Knieorthesen zur Behandlung des Patellofemoralen Schmezsyndroms
Abstract
Background
Patellofemoral pain syndrome (PFPS) is a painful musculoskeletal condition, which is characterised by knee pain located in the anterior aspect (front) and retropatellar region (behind) of the knee joint. Various non‐operative interventions are suggested for the treatment of this condition. Knee orthoses (knee braces, sleeves, straps or bandages) are worn over the knee and are thought to help reduce knee pain. They can be used in isolation or in addition to other treatments such as exercise or non‐steroidal anti‐inflammatory medications.
Objectives
To assess the effects (benefits and harms) of knee orthoses (knee braces, sleeves, straps or bandages) for treating PFPS.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (11 May 2015), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2015 Issue 5), MEDLINE (1946 to 8 May 2015), EMBASE (1980 to 2015 Week 18), SPORTDiscus (1985 to 11 May 2015), AMED (1985 to 8 May 2015), CINAHL (1937 to 11 May 2015), PEDro (1929 to June 2015), trial registries and conference proceedings.
Selection criteria
Randomised and quasi‐randomised controlled clinical trials evaluating knee orthoses for treating people with PFPS. Our primary outcomes were pain and function.
Data collection and analysis
Two review authors independently assessed studies for eligibility, assessed study risk of bias and extracted data. We calculated mean differences (MD) or, where pooling data from different scales, standardised mean differences (SMD) with 95% confidence intervals (CI) for continuous outcomes and risk ratios (RR) with 95% CIs for binary outcomes. We pooled data using the fixed‐effect model.
Main results
We included five trials (one of which was quasi‐randomised) that reported results for 368 people who had PFPS. Participants were recruited from health clinics in three trials and were military recruits undergoing training in the other two trials. Although no trials recruited participants who were categorised as elite or professional athletes, military training does comprise intensive exercise regimens. All five trials were at high risk of bias, including performance bias reflecting the logistical problems in these trials of blinding of participants and care providers. As assessed using the GRADE approach, the available evidence for all reported outcomes is 'very low' quality. This means that we are very uncertain about the results.
The trials covered three different types of comparison: knee orthosis and exercises versus exercises alone; one type of orthosis versus another; and knee orthosis versus exercises. No trials assessed the mode of knee orthosis use, such as whether the orthosis was worn all day or only during physical activity. Two trials had two groups; two trials had three groups; and one trial had four groups.
All five trials compared a knee orthosis (knee sleeve, knee brace, or patellar strap) versus a 'no treatment' control group, with all participants receiving exercises, either through a military training programme or a home‐based exercise programme. There is very low quality evidence of no clinically important differences between the two groups in short‐term (2 to 12 weeks follow‐up) knee pain based on the visual analogue scale (0 to 10 points; higher scores mean worse pain): MD ‐0.46 favouring knee orthoses, 95% CI ‐1.16 to 0.24; P = 0.19; 234 participants, 3 trials). A similar lack of clinically important difference was found for knee function (183 participants, 2 trials). None of the trials reported on quality of life measures, resource use or participant satisfaction. Although two trials reported on the impact on sporting or occupational participation, one trial (35 participants) did not provide data split by treatment group on the resumption of sport activity and the other reported only on abandonment of military training due to knee pain (both cases were allocated a knee orthosis). One trial (59 participants, 84 affected knees) recording only adverse events in the two knee orthoses (both were knee sleeves) groups, reported 16 knees (36% of 44 knees) had discomfort or skin abrasion.
Three trials provided very low quality evidence on single comparisons of different types of knee orthoses: a knee brace versus a knee sleeve (63 participants), a patella strap with a knee sleeve (31 participants), and a knee sleeve with a patellar ring versus a knee sleeve only (44 knees). None of three trials found an important difference between the two types of knee orthosis in pain. One trial found no clinically important difference in function between a knee brace and a knee sleeve. None of the three trials reported on quality of life, resource use or participant satisfaction. One trial comparing a patella strap with a knee sleeve reported that both participants quitting military training due to knee pain were allocated a knee sleeve. One poorly reported trial found three times as many knees with adverse effects (discomfort or skin abrasion) in those given knee sleeves with a patella ring than those given knee sleeves only.
One trial compared a knee orthosis (knee brace) with exercise (66 participants). It found very low quality evidence of no clinically important difference between the two intervention groups in pain or knee function. The trial did not report on quality of life, impact on sporting or occupational participation, resource use, participant satisfaction or complications.
Authors' conclusions
Overall, this review has found a lack of evidence to inform on the use of knee orthoses for treating PFPS. There is, however, very low quality evidence from clinically heterogeneous trials using different types of knee orthoses (knee brace, sleeve and strap) that using a knee orthosis did not reduce knee pain or improve knee function in the short term (under three months) in adults who were also undergoing an exercise programme for treating PFPS. This points to the need for good‐quality clinically‐relevant research to inform on the use of commonly‐available knee orthoses for treating PFPS.
PICO
Laienverständliche Zusammenfassung
Knieschienen, Bandagen oder Gurte zur Behandlung des vorderen Knieschmerzes (Patellofemorales Schmerzsyndrom)
Hintergrund
Das Patellofemorale Schmerzsyndrom (PFSS) ist ein schmerzhaftes Knieleiden, von dem häufig junge, körperlich aktive Menschen betroffen sind. Es ist durch einen Schmerz auf der Vorderseite des Knies oder hinter der Patella (Kniescheibe) gekennzeichnet. Es besteht die Ansicht, dass dieser möglicherweise durch eine Fehlausrichtung der Kniescheibe während Kniebewegungen hervorgerufen wird. Als Hilfestellung empfehlen manche Physiotherapeuten, oder kaufen sich Betroffene, Knieschienen, ‐bandagen oder ‐gurte ('Orthesen' genannt), von denen angenommen wird, dass sie die Fehlausrichtung korrigieren.
Reviewfrage
Wir wollten herausfinden, ob das Tragen von Knieorthesen bei Menschen mit vorderem Knieschmerz den Knieschmerz verringert, die Funktionsfähigkeit des Knies verbessert und die Fähigkeit zur Durchführung von Alltagsaktivitäten und Sport steigert. Wir wollten auch herausfinden, ob es in Zusammenhang mit der Verwendung einer Knieorthese unerwünschte Wirkungen wie beispielsweise Hautprobleme gibt. Außerdem wollten wir herausfinden, welche Art von Knieorthese die beste ist, und ob das Tragen einer Knieorthese besser ist als andere Behandlungsarten wie beispielsweise Übungen.
Studienmerkmale
Wir suchten bis Juni 2015 in elektronischen Datenbanken und anderen Quellen und fanden fünf für die Reviewfrage bedeutsame Studien, die über die Ergebnisse von 368 Erwachsenen mit PFSS berichteten. In drei Studien wurden die Teilnehmer aus verschiedenen Gesundheitseinrichtungen rekrutiert (aufgenommen), in den anderen beiden Studien waren sie Militärkadetten. Alle fünf Studien waren klein und von einem hohen Verzerrungsrisiko (Risiko der Verfälschung der Ergebnisse) betroffen, was bedeutet, dass ihre Ergebnisse möglicherweise nicht zuverlässig sind.
Die Studien umfassten drei unterschiedliche Arten von Vergleich: Knieorthese und Übungen gegenüber alleinigen Übungen, eine Art Orthese gegenüber einer anderen und Knieorthese gegenüber Übungen. Keine Studie untersuchte die Verwendungsweise einer Knieorthese, wie zum Beispiel ob die Orthese den ganzen Tag über oder nur während körperlicher Aktivität getragen wurde.
Hauptergebnisse
Alle fünf Studien verglichen eine Knieorthese (entweder Bandage, Schiene oder Gurt) zuzüglich Übungen mit alleinigen Übungen. Diese erbrachten Evidenz (einen wissenschaftlichen Beleg) sehr niedriger Qualität dafür, dass das Tragen einer Knieorthese möglicherweise keinen Unterschied macht in Bezug auf den Knieschmerz (Daten von drei Studien) und die Funktionsfähigkeit (Daten von zwei Studien). Keine der drei Studien machte Angaben zur Lebensqualität, Ressourcennutzung (Kosten) oder Patientenzufriedenheit. Eine Studie berichtete, dass beide Teilnehmer, die ihre militärische Ausbildung wegen Knieschmerzen aufgaben, eine Knieorthese zugewiesen bekommen hatten. Eine mangelhaft dargestellte Studie fand bei mehr als einem Drittel der Knie derjenigen, die eine Kniebandage erhalten hatten, Beschwerden oder Abschürfungen.
Drei Studien erbrachten Evidenz von sehr niedriger Qualität zu einzelnen Vergleichen verschiedener Arten von Knieorthesen: eine Knieschiene gegenüber einer Kniebandage (63 Teilnehmer), ein Patellaband (‐gurt) mit einer Kniebandage (31 Teilnehmer), und eine Kniebandage mit einem Patellaring (einem stabilisierenden Rand) gegenüber einer alleinigen Kniebandage (44 Knie). Keine der drei Studien fand einen bedeutsamen Unterschied zwischen den Arten von Knieorthese in Bezug auf den Knieschmerz. Eine Studie fand keinen bedeutsamen Unterschied in der Funktionsfähigkeit zwischen einer Knieschiene und einer Kniebandage. Keine der drei Studien machte Angaben zur Lebensqualität, Ressourcennutzung oder Patientenzufriedenheit. Eine Studie, die einen Patellagurt mit einer Kniebandage verglich berichtete, dass beide Teilnehmer, die ihre militärische Ausbildung wegen Knieschmerzen aufgaben, eine Kniebandage zugewiesen bekommen hatten. Eine mangelhaft dargestellte Studie fand bei mehr als dreimal so vielen Knien derjenigen, die eine Kniebandage mit einem Patellaring erhalten hatten, Beschwerden oder Hautabschürfungen im Vergleich mit denjenigen, die nur eine Kniebandage erhalten hatten.
Eine Studie (66 Teilnehmer) verglich eine Knieorthese (Knieschiene) mit Übungen. Sie erbrachte Evidenz von sehr niedriger Qualität für keinen klinisch bedeutsamen Unterschied zwischen den beiden Behandlungsgruppen in Bezug auf den Schmerz oder die Funktionsfähigkeit des Knies. Sie enthielt keine Angaben zu anderen Endpunkten (Zielen) einschließlich Komplikationen.
Schlussfolgerungen
Insgesamt fanden wir einen Mangel an Evidenz für eine informierte Aussage über die Verwendung von Knieorthesen zur Behandlung des PFSS. Unser Review ergab Evidenz sehr niedriger Qualität aus Studien, die unterschiedliche Knieorthesen (Knieschiene, ‐bandage und ‐gurt) testeten, dafür, dass der Gebrauch einer Knieorthese bei Erwachsenen, die zusätzlich ein Übungsprogramm zur Behandlung des PFSS durchführten, möglicherweise kurzfristig (unter drei Monaten) den Knieschmerz nicht verringert oder die Funktionsfähigkeit nicht verbessert. Diese Ergebnisse weisen auf den Bedarf an klinisch relevanter Forschung guter Qualität hin, um eine informierte Aussage über die Verwendung verbreitet verfügbarer Knieorthesen zur Behandlung des PFSS zu ermöglichen.
Authors' conclusions
Summary of findings
| Knee orthosis and exercise versus exercise alone for patellofemoral pain syndrome (PFPS) | ||||||
| Patient or population: Adults (recruited from health clinics or military recruits) with PFPS (duration of symptoms ranged from acute, under 2 to 3 weeks in two trials, to predominantly chronic in three trials: mean durations 8.3 months, 21 months, 21 months) Settings: Health clinics, home and military training establishments Intervention: Knee orthosis (various types: knee sleeve, knee brace or patellar strap) and exercise (military training, home exercise programme) Comparison: Exercise alone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Exercise alone | Knee orthosis and exercise | |||||
| Pain score (VAS) Scale from: 0 to 10 (higher scores mean worse pain) Follow‐up: 3 to 12 weeks (short‐term) | The mean pain score for the exercise alone group ranged across the control groups from 2.7 to 3.2 points; the mean change score from ‐0.47 to ‐0.96 points | The mean pain score in the knee orthosis and exercise group was 0.46 points lower (1.16 lower to 0.24 higher) | MD ‐0.46 (‐1.16 to 0.24) | 234 (3) | ⊕⊝⊝⊝ | The MD and 95% CIs do not include clinically important treatment effects. MCID: 30 mm on an 100 mm VAS (Lee 2003) |
| Functional outcomes Scale various 2 Follow‐up: 6 and 12 weeks (short‐term) | The mean functional score in the knee orthosis and exercise group was 0.15 points lower (0.69 lower to 0.38 higher) The mean difference in knee function (short‐term) in the knee orthosis group was 0.25 standard deviations lower (0.55 lower to 0.05 higher) | SMD ‐0.25 (‐0.55 to 0.05) | 183 (2) | ⊕⊝⊝⊝ | Lower values equate to higher disability. The SMD result equates to a small difference at most and in absolute terms, the mean differences for each trial were small (e.g. 0.9 for a range 0 to 68) and not clinically important | |
| Quality of Life and General Health Assessments | See comment | See comment | No study reported this outcome | |||
| Impact on sporting and occupational participation | See comment | See comment | 51 (1)4 | ⊕⊝⊝⊝ | One trial reported that 2 out of 31 (6.5%) participants in the knee orthosis groups versus 0 of 20 (0%) in the control group withdrew from their military training programme. | |
| Resource use | See comment | See comment | No study reported this outcome | |||
| Participant satisfaction | See comment | See comment | No study reported this outcome | |||
| Complications Follow‐up: 14 weeks6 | See comment | See comment | 59 with 84 affected knees (1) | ⊕⊝⊝⊝ | Trial reported 16 complications (skin abrasions or discomfort) for 44 knees (36%) of participants in the knee orthosis group. | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including selection bias (1 trial) and performance bias (all 3 trials)), and one level for indirectness (this reflects the clinical heterogeneity such as variation in the interventions and outcome measures and measurement, and the generally inadequate description of these). There was, however, no statistical heterogeneity in the pooled data. 2. One trial reported WOMAC functional scores (0 to 68; higher values mean worse function) at six weeks and the other the results of a modified version of the Knee Function Scale (0 to 53; higher values mean better function) at 12 weeks. 3. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including selection bias (1 trial) and performance bias (both trials)), and one level for imprecision (wide confidence intervals and limited data). 4. Data on resumption of sports activities were not split by treatment group in one trial (35 participants). 5. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including performance and detection biases), and one level for indirectness (abandonment of military training may be for other reasons than serious knee pain). 6. The single study recording this outcome did not record complications for all groups. The follow‐up for complications appeared be during use; i.e. the basic military training programme of 14 weeks.. 7. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including performance and detection biases and serious unit of analyses issues relating to the inclusion of participants with anterior knee pain in both knees), and imprecision (incomplete data from one small trial). | ||||||
Background
Description of the condition
The term 'patellofemoral pain syndrome' (PFPS) is associated with anterior and retropatellar pain (Grelsamer 2009). This term has been used interchangeably with other terms, most notably anterior knee pain and patellofemoral syndrome (Grelsamer 2009). It is more commonly seen in females than in males, and has an estimated prevalence of 12% to 45% amongst young, physically active people (Bizzini 2003; Cook 2010; Dixit 2007; Roush 2012). This wide variation has been attributed to the diversity of people who may experience this condition; from sedentary adolescents to military recruits during basic training (Callaghan 2007). PFPS is characterised by pain behind and around the patella, which is aggravated during prolonged sitting, descending stairs or slopes, squatting or kneeling (Dixit 2007; Grelsamer 2009).
The aetiology of PFPS remains unclear (Lankhorst 2012; Waryasz 2008). However, the basic premise is that the patella 'moves' abnormally within the femoral trochlear. This is termed patella maltracking. The patella is most frequently thought to maltrack laterally and therefore tries to deviate against the lateral femoral trochlear. Repetitive maltracking is associated with increased sheering and compressive forces between the retropatellar and femoral trochlear articulation (Song 2011; Waryasz 2008). The causes of maltracking are largely acknowledged to be multifactorial. Factors that may contribute to this include lateral retinaculum shortening (Hudson 2009), an imbalance between the activation and intensity of vastus lateralis and vastus medialis muscles (Chester 2008), reduced hip muscle control (Barton 2013; Cowan 2009), hamstring, quadriceps or calf muscle tightness (Erkula 2002; Waryasz 2008), excessive tibial rotation from foot pronation (Barton 2011), femoral anteversion (Keser 2008) and trochlear dysplasia (Parikh 2011).
The diagnosis of PFPS is usually derived from a person's reported history and their symptoms. A physical examination is important to exclude other injuries such as meniscal or ligament tear, tendinopathy, fracture and dislocation (Dixit 2007). Whilst no specific criteria exist, typically a person diagnosed with PFPS will have had symptoms for greater than six weeks, which reflects the standard research eligibility criteria found in the literature. Physical examination is also necessary to assess the various different factors, listed above, which may contribute to the presentation of PFPS.
Conservative treatment is widely accepted as the primary management of PFPS (Powers 2012) with one particular high‐quality randomised controlled trial (Van Linschoten 2009) showing that conservative treatment had better outcomes in pain and function in both the short‐ and long‐term compared to a 'wait and see' group. In part reflecting the multifactorial nature of PFPS, a number of different interventions have been advocated. These include quadriceps strengthening and stretching exercises (Chiu 2012), patellar adhesive taping and biofeedback exercises (Cowan 2002), foot orthotics (Barton 2010), manual therapy (Brantingham 2012), acupuncture (Jensen 1999) and knee orthoses (Bizzini 2003; Powers 2004).
Description of the intervention
This review examined the use of knee orthoses for people with PFPS. Knee orthoses are essentially external, non‐adhesive devices that aim to modify the position of the patella. The term 'knee orthosis' encompasses a variety of different interventions including knee braces, sleeves, bandages and straps. They are frequently made of neoprene and are available in a variety of sizes to account for different limb circumferences (Shellock 2000). The majority of orthoses have a 'patella hole', which is a hole cut out of a neoprene sleeve. In addition, in some designs, a strap or buttress is incorporated into the orthosis. These features are intended to help maintain the patella in a more central position (Chew 2007).
Knee orthoses have been described as simple, inexpensive and associated with negligible adverse effects (Warden 2008). People can purchase orthoses independently, or they may be prescribed by a healthcare professional. The user can apply the knee orthosis without assistance, which allows them greater control over managing their knee condition. Knee orthoses can be worn during normal activities of daily living, as well as during sporting and occupational pursuits. There is no consensus as to whether bracing should be used as an adjunct to treatment or on its own for the treatment of pain for those with PFPS (Dixit 2007).
How the intervention might work
Whilst consensus regarding the aetiology of PFPS is lacking, abnormal patellar tracking is largely considered to be the primary cause (Powers 2004). It has been suggested that knee orthoses work by centralising the patella within the femoral trochlea, thereby correcting abnormal patellar tracking and reducing pain (Powers 2004). However, whilst some studies have corroborated that knee orthoses can alter patellar alignment (Shellock 1994; Shellock 2000), others have reported the contrary during radiological investigations (Muhle 1999; Powers 1999; Powers 2004).
Knee orthoses may also have other therapeutic effects. For instance, wearing the neoprene orthosis may have a thermal effect, which could increase sensory feedback and proprioception, while also altering knee circulation (Herrington 2005; Shellock 1995; Van Tiggelen 2004). Added to this, Earl 2004 reported that knee orthoses work by 'unloading' the patellofemoral joint when orthoses are used during exercise compared with not wearing a brace. They postulated that a knee orthosis, by reducing contact forces between the patella and the femoral trochlea, may reduce the symptoms related to PFPS. Through this symptomatic relief, it is speculated that knee orthoses can facilitate greater exercise tolerance and capability, thus optimising the clinical effects of exercise (Swart 2012).
Why it is important to do this review
The use of knee orthoses has been widely documented in the literature for assisting the management of people with PFPS. However, no systematic reviews have rigorously assessed their application for this population. There remains mixed evidence as to the effectiveness of knee orthoses for this population.
Patellofemoral pain syndrome is acknowledged as a potentially disabling condition, which can impact on the occupational and sporting pursuits of children and young adults. Furthermore, previous authors have acknowledged a potential link between adolescent PFPS and the development of patellofemoral osteoarthritis (Thomas 2010; Utting 2005). The failure of treatment for PFPS is currently high. Over 90% of people with PFPS continue to experience pain for more than four years following treatment (Stathopulu 2003). Given this impact, both in the short‐ and potentially longer‐term, and limited consensus in the effectiveness of knee orthoses, this review is important to better inform clinicians and the public on the use of these interventions for treating this musculoskeletal condition.
Objectives
To assess the effects (benefits and harms) of knee orthoses (knee braces, sleeves, straps or bandages) for treating PFPS.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) and quasi‐randomised (using a method of allocating participants to a treatment that is not strictly random, e.g. by hospital number) controlled clinical trials evaluating knee orthoses for treating PFPS. Cross‐over study designs were excluded due to the potential for treatment 'carry‐over' from one randomised arm to another, irrespective of the duration of the 'wash‐out' period.
Types of participants
We included trials of participants subjectively reporting pain diagnosed by trial authors as 'patellofemoral pain syndrome', 'patellofemoral pain', 'anterior knee pain syndrome', 'patellar dysfunction', 'chondromalacia patellae', 'patellar syndrome', 'patellofemoral syndrome' or 'chondropathy'. No restrictions were placed on the age of the participant, duration of symptoms or stage of disease as we planned to explore these variables as subgroup analyses.
Trials where participants were asymptomatic or non‐pathological were excluded. Trials that recruited participants with a history of fracture, patellar dislocation, patellar tendinopathy, Hoffa's syndrome, Osgood Schlatter syndrome, Sinding‐Larsen‐Johansson syndrome, iliotibial band friction syndrome, osteoarthritis, rheumatoid arthritis, plica syndromes, or tibiofemoral injury or dysfunction were also excluded.
Trials reporting the use of orthoses following operative interventions (either immediately post‐operatively or at any point following surgery) were excluded.
Trials including mixed population studies where a percentage of the cohort may have some other (possibly undiagnosed) knee pathology, such as patellar tendinopathy, were excluded unless the results for the PFPS cohort were presented separately or the numbers of such 'undiagnosed' participants were small and sufficiently balanced between the intervention groups.
Types of interventions
We included trials evaluating the use of a knee orthosis. A knee orthosis was defined as a device that aimed to control or change patellar tracking or loading or both, and could have taken the form of a knee brace, sleeve, bandage or strap.
Comparisons included:
-
Knee orthosis and non‐operative intervention (e.g. exercise) versus the same non‐operative intervention alone.
-
One type of knee orthosis versus another.
-
Knee orthosis versus another non‐operative intervention (e.g. exercise).
-
Mode of knee orthosis use: e.g. length of time worn per day; whether orthosis is only worn during physical activity versus all day.
Trials looking at adhesive taping techniques were not included as they have been assessed in another Cochrane review (Callaghan 2012).
Types of outcome measures
Primary outcomes
-
Pain, e.g. during activity or at rest, measured using a visual analogue scale (VAS) or similar, preferably at 12 months after commencing the intervention. Pain could be assessed during a specific activity (e.g. single leg squat), or more globally, e.g. as usual pain during the previous week.
-
Functional outcomes, e.g. Western Ontario and McMaster Universities Index (WOMAC) (Klassbo 2003); Knee Injury and Osteoarthritis Outcome Score (KOOS) (Roos 1998); Lower Extremity Functional Scale (LEFS) (Blinkley 1999); Kujala Patellofemoral Disorder Score/Anterior Knee Pain Scale (Kujala 1993)
Secondary outcomes
-
Quality of life and general health assessments, e.g. EQ‐5D (EuroQol Group 1990); Short Form‐12 (Ware 1996).
-
Impact on sporting or occupational participation, e.g. duration of occupational sick leave, or time to return to sports at the same pre‐injury level.
-
Resource use/costs of intervention.
-
Participant satisfaction, e.g. Likert scale, VAS or validated score.
-
Complications of orthoses, e.g. allergies or subsequent injury.
Biomechanical outcomes such as postural sway, joint proprioception, force‐plate distribution and muscle dynamometry were not included in this review.
For a study to be included in the review, it had to have measured one or more of the listed outcomes.
Timing of outcome assessment
For each outcome, the primary end‐point for analysis was 12 months. Short‐term (zero to three months), medium‐term (more than three months up to 12 months) and long‐term (12 months and over) analyses were also planned in the protocol (Smith 2013). If there were multiple points within a category, the latest follow‐up period was recorded.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (11 May 2015), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2015 Issue 5), MEDLINE (1946 to May Week 1 2015), MEDLINE In‐Process & Other Non‐Indexed Citations (8 May 2015), MEDLINE Daily Update (8 May 2015), EMBASE (1980 to 2015 Week 18), SPORTDiscus (1985 to 11 May 2015), Allied and Complementary Medicine (AMED) (1985 to 8 May 2015), the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (1937 to 11 May 2015), and the Physiotherapy Evidence Database (PEDro) (1929 to June 2015). There were no restrictions on language, date or publication status.
We searched the WHO International Clinical Trials Registry Platform, the ISRCTN registry, ClinicalTrials.gov and OpenGrey (System for Information on Grey Literature in Europe) for ongoing or unpublished trials (June 2015). We also searched The Bone and Joint Journal Orthopaedic Proceedings for conference proceedings and abstracts (June 2015).
In MEDLINE, a subject‐specific search was combined with the Cochrane Highly Sensitive Search Strategy to identify randomised trials (sensitivity‐maximising version), as described by Lefebvre 2011. Search strategies and associated platforms for all databases are shown in Appendix 1.
Searching other resources
We scrutinised the reference lists of all pertinent review papers and eligible trials.
Data collection and analysis
Selection of studies
Two review authors (TS and BD) independently screened the titles and abstracts of the search strategy results to identity all potentially eligible trials, for which full‐text reports were sought. The same two authors independently performed study selection. Disagreements in respect to final eligibility were resolved through discussion between the two review authors. The final eligibility of all papers was adjudicated by a third review author (TM).
Data extraction and management
Two review authors (TM and BD) independently reviewed and extracted data from each included trial. Disagreements on data extracted from the original papers were resolved through discussion between the two review authors. Adjudication by a third review author (TS) was not required for the data extraction phase.
Assessment of risk of bias in included studies
Two review authors (TM and BD) independently assessed the risk of bias of the included trials using The Cochrane 'Risk of bias' tool (Higgins 2011a). The following domains were evaluated: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data reporting, selective outcome reporting and other sources of bias. Since orthoses are visible interventions, worn by participants, we acknowledged that it was impossible to blind participants or personnel to group allocation. However, some blinding of outcome assessment would still be possible. Any disagreements were resolved through discussion, adjudicated if necessary by a third review author (TS), until a consensus was reached.
Measures of treatment effect
We calculated risk ratios (RR) with 95% confidence intervals (CI) for dichotomous outcomes and mean differences (MD) with 95% CI for continuous outcomes. For pooling continuous outcome data where different scales or scores were used, we calculated standardised mean differences (SMD). To assist interpretation, we used mean differences for pain visual analogue scales.
Unit of analysis issues
We included two trials that involved a substantial number of participants treated for bilateral symptoms and which reported data for knees rather than participants. Where possible we reported participant data and used the number of participants as denominators for continuous outcomes to provide a conservative estimate. We performed sensitivity analyses where possible to explore the effects on the confidence intervals when using the number of knees as denominators. We were alert to other potential unit of analysis issues such as those relating to multiple observations for the same outcome. Thus, each follow‐up period, within the categories defined in Types of outcome measures, was assessed separately to minimise the risks of unit of analysis errors (Deeks 2011).
Dealing with missing data
We contacted trialists to provide missing data. Unless we could calculate missing standard deviations from standard errors, exact P values or 95% confidence intervals, we did not impute these or any other missing outcome data. If a paper only provided imputed data, we emailed the corresponding study author to request the specific data required on outcomes only from participants who were assessed. Where possible and appropriate, we used intention‐to‐treat analysis results for all review analyses.
Assessment of heterogeneity
We evaluated study heterogeneity from an inspection of the characteristics of the included studies. We assessed statistical heterogeneity using Chi² and I² statistics, in addition to visual inspection of the forest plots (Higgins 2003). We interpreted I² values as recommended by Deeks 2011. Thus, an I² value of 0% to 40% might 'not be important'; 30% to 60% may represent 'moderate' heterogeneity; 50% to 90% may represent 'substantial' heterogeneity; and 75% to 100% represents 'considerable' heterogeneity.
Assessment of reporting biases
We did not construct a funnel plot to assess possible publication bias (Sterne 2011) as there were insufficient data.
Data synthesis
When there was heterogeneity between the studies in respect to the interventions, population or method of assessment, we presented a narrative review of the results. Otherwise, where possible, we pooled results of comparable groups of trials using both fixed‐effect and random‐effects models. The choice of the model to report was guided by a careful consideration of the degree of heterogeneity, as classified in the Assessment of heterogeneity section, and whether it could be explained through study design or cohort differences, in addition to other factors such as the number and size of studies that were included. We considered not pooling data where there was considerable heterogeneity (I² > 75%) that could not be explained by the diversity of methodological or clinical features among the trials.
To assess treatment effect, we used mean differences to assess continuous data, whilst risk ratios were used to assess dichotomous data. We presented 95% CIs throughout. When there was insufficient data to perform this assessment of treatment effect, or significant heterogeneity was evident, we presented a narrative review of the original trial's findings.
Subgroup analysis and investigation of heterogeneity
Planned subgroup analyses included:
-
Different forms of orthoses: custom‐made orthoses; prefabricated ('off‐the‐shelf') versions; bandages; straps.
-
Age (18 years or over versus under 18 years) and gender.
-
Level of activity (participants who were professional athletes or in the military forces versus recreational athletes).
There was a lack of data to conduct subgroup analyses for these parameters.
We considered factors such as age, gender, duration of PFPS symptoms prior to randomisation, type of intervention, length of follow‐up, level of pre‐injury activity and adjusted/unadjusted analyses during the interpretation of heterogeneity.
Sensitivity analysis
We planned to conduct sensitivity analyses to explore different aspects of trial and review methodology, for example, assessing outcomes after the exclusion of trials at high risk of selection bias. However, all included trials were at high risk of various biases and it was inappropriate to discriminate between these. As all trials described their population sufficiently, no sensitivity analyses were performed to see the effect of excluding trials where the population was poorly defined. There were insufficient data to explore the effects of missing data, such as studies that presented more than or equal to 90% of their originally randomised cohort at follow‐up, as recommended by Higgins 2011b. The only sensitivity analyses performed were to explore the effects of unit of analysis issues relating the inclusion of participants with bilateral symptoms.
'Summary of findings' tables
We summarised the results for the main comparison described in Types of interventions in a 'Summary of findings' table. For all comparisons, we used the GRADE approach to assess the quality of evidence related to each of the primary outcomes and, if possible, to at least the first two secondary outcomes listed in Types of outcome measures (Schünemann 2011).
Results
Description of studies
Results of the search
A summary of the study selection process is shown in Figure 1.

Study flow diagram
The search was completed in June 2015. We screened a total of 3463 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (20 records); CENTRAL (319), MEDLINE (452), EMBASE (500), AMED (99), SportDiscus (63), CINAHL (85), the WHO International Clinical Trials Registry Platform (133), Current Controlled Trials (42), the PEDro database (1682) and OpenGrey (68). We also identified 128 potentially eligible trials from a search of the Bone and Joint Journal's Orthopaedic Proceedings.
The search identified a total of 33 trials for potential inclusion, for which, where possible, full reports were obtained. We included five trials (Evcik 2010; Finestone 1993; Lun 2005; Miller 1997; Moller 1986) and excluded 26 (Antich 1986; Avraham 2007; BenGal 1997; Denton 2005; Draper 2009; Farkas 1997; Fukuschima 1992; Greenwald 1996; Gulling 1996; Lindberg 1988; Lysholm 1984; McCrory 2004; McCrory 2007; Palumbo 1981; Powers 1999; Powers 2004; Roostayi 2009; Sathe 2002; Selfe 2008; Selfe 2011; Straub 2012; Timm 1998; Van Tiggelen 2004; Van Tiggelen 2011; Wijnen 1996; Worrell 1998). Two ongoing studies were identified (DRKS00003291; IRCT138810293101N1); of these, one was excluded (IRCT138810293101N1). No studies await classification.
Included studies
This review included five trials which recruited a total of 391 participants and reported results for 368 of these. Details of the individual trials are presented in the Characteristics of included studies.
Design
All five included trials were described as randomised trials but provided either no or limited information on the method used. Based on the information supplied, Evcik 2010 appears to be quasi‐randomised. Two trials had two groups (Evcik 2010; Moller 1986); two trials had three groups (Finestone 1993; Miller 1997); and one trial had four groups (Lun 2005). From the description provided and the numbers allocated in each group in Finestone 1993, it is uncertain whether there was randomisation between the two orthosis groups (see below). The unit of randomisation appeared to be individual participants in all five trials. Two trials were described as single‐blinded (Evcik 2010; Lun 2005).
Sample size
The number of participants for whom data were reported in each trial ranged from 35 (Moller 1986) to 129 (Lun 2005).
Setting
The trials were performed in one of five different countries: Canada (Lun 2005), Denmark (Moller 1986), Israel (Finestone 1993), Turkey (Evcik 2010), and USA (Miller 1997). All trials were single‐centre trials.
Participants
Participants in two trials were military recruits undergoing training (Finestone 1993; Miller 1997). The other three trials recruited participants from health clinics (Evcik 2010; Lun 2005; Moller 1986). Although no trials recruited participants who were categorised as elite or professional athletes, military training does comprise intensive exercise regimens.
The percentages of male participants in the individual trials ranged from 16% in Evcik 2010 to 100% in Finestone 1993. There were more females than males in the three non‐military trials. Participant age was not reported in the two military recruit trials. The mean age of participants was 42 years in Evcik 2010, 35 years in Lun 2005, and 23 years in Moller 1986.
Two trials recruited participants with bilateral symptoms: 25 participants (42%) in Finestone 1993 and 57 participants (44%) in Lun 2005.
Duration of symptoms varied considerably across the five trials. Symptoms were acute in both two military training trials. In Finestone 1993, duration of symptoms within two weeks of starting military training and in Miller 1997, within three weeks of starting military training. The mean duration of symptoms was 8.3 months in Lun 2005 and 21 months in both Evcik 2010 and Moller 1986. Duration of symptoms ranged from 1 to 80 months in Evcik 2010 and 3 to 120 months in Moller 1986.
The eligibility criteria for each study are presented in the Characteristics of included studies tables. The most frequently used criterion to determine PFPS in trial cohorts was reported pain on activities such as squatting, prolonged sitting, ascending or descending stairs, walking or running which was used in four trials (Evcik 2010; Finestone 1993; Lun 2005; Miller 1997). Positive signs of symptoms on physical examination including Clarke's compression test, apprehension test, maltracking or patellar tilting were used in two trials (Evcik 2010; Finestone 1993), whilst one trial included radiological evidence of patellofemoral congruence (Evcik 2010), and another trial (Moller 1986) based inclusion on the Turba Score (Turba 1979) for signs and symptoms of PFPS.
Interventions
Three trials tested more than one intervention (Finestone 1993; Lun 2005; Miller 1997). Consequently, these trials appeared in more than one comparison in the analyses.
1. Orthoses
Five different orthoses were used in the included trials. These were categorised for analysis as either knee braces, knee sleeves or patellar straps.
Four trials assessed four different knee sleeves (Evcik 2010; Finestone 1993; Lun 2005; Miller 1997). Evcik 2010 tested a neoprene knee sleeve with a patella cut‐out (Altex Patellar Knee Support, AL‐2285C). In Finestone 1993, participants received either an unnamed elastic neoprene knee sleeve without patella cut‐out or a Genutrain knee sleeve with a silicone patellar ring (Bauerfeind GmbH, Kempen, Germany). In Lun 2005, the knee sleeve group participants received an unnamed, simple elastic neoprene knee sleeve, which did not have a patella cut‐out. Miller 1997 tested a neoprene knee sleeve with a patella cut‐out and additional supportive straps above and below the patellar (Palumbo Dynamic Knee Brace ‐ Dynorthotics, Vienna, Virginia).
Two trials assessed knee braces (Lun 2005; Moller 1986). Lun 2005 randomised a group to a Special FX Knee Brace (Generation II Orthotics Inc, Richmond, British Columbia, USA), which was a knee brace that included a Y‐shaped inferior patellar buttress pad and external stabilisation strap for the patellofemoral joint. Moller 1986 evaluated the use of a custom‐made knee brace made of orthoplast. This was worn from the mid‐thigh region to the foot, cupping the heel. The brace permitted a knee range of motion from zero to 30 degrees of flexion. In comparison, all other knee orthoses permitted unrestricted knee range of motion. Moller 1986 was the only study that did not use a pre‐fabricated (off‐the‐shelf) knee orthosis.
One study assessed the outcomes of the use of a patella strap (Miller 1997). This was the Cho‐Pat Knee Strap (Cho‐Pat Inc, Hainesport, New Jersey, USA), which was a neoprene buttress strap that was positioned over the inferior pole of the patella‐superior aspect of the patellar tendon when standing. The orthosis was purported to reduce patellofemoral joint contact pressures by off‐loading the patellar tendon (Miller 1997).
In two trials, participants randomised to these interventions were instructed to wear these orthoses throughout the day and during physical activity, and only to remove them for sleeping or rest periods (Evcik 2010; Lun 2005). Miller 1997 instructed their participants to wear either their knee sleeve or patella strap orthoses during exercising and all military training activities. Two trials did not specify when knee orthoses were worn by their participants (Finestone 1993; Moller 1986). However, Finestone 1993 reported that recruits were not allowed to discontinue their knee orthoses "without permission of their medical officer".
The knee orthoses were worn for the duration of the trial's follow‐up periods with the exception of Moller 1986. Moller 1986 required participants to wear the orthosis for six weeks, and evaluated outcomes up to 12 months following randomisation.
2. Exercise prescriptions
The exercise prescription provided to participants differed between the included trials. In Finestone 1993, participants were advised to continue with their basic military training with no additional therapeutic exercises. In Miller 1997, participants continued on with their military training but were also enrolled on a physical therapy programme. The other three trials used a home‐based exercise programme (Evcik 2010; Lun 2005; Moller 1986). All programmes incorporated basic quadriceps strengthening exercises. These included isometric and isotonic exercises (Evcik 2010), progressive squats and lunges (Lun 2005) and targeted vastus medialis strengthening (Miller 1997). Moller 1986 also included targeted hamstring strengthening whilst two trials also included stretching as part of their prescription (Lun 2005; Miller 1997). Full details of these programmes are presented in the Characteristics of included studies table.
The duration and intensity of the exercises also varied in their prescription across the trials. This ranged from one set of 10 or more repetitions five times a week (Evcik 2010), to up to 15 minutes of exercises four times a day (Moller 1986). Miller 1997 did not document clearly how many repetitions and how frequently exercises were prescribed and completed.
3. Other co‐interventions
Only Miller 1997 acknowledged the inclusion of a second intervention as part of their exercise programme or orthosis programme. All participants in this trial were also prescribed 800 milligrams of ibuprofen, administered three‐times daily.
Comparisons
All five trials compared a knee orthosis versus a 'no treatment' control group, with all participants in the comparison receiving exercises, either through a military training programme (Finestone 1993), a physical therapy programme as well as military training (Miller 1997), or a home‐based exercise programme.
Two trials directly compared different categories of knee orthoses (Lun 2005; Miller 1997). Lun 2005 compared a knee brace with a knee sleeve, and Miller 1997 compared a patellar strap with a knee sleeve. Although one group in Finestone 1993 was given a knee sleeve with a patellar ring and another group was given a knee sleeve only, we are unsure whether group allocation to the two different knee orthoses was randomised.
One trial also compared a knee orthosis (knee brace) with exercise (Lun 2005).
None of the trials compared different modes of using the same knee orthosis.
Outcomes
Knee pain was reported by all five trials, with three trials using a VAS to measure this (Evcik 2010; Lun 2005; Miller 1997). Pain was assessed on a VAS during sporting activity, one hour after sporting activity and following 30 minutes of sitting with knees flexed in Lun 2005, whilst the change in VAS pain scores from pre‐intervention to final follow‐up was assessed in Miller 1997. A numerical rating of knee pain during activities was used in one trial (Finestone 1993). In addition, the resolution of pain was also assessed in Finestone 1993 using a subjectively rated one to four Likert pain assessment. Moller 1986 assessed swelling, pain, symptoms of instability, and limitations of activity using criteria developed by Turba 1979. This involved a numerical rating system to categorise patient outcomes as excellent, good, fair or poor.
Functional outcomes were assessed in two trials (Evcik 2010; Lun 2005). Evcik 2010 used both the WOMAC score (Klassbo 2003) and the Fulkerson‐Shea Patellofemoral Evaluation score (Owens 2002). Lun 2005 using a modified version of the Knee Function Scale that had been previously utilised and validated in PFPS (Werner 1993).
Participant satisfaction with their treatment was assessed in Finestone 1993 using a one to four Likert system rating. No other studies specifically assessed patient satisfaction.
The impact on sporting or occupational participation was reported in two trials (Miller 1997; Moller 1986). Miller 1997 documented the number of military personnel (their participants) who continued their two months of basic military training. Moller 1986 assessed how many participants returned to sport 12 months post‐randomisation.
The incidence of complications was assessed in one study (Finestone 1993). This was a planned strategy rather than an ad hoc assessment of recording complications.
No trials reported data on a number of important outcome measures including LEFS (Blinkley 1999), the Kujala Patellofemoral Disorder Score (Kujala 1993) or the KOOS (Roos 1998) scores for functional outcomes, health‐related quality of life or general health assessments, or data on resource use or costs of the interventions.
Follow‐up periods
Trial follow‐up periods for the included trials ranged from six weeks (Evcik 2010) to 12 months post‐randomisation (Moller 1986). Miller 1997 assessed outcomes up to eight weeks, Lun 2005 assessed their participants to 12 weeks, whilst Finestone 1993 assessed outcomes fortnightly over a 14‐week basic military training programme, and then two months following completion of training.
Data were collected at intervals within these follow‐up periods in four trials (Finestone 1993; Lun 2005; Miller 1997; Moller 1986). Finestone 1993 assessed their outcomes every two weeks within their 14‐week follow‐up period, and two months after completion of basic military training. Outcomes were assessed at baseline, three, six and 12 weeks post‐randomisation in Lun 2005. The Miller 1997 cohort were assessed weekly for the duration of their eight‐week follow‐up period. Moller 1986 assessed their participants at six weeks, three months and 12 months post‐randomisation.
Excluded studies
The reasons for not including 27 potentially eligible papers following the search strategy results are summarised in the Characteristics of excluded studies.
Sixteen studies were excluded because they were neither randomised nor quasi‐randomised controlled trials (Draper 2009; Farkas 1997; Fukuschima 1992; Greenwald 1996; Gulling 1996; IRCT138810293101N1; Lindberg 1988; Lysholm 1984; McCrory 2004; McCrory 2007; Palumbo 1981; Powers 1999; Powers 2004; Roostayi 2009; Sathe 2002; Worrell 1998). Two further studies were excluded because randomisation was used only to allocate the order of interventions tested within participants (Selfe 2011; Straub 2012). Two trials were excluded since they investigated the use of knee orthoses in the 'prevention' rather than 'treatment' of PFPS (BenGal 1997; Van Tiggelen 2004). In three trials, no form of knee orthosis was investigated (Antich 1986; Avraham 2007; Wijnen 1996). Two studies were excluded since they were considered as testing a resistance exercise device rather than a brace (Denton 2005; Timm 1998). Both studies used a Protonics exercise device knee brace (Inverse Technology Corporation, Lincoln, NE) but since the intervention involved a specific exercise programme, it is predominantly an exercise intervention rather than a knee orthosis. One trial was excluded since it recruited participants who were without signs or symptoms of PFPS (Selfe 2008). One trial was excluded since it did not report any of the pre‐defined outcome measures of interest, solely documenting concentric isokinetic muscle outcomes (Van Tiggelen 2011).
Ongoing studies
Details of the one ongoing trial are provided in the Characteristics of ongoing studies. DRKS00003291 is a multicentre trial based in Germany that aims to compare Patella Pro Orthosis plus physiotherapy versus physiotherapy alone in 135 people who have had PFPS lasting between two months and two years.
Risk of bias in included studies
All five included trials were critically appraised using Cochrane's 'Risk of bias' tool (Higgins 2011a). The results for each included trial are presented in the Characteristics of included studies. A summary of the risk of bias results is presented graphically in Figure 2 and Figure 3. All five trials were judged at high risk of bias from a minimum of three domains, of which one was performance bias reflecting the logistical problems in these trials of blinding of participants and care providers.
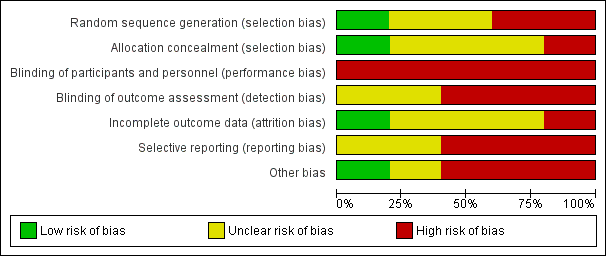
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Only Lun 2005 provided adequate details of the method of sequence generation (use of a random number generator) and allocation concealment (independent assignment); based on this information, we judged this trial to have a low risk of selection bias. We judged Evcik 2010 to be a high risk of selection bias reflecting the quasi‐randomisation method of sequence generation, which was described as being based on "consecutive admissions". The other three trials provided no details of their methods and we judged these at unclear risk of bias for both domains, except for sequence generation for Finestone 1993. We judged this trial at high risk of bias because of the lack of clarity on the allocation into one or other of the two knee‐sleeve groups.
Blinding
All five included trials had a high risk of performance bias in respect of blinding of participants and trial personnel. Due to the nature of knee orthoses and exercise interventions, it may be considered logistically impossible to blind participants or clinicians to group allocation. Lun 2005 was the only paper to document who applied the orthoses under investigation. None of the trials reported whether any standardised information or 'scripts' were used to inform the participants about their orthoses and how and when to wear them in a standardised way. Accordingly, there was a high risk of bias from not standardising assessments via this means and by not blinding clinicians or researchers or both to group allocation.
Both Evcik 2010 and Lun 2005 claimed to be 'single‐blinded' but measures to ensure effective blinding to group allocation were not described. Since subjective outcomes reported by the patients were not blinded, we judged both trials to be at unclear risk of bias. We judged the other three trials to be at high risk of detection bias.
Incomplete outcome data
Although all five trials seemed to document the number of participants who started and completed the trial, only Evcik 2010 was at low risk of bias relating to incomplete data. Three trials were at unclear risk of bias, reflecting lack of data on the numbers of participants, rather than knees, allocated to the interventions in Finestone 1993, greater than 10% loss to follow‐up in Miller 1997, and incomplete reporting of results in Moller 1986. We judged Lun 2005 at high risk of attrition bias reflecting the post‐randomisation exclusions for which the group allocation was not reported, and discrepancies between table and figures reporting pain and function data in the report.
Selective reporting
No trials published a priori protocols. Three trials demonstrated a high risk of reporting bias within their papers (Finestone 1993; Miller 1997; Moller 1986), either through not presenting numerical data to support the conclusions made within the paper (Moller 1986) or not presenting all follow‐up interval data for pre‐specified outcome measurements (Finestone 1993; Miller 1997). Of note, whilst Miller 1997 reported that their cohort was followed for eight weeks, only the one week, and two to three week data was presented in the paper. Two trials clearly presented all outcomes outlined in their methods sections (Evcik 2010; Lun 2005) and so were judged at unclear risk of bias.
Other potential sources of bias
Three trials were at high risk of other bias (Finestone 1993; Lun 2005; Moller 1986). This reflected unresolvable unit of analyses issues relating to inclusion of participants with bilateral symptoms in Finestone 1993 and Lun 2005; and a very poorly described and probably executed data collection process in Moller 1986. We judged that the lack of baseline characteristics data for the individual groups in Miller 1997 put this trial at unclear risk of other bias.
Effects of interventions
As described, two trials recruited participants with bilateral symptoms: 25 participants (42%) in Finestone 1993 and 57 participants (44%) in Lun 2005. Accordingly there were unit of analysis issues to be considered when conducting our analyses. Additionally, there were data discrepancies between table and figures in the article by Lun 2005, a trial that contributes to all three main comparisons for which there are data. Given the sparse data, no subgroup analysis was undertaken.
Comparison 1: Knee orthosis and non‐operative intervention (e.g. exercise) versus non‐operative intervention alone
All five included trials compared the use of a knee orthosis and an exercise programme with an exercise programme alone. Lun 2005 and Moller 1986 assessed knee braces; Evcik 2010, Finestone 1993, Lun 2005 and Miller 1997 assessed knee sleeves; and Miller 1997 also assessed a knee strap. Four trials presented short‐term outcomes (Evcik 2010; Lun 2005; Miller 1997; Moller 1986). Finestone 1993 presented medium term data with final follow‐up completed two months after a 14 weeks military training programme. One trial presented long‐term outcomes at 12 months (Moller 1986).
Primary outcomes
Pain
Individually, none of the three trials providing pain VAS (0 to 10; higher scores mean worse pain) data found a significant difference between knee orthosis versus no knee orthosis at the latest follow‐up for which data were provided (Evcik 2010; Lun 2005; Miller 1997). Pooled final pain score data from Evcik 2010 (knee sleeve) at six weeks and Lun 2005 (knee brace and knee sleeve) at 12 weeks, and change score data up to two or three weeks for Miller 1997 (knee sleeve and patellar strap) showed no clinically important or statistically significant difference between knee orthosis plus exercise versus exercise alone (MD ‐0.46 favouring knee orthoses, 95% CI ‐1.16 to 0.24; P = 0.19; 234 participants; Analysis 1.1; Figure 4). Although the populations and pain measures and timing are clinically heterogeneous, the lack of statistical heterogeneity is notable (Heterogeneity: Chi² = 1.11, df = 4 (P = 0.89); I² = 0%). A sensitivity analysis using the number of knees as denominators in Lun 2005 showed a similar result, with the expected narrowing of the confidence interval ((MD ‐0.41, 95% CI ‐1.04 to 0.23; Analysis 1.2).

Forest plot 1.1. Comparison: knee orthosis and exercises versus exercises alone. Outcome: pain during activity (0 to 10; higher score means worse pain)
Lun 2005 reported finding no statistically significant differences between the two groups for either knee orthosis in any of the three pain assessment scores (0 to 10: higher values mean worse pain) at 12 weeks post‐commencement of treatment. Pooled data from the two knee orthosis groups for the three pain measures (pain during sporting activity; pain one hour after sporting activity; pain following 30 minutes of sitting with knees flexed) are presented in Analysis 1.3. Also presented are sensitivity analyses using the number of knees as denominators, which as above display narrower confidence intervals. The pooled results showed no between group differences in two of the pain measures. Although the results favoured the control (exercise only) group for pain assessed one hour after sporting activity, the mean differences were not clinically important. As noted above, we also have concerns over data discrepancies in Lun 2005 where the labelling of mean values presented in the graphs indicated the converse applied.
Finestone 1993 used a subjectively rated four‐point Likert pain scale (1 (discomfort) to 4 (very severe pain, potentially stopping training). They reported no statistically significant difference in pain scores at end of training between participants randomised to receive a knee sleeve (22 knees; mean score decreased 2.05 points) or a knee sleeve with a patella ring (22 knees; mean score decreased 1.48 points) and basic military training, compared with basic military training alone (40 knees; mean score decreased 1.69 points) at 14 weeks post‐randomisation (reported P > 0.05).
In Moller 1986, pain was measured as part of the Turba Score, which was reported at 12 weeks and 12 months follow‐up. They found little difference between the two groups in the numbers of participants with excellent or good results, reflecting a reduction in symptoms including swelling, pain and instability and improved function at either follow‐up (Analysis 1.4).
Function
Evcik 2010 reported WOMAC functional scores (0 to 68; higher values mean worse function) at six weeks and Lun 2005 reported the results of a modified version of the Knee Function Scale (0 to 53; higher values mean better function). Pooled data from Evcik 2010 (knee sleeve) and Lun 2005 (knee brace and knee sleeve) favoured the control (exercise only) group (SMD ‐0.25, 95% CI ‐0.55 to 0.05; P = 0.10; Analysis 1.5). A sensitivity analysis using the number of knees as denominators also favoured the control group (SMD ‐0.28, 95% CI ‐0.55 to ‐0.01; P = 0.04; Analysis 1.5). The SMD result equates to a small difference at most and in absolute terms, the mean differences for each trial were small and not clinically important.
Secondary outcomes
Quality of life
No studies reported this outcome.
Impact on sport/participation
Two trials assessed outcomes on the impact on sport participation in very different populations (Miller 1997; Moller 1986). Two participants in the knee orthosis group (both were in the knee sleeve group) withdrew from the two‐month military training programme (2/31 versus 0/20; RR 3.28, 95% CI 0.17 to 64.99; Analysis 1.6). The data on this outcome were incomplete for Moller 1986, which reported that 29 of the 35 participants had given up sports activities at the start and that after three months, three participants of the knee brace group and two in the control group had resumed their previous activities. At 12 months, an overall total of eight participants could perform their previous activities.
Resource use
No studies reported this outcome.
Participant satisfaction
This outcome was measured but not reported in Finestone 1993.
Complications
Only Finestone 1993 actively recorded complications and in the knee orthosis groups only. Sixteen complications, consisting of discomfort or local skin abrasions, were recorded for the 44 knees in the two knee orthosis groups: 4 (18% of 22 knees) occurred in the knee sleeve group and 12 (55% of 22 knees) occurred in the knee sleeve with patellar ring group.
Comparison 2: One type of knee orthosis versus another
Three trials compared different types of knee orthoses (Finestone 1993; Lun 2005; Miller 1997); all participants in the three trials also received exercises. However, we are uncertain whether there was random allocation between the two types of knee orthoses used in Finestone 1993. Lun 2005 compared a knee brace with a knee sleeve, Miller 1997 compared a patellar strap with a knee sleeve, and Finestone 1993 compared knee sleeve with a patellar (cut‐out) ring versus a knee sleeve only.
Primary outcomes
Pain
Three trials reported pain as an outcome (Finestone 1993; Lun 2005; Miller 1997).
Finestone 1993 used a subjectively rated four point Likert pain scale (1 (discomfort) to 4 (very severe pain, potentially stopping training). Finestone 1993 reported no statistically significant difference in pain scores at end of training between participants randomised to receive a knee sleeve (22 knees; mean score decreased 2.05 points) or a knee sleeve with a patella ring (22 knees; mean score decreased 1.48 points).
Miller 1997 found no difference between a patellar strap versus a knee sleeve in change of pain scores from pre‐intervention to two to three weeks following the commencement of interventions (MD 0.26, 95% CI ‐1.80 to 2.32; 31 participants; Analysis 2.1).
Lun 2005 found no difference between a knee brace versus knee sleeve in pain during sporting activity scores at 12 weeks (MD ‐0.10, 95% CI ‐1.43 to 1.23; 63 participants; Analysis 2.1). Similar findings applied to pain assessed following 30 minutes sitting with knees flexed (data not shown). Lun 2005 found no clinically important difference between the two orthoses in pain one hour after sporting activity scores at 12 weeks (MD 0.70 favouring knee sleeve, 95% CI ‐0.46 to 1.86; 63 participants; Analysis 2.1). Sensitivity analysis using the number of knees as denominators also demonstrated the lack of differences between the two groups, with narrower confidence intervals.
Function
Only Lun 2005 assessed function as an outcome. Lun 2005 found no clinically important or statistically significant difference between the two orthoses in respect to functional outcomes when assessed using the Knee Function Scale (Werner 1993) (MD ‐1.00, 95% CI ‐4.95 to 2.95; 63 participants; Analysis 2.2) at 12 weeks post‐commencement of treatment.
Secondary outcomes
Quality of life
No studies reported this outcome.
Impact on sport/participation
Miller 1997 reported the impact on sporting activity. Two participants in the knee sleeve group withdrew from the two‐month military training programme (0/13 versus 2/18; RR 0.27, 95% CI 0.01 to 5.22; 31 participants; Analysis 2.3).
Resource use
No studies reported this outcome.
Participant satisfaction
This outcome was measured but not reported in Finestone 1993.
Complications
Finestone 1993 reported 16 complications, consisting of discomfort or local skin abrasions, in the two knee sleeve groups (44 knees). Three times as many complication occurred in the knee sleeve with patellar ring group than in the knee sleeve only group: 12/22 versus 4/22; RR 3.00, 95% CI 1.14 to 7.87; Analysis 2.4). However, as well as unit of analyses problems (data were presented by knees only), it is not clear that the two knee orthoses were allocated randomly.
Comparison 3: Knee orthosis versus another non‐operative intervention (e.g. exercise)
The single trial in this category compared the use of a knee orthosis versus an exercise programme in 66 participants with PFPS (Lun 2005). Thirty‐one participants had bilateral symptoms.
Primary outcomes
Pain
Lun 2005 found no clinically important or statistically significant differences between the two groups in any of the three pain assessment scores (0 to 10: higher values mean worse pain) at 12 weeks post‐commencement of treatment (66 participants; Analysis 3.1): pain during sporting activity (MD ‐0.20 favouring exercise, 95% CI ‐1.22 to 0.82), pain one hour after sporting activity (MD 0.40, 95% CI ‐0.57 to 1.37) and pain following 30 minutes of sitting with knees flexed (MD 0.40, 95% CI: ‐0.76 to 1.56). Sensitivity analyses using the number of knees as denominators also demonstrated the lack of differences between the two groups, with narrower confidence intervals (Analysis 3.2).
Function
Lun 2005 found no clinically important or statistically significant differences between the two groups in functional outcome (0 to 53: higher scores mean greater function) at 12 weeks (MD ‐2.00 favouring exercise, 95% CI ‐5.88 to 1.88; 66 participants; Analysis 3.3). Sensitivity analyses using the number of knees as denominators also demonstrated the lack of differences between the two groups, with narrower confidence intervals (Analysis 3.3).
Secondary outcomes
Lun 2005 did not report on quality of life; impact on sport or occupational participation, resource use, participant satisfaction or complications.
Comparison 4: Mode of knee orthosis use
None of the included trials compared clinical outcomes of the parameters of knee orthosis use such as length of time worn and whether they were worn only during sporting or occupational pursuits or all day or night.
Discussion
Summary of main results
This review included five single‐centre trials reporting results for 368 adults, who were recruited from routine healthcare settings (three trials) or military training (two trials). The evidence for all available outcomes for all comparisons was rated very low quality. This means that we are very uncertain about the results. The trials covered three different types of comparison: knee orthosis and exercises versus exercises alone; one type of orthosis versus another; and knee orthosis versus exercises. No trials assessed the mode of knee orthosis use, such as whether the orthosis was worn all day or only during physical activity.
All five trials compared a knee orthosis (knee sleeve, knee brace, or patellar strap) versus a 'no treatment' control group, with all participants receiving exercises, either through a military training programme or a home‐based exercise programme. The evidence available for this comparison is summarised in summary of findings Table for the main comparison. This shows there is very low quality evidence of no clinically important differences between the two groups in short‐term (2 to 12 weeks follow‐up) knee pain (234 participants, 3 trials) or knee function (183 participants (2 trials)). None of the trials reported on quality of life measures such as the EQ‐5D, resource use or participant satisfaction. Although two trials reported on the impact on sporting or occupational participation, one trial (35 participants) did not provide data split by treatment group on the resumption of sport activity and the other reported only on abandonment of military training due to knee pain (both cases were allocated a knee orthosis). One trial (59 participants, 84 affected knees) recording only adverse events in the two knee orthoses (both were knee sleeves) groups, reported 16 knees (36% of 44 knees) with discomfort or skin abrasion.
Three trials provided very low quality evidence on single comparisons of different types of knee orthosis: a knee brace versus a knee sleeve (Lun 2005: 63 participants), a patella strap with a knee sleeve (Miller 1997: 31 participants), and a knee sleeve with a patellar ring versus a knee sleeve only (Finestone 1993: 44 knees). None of the three trials found an important difference between the two types of knee orthosis in pain. Only Lun 2005 reported on knee function, finding no clinically important difference between a knee brace and a knee sleeve. None of the trials reported on quality of life, resource use or participant satisfaction. Miller 1997 reported that both participants quitting military training due to knee pain were allocated a knee sleeve. While it is not clear whether Finestone 1993 randomised the allocation of the two knee sleeves, they found three times as many knees with adverse effects (discomfort or skin abrasion) in those given knee sleeves with a patella ring than those given knee sleeves only (12/22 versus 4/22).
One trial compared a knee orthosis (knee brace) with exercise (Lun 2005; 66 participants). It found very low quality evidence of no clinically important difference between the two intervention groups in pain or knee function. Lun 2005 did not report on quality of life, impact on sporting or occupational participation, resource use, participant satisfaction or complications.
Overall completeness and applicability of evidence
Despite our comprehensive search, we could include only five small trials, with a maximum of 45 participants in an intervention group. Of the 591 recruited participants, we could pool data for a maximum of 234 (40%) participants for one outcome (pain) of our main comparison. The data available for other outcomes and comparisons were even more limited. Of particular note is the lack of data on complications, such as skin abrasions or irritation for people prescribed knee braces, an outcome reported only in Finestone 1993.
Below we consider applicability of evidence in terms of the sport activity, age and gender of the trial participants, the types of knee orthoses under test, and outcome measurement including timing.
The current evidence has investigated adults in routine healthcare settings (three trials) or military training (two trials). Although military recruits would have participated in intensive exercise regimens, no trials specifically recruited participants categorised as elite or professional athletes. This was a surprising finding given that previous literature has suggested that PFPS is frequently seen in this population, most notably those who participate in football, volleyball and running (Blønd 1998; Myer 2010; Nejati 2011). In both athletes and military trainees, PFPS is highly prevalent and can be a major problem resulting in career change (Rauh 2010). Furthermore, while PFPS is clinically seen in adolescent and childhood populations (Bizzini 2003; Cook 2010; Dixit 2007), none of the included trials focused on this population. This limits the applicability of these findings to adults only, given the differences between children and adults in normal everyday activities undertaken, growth and development factors and potentially compliance with wearing knee orthoses.
The incidence of PFPS is highest in young, physically active females (Boling 2010). This has been attributed to a difference in biomechanical features between the genders (Barton 2009; Nakagawa 2012). It remains unclear whether the biomechanical effects in modifying patellar tracking that knee orthoses are purported to offer (Shellock 1994; Shellock 2000) have a different efficacy between males and females. Moreover, there were insufficient data from the trials in this review to perform subgroup analyses based on gender.
The current evidence has centred around evaluating the effectiveness of knee sleeves and knee braces. This is consistent with usage of these devices and with findings of previous summaries of the literature (Crossley 2001). Only Miller 1997 investigated clinical outcomes of a patellar strap, whilst no trials investigated the use of knee bandages. Overall, there were insufficient data for either direct or indirect comparisons of the knee orthoses tested by the included trials to draw conclusions on the relative effects of the different knee orthoses. Indeed, the statistical homogeneity of the results for pain is notable given the heterogeneity in the populations, outcome measurement, including timing, and the knee orthoses. The descriptions of the application of the knee orthoses were incomplete, particularly in two trials (Finestone 1993; Moller 1986). Moreover, there is no evidence available to inform on the optimal parameters for using knee orthoses, e.g. during exercise only versus during waking hours. Also of note is that an exercise programme was a co‐intervention for the comparisons of knee orthoses versus control; no trial compared knee orthosis alone versus no knee orthosis.
Although the Kujala Patellofemoral Disorder Score (Kujala 1993) and WOMAC score (Klassbo 2003) have been shown to be valid for people with PFPS (Kujala 1993; Laprade 2002), several outcome measures presented in this review, such as the Turba score (Turba 1979) and Knee Function Score (Werner 1993), have not been validated.
The timing of outcome assessment of the included trials also limits applicability. All but Moller 1986 evaluated outcomes of knee orthoses within three months, and so it is unclear whether the results would differ if the knee orthosis was worn for longer. Where the same generic outcome was assessed, the trials used different measures and at different times. This hampers interpretation of the results and their applicability. Context is also important as illustrated by Miller 1997), where our secondary outcome of impact on sporting or occupational participation, was measured only in relation to participants discontinuing a basic military training programme due to incapacitating anterior knee pain. The relevance and applicability of this rather blunt outcome to other populations is very questionable. No trials assessed participant satisfaction, which is important in terms of the expectation of sustained use of knee orthosis by people with PFPS.
Quality of the evidence
We included five trials (one of which was quasi‐randomised) that reported results for 368 people who had PFPS. All five trials were at high risk of bias, including performance bias reflecting the logistical problems in these trials of blinding of participants and care providers (see Figure 2). As assessed using the GRADE approach, the available evidence for all reported outcomes is 'very low' quality, therefore raising major questions on the reliability of the results.
The rationales for downgrading the evidence by three levels for individual outcomes for the comparison of knee orthosis and exercise versus exercise alone are provided in the footnotes of summary of findings Table for the main comparison. For the comparisons of difference knee orthoses and knee orthosis versus exercise, we downgraded the evidence two levels for major study limitations resulting in very serious risk of bias and one level for imprecision reflecting that the results were from small single trials.
Potential biases in the review process
Efforts were made to limit potential biases during the review process. This included the searching of a variety of relevant published and grey literature/trial registry databases with no language restriction to ensure we identified all relevant trials. Secondly, two review authors independently conducted the trial identification, data extraction and assessment of risk of bias, adjudicated by a third review author. Through this, the process of verification of data was ensured to minimise the risk of misreporting of trial findings. The analysis results were verified by all review authors, including a medical statistician (AC). We adopted a purposefully conservative approach to the use and interpretation of data from the two trials that presented substantial unit of analysis issues.
Agreements and disagreements with other studies or reviews
We identified two recent literature reviews that considered the use of knee orthosis for treating PFPS (Al‐Hakim 2012; Swart 2012). Al‐Hakim 2012, which was a narrative review that evaluated the use of all non‐surgical interventions for PFPS, provided brief summaries of the individual findings of no benefit from knee orthoses reported by two studies included in our review (Finestone 1993; Miller 1997). Swart 2012, which was a systematic review that evaluated the use of lower limb orthoses and taping, identified three trials testing knee orthoses (Denton 2005; Lun 2005; Miller 1997). Of note is that Denton 2005 is excluded in our review because we consider the intervention tested is essentially a resistive exercise device and not a knee orthosis. Similar to our review, Swart 2012 concluded that more high quality studies were needed "to draw definitive conclusions".
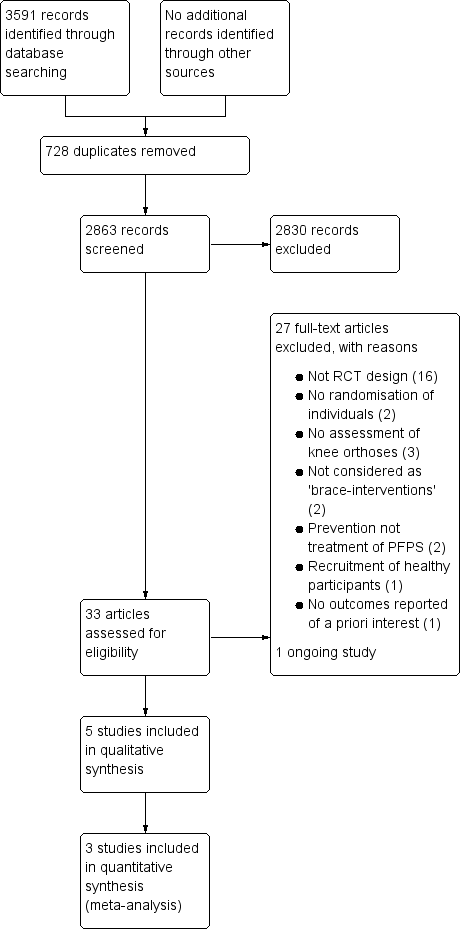
Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
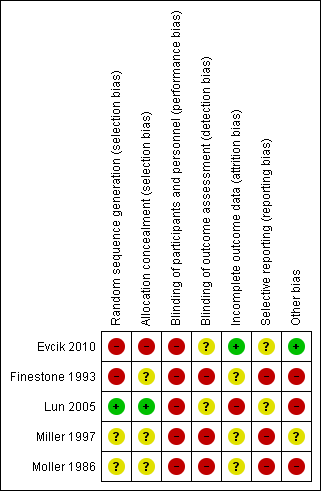
Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Forest plot 1.1. Comparison: knee orthosis and exercises versus exercises alone. Outcome: pain during activity (0 to 10; higher score means worse pain)

Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 1 Pain during activity (0 to 10; higher score means worse pain).
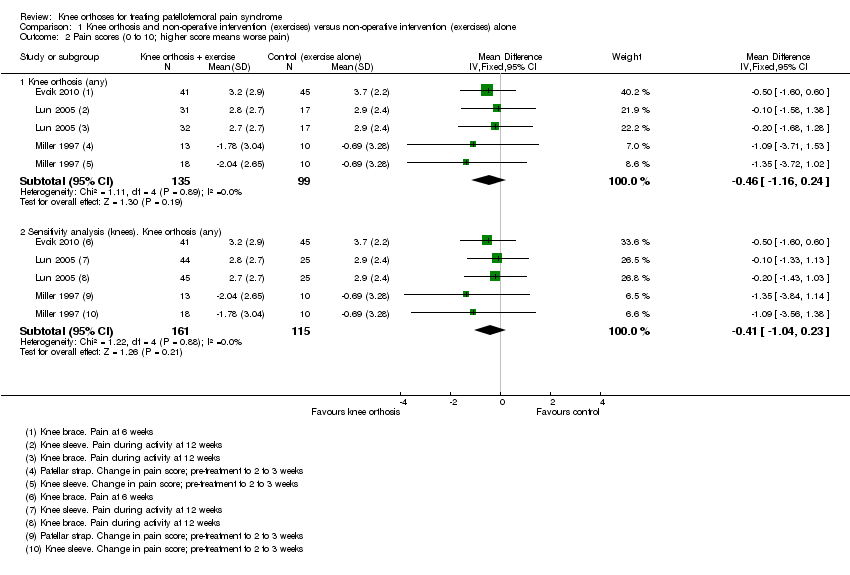
Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 2 Pain scores (0 to 10; higher score means worse pain).

Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 3 Different pain scores (0 to 10; higher score means worse pain) at 12 weeks.
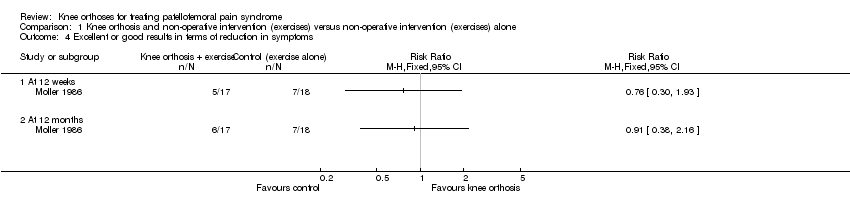
Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 4 Excellent or good results in terms of reduction in symptoms.

Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 5 Functional scores (higher score means higher function).
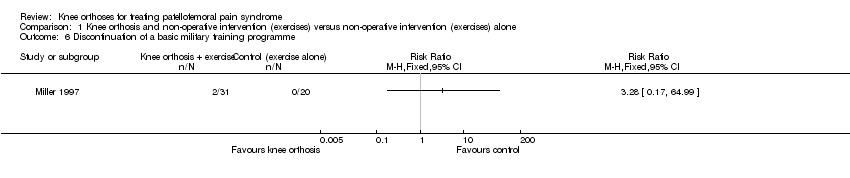
Comparison 1 Knee orthosis and non‐operative intervention (exercises) versus non‐operative intervention (exercises) alone, Outcome 6 Discontinuation of a basic military training programme.

Comparison 2 One type of orthosis versus another type, Outcome 1 Pain score (0 to 10: higher score means worse pain).

Comparison 2 One type of orthosis versus another type, Outcome 2 Functional score (0 to 53: higher scores means greater function).
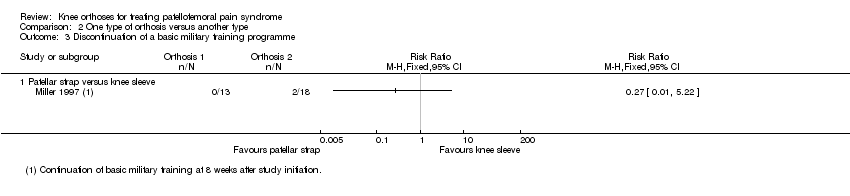
Comparison 2 One type of orthosis versus another type, Outcome 3 Discontinuation of a basic military training programme.

Comparison 2 One type of orthosis versus another type, Outcome 4 Complications.

Comparison 3 Orthosis versus exercise, Outcome 1 Pain during activity (0 to 10: higher score means worse pain).
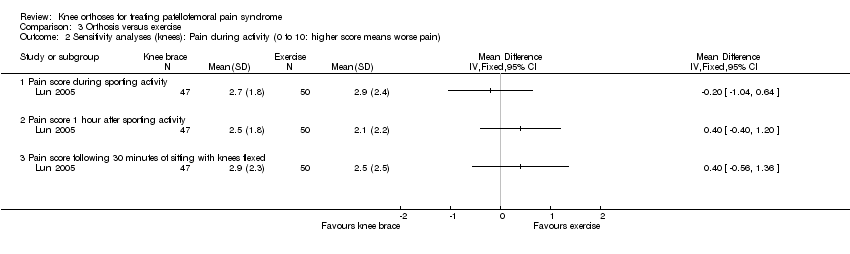
Comparison 3 Orthosis versus exercise, Outcome 2 Sensitivity analyses (knees): Pain during activity (0 to 10: higher score means worse pain).

Comparison 3 Orthosis versus exercise, Outcome 3 Functional scores (0 to 53: higher scores means greater function).
| Knee orthosis and exercise versus exercise alone for patellofemoral pain syndrome (PFPS) | ||||||
| Patient or population: Adults (recruited from health clinics or military recruits) with PFPS (duration of symptoms ranged from acute, under 2 to 3 weeks in two trials, to predominantly chronic in three trials: mean durations 8.3 months, 21 months, 21 months) Settings: Health clinics, home and military training establishments Intervention: Knee orthosis (various types: knee sleeve, knee brace or patellar strap) and exercise (military training, home exercise programme) Comparison: Exercise alone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Exercise alone | Knee orthosis and exercise | |||||
| Pain score (VAS) Scale from: 0 to 10 (higher scores mean worse pain) Follow‐up: 3 to 12 weeks (short‐term) | The mean pain score for the exercise alone group ranged across the control groups from 2.7 to 3.2 points; the mean change score from ‐0.47 to ‐0.96 points | The mean pain score in the knee orthosis and exercise group was 0.46 points lower (1.16 lower to 0.24 higher) | MD ‐0.46 (‐1.16 to 0.24) | 234 (3) | ⊕⊝⊝⊝ | The MD and 95% CIs do not include clinically important treatment effects. MCID: 30 mm on an 100 mm VAS (Lee 2003) |
| Functional outcomes Scale various 2 Follow‐up: 6 and 12 weeks (short‐term) | The mean functional score in the knee orthosis and exercise group was 0.15 points lower (0.69 lower to 0.38 higher) The mean difference in knee function (short‐term) in the knee orthosis group was 0.25 standard deviations lower (0.55 lower to 0.05 higher) | SMD ‐0.25 (‐0.55 to 0.05) | 183 (2) | ⊕⊝⊝⊝ | Lower values equate to higher disability. The SMD result equates to a small difference at most and in absolute terms, the mean differences for each trial were small (e.g. 0.9 for a range 0 to 68) and not clinically important | |
| Quality of Life and General Health Assessments | See comment | See comment | No study reported this outcome | |||
| Impact on sporting and occupational participation | See comment | See comment | 51 (1)4 | ⊕⊝⊝⊝ | One trial reported that 2 out of 31 (6.5%) participants in the knee orthosis groups versus 0 of 20 (0%) in the control group withdrew from their military training programme. | |
| Resource use | See comment | See comment | No study reported this outcome | |||
| Participant satisfaction | See comment | See comment | No study reported this outcome | |||
| Complications Follow‐up: 14 weeks6 | See comment | See comment | 59 with 84 affected knees (1) | ⊕⊝⊝⊝ | Trial reported 16 complications (skin abrasions or discomfort) for 44 knees (36%) of participants in the knee orthosis group. | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including selection bias (1 trial) and performance bias (all 3 trials)), and one level for indirectness (this reflects the clinical heterogeneity such as variation in the interventions and outcome measures and measurement, and the generally inadequate description of these). There was, however, no statistical heterogeneity in the pooled data. 2. One trial reported WOMAC functional scores (0 to 68; higher values mean worse function) at six weeks and the other the results of a modified version of the Knee Function Scale (0 to 53; higher values mean better function) at 12 weeks. 3. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including selection bias (1 trial) and performance bias (both trials)), and one level for imprecision (wide confidence intervals and limited data). 4. Data on resumption of sports activities were not split by treatment group in one trial (35 participants). 5. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including performance and detection biases), and one level for indirectness (abandonment of military training may be for other reasons than serious knee pain). 6. The single study recording this outcome did not record complications for all groups. The follow‐up for complications appeared be during use; i.e. the basic military training programme of 14 weeks.. 7. The quality of the evidence was downgraded two levels for major study limitations resulting in very serious risk of bias (including performance and detection biases and serious unit of analyses issues relating to the inclusion of participants with anterior knee pain in both knees), and imprecision (incomplete data from one small trial). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during activity (0 to 10; higher score means worse pain) Show forest plot | 3 | 234 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐1.16, 0.24] |
| 1.1 Knee sleeve | 3 | 162 | Mean Difference (IV, Fixed, 95% CI) | ‐0.48 [‐1.31, 0.35] |
| 1.2 Patellar strap | 1 | 23 | Mean Difference (IV, Fixed, 95% CI) | ‐1.09 [‐3.71, 1.53] |
| 1.3 Knee brace | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.68, 1.28] |
| 2 Pain scores (0 to 10; higher score means worse pain) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Knee orthosis (any) | 3 | 234 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐1.16, 0.24] |
| 2.2 Sensitivity analysis (knees). Knee orthosis (any) | 3 | 276 | Mean Difference (IV, Fixed, 95% CI) | ‐0.41 [‐1.04, 0.23] |
| 3 Different pain scores (0 to 10; higher score means worse pain) at 12 weeks Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 Pain during activity | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐1.20, 0.90] |
| 3.2 Sensitivity analysis (knees). Pain during activity | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐1.02, 0.72] |
| 3.3 Pain 1 hour after sporting activity | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐0.19, 1.69] |
| 3.4 Sensitivity analysis (knees). Pain 1 hour after sporting activity | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.75 [‐0.04, 1.53] |
| 3.5 Pain after 30 minutes sitting with knees flexed | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.82, 1.32] |
| 3.6 Sensitivity analysis (knees). Pain after sitting with knees flexed | 1 | 139 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.64, 1.14] |
| 4 Excellent or good results in terms of reduction in symptoms Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 At 12 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 At 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Functional scores (higher score means higher function) Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Knee orthosis (any) | 2 | 183 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.55, 0.05] |
| 5.2 Sensitivity analysis (knees): Knee orthosis (any) | 2 | 225 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.55, ‐0.01] |
| 6 Discontinuation of a basic military training programme Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain score (0 to 10: higher score means worse pain) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Patellar strap versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Functional score (0 to 53: higher scores means greater function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Knee brace versus knee sleeve | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Knee brace versus knee sleeve (sensitivity analysis: knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Discontinuation of a basic military training programme Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Patellar strap versus knee sleeve | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Complications Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Knee sleeve and patella ring versus knee sleeve without patellar ring | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain during activity (0 to 10: higher score means worse pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Pain score during sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Pain score 1 hour after sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Pain score following 30 minutes of sitting with knees flexed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Sensitivity analyses (knees): Pain during activity (0 to 10: higher score means worse pain) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Pain score during sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Pain score 1 hour after sporting activity | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Pain score following 30 minutes of sitting with knees flexed | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Functional scores (0 to 53: higher scores means greater function) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Participants = denominators | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Sensitivity analysis (knees) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

