انجام دیلاتاسیون متناوب توسط خود فرد در مدیریت بیماری تنگی مجرای ادرار در مردان
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع اضافی
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Full text. July 2004 ‐ June 2008. Objective: find out the role of intermittent self‐dilatation for the prevention of recurrent urethral stricture. Quasi‐randomisation: alternate allocation. Statistical methods: not described. | |
| Participants | Pakistan. 146 men with anterior urethral stricture. Age: not stated. Exclusions: posterior urethral stricture; post‐urethroplasty; stricture; unable to perform intermittent self‐dilatation; >3 strictures; stricture >4cm; obliterative urethral stricture; para‐urethral abscess; fistula. | |
| Interventions | Group A (n = 73): optical urethrotomy Group B (n = 73): optical urethrotomy then intermittent self‐dilatation for 5 months | |
| Outcomes | PROs: no Health economic: no Adverse events: no Acceptability: no Recurrence rate: Number of men with urethral stricture 8 months after optical urethrotomy. Definition of recurrence: urethrogram. Group A : 42/73 Group B: 26/73 | |
| Notes | intermittent self‐dilatation programme: daily for 4 weeks; alternate days for 4 weeks; every 3 days for 4 weeks; weekly for 8 weeks. Withdrawals: nil. Subgroups: first versus recurrent stricture; stricture length; aetiology | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: 'divided into two groups on alternate basis.' |
| Allocation concealment (selection bias) | High risk | Quote: 'divided into two groups on alternate basis.' |
| Blinding (performance bias and detection bias) | High risk | Not stated. Impossible to blind participants. Outcome assessors probably not blind. |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Funding/COI | Unclear risk | No statement. |
| Methods | Full text. Objective: find the effect of treatment of recurrent urethral stricture by optical urethrotomy followed by intermittent self‐dilatation for 3 months. States randomised; no details. Statistical methods: Chi2. | |
| Participants | Denmark. 61 men with recurrent anterior urethral stricture. Age: range 18‐87; Median: Observation 76; Intervention 70 Exclusions: prostatic urethral stricture, bladder cancer. | |
| Interventions | Observation (n = 33): optical urethrotomy Intervention (n = 28): optical urethrotomy then intermittent self‐dilatation for 3 months | |
| Outcomes | PROs: no Health economic: no Adverse events: Intervention: 2/28 urethral haemorrhage; Observation: nil reported. Acceptability: no Recurrence rate: Number of men with recurrent urethral stricture 1 year after optical urethrotomy. Definition of recurrence: flow rate < 10ml/s. Observation: 23/28 Intervention: 18/23 Time to recurrence: Median time after optical urethrotomy: Observation: 4 (range 2‐12) months Intervention: 7 (range 5‐15) months | |
| Notes | intermittent self‐dilatation programme: twice weekly for 1 month then weekly for 2 months Withdrawals: Observation: 3 death, 1 DNA Intervention: 2 bleeding, 2 death, 1 DNA Subgroups: no. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Abstract states 'randomized to undergo internal urethrotomy'; thereafter described as allocated to groups. |
| Allocation concealment (selection bias) | High risk | Probably not done. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Impossible to blind participants. Outcome assessors probably not blind. |
| Incomplete outcome data (attrition bias) | High risk | 2 men in intervention group withdrawn owing to haemorrhage should have been evaluated for recurrence. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Funding/COI | Unclear risk | No statement. |
| Methods | Full text. 1985‐89. Objective: ascertain the duration of intermittent self‐dilatation required to allow stabilization of urethral strictures following urethrotomy. Randomisation: odd/even hospital number. Statistical methods: Chi2 with Yates' correction; Wilcoxon signed rank test. | |
| Participants | UK. 101 men with recurrent urethral stricture. Age: range 24‐78, median 67. Exclusions: nil (states all men with the disease attending the department) | |
| Interventions | Group 1: optical urethrotomy then intermittent self‐dilatation for 6 months Group 2: optical urethrotomy then intermittent self‐dilatation for 3 years (intended). | |
| Outcomes | PROs: no Health economic: no Adverse events: Not stratified by group: overall: 21 death, 6 UTI, 'several' haematuria. Acceptability: No objective assessment. Quote 'most patients ... took to the procedure very easily.' Recurrence rate: Number of men with recurrent urethral stricture. Census time point unclear; follow‐up range 24‐78 months. Definition of recurrence: cystoscopy. Group 1 (6 months): 19/48 Group 2A (12‐36 months): 4/28 Group 2B (> 36 months): 0/10 Time to recurrence: no | |
| Notes | intermittent self‐dilatation programme: twice weekly for 1 month then weekly. Withdrawals: 8/21 men who died of 'unrelated disease' in the study period with insufficient follow‐up, 7 DNA (Group 1 = 3; Group 2 = 4) Protocol not followed: significant deviation from intended 36‐month programme of intermittent self‐dilatation in Group 2 owing to death, administrative error and patient preference. Subgroups: no. 10 men on permanent intermittent self‐dilatation after optical urethrotomy = zero recurrence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Odd/even hospital number. |
| Allocation concealment (selection bias) | High risk | Odd/even hospital number. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Probably not done. |
| Incomplete outcome data (attrition bias) | High risk | Number of patients withdrawn sufficient to introduce clinically relevant bias. |
| Selective reporting (reporting bias) | High risk | Narrative presentation of results; post‐hoc analysis; variable follow‐up and time point of recurrence not stated. |
| Funding/COI | Unclear risk | No statement. |
| Methods | Full text. Objective: evaluate intermittent self‐dilatation in combination with triamcinolone gel for lubrication of the catheter after optical urethrotomy. Double‐blind, placebo‐controlled trial. Randomisation: random numbers table. Statistical methods: Chi2, Student's t test. | |
| Participants | Iran. 70 male participants with urethral stricture. Age: range 10‐80; Mean: intervention 37.7; Control 34.5 Exclusions: complete urethral obstruction; stricture > 1.5 cm. | |
| Interventions | Control (n = 35): optical urethrotomy then intermittent self‐dilatation with water‐based lubricant for 6 months. Intervention (n=35): optical urethrotomy then intermittent self‐dilatation with 1 ml 1% triamcinolone gel for 6 months. | |
| Outcomes | PROs: no Health economic: no Adverse events: Not objectively reported. Metaquote: 'no febrile UTIs or complications specific to Triamcinolone.' Acceptability: No objective assessment. Quote 'all of the patients who completed the prescribed CISC program considered the method fully acceptable.' Recurrence rate: Number of men with recurrent urethral stricture 12 months after optical urethrotomy. Definition of recurrence: cystoscopy. Control: 15/34 Intervention: 9/30 P = 0.24 Time to recurrence: no | |
| Notes | intermittent self‐dilatation: daily week 1, alternate days week 2, twice weekly week 3, weekly week 4, every 2 weeks for 1 month, monthly for 3 months. Withdrawals: Control: 1 DNA Intervention: 5 DNA Subgroups: no. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Refers to random table. Probably done. |
| Allocation concealment (selection bias) | High risk | Not described. Probably not done. |
| Blinding (performance bias and detection bias) | Low risk | Quotes: 'the patient and the physicians involved in the research project were blind to the type of the lubricants' which were 'packed in similar tubes.' |
| Incomplete outcome data (attrition bias) | High risk | Imbalance in numbers across intervention groups possibly related to outcome and sufficient to introduce clinically relevant bias in intervention effect estimate. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Funding/COI | Unclear risk | No statement. |
| Methods | Full text. 1986‐2005. Objective: to answer the question 'does post‐op intermittent self‐dilatation influence long term results of optical urethrotomy?' States randomised; no details. Statistical methods: Chi2 | |
| Participants | USA. 72 men with < 1cm pendulous penile urethral stricture following hypospadias repair. Age: not stated, presumed adults, conclusion refers to follow‐up through adulthood. Exclusions: meatal or bulbar stricture. | |
| Interventions | Control: optical urethrotomy (n = 37) Intervention: optical urethrotomy then intermittent self‐dilatation for 3 months (n = 35) | |
| Outcomes | PROs: no Health economic: no Adverse events: no Acceptability: no Recurrence rate: Number of men with recurrent urethral stricture 2 years after optical urethrotomy. Definition of recurrence: re‐intervention. Control: 28/37 Intervention: 27/35 Time to recurrence: no | |
| Notes | intermittent self‐dilatation programme: daily. Withdrawals: not reported. Subgroups: type of hypospadias repair: tubularised graft, tubularised flap, onlay flap, urethral plate. Authors' conclusion: addition of intermittent self‐dilatation following optical urethrotomy has no benefit for preventing stricture recurrence [in men who have had hypospadias surgery]. Note: patients recruited over 19‐year period. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quotes: 'randomized to treatment based on 1 of 4 types of initial hypospadias repair'; 'arbitrarily assigned to treatment.' Probably not done. |
| Allocation concealment (selection bias) | High risk | Randomised according to type of hypospadias repair. Probably not done. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Impossible to blind participants. Outcome assessors probably not blind. |
| Incomplete outcome data (attrition bias) | Unclear risk | Number randomised not stated. Reports only patients that completed the study. |
| Selective reporting (reporting bias) | Unclear risk | Unclear. Presents analysis that was not pre‐specified. |
| Funding/COI | Unclear risk | No statement. |
| Methods | Full text. June 2007 ‐ June 2010. Objective: determine the role of intermittent self‐dilatation in the prevention of recurrence of urethral stricture after optical urethrotomy; study the frequency of postoperative complications and tolerability of intermittent self‐dilatation. States randomised; no details. | |
| Participants | Pakistan. 60 men with anterior urethral stricture. Age: range 20‐38; mean Control 37.3, Treatment 42.5 Exclusions: prostate or bladder cancer, inability to learn intermittent self‐dilatation. | |
| Interventions | Control: optical urethrotomy (n = 30) Treatment: optical urethrotomy then intermittent self‐dilatation for 1 year (n = 30) | |
| Outcomes | PROs: no. Health economic: no. Adverse events: Control: 3 UTI; 1 epididymitis Treatment: 4 UTI, zero epididymitis. Acceptability: no objective assessment. Quote 'All of the patients who completed the prescribed CISC program considered the method fully acceptable.' Recurrence rate: Number of men with recurrent urethral stricture 12 months after optical urethrotomy. Definition of recurrence: cystoscopy. Control: 12/26 Treatment: 4/22 P < 0.01 Time to recurrence: no | |
| Notes | intermittent self‐dilatation: twice a day for 1 week, once a day for 4 weeks, then weekly for one year. Withdrawals: Control: 4 (2 DNA, 1 emigration, 2 symptomatic declined cystoscopy) Treatment: 8 (4 DNA, 1 death, 3 unable to perform intermittent self‐dilatation) Subgroups: no. Large sections of this paper including the results are described verbatim in Kjaergaard 1994; numbers similar. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote 'randomly divided into treatment group and control group.' Insuffucient information to make judgement. |
| Allocation concealment (selection bias) | High risk | Not stated. Probably not done. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Impossible to blind participants. Outcome assessors probably not blind. |
| Incomplete outcome data (attrition bias) | High risk | Number of participants withdrawn from treatment arm enough to impact effect estimate. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Funding/COI | Unclear risk | Not stated. |
| Methods | Full text. August 1987 ‐ August 1991. Objective: investigate the effect of intermittent self‐dilatation on the prevention of urethral stricture after optical urethrotomy. States randomised. Statistical methods: Life‐table, logrank, Fisher's exact test. | |
| Participants | Denmark. 55 men with anterior urethral stricture. Age: range 28‐85 (median 68) Exclusions: prostate or bladder cancer, inability to learn intermittent self‐dilatation. | |
| Interventions | Control: optical urethrotomy (n = 24) Treatment: optical urethrotomy then intermittent self‐dilatation for 1 year (n = 31). | |
| Outcomes | PROs: no Health economic: no Adverse events: Number of men with positive urine culture or epididymitis Control: 5/22 Treatment: 1/21 P = 0.4 Acceptability: Not objectively assessed. Quote 'All of the patients who completed the prescribed CIC programme considered the method fully acceptable.' Recurrence rate: Number of men with recurrent urethral stricture 12 months after optical urethrotomy. Definition of recurrence: cystoscopy. Control: 15/22 Treatment: 4/21 P < 0.01 | |
| Notes | intermittent self‐dilatation programme: weekly. Withdrawals: Control: 2 (2 protocol violation) Treatment: 10 (4 DNA, 1 death, 1 rUTI, 4 unable to perform intermittent self‐dilatation) Subgroups: no. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation is unclear. Insufficient detail to make a judgement. |
| Allocation concealment (selection bias) | High risk | Not stated. Probably not done. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Probably not done. |
| Incomplete outcome data (attrition bias) | High risk | Number of participants withdrawn from treatment arm enough to impact effect estimate. |
| Selective reporting (reporting bias) | High risk | Pre‐stated outcomes not reported: time to recurrence; second year data. |
| Funding/COI | Unclear risk | Astra Meditec Limited, Denmark supplied LoFric catheters for this study. |
| Methods | Full text. 1989‐1991. No stated objective. States randomly allocated; no details. Statistical methods: Log rank x2 | |
| Participants | UK. 51 men with anterior urethral stricture. Age: not stated. Exlcusions: not stated. | |
| Interventions | Control: optical urethrotomy (n = 21) Treatment: optical urethrotomy then intermittent self‐dilatation for 3 months (n = 23) | |
| Outcomes | PROs: no Health economic: no Adverse events: Zero UTI intermittent self‐dilatation arm. Quote 'none developed urinary tract infections.' Acceptability: No objective assessment. Quote 'patients generally found the procedure acceptable.' Recurrence rate: Number of men with recurrent urethral stricture 12 months after optical urethrotomy. Definition of recurrence: flow rate < 12 ml/s. Control: 8/21 Treatment: 6/23 Time to recurrence: no | |
| Notes | intermittent self‐dilatation programme: twice daily for 2 weeks, daily for 3 weeks, twice weekly for 3 weeks, weekly for 4 weeks. Withdrawals: 7 (6 DNA, 1 death); not stratified by arm. Subgroups: First or recurrent stricture. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: 'Patients were randomly allocated.' No further details. |
| Allocation concealment (selection bias) | High risk | Not described. Probably not done. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Probably not done. |
| Incomplete outcome data (attrition bias) | High risk | 6/51 patients entered into the trial did not attend follow‐up, allocation unspecified. Sufficient to impact on intervention effect. |
| Selective reporting (reporting bias) | High risk | No pre‐stated objective. UTI data incompletely reported. |
| Funding/COI | Unclear risk | Not stated. |
| Methods | Full text. October 1998 ‐ June 1999. Objective: compare clean intermittent self catheterisation and urethral dilation with sounds in the management of recurrent urethral strictures. Randomised study; random number sequence generated by computer. Statistical methods: Chi2, Fisher's exact test. | |
| Participants | Kenya. 49 male patients with recurrent urethral stricture. Age: range 15‐75; mean Control 40.0, Treatment 40.7 Exclusions: none stated. | |
| Interventions | Control (Group B): dilatation with sounds at 1, 3 and 6 months (n = 22) Treatment (Group A): intermittent self‐dilatation for 6 months (n = 27) | |
| Outcomes | PROs: quality of life; non‐validated questionnaire; at 1, 3 and 6 months. Respectively: Control: 6/22, 15/17, 12/15 unhappy Treatment: 0/25, 3/25, 3/20 unhappy P = 0.01, 0.01, 0.12 Health economic: no Adverse events: No objective assessment. Quote 'higher rate of infection in the dilatation group at 3 and 6 months.' Acceptability: no. Recurrence rate: no. Flowrate: At baseline (preoperative), 1, 3 and 6 months. Respectively: Control mean: 9.9 ± 10.7, 8.2 ± 3.9, 5.4 ± 3.4, 7.7 ± 2.7 ml/s Treatment mean: 11.7 ± 10.9, 18.9 ± 9.9, 18.9 ± 9.8, 18.6 ± 11.5 ml/s P = 0.80, 0.0002, 0.0002, 0.002 | |
| Notes | intermittent self‐dilatation programme: twice daily. Withdrawals: unclear: states 13 and 10 lost to follow‐up at 3 and 6 months respectively, does not tally with results table. Subgroups: no | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number sequence generated by computer. Probably done. |
| Allocation concealment (selection bias) | High risk | Not described. Probably not done. |
| Blinding (performance bias and detection bias) | High risk | No details. Probably not done. |
| Incomplete outcome data (attrition bias) | High risk | Flowrate means and unspecified measure of dispersion given. Quality of Life (QoL) data missing for 14/49 patients at 6 months. Report states n = 10 and 13 lost to follow‐up at 3 and 6 months respectively. |
| Selective reporting (reporting bias) | High risk | Non‐specific pre‐stated objective. QoL Likert‐type scale stated in methods but not presented in results. |
| Funding/COI | Unclear risk | Not stated. |
| Methods | Full text. August 2005 ‐ February 2008. Objective: compare intermittent self‐dilatation after optical urethrotomy for urethral stricture using a low‐friction hydrophilic catheter (LoFric) or standard Nelaton polyvinyl chloride (PVC) catheter. States block randomisation. Statistical methods: Life table, log rank, Chi2. | |
| Participants | Tunisia. 62 men with anterior or posterior urethral stricture < 2cm. Age: range 21‐86; mean Control 60.9, Treatment 62 Exclusions: prostate or bladder cancer, patients requiring antibiotic prophylaxis, need for CISC for bladder drainage, incapable of following study protocol. | |
| Interventions | Control: optical urethrotomy then intermittent self‐dilatation with Nelaton catheter (n = 31). Treatment: optical urethrotomy then intermittent self‐dilatation with LoFric catheter (n = 31). | |
| Outcomes | PROs: Ease of use after 6 catheter insertions: 5‐item VAS non‐validated questionnaire (trouble, convenience, pain, comfort, general opinion). Mean pain, comfort and opinion scores favoured LoFric; trouble and convenience NS. Health economic: no Adverse events: Control: 7 (1 prostatitis, 2 bleeding, 4 positive urine culture) Treatment: 1 positive urine culture Acceptability: Number of men who considered the treatment acceptable. Means of assessment of acceptability to patients not described. Control: 7/28 Treatment 30/31 Recurrence rate: Definition of recurrence: flow rate < 14 ml/s Number of men with recurrent urethral stricture 2 years after optical urethrotomy. Control: 7/28 Treatment: 2/31 P = 0.15 Time to recurrence: no. | |
| Notes | intermittent self‐dilatation programme: twice monthly for 3 months then monthly for 1 year Witdrawals: n = 3 Nelaton arm (1 DNA, 2 rUTI). Authors conclude: LoFric catheter significantly increased the degree of comfort and satisfaction and decreased the feeling of pain when the catheter was removed or inserted, when compared with a conventional PVC catheter. Note: Results state only 10/31 in treatment arm able to perform intermittent self‐dilatation at home without problems. Subgroups: no. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States block randomisation. No further details. |
| Allocation concealment (selection bias) | High risk | Not stated. Probably not done. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Probably not done. |
| Incomplete outcome data (attrition bias) | Unclear risk | 3 control group patients withdrawn (2 UTI, 1 DNA); none from the treatment group. |
| Selective reporting (reporting bias) | High risk | Time to first recurrence analysis stated in Methods but not reported in Results. Results conflict with statement that only 10/31 in treatment arm able to perform intermittent self‐dilatation at home without problems. |
| Funding/COI | Unclear risk | Not stated. |
| Methods | Full text. Objective: compare the effect of treatment of urethral stricture by optical urethrotomy followed by intermittent self‐dilatation for 6 versus 12 months. Randomised study; method of randomisation not described. Statistical methods: Student's t test, Chi2. | |
| Participants | Finland. 49 men with recurrent urethral stricture. Age: mean Group A 58, Group B 62 Exlcusions: prostate or bladder cancer, scarred prostatic urethra; inadequate vision, dexterity, mental capacity. | |
| Interventions | Group A: optical urethrotomy and intermittent self‐dilatation for 12 months (n = 24). Group B: optical urethrotomy and intermittent self‐dilatation for 6 months (n = 25). | |
| Outcomes | PROs: no. Health economic: no. Adverse events: Asymptomatic bacteruria n = 10/48 Symptomatic bacteruria n = 2/48 Acceptability: 1/48 unable to perform intermittent self‐dilatation. Recurrence rate: Number of men with recurrent urethral stricture 1 year after optical urethrotomy Definition of recurrence: need for further treatment. Group A: 3/24 Group B: 2/24 All recurrences occurred > 6 months therefore number of men with recurrent urethral stricture 6 months ‐ 1 year after optical urethrotomy: Group A (intermittent self‐dilatation): 3/24 Group B (no intermittent self‐dilatation): 2/24 Flowrate: 3, 6, 9 and 12 months after optical urethrotomy. Group A mean: 18 ± 7, 17 ± 9, 17 ± 3, 18 ± 6 ml/s Group B mean: 17 ± 6, 17 ± 7, 14 ± 7, 12.5 ± 3 ml/s At 12 months p < 0.05 | |
| Notes | intermittent self‐dilatation: twice weekly for 1 month then weekly. Withdrawals: n = 1 (Group B) unable to perform intermittent self‐dilatation at home. Subgroups: no. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States randomised into 2 groups. No further details. |
| Allocation concealment (selection bias) | High risk | Not stated. Probably not done. |
| Blinding (performance bias and detection bias) | High risk | Not stated. Probably not done. |
| Incomplete outcome data (attrition bias) | Unclear risk | Means and SD presented only. |
| Selective reporting (reporting bias) | Low risk | Expected outcomes reported. |
| Funding/COI | Unclear risk | Not stated. |
Abbreviations
CISC clean intermittent self‐catherisation
CONSORT Consolidated Standards of Reporting Trials
DNA did not attend
ISD intermittent self‐dilatation
LUTS lower urinary tract symptoms
NS Not statistically‐significant
PRO patient‐reported outcome
PROM patient‐reported outcome measure
PVC polyvinyl chloride
QALY quality‐adjusted life year
QoL quality of life
rUTI recurrent urinary tract infection
VAS visual analogue scale
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Full text. Evaluates technique called 'hydraulic self‐dilatation' (manual occlusion of the meatus during voiding) following optical urethrotomy. Not intermittent self‐dilatation. | |
| Abstract only. Full text sought from author and publisher and not available. Probably observational case series of optical urethrotomy plus intermittent self‐dilatation. Probably non‐randomised study. | |
| Abstract only. Full text sought from author and publisher and not available. Evaluates optical urethrotomy versus optical urethrotomy then intermittent self‐dilatation. Described as comparative cross‐sectional study. Participants 'divided into groups.' Probably non‐randomised study. | |
| Full text. Optical urethrotomy alone versus serial urethral dilatation performed by a surgeon. Not intermittent self‐dilatation. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrent urethral stricture Show forest plot | 6 | 404 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.48, 1.00] |
| Analysis 1.1  Comparison 1 ISD versus no treatment, Outcome 1 Recurrent urethral stricture. | ||||
| 2 Adverse events Show forest plot | 2 | 91 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.11, 3.26] |
| Analysis 1.2  Comparison 1 ISD versus no treatment, Outcome 2 Adverse events. | ||||
| 2.1 Urinary tract infection/bacteriuria | 2 | 91 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.11, 3.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrent urethral stricture Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 One programme of ISD versus another, Outcome 1 Recurrent urethral stricture. | ||||
| 1.1 Short duration versus long duration of treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrent urethral stricture (type of catheter) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 One device for ISD versus another, Outcome 1 Recurrent urethral stricture (type of catheter). | ||||
| 1.1 LoFric vs PVC | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Recurrent urethral stricture (catheter lubrication) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 3.2  Comparison 3 One device for ISD versus another, Outcome 2 Recurrent urethral stricture (catheter lubrication). | ||||
| 2.1 Triamcinolone gel versus water‐based lubricant | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 3.3 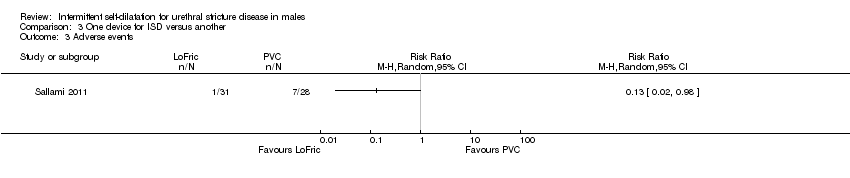 Comparison 3 One device for ISD versus another, Outcome 3 Adverse events. | ||||
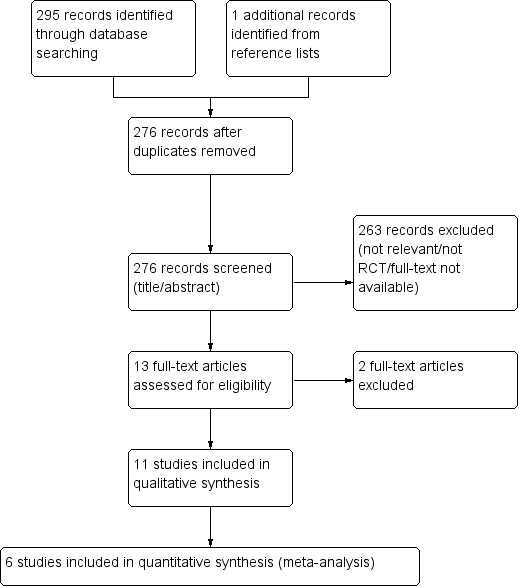
PRISMA study flow diagram
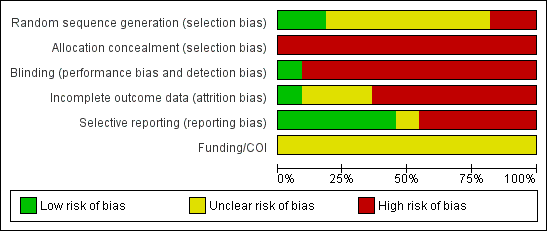
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
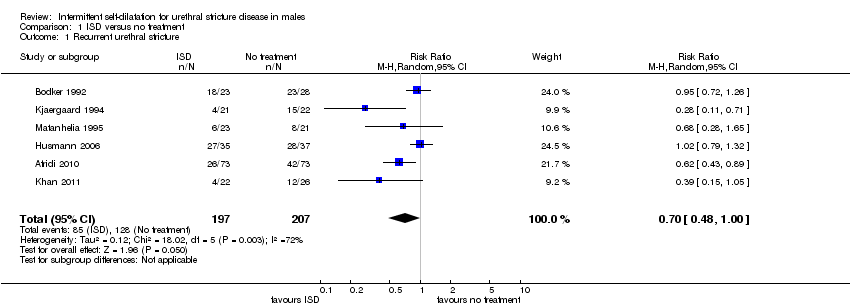
Comparison 1 ISD versus no treatment, Outcome 1 Recurrent urethral stricture.
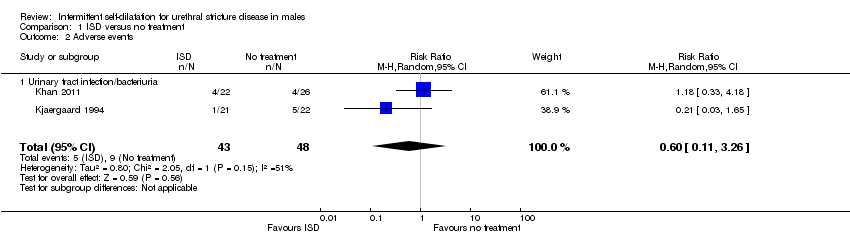
Comparison 1 ISD versus no treatment, Outcome 2 Adverse events.
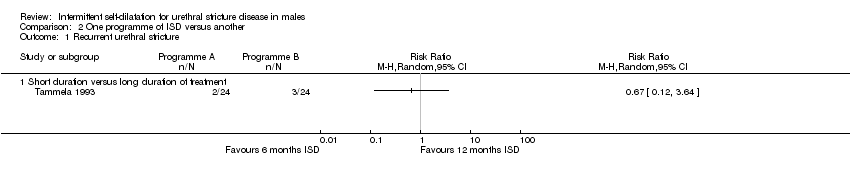
Comparison 2 One programme of ISD versus another, Outcome 1 Recurrent urethral stricture.
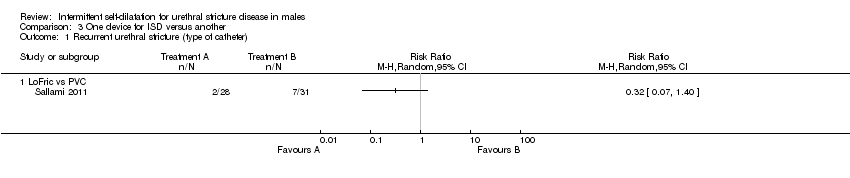
Comparison 3 One device for ISD versus another, Outcome 1 Recurrent urethral stricture (type of catheter).

Comparison 3 One device for ISD versus another, Outcome 2 Recurrent urethral stricture (catheter lubrication).
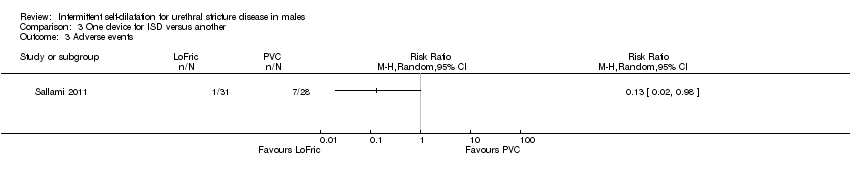
Comparison 3 One device for ISD versus another, Outcome 3 Adverse events.
| Intermittent self‐dilatation compared to no treatment for males after urethral stricture surgery | ||||||
| Population: males after urethral stricture surgery | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No treatment | Intermittent self‐dilatation | |||||
| Recurrent urethral stricture | 618 per 1000 | 433 per 1000 | RR 0.7 | 404 | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by two for risk of bias: all six trials comprising the quantitative synthesis were judged high risk of bias in two or more domains. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrent urethral stricture Show forest plot | 6 | 404 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.48, 1.00] |
| 2 Adverse events Show forest plot | 2 | 91 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.11, 3.26] |
| 2.1 Urinary tract infection/bacteriuria | 2 | 91 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.11, 3.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrent urethral stricture Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Short duration versus long duration of treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recurrent urethral stricture (type of catheter) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 LoFric vs PVC | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Recurrent urethral stricture (catheter lubrication) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Triamcinolone gel versus water‐based lubricant | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |

