益生菌用於預防神經性膀胱障礙病人之泌尿道感染
Abstract
Background
Neuropathic or neurogenic bladder describes a process of dysfunctional voiding as the result of injury in the brain, spinal cord or nerves innervating the bladder. People with neuropathic bladder, such as from spinal cord injury (SCI), are at significant risk of morbidity from urinary tract infections (UTI). Effective methods to prevent UTI in people with SCI have been sought for many years. Probiotics (micro‐organisms that exert beneficial health effects in the host) have been recommended for bacterial interference of the urological tract to reduce colonisation by uropathogen and to manage the dual problems of infection and antibiotic resistance.
Objectives
This review looked at the benefits and harms of probiotics in preventing symptomatic UTI in people with neuropathic bladder compared with placebo, no therapy, or non‐antibiotic prophylaxis (cranberry juice, methenamine hippurate, topical oestrogen).
Search methods
We searched the Cochrane Kidney and Transplant Specialised Register up to 10 March 2017 through contact with the Information Specialist using search terms relevant to this review. Studies in the Specialised Register are identified through searches of CENTRAL, MEDLINE, and EMBASE, conference proceedings, the International Clinical Trials Register (ICTRP) Search Portal, and ClinicalTrials.gov.
Selection criteria
All randomised controlled trials (RCTs), quasi‐RCTs and cross‐over RCTs looking at the use of probiotics for the prophylaxis of UTI in people with neuropathic bladders was considered for inclusion. Men, women and children of all ages with neuropathic bladders from neurological injury such as suprapontine, supra sacral and sacral aetiologies was included. All bladder management types, including reflex voiding, time voiding, indwelling and intermittent catheterization were eligible for this review.
Studies comparing probiotics to placebo, no treatment or other non‐antibiotic prophylaxis was included. Studies comparing probiotics with antibiotics or in combination with antibiotics were excluded.
Data collection and analysis
Summary estimates of effect were obtained using a random‐effects model, and results were expressed as risk ratios (RR) and their 95% confidence intervals (CI) for dichotomous outcomes, and mean difference (MD) or standardised mean difference (SMD) and 95% CI were planned for continuous outcomes.
Main results
This review includes a total of three studies (one cross‐over and two parallel RCTs) which involved 110 participants. All three studies looked at intravesical instillation of a low virulent Escherichia coli (E. coli) strain in reducing the risk of symptomatic UTI in participants with neuropathic bladder, predominantly from SCI. Two studies used the E. coli 83972 strain and one study used the E. coli HU2117 strain.
We did not find any RCTs involving other probiotics or other routes of administration for preventing UTI in people with neuropathic bladder.
There was consistency in definition of symptomatic UTI in all three studies. Symptoms that all studies considered were relevant to diagnose UTI were adequately defined. All three studies defined microbiological diagnosis of symptomatic UTI.
Asymptomatic bacteriuria was not considered an outcome measure in any of the included studies; however it was defined in two studies to establish successful inoculation.
It is uncertain if the risk of symptomatic UTI is reduced with bladder inoculation using E. coli because the certainty of the evidence is very low (3 studies, 110 participants: RR 0.32, 95% CI 0.08 to 1.19; I2 = 82%).
Two studies reported adverse events. One study reported one episode of autonomic dysreflexia. One study reported three symptomatic UTI occurring in two patients, and two studies mentioned the absence of septicaemia and pyelonephritis. Intravesical instillation was reported as "generally safe". One study reported high attrition rates in participants due to the need to adhere to strict instillation protocols.
The overall quality of the studies was poor. All three studies had high risk of attrition bias due to failure of an intention‐to‐treat analysis which undermines the randomisation process and weakened the results of the studies. All three studies also had high risk of reporting bias.
Authors' conclusions
In this review, there were no studies identified addressing oral probiotics in preventing UTI in people with neuropathic bladder. It is uncertain if the risk of symptomatic UTI is reduced in people with neuropathic bladders via intravesical instillation of non‐pathogenic E. coli as data were derived from small studies with high risk of bias.
Although very minimal levels of harm was reported with this procedure, due to variable success rates, the need for strict adherence to instillation protocols together with high attrition rates in these studies, it is doubtful bladder instillation will be a widely accepted intervention in its current form.
It is recommended that further appropriately powered RCTs with more robust methodological reporting be carried out.
PICO
Plain language summary
益生菌用於預防神經系統受損造成膀胱障礙病人之泌尿道感染
本篇議題是什麼?
膀胱功能可能會在神經系統受損後發生改變,尤其是患有多發性硬化症、脊髓損傷或中風病人最為常見,這類膀胱功能障礙被稱為神經性膀胱障礙。神經性膀胱障礙會增加膀胱反覆感染之風險,但目前尚無有效的方法可以預防,且也不鼓勵長期使用抗生素,其原因是容易影響抗生素未來使用上的效果。益生菌為對身體有益處之細菌,目前有些證據顯示,在停經婦女身上使用益生菌可以達到預防膀胱感染之效果。
我們做了什麼?
本篇文獻回顧探討益生菌對於神經性膀胱障礙病人預防膀胱感染之效果。
我們發現了什麼?
我們針對至2017年三月前的文獻進行回顧,並依照我們的篩選標準納入了三個研究,共包含110位受試者,這三個研究皆旨於探討針對患有神經性膀胱障礙者,尤其是因為脊髓損傷導致神經性膀胱障礙之病人,直接在膀胱內導入益生菌產生無害的菌落,是否能預防泌尿道感染。其中兩個研究指出這樣的做法大多是安全無虞的,然而本文獻回顧發現,普遍來說,這些研究之設計品質不夠嚴謹,具有高偏差風險。我們發現在神經性膀胱障礙者身上,使用益生菌在膀胱中移生以預防泌尿道感染之效果是存疑的,此外,研究過程中的移生成功率並不穩定,且由於導入過程具有侵入性,需要受試者的高度參與。
我們在回顧的過程中,沒有發現其他針對膀胱障礙病人身上,探討使用其他益生菌或者是其他給予途徑以預防泌尿道感染之研究。
結論
益生菌在因脊髓損傷導致神經性膀胱障礙之病人身上,預防泌尿道感染之效益有待進一步釐清,未來尚需要執行更多設計更嚴謹的研究。
Authors' conclusions
Summary of findings
| Intravesical bacterial interference versus placebo for preventing urinary tract infection in people with neuropathic bladder | |||||
| Patient or population: people with neuropathic bladder | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants (studies) | Quality of the evidence | |
| Risk with placebo | Risk with intravesical bacterial interference | ||||
| Symptomatic UTI | 613 per 1,000 | 196 per 1,000 | RR 0.32 | 110 (3) | ⊕⊝⊝⊝1 |
| GRADE Working Group grades of evidence | |||||
| 1Risk of bias was assessed at high in most domains, with heterogeneity and small studies, suggesting that results overestimate intravesical bacterial interference versus placebo | |||||
Background
Description of the condition
Neuropathic or neurogenic bladder describes a process of dysfunctional voiding as the result of neurological injury (Kaynan 2008). The International Continence Society states that neuropathic bladder can only be diagnosed in the presence of neurological pathology (Stohrer 1999). Neurologic control of bladder function is at multiple levels throughout the central nervous system and subject to multiple pathophysiologic processes (Kaynan 2008). Neurological diseases that affect bladder function can be classified according to the location of the lesion: suprapontine, supra sacral or sacral. Examples of neurological disorders leading to voiding dysfunction include cerebral palsy, stroke, Parkinson's disease, dementia, spinal cord injury (SCI), multiple sclerosis, transverse myelitis, poliomyelitis, and radical pelvic surgery (Kaynan 2008). Tumours affecting the central nervous system can also cause voiding dysfunction.
Traumatic and non‐traumatic causes of SCI can lead to neuropathic bladders. Aetiologies of non‐traumatic SCI are congenital, vascular, demyelinating, toxic, infectious, inflammatory, or malignancy (Kim 2010). People with neuropathic bladder from SCI are at significant risk of morbidity from urinary tract infection (UTI); the average is about two episodes annually (Waites 1993). The problem of frequent UTI is amplified by the high prevalence of multiresistant organism(s) (MRO) in SCI populations which combine to exacerbate the clinical, social and economic consequences of disease for this patient population. This makes UTI more expensive and difficult to treat and MRO prevalence more difficult to control (Haran 2007; Kitagawa 2002; Lee 2008; Murphy 2003).
An effective way to prevent UTI in people with neuropathic bladder, especially people with SCI has been sought for many years. In 1998, 73% of patients in an Australian SCI unit were attempting non‐antibiotic based UTI prevention (Lee 2007). A recent randomised controlled trial (RCT) of 305 subjects with SCI conclusively demonstrated that the current common methods of non‐antibiotic UTI prevention were ineffective (Lee 2007). UTI prevention, particularly the more difficult to treat MRO‐UTI, is a clinical imperative for people with SCI and neuropathic bladder.
Thom 1999 showed that up to 73% of patients with SCI in the US become MRO‐colonised during inpatient treatment; and Mylotte 2000 found 44% were colonised with multiresistant Staphylococcus aureus in surveillance cultures. The problem is not confined to hospitals only; Waites 2000 found that 33% of an outpatient SCI population were MRO colonised. High colonisation rates have been attributed to neuropathic bladder and bladder management type (particularly indwelling catheterization), high rates of antibiotic use, mechanical ventilation and pressure ulcers (Girard 2006; Mylotte 2000; Thom 1999; Waites 2000). Girard 2006 found that UTI accounted for the high prevalence of nosocomial infections among people with SCI in rehabilitation units. In most settings continence is most commonly managed using bladder management techniques such as intermittent, indwelling, suprapubic and urethral catheterization; external collection device; or reflex voiding.
Description of the intervention
Currently there is no proven prophylaxis for UTI in people with neuropathic bladder, such as people with SCI. A recent research directions document recommended probiotic studies in SCI for “bacterial interference” of the urological tract to “reduce colonisation by uropathogen and manage the dual problems of infection and pathogen resistance to anti‐microbials” (Hayes 2007). Probiotics are defined as “a preparation of or a product containing viable, defined micro‐organisms in sufficient numbers, which alter the microflora (by implantation or colonisation) in a compartment of the host and by that exert beneficial health effects in this host” (Schrezenmeir 2001). There are many species and strains of probiotics available, prepared in different formulations, and administered through a variety of routes. Falagas 2006 suggested that Lactobacillus rhamnose GR‐1 and Lactobacillus reuteri RC‐14 could be the most effective probiotics for UTI prevention. A dose‐finding RCT determined that oral doses above 8 x 108 colony forming units (CFU)/d were necessary to colonise the vagina and prevent urogenital infection in women (Reid 2001).
How the intervention might work
The most common route of urinary infection is the ascension of host pathogens from the rectum and vagina to the urethra and bladder. Similarly, naturally occurring probiotic organisms in healthy people can spread from the rectum and perineum and form a barrier to uropathogen (Reid 2006). It may be possible to artificially boost probiotic colonisation through probiotic instillation via oral, vaginal or intravesical routes.
The Lactobacillus GR‐1 probiotic strain produces bacteriocins that influence the growth and biofilm development of uropathogen through down‐regulation of the inflammatory processes (Reid 2006). It is reported that a single intravaginal insertion of Lactobacillus GR‐1 can also up‐regulate host defence factors known to be important in fighting infection (Reid 2006). Similarly, studies with Lactobacillus RC‐14 strain have shown that it can up‐regulate mucin production which may act as a barrier to infection (Reid 2006), and down‐regulate virulence factor expression in pathogens such as staphylococci (Laughton 2006). The organism also affects cell membrane components in Escherichia coli and produces biosurfactants that inhibit their adhesion to surfaces (Valraeds 1998). Lactobacillus acidophilus has also been shown to coat biomaterial surfaces and thus decrease the adhesion of uropathogen (Hawthorn 1990) and inhibit Enterococcus faecalis, E. coli and Staphylococcus epidermidis from a urine suspension to silicone rubber (surlactin) (Valraeds 1998).
Why it is important to do this review
For people with a neuropathic bladder, the treatment of a simple UTI is becoming more complicated as the prevalence of MRO‐UTI rises. Such infections can be life threatening, or at the very least, expensive to treat with intravenous antibiotics with the possibility of side‐effects and increased demands on resources (Murphy 2003; Romero‐Vivas 1995). These resource demands include use of isolation rooms and specific isolation wards, more stringent use of personal protective equipment and auditing, plus an increased risk of transmission to other patients. Colonising MRO have the potential to adversely affect the individual should their immune system become compromised or if there is cross‐contamination of body systems (most commonly bowel flora contaminating the urological tract). The most common clinical infection for people with a neuropathic bladder is UTI, for which there are no urinary prophylactic substances with proven efficacy (Falagas 2006; Girard 2006; Haran 2005; Haran 2007; Lee 2008).
Many people with SCI have neuropathic bladder. The high prevalence of MRO colonisation puts people with SCI at high risk of both entry to the hospital system, but also attendant care visits necessary for SCI care among people in the community. MRO clusters that frequently occur in SCI units put other services such as emergency, investigative, ward based, theatre, radiology and outpatient at risk of cross infection and require additional resources and training to manage. Current practice for SCI‐UTI management is that asymptomatic bacteriuria is not treated because it is not associated with adverse urological outcomes in the spinal injured population (Cardenas 1995; NIDRRCS 1992) and contributes to antibiotic resistance.
UTI are likely to pose more problems in the future as organisms continue to become more resistant to available antibiotics. UTI are increasingly difficult and expensive to treat, and therefore, exploring the use of probiotics to reduce MRO colonisation and resultant UTI is crucial to reducing significant health system demands from current and future prevalence. Non‐antibiotic prophylaxis is needed to prevent UTI in people with neuropathic bladder.
Objectives
This review looked at the benefits and harms of probiotics in preventing symptomatic UTI in people with neuropathic bladder compared with placebo, no therapy, or non‐antibiotic prophylaxis (cranberry juice, methenamine hippurate, topical oestrogen).
Methods
Criteria for considering studies for this review
Types of studies
All RCTs, quasi‐RCTs (RCTs in which allocation to treatment was obtained by alternation, use of alternate medical records, date of birth or other predictable methods) and randomised cross‐over studies looking at the use of probiotics for the prophylaxis of UTI in people with neuropathic bladders were considered for inclusion.
Types of participants
Inclusion criteria
Men, women and children of all ages with neuropathic bladders from neurological injury such as suprapontine, supra sacral and sacral aetiologies were included. All bladder management types, including reflex voiding, time voiding, indwelling and intermittent catheterization were eligible for this review.
Exclusion criteria
Men, women and children with normal bladders were excluded. Normal bladder is defined as absence of a neurological condition causing neuropathic bladder.
Types of interventions
Inclusion criteria
-
Studies evaluating probiotic products administered with the objective of preventing UTI were sought. There were no restrictions based on the dose, frequency, formulation, duration or mode of administration of the product. Studies comparing probiotics to placebo, no treatment or other non‐antibiotic prophylaxis were included.
Exclusion criteria
-
Studies involving treatment of symptomatic UTI with probiotics were excluded.
-
Studies comparing probiotics with antibiotics or in combination with antibiotics as prophylaxis were beyond the scope of this review and were excluded.
Types of outcome measures
Numbers of occurrences of each of the following outcome measures were examined. A comparison with control were made during and after the treatment period.
Primary outcomes
-
Symptomatic urinary tract infection
-
The primary outcome measure was the number of symptomatic UTI according to defined clinical criteria, along with a positive quantitative urine culture. This is the most clinically significant outcome measure for populations at long‐term risk of recurrent UTI, such as people with neuropathic bladder.
-
Symptoms of UTI in the general population include dysuria, frequency, urgency, voiding of small volumes, abrupt onset, suprapubic pain, and presence of pyuria (Stamm 1988). In SCI patients, relevant symptoms should be explained by other intercurrent pathology and include: temperature, autonomic dysreflexia, increased frequency of muscle spasms or spasticity, failure of usual control of urinary incontinence, and new abdominal discomfort (NIDRRCS 1992).
-
-
Quantitative urine culture
-
Numbers of UTI confirmed by appropriate microbiological criteria. Bacteriuria on quantitative urine analysis of more than 100,000 organisms of a single species/mL was the accepted standard; however, the colony count may vary from 100 to 100,000 depending on the clinical setting (Stamm 1988). Therefore in some situations, such as a clean suprapubic tap, a colony count of less than 100,000 was acceptable.
-
Secondary outcomes
-
Numbers with at least one asymptomatic bacterial UTI
-
Asymptomatic bacteriuria refers to isolation of a specified quantitative count of bacteria in an appropriately collected urine specimen from a person without symptoms of signs referable to urinary infection (Nicolle 2005). According to the Infectious Disease Society of America (Nicolle 2005):
-
-
For asymptomatic women, bacteriuria is defined as two consecutive voided urine specimens with isolation of the same bacterial strain in quantitative counts ≥ 100,000 CFU/mL
-
A single, clean‐catch voided urine specimen with one bacterial species isolated in a quantitative count ≥ 100,000 CFU/mL identifies bacteriuria in men
-
A single catheterised urine specimen with one bacterial species isolated in a quantitative count ≥ 100 CFU/mL identifies bacteriuria in women or men
-
In children any bacteria isolated, regardless of the quantitative count on suprapubic aspiration or catheter urine identifies bacteriuria (Kilham 2009).
-
-
Adverse reactions
-
Adverse reactions were recorded as the proportion of people who reported side effects, and a description of these side effects such as bloating, flatulence, diarrhoea or any alteration to bowel movements (Fioramonti 2003). We also reported numbers of people who withdrew from studies due to side effects; a description of these side effects were included.
-
Numbers of patients with at least one confirmed case of bacteraemia or fungaemia on blood cultures were reported. Rare cases of bacteraemia, fungaemia, and infections in other body organs have been reported (Marteau 2003).
-
Search methods for identification of studies
Electronic searches
We searched the Cochrane Kidney and Transplant Specialised Register up to 10 March 2017 through contact with the Information Specialist using search terms relevant to this review. The Specialised Register contain studies identified from the following sources.
-
Monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL)
-
Weekly searches of MEDLINE OVID SP
-
Handsearching of kidney‐related journals and the proceedings of major kidney conferences
-
Searching of the current year of EMBASE OVID SP
-
Weekly current awareness alerts for selected kidney and transplant journals
-
Searches of the International Clinical Trials Register (ICTRP) Search Portal and ClinicalTrials.gov.
Studies contained in the Specialised Register were identified through search strategies for CENTRAL, MEDLINE, and EMBASE based on the scope of Cochrane Kidney and Transplant. Details of these strategies, as well as a list of handsearched journals, conference proceedings and current awareness alerts, are available in the Specialised Register section of information about Cochrane Kidney and Transplant.
See Appendix 1 for search terms used in strategies for this review.
Searching other resources
-
Reference lists of clinical practice guidelines, review articles and relevant studies.
-
Letters seeking information about unpublished or incomplete studies to investigators known to be involved in previous studies.
Data collection and analysis
Selection of studies
The search strategies described were used to obtain titles and abstracts of studies that may be relevant to the review. Titles and abstracts were screened independently by two authors, who discarded studies that were not applicable; however, studies and reviews that might include relevant data or information on studies were retained initially. Two authors independently assessed retrieved abstracts and, if necessary the full text, of these studies to determine which studies satisfy the inclusion criteria.
Data extraction and management
Data extraction were carried out independently by two authors using standard data extraction forms. Studies reported in non‐English language journals were to be translated before assessment. Where more than one publication of one study exists, reports were grouped together and the publication with the most complete data was used in the analyses. When relevant outcomes were only published in earlier versions these data were used. Any discrepancy between published versions were highlighted.
Assessment of risk of bias in included studies
The following items were assessed using the risk of bias assessment tool (Higgins 2011) (see Appendix 2).
-
Was there adequate sequence generation (selection bias)?
-
Was allocation adequately concealed (selection bias)?
-
Was knowledge of the allocated interventions adequately prevented during the study?
-
Participants and personnel (selection bias)
-
Outcome assessors (detection bias)
-
-
Were incomplete outcome data adequately addressed (attrition bias)?
-
Are reports of the study free of suggestion of selective outcome reporting (reporting bias)?
-
Was the study apparently free of other problems that could put it at a risk of bias?
Measures of treatment effect
For dichotomous outcomes (e.g. symptomatic UTI, bacteriuria, positive urine culture) results were expressed as risk ratio (RR) with 95% confidence intervals (CI). Where continuous scales of measurement are used to assess the effects of treatment (e.g. time to UTI), the mean difference (MD) were to be used, or the standardised mean difference (SMD) if different scales had been used.
Unit of analysis issues
Care was taken in situations where total numbers of events are reported. Authors did not have to be contacted for clarification to distinguish the number of people who had events from the total number of events. Clarification did not need to be sought from authors to differentiate numbers of people who had events and numbers of events/person. Authors were contacted in situations where data were incomplete or censored. In cases where clarification could not be obtained from primary study data to resolve episodes of participant discrepancy, a narrative summary of data was presented, but these data were not included in the meta‐analysis for that outcome.
In studies that have two or more experimental arms, we investigated the most appropriate approach to pool results for meta‐analysis. If a consensus approach could not be reached, statistical support was sought to resolve the method to be applied. For randomised cross‐over studies, data to the point of first cross‐over were used for pooling into a meta‐analysis.
Dealing with missing data
Any further information required from the original author was requested by written correspondence (e.g. emailing corresponding author/s) and any relevant information obtained in this manner was included in the review. Evaluation of important numerical data such as screened, randomised patients as well as intention‐to‐treat, as‐treated and per‐protocol population were carefully performed. Attrition rates, for example drop‐outs, losses to follow‐up and withdrawals were investigated. Issues of missing data and imputation methods (for example, last‐observation‐carried‐forward) were critically appraised (Higgins 2011).
Assessment of heterogeneity
We first assessed the heterogeneity by visual inspection of the forest plot. Heterogeneity was then analysed using a Chi2 test on N‐1 degrees of freedom, with an alpha of 0.05 used for statistical significance and with the I² test (Higgins 2003). A guide to the interpretation of I2 values is as follows.
-
0% to 40%: might not be important
-
30% to 60%: may represent moderate heterogeneity
-
50% to 90%: may represent substantial heterogeneity
-
75% to 100%: considerable heterogeneity.
The importance of the observed value of I2 depends on the magnitude and direction of treatment effects and the strength of evidence for heterogeneity (e.g. P‐value from the Chi2 test, or a confidence interval for I2) (Higgins 2011).
Assessment of reporting biases
If possible, funnel plots were used to assess for the potential existence of small study bias (Higgins 2011).
Data synthesis
Data was pooled using the random‐effects model but the fixed‐effect model were also used to ensure robustness of the model chosen and susceptibility to outliers.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis were used to explore possible sources of heterogeneity (e.g. participants, interventions and study quality). Heterogeneity among participants could be related to age, duration since SCI and presence of abnormal renal tract pathology. Subgroup analyses may be performed for those with and without SCI, and those with neuropathic bladders of supra sacral or sacral origin. Heterogeneity in treatments could be related to route of administration of the probiotics (oral versus direct bladder inoculation), duration of therapy (less or more than one month), number of probiotics and concurrent use of probiotics and other non‐antibiotic urinary antiseptics. Adverse effects were tabulated and assessed with descriptive techniques, as they are likely to be different for the various agents used. Where possible, the risk difference with 95% CI were calculated for each adverse effect, either compared to no treatment or to another agent.
Sensitivity analysis
Sensitivity analysis to assess for whether conclusions are robust were undertaken separately for the following categories.
-
Studies with proper randomisation and concealment of allocation compared to those without these characteristics.
-
Studies performed with and without intention‐to‐treat analyses.
-
Data are missing from the treatment arm and these patients were assumed to have the worst possible outcome.
'Summary of findings' tables
We presented the main results of the review in 'Summary of findings' tables. These tables present key information concerning the quality of the evidence, the magnitude of the effects of the interventions examined, and the sum of the available data for the main outcomes (Schünemann 2011a). The 'Summary of findings' tables also include an overall grading of the evidence related to each of the main outcomes using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach (GRADE 2008). The GRADE approach defines the quality of a body of evidence as the extent to which one can be confident that an estimate of effect or association is close to the true quantity of specific interest. The quality of a body of evidence involves consideration of within‐trial risk of bias (methodological quality), directness of evidence, heterogeneity, precision of effect estimates and risk of publication bias (Schünemann 2011b). We presented the following outcome in the 'Summary of findings' tables.
-
Symptomatic UTI
Other outcomes like quantitative urine culture, asymptomatic UTI and adverse events were unable to be included in the Summary of Findings table due to lack of data.
Results
Description of studies
Results of the search
We searched the Specialised Register and identified 63 records. After checking the references lists an addition eight records were identified. Titles and abstracts were screened and 49 records were excluded (not RCT, wrong population or intervention). The remaining 22 records represented 12 studies. After full‐text review, three studies (five records) were included and eight studies (15 records) were excluded.
One ongoing study was identified (ProSCIUTTU Study 2016) and will be assessed in a future update of this review (Figure 1).

Study flow diagram.
Included studies
Three studies (Darouiche 2005; Darouiche 2011; Sunden 2010) were included enrolling 110 participants (see Characteristics of included studies). All three studies were randomised, placebo‐controlled, double‐blind RCTs involving intravesical instillation of non‐pathogenic E. coli for the prevention of UTI in people with neuropathic bladder. We did not identify any study which evaluated other routes of administration or other types of probiotics.
Two E. coli strains were used ‐ E. coli HU2117 (Darouiche 2011) and E. coli 83972 (Darouiche 2005; Sunden 2010). All three studies involved inserting 10 to 30 mL of fluid containing either normal saline or E. coli suspension directly into the bladder once or twice/day for three consecutive days. Two studies enrolled persons with known neuropathic bladder (Darouiche 2005; Darouiche 2011). More than 40% of the participants in Sunden 2010 had participants with known neuropathic bladder. There was heterogeneity in bladder management type between the three studies with intermittent catheterization being predominant in Sunden 2010 and indwelling or suprapubic catheterization being predominant in Darouiche 2005. All three studies had an adequate follow‐up period of one year or more.
Symptomatic UTI was measured in all three studies. Two studies (Darouiche 2005; Darouiche 2011) used similar criteria for diagnosing symptomatic UTI which was a combination of symptoms as well as microbiological urine culture. Bacteriuria of ≥ 105 CFU/mL with symptoms were classified as UTI. Sunden 2010 defined UTI on self‐reported symptoms by participants only, although they did perform urine cultures for confirmation.
Two studies reported adverse events (Darouiche 2005; Sunden 2010). Sunden 2010 reported that there was an absence of serious side effects such as pyelonephritis. Darouiche 2005 reported one episode of autonomic dysreflexia occurring in one patient during bladder instillation which was resolved after the catheter used for instillation was unclamped. Sunden 2010 reported symptomatic UTI in participants who had long‐term colonisation with E. coli 83972 but these symptoms were easily resolved with appropriate antibiotic therapy.
Two studies had grants from non‐profit organisation (Darouiche 2005; Darouiche 2011). Sunden 2010 had their majority of funding from non‐profit organisation although they did disclose some funding from a commercial company.
Excluded studies
Eight studies were excluded (see Characteristics of excluded studies). Two studies did not enrol participants with neuropathic bladder (Czaja 2007; Kontiokari 2001); four compared probiotics to antibiotics, which was outside the scope of this review (Lee 2007a; Mohseni 2013; NAPRUTI Study II 2006; Reid 1992); and two studies were terminated before the participants were enrolled (NCT00767988; NCT00789464).
Risk of bias in included studies

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
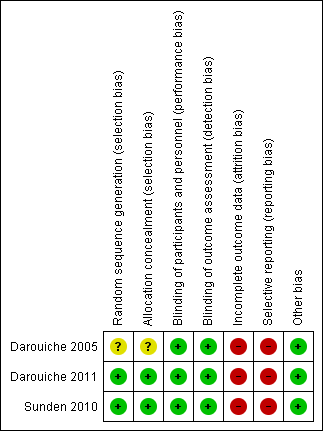
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation was computer generated in two studies (low risk) (Darouiche 2011; Sunden 2010) and not reported in the third study (unclear risk) (Darouiche 2005).
Allocation concealment was not reported in one study (unclear risk) (Darouiche 2005) and was adequate in two studies (low risk) (Darouiche 2011; Sunden 2010).
Blinding
Blinding of participants was reported in all three studies (Darouiche 2005; Darouiche 2011; Sunden 2010). It was stated that assessors were also blinded in all three studies (Darouiche 2005; Darouiche 2011; Sunden 2010).
Incomplete outcome data
All three studies (Darouiche 2005; Darouiche 2011; Sunden 2010) had high risk of bias due to attrition as they either excluded analysing patients who failed bladder colonisation with E. coli in the results they analysed or included them in the placebo arm to analyse post randomisation which violates the intention to treat principle. Darouiche 2011 had more than 50% dropouts post randomisation and majority were in the treatment arm.
Selective reporting
Two studies did not have secondary outcomes of interest to our review (Darouiche 2005; Sunden 2010) and Darouiche 2011 outlined the practical limitations of this procedure in preventing UTI. Our prespecified secondary outcome of asymptomatic UTI were not addressed by any of the studies.
Other potential sources of bias
All studies appeared to be free of other biases.
Effects of interventions
Symptomatic urinary tract infection
There was consistency in definition of symptomatic UTI in all three studies. Symptomatic UTI were defined as a constellation of symptoms as well as presence of bacteriuria or pyuria (Darouiche 2005; Darouiche 2011; Sunden 2010). Symptoms that all studies considered were relevant to diagnose UTI were adequately defined e.g. fever, suprapubic pain, frequency, urgency and for spinal cord patients, autonomic dysreflexia and increased spasticity.
Successful bladder colonisation with E. coli varied with different strains. The E. coli 83972 strain had success rates of 60% to 70% (Darouiche 2005; Sunden 2010) but the E. coli HU2117 only had a 37% success rate of inoculation (Darouiche 2011). In those patients who had successful colonisation with E. coli:
-
The time to first symptomatic UTI post successful colonisation was longer: Sunden 2010 reported median 11.3 months in treatment group versus 5.7 months in placebo, P = 0.013 with E. coli 83972
-
The number of symptomatic UTI in the follow up one year period was lower: Darouiche 2005 reported 46% in treatment group versus 93% in placebo group reported at least 1 episode of UTI (P = 0.01) with E. coli 83972; Darouiche 2011 reported 29% in treatment group versus 70% in placebo group reported at least one episode of UTI, (P = 0.49) with E. coli HU2117.
It is uncertain if the risk of symptomatic UTI is reduced with bladder inoculation using E. coli because the certainty of the evidence is very low (Analysis 1.1 (3 studies, 110 participants): RR 0.32, 95% CI 0.08 to 1.19; I2 = 82%). As Sunden 2010 was a cross‐over study, for the meta‐analysis, only the results of the first part of the cross‐over were included.
Quantitative urine culture
Two studies (Darouiche 2005; Darouiche 2011) defined microbiological diagnosis of symptomatic UTI i.e. bacteriuria on quantitative urine analysis of more than 100,000 organisms or CFU/mL. Two studies (Darouiche 2005; Darouiche 2011) also accepted symptoms and the presence of pyuria (> 10 white blood cells/high power field) as diagnostic of UTI. Sunden 2010 did not define what they considered "uropathogenic growth" or how they established successful colonisation although they mentioned that urine cultures were taken.
Asymptomatic urinary tract infections
Asymptomatic bacteriuria was not considered an outcome measure in any of the included studies. It was defined in two studies (Darouiche 2005; Darouiche 2011) to establish successful inoculation. As both studies were from the same group of investigators, they defined it as growth of ≥ 103 CFU/mL.
None of the studies reported on the rate of asymptomatic bacteriuria or asymptomatic UTI post intervention.
Adverse events
Reporting of adverse events is limited as only two studies reported adverse events (Darouiche 2005; Sunden 2010). Darouiche 2005 reported one episode of autonomic dysreflexia as well as absence of septicaemia and UTI attributable for E. coli 83972. Sunden 2010 commented that there were no significant side effects including pyelonephritis. In a later second publication, Sunden 2010 reported symptomatic UTI in participants who had long‐term colonisation with E. coli 83972 but these symptoms were easily resolved with appropriate antibiotic therapy.
While being reported as "generally safe", bladder instillation is an invasive form of intervention which demands a high level of commitment on the part of patients. The secondary outcome in Darouiche 2011 investigated the practical limitations of inducing and maintaining bladder colonisation. They reported declining participant participation as instillation cycles increased as it required three full day clinic visits per instillation cycle and cycles may have to be repeated.
Discussion
Summary of main results
In this review, there were no studies identified that evaluated oral probiotics in preventing UTI in people with neuropathic bladder. Most of the evidence for preventing or prolonging UTI in people with neuropathic bladders are derived from three studies involving intravesical instillation of non‐pathogenic E. coli involving mainly the population with neuropathic bladder from SCI.
It is uncertain if the risk of symptomatic UTI is reduced with bladder inoculation using E. coli because the certainty of the evidence is very low (RR 0.32, 95% CI 0.08 to 1.19). Heterogeneity was high, numbers of participants per study small, and there was a high risk of attrition and reporting bias.
We conclude that the quality of evidence is very low to determine whether intravesical instillation with E. coli compared to placebo will lead to UTI prevention in people with neuropathic bladder.
Moreover, the success of intravesical installation with non‐pathogenic bacteria is variable. There are also practical limitations to carrying out the procedure as it involves high patient compliance and dedication. The procedure also needs to be repeated as the bacteria can be spontaneously cleared, especially if there is concurrent use of antibiotics.
Adverse events were also poorly reported in all studies although the procedure was reported as "generally safe". Hence, there are outstanding uncertainties as to whether the benefits of intravesical instillation outweigh the harms.
Overall completeness and applicability of evidence
This review suggests that there is a lack of evidence (few studies) that intravesical instillation with non‐pathogenic bacteria in adults with neuropathic bladder is effective in preventing symptomatic UTI.
Due to multiple exclusion criteria in these small studies, especially in relation to immunosuppression, presence of other infections, and other urogenital tract intervention/abnormalities, the limited evidence is only applicable to a selective group of the adult population with neuropathic bladder. In addition, there is heterogeneity between bladder management types as well as male predominance between the studies.
From the evidence presented and due to variable success rates, the need for strict adherence to instillation protocols together with high attrition rates in these studies, intravesical instillation with non‐pathogenic bacteria is unlikely to be a widely accepted intervention. However, with innovative therapy and with additional support for participants undergoing this procedure, it may be worthy of further study.
Quality of the evidence
Overall, the studies were of poor quality. All three studies (Darouiche 2005; Darouiche 2011; Sunden 2010) investigated patients with neuropathic bladder had adequate performance and detection bias, but had high attrition and reporting bias. The main weakness in all three studies was exclusion from analysis of patients who failed inoculation or analysing them in the placebo arm post randomisation (i.e. not analysing via intention‐to‐treat). Failure of an intention‐to‐treat analysis undermines the randomisation process and weakened the results of the studies. There was also a high gender bias in two studies. (Darouiche 2005; Darouiche 2011).
Potential biases in the review process
Publication bias could not be fully excluded. Bias from the literature search was attempted to be controlled by: Cochrane independently performing literature searches as well as two other authors using hand searching and searching multiple databases as well as references from included studies. No language restrictions were applied. Letters, abstracts and unpublished studies were accepted to reduce publication bias. If a duplicate publication was suspected, it was screened by two authors, and if confirmed, the publication with the most and/or the longest follow‐up data was used for the review.
[Escherichia coli (explode)] was not used as a search term in this review as it did not yield any additional studies.
Agreements and disagreements with other studies or reviews
To date, there is no known systematic review conducted in regards to probiotics in patients with neuropathic bladder. There are also no known reported studies of bladder inoculation of non‐pathogenic bacteria in children or normal adult population with recurrent UTI.
From literature review, there are other pilot non‐RCTs which have been conducted (Darouiche 2001; Hull 2000; Prasad 2009) mainly by the same research group which reported lower rates of UTI per year in participants with successful colonisers compared to the year prior to intervention. There is also one small pilot non‐RCT (Uehera 2006) which reported a reduction in UTI recurrence in patients with neuropathic bladder with daily insertion of Lactobacillus vaginal suppositories. To date, no other studies involving probiotic vaginal suppositories in women with neurogenic bladders have been conducted.
The authors are aware that there is a Cochrane review regarding probiotics for preventing UTI in adults and children (Schwenger 2015). Our review also concurs with theirs that there is currently low evidence of probiotics in preventing UTI, with overestimation of treatment effect and high risk of bias although their conclusion apply to a broader patient population. In regards to the efficacy of probiotics in other patient population, in the systemic review conducted by Barrons 2008, the authors conclude that studies of lactobacilli for prophylaxis in UTI in women remain inconclusive. NAPRUTI Study II 2006 reported that oral capsules of Lactobacillus rhamnose GR‐1 and Lactobacillus reuteri RC‐14 did reduced the mean number of symptomatic UTI in post‐menopausal women with recurrent UTI. However, the combination probiotics did not meet the non‐inferiority criteria in preventing UTI compared with trimethoprim‐sulfamethoxazole. In children, a review by Nickavar 2011 concluded that there is insufficient data about the preventative effects of probiotics in recurrent UTI for that population.
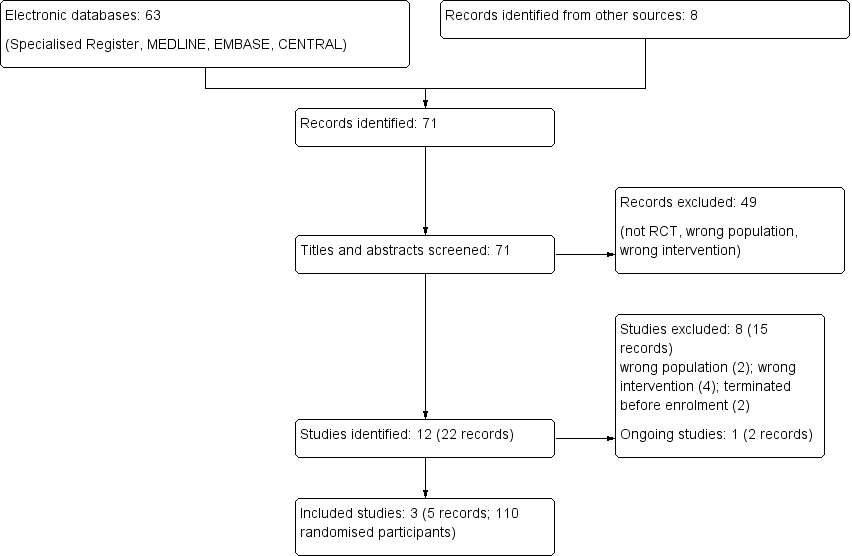
Study flow diagram.
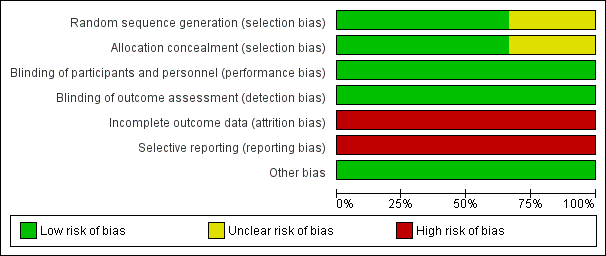
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
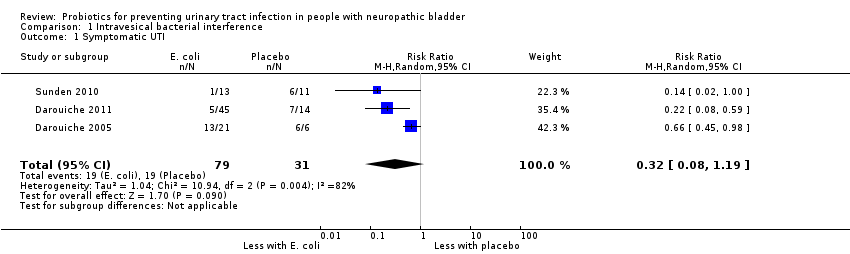
Comparison 1 Intravesical bacterial interference, Outcome 1 Symptomatic UTI.
| Intravesical bacterial interference versus placebo for preventing urinary tract infection in people with neuropathic bladder | |||||
| Patient or population: people with neuropathic bladder | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants (studies) | Quality of the evidence | |
| Risk with placebo | Risk with intravesical bacterial interference | ||||
| Symptomatic UTI | 613 per 1,000 | 196 per 1,000 | RR 0.32 | 110 (3) | ⊕⊝⊝⊝1 |
| GRADE Working Group grades of evidence | |||||
| 1Risk of bias was assessed at high in most domains, with heterogeneity and small studies, suggesting that results overestimate intravesical bacterial interference versus placebo | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Symptomatic UTI Show forest plot | 3 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.08, 1.19] |

