تاثیر استفاده از درناژ شکمی برای پیشگیری از آبسههای داخل صفاقی پس از آپاندکتومی باز در آپاندیسیتهای عارضهدار
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomised controlled trial | |
| Participants | Country: India Adults: 70 (81%) Normal appendix: 0 (0%) Simple appendicitis: 0 (0%) Gangrenous appendicitis: 0 (0%) Perforated appendicitis: 86 (100%) Appendiceal phlegmon or abscess: 0 (0%)
Exclusion criteria:
| |
| Interventions | Participants with complicated appendicitis (n = 86) were randomly assigned to 2 groups | |
| Outcomes | The outcomes reported were wound infection, intra‐peritoneal abscess, duration of postoperative fever, postoperative complications, mortality, and hospital stay | |
| Notes | The drainage tube (corrugated rubber drain) was placed down into the right iliac fossa | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no post‐randomisation dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: all of the primary outcomes were reported. There was some selective outcome reporting in the secondary outcomes, but the review authors considered this trial to be free of selective reporting for the primary outcomes |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
| Methods | Quasi‐randomised controlled trial | |
| Participants | Country:USA Adults: 0 (0%) Normal appendix: 0 (0%) Simple appendicitis: 0 (0%) Gangrenous appendicitis: 0 (0%) Perforated appendicitis: 43 (100%) Appendiceal phlegmon or abscess: 0 (0%)
Exclusion criteria:
| |
| Interventions | Participants with complicated appendicitis (n = 43) were randomly assigned to 2 groups | |
| Outcomes | The outcomes reported were intra‐peritoneal abscess, postoperative complications, mortality, and hospital stay | |
| Notes | The drainage tube (Penrose drain) was placed through the wound down into the right iliac fossa and pelvis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Transperitoneal drainage was used in children with even hospital numbers and no drainage or wound drainage alone was used in children with odd hospital numbers" Comment: the allocation was performed on the basis of a pseudo‐random sequence (odd/even hospital number) |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no post‐randomisation dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: all of the primary outcomes were reported. There was some selective outcome reporting in the secondary outcomes, but the review authors considered this trial to be free of selective reporting for the primary outcomes |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
| Methods | Randomised controlled trial | |
| Participants | Country: Kenya Age (27 to 54): 46 (51%) Normal appendix: 0 Simple appendicitis: 0 Gangrenous appendicitis: 0 (0%) Perforated appendicitis: 79 (87.8%) Appendiceal phlegmon or abscess: 11 (12.2%)
Exclusion criteria:
| |
| Interventions | Participants with complicated appendicitis (n = 90) were randomly assigned to 2 groups | |
| Outcomes | The outcomes reported were wound infection, intra‐peritoneal abscess, morbidity, postoperative complications, hospital stay, and duration of antibiotic use | |
| Notes | The drainage tube (PVC suction catheter) was placed through a separate incision down into the right iliac fossa | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no post‐randomisation dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: all of the primary outcomes were reported. There was some selective outcome reporting in the secondary outcomes, but the review authors considered this trial to be free of selective reporting for the primary outcomes |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
| Methods | Randomised controlled trial | |
| Participants | Country: Pakistan Age (26 to 33): 26 (38%) Age (34 to 39): 11 (16%) Normal appendix: 0 Simple appendicitis: 0 Gangrenous appendicitis: 0 (0%) Perforated appendicitis: 68 (100%) Appendiceal phlegmon or abscess: 0 (0%)
Exclusion criteria:
| |
| Interventions | Participants with complicated appendicitis (n = 68) were randomly assigned to 2 groups | |
| Outcomes | The outcomes reported were wound infection and hospital stay | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "These patients were randomly allocated into 2 treatment groups using lottery method" Comment: no information provided about the method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no post‐randomisation dropouts |
| Selective reporting (reporting bias) | High risk | Comment: the primary outcome was not reported |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
| Methods | Quasi‐randomised controlled trial | |
| Participants | Country: USA Adults: not mentioned Normal appendix: 0 (0%) Simple appendicitis: 66 (23%) Suppurative appendicitis: 123 (44%) Gangrenous appendicitis: 32 (11%) Perforated appendicitis: 62 (22%) Appendiceal phlegmon or abscess: 0 (0%)
Exclusion criteria:
| |
| Interventions | Participants with complicated appendicitis (n = 94) were randomly assigned to 2 groups | |
| Outcomes | The outcomes reported were wound infection, intra‐peritoneal abscess, postoperative complications, and mortality | |
| Notes | The drainage tube (Penrose drain) was placed through a separate incision down into the right iliac fossa | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "A Penrose drain was inserted through a separate stab wound if the final digit of the patient's hospital number was an odd figure. An even final digit dictated exclusion of any form of peritoneal drainage". Comment: the allocation was performed on the basis of a pseudo‐random sequence (odd/even hospital number) |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no post‐randomisation dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: all of the primary outcomes were reported. There was some selective outcome reporting in the secondary outcomes, but the review authors considered this trial to be free of selective reporting for the primary outcomes |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
| Methods | Randomised controlled trial | |
| Participants | Country: Turkey Number randomised: 140 Adults: 0 (0%) Normal appendix: 0 (0%) Simple appendicitis: 0 (0%) Gangrenous appendicitis: 0 (0%) Perforated appendicitis: 140 (100%) Appendiceal phlegmon or abscess: 0 (0%)
Exclusion criteria:
| |
| Interventions | Participants with complicated appendicitis (n = 140) were randomly assigned to 2 groups | |
| Outcomes | The outcomes reported were wound infection, intra‐peritoneal abscess, postoperative complications, mortality, hospital stay, and duration before oral intake | |
| Notes | 2 drainage tubes (Penrose drains) were placed through the wound down into the right iliac fossa and pelvis, respectively | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: no information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: no information provided |
| Incomplete outcome data (attrition bias) | Low risk | Comment: there were no post‐randomisation dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: all of the primary outcomes were reported. There was some selective outcome reporting in the secondary outcomes, but the review authors considered this trial to be free of selective reporting for the primary outcomes |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| A non‐randomised study | |
| A non‐randomised study | |
| A non‐randomised study | |
| Randomised controlled trial about extraperitoneal wound drainage (wound drainage versus no wound drainage) | |
| A non‐randomised study | |
| Randomised controlled trial in which antibiotic regimens were used in a non‐random manner | |
| A non‐randomised study | |
| Randomised controlled trial in which antibiotic regimens were used in a non‐random manner | |
| A non‐randomised study | |
| A non‐randomised study | |
| A non‐randomised study | |
| Randomised controlled trial about peritoneal lavage versus abdominal drainage |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐peritoneal abscess Show forest plot | 5 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.47, 3.21] |
| Analysis 1.1 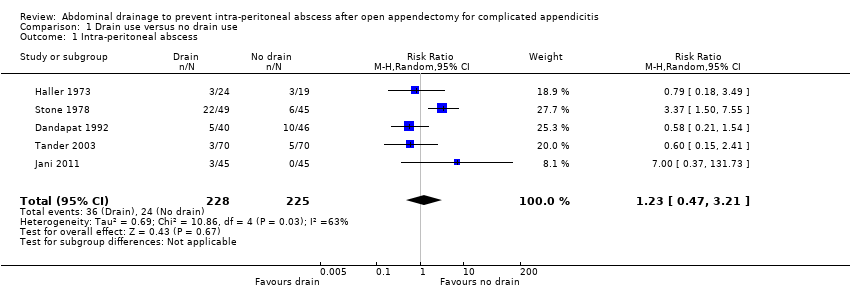 Comparison 1 Drain use versus no drain use, Outcome 1 Intra‐peritoneal abscess. | ||||
| 2 Wound infection Show forest plot | 5 | 478 | Risk Ratio (M‐H, Random, 95% CI) | 2.01 [0.88, 4.56] |
| Analysis 1.2  Comparison 1 Drain use versus no drain use, Outcome 2 Wound infection. | ||||
| 3 Morbidity Show forest plot | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 6.67 [2.13, 20.87] |
| Analysis 1.3  Comparison 1 Drain use versus no drain use, Outcome 3 Morbidity. | ||||
| 4 Mortality Show forest plot | 4 | 363 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 4.88 [1.18, 20.09] |
| Analysis 1.4  Comparison 1 Drain use versus no drain use, Outcome 4 Mortality. | ||||
| 5 Hospital stay Show forest plot | 3 | 298 | Mean Difference (IV, Random, 95% CI) | 2.17 [1.76, 2.58] |
| Analysis 1.5 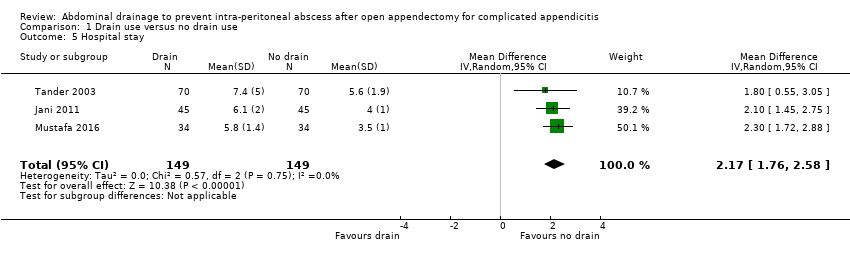 Comparison 1 Drain use versus no drain use, Outcome 5 Hospital stay. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐peritoneal abscess Show forest plot | 3 | 316 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.28, 2.02] |
| Analysis 2.1  Comparison 2 Drain use versus no drain use (sensitivity analyses by excluding quasi‐randomised trials), Outcome 1 Intra‐peritoneal abscess. | ||||
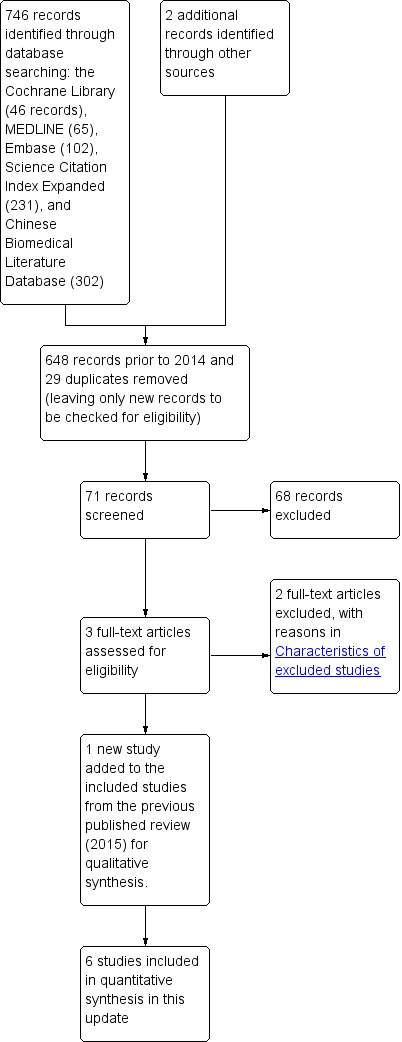
Study flow diagram.
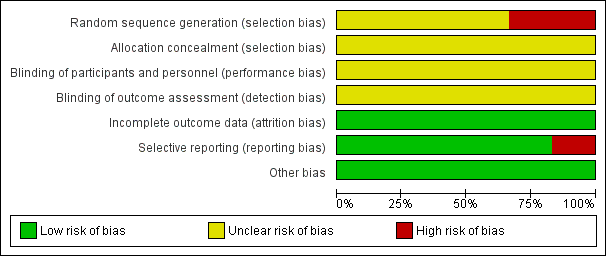
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Trial sequential analysis of drain use versus no drain use for intra‐peritoneal abscess. Analysis was performed with an event rate of 10.7% (Pc) in the control group, a risk ratio reduction of 20%, alpha 5%, beta 20%, and observed diversity 63%. The cumulative Z‐curve did not cross the trial sequential boundaries (inward sloping etched lines). The results showed that the observed diversity‐adjusted required information size was 2,570 participants, corresponding to 20.3% of the total sample size in the included trials. Accordingly, the meta‐analysis did not support or refute an intervention effect as data were too few.

Comparison 1 Drain use versus no drain use, Outcome 1 Intra‐peritoneal abscess.

Comparison 1 Drain use versus no drain use, Outcome 2 Wound infection.

Comparison 1 Drain use versus no drain use, Outcome 3 Morbidity.

Comparison 1 Drain use versus no drain use, Outcome 4 Mortality.

Comparison 1 Drain use versus no drain use, Outcome 5 Hospital stay.

Comparison 2 Drain use versus no drain use (sensitivity analyses by excluding quasi‐randomised trials), Outcome 1 Intra‐peritoneal abscess.
| Abdominal drainage to prevent intra‐peritoneal abscess after open appendectomy for complicated appendicitis | ||||||
| Patient or population: people undergoing emergency open appendectomy for complicated appendicitis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Risk with no drain use | Risk with drain use | |||||
| Intra‐peritoneal abscess Follow‐up: 14 days | 107 per 1000 | 131 per 1000 | RR 1.23 | 453 | ⊕⊝⊝⊝ | |
| Wound infection Follow‐up: 30 days | 254 per 1000 | 511 per 1000 | RR 2.01 | 478 | ⊕⊝⊝⊝ | |
| Morbidity Follow‐up: 30 days | 67 per 1000 | 445 per 1000 | RR 6.67 | 90 | ⊕⊝⊝⊝ | |
| Mortality Follow‐up: 30 days month | 6 per 1000 | 27 per 1000 | Peto OR 4.88 | 363 | ⊕⊕⊕⊝ | |
| Hospital stay (days) | The mean hospital stay in the control groups was 4.60 days | The mean hospital stay in the intervention groups was | MD 2.17 days higher | 298 | ⊕⊝⊝⊝ | |
| Hospital cost | Not reported | |||||
| Pain | Not reported | |||||
| Quality of life | Not reported | |||||
| *The basis for the assumed risk is the mean comparison group proportion in the studies. The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| a Downgraded two levels for very serious risk of bias. b Downgraded one level for severe inconsistency (substantial heterogeneity as indicated by the I2 statistic). c Downgraded one level for serious imprecision. For abscess, morbidity and infection, the confidence interval includes appreciable benefit and harm, and the sample size is small. For mortality, there are few events (8 deaths in total) d Downgraded one level for serious imprecision (small sample size). | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐peritoneal abscess Show forest plot | 5 | 453 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.47, 3.21] |
| 2 Wound infection Show forest plot | 5 | 478 | Risk Ratio (M‐H, Random, 95% CI) | 2.01 [0.88, 4.56] |
| 3 Morbidity Show forest plot | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 6.67 [2.13, 20.87] |
| 4 Mortality Show forest plot | 4 | 363 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 4.88 [1.18, 20.09] |
| 5 Hospital stay Show forest plot | 3 | 298 | Mean Difference (IV, Random, 95% CI) | 2.17 [1.76, 2.58] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Intra‐peritoneal abscess Show forest plot | 3 | 316 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.28, 2.02] |

