نقش موسیقی در مدیریت بالینی بیخوابی در بزرگسالان
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع مطالعات در انتظار ارزیابی
منابع مطالعات در حال انجام
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial Design: 2‐arm parallel group design Blindness: single‐blinded, technician scoring PSG and researchers responsible for statistical analysis not aware of group allocation | |
| Participants | Adults who experienced insomnia for at least 1 month, documented by a PSQI score > 5 N: 50 Age: mean 32 (SD 11) years; range 22 to 58 years Sex: 3 males; 47 females Setting: sleep laboratory Country: Taiwan | |
| Interventions |
Music characteristics: Rural Spring Field, Woman under the Moon (Chinese music), Going Home (Czech music), Destiny, Heart Lotus (Taiwanese music), and Memory (composed by the authors). Tempos ranged from 60 to 85 bpm, minor tonalities, smooth melodies, and no dramatic changes in volume or rhythm. The music was expected to be familiar to participants Length of sessions: 45 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 consecutive days | |
| Outcomes |
We contacted the author 16 December 2014 to obtain data on the raw post‐scores, but we have not yet received a reply | |
| Notes | Trial start and end dates: the trial was conducted from May 2010 to June 2011 Funding sources: the trial was funded by the National Science Counsil, Taiwan | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned (...), using the drawing of lots" (Chang 2012; p 924) |
| Allocation concealment (selection bias) | Low risk | "All lots (labels) are packed in a jar that was prepared by another person. Researchers therefore did not know beforehand which group each participant would be assigned to" (Chang 2012; p 924) |
| Blinding of participants and personnel (performance bias) | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is unclear if this affected the objective sleep measures, but likely that it affected the subjective measures of sleep. Blinding of personnel at the sleep laboratory was not reported. Since the intervention was music, it is likely that they were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | The technician scoring the polysomnography and the researchers doing the statistical analyses were not aware to which group the data belonged |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts and no missing data |
| Selective reporting (reporting bias) | Unclear risk | We found no published protocol on this study. Sleep efficiency, based on a self‐report questionnaire, was not reported. All other measures of interest were included in the analysis |
| Other bias | High risk | Baseline differences in measures of depression and self‐reported number of awakenings, with the music group experiencing significantly more depression and arousals than the control group |
| Methods | Randomised controlled trial Design: 3‐arm parallel group design Blindness: single blinded, group allocation was coded for the person doing the statistics (Harmat 2014 [pers comm]) | |
| Participants | Students with poor sleep documented by PSQI scores > 5 N: 94 (64 included in this review) Age: mean 22.6 (SD 2.9) years; range 19 to 28 years Sex: 21 males; 73 females Setting: homes of the participants Country: Hungary | |
| Interventions |
Music characteristics: The Most Relaxing Classical (2 CD, Edited by Virgin 1999). Popular pieces from Baroque to Romantic Length of sessions: 45 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 weeks | |
| Outcomes |
| |
| Notes | Trial start and end dates: the trial was conducted in 2006 Funding sources: the work was supported by the Hungarian Ministry of Education, the National Research Fund (Hungary), the Ferenc Faludi Academy, and the János Bolyai Research Fellowship of the Hungarian Academy of Sciences | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using a computerised randomisation table and variable block randomisation |
| Allocation concealment (selection bias) | Unclear risk | No information on allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) | Low risk | The group allocation was coded (Harmat 2014 [pers comm]) |
| Incomplete outcome data (attrition bias) | Low risk | No attrition in the included groups (Harmat 2014 [pers comm]) |
| Selective reporting (reporting bias) | Low risk | We found no published protocol on this study. Outcomes from the no‐intervention control group were not reported in the publication, but were provided by the first author at request (Harmat 2014 [pers comm]). These data did not alter the results or conclusions of the trial |
| Other bias | High risk | The trial design involved a difference between the intervention and control group. The intervention group registered sleep quality once a week, whereas the control group only registered sleep quality before and after the intervention period. In addition, the intervention group, but not the control group, was contacted weekly by telephone to assess compliance with the protocol |
| Methods | Quasi‐randomised controlled trial Design: 2‐arm parallel group design Blindness: not blinded | |
| Participants | Traumatised refugees with sleep problems documented by PSQI score > 5 N: 15 (19 included; 4 dropped out) Age: mean 37 years; range 26 to 57 Sex: 6 males; 9 females Setting: homes of the participants Country: Denmark | |
| Interventions |
Music characteristics: MusiCure compilation 'Inducing Sleep' (Tracks 1, 2, and 5; Eje 2004). Tempo 52 bpm, stable dynamic contour and repetitive structure Instruments: piano, harp, guitar, oboe, cello, and nature sounds (waves and birdsong) Length of sessions: 60 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 weeks | |
| Outcomes |
| |
| Notes | Trial start and end dates: the trial was conducted in 2010 Funding sources: the work was supported by Trygfonden and the Danish Ministry for Refugee, Immigration and Integration Affairs | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Used an alternation procedure based on gender |
| Allocation concealment (selection bias) | High risk | Allocation could be foreseen due to the alternation procedure |
| Blinding of participants and personnel (performance bias) | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) | High risk | 4 participants dropped out. Data from dropouts were excluded in the final analyses. No missing data |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported and included in the analysis |
| Other bias | High risk | Baseline difference in sleep quality with the music group experiencing more sleep problems than the control group |
| Methods | Randomised using a computer‐based randomisation list (Kullich 2014b [pers comm]) Design: 2‐arm parallel group design Blindness: single blinded. Data assessment performed by non‐trial personnel (Kullich 2014b [pers comm]) | |
| Participants | Adults with low back pain and sleep difficulties (PSQI scores > 5) N: 65 Age: mean age reported by group. Music group mean age 47.0 (SD 9.7); control group mean age 49.7 (SD 7.9); range 21 to 68 Sex: 41 males; 24 females Setting: rehabilitation facility Country: Austria | |
| Interventions |
Music characteristics: CD 'Entspannung bei Schmerzen' (Mentalis Verlag, ISBN: 3‐932239‐95‐4). No further information provided Length of sessions: 25 minutes Frequency of sessions: once a day, no time specified Duration of intervention period: 3 weeks +/‐ 2 days | |
| Outcomes |
| |
| Notes | Trial start and end dates: there is no information on when the trial was conducted Funding sources: the trial was supported by the Ludwig Boltzmann Institut (Saalfelden), the Herbert von Karajan Centrum (Wien), Salzburg University, and the Mozart University (Salzburg) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based randomisation list (Kullich 2014b [pers comm]) |
| Allocation concealment (selection bias) | Low risk | Allocation done by another person (not the doctor) who referred the participant to the trial (Kullich 2014b [pers comm]) |
| Blinding of participants and personnel (performance bias) | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective measures of sleep. There was no information on the blinding of the personnel at the rehabilitation facility |
| Blinding of outcome assessment (detection bias) | Low risk | Data were assessed by non‐trial personnel (secretary). Data analysis was performed by a researcher who was aware of group allocation, but did not know the patients (Kullich 2014b [pers comm]) |
| Incomplete outcome data (attrition bias) | Low risk | No attrition or missing data (Kullich 2014b [pers comm]) |
| Selective reporting (reporting bias) | Low risk | We found no published protocol on this study, but there was no indication of selective reporting. Measures on sleep quality were reported without SDs in the publication, but these were provided by the first author on request (Kullich 2014a [pers comm]). These data did not alter the conclusions of the trial |
| Other bias | Low risk | No other risk of bias detected |
| Methods | Randomised controlled trial Design: 2‐arm parallel group design Blindness: not blinded | |
| Participants | Older adults with sleep problems documented by PSQI scores > 5 N: 60 Age: mean 67 (SD 5) years; range 60 to 83 Sex: not reported Setting: homes of the participants Country: Taiwan | |
| Interventions |
Music characteristics: the choices of music included 5 types of Western music (new age, eclectic, popular oldies, classical, and slow jazz), and 1 type of Chinese music (folk music). Tempos ranged from 60 to 80 bpm without accented beats, percussive characteristics or syncopation. The music was expected to be familiar to the participants Length of sessions: 45 minutes Frequency of sessions: daily at bedtime Duration of intervention period: 3 weeks | |
| Outcomes |
| |
| Notes | Trial start and end date: the trial was conducted in 2000 Funding sources: no information provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permuted block randomisation with sealed envelopes stratified on gender |
| Allocation concealment (selection bias) | Low risk | "The envelopes were prepared by a different person so that the investigator (first author) was blind to block size and order of assignment" (Lai 2005; p 235) |
| Blinding of participants and personnel (performance bias) | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear information on attrition. One man was withdrawn due to hospitalisation. No information on completeness of data |
| Selective reporting (reporting bias) | Low risk | We found no published protocol on this study, but there was no indication of selective reporting |
| Other bias | High risk | Baseline differences in 2 sleep component scores with the music group experiencing shorter sleep duration and more daytime dysfunction |
| Methods | Randomised controlled trial Design: 2‐arm parallel group design Blindness: not blinded | |
| Participants | Older adults with poor sleep quality, documented by PSQI scores > 5 N: 60 Age: mean 64 years; range 57 to 68 years Sex: 20 males; 40 females Setting: homes of the participants Country: Singapore | |
| Interventions |
Music characteristics: the 4 types of researcher selected music included 1) Western classical (Bach: Allemande, Sarabande; Mozart: Romance from Eine kleine Nachtmusik; Chopin: Nocturne); 2), Chinese classical (Spring River in the Moonlight; Variation on Yang Pass); 3) New Age (Shizuki, Lord of the Wind); and 4) Jazz (Everlasting; Winter Wonderland; In Love in Vain). All compositions were soft, with no lyrics, and tempos ranging from 60 to 80 bpm Length of sessions: 40 minutes Frequency of sessions: once a day, no time specified Duration of intervention period: 5 weeks | |
| Outcomes |
| |
| Notes | Trial start and end dates: the trial was conducted from January 2012 to January 2013 Funding sources: no information provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Two cards were put inside a bag in each draw, with one labelled as "intervention" and the other as "control". Each participant was asked to draw one card from the bag to allocate him or her into either the intervention or control group" (Shum 2014; p 51) |
| Allocation concealment (selection bias) | Low risk | The above mentioned procedure makes it unlikely that the allocation was foreseen |
| Blinding of participants and personnel (performance bias) | High risk | Due to the nature of the intervention, blinding of participants was not possible. It is likely that this affected the subjective outcome measures. The intervention was used at home with no personnel involved |
| Blinding of outcome assessment (detection bias) | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts and no missing data |
| Selective reporting (reporting bias) | Unclear risk | We found no published protocol on this study. The primary outcome of sleep quality (PSQI ‐ global scale) was fully reported, but the results of the component scores were not reported, which is common in other trials using the PSQI |
| Other bias | Low risk | No other risk of bias detected |
BDI: Beck Depression Inventory.
BPM: beats per minute.
CD: compact disc.
GEE: generalised estimating equation.
PSG: polysomnograpgh.
PSQI: Pittsburgh Sleep Quality Index.
REM: rapid eye movement.
SD: standard deviation.
TAU: treatment‐as‐usual.
TST: total sleep time.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not RCT or qRCT (no control group) | |
| Intervention not music listening (active music making (choir)) | |
| Comparison of 2 interventions (music listening versus muscle relaxation techniques) | |
| Not RCT or qRCT (within‐subject design) | |
| Not a clinical trial (reflections on practice) | |
| Not a clinical trial (experimental trial investigating the impact of music on wakefulness) | |
| Not RCT or qRCT (no control group) | |
| Not RCT or qRCT (no control group) | |
| Participants not adults with insomnia (not all participants had insomnia. No inclusion criteria of insomnia and PSQI < 5) | |
| Participants not adults with insomnia (young adults with different sleep latencies. Poor sleepers (PSQI < 5) excluded) | |
| Not RCT or qRCT (no randomisation) | |
| Intervention not music listening (intervention a combination of music, massage, and aromatherapy) | |
| Comparison of 2 interventions (music listening versus hypnotic medications) | |
| Participants not adults with insomnia (infants) | |
| Not RCT or qRCT (no randomisation) | |
| Participants not adults with insomnia (children) | |
| Intervention not music listening (comprehensive sleep management including music) | |
| Participants not adults with insomnia (infants) | |
| Not RCT or qRCT (no randomisation). Participants not adults with insomnia (healthy volunteers) | |
| Participants not adults with insomnia (ICU patients with no documentation of insomnia) | |
| Participants not adults with insomnia (some participants were 'good sleepers') | |
| Not RCT or qRCT (no randomisation). Participants not adults with insomnia (healthy university students who normally listened to music at bedtime) | |
| Not RCT or qRCT (no control group) | |
| Comparison of 2 interventions (individualized versus non‐individualized 'brain music') | |
| Participants not adults with insomnia (healthy university students with no sleep problems) | |
| Comparison of 2 interventions (live music with nursing presence versus pre‐recorded music) | |
| Intervention not music listening (music videos) | |
| Participants not adults with insomnia (healthy university students) | |
| Not RCT or qRCT (no randomisation). Comparison of 2 interventions (individualized versus non‐individualized 'brain music') | |
| Not RCT or qRCT (within‐subject design comparing healthy adults of old age to older adults with senile dementia of the Alzheimer type) | |
| Intervention not music listening (vibroacustic intervention) | |
| Participants not adults with insomnia (children) | |
| Participants not adults with insomnia (infants) | |
| Not RCT or qRCT (no control group) | |
| Participants not adults with insomnia (pre‐operative patients with no documentation of insomnia) | |
| No sleep outcome measure | |
| Not RCT or qRCT (no control group) | |
| Not RCT or qRCT (no control group) | |
| Participants not adults with insomnia (university students. Around half the participants experienced no sleep problems) | |
| Not RCT or qRCT (no control group) | |
| No sleep outcome measure (sleep only registered in intervention group, not control group) | |
| Participants not adults with insomnia (post‐operative patients with no documentation of insomnia) | |
| Not RCT or qRCT (no control group). Intervention not music listening (combination of interventions, including back rubs, warm drinks, aroma therapy, and relaxation music) | |
| Participants not adults with insomnia (patients at cardiac care unit with no documentation of insomnia) | |
| Participants not adults with insomnia (some participants were 'good sleepers' with PSQI scores < 5) | |
| Comparison of 2 interventions (music listening versus tactile touch) | |
| Not a clinical trial (experimental trial testing the Attentional Behavioral Cognitive (ABC) relaxation theory) | |
| Not RCT or qRCT (no control group) | |
| Participants not adults with insomnia (patients at intensive care unit with unclear documentation of insomnia) | |
| Not RCT or qRCT (no control group) | |
| Participants not adults with insomnia (children) | |
| Intervention not music listening (feedback of neural EEG‐activity using single tones derived through mathematical algorithms) | |
| Not RCT or qRCT (no control group). Intervention not music listening (active music therapy) | |
| Participants not adults with insomnia (pre‐operative patients with no documentation of insomnia) | |
| Comparison of 2 interventions (music listening versus progressive muscular relaxation) |
EEG: electroencephalography.
PSQI: Pittsburgh Sleep Quality Index.
qRCT: quasi‐randomised controlled trial.
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomised controlled trial |
| Participants | Post‐operative patients |
| Interventions |
|
| Outcomes | Sleep quality (PSQI) Well‐being Consumption of analgesics, hypnotics, and sedatives |
| Notes | This is an unpublished trial. On 9 September 2014, we requested further information from the author, but have yet to receive a response |
PSQI: Pittsburgh Sleep Quality Index.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Music for insomnia |
| Methods | Randomised controlled trial |
| Participants | Adults with insomnia |
| Interventions |
|
| Outcomes | Subjective sleep quality (PSQI) and objective sleep measures (PSG + actigraphy) |
| Starting date | February 2015 |
| Contact information | |
| Notes |
| Trial name or title | Music intervention in the treatment of sleep disorders for depressed patients |
| Methods | Randomised controlled trial |
| Participants | Inpatients with depression and insomnia |
| Interventions |
|
| Outcomes | Subjective sleep quality and objective sleep quality (actigraphy) |
| Starting date | April 2014 |
| Contact information | k.cattapan@sanatorium‐kilchberg.ch |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment Show forest plot | 5 | 264 | Mean Difference (IV, Random, 95% CI) | ‐2.80 [‐3.42, ‐2.17] |
| Analysis 1.1 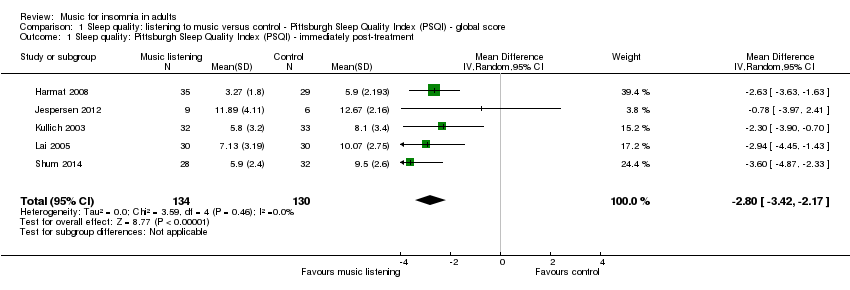 Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment. | ||||
| 2 Subgroup (PSQI) by music selection ‐ immediatly post‐treatment Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 2 Subgroup (PSQI) by music selection ‐ immediatly post‐treatment. | ||||
| 2.1 Researcher‐selected music | 3 | 144 | Mean Difference (IV, Random, 95% CI) | ‐2.42 [‐3.24, ‐1.60] |
| 2.2 Participant‐selected music (choice among researcher pre‐selected music) | 2 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.35 [‐4.28, ‐2.42] |
| 3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment. | ||||
| 3.1 Music listening alone | 3 | 149 | Mean Difference (IV, Random, 95% CI) | ‐2.85 [‐3.92, ‐1.78] |
| 3.2 Music listening and relaxation instructions | 2 | 125 | Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐3.74, ‐1.54] |
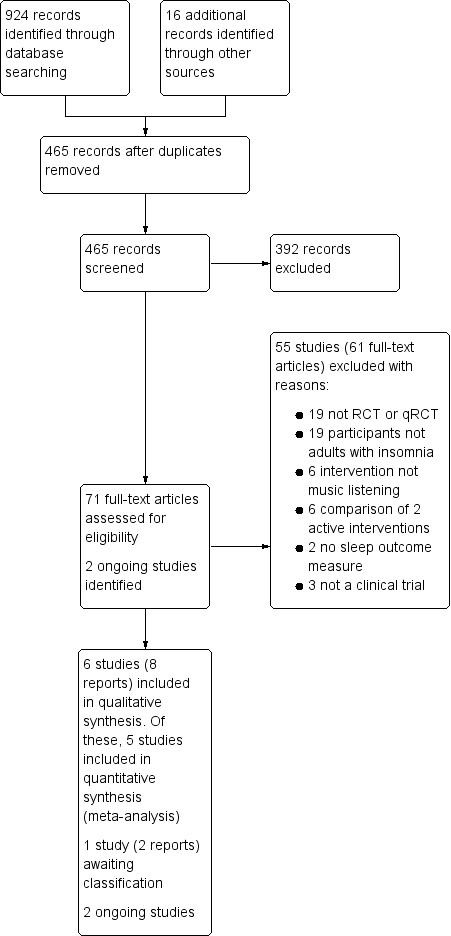
Study flow diagram
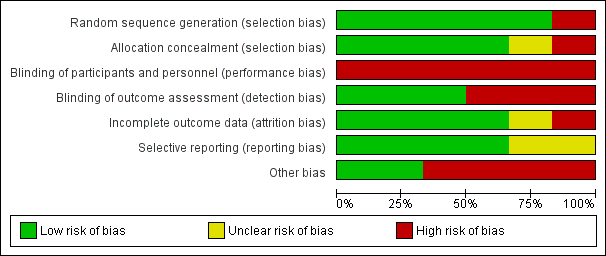
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included trials
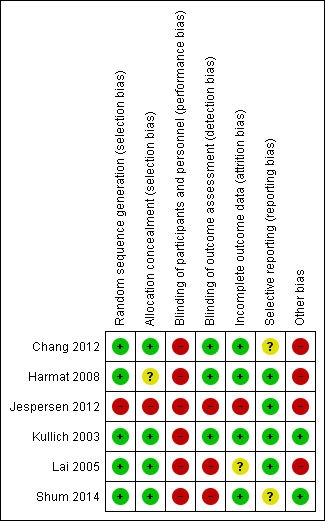
Risk of bias summary: review authors' judgements about each risk of bias item for each included trial

Forest plot of comparison: 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, outcome: 1.1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment.

Forest plot of comparison: 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, outcome: 1.2 Subgroup (PSQI) by music selection ‐ immediately post‐treatment.

Forest plot of comparison: 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, outcome: 1.3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment.
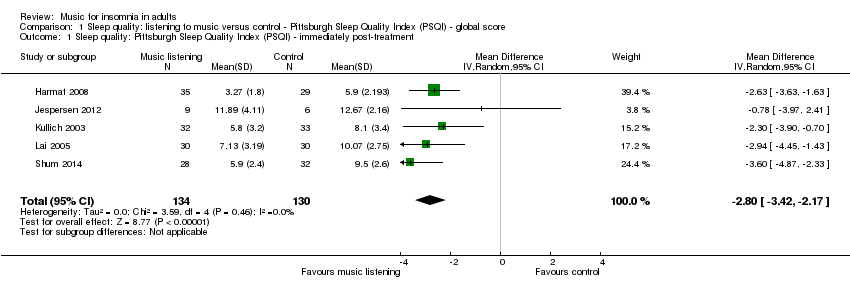
Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment.

Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 2 Subgroup (PSQI) by music selection ‐ immediatly post‐treatment.

Comparison 1 Sleep quality: listening to music versus control ‐ Pittsburgh Sleep Quality Index (PSQI) ‐ global score, Outcome 3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment.
| Listening to music compared to no treatment or treatment‐as‐usual (TAU) for adults with insomnia | ||||||
| Patient or population: adults with insomnia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment or TAU | Listening to music | |||||
| Sleep quality ‐ immediately post‐treatment Follow‐up: 21 to 35 days | The mean score in the intervention groups was | 264 | ⊕⊕⊕⊝ | A lower score indicates better sleep quality (i.e. fewer sleep problems). The change is about the size of one standard deviation which is considered a clinically relevant change. The studies included participants with a complaint of poor sleep (PSQI > 5)¹. | ||
| Sleep onset latency ‐ immediately post‐treatment Follow‐up: 3 days | See comment | See comment | 50 | ⊕⊕⊝⊝ | The one trial reporting this outcome found no evidence of an effect of the intervention. The data were not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. | |
| Total sleep time ‐ immediately post‐treatment | See comment | See comment | 50 | ⊕⊕⊝⊝ | The one study reporting this outcome found no evidence of an effect of the intervention. The data were not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. | |
| Sleep interruption ‐ immediately post‐treatment | See comment | See comment | 50 | ⊕⊕⊝⊝ | The one study reporting this outcome found no evidence of an effect of the intervention. The data are not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. | |
| Sleep efficiency ‐ immediately post‐treatment | See comment | See comment | 50 | ⊕⊕⊝⊝ | The one study reporting this outcome found no evidence of an effect of the intervention. The data were not available for analysis. The study included participants that had reported poor sleep for at least one month (PSQI > 5)¹. | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Pittsburgh Sleep Quality Index. 0 indicates good sleep quality and 21 indicates severe sleep problems. Clinical cut off > 5 (Buysse 1989). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sleep quality: Pittsburgh Sleep Quality Index (PSQI) ‐ immediately post‐treatment Show forest plot | 5 | 264 | Mean Difference (IV, Random, 95% CI) | ‐2.80 [‐3.42, ‐2.17] |
| 2 Subgroup (PSQI) by music selection ‐ immediatly post‐treatment Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Researcher‐selected music | 3 | 144 | Mean Difference (IV, Random, 95% CI) | ‐2.42 [‐3.24, ‐1.60] |
| 2.2 Participant‐selected music (choice among researcher pre‐selected music) | 2 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.35 [‐4.28, ‐2.42] |
| 3 Subgroup (PSQI) by relaxation instructions ‐ immediately post‐treatment Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Music listening alone | 3 | 149 | Mean Difference (IV, Random, 95% CI) | ‐2.85 [‐3.92, ‐1.78] |
| 3.2 Music listening and relaxation instructions | 2 | 125 | Mean Difference (IV, Random, 95% CI) | ‐2.64 [‐3.74, ‐1.54] |

