Abordaje de la arteria femoral totalmente percutáneo versus disección quirúrgica para la reparación endovascular programada del aneurisma abdominal bifurcado
Información
- DOI:
- https://doi.org/10.1002/14651858.CD010185.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 21 febrero 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Vascular
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
MG: was responsible for trial selection, data extraction, data analysis, and writing the review update
AJ: was responsible for drafting the protocol, trial selection, data extraction, and data analysis in the previous review, and for trial selection and data extraction in this review
SEY: was responsible for trial selection and data extraction in the previous review
MC: was responsible for reviewing the draft protocol and draft review
Sources of support
Internal sources
-
University of Southampton National Institute of Health Research Academic Foundation Programme, UK.
AIRJ was supported by the University of Southampton National Institute of Health Research Academic Foundation Programme.
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK.
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
-
National Insitute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Programme Grant funding to Cochrane Vascular (13/89/23). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
MG: none known
AJ: has declared that he received travel and accommodation expenses for attendance of the Technologies in Endovascular Aortic Repair conference, December 2015. Funding was directly from the conference organisers and enabled an oral presentation of a previous iteration of this review. No other declarations of interest are known
SEY: none known
MC: none known
Acknowledgements
The authors would like to thank all the staff at Cochrane Vascular for all their help, support and patience throughout this review process.
Version history
| Published | Title | Stage | Authors | Version |
| 2023 Jan 11 | Totally percutaneous versus surgical cut‐down femoral artery access for elective bifurcated abdominal endovascular aneurysm repair | Review | Qi Wang, Jing Wu, Yanfang Ma, Ying Zhu, Xiaoyang Song, Shitong Xie, Fuxiang Liang, Madelaine Gimzewska, Meixuan Li, Liang Yao | |
| 2017 Feb 21 | Totally percutaneous versus surgical cut‐down femoral artery access for elective bifurcated abdominal endovascular aneurysm repair | Review | Madelaine Gimzewska, Alexander IR Jackson, Su Ern Yeoh, Mike Clarke | |
| 2014 Feb 27 | Totally percutaneous versus standard femoral artery access for elective bifurcated abdominal endovascular aneurysm repair | Review | Alexander Jackson, Su Ern Yeoh, Mike Clarke | |
| 2012 Nov 14 | Totally percutaneous versus standard femoral artery access for elective bifurcated abdominal endovascular aneurysm repair | Protocol | Alexander Jackson, Su Ern Yeoh, Mike Clarke | |
Differences between protocol and review
The outcome 'Bleeding complications and haematoma' was added to the original review.
The outcome 'Duration of hospital stay' was added to this version of the review.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Humans;
PICO

Study flow diagram

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
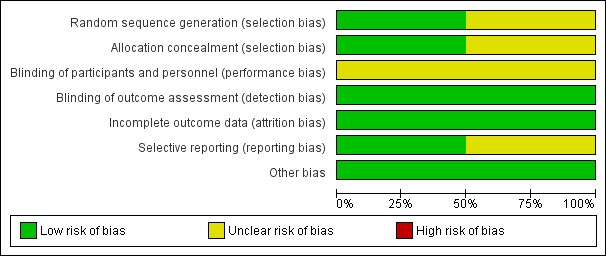
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Comparison 1 Percutaneous vs cut‐down femoral artery access, Outcome 1 Short‐term mortality rate (30‐day or in‐hospital).

Comparison 1 Percutaneous vs cut‐down femoral artery access, Outcome 2 Aneurysm exclusion.

Comparison 1 Percutaneous vs cut‐down femoral artery access, Outcome 3 Major complications.

Comparison 1 Percutaneous vs cut‐down femoral artery access, Outcome 4 Major complications (6 months).
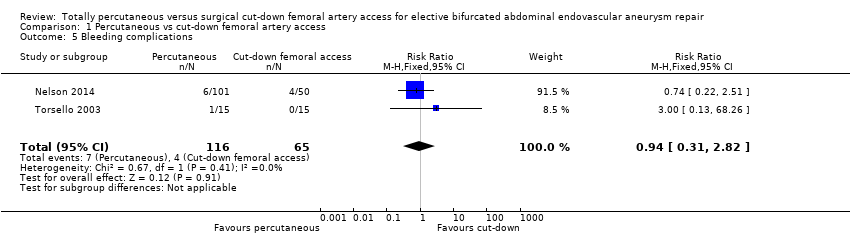
Comparison 1 Percutaneous vs cut‐down femoral artery access, Outcome 5 Bleeding complications.

Comparison 1 Percutaneous vs cut‐down femoral artery access, Outcome 6 Operating time (minutes).
| Totally percutaneous compared to cut‐down femoral artery access for elective bifurcated abdominal endovascular aneurysm repair | ||||||
| Patient or population: people undergoing elective bifurcated abdominal endovascular aneurysm repair | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with cut‐down femoral artery access | Risk with totally percutaneous | |||||
| Short‐term mortality rate (30‐day or in‐hospital) | See comment | See comment | RR 1.50 | 181 | ⊕⊕⊕⊝ | It was not possible to calculate risk as only one event occurred. Note that although 2 RCTs included, only one contributes to effect estimate (no events in Torsello 2003) |
| Failure of aneurysm exclusion | Study population | RR 0.17 (0.01 to 4.02) | 151 | ⊕⊕⊕⊝ | ||
| 20 per 1000 | 3 per 1000 | |||||
| Wound infection rate (30‐day or in‐hospital) | See comment | See comment | not estimable | 181 | ⊕⊕⊕⊝ | Risk and relative effect were not estimable as no events occurred |
| Major complications (30‐day or in‐hospital) | Study population | RR 0.91 | 181 | ⊕⊕⊕⊝ | ||
| 200 per 1000 | 182 per 1000 | |||||
| Long term complications | Study population | RR 1.03 | 134 | ⊕⊕⊕⊝ | ||
| 95 per 1000 | 98 per 1000 | |||||
| Bleeding complications and haematoma (30‐day or in‐hospital) | Study population | RR 0.94 | 181 | ⊕⊕⊕⊕ | ||
| 62 per 1000 | 58 per 1000 | |||||
| Operating time (minutes) | The mean operating time was 99 minutes | The mean operating time in the intervention group was 31.46 minutes lower (47.51 lower to 15.42 lower) | ‐ | 181 | ⊕⊕⊕⊝ | |
| * The basis for the assumed risk for 'Study population' was the average risk in the comparison group (i.e. total number of participants with events divided by the total number of participants in the comparison group included in the meta‐analysis. The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) and calculated where possible from the data provided in the studies. | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We downgraded by one level due to the low number of events and imprecision (wide confidence intervals include both harm and benefit) | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Short‐term mortality rate (30‐day or in‐hospital) Show forest plot | 2 | 181 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.06, 36.18] |
| 2 Aneurysm exclusion Show forest plot | 1 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.01, 4.02] |
| 3 Major complications Show forest plot | 2 | 181 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.50, 1.68] |
| 4 Major complications (6 months) Show forest plot | 1 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.34, 3.15] |
| 5 Bleeding complications Show forest plot | 2 | 181 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.31, 2.82] |
| 6 Operating time (minutes) Show forest plot | 2 | 181 | Mean Difference (IV, Fixed, 95% CI) | ‐31.46 [‐47.51, ‐15.42] |

