Laser untuk pembuangan karies gigi desidus dan gigi kekal
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Design: parallel‐group randomised controlled clinical trial Centres: 1 Date: May 2013 to December 2013 Setting: secondary care Operators: not reported | |
| Participants | Setting: University Department of Paediatric Dentistry Geographical area: Bulgaria Sample: 90 participants (45 laser versus 45 drill); number of treated teeth as well as prepared dental cavities not reported Age: 6 to 12 years Sex: not reported Baseline: participants were affected by occlusal and proximal caries involving primary and permanent molar. Methods used for caries diagnosis as well as pulpal vitality testing were not described Inclusion criteria: children aged 6 to 12 years; 1 or more dentine carious lesions (D3 threshold, WHO system), without pulp involvement or pain, located on the occlusal or proximal surface of a primary or a permanent molar; signed informed consent form from parent; native language of the child Bulgarian Exclusion criteria: previous laser treatment of carious lesions prior the present study | |
| Interventions | Intervention: Er:YAG laser: wavelength: 2940 nm pulse energy: 200 to 300 mJ/pulse (permanent teeth); 100 to 200 mJ/pulse (primary teeth) pulse duration: 250 μsec repetition rate: 20 Hz cooling method: water Control: drill in high‐speed and low‐speed dental handpieces | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes | Funding: unclear | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the methodology of random sequence generation was not mentioned Quote: "A group of ninety 6‐12‐years‐old patients ... who met the inclusion criteria and were treated at the Department of Pediatric Dentistry in Plovdiv, Bulgaria during the period May – December 2013, was |
| Allocation concealment (selection bias) | Unclear risk | The allocation concealment was not described in the study |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | The trial examined episodes of pain (but not caries removal). The study provides only descriptive results regarding pain and was thus considered unclear |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. The primary outcome caries removal was not reported |
| Other bias | Unclear risk | It was unclear whether the study was funded or not |
| Methods | Design: parallel‐group randomised controlled clinical trial; participants randomised to treatment in a 2:1 ratio laser to conventional dental drill Date: not reported Centres: 2 Setting: secondary care Operators: single operator at each site (skilled paediatric dentists) | |
| Participants | Setting: University School of Dentistry Clinic Geographical area: USA Sample: 124 children and adolescents; 124 teeth; 124 dental cavities (82 laser versus 42 drill) Age: 4 to18 years, mean 10.4 years Sex: males 53% Baseline: patients of different ethnicity (Caucasian (understood to be white), African‐American, Hispanic, Asian and Native American) were affected by caries requiring Black's Classes I to V cavities preparation for its removal. Caries depth varied: shallow dentine, deep dentine, enamel and enamel/shallow dentine. Caries diagnosis was performed through visual, tactile (dental explorer) and radiographic analysis. Dental pulp evaluation was performed by means of thermal testing with ice/ethylene‐oxide application and intraoral X‐rays taken to evaluate the presence of apical pathosis Inclusion criteria: carious lesion in at least 1 tooth that required restoration and a contralateral healthy tooth as a control Exclusion criteria: periodontitis, pulpitis, severe wear on occlusal surface, previous restorations of the proposed treatment tooth, active local or systemic infections, involvement in other investigational treatment, refusal to give informed consent, mental incompetence, imprisonment, knowledge of pregnancy and refusal to co‐operate with the evaluation visits | |
| Interventions | Intervention: Er:YAG: wavelength: 294 μm pulse energy: 200 to 300 mJ/pulse (permanent teeth); 100 to 200 mJ/pulse (primary teeth) pulse duration: 250 μsec repetition rate : 20 Hz cooling method: air‐water spray Control: traditional carbide dental drill in standard air‐turbine handpiece | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to treatment in a 2:1 ratio laser to conventional dental drill Randomisation was performed by generating number list (information obtained by contacting authors) |
| Allocation concealment (selection bias) | Unclear risk | The generated number and assignment were placed in a sealed envelope, hence concealed (information obtained by contacting authors). However, it was unclear whether the envelopes were opaque or serially numbered |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcomes were evaluated by the investigator and by an "an independent evaluator" but no clear statement on the blinding procedure was provided |
| Incomplete outcome data (attrition bias) | Unclear risk | The study evaluated both primary outcomes. The investigators were able to perform caries removal in both groups of participants with no missing data. However, the evaluation of episodes of pain was performed only on the participants that did not receive any anaesthesia: 78/82 participants allocated to laser and 31/42 in the drill group. Of the 124 participants treated, 112 were available for the 3‐month follow‐up visit, when pulpal vitality was assessed |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. The primary outcome, caries removal, was reported, however information regarding pain treatment was not completely reported and therefore hindered the performance of meta‐analysis |
| Other bias | High risk | The study was supported by a for‐profit company: "This study was supported by Continuum Biomedical under a research agreement with the University of California, San Francisco, and the University of Kentucky, Louisville" |
| Methods | Design: split‐mouth randomised controlled clinical trial Centres: 15 dentists in the UK Date: not reported Setting: primary and secondary care Operators: 15 in total (9 general dental practitioners, 1 community dentist and 5 hospital dentists). All the dentists received a course of instruction on the use of the laser | |
| Participants | Setting: hospitals and private dental offices Geographical area: UK Sample: 77 participants; 154 teeth; 154 dental cavities (77 laser group versus 77 drill group) Age: 3.5 to 68 years Sex: not reported Baseline: participants were affected by caries requiring Black's Classes I to III and Class V cavities preparation for its removal. Primary and/or permanent anterior, premolar and molar teeth were affected by caries. The caries depth ranged by less to more than half‐way through dentine. Methods used for caries diagnosis as well as pulpal vitality testing were not described Inclusion criteria: participants required treatment of 2 matching primary carious cavities Exclusion criteria: photosensitivity disorder, a convulsive disorder such as epilepsy, or having a cardiac pacemaker | |
| Interventions | Intervention: Er:YAG: wavelength: 2.94 μm pulse energy: 150 to 400 mJ/pulse pulse duration: not reported pulse frequency: 2 Hz to 3 Hz cooling method: water spray Control: conventional drill in dental handpieces | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | In order to avoid bias, the cavities were completed at 2 separate appointments, on different days, with the order of methods being determined by opening an opaque, sealed envelope containing information randomly generated by computer |
| Allocation concealment (selection bias) | Low risk | In order to avoid bias, the cavities were completed at 2 separate appointments, on different days, with the order of methods being determined by opening an opaque, sealed envelope containing information randomly generated by computer. |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information was provided |
| Incomplete outcome data (attrition bias) | Unclear risk | Of the 82 cases started, 5 were not completed. In 40 out of 77 visits assigned for laser treatment, the dentist had to use a conventional handpiece in addition to the laser to complete the cavity preparation |
| Selective reporting (reporting bias) | High risk | The study protocol was not available. The primary outcomes, caries removal and episodes of pain, were not reported |
| Other bias | High risk | The study was supported by a for‐profit company: "The authors would like to thank Richard Whatley, Richard Collard and Vic Peterson of KaVo (UK) Ltd for their exceptional generosity and support for this study" |
| Methods | Design: split‐mouth randomised controlled clinical trial Centres: 1 Date: not reported Setting: secondary care Operators: 2 dentists | |
| Participants | Setting: University School of Dentistry Clinic Geographical area: USA Sample: 66 adult participants; 132 teeth; 132 dental cavities (66 laser group versus 66 drill group) Age: 20 to 84 years, median 41 years Sex: males 63% Baseline: participants were affected by caries requiring Black's Classes I, III, and/or Class V cavities preparation for its removal, with sound pulpal tissues (electric pulp tester). Both the presence and depth of caries were diagnosed through clinical as well as radiological procedures Inclusion criteria: 18 years of age or older; having at least 1 carious lesion on each of 2 separate teeth that represented Black's Classes I, III, and Class V preparations Exclusion criteria: participants with systemic illness and under active medical care or medical control; being pregnant; wearing cardiac rhythm electronic control devices. Moreover, further exclusion criteria were: non‐vital teeth; caries extending more than two‐thirds of the distance through dentine as assessed clinically, radiographically, or both; teeth that required more than 1 restoration in the same tooth; and teeth with radiographic evidence of apical radiolucency | |
| Interventions | Intervention: Er,Cr:YSGG: wavelength: 2.78 μm pulse energy: 0 to 300 mJ/pulse pulse duration: 140 μm repetition rate: 20 Hz cooling method: air‐water spray Control: drill in air turbine handpiece (20,000 to 24,000 rotations per minute with air‐water spray) | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the study reported that it was randomised but did not report the method used to generate random sequence Quote: "We randomly selected tooth pairs for treatment A, LPHKS (laser) preparations, or for treatment B, air turbine/bur dental surgery" |
| Allocation concealment (selection bias) | Unclear risk | Comment: investigators used sealed envelopes to allocate treatment, but it was unclear whether the envelopes were opaque and sequentially numbered Quote: "We did this by selecting a sealed envelope designating either treatment A or treatment B and used whichever method was named in the envelope to treat the tooth with the lower tooth number (1‐32); the higher‐numbered tooth received the other treatment" |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Low risk | 3 blinded evaluators were involved in this study |
| Incomplete outcome data (attrition bias) | Unclear risk | There was 12% attrition Quote: "From the total of 75 tooth pairs entered into the study, three participants failed to return for recall visits, and another six did not return for the final six month assessment. The results, therefore, are based on 66 pairs for which complete data were available" |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. The primary outcome episodes of pain was not reported |
| Other bias | High risk | The study was supported by a for‐profit company: "This study was sponsored by a grant from BioLase Technology Inc., San Clemente, California" |
| Methods | Design: parallel‐group randomised controlled clinical trial Setting: secondary care Date: not reported Operators: not reported | |
| Participants | Setting: University School of Dentistry Clinic Geographical area: USA Sample: 90 adult participants; 190 teeth and 215 cavities in laser group versus 186 teeth and 207 cavities in drill group Age: 18 to 61 years Sex: males 40% Baseline: participants presented all third molar, tested in the study, with sound dental pulp assessed through thermal testing consisting of placement of a stick (0° C) on the facial surface of the tooth for 5 seconds. Caries diagnosis method used in the trial was not described Inclusion criteria: adult participants (> 18 years) requiring third molar extraction, having at least 2 teeth with pit‐and‐fissure caries located on occlusal, buccal or lingual surfaces above the cemento‐enamel junction. The evaluated teeth had to be symptom‐free, fully developed and completely erupted Exclusion criteria: visible, tactile or radiographic evidence of periapical pathosis, incompletely formed roots, previous restorations, evidence of periodontitis or pulpitis, or gross radiographic evidence of caries that had penetrated into dentine | |
| Interventions | Intervention: Nd:YAG laser: wavelength: 1.064 μm pulse duration: 150 μsec pulse energy: 100 mJ repetition rates: 10 Hz to 20 Hz Control: 1/2 round carbide crosscut fissure (701) or pear‐shaped (330) bur in a high‐speed handpiece | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: authors reported randomisation but provided insufficient information regarding random sequence generation Quote: "Carious lesions were randomised to drill or laser treatment" |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Pulp diagnosis, enamel surface condition, preparations and restorations were assessed by blinded evaluators Clinical evaluations were made prior to treatment, immediately following treatment, and at 1 week, 1, 3 and 6 months post‐treatment |
| Incomplete outcome data (attrition bias) | Unclear risk | The study reported 3 dropouts but it was unclear from which of the two samples they combined for analysis |
| Selective reporting (reporting bias) | High risk | The study protocol was not available. The study did not report on episodes of pain and although it reported on caries removal in the methods, no data was provided |
| Other bias | High risk | The study was supported by a for‐profit company: "The study was funded by Incisive Technologies Inc. (San Carlos, CA, USA) and American Dental Technologies Inc. (Corpus Christi, TX, USA) and NIDCR DE12091 (DF)" |
| Methods | Design: split‐mouth randomised controlled clinical trial Date: April 1991 to February 1992 Centres: 5 Setting: secondary care Operators: not reported | |
| Participants | Setting: university clinics Geographical area: Germany Sample: 103 participants, 194 teeth (97 in laser group versus 97 in drill group), 206 cavities (in 12 cases 1 tooth included 2 lesions prepared on different occasions by laser and mechanical means) Age: 18 to 72 years; mean age 32.8 years (SD 12.5) Sex: males 47% Baseline: type of teeth treated not specified. Participants affected by occlusal, lingual, buccal and proximal caries. Caries depth was assessed by means of intraoral X‐ray. All decayed teeth showed sound dental pulpal tissues (thermal vitality testing and intraoral X‐ray) Inclusion criteria: > 18 years of age Exclusion criteria: photodermatosis, diabetes, alcoholism, and haemorrhagic disorders including haemophilia and leukaemia; moreover, virus infections and neoplasias of the skull were also excluded, as were people with a history of epilepsy or psychiatric disturbances | |
| Interventions | Intervention: Er:YAG laser: wavelength: 2.94 μm pulse duration: 250 μsec pulse energy: 250 mJ (for enamel); 150 mJ to 300 mJ (for dentine) repetition rates: 2 Hz to 4 Hz (for enamel); 1 Hz to 3 Hz (for dentine) cooling method: water spray Control: drill in high‐speed and low‐speed water‐cooled handpieces | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The decision as to which tooth should be prepared by laser or mechanical means and the sequence of treatment was selected at random by means of a computer program (based on Fortran 77), developed at the Institute of Medical Documentation and Statistics, University of Ulm" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Authors reported "Data were analysed by an independent examiner" but no clear statement on the blinding of the outcome assessor procedure was provided |
| Incomplete outcome data (attrition bias) | Unclear risk | For the outcome participant discomfort "The scoring of 13 participants was excluded from the study due to incomplete data" |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. The primary outcome caries removal was not reported |
| Other bias | Unclear risk | It was unclear whether the study was funded or not |
| Methods | Design: split‐mouth randomised controlled clinical trial Centres: 1 Date: not reported Setting: secondary care Operators: 1 single experienced paediatric dentist | |
| Participants | Setting: Hospital Paediatric Dental Clinic Geographical area: Taiwan Sample: 40 children, 40 teeth, 80 cavities (40 in laser group versus 40 in drill group) Age: 3.5 to 12 years Sex: males 50% Baseline: children with 2 primary maxillary anterior teeth affected by caries requiring Black's Class III or IV cavities preparation for its removal. Caries was clinically diagnosed, whereas pulpal vitality was assessed by means of intraoral X‐ray Inclusion criteria: 2 upper incisive carious teeth having the same type of primary caries lesion (Black's Class III or IV) and approximately equal‐sized cavities Exclusion criteria: teeth with pathological condition other than dental caries or with evidence of periapical radiolucency found in the intraoral X‐ray | |
| Interventions | Intervention: Er:YAG laser: wavelength: 2.94 μm pulse energy: 700 mJ pulse duration: not reported pulse frequency: 10 Hz cooling method: water Control: conventional high‐speed dental handpiece | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence of treatment was selected at random by means of flipping a coin |
| Allocation concealment (selection bias) | Unclear risk | Participants or investigators enrolling participants could possibly foresee assignments since the random sequence was generated by means of flipping a coin |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | No apparent attrition |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. The primary outcome caries removal was not reported |
| Other bias | High risk | Quote: "This study was supported by the Taipei Veterans General Hospital, Taiwan (grant VGH91‐73), to whom we extend our thanks" |
| Methods | Design: split‐mouth randomised controlled clinical trial Centres: 1 Date: not reported Setting: secondary care Operators: 1 single experienced dentist | |
| Participants | Setting: University School of Dentistry Clinic Geographical area: Turkey Sample: 27 participants; 54 teeth; 108 cavities (54 in laser group versus 54 in drill group) Age: 19 to 21 years Sex: males 22% Baseline: participants with first and second permanent molars affected by non‐cavitated enamel caries. These lesions were assessed by visual inspection and a laser fluorescence device (DIAGNOdent) as well as by bitewing radiography. Visual inspections were performed with participants positioned in a dental chair, with reflector light, air/water spray and a plane buccal mirror Inclusion criteria: first and second permanent molars with at least 2 active occlusal non‐cavitated superficial carious lesions Exclusion criteria: frank occlusal cavitation, poor oral hygiene, serious systemic diseases and bruxism | |
| Interventions | Intervention: Er,Cr:YSGG laser: wavelength: 2.780 μm pulse energy: 275 mJ (for enamel) pulse frequency: 20 Hz pulse duration: 140 μsec cooling method: air water Control: diamond bur in high‐speed handpiece | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Distribution of the cavity preparation techniques per tooth was done using a table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement of 'low risk' or 'high risk' |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow the performance of blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Evaluation was done by 2 other independent investigators not involved with the treatment procedures using a mirror, explorer and air stream. The investigators were calibrated to a predetermined level of inter‐ and intra‐examiner agreement at least 95% per single criterion. Any discrepancy between evaluators was resolved at chairside |
| Incomplete outcome data (attrition bias) | Low risk | No apparent attrition |
| Selective reporting (reporting bias) | High risk | The study protocol was not available. The primary outcomes, caries removal and episodes of pain, were not reported |
| Other bias | Unclear risk | It was unclear whether the study was funded or not |
| Methods | Design: split‐mouth randomised controlled clinical trial Centres: 1 Date: 2009 to 2011; the months were not reported Setting: secondary care Operators: treatments were provided by 1 doctor | |
| Participants | Setting: University School of Dentistry Clinic Geographical area: China Sample: 53 children; 120 teeth Age: 3 to 15 years; mean age 8.6 years (SD 3.1) Sex: males 40% Baseline: participants with primary and permanent, anterior and molar teeth affected by unclassified caries in terms of dental surface location. The lesions depth varied by enamel to shallow or deep dentine. Methods used for caries diagnosis were not described. There was also a lack of information about pulpal vitality of decayed teeth Inclusion criteria: children who were generally healthy and had 2 teeth with caries of equivalent degree Exclusion criteria: clinical or radiological signs, or both of pulp infection involving tested teeth | |
| Interventions | Intervention: Er:YAG laser: wavelength: 2.94 μm pulse energy: 100 mJ to 700 mJ pulse duration: 450 μsec repetition rate: 5 Hz to 20 Hz cooling method: water/air Control: sterile hand excavator and traditional drill in handpiece | |
| Outcomes | Primary outcomes
Secondary outcomes
| |
| Notes |
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Teeth were randomly assigned to either group by a coin toss |
| Allocation concealment (selection bias) | Unclear risk | Investigators enrolling participants could possibly foresee assignments given that the method used for assignment was based on a coin toss |
| Blinding of participants and personnel (performance bias) | High risk | The type of intervention does not allow blinding of the personnel. However, authors reported that children were unaware of the method of preparation of cavities |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcomes were evaluated by the investigator and by an "an independent evaluator" but no clear statement on the blinding procedure was provided |
| Incomplete outcome data (attrition bias) | Unclear risk | 1 out of 60 teeth in laser group was reassigned into the bur group because the child refused laser treatment. Of 32 recalled children, at 6 months' visit 4 children dropped out, and at 12 months' visit a further 8 children were lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available. The primary outcome caries removal was reported in the methods but no data was provided |
| Other bias | Unclear risk | It was unclear whether the study was funded or not |
Er,Cr:YSGG: erbium, chromium: yttrium‐scandium‐gallium‐garnet.
Er:YAG: erbium‐doped yttrium aluminium garnet.
Nd:YAG: neodymium‐doped yttrium aluminium garnet.
SD: standard deviation.
WHO: World Health Organization.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This study is a controlled clinical trial | |
| The allocation depended on the availability of laser instrumentation. Consequently, the study was considered not randomised and finally excluded | |
| The allocation depended on the availability of laser instrumentation. Consequently, the study was considered not randomised and finally excluded. Quote: "The laser‐treated participant population was randomised by availability of laser instrumentation" | |
| The study was a continuation of Cozean 1998a. It was unclear which participants were allocated to the treatment group. However, the allocation depended on the availability of laser instrumentation. Consequently, the study was considered not randomised and finally excluded. Quote: "Randomization was achieved by the availability of the laser instrumentation" | |
| Incorrect unit of analysis: "..each cavity was divided into two areas that were randomly treated either with the fluorescence controlled Er:YAG laser or with rotary burs" | |
| A narrative review regarding the applications of lasers in restorative dentistry, including a comparison of the applications of lasers for major restorative dental procedures and conventional clinical approaches | |
| This was an in vitro study with the objective of determining the caries‐removal effectiveness and minimal‐invasiveness potential of traditional and innovative tooth ablation techniques | |
| The allocation depended on the availability of laser instrumentation. Consequently, the study was considered not randomised and finally excluded | |
| In vitro study that aimed to determine the effect of 3 different caries removal procedures on micro‐tensile bond strength of decayed human dentine | |
| This poster presentation was potentially eligible. However, the data were insufficient for use in analysis, and attempts to identify any subsequent full‐text or to contact the authors failed | |
| This poster presentation was potentially eligible. However, the data were insufficient for use in analysis, and attempts to identify any subsequent full‐text or to contact the authors failed. |
Er:YAG: erbium‐doped yttrium aluminium garnet.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Unclear |
| Participants | 20 children with at least 2 active occlusal caries lesions with dentine cavitation on the surface of counterparts primary molars |
| Interventions | (I) Er:YAG laser (250 mJ I 4 Hz) (II) Conventional method (high‐speed turbine and low‐speed rotation) |
| Outcomes |
|
| Notes |
Er:YAG: erbium‐doped yttrium aluminium garnet.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Caries removal (clinical) Show forest plot | 2 | Risk Ratio (Random, 95% CI) | 1.00 [0.99, 1.01] | |
| Analysis 1.1  Comparison 1 Laser versus standard drill, Outcome 1 Caries removal (clinical). | ||||
| 2 Pain Show forest plot | 3 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Laser versus standard drill, Outcome 2 Pain. | ||||
| 2.1 6‐face rating scale (moderate and high pain) | 2 | Risk Ratio (Random, 95% CI) | 0.40 [0.28, 0.57] | |
| 2.2 Modified simple 4‐face scale | 1 | Risk Ratio (Random, 95% CI) | 0.21 [0.11, 0.42] | |
| 3 Marginal integrity of restorations Show forest plot | 3 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 Laser versus standard drill, Outcome 3 Marginal integrity of restorations. | ||||
| 3.1 6 months follow‐up | 3 | Risk Ratio (Random, 95% CI) | 1.0 [0.21, 4.78] | |
| 3.2 1 year follow‐up | 2 | Risk Ratio (Random, 95% CI) | 1.59 [0.34, 7.38] | |
| 3.3 2 years follow‐up | 1 | Risk Ratio (Random, 95% CI) | 1.0 [0.21, 4.74] | |
| 4 Durability of restoration Show forest plot | 4 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Laser versus standard drill, Outcome 4 Durability of restoration. | ||||
| 4.1 6 months follow‐up | 4 | Risk Ratio (Random, 95% CI) | 2.40 [0.65, 8.77] | |
| 4.2 1 year follow‐up | 2 | Risk Ratio (Random, 95% CI) | 1.40 [0.29, 6.78] | |
| 4.3 2 years follow‐up | 1 | Risk Ratio (Random, 95% CI) | 0.50 [0.02, 14.60] | |
| 5 Pulpal inflammation or necrosis Show forest plot | 4 | Risk Ratio (Random, 95% CI) | 1.29 [0.32, 5.14] | |
| Analysis 1.5  Comparison 1 Laser versus standard drill, Outcome 5 Pulpal inflammation or necrosis. | ||||
| 5.1 1 week | 3 | Risk Ratio (Random, 95% CI) | 1.51 [0.26, 8.75] | |
| 5.2 6 months | 2 | Risk Ratio (Random, 95% CI) | 0.99 [0.10, 9.41] | |
| 6 Participant discomfort (3‐degree rating scale) Show forest plot | 1 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Laser versus standard drill, Outcome 6 Participant discomfort (3‐degree rating scale). | ||||
| 6.1 Very uncomfortable | 1 | Risk Ratio (Random, 95% CI) | 0.04 [0.01, 0.32] | |
| 6.2 Uncomfortable | 1 | Risk Ratio (Random, 95% CI) | 0.50 [0.33, 0.75] | |
| 7 Participant discomfort (5‐degree rating scale) Show forest plot | 1 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 Laser versus standard drill, Outcome 7 Participant discomfort (5‐degree rating scale). | ||||
| 7.1 Mild discomfort | 1 | Risk Ratio (Random, 95% CI) | 0.12 [0.01, 2.32] | |
| 7.2 Moderate discomfort | 1 | Risk Ratio (Random, 95% CI) | 0.33 [0.04, 3.12] | |
| 8 Need for anaesthesia Show forest plot | 4 | Risk Ratio (Random, 95% CI) | 0.37 [0.19, 0.72] | |
| Analysis 1.8  Comparison 1 Laser versus standard drill, Outcome 8 Need for anaesthesia. | ||||
| 8.1 Children | 3 | Risk Ratio (Random, 95% CI) | 0.25 [0.10, 0.65] | |
| 8.2 Adults | 1 | Risk Ratio (Random, 95% CI) | 0.55 [0.21, 1.42] | |
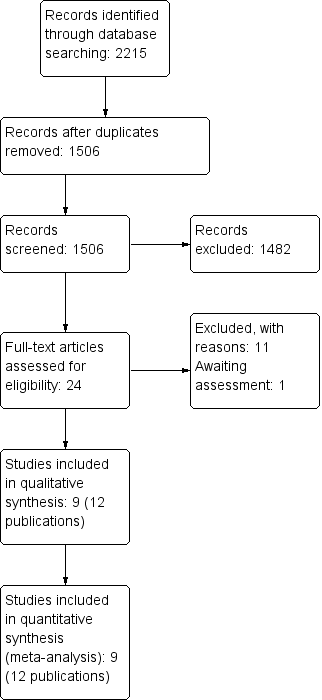
Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
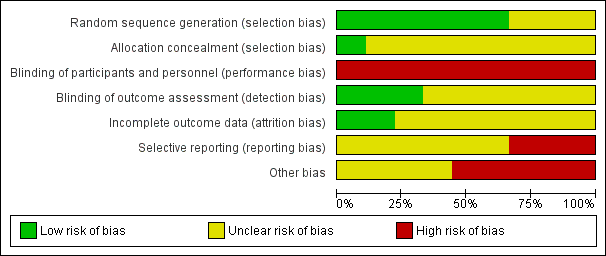
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Forest plot of comparison: 1 Laser versus standard drill, outcome: 1.1 Caries removal (clinical).

Forest plot of comparison: 1 Laser versus standard drill, outcome: 1.2 Pain.

Forest plot of comparison: 1 Laser versus standard drill, outcome: 1.4 Durability of restoration.

Forest plot of comparison: 1 Laser versus standard drill, outcome: 1.5 Pulpal inflammation or necrosis.

Forest plot of comparison: 1 Laser versus standard drill, outcome: 1.8 Need for anaesthesia.

Comparison 1 Laser versus standard drill, Outcome 1 Caries removal (clinical).

Comparison 1 Laser versus standard drill, Outcome 2 Pain.
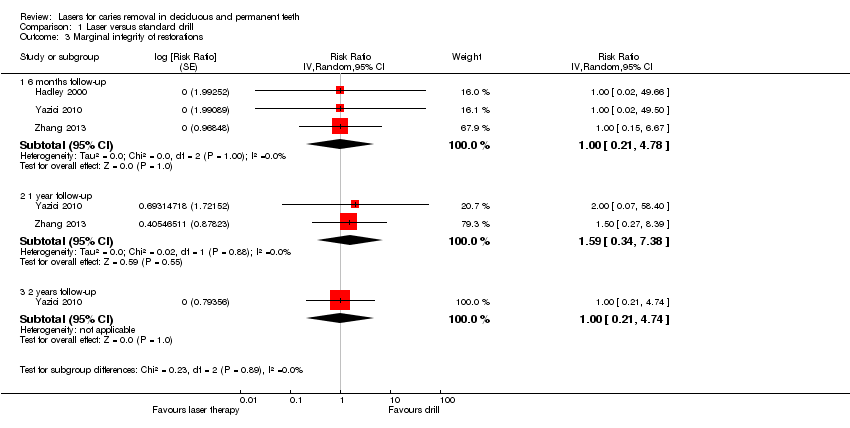
Comparison 1 Laser versus standard drill, Outcome 3 Marginal integrity of restorations.
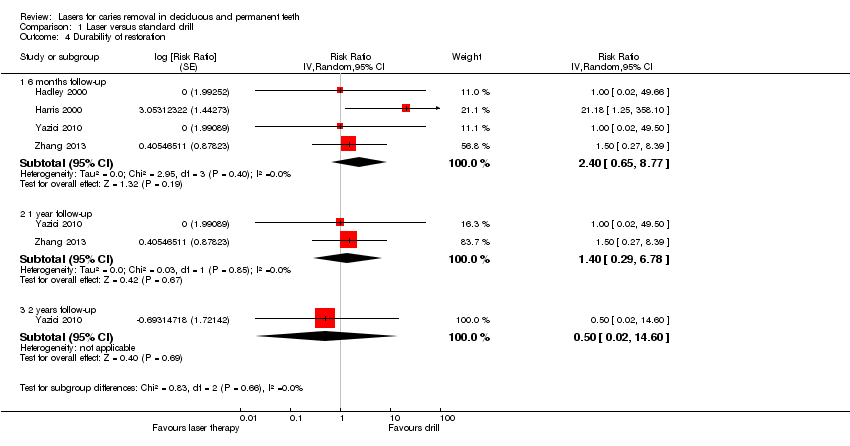
Comparison 1 Laser versus standard drill, Outcome 4 Durability of restoration.

Comparison 1 Laser versus standard drill, Outcome 5 Pulpal inflammation or necrosis.
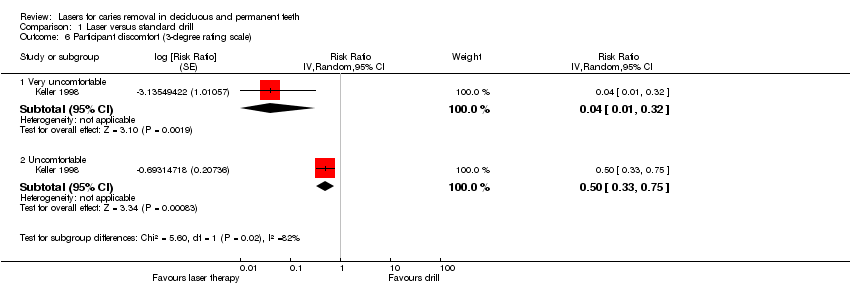
Comparison 1 Laser versus standard drill, Outcome 6 Participant discomfort (3‐degree rating scale).

Comparison 1 Laser versus standard drill, Outcome 7 Participant discomfort (5‐degree rating scale).
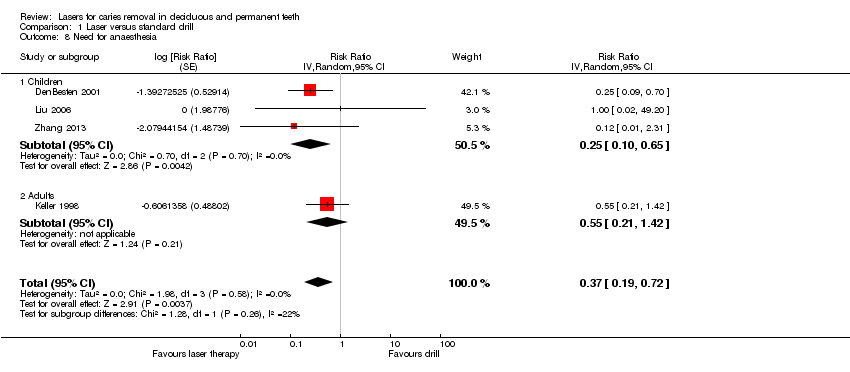
Comparison 1 Laser versus standard drill, Outcome 8 Need for anaesthesia.
| Laser compared to standard drill for caries removal in deciduous and permanent teeth | ||||||
| Patient or population: people with caries in deciduous and permanent teeth | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard drill | Laser | |||||
| Caries removal (during treatment) | 995 per 1000 | 995 per 1000 | RR 1.00 | 190 participants; 256 teeth; 256 cavity preparations | ⊕⊕⊝⊝ | |
| Pain ‐ 6‐face rating scale (moderate and high pain) (during treatment) | 760 per 1000 | 304 per 1000 | RR 0.40 | 143 participants | ⊕⊕⊝⊝ | |
| Need for anaesthesia ‐ children (during treatment) | 97 per 1000 | 24 per 1000 | RR 0.25 | 217 participants | ⊕⊕⊝⊝ | |
| Durability of restoration ‐ 6 months follow‐up | 8 per 1000 | 20 per 1000 | RR 2.40 | 236 participants; 682 teeth | ⊕⊕⊝⊝ | |
| Marginal integrity of restorations ‐ 6 months follow‐up | 7 per 1000 | 7 per 1000 | RR 1.00 | 146 participants; 306 teeth | ⊕⊕⊝⊝ | |
| Pulpal inflammation or necrosis ‐ 1 week follow‐up | 5 per 1000 | 7 per 1000 | RR 1.51 | 317 participants; 694 teeth; 752 cavity preparations | ⊕⊕⊝⊝ | |
| Pulpal inflammation or necrosis ‐ 6 months follow‐up | 4 per 1000 | 4 per 1000 | RR 0.99 | 156 participants; 508 teeth; 554 cavity preparations | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1The evidence was downgraded by two levels because of very serious concern regarding the risk of bias: (1) the two studies did not report sufficient information regarding the allocation concealment (DenBesten 2001; Hadley 2000); (2) both studies were at high risk of performance bias; (3) neither of the two studies was at low risk of selective reporting bias; (4) serious concern related to funding (other bias). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Caries removal (clinical) Show forest plot | 2 | Risk Ratio (Random, 95% CI) | 1.00 [0.99, 1.01] | |
| 2 Pain Show forest plot | 3 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 6‐face rating scale (moderate and high pain) | 2 | Risk Ratio (Random, 95% CI) | 0.40 [0.28, 0.57] | |
| 2.2 Modified simple 4‐face scale | 1 | Risk Ratio (Random, 95% CI) | 0.21 [0.11, 0.42] | |
| 3 Marginal integrity of restorations Show forest plot | 3 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 3.1 6 months follow‐up | 3 | Risk Ratio (Random, 95% CI) | 1.0 [0.21, 4.78] | |
| 3.2 1 year follow‐up | 2 | Risk Ratio (Random, 95% CI) | 1.59 [0.34, 7.38] | |
| 3.3 2 years follow‐up | 1 | Risk Ratio (Random, 95% CI) | 1.0 [0.21, 4.74] | |
| 4 Durability of restoration Show forest plot | 4 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 4.1 6 months follow‐up | 4 | Risk Ratio (Random, 95% CI) | 2.40 [0.65, 8.77] | |
| 4.2 1 year follow‐up | 2 | Risk Ratio (Random, 95% CI) | 1.40 [0.29, 6.78] | |
| 4.3 2 years follow‐up | 1 | Risk Ratio (Random, 95% CI) | 0.50 [0.02, 14.60] | |
| 5 Pulpal inflammation or necrosis Show forest plot | 4 | Risk Ratio (Random, 95% CI) | 1.29 [0.32, 5.14] | |
| 5.1 1 week | 3 | Risk Ratio (Random, 95% CI) | 1.51 [0.26, 8.75] | |
| 5.2 6 months | 2 | Risk Ratio (Random, 95% CI) | 0.99 [0.10, 9.41] | |
| 6 Participant discomfort (3‐degree rating scale) Show forest plot | 1 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 6.1 Very uncomfortable | 1 | Risk Ratio (Random, 95% CI) | 0.04 [0.01, 0.32] | |
| 6.2 Uncomfortable | 1 | Risk Ratio (Random, 95% CI) | 0.50 [0.33, 0.75] | |
| 7 Participant discomfort (5‐degree rating scale) Show forest plot | 1 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 7.1 Mild discomfort | 1 | Risk Ratio (Random, 95% CI) | 0.12 [0.01, 2.32] | |
| 7.2 Moderate discomfort | 1 | Risk Ratio (Random, 95% CI) | 0.33 [0.04, 3.12] | |
| 8 Need for anaesthesia Show forest plot | 4 | Risk Ratio (Random, 95% CI) | 0.37 [0.19, 0.72] | |
| 8.1 Children | 3 | Risk Ratio (Random, 95% CI) | 0.25 [0.10, 0.65] | |
| 8.2 Adults | 1 | Risk Ratio (Random, 95% CI) | 0.55 [0.21, 1.42] | |

