Técnica de "rendezvous" laparoscópica‐endoscópica versus esfinterotomía endoscópica preoperatoria en pacientes sometidos a colecistectomía laparoscópica para los cálculos de la vesícula biliar y el conducto biliar
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Parallel randomised controlled clinical trial Randomisation ratio: superiority design | |
| Participants | 120 patients with cholecysto‐choledocholithiasis detected by transabdominal ultrasound and magnetic resonance cholangiopancreatography (MRCP); mean age 54.2 years, male 43%; history of relapsing pancreatitis: 30%; bile duct diameter < 8 mm: 12.5% Inclusion criteria: gallbladder and main bile duct stones and one or more of the following patient‐related risk factors for post‐ERCP pancreatitis: age < 60 years;history of relapsing pancreatitis; bile duct diameter < 8 mm Exclusion criteria: chronic pancreatitis and previous sphincterotomy Diagnostic criteria: gallbladder and main bile duct stones detected by both transabdominal ultrasound and MRCP | |
| Interventions | Number of study centres: one Treatment before study: not reported Type of interventions: 60 participants treated in a single step with videolaparoscopic cholecystectomy, intraoperative cholangiography, and endoscopic sphincterotomy during the surgical procedure with the rendezvous technique versus 60 treated with preoperative ERCP and endoscopic sphincterotomy using a traditional method of bile duct cannulation | |
| Outcomes | Rate of acute pancreatitis, level of amylasemia | |
| Notes | Run‐in period: from January 2002 to September 2004 Study terminated before regular end (for benefit or because of adverse events): no Follow‐up: not reported Funding sources: no information reported Declaration of interest: no information reported Country: Italy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation into two groups |
| Allocation concealment (selection bias) | Unclear risk | No report on concealment of randomisation |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | The outcomes assessors were not blinded. |
| Incomplete outcome data (attrition bias) | High risk | in the LERV group "in one patient, the guidewire did not pass through the papilla, so it was necessary to make a precut. In two participants, conversion to open surgery with choledochotomy was needed: in one case due to prepapillary giant impacted stones and in the other case due to a technical problem (loss of the wire in the intestinal loops). The latter patient did not undergo the endoscopic procedure and was therefore excluded from the statistical analysis". In the other group (preoperative ERCP and endoscopic sphincterotomy performed using a traditional method of bile duct cannulation), the precut technique was needed in one patient. |
| Selective reporting (reporting bias) | Unclear risk | The trial protocol was not available. |
| Other bias | High risk | The learning curve was not reported. |
| for‐profit bias | Unclear risk | Information about sponsorship or trial support not reported |
| Methods | Parallel randomised controlled clinical trial Randomisation ratio: superiority design | |
| Participants | 91 elective patients with cholelithiasis and common bile duct stones diagnosed at MRCP; mean age 59.5 years; male 38.4%; normal value of total bilirubin: 72.5%; normal value of gamma GT: 92%; normal value of AST: 80.15%; normal value of amylase: 26%; common bile duct diameter ⋝10 mm: 62.6% Inclusion criteria: people with gallbladder and main bile duct stones Exclusion criteria: acute cholangitis, necrotizing pancreatitis, age < 18 years, ASA status IV and V Diagnostic criteria: gallbladder and main bile duct stones were detected by transabdominal ultrasound and MRCP | |
| Interventions | Number of study centres: one Treatment before study: not reported Type of interventions: 46 participants treated in a single step with videolaparoscopic cholecystectomy, intraoperative cholangiography, and endoscopic sphincterotomy during the surgical procedure with the rendezvous technique, and 45 treated with preoperative ERCP and endoscopic sphincterotomy using a traditional method of bile duct cannulation. | |
| Outcomes | Morbidity, clinical pancreatitis, hyperamylasaemia, failure rate, mean hospital stay (days) | |
| Notes | Run‐in period: from May 2001 to August 2005 Study terminated before regular end (for benefit or because of adverse events): no Follow‐up: 19 to 20 months Funding sources: no information reported Declaration of interest: no information reported Country: Italy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Not clearly stated whether the outcome assessors were blinded to the treatments or not. |
| Incomplete outcome data (attrition bias) | Low risk | None |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. |
| Other bias | High risk | The learning curve was not reported. |
| for‐profit bias | Unclear risk | Information about sponsorship or trial support not reported |
| Methods | Parallel randomised controlled clinical trial Randomisation ratio: superiority design | |
| Participants | 123 patients referred for laparoscopic cholecystectomy; mean age not reported; sex not reported; total bilirubin: intraoperative ERCP: 3.1 mg/dl (SD 2.9), pre‐operative ERCP: 2.0 mg/dl (SD 2.0); GGT: intraoperative ERCP 441 IU (SD 326 IU), pre‐operative ERCP: 334 IU (SD 281 IU) Inclusion criteria: people with intermediate risk of choledocholithiasis; one of the following major screening criteria: recent episode of cholangitis; bilirubin level > 3.5 mg/dl, or ultrasound evidence of a shadowing object within the bile duct; or at least two of the following minor screening criteria: recent episode of acute pancreatitis, cholecystitis or jaundice; elevated liver function tests above the normal limits; or a dilated common bile duct > 8 mm on ultrasound Exclusion criteria: age > 18 years to < 80 years Diagnostic criteria: gallbladder and main bile duct stones were detected by transabdominal ultrasound. Computed tomography or MRCP were optional, and rarely used in either study group. | |
| Interventions | Number of study centres: one Treatment before study: not reported Type of interventions: 59 participants treated in a single step with videolaparoscopic cholecystectomy, intraoperative cholangiography, and endoscopic sphincterotomy during the surgical procedure with the rendezvous technique versus 64 treated with preoperative ERCP and endoscopic sphincterotomy performed using a traditional method of bile duct cannulation. | |
| Outcomes | Success rate (on an intention‐to‐treat basis), total morbidity (mild to moderate morbidity, severe morbidity), post‐ERCP morbidity (mild to moderate morbidity, severe morbidity), post‐ERCP acute pancreatitis, post‐ERCP cholecystitis, post‐ERCP cholangitis, post‐ERCP papillar bleeding, morbidity of cholecystectomy | |
| Notes | Run‐in period: from June 1999 to June 2003 Study terminated before regular end (for benefit or because of adverse events): no Follow‐up: 24 months Funding sources: no information reported Declaration of interest: none declared Country: Spain | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Not clearly stated whether the outcomes assessors were blinded to the treatments or not. |
| Incomplete outcome data (attrition bias) | Low risk | None |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. |
| Other bias | High risk | The learning curve was not reported. |
| for‐profit bias | Unclear risk | Information about sponsorship or trial support not reported |
| Methods | Parallel randomised controlled clinical trial Randomisation ratio: superiority design | |
| Participants | 83 patients with a diagnosis of cholecysto‐choledocholithiasis; mean age 47.95 years; male 36.1%; mean total serum bilirubin: 7.2 mg/dl; mean serum alkaline phosphatase: 619 IU/L; mean common bile duct diameter: 12.6 mm Inclusion criteria: people with diagnosis of cholelithiasis and choledocholithiasis Exclusion criteria: persons with stones in CBD > 12 mm, after undergoing laparoscopic CBD exploration Diagnostic criteria: abdominal ultrasound and MRCP | |
| Interventions | Number of study centres: one Treatment before study: not reported Type of interventions: 42 participants treated in a single step with video laparoscopic cholecystectomy, intraoperative cholangiography, and endoscopic sphincterotomy during the surgical procedure with the rendezvous technique versus 41 treated with preoperative ERCP and endoscopic sphincterotomy. | |
| Outcomes | Success rate of CBD clearance, incidence of multiple endoscopic procedures within 30 days of the procedure, incidence of hyperamylasaemia within 48 hours post‐ERCP, incidence of severe pancreatitis within 48 hours post‐ERCP, post‐operative hospital stay, number of deaths within 30 days of intervention, patient satisfaction concerning the surgical procedure carried out, endoscopic surgeon's satisfaction with the endoscopic procedure | |
| Notes | Run‐in period: from 2005 to 2012 Study terminated before regular end (for benefit or because of adverse events): no Follow‐up: not reported Funding sources: none Declaration of interest: none declared Country: India | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Not clearly stated whether the outcomes assessors were blinded to the treatments or not. |
| Incomplete outcome data (attrition bias) | Low risk | None |
| Selective reporting (reporting bias) | High risk | The study protocol was not available. Mortality not reported in the results, though it was declared as an outcome in the method section. |
| Other bias | High risk | The learning curve was not reported. |
| for‐profit bias | Low risk | Free of industry sponsorship or other for‐profit support |
| Methods | Randomised controlled clinical trial Randomisation ratio: superiority design Interim analysis of the first 100 randomised patients | |
| Participants | 100 patients with cholecysto‐choledocholithiasis; one patients from the control group withdrew consent after randomisation; mean age: 67.5 years; male: 46.5%; median common bile duct diameter: 9 mm; mean BMI: 27; ASA I: 51.5%, II: 37.5%, III: 11% Inclusion criteria: people with stones in gallbladder and CBD Exclusion criteria: age < 18 years, ASA status IV and V, BMI > 35, previous ERCP attempt, history of upper abdominal surgery, and pregnancy Diagnostic criteria: gallbladder and main bile duct stones were detected by both transabdominal ultrasound and MRCP | |
| Interventions | Number of study centres: one Treatment before study: not reported Type of interventions: 50 patients treated in a single step with videolaparoscopic cholecystectomy, intraoperative cholangiography, and endoscopic sphincterotomy during the surgical procedure with the rendezvous technique versus 49 treated with preoperative ERCP and endoscopic sphincterotomy using a traditional method of bile duct cannulation | |
| Outcomes | Mortality, morbidity, conversions, clinical pancreatitis, serum amylase, failure rate, hospital stay (days) | |
| Notes | Run‐in period: from September 2006 to April 2009 Study terminated before regular end (for benefit or because of adverse events): no Follow‐up: not reported Funding sources: no information reported Declaration of interest: none declared Country: Greece | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization created by a computer‐generated list in blocks of 20 patients. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Not clearly stated whether the outcomes assessors were blinded to the treatments or not. |
| Incomplete outcome data (attrition bias) | Low risk | One patient from the control group withdrew consent after randomisation. |
| Selective reporting (reporting bias) | Low risk | The trial was registered at one of the available official sites for clinical trials registration (ClinicalTrials.gov ID: NCT00416234). |
| Other bias | Low risk | Interim analysis planned after completion of the first 100 patients |
| for‐profit bias | Unclear risk | Information about sponsorship or trial support not reported |
ERCP = endoscopic retrograde cholangiopancreatography; LERV = laparoscopic‐endoscopic rendezvous; CBD = common bile duct; MRCP = magnetic resonance cholangiopancreatography; ASA = American Society of Anesthesiologists; BMI = body mass index; AST = aspartate aminotransferase
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| A controlled non‐randomised clinical study with three equally numbered study groups: 16 people with cholelithiasis underwent LERV; 16 people with common bile duct stones underwent endoscopic sphincterotomy before laparoscopic cholecystectomy, and 16 people with papillitis underwent open cholecystectomy and transduodenal sphincterotomy. | |
| A controlled non‐randomised clinical study with two groups of persons with cholelithiasis and common bile duct stones or papillitis: 70 underwent LERV and 80 underwent endoscopic sphincterotomy before laparoscopic cholecystectomy. | |
| A controlled non‐randomised clinical study with two groups of participants with cholelithiasis and common bile duct stones or papillitis: 21 underwent laparoscopic cholecystectomy combined with intraoperative endoscopic sphincterotomy and 17 had endoscopic sphincterotomy before laparoscopic cholecystectomy. In the early patients, the investigators tried to pass a guided wire through the cystic duct into the CBD to facilitate bile duct cannulation at subsequent endoscopy (the LERV technique described by Cavina and colleagues), but they found it technically difficult, and also experienced difficulties during laparoscopic cholecystectomy (due to bowel insufflation), so this step was omitted in most cases. | |
| A controlled non‐randomised clinical trial of two groups of participants with cholelithiasis and common bile duct stones or papillitis: 21 underwent LERV and 17 had endoscopic sphincterotomy before laparoscopic cholecystectomy. | |
| A controlled non‐randomised clinical trial: 21 underwent LERV and 17 had endoscopic sphincterotomy before laparoscopic cholecystectomy. | |
| A controlled non‐randomised clinical trial with three groups of participants with cholelithiasis and common bile duct stones or papillitis: 8 underwent LERV, 73 had endoscopic sphincterotomy before laparoscopic cholecystectomy, and 16 combined laparoscopic cholecystectomy and CBD exploration (LCBDE). | |
| A controlled non‐randomised clinical trial with two groups of participants with cholelithiasis and common bile duct stones or papillitis: 35 underwent LERV and 41 had endoscopic sphincterotomy before laparoscopic cholecystectomy. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Overall morbidity (30 days postoperative) Show forest plot | 4 | 434 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.29, 1.20] |
| Analysis 1.1 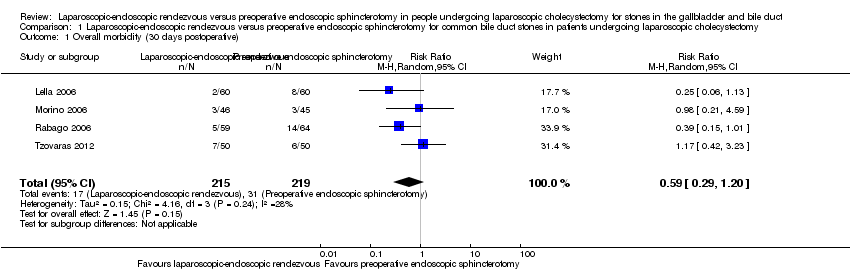 Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 1 Overall morbidity (30 days postoperative). | ||||
| 2 Overall morbidity (30 days postoperative) Show forest plot | 4 | 434 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.32, 0.99] |
| Analysis 1.2  Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 2 Overall morbidity (30 days postoperative). | ||||
| 3 Failure of primary clearance Show forest plot | 5 | 517 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.22, 1.38] |
| Analysis 1.3 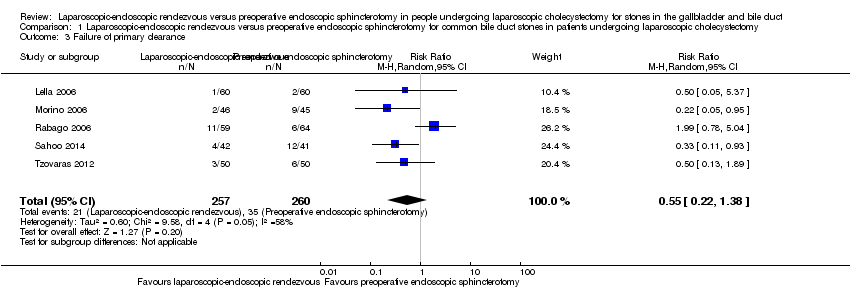 Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 3 Failure of primary clearance. | ||||
| 4 Failure of primary clearance Show forest plot | 5 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.37, 1.01] |
| Analysis 1.4 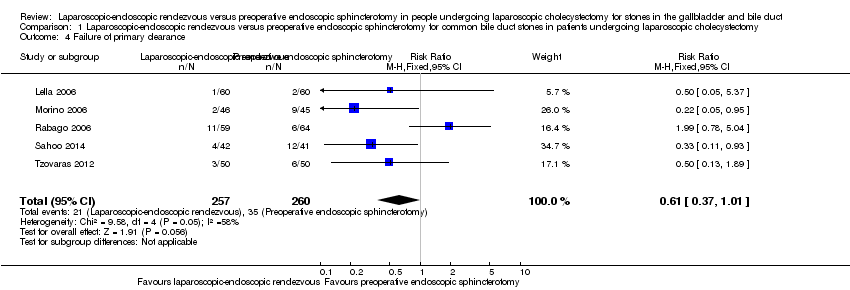 Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 4 Failure of primary clearance. | ||||
| 5 Clinical postoperative pancreatitis Show forest plot | 5 | 517 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.09, 1.14] |
| Analysis 1.5 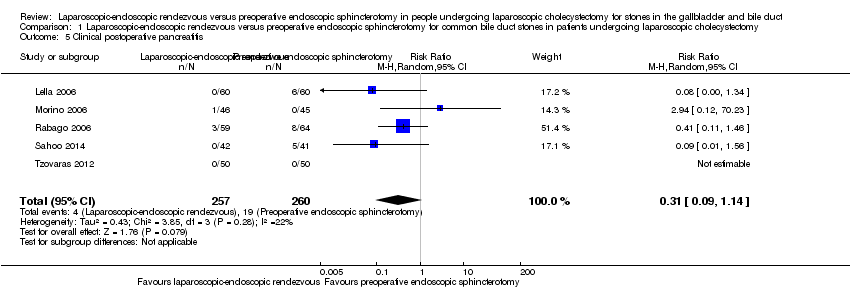 Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 5 Clinical postoperative pancreatitis. | ||||
| 6 Clinical postoperative pancreatitis Show forest plot | 5 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.11, 0.69] |
| Analysis 1.6  Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 6 Clinical postoperative pancreatitis. | ||||
| 7 Operative time Show forest plot | 3 | 313 | Mean Difference (IV, Random, 95% CI) | 34.07 [11.41, 56.74] |
| Analysis 1.7 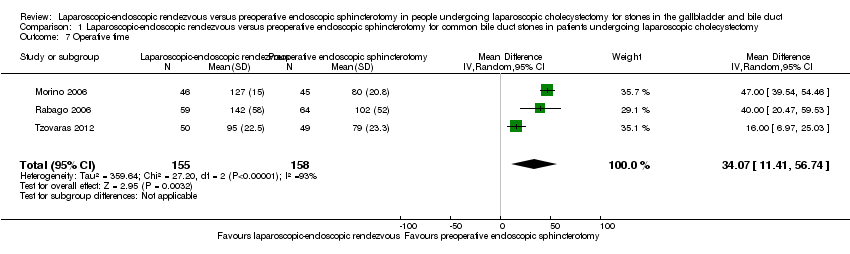 Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 7 Operative time. | ||||
| 8 Operative time Show forest plot | 3 | 313 | Mean Difference (IV, Fixed, 95% CI) | 34.85 [29.34, 40.37] |
| Analysis 1.8 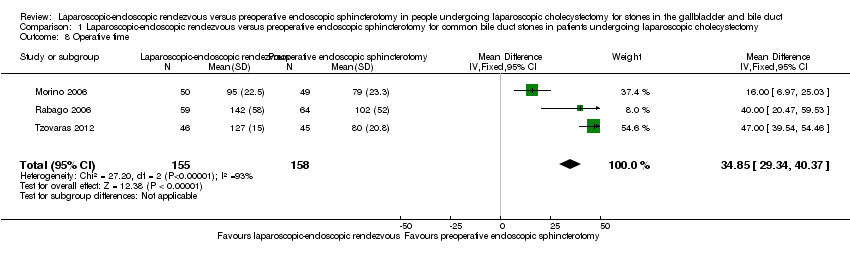 Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 8 Operative time. | ||||
| 9 Length of hospital stay Show forest plot | 5 | 515 | Mean Difference (IV, Random, 95% CI) | ‐3.01 [‐3.51, ‐2.50] |
| Analysis 1.9  Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 9 Length of hospital stay. | ||||
| 10 Length of hospital stay Show forest plot | 5 | 515 | Mean Difference (IV, Fixed, 95% CI) | ‐3.00 [‐3.37, ‐2.64] |
| Analysis 1.10  Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 10 Length of hospital stay. | ||||

Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias graph: review authors' judgements about each risk of bias item presented for each trial

Trial Sequential Analysis of operating time. DARIS = Pc 49.52%; RRR 20%; alpha 1.6%; beta 20 %; diversity 94%.
The cumulative Z‐curve (blue line) immediately crosses the conventional boundary line. This suggests that there was a difference in the operating time between laparoscopic‐endoscopic rendezvous and preoperative endoscopic sphincterotomy, with a low risk of random error. The horizontal green lines illustrate the conventional level of statistical significance, which was intersected from the first trial. With 313 patients randomised, we had sufficient evidence to accept that preoperative endoscopic sphincterotomy took less operative time than laparoscopic‐endoscopic rendezvous. We used Trial Sequential Analysis software to conduct the analysis and to generate the figure.
Legend: square symbol: Z‐score for single study; diamond symbol: trial sequential monitoring boundary for benefit score for single study.
Abbreviations: DARIS: diversity‐adjusted required information size; Pc: control group proportion observed in the trials; RRR = a relative risk reduction.

Trial Sequential Analysis of length of hospital stay. DARIS = Pc 50.29%; RRR 20%; alpha 1.6%; beta 20 %; diversity 49%.
The horizontal green lines illustrate the conventional level of statistical significance, which was intersected from the first trial. In the analysis with 515 patients randomised, we had sufficient evidence to accept that laparoscopic‐endoscopic rendezvous resulted in a shorter hospital stay than preoperative endoscopic sphincterotomy. We used Trial Sequential Analysis software to conduct the analysis and to generate the figure.
Legend: square symbol: Z‐score for single study; diamond symbol: trial sequential monitoring boundary for benefit score for single study.
Abbreviations: DARIS: diversity‐adjusted required information size; Pc: control group proportion observed in the trials; RRR = a relative risk reduction.

Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 1 Overall morbidity (30 days postoperative).
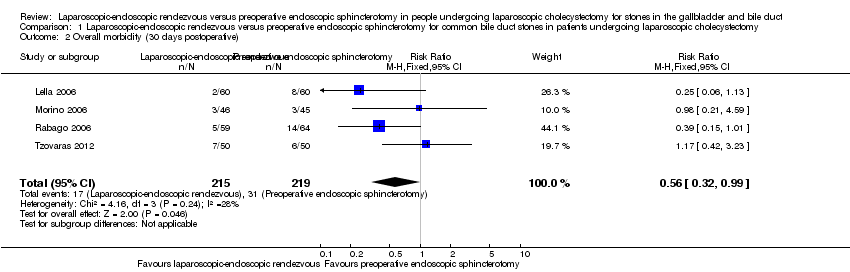
Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 2 Overall morbidity (30 days postoperative).
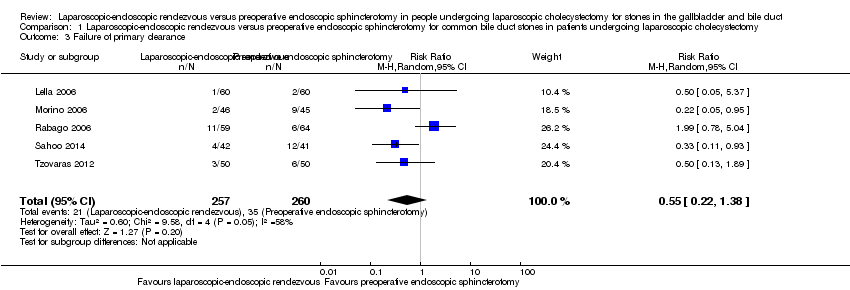
Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 3 Failure of primary clearance.
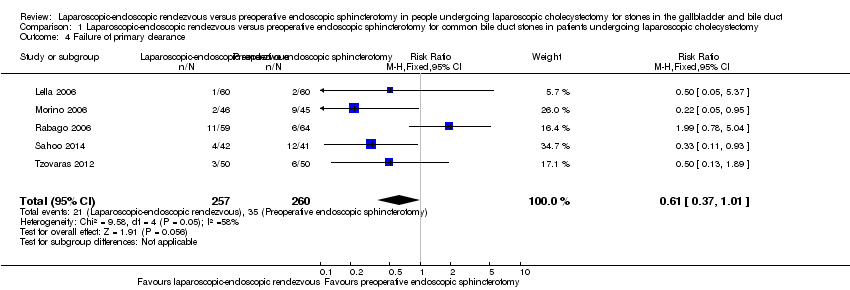
Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 4 Failure of primary clearance.

Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 5 Clinical postoperative pancreatitis.

Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 6 Clinical postoperative pancreatitis.

Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 7 Operative time.

Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 8 Operative time.
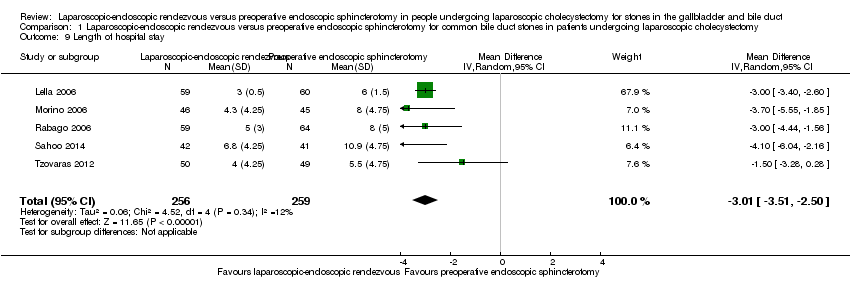
Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 9 Length of hospital stay.
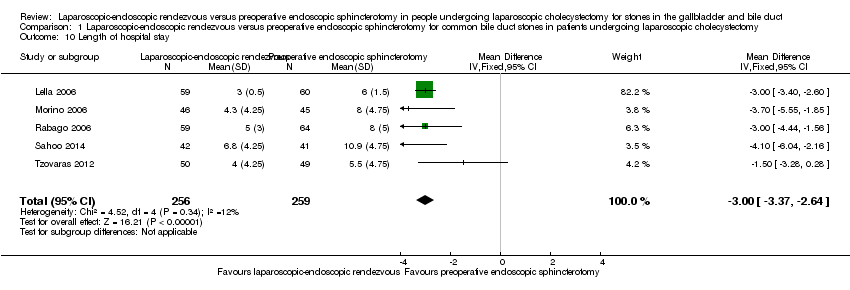
Comparison 1 Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy for common bile duct stones in patients undergoing laparoscopic cholecystectomy, Outcome 10 Length of hospital stay.
| Laparoscopic‐endoscopic rendezvous versus preoperative endoscopic sphincterotomy in people undergoing laparoscopic cholecystectomy for stones in the gallbladder and common bile duct | ||||||
| Population: patients with stones in the gallbladder and common bile duct undergoing laparoscopic cholecystectomy Control: preoperative endoscopic sphincterotomy | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with preoperative endoscopic sphincterotomy | Risk with laparoscopic‐endoscopic rendezvous | |||||
| Overall mortality (30‐day postoperative; procedure‐ and non‐procedure related) | Study population | 516 | ⊕⊕⊝⊝ | Only 1 death in 1 trial reported, in the LERV group | ||
| 0 per 1000 | 0 per 1000 | |||||
| Overall morbidity (30‐day postoperative; procedure‐ and non‐procedure related) | Study population | RR 0.59 | 433 | ⊕⊕⊝⊝ | No trials defined overall morbidity in the methods section. | |
| 142 per 1000 | 84 per 1000 | |||||
| Moderate | ||||||
| 128 per 1000 | 75 per 1000 | |||||
| Failure of primary clearance | Study population | RR | 516 | ⊕⊝⊝⊝ | ||
| 131 per 1000 | 72 per 1000 | |||||
| Moderate | ||||||
| 102 per 1000 | 56 per 1000 | |||||
| Clinical postoperative pancreatitis | Study population | RR 0.31 | 516 | ⊕⊕⊝⊝ | ||
| 73 per 1000 | 23 per 1000 | |||||
| Moderate | ||||||
| 100 per 1000 | 31 per 1000 | |||||
| Operative time | The mean operative time in the control groups was 88.6 minutes | The mean operative time in the LEVR groups was 34.07 minutes higher (11.41 to 56.74 higher) | MD: 34.07 (11.41 to 56.74) | 313 | ⊕⊝⊝⊝ | TSA: 23.07 (15.32 to ‐30.81) |
| Length of hospital stay | The mean length of hospital stay in the control groups was 7.5 days | The mean length of hospital stay in the LEVR groups was 3.01 days shorter (3.51 to 2.5 days shorter) | MD: ‐3.01 (‐3.51 to ‐2.50) | 515 | ⊕⊕⊝⊝ | TSA: ‐2.87 (3.66 to ‐2.07) |
| *The risk in the intervention (LEVR) group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to risk of bias: high risk of performance and detection bias in all the trials, unclear risk of selection bias in two trials, unclear risk of selective reporting in three trials and high risk in one trial, unclear risk of for‐profit bias in four trials | ||||||
| Author | |||||
| Hemobilia | NR | X | NR | X | NR |
| Acute respiratory failure with admission to intensive care unit | NR | X | NR | no | NR |
| Early incisional hernia | NR | X | NR | no | NR |
| Bile leak | NR | no | NR | X | NR |
| Cholangitis | NR | no | NR | X | NR |
| Bleeding from sphincterotomy | NR | no | NR | X | NR |
| Bleeding form drain site | NR | no | NR | X | NR |
| Collection/biloma | NR | no | NR | X | NR |
| Wound infection | NR | no | NR | X | NR |
| Urinary retention (UTI) | NR | no | NR | X | NR |
| Duodenal perforation | X | no | NR | no | X |
| NR: the authors did not report the type of post‐operative complications | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Overall morbidity (30 days postoperative) Show forest plot | 4 | 434 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.29, 1.20] |
| 2 Overall morbidity (30 days postoperative) Show forest plot | 4 | 434 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.32, 0.99] |
| 3 Failure of primary clearance Show forest plot | 5 | 517 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.22, 1.38] |
| 4 Failure of primary clearance Show forest plot | 5 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.37, 1.01] |
| 5 Clinical postoperative pancreatitis Show forest plot | 5 | 517 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.09, 1.14] |
| 6 Clinical postoperative pancreatitis Show forest plot | 5 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.11, 0.69] |
| 7 Operative time Show forest plot | 3 | 313 | Mean Difference (IV, Random, 95% CI) | 34.07 [11.41, 56.74] |
| 8 Operative time Show forest plot | 3 | 313 | Mean Difference (IV, Fixed, 95% CI) | 34.85 [29.34, 40.37] |
| 9 Length of hospital stay Show forest plot | 5 | 515 | Mean Difference (IV, Random, 95% CI) | ‐3.01 [‐3.51, ‐2.50] |
| 10 Length of hospital stay Show forest plot | 5 | 515 | Mean Difference (IV, Fixed, 95% CI) | ‐3.00 [‐3.37, ‐2.64] |

