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐3.77, 2.37] |
| 12.2 Dealing with illness scale | 1 | 69 | Mean Difference (IV, Random, 95% CI) | ‐1.80 [‐7.62, 4.02] |
| 12.3 HIV‐related life‐stressor burden score (score out of 5) | 1 | 166 | Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.06, 0.22] |
| 12.4 Life experiences survey (score out of 3) | 1 | 39 | Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐3.00, 0.28] |
| 12.5 Impact of event scale (score out of 75) | 2 | 232 | Mean Difference (IV, Random, 95% CI) | ‐1.33 [‐3.60, 0.95] |
| 13 Stress scores at longest follow‐up; subgrouped by control Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Standard care ± a minimal intervention (< 1 day) | 3 | 274 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐1.46, 0.71] |
| 13.2 Alternative group therapy | 4 | 454 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.05, 0.22] |
| 13.3 Individual therapy | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Coping scores Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 Baseline mean scores | 5 | 1022 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.11, 0.14] |
| 14.2 Mean score at end of group sessions | 5 | 762 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.16, 0.19] |
| 14.3 Mean score at longest follow‐up (6 months after randomization) | 5 | 697 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.11, 0.19] |
| 15 Coping scores at longest follow‐up; subgrouped by coping score used Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 Dealing with illness: coping subscale (score out of 120) | 1 | 69 | Mean Difference (IV, Random, 95% CI) | 1.90 [‐1.79, 5.59] |
| 15.2 Cognitive behavioural self‐efficacy scale (score out of 28) | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐1.29, 0.97] |
| 15.3 Coping self‐efficacy scale (score out of 260) | 2 | 236 | Mean Difference (IV, Random, 95% CI) | 1.76 [‐6.53, 10.05] |
| 15.4 Avoidant coping scale (score out of 69) | 1 | 163 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐5.26, 1.86] |
| 16 Coping scores at longest follow‐up; subgrouped by control Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Standard care ± a minimal intervention (< 1 day) | 2 | 235 | Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.21, 0.59] |
| 16.2 Alternative group therapy | 4 | 454 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.67, 0.17] |
| 16.3 Individual therapy | 1 | 229 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐1.29, 0.97] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Depression scores Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Baseline mean scores | 3 | 286 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.35, 0.12] |
| 1.2 Mean scores at end of group sessions (8 weeks after randomization) | 3 | 242 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.48, 0.04] |
| 1.3 Mean score at longest follow‐up | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.49, 0.03] |
| 2 Anxiety scores Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Baseline mean scores | 2 | 210 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.29, 0.27] |
| 2.2 Mean scores at end of group sessions (8 weeks after randomization) | 2 | 178 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.53, 0.07] |
| 2.3 Mean score at longest follow‐up | 2 | 162 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.47, 0.15] |
| 3 Stress scores Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Baseline mean scores | 2 | 169 | Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐3.50, 1.46] |
| 3.2 Mean scores at end of treatment | 2 | 139 | Mean Difference (IV, Random, 95% CI) | ‐2.29 [‐4.46, ‐0.11] |
| 3.3 Mean score at longest follow‐up | 2 | 137 | Mean Difference (IV, Random, 95% CI) | ‐2.02 [‐4.23, 0.19] |

