Acupuncture for primary hypercholesterolaemia
Abstract
This is a protocol for a Cochrane Review (Intervention). The objectives are as follows:
To assess the effects of acupuncture for primary hypercholesterolaemia.
Background
Description of the condition
Hypercholesterolaemia is a metabolic derangement characterised by elevated levels of serum cholesterol in the blood. In 2008 the estimated global prevalence of hypercholesterolaemia amongst adults was 39%, with the highest rates in Europe (54%) and the lowest in Africa (23%). It is also noted that the prevalence rate of hypercholesterolaemia increases in accordance with the income level of the country, with the highest rates in high income countries (WHO 2011). Hypercholesterolaemia is estimated to attribute to 2.6 million deaths annually (4.5% of total annual deaths) and accounts for 29.7 million disability adjusted life years (DALYs) (2% of total DALYs) (WHO 2009).
There is currently no world‐wide standard definition of hypercholesterolaemia and definitions can vary from country to country. The American Heart Association guidelines outlined by the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation and treatment of high blood cholesterol in adults, defines hypercholesterolaemia as a total serum cholesterol level greater than or equal to 6.20 mmol/L (240 mg/dL) (NCEP 2002).
Cholesterol is transported in the blood in the form of lipoprotein particles which are categorised according to increasing density. The two main lipoproteins found within the bloodstream are low density lipoprotein (LDL) and high density lipoprotein (HDL). LDL makes up approximately 60% to 70% of total serum cholesterol (NCEP 2002) and serves to transport cholesterol to peripheral tissues (outside of the liver and intestine) and regulates de novo cholesterol synthesis within these tissues (Berg 2002). The remaining 20% to 30% of serum cholesterol is mostly made up of HDL (NCEP 2002) which binds and esterifies cholesterol released from peripheral tissues and transfers them to tissues that utilise cholesterol for steroid hormone synthesis or returns it back to the liver in the process called reverse cholesterol transport (Berg 2002). Excess LDL‐cholesterol in the blood stream is oxidated to become oxidised LDL which is then taken up by macrophages to form foam cells. These foam cells become trapped in arterial walls, forming a fatty streak which consequently gets overlaid by a layer of scar tissue, forming a fibrous plaque (Berg 2002). Unstable plaques are prone to rupture and luminal thrombosis formation which is responsible for acute coronary syndromes such as myocardial infarction, unstable angina and coronary death. Approximately 16% of cardiovascular deaths can be attributed to hypercholesterolaemia (WHO 2009).
Past studies have shown that there is a direct relationship between total serum cholesterol levels and occurrence of coronary events. Any LDL‐cholesterol level greater than 100 mg/dL appears to be atherogenic (conducive to the formation of plaques on arterial wall), with higher levels of LDL‐cholesterol corresponding to greater risks of coronary heart disease (NCEP 2002). This relationship can be shown most prominently in genetic forms of hypercholesterolaemia, such as familial hypercholesterolaemia, where advanced coronary atherosclerosis (large amounts of deposits of plaques containing cholesterol on coronary arterial walls) and premature chronic heart disease still occur despite the absence of other risk factors (Brown 1986). A LDL‐cholesterol and total serum cholesterol concentration reduction of 0.6 mmol/L is associated with a 50% reduction in risk of ischaemic heart disease in men aged 40, and a 20% reduction in men aged 70 and over. Although there is little reduction in risk in the first two years, a full reduction in ischaemic heart disease risk can be achieved within five years with similar reduction rates in women (Law 1994).
Unlike familial hypercholesterolaemia, which is caused by a genetic defect on chromosome 19, and secondary hypercholesterolaemia where other diseases such as liver dysfunction, nephrotic syndrome or endocrine disorders cause elevated levels of cholesterol, the exact mechanisms of 'primary' hypercholesterolaemia remain unclear. It has been suggested that several different causes can result in primary hypercholesterolaemia, including age and the suppression of LDL‐receptor activity due to the large consumption of cholesterol and saturated fatty acids (Vega 1991).
Description of the intervention
Current first line treatment for hypercholesterolaemia is statin therapy which involves a class of drugs that competitively inhibits HMG‐CoA reductase, the rate limiting enzyme of cholesterol synthesis. Reduced cholesterol synthesis results in up‐regulation of LDL‐receptor synthesis which increases LDL‐clearance from plasma into hepatocytes (Maron 2000). Statins are generally well tolerated with mild adverse effects that include myalgia, insomnia, gastrointestinal disturbances and rash. Major adverse effects of statin therapy include angio‐oedema (a vascular reaction characterised by dilatation and increased permeability of capillaries causing localised oedema in skin or mucosal tissue) and myositis (inflammation of voluntary muscles), however occurrences of these are rare (Rang 2007). Commonly used statin drugs include simvastatin, pravastatin, atorvastatin and lovastatin.
Acupuncture is an ancient therapeutic needling therapy originating in China many centuries ago. The first documented evidence for acupuncture can be found in the yellow emperor's classic of internal medicine dating from 100 B.C. which contains a compilation of centuries of traditions and texts. Although the precise anatomical locations of acupoints were established later, the concept of Qi and channels through which Qi flows was well established (White 2004).
In Traditional Chinese Medicine philosophy, all phenomena seen in the universe are composed of Qi. Although it is commonly translated as 'vital energy', it is more accurately described as a state between matter and energy where it can be seen as energy that is about to materialise or matter on the verge of transforming into energy. Unlike Western thinking, matter and energy were seen as a continuous state. In a physical aspect, Qi is associated with movement, activation, tension and engineering while from a psychological perspective, Qi is associated with desire, resolution, motivation and awareness of possibilities. Within the body Qi has five main functions: protection, movement, warming the body, transformation and stability (Kaptchuck 2000).
Within the body there is a system of channels whose primary function is to distribute and circulate Qi, termed Meridian channels. Each channel has a number of fixed acupoints, which when stimulated either by needling or other methods, change the flow of Qi along the channel which then affects and alters the body systems, producing a therapeutic effect (Birch 1999). Although multiple studies have been conducted to verify the physical existence of the Meridian channels, there has been little conclusive evidence to date of their existence.
Although acupuncture in its most traditional sense is defined as puncturing body acupoints with needles, it is often combined with moxibustion and other forms of stimulation. Other common forms of acupuncture include electroacupuncture which involves stimulating acupuncture points using electricity and acupressure which involves applying external pressure to the acupoints. For the purposes of this review acupuncture will be defined in a broad sense to include body needling, electroacupuncture and acupressure.
Adverse effects of the intervention
When acupuncture therapy is administered by trained physicians there are very few major adverse effects. In a study conducted by Melchart 2004 involving 97,733 patients, 7.1% had mild adverse effects due to acupuncture, with the most common effect being needling pain and haematoma. Other adverse effects associated with acupuncture include faintness, nausea and tiredness (Ernst 2001). Major adverse effects that can be caused by acupuncture therapy include pneumothorax and infection, however these are usually associated with poor training and aseptic technique (Zhang 2010). In summary, adverse effects of acupuncture therapy need to be assessed systematically before more definite conclusions can be made.
How the intervention might work
Although the exact mechanism of action by which acupuncture can reduce serum cholesterol levels is unknown, it is likely that it works by a combination of different pathways. Animal studies have shown that electroacupuncture at ST40 alters the expression of certain genes such as LXRα and CYP7α1 which are involved in cholesterol metabolism in the liver (Li 2007). Acupuncture also affects enzymatic pathways within in the body by up‐regulating of acyl‐coenzyme A oxidase 1 and 2 responsible for lipid oxidation, down‐regulating of stearoyl‐coenzyme A desaturase 1 responsible for catalysing the biosynthesis of monosaturated fatty acids (Kang 2007), and increasing β‐endorphin levels which stimulate lipolysis (Cabioğlu 2005). Acupuncture may also reduce cholesterol levels by acting on the neuroendocrine pathways such as increasing serotonin levels in the central nervous system (Wenhe 1981) and preserving satiation (Shiraishi 1995), leading to appetite suppression.
Why it is important to do this review
We are unaware of a systematic review on acupuncture for primary hypercholesterolaemia. Studies in obese participants have shown that acupuncture is an effective treatment for reducing total cholesterol (TC), LDL‐ and triglyceride (TG) serum levels (Cabioğlu 2005). Acupuncture is widely used by the general public and officially recognised by governments within Asia. Since its introduction into Western society in the 19th century, acupuncture has been slowly gaining popularity amongst the public as a ‘natural’ alternative to Western medicine. In Australia it has been estimated that approximately 9.2% of the population use acupuncture (Xue 2008). However, scepticism remains about the true therapeutic effects and mechanisms of action of acupuncture therapy especially in the West. Given that hypercholesterolaemia is a risk factor for causing cardiovascular events, there is a need for a systematic and evidence‐based evaluation of the efficacy of acupuncture therapy in the treatment of this condition.
Objectives
To assess the effects of acupuncture for primary hypercholesterolaemia.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
We will include male or female participants of any ethic origin who are 18 years or older with primary hypercholesterolaemia.
Diagnostic criteria
For this review, we will accept all definitions of hypercholesterolaemia. We will exclude patients with familial and secondary hypercholesterolaemia.
Types of interventions
Intervention
We will consider acupuncture including body needling, electroacupuncture and acupressure. We will exclude other methods of acupuncture such as surface electrodes and laser acupuncture.
Control
We will compare acupuncture to no intervention, placebo acupuncture (sham acupuncture), statin therapy and other non‐acupuncture interventions. We will exclude trials comparing different forms of acupuncture or different acupoints.
Types of outcome measures
Primary outcomes
-
Cardiovascular events (including myocardial infarction, peripheral arterial disease, angina pectoris, and stroke).
-
Serum lipid levels (including triglycerides, total cholesterol, LDL‐cholesterol, and HDL‐cholesterol).
-
Adverse effects.
Secondary outcomes
-
All‐cause mortality.
-
Health‐related quality of life (measured by a validated instrument).
-
Costs.
Timing of outcome measurement
-
Short‐term: greater than two weeks to one month (30 days).
-
Medium‐term: greater than one month to six months.
-
Long‐term: greater six months.
Summary of findings table
We will establish a 'Summary of findings' table using the following outcomes listed according to priority.
-
Cardiovascular events.
-
Health‐related quality of life.
-
All‐cause mortality.
-
Adverse effects.
-
Total serum cholesterol levels.
-
Costs.
Search methods for identification of studies
Electronic searches
We will use the following sources from inception to present time for the identification of trials.
-
The Cochrane Library.
-
MEDLINE.
-
EMBASE.
-
Chinese National Knowledge Infrastructure.
-
Chinese BioMedical Literature Database.
-
VIP database for Chinese Technical Periodicals.
-
China's important Conference Papers Database.
-
China Dissertation Database.
We will also search databases of ongoing trials (controlled‐trials.com/ with links to several databases and clinicaltrialsregister.eu/). We will provide information including trial identifier about recognised studies in the table 'Characteristics of ongoing studies' and the appendix 'matrix of study endpoints (protocol/trial documents)'. For every included study we will try to find its protocol, either in databases of ongoing trials, in publications of study designs, or both, and specify data in the appendix 'matrix of study endpoints (protocol/trial documents)'.
For detailed search strategies please see Appendix 1 (searches will not be older than six months at the moment the final review draft is checked into the Cochrane Information Management System for editorial approval). We will use PubMed's 'My NCBI' (National Center for Biotechnology Information) email alert service for identification of newly published studies using a basic search strategy (see Appendix 1).
If we detect additional key words of relevance during any of the electronic or other searches, we will modify the electronic search strategies to incorporate these terms. We will include studies published in any language.
We will send results of electronic searches to the editorial base of the Cochrane Metabolic and Endocrine Disorders Group.
Searching other resources
We will try to identify additional studies by searching the reference lists of retrieved included trials, (systematic) reviews, meta‐analyses and Health Technology Assessment reports.
Data collection and analysis
Selection of studies
To determine the studies to be assessed further, two review authors (RN, WC) will independently scan the abstract, title or both sections of every record retrieved. We will investigate all potentially relevant articles as full‐text. Where differences in opinion exist, they will be resolved by a third party (DL). If resolving disagreement is not possible, we will add the article to those 'awaiting assessment' and we will contact study authors for clarification. We will attach an adapted PRISMA (preferred reporting items for systematic reviews and meta‐analyses) flow chart of study selection (Figure 1) (Liberati 2009).
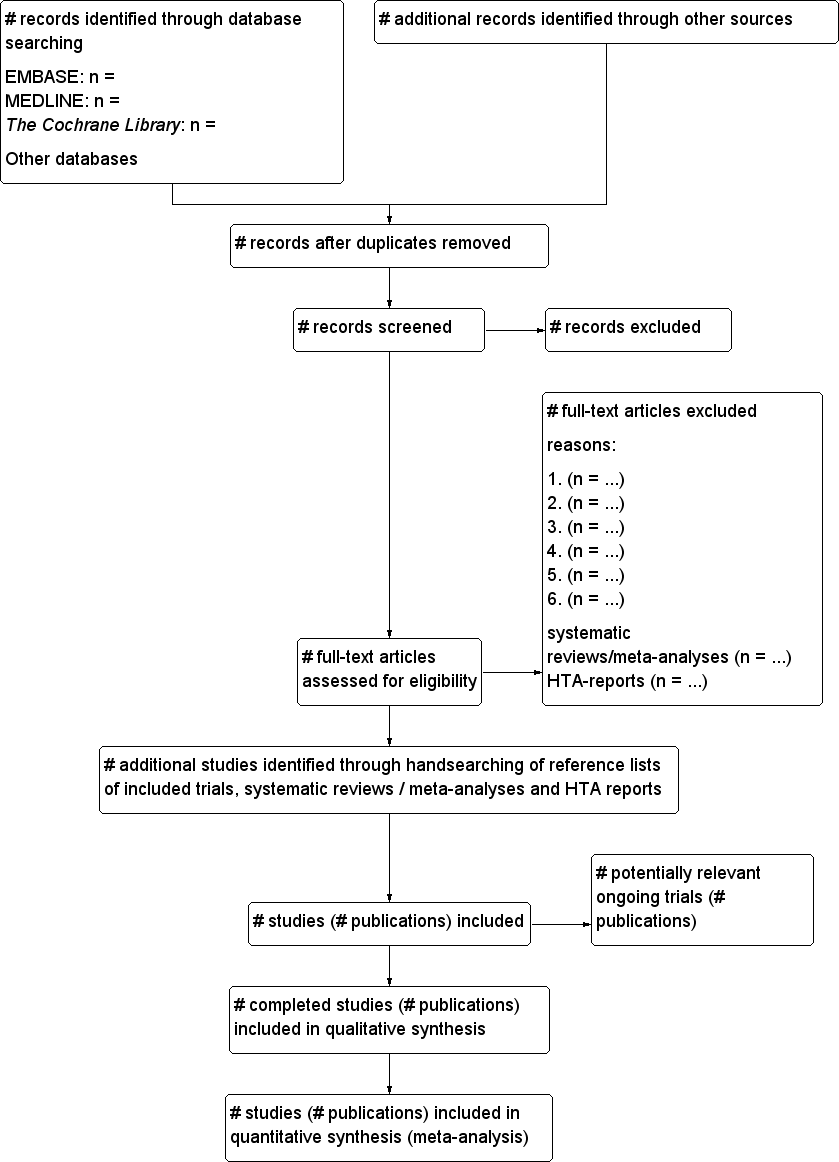
Study flow diagram.
Data extraction and management
For studies that fulfil inclusion criteria, two review authors (RN, WC) will independently abstract relevant population and intervention characteristics using standard data extraction templates (for details see Table 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6; Appendix 7; Appendix 8; Appendix 9; Appendix 10). We will resolve any disagreements by discussion, or if required by a third party.
| Characteristic Study ID | Intervention(s) and | [n] screened/eligible | [n] randomised | [n] safety | [n] ITT | [n] finishing study | [%] randomised |
| Study 1 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Study 2 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Study 3 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Study 4 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Total | All interventions | ... | ... | ||||
| All controls | ... | ... | |||||
| All interventions and controls | ... | ... | |||||
"‐" denotes not reported
ITT: intention‐to‐treat
We will extract the standards for reporting interventions in clinical trials of acupuncture (STRICTA) 2010 items of information (MacPherson 2010) for individual studies and evaluate their quality of reporting (Appendix 11).
We will send an email request to contact investigators of published studies to enquire whether they are willing to answer questions regarding their trials. We will publish the results of this survey in Appendix 12. Thereafter, we will seek relevant missing information on the trial from the original author(s) of the article, if required.
Dealing with duplicate publications and companion papers
In the case of duplicate publications and companion papers of a primary study, we will try to maximise yield of information by simultaneous evaluation of all available data.
Assessment of risk of bias in included studies
Two review authors (DL, WC) will assess each trial independently. We will resolve possible disagreements by consensus, or with consultation of a third party. In cases of disagreement, we will consult the rest of the group and make a judgement based on consensus.
We will assess risk of bias using the Cochrane Collaboration’s tool (Higgins 2011;Higgins 2011a). We will use the following bias criteria.
-
Random sequence generation (selection bias).
-
Allocation concealment (selection bias).
-
Blinding (performance bias and detection bias), separated for blinding of participants and personnel and blinding of outcome assessment.
-
Incomplete outcome data (attrition bias).
-
Selective reporting (reporting bias) ‐ see Appendix 6.
-
Other bias.
We will judge risk of bias criteria as 'low risk', 'high risk' or 'unclear risk' and evaluate individual bias items as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We will attach a 'Risk of bias' figure and a 'Risk of bias' summary figure.
We will assess the impact of individual bias domains on study results at endpoint and study levels.
For blinding of participants and personnel (performance bias), detection bias (blinding of outcome assessors) and attrition bias (incomplete outcome data) we intend to evaluate risk of bias separately for subjective and objective outcomes.
We define the following endpoints as subjective outcomes.
-
Cardiovascular events.
-
Health‐related quality of life.
-
Adverse effects.
We define the following outcomes as objective outcomes.
-
Serum lipid levels.
-
All‐cause mortality
-
Economic costs.
Measures of treatment effect
We will express dichotomous data as odds ratios (ORs) or risk ratios (RRs) with 95% confidence intervals (CIs). We will express continuous data as mean differences (MDs) with 95% CIs.
Unit of analysis issues
We will exclude cross‐over trials, cluster‐randomised trials and multiple observations for the same outcome.
Dealing with missing data
We will obtain relevant missing data from authors, if feasible, and carefully perform evaluations of important numerical data such as screened, randomised patients as well as intention‐to‐treat, as‐treated and per‐protocol populations. We will investigate attrition rates, for example, dropouts, losses to follow‐up and withdrawals, and critically appraise issues of missing data and imputation methods (e.g. last‐observation‐carried‐forward).
Assessment of heterogeneity
In the event of substantial clinical, methodological or statistical heterogeneity, we will not report study results as meta‐analytically pooled effect estimates.
We will identify heterogeneity by visual inspection of the forest plots and by using a standard Chi2 test with a significance level of α = 0.1, in view of the low power of this test. We specifically will examine heterogeneity employing the I2 statistic which quantifies inconsistency across studies to assess the impact of heterogeneity on the meta‐analysis (Higgins 2002; Higgins 2003), where an I2 statistic of 75% or more indicates a considerable level of inconsistency (Higgins 2011).
When we find heterogeneity, we will attempt to determine potential reasons for it by examining individual study and subgroup characteristics.
We expect the method of acupuncture administration to introduce clinical heterogeneity.
Assessment of reporting biases
We will use funnel plots in case we include 10 studies or more for a given outcome to assess small study effects. Owing to several possible explanations for funnel plot asymmetry we will interpret results carefully (Sterne 2011).
Data synthesis
Unless there is good evidence for homogeneous effects across studies we will primarily summarise low risk of bias data by means of a random‐effects model (Wood 2008). We will interpret random‐effects meta‐analyses with due consideration of the whole distribution of effects, ideally by presenting a prediction interval (Higgins 2009). A prediction interval specifies a predicted range for the true treatment effect in an individual study (Riley 2011). In addition, we will perform statistical analyses according to the statistical guidelines referenced in the latest version of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Subgroup analysis and investigation of heterogeneity
We will mainly carry out subgroup analyses of our primary outcome parameter(s) (see above) and investigate interaction.
We plan to conduct a subgroup analysis based on age (depending on data).
Sensitivity analysis
We will perform sensitivity analyses in order to explore the influence of the following factors on effect sizes.
-
Restricting the analysis to published studies.
-
Restricting the analysis, taking into account risk of bias, as specified above.
-
Restricting the analysis to very long or large studies to establish how much they dominate the results.
-
Restricting the analysis to studies using the following filters: diagnostic criteria, language of publication, source of funding (industry versus other), and country.
We will also test the robustness of the results by repeating the analysis using different measures of effect size (RR, OR etc.) and different statistical models (fixed‐effect and random‐effects models).
| Characteristic Study ID | Intervention(s) and | [n] screened/eligible | [n] randomised | [n] safety | [n] ITT | [n] finishing study | [%] randomised |
| Study 1 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Study 2 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Study 3 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Study 4 | intervention 1 | ||||||
| intervention 2 | |||||||
| control 1 | |||||||
| control 2 | |||||||
| total: | |||||||
| Total | All interventions | ... | ... | ||||
| All controls | ... | ... | |||||
| All interventions and controls | ... | ... | |||||
| "‐" denotes not reported ITT: intention‐to‐treat | |||||||

