Školski edukativni programi za prevenciju nenamjernih ozljeda kod djece i mladih
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | CBA | |
| Participants | School children in grades kindergarten to grade 5 and their families in Muskogee, Oklahoma from private and state schools located in both rural and urban settings. Number of participants: not reported. 4750 observations of children's behaviour were made and 6300 pre‐ and postintervention questionnaires were distributed. | |
| Interventions | Intervention: 18 or 27 lesson curricula stratified by grade (30‐ to 45‐minute sessions). Smoke alarm giveaway. School cycle fairs with helmet giveaways. Safety pen pal letters. Letters to parents. Injury prevention talks at parent‐teacher meetings. Control: no injury prevention curriculum. Opportunity for smoke alarm to be installed. | |
| Outcomes | Observed seat‐belt use of occupants in the front seat of a vehicle and cycle helmet use during and 2 weeks after the intervention. Self‐reported behaviour, including driver and passenger seat‐belt use and cycle helmet use. Safety knowledge measured using written questions for children in kindergarten to grade 1, and true or false and multiple choice questionnaire for children in grades 2 and 3 and grades 4 and 5. | |
| Injury mechanisms | Vehicle safety; smoke alarms and fire; cycle safety helmet use; brain and spinal cord injuries; home safety; pedestrian safety; first aid; traffic signs and signals; intersections and railroad crossings; water safety. | |
| Notes | Did not present the characteristics of the control and intervention groups. Measurement of observed seat‐belt use 3 months' post‐intervention did not occur as many of the students had emigrated or immigrated, leading to a change in the population. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | High risk | Schools chose to be in the intervention group. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐reported outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Number allocated at baseline not reported. |
| Selective reporting (reporting bias) | High risk | Seat‐belt use outcome reported incompletely. |
| Other bias | Unclear risk | No baseline data presented. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | High risk | Did not adjust for confounding. Pre‐programme, more control school pupils used seat belts. |
| Methods | CBA | |
| Participants | Children in year 9 of high school (95% were aged 13 to 14 years) from schools in an urban deprived area of Queensland, Australia. Number of participants: 360 students in the intervention group (97% of all eligible students) and 180 students (45% of all eligible students) in the control group. | |
| Interventions | Intervention: SPIY programme. teacher training, a teacher's manual and student workbook for 8 lessons carried out in the school. Each lesson lasted 50 minutes, and included presentations of risk‐taking and injury scenarios, introduction to first aid and cognitive behavioural activities to prevent the risk‐taking behaviour, including protecting friends. Control: usual curriculum. The SPIY programme was made available after the study. | |
| Outcomes | Self‐reported risk behaviour measured using the Australian Self‐Report Delinquency Scale, 2 weeks postintervention. | |
| Injury mechanisms | Poisoning; road traffic accidents: cars, cycles, motorbike, pedestrian. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | High risk | Schools selected which group they wanted to be in (intervention vs control). |
| Blinding of participants and personnel (performance bias) | High risk | Parents were sent information that an evaluation of an injury prevention programme was taking place. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐reported outcomes, high risk of allocations being detected. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition was > 20% as the analyses were only based on children with complete before‐and‐after data. |
| Selective reporting (reporting bias) | Unclear risk | The authors only reported data for children with before‐and‐after data. |
| Other bias | High risk | The study did not take into account clustering effects. Only 45% of control group children were included (197 children) compared to 97% of the intervention group, indicating a differential selection bias. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Unclear risk | Although groups had similar sociodemographic factors, because schools self‐selected which groups they were in there could have been some residual confounding. |
| Methods | RCT | |
| Participants | Children aged 11 to 16 years and parents with a Hispanic background, attending state‐based high schools in US. Number of participants: 293 students in the intervention group and 367 in the intervention group. | |
| Interventions | Intervention: first aid and home safety educational programme. Focus was on responding to emergency situations and the prevention of injuries. This included household safety, giving emergency care, controlling bleeding and treating burns. Involved 8 sessions over a 7‐ to 10‐week period, including homework. Each session lasted 2 hours. Control: tobacco and alcohol prevention programme delivered over a 7‐ to 10‐week period by teachers. This included refusal skills, health effects of smoking and peer pressure. Each session lasted 2 hours, with homework for children to take away. | |
| Outcomes | Proportion of adolescents who reported that their household had made home safety behaviour change, including practicing a fire escape plan, 1 year after the intervention. | |
| Injury mechanisms | First aid; smoke, fire and flames; heat/hot surfaces; sport/physical activity; household safety; poisoning. | |
| Notes | Sex of children was balanced between groups. 67% of respondents reported low income, 3 children under the age of 18 years, and were classified as very Mexican orientated on Acculturation Scale for Mexican Americans (ARSMA) scale. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, but no further information provided. |
| Allocation concealment (selection bias) | Unclear risk | Not applicable ‐ non‐randomised study. |
| Blinding of participants and personnel (performance bias) | High risk | Not possible to blind participants. |
| Blinding of outcome assessment (detection bias) | Low risk | Evaluation staff blinded to condition. Self‐reported outcome measures. |
| Incomplete outcome data (attrition bias) | High risk | Attrition was > 20% for the behavioural skills testing outcomes. Intention‐to‐treat analysis unclear as not mentioned. |
| Selective reporting (reporting bias) | Unclear risk | Report most outcomes, but home safety behaviour changes are not all reported. |
| Other bias | Low risk | No baseline data for home safety behaviours, but groups were otherwise similar. |
| Methods | RCT | |
| Participants | School children aged 10 to 14 years in state‐based primary schools in a city in Israel. Number of participants: 308 students in the intervention group and 254 students in the control group. | |
| Interventions | Intervention: schools delivered a targeted burn prevention programme developed by a plastic surgery research unit in Beer‐Sheva, Israel. The programme aimed to raise awareness, increase knowledge, and change attitudes and behaviour related to burn prevention. Multi‐methods of teaching were used including: a slide set, home checklist, set of photographs and colouring book. Control: no intervention. | |
| Outcomes | Safety knowledge was tested using a questionnaire immediately post and 10 weeks following the intervention. | |
| Injury mechanisms | Burn injuries. | |
| Notes | Groups appeared balanced for baseline characteristics following randomisation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, but no further information about how it was done. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make a judgement. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding or any attempt to conceal allocation (not possible to blind participants). |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not clear how test results were marked. |
| Incomplete outcome data (attrition bias) | High risk | High attrition bias as outcome data were based on < 80% of original sample. |
| Selective reporting (reporting bias) | High risk | Did not report parents' outcomes, which was 1 of the study objectives. |
| Other bias | Unclear risk | Did not use cluster level analyses. Did not adequately explain scoring system. |
| Methods | RCT | |
| Participants | Boys and girls aged 13 to 14 years attending school in Australia. Number of participants: 77 students in the intervention group and 196 students in the control group. | |
| Interventions | Intervention: a risk and injury prevention curriculum for adolescents, involving 8 sessions lasting 50 minutes, delivered weekly. Students were presented with risk‐taking injury scenarios, incorporating multiple activities including role plays and discussion. The sessions utilised cognitive behavioural change principles. Control: no intervention. | |
| Outcomes | Proportion of children with a self‐reported transport injury over a 3‐month period was measured using the Extended Adolescent Injury Checklist (Chapman 2011) 6 months following the intervention. | |
| Injury mechanisms | Cycle, motor cycle, motor vehicle. | |
| Notes | Sex of children differed slightly between groups at baseline (46% male in control group, 56% male in intervention group), but were similar at follow‐up (50% male in control group, 51% male in intervention group). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | States 'randomly assigned' but no detail of randomisation method given. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information given about allocation process. |
| Blinding of participants and personnel (performance bias) | High risk | Not possible to conceal allocation due to study design. Participants aware that they were in intervention group. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details given regarding how the questionnaires used to collect self‐reported outcomes were assessed, or if those marking were masked. |
| Incomplete outcome data (attrition bias) | Unclear risk | Study did not address incomplete outcome data. Response rate with active parental consent was similar across baseline and follow‐up groups. Intention‐to‐treat analysis was not mentioned. |
| Selective reporting (reporting bias) | Unclear risk | No protocol described. |
| Other bias | High risk | Only students whose parents signed consent forms for children to participate in the programme were included. |
| Methods | RCT (clustered) | |
| Participants | Primary school children aged 10 to 12 years from state‐based schools in urban and suburban areas of the Netherlands. Number of participants: 1117 students in the intervention group and 1091 students in the control group. | |
| Interventions | Intervention: the I‐Play programme consisted of 2 PE lessons per week over an 8‐month period delivered by a teacher. Children received 5 minutes of exercises at the beginning and end of lessons. Parents and children received monthly newsletters for 8 months and were offered access to a website developed by the programme. Control: received usual PE classes. | |
| Outcomes | Rate of physical activity injury measured by weekly self‐reporting. Self‐reported behaviour and safety practices (wearing protective equipment during organised sport and leisure activities and appropriate footwear during PE) measured by 5‐point Likert scale at 8 months. Safety knowledge of injury prevention measured by multiple choice questions at the 8‐month follow‐up only. | |
| Injury mechanisms | Sports/physical activity injuries. | |
| Notes | Age and sex of children were balanced at baseline. BMI higher in the control group. Number of children from low socioeconomic group was higher in the intervention group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information given to make a judgement. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information given to make a judgement. |
| Blinding of participants and personnel (performance bias) | High risk | Not possible to blind participants or people delivering the intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No detail of who assessed or marked test papers. |
| Incomplete outcome data (attrition bias) | Low risk | Good retention of participants. Potential bias due to exclusion of social modelling from analysis (but not included in this review). Intention‐to‐treat analysis was carried out. |
| Selective reporting (reporting bias) | Low risk | Appeared to report all outcomes measured, but no protocol available. |
| Other bias | Low risk | No sample size calculation available, did not report intraclass correlation coefficient. |
| Methods | Non‐RCT | |
| Participants | Boys and girls in grades 3 to 6 (aged 8 to 12 years). Participants were classmates of 1 of 6 injured children who had been admitted into hospital. Number of participants: 206 students in the intervention group and 306 students in the control group. | |
| Interventions | Intervention: aim was to help injured children with the transition from hospital back to school. Single session whereby an injured child attended a class presentation and interacted with classmates. A nurse then gave a presentation on injury occurrence and prevention, and this involved discussions, short videos and written materials. Following on from this, each child received an injury prevention workbook, educational hand‐outs, pencils and stickers. Control 1: safety education using the injured child's injury scenario, as well as educational interventions. Control 2: no presentation. Children had to complete 2 tests in injury prevention and anatomy and did not receive any safety education. | |
| Outcomes | Safety knowledge measured using specially developed multiple choice questions, administered immediately postintervention and at 1‐month follow‐up. | |
| Injury mechanisms | Motor vehicle, cycle, pedestrian. | |
| Notes | Control schools were matched to intervention schools by grade, ethnic composition, type of school and socioeconomic status of the injured child. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | High risk | Intervention schools were selected by identifying injured children. There was no mention of how control schools were identified. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding. |
| Blinding of outcome assessment (detection bias) | High risk | Teachers read out the questions. |
| Incomplete outcome data (attrition bias) | Unclear risk | No numbers provided at baseline. |
| Selective reporting (reporting bias) | Unclear risk | Unclear how the outcomes reported in conclusion section were ascertained. |
| Other bias | Unclear risk | No baseline data presented. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Low risk | Control schools were matched to intervention schools by grade, ethnic composition, type of school and socioeconomic status of the injured child. |
| Methods | RCT | |
| Participants | 1049 children from state and public schools who were in the second year of high school (mean age 16 years) from an urban area in Brazil. Number of participants: 572 students in the intervention group and 477 students in the control group. | |
| Interventions | Intervention: 'Think Well' (English translation) project, inspired by 'Think First'. Intervention lasted 60 minutes and was conducted by researchers trained by the research co‐ordinator, and included a video of injured young people discussing their accident and its impact and a brain and spinal cord trauma prevention lecture (basic neuroanatomy, age‐related risks, main causes of neurotrauma, general guidelines to prevent neurotrauma). Control: no intervention. | |
| Outcomes | Self‐reported behaviour and practices, plus safety knowledge assessed using a test instrument specially developed by the Neurology and Neurosurgery Multidisciplinary Academic League at the University of Caxias do Sul, administered 1 week and 5 months following intervention. | |
| Injury mechanisms | Traumatic brain and spinal cord injuries: swimming, cycle, motorcycle, falls. | |
| Notes | Sex and age of children did not differ between groups at baseline. Significantly more children in the intervention group had ridden a cycle and had skateboarded/rollerbladed (75.8% had ridden a cycle vs 40.6% had skateboarded/rollerbladed) than in the control group (66.8% had ridden a cycle and 27% had skateboarded/rollerbladed). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. States "controlled and randomised study" only. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information given to make a judgement. |
| Blinding of participants and personnel (performance bias) | High risk | It was not possible to blind participants. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Does not describe how tests were marked. |
| Incomplete outcome data (attrition bias) | High risk | Only students who gave consent and with complete data at baseline where included. Attrition was high in both the intervention and control group. Intervention: 1053 number allocated, at baseline = 572, 1 week = 547, 5 months = 513. Control: 1051 number allocated, at baseline = 477, 1 week = 436, 5 months = 416. Intention‐to‐treat analysis unclear as not mentioned. |
| Selective reporting (reporting bias) | High risk | ≥ 1 outcomes of interest in the review were reported incompletely so they could not be entered in a meta‐analysis: knowledge scores were presented in a graph with no specific data provided. |
| Other bias | Low risk | Did not appear to be at risk of other bias. |
| Methods | CBA | |
| Participants | 1292 children aged between 10 and 11 years from Oxfordshire UK. Number of participants: 657 students in the intervention group and 635 students in the control group. | |
| Interventions | Intervention: IMPS. Teachers were given a resource pack, available for 1 academic year, which covered basic life support training, interactional videos illustrating a range of accidents such as burns and how to respond. This was then followed by a hospital visit, whereby children were given a tour of the accident and emergency department by IMPS trainers. Control: schools with no prior exposure to IMPS. Normal curriculum. | |
| Outcomes | Safety knowledge assessed using a specially developed quiz 5 months after the intervention. A hypothetical basic life support scenario was used to measure observed safety skills and behaviour retained after the intervention. Self‐reported behaviour and safety practices assessed using a validated 'draw and write' test. | |
| Injury mechanisms | Road safety, accidents in the home, fire, electricity, poisons, waterways. | |
| Notes | Control schools were matched on location, size and Standard Assessment Test results. Intervention schools were those that were already enrolled in the IMPS programme. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | High risk | Schools self‐selected an intervention. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding. |
| Blinding of outcome assessment (detection bias) | High risk | For observed outcomes, the trainers were unblinded. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition was < 20% for all outcomes and in both intervention and control groups. |
| Selective reporting (reporting bias) | Unclear risk | Some inconsistencies in the reporting of findings (e.g. between tables and the text). |
| Other bias | Unclear risk | Tables comparing the characteristics of schools were not included. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Low risk | Control schools were matched on location, size and Standard Assessment Test results. |
| Methods | RCT | |
| Participants | School children in grade 3 and 4 in state‐based primary schools in the US. Number of participants: 1187 students in the intervention group and 730 students in the control group. | |
| Interventions | Intervention: schools delivered the 'Learn Not to Burn' curriculum, which was developed by a collaboration of fire protection organisations and a burn centre in North Carolina. The programme was based upon 22 key behaviours for burn prevention, but no other details of the programme or teaching methods were described. Control: schools used "other methods of fire safety education" (not described) or "no established fire safety curriculum". | |
| Outcomes | Students' knowledge of burn prevention assessed using a test administered at the end of the academic year following intervention. | |
| Injury mechanisms | Burn‐related injuries and deaths. | |
| Notes | No characteristics of participants presented to enable judgement on how well balanced groups were. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | States 'randomly drawn' and 'stratified random sample' but no description of sequence generation or process. No baseline characteristics presented to enable judgement regarding success of randomisation. 1 set of analyses included data volunteered by schools not included in randomisation process. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information about allocation process given. No mention of allocation concealment. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding or any attempt to conceal allocation (not possible to blind participants). |
| Blinding of outcome assessment (detection bias) | High risk | Stated "tests were graded by the teachers in the study schools". Possible that marking could have been biased. |
| Incomplete outcome data (attrition bias) | High risk | Incomplete data occurred due to test scores not received from schools (higher in control group), and incorrect tests used. Districts that changed group were correctly excluded. |
| Selective reporting (reporting bias) | High risk | No protocol described. Outcomes not reported completely. |
| Other bias | High risk | Misclassification bias is possible due to control districts using similar burn prevention curriculum to the Learn Not to Burn. Additional data were included from schools not originally included in the study sample, although these are reported separately. |
| Methods | CBA | |
| Participants | 1400 children from 64 classrooms (grades 1 to 3) in the US. Number of participants: 735 students in the intervention group and 665 students in the control group. | |
| Interventions | Reporting Phase III of the Think First For Kids curriculum. Only children were the recipients of the intervention, which was carried out by teachers within schools. Intervention: Think First For Kids programme. 6‐week, 6‐subject curriculum was integrated into the usual school curriculum. The units looked at the structure and function of the brain and spinal cord; road traffic safety (e.g. motor vehicle safety); conflict resolution; and water, sports, playground and recreational safety. There were 3 intervention groups (for the 3 grades). Control: no intervention. | |
| Outcomes | Safety knowledge (brain and spinal cord injury, water safety, cycle safety, motor vehicle/pedestrian safety and playground/sports safety) assessed using questions designed to measure the effectiveness of the programme 1 week after the intervention. | |
| Injury mechanisms | Brain and spinal cord injuries: motorcycle injuries; pedestrian injuries; cycle safety; conflict resolution and weapon's safety; water safety; playground, recreation and sports safety. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | Unclear risk | Not report. |
| Blinding of participants and personnel (performance bias) | High risk | Insufficient information provided about the blinding process. Participants were likely to know that they received the intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information provided about the blinding process. |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information about the missing outcome data. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information about the outcome reporting to determine risk. |
| Other bias | Unclear risk | May be risk of bias but there was insufficient information to assess whether an important risk of bias existed. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Unclear risk | No baseline data provided to enable a comparison of the groups. |
| Methods | RCT | |
| Participants | Participants were elementary children in grades 1, 2 and 3 and their parents, from 2 urban areas in San Diego County (US). Number of participants: 1126 students in the intervention group and 851 students in the control group. | |
| Interventions | Intervention: Think First For Kids programme. Children had 6 contacts, each lasting 35‐40 minutes, over a 6‐week period. There were 6 modules involving a range of video, a spinal cord speaker, hands on interactive teaching, maths, visual reinforcement and discussion. The intervention was delivered by teachers, district nurse, life skills educators as well as an external speaker/brain and spinal cord patient as well as input from parents in the form of parental support with a homework component. Control: unclear. | |
| Outcomes | Self‐reported behaviour and safety skills and safety knowledge assessed using forced choice format questionnaires, 10 days following intervention. | |
| Injury mechanisms | Brain and spinal cord injuries: violence and weapons safety; playground, recreation and sports safety; cycle safety; water safety; vehicle safety. | |
| Notes | Intervention and control schools were matched on district, socioeconomic status, school‐defined reading scores and race/ethnic composition. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided about the randomisation process. |
| Allocation concealment (selection bias) | Unclear risk | No information provided about the allocation process to determine if low or high risk, although children were matched on district, socioeconomic status, reading scores and ethnicity in the school. |
| Blinding of participants and personnel (performance bias) | High risk | Not described. Participants were likely to know that they had received the intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient information provided about the blinding process. |
| Incomplete outcome data (attrition bias) | Unclear risk | Post‐test results could not be matched for 20% of students, though the paper did not report whether these were control or intervention students. Intention‐to‐treat analysis not mentioned. |
| Selective reporting (reporting bias) | High risk | The authors did not separate out behaviour and knowledge outcomes and did not report the module scores. |
| Other bias | Low risk | Did not appear to be at risk of other bias. |
| Methods | RCT (clustered) Allocation occurred at the school level, with schools divided into 3 groups based on the proportion of children who were receiving free meals (representing deprivation). Using these 3 groups, schools were then randomly allocated to the intervention and control groups. | |
| Participants | Children were aged 7 to 10 years (in years 3, 4 and 5) and were from state‐funded primary schools in the UK. Number of participants: 240 students in the intervention group and 219 students in the control group. | |
| Interventions | Intervention: 'Risk Watch' programme. Teachers were trained by fire service personnel and received 'Risky boxes' containing background information, lesson plans and activities for pupils. The boxes were age‐specific (1 box for years 3 and 4, and 1 box for year 5). Participating schools had to teach at least 1 of 4 injury topics (cycle and pedestrian, falls, poisoning, fire and burns). Control: usual curriculum. Control schools agreed to teach at least 1 'Risk Watch' topic once the evaluation had been completed. | |
| Outcomes | Observed safety skills assessed by observation and role play in age‐appropriate injury scenarios ('stop, drop and roll', road safety and poisoning secondary intervention skills in years 3 and 4, fire and road safety skills and appropriate use of cycle helmets in year 5). Self‐reported behaviour and safety practices (fire and burn prevention, poisoning prevention, falls prevention, and cycle and pedestrian safety) measured using age‐appropriate pencil and paper questionnaires. Safety knowledge (fire and burn prevention, poisoning prevention, falls prevention and cycle and pedestrian safety) measured using age‐appropriate questionnaires, with questions illustrated pictorially. | |
| Injury mechanisms | Cycle and pedestrian; falls, fire and burns, poisoning. | |
| Notes | Children in the intervention group were more likely to be younger and to come from families without access to a car than children in the control group. Outcome data obtained from published and unpublished data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Although the allocation schedule was generated by computer, all schools included in the study were those who had agreed to undertake the programme. |
| Allocation concealment (selection bias) | Unclear risk | Unclear how the independent researcher allocated schools to the treatment groups. |
| Blinding of participants and personnel (performance bias) | High risk | "It was not possible to blind participants or teachers to treatment group allocation". |
| Blinding of outcome assessment (detection bias) | High risk | Blinding was attempted, but it is likely that this was broken. |
| Incomplete outcome data (attrition bias) | Low risk | Attrition < 20% in both treatment arms. Intention‐to‐treat analysis not mentioned. |
| Selective reporting (reporting bias) | Low risk | The study's prespecified outcomes of interest were reported in the prespecified way. |
| Other bias | Unclear risk | Unclear if there were any difference between schools who agreed to carry out the programme and those who did not, and if this could have introduced bias. |
| Methods | RCT (clustered) | |
| Participants | High‐school children aged 13 to 18 years from 123 rural‐based schools across 10 states in the US. Number of participants: 5113 students in the intervention group and 2955 students in the control group. | |
| Interventions | Intervention 1: Marketing & Promotion of Partners programme: formal training for trainers delivering programme; printed instruction guides; support from local agribusinesses; educational CD ROMs, videos, booklets; national conventions for trainers; newsletters for trainers; refresher training session. Intervention 2: Marketing & Promotion of Partners programme: formal training for trainers delivering programme; printed instruction guides; support from local agribusinesses; educational CD ROMs, videos, booklets; National conventions for trainers; biweekly contact with Partners programme facilitator; quarterly mailings of topic‐specific guides; free PPE to accompany lesson plans; personal contact with public health office. Control: Marketing & Promotion of Partners programme only. | |
| Outcomes | All outcomes were measured immediately and 1 year postintervention using the specially developed student instrument including: Self‐reported injury incidence proportion in the last 3 months; Safety knowledge (self‐reported learning); Self‐reported behaviour and safety practices including: safety consciousness and dangerous risk taking. | |
| Injury mechanisms | Agricultural injuries. | |
| Notes | Pre‐intervention sample consisted of 48% farm residents and 68% males. Postintervention groups (who had matched data) were balanced across sexes and age groups, with approximately 68% male and 42% farm residents. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | No information provided regarding allocation concealment. |
| Blinding of participants and personnel (performance bias) | High risk | Not possible to blind participants or those delivering intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Stated that "Data entry was conducted by trained staff who used a glossary to deal with aberrant responses" ‐ no mention of blinding. |
| Incomplete outcome data (attrition bias) | High risk | Started with 8068 children in 111 schools, but only analysed matched data for 3081 children (92 schools). No discussion regarding possible differences in children for whom both sets of data were not available. May have become underpowered. No sensitivity analyses. Intention‐to‐treat analysis was unclear as not mentioned. |
| Selective reporting (reporting bias) | Unclear risk | Did not report all advisor outcomes, only those that were significant. Did report on all outcomes arising for the test instrument, but no protocol available. |
| Other bias | High risk | Risk of being underpowered; no discussion regarding sample size achieved. Adjusted analyses for clustering effect not reported. |
| Methods | CBA | |
| Participants | School children aged 6 to 16 years in state‐based primary and middle schools in Guangdong province, China. Number of participants: 3988 students in the intervention group and 651 students in the control group. | |
| Interventions | Intervention: a multi‐component prevention programme delivered through schools. The programme aimed to raise awareness, increase knowledge and reduce the incidence of injuries to students. At least 2 classes on injury prevention per term were delivered to students, with a booklet on injury prevention provided for each student. A letter was also sent to families of children asking them to collaborate with health and safety education. A mass media campaign was used to promote public awareness regarding injury prevention. Teachers selected from each school were trained to take part in a rota to watch over the safety of students during physical activity classes, and during peak hours (morning, noon and afternoon) when parents dropped or collected their children. A school injury reporting system to the municipal Centre for Disease Control and Prevention was also set up. Meetings were held between healthcare teachers and school doctors to evaluate progress and gather feedback every 2 months. Control: no intervention. | |
| Outcomes | Injury incidence rates (mild/moderate/severe) reported through surveys at baseline and postintervention. Safety knowledge tested by questions on injury prevention and safety. Cost:benefit analysis using cost per unit of injury. | |
| Injury mechanisms | Pedestrian, cycle, motorcycle, vehicle (non‐specific), falls, heat and hot surfaces, sport/physical activity. | |
| Notes | Translated from Chinese. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | Unclear risk | No allocation concealment mentioned. |
| Blinding of participants and personnel (performance bias) | High risk | No mention of blinding. Participants were likely to know that they had received the intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No mention of blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition 2.3% in intervention group; not reported for control group. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported in prespecified ways. |
| Other bias | Unclear risk | No baseline data available to compare demographics of intervention and control groups. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | High risk | Did not adjust for confounding. Cluster analyses were presented by injury severity rather than by school. |
| Methods | Non‐RCT | |
| Participants | Participants were from 2 high schools (grades 10, 11 and 12) in the US, matched for socioeconomic factors but geographically separated, with enrolment of participants occurring in 4 sections of a physics class. Number of participants: 129 students in the intervention group and 74 students in the control group. | |
| Interventions | Intervention: a 5‐component course consisting of audio‐visual aids, physical demonstration and a didactic lecture. A researcher delivered the course over 1 week, with each contact lasting 1 hour. The 5 components were basic energy lesson; safety features of vehicles including seat belts; occupant kinematics and forces/crash prevention, e.g. airbags; review of days 1 to 3 and a demonstration of a rollover, students then designed crash vehicles; the students tested their crash design. Control: usual physics lesson. | |
| Outcomes | All outcomes measured by questionnaire 2 weeks, and 6 months after intervention. Self‐reported behaviour and practices (seat‐belt use, speeding and drink driving). Safety knowledge (physics of crashes, demographics of people involved in crashes and characteristics of automobiles). | |
| Injury mechanisms | Pedestrian, cycle, motorcycle, vehicle (non‐specific). | |
| Notes | No sample size calculation; non‐significant results may have occurred due to lack of power. There was a difference in the school grade of control and intervention groups at baseline. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | Unclear risk | Allocation was not described, except that they were 'chosen'. |
| Blinding of participants and personnel (performance bias) | High risk | It was clear which group the participants were in as the intervention group received the lessons and the control group had lessons as normal ‐ blinding not possible. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Paper did not report who analysed the data. |
| Incomplete outcome data (attrition bias) | High risk | Only results for students with scores for before instruction (time T1), and at 2 weeks (T2) and then T1 and T3 scores (6 months after instruction was completed) were included. No imputation for the missing data was carried out. There was also a large dropout rate in the control group at T3 (differential). |
| Selective reporting (reporting bias) | Unclear risk | Unclear how many children were in each group for the analyses and the authors did not mention removing outliers. |
| Other bias | Unclear risk | Methods of adjustment used in the regression modelling not described. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | High risk | There were slightly more males in the intervention group, and a difference of 1 school grade between most of the intervention and control group. Schools were matched on socioeconomic status. |
| Methods | CBA | |
| Participants | Primary school children aged 7.5 to 10 years from 4 schools in Toronto, Canada. Number of participants: 96 students in the intervention group and 36 students in the control group. | |
| Interventions | Intervention: Go AHEAD programme. single sessions delivered by teacher in the presence of a project co‐ordinator/trained facilitator. Activity‐based stations that looked at 4 safety topics: cycling and road use; reducing sports injury; creating a safety banner as a group; vehicle and road safety. Control: no intervention. | |
| Outcomes | Outcomes measured using questionnaire administered prior to and 4 months following intervention, including: Self‐reported behaviour and safety practices (helmet wearing, seat‐belt use). Safety knowledge (correct use of safety equipment). | |
| Injury mechanisms | Cycle, vehicle (non‐specific), sport/physical activity, sun. | |
| Notes | Intervention and controls were from the same class. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | Unclear risk | Allocation of schools to groups not described. |
| Blinding of participants and personnel (performance bias) | High risk | Intervention group participants taught separately in the gym, so not possible to conceal allocation to teachers. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No detail of who assessed or marked test papers. |
| Incomplete outcome data (attrition bias) | Unclear risk | Number followed up for secondary outcomes not reported. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available; primary and secondary outcomes not prespecified. |
| Other bias | Unclear risk | No baseline data. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Unclear risk | Intervention and controls were from the same class. No table of characteristics provided. |
| Methods | RCT | |
| Participants | Participants were high‐school agriculture students in the 9th and 10th grades from Kentucky, US. Number of participants: 373 students in the intervention group and 417 students in the control group. | |
| Interventions | Intervention: Agricultural Disability Awareness and Risk Education (AgDARE) programme utilised 2 simulation exercise modules: narrative and physical. Narrative (cognitive) simulations which involved problem‐solving activities, whereby students were told a story and used pencil and paper to make decisions about work behaviours. Students received instant feedback about their choices, which helped to reinforce the realities of the story being told. In the physical simulations, students had to pretend to have a disability while different farm tasks were simulated. The 2 simulation exercise modules were carried out for each of the 4 topics. The intervention was delivered by 2 research assistants and 2 public health nurses. Due to students' often conflicting commitments, not all students could complete the whole curriculum. Control: no intervention. | |
| Outcomes | Observed safety behaviour (during farm work) measured by visits 1 year after the intervention. Self‐reported behaviour and safety practices measured by Stages of Change questionnaire pre‐ and postintervention. | |
| Injury mechanisms | Agricultural injuries. | |
| Notes | Control group students were more likely to be older than students in the intervention group. There were no significant differences between the groups in the number of years they had lived or worked on a farm. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors reported that the schools were randomly assigned. But there was no further information provided. In addition, initial schools were selected based on the strength of their agricultural programmes. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information about the allocation process to determine if high or low risk. |
| Blinding of participants and personnel (performance bias) | High risk | Study did not address blinding of participants and personnel. Participants are likely to know that they have received the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | The people who conducted the interventions were the same ones who assessed the outcomes, particularly the observed behaviours. |
| Incomplete outcome data (attrition bias) | High risk | Only students who completed at least 2 out of the 4 units of instruction were included. There was no mention of missing data points as a result of this. Intention‐to‐treat analysis not mentioned. |
| Selective reporting (reporting bias) | High risk | No clear description of the method of scoring for the assessment tools used. |
| Other bias | Unclear risk | Insufficient information to assess whether an important risk of bias existed. |
| Methods | Non‐RCT | |
| Participants | Children and their teachers in state‐based preschool and grades 1, 3 and 5 from urban and rural areas of Birmingham, US. Intervention and control group participants were enrolled in the same 3 schools. There were 4 intervention groups (by grade level). Number of participants: 266 students in the intervention group and 229 students in the control group. | |
| Interventions | Intervention: special injury prevention curriculum delivered over 3 months by a teacher. An 8‐component curriculum was developed for each grade level. This included spinal cord awareness and water safety. Teachers had a choice of at least 3 activities to teach each concept. A cartoon character was used to represent behaviours presented in the curriculum (e.g. Alli cat for falls, as cats always land on their feet). Control: unclear ‐ not reported. | |
| Outcomes | Outcomes were assessed by questionnaire, 4 months following the intervention. Self‐reported behaviour and practices (seat‐belt use). Safety knowledge (relating to a range of injury mechanisms). | |
| Injury mechanisms | Pedestrian, cycle, vehicle (non‐specific), falls, swimming/drowning, sport/physical activity. | |
| Notes | No baseline characteristics were presented, although study reported that intervention and control group participants were taken from the same 3 schools (with students from a range of socioeconomic backgrounds). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | Unclear risk | Allocation method not reported. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding ‐ teachers were aware of the group allocations. |
| Blinding of outcome assessment (detection bias) | High risk | Teachers were aware of group allocations and assessed the outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Number allocated to each of the groups at baseline not reported. No mention of any missing data, or the number of children absent and pre‐ and post‐testing. |
| Selective reporting (reporting bias) | Unclear risk | The seat‐belt use outcome was reported incompletely (missing exact figures), so that it could not be entered in a meta‐analysis. |
| Other bias | Unclear risk | There may be risk of bias, but there was insufficient information to assess whether an important risk of bias existed. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Unclear risk | Intervention and control group participants were taken from the same 3 schools (from low, middle and upper socioeconomic backgrounds), but no baseline characteristics presented. |
| Methods | RCT(clustered) | |
| Participants | Primary‐ and middle‐school aged children from 10 state schools (approximately 10,000 students) in a city setting in China. In each arm, there were 3 primary schools and 2 middle schools. Analyses were not carried out in the oldest children as they left school before outcomes were ascertained. Sex and ages not specified. Number of participants: 8305 children remained and outcomes were analysed for 7605 students. | |
| Interventions | Intervention: aimed mainly at children but also included parents. Mainly delivered in schools but some information materials did go home to parents. Intervention consisted of multiple components: distributing booklets and leaflets with information on injury prevention to students and parents; helping students to publish "blackboard bulletins" by offering them relevant materials; offering posters on safety education to schools. Unclear who delivered the intervention. Frequency and duration of contacts not specified. Intervention ran over an 11‐month period. Control: general information on food hygiene and disease prevention. Method of delivery not specified. | |
| Outcomes | Outcomes measured 1 year after intervention, including: Self‐reported injury incidence rate (overall, at school, at home, travelling to school, falls, road transport and recurrent injuries). Injury‐related behaviour, assessed by questionnaire. | |
| Injury mechanisms | Fall injuries. | |
| Notes | Only available as an English abstract. This was a PhD thesis and the full thesis could not be obtained through inter‐library loans. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. Just says "randomly assigned". |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) | High risk | No details given. Participants are likely to have known that they received the intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) | Unclear risk | No details given. Unclear if intention‐to‐treat analysis used. |
| Selective reporting (reporting bias) | Low risk | Only analysed data for students that had complete follow‐up data but this was 91.57% of all children. Unclear how the 8.43% of children not followed up differed. |
| Other bias | Unclear risk | Only the abstract was available in English and a full copy of the thesis could not be obtained. It was unclear, therefore, whether there was selective reporting in the full document. Only a subset of data were reported in the abstract. Did not appear to have taken clustering into account but without the full thesis it is difficult to know for sure. |
| Methods | CBA | |
| Participants | Children were grouped by grade level: kindergarten and grade 1; elementary school; and the first 3 grades of high school. The schools were from an urban area in Greece. Number of participants: 1400 children included in the evaluation. 641 children in the intervention group (693 minus 28 (pupils who did not receive the intervention) ‐ 24 (pupils absent during the evaluation)) and 759 control group children. | |
| Interventions | Intervention: special day event. Presentation of age‐adjusted educational materials by health professionals in collaboration with teachers. Comprised a short audio‐visual presentation, a discussion about pupils' personal experiences, comments on how relevant events could have been averted, drama plays or a combination of these. Take home materials were also provided (e.g. leaflets, crosswords, stickers, badges with water safety messages). Control: no intervention. | |
| Outcomes | Safety knowledge (water safety), assessed by multiple choice and open‐ended questions. | |
| Injury mechanisms | Water safety, swimming/drowning. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | Unclear risk | No mention of how schools were allocated to the intervention and control groups. |
| Blinding of participants and personnel (performance bias) | High risk | Study did not address blinding of participants and personnel. Participants were likely to know that they have received the intervention. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Study did not address blinding of outcome assessor. |
| Incomplete outcome data (attrition bias) | Low risk | Reasons for missing outcome data were unlikely to be related to the true outcome. |
| Selective reporting (reporting bias) | Low risk | All the study's prespecified outcomes reported in the specified ways. |
| Other bias | Low risk | Study appeared to be free of other sources of bias. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Unclear risk | There were some differences between the baseline characterises of intervention and control groups. No matching. |
| Methods | Non‐RCT | |
| Participants | School children aged 10 to 13 years from 4 primary schools in Netherlands. Number of participants: 31 students in the intervention group and 32 students in the control group. | |
| Interventions | Intervention: pedestrian and cyclist safety instruction was given using a real lorry placed in the school yard. Limitations in the driver's field of view were demonstrated, and information on safe behaviour was provided. Blind spots were further illustrated through graphic representations and videos. Each intervention group assessed 1 of 2 blind spot programmes: awareness (addressing carelessness) and competency (addressing blind spot hazards only). Control: no intervention. | |
| Outcomes | Self‐reported behaviour and safety practices (correct positioning of cycle or self as pedestrian) 1 month after intervention. | |
| Injury mechanisms | Pedestrian and cycle. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | High risk | Selected schools that "already used the programmes on a regular basis". |
| Blinding of participants and personnel (performance bias) | High risk | Stated that "At the intervention schools… participants, instructors and school staff were informed about the purpose of the evaluation". Not clear whether control groups were informed about participation in the study, and their status within it. |
| Blinding of outcome assessment (detection bias) | High risk | Staff and students were aware of the purpose of the evaluation. |
| Incomplete outcome data (attrition bias) | Low risk | No discussion regarding any missing participants at post‐test. Numbers indicated that 100% of sample completed post‐test in all groups. |
| Selective reporting (reporting bias) | Low risk | Protocol not available, but complexity levels stated a priori, and were related to hypotheses which are clearly stated in the introduction. |
| Other bias | Low risk | Appeared to be free of other bias. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Unclear risk | Although schools matched for geographical location, characteristics of the schools not reported. |
| Methods | RCT | |
| Participants | School children in grades 1‐6 in state‐based middle schools in Jiujang province, China. Number of participants: 1200 students in the intervention group and 1268 students in the control group. | |
| Interventions | Intervention: peer educators trained to deliver weekly sessions to students. The session could be an activity, presentation, game or themed discussion on injury prevention. The peer educators also passed on health and safety information. Control: no intervention. | |
| Outcomes | Outcomes measured by questionnaire over 2 years following intervention. Self‐reported injury incidence rates (sports, falls, traffic, burns, other type). Safety knowledge (sports, falls, traffic, burn, health, other). | |
| Injury mechanisms | Common injuries (non‐specific). | |
| Notes | Original paper in Chinese. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was mentioned, but no detail reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Stated that double‐blind method was used but there was insufficient detail about what this meant. |
| Blinding of outcome assessment (detection bias) | Unclear risk | People were trained to deploy the questionnaires. Data entry was quality controlled. However, unclear whether data entry was blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Outcomes reported on 87% of participants at follow‐up in the intervention arm and on 96% in the control arm. |
| Selective reporting (reporting bias) | Low risk | Injury and knowledge outcomes reported as described in methods. |
| Other bias | Unclear risk | No risk identified through imbalance in demographics between groups. |
| Methods | CBA | |
| Participants | Participants were children from 2 regions in Canada. Intervention group children were from 24 classes (15 schools) in Regina and the control group were from Saskatoon (20 classes). The 2 groups were matched for ages, grade and socioeconomic status. Number of participants: 350 students in the intervention group and 313 students in the control group. | |
| Interventions | Intervention: 1 × 1‐hour duration Think First programme presentation involving: video of teenagers with brain and spinal cord injuries; educational session with audio‐visual aids; description of brain anatomy and pathophysiology; account of experience from person with a brain/spinal cord injury. Control: usual curriculum. | |
| Outcomes | Outcomes were measured over a 4‐month period using questionnaire. Self‐reported behaviour and safety practices. Safety knowledge. | |
| Injury mechanisms | Cycle, vehicle (non‐specific), swimming/drowning. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | High risk | Intervention schools selected from those already scheduled to receive the Think First programme. |
| Blinding of participants and personnel (performance bias) | High risk | As there was a first aid component to the intervention, participants would have been aware that they were receiving some training. |
| Blinding of outcome assessment (detection bias) | High risk | Self‐reported outcomes. |
| Incomplete outcome data (attrition bias) | High risk | Attrition was > 20% in the intervention group and was 0% in the control group. In addition, as 600 responses were discarded due to characteristics such as age and education, this could have introduced further bias. |
| Selective reporting (reporting bias) | Low risk | All outcomes appeared to be reported in the prespecified ways. |
| Other bias | Low risk | Study appeared to be free of other sources of bias. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Low risk | Control schools were matched to intervention schools for age, grade and socioeconomic background. |
| Methods | CBA | |
| Participants | Participants were boys and girls aged 11 and 15 years (3 middle schools and 3 high schools) from state schools in the US, located in rural, urban and suburban settings. Number of participants: 663 (372 middle school and 249 high school) in the intervention group and 78 children in the control group. | |
| Interventions | Intervention: Think First programme. Intervention was delivered by Think First project staff and a victim of injury. Children were presented with a short film, were given a lecture and a talk by a victim of a traumatic brain or spinal cord injury, which was followed by a question and answer session. The focus of the talks was on action regarding seat‐belt use, use of motorcycle helmets, cycle helmets, as well as the avoidance of drugs and alcohol while driving or participating in sports. Also included was the importance of checking for the depth of water when swimming or diving. Control: received the same intervention, although delayed until after data collection. | |
| Outcomes | Observed behaviour (seat belt and helmet wearing on leaving school). Self‐reported behaviour and practices assessed by questionnaire. Safety knowledge assessed by questionnaire. All outcomes were measured at 2 weeks' and 3 months' post‐intervention. | |
| Injury mechanisms | Pedestrian, cycle, motorcycle, vehicle (non‐specific) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | High risk | Intervention schools were a convenience sample. In addition, the baseline characteristics of the 2 groups were different ‐ participants in the control group were older. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and people delivering the intervention not blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Students aware of group allocations when they completed the questionnaires. Not reported whether people assessing the behaviour outcomes were blinded to the group allocations. |
| Incomplete outcome data (attrition bias) | High risk | High attrition at 3 months in the intervention group. Only 37.4% of the total number of children allocated to the intervention group at baseline were followed up. |
| Selective reporting (reporting bias) | High risk | For behavioural outcomes, only selected items reported. |
| Other bias | High risk | Control group used a shortened questionnaire. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | High risk | Control and intervention groups not matched, no adjustment for confounding mentioned. |
| Methods | RCT | |
| Participants | Primary school children aged 7 to 13 years and their parents from schools in urban and rural areas of China. Number of participants: 3172 students in the intervention group and 2698 students in the control group. | |
| Interventions | Intervention: 1 lecture, plus leaflets on injury prevention given each semester (2 per year) to teachers and parents. Teachers gave 2 lectures on injury prevention each semester to students. Safety practice posters were also given to children during classes. A safety course was given to children before their summer and winter school holidays. Control: health education and promotion on prevention of pneumonia, iron‐deficiency anaemia, rickets and common communicable diseases were given to teachers, parents and children using the same schedule as the intervention group. | |
| Outcomes | Medically attended injury incidence rates measured by injury surveillance system over 2 years. | |
| Injury mechanisms | Pedestrian, motorcycle, vehicle (non‐specific), swimming/drowning, household safety, poisoning. | |
| Notes | Location, facilities, situation of sports fields, faculties and socioeconomic status were reported as similar in rural and urban schools prior to randomisation. Translated from Chinese. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Paper stated "randomly allocated". No further information given. |
| Allocation concealment (selection bias) | Unclear risk | Only stated "randomly allocated". Did not report who performed allocation or if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | Low risk | No mention of blinding; but injury outcome measured by records of hospital attendance/insurance claims, therefore, unlikely to have introduced differential bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Stated "trained health personnel kept records of child injuries based on copies of hospital records", but no mention of personnel being blinded to allocation |
| Incomplete outcome data (attrition bias) | Low risk | Appeared that there was no loss to follow‐up from initial questionnaires sent through to injury outcome recording. No mention of any missing data. Not specified, but appeared to use intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Insufficient information to judge if all prespecified outcomes were included. |
| Other bias | Low risk | Did not appear to be at risk of other bias. |
| Methods | CBA | |
| Participants | Primary school children in grades 1 to 5, from 19 elementary schools from a mixture of socioeconomic backgrounds. Number of participants: 18,876. The number in the control and intervention arms was not stated. | |
| Interventions | Information not provided ‐ but named as 'Think First For Kids' programme which is described in other studies. | |
| Outcomes | Observed behaviour, made by parent or guardian (pedestrian, sport, interpersonal and car safety behaviours). Self‐reported behaviour and safety practices. Safety knowledge. | |
| Injury mechanisms | Pedestrian, cycle, motorcycle, vehicle (non‐specific). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation to intervention/control (selection bias) (for non‐RCT and CBA studies) | Unclear risk | Did not report the number of schools in intervention and control groups or how school were selected to receive Think First For Kids programme. |
| Blinding of participants and personnel (performance bias) | High risk | Insufficient information about the blinding process. Participants were likely to know that they received the intervention. |
| Blinding of outcome assessment (detection bias) | High risk | Parents/guardians assessed their own children's observed behaviours, though it was unclear if they were informed as to whether their child was in a control or intervention group. |
| Incomplete outcome data (attrition bias) | Unclear risk | Insufficient information provided to know how incomplete data were addressed. |
| Selective reporting (reporting bias) | Unclear risk | Numbers not reported. A graph was included but there were no data points and the multi‐variate analysis only included the confidence interval and not the point estimate. |
| Other bias | Unclear risk | Insufficient detail in the summary. |
| Risk of bias due to confounding (for non‐RCTs and CBA studies) | Low risk | Schools were matched on socioeconomic status, reading scores, ethnicity and school district. No information provided to enable assessment of the balance of characteristics between groups. |
BMI: body mass index; CBA: controlled before‐and‐after; IMPS: Injury Minimization Programme for Schools; PE: physical exercise; RCT: randomised controlled trial; SPIY: Skills for Preventing Injury in Youth.
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report participants of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report outcomes of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report participants of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. | |
| Did not report study design of interest. | |
| Did not report intervention of interest. | |
| Did not report study design of interest. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Injury rates at follow‐up, adjusted for baseline injury rates in non‐randomised studies Show forest plot | 3 | 2073 | Rate Ratio (Random, 95% CI) | 0.73 [0.49, 1.08] |
| Analysis 1.1 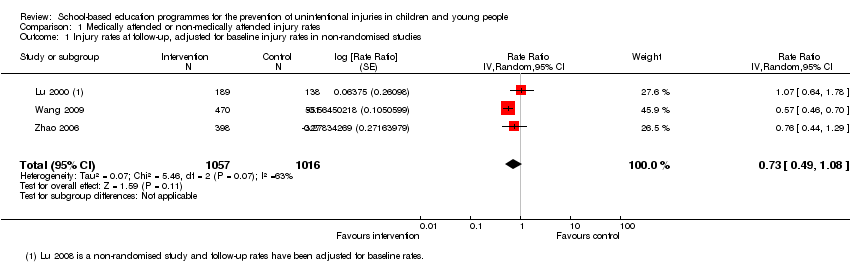 Comparison 1 Medically attended or non‐medically attended injury rates, Outcome 1 Injury rates at follow‐up, adjusted for baseline injury rates in non‐randomised studies. | ||||

PRISMA flow chart detailing the process of study selection for all studies included in the review. CBA: controlled before‐and‐after study; RCT: randomised controlled trial.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Injury rates, outcome: 1.1 Injury rates at follow‐up.

Comparison 1 Medically attended or non‐medically attended injury rates, Outcome 1 Injury rates at follow‐up, adjusted for baseline injury rates in non‐randomised studies.
| School injury prevention programmes compared to controls for the prevention of unintentional injuries in children and young people | ||||||
| Patient or population: children and young people | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Injury rate, adjusted for clustering, with control | Injury rate, adjusted for clustering, with School injury prevention programmes | |||||
| Self‐reported medically or non‐medically attended unintentional injuries or injuries with an unspecified intent (injury rates adjusted for clustering) | 367 per 1000 person‐years | 243 per 1000 person‐years | Rate ratio 0.76 | 12,977 (2073 person‐years adjusted for clustering) | ⊕⊕⊝⊝ | We excluded 4 studies from the meta‐analysis due to varied interventions (e.g. sports, agriculture or risk‐taking injury prevention). Their findings were consistent with the meta‐analysis studies. |
| Safety skills | Both studies found an improvement in observed safety skills (Kendrick 2007 ‐ fire and burn prevention skills: odds ratio 8.93 (95% CI 1.67 to 47.78, P = 0.01); Frederick 2000 ‐ basic life support skills, P < 0.005 for assessment of danger, responsiveness and circulation). | ‐ | 1751 | ⊕⊕⊝⊝ | Interventions and safety skills observed were varied in these 2 studies. | |
| Behaviour | All 4 studies (5 articles) reported that observed safety behaviour showed evidence of improved practices and 13/19 studies describing self‐reported behaviour reported improved practices. | ‐ | 52,950 | ⊕⊝⊝⊝ | Behaviours included safety equipment wearing, road risk‐taking behaviour, agriculture and sports‐related injury behaviours. | |
| Safety knowledge | Of the 21 studies assessing changes in safety knowledge, 19 reported an improvement in at least 1 question domain in the intervention compared to the control group. | ‐ | 55,732 (9 RCTs, 5 non‐RCTs, 7 CBA) | ⊕⊝⊝⊝ | Outcomes included a wide range of knowledge testing instruments and topics. | |
| Cost‐effectiveness | For every 1 Chinese Yuan spent, 13.90 was saved (cost:benefit ratio 1:13.9) | ‐ | 4639 | ⊕⊝⊝⊝ | Only 1 study reported economic outcomes and should, therefore, be interpreted with caution. | |
| CI: confidence interval; CBA: controlled before‐and‐after study; RCT: randomised controlled trial; non‐RCT: non‐randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded twice because of inconsistency as the I2 = 63%, indicating substantial heterogeneity and because there was imprecision in the results (the rate ratio was 0.76 but the confidence intervals spanned 1). Two of the studies were RCTs with a low risk of bias. 2 Downgraded twice because of a serious risk of bias (one of the two studies was a CBA resulting in selection biases relating to which schools participated in studies) and inconsistency, which was rated as serious because the two studies had different intervention types with different outcome measures. Imprecision was serious as there were wide confidence intervals in one of the two included studies, as well as a paucity of data. However, the effect sizes were classed as large as there was a nearly nine times greater odds of fire and burn prevention skills in the Risk Watch programme (Kendrick 2007), and 33% greater skills assessment in the Injury Minimisation Programme for Schools (IMPS) relating to assessment of danger (Frederick 2000). 3 Downgraded three times because 10 studies were CBA or non‐RCT design with high risk of selection bias of included schools, there was serious inconsistency in methods of collecting data and intervention types, and this may have contributed to the wide range of effect sizes and directions seen (no effect or some effect), There was often wide confidence intervals in results presented. 4 Downgraded three times because 11 studies were CBA or non‐RCT design with high risk of selection bias of included schools; there was serious inconsistency in knowledge tested, questionnaire designs and methods of collecting data, a wide range of intervention types and pedagogical approaches and this may have contributed to the wide range of effect sizes and directions seen (no effect or some effect). Results were presented in a way that often made precision difficult to compare. 5 Downgraded three times because this was one study, limited in applicability with high or unclear risk of bias across multiple domains. | ||||||
| Study ID | Age (years) | |||||||||||||
| 4/5 | 5/6 | 6/7 | 7/8 | 8/9 | 9/10 | 10/11 | 11/12 | 12/13 | 13/14 | 14/15 | 15/16 | 16/17 | 17/18 | |
| ‐ | ● | ● | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ● | ● | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ‐ | |
| ‐ | ‐ | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | |
| ‐ | ‐ | ‐ | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ‐ | ‐ | |
| ● | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ● | ● | ● | ● | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ‐ | ‐ | ‐ | |
| ‐ | ● | ● | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ● | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ● | ● | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ● | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐: not applicable; ●: age range covered. | ||||||||||||||
| Study ID | Injury mechanism | ||||||||||||
| Pedestrian | Cycle | Motorcycle | Vehicle (non‐specific) | Falls | Swimming/ drowning/ diving | Smoke/ fire/ flames | Heat and hot surfaces | Sport/ physical activity | Sun | Household safety | Agricultural injuries | Poisoning | |
| ‐ | ● | ‐ | ● | ‐ | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ● | ‐ | ● | ‐ | ● | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ‐ | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ● | ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ● | ● | ‐ | ● | ● | ● | ‐ | ‐ | ● | ‐ | ● | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ‐ | ● | ‐ | ● | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ● | ‐ | ● | ‐ | ● | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ‐ | ‐ | ● | ‐ | ● | ● | ‐ | ‐ | ‐ | ‐ | ● | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | |
| ● | ● | ● | ● | ● | ‐ | ‐ | ● | ● | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ● | ‐ | ● | ‐ | ● | ‐ | ‐ | ● | ● | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | |
| ● | ● | ● | ● | ● | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | ||
| ‐ | ‐ | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐ | ● | ‐ | ● | ‐ | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ● | ‐ | ● | ● | ‐ | ● | ‐ | ‐ | ‐ | ‐ | ● | ‐ | ● | |
| ● | ● | ● | ● | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | |
| ‐: outcome not measured; ●: outcome measured. | |||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Injury rates at follow‐up, adjusted for baseline injury rates in non‐randomised studies Show forest plot | 3 | 2073 | Rate Ratio (Random, 95% CI) | 0.73 [0.49, 1.08] |


