Tratamiento de heridas a presión negativa para el tratamiento de las heridas del pie en pacientes con diabetes mellitus
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | 2‐arm RCT; undertaken in USA (in wound and academic centres) | |
| Participants | 162 adult participants Inclusion criteria: presence of: (1) wound from a diabetic foot amputation to the transmetatarsal level of the foot; (2) adequate perfusion; (3) University of Texas grade 2 or 3 Exclusion criteria: people presenting with (1) active Charcot arthropathy of the foot; (2) wounds resulting from burns; (3) venous insufficiency; (4) untreated cellulitis or osteomyelitis (after amputation); (5) collagen vascular disease; (6) malignant disease in the wound; or people treated with: (7) corticosteroids; (8) immunosuppressive drugs or chemotherapy; (9) NPWT (in the last 30 days); (10) growth factors; (11) normothermic therapy; (12) hyperbaric medicine; (13) bioengineered tissue products (in the last 30 days) Key baselines co‐variates: Wound area (cm2): Group A: 19.2 (SD = 17.6) Group B: 22.3 (SD = 23.4)
Wound duration (months): Group A: 1.8 (SD = 5.9) Group B: 1.2 (SD = 3.9) 75.3% of the study population had wounds that were < 30 days' duration (classed as acute wounds by the author) and 24.7% had wounds that were > 30 days' duration (classed as chronic wounds by authors) | |
| Interventions | Group A (n = 85): moist wound therapy with alginates, hydrocolloid, foam or hydrogel dressings – adhering to standardised guidelines at the discretion of attending clinician. Dressings changed every other day unless recommended by treating clinician Group B (n = 77): NPWT (VAC® system) no information provided regarding the pressure applied or the cycle (e.g. constant/cyclical etc); dressing changes every 48 h. Treatment conducted until wound closure or completion of 112 day assessment.
All participants received: (1) off‐loading therapy, preventatively and therapeutically as indicated ‐ a pressure relief sandal or walker was provided for all participants; (2) sharp debridement within 2 days of randomisation and as deemed necessary by treating clinician; and, (3) measurement of pre‐albumin, albumin and HbA1c levels in 7 days before entering the study. Low pre‐study albumin levels resulted in consultation with nutritionist, and dietary supplement initiated if needed. | |
| Outcomes | Primary outcome: (1) number of wounds completely healed (defined as 100% re‐epithelialisation without drainage and INCLUDED closure via surgery where the decision for surgical closure was made by treating clinician); (2) time to wound healing; (3) amputation Secondary outcomes: (1) other adverse events (serious and non‐serious); (2) resource use | |
| Notes | Follow‐up: 112 days (16 weeks) Outcome assessment: based on data from wound assessments and digital photographs taken by treatment clinicians at days 0, 7, 14, 28, 42, 56, 84 and 112 A secondary analysis of trial data reported that 75% of wounds were ≤ 1 month in duration (classed by authors as acute) and 25% were > 1 month in duration (classed by authors as chronic). We note that mean baseline values for ulcer duration were obviously very skewed Funding: study funded by KCI – manufacturers of the VAC® intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was accomplished by using www.randomizer.org to generate 15 blocks of 10 random numbers each." Comment: adequate methodology |
| Allocation concealment (selection bias) | Low risk | Quote: "Numbers were systematically assigned to each treatment group, and sealed envelopes containing opaque, black paper labelled with assigned treatment and patient ID number were sequentially numbered and provided to each site. The black paper was added to ensure that the contents of the envelopes were not visible prior to opening." Comment: adequate methodology |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: it is understandably not possible to blind participants and patients to whether or not they receive NPWT. However, given this, it is important that any decision‐making that might be affected by performance bias is recognised and blinding is introduced where possible. We note that unblinded health professionals were able to make decisions about closure surgery that could then have resulted in more wounds being closed (and classed as healed) or amputated in one group compared to the other. As a result of this we classed the risk of bias for this domain as unclear. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "Neither patients nor investigators were masked to the randomised treatment assignment . . . However, notes that the masking component of the study dealt specifically with planimetry measurements from digital photographs . . . concordance between the investigator and the digital planimetry provided independent confirmation of the primary efficacy endpoint of complete wound healing." Comment: assessment of healing seems to have had a blinded component |
| Incomplete outcome data (attrition bias) | Low risk | Comment: no evidence of incomplete outcome data |
| Other bias | Low risk | No evidence of other bias |
| Methods | 2‐arm RCT; undertaken in USA | |
| Participants | 342 adult participants Inclusion criteria: (1) stage 2 or 3 (Wagner’s scale) calcaneal, dorsal or planter foot ulcer; ulcer ≥ 2 cm2 in area after debridement; (3) adequate blood perfusion (various tests and cut‐offs reported) Exclusion criteria: (1) recognised active Charcot disease; (2) ulcers resulting from electrical, chemical or radiation burns; (3) collagen vascular disease; (4) ulcer malignancy; (5) untreated osteomyelitis or cellulitis; (6) uncontrolled hyperglycaemia; (7) inadequate lower extremity perfusion; (8) pregnant or nursing mothers; or ulcer treatment within 30 days of trial start with (9) normothermic or hyperbaric oxygen therapy, (10) corticosteroids, (11) immunosuppressive drugs, (12) chemotherapy, (13) recombinant or autologous growth factor products, (14) skin and dermal substitutes; or (15) use of any enzymic debridement treatment. Key baselines co‐variates: Wound area (cm2): Group A: 11.0 (SD = 12.7) Group B: 13.5 (SD = 18.2)
Wound duration (months) Group A: 6.9 (SD = 12.2) Group B: 6.6 (SD = 10.8) | |
| Interventions | Group A (n = 169): advanced moist wound therapy dressings used according to guidelines/local protocols ‐ noted as being predominantly hydrogels and alginates Group B (n = 172): NPWT (VAC® system) applied according to manufacturer’s instructions, but no information provided about the pressure applied or the cycle (e.g. constant/cyclical etc). Treatment continued until wound closure, or until there was sufficient granulation tissue formation for healing by primary and secondary intention All participants received: (1) assessment and debridement of ulcers within 2 days of randomisation; (2) off‐loading therapy as deemed necessary | |
| Outcomes | Primary outcome: (1) number of wounds completely healed (defined as 100% re‐epithelialisation without drainage or dressing requirement and INCLUDED closure via surgery where the decision for surgical closure was made by treating clinician); (2) time to wound healing; (3) amputation Secondary outcomes: (1) other adverse events (serious and non‐serious); (2) resource use | |
| Notes | Follow‐up: 112 days (16 weeks) Outcome assessment: participants examined weekly for the first 4 weeks and then every other day until day 112, or ulcer closure by any means. Participants achieving closure were followed up at 3 and 9 months Funding: study funded by KCI – manufacturers of the VAC® intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:"Randomization was accomplished by generating blocks of numbers through http://www.randomizer.org." Comment: adequate methodology |
| Allocation concealment (selection bias) | Low risk | Quote: "Numbers were assigned to a treatment group and sealed in opaque envelopes containing black paper labelled with treatment and patient ID. Envelopes were sequentially numbered before clinical trial site distribution. At patient randomisation, treatment was assigned on the basis of the next sequentially labelled envelope." Comment: adequate methodology |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: It is understandably not possible to blind participants and patients to whether or not they receive NPWT. However, given this, it is important that any decision‐making that might be affected by performance bias is recognised and blinding is introduced where possible. We note that unblinded health professionals were able to make decisions about undertaking closure surgery that could then have resulted more wounds being closed (and classed as healed) or amputated in one group compared with the other. As a result of this we classed the risk of bias for this domain as unclear |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "Blinded photographic evaluation was conducted." Comment. whilst the main report has no discussion of blinded outcome assessment, it is mentioned in the conference abstract describing the study. However as with Armstrong 2005 we note that unblinded health professionals in 1 group were able to make decisions about undertaking closure surgery that could then have resulted more wounds being closed (and classed as healed) or amputated. As a result of this we classed the risk of bias for this domain as unclear |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: 3 participants were excluded from analysis in each arm as they did not receive the trial treatment allocated. There were relatively low numbers of exclusions, although ideally data on these participants would have been included in the RCT report. Additionally, 31% of participants in the NPWT group and 25% in the dressing group were classed as being 'discontinued' for reasons that included adverse events, ineffective treatment and also death. It is not clear whether participants who were discontinued for reasons other than death were also censored from the analysis, rather than being followed up. If discontinuation did result in censoring in this open trial it may have introduced bias |
| Other bias | Low risk | No evidence of other bias |
| Methods | 2‐arm RCT; undertaken in Turkey | |
| Participants | 67 adult participants. Inclusion criteria: diabetic foot ulcers Exclusion criteria: not reported Key baselines co‐variates: Wound area (cm2): Group A: 29.7 (SD 5.2) Group B: 35.7 (SD 6.4)
Wound duration (weeks): Group A: 8.8 (SD 7.2) Group B: 11.3 (9.2) | |
| Interventions | Group A (n = 37): conventional wound care treatment (described as daily wound care, debridement and treatment of gangrenous tissue where required and use of sterilized gauze dressing). Group B (n = 30): NPWT (VAC® system) Clinical measures included standard diabetic treatment, daily wound care including antiseptic bath, debridement, toe removal for gangrene when necessary, and wound care with conventional methods or VAC®. | |
| Outcomes | Primary outcome: time‐to‐healing Secondary outcomes: health‐related quality of life measured with SF‐36 (not clearly reported) | |
| Notes | Follow‐up: final SF‐36 form completed 1 month after wound healing (mean in 4th month of study) Outcome assessment: healing time calculated as the time from hospital admission to re‐epithelization Funding: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation of the patients was arranged by the free use web based system (http://www.tufts.edu\˜gdall/PLAN.HTM)" Comment: classed as an adequate method |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Other bias | Low risk | No evidence of other risk of bias |
| Methods | 2‐arm RCT; undertaken in India | |
| Participants | 48 participants (recruited from inpatient wards), 15 of whom were reported to have DM and a foot ulcer. Data for these 15 participants only are presented Inclusion criteria: people admitted to general surgery, physical medicine, and rehabilitation wards and referred by the surgical consultants for care of an acute or chronic extremity, sacral, or abdominal wound that could not be treated with primary closure Exlusion criteria: (1) ischaemic wounds; or wounds: (2) in anatomical locations where an adequate seal around the wound site could not be obtained; (3) with exposed bowel or blood vessels; (4) with necrotic tissue that could not be debrided; (5) with communicating fistulae; (6) with malignancy; (7) with recent grafts; or (8) presence of osteomyelitis; or (9) patient receiving therapeutic anticoagulation Key baselines co‐variates (foot ulcers in people with diabetes only): Wound area (cm2): Group A: 48.1 (SD = 53.5) Group B: 25.7 (SD = 9.7)
Wound duration (days): Group A: 5.2 (SD = 2.3) Group B: 8.5 (SD = 8.3) | |
| Interventions | Group A (n = 9): saline‐soaked gauze and dry pads used to cover the wound. Dressing changes typically performed twice daily; frequency adjusted according to the judgment of the treating physician Group B (n = 6): locally‐constructed (homemade) device: a sterilized, porous packing material obtained from a local source was cut to fit the wound. A 14‐French suction catheter was tunnelled into the packing material, which then was placed into the wound cavity. A sterile adhesive plastic drape (Dermincise, Vygon, UK) was cut to overlap the surrounding skin and applied over the packing material, forming an airtight seal. Tubing was used to attach the free end of the suction catheter to a wall suction canister. The TNP timer was placed in circuit between the wall suction apparatus and the wall suction canister The TNP timer, constructed from local electronics, was designed to cycle wall suction intermittently using a simple timed switch and a system of valves. For the study protocol, the timer was set to cycle for 2 minutes on, followed by 5 minutes off. Wall suction pressure was set at 125 mmHg. In sensitive wounds, suction was reduced to a tolerable level (usually 50 mmHg to 100 mmHg) until it could be comfortably increased. For oedematous wounds, the suction was kept on a continuous setting until oedema had been reduced and an intermittent regimen could be followed. The dressing was changed every 2 days unless otherwise scheduled by the treating physician. Wounds were debrided as required to keep the wound bed free of necrotic tissue. Patients receiving NPWT who no longer required hospitalisations for their primary diagnosis, or could not afford to remain in the hospital, remained in the study with conventional wound dressings in the outpatient setting, but outcomes were analysed in the original treatment groups Wounds in both treatment groups were debrided before dressing application | |
| Outcomes | Primary outcome: number of days to satisfactory healing, defined as complete wound closure by secondary intention or wound readiness for delayed primary closure as determined by the study investigator and treating surgeon Secondary outcomes: none reported separately for foot ulcers | |
| Notes | Participants were followed until wound closure or being lost to follow‐up for an average of 26.3 days (+/‐ 18.5) in the control and 33.1 days (+/‐ 37.3) in the treatment group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Wounds that met inclusion and exclusion criteria were assessed for size (in a manner that allowed blinding) and then block‐randomized using a concealed computer‐generated table in a 1‐to‐2 ratio of TNP closure versus conventional wound dressing." Comment: adequate method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Following enrolment, wound size was assessed using computer‐aided measurements of digital photographs and block‐randomized to the study arms using a concealed allocation table." Comment: unclear how allocation concealment was conducted |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Seems that participants were analysed in groups as randomised |
| Other bias | Unclear risk | No evidence of other risk of bias |
| Methods | 3‐arm RCT; undertaken in Croatia | |
| Participants | 27 adult participants Inclusion criteria: complicated diabetic ulcer (sic) managed to international guidelines for treatment protocol (confirmed with the author that these were all foot wounds) Key baselines co‐variates: not reported Wound duration (months): not reported | |
| Interventions | Group A (n = 8): classic gauze Group B (n = 12): moist dressings Surgical debridement, off‐loading, co‐morbidity treatment and appropriate wound care were performed | |
| Outcomes | Primary outcome: healing rate (author defined as wound closure – personal contact) | |
| Notes | Follow‐up: 2 months, extracted from abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | No evidence of other risk of bias |
Abbreviations
< = less than
> = more than
≤ = less than or equal to
≥ = more than or equal to
h = hour(s)
NPWT = negative pressure wound therapy
RCT = randomised controlled trial
SD = standard deviation
TNP = topical negative pressure (synonym for NPWT)
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Included multiple wounds types. Unable to obtain diabetic foot wound data separately | |
| Included multiple wounds types. Unable to obtain diabetic foot wound data separately | |
| No relevant outcome reported | |
| No relevant outcome reported | |
| Not an RCT, as participants allocated using alternation | |
| No relevant outcome reported | |
| Treatment with NPWT was not the only systematic difference between groups (intervention group receiving NPWT also received autologous fibroblasts and skin grafting) | |
| Not an RCT, as participants allocated using alternation. Coin flipped for first participant and then participants allocated by alternation | |
| Not a diabetic foot wound study population | |
| Included multiple wounds types. Unable to obtain diabetic foot wound data separately | |
| Included multiple wounds types. Unable to obtain diabetic foot wound data separately | |
| Included wounds in people with diabetes in regions other than the foot (legs and back). Unable to obtain diabetic foot wound data separately | |
| No relevant outcome reported |
Abbreviations
NPWT = negative pressure wound therapy
RCT = randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Not clear: could be an RCT |
| Participants | People with DM and foot ulcers n = 38 |
| Interventions | NPWT |
| Outcomes | Not clear ‐ seems to be wound dimensions |
| Notes | Requires translation from Chinese |
| Methods | RCT |
| Participants | Mixed ‐ request data for foot wound participants and further details |
| Interventions | NPWT |
| Outcomes | Requested wound healing data from authors |
| Notes |
Abbreviations
DM = diabetes mellitus
NPWT = negative pressure wound therapy
RCT = randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | RCT PICO pilot study (Smith and Nephew) |
| Methods | RCT |
| Participants | Chronic and sub‐acute wounds (some potentially foot wounds in people with DM). Planned sample size of 100 |
| Interventions | NPWT vs standard care |
| Outcomes | Time to wound closure |
| Starting date | |
| Contact information | Emma.Whatley@smith‐nephew.com |
| Notes | ISRCTN record states end date of Aug 2012. Project Manager e‐mail: "I can confirm that recruitment for the study has not yet finished and that we currently have no DFU’s in the study. We expect that this might change with the possible addition of a new site. We are hoping to have some data by the middle of next year." |
| Trial name or title | Treatment of diabetic foot wounds by Vacuum‐Assisted Closure (VAC®): A multi‐centre randomised controlled trial (KCI) |
| Methods | RCT |
| Participants | Chronic or post‐amputation wounds on the feet of people with diabetes |
| Interventions | NPWT vs conventional moist wound therapy |
| Outcomes | Time to complete healing, percentage of wounds closed, recurrence, resource use, adverse events |
| Starting date | June 2011 |
| Contact information | Ms D Seidel: doerthe.seidel@uni‐wh.de |
| Notes | End date cited as Sept 2013 |
Abbreviations
DM = diabetes mellitus
DFU = diabetic foot ulcer
NPWT = negative pressure wound therapy
RCT = randomised controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion of wounds healed Show forest plot | 2 | 503 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [1.18, 1.84] |
| Analysis 1.1  Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 1 Proportion of wounds healed. | ||||
| 2 Time to healing Show forest plot | 2 | Hazard Ratio (Fixed, 95% CI) | 1.85 [1.40, 2.45] | |
| Analysis 1.2 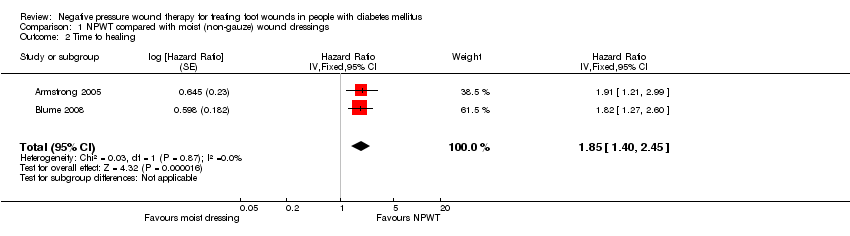 Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 2 Time to healing. | ||||
| 3 Amputations Show forest plot | 2 | 503 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.17, 0.74] |
| Analysis 1.3 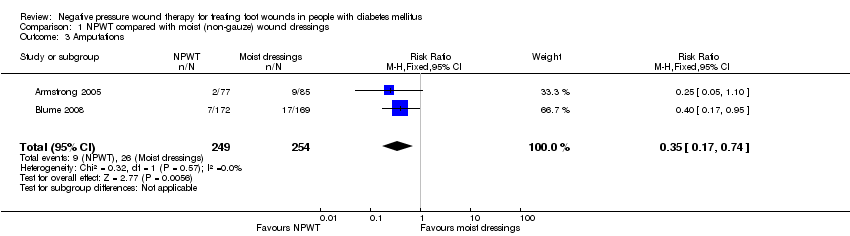 Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 3 Amputations. | ||||
| 4 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 4 Adverse events. | ||||
| 4.1 All adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Treatment‐related adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion of wounds healed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.1 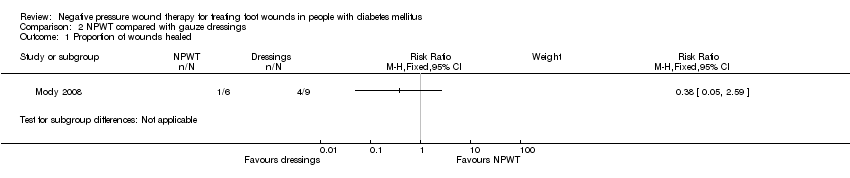 Comparison 2 NPWT compared with gauze dressings, Outcome 1 Proportion of wounds healed. | ||||

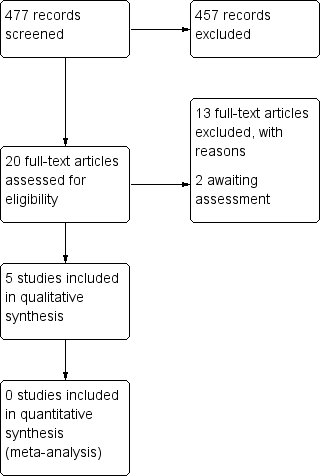
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
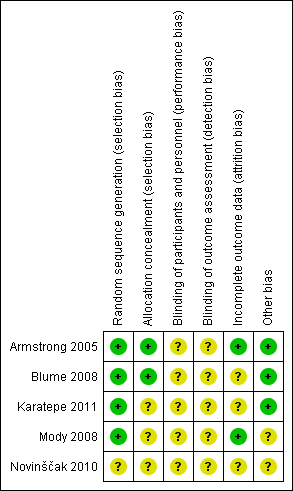
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 1 Proportion of wounds healed.
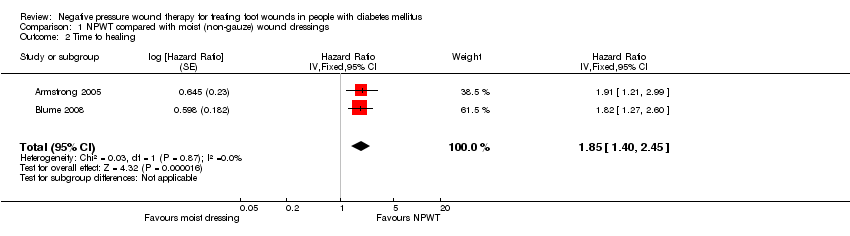
Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 2 Time to healing.
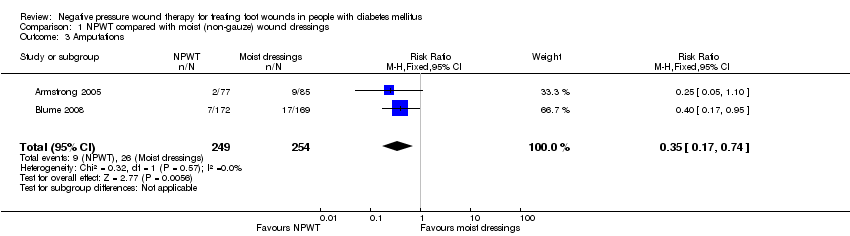
Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 3 Amputations.

Comparison 1 NPWT compared with moist (non‐gauze) wound dressings, Outcome 4 Adverse events.
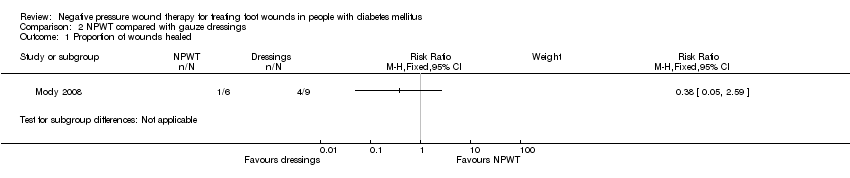
Comparison 2 NPWT compared with gauze dressings, Outcome 1 Proportion of wounds healed.
| NPWT compared to Moist dressings for healing post‐operative wounds in people with diabetes | ||||||
| Patient or population: patients with healing post‐operative wounds in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Moist dressings | NPWT | |||||
| Proportion of wounds healed | Study population | RR 1.44 | 162 | ⊕⊕⊝⊝ | ||
| 388 per 1000 | 559 per 1000 | |||||
| Moderate | ||||||
| Time to ulcer healing | Study population | HR 1.91 | 162 | ⊕⊕⊝⊝ | ||
| 388 per 1000 | 609 per 1000 | |||||
| Moderate | ||||||
| Amputation | Study population | RR 0.25 | 162 | ⊕⊝⊝⊝ | ||
| 106 per 1000 | 26 per 1000 | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 There was the potential for performance bias as unblinded health professionals were able to make decisions about undertaking closure surgery that could then have resulted more wounds being closed (and classed as healed) or amputated in one group compared with the other. | ||||||
| NPWT compared to Moist dressings for debrided foot ulcers in people with diabetes | ||||||
| Patient or population: patients with debrided foot ulcers in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Moist dressings | NPWT | |||||
| Proportion of wounds healed | Low risk of healing1 | RR 1.49 | 341 | ⊕⊕⊝⊝ | ||
| 340 per 1000 | 507 per 1000 | |||||
| Moderate risk of healing1 | ||||||
| 530 per 1000 | 790 per 1000 | |||||
| High risk of healing1 | ||||||
| 650 per 1000 | 968 per 1000 | |||||
| Time to healing | Low risk of healing4 | HR 1.82 | 341 | ⊕⊕⊝⊝ | ||
| 340 per 1000 | 531 per 1000 | |||||
| Moderate risk of healing4 | ||||||
| 530 per 1000 | 747 per 1000 | |||||
| High risk of healing4 | ||||||
| 650 per 1000 | 852 per 1000 | |||||
| Amputation | Study population | RR 0.40 | 341 | ⊕⊕⊝⊝ | ||
| 101 per 1000 | 40 per 1000 | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Baseline risk of healing obtained from external source in which data from 27,630 patients with a diabetic neuropathic foot ulcer was used to develop a simple prognostic model to predict likelihood of ulcer healing (Margolis DJ, Allen‐Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627‐31). It is important to note that given an outcome of ulcer healing, low risk refers to a low risk of healing and thus reflects the most severe patient populations. Conversely high risk refers to a high risk of healing. | ||||||
| NPWT compared to Gauze dressings for debrided foot ulcers in people with diabetes | ||||||
| Patient or population: patients with debrided foot ulcers in people with diabetes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Gauze dressings | NPWT | |||||
| Proportion of wounds healed | Low risk of healing1 | RR 0.38 | 15 | ⊕⊝⊝⊝ | ||
| 340 per 1000 | 129 per 1000 | |||||
| Moderate risk of healing1 | ||||||
| 530 per 1000 | 201 per 1000 | |||||
| High risk of healing1 | ||||||
| 650 per 1000 | 247 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Baseline risk of healing obtained from external source in which data from 27,630 patients with a diabetic neuropathic foot ulcer was used to develop a simple prognostic model to predict likelihood of ulcer healing (Margolis DJ, Allen‐Taylor L, Hoffstad O, Berlin JA. Diabetic neuropathic foot ulcers: predicting which ones will not heal. Am J Med. 2003;115:627‐31). It is important to note that given an outcome of ulcer healing, low risk refers to a low risk of healing and thus reflects the most severe patient populations. Conversely high risk refers to a high risk of healing. | ||||||
| Armstrong 2005 | 16 weeks | Diabetic foot amputation to trans‐metatarsal level | Group A: moist wound therapy with alginates, hydrocolloid, foam or hydrogel dressings (n = 85) Group B: NPWT (VAC system, dressing changes every 48 h. Treatment conducted until wound closure or completion of 112‐day assessment (n = 77) | Number of wounds completely healed Group A: 33/85 (38.8%) Group B: 43/77 (55.8%) Of healed wounds —healed by secondary intention (without primary/surgical wound closure) Group A: 25/33 (75.8%) Group B: 31/43 (72.1%) Remaining wounds were closed following surgery. Time to wound healing median time to healing Group A: 77 days (IQR 40 to 122) Group B: 56 days (IQR 26 to 92) Log rank = p = 0.005 Amputation Number of participants undergoing further amputation Group A: 9/85 (10.6%) Major = 5/Minor = 4 Group B: 2/77 (2.3%) Major = 0/Minor = 2 There was no difference noted in time to healing for acute or chronic wounds. | Adverse events Participants who had one or more adverse events Group A: 46/85 (54.1%) Group B: 40/77 (51.9%) Participants who had one or more treatment‐related adverse events Group A: 11/85 (12.9%) 5 classified as serious Group B: 9/77 (11.7%) 1 classified serious Resource use Average total cost per participant Group A: USD 36,887 Group B: USD26,972 Average total direct cost per participants for those treated for 8 weeks or longer Group A: USD 36,096 Group B: USD 27,270 Average per participant cost to achieve 100% healing Group A: USD 38,806 Group B: USD 25,954 |
| Blume 2008 | 16 weeks | Ulceration of the foot in people with diabetes | Group A: advanced moist wound therapy dressings used according to guidelines/local protocols (n = 169) Group B: NPWT (VAC system), applied according to manufacturer’s instructions. (n = 172) | Number of wounds completely healed (six participants excluded in paper as did not receive treatment, added back into denominator here) Group A: 48/169 (28.4%) Group B: 73/172 (42.4%) Proportion of wounds closed using surgery (unclear if considered part of healed group) Group A: 14/169 (8.3%) Group B: 16/172 (9.3%) Time to wound healing median time to healing Group A: could not be estimated Group B: 96 days (95% CI 75.0 to 114.0) Log rank taken as P value 0.001 Amputation Number of participants undergoing amputation* Group A: 17/169 (10.1%) Major = 4; minor = 13 Group B: 7/172 (4.1%) Major = 5; minor = 2 | Adverse events Limited data: not extracted Resource use – taken from conference abstract that we think is related to this main publication. Mean estimated total costs of inpatient services per participant Group A: USD 8570 (95%CI USD 5922 to USD 11,432) Group B: USD 5206 (95%CI USD 3172 to USD 7561) |
| Karatepe 2011 | Not specified. Last assessment one month after healing | Diabetic foot ulcers | Group A: conventional wound care treatment: based on text in report taken to be dry gauze (n = 37) Group B: NPWT (VAC system) (n = 30) | Time to healing Median time to healing Group A: 4.4 weeks Group B: 3.9 weeks Mean value presented but not extracted. No specific P value presented | Health‐related quality of life SF‐36: Data not presented. |
| Mody 2008 | Not specified: until healing or loss to follow‐up | Diabetic foot ulcers | Group A: wet‐to‐dry gauze (n = 9) Group B: locally‐constructed NPWT (n = 6) | Number of wounds completely healed By secondary intention: Group A: 1/9 (11.0%) Group B: 1/6 (16.6%) By delayed primary closure: Group A: 3/9 (33%) Group B: 0/6 (0%) | |
| Novinščak 2010 | 2 months | Complicated diabetic foot ulcers | Group A: classic gauze (n = 8) Group B: dressings (moist) (n = 12) | Healing rate (percentage with wound closure – defined by author on contact) Group A: 4/8* (50%) Group B: 9/12* (75%) Group C: * could not be calculated (90%) *Figure calculated by review author as only proportions obtained from study author |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion of wounds healed Show forest plot | 2 | 503 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [1.18, 1.84] |
| 2 Time to healing Show forest plot | 2 | Hazard Ratio (Fixed, 95% CI) | 1.85 [1.40, 2.45] | |
| 3 Amputations Show forest plot | 2 | 503 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.17, 0.74] |
| 4 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 All adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Treatment‐related adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion of wounds healed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |