Tratamiento de heridas a presión negativa para el tratamiento de las heridas del pie en pacientes con diabetes mellitus
Resumen
Antecedentes
Las úlceras del pie en los pacientes con diabetes son un problema de salud prevalente y grave a nivel mundial. El tratamiento de heridas a presión negativa puede utilizarse para tratar estas heridas y se necesita un resumen claro y actual de las pruebas actuales para facilitar la toma de decisiones con respecto a su uso.
Objetivos
Evaluar los efectos del tratamiento de heridas a presión negativa comparado con la atención estándar u otros tratamientos coadyuvantes en la cicatrización de las úlceras del pie en pacientes con DM.
Métodos de búsqueda
En julio de 2013, se realizaron búsquedas en las siguientes bases de datos para identificar informes de ensayos controlados aleatorios relevantes (ECA): Registro Especializado del Grupo Cochrane de Heridas (Cochrane Wounds Group); Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials, CENTRAL); The Database of Abstracts of Reviews of Effects (DARE); The NHS Economic Evaluation Database; Ovid MEDLINE; Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations); Ovid EMBASE; y EBSCO CINAHL.
Criterios de selección
ECA publicados o no publicados que evaluaran los efectos del tratamiento de heridas a presión negativa de cualquier marca para las úlceras del pie en pacientes con diabetes, de forma independiente de la fecha de publicación o el idioma de publicación. Se hizo un esfuerzo especial para identificar los estudios no publicados.
Obtención y análisis de los datos
Dos autores de la revisión, de forma independiente, seleccionaron los estudios, evaluaron el riesgo de sesgo y extrajeron los datos.
Resultados principales
La revisión incluyó cinco estudios que asignaron al azar a 605 participantes. Dos estudios (502 participantes en total) compararon el tratamiento de heridas a presión negativa con apósitos húmedos estándar para heridas. El primero de los mismos se realizó en pacientes con DM y heridas posteriores a la amputación e informó que significativamente más pacientes presentaron la cicatrización en el grupo de tratamiento de heridas a presión negativa comparado con el grupo de apósitos húmedos: (cociente de riesgos 1,44; IC del 95%: 1,03 a 2,01). El segundo estudio, realizado en pacientes con úlceras del pie desbridadas, también informó un aumento estadísticamente significativo de la proporción de úlceras cicatrizadas en el grupo de tratamiento de heridas a presión negativa comparado con el grupo de apósitos húmedos: (cociente de riesgos 1,49; IC del 95%: 1,11 a 2,01). Sin embargo, se observó que estos estudios estuvieron en riesgo de sesgo de realización, de manera que se requiere cuidado en cuanto a su interpretación. Los hallazgos de los tres estudios restantes proporcionaron datos limitados debido a que eran pequeños, con un informe limitado, y también presentaron un riesgo incierto de sesgo.
Conclusiones de los autores
Hay algunas pruebas para sugerir que el tratamiento de heridas a presión negativa es más efectivo para cicatrizar las úlceras del pie posoperatorias y las úlceras del pie en pacientes con DM comparado con los apósitos húmedos para heridas. Sin embargo, estos hallazgos son inciertos debido al posible riesgo de sesgo de los estudios originales. Las limitaciones en las pruebas de los ECA actuales sugieren que se necesitan ensayos adicionales para reducir la incertidumbre alrededor de la toma de decisiones con respecto al uso de THPN para tratar las úlceras del pie en pacientes con DM.
PICOs
Resumen en términos sencillos
Tratamiento de heridas a presión negativa para el tratamiento de las heridas del pie en pacientes con diabetes mellitus
La diabetes, caracterizada por concentraciones sanguíneas altas de glucosa, es un trastorno común que afecta a alrededor de 2 800 000 personas en el Reino Unido (cerca del 4,3% de la población). Algunas personas con diabetes pueden desarrollar úlceras en los pies. Estas heridas pueden tardar mucho tiempo en cicatrizar, ser dolorosas e infectarse. La ulceración del pie en los pacientes con diabetes también puede dar lugar a un riesgo mayor de amputación de partes del pie o la pierna. En general, los pacientes con diabetes presentan un riesgo mayor de amputación del miembro inferior que los pacientes sin diabetes. El tratamiento de heridas a presión negativa es un tratamiento de la herida que incluye la aplicación de succión a la herida. Se utiliza cada vez más en todo el mundo aunque su efectividad no está clara. También es costoso en comparación con los tratamientos como los apósitos. Se encontraron cinco ensayos controlados aleatorios que compararon el tratamiento de heridas a presión negativa con otros tratamientos. Se encontraron algunas pruebas preliminares de que el tratamiento de heridas a presión negativa aumenta la cicatrización de las heridas del pie en los pacientes con diabetes comparado con otros tratamientos. Sin embargo, los hallazgos no son concluyentes y se necesitan más ensayos aleatorios controlados de mejor calidad.
Authors' conclusions
Summary of findings
| NPWT compared to Moist dressings for healing post‐operative wounds in people with diabetes | ||||||
| Patient or population: patients with healing post‐operative wounds in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Moist dressings | NPWT | |||||
| Proportion of wounds healed | Study population | RR 1.44 | 162 | ⊕⊕⊝⊝ | ||
| 388 per 1000 | 559 per 1000 | |||||
| Moderate | ||||||
| Time to ulcer healing | Study population | HR 1.91 | 162 | ⊕⊕⊝⊝ | ||
| 388 per 1000 | 609 per 1000 | |||||
| Moderate | ||||||
| Amputation | Study population | RR 0.25 | 162 | ⊕⊝⊝⊝ | ||
| 106 per 1000 | 26 per 1000 | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 There was the potential for performance bias as unblinded health professionals were able to make decisions about undertaking closure surgery that could then have resulted more wounds being closed (and classed as healed) or amputated in one group compared with the other. | ||||||
| NPWT compared to Moist dressings for debrided foot ulcers in people with diabetes | ||||||
| Patient or population: patients with debrided foot ulcers in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Moist dressings | NPWT | |||||
| Proportion of wounds healed | Low risk of healing1 | RR 1.49 | 341 | ⊕⊕⊝⊝ | ||
| 340 per 1000 | 507 per 1000 | |||||
| Moderate risk of healing1 | ||||||
| 530 per 1000 | 790 per 1000 | |||||
| High risk of healing1 | ||||||
| 650 per 1000 | 968 per 1000 | |||||
| Time to healing | Low risk of healing4 | HR 1.82 | 341 | ⊕⊕⊝⊝ | ||
| 340 per 1000 | 531 per 1000 | |||||
| Moderate risk of healing4 | ||||||
| 530 per 1000 | 747 per 1000 | |||||
| High risk of healing4 | ||||||
| 650 per 1000 | 852 per 1000 | |||||
| Amputation | Study population | RR 0.40 | 341 | ⊕⊕⊝⊝ | ||
| 101 per 1000 | 40 per 1000 | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Baseline risk of healing obtained from external source in which data from 27,630 patients with a diabetic neuropathic foot ulcer was used to develop a simple prognostic model to predict likelihood of ulcer healing (Margolis DJ, Allen‐Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627‐31). It is important to note that given an outcome of ulcer healing, low risk refers to a low risk of healing and thus reflects the most severe patient populations. Conversely high risk refers to a high risk of healing. | ||||||
| NPWT compared to Gauze dressings for debrided foot ulcers in people with diabetes | ||||||
| Patient or population: patients with debrided foot ulcers in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Gauze dressings | NPWT | |||||
| Proportion of wounds healed | Low risk of healing1 | RR 0.38 | 15 | ⊕⊝⊝⊝ | ||
| 340 per 1000 | 129 per 1000 | |||||
| Moderate risk of healing1 | ||||||
| 530 per 1000 | 201 per 1000 | |||||
| High risk of healing1 | ||||||
| 650 per 1000 | 247 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Baseline risk of healing obtained from external source in which data from 27,630 patients with a diabetic neuropathic foot ulcer was used to develop a simple prognostic model to predict likelihood of ulcer healing (Margolis DJ, Allen‐Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627‐31). It is important to note that given an outcome of ulcer healing, low risk refers to a low risk of healing and thus reflects the most severe patient populations. Conversely high risk refers to a high risk of healing. | ||||||
Background
Description of the condition
Diabetes mellitus (DM) is a chronic condition caused by impaired regulation of blood glucose levels. Normally the hormone insulin regulates blood glucose, but in people with type 1 DM production of insulin no longer occurs. Type 2 DM is characterised by cellular insensitivity to insulin, allied with a failure of compensatory pancreatic insulin secretion. In the UK approximately 90% of people with DM have Type 2 (Department of Health 2010).
In the adult population of the UK, the prevalence of diagnosed DM is approximately 4.5% ‐ or 2.9 million people (Diabetes UK 2011). In the United States (USA) the 2010 prevalence of diagnosed DM (all ages) was approximately 6% (Centers for Disease Control and Prevention 2011), and in Canada in 2008/09, for those over one year of age, it was 6.8% (Public Health Agency of Canada 2011). Many cases of DM, however, are undiagnosed, and, when these cases are also taken into consideration, the adjusted 2010 prevalence estimates increase to 10.3% for the USA, 9.2% for Canada, 7.8% for India, and 10.8% for Mexico. The global prevalence of DM is projected to rise further over the next 20 years, largely driven by aging populations, obesity and increasingly sedentary lifestyles (Shaw 2010).
DM is a serious health problem because of the associated glucose‐related complications of the disease, including the specific 'microvascular’ complications such as retinopathy, nephropathy and neuropathy, i.e. damage to the retina, kidney and nerves. Coupled with this, insulin resistance increases the risk of macrovascular complications including cardiovascular, cerebrovascular and peripheral arterial disease (PAD). The particular combination of peripheral neuropathy and peripheral vascular disease contributes to the development of foot ulceration, which may lead to surgical debridement or amputation of the foot or lower limb.
Foot wounds in people with diabetes mellitus
There are two main types of foot wounds that can affect people with DM, which are summarised below.
Foot ulcers
Both PAD and neuropathy are risk factors for the development of chronic foot ulceration in people with DM (Pecoraro 1990; Reiber 1999). PAD and neuropathy can occur separately (the ischaemic foot or the neuropathic foot respectively), or in combination (the neuroischaemic foot). Foot ulceration is reported to affect 15% or more of people with DM at some time in their lives (Reiber 1996; Singh 2005). Estimates of the prevalence of foot ulceration vary, but around 1% to 4% of people with DM have foot ulcers at any given time (Abbott 2002; Kumar 1994). Figures for 2008 showed that, for those people with DM in receipt of US Medicare, the prevalence of the presence of least one foot ulcer was 8% (Margolis 2011).
An ulcer forms as a result of damage to the epidermis (outermost layer of skin) and subsequent loss of underlying tissue. A foot ulcer is specifically defined by the International Consensus on the Diabetic Foot as a wound that extends through the full thickness of the skin below the level of the ankle (Apelqvist 2000a). This definition is not concerned with duration of the ulcer (although some definitions of chronic ulceration require a duration of six weeks or more), and includes ulcers that extend to muscle, tendon and bone. The severity of foot ulcers in people with DM can be graded using a number of systems. The Wagner wound classification system was one of the first described and has, historically, been widely used, although it is now rarely used in clinical practice. This system assessed ulcer depth and the presence of osteomyelitis (bone infection) or gangrene and graded them as: grade 0 (pre‐ or post‐ulcerative lesion), grade 1 (partial/full‐thickness ulcer), grade 2 (probing to tendon or capsule), grade 3 (deep with osteitis (inflammation of the bone)), grade 4 (partial foot gangrene) and grade 5 (whole foot gangrene) (Wagner 1981). Newer grading systems, such as the PEDIS system (Schaper 2004), the University of Texas Wound Classification System (Oyibo 2001), and SINBAD have been developed since (Ince 2008), with the SINBAD system being the best validated (Karthikesalingam 2010).
Foot ulcers in people with DM have a serious impact on health‐related quality of life, particularly with respect to physical functioning and role‐limitations due to physical and emotional issues (Nabuurs‐Franssen 2005; Ribu 2006). They also represent a major use of health resources, incurring costs not only for dressings, but also staff costs (for podiatrists, nurses, doctors), tests and investigations, antibiotics and specialist footwear. In 2010‐11 the estimated NHS spend on foot ulceration and amputation in people with DM in England was GBP 639 to GBP 662 million (Kerr 2012). The economic impact is also high in terms of the personal costs to patients and carers, for example, costs associated with lost work time and productivity while the patient is unable to bear weight or is hospitalised. As many as 85% of foot‐related amputations are preceded by ulceration (Apelqvist 2000b; Pecoraro 1990).
In terms of ulcer healing, a meta‐analysis of trials in which people with neuropathic ulcers received good wound care, reported that 24% of ulcers completely healed by 12 weeks and 31% by 20 weeks (Margolis 1999). Reasons for delayed healing can include: infection (especially osteomyelitis (bone infection)), co‐morbidities such as peripheral vascular disease and end‐stage renal disease, and the size and depth of an ulcer at presentation. Even when ulcers do heal, the risk of recurrence is high. Pound 2005 reported that 62% of ulcer patients (from a sample of 231 people) became ulcer‐free at some stage over a 31‐month observation period, however, 40% of the ulcer‐free group went on to develop a new, or recurrent, ulcer after a median of 126 days. Indeed, the ulcer recurrence rate over five years can be as high as 70% (Dorresteijn 2010; Van Gils 1999). Failure of ulcers to heal may result in amputation, and people with DM have a 10 to 20‐fold higher risk of losing a lower limb, or part of a lower limb, to non‐traumatic amputation than those without DM (Morris 1998; Wrobel 2001).
Surgical wounds to the foot in people with diabetes mellitus
The risk of lower limb amputation is much greater for people with DM than for those without. The major underlying pathophysiology associated with amputation are neuropathy and ischaemia. Lower limb amputation can have devastating consequences for people's health status and health‐related quality of life (Tennvall 2000), as well as having a large financial impact on healthcare providers and users. In the UK, from 1 April 2007 to 31 March 2010, a total of 16,693 lower limb amputations were recorded in people with DM (Holman 2012). Of these 10,216 were classed as minor amputations (usually defined as below the ankle joint), and 6,477 as major amputations (usually defined as above the ankle joint). The UK cost of 'foot procedures related to diabetes or arterial disease and procedures to amputation stumps' was estimated as approximately GBP 17 million over 2009/10. In the US, the 2008 prevalence of lower extremity amputation in Medicare recipients was 1.8%, with a total mean annual Medicare reimbursement cost for each person with DM and a lower extremity amputation estimated at USD 54,000. Ulcers are often considered to be chronic wounds, whilst post‐surgical amputation sites are considered to be acute wounds, unless they do not heal (Ubbink 2008a).
As well as amputation debridement (regarded as an important component of the treatment of 'chronic' foot wounds, such as ulcers or non‐healing surgical wounds, in people with DM) can sometimes be undertaken as a surgical procedure. Debridement involves removal of dead tissue and callus (along with pressure‐relief/offloading, treatment of infection and revascularisation, where necessary). As in other areas of wound care, sharp (surgical) debridement of diabetic foot wounds is recommended in guidelines in order to promote wound healing by 'converting' a chronic wound to an acute wound via removal of dead tissue and slough (Steed 2006). Whilst this practice is common, there is little evidence that surgical debridement promotes healing of diabetic foot wounds (Eneroth 2008; Lebrun 2010), but debridement of necrotic tissue with eschar from wounds, including diabetic foot wounds, can sometimes be a requirement prior to the use of wound treatments such as negative pressure wound therapy (NPWT) (KCI 2012b)
Description of the intervention
Any intervention that promotes healing, or reduces amputation rates, or both, in foot wounds in people with DM would be make an important difference, and a number of health technologies are marketed with these outcomes in mind. The evidence, however, for the clinical and cost‐effectiveness of these technologies is frequently lacking. A recent suite of Cochrane reviews (Dumville 2011a; Dumville 2011b; Dumville 2012a; Dumville 2012b), and an associated mixed treatment comparison (Dumville 2012c), found no robust evidence to suggest that any one dressing was more effective than another in terms of healing foot ulcers in people with DM. A similar conclusion was drawn following a systematic review by the International Working Group of the Diabetic Foot (Game 2012).
Negative pressure wound therapy (NPWT) is a technology that is currently used widely in wound care. NPWT is promoted for use on complex wounds ‐ including foot wounds in people with DM ‐ as an adjunct (additional) therapy to standard care. NPWT involves the application of a wound dressing through which a negative pressure (or vacuum) is applied, with wound and tissue fluid being collected into a canister. The intervention was developed in the 1990s, and the uptake of NPWT in the healthcare systems of developed countries has been dramatic. A US Department of Health report estimated that between 2001 and 2007 Medicare payments for NPWT pumps and associated equipment increased from USD 24 million to USD 164 million (an increase of almost 600%) (Department of Health and Human Services 2009). Initially only one NPWT manufacturer supplied NPWT machines (the V.A.C system: KCI, San Antonio Texas), however, as the NPWT market has grown, a number of different commercial NPWT systems have been developed, with machines becoming smaller and more portable. Indeed, the most recent introduction to the market is a single use, or 'disposable', negative pressure product. Ad hoc, homemade, negative pressure devices are also used, especially in resource‐poor settings. These devices tend to use simple wound dressings, such as gauze, or transparent occlusive (non‐permeable) dressings, with negative pressure generated in hospital by vacuum suction pumps.
A number of different healthcare professionals prescribe and apply NPWT, and it is now used both in secondary and primary (community) care, particularly following the introduction of ambulatory systems. Whilst the NPWT systems outlined above differ in a number of respects ‐ such as type of pressure (constant or cyclical) applied to the wound, the material in contact with the surface of the wound and also the type of dressing used ‐ the principle of applying a negative pressure to the wound in a closed environment is the same for all products.
How the intervention might work
NPWT ostensibly assists in wound management by collecting high volumes of wound exudate, reducing the frequency of dressing changes by keeping anatomically‐challenging wounds (such foot wounds) clean, and reducing odour. Manufacturers, however, also suggest that the application of mechanical force to the wound provides biologically‐plausible processes by which wound healing is promoted, i.e. the drawing together of wound edges, increased perfusion, and the removal of infectious material and exudate (KCI 2012a). NPWT might have a beneficial effect by encouraging off‐loading (i.e. reducing the weight taken on the foot, as some NPWT systems make ambulation difficult) and preventing unnecessary dressing changes and repeated exposures to the environment.
There are some potentially negative aspects associated with NPWT; these include wound maceration (softening due to exposure to liquid), retention of dressings, and wound infection as well as other injuries (FDA 2011). NPWT devices are usually worn continually by patients during treatment, they can interfere with mobility, and, anecdotally, are often noisy, which prevents some patients from sleeping.
Why it is important to do this review
NPWT is an expensive ‐ yet widely used ‐ health technology for the management of complex wounds, and there is potential for its use to increase. Indeed, in the UK NPWT can now be prescribed by primary care physicians (who may not have specific training in wound care). A Cochrane review that examines the clinical effectiveness of NPWT for chronic wounds has already been published, but, given that foot wounds in patients with DM present unique challenges though their varied and complex pathophysiology, we feel this focused review will add value to previous publications. Indeed, this proposed review will include all foot wounds in people with DM (both surgical and non‐surgical), and an important focus will be clarification and consideration of the study populations and the impact of their aetiologies (causes) on interpretation of trial evidence in this area.This scope means that, for people with DM, we will present evidence from foot wounds caused by surgical debridement and recent amputation, in addition to evidence for the effects of NPWT on non‐surgically treated foot ulcers or other non‐healing foot wounds. This approach will provide an up‐to‐date and comprehensive overview of evidence for NPWT for all types of foot wound in people with DM, with a focus on considering the type of diabetic foot wound to which current evidence relates.
Furthermore, as a previous study has highlighted (Peinemann 2008), there is a large number of trials of NPWT that have either been discontinued or remain unpublished. Peinemann et al found that nine out of 19 completed or discontinued NPWT randomised controlled trials (RCTs) were unpublished. Furthermore, these nine unpublished studies included the majority of planned or analysed patients (70% of the total participants). Thus any review of NPWT requires a clear strategy for investigating unpublished sources of literature and the reasons for discontinuation with, or without, non‐publication of studies.
In conclusion, we feel that a Cochrane review that comprehensively identifies, interrogates, presents and synthesises evidence of the effects of NPWT on the outcomes of foot wounds in people with DM will be a valuable piece of research. The review is relevant to clinical policy and consumer decision‐makers in providing a robust overview of current evidence, and to researchers and funders in highlighting areas of uncertainty that may be addressed by future research. This is relevant, since the draft National Institute of Health and Clinical Excellence (NICE) Clinical Guideline "Diabetic foot problems: In‐patient management of diabetic foot problems" (NICE 2011), recommends that "negative pressure wound therapy should not be routinely used to treat diabetic foot problems, but may be considered in the context of a clinical trial or as rescue therapy (when the only other option is amputation)."
Objectives
To assess the effects of negative pressure wound therapy compared with standard care or other therapies in the healing of foot wounds in people with diabetes mellitus (DM).
Methods
Criteria for considering studies for this review
Types of studies
Published or unpublished RCTs that evaluate the effects of any brand of NPWT in the treatment of diabetic foot wounds, irrespective of publication status or language of publication.
Types of participants
Trials recruiting people with Type 1 or Type 2 DM, with foot wounds below the ankle, regardless of underlying aetiology (i.e. ischaemic, neuropathic or neuroischaemic). This includes diabetic foot ulcers, or wounds resulting from amputation or other surgical treatment, or both. We included trials involving people of any age and from any setting.
Where trials with broad inclusion criteria have recruited participants with diabetic foot wounds as part of a larger chronic wound study population e.g. alongside participants with pressure ulcers or leg ulcers, these trials were excluded unless the results for the subgroup of participants with diabetic foot wounds were reported separately or were available from authors on request.
Types of interventions
Any brand of NPWT (including studies that investigated homemade or ad hoc negative pressure devices) compared with standard care (such as advanced wound dressings and gauze) or other treatments, so that NPWT was the only difference between trial arms.
Types of outcome measures
Primary outcomes
Complete wound healing
Trialists measure and report wound healing in many different ways, including: time to complete wound healing, proportion of wounds healed during follow‐up and rates of change of wound size. For this review we regarded trials that reported one or more of the following, as providing the best measures of outcome in terms of relevance and rigour.
-
Time to wound healing within a specific time period, correctly analysed using survival, time‐to‐event, approaches ‐ ideally with adjustment for relevant co‐variates such as size of wound at baseline (start of trial). We assumed that the period of time in which healing could occur was the duration of the trial, unless otherwise stated.
-
Number of wounds completely healed during follow‐up (frequency of complete healing).
-
Change (and rate of change) in wound size, when adjusted for baseline size ‐ ideally analysed using multi‐level modelling or (multiple) linear regression.
We note that, since wound healing is a subjective outcome, it can be at high risk of measurement bias when outcome assessment is not blinded.
Amputation
-
Major amputation (defined as any amputation above the ankle joint).
-
Minor amputation (defined as any amputation below the level of the ankle joint).
Secondary outcomes
-
Participant health‐related quality of life/health status (measured using a standardised generic questionnaire such as EQ‐5D, SF‐36, SF‐12 or SF‐6 or wound‐specific questionnaires such as the Cardiff wound impact schedule at noted time points.We did not include ad hoc measures of quality of life that were not likely to be validated and would not be common to multiple trials.
-
Other adverse events, including infection and pain (measured using survey/questionnaire/data capture process or visual analogue scale), where a clear methodology for the collection of adverse event data was provided.
-
Resource use (including measurements of resource use such as number of dressing changes, nurse visits, length of hospital stay and re‐operation/intervention).
-
Wound recurrence.
Search methods for identification of studies
Electronic searches
In July 2013, we searched the following databases to identify reports of RCTs:
-
Cochrane Wounds Group Specialised Register (searched 30 July 2013);
-
The Cochrane Central Register of Controlled Trials (CENTRAL) (2013, Issue 7);
-
The Database of Abstracts of Reviews of Effects (DARE) (2013, Issue 7);
-
The NHS Economic Evaluation Database (2013, Issue 7);
-
Ovid MEDLINE (1946 to January Week 30 2013);
-
Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations July 29, 2013);
-
Ovid EMBASE (1974 to 2013 Week );
-
EBSCO CINAHL (1982 to 26 July 2013).
The following search strategy was used in the Cochrane Central Register of Controlled Trials (CENTRAL):
#1 MeSH descriptor: [Foot Ulcer] explode all trees437
#2 MeSH descriptor: [Diabetic Foot] explode all trees390
#3 (diabet* near/3 ulcer*):ti,ab,kw 524
#4 (diabet* near/5 (foot or feet)):ti,ab,kw 847
#5 (diabet* near/5 wound*):ti,ab,kw 171
#6 (diabet* near/3 defect*):ti,ab,kw 14
#7 MeSH descriptor: [Amputation] explode all trees299
#8 MeSH descriptor: [Amputation Stumps] explode all trees44
#9 (diabetic near/3 amputat*):ti,ab,kw 31
#10 MeSH descriptor: [Debridement] explode all trees411
#11 (debrid* or slough* or deslough*):ti,ab,kw 1141
#12 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 2336
#13 MeSH descriptor: [Negative‐Pressure Wound Therapy] explode all trees62
#14 MeSH descriptor: [Suction] explode all trees719
#15 MeSH descriptor: [Vacuum] explode all trees115
#16 MeSH descriptor: [Drainage] explode all trees1896
#17 ("negative pressure" or negative‐pressure or TNP):ti,ab,kw 502
#18 (sub‐atmospheric or subatmospheric):ti,ab,kw 20
#19 ((seal* next surface*) or (seal* next aspirat*)):ti,ab,kw 17
#20 (wound near/2 suction*):ti,ab,kw 62
#21 ((foam next suction) or (suction next dressing*)):ti,ab,kw 0
#22 (vacuum assisted closure or VAC):ti,ab,kw 234
#23 ((vacuum next therapy) or (vacuum next dressing*) or (vacuum next seal*) or (vacuum next assist*) or (vacuum near closure) or (vacuum next compression) or (vacuum next pack*) or (vacuum next drainage)):ti,ab,kw 162
#24 #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 87386
#25 #12 and #24 403
We adapted this strategy to search Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL. We combined the Ovid MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximising version (2008 revision) (Lefebvre 2011). We combined the EMBASE search with the Ovid EMBASE filter developed by the UK Cochrane Centre (Lefebvre 2011). We combined the CINAHL searches with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN 2012). We did not restrict studies with respect to language, date of publication or study setting.
We searched the following clinical trials registries:
-
ClinicalTrials,gov (http://www.clinicaltrials.gov/) Febuary 2013;
-
WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/Default.aspx) Febuary 2013;
-
Current Controlled Trials (http://www.controlled‐trials.com/); Febuary 2013.
Searching other resources
We were keen to explore sources of unpublished data. To maximise identification of unpublished or studies that were not located during the search stage we searched the reference lists of the included studies and of previous systematic reviews. We also examined the content of European Wound Management conference proceedings (2012‐2013) and systematic reviews in the field that might refer to data we had not found, and contacted key manufacturers (KCI, and Smith & Nephew) to ask about unpublished (as well as on‐going) work. We also contacted key authors in the field.
Data collection and analysis
Selection of studies
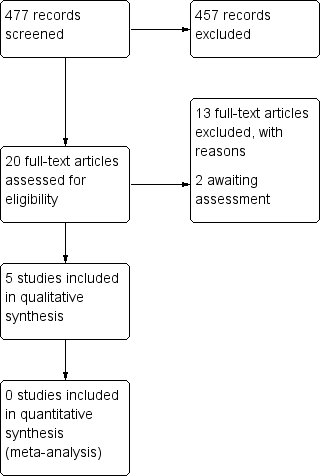
Two review authors independently assessed the titles and abstracts of retrieved studies for relevance. After this initial assessment, we obtained full copies of all studies felt to be potentially relevant. Two review authors independently checked the full papers for eligibility; disagreements were resolved by discussion and, where required, the input of a third review author. We recorded all reasons for exclusion of studies for which we had obtained full copies. We completed a PRISMA flowchart to summarise this process (Liberati 2009).
Data extraction and management
We extracted and summarised details of the eligible studies using a data extraction sheet. Two review authors extracted data independently and resolved disagreements by discussion, drawing on a third reviewer where required. Where data were missing from reports, we attempted to contact the study authors to obtain this information. We included studies published in duplicate once, but extracted the maximal amount of data. We extracted the following data, where possible:
-
country of origin;
-
participants' type of DM;
-
wound aetiology (e.g. PAD)
-
type of wound, including site on foot;
-
unit of investigation (per patient) ‐ single wound, or foot, or patient, or multiple wounds on the same patient;
-
care setting;
-
number of participants randomised to each trial arm;
-
eligibility criteria and key baseline participant data;
-
details of the dressing/treatment regimen received by each group;
-
details of any co‐interventions;
-
number of post‐amputation/debridement wounds closed surgically;
-
primary and secondary outcome(s) (with definitions);
-
outcome data for primary and secondary outcomes (by group);
-
duration of follow‐up;
-
number of withdrawals (by group);
-
adverse events;
-
publication status of study; and,
-
source of funding for trial.
Assessment of risk of bias in included studies
Two review authors independently assessed each included study using the Cochrane Collaboration tool for assessing risk of bias (Higgins 2011). This tool addresses six specific domains, namely, sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other issues (e.g. extreme baseline imbalance, issues with unit of investigation). We assessed blinding of participants and health professionals, and blinded outcome assessment separately. We were aware that blinding of participants and health professionals to treatment received would not be possible, but it was important to understand if, and how, studies had compensated for this where required, i.e. where outcomes such as wound closure and amputation could be at risk of performance bias. We completed a 'Risk of Bias' table for each eligible study. Disagreements about risk of bias assessment were resolved by discussion. Where possible, when a lack of reported information resulted in an unclear decision, authors were contacted for clarification.
We classified trials as being at high risk of bias if they were rated 'high' for one or more of three key criteria, namely, randomisation sequence, allocation concealment and blinded outcome assessment. We also considered the potential for performance and measurement bias for each primary and secondary outcome extracted.
Measures of treatment effect
Where possible, studies were grouped according to wound type. Where possible, we presented the outcome results for each trial with 95% confidence intervals (CI). We reported estimates for dichotomous outcomes (e.g. ulcers healed during a particular time period) as risk ratios (RR). We used the RR rather than odds ratio (OR), since, when event rates are high, as is the case for many trials reporting wound healing, ORs (when interpreted as RR) can give an inflated impression of the effect size (Deeks 2002). We planned to report outcomes relating to continuous data (e.g. percentage change in ulcer area) as mean differences (MD) and overall effect size (with 95% CI). Where a study reported data on time‐to‐healing (the probability of healing over a consecutive time period) we planned to report and plot these data (where possible) using hazard ratio estimates. However, where the hazard ratio was not reported, but data regarding the number of events and the P value for a log rank test (reported to at least two significant figures) were reported, we employed methods proposed by Parmar 1998 to calculate the hazard ratio indirectly. Where log rank test P values were published to only one significant figure the robustness of the calculated hazard ratio for the highest possible P value was investigated to test robustness of estimates. Hazard ratios and associated 95% CIs were then calculated using the inverse variance option in RevMan (RevMan 2011).
Unit of analysis issues
We recorded whether trials presented outcomes in relation to a wound, a foot, a participant or as multiple wounds on the same participant. We also recorded occasions where multiple wounds on a participant were (incorrectly) treated as independent within a study, rather than having within‐patient analysis methods applied. This was recorded as part of the risk of bias assessment. For wound healing and amputation, unless otherwise stated, where the number of wounds appeared to equal the number of participants, we treated the wound as the unit of analysis. For other adverse event outcomes, in order to facilitate further analyses, we aimed to establish whether data were presented at the level of the participant, because in this area there is potential for data to refer to multiple events occurring to a single person (or wound per person), which means that data cannot be analysed further without violating the assumption of independence.
Dealing with missing data
It is common to have data missing from trial reports. Excluding participants post‐randomisation from the analysis, or ignoring those participants who are lost to follow‐up compromises the randomisation, and potentially introduces bias into the trial. In individual studies, where data on the proportion of ulcers healed were presented, we assumed that if randomised participants were not included in an analysis, their wound did not heal (i.e. they would be considered in the denominator but not the numerator). Where a trial did not specify participant group numbers prior to drop‐out, we presented only complete case data. In a time‐to‐healing analysis using survival analysis methods, drop‐outs should be accounted for as censored data. Hence all participants contributed to the analysis. Such analysis assumes that drop‐outs are missing at random (i.e. not associated with time‐to‐healing). We present data for area change, and for all secondary outcomes, as a complete case analysis.
Assessment of heterogeneity
We considered both clinical and statistical heterogeneity. Wherever appropriate, that is, where studies appeared similar in terms of wound type, intervention type, duration and outcome type, we planned to pooled data using meta‐analysis (conducted using RevMan 5.1 (RevMan 2011)). We planned to assess statistical heterogeneity using the Chi² test (a significance level of P less than 0.1 was considered to indicate heterogeneity) and the I² estimate (Higgins 2003). The I² estimate examines the percentage of total variation across studies due to heterogeneity rather than to chance. Values of I² higher than 50% indicate a high level of heterogeneity. In the absence of clinical heterogeneity and in the presence of statistical heterogeneity (I² over 50%), we envisioned using a random‐effects model, however, we did not anticipate pooling studies where heterogeneity was very high (I² over 75%). Where there was no clinical or statistical heterogeneity we used a fixed‐effect model.
Data synthesis
We combined studies using a narrative overview, with meta‐analyses of outcome data where appropriate (in RevMan 5). The decision to include studies in a meta‐analysis depended on the availability of treatment effect data and assessment of heterogeneity. For time‐to‐event data, we planned to use the inverse variance method on the estimated hazard ratio and standard error, when reported or calculated from available data.
Where relevant, and possible, we planned to conduct sensitivity analyses to investigate the potential impact of studies at high risk of bias on pooled results.
Subgroup analysis and investigation of heterogeneity
We considered whether there was potential heterogeneity between wounds types, i.e. foot ulcers and surgical wounds resulting from surgical debridement of an ulcer, or amputation on any part of a diabetic foot. Where there was evidence of between‐trial heterogeneity in trial‐level co‐interventions, especially off‐loading, we envisaged a sub‐group analysis being conducted based on variations in co‐interventions, e.g. all trial participants reported to receive adequate offloading protocol/advice being compared with trial participants who received unclear advice about offloading ‐ however, this was not required. Finally, depending on the number and heterogeneity of included studies, we considered using meta‐regression to investigate wound aetiology as a possible explanatory variable.
Summary of findings
We present the main results of the review in 'Summary of findings' tables, which provide key information concerning the quality of evidence, the magnitude of effect of the interventions examined, and the sum of available data on the main outcomes, as recommended by the Cochrane Collaboration (Schunemann 2011a). We included the following main outcomes in the 'Summary of findings' tables:
-
complete wound healing;
-
amputation.
The 'Summary of findings' tables include an overall grading of the evidence related to each of the main outcomes, using the GRADE approach (Schunemann 2011b).
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies for full details of the studies identified. Two studies are awaiting classification, one requiring further details before a decision regarding eligibly can be decided (Tuncel 2013) and one requiring translation (Sun 2007). Two studies have been identified as on‐going: ISRCTN34166832 and ISRCTN90301130. To date ISRCTN34166832 has not recruited any participants relevant to this review (personal communication, see Characteristics of ongoing studies).
Included studies
A total of five studies randomising 605 participants were included in this review. Four studies were two‐armed (Armstrong 2005; Blume 2008; Karatepe 2011; Mody 2008), and one was three‐armed (Novinščak 2010). All studies were parallel studies. Two studies were undertaken in the USA (Armstrong 2005; Blume 2008), one in Turkey (Karatepe 2011); one in Croatia (Novinščak 2010) and one in India (Mody 2008). Populations evaluated in the studies were people with DM and foot wounds: resulting from amputation (Armstrong 2005) and classed as foot ulcers (Blume 2008; Karatepe 2011; Mody 2008; Novinščak 2010). NPWT treatments for all studies except Novinščak 2010 (no details provided) and Mody 2008 (non‐commercial system) were the VAC® system (Kinetic Concepts Inc., TX, USA). Comparison arms received a variety of treatments including:
(a) Advanced moist wound therapy (moist wound therapy with alginates, hydrocolloid, foam or hydrogel dressings (Armstrong 2005); advanced moist wound therapy dressings, predominantly hydrogels and alginates (Blume 2008); moist dressings (not gauze) (Novinščak 2010); or,
(b) Gauze (moist gauze dressing (Mody 2008), dry gauze (Novinščak 2010), and sterilized gauze (Karatepe 2011)).
Follow‐up times were: eight weeks (Novinščak 2010); 16 weeks (Armstrong 2005; Blume 2008), or unclear (Karatepe 2011; Mody 2008). In terms of primary outcomes, four studies reported proportion of wounds healed (Armstrong 2005; Blume 2008; Novinščak 2010; Mody 2008); three reported time‐to‐healing data (Armstrong 2005; Blume 2008; Karatepe 2011), and two reported data on major and/or amputations recorded during study follow‐up (Armstrong 2005; Blume 2008). For further details see Table 1 .
| Armstrong 2005 | 16 weeks | Diabetic foot amputation to trans‐metatarsal level | Group A: moist wound therapy with alginates, hydrocolloid, foam or hydrogel dressings (n = 85) Group B: NPWT (VAC system, dressing changes every 48 h. Treatment conducted until wound closure or completion of 112‐day assessment (n = 77) | Number of wounds completely healed Group A: 33/85 (38.8%) Group B: 43/77 (55.8%) Of healed wounds —healed by secondary intention (without primary/surgical wound closure) Group A: 25/33 (75.8%) Group B: 31/43 (72.1%) Remaining wounds were closed following surgery. Time to wound healing median time to healing Group A: 77 days (IQR 40 to 122) Group B: 56 days (IQR 26 to 92) Log rank = p = 0.005 Amputation Number of participants undergoing further amputation Group A: 9/85 (10.6%) Major = 5/Minor = 4 Group B: 2/77 (2.3%) Major = 0/Minor = 2 There was no difference noted in time to healing for acute or chronic wounds. | Adverse events Participants who had one or more adverse events Group A: 46/85 (54.1%) Group B: 40/77 (51.9%) Participants who had one or more treatment‐related adverse events Group A: 11/85 (12.9%) 5 classified as serious Group B: 9/77 (11.7%) 1 classified serious Resource use Average total cost per participant Group A: USD 36,887 Group B: USD26,972 Average total direct cost per participants for those treated for 8 weeks or longer Group A: USD 36,096 Group B: USD 27,270 Average per participant cost to achieve 100% healing Group A: USD 38,806 Group B: USD 25,954 |
| Blume 2008 | 16 weeks | Ulceration of the foot in people with diabetes | Group A: advanced moist wound therapy dressings used according to guidelines/local protocols (n = 169) Group B: NPWT (VAC system), applied according to manufacturer’s instructions. (n = 172) | Number of wounds completely healed (six participants excluded in paper as did not receive treatment, added back into denominator here) Group A: 48/169 (28.4%) Group B: 73/172 (42.4%) Proportion of wounds closed using surgery (unclear if considered part of healed group) Group A: 14/169 (8.3%) Group B: 16/172 (9.3%) Time to wound healing median time to healing Group A: could not be estimated Group B: 96 days (95% CI 75.0 to 114.0) Log rank taken as P value 0.001 Amputation Number of participants undergoing amputation* Group A: 17/169 (10.1%) Major = 4; minor = 13 Group B: 7/172 (4.1%) Major = 5; minor = 2 | Adverse events Limited data: not extracted Resource use – taken from conference abstract that we think is related to this main publication. Mean estimated total costs of inpatient services per participant Group A: USD 8570 (95%CI USD 5922 to USD 11,432) Group B: USD 5206 (95%CI USD 3172 to USD 7561) |
| Karatepe 2011 | Not specified. Last assessment one month after healing | Diabetic foot ulcers | Group A: conventional wound care treatment: based on text in report taken to be dry gauze (n = 37) Group B: NPWT (VAC system) (n = 30) | Time to healing Median time to healing Group A: 4.4 weeks Group B: 3.9 weeks Mean value presented but not extracted. No specific P value presented | Health‐related quality of life SF‐36: Data not presented. |
| Mody 2008 | Not specified: until healing or loss to follow‐up | Diabetic foot ulcers | Group A: wet‐to‐dry gauze (n = 9) Group B: locally‐constructed NPWT (n = 6) | Number of wounds completely healed By secondary intention: Group A: 1/9 (11.0%) Group B: 1/6 (16.6%) By delayed primary closure: Group A: 3/9 (33%) Group B: 0/6 (0%) | |
| Novinščak 2010 | 2 months | Complicated diabetic foot ulcers | Group A: classic gauze (n = 8) Group B: dressings (moist) (n = 12) | Healing rate (percentage with wound closure – defined by author on contact) Group A: 4/8* (50%) Group B: 9/12* (75%) Group C: * could not be calculated (90%) *Figure calculated by review author as only proportions obtained from study author |
Excluded studies
Thirteen studies were excluded after investigation of the full text. In total: one study did not have a population with foot wounds and the study population could not be confirmed in a further study; four studies had study populations with multiple wound types and we were unable to obtain separate data on people with DM and foot wounds; four studies contained no relevant outcomes; two studies were not considered to be RCTs, and one study evaluated NPWT as part of a range of treatments, so this intervention was not the only difference between trial groups. See Characteristics of excluded studies for further details.
See Figure 1 for study flow diagram.
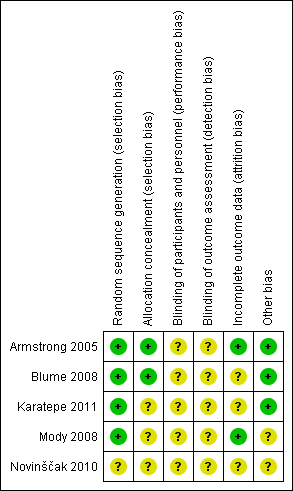
Risk of bias in included studies
See Figure 2; Figure 3 for corresponding figures.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Adequacy of randomisation process
All included studies were described as 'randomised' with four studies providing information to confirm that adequate sequence generation had taken place (Armstrong 2005; Blume 2008; Karatepe 2011; Mody 2008); these were judged to be at low risk of bias for this domain (all studies using computer‐generated sequences). Novinščak 2010 did not described how randomisation took place, and were judged to be at unclear risk of bias for this domain.
Allocation concealment
Two of the five studies were judged to be at low risk of bias for allocation concealment (Armstrong 2005; Blume 2008). Both studies employed "sealed envelopes containing opaque, black paper labelled with assigned treatment and patient ID number that were sequentially numbered and provided to each site", which we deemed to be robust. The remaining studies did not contain enough detail for us to make a judgement for this domain, and so were judged as being at unclear risk of bias.
Blinding
All studies were deemed to be at unclear risk of bias. We note that whilst Armstrong 2005 and Blume 2008 appeared to undertake some blinded outcome assessment, we questioned the potential impact of non‐blinded decisions regarding the use of further surgery. There was no indication that the decision to undertake closure or amputation was guided by the protocol to ensure that there were no differences in performance between groups for reasons other than the treatment received (e.g. surgery was an option only when wounds reached a particular size or condition), or was undertaken by a blinded committee to ensure consistency between groups. Given the non‐blinded status of health professionals to treatment received, there may have been the potential for performance bias in promoting surgery (thus closure or amputation) in one group compared with the other.
Incomplete outcome data
Two studies were deemed to be at low risk of bias for attrition bias (Armstrong 2005; Mody 2008). Three studies were classed as being at unclear risk of bias: Blume 2008 reported a small number of post‐randomised exclusions, as well as being unclear about whether there was a large number of early censoring in the analysis; Karatepe 2011 and Novinščak 2010 reported very little information regarding participant flow through the study.
Effects of interventions
See: Summary of findings for the main comparison NPWT compared to Moist dressings for healing post‐operative wounds in people with diabetes; Summary of findings 2 NPWT compared to Moist dressings for debrided foot ulcers in people with diabetes; Summary of findings 3 NPWT compared to Gauze dressings for debrided foot ulcers in people with diabetes
Outcome data are summarised in Table 1.
1. NPWT compared with moist (non‐gauze) dressings
a. Post‐operative wounds
One study was included in this analysis. Armstrong 2005 randomised 162 participants who had previously undergone diabetic foot amputation (to the trans‐metatarsal level) to receive NPWT (dressing changed every 48 hours) or treatment with alginate, hydrocolloid, foam or hydrogel dressings. Participants were followed for 16 weeks.
Primary outcomes
Proportion of wounds healed
There was a statistically significant increase in the number of wounds healed in the group treated with NWPT (43/77; 56.0%) compared with the moist dressing group (33/85; 38.8%) (RR 1.44; 95% CI 1.03 to 2.01) (Analysis 1.1). This meant that people in the NPWT group had 1.44 times the 'risk' of healing of people in the moist dressing group. The study was classed as being at low risk of bias in all assessed domains except blinding, for which it was classed as unclear. Whilst 'wounds healed' did undergo blinded outcome assessment, health professionals were aware of treatment received during the study and could decide to close wounds via surgery. There was no indication in the study report(s) that this decision to stop NPWT treatment and recommend surgery was guided by specific decision rules (e.g. size of wound), or was made in a blinded fashion. Thus, potentially, different numbers and types of participants within groups may have had wounds 'closed' ‐ introducing bias if this decision was based only on knowledge of treatment being received. In total, 12/77 (22%) of participants in the NPWT group had wounds classed as healed following closure via surgery compared with 8/85 (9%) of participants in the dressing group. From study data it is not clear if NPWT improves wounds so that surgery becomes an appropriate option for more people, or whether there is a bias here. If wounds healed after surgical closure are treated as a secondary outcome, and only wounds that healed by secondary intention (i.e. without surgery) are considered, the finding becomes non‐significant (RR 1.37: 95% CIs 0.89 to 2.10) (analysis not presented graphically here).
Time to ulcer healing
Armstrong 2005 reported that time to complete wound closure was significantly shorter in the NPWT group (median time‐to‐healing of 56 days) compared with the moist dressing group (median time‐to‐healing 77 days). We note that these reported figures do not agree with the Kaplan‐Meier curve reported in the paper, where median values seemed to be higher. The results of the time to wound closure analysis were reported by the authors as being a statistically significant result (P value 0.005: results from a log rank test). Using the observed numbers of events and total numbers in each group together with the reported P value to calculate the log‐hazard ratio and its standard error (Parmar 1998), we calculated the log hazard ratio to be 0.645 (0.69 where maximum P value of log rank test assumed, as only reported to one significant figure) with a standard error of 0.23, which equals a hazard ratio of 1.91 with 95% CI 1.21 to 2.99. Thus our calculations suggest that, at any point during follow‐up, the hazard (or chance) of healing in those allocated to NWPT was 1.9 times that of those allocated to the moist dressing group (Analysis 1.2). As above, there is the potential for the time‐to‐healing outcome to be biased by the undertaking of closure surgery in a non‐blinded and non‐protocol‐driven manner.
Amputations
A greater proportion of people in the moist dressing group had an amputation though this difference was not statistically significant (NWPT group 2/77 (3%); moist dressing group 9/85 (11%) (RR 0.25, 95% CI 0.05 to 1.10) (Analysis 1.3). Five of the amputations in the moist dressing group were classed as major, but there were no major amputations in the NPWT‐treated group. We note that the study was not powered to detect a difference in number of amputations, and the number of events was low. Also it is not clear whether decisions about amputation were covered by decision rules in the protocol to avoid any potential performance bias.
Secondary outcomes
Adverse events
There was no statistically significant difference in the number of participants experiencing one or more adverse events in the NPWT group (40/77; 52%) compared with the moist dressing group (46/85; 54%) (RR 0.96; 95% CI 0.72 to 1.28) (Analysis 1.4). Neither was there a statistically significant difference when only treatment‐related adverse events were considered (RR 0.90; 95% CI 0.40 to 2.06) (Analysis 1.4).
Resource use
Armstrong 2005 study reported an average total cost per participant of USD 26,972 in the NPWT group compared with USD 36,887 in the most dressing group ‐ no standard deviation data were reported, and data have not been analysed further here. The difference was driven by those in the dressing group reporting a greater number of: outpatient visits, dressing changes and surgical debridements. No cost effectiveness or cost utility analysis to reflect incremental differences in cost to benefit (with uncertainty around these) was reported.
b. Foot ulcers
Two studies were included in this analysis. Blume 2008 randomised 341 participants with DM and foot ulcers to NPWT (applied according to manufacturer’s instructions) or advanced moist wound‐therapy dressings (predominately hydrogels and alginates) with a 16‐week follow‐up. Study inclusion criteria specified that ulcers should be Wagner Grades 2 or 3 and with an area of 2 cm2 or greater. Novinščak 2010 randomised 19 participants with complicated diabetic foot ulcers to NPWT (no further details provided) or moist dressings (no further details provided) with a two‐month follow‐up.
Primary outcomes
Proportion of wounds healed
Blume 2008 there was a statistically significant increase in the number of wounds healed in the NWPT group (73/172; 42%) compared with the moist dressing group (48/169; 28%) (RR 1.49; 95% CI 1.11 to 2.01) (Analysis 1.1). This means, on average, the NPWT group were49% more likely to heal compared with the moist dressing group. The study was classed as being at low risk of bias for all domains except for incomplete outcome data and blinded outcome assessment, which were classed as unclear. Incomplete outcome assessment was classed as unclear because 31% of participants in the NPWT group and 25% in the dressing group were classed as 'discontinued' in the study CONSORT flow diagram. Reasons for discontinuation included adverse events, ineffective treatment withdrawal by the investigator, and death. It is not clear whether participants who were discontinued for reasons other than death were also censored from the analysis, rather than being followed up. If discontinuation did result in censoring in this open trial it may have introduced bias. Blinded outcome assessment was classed as unclear for similar reasons to the Armstrong 2005 trial. Unblinded health professionals were able to make decisions about doing closure surgery that did not appear to be pre‐specified by the study protocol; this could have resulted more wounds being closed (and classed as healed) in one group.
Novinščak 2010 reported that 90% of participants treated in the NPWT group (n = 7) had a healed wound compared with 75% in the moist dressing group (n = 12). Data were not analysed further since actual numbers of participants healed were not provided, and we were unable to calculate how the figure of 90% had been reached in a group of seven participants (since 6/7 equals 86%). The study report contained limited data and was classed as being at unclear risk of bias for all domains.
Time to ulcer healing
Blume 2008 reported that time to complete wound closure was significantly shorter in the NPWT group, with median time‐to‐healing of 96 days (95% CI 75 to 112), compared with the moist dressing group, in which the median number of participants healed was not reached over the 16‐week follow‐up. A log rank test returned a P value of 0.001. Using the method of Parmar 1998 the log hazard ratio was calculated as 0.598 (0.581 where maximum P value of log rank test assumed as only reported to one significant figure) with a standard error of 0.182, which equals a hazard ratio of: 1.82 with 95% CI 1.27 to 2.60. These calculations suggested that, at any point during follow‐up, the hazard (or chance) of healing for those allocated to NWPT was 1.8 times that of those allocated to the moist dressing group (Analysis 1.2). As above, there was potential for the time‐to‐healing outcome to have been affected by the undertaking of closure surgery in a non‐blinded and non‐protocol‐driven way.
Amputations
Blume 2008 reported a statistically significant reduction in the number of amputations between the NWPT group (7/172; 4%) compared with the moist dressing group (17/169; 10%) (RR 0.40, 95% CI 0.17 to 0.95) (Analysis 1.3). Five of the amputations in the NPWT group were classed as major, compared with four in the moist dressing group. Again, it was not clear whether, in order to avoid any potential performance bias, decisions about amputation were covered by decision rules in the protocol .
Secondary outcomes
Resource use
Blume 2008 reported the mean estimated total costs of inpatient services per participant as USD 5206 (95% CI USD 3172 to 7561) in the NPWT group compared with USD 8570 (95% CI USD 5922 to USD 11,432) in the dressing group. No further resource use/cost data were presented, and data were not analysed in the context of costs versus benefits.
c. Pooled data
We did not pool any data for this comparison due to clinical heterogeneity between studies.
Summary of NPWT compared with moist (non‐gauze) wound dressings
There is some evidence of greater healing of diabetic foot wounds (resulting from partial amputation or ulceration) over a 16‐week period with NPWT compared with moist dressings. Data also suggest that people allocated to NPWT were at a significantly reduced risk of amputation compared with those allocated to moist dressings. There is some weak evidence that NPWT might also be a cheaper treatment than moist dressings. However, the studies from which these findings are drawn are at unclear risk of bias. It is important to recognise that, potentially, decisions regarding closure surgery and amputation might have been affected by health professionals' knowledge of treatments received (summary of findings Table for the main comparison; summary of findings Table 2).
2. NPWT compared with gauze dressings
a. Post operative wounds
No included studies
b. Foot ulcers
Three studies were included in this analysis of foot ulcers. Karatepe 2011 randomised 67 participants with DM and foot ulcers to NPWT or daily wound care that consisted of debridement and treatment of gangrenous tissue, where required, and use of sterilized gauze dressing. Participants were followed for an unspecified period. Mody 2008 recruited a total of 48 participants: 15 of these were reported to have diabetic foot ulcers, with nine treated with wet to dry gauze, and six treated with a locally‐constructed NPWT machine. Novinščak 2010 was described in the previous comparison.
Primary outcomes
Proportion of wounds healed
Karatepe 2011 did not report data on proportion of wounds healed. Mody 2008 reported that 1/6 (16.6%) participants allocated to NPWT had healed (by secondary intention) compared with 4/9 (44.4%) allocated to dressings (one by secondary intention and three by delayed primary closure, i.e. stitching after surgery) RR: 0.38 95% CI 0.05 to 2.59 (Analysis 2.1). Novinščak 2010 reported that 90% of participants treated in the NPWT group (n = 7) had a healed wound compared with 50% in the moist dressing group (n = 8). Data were not analysed further, as study figures were not provided, and we were unable to calculate how 90% had been reached in a group of seven participants (as 6/7 equals 86%). The study report contained limited data, and was classed as being at unclear risk of bias for all domains.
Time to ulcer healing
Karatepe 2011 reported that median time‐to‐healing was 3.9 weeks in the NPWT group compared with 4.4 weeks in the gauze group. Limited data were presented and a hazard ratio could not be calculated. Novinščak 2010 did not report data on time to ulcer healing.
Amputation
The three studies did not report relevant data about amputation (Karatepe 2011; Mody 2008; Novinščak 2010).
Secondary outcomes
Health related quality of life
Karatepe 2011 reported collection of SF‐36 data ‐ however these were not presented, and were not available.
c. Pooled data
Due to limited data we did not pool any data for this comparison.
Summary of NPWT compared with gauze dressings
There was limited RCT‐derived data from which to draw conclusions regarding the comparative effectiveness of NPWT when compared to gauze dressings summary of findings Table 3.
Discussion
Summary of main results
There is some evidence that NPWT is a clinically effective treatment (in terms of reducing time‐to‐healing and reducing risk of amputations) for foot wounds in people with DM. This relates to wounds that are post‐operative and of relatively short duration as well as chronic, but debrided, ulcers. These findings are predominantly based on two studies that compared the VAC® system with moist wound dressings (Armstrong 2005; Blume 2008). However, it is important to note that the risk of bias in these two studies was difficult to assess and the results presented must be considered in this light. Evidence from the three other included studies was limited by small sample sizes, the collection and reporting of limited outcome data, as well as a lack of detail about the type of foot wounds being assessed. Individually and collectively, these three studies make a limited contribution to the findings presented here.
Quality of the evidence
The two largest studies included in this review Armstrong 2005 and Blume 2008 were similar in design (both were funded by the manufacturer of VAC® ‐ KCI) although they evaluated different types of foot wounds. Whilst these studies were deemed to be at low risk of bias for random sequence generation and allocation concealment, the risk of performance and detection bias for both was unclear, since study reports suggested that key decisions regarding the treatment of wounds, such as closure surgery and further amputation, were made by unblinded health professionals and were not guided by a trial protocol in a way that would minimise potential performance bias. This issue has been noted in other reviews (e.g. Medical Advisory Secretariat 2006), and the validity of combining wounds closed by secondary intention and those closed by surgery questioned. For Blume 2008 it was also unclear whether the studies analysis was as close to an intention‐to‐treat analysis as would be possible with the data collected.
We also note that the included studies had limited information about the receipt of important adjunctive therapies such as off‐loading. Whilst these therapies were often noted as being delivered where required, it would be useful to know whether their delivery was balanced between studies groups, as they are such an important part of routine care.
Potential biases in the review process
In this, as in other areas, all RCT study data should be available in the public domain to enable decision‐making to be informed by the most comprehensive evidence base possible. However, previous work highlighted the large number of RCTs of NPWT that have either been terminated, or have been completed but remain unpublished (Peinemann 2008). Extensive searching here did not locate further unpublished studies beyond those previously identified (Peinemann 2008), However, there may well be other studies of which we are not aware. We also note that some studies were excluded because they evaluated interventions on multiple wound types, and specific data for foot wounds in people with DM were not available.
Agreements and disagreements with other studies or reviews
One previous systemic review with a title suggesting a focus on diabetic foot ulcers has been published (Noble‐Bell 2008). The review included four studies that were classed as RCTs, however two of these were excluded from our review ((Etoz 2007 (n = 24); McCallon 2000 (n = 10)), as they used a method of allocation based on alternation and we consider this a quasi‐randomised method of allocation. One further study was excluded from our review as it did not report relevant outcome data (Eginton 2003). The remaining study included in our review (Armstrong 2005). The Noble‐Bell 2008 review highlighted the positive findings from Armstrong 2005, whilst recommending further larger RCTs in a wider number of diabetic foot‐wound groups. We summarise the same RCT findings but recommend more cautious interpretation of Armstrong 2005.
All other relevant key reviews have assessed the effectiveness of NPWT across wound types, including foot wounds in people with DM. The relevant Cochrane review concludes that "Trials comparing TNP [NPWT] with alternative treatments for chronic wounds have methodological flaws and data do demonstrate a beneficial effect of TNP on wound healing, however more, better quality research is needed" (Ubbink 2008b). However, no studies included in the Ubbink 2008b review are included here; ‐ partly because this previous review only considered chronic wounds, partly because we did not consider unadjusted change in wound size data as an outcome and finally, because more recent studies are available e.g. Blume 2008.
Finally, recent NICE guidelines reviewed the data regarding use of NPWT for treatment of foot wounds in people with DM (NICE 2011). They included three studies: two of which we include here (Armstrong 2005; Blume 2008) and one which we excluded (as above) Etoz 2007. The review conducted within the Guideline also found that "two RCTs with a total number of 497 participants showed that participants who received NPWT with standard wound care were significantly less likely to have an amputation, and significantly more likely to have complete wound closure, when compared with participants who received standard wound care alone." However, the GRADE assessment of the evidence in the NICE guideline regarded this as low quality evidence. The NICE Guideline Development Group recommended that, " . . . a health economic evaluation should be carried out to further assess its [NPWT] cost effectiveness as an adjunctive treatment for diabetic foot problems . . . " (page 128). The Guideline Development Group also "recommended the use of the intervention in the context of a clinical trial or as a rescue therapy to prevent amputation" (page 128). The findings from our review agree that further robust RCT research would help to reduce uncertainty regarding the effectiveness of NPWT in the treatment of foot wounds in people with DM. Robust studies should focus on ensuring confidence that differences in outcomes, such as healing and amputations, can be attributed to the intervention, rather than occurring as a result of bias. We note that, despite these recommendations, we found only one on‐going RCT in the UK (ISRCTN34166832), and this is not specific to foot wounds in people with DM .

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
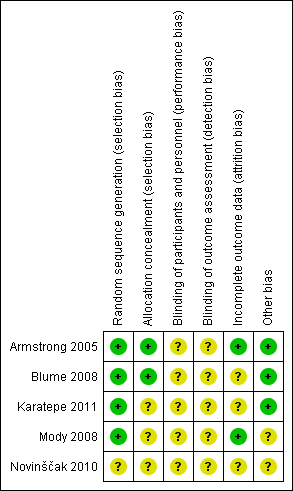
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 1 Proportion of wounds healed.
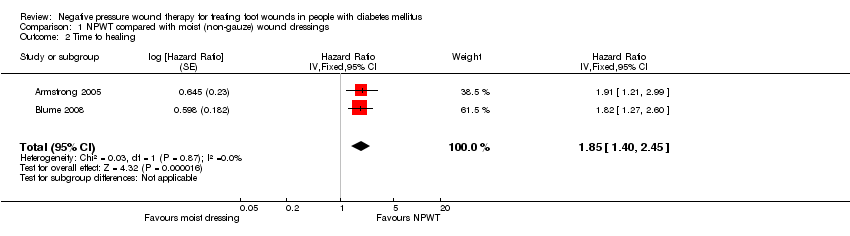
Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 2 Time to healing.
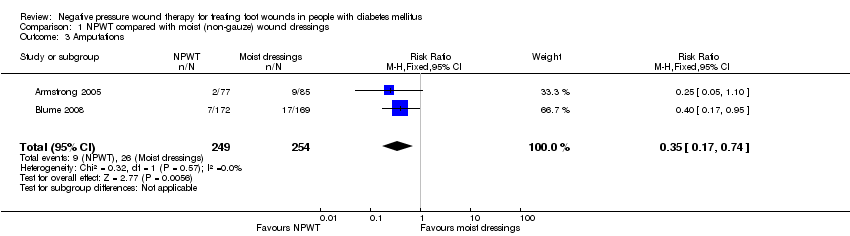
Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 3 Amputations.

Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 4 Adverse events.
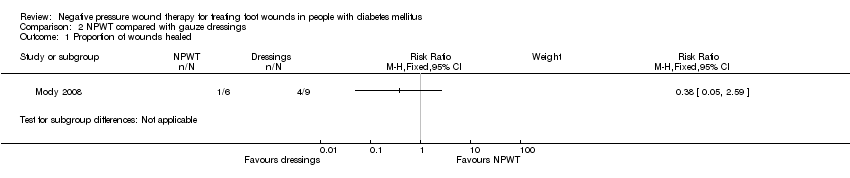
Comparison 2 NPWT compared with gauze dressings, Outcome 1 Proportion of wounds healed.
| NPWT compared to Moist dressings for healing post‐operative wounds in people with diabetes | ||||||
| Patient or population: patients with healing post‐operative wounds in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Moist dressings | NPWT | |||||
| Proportion of wounds healed | Study population | RR 1.44 | 162 | ⊕⊕⊝⊝ | ||
| 388 per 1000 | 559 per 1000 | |||||
| Moderate | ||||||
| Time to ulcer healing | Study population | HR 1.91 | 162 | ⊕⊕⊝⊝ | ||
| 388 per 1000 | 609 per 1000 | |||||
| Moderate | ||||||
| Amputation | Study population | RR 0.25 | 162 | ⊕⊝⊝⊝ | ||
| 106 per 1000 | 26 per 1000 | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 There was the potential for performance bias as unblinded health professionals were able to make decisions about undertaking closure surgery that could then have resulted more wounds being closed (and classed as healed) or amputated in one group compared with the other. | ||||||
| NPWT compared to Moist dressings for debrided foot ulcers in people with diabetes | ||||||
| Patient or population: patients with debrided foot ulcers in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Moist dressings | NPWT | |||||
| Proportion of wounds healed | Low risk of healing1 | RR 1.49 | 341 | ⊕⊕⊝⊝ | ||
| 340 per 1000 | 507 per 1000 | |||||
| Moderate risk of healing1 | ||||||
| 530 per 1000 | 790 per 1000 | |||||
| High risk of healing1 | ||||||
| 650 per 1000 | 968 per 1000 | |||||
| Time to healing | Low risk of healing4 | HR 1.82 | 341 | ⊕⊕⊝⊝ | ||
| 340 per 1000 | 531 per 1000 | |||||
| Moderate risk of healing4 | ||||||
| 530 per 1000 | 747 per 1000 | |||||
| High risk of healing4 | ||||||
| 650 per 1000 | 852 per 1000 | |||||
| Amputation | Study population | RR 0.40 | 341 | ⊕⊕⊝⊝ | ||
| 101 per 1000 | 40 per 1000 | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Baseline risk of healing obtained from external source in which data from 27,630 patients with a diabetic neuropathic foot ulcer was used to develop a simple prognostic model to predict likelihood of ulcer healing (Margolis DJ, Allen‐Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627‐31). It is important to note that given an outcome of ulcer healing, low risk refers to a low risk of healing and thus reflects the most severe patient populations. Conversely high risk refers to a high risk of healing. | ||||||
| NPWT compared to Gauze dressings for debrided foot ulcers in people with diabetes | ||||||
| Patient or population: patients with debrided foot ulcers in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Gauze dressings | NPWT | |||||
| Proportion of wounds healed | Low risk of healing1 | RR 0.38 | 15 | ⊕⊝⊝⊝ | ||
| 340 per 1000 | 129 per 1000 | |||||
| Moderate risk of healing1 | ||||||
| 530 per 1000 | 201 per 1000 | |||||
| High risk of healing1 | ||||||
| 650 per 1000 | 247 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Baseline risk of healing obtained from external source in which data from 27,630 patients with a diabetic neuropathic foot ulcer was used to develop a simple prognostic model to predict likelihood of ulcer healing (Margolis DJ, Allen‐Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627‐31). It is important to note that given an outcome of ulcer healing, low risk refers to a low risk of healing and thus reflects the most severe patient populations. Conversely high risk refers to a high risk of healing. | ||||||
| Armstrong 2005 | 16 weeks | Diabetic foot amputation to trans‐metatarsal level | Group A: moist wound therapy with alginates, hydrocolloid, foam or hydrogel dressings (n = 85) Group B: NPWT (VAC system, dressing changes every 48 h. Treatment conducted until wound closure or completion of 112‐day assessment (n = 77) | Number of wounds completely healed Group A: 33/85 (38.8%) Group B: 43/77 (55.8%) Of healed wounds —healed by secondary intention (without primary/surgical wound closure) Group A: 25/33 (75.8%) Group B: 31/43 (72.1%) Remaining wounds were closed following surgery. Time to wound healing median time to healing Group A: 77 days (IQR 40 to 122) Group B: 56 days (IQR 26 to 92) Log rank = p = 0.005 Amputation Number of participants undergoing further amputation Group A: 9/85 (10.6%) Major = 5/Minor = 4 Group B: 2/77 (2.3%) Major = 0/Minor = 2 There was no difference noted in time to healing for acute or chronic wounds. | Adverse events Participants who had one or more adverse events Group A: 46/85 (54.1%) Group B: 40/77 (51.9%) Participants who had one or more treatment‐related adverse events Group A: 11/85 (12.9%) 5 classified as serious Group B: 9/77 (11.7%) 1 classified serious Resource use Average total cost per participant Group A: USD 36,887 Group B: USD26,972 Average total direct cost per participants for those treated for 8 weeks or longer Group A: USD 36,096 Group B: USD 27,270 Average per participant cost to achieve 100% healing Group A: USD 38,806 Group B: USD 25,954 |
| Blume 2008 | 16 weeks | Ulceration of the foot in people with diabetes | Group A: advanced moist wound therapy dressings used according to guidelines/local protocols (n = 169) Group B: NPWT (VAC system), applied according to manufacturer’s instructions. (n = 172) | Number of wounds completely healed (six participants excluded in paper as did not receive treatment, added back into denominator here) Group A: 48/169 (28.4%) Group B: 73/172 (42.4%) Proportion of wounds closed using surgery (unclear if considered part of healed group) Group A: 14/169 (8.3%) Group B: 16/172 (9.3%) Time to wound healing median time to healing Group A: could not be estimated Group B: 96 days (95% CI 75.0 to 114.0) Log rank taken as P value 0.001 Amputation Number of participants undergoing amputation* Group A: 17/169 (10.1%) Major = 4; minor = 13 Group B: 7/172 (4.1%) Major = 5; minor = 2 | Adverse events Limited data: not extracted Resource use – taken from conference abstract that we think is related to this main publication. Mean estimated total costs of inpatient services per participant Group A: USD 8570 (95%CI USD 5922 to USD 11,432) Group B: USD 5206 (95%CI USD 3172 to USD 7561) |
| Karatepe 2011 | Not specified. Last assessment one month after healing | Diabetic foot ulcers | Group A: conventional wound care treatment: based on text in report taken to be dry gauze (n = 37) Group B: NPWT (VAC system) (n = 30) | Time to healing Median time to healing Group A: 4.4 weeks Group B: 3.9 weeks Mean value presented but not extracted. No specific P value presented | Health‐related quality of life SF‐36: Data not presented. |
| Mody 2008 | Not specified: until healing or loss to follow‐up | Diabetic foot ulcers | Group A: wet‐to‐dry gauze (n = 9) Group B: locally‐constructed NPWT (n = 6) | Number of wounds completely healed By secondary intention: Group A: 1/9 (11.0%) Group B: 1/6 (16.6%) By delayed primary closure: Group A: 3/9 (33%) Group B: 0/6 (0%) | |
| Novinščak 2010 | 2 months | Complicated diabetic foot ulcers | Group A: classic gauze (n = 8) Group B: dressings (moist) (n = 12) | Healing rate (percentage with wound closure – defined by author on contact) Group A: 4/8* (50%) Group B: 9/12* (75%) Group C: * could not be calculated (90%) *Figure calculated by review author as only proportions obtained from study author |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion of wounds healed Show forest plot | 2 | 503 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [1.18, 1.84] |
| 2 Time to healing Show forest plot | 2 | Hazard Ratio (Fixed, 95% CI) | 1.85 [1.40, 2.45] | |
| 3 Amputations Show forest plot | 2 | 503 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.17, 0.74] |
| 4 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 All adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Treatment‐related adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion of wounds healed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |