مداخلات میکرو‐تهاجمی برای مدیریت پوسیدگی پروگزیمال دندانی در دندانهای شیری و دائمی
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع مطالعات در حال انجام
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Split‐mouth randomised controlled trial Funded partially by manufacturer of sealant patch (Ivoclar, Schaan, Liechtenstein) Clinical follow‐up after 6 and 12 months and radiographic evaluation after 2 and 3 years Drop‐out 30% and 40% after 2 and 3 years, respectively Setting: not specified | |
| Participants | 50 participants, mean age 21 years (SD 6) with high caries risk (baseline mean DMFT 8.67) Inclusion criteria: two proximal carious lesions, confirmed with radiograph, extending into enamel or outer dentine in teeth with vital pulps Exclusion criteria: general disease, allergies, pregnancy, presence of cavitation on tested or control proximal surfaces | |
| Interventions | Two treatment arms: Group 1: bonding (Heliobond, Ivoclar) + adhesive polyurethane patch (Ivoclar) + occlusal sealing (and oral health instructions including flossing and use of fluoridated toothpaste) Group 2: oral health instructions including flossing and use of fluoridated toothpaste In group 1, an orthodontic separating rubber ring was placed between teeth in first visit, and after 3‐5 days teeth were cleaned using paste and floss, then sealed (isolation of adjacent tooth by metal matrix band, etching using 37% phosphoric acid for 60 s, application of bonding and patch, light‐curing for 20 s from buccal and oral aspects, respectively, occlusal sealing, recontouring and finishing of proximal seal with finishing discs and strips) | |
| Outcomes | Radiographic lesion progression as assessed by two blinded dentists according to scoring system (0 = no visible radiolucency; 1 = radiolucency in the enamel; 2 = radiolucency in the outer half of the dentine; 3 = radiolucency in the inner half of the dentine; 4 = restoration) Retention and adaptation of patch according to modified Ryge criteria assessed by dentists different from operators Authors stated that no adverse effect on general or dental health could be recorded. None of the other secondary outcomes were measured. | |
| Notes | Intraexaminer reproducibility of radiographic assessments of the two examiners was 92% and 82%, and the agreements of each examiner with the gold standard were 92% and 80%. Interexaminer concordance was 90%. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "by toss of coin" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided; no indication for blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The examiners were different from the dentist who applied the sealants. Two dentists blindly and randomly assessed the radiographs separately and then compared their readings." Comment: low risk of bias assumed, as radiographic assessment was blind |
| Incomplete outcome data (attrition bias) | Unclear risk | Missing data rate 40% (> 25%) after 3 years; however, split‐mouth design reduces attrition bias |
| Selective reporting (reporting bias) | Low risk | Outcomes reported matched pre‐specified assessed outcomes. |
| Other bias | Low risk | No indication for other bias |
| Methods | Split‐mouth randomised controlled trial Partially funded by manufacturer of resin infiltration kit (DMG, Hamburg, Germany) Clinical and radiographic follow‐up for one year Drop‐out 14%, further 6% had no radiographic follow‐up Setting: public dental health service in Greenland | |
| Participants | 48 children (52% male, 48% female), mean age 7 years (range 5‐8) with high caries risk (mean dmft was 8.1) Inclusion criteria: children who had radiographs taken in January 2008 showing presence of at least 2 proximal lesions in enamel or outer dentine on deciduous molars. Lesions on the mesial surface on primary first molars were not included as the contact area to the canines was found too narrow. Exclusion criteria: presence of caries‐related diseases. | |
| Interventions | Two treatment arms: Group 1: resin infiltration using Icon pre‐product (DMG) + application of 2.26% sodium fluoride varnish Group 2: 2.26% sodium fluoride varnish For group 1, proximal surfaces were cleaned by floss; rubber dam applied; the adjacent tooth protected by a plastic or metal strip; 15% HCl acid placed on the lesion for 120 s; the surface rinsed, dried and dehydrated twice by treating with 95% ethanol and air‐drying; the infiltrant resin applied to the lesion for 120 s, polymerised according to the manufacturer’s instructions; resin applied again for 30 s and polymerised, and eventually fluoride varnish applied to the lesion. Group 2 received fluoride varnish only. Varnish application was repeated in both groups after 1 year. | |
| Outcomes | Clinical lesion progression according to ICDAS Radiographic progression according to scoring (1 = radiolucency in the outer half of the enamel; 2 = radiolucency in the inner half of the enamel, 3 = radiolucency in the outer half of the dentine; 4 = radiolucency in the inner half of the dentine; 5 = restoration). Authors stated that no side effects of the infiltration or the Duraphat treatments were observed, either from the participants’ files or from direct questioning of the children and the parents. None of the other secondary outcomes were reported. | |
| Notes | If more than two lesions were present, lesions were selected using a random number table. ICDAS scoring had reliability of 94%. Clinical calibration was done on 6 children with 48 primary molar teeth. In 4.1% of the recordings the 2 examiners disagreed about the score. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random number tables used" |
| Allocation concealment (selection bias) | Low risk | Quote: "prepared lists for allocation" |
| Blinding of participants and personnel (performance bias) | High risk | No information provided; no indication for blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "For all readings the examiner was blinded as to whether the examined radiograph was baseline or final and as to whether the lesion was a test or a control lesion." Comment: low risk of detection bias for radiographic assessment |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "[m]issing data rate 19% after 1.5 years" Comment: missing data rate < 25% |
| Selective reporting (reporting bias) | High risk | 6‐month clinical evaluation was not reported, and radiographic evaluation was incomplete as well |
| Other bias | High risk | Unbalanced allocation of lesions according to ICDAS scores |
| Methods | Clustered split‐mouth randomised controlled trial Part of a bigger study involving a total of 50 participants Radiographic follow‐up after 2 years Drop‐out 0% after 2 years Setting: navy dental clinic in Chile | |
| Participants | 7 participants (72% male, 28% female), mean age 15 years (range 10‐20), with unclear caries risk; 71 lesions randomly allocated to intervention or control. Inclusion criteria: radiographic detection of one or more surface with incipient proximal carious lesions on molars and premolars Unclear who performed initial examination | |
| Interventions | Two treatment arms: Group 1: resin sealant (Concise, 3M Espe, Neuss, Germany) Group 2: application of fluoride varnish twice yearly In group 1, access was first gained to confirm the presence of enamel lesions and their clinical status by temporary tooth separation. After 1–2 days, the surface was cleaned, dried and a cotton roll or rubber dam applied. The carious tooth area and the 1 mm enamel surrounding the lesion were etched for 20 s with a 35% phosphoric acid gel, washed and dried, whilst the adjacent surface was protected with a nylon adhesive strip. When the proximal surface was completely dried, a light‐cured, low‐viscosity pit and fissure was applied using a brush. After 30 s, the sealant was light cured. During sealing, dental floss was placed in the interdental sulcus space to avoid sealant flow to the cervical zone. After sealing, excess sealant was removed with an explorer, and the margins polished with a fine polishing strip. | |
| Outcomes | Radiographic progression according to scoring (0 = no visible radiolucency; 1 = radiolucency in the enamel; 2 = radiolucency in the outer half of the dentine; 3 = radiolucency in the inner half of the dentine; and 4 = restoration). Authors did not state if they measured adverse events and none were reported. | |
| Notes | Intraexaminer reliability showed a kappa of 0.86 when the calculations included carious surfaces (scores 1–4). For surfaces with score 1, kappa was 0.84. Clustering of lesions and unequal distribution; unclear lesion depths | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random numbers were used to decide which surfaces should be treated with sealant or fluoride varnish." |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No blinding reported |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Radiographs were analysed blindly in a random order by one observer." |
| Incomplete outcome data (attrition bias) | Low risk | Missing data rate 0% after 2 years (< 25%) |
| Selective reporting (reporting bias) | Low risk | No indication for selective reporting |
| Other bias | High risk | Unclear how lesion depths distributed in groups; severe clustering of lesions |
| Methods | Split‐mouth randomised controlled trial Partially funded by Colfuturo and the Universidad El Bosque Radiographic follow‐up after 18 months Drop‐out 12% after 18 months Setting: dental schools in Denmark and Colombia | |
| Participants | 82 participants (age range 15‐39 years) attending dental faculties in Copenhagen (N = 43) or Bogota (N = 39) with mostly moderate (62% in Denmark and 61% in Colombia) or high (28% in Denmark and 33% in Colombia) caries risk Inclusion criteria: individuals with at least two initial proximal lesions in enamel up to outer third of dentine on the bitewing radiographs and corresponding bleeding after gentle probing in the gingiva next to the lesion | |
| Interventions | Two treatment arms: Group 1: resin sealant (Gluma One Bond, Heraeus Kulzer, Hanau, Germany, or Concise, 3M Espe) + flossing advice Group 2: flossing advice If necessary, a proximal temporary space was created by means of an elastic orthodontic band placed in the proximal space concerning the selected test lesion for 2 days. At the second appointment, the surface was cleaned, cotton rolls used for partial isolation, a matrix band placed around the lesion tooth or the neighbouring tooth surfaces were covered with a Teflon tape, a wooden edge was placed in the interdental space, the sealing material was applied with the aid of applicator tips and dental floss, the sealants light cured, and the surface polished. | |
| Outcomes | Radiographic progression as assessed by scoring (1 = enamel, 2 = around enamel‐dentine junction, 3 = outer third dentine, 4 = inner third, 5 = not assessable, 6 = restored) by a blinded independent examiner Radiographic progression as assessed by pairwise radiographic reading: A blinded independent examiner was asked to determine the progression status of the right positioned against the left positioned radiograph, with a further randomisation concerning the position of baseline or follow‐up images. Radiographic progression as assessed via digital subtraction radiography using Compare software (Dental Health Unit, University of Manchester, United Kingdom) by an external trained examiner 10 days after the visual assessment of conventional radiographs None of the secondary outcomes were reported. Authors did not state if they measured adverse events and none were reported. | |
| Notes | The contact area was wide in most test (75%) and control (88%) lesions. Test and control lesions differed with respect to tooth types (more test lesions on premolars), depth of the lesions (more test lesions were scored 3), location in the jaw (more control lesions were located in the lower jaw) and proximal surface area (more control lesions were on surfaces with a wide contact area to the neighbouring tooth). Intraexaminer reproducibility for the visual independent readings were kappa of 0.84 and 96% agreement; for the paired readings, kappa was 0.44 and the agreement 68%; and for the subtraction readings kappa was 0.87 and agreement 92%. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A random number table was used." |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No indication for blinding of operator or participants |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "assessed by an external examiner who was blinded" |
| Incomplete outcome data (attrition bias) | Low risk | Missing data rate 12% (< 25%) |
| Selective reporting (reporting bias) | Low risk | No indication for reporting bias |
| Other bias | Low risk | No indication for other bias |
| Methods | Split‐mouth randomised controlled trial No funding information Radiographic follow‐up after 2.5 years Drop‐out 20% and 39% after 1.5 and 2.5 years, respectively Setting: university dental clinic in Colombia | |
| Participants | 91 preschoolers (51% male, 49% female), mean age 5 years (range 4‐6), with low (23%), moderate (25%) or high (52%) caries risk (mean dmft 1.8) and low socioeconomic status from Bogota, Colombia Inclusion criteria: children aged 4‐6 years with radiographically determined proximal caries on at least 2 distal surfaces on primary first molar teeth with lesion depths involving the enamel up to the outer third of the dentine and gingival bleeding Exclusion criteria: systemic disease, cavitated lesions/restorations involving the mesial surfaces of second primary molar teeth, refusal of radiographs Examiners: dental students | |
| Interventions | Two treatment arms: Group 1: resin sealant (Single One Bond, 3M Espe) + flossing advice. Group 2: flossing advice In group 1, a proximal temporary elective space was created by means of an elastic orthodontic band placed for 2 days between the first and second primary molar, involving the selected test and control lesions. Surfaces were cleaned, cotton rolls used for partial isolation, the neighbouring tooth surfaces covered with a Teflon tape, and a wooden edge placed in the interdental cervical surface. Adhesive was applied following the manufacturer’s instructions, with the aid of ultrafine applicator tips and dental floss, followed by light‐curing and polishing. | |
| Outcomes | Radiographic lesion progression according to scoring (0 = no radiolucency, 1 = radiolucency restricted to the outer half of the enamel, 2 = radiolucency involving the inner half of the enamel to the enamel dentine junction, 3 = radiolucency in the outer third of the dentine, and 4 = radiolucency in the inner two thirds of the dentine). Assessment by one blinded independent examiner None of the secondary outcomes were reported. Authors did not state if they measured adverse events, and none were reported. | |
| Notes | There was no difference in distribution pattern related to lesion depth between test and control lesion. The main author selected two lesions; if more than two were available, a random number table was used for selection. Intraexaminer reproducibility for the radiographic scoring: kappa 0.76. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random allocation sequence generated with a random number table" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided, presumably no blinding performed |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Lesions were scored on the radiographs independently by an external examiner who was not familiar with the study design." Comment: low risk of detection bias |
| Incomplete outcome data (attrition bias) | Unclear risk | Missing data rate 39% after 2.5 years (> 25%); however, split‐mouth design reduces attrition bias |
| Selective reporting (reporting bias) | Low risk | No indication for reporting bias |
| Other bias | Low risk | No indication for other bias |
| Methods | Multi‐arm split‐mouth randomised controlled trial Partially funded by DMG Radiographic follow‐up after 1, 2, and 3 years Drop‐out 5% after 1 and 3 years Setting: dental school in Colombia | |
| Participants | 39 participants (72% female, 28% male), mean age 21 years (range 16‐31), with moderate to high caries risk (mean DMFT 4.9) attending the Universidad El Bosque, Colombia Inclusion criteria: presence of three posterior proximal lesions (radiolucency in outer dentine or enamel dentine junction) as detected radiographically Exclusion criteria: leaving the city in the next three years; current orthodontic treatment | |
| Interventions | Three treatment arms: Group 1: resin infiltration (Icon pre‐product, DMG) + flossing advice Group 2: resin sealant (Prime Bond NT, Dentsply, Konstanz, Germany) + flossing advice Group 3: placebo proximal sealing + flossing advice For group 1, teeth were initially separated using orthodontic elastic bands. At the second visit, rubber dam and plastic wedges were placed, a plastic strip used to isolate the adjacent tooth, the surface etched with 15% hydrochloric acid for 120 s, rinsed and dried, desiccated using 95% ethanol and air‐drying, resin infiltrated for 120 s, light cured, infiltrant re‐applied for 30 sec, and light cured once more. For group 2, pretreatment was similar, with sealing of the lesion performed using an adhesive. For group 3 (placebo), a micro‐brush was passed through the spaces between teeth for 30 sec, with the procedure repeated after 2 min. All individuals received routine instructions on flossing. | |
| Outcomes | Pairwise subjective comparison by coding the lesions on the most recent film and reading this code against baseline (0 = no radiolucency, 1 = radiolucency restricted to the outer half of the enamel, 2 = radiolucency involving the inner half of the enamel to the enamel‐dentine junction, 3 = radiolucency in the outer third of the dentine, and 4 = radiolucency in the inner two thirds of the dentine) Digital subtraction radiography was performed using Image Tool (UTHSCSA, San Antonio, TX, USA). Authors stated that no adverse events (pain, vitality loss, staining) occurred. None of the other secondary outcomes were reported. | |
| Notes | If a participant had more than 3 eligible lesions, investigators randomly selected 3. The intra‐rater reliability for the pairwise and the subtraction radiographic methods (kappa values) was 0.74 and 0.78, respectively. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly permuted blocks" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Placebo involved moving a microbrush between the teeth; and operator was blind to the radiographic score of lesions." Comment: no blinding of operators; unclear if blinding sufficient to conceal allocation from participants |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Blinded to the selected treatment groups. Radiographic assessment independently by an external examiner" |
| Incomplete outcome data (attrition bias) | Low risk | Missing data rate 5% after 3 years (< 25%) |
| Selective reporting (reporting bias) | High risk | DSR evaluation only after one year |
| Other bias | Low risk | No indication for other bias |
| Methods | Clustered split‐mouth randomised controlled trial Partially funded by DMG Radiographic follow‐up after 18 months with additional follow‐up planned after 36 and 60 months Drop‐out 0% and 9% after 18 and 36 months, respectively Setting: university dental clinic in Germany | |
| Participants | 22 participants (64% female, 36% male), mean age 25 years (range 18‐35), with low (32%), moderate (36%), and high (32%) caries risk; total of 29 lesion pairs, attending the Berlin University dental clinic Inclusion criteria: presence of 2 or more non‐cavitated proximal caries lesions with radiolucencies involving the inner half of enamel up to the outer third of dentine, aged 18‐35 yrs Exclusion criteria: pregnant, participating in another study, incapable of contracting, institutionalised Radiographs taken using standardised conventional bitewing radiographs with individualised holder. One investigator scored lesions using a light box. | |
| Interventions | Two treatment arms: Group 1: resin infiltration (Icon pre‐product, DMG) + fluoride varnish application + oral hygiene and dietary advice Group 2: fluoride varnish application + oral hygiene and dietary advice For group 1, rubber dam was applied, teeth were separated by plastic wedges, polyurethane foil placed in the contact area with a plastic holder to protect the adjacent tooth, 15% HCl etching gel applied by syringe in the area below the contact point for 120 s, the gel washed off with air‐water‐spray for 30 s, the lesion desiccated by air‐blowing for 10 s, ethanol applied for 10 s, the lesion desiccated using air‐blowing again for 10 s. Eventually, an infiltrant was applied and after 5 min of penetration time, excess material removed by air‐blowing and flossing. The resin was light cured for 1 min from the buccal, occlusal, and oral aspects. The infiltration step was repeated with a penetration time of 1 min. For group 2, operators performed a sham‐infiltration, with water instead of HCl gel and infiltrant. The operators, however, were aware of this. | |
| Outcomes | Radiographic progression as assessed by scoring (E1 = up to outer half of enamel, E2 = up to inner half of enamel, D1 = up to outer third of dentine, D2 = up to middle third of dentine, D3 = up to inner third of dentine) of lesions at baseline and follow‐up examination Radiographic progression as assessed by pairwise assessment of lesions for progression, regression, or stability Radiographic progression as assessed by DSR Subjective and clinical adverse events, such as loss of vitality, staining, or gingival alterations were measured and none were reported. None of the other secondary outcomes were reported. | |
| Notes | Inter‐rater reliability (kappa) was moderate (0.59) for radiographic staging, substantial (0.67) for pairwise comparison, and almost perfect (0.81) for DSR. Intra‐rater reliability ranged from moderate to almost perfect (0.51‐0.89). Potential industry and profession bias (the trialists are appointed as inventors and patent‐holders of the technique) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "From each pair, 1 lesion was allocated to the test and 1 to the control group, respectively, by computer‐generated randomly permuted blocks." |
| Allocation concealment (selection bias) | Low risk | Quote: "in sealed envelopes" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Quote: "Patients were blinded to lesion allocation throughout the whole study period as a placebo treatment was performed on the control lesions." Comment: Operators were not necessarily blinded, but it is unclear how this might affect outcomes. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Examiner was blinded with regard to treatment group allocation of teeth." |
| Incomplete outcome data (attrition bias) | Low risk | Missing data rate 9% (< 25%) after 3 years |
| Selective reporting (reporting bias) | Low risk | No indication for reporting bias |
| Other bias | Low risk | No indication for other bias |
| Methods | Cluster split‐mouth randomised controlled trial Drop‐out 0% after 12 months Radiographic follow‐up after 6 and 12 months Funding by the Postgraduate Research Fund, Faculty of Dentistry, Chulalongkorn University (Thailand) Setting: university paediatric dentistry clinic in Thailand | |
| Participants | 26 participants, mean age 13 years (range 7‐19). Inclusion criteria: at least one contralateral pair of permanent posterior teeth with proximal caries lesions shown by radiograph to extend into the outer half or inner half of enamel, and plaque stagnation, as detected by explorer. Exclusion criterion: no contact between teeth | |
| Interventions | Two treatment arms: Group 1: glass ionomer sealant + fluoridation gel + toothpaste advice Group 2: fluoridation gel + toothpaste advice The test teeth were separated using an orthodontic ring. After two days, the lesion was air dried and the roughness assessed by a second, independent examiner. The surface was cleaned using floss and water, dentine conditioner (GC, Tokyo, Japan) was applied for 20 s and rinsed away, and the surface was dried. Glass ionomer sealant (Fuji VII, GC) was then applied on a metal matrix, which was moved up and down between the teeth. The sealant was light cured for 40 s according to manufacturer's instructions and a varnish (GC, Tokyo) applied using a sponge. Then, 1.23% acidulated phosphate fluoride gel was applied using a tray. This was repeated after 6 months. The control teeth only received the fluoride gel application after the initial treatment and after 6 months. | |
| Outcomes | Radiographic progression as assessed by radiographic scoring (1 = outer half of the enamel, 2 = inner half of the enamel) Radiographic progression as assessed by measurement of lesion depths on a continuous scale None of the secondary outcomes were reported. Authors did not state if they measured adverse events, and none were reported. | |
| Notes | Intraclass correlation coefficient of the examinations was 0.97 for the 2 ratings at a 95% confidence interval. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "drawing lots" |
| Allocation concealment (selection bias) | Low risk | Quote: "The sequence was concealed." Comment: no further information available |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "Participants were not blinded." |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Blinded examination. Glass ionomer sealant was radiographically not detectable." |
| Incomplete outcome data (attrition bias) | Low risk | Missing data rate 0% after 12 months |
| Selective reporting (reporting bias) | Low risk | No indication for reporting bias |
| Other bias | Low risk | No indication for other bias |
dmft/DMFT: decayed, missing or filled teeth (primary/permanent);DSR: digital subtraction radiography;HCl: hydrochloric acid; ICDAS: International Caries Detection and Assessment System; s: second.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| No intervention using sealant was included | |
| Not a randomised controlled trial | |
| No intervention using sealant was included | |
| No intervention using sealant was included | |
| No proximal sealing was applied | |
| Not a clinical study | |
| No intervention using sealant was included | |
| Not a randomised controlled trial | |
| No proximal sealing was applied | |
| Not a clinical study | |
| No intervention using sealant was included | |
| No intervention using sealant was included | |
| No intervention using sealant was included | |
| Not a clinical study | |
| No proximal lesions were included | |
| No intervention using sealant was included | |
| No intervention using sealant was included | |
| No intervention using sealant was included | |
| No intervention using sealant was included | |
| Not a clinical study | |
| No intervention using sealant was included | |
| Not a clinical study | |
| Not a clinical study | |
| No intervention using sealant was included | |
| Not a clinical study | |
| No intervention using sealant was included | |
| No intervention using sealant was included | |
| No intervention using sealant was included |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Resin infiltration on the sealing of proximal early caries lesions: a randomised trial |
| Methods | Split‐mouth randomised controlled trial No funding statement Drop‐out 0% after 12 months |
| Participants | 9 participants (56% female, 44% male), aged 5‐40 years, with ≥ 2 lesions up to the enamel‐dentinal junction. Total of 26 lesions. Exclusion criteria: pregnancy, history of tumours of salivary glands, lesions without adjacent tooth, ongoing orthodontic treatment |
| Interventions | Two treatment arms: Group 1: resin infiltration (Icon, DMG) + fluoride varnish application + oral hygiene and dietary advice Group 2: fluoride varnish application + oral hygiene and dietary advice For group 1, resin infiltration was performed according to manufacturer's instructions. In addition, fluoride varnish, dietary advice and oral hygiene instruction were provided. Group 2 received non‐invasive treatments only. |
| Outcomes | Lesion progression according to pairwise reading and digital subtraction radiography |
| Starting date | NA |
| Contact information | Marisa Maltz, Odontologia Preventiva e Social. Porto Alegre, Universidade Federal do Rio Grande do Sul, [email protected] |
| Notes | At 12 months, 2/13 infiltrated and 1/13 non‐invasively treated lesions progressed according to pairwise reading. DSR found 3/13 and 0/13 lesions to progress, respectively. |
| Trial name or title | Radiographic progression of infiltrated caries lesions in vivo |
| Methods | Split‐mouth randomised controlled trial Funded by DMG, Hamburg Drop‐out 23% after 12 months |
| Participants | 12 participants (aged 18 to 24 years) with DMFT of 3 or more; having at least two early caries lesions in proximal posterior tooth surfaces; lesions needed to be visible on radiograph Exclusion criteria: current participation in another clinical study; medically compromised subjects; hyposalivation; pregnancy; allergic to methylmethacrylates or latex; symptomatic teeth |
| Interventions | Group 1: resin infiltration (Icon, DMG) plus oral hygiene, diet counselling, fluoride varnish Group 2: control (sham treatment) plus oral hygiene, diet counselling, fluoride varnish |
| Outcomes | Lesion progression according to pairwise reading and DSR. |
| Starting date | March 2013, estimated completion December 2016 |
| Contact information | Mathilde Peters, University of Michigan ([email protected]) |
| Notes | ClinicalTrials.gov Identifier: NCT01584024 |
DMFT: decayed, missing or filled teeth (primary/permanent);DSR: digital subtraction radiography.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Caries progression follow‐up 12 to 36 months ‐ DSR>Pairwise>Scoring Show forest plot | 7 | 602 | Odds Ratio (Random, 95% CI) | 0.24 [0.14, 0.41] |
| Analysis 1.1  Comparison 1 Proximal sealing versus control/placebo, Outcome 1 Caries progression follow‐up 12 to 36 months ‐ DSR>Pairwise>Scoring. | ||||
| 1.1 Resin sealant versus control | 3 | 330 | Odds Ratio (Random, 95% CI) | 0.26 [0.13, 0.53] |
| 1.2 Resin infiltration versus control/placebo | 2 | 130 | Odds Ratio (Random, 95% CI) | 0.15 [0.06, 0.39] |
| 1.3 Glass ionomer sealant versus control | 1 | 82 | Odds Ratio (Random, 95% CI) | 0.13 [0.01, 2.51] |
| 1.4 Sealant patch versus control | 1 | 60 | Odds Ratio (Random, 95% CI) | 1.0 [0.14, 7.22] |
| 2 Caries progression follow‐up 12 to 30 months ‐ Scoring Show forest plot | 5 | 468 | Odds Ratio (Random, 95% CI) | 0.27 [0.17, 0.44] |
| Analysis 1.2  Comparison 1 Proximal sealing versus control/placebo, Outcome 2 Caries progression follow‐up 12 to 30 months ‐ Scoring. | ||||
| 2.1 Resin sealant versus control | 2 | 256 | Odds Ratio (Random, 95% CI) | 0.33 [0.18, 0.59] |
| 2.2 Resin infiltration versus control/placebo | 2 | 130 | Odds Ratio (Random, 95% CI) | 0.19 [0.08, 0.46] |
| 2.3 Glass ionomer sealant versus control | 1 | 82 | Odds Ratio (Random, 95% CI) | 0.13 [0.01, 2.52] |
| 3 Caries progression follow‐up 18 to 36 months ‐ Pairwise Show forest plot | 4 | 330 | Odds Ratio (Random, 95% CI) | 0.31 [0.18, 0.53] |
| Analysis 1.3 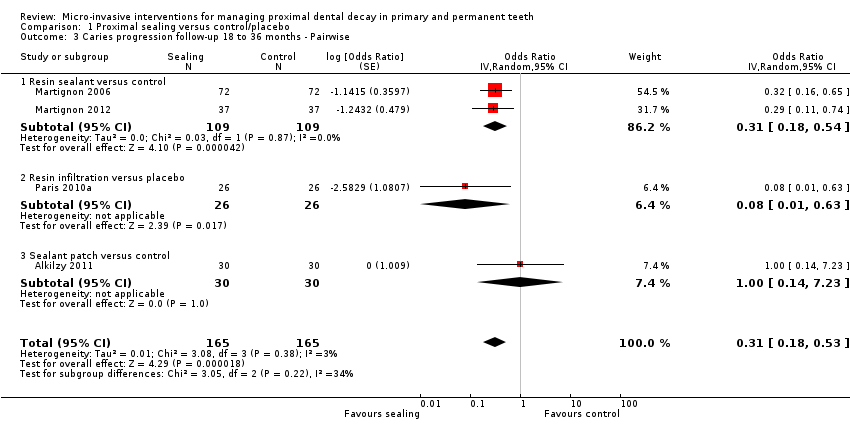 Comparison 1 Proximal sealing versus control/placebo, Outcome 3 Caries progression follow‐up 18 to 36 months ‐ Pairwise. | ||||
| 3.1 Resin sealant versus control | 2 | 218 | Odds Ratio (Random, 95% CI) | 0.31 [0.18, 0.54] |
| 3.2 Resin infiltration versus placebo | 1 | 52 | Odds Ratio (Random, 95% CI) | 0.08 [0.01, 0.63] |
| 3.3 Sealant patch versus control | 1 | 60 | Odds Ratio (Random, 95% CI) | 1.0 [0.14, 7.23] |
| 4 Caries progression follow‐up 12 to 18 months ‐ Digital Substraction Radiography Show forest plot | 3 | 270 | Odds Ratio (Random, 95% CI) | 0.18 [0.06, 0.50] |
| Analysis 1.4  Comparison 1 Proximal sealing versus control/placebo, Outcome 4 Caries progression follow‐up 12 to 18 months ‐ Digital Substraction Radiography. | ||||
| 4.1 Resin sealant versus control | 2 | 218 | Odds Ratio (Random, 95% CI) | 0.23 [0.07, 0.70] |
| 4.2 Resin infiltration versus placebo | 1 | 52 | Odds Ratio (Random, 95% CI) | 0.05 [0.01, 0.45] |

Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Forest plot of comparison: 1 Proximal sealing versus control/placebo, outcome: 1.1 Caries progression follow‐up 12 to 36 months ‐ DSR>Pairwise>Scoring
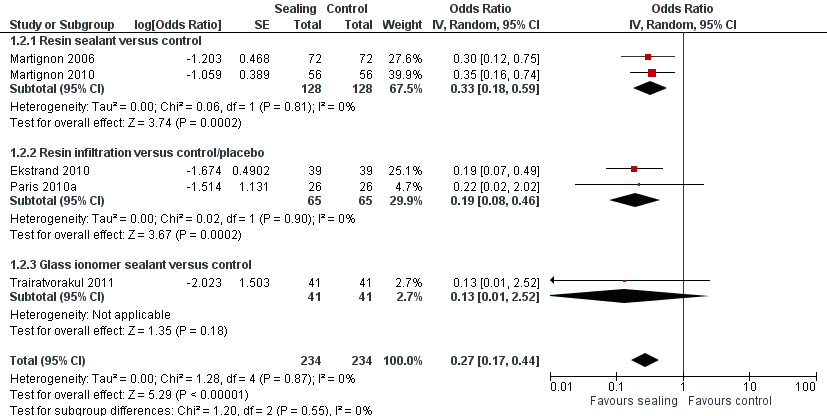
Forest plot of comparison: 1 Proximal sealing versus control/placebo, outcome: 1.2 Caries progression follow‐up 12 to 30 months ‐ Scoring
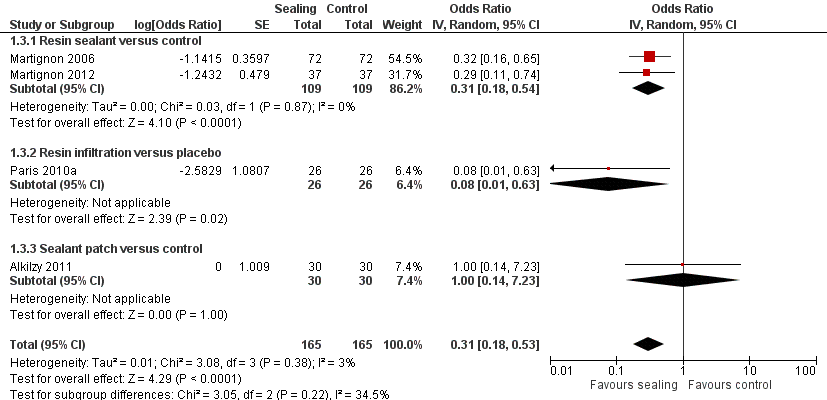
Forest plot of comparison: 1 Proximal sealing versus control/placebo, outcome: 1.2 Pairwise

Forest plot of comparison: 1 Proximal sealing versus control/placebo, outcome: 1.4 Caries progression follow‐up 12 to 18 months ‐ Digital Substraction Radiography.
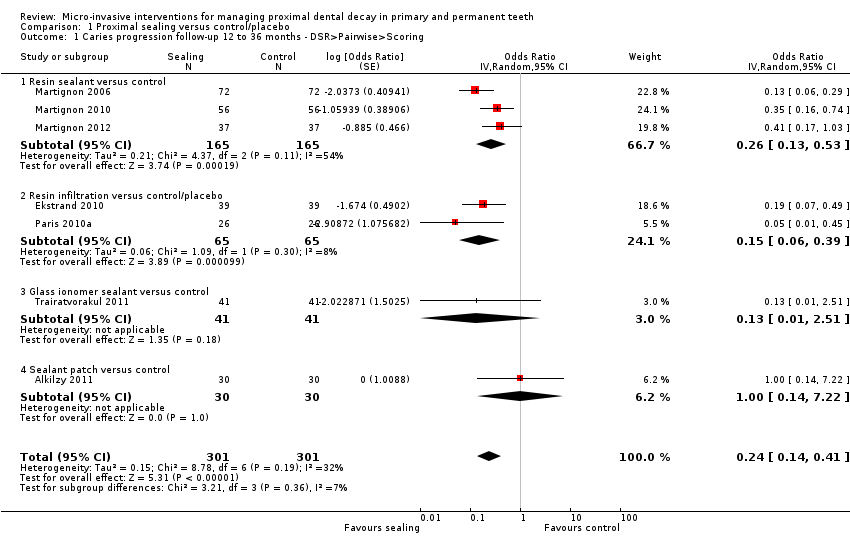
Comparison 1 Proximal sealing versus control/placebo, Outcome 1 Caries progression follow‐up 12 to 36 months ‐ DSR>Pairwise>Scoring.

Comparison 1 Proximal sealing versus control/placebo, Outcome 2 Caries progression follow‐up 12 to 30 months ‐ Scoring.

Comparison 1 Proximal sealing versus control/placebo, Outcome 3 Caries progression follow‐up 18 to 36 months ‐ Pairwise.

Comparison 1 Proximal sealing versus control/placebo, Outcome 4 Caries progression follow‐up 12 to 18 months ‐ Digital Substraction Radiography.
| Micro‐invasive versus non‐invasive treatments for managing dental decay in primary and permanent teeth | ||||||
| Patient or population: people with dental decay on proximal surfaces of primary and permanent teeth Comparison: non‐invasive treatments (e.g. fluoride varnish, advice to floss) Radiographic follow‐up period: 6 months to 3 years | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Odds Ratio | № of participants | Quality of the evidence | Comments | |
| Risk with control | Risk with Sealing | |||||
| Caries progression measured by DSR > pairwise > visual scoring (12 months to 36 months follow‐up) | Study population | OR 0.24 | 602 (7 RCTs) | ⊕⊕⊕⊝ | The quality of evidence for caries progression measured by scoring (12 to 30 months), including 468 participants (5 RCTs), OR 0.27 (95% CI 0.17 to 0.44), was moderatea,b,c. The quality of evidence for caries progression measured by pairwise (18 to 36 months), including 330 participants (4 RCTs), OR 0.31 (95% CI 0.18 to 0.53), was moderatea,b,c. The quality of evidence for caries progression measured by digital substraction radiography (12 months to 18 months), including 270 participants (3 RCTs), OR 0.18 (95% CI 0.06 to 0.50), was moderatea,b,c. | |
| 547 per 1000 | 284 per 1000 | |||||
| Moderate | ||||||
| 649 per 1000 | 337 per 1000 | |||||
| Change in decayed, missing and filled (DMF/dmf) figures at surface, tooth and whole mouth level. | — | — | — | — | — | No studies reported on caries measured as change in decayed, missing and filled (DMF/dmf) figures at surface, tooth or whole mouth level |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aOne or more studies lacked sufficient blinding of participants, personnel or both. Downgraded one level. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Caries progression follow‐up 12 to 36 months ‐ DSR>Pairwise>Scoring Show forest plot | 7 | 602 | Odds Ratio (Random, 95% CI) | 0.24 [0.14, 0.41] |
| 1.1 Resin sealant versus control | 3 | 330 | Odds Ratio (Random, 95% CI) | 0.26 [0.13, 0.53] |
| 1.2 Resin infiltration versus control/placebo | 2 | 130 | Odds Ratio (Random, 95% CI) | 0.15 [0.06, 0.39] |
| 1.3 Glass ionomer sealant versus control | 1 | 82 | Odds Ratio (Random, 95% CI) | 0.13 [0.01, 2.51] |
| 1.4 Sealant patch versus control | 1 | 60 | Odds Ratio (Random, 95% CI) | 1.0 [0.14, 7.22] |
| 2 Caries progression follow‐up 12 to 30 months ‐ Scoring Show forest plot | 5 | 468 | Odds Ratio (Random, 95% CI) | 0.27 [0.17, 0.44] |
| 2.1 Resin sealant versus control | 2 | 256 | Odds Ratio (Random, 95% CI) | 0.33 [0.18, 0.59] |
| 2.2 Resin infiltration versus control/placebo | 2 | 130 | Odds Ratio (Random, 95% CI) | 0.19 [0.08, 0.46] |
| 2.3 Glass ionomer sealant versus control | 1 | 82 | Odds Ratio (Random, 95% CI) | 0.13 [0.01, 2.52] |
| 3 Caries progression follow‐up 18 to 36 months ‐ Pairwise Show forest plot | 4 | 330 | Odds Ratio (Random, 95% CI) | 0.31 [0.18, 0.53] |
| 3.1 Resin sealant versus control | 2 | 218 | Odds Ratio (Random, 95% CI) | 0.31 [0.18, 0.54] |
| 3.2 Resin infiltration versus placebo | 1 | 52 | Odds Ratio (Random, 95% CI) | 0.08 [0.01, 0.63] |
| 3.3 Sealant patch versus control | 1 | 60 | Odds Ratio (Random, 95% CI) | 1.0 [0.14, 7.23] |
| 4 Caries progression follow‐up 12 to 18 months ‐ Digital Substraction Radiography Show forest plot | 3 | 270 | Odds Ratio (Random, 95% CI) | 0.18 [0.06, 0.50] |
| 4.1 Resin sealant versus control | 2 | 218 | Odds Ratio (Random, 95% CI) | 0.23 [0.07, 0.70] |
| 4.2 Resin infiltration versus placebo | 1 | 52 | Odds Ratio (Random, 95% CI) | 0.05 [0.01, 0.45] |

