Farmacoterapia combinada para el tratamiento de la fibromialgia en adultos
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Randomised, double‐blind, parallel‐group design study | |
| Participants | 42 people with FM of both genders, aged 18‐60 years, were included in the study after approval by the Ethics Committee (number 1711/09) and signing the consent form. Participants' inclusion followed the 1990 ACR criteria | |
| Interventions | Group 1: 240 mg lidocaine in 125 mL of saline solution, once a week for 4 weeks (T1, T2, T3 and T4) Group 2: 125 mL of saline, once a week for 4 weeks (T1, T2, T3 and T4) All participants received amitriptyline | |
| Outcomes | The following were assessed: pain intensity before treatment (T0) and at 1, 2, 3, 4 and 8 weeks after treatment; clinical manifestations; FIQ before and at 4 and 8 weeks after; the levels of IL 1, 6 and 8 before and at 4 and 8 weeks after treatment | |
| Notes | This study was registered in ClinicalTrials.Gov ID: NCT01391598 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using Randomizer software (Urbaniak & Plous, Lancaster, PA, USA). The randomly selected groups were placed in numbered envelopes. The envelopes were then randomly selected on the day of administration of the solution to define in which group each patient was included. The solution was prepared by a nurse, and the researcher did not know which treatment the participants were receiving. |
| Allocation concealment (selection bias) | Unclear risk | Blinding method not described. "This work was a prospective, randomized, double‐blind and placebo‐controlled study." |
| Blinding of participants and personnel (performance bias) | Unclear risk | Blinding method not described. "This work was a prospective, randomized, double‐blind and placebo‐controlled study." |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding method not described. "This work was a prospective, randomized, double‐blind and placebo‐controlled study." |
| Incomplete outcome data (attrition bias) | Unclear risk | Four participants (2/group) lost to follow‐up and no mention of ITT analysis or handling of missing data |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section are reported in the results section. |
| Size of study | Unclear risk | 4 weeks' trial duration may be associated with a higher risk of bias compared to ≥ 12 weeks |
| Trial Duration | Unclear risk | 19 participants per treatment arm may be associated with a higher risk of bias compared to ≥ 50 |
| Similarities of Baseline Characteristics | Unclear risk | No significant differences between treatment groups |
| Study characteristics | ||
| Methods | Multicentre, randomised, double‐blind, placebo‐controlled, parallel‐design, 13‐week trial | |
| Participants | 18‐75 year olds diagnosed with FM using 1990 ACR criteria, with pain scores of ≥ 40 mm on a 100 mm VAS. 443 were screened, 315 were randomised, 313 were eligible for ITT efficacy analysis, and 312 were eligible for safety analysis. Mean age: 49 (active treatment arm); 51 (placebo arm); proportion of women: 93% (active treatment arm) and 95% (placebo arm) Screening and washout phase occurred for up to 3 weeks before study start. Potential participants were excluded if tramadol therapy had failed previously, if they had used tramadol within the prior 30 days, and if they had any other pain that was more severe than FM pain. | |
| Interventions | Tramadol/paracetamol (acetaminophen): 1 tablet/d containing 37.5 mg tramadol and 325 mg paracetamol (acetaminophen) titrated up over 10 days to 4 tablets/d; thereafter, 1‐2 tablets 4 times/d up to a maximum of 8 tablets daily (300 mg tramadol + 2600 mg paracetamol (acetaminophen)); versus Placebo: matching placebo was given in a similar schedule. Both treatments lasted 13 weeks. | |
| Outcomes | Time to discontinuation due to lack of efficacy or any reason, pain on a 100 mm VAS, pain relief rating scale from ‐1 to 4, and adverse events, all recorded on days 1, 14, 28, 56, and 91; number of tender points (of 18), myalgic score (0‐3), 10‐item FIQ, SF‐36, and 12‐item sleep questionnaire, all recorded at the first (day 1) and last (day 91) visits. Adverse events were also recorded at each study visit; these were either spontaneously reported by the participants or reported in response to general nondirected questioning. | |
| Notes | Of 315 randomised, 175 withdrew (77 from active treatment, 98 from placebo arm); efficacy analysis was on an ITT basis, for which there were 313 eligible participants (took at least 1 dose of medication and had at least 1 efficacy measurement taken); 312 participants were used in safety analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were assigned sequentially in 1:1 fashion at each site using a randomised list of medication codes", but how the randomised list was generated is unclear. |
| Allocation concealment (selection bias) | Low risk | "Tramadol/paracetamol (acetaminophen) or matching placebo tablets were prepared by the sponsor and dispensed in bottles containing 100 tablets." |
| Blinding of participants and personnel (performance bias) | Low risk | "Each bottle had a two‐part tear‐off label; study medication identification was concealed and could only be revealed in case of emergency. Treatment assignments were not revealed to study subjects, investigators, clinical staff, or study monitors until all subjects had completed therapy and the database had been finalized." |
| Blinding of outcome assessment (detection bias) | Low risk | "Treatment assignments were not revealed to study subjects, investigators, clinical staff, or study monitors until all subjects had completed therapy and the database had been finalized." |
| Incomplete outcome data (attrition bias) | Low risk | 77/158 combination arm participants discontinued prematurely (39 due to lack of efficacy), and 98/157 placebo arm participants discontinued prematurely (72 due to lack of efficacy). Other reasons for premature discontinuation were protocol violation, adverse events, choice, and loss to follow‐up. Distribution was even between the groups (more discontinued from the placebo arm due to lack of efficacy, but this was the primary outcome of the study). |
| Selective reporting (reporting bias) | Unclear risk | The protocol for this trial was not registered. |
| Size of study | Unclear risk | 50‐199 participants per arm (156 in the combination arm, and 157 in the placebo arm) |
| Trial Duration | Low risk | ≥ 7 weeks (13‐week trial) |
| Similarities of Baseline Characteristics | Low risk | There were no significant differences between groups in terms of age, sex ratio, and pain scores at baseline |
| Study characteristics | ||
| Methods | Randomised, double‐blind, parallel‐design, 6‐week trial | |
| Participants | 18‐65 year old women diagnosed with FM using the 2010 ACR criteria, who were refractory to their current treatments, and who had a pain score of ≥ 50 on a 100 mm VAS during the baseline week before randomisation. 63 participants were randomised; 57 participants completed the study; all 63 participants were included in the statistical analyses on an ITT basis. Mean age: 49.8 (amitriptyline), 47.4 (melatonin), 49.7 (amitriptyline + melatonin). Participants were allowed to remain on medications, but the medication doses could not be adjusted once the study started. Potential participants were excluded if they had inflammatory rheumatic disease, autoimmune disease, other painful disorder, history of substance abuse, pregnant or breastfeeding, or history of neurologic, oncologic, or ischemics heart disease, or kidney or hepatic insufficiency. Participants were not excluded if they had a history of major depressive disorder as long as it wasn't the main reason for their functional impairment or study enrolment. | |
| Interventions | Amitriptyline + melatonin: 25 mg amitriptyline + 10 mg melatonin at bedtime every day; versus Amitriptyline + placebo: 25 mg amitriptyline + placebo at bedtime every day; versus Melatonin + placebo: 10 mg melatonin + placebo at bedtime every day All treatments lasted 6 weeks | |
| Outcomes | Pain scores on a 100 mm VAS recorded daily during the week before treatment and during the last week of treatment; pain reduction on a NPS from 0‐10 during the conditioned pain modulation task; amount of analgesics used during the last week of treatment; number of tender points; FIQ scores; pressure pain thresholds assessed using an algometer; Pittsburgh Sleep Quality Index; and brain‐derived neurotrophic factor serum levels. Outcomes were assessed at baseline and after 6 weeks of treatment. Adverse events were assessed through questioning about any changes that occurred during treatment. | |
| Notes | Small trial: 21 participants per arm | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Before the recruitment phase, envelopes containing the protocol materials were prepared. Each envelope was sealed and numbered sequentially and contained an allocated treatment." However, it is not clear how the randomisation was obtained. |
| Allocation concealment (selection bias) | Low risk | "Each envelope was sealed and numbered sequentially and contained an allocated treatment. After the participant consented to participate in the trial, in the sequence, the nurse, who administered the medications, opened the envelope. During the entire protocol timeline, two investigators who were not involved in patient evaluations were responsible for blinding and randomization procedures. Other individuals who were involved in patient care were unaware of the treatment group to which the patients belonged." |
| Blinding of participants and personnel (performance bias) | Low risk | All participants took the same number of capsules, regardless of whether they contained active or placebo medication. "The capsules were manufactured in such a way that the placebo and active treatment had the same size, color, smell and flavor." |
| Blinding of outcome assessment (detection bias) | Low risk | "Other individuals who were involved in patient care were unaware of the treatment group to which the patients belonged...Two independent medical examiners that were blind to the group assignments were trained to administer the pain scales and conduct the psychological tests." "We used the double‐dummy method and shield placement to prevent the patient and team members from following the patients to control assessment bias." |
| Incomplete outcome data (attrition bias) | Low risk | 21 participants per group were recruited; 2 participants per group withdrew before study completion due to major side effects. Withdrawals from the study were evenly distributed across groups. |
| Selective reporting (reporting bias) | Low risk | Protocol registered at www.clinicaltrials.gov was comparable to the published data reported. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (6‐week trial) |
| Similarities of Baseline Characteristics | High risk | There was no statistically significant difference between groups in terms of sex ratio and age at baseline. But pain scores were significantly higher in the combination group than the other groups at baseline. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, cross‐over design, four 6‐week period trial | |
| Participants | 18‐70 year olds diagnosed with FM using the 1990 ACR criteria, who had daily pain scores of ≥ 4/10 for ≥ 3 months, with alanine transaminase (ALT) and aspartate transaminase (AST) ≤ 20% and serum creatinine ≤ 50% than the upper normal limit. Participants were required to discontinue prohibited drugs starting 7 days before study treatment. Participants could take NSAIDs, paracetamol (acetaminophen), and/or opioids (≤ 200 mg oral morphine equivalents) at a steady dose throughout the trial. 41 participants were recruited; 33 participants completed all 4 treatment periods; 39 participants completed at least 2 treatment periods, and were included in efficacy analyses. All 41 participants who took at least 1 dose of any medication on trial were included in adverse event analyses. Median age: 56; 88% of participants were female. Potential participants were excluded if they had a painful condition as severe as (or worse than) but distinct from FM, major organ system disease, hypersensitivity to any study drugs, severe mood disorder, history of significant abuse of illicit drugs, prescription drugs, or alcohol, uncontrolled hypertension, diabetes, HIV, narrow‐angle glaucoma, or malignancies, if they were taking drugs that interact adversely with study drugs, if they had problems of fructose intolerance, glucose galactose malabsorption, or sucrose isomaltase insufficiency, or if they were pregnant or breastfeeding. | |
| Interventions | Pregabalin + duloxetine: 75 mg pregabalin twice a day + 30 mg duloxetine twice a day, both titrated up to the MTD during the first 24 days of treatment (to a maximum of 450 mg pregabalin and 120 mg duloxetine), remaining at the MTD from days 25‐31, and tapering down from days 32‐41, with day 42 a complete washout; versus Pregabalin + placebo: pregabalin in the same regimen described above + placebo capsules; versus Duloxetine + placebo: duloxetine in the same regimen described above + placebo capsules; versus Double placebo: placebo capsules only. Treatments lasted 6 weeks each | |
| Outcomes | The following outcomes were assessed during the 7 days at MTD: pain intensity over the past 24 h, worst pain intensity over the past 24 h, and nocturnal pain intensity, each rated on a NRS from 0‐10 every day and averaged across the 7 days; global pain relief from ‐1 to 4; SSF‐MPQ; FIQ; Brief Pain Inventory; Beck Depression Inventory‐II; SF‐36; Beck Anxiety Inventory; Medical Outcomes Study Sleep Scale; number of tender points; blinding questionnaires; and study drug MTDs. Adverse events were also evaluated by open‐ended questioning over the phone twice a week with a research nurse. | |
| Notes | Small trial: 39 participants analyzed for treatment efficacy. The study was stopped prematurely due to an interim analysis that indicated superiority of the combination treatment over 1 monotherapy treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "As per a balanced Latin Square crossover, double‐dummy design, participants were allocated, in a double‐blind randomised fashion, to one of 24 possible sequences. A trial pharmacist prepared a concealed allocation schedule by computer‐randomizing these sequences, in blocks of four, to a consecutive number series. Participants were assigned the next consecutive number and the corresponding sequence of study medications was dispensed." |
| Allocation concealment (selection bias) | Low risk | "A trial pharmacist prepared a concealed allocation schedule." |
| Blinding of participants and personnel (performance bias) | Low risk | "For each set of capsules, active drug and placebo capsules were identical in appearance." "According to blinding questionnaire responses, correct guesses about treatment assignment among participants receiving placebo, pregabalin, duloxetine, and combination were made by 52%, 38%, 43%, and 31% of participants respectively." |
| Blinding of outcome assessment (detection bias) | Low risk | "Among participants receiving placebo, pregabalin, duloxetine, and combination, correct guesses made by the research nurse about treatment assignment were made for 45%, 29%, 43%, and 34%, respectively." |
| Incomplete outcome data (attrition bias) | Low risk | The number of study dropouts and the reasons for withdrawal are outlined in the text and in Figure 1. Of 41 participants recruited, 39 were included in efficacy analyses (those who completed at least 2 treatment periods). 33 participants completed all 4 treatment periods. |
| Selective reporting (reporting bias) | Low risk | Protocol registered at www.controlled‐trials.com was comparable to the published data reported |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (6‐week treatment periods) |
| Similarities of Baseline Characteristics | Low risk | Age, sex ratio, and pain scores were reported at baseline. Statistical comparisons were not made between groups, but since this is a cross‐over trial, little difference is expected |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, parallel design, 6‐week trial | |
| Participants | Men and women who met the diagnostic criteria for FM modified from Yunus 1981, and who scored ≥ a 4 on a 10 cm VAS evaluating either pain or FM symptoms; 62 participants were randomised, and 58 completed the study Mean age: 43.8; 95% of the participants were female. Analgesics, antidepressants, anti‐inflammatory medications, sleeping medications, and other central nervous system‐active medications were discontinued 72 h before the first study visit; 10% of participants, evenly distributed across treatment groups, took the only allowable medication (paracetamol [acetaminophen]) aside from study drugs. Potential participants were excluded if they had a history of peptic ulcer disease or cardiac arrhythmias, or if they were taking medications that could not be stopped. | |
| Interventions | Amitriptyline + naproxen: 500 mg naproxen twice/d + 25 mg amitriptyline once/night; versus Naproxen + placebo: 500 mg naproxen twice/d + amitriptyline placebo; versus Amitriptyline + placebo: 25 mg amitriptyline once/night + naproxen placebo; versus Double placebo: 2 doses of placebo/d. All treatments lasted 6 weeks. | |
| Outcomes | The following outcomes were assessed at pretreatment, and at weeks 2, 4, and 6: participant‐administered 10 cm VAS scales assessing a) global FM symptoms, b) pain or stiffness, c) fatigue, d) difficulty with sleep, and e) feelings upon awakening; physician‐administered 10 cm VAS for global evaluation; and tender point score. The authors did not specify how adverse events were assessed. | |
| Notes | This is a small trial, with 58 study completers; sample sizes per treatment arm are not indicated. Statistical analysis did not assess the efficacy of each regimen, but instead assessed the efficacy of each drug. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “…each patient was randomly assigned to 1 of 4 treatment groups using a method that assured balanced assignment (19)." Reference 19 has a list of potential options, but which one was chosen for this study is not stated. |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of participants and personnel (performance bias) | Unclear risk | All participants took the same number of tablets, regardless of whether they contained active drug or placebo. "Patients, as well as the examining physician, were ‘blinded’ as to specific treatment." However, tablet appearance is not mentioned |
| Blinding of outcome assessment (detection bias) | Unclear risk | "Patients, as well as the examining physician, were ‘blinded’ as to specific treatment." No mention of how physicians were blinded |
| Incomplete outcome data (attrition bias) | Low risk | 4 out of 62 participants failed to return for a second study visit, and were therefore classified as study dropouts and were not included in the analysis. The dropout rate was low, and was similar across all 4 treatment arms (1 per arm) |
| Selective reporting (reporting bias) | Unclear risk | The protocol for this trial was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (6 weeks) |
| Similarities of Baseline Characteristics | Unclear risk | Age, sex ratio, and pain scores were reported at baseline, but not by treatment group. The study authors stated that pain scores did not differ between groups at baseline, but the comparison for age or sex ratio between groups was not shown. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, cross‐over design, four 6‐week period trial | |
| Participants | 18‐60 year olds diagnosed with FM using the 1990 ACR criteria, who had a pain rating of ≥ 30 on a 100 mm VAS and who had a score of ≤ 18 on the Hamilton Rating Scale for Depression, and who had been experiencing FM symptoms for 2‐20 years prior to enrollment. 31 participants were randomised; 19 completed the study; 24 completed at least 1 treatment period and were included in the analysis. Mean age: 43.2; 90% of participants were female. All central nervous system active medications, NSAIDs, and analgesics (excluding paracetamol [acetaminophen]) were discontinued for at least 1 week before the study start. Potential participants were excluded if they had a history of systemic illness including cardiac, kidney, hematologic, or liver disease, or if they had major depression. | |
| Interventions | Amitriptyline + fluoxetine: 20 mg fluoxetine every morning + 25 mg amitriptyline at bedtime; versus Amitriptyline + placebo: fluoxetine placebo every morning + 25 mg amitriptyline at bedtime; versus Fluoxetine + placebo: 20 mg fluoxetine every morning + amitriptyline placebo at bedtime; versus Double placebo: 1 fluoxetine placebo every morning, and 1 amitriptyline placebo at bedtime. All treatments lasted 6 weeks, with 2‐week washout periods between each treatment phase. | |
| Outcomes | All evaluations were done at the beginning and at the end of each of the 6‐week treatments for a total of 8 evaluations. Outcomes included: tender point score (sum of scores for each of 9 tender points); physician‐administered 100 mm VAS for global well‐being; participant‐administered 100 mm VAS for pain, sleep disturbance, fatigue, feeling refreshed upon awakening, and global well‐being; FIQ scores; Beck Depression Inventory scores; and adverse reactions to medications. Additionally, change scores within each treatment period were calculated for each outcome, and a composite change score out of 100 was calculated using the average of the changes in VAS scores for global well‐being and pain, tender point score, and physician global VAS to measure change within each treatment period. | |
| Notes | 31 participants were enrolled; 19 completed the study; 12 withdrew. Of the 12 withdrawals, 5 completed at least 1 treatment period, leaving 24 participants for which there was evaluable information. However, sample sizes reported in Table 2, range from 18‐22, and this is not explained anywhere in the report. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The order of treatment was generated from a table of random numbers" |
| Allocation concealment (selection bias) | Low risk | "Using randomization tables, the pharmacy assigned patients…" implying that investigators were not involved in the randomisation |
| Blinding of participants and personnel (performance bias) | Low risk | All participants took the same number of tablets, regardless of whether they contained active drug or placebo, and "All tablets were identical in appearance" |
| Blinding of outcome assessment (detection bias) | Low risk | "All evaluations were done by a physician who had no prior contact with the patients" |
| Incomplete outcome data (attrition bias) | Unclear risk | Of the 12 participants who dropped out of the study, 4 were in the fluoxetine arm, 1 was in the amitriptyline arm, 5 were in the combination arm, 1 was in the double placebo arm, and 1 was in a washout period following the combination treatment phase. Reasons cited for dropping out and treatment arm were given for each participant. It is stated that "all data on patients who completed at least 1 treatment period were analyzed for outcome", which implies that 7 of the 12 participants who dropped out during the first treatment period were not analyzed, leaving 24 participants for analysis. However, the final sample size is not clear, and the sample sizes shown for each of 9 outcomes in a table range from 18‐22, while the abstract implies that 19 participants were analyzed. |
| Selective reporting (reporting bias) | Unclear risk | The protocol for this trial was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (6 weeks) |
| Similarities of Baseline Characteristics | Low risk | Age, sex ratio, and pain scores were reported at baseline. Comparisons were not made between groups since this is a cross‐over study. Comparisons were made between those who completed the trial and those who dropped out, and no significant differences were seen. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, parallel‐design, 8‐week trial | |
| Participants | 18‐65 year olds diagnosed with FM using the 1990 ACR criteria. 101 participants were enrolled and completed the study; Mean age: 38.8; 94% of participants were female. Potential participants were excluded if they had any other marked pathologic disorder that may have interfered with the study outcomes, if they were pregnant or breastfeeding, or if they were taking analgesic or anti‐inflammatory drugs or antioxidant therapy. | |
| Interventions | Fluoxetine + high‐dose melatonin: 20 mg fluoxetine every morning + 5 mg melatonin every night; versus Fluoxetine + low‐dose melatonin: 20 mg fluoxetine every morning + 3 mg melatonin every night; versus Fluoxetine + placebo: 20 mg fluoxetine every morning + melatonin placebo every night; versus Melatonin + placebo: 5 mg melatonin every night + fluoxetine placebo every morning. All treatments lasted 60 days. | |
| Outcomes | The following outcomes were assessed at baseline and after 60 days/8 weeks of treatment: health‐related quality of life parameters from the FIQ (physical improvement, feel good, work missed, and doing work), and symptoms parameters from the FIQ (pain, fatigue, rest/sleep, stiffness, anxiety, and depression), and total FIQ score. Adverse events were not reported in this study. | |
| Notes | This is a small trial, with 23‐27 participants per treatment arm. No between‐group comparisons were made; only within‐group differences from baseline to day 60 (or week 8) of treatment were analyzed. However, statements about the superiority of one treatment over the other are made without justification. The first health‐related quality of life parameter listed (physical improvement) is incorrect – the FIQ assesses physical impairment. In the abstract and results sections, the authors imply that treatments were given for 8 weeks, but in the methods section, they imply that treatments were given for 60 days. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were randomly allocated into four groups”. There are no details about how randomisation was generated. |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of participants and personnel (performance bias) | Unclear risk | All participants took the same number of capsules, regardless of whether they contained active drug or placebo. It is not clear whether or not all capsules were identical. |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is no information given to permit judgement. |
| Incomplete outcome data (attrition bias) | Unclear risk | There is no information given to permit judgement. |
| Selective reporting (reporting bias) | High risk | Inappropriate statistics were done for the conclusions drawn, with only within‐group comparisons made. Very little detail is given in the methods about outcomes. The protocol was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Low risk | ≥ 7 weeks (8 weeks) |
| Similarities of Baseline Characteristics | Unclear risk | Age, sex ratio, and pain scores at baseline were reported, but no statistical comparisons were made between groups. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, parallel‐design, 5‐week trial | |
| Participants | Those diagnosed with FM using Yunus 1981 criteria. Aged ≥ 18 years. Participants completed a 1‐week, single‐blind washout period during which they received 4 ibuprofen placebo pills/d and 1 alprazolam placebo pill/d before starting the double‐blind phase of the study. 64 were randomised; 3 withdrew before the double‐blind phase, leaving 61 evaluable participants (those who took double‐blind medication for at least 1 week and had at least 1 assessment); 45 completed the entire study. Mean age: 48.4; 92% of evaluable participants were female. Potential participants were excluded if they were pregnant or breastfeeding, if they had a history of allergy/sensitivity to benzodiazepines, ibuprofen, or aspirin, history of peptic ulcer or gastrointestinal bleeding, alcohol or drug abuse, history of psychosis or schizophrenia, major depression or suicidal ideation, FM due to autoimmune disease, malignancy, endocrine/metabolic, hepatic, or renal disease. Participants were not excluded if they had previous psychiatric illness as long as they were not ill at the time of enrolment. | |
| Interventions | Ibuprofen + alprazolam: 600 mg ibuprofen 4 times/d + alprazolam titrated up based on side effects and treatment response from 0.5 mg at bedtime, up to a maximum of 6 mg/d; versus Ibuprofen + placebo: 600 mg ibuprofen 4 times/d + alprazolam placebo; versus Alprazolam + placebo: ibuprofen placebo 4 times/d + alprazolam titrated from 0.5 mg at bedtime up to a maximum of 6 mg/d; versus Double placebo: ibuprofen placebo 4 times/d + alprazolam placebo at bedtime. Treatments lasted 5 weeks. | |
| Outcomes | The following outcomes were assessed at the end of the washout week, and at the end of each subsequent treatment week: Hamilton Depression Rating Scale scores; Hamilton Anxiety Rating Scale scores; Beck Depression Inventory scores; pain, pain relief, and physical activity scored using a 100 mm VAS; number of tender points; severity of tenderness and muscle spasms or tension (none, mild, moderate, severe); global index of improvement using the clinician’s and participant’s clinical global improvement rating scale; and the number and type of adverse events experienced by participants. | |
| Notes | This is a small trial, with 14‐17 participants per arm. Participants were rated as having 0, 1, 2, or 3+ tender points during the musculoskeletal exam of 16 sites. Participants could have > 3 tender points per site, but the maximum score per site was 3, leading to a maximum tender points score of 48. After the 4th week evaluation, alprazolam dose (or matching placebo for the appropriate arms) was tapered; participants were told that alprazolam dose would be decreased and ibuprofen dose would remain steady for the last week of the trial. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomised to treatment". No details were given on how the randomisation was obtained |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement |
| Blinding of participants and personnel (performance bias) | Unclear risk | All participants took the same number of tablets, regardless of whether they contained active drug or placebo. It is not clear whether or not the tablets were identical to each other. Although there are no explicit statements of blinding, there are statements implying that investigators were blinded, for example, "However, when the blind was broken at the conclusion of the study, we were surprised to discover that the only active medication this subject received was ibuprofen" |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is no information given to permit judgement. |
| Incomplete outcome data (attrition bias) | Unclear risk | "There was no significant between‐group difference in drop‐out pattern or ratio of completers to non‐completers". Reasons for dropout: side effects (3), ineffective medications (11), termination to go on vacation (1), no reason recorded (2); the breakdown of dropouts between treatment groups is not given. The 18% dropout rate is cited as fairly high, but no explanation for it is provided. 17 study withdrawals were detailed, but the final sample size reported accounts for only 16 dropouts. |
| Selective reporting (reporting bias) | High risk | There are two outcome measures for which there are no results presented: severity of tenderness and muscle spasms or tension, and tender point score. The protocol was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (5 weeks) |
| Similarities of Baseline Characteristics | Unclear risk | Age and sex ratio at baseline were reported, but not by treatment group. The authors stated that there was no between‐group difference for age and sex ratio. Baseline pain scores are not mentioned. |
| Study characteristics | ||
| Methods | Randomised, parallel‐design, 12‐month trial | |
| Participants | Those diagnosed with FM using the 1990 ACR criteria and who had migraine without aura. Participants underwent a washout period for 1 month, and a subsequent 1‐month period during which they took placebo; after this, participants were randomised into 4 treatment arms. 200 participants were enrolled; no information is given regarding mean age of participants, or proportion of women Potential participants were excluded if they had systemic diseases, hypertension, liver diseases or dysfunction, stomach diseases, ocular diseases, or mood disturbances, or if they were pregnant or breastfeeding. | |
| Interventions | MAOI + 5‐HTP: 5‐10 mg/d paragyline or 10‐15 mg/d phenelzine + 400 mg/d 5‐HTP; versus MAOI: 5‐10 mg/d paragyline or 10‐15 mg/d phenelzine; versus 5‐HTP: 400 mg/d 5‐HTP; versus Amitriptyline: 10‐50 mg/d amitriptyline All treatments lasted 12 months. | |
| Outcomes | Daily pain was scored on a VAS from 0‐4, from which average pain levels were calculated during the 1‐month of placebo, and during the 12 months of active treatment; participants were asked to indicate all adverse events that occurred during treatment. | |
| Notes | All participants also suffered from migraines without aura, diagnosed using the criteria outlined in 1988 by the International Headache Society. No details are given on how average pain scores were calculated, and no details are given on the blinding of the trial. Although all participants were given placebo during an initial washout phase, blinding is not mentioned anywhere in the study. Sample size of 50 participants per arm is inferred – no direct statements about sample size are made in the paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of participants and personnel (performance bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is no information given to permit judgement. |
| Incomplete outcome data (attrition bias) | Unclear risk | "No one of the patients who experienced side‐effects withdrew of the study" is the only statement about dropouts. Total sample size of 200 is mentioned, but no breakdown is given (although 50/group can be inferred for 2 of the 4 groups). It is not possible to assess whether or not there were any dropouts. |
| Selective reporting (reporting bias) | High risk | Very little detail is provided in the methods about outcomes of interest. The statistical analyses used were inappropriate, and the authors make statements that are not supported statistically (analyses only compared each active treatment group to placebo, not to other treatment groups). There are statements in the results section about anxiety/mood changes as assessed by self‐administered questionnaires, but this is not mentioned in the methods. The protocol was not registered. |
| Size of study | Unclear risk | 50‐199 participants per arm |
| Trial Duration | Low risk | ≥ 7 weeks (52 weeks) |
| Similarities of Baseline Characteristics | Unclear risk | Sex ratio and age at baseline were not reported. Baseline pain scores were reported, but not compared between groups. |
| Study characteristics | ||
| Methods | Placebo‐controlled, randomised, double‐blind, parallel‐group design | |
| Participants | Female or male patients, 18–70 years of age, who met the 2010 ACR Preliminary Diagnostic Criteria for FM were eligible for inclusion | |
| Interventions | Enrolled patients received either an acute treatment dosage of famciclovir + celecoxib or placebo for the first week. IMC‐1 group participants subsequently received a chronic suppressive dosage of famciclovir + celecoxib for the remaining 15 weeks of the study, whereas placebo‐enrolled participants remained on placebo treatment. | |
| Outcomes | The primary efficacy outcome was response to treatment as assessed by the change from baseline in FM pain. To assess change in FM pain, both the 24‐h recall NRS score and the 7‐d recall pain score from the FIQ‐R were analyzed. | |
| Notes | Specific doses of study medications not specified in trial publication | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Specific randomisation methods not specified. "To ensure balanced assignment of patients across treatment groups at each site, a centralized by‐site randomization scheme was utilized." |
| Allocation concealment (selection bias) | Low risk | Specific randomisation methods not specified. "To ensure balanced assignment of patients across treatment groups at each site, a centralized by‐site randomization scheme was utilized." |
| Blinding of participants and personnel (performance bias) | Low risk | For blinding purposes, famciclovir and celecoxib were overencapsulated; the same filler was used for both active and placebo capsules, and active and placebo study drug supplies were identical in appearance. |
| Blinding of outcome assessment (detection bias) | Low risk | For blinding purposes, famciclovir and celecoxib were overencapsulated; the same filler was used for both active and placebo capsules, and active and placebo study drug supplies were identical in appearance. |
| Incomplete outcome data (attrition bias) | Unclear risk | 39% dropout rate in placebo group; 17% dropout rate in combination group; all participants who received at least 1 dose of study medication were included in the ITT analyses. The imputation method utilized for this study was a hybrid baseline observation carried forward (BOCF)/last observation carried forward (LOCF) approach to account for missing data and the reason for the data being missing |
| Selective reporting (reporting bias) | Low risk | All outcomes mentioned in the methods section are reported in the results section. |
| Size of study | Unclear risk | N = 45‐57 per arm which is between 50‐200 |
| Trial Duration | Low risk | 16‐week treatment period |
| Similarities of Baseline Characteristics | Unclear risk | Baseline characteristics were comparable across treatment groups |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, parallel‐design, 8‐week trial | |
| Participants | Those diagnosed with FM using the 1990 ACR criteria who were 18‐70 years of age, had widespread pain at study entry, had lab tests within the normal limit, and who did not have more than 2 locations with degenerative radiographic signs (X‐rays of cervical and lumbar spine, hands, knees, and hips were taken). 322 patients were invited to participate; 164 were randomised and were evaluated on an ITT basis; 134 completed at least 3 weeks of treatment and were analyzed as the "evaluable cohort"; 110 completed all 8 weeks. Mean age: 43; 93% of participants were female. Psychotropic drugs, NSAIDs, and analgesics were halted at least 3 weeks before study initiation; participants were allowed to take paracetamol (acetaminophen) during this washout period. Potential participants were excluded if they were pregnant or breastfeeding, had a history of hypersensitivity to NSAIDs or benzodiazepines, had peptic ulceration, inflammatory joint diseases, connective tissue diseases, hematologic, muscular, neurologic, renal, or infectious disorders, if they did not take trial medication for at least 3 weeks, or if they took forbidden medications during the study (NSAIDs, analgesics, or psychotropic drugs). | |
| Interventions | Tenoxicam + bromazepam: 20 mg tenoxicam every morning + 3 mg bromazepam at bedtime every day; versus Tenoxicam + placebo: 20 mg tenoxicam every morning + bromazepam placebo at bedtime every day; versus Bromazepam + placebo: tenoxicam placebo every morning + 3 mg bromazepam at bedtime every day; versus Double placebo: tenoxicam placebo every morning and bromazepam placebo at bedtime every day. All treatments lasted 8 weeks. | |
| Outcomes | The following were assessed at baseline and after 8 weeks on treatment: patient global assessment of FM compared to baseline on a scale of 3 (worse, no change or minimally improved, markedly approved or asymptomatic); sleep quality; duration of morning stiffness in minutes; pain on a 10 cm VAS; number of tender points. The study authors did not specify how adverse events were assessed. | |
| Notes | Analysis was done both on the subset of participants who completed at least 3 weeks of treatment, and on all participants randomised on an ITT basis. No raw numbers or means are presented in the results section; instead, the proportion/number of participants experiencing clinically significant improvement compared to baseline is given, defined in the methods section for each outcome variable. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "…we calculated that 41 patients would be needed to be randomised to each treatment group. The assignment scheme was generated using a table of random numbers…". |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of participants and personnel (performance bias) | Unclear risk | All participants took the same number of capsules regardless of whether they contained active drug or placebo, but no mention of whether the capsules were all identical. |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is no information given to permit judgement. |
| Incomplete outcome data (attrition bias) | High risk | 164 were randomised, and 54 withdrew before 8 weeks. Participants dropped out due to side effects, lack of efficacy, "other" reasons unrelated to study medication, and 30 were lost to follow‐up. There is an uneven dropout rate between the groups, with the combination group experiencing lower numbers of dropouts (6 total, vs. 15, 17, and 16 for placebo, tenoxicam, and bromazepam groups, respectively). |
| Selective reporting (reporting bias) | Unclear risk | Averages for each outcome are not reported. Instead, the number of participants reporting improvement in each outcome is reported. The protocol was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Low risk | ≥ 7 weeks (8 weeks) |
| Similarities of Baseline Characteristics | Low risk | Age, sex ratio, and pain scores at baseline were reported, and did not differ between treatment groups. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, parallel‐design, 6‐week trial | |
| Participants | 18‐65 year olds who had continuous musculoskeletal pain for 3 months and tenderness in at least 5 of 16 standard tender points. 78 were randomised; 76 were eligible for safety analysis; 63 were eligible for efficacy analysis. Mean age: 47.3; 88.5% of participants were female. Participants went through a 2‐week washout period during which they were only permitted to take paracetamol (acetaminophen); at the end of this 2‐week washout period, baseline measures were obtained. Potential participants were excluded if they had other rheumatic diseases, chronic infections, untreated endocrine disorders, unstable seizure diathesis, psychiatric disorders, or active peptic ulceration. | |
| Interventions | Ibuprofen + alprazolam: 600 mg ibuprofen 4 times/d + 0.5 mg alprazolam at bedtime every day, increased in 0.5 mg increments starting at week 3 of treatment to a maximum of 3.0 mg/d or until experiencing an adverse effect; versus Ibuprofen + placebo: 600 mg ibuprofen 4 times/d + alprazolam placebo at bedtime; versus Alprazolam + placebo: ibuprofen placebo 4 times/d + 0.5 mg alprazolam at bedtime every day, increased in 0.5 mg increments starting at week 3 up to a maximum of 3.0 mg/d or until experiencing an adverse effect; versus Double placebo: ibuprofen placebo 4 times/d + alprazolam placebo at bedtime every day. All treatments lasted 6 weeks. | |
| Outcomes | Severity of tenderness at 16 soft tissue sites assessed with a dolorimeter; tender point index (sum of severities at all 16 sites); pain on a 10 cm VAS; duration of morning stiffness in minutes; physician’s global perception of overall FM severity on a 10‐cm VAS; Health Assessment Questionnaire disability index assessing functional status; Hamilton Depression Scale, Hamilton Anxiety Scale, and Center for Epidemiologic Studies Depression Scale to assess psychological status; presence of any adverse events experienced was assessed by using a 24‐item checklist to question participants at each visit. These items were evaluated at baseline and after 6 weeks of treatment. | |
| Notes | 2/78 participants met the FM diagnostic criteria from Yunus 1981 and from Wolfe 1985; 69/78 participants met the FM diagnostic criteria from Smythe 1978 and from Campbell 1983; 68/78 participants met the FM diagnostic criteria of the 1990 ACR. The first 6 weeks of this study were double‐blinded; following this, an open‐label study in which all participants were treated with ibuprofen + alprazolam was conducted for an additional 24 weeks. Although statistical analyses were used to compare the change from baseline to week 6 of treatment between groups, it is unclear how often outcome measures were taken; Figure 1 implies that tender point index and dolorimeter score were assessed at weeks 2 and 4 of treatment as well. It is not explicitly stated in the methods section how often outcome measures were assessed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of participants and personnel (performance bias) | Low risk | All participants took the same number of tablets regardless of whether they contained active drug or placebo. Medication is referred to as "coded". No mention of whether the tablets were all identical. |
| Blinding of outcome assessment (detection bias) | Low risk | "All patients and staff were blinded to the randomization". |
| Incomplete outcome data (attrition bias) | Low risk | 102 were entered into study, 24 were excluded because they didn't meet eligibility criteria. Of the 78 remaining who were randomised, 2 were immediately lost to follow‐up, and 76 were included in the safety analysis; in the blinded portion of the study, of these 76 participants, 13 were withdrawn before week 6, therefore 63 were included in efficacy analysis. The balance of these withdrawals across treatment groups is not given, but the final sample sizes are fairly balanced, implying that the dropouts occurred evenly across groups. |
| Selective reporting (reporting bias) | Unclear risk | The protocol for this trial was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (6 weeks) |
| Similarities of Baseline Characteristics | Unclear risk | Age, sex ratio, and pain scores at baseline were reported, but not by treatment group, and they were not compared statistically between groups. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, cross‐over design, two 4‐week period trial | |
| Participants | Those diagnosed with FM using the 1990 ACR criteria. 29 participants were screened; 24 were randomised; 20 completed the blinded trial. Participants discontinued all FM medications (analgesic and sedative‐hypnotic drugs) 2 weeks before study start. Mean age: 49; 87.5% of participants were female There were no exclusion criteria listed. | |
| Interventions | Malic acid: 3 tablets (200 mg malic acid (Super Malic) + 50 mg magnesium hydroxide per tablet) twice a day for 4 weeks; versus Placebo: 3 placebo tablets twice a day for 4 weeks | |
| Outcomes | Pain on a 10‐cm VAS; tender point index (sum of tenderness severity at 18 tender points); tender point average (mean tenderness at 18 tender points measured by dolorimeter); Health Assessment Questionnaire score; Centre for Epidemiologic Studies‐Depression Scale score; Hassle Scale score. Outcomes were assessed at baseline (Week 0), at the end of the first treatment period (Week 4), at the end of the first washout (Week 6), at the end of the second treatment period (Week 10), and at the end of the second washout (Week 12). Adverse events were self‐reported by participants in daily diaries. | |
| Notes | Participants took study drug and placebo for 4 weeks each, with a 2‐week washout in between. After the double‐blind trial, participants went through another 2‐week washout, and then were placed on the study medication for 6 months as part of an open‐label trial. Final sample size for efficacy analysis is unclear; 24 participants were included in the adverse event assessment, but 4/24 participants withdrew from the trial at varying time points (3 between Week 0 and Week 4, and 1 between Week 6 and Week 10). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Those who successfully discontinued prestudy medications were randomised to 1 of 2 treatment sequences…" ‐ no other are details given. |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of participants and personnel (performance bias) | Low risk | "Manufacturer provided an identically coated placebo that matched Super Malic with regard to appearance and taste". |
| Blinding of outcome assessment (detection bias) | Unclear risk | Aside from being called a double‐blind trial, there is no mention that the assessors were blinded to participant treatment. |
| Incomplete outcome data (attrition bias) | Unclear risk | 24 were randomised; 4 were withdrawn before end of trial (Week 10): 3 decided not to continue during the first treatment period (Week 0 to 4), and 1 dropped out after Week 6 but before Week 10. Therefore, 20 participants completed the blinded trial. "The dropouts did not significantly differ from the completing study patients with respect to any of the baseline variables (data not shown)". Study authors don't mention which treatment the dropouts were on when they left the study. Moreover, the final sample size is not stated, and the statistical analysis description does not detail which participants were included in the analyses. The abstract implies 24 participants, but this does not account for the study withdrawals described. |
| Selective reporting (reporting bias) | Unclear risk | The protocol for this trial was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (4 weeks) |
| Similarities of Baseline Characteristics | Low risk | Age, sex ratio, and pain scores at baseline were reported, and compared between the 2 cross‐over treatment sequence groups. They did not differ statistically at baseline. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, placebo‐controlled, parallel‐design, 8‐week trial | |
| Participants | Women diagnosed with FM using the criteria of Smythe 1979 and Yunus 1981. 58 participants were randomised; 43 participants completed the study. Mean age: 47.4 Participants had been suffering from FM for 4‐47 years. Participants discontinued all analgesic and sedative medications for 72 h before study start. Potential participants were excluded if they used prohibited drugs within 72 h of study start, or if they had any coexisting disorders | |
| Interventions | Carisprodol: 2 tablets containing 200 mg carisoprodol (Somadril comp®) + 160 mg paracetamol (acetaminophen) + 32 mg caffeine 3 times/d; versus Placebo: 2 placebo tablets 3 times/d. Treatments lasted 8 weeks each. | |
| Outcomes | Outcomes were assessed at baseline and after 8 weeks of treatment. Participants rated their pain, sleep, and general feelings of sickness each on 10 cm VAS every day; participants recorded any extra medications they took during the study and any adverse events experienced on a daily basis; pressure pain threshold at 10 tender points was assessed at baseline and after 8 weeks of treatment using a dynamometer. | |
| Notes | Small trial: 20 participants in the active treatment group and 23 participants in the placebo group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were randomly selected and each patient received one bottle containing either active medication…or placebo." No other details are given. |
| Allocation concealment (selection bias) | Unclear risk | No information given, except that there were randomisation codes, and participants received a bottle of medication at the start (which contained either active or placebo drugs). |
| Blinding of participants and personnel (performance bias) | Low risk | "There were no detectable difference between the placebo tablets and the tablets containing active compounds regarding color, form, size or taste." |
| Blinding of outcome assessment (detection bias) | Low risk | Placebo tablets were identical, so participants remained blinded. Other outcome measures taken by study personnel were objective measures (using a dynamometer), so the data are likely to be unaffected by assessor bias. |
| Incomplete outcome data (attrition bias) | Unclear risk | 58 participants were enrolled and randomised, 43 of whom completed the study (23 placebo, 20 active). "Of the 58 patients who initially agreed to participate, 15 dropped out. Two of 15 did not return the VAS and gave no reason for their noncompliance. Three of 15 dropped out due to lack of therapeutic effect. One of 15 decided not to participate as therapy was not required due to less pain than normal. The remaining 9 of 15 were excluded due to incomplete scoring of the VAS during the 8‐week period of the study. Five patients completed 7 weeks, two completed 5 weeks, one completed 4 weeks, and one completed 3 weeks". The balance across treatment groups for dropouts is not given. |
| Selective reporting (reporting bias) | Unclear risk | The protocol for this trial was not registered. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Low risk | ≥ 7 weeks (8 weeks) |
| Similarities of Baseline Characteristics | Unclear risk | Age, sex ratio, and pain scores at baseline were reported, but no statistical comparisons between groups were made. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, parallel‐design, 4‐week trial | |
| Participants | 18‐60 year old women diagnosed with FM using the 1990 ACR criteria. 30 participants were randomised and completed the study. Mean age: 44.7 in the amitriptyline arm, 40.9 in the amitriptyline + lidocaine arm. Potential participants were excluded if they had alterations in thyroid, rheumatological, renal, or hepatic function, if they had trauma, if they had rheumatic, neuromuscular, or psychiatric disease, if they had infectious arthropathy, or drug hypersensitivity, or if they were pregnant. | |
| Interventions | Amitriptyline + lidocaine: 12.5 mg amitriptyline every night for the first week, increased to 25 mg every night for the remaining 3 weeks + 240 mg lidocaine in 125 mL saline infused i.v. over 1 h once a week for 4 weeks; versus: Amitriptyline + placebo: 12.5 mg amitriptyline every night for the first week, increased to 25 mg every night for the remaining 3 weeks + 125 mL saline infused i.v. over 1 h once a week for 4 weeks. | |
| Outcomes | All outcomes were assessed at baseline, and weeks 1, 2, 3, and 4, but data are only provided for baseline and week 4. At these time points, pain was reported on a verbal numerical scale from 0‐10 and the number of tender points was assessed; additionally, the number of participants experiencing sleep disorders, fatigue, subjective edema, morning stiffness paraesthesia, and headache was recorded. Adverse events were not assessed in this study. | |
| Notes | Small trial: 15 participants per arm. Participants had been suffering from pain for an average of 5.6 years (amitriptyline alone arm) and 6.8 years (amitriptyline + lidocaine arm) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The patients were allocated to two groups with the same number of patients by drawing lots". |
| Allocation concealment (selection bias) | Unclear risk | There is no information given to permit judgement. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants in the placebo group received saline through i.v. instead of lidocaine. However, it is unclear whether the solutions were identical and if not, if data collectors and participants were protected from seeing the i.v. bags. |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is no information given to permit judgement. |
| Incomplete outcome data (attrition bias) | Low risk | A diagram of their protocol flow indicates that all participants randomised to the study completed it (no study dropouts) |
| Selective reporting (reporting bias) | High risk | How some outcome measures were assessed is not fully described. One outcome measure in the methods section (number of participants experiencing depression) is not reported in the results section, and two outcome measures reported in the results section (number of participants experiencing headache and morning stiffness) are not described in the methods section. Data collected at time points between baseline and week 4 (weeks 1, 2, and 3) are not shown. |
| Size of study | High risk | < 50 participants per arm |
| Trial Duration | Unclear risk | 3‐6 weeks (4 weeks) |
| Similarities of Baseline Characteristics | Low risk | Age, sex ratio, and pain scores at baseline were reported, and no statistically significant differences were found between treatment groups. |
| Study characteristics | ||
| Methods | Randomised, double‐blind, N‐of‐1 cross‐over design, six 6‐week period trial | |
| Participants | 18‐60 year olds diagnosed with FM using the 1990 ACR criteria who scored ≤ 18 on the Beck Depression Inventory scale. Participants halted their current FM medications for at least 1 week before study start, and were only allowed to take paracetamol (acetaminophen) in addition to their study medications for pain. 58 participants were enrolled; analyses were done on data from participants who completed at least 2 periods (1 session on each therapy, n = 46) and on data from participants who completed all 6 periods (3 sessions on each therapy, n = 34). Mean age: 43 years; 96.5% of participants were female. Potential participants were excluded if they had contraindications to study drugs, if they had comorbid conditions that might confound FM diagnosis or assessments, if women of childbearing potential did not agree to use appropriate contraception, if they did not stop current FM medications for at least 1 week prior to trial start, or if they used analgesics during the study period (with paracetamol [acetaminophen] being the exception). | |
| Interventions | Amitriptyline + fluoxetine: 20 mg fluoxetine every morning + 25 mg amitriptyline every night; versus Amitriptyline + placebo: placebo every morning + 25 mg amitriptyline every night. Treatments lasted 6 weeks each; participants were given each treatment 3 times for a total of six 6‐week treatment periods. | |
| Outcomes | The following outcomes were assessed at baseline, at the end of each 6‐week treatment period, and at a 3‐month follow‐up visit: FIQ score; participant‐assessed 100 mm VAS scores on global well‐being, pain, sleep, fatigue, and feeling refreshed upon awakening; physician‐assessed 100 mm VAS scores on global well‐being and stress; tender point examination score consisting of the sum of scores for each of 18 FM tender points. Participants were also asked at each study visit to report any other medications taken and any adverse events experienced. | |
| Notes | Small trial: 58 participants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A central pharmacy prepared the blinded, random‐ordered treatment kits and block‐randomised the first treatment sets, so for every 20 kits prepared, 10 started treatment with AMT [amitriptyline] and 10 started with AMT+FL [amitriptyline + fluoxetine]" |
| Allocation concealment (selection bias) | Low risk | "A central pharmacy prepared the blinded, random‐ordered treatment kits" |
| Blinding of participants and personnel (performance bias) | Unclear risk | All participants took the same number of pills, regardless of which treatment they were on; however, there is no information on whether all pills were identical. |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is no information given to permit judgement. |
| Incomplete outcome data (attrition bias) | Low risk | Number of withdrawals and reasons for withdrawal are clearly outlined in Table 2. |
| Selective reporting (reporting bias) | Unclear risk | The protocol for this trial was not registered. |
| Size of study | High risk | < 50 participants |
| Trial Duration | Unclear risk | 3‐6 weeks (6 weeks) |
| Similarities of Baseline Characteristics | Low risk | Age, sex ratio, and pain scores at baseline were reported, but not compared between treatment groups since this is a cross‐over study. Baseline characteristics were compared between recruitment sites (center vs. community), and no difference was found. |
ACR: American College of Rheumatology; FIQ: Fibromyalgia Impact Questionnaire; FM: fibromyalgia; ITT: Intention to treat; i.v.: intravenous; MAOI: Monoamine Oxidase Inhibitor; MTD: Maximal Tolerated Dose; N: number (sample size); NPS: numerical pain scale; NPS: Numerical Pain Scale; NRS: numerical rating scale; NSAIDs: Non‐steroidal anti‐inflammatory drugs; SF‐MPQ: Short‐Form McGill Pain Questionnaire; SF‐36: Short Form 36 Health Survey; VAS: Visual Analogue Scale; 5‐HTP: 5‐Hydroxytryptophan
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Micronutrients and vitamins are considered to be non‐pharmacological therapy | |
| Open‐label study | |
| Study population used in a previous study included in this systematic review. | |
| Open‐label study | |
| Open‐label study | |
| Open‐label study | |
| Open‐label study | |
| Not exclusive to fibromyalgia | |
| Open‐label add‐on study | |
| Conference abstract and add‐on study | |
| Add‐on study | |
| Conference abstract, open‐label add‐on study | |
| Open‐label study | |
| Open‐label study | |
| Add‐on study | |
| Non‐pharmacological therapy (Vasolastine and Rheumajecta) | |
| Review of a study included in this systematic review | |
| Non‐pharmacological therapy | |
| Patient population does not have fibromyalgia (soft tissue rheumatism) | |
| Open‐label add‐on study | |
| Open‐label study using non‐pharmacological therapy (coenzyme Q10 and Gingko biloba extract) | |
| Open‐label study | |
| Letter to the editor | |
| Patient population does not have fibromyalgia (myofascial pain syndrome), and botulinum toxin is considered to be non‐pharmacological therapy | |
| Patient population does not have fibromyalgia (myofascial pain syndrome and chronic muscle spasm), and botulinum toxin is considered to be non‐pharmacological therapy | |
| Add‐on study | |
| Conference abstract | |
| Single‐blinded study | |
| Open‐label study | |
| Study proposal and hypothesis | |
| Open‐label add‐on study | |
| Open‐label case series | |
| Patient population does not have fibromyalgia (arterial circulatory disorders, muscle rheumatism, muscle trauma, arthritis and osteoarthritis, and neuralgia) | |
| Conference abstract, and open‐label add‐on case series | |
| Duplicated data from Vlainich 2010 | |
| Conference abstract, non‐randomised study | |
| Non‐pharmacological therapy (herb partitioned moxibustion) |
Characteristics of ongoing studies [ordered by study ID]
| Study name | Lidocaine on manifestations of fibromyalgia (LIMAFIBRO) |
| Methods | Phase 1, double‐blind, randomised, parallel‐design, 4‐week trial |
| Participants | Adults with fibromyalgia having pain in the 4 quadrants of the body for at least 3 months |
| Interventions | Amytriptyline+ lidocaine: daily treatment with 25 mg amitriptyline for 4 weeks + once‐weekly i.v. administration of 240 mg lidocaine versus Amytriptyline + placebo: daily treatment with 25 mg amitriptyline for 4 weeks + once‐weekly i.v. administration of saline placebo |
| Outcomes | Pain intensity and clinical manifestations of fibromyalgia |
| Starting date | January 2005 |
| Contact information | Study Chair: Rioko K. Sakata, Federal University of São Paulo. Responsible Party: Roberto Vlainich, Federal University of São Paulo |
| Notes | Similar to Vlainich 2010 |
| Study name | Study to assess the clinical benefit of droxidopa and droxidopa/carbidopa in subjects with fibromyalgia (FMS201) |
| Methods | Phase 2, double‐blind, randomised, placebo‐controlled, parallel‐design, 8‐week trial |
| Participants | Adults with fibromyalgia (diagnosed based on 1990 ACR criteria) who had pain VAS scores of 20 mm‐90 mm on the SF‐MPQ at screening and baseline visits |
| Interventions | Droxidopa: 200 mg, 400 mg, or 600 mg daily versus Carbidopa: 25 mg or 50 mg daily versus Droxidopa + carbidopa: their combination (all possible dosage pairings) versus Placebo |
| Outcomes | Pain, depression, fatigue, sleep disorder, quality of life, dose response relationship, optimal dose for treatment of fibromyalgia, adverse events, blood pressure, heart rate, ECG, and laboratory findings |
| Starting date | January 2009 |
| Contact information | Principal Investigator: Ernest Choy, Department of Rheumatology, Kings College London. Sponsor: Chelsea Therapeutics, UK |
| Notes |
| Study name | A study of IMC‐1 in patients with fibromyalgia |
| Methods | Phase 2, double‐blind, randomised, placebo‐controlled, parallel‐design, 16‐week trial |
| Participants | Adults with fibromyalgia |
| Interventions | IMC‐1: proprietary combination of famciclovir and celecoxib versus Placebo |
| Outcomes | Change in pain from baseline to week 16 of treatment, patient global impression of change from baseline to week 16 of treatment, FIQ scores |
| Starting date | May 2013 |
| Contact information | Sponsor/responsible party: Innovative Med Concepts, LLC |
| Notes | Identified in database search as a conference abstract (Pridgen 2014) |
ACR: American College of Rheumatologists; ECG: Electrocardiogram; FIQ: Fibromyalgia Impact Questionnaire; i.v.: intravenous; SF‐MPQ: Short‐Form McGill Pain Questionnaire;

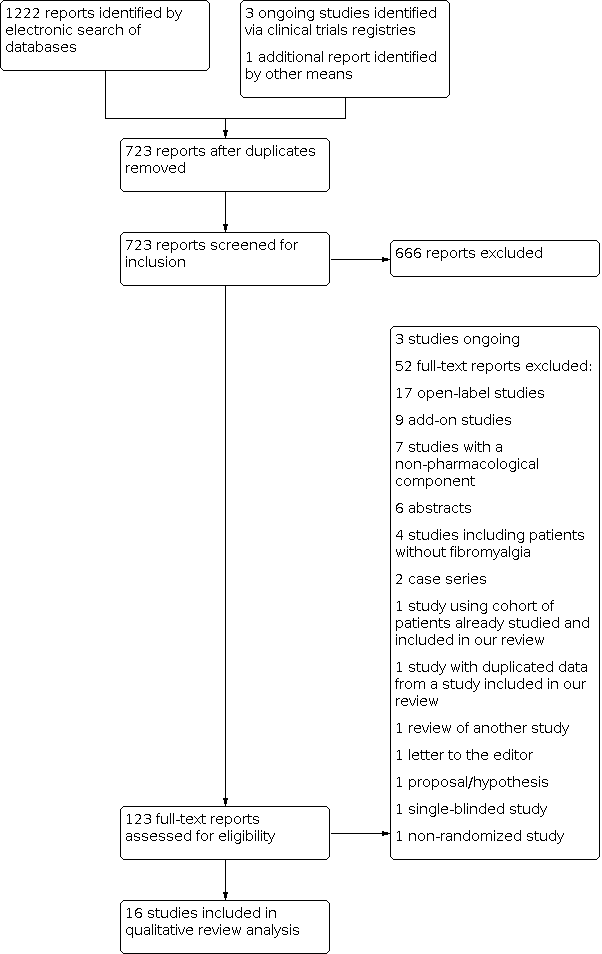
Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
| Any combination of two or more drugs compared with placebo or other comparators, or both, for fibromyalgia | ||
| Patient or population: adults with fibromyalgia Settings: community Intervention: any combination of two or more drugs (note: our searches found nine combinations of drugs) Comparison: placebo and/or other comparators | ||
| Outcome | Result | GRADE |
|---|---|---|
| Patient‐reported pain relief of 30% or greater | No or insufficient data for analysis for any combination of drugs | Very low quality, as no data for analysis |
| Patient‐reported pain relief of 50% or greater | No or insufficient data for analysis for any combination of drugs | Very low quality, as no data for analysis |
| Patient‐reported global impression of clinical change much or very much improved (moderate improvement) | No or insufficient data for analysis for any combination of drugs | Very low quality, as no data for analysis |
| Any pain‐related outcome indicating some improvement | No or insufficient data for analysis for any combination of drugs | Very low quality, as no data for analysis |
| Participants experiencing any adverse event | No or insufficient data for analysis for any combination of drugs | Very low quality, as no data for analysis |
| Participants experiencing any serious adverse event | No or insufficient data for analysis for any combination of drugs | Very low quality, as no data for analysis |
| Withdrawals due to adverse events | No or insufficient data for analysis for any combination of drugs | Very low quality, as no data for analysis |
| GRADE Working Group grades of evidence | ||
| First author, year | Trial comparisons | |||
|---|---|---|---|---|
| Placebo‐controlled | Combination vs. only 1 component | Combination vs. both components | Combination vs. other | |
| + | + | |||
| + | ||||
| + | ||||
| + | + | |||
| + | + | |||
| + | + | |||
| + | ||||
| + | + | |||
| + | +a | |||
| + | + | |||
| + | + | |||
| + | + | |||
| + | ||||
| + | ||||
| + | ||||
| + | ||||
| aNicolodi 1996 compared a monoamine oxidase inhibitor, 5‐hydroxytryptophan, their combination, and amitriptyline. | ||||