조산아 또는 저체중아의 동맥관 개존증을 위한 파라세타몰(아세트아미노펜)
초록
배경
조산아의 동맥관 개존증(PDA)에 대한 다양한 관리 전략은 기대 관리, 수술 또는 비선택적 사이클로옥시게나제 억제제를 사용한 의학적 치료이다. 무작위 통제 시험(RCT)은 파라세타몰이 PDA 폐쇄를 위한 효과적이고 안전한 약제일 수 있다고 제안했다.
목적
조산아 또는 저체중아에서 심초음파로 진단된 PDA의 예방 또는 치료를 위해 위약, 무중재 또는 다른 프로스타글란딘 억제제와 비교하여 임의의 투여 경로를 통한 단일 요법 또는 병용 요법의 일부로서 파라세타몰의 효능 및 안전성을 결정하기 위함이다.
검색 전략
2021년 10월 13일에 CENTRAL, MEDLINE, Embase 및 3개의 임상시험 등록부를 검색했고 2022년 3월 1일에 다른 데이터베이스 1개를 검색했다. 또한 추가 연구를 확인하기 위해 참고 문헌을 확인하고 연구 저자에게 연락했다.
선정 기준
미숙아의 용량, 기간 및 투여 방식에 관계없이 파라세타몰(단일 제제 또는 병용 요법)을 무중재, 위약 또는 PDA 폐쇄에 사용되는 기타 제제와 비교한 RCT 및 준 RCT를 포함했다. 두 명의 독립적인 저자가 검색 결과를 검토하고 토론을 통해 잠재적으로 적합한 기사를 최종 선택했다.
자료 수집 및 분석
Cochrane Neonatal의 방법에 따라 데이터 수집 및 분석을 수행했다. GRADE 접근법을 사용하여 첫 번째 치료 과정 후 관 폐쇄 실패, 초기 입원 중 모든 원인 사망, 괴사성 장염(NEC)의 결과에 대한 근거의 확실성을 평가했다.
주요 결과
이 업데이트에는 2278명의 유아를 등록한 27개의 연구를 포함했다. 27개 연구에서 비뚤림의 전반적인 위험이 낮음에서 불분명까지 다양하다고 생각했다. 24개의 진행 중인 연구를 확인했다.
파라세타몰 대 이부프로펜
첫 번째 과정 후 관 폐쇄 실패에 대해 파라세타몰과 이부프로펜 사이에 거의 차이가 없었을 것이다(위험비(RR) 1.02, 95% 신뢰 구간(CI) 0.88 ~ 1.18, 18개 연구, 1535명의 유아, 근거 확실성 중간). 입원 중 모든 원인으로 인한 사망(RR 1.09, 95% CI 0.80 ~ 1.48, 8건의 연구, 734명의 영아, 근거 확실성 중간) 및 NEC(RR 1.30, 95 % CI 0.87 ~ 1.94, 10건의 연구, 1015명의 유아, 근거 확실성 중간)에 대해서는 파라세타몰과 이부프로펜 사이에 거의 차이가 없다.
파라세타몰 대 인도메타신
첫 번째 과정 후 관 폐쇄 실패에 대해 파라세타몰과 인도메타신 사이에는 거의 또는 전혀 차이가 없었다(RR 1.02, 95% CI 0.78 ~ 1.33; 4건의 연구, 380명의 유아; 근거 확실성 낮음). 입원 중 모든 원인으로 인한 사망에 대해 파라세타몰과 인도메타신 사이에는 거의 또는 전혀 차이가 없었다(RR 0.86, 95% CI 0.39 ~ 1.92; 2건의 연구, 114명의 영아; 근거 확실성 낮음). NEC의 비율은 인도메타신 그룹(9.2%)에 비해 파라세타몰 그룹(3.7%)에서 더 낮을 수 있다(RR 0.42, 95% CI 0.19 ~ 0.96; 4개 연구, 384명의 유아, 근거 확실성 낮음).
예방적 파라세타몰 대 위약/무중재
위약/무중재(61%)에 비해 예방적 파라세타몰(17%)은 한 과정 후 관 폐쇄 실패를 줄일 수 있다(RR 0.27, 95% CI 0.18 ~ 0.42; 3건의 연구, 240명의 영아; 근거 확실성 낮음). 예방적 파라세타몰과 위약 사이에는 입원 기간 동안 모든 원인으로 인한 사망에 대한 중재/중재가 거의 또는 전혀 차이가 없었다(RR 0.59, 95% CI 0.24 ~ 1.44; 3건의 연구, 240명의 유아; 근거 확실성 낮음). NEC를 보고된 연구는 없다.
초기 파라세타몰 치료 대 위약/무중재
조기 파라세타몰 치료(28%)는 위약/중재 없음(79%)에 비해 출생 후 14일 이전에 사용했을 때 한 과정 후 관 폐쇄 실패를 줄일 수 있다(RR 0.35, 95% CI 0.23 ~ 0.53; 2개 연구, 127명의 유아 ; 낮은 근거 확실성). 입원 또는 NEC 동안 모든 원인으로 인한 사망에 대해 보고된 연구는 없다.
후기 파라세타몰 치료 대 위약/무중재
출생 후 14일 이후에 사용했을 때 1회 치료 과정 후 관 폐쇄 실패에 대해 말기 파라세타몰과 위약 사이(RR 0.85, 95% CI 0.72 ~ 1.01; 1 연구, 55명의 영아; 근거 확실성) 또는 NEC(RR 1.04, 95% CI 0.07~15.76, 1건의 연구, 55명의 영아, 낮은 근거 확실성)에서 차이는 거의 없었다. 입원 중 모든 원인으로 인한 사망에 대한 데이터는 보고되지 않았다.
파라세타몰과 이부프로펜 병용 대 이부프로펜과 위약 병용 또는 중재 없음
파라세타몰과 이부프로펜은 이부프로펜과 위약에 비해 차이가 거의 없거나 첫 번째 과정 후 관 폐쇄 실패에 대한 중재가 없었다(RR 0.77, 95% CI 0.43 ~ 1.36; 2건의 연구, 111명의 유아, 근거 확실성 낮음). 파라세타몰과 이부프로펜은 이부프로펜과 위약 또는 NEC에 대한 중재가 없는 것과 비교하여 차이가 거의 또는 전혀 없었다(RR 0.33, 95% CI 0.01 ~ 7.45; 1건의 연구, 24명의 유아, 근거 확실성 낮음). 입원 중 모든 원인으로 인한 사망에 대한 데이터는 보고되지 않았다.
연구진 결론
중간 정도의 확실성 근거는 파라세타몰과 이부프로펜 사이의 효과에 거의 또는 전혀 차이가 없음을 시사한다. 확실성이 낮은 근거는 파라세타몰과 인도메타신 사이의 효과에 거의 또는 전혀 차이가 없음을 시사한다. 확실성이 낮은 근거는 예방적 파라세타몰이 위약/무중재보다 더 효과적일 수 있음을 시사한다. 확실성이 낮은 근거는 초기 파라세타몰 치료가 위약/무중재보다 더 효과적일 수 있음을 시사합니다. 낮은 확실성 근거는 후기 파라세타몰 치료와 위약 사이에 거의 또는 전혀 차이가 없을 수 있으며 첫 번째 치료 과정 후 PDA 폐쇄에 대해 파라세타몰과 이부프로펜의 조합 대 이부프로펜 단독 사이의 효과에 거의 또는 전혀 차이가 없음을 시사한다. 이 연구에 포함된 대부분의 신생아는 중등도 조산아였다. 따라서 극도로 낮은 출생 체중(ELBW: 출생 체중 < 1000g)과 극도로 낮은 재태 연령 신생아(ELGANs < 28주 임신)에서 PDA 치료를 위한 파라세타몰의 효능과 안전성을 확립하려면 추가 연구가 필요하다.
PICOs
쉬운 말 요약
조산아 및 저체중아의 동맥관 개존(PDA, 태아 생존에 필요한 혈관)에 대한 파라세타몰(아세트아미노펜)의 이점과 위해는 무엇인가?
배경
미숙아(미숙아) 또는 작은 아기의 일반적인 합병증은 동맥관 개존증(PDA)이다. (아직) 기능하지 않는 폐로의 혈액 순환은 출생 전에 불필요하다. 이것은 태반이 태아 혈액 공급에 산소를 공급하기 때문이다. PDA는 폐동맥(출생 후 심장에서 산소가 고갈된 혈액을 심장에서 폐로 보내는 혈관)과 대동맥(폐에서 폐정맥에 의해 심장으로 되돌아오는 신선한 산소가 공급된 혈액을 받는 혈관, 심장에서 멀어지고 몸 주위의 여행 시작)을 연결하는 임시 태아 혈관이다. 즉, PDA는 폐를 통한 태아의 혈액 순환을 '단락'시킨다. 자궁에서 생명을 유지하는 데 필요하지만 출산 후에는 닫혀야 한다. 때때로 PDA는 아기의 미성숙 발달 단계로 인해 열려 있다.
조산아의 PDA는 생명을 위협하는 합병증과 관련이 있다. PDA의 일반적인 치료법은 프로스타글란딘 생성을 억제하고 PDA 폐쇄를 촉진하는 인도메타신 또는 이부프로펜 약물이었다. 프로스타글란딘은 특히 연조직이 손상된 곳에서 전신(즉, 특정 기관이 아님)에서 만들어지는 화학적 화합물이다. 이들의 생성(또는 '합성')은 치유 과정에서 중요한 역할을 한다. 그들은 동맥관을 개방(또는 '특허') 상태로 유지하는 데 중요한 역할을 하는 것으로 알려져 있으므로 생성을 낮추면 동맥관 폐쇄를 촉진할 수 있다.
최근에는 유아, 어린이 및 성인의 발열이나 통증을 치료하는 데 일반적으로 사용되는 파라세타몰(아세트아미노펜)이 잠재적으로 부작용이 적은 이부프로펜의 대안으로 제안되었다. 많은 임상 시험에서 파라세타몰이 PDA 폐쇄의 대안이 될 수 있다고 제안했다. 파라세타몰이 PDA를 닫는 데 정확히 어떻게 작용하는지는 알려져 있지 않지만 아마도 프로스타글란딘 합성의 억제와 관련이 있을 것이다.
무엇을 확인하고 싶었는가?
조산아나 저체중아의 PDA 폐쇄를 위해 위약(활성 치료 효과가 없는 물질), 무중재 또는 비스테로이드성 항염증제(인도메타신 및 이부프로펜)와 비교했을 때 항염증 특성이 약한 파라세타몰이 얼마나 효과적이고 안전한가?
무엇을 했는가?
미숙아 또는 작은 아기의 중요한 PDA를 위해 이부프로펜, 인도메타신, 위약 또는 무중재와 비교하여 단독으로 또는 이부프로펜과 함께 사용된 파라세타몰의 단기(유익 및 안전성) 및 장기(신경발달) 효과를 살펴본 연구를 검색했다. 치료를 조기(< 14일) 및 후기(≥ 14일) 치료로 분류했다.
무엇을 찾았는가?
미숙아 2,278명을 등록한 27건의 연구를 확인했다. 이 연구는 예방적 치료(예방) 또는 PDA 치료를 위해 파라세타몰 단독 또는 이부프로펜과 이부프로펜, 인도메타신, 위약의 병용 또는 중재 없음의 효능과 안전성을 비교했다. 이 주제에 대해 24개의 진행 중인 연구를 확인했다.
포함된 연구 결과를 종합했을 때 다음을 발견했다.
‐ 파라세타몰의 PDA 폐쇄 성공률은 아마도 위약보다 높았고 이부프로펜 및 인도메타신과 비슷했을 가능성이 높다.
‐ 파라세타몰은 신장과 장에 유해한 영향이 적은 것으로 보인다.
‐ 24개월 및 5세까지의 어린이를 추적한 두 개의 소규모 연구에서 파라세타몰을 투여한 어린이와 비실험적 약물 또는 위약을 투여한 어린이 사이의 신경 발달 장애에 거의 또는 전혀 차이가 없었다.
첫 번째 치료 과정 후 PDA 폐쇄의 주요 결과에 대해 다음을 발견했다.
‐ 파라세타몰과 이부프로펜 사이의 효과에 거의 또는 전혀 차이가 없다는 중간 정도의 근거;
‐ 파라세타몰과 인도메타신 사이에 효과의 차이가 거의 없거나 전혀 없다는 낮은 확실성 근거;
‐ 예방적 파라세타몰이 위약/무중재보다 더 효과적일 수 있다는 낮은 확실성 근거;
‐ 초기 파라세타몰 치료가 위약/무중재보다 더 효과적일 수 있다는 근거 확실성이 낮음;
‐ 후기 파라세타몰 치료와 위약 사이에 거의 또는 전혀 차이가 없다는 낮은 확실성 근거,
‐ 이부프로펜과 파라세타몰의 조합과 이부프로펜 단독의 효과 차이가 거의 또는 전혀 없다는 낮은 확실성 근거.
이 연구에 포함된 대부분의 영아는 중등도 조산아였다. 따라서 극초저체중 아기(ELGAN: 임신 28주 미만) 또는 초저체중아(ELBW: 출생 체중 1000g 미만)에서 PDA 치료를 위한 파라세타몰의 효능과 안전성을 확립하려면 추가 연구가 필요하다.
의료 서비스 제공자는 연구에서 항상 '맹검'(유아가 어떤 약을 받았는지 알지 못함)인 것은 아니다. 따라서 근거의 질(확실성)이 보통이거나 낮다고 판단했다.
이 근거는 얼마나 최신인가?
이 리뷰는 이전 리뷰의 업데이트다. 근거는 2021년 10월까지 업데이트되었다.
Authors' conclusions
Summary of findings
| Paracetamol (oral or IV) versus ibuprofen (oral or IV) for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Oral/IV ibuprofen | Oral/IV paracetamol | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | High‐risk study population | RR 1.02 | 1535 | ⊕⊕⊕⊝ |
| |
| 299 per 1000 | 308 per 1000 | |||||
| All‐cause mortality during initial hospital stay | High‐risk study population | RR 1.09 | 734 | ⊕⊕⊕⊝ |
| |
| 166 per 1000 | 181 per 1000 | |||||
| Necrotizing enterocolitisduring initial hospital stay (by radiological diagnosis) | 70 per 1000 | 91 per 1000 (61 to 136) | RR 1.30 | 1015 | ⊕⊕⊕⊝ |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aFor all three key critical outcomes, we downgraded the evidence by one level to moderate certainty, due to concerns regarding blinding of personnel and outcome assessment. | ||||||
| Paracetamol (oral or IV) versus indomethacin (IV) for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm infants with PDA Settings: neonatal intensive care unit in India, Egypt, and the USA Intervention: paracetamol Comparison: indomethacin | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Indomethacin | Paracetamol | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | High‐risk study population | RR 1.02 (0.78 to 1.33) | 380 | ⊕⊕⊝⊝ Lowa
|
| |
| 297 per 1000 | 303 per 1000 | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | 186 per 1000 | 160 per 1000 (73 to 358) | RR 0.86 (0.39 to 1.92) | 114 (2 studies) | ⊕⊕⊝⊝ Lowb |
|
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis) | 93 per 1000 | 39 per 1000 (18 to 89) | RR 0.42 (0.19 to 0.96) | 384 (4 studies) | ⊕⊕⊝⊝ |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded evidence by two levels to low certainty due to concerns regarding blinding of personnel and outcome assessment, and high heterogeneity. | ||||||
| Prophylactic administration of paracetamol (oral or IV) versus placebo (IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm infants with PDA Settings: neonatal intensive care units in Finland and Iran Intervention: paracetamol Comparison: placebo or no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Placebo or no intervention | Paracetamol | |||||
| Failure of PDA closure after first course (assessed by post‐treatment ECHO) | High‐risk study population | RR 0.27 (0.18 to 0.42) | 240 | ⊕⊕⊝⊝
|
| |
| 612 per 1000 | 165 per 1000 | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | High‐risk study population | RR 0.59 (0.24 to 1.44) | 240 | ⊕⊕⊝⊝
|
| |
| 91 per 1000 | 54 per 1000 | |||||
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis)
| High‐risk study population | Not reported | Not reported | Not reported | Not reported | |
| Data not available | Data not available | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence by two levels to low certainty due to concerns regarding selection bias, blinding of personnel, and high heterogeneity. | ||||||
| Early paracetamol (oral or IV, < 14 days postnatal age) versus placebo (oral or IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Placebo/no intervention | Oral/IV paracetamol | |||||
| Failure of PDA closure after first course of treatment (by post‐treatment ECHO) | High‐risk study population | RR 0.35 (0.23 TO 0.53) | 127 (2 studies) | ⊕⊕⊝⊝
|
| |
| 790 per 1000 | 277 per 1000 (182 to 419) | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence by two levels to low certainty due to concerns regarding selection bias, blinding of personnel and outcome assessors, and high heterogeneity. | ||||||
| Late paracetamol (oral or IV, ≥ 14 days postnatal age) versus placebo (oral or IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Placebo/no intervention | Oral/IV paracetamol | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | High‐risk study population | RR 0.85 (0.72 to 1.01) | 55 (1 study) | ⊕⊕⊝⊝ |
| |
| 1000 per 1000 | 850 per 1000 (720 to 1000) | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis) | 36 per 1000 | 37 per 1000 (3 to 563) | RR 1.04 (0.07 to 15.76) | 55 (1 study) | ⊕⊕⊝⊝ |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence for both failure of PDA closure after first course of treatment and NEC by two levels to low certainty due to concerns regarding indirectness and imprecision. | ||||||
| Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Ibuprofen plus placebo | Paracetamol plus ibuprofen | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | 313 per 1000 | 241 per 1000 (134 to 425) | RR 0.77 (0.43 to 1.36) | 111 (2 studies) | ⊕⊕⊝⊝ | |
| All‐cause mortality during initial hospital stay (by clinical assessment) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Necrotizing enterocolitis during initial hospital stay (radiological diagnosis) | 83 per 1000 | 28 per 1000 (1 to 621) | RR 0.33 (0.01 to 7.45)
| 24 (1 study) | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence for both failure of PDA closure after first course of treatment and NEC by two levels to low certainty due to concerns regarding selection bias, blinding of personnel, outcome assessment, and imprecision. | ||||||
Background
Description of the condition
The ductus arteriosus connects the pulmonary artery to the descending aorta (Clyman 2000). Normal fetal circulation is dependent on the placenta and the patency of the ductus arteriosus (Mathew 1998). During fetal life, the ductus arteriosus diverts most of the combined ventricular output away from the lungs (Clyman 2000). Following birth, and with the separation of the placenta and initiation of breathing, the circulation changes and the ductus closes (Mathew 1998). In full‐term newborns, this happens within 24 to 48 hours after birth (Clyman 2000). In preterm newborns, the ductus frequently fails to close. The failure of the ductus arteriosus to constrict after birth is due to lower intrinsic tone, less ductal muscle fibre, and fewer subendothelial cushions in preterm as compared to term infants (Hammerman 1995). The immature ductus arteriosus has higher sensitivity to the vasodilating effects of prostaglandins and nitric oxide (Hammerman 1995). This is aggravated by hemodynamic derangements due to respiratory distress syndrome and surfactant therapy (Hammerman 1995). The clinical consequences of a PDA are related to the degree of left to right shunting through the ductus. Despite the ability of the left ventricle, in preterm infants, to increase its output in the face of a left to right shunt, blood flow distribution to vital organs is altered due to a drop in diastolic pressure and localised vasoconstriction (Clyman 2000). The presence of a PDA is associated with reduced middle cerebral artery blood flow velocity (Weir 1999). The hemodynamic instability caused by the left to right shunt has been associated with gastrointestinal, cerebral, and renal effects, including spontaneous intestinal perforation and necrotizing enterocolitis (NEC), intraventricular hemorrhage (IVH), decreased kidney function, and bronchopulmonary dysplasia (BPD) and, if not managed, may lead to death. To date, intervention studies with the intention of treatment and closure of PDA have failed to show a decrease in incidence in morbidity or mortality when the PDA is treated. Furthermore, many centers follow a conservative approach without an increase in morbidity or mortality (Sung 2016).
In the two published Cochrane Reviews of prophylactic use of ibuprofen and indomethacin to close a PDA in preterm infants, the spontaneous closure rates in the control groups were 58% and 57%, respectively (Fowlie 2010; Ohlsson 2020a).
Description of the intervention
A PDA can be treated with expectant management (Sung 2016), surgically, or medically with one of two prostaglandin inhibitors: indomethacin or ibuprofen. Surgical closure of a symptomatic PDA improves hemodynamics and lung compliance (Naulty 1978). However, medical treatment is still considered the treatment of choice because of the risks related to the surgery. In a large Canadian cohort (n = 3779) of very low birth weight infants, 28% received treatment for a PDA: 75% were treated with indomethacin alone, 8% with surgical ligation alone, and 17% received both indomethacin and surgical ligation (Lee 2000). Infants with lower birth weights were more likely to be treated surgically (Lee 2000). Prostaglandins play a significant role in keeping the ductus arteriosus patent (Mathew 1998). Inhibiting prostaglandin synthesis with non‐selective blockers of both cyclo‐oxygenase (COX) 1 and 2 is effective for the non‐surgical closure of PDA (Clyman 2000). However, indomethacin use is associated with transient or permanent derangement of renal function, NEC, gastrointestinal hemorrhage or perforation, alteration of platelet function, and impairment of cerebral blood flow or cerebral blood flow velocity (Edwards 1990; Ohlsson 1993; Seyberth 1983; Wolf 1989).
Ibuprofen, a propionic acid derivative and non‐selective COX inhibitor, is as effective as indomethacin in closing a PDA and reduces the risk of NEC (Ohlsson 2020b). There is less evidence of transient renal insufficiency following treatment with ibuprofen compared to indomethacin (Ohlsson 2020b).
Another non‐steroidal anti‐inflammatory drug (NSAID), mefenamic acid, has been reported to close a PDA (Sakhalkar 1992), but no randomized controlled trials have been reported (Ohlsson 2020a; Ohlsson 2020b).
In the sheep fetus, Peterson showed that acetaminophen has potent activity on the ductus arteriosus and produces a constriction in therapeutic analgesic quantities (Peterson 1985). In humans, Simbi 2002 reported on a pregnant woman near term who took nimesulide 400 mg and acetaminophen 500 mg twice daily for three days as a medication for pain. The woman noticed diminished fetal movements and, one day later, ultrasound confirmed lack of fetal movements and breathing. A constricted ductus arteriosus was confirmed by fetal echocardiography. Following caesarean section, the male infant presented with severe mixed acidosis. An echocardiogram showed an almost completely constricted ductus arteriosus. Following intensive care, the infant improved and was discharged home on day 12 after birth. At three months' follow‐up, the infant was doing well. Either nimesulide or acetaminophen, or both, could be responsible for ductal closure in this case.
The complications associated with the use of indomethacin and possibly ibuprofen have encouraged the search for an alternative drug to treat a PDA. In 2011, paracetamol was suggested as an alternative (Hammerman 2011). Hammerman and colleagues reported on five preterm infants (postmenstrual age (PMA) 26 to 32 weeks at birth and postnatal age of 3 to 35 days) with large, hemodynamically significant PDAs (Hammerman 2011). The infants had failed or had contraindications for treatment with ibuprofen. All infants were treated with oral paracetamol 15 mg/kg per dose every six hours. The treatment resulted in ductal closure in all infants within three days. No side effects were observed. The authors suggested that paracetamol could offer important therapeutic advantages over non‐steroidal anti‐inflammatory drugs (indomethacin and ibuprofen) as paracetamol has no peripheral vasoconstrictive effect, can be given to infants with clinical contraindications to NSAIDs, and appears to be effective after ibuprofen treatment failure (Hammerman 2011).
Unconjugated hyperbilirubinemia impacts upon clearance of paracetamol (Palmer 2008). Acetaminophen‐induced hepatic failure with encephalopathy has been described in a term newborn who received oral acetaminophen every four hours by the parents following circumcision (Walls 2007).
Paracetamol can be given as prophylaxis for a PDA within 24 hours after birth or as early (< 14 days' postnatal age), late (> 14 days' postnatal age), and combination (ibuprofen plus paracetamol) treatment for a PDA diagnosed by echocardiography (ECHO). We include all approaches in this review.
How the intervention might work
Paracetamol is an analgesic, antipyretic derivative of acetanilide with weak anti‐inflammatory properties. It is used as a common analgesic in all age groups, but may cause liver, blood cell, and kidney damage (NLM 2012). In low concentrations paracetamol stimulates, and in high concentrations inhibits, the synthesis of prostaglandins. In vivo (in adults) 500 mg of paracetamol causes a pronounced reduction of prostacyclin synthesis but has no effect on thromboxane synthesis (Grèen 1989). Because in vitro paracetamol is a weak inhibitor of both COX 1 and COX 2, the possibility exists that it inhibits a so far unidentified form of COX, perhaps a COX 3 (Botting 2000). In a murine model, paracetamol was found to be less potent than indomethacin for constriction of the mouse ductus arteriosus in vitro (El‐Khuffash 2014).
Since the report in 2011 by Hammerman and colleagues (Hammerman 2011), there have been many case series of treatment of a PDA with paracetamol in preterm infants. In five case series, a total of 38 infants with different contraindications for the use of ibuprofen or indomethacin were included (Kessel 2014; Nadir 2014; Sinah 2013; Terrin 2014; Yurttutan 2013). Paracetamol was administered orally, intravenously, or via nasogastric tube, and the dose and duration of treatment varied: orally 15 mg/kg every eight hours for 48 hours (Sinah 2013); 15 mg/kg every six hours for three days (Yurttutan 2013); 15 mg/kg every six hours for up to seven days (Nadir 2014); via nasogastric tube 15 mg/kg every six hours for three to seven days (Kessel 2014); or intravenously 7.5 mg/kg to 15 mg/kg every four to six hours, with a maximum daily dose of 60 mg/kg (duration of treatment three days in five of seven cases) (Terrin 2014). In these case reports, the PDA closed in 33 of the 38 cases treated with paracetamol (86%). Kessel and colleagues measured plasma paracetamol concentrations before the fifth dose and ninth dose and 24 hours after the last dose (Kessel 2014). Most measured paracetamol blood concentrations were comparable to those recommended for pain and fever control (10 mg/mL to 20 mg/mL) (Arana 2001).
In another published case series, El‐Khuffash 2014 retrospectively evaluated the clinical effectiveness of paracetamol on the closure of a PDA, and prospectively examined its effect on the in vitro term and preterm murine ductus arteriosus. A total of 21 infants were included in the study from the Mount Sinai Hospital, Toronto, Ontario, Canada and the Rotunda Maternity Hospital, Dublin, Ireland. At the Canadian site, paracetamol was either given orally as a short course (15 mg/kg every six hours for 48 hours) or a long course of 15 mg/kg every six hours for seven days. At the Irish site, paracetamol was given intravenously, 15 mg/kg every six hours for a minimum of 48 hours, until PDA closure was confirmed on echocardiography or up to a maximum of six days. In both centers, the decision to administer paracetamol treatment to neonates with a hemodynamically significant PDA was after failure of two courses of either ibuprofen or indomethacin, or if there were contraindications to medical treatments (El‐Khuffash 2014). No changes in PDA hemodynamics were seen in the five infants treated with a short course of paracetamol. In six of the seven infants treated with a long course, the PDA closed. In eight of the nine infants treated with intravenous paracetamol, the PDA closed (El‐Khuffash 2014). Paracetamol drug levels were not ascertained. The authors concluded that the effectiveness of paracetamol on PDA closure may depend on the duration of treatment and the mode of administration (El‐Khuffash 2014). The inhibitory effect of paracetamol on prostaglandin E₂ (PGE₂) may not be present at lower gestational ages (El‐Khuffash 2014).
Recently, concerns have been raised that prenatal or neonatal exposure, or both, to paracetamol could have adverse effects on brain development. Viberg and colleagues examined whether neonatal paracetamol exposure in mice could affect the development of the brain (Viberg 2014), manifested as adult behaviour and cognitive deficits, as well as changes in the response to paracetamol. They concluded that exposure to and presence of paracetamol during a critical period of brain development in mice can induce long‐lasting effects on cognitive function and alter the adult response to paracetamol (Viberg 2014).
In an ecological study conducted in humans and using country‐level data for the period 1984 to 2005, prenatal use of paracetamol was correlated with autism or autism spectrum disorder (ASD) (Bauer 2013). To explore the relationship of early neonatal paracetamol exposure to autism and ASD, population‐weighted average male autism prevalence rates for all available countries and US states were compared to male circumcision rates, a procedure for which paracetamol has been widely prescribed since the mid‐1990s. For studies including boys born after 1995, there was a strong correlation between country‐level autism and ASD prevalence in males and a country's circumcision rate (r = 0.98) (Bauer 2013). In a Spanish birth cohort study, prenatal acetaminophen exposure was associated with a greater number of autism‐spectrum symptoms in males and showed adverse effects on attention‐related outcomes for both genders (Avella‐Garcia 2016). Ystrom 2017, in a study based on the Norwegian Mother and Child Cohort study, including 2246 children with attention deficit hyperactivity disorder (ADHD), found that long‐term maternal use of paracetamol during pregnancy was substantially associated with ADHD in offspring.
In a study from Sweden, Bornehag 2017 reported on a possible association of prenatal exposure to acetaminophen and language delay in girls at 30 months of age. The same group reviewed nine prospective cohort studies that reported on associations between prenatal use of paracetamol and neurodevelopmental outcomes in the offspring (Bauer 2018). All included studies suggested an association between prenatal paracetamol exposure and the neurodevelopmental outcomes of ADHD, ASD, or lower intelligence quotient (IQ). Longer duration of paracetamol use was associated with increased risk. Associations were strongest for hyperactivity and attention‐related outcomes (Bauer 2018).
It is therefore of extreme importance that infants enrolled in trials of paracetamol either for pain relief or for closure of a PDA be followed in the long term with conventional developmental tests and tests to diagnose autism and ASD (APA 2013).
Why it is important to do this review
There is marked variation in clinical practice as to whether to treat PDA or not, and if the decision is made to treat, with what agent. Combination treatment (ibuprofen plus paracetamol) targeting two separate enzyme sites has recently been evaluated as a management strategy for treatment of PDA in preterm infants with varying results. This strategy was not in clinical practice during the previous version of the review (Ohlsson 2020c). Thus, we felt it was important to perform an up‐to‐date literature search in an attempt to synthesize evidence of this comparison and to present the current evidence to the scientific community. Moreover, we identified a number of ongoing studies (n = 19) in our previous update and we were keen to discover if new study data had since emerged.
For the management of PDA, clinicians often use multiple (two to three) courses of pharmacotherapy and, if unsuccessful, proceed to definitive approaches for ductal closure (ligation/transcatheter). Hence, it is important to explore the efficacy of paracetamol on the failure of ductal closure after the second course and after a total of two courses of treatment. In view of findings in mice of adverse effects on brain development following neonatal exposure to paracetamol, and in humans of an association of neonatal exposure to paracetamol and autism or ASD and language delay, it is important that we continually review the efficacy and safety of paracetamol for the management of PDA in preterm and low birth weight neonates.
Objectives
To determine the efficacy and safety of paracetamol as monotherapy or as part of combination therapy via any route of administration, compared with placebo, no intervention, or another prostaglandin inhibitor, for prophylaxis or treatment of an echocardiographically‐diagnosed PDA in preterm or low birth weight infants.
Methods
Criteria for considering studies for this review
Types of studies
We considered randomized and quasi‐randomized controlled trials for inclusion.
Types of participants
We included infants born preterm (< 37 weeks' postmenstrual age) or with low birth weight (< 2500 g at birth) who had an echocardiographic diagnosis of a PDA regardless of their postnatal age. In the Cochrane Review of ibuprofen for the treatment of a PDA, all 20 included studies made the diagnoses of a PDA by echocardiography (Ohlsson 2020b), and it is likely that that would be the case in studies of the effectiveness of paracetamol in closing a PDA. For prophylactic administration of paracetamol (orally or intravenously (IV)) versus placebo (IV) or no intervention within 24 hours after birth for a PDA, ECHO confirmation of a PDA was not required.
Types of interventions
We included paracetamol (given via any route for the purpose of closure of a PDA) administered alone or in combination in any dose versus placebo or no intervention or versus another prostaglandin inhibitor. If the intention for administration of paracetamol was not closure of a PDA, we excluded the study. We included studies that used any therapeutic regimen of paracetamol. We conducted six comparisons for this review, described below in the 'Summary of findings and assessment of the certainty of the evidence' section.
Types of outcome measures
Primary outcomes
-
Failure of PDA closure after the first course of paracetamol treatment (closure and failure of closure confirmed by echocardiographic criteria)
-
Neurodevelopmental impairment (neurodevelopmental outcome assessed by a standardized and validated assessment tool or a child developmental specialist, or both) at any age reported (outcome data grouped at 12, 18, 24, 36, and 60 months, if available)
-
Death or disability (outcome data grouped at 12, 18, 24, 36, and 60 months, if available)
Secondary outcomes
-
All‐cause mortality during initial hospital stay
-
Neonatal mortality (death during the first 28 days of life)
-
Re‐opening of the ductus arteriosus (defined as echocardiographic evidence of closure followed by re‐opening of the PDA at a later stage)
-
Failure of PDA closure after second course of paracetamol treatment (closure and failure of closure confirmed by echocardiographic criteria) (added as an outcome in 2021)
-
Failure of PDA closure after a total of two courses of paracetamol treatment (closure and failure of closure confirmed by echocardiographic criteria)
-
Surgical closure of the PDA (added as an outcome in 2021)
-
Treatment with indomethacin, ibuprofen, or another prostaglandin inhibitor to close the PDA following treatment failure
-
Duration of ventilator support (days)
-
Duration of need for supplementary oxygen (O₂) (days)
-
Pulmonary hemorrhage (blood‐stained liquid flowing from the trachea of the infant)
-
Pulmonary hypertension (defined as an increased mean pulmonary arterial pressure of 25 mmHg at rest) (Van Loon 2011)
-
Bronchopulmonary dysplasia (BPD) at 36 weeks' postmenstrual age (defined as O₂ requirement at 36 weeks' postmenstrual age in addition to compatible clinical and roentgenographic findings)
-
BPD defined according to the new criteria (i.e. mild BPD defined as a need for supplemental O₂ for ≥ 28 days but not at 36 weeks' postmenstrual age or discharge; moderate BPD as O₂ for ≥ 28 days plus treatment with < 30% O₂ at 36 weeks' postmenstrual age; and severe BPD as O₂ for ≥ 28 days plus ≥ 30% O₂ or positive pressure, or both, at 36 weeks' postmenstrual age (Ehrenkranz 2005))
-
Intraventricular hemorrhage (IVH) (Grade I to IV) (Papile 1978)
-
Severe IVH (Grade III to IV)
-
Periventricular leukomalacia (PVL)
-
Necrotizing enterocolitis (NEC) (stage ≥ 2) (Bell 1978)
-
Intestinal perforation
-
Gastrointestinal bleed or stools positive for occult blood
-
Retinopathy of prematurity (ROP) (according to the international classification of ROP) stage 3 or higher (ICCROP 2005)
-
Oliguria (decreased urine output defined as < 1 mL/kg/h during treatment)
-
Acute kidney injury (defined by authors as there is no consensus definition)
-
Sepsis (clinical symptoms and signs of sepsis and a positive blood bacterial culture); this outcome was added at the full review stage
-
Post‐pre treatment difference in serum or plasma levels of creatinine (mg/dL) (added as an outcome in 2021)
-
Post‐pre treatment difference in serum or plasma levels of aspartate transaminase (AST) (U/L) (added as an outcome in 2021)
-
Post‐pre treatment difference in serum or plasma levels of alanine transaminase (ALT) (U/L) (added as an outcome in 2021)
-
Number of infants with AST or ALT levels greater than 100 U/L
-
Serum bilirubin (μmol/L) following treatment
-
Hyperbilirubinemia (serum bilirubin level higher than the exchange level according to the postnatal age and body weight)
-
Incidence of liver failure; evidence of acute liver injury combined with either severe coagulopathy (International Normalized Ratio (INR) > 2.0 or prothrombin time (PT) > 20 seconds) or encephalopathy with moderate coagulopathy (INR ≥ 1.5 or PT ≥ 15 seconds) (Sundaram 2011)
-
Duration of hospitalization (total length of hospitalization from birth to discharge home or death) (days)
-
Autism or autism spectrum disorder (ASD) in childhood (APA 2013); this outcome was added at the full review stage
-
Language delay; this outcome was added in 2017
-
Other adverse effects as reported by the study authors (i.e. not prespecified)
-
Other neurodevelopmental outcomes: Severity of cerebral palsy (CP), attention deficit hyperactivity disorder (ADHD), pervasive developmental disorder, blindness, deafness (added as an outcome in 2021)
Search methods for identification of studies
The Neonatal Group Information Specialist developed new search strategies to increase the sensitivity of the search. The Information Specialist developed the strategies in consultation with the review authors.
Electronic searches
We searched the following databases on 13 October 2021 without date, language, or publication status restrictions (Ovelman 2020):
-
Cochrane Central Register of Controlled Trials (CENTRAL 2021, Issue 10) (Appendix 1);
-
Ovid MEDLINE and Epub Ahead of Print, In‐Process, In‐Data‐Review & Other Non‐Indexed Citations, Daily and Versions 1946 to 13 October 2021 (Appendix 2);
-
OVID Embase 1974 to 13 October 2021 (Appendix 3).
We searched the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO) on 1 March 2022 (Appendix 4). We used methodological filters based on those developed by Cochrane (Cochrane 2021; Lefebvre 2011), and the Canadian Agency for Drugs and Technologies in Health (CADTH 2016), to limit retrieval to randomized controlled trials, quasi‐randomized trials, and systematic reviews.
This is the third update of this review. Previous search details are listed in Appendix 5 and Appendix 6.
Searching other resources
We searched the following clinical trials registries for ongoing or recently completed trials up to October 2021 (Appendix 7):
-
World Health Organization International Clinical Trials Registry Platform (ICTRP) search portal (trialsearch.who.int/);
-
U.S. National Library of Medicine’s ClinicalTrials.gov (clinicaltrials.gov);
-
ISRCTN Registry (www.isrctn.com/).
We also searched the reference lists of related systematic reviews and trials selected for inclusion in this review in order to identify additional relevant articles.
Data collection and analysis
We used standard methods recommended by Cochrane (Higgins 2020) and Cochrane Neonatal.
Selection of studies
Two review authors (BJ, SM) independently assessed study eligibility for inclusion in this review according to the prespecified selection criteria. Consensus was achieved by involving a third review author (PS).
Data extraction and management
Two review authors (BJ, SM) independently extracted data from the new full‐text articles using a specifically designed spreadsheet and customized form to manage information. We used these forms to decide trial inclusion and exclusion, extract data from eligible trials, and for requesting additional published information from authors of the original reports. We entered and cross‐checked data using Review Manager 5 (RevMan 5) software (Review Manager 2020). We compared the extracted data for any differences. If noted, we resolved differences by mutual discussion and consensus and involving a third review author (PS). We contacted the authors of three identified trials, and we obtained unpublished data from the Oncel group (Oncel 2014), the Dang group (Dang 2013), and the Dash group (Dash 2015). In the previous version, PS and AO collected data using a similar process. PS resolved any differences.
Assessment of risk of bias in included studies
Two review authors (BJ, SM) independently assessed the risk of bias (low, high, or unclear) of all included trials using the Cochrane risk of bias tool for the following domains (Higgins 2011):
-
sequence generation (selection bias);
-
allocation concealment (selection bias);
-
blinding of participants and personnel (performance bias);
-
blinding of outcome assessment (detection bias);
-
incomplete outcome data (attrition bias);
-
selective reporting (reporting bias);
-
any other bias.
We resolved any disagreements through discussion or by involving a third assessor to reach consensus. In the previous version of the review, PS and AO assessed risk of bias using a similar process. PS resolved any differences. See Appendix 8 for a more detailed description of risk of bias for each domain.
Measures of treatment effect
We analyzed treatment effects in the individual trials using RevMan 5 (Review Manager 2020).
Dichotomous data
We reported dichotomous data using risk ratio (RR) and risk difference (RD) with respective 95% confidence intervals (CI). For those outcomes with a statistically significant RD for the pooled estimate from the meta‐analysis, we calculated the number needed to treat for an additional beneficial outcome (NNTB) or number needed to treat for an additional harmful outcome (NNTH) and respective 95% CI.
Continuous data
We reported continuous data using mean difference (MD) with 95% CI.
Unit of analysis issues
The unit of randomization was the individual infant. We did not include cross‐over or cluster‐randomized trials as those trial designs are unlikely for the intervention studied in this review — indeed, we identified no cross‐over or cluster‐randomized trials. We only considered an infant once, even though the infant might have been randomized twice by investigators. We planned to contact the authors in order to provide data resulting from the first randomization. If we could not separate data from the first randomization, we planned to exclude the study. We included studies with multiple arms in meta‐analysis by making multiple pair‐wise comparisons between all possible pairs of intervention groups and ensuring that study arms were not counted multiple times in the same meta‐analyses.
Dealing with missing data
We requested additional data from the authors of each included trial when data on important outcomes were missing or needed clarification. We did receive clarifying information from the authors of the following included trials: Dang 2013; Dash 2015; and Oncel 2014. The authors clarified that all the published analyses, and those they provided to us, were intention‐to‐treat analyses.
Assessment of heterogeneity
We used RevMan 5 software to assess the heterogeneity of treatment effects between trials (Review Manager 2020). We used the two formal statistics described below.
-
The Chi² test, to assess whether observed variability in effect sizes between studies was greater than would be expected by chance. Since this test has low power when the number of studies included in the meta‐analysis is small, we set the alpha probability at the 10% level of significance.
-
The I² statistic to ensure that pooling of data was valid. We graded the degree of heterogeneity as: none, low, moderate, and high for values of less than 25%, 25% to 49%, 50% to 74%, and 75% or higher, respectively (Higgins 2003).
Assessment of reporting biases
We attempted to identify the study protocols for the trials we selected for inclusion (see the Characteristics of included studies table). We planned to assess reporting and publication bias by examining the degree of asymmetry of a funnel plot in RevMan 5 provided that a sufficient number of studies (n = 10) were available (Review Manager 2020).
Data synthesis
We performed statistical analyses according to the recommendations of Cochrane Neonatal (neonatal.cochrane.org/resources-review-authors). We analyzed all infants randomized on an intention‐to‐treat basis. We analyzed treatment effects in the individual trials. We used a fixed‐effect model in the meta‐analysis to combine the data. Where substantial heterogeneity existed, we examined the potential cause of heterogeneity in subgroup and sensitivity analyses. When we judged meta‐analysis to be inappropriate, we planned to analyze and interpret individual trials separately. For estimates of RR and RD, we used the Mantel‐Haenszel method. For measured quantities, we used the inverse‐variance method. We would have used the standardized mean difference (SMD) to combine trials that measured the same outcome but used different scales.
Subgroup analysis and investigation of heterogeneity
We considered 'gestational age (< 32 weeks)' for subgroup analysis in the current update by restricting studies that reported outcomes in preterm infants of less than 32 weeks' gestational age for the comparison of paracetamol versus ibuprofen or paracetamol versus indomethacin. We selected this subgroup as infants of this age group have a high risk of developing PDA with short‐ and long‐term clinical implications (Nielsen 2022).
For this update, we were unable to consider the previously defined subgroups (Ohlsson 2020c): gestational age of less than 28 weeks, 28 to 32 weeks, 33 to 36 weeks; and birth weight (< 1000 g, 1001 g to 1500 g, 1501 g to 2500 g) as there were insufficient data to draw clinically relevant, meaningful conclusions.
Sensitivity analysis
We planned to perform a sensitivity analysis to determine if the findings were affected by including only studies of adequate methodology, defined as adequate randomization and allocation concealment, blinding of intervention and measurement, and less than 10% losses to follow‐up.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the certainty of the evidence for the following comparisons:
-
paracetamol versus ibuprofen;
-
paracetamol versus indomethacin;
-
prophylactic paracetamol versus placebo or no intervention;
-
early paracetamol (< 14 days' postnatal age) versus placebo or no intervention;
-
late paracetamol (≥ 14 days' postnatal age) versus placebo or no intervention;
-
combination treatment (paracetamol plus ibuprofen versus ibuprofen plus placebo or no intervention).
We chose three critical outcomes: failure of PDA closure after the first course of treatment; all‐cause mortality during initial hospital stay; and necrotizing enterocolitis. These outcomes (the former a primary outcome, the latter two secondary outcomes) were deemed critical after discussion amongst all the review authors.
Two authors (BJ, PS) independently assessed the certainty of the evidence for each of the outcomes above. We considered evidence from RCTs as high certainty but downgraded the evidence one level for serious (or two levels for very serious) limitations based upon the following: design (risk of bias), consistency across studies, directness of the evidence, precision of estimates, and presence of publication bias. We used the GRADEpro GDT Guideline Development Tool to create summary of findings Table 1, summary of findings Table 2, summary of findings Table 3, summary of findings Table 4, summary of findings Table 5, and summary of findings Table 6 to report the certainty of the evidence. We resolved any differences in GRADE assessment by consensus and involving a third review author.
The GRADE approach results in an assessment of the certainty of a body of evidence in one of four grades:
-
high certainty: further research is very unlikely to change our confidence in the estimate of effect;
-
moderate certainty: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate;
-
low certainty: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate;
-
very low certainty: we are very uncertain about the estimate.
Results
Description of studies
Results of the search
For this 2022 update, our electronic database search yielded 493 records and our search of trials registers retrieved 120 records. After removing 199 duplicates, we screened a total of 414 records. After excluding 366 clearly irrelevant records, we assessed 48 full‐text articles for eligibility. Of these, we excluded four studies (see Excluded studies) and 24 ongoing studies (25 reports). Thus, this 2022 update search included 19 new studies (Asadpour 2018; Babaei 2018; Bagheri 2016; Bagheri 2018; Balachander 2020; Dani 2021; Davidson 2021; El‐Farrash 2019; Ghaderian 2019a; Ghaderian 2019b; Hochwald 2018; Jafari 2019; Kluckow 2019; Kumar 2020; Meena 2020; Oboodi 2020; Schindler 2021;Shahmirzadi 2021; Tauber 2020). Overall, a total of 27 RCTs (19 new studies plus eight studies from previous review version) involving 2278 infants are included in the current review. For details see Figure 1.
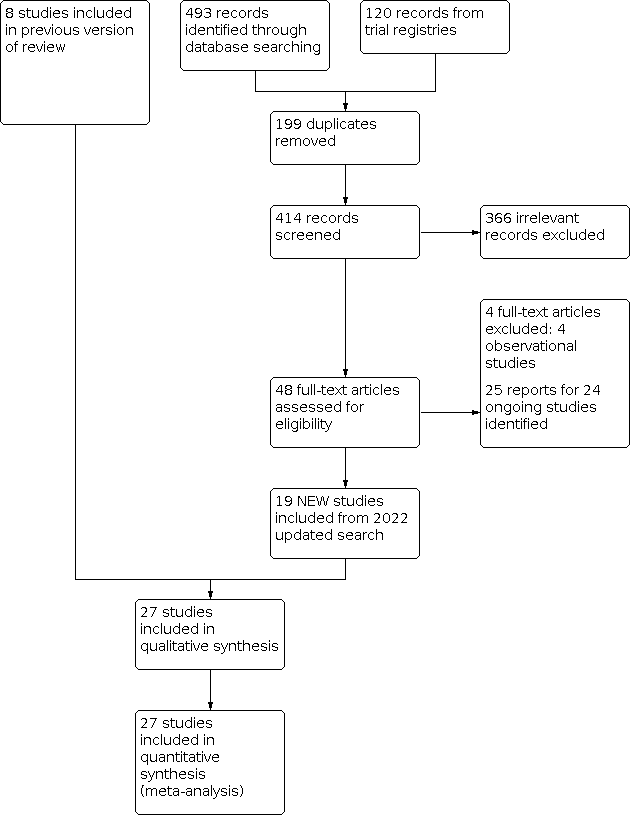
Study flow diagram for 2022 review update
We also identified 24 ongoing studies (25 reports) (ACTRN12613000289718; ChiCTR‐TRC‐13003912; CTRI/2017/10/009989; CTRI/2017/10/010012; CTRI/2018/02/011942; EUCTR2015‐003177‐14‐ES; EUCTR2019‐004297‐26‐FR; IRCT20111011007763N2; IRCT20120215009014N321; IRCT20130812014333N118; IRCT20171227038102N1; IRCT20190505043478N1; IRCT20200218046538N1; NCT01291654; NCT02056223; NCT02819414; NCT03604796; NCT03641209; NCT03648437; NCT04037514; NCT04459117; NCT04986839; TCTR20201104001).
Included studies
We included a total of 27 studies with 2278 participants. Individual study characteristics, inclusion criteria, treatment details, and outcomes can be found the Characteristics of included studies table.
Studies comparing oral/intravenous (IV) paracetamol and oral/IV ibuprofen
Eighteen studies that enrolled 1535 infants compared oral/IV paracetamol to oral/IV ibuprofen. The following section provides a brief description of the included studies.
Al‐Lawama 2017 was a single‐center study in the neonatal intensive care unit (NICU) of Jordan University Hospital, Amman, Jordan. It aimed to evaluate the effectiveness and safety profiles of oral paracetamol versus oral ibuprofen for PDA closure in preterm infants up to and including 32 weeks' gestational age, or birth weight of up to 1500 g, with a hemodynamically significant PDA. Infants were randomised to either oral paracetamol (10 mg/kg every six hours for three days; n = 11) or oral ibuprofen (10‐5‐5 mg/kg/dose; n = 11) for PDA treatment. The study's primary outcomes included mortality and primary PDA closure rate. The baseline characteristics were similar between the two groups. The authors found no significant difference in the mortality or primary closure rates between the two groups.
Asadpour 2018 was a single‐center, randomized controlled trial (RCT) at Hajar Hospital in Shahrekord, Iran, from 2016 to 2017. It aimed to compare the efficacy of oral paracetamol and oral Ibuprofen for the closure of PDA in preterm infants under 37 weeks' gestational age with PDA. Infants were randomised to either oral paracetamol (10 mg/kg every six hours for three days; n = 25) or oral ibuprofen (10‐5‐5 mg/kg/dose; n = 25) for PDA treatment. The study's outcomes included PDA closure rate, bilirubin, serum creatinine, blood urea nitrogen, aspartate transaminase (AST), alanine transaminase (ALT) pre‐post treatment in both groups and gastrointestinal complications, mortality, and primary PDA closure. The baseline characteristics were similar between the two groups. The authors found no significant difference in the PDA closure rates between the two groups. Of note, infants who received paracetamol had higher post‐treatment ALT levels compared to the ibuprofen group but no infant had overt hepatotoxicity. In addition, infants who received ibuprofen had higher gastrointestinal complications compared to the paracetamol group (0/25 in the paracetamol group versus 5/25 in the ibuprofen group; P = 0.05).
Bagheri 2016 was a single‐center RCT in the NICU of Afzalipour Hospital, Kerman, Iran, from July 2014 to November 2014. It aimed to compare the efficacy of oral paracetamol and oral Ibuprofen for the closure of PDA in preterm infants under 37 weeks' gestational age and postnatal age of 14 days or less, with a hemodynamically significant PDA. Infants were randomised to either oral paracetamol (15 mg/kg every six hours for three days; n = 67) or oral ibuprofen (20‐10‐10 mg/kg/dose; n = 62) for PDA treatment. The study's outcomes included failure of ductal closure after the first and second course of treatment. The baseline characteristics were similar between the two groups. The authors found no significant difference in the PDA closure rates after the first and second course of treatment between the two groups.
Balachander 2020 was a single‐center RCT in the NICU in Pondicherry, India, from October 2014 to January 2016. It aimed to compare the efficacy of oral paracetamol and oral ibuprofen for PDA closure confirmed by echocardiography in preterm infants up to and including 37 weeks' gestational age with a hemodynamically significant PDA. Infants were randomised to either oral paracetamol (15 mg/kg every six hours for two days; n = 55) or oral ibuprofen (10‐5‐5 mg/kg/dose; n = 55) for PDA treatment. The study's outcomes included PDA closure rates, mortality, cardiorespiratory morbidity, and adverse effects. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to PDA closure, mortality, or cardiorespiratory morbidity. The infants who received ibuprofen had a significantly higher occurrence of acute kidney injury (AKI) compared to the paracetamol group (27.3% in the ibuprofen group versus 9.1% in the paracetamol group, P = 0.02).
Dang 2013 was a single‐center study in Changchun, China. It aimed to compare the effectiveness and safety profiles of oral paracetamol and oral ibuprofen for PDA closure in preterm infants up to and including 34 weeks' gestational age and postnatal age of 14 days or less, with an echocardiographically confirmed hemodynamically significant PDA. Infants were randomised to either oral paracetamol (15 mg/kg every six hours for three days; n = 80) or oral ibuprofen (10‐5‐5 mg/kg/dose; n = 80) for PDA treatment. The study's outcomes included PDA closure rates, mortality, oliguria, AKI, intraventricular hemorrhage (IVH), gastrointestinal bleeding, necrotizing enterocolitis (NEC), hyperbilirubinemia, bronchopulmonary dysplasia (BPD), periventricular leukomalacia (PVL), retinopathy of prematurity (ROP), sepsis, and serum creatinine. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to PDA closure. The infants who received paracetamol had significantly lower hyperbilirubinemia (20% in the paracetamol group versus 35% in the ibuprofen group, P = 0.03) and gastrointestinal bleeding (2.5% in the paracetamol group versus 10% in the ibuprofen group, P = 0.03) compared to the ibuprofen group.
Dani 2021 was a multi‐center RCT in five NICUs in Italy. It aimed to assess the efficacy and safety of IV paracetamol versus IV ibuprofen for the treatment of hemodynamically significant PDAs in preterm infants with a gestational age of 25to31 weeks, and echocardiographic evidence of a hemodynamically significant PDA between 24 and 72 hours of life. Infants were randomised to either IV paracetamol (15 mg/kg every six hours for three days; n = 52) or IV ibuprofen (10‐5‐5 mg/kg/dose; n = 49) for PDA treatment. The study's outcomes included failure to close the PDA after the first and second course of treatment, failure to constrict the PDA after the first and second course of treatment, re‐opening rate, and incidence of surgical closure 30 days after enrolment. The baseline characteristics were similar between the two groups. Paracetamol was less effective in closing hemodynamically significant PDAs than ibuprofen (52% in the paracetamol group versus 78% in the ibuprofen group; P = 0.026) after the first course of treatment. The constriction rate of the PDA, re‐opening rate, the need for surgical closure, and the occurrence of adverse effects were similar between the two groups.
El‐Farrash 2019 was a double‐blind RCT in the NICU of an obstetrics and gynaecology hospital, at Ain Shams University in Cairo, Egypt, from June 2015 to June 2017. It aimed to evaluate the efficacy and safety of oral paracetamol versus oral ibuprofen in preterm infants of up to and including 34 weeks' gestational age and a postnatal age of two to seven days with a hemodynamically significant PDA. Infants were randomised to either oral paracetamol (15 mg/kg every six hours for three days; n = 30) oral ibuprofen (10‐5‐5 mg/kg/dose; n = 30) for PDA treatment. The study's outcomes included PDA closure after the first and second course of treatment, surgical ligation, mortality, IVH, NEC, gastrointestinal bleeding, intestinal perforation, AKI, hepatotoxicity, and BPD. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and other prespecified secondary outcomes, including rates of adverse effects.
El Mashad 2017 was a three‐arm, single‐center RCT in the NICU of Tanta University Hospital Pediatric Department, Tanta, Egypt. It compared the effectiveness and side effects of paracetamol, indomethacin, and ibuprofen in the closure of hemodynamically significant PDAs in preterm infants under 28 weeks' gestational age or a birth weight of less than 1500 g in the first two weeks of life with a hemodynamically significant PDA diagnosed with echocardiography. Infants were randomised to IV paracetamol (15 mg/kg every six hours for three days; n = 100), IV ibuprofen (10‐5‐5 mg/kg/dose; n = 100), or IV indomethacin (0.2 mg/kg for three doses 12 hours apart; n = 100) for PDA treatment. The study's outcomes included PDA closure after the first and second course of treatment and adverse effects. The baseline characteristics were similar between the three groups. The authors found no significant difference between the three groups with regards to ductal closure rates after the first and second course of treatment. There was a significant increase in serum creatinine levels and serum blood urea nitrogen (BUN) and a significant reduction in platelet count and urine output in the ibuprofen and indomethacin groups compared to the paracetamol group. There was a significant increase in bilirubin levels in the ibuprofen group compared to the indomethacin or paracetamol group.
Ghaderian 2019a was a multi‐center, non‐inferiority, randomized, double‐blind clinical trial in the Al‑Zahra and Shahid Beheshti Hospitals at the Isfahan University of Medical Sciences, Iran. It compared the effectiveness of oral ibuprofen and a low dose of IV paracetamol in the management of PDA in preterm infants up to and including 34 weeks' gestational age and a weight of 1000 g or more with echocardiographic evidence of PDA. Infants were randomised to IV paracetamol (15 mg/kg/dose every six hours for two days; n = 20) or oral ibuprofen (10‐5‐5 mg/kg/dose; n = 20) . The study's outcomes included PDA closure rates after the first and second course of treatment. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates after the first and second course of treatment.
Ghaderian 2019b was a multi‐center, parallel‐group, double‐blind, non‐inferiority RCT in the NICUs of the Al‐Zahra and Shahid Beheshti Hospitals, affiliated to the Isfahan University of Medical Sciences, Isfahan, Iran from January 2017 to October 2018. It aimed to compare the efficacy of oral ibuprofen and oral acetaminophen for closure of symptomatic PDA in preterm neonates of less than 32 weeks' gestational age, or a birth weight of less than 1500 g, and less than 14 days' postnatal age, with a hemodynamically significant PDA. Infants were randomised to oral paracetamol (15 mg/kg/dose every six hours for two days; n = 20) or oral ibuprofen (10‐5‐5 mg/kg/dose every 24 hours; n = 20). Outcomes included PDA closure rates after the first and second course of treatment. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates after the first and second course of treatment.
Jafari 2019 was a single‐center RCT in the NICU of Ayatollah Mousavi Hospital in Zanjan, Iran, from 21 March 2017 to 21 March 2018. It compared the safety and efficacy of IV paracetamol and IV ibuprofen for treatment of PDA in low birth weight infants at a postnatal age of 48 to 72 hours with echocardiographic diagnosis of a hemodynamically significant PDA. Infants were randomised to IV paracetamol (15 mg/kg/dose every six hours for three days; n = 16) or IV ibuprofen (10‐5‐5 mg/kg/dose every 24 hours; n = 14). The study's outcomes included PDA closure, all‐cause mortality, duration of mechanical ventilation, length of stay, IVH (all grades), ROP, pneumothorax, and BPD. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and other prespecified secondary outcomes.
Kumar 2020 was a randomised, two‐arm, active‐controlled, blinded, non‐inferiority RCT in three centers across India from April 2014 to June 2017. It compared the efficacy and safety of ibuprofen and paracetamol in the closure of PDAs in preterm neonates under 32 weeks' gestational age with hemodynamically significant PDAs. A screening echocardiography was performed in asymptomatic neonates to detect hemodynamically significant PDAs (between 48 and 72 hours of age in those at 29 to 31 weeks' gestational age, and in the first 48 hours in those at less than 28 weeks' gestational age). Infants were randomised to oral paracetamol (15 mg/kg every six hours for three consecutive days; n = 81) or oral ibuprofen (10‐5‐5 mg/kg/dose every 24 hours; n = 80). The study's outcomes included closure rate of hemodynamically significant PDA by 24 hours from the last dose of the study drug, irrespective of the course of the drug; rate of hemodynamically significant PDA closure by 24 hours after the first course of the study drug, rate of re‐opening following the first course, need for surgical ligation for hemodynamically significant PDA closure, all‐cause mortality in hospital, and adverse events, including azotemia, oliguria, hepatitis with deranged liver transaminase values, deranged coagulation, severe IVH (grade 3 and intraparenchymal extension), PVL, NEC (definite and advanced stage per modified Bell staging), BPD, and ROP necessitating therapy. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and other prespecified secondary outcomes.
Oncel 2014 was a single‐center study in Ankara, Turkey. It compared the effectiveness and safety of oral paracetamol and oral ibuprofen for the closure of PDA in preterm infants up to and including 30 weeks' gestational age, birth weight of 1250 g or less, postnatal age of 48 to 96 hours with echocardiographic diagnosis of hemodynamically significant PDA. Infants were randomised to oral paracetamol (15 mg/kg/dose every six hours for three days; n = 40) or oral ibuprofen (10‐5‐5 mg/kg/dose every 24 hours; n = 40). The study's outcomes included rates of ductal closure, all‐cause mortality during initial hospital stay, neonatal mortality (first 28 days of life), infant mortality, re‐opening of the ductus arteriosus, surgical closure of the PDA, duration of ventilatory support, duration of need for supplementary oxygen, pulmonary hemorrhage, pulmonary hypertension, BPD (at 28 days' and at 36 weeks' postmenstrual age, severe BPD at 36 weeks' postmenstrual age), IVH (all grades and Grade III to IV), PVL, NEC, intestinal perforation, gastrointestinal bleeding, ROP (any stage, stage ≥ 3, ROP requiring laser treatment), oliguria (urine output < 1 mL/kg/h), serum levels after treatment of creatinine, bilirubin, AST, ALT, liver failure, duration of hospital stay, and sepsis. In 2017, the authors published neurodevelopmental outcomes of the infants enrolled in this trial. They reported on 30 children in the paracetamol group and 31 children in the ibuprofen group. They reported on neurodevelopmental impairment, mental development index (MDI) of less than 70, psychomotor developmental index (PDI) of less than 70, moderate to severe cerebral palsy, blindness, deafness, and MDI and PDI at 18 to 24 months' corrected age. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and other prespecified secondary short‐ and long‐term outcomes.
Shahmirzadi 2021 was a single‐center study at Amiralmomenin Hospital, Semnan, Iran between May 2018 and May 2019. It evaluated the efficacy and gastrointestinal complications of IV paracetamol and oral ibuprofen for the closure of PDA in preterm infants born at less than 37 weeks' gestational age, less than 14 days' postnatal age, and diagnosis of PDA. Infants were randomised to IV paracetamol (15 mg/kg/dose every six hours for two days; n = 23) or oral ibuprofen (10‐5‐5 mg/kg/dose every 24 hours; n = 17). The study's outcomes included failure of ductal closure after treatment, NEC, gastrointestinal bleeding, and feeding intolerance. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and prespecified secondary outcomes.
Tauber 2020 was a prospective RCT between January 2017 and May 2019. It compared the efficacy of IV paracetamol and IV ibuprofen for closure of PDA in preterm infants at 23 to 29weeks' gestational age at birth with a hemodynamically significant PDA diagnosed by echocardiogram within the first two weeks of life. Infants were randomised to IV paracetamol (15 mg/kg/dose every six hours for three days; n = 5) or IV ibuprofen (10‐5‐5 mg/kg/dose every 24 hours; n = 5). The study's outcomes included PDA closure rates and safety outcomes. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and prespecified secondary outcomes.
Yang 2016 was a single‐center study in Xuzhou, Jiangsu, China. It aimed to understand the effect of paracetamol treatment on preterm infants of less than 37 weeks' gestational age with a hemodynamically significant PDA between 15 hours and 10 days postnatal age, aiming to utilise and develop plasma and urinary prostaglandin E2 (PGE₂) levels as indicators of progress of PDA closure in a non‐invasive manner. Infants were randomised to oral paracetamol (15 mg/kg/dose every six hours for three days; n = 44) or oral ibuprofen (10‐5‐5 mg/kg/dose every 24 hours; n = 43). The study's outcomes included failure of primary ductal closure, oliguria (< 1 mL/kg/h), stools positive for occult blood, IVH, NEC, BPD, plasma PGE₂ (ng/L), urine PGE₂ (ng/L), platelet count (x10⁹/L), serum creatinine (µmol/L) and ALT (U/L) after treatment. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and prespecified secondary outcomes.
Studies comparing oral/IV paracetamol and oral/IV indomethacin
Four studies that enrolled 380 infants compared oral/IV paracetamol to oral/IV indomethacin. The following section provides a brief description of the included studies.
Dash 2015 was a single‐center study in Mumbai, India. It compared the effectiveness of oral paracetamol and IV indomethacin for closure of a PDA in preterm neonates with a birth weight of 1500 g or less and echocardiographic diagnosis of hemodynamically significant PDA within the first 48 hours of life. Infants were randomised to oral paracetamol (15 mg/kg/dose every six hours for seven days; n = 38) or IV indomethacin (0.2 mg/kg/dose once daily for three days; n = 39). The study's outcomes included failure to close the PDA, surgical ligation, ROP, gastrointestinal bleeding, NEC, pulmonary hemorrhage, IVH, sepsis, daily urine output, serum creatinine, serum bilirubin, and platelet count. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and prespecified secondary outcomes.
Davidson 2021 was a multi‐center, non‐inferiority RCT at two level 3 NICUs and one level 4 NICU in Memphis, Tennessee, USA, from June 2016 to September 2018. It compared the rate of successful treatment of a hemodynamically significant PDA after use of IV acetaminophen or IV indomethacin in preterm infants of 22 to 32 weeks' gestational age, birth weight of less than 1500 g, up to and including 21 days' postnatal age, platelet count greater than 50 × 109/L, no previous pharmacological treatment for PDA, and strict echocardiogram criteria for ascertaining the hemodynamic significance of PDA. Infants were randomised to IV paracetamol (15 mg/kg/dose every six hours for three days; n = 17) or IV indomethacin (postnatal age‐adjusted dosing every 12 hours; n = 20). The study's outcomes included rate of successful PDA treatment, additional PDA treatment, surgical or transcatheter closure, duration of invasive mechanical ventilation, respiratory support at 36 weeks' postmenstrual age, NEC, IVH (Grade 3 or 4), ROP, days to full feeds (150 cc/kg/d), gastrointestinal perforation, length of stay, renal dysfunction, creatinine elevation greater than 1.5 mg/dL during treatment, and discharge disposition. The baseline characteristics were similar between the two groups except for left atrial size to aortic root ratio (LA:Ao ratio), which was higher in the indomethacin group. The authors found a significant difference between the two groups with regards to ductal closure rates favouring the indomethacin group (11/20 in the indomethacin group versus 1/17 in the paracetamol group; P = 0.002). There were no differences between the two groups for other prespecified secondary outcomes.
Meena 2020 was a single‐center, three‐arm RCT in the Division of Pediatric Cardiology, Department of Pediatrics, MDM and Umaid Hospital, Dr SN Medical College, Jodhpur, India. It compared the efficacy and safety of ibuprofen, indomethacin, and paracetamol in the closure of PDA in preterm neonates of less than 37 weeks' gestational age, in the first 28 days of life, with hemodynamically significant PDA. Infants were randomised to IV paracetamol (15 mg/kg/dose every six hours for three days; n = 35), oral ibuprofen (10‐5‐5 mg/kg/dose; n = 35), or oral indomethacin (postnatal age‐adjusted dosing at 12‐hourly intervals; n = 35) for PDA treatment. The study's outcomes included PDA closure after the first and second course of treatment and adverse effects in each group. The baseline characteristics were similar between the three groups. The authors found no significant difference between the groups with regards to ductal closure rates after the first and second course of treatment. There was significant increase in BUN and serum creatinine post‐treatment in the ibuprofen and indomethacin groups. There were no significant differences for other prespecified secondary outcomes between the three groups.
Studies comparing prophylactic oral/IV paracetamol versus placebo/no intervention
Three studies that enrolled 240 infants compared oral/IV paracetamol to oral/IV indomethacin. The following section provides a brief description of the included studies.
Asbagh 2015 was a single‐center study in Tehran, Iran, from March 2012 to March 2013. It aimed to determine the effectiveness of prophylactic treatment with oral paracetamol for PDA in preterm infants of 32 weeks' gestational age or less, birth weight of 1500 g or less, and a postnatal age of less than 24 hours. Infants were randomised to prophylactic oral paracetamol (15 mg/kg/dose every six hours for 48 hours; n = 16) or no intervention (n = 16). The study's outcomes included failure to close a PDA by four to five days, death, and needing treatment with ibuprofen. The baseline characteristics were similar between the two groups. The authors found no significant difference between the two groups with regards to ductal closure rates and prespecified secondary outcomes.
Bagheri 2018 was a single‐center RCT in the NICU of the Afzalipour tertiary hospital, Kerman, Iran, between November 2015 and 2016. It aimed to assess the efficacy of prophylactic IV paracetamol versus no intervention in decreasing the rate of ductal patency in preterm infants of 34 weeks' gestational age or less. Infants were randomised to prophylactic IV paracetamol (20 mg/kg immediately followed by 7.5 mg/kg every six hours during the first three days; n = 80) or no intervention (n = 80). The study's outcomes included frequency of PDA on day four of life, all‐cause mortality, duration of mechanical ventilation, and duration of hospitalization. The baseline characteristics were similar between the two groups. The authors found a significant difference between the two groups with regards to the frequency of PDA favouring the prophylactic paracetamol group (12/80 in prophylactic paracetamol group versus 57/80 in the no‐intervention group; P < 0.001). There were no significant differences between the two groups for other prespecified secondary outcomes.
Härkin 2016 was a single‐center study in the NICU of Oulu University Hospital, Oulu, Finland. It studied the biologic effect of prophylactic paracetamol on early closure of PDA in preterm infants of less than 32 weeks' gestational age and of less than 24 hours of age. Infants were randomised to prophylactic IV paracetamol (20 mg/kg followed by 7.5 mg/kg/dose every six hours for four days; n =23) or placebo (0.45% NaCl; n = 25). The study's outcomes included decrease in ductal calibre without side effects and failure to close a PDA by four to five days, permanent closure of PDA, oliguria (< 1 mL/kg/h), polyuria (> 5 mL/kg/h), hypernatremia (> 150 mmol/L), sepsis, supplemental oxygen at 28 days, supplemental oxygen at 36 weeks' postmenstrual age, ROP treated, IVH grades 1 to 2, IVH grades 3 to 4, NEC stage 3, death, days of supplemental oxygen, and the highest serum bilirubin (µmol/L). In 2019, the authors published growth, cardiac, and neurodevelopmental outcomes of the infants enrolled in this trial at two years' corrected age. They reported on 23 children in the paracetamol group and 21 children in the control group. The baseline characteristics were similar between the two groups. The mean (95% CI) postnatal ages for ductal closure were 177 hours (31.1 to 324) for the paracetamol‐treated group versus 338 hours (118 to 557) for controls (P = 0.045). There were no significant differences between the two groups for other prespecified short‐ and long‐term outcomes.
Studies comparing early (< 14 days' postnatal age) oral/IV paracetamol versus placebo/no intervention
Two studies that enrolled 127 infants compared early oral/IV paracetamol to placebo or no intervention. The following section provides a brief description of the included studies.
Babaei 2018 was a single‐center RCT in the NICU of the Imam Reza Hospital in Kermanshah City, Iran in 2015. It aimed to evaluate the effect of oral acetaminophen on closure of PDA in preterm neonates of 34 weeks' gestational age or less, postnatal age of less than 14 days, and with a hemodynamically significant PDA. Infants were randomised to the oral paracetamol group (15 mg/kg/dose every six hours for 72 hours; n = 36) or a control group which received no intervention (n = 33). The study's outcomes included primary and secondary closure rate of PDA and hepatotoxicity. The baseline characteristics were similar between the two groups. The authors found a significant difference between the two groups with regards to overall PDA closure rates favouring the paracetamol group (34/36 in paracetamol group versus 5/33 in the no‐intervention group; P = 0.001). There were no significant differences between the two groups for other prespecified secondary outcomes.
Schindler 2021 was a double‐blind, placebo‐controlled, parallel, two‐arm, randomised, phase II, single‐center trial between November 2016 and March 2019. It investigated whether early treatment with paracetamol reduced the number of infants requiring intervention for PDA and assessed the safety profile of paracetamol compared to placebo in preterm infants born at less than 29 weeks' gestational age, less than six hours old, and with a ductus arteriosus of 1.0 mm diameter or greater with less than 30% right to left shunt (implying normal circulatory adaptation). Infants were randomised to IV paracetamol (15 mg/kg followed by 7.5 mg/kg/dose every six hours for five days; n =29) or placebo (IV 5% dextrose 1.5 mL/kg, followed by 0.75 mL every six hours for five days; n = 29). The study's outcomes included any intervention for management of PDA up to five days' postnatal age, closure of ductus arteriosus at five days' postnatal age, size of the ductus arteriosus at 48 hours and at five days' postnatal age, ductal re‐opening during admission, ductus arteriosus parameters, systemic blood flow measurements, adverse events during the treatment period, mortality, pulmonary hemorrhage, NEC, early‐onset sepsis, late‐onset sepsis, IVH, PVL, BPD, and ROP. The baseline characteristics were similar between the two groups. The authors found a significant difference between the two groups with regards to any intervention for PDA up to five days of life favouring the paracetamol group (6/29 in paracetamol group versus 17/29 in placebo group; P = 0.003). There were no significant differences between the two groups for other prespecified secondary outcomes.
Studies comparing late (> 14 days' postnatal age) oral/IV paracetamol versus placebo/no intervention
One study in 55 infants compared late oral/IV paracetamol to placebo or no intervention. The following section provides a brief description of this study.
Kluckow 2019 was a multi‐center, prospective, randomised, blinded, placebo‐controlled pilot trial in three Australian tertiary NICUs from March 2012 to December 2015. It aimed to explore the efficacy and risks of oral paracetamol in late treatment of PDA in preterm infants of less than 33 weeks' gestational age and postnatal age of more than two weeks, with a hemodynamically significant PDA and tolerating at least 50% of enteral feeds. Infants were randomized to oral paracetamol (loading dose of 25 mg/kg/dose followed by 15 mg/kg per dose. The maintenance dosing interval was a 12‐hourly interval in preterm infants of less than 32 weeks' postmenstrual age, an 8‐hourly interval in infants of 32 to 36 weeks' postmenstrual age, and a 6‐hourly interval in term infants, for a total of five days; n = 27) or placebo (same volume and similar to paracetamol in consistency and colour; n = 28). The study's outcomes included PDA closure, significant (> 25%) constriction of ductal diameter, safety of paracetamol assessed by determining serum paracetamol levels and liver function tests, change in respiratory status (pre‐treatment versus post‐treatment), feed intolerance, abdominal distension, mortality, and BPD. The baseline characteristics were similar between the two groups except for a higher number of males in the paracetamol group. There was a significant difference between the two groups favouring the paracetamol group with regards to ductal closure (4/27 in the paracetamol group versus 0/28 in the placebo group; P = 0.03) and significant constriction of PDA (13/23 in the paracetamol group versus 7/28 in the placebo group; P < 0.001). There were no differences between the two groups for other prespecified secondary outcomes.
Studies comparing combination treatment (ibuprofen plus paracetamol) versus ibuprofen plus placebo/no intervention
Two studies that enrolled 111 infants compared oral/IV ibuprofen plus paracetamol to oral/IV ibuprofen plus placebo or no intervention. The following section provides a brief description of these two studies.
Hochwald 2018 was a randomised, double‐blind, prospective pilot study in the NICU of Rambam Medical Center in Haifa, Israel, between 2014 and 2016. It compared the closure rate of hemodynamically significant PDA for IV ibuprofen plus paracetamol versus ibuprofen plus placebo in preterm infants of 24 to 31 weeks' gestational age with a hemodynamically significant PDA. Infants were randomised to IV paracetamol plus ibuprofen (ibuprofen 10‐5‐5 mg/kg/dose and paracetamol: loading dose of 20 mg/kg followed by 10 mg/kg every six hours for three days; n = 12) or ibuprofen plus placebo (10‐5‐5 mg/kg/dose and placebo [0.9% normal saline]; n =12). The study's outcomes included failure of ductal closure after one or two courses, need for a second course, need for surgical ligation, rates of ductal re‐opening, duration of ventilation, pneumothorax, pulmonary hemorrhage, BPD, IVH, NEC, gastrointestinal bleeding, ROP, sepsis, and death. Safety parameters included an increase in serum creatinine, decrease in urine output to less than 1 mL/kg/h, AST or ALT levels, as well as paracetamol levels. The baseline characteristics were similar between the two groups. There were no differences between the two groups for ductal closure rates and prespecified secondary outcomes.
Oboodi 2020 was a three‐arm, multi‐center RCT in the NICUs of two hospitals (Nemazee Hospital and Hafez Hospital) affiliated with the Shiraz University of Medical Science, Iran from March 2016 to March 2017. It evaluated the efficacy and safety of ibuprofen plus paracetamol, ibuprofen alone, and paracetamol alone for PDA closure in preterm infants with a hemodynamically significant PDA and a postnatal age up to 14 days. Infants were randomised to oral ibuprofen plus IV paracetamol (ibuprofen 10‐5‐5 mg/kg/dose for three doses 24 hours apart and paracetamol: 15 mg/kg every six hours for three days; n = 19) or oral ibuprofen (10‐5‐5 mg/kg/dose for three doses 24 hours apart; n = 68) or IV paracetamol (15 mg/kg every six hours for three days; n = 67). The study's outcomes included ductal closure rates after first and second course of treatment, platelet count, blood urea nitrogen, bilirubin, serum creatinine, AST and ALT pre‐ and post‐treatment course, NEC, renal or liver dysfunction, bleeding tendency, IVH grade 3 or 4, and intestinal perforation. The baseline characteristics were similar between the two groups. There were no differences between the two groups for ductal closure rates and prespecified secondary outcomes.
Excluded studies
We excluded four studies, which were all observational in nature (Cakir 2021; Höck 2020; King 2020; Shah 2021). See Characteristics of excluded studies.
Risk of bias in included studies
The risk of bias in included studies is shown in Figure 2 and Figure 3. Fourteen of the 27 included studies had high risk of bias in the blinding of participants and personnel domain. We assessed five studies to be of low risk of bias across all domains (El‐Farrash 2019; Härkin 2016; Hochwald 2018; Kluckow 2019; Kumar 2020; see Figure 3).

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
We assessed the risk of selection bias regarding random sequence generation to be high in two studies (Asadpour 2018; Ghaderian 2019a), unclear in three studies (Babaei 2018; Meena 2020; Tauber 2020), and low in the remaining 22 studies (Al‐Lawama 2017; Asbagh 2015; Bagheri 2016; Bagheri 2018; Balachander 2020; Dang 2013; Dani 2021; Dash 2015; Davidson 2021; El‐Farrash 2019; El Mashad 2017; Ghaderian 2019b; Härkin 2016; Hochwald 2018; Jafari 2019; Kluckow 2019; Kumar 2020; Oboodi 2020; Oncel 2014; Schindler 2021; Shahmirzadi 2021; Yang 2016). Asadpour 2018 reported that infants were "[randomly] allocated in 1:1 ratio by convenient sampling method". Ghaderian 2019a reported that "[neonates] were allocated in either group based on even or odd hospital registration number".
Fifteen studies used sequentially‐numbered, sealed, opaque envelopes for allocation to the two treatment groups and thus we judged these to be of low risk of selection bias due to allocation concealment (Al‐Lawama 2017; Asadpour 2018; Balachander 2020; Dang 2013; Dani 2021; Dash 2015; Davidson 2021; El‐Farrash 2019; El Mashad 2017; Härkin 2016; Hochwald 2018; Kluckow 2019; Kumar 2020; Oncel 2014; Schindler 2021). The risk of selection bias regarding allocation concealment was unclear in 11 studies (Asbagh 2015; Babaei 2018; Bagheri 2016; Ghaderian 2019a; Ghaderian 2019b; Jafari 2019; Meena 2020; Oboodi 2020; Shahmirzadi 2021; Tauber 2020; Yang 2016). Bagheri 2018 reported that the "[control] group didn't receive any medication" so we deemed this study as being at high risk of bias for allocation concealment.
Blinding
Performance bias
Fourteen studies had high risk of bias in the domain of blinding of participants and personnel (Al‐Lawama 2017; Bagheri 2016; Bagheri 2018; Balachander 2020; Dang 2013; Dani 2021; Dash 2015; Davidson 2021; El Mashad 2017; Ghaderian 2019a; Ghaderian 2019b; Oncel 2014; Tauber 2020; Yang 2016). Six studies had low risk of bias in the domain of blinding of participants and personnel (El‐Farrash 2019; Härkin 2016; Hochwald 2018; Kluckow 2019; Kumar 2020; Schindler 2021), and the remaining seven studies were unclear (Asadpour 2018; Asbagh 2015; Babaei 2018; Jafari 2019; Meena 2020; Oboodi 2020; Shahmirzadi 2021).
Detection bias
In the domain of blinding of outcome assessment, 13 studies had low risk of bias (Bagheri 2016; Bagheri 2018; Balachander 2020; Dani 2021; Davidson 2021; El‐Farrash 2019; El Mashad 2017; Ghaderian 2019a; Ghaderian 2019b; Härkin 2016; Hochwald 2018; Kluckow 2019; Kumar 2020). Three studies had high risk of bias (Dang 2013; Dani 2021; Oncel 2014) and the remaining 11 studies had unclear risk of bias (Al‐Lawama 2017; Asadpour 2018; Asbagh 2015; Babaei 2018; Jafari 2019; Meena 2020; Oboodi 2020; Schindler 2021; Shahmirzadi 2021; Tauber 2020; Yang 2016).
Incomplete outcome data
With the exception of Bagheri 2016, we assessed all included studies as having a low risk of attrition bias as they reported outcome data for all prespecified outcomes and for all enrolled infants. We assessed Bagheri 2016 as having a high risk of bias in this domain as not all infants randomized were subsequently analyzed.
Selective reporting
The protocols for 14 studies were available to us as the trials were registered prospectively (Babaei 2018; Dang 2013; Dani 2021; Davidson 2021; El‐Farrash 2019; Ghaderian 2019b; Härkin 2016; Hochwald 2018; Kluckow 2019; Kumar 2020; Oboodi 2020; Oncel 2014; Schindler 2021; Tauber 2020). We assessed these as having a low risk of reporting bias as there did not seem to be any deviations from the protocols for these studies. We judged the remaining 13 studies to have an unclear risk of bias in this domain: five studies were registered retrospectively (Al‐Lawama 2017; Balachander 2020; Bagheri 2018; Dash 2015; Jafari 2019); eight studies were not registered (Asadpour 2018; Asbagh 2015; Bagheri 2016; El Mashad 2017; Ghaderian 2019a; Meena 2020; Shahmirzadi 2021; Yang 2016).
Other potential sources of bias
We identified no other potential sources of bias in the 27 included studies.
Effects of interventions
See: Summary of findings 1 Paracetamol versus ibuprofen for PDA in preterm or low birth weight infants; Summary of findings 2 Paracetamol versus indomethacin for PDA in preterm or low birth weight infants ; Summary of findings 3 Prophylactic administration of paracetamol versus placebo or no intervention for PDA in preterm or low birth weight infants; Summary of findings 4 Early paracetamol versus placebo/no intervention for PDA in preterm or low birth weight infants; Summary of findings 5 Late paracetamol versus placebo/no intervention for PDA in preterm or low birth weight infants; Summary of findings 6 Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention for PDA in preterm or low birth weight infants
Comparison 1. Paracetamol (oral or IV) versus ibuprofen (oral or IV)
See summary of findings Table 1.
Primary outcomes
Failure of PDA closure after first course of paracetamol treatment
Eighteen studies (1535 infants) reported this outcome (Al‐Lawama 2017; Asadpour 2018; Bagheri 2016; Balachander 2020; Dang 2013; Dani 2021; El‐Farrash 2019; El Mashad 2017; Ghaderian 2019a; Ghaderian 2019b; Jafari 2019; Kumar 2020; Meena 2020; Oboodi 2020; Oncel 2014; Shahmirzadi 2021; Tauber 2020; Yang 2016). There was probably little to no difference between the paracetamol and the ibuprofen groups in failure of PDA closure after the first course of treatment (RR 1.02, 95% 0.88 to 1.18; I2 = 16%. RD 0.01, 95% CI −0.04 to 0.05; I2= 29%; moderate‐certainty evidence; Analysis 1.1). Visual inspection of the funnel plot did not reveal publication bias (Figure 4).

Funnel plot: failure of PDA closure after first course of treatment for comparison 'Paracetamol (oral or IV) versus ibuprofen (oral or IV)'
Neurodevelopmental impairment at 18 to 24 months (corrected age)
One study reported this outcome in 61 children (Oncel 2014). There was little to no difference between the paracetamol and the ibuprofen groups in the incidence of neurodevelopmental impairment (RR 0.93, 95% CI 0.44 to 1.96. RD −0.02, 95% CI −0.25 to 0.21; low‐certainty evidence; Analysis 1.2). Tests for heterogeneity were not applicable.
There were little to no differences between the groups for the following outcomes in the follow‐up report by Oncel 2014: mental development index (MDI) of less than 70, Analysis 1.31; psychomotor developmental index (PDI) of less than 70, Analysis 1.32; moderate to severe cerebral palsy, Analysis 1.33; deafness, Analysis 1.34; blindness, Analysis 1.35; MDI, Analysis 1.36; or PDI, Analysis 1.37. As there was only one study included in these analyses, tests for heterogeneity were not applicable.
Death or disability at 18 to 24 months
No studies reported this outcome (including the follow‐up study of Oncel 2014).
Secondary outcomes
All‐cause mortality during initial hospital stay
Eight studies (734 infants) reported this outcome (Al‐Lawama 2017; Balachander 2020; Dang 2013; Dani 2021; El‐Farrash 2019; Jafari 2019; Kumar 2020; Oncel 2014). There was probably little to no difference between the paracetamol and the ibuprofen groups for all‐cause mortality during the initial hospital stay (RR 1.09, 95% CI 0.80 to 1.48; I² = 0%. RD 0.01, 95% CI −0.04 to 0.07; I² = 0%; moderate‐certainty evidence; Analysis 1.3).
Re‐opening of the ductus arteriosus
Defined as echocardiographic evidence of closure followed by re‐opening of PDA at a later stage.
Five studies (458 infants) reported this outcome (Balachander 2020; Dang 2013; Dani 2021; Kumar 2020; Oncel 2014). There was little to no difference between the paracetamol and the ibuprofen groups in the risk of re‐opening of the ductus arteriosus (RR 1.35, 95% CI 0.85 to 2.12, I² = 0%. RD 0.04, 95% CI ‐0.02 to 0.1; I² = 2%; Analysis 1.5).
Failure of PDA closure after second course of treatment
Thirteen studies reported this outcome in 393 infants (Al‐Lawama 2017; Asadpour 2018; Bagheri 2016; Balachander 2020; Dang 2013; El Mashad 2017; El‐Farrash 2019; Ghaderian 2019a; Ghaderian 2019b; Kumar 2020; Meena 2020; Oboodi 2020; Oncel 2014). There was little to no difference in failure of PDA closure after the second course of treatment (RR 0.97, 95% CI 0.78 to 1.21; I² = 0%. RD −0.01, 95% CI −0.11 to 0.08; I² = 0%; Analysis 1.6). Visual inspection of the funnel plot did not reveal publication bias (Figure 5).

Funnel plot: failure of PDA closure after second course of treatment for comparison 'Paracetamol (oral or IV) versus ibuprofen (oral or IV)'
Surgical closure of the PDA
Six studies (603 infants) reported this outcome (Dani 2021; El‐Farrash 2019; El Mashad 2017; Kumar 2020; Oncel 2014; Tauber 2020). There was little to no difference between the paracetamol and the ibuprofen groups in surgical closure of the PDA (RR 0.61, 95% CI 0.34 to 1.08, I² = 0%. RD −0.04, 95% CI −0.08 to 0.00; I² = 0%; Analysis 1.7).
Duration of need for supplementary oxygen (days)
One study (90 infants) reported this outcome (Oncel 2014). There was little to no difference between the paracetamol and the ibuprofen groups in the duration of need for supplementary oxygen (O₂) favouring the paracetamol group (mean difference (MD) −12.40 days, 95% CI −22.97 to −1.83; Analysis 1.9). The test for heterogeneity was not applicable.
Pulmonary hemorrhage
Defined as blood‐stained liquid flowing from the trachea of the infant.
Five studies (442 infants) reported this outcome (Al‐Lawama 2017; El‐Farrash 2019; El Mashad 2017; Meena 2020; Oncel 2014). There was little to no difference between the paracetamol and the ibuprofen groups in the risk of pulmonary hemorrhage (RR 0.87, 95% CI 0.36 to 2.09, I² = 0%. RD −0.01, 95% CI −0.04 to 0.03; I² = 0%; Analysis 1.10).
Intraventricular hemorrhage (IVH) (Grade I‐IV)
Eight studies reported this outcome, in 800 infants (Al‐Lawama 2017; Balachander 2020; Dang 2013; Dani 2021; El Mashad 2017; Jafari 2019; Oncel 2014; Yang 2016). There was probably little to no difference between the paracetamol and the ibuprofen groups in the risk of IVH (RR 0.97, 95% CI 0.77 to 1.22; I² = 0%. RD −0.01, 95% CI −0.05 to 0.04; I² = 0%; Analysis 1.15).
Severe IVH (Grade III‐IV)
Six studies reported this outcome, in 544 infants (Al‐Lawama 2017; Dang 2013; Dani 2021; Jafari 2019; Kumar 2020; Oncel 2014). There was probably little to no difference between the paracetamol and the ibuprofen groups in the risk of severe IVH (RR 0.63, 95% CI 0.28 to 1.43; I² = 0%. RD −0.02, 95% CI −0.05 to 0.02; I² = 0%; Analysis 1.16).
Periventricular leukomalacia (PVL)
Four studies reported this outcome, in 421 infants (Al‐Lawama 2017; Dang 2013; Kumar 2020; Oncel 2014). There was little to no difference between the paracetamol and the ibuprofen groups in the risk of PVL (RR 1.40, 95% CI 0.56 to 3.50; I² = 0%. RD 0.01, 95% CI −0.03 to 0.05; I² = 0%; Analysis 1.17).
Necrotizing enterocolitis (NEC)
Ten studies (1015 infants) reported this outcome (Al‐Lawama 2017; Balachander 2020; Dang 2013; Dani 2021; El Mashad 2017; Kumar 2020; Meena 2020; Oncel 2014; Shahmirzadi 2021; Yang 2016). There was probably little to no difference between the paracetamol and the ibuprofen groups for NEC (RR 1.30, 95% CI 0.87 to 1.94; I² = 0%. RD 0.02, 95% CI −0.01 to 0.05, I² = 17%; moderate‐certainty evidence; Analysis 1.18).
Gastrointestinal bleed
Seven studies (693 infants) reported gastrointestinal bleeding (Asadpour 2018; Dang 2013; El Mashad 2017; Meena 2020; Oncel 2014; Shahmirzadi 2021; Yang 2016). There may be a reduction in the incidence of gastrointestinal bleeding in the paracetamol group compared to the ibuprofen group (RR 0.37, 95% CI 0.19 to 0.73; I² = 10%. RD −0.05, 95% CI −0.09 to −0.02; I² = 25%; Analysis 1.20). The NNTB was 20, 95% CI 12 to 54.
Oliguria
Decreased urine output defined as < 1 mL/kg/h during treatment.
Five studies (608 infants) reported this outcome (Balachander 2020; Dang 2013; Kumar 2020; Oncel 2014; Yang 2016). Oliguria did not occur in any infant in the study by Oncel 2014. There was likely a reduction in oliguria favouring the paracetamol group, in the comparison between paracetamol and ibuprofen (RR 0.47, 95% CI 0.30 to 0.76; I2 = 0%. RD −0.08, 95% CI −0.13 to ‐0.03; I2= 76%; Analysis 1.23).
Sepsis
Clinical symptoms and signs of sepsis and a positive blood bacterial culture.
Seven studies (844 infants) reported this outcome (Al‐Lawama 2017; Balachander 2020; Dang 2013; Dani 2021; El Mashad 2017; Kumar 2020; Oncel 2014). There was little to no difference between the paracetamol and the ibuprofen groups in the risk for sepsis (RR 0.93, 95% CI 0.72 to 1.22; I² = 0%. RD −0.01, 95% CI −0.07 to 0.04; I2=15%; Analysis 1.24).
Post‐pre difference in serum or plasma levels of creatinine (mg/dL)
Six studies (557 infants) reported this outcome (Asadpour 2018; El‐Farrash 2019; El Mashad 2017; Meena 2020; Oncel 2014; Yang 2016). There was likely a reduction, favouring the paracetamol group, in post‐pre treatment difference in serum creatinine levels in the comparison between paracetamol and ibuprofen (MD −0.12 mg/dL, 95% CI −0.13 to −0.10; I² = 88%; Analysis 1.25). This result indicates that creatinine levels were probably higher post‐treatment with ibuprofen compared with paracetamol.
Serum bilirubin (μmol/L) following treatment
Four studies reported this outcome, in 400 infants (Asadpour 2018; El‐Farrash 2019; El Mashad 2017; Oncel 2014). There was likely a reduction in serum bilirubin (μmol/L) following treatment in both the paracetamol and the ibuprofen groups, with lower serum bilirubin levels in the paracetamol group (MD −10.56 µmol/L, 95% CI −13.16 to −7.96; I² = 82%; Analysis 1.28).
Hyperbilirubinemia
Defined as a serum bilirubin level higher than the exchange level according to the postnatal age and body weight.
One study reported this outcome in 160 infants (Dang 2013). There was likely a reduction in hyperbilirubinemia favouring the paracetamol group compared to the ibuprofen group (RR 0.57, 95% CI 0.34 to 0.97; RD −0.15, −0.29 to −0.01; NNTB 7, 95% CI 3 to 100; Analysis 1.29).
Other secondary outcomes
There were little to no differences between the paracetamol (oral or IV) group compared to the ibuprofen group (oral or IV) for the following outcomes.
-
Neonatal mortality (death during the first 28 days of life), as illustrated in Analysis 1.4.
-
Duration of ventilator support (days) (Analysis 1.8).
-
Pulmonary hypertension (defined as an increased mean pulmonary arterial pressure of 25 mmHg at rest) (Analysis 1.11).
-
BPD at 36 weeks' postmenstrual age (defined as O₂ requirement at 36 weeks' postmenstrual age in addition to compatible clinical and roentgenographic findings) (Analysis 1.12).
-
Moderate to severe BPD according to the new criteria (i.e. moderate BPD defined as O₂ for ≥ 28 days plus treatment with < 30% O₂ at 36 weeks' postmenstrual age; and severe BPD as O₂ for ≥ 28 days plus ≥ 30% O₂ or positive pressure at 36 weeks' postmenstrual age, or both) (Analysis 1.13).
-
Severe BPD defined according to the new criteria (i.e. severe BPD defined as O₂ for ≥ 28 days plus ≥ 30% O₂ or positive pressure at 36 weeks' postmenstrual age, or both (Analysis 1.14)).
-
Intestinal perforation (Analysis 1.19).
-
ROP stage 3 or higher (according to the international classification of ROP) (Analysis 1.21).
-
ROP requiring treatment (Analysis 1.22).
-
Serum or plasma levels of aspartate transaminase (AST) (U/L) following treatment (Analysis 1.26).
-
Post‐pre difference in serum or plasma levels of ALT (U/L) (Analysis 1.27).
-
Duration of hospitalization (total length of hospitalization from birth to discharge home or death, in days) (Analysis 1.30).
Incidence of liver failure
Defined as evidence of acute liver injury combined with either severe coagulopathy (international normalized ratio (INR) > 2.0 or prothrombin time (PT) > 20 seconds) or encephalopathy with moderate coagulopathy (INR ≥ 1.5 or PT ≥ 15 seconds).
One study (90 infants) reported this outcome (Oncel 2014). Liver failure did not occur in any infant enrolled in the study.
Autism or autism spectrum disorder (ASD) in childhood
As defined by the American Psychiatric Association (APA 2013).
No study has reported on this outcome, but Oncel 2014 indicates in his follow‐up study that the authors plan to re‐evaluate their cohort in terms of autism spectrum disorders in the future.
Other side effects reported by the authors (not prespecified)
Oncel 2014 found no other side effects.
The following outcomes were not reported: treatment with indomethacin, ibuprofen or another prostaglandin inhibitor to close the PDA, acute kidney injury, number of infants with AST or ALT greater than 100 U/L, and language delay.
Comparison 1 subgroup analysis: paracetamol (oral or IV) versus ibuprofen (oral or IV) in infants of less than 32 weeks' gestational age
Primary outcomes
Failure of PDA closure after first course of paracetamol treatment
Six studies reported this outcome in 584 infants (Al‐Lawama 2017; Dani 2021; El Mashad 2017; Kumar 2020; Oncel 2014; Tauber 2020). There was little to no difference between the paracetamol and ibuprofen groups for failure of PDA closure after one course of treatment (RR 1.29, 95% CI 1.00 to 1.66; I2 = 47%. RD 0.07, 95% CI 0.00 to 0.15; I2= 59%; Analysis 7.1).
Neurodevelopmental impairment at 18 to 24 months corrected age
No studies reported on this outcome.
Death or disability at 18 to 24 months
No studies reported on this combined outcome.
Secondary outcomes
There was little to no difference between the paracetamol (oral or IV) and ibuprofen (oral or IV) groups for the following outcomes:
-
all‐cause mortality during initial hospital stay (Analysis 7.2);
-
failure of PDA closure after two courses of treatment (Analysis 7.3);
-
surgical ligation of PDA (Analysis 7.4);
-
IVH (all grades) (Analysis 7.5);
-
severe IVH (Analysis 7.6);
-
NEC (Analysis 7.7);
-
gastrointestinal bleed or stools positive for occult blood (Analysis 7.8).
Comparison 2. Paracetamol (oral or IV) versus indomethacin (oral or IV)
See summary of findings Table 2.
Primary outcomes
Failure of PDA closure after first course of treatment
Four studies reported this outcome in 380 infants (Dash 2015; Davidson 2021; El Mashad 2017; Meena 2020). There was little to no difference between the paracetamol and indomethacin groups (RR 1.02, 95% CI 0.78 to 1.33, I² = 76%. RD 0.01, 95% CI −0.07 to 0.08; I² = 85%; low‐certainty evidence; Analysis 2.1).
Neurodevelopmental impairment at 18 to 24 months (corrected age)
No studies reported this outcome.
Death or disability at 18 to 24 months
No studies reported this outcome.
Secondary outcomes
All‐cause mortality during initial hospital stay
Two studies reported this outcome in 114 infants (Dash 2015; Davidson 2021). There was little to no difference between the paracetamol and indomethacin groups for all‐cause mortality during initial hospital stay (RR 0.86, 95% CI 0.39 to 1.92, I² = 0%. RD −0.03, 95% CI −0.16 to 0.11; I² = 0%; low‐certainty evidence; Analysis 2.2).
Pulmonary hemorrhage
Three studies reported this outcome in 347 infants (Dash 2015; El Mashad 2017; Meena 2020). There was little to no difference between the paracetamol and indomethacin groups (RR 0.77, 95% CI 0.28 to 2.10; I² = 48%. RD −0.01, 95% CI −0.05 to 0.03; I² = 62%; Analysis 2.5).
IVH (Grade I‐IV)
Two studies reported this outcome in 275 infants (Dash 2015; El Mashad 2017). There was little to no difference between the paracetamol and indomethacin groups (RR 0.82, 95% CI 0.42 to 1.63; I² = 49%. RD −0.02, 95% CI −0.09 to 0.05; I² = 29%; Analysis 2.7).
NEC
Four studies reported this outcome in 384 infants (Dash 2015; Davidson 2021; El Mashad 2017; Meena 2020). There was likely a reduction for risk of NEC in the paracetamol group compared with the indomethacin group (RR 0.42, 95% CI 0.19 to 0.96; I² = 0%. RD −0.05, 95% CI −0.10 to ‐0.01; I² = 0%; low‐certainty evidence; Analysis 2.10).
Gastrointestinal bleed
Three studies reported this outcome in 347 infants (Dash 2015; El Mashad 2017; Meena 2020). There was little to no difference between the paracetamol and indomethacin groups (RR 0.63, 95% CI 0.32 to 1.25; I² = 71%. RD −0.04, 95% CI −0.10 to 0.02; I² = 54%; Analysis 2.11).
Sepsis
Three studies reported this outcome in 314 infants (Dash 2015; Davidson 2021; El Mashad 2017). There was little to no difference between the paracetamol and indomethacin groups (RR 1.04, 95% CI 0.59 to 1.82; I² = 0%. RD 0.01, 95% CI −0.07 to 0.08; I² = 0%; Analysis 2.14).
Post‐pre difference in serum creatinine (mg/dL)
Two studies reported this outcome in 270 infants (El Mashad 2017; Meena 2020). The post‐pre difference in serum creatinine was probably lower in the paracetamol group compared with the indomethacin group (MD −0.37, 95% CI −0.40 to −0.34; I2= 95%; Analysis 2.15). This result indicates that creatinine levels were likely higher post‐treatment with indomethacin compared with paracetamol.
Serum bilirubin (µmol/L) following treatment
One study reported this outcome in 200 infants (El Mashad 2017). The serum bilirubin was likely higher in the paracetamol group compared with the indomethacin group (MD 1.03 µmol/L, 95% CI 0.13 to 1.93; Analysis 2.16). Tests for heterogeneity were not applicable. The increase in serum bilirubin is not clinically relevant.
Other secondary outcomes
There were little to no differences between the paracetamol (oral or IV) group compared to the indomethacin group (oral or IV) for the following outcomes:
-
failure of PDA closure after second course of treatment (Analysis 2.3);
-
surgical closure of PDA (Analysis 2.4);
-
BPD at 36 weeks' postmenstrual age (Analysis 2.6);
-
IVH (Grade III‐IV) (Analysis 2.8);
-
PVL (Analysis 2.9);
-
severe ROP requiring treatment (Analysis 2.12);
-
acute kidney injury (Analysis 2.13).
The following outcomes were not reported: neonatal mortality, re‐opening of the ductus arteriosus, failure of PDA closure after two courses, treatment with indomethacin, ibuprofen or another prostaglandin inhibitor to close the PDA, duration of ventilator support, duration of supplementary oxygen, pulmonary hypertension, BPD defined as per new criteria, intestinal perforation, decreased urine output, post‐pre difference in AST (U/L), post‐pre difference in ALT (U/L), number of infants with AST or ALT greater than 100 U/L, hyperbilirubinemia, liver failure, duration of hospitalization, ASD, language delay and other side effects.
Comparison 2 subgroup analysis: paracetamol (oral or IV) versus indomethacin (IV) in infants of less than 32 weeks' gestational age
Primary outcome
Failure of PDA closure after first course of treatment
Three studies reported this outcome in 310 infants (Dash 2015; Davidson 2021; El Mashad 2017). There was little to no difference between the paracetamol and indomethacin groups for failure of PDA closure after the first course of treatment (RR 1.27, 95% CI 0.86 to 1.87; I2 = 65%. RD 0.05, 95% CI ‐0.03 to 0.13; I2= 89%; Analysis 8.1).
Neurodevelopmental impairment at 18 to 24 months corrected age
No studies reported this outcome.
Death or disability at 18 to 24 months
No studies reported this outcome.
Secondary outcomes
There were little to no differences between the paracetamol (oral or IV) group compared to the indomethacin group (oral or IV) for the following outcomes:
-
all‐cause mortality during initial hospital stay (Analysis 8.2);
-
failure of PDA closure after two courses of treatment (Analysis 8.3);
-
surgical closure of PDA (Analysis 8.4);
-
IVH (Grade I‐IV) (Analysis 8.5);
-
severe IVH (Grade III‐IV) (Analysis 8.6);
-
NEC (Analysis 8.7);
-
gastrointestinal bleed (Analysis 8.8).
Comparison 3. Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention
See summary of findings Table 3.
Primary outcomes
Failure of PDA closure after first course of prophylaxis
Three studies reported this outcome in 240 infants (Asbagh 2015; Bagheri 2018; Härkin 2016). Paracetamol likely reduced the rate of failure of PDA closure after one course of prophylaxis compared to placebo or no intervention (RR 0.27, 95% CI 0.18 to 0.42; I² = 43%. RD −0.45, 95% CI −0.55 to −0.34; I² = 78%; NNTB 3, 95% CI 1.8 to 3; low‐certainty evidence; Analysis 3.1).
Neurodevelopmental impairment at 18 to 24 months (corrected age)
Juujärvi 2019 and Juujärvi 2021 reported two‐ (n = 44) and five‐year (n = 39) follow‐up of the prophylactic paracetamol trial conducted by Härkin 2016. They concluded that exposure to prophylactic paracetamol in very preterm infants was probably not associated with increased neurodevelopmental impairment or other adverse consequences compared to placebo both at two‐ and five‐year follow‐up visits (cerebral palsy, Analysis 3.11; autism spectrum disorder, Analysis 3.12; ADHD, Analysis 3.13; and pervasive developmental disorder, Analysis 3.14 at five‐year follow‐up).
Death or disability at 18 to 24 months
No studies reported on this combined outcome.
Secondary outcomes
All‐cause mortality during initial hospital stay
Three studies reported this outcome in 240 infants (Asbagh 2015; Bagheri 2018; Härkin 2016). There was little to no difference between the paracetamol group and the placebo or no intervention group (RR 0.59, 95% CI 0.24 to 1.44; I² = 0%. RD −0.04, 95% CI −0.11 to 0.03; I² = 0%; low‐certainty evidence; Analysis 3.2).
Other secondary outcomes
For the following outcomes, one study reported on 48 infants (Härkin 2016). As only one study was included in the different analyses, tests for heterogeneity were not applicable. There was probably little to no difference between the paracetamol and placebo groups for the following outcomes:
-
Duration of need for supplementary oxygen (Analysis 3.3);
-
BPD at 36 weeks' postmenstrual age (Analysis 3.4);
-
IVH grades (Grade I‐IV) (Analysis 3.5);
-
Severe IVH (Grade III‐IV) (Analysis 3.6);
-
Intestinal perforation (Analysis 3.7);
-
ROP requiring treatment (Analysis 3.8);
-
Oliguria (Analysis 3.9);
-
Sepsis (Analysis 3.10).
The following outcomes were not reported: neonatal mortality, re‐opening of the ductus arteriosus, failure of PDA closure after second course, failure of PDA closure after two courses, surgical closure of the PDA, treatment with indomethacin, ibuprofen or another prostaglandin inhibitor to close the PDA, duration of ventilator support, pulmonary hemorrhage, pulmonary hypertension, BPD defined as per new criteria, PVL, NEC, intestinal perforation, gastrointestinal bleed, acute kidney injury, post‐pre treatment difference in creatinine, post‐pre treatment difference in AST (U/L), post‐pre treatment difference in ALT (U/L), number of infants with AST or ALT greater than 100 U/L, hyperbilirubinemia, liver failure, duration of hospitalization, ASD, language delay, and other side effects.
Comparison 4. Early paracetamol (oral or IV) versus placebo (oral or IV) or no intervention
See summary of findings Table 4.
Primary outcomes
Failure of PDA closure after first course of treatment
Two studies reported this outcome in 127 infants (Babaei 2018; Schindler 2021). There was likely a reduction in the early paracetamol group compared to the placebo or no intervention group in the failure of PDA closure after one course of treatment, favouring the paracetamol group (RR 0.35, 95% CI 0.23 to 0.53; I2 = 0%. RD −0.51, 95% CI −0.66 to ‐0.37; I2= 33%; low‐certainty evidence; Analysis 4.1).
Neurodevelopmental impairment at 18 to 24 months (corrected age)
Neither study reported this outcome.
Death or disability at 18 to 24 months
Neither study reported this outcome.
Secondary outcomes
All‐cause mortality during initial hospital stay
Neither study reported this outcome.
Failure of PDA closure after two courses of treatment
One study reported this outcome in 69 infants (Babaei 2018). There was likely a reduction in the early paracetamol group compared to the placebo or no intervention group for failure of PDA closure after two courses of treatment, favouring the paracetamol group (RR 0.07, 95% CI 0.02 to 0.25; RD −0.79, 95% CI −0.94 to ‐0.65; Analysis 4.2). Tests for heterogeneity were not applicable.
NEC
Neither study reported this outcome.
The following outcomes were not reported: neonatal mortality, re‐opening of the ductus arteriosus, failure of PDA closure after second course, surgical closure of the PDA, treatment with indomethacin, ibuprofen or another prostaglandin inhibitor to close the PDA, duration of ventilator support, duration of supplementary oxygen, pulmonary hemorrhage, pulmonary hypertension, BPD at 36 weeks' postmenstrual age, BPD defined as per new criteria, IVH grade (I to IV), severe IVH (grade III to IV), PVL, intestinal perforation, gastrointestinal bleed, ROP stage 3 or greater, decreased urine output, acute kidney injury, sepsis, post‐pre treatment difference in creatinine, post‐pre treatment difference in AST (U/L), post‐pre treatment difference in ALT (U/L), number of infants with AST or ALT greater than 100 U/L, serum bilirubin, hyperbilirubinemia, liver failure, duration of hospitalization, ASD, language delay and other side effects.
Comparison 5. Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention
See summary of findings Table 5. Kluckow 2019 was the only included study that examined this comparison, in 55 infants. As only one study was included in the different analyses, tests for heterogeneity were not applicable.
Primary outcomes
Failure of PDA closure after first course of treatment
One study reported this outcome in 55 infants (Kluckow 2019). There was little to no difference between the late paracetamol and placebo groups for failure of PDA closure after one course of treatment (RR 0.85, 95% CI 0.72 to 1.01; RD −0.15, 95% CI −0.29 to ‐0.00; low‐certainty evidence; Analysis 5.1).
Neurodevelopmental impairment at 18 to 24 months (corrected age)
Kluckow 2019 did not report this outcome.
Death or disability at 18 to 24 months
Kluckow 2019 did not report this outcome.
Secondary outcomes
All‐cause mortality during initial hospital stay
Kluckow 2019 did not report this outcome.
NEC
One study reported this outcome in 55 infants (Kluckow 2019). There was little to no difference between the late paracetamol and placebo groups for NEC (RR 1.04, 95% CI 0.07 to 15.76; RD 0.00, 95% CI −0.10 to 0.10; low‐certainty evidence; Analysis 5.5).
Other secondary outcomes
For the following outcomes, Kluckow 2019 reported on 55 infants. There was probably little to no difference between the late paracetamol and placebo groups for the following outcomes:
-
Surgical closure of PDA (Analysis 5.2);
-
Pulmonary hemorrhage (Analysis 5.3);
-
BPD at 36 weeks' postmenstrual age (Analysis 5.4);
-
ROP requiring treatment (Analysis 5.6);
-
Acute kidney injury (Analysis 5.7).
Failure of PDA closure/non‐significant PDA after treatment
There was probably a reduction in failure of PDA closure/non‐significant PDA after treatment, favouring the late paracetamol group compared to the placebo group (RR 0.49, 95% CI 0.29 to 0.84; RD −0.38, 95% CI −0.62 to ‐0.14; Analysis 5.8).
The following outcomes were not reported: neonatal mortality, re‐opening of the ductus arteriosus, failure of PDA closure after second course, treatment with indomethacin, ibuprofen or another prostaglandin inhibitor to close the PDA, duration of ventilator support, duration of supplementary oxygen, pulmonary hypertension, BPD defined as per new criteria, IVH grade (I to IV), severe IVH (grade III to IV), PVL, intestinal perforation, gastrointestinal bleed, decreased urine output, sepsis, post‐pre treatment difference in creatinine, post‐pre treatment difference in AST (U/L), post‐pre treatment difference in ALT (U/L), number of infants with AST or ALT greater than 100 U/L, serum bilirubin, hyperbilirubinemia, liver failure, duration of hospitalization, ASD, language delay and other side effects.
Comparison 6. Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention
See summary of findings Table 6.
Primary outcomes
Failure of PDA closure after first course of treatment
Two studies reported this outcome in 111 infants (Hochwald 2018; Oboodi 2020). There was little to no difference between the ibuprofen plus paracetamol group and the ibuprofen plus placebo or no intervention group for failure of PDA closure after one course of treatment (RR 0.77, 95% CI 0.43 to 1.36; I² = 0%. RD −0.09, 95% CI −0.27 to 0.09; I2= 7%; low‐certainty evidence; Analysis 6.1).
Neurodevelopmental impairment at 18 to 24 months (corrected age)
Neither study reported this outcome.
Death or disability at 18 to 24 months
Neither study reported this outcome.
Secondary outcomes
All‐cause mortality during initial hospital stay
Neither study reported this outcome.
Failure of PDA closure after two courses of treatment
Two studies reported this outcome in 111 infants (Hochwald 2018; Oboodi 2020). There was likely a reduction for failure of PDA closure after two courses of treatment favouring the ibuprofen plus paracetamol group compared to the ibuprofen plus placebo or no intervention group (RR 0.28, 95% CI 0.08 to 0.99; I2 = 0%. RD −0.18, 95% CI −0.31 to ‐0.06; I2= 81%; Analysis 6.2).
NEC
One study reported this outcome in 24 infants (Hochwald 2018). There was little to no difference between the ibuprofen plus paracetamol group compared to the ibuprofen plus placebo group for risk of NEC (RR 0.33, 95% CI 0.01 to 7.45; RD −0.08, 95% CI −0.29 to 0.12; low‐certainty evidence; Analysis 6.7).
Other secondary outcomes
For the following outcomes, one study reported on 24 infants (Hochwald 2018). As only one study was included in the different analyses, tests for heterogeneity were not applicable. There was probably little to no difference between the ibuprofen plus paracetamol group versus the ibuprofen plus placebo group for the following outcomes:
-
BPD at 36 weeks (Analysis 6.3);
-
IVH (Grade I‐IV) (Analysis 6.4);
-
Severe IVH (Grade III‐IV) (Analysis 6.5);
-
PVL (Analysis 6.6);
-
Oliguria (Analysis 6.8).
The following outcomes were not reported: neonatal mortality, re‐opening of the ductus arteriosus, failure of PDA closure after second course, surgical closure of the PDA, treatment with indomethacin, ibuprofen or another prostaglandin inhibitor to close the PDA, duration of ventilator support, duration of supplementary oxygen, pulmonary hemorrhage, pulmonary hypertension, BPD defined as per new criteria, intestinal perforation, gastrointestinal bleed, ROP stage 3 or above, acute kidney injury, sepsis, post‐pre treatment difference in creatinine, post‐pre treatment difference in AST (U/L), post‐pre treatment difference in ALT (U/L), number of infants with AST or ALT greater than 100 U/L, serum bilirubin, hyperbilirubinemia, liver failure, duration of hospitalization, ASD, language delay and other side effects.
Discussion
Summary of main results
Evidence from 27 studies in 2278 preterm infants contributing data to the primary outcomes of this review showed that there is probably little or no difference in effectiveness between paracetamol and non‐selective COX inhibitors for PDA treatment. From the safety standpoint, paracetamol has a favourable adverse effect profile compared to non‐selective COX inhibitors. The certainty of the evidence was moderate for the primary outcome. The comparisons included paracetamol to ibuprofen (eighteen studies) (Al‐Lawama 2017; Asadpour 2018; Bagheri 2016; Balachander 2020; Dang 2013; Dani 2021; El‐Farrash 2019; El Mashad 2017; Ghaderian 2019a; Ghaderian 2019b; Jafari 2019; Kumar 2020; Meena 2020; Oboodi 2020; Oncel 2014; Shahmirzadi 2021; Tauber 2020; Yang 2016); prophylactic paracetamol to placebo or no intervention (three studies) (Asbagh 2015; Bagheri 2018; Härkin 2016); paracetamol to indomethacin (four studies) (Dash 2015; Davidson 2021; El Mashad 2017; Meena 2020); early paracetamol to placebo or no intervention (two studies) (Babaei 2018; Schindler 2021); late paracetamol to placebo (one study) (Kluckow 2019); and the combination of paracetamol and ibuprofen to ibuprofen plus placebo or no intervention (two studies) (Hochwald 2018; Oboodi 2020). There were two three‐arm studies, comparing paracetamol to ibuprofen as well as indomethacin (El Mashad 2017; Meena 2020). The Oboodi 2020 study compared paracetamol to ibuprofen and to paracetamol plus ibuprofen in a three‐arm study.
In the current version of the review, we added new outcomes, including failure of PDA closure after second course and after a total of two courses of paracetamol treatment; these were not planned a priori in the first version of the protocol (Ohlsson 2012). We deemed these outcomes important as clinicians often use multiple courses of pharmacotherapy (two to three) and, if unsuccessful, proceed to definitive approaches for PDA closure (ligation/transcatheter). Thus, it is important to know the efficacy after the second course and after a total of two courses to guide ongoing management.
There is probably little or no difference in effectiveness between paracetamol and ibuprofen or indomethacin in closing a PDA after the first course (closure and failure of closure confirmed by echocardiographic criteria). Adverse effects and morbidities were less common in the paracetamol groups compared with the ibuprofen or the indomethacin groups. Gastrointestinal bleed or stools positive for occult blood may be less likely to occur in the paracetamol versus the ibuprofen group. Necrotizing enterocolitis was probably less likely to occur in infants given paracetamol compared to those given indomethacin. Post‐pre difference in serum or plasma creatinine were probably lower in the paracetamol versus the ibuprofen and versus the indomethacin groups. Urine output was probably higher in infants given paracetamol versus those given ibuprofen and versus indomethacin. The serum bilirubin levels were probably higher in the paracetamol group compared to the ibuprofen and the indomethacin groups after treatment.
In the current version of the review, we added three comparisons which were not planned a priori in the first version of the protocol (Ohlsson 2012): early paracetamol, late paracetamol and combination (ibuprofen plus paracetamol) approaches for PDA treatment in preterm infants. Combination treatment (ibuprofen plus paracetamol) targeting two separate enzyme sites has recently been evaluated as a management strategy for treatment of PDA in preterm infants with varying results. Low‐certainty evidence suggest that early paracetamol treatment may be more efficacious than placebo/no intervention in closing a PDA after the first course. Late paracetamol treatment was probably similar to placebo in closing a PDA after the first course. It may have benefit in constriction of a PDA not needing additional treatment compared to placebo; however, the certainty of the evidence is low. There is probably little or no difference in effectiveness between combination treatment (ibuprofen plus paracetamol) and ibuprofen plus placebo/no intervention in closing a PDA after the first course. Combination treatment (ibuprofen plus paracetamol) may be more effective than ibuprofen plus placebo/no intervention after two treatment courses; however, the certainty of evidence is low. It would be important to present the current evidence pertaining to combination treatment to the scientific community before incorporation as a routine practice across neonatal units.
Subgroup analysis in infants of less than 32 weeks' gestation revealed that there is probably little or no difference in effectiveness between paracetamol and ibuprofen and indomethacin for PDA closure after the first course of treatment. Adverse effects and morbidities were similar in the paracetamol group compared with the ibuprofen or the indomethacin groups.
Overall completeness and applicability of evidence
In this review, we have included data on 2278 infants enrolled in 27 trials that compared the efficacy and safety of paracetamol with ibuprofen, indomethacin, and placebo/no intervention for PDA closure in preterm infants. Larger trials are required in extremely preterm infants to confirm the current promising evidence on efficacy as well as safety. Viberg and colleagues reported that paracetamol administration during neonatal brain development affects cognitive function and alters its analgesic and anxiolytic response in adult male mice (Viberg 2014). The dose of paracetamol used in mice was similar to that used in the two studies included in this review. In view of the possible negative impact of paracetamol on the developing brain reported in mice (Viberg 2014), the long‐term effects of paracetamol used for PDA closure or prevention and treatment of pain need to be studied carefully. In addition, in an ecological study conducted in humans and using country‐level data for the period 1984 to 2005, postnatal use of paracetamol was associated with autism or ASD (Bauer 2013). In 2017, Bornehag 2017 reported in a study from Sweden of a possible association between maternal prenatal exposure to paracetamol and language delay in 30‐month‐old girls (parental report of use of fewer than 50 words).
There is an increasing body of evidence demonstrating that the high efficacy (about 68%) of treatment reported in clinical trials has not translated to effective treatment in clinical practice among extremely low gestational age neonates (ELGANs < 28 weeks' gestational age) with PDA. Initial observational studies (Roofthooft 2015), and more recently, RCTs have reported less than 25% treatment success when acetaminophen is administered to ELGANs (Dani 2021; Davidson 2021; Liebowitz 2019). There are several potential reasons for this poor translation. First, while ELGANs are the patients being treated for PDA in contemporary practice, they were underrepresented in clinical trials which almost exclusively enrolled moderately preterm neonates (79% of RCTs enrolled neonates with mean gestational age at birth > 30 weeks). Most importantly, the acetaminophen dose and administration frequency evaluated in clinical trials was selected based on extrapolation from studies of pediatric analgesia. True pharmacokinetic studies of proper dose and duration of paracetamol for PDA treatment are lacking.
There are at least 24 ongoing trials that would provide additional evidence regarding this topic. The researchers should be encouraged to include pharmacokinetic data to determine optimal dosing regimen, have ELGANs as a population of interest, and study various durations of treatment and mode of administration (El‐Khuffash 2014). Long‐term follow‐up should be planned to at least 18 to 24 months and preferably to school age.
Applicability of current evidence regarding similar effectiveness of paracetamol should be appropriately evaluated considering local context. Cost of oral paracetamol is very low compared to intravenous indomethacin or intravenous ibuprofen. Oral paracetamol has a favourable side effect profile and thus a unit may decide to use paracetamol as primary agent. However, we strongly recommend that neonates should be followed for neurodevelopmental assessment and further information should be gathered about paracetamol's impact.
Certainty of the evidence
Although healthcare providers and researchers were aware of group assignment in many studies, we considered the included trials to be of good quality because, in most studies, the random sequence was computer‐generated and allocation to study groups was by opaque, sequentially‐numbered, and sealed envelopes. The certainty of the evidence, using GRADE, was moderate for the primary outcome 'failure of PDA closure after the first course of treatment' in the comparison of paracetamol versus ibuprofen and moderate for other important outcomes — all‐cause mortality and NEC. We downgraded evidence by one level due to concerns about blinding of personnel and outcome assessment. For prophylactic paracetamol versus placebo or no intervention, the certainty of the evidence was low for 'failure of PDA closure after the first course of treatment' and all‐cause mortality. We downgraded evidence due to concerns about selection bias, blinding of personnel, and high heterogeneity. For the paracetamol versus indomethacin comparison, we assessed the certainty of the evidence for the outcomes 'failure of PDA closure after the first course of treatment', all‐cause mortality, and NEC as low due to concerns about blinding of personnel, outcome assessment, and imprecision. For early, late, and combination treatment, the overall certainty of the evidence was low for the three key outcomes. For early and combination treatment, the reasons for downgrading the evidence were concerns about selection bias, blinding of personnel, outcome assessment, imprecision, and high heterogeneity. For late treatment, we downgraded the evidence due to concerns about indirectness and imprecision. Overall, in order to improve the certainty of the evidence, future trials need to include the features indicated above and in the Implications for research section.
Potential biases in the review process
We deviated from the original protocol (e.g. decisions to amend the types of subgroup analyses) to minimize multiple subgroups to be able to draw meaningful, clinically relevant conclusions. Departures from the protocol were primarily related to clarification of inclusion criteria and relevant outcomes. None of the review authors are involved in any of the trials included in the review.
Agreements and disagreements with other studies or reviews
We are aware of three recent systematic reviews with meta‐analyses on the topic (Marconi 2019; Pranata 2020; Xiao 2020). In the previous version of this review (Ohlsson 2020c), we included eight trials (Al‐Lawama 2017; Asbagh 2015; Dang 2013; Dash 2015; El Mashad 2017; Härkin 2016; Oncel 2014; Yang 2016).
Pranata 2020 included eight trials (N = 1290) comparing oral paracetamol and oral ibuprofen for PDA treatment in preterm infants (Al‐Lawama 2017; Bagheri 2016; Balachander 2020; Dang 2013; El‐Farrash 2019; Ghaderian 2019a; Oncel 2014; Yang 2016). They concluded that there "was no significant difference between the efficacy of oral paracetamol and oral ibuprofen. However, the rate of renal dysfunction and gastrointestinal bleeding were higher in oral ibuprofen.”
Marconi 2019 conducted a systematic review and network meta‐analysis of 64 RCTs and 24 observational studies, including 14,568 participants, evaluating all pharmacological agents used for PDA treatment. They concluded that “active pharmacological treatment, with indomethacin, ibuprofen, or paracetamol, is inversely associated with failure to close the PDA compared to non‐treatment. Ibuprofen should be preferred to indomethacin to avoid occurrence of IVH or oliguria, paracetamol should be preferred to indomethacin to avoid oliguria.”
Xiao 2020 conducted a meta‐analysis including 15 trials (N = 1313). They concluded that “paracetamol can induce early patent ductus arteriosus closure without significant side effects”.
This updated review contains the most comprehensive analyses of existing studies, considers all methods of administering paracetamol for PDA treatment, and includes all comparators tested in randomized trials.
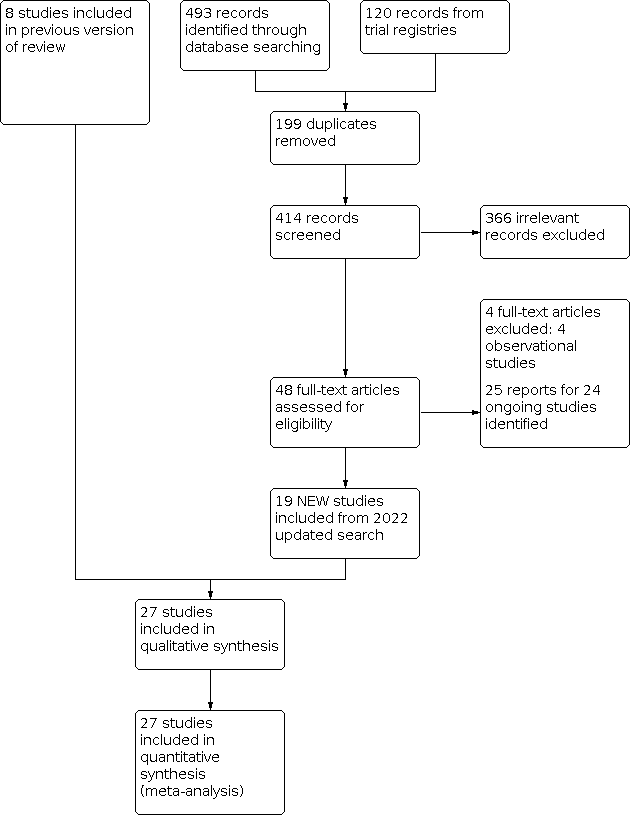
Study flow diagram for 2022 review update

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Funnel plot: failure of PDA closure after first course of treatment for comparison 'Paracetamol (oral or IV) versus ibuprofen (oral or IV)'

Funnel plot: failure of PDA closure after second course of treatment for comparison 'Paracetamol (oral or IV) versus ibuprofen (oral or IV)'

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 1: Failure of PDA closure after first course of treatment

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 2: Neurodevelopmental impairment

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 3: All‐cause mortality during initial hospital stay

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 4: Neonatal mortality (deaths during the first 28 days of life)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 5: Re‐opening of the ductus arteriosus

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 6: Failure of PDA closure after second course of treatment

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 7: Surgical closure of the PDA

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 8: Duration of ventilator support (days)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 9: Duration of need for supplementary oxygen (days)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 10: Pulmonary hemorrhage

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 11: Pulmonary hypertension

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 12: Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 13: Moderate to severe BPD (according to the new criteria)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 14: Severe BPD (according to the new criteria)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 15: Intraventricular hemorrhage (IVH, Grade I‐IV)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 16: Severe IVH (Grade III‐IV)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 17: Periventricular leukomalacia

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 18: Necrotizing enterocolitis (NEC)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 19: Intestinal perforation

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 20: Gastrointestinal bleed

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 21: Retinopathy of prematurity stage ≥ 3

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 22: Retinopathy of prematurity requiring treatment

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 23: Oliguria (< 1 mL/kg/h)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 24: Sepsis

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 25: Post‐pre difference in serum or plasma levels of creatinine (mg/dL)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 26: Serum levels of aspartate transaminase (AST) IU/L

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 27: Post‐pre difference in serum levels of alanine aminotransferase (ALT) (IU/L)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 28: Serum bilirubin following treatment (µmol/L)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 29: Hyperbilirubinemia (serum bilirubin level higher than the exchange level according to the postnatal age and BW)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 30: Duration of hospitalization (days)

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 31: Mental developmental index (MDI) < 70

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 32: Psychomotor developmental index (PDI) < 70

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 33: Moderate to severe cerebral palsy

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 34: Deafness

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 35: Blindness

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 36: Mental developmental index

Comparison 1: Paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 37: Psychomotor developmental index

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 1: Failure of PDA closure after first course of treatment

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 2: All‐cause mortality during initial hospital stay

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 3: Failure of PDA closure after second course of treatment

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 4: Surgical closure of the PDA

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 5: Pulmonary hemorrhage

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 6: Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 7: Intraventricular hemorrhage (IVH, Grade I‐IV)

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 8: IVH (Grade III‐IV)

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 9: Periventricular leukomalacia

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 10: Necrotizing enterocolitis (NEC)

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 11: Gastrointestinal bleed

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 12: Retinopathy of prematurity requiring treatment

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 13: Acute kidney injury

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 14: Sepsis

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 15: Post‐pre difference in serum creatinine (mg/dL)

Comparison 2: Paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 16: Serum bilirubin following treatment (µmol/L)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 1: Failure of PDA closure after first course of prophylaxis

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 2: All‐cause mortality during initial hospital stay

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 3: Duration of need for supplementary oxygen (days)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 4: Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 5: Intraventricular hemorrhage (IVH, Grade I‐IV)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 6: Severe IVH (Grade III‐IV)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 7: Intestinal perforation

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 8: Retinopathy of prematurity requiring treatment

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 9: Oliguria (< 1 mL/kg/h)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 10: Sepsis

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 11: Cerebral palsy (5 years' follow‐up)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 12: Autism spectrum disorder (5 years' follow‐up)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 13: Attention deficit hyperactivity disorder (5 years' follow‐up)

Comparison 3: Prophylactic paracetamol (oral or IV) versus placebo (IV) or no intervention, Outcome 14: Pervasive developmental disorder (5 years' follow‐up)

Comparison 4: Early paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 1: Failure of PDA closure after first course of treatment

Comparison 4: Early paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 2: Failure of PDA closure after two courses of treatment

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 1: Failure of PDA closure after one course of treatment

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 2: Surgical closure of PDA

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 3: Pulmonary hemorrhage

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 4: Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 5: Necrotizing enterocolitis (NEC)

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 6: Retinopathy of prematurity requiring treatment

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 7: Acute kidney injury

Comparison 5: Late paracetamol (oral or IV) versus placebo (oral or IV) or no intervention, Outcome 8: Failure of PDA closure/non‐significant PDA after treatment

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 1: Failure of PDA closure after first course of treatment

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 2: Failure of PDA closure after two courses of treatment

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 3: Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 4: Intraventricular hemorrhage (IVH, Grade I‐IV)

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 5: Severe IVH (Grade III‐IV)

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 6: Periventricular leukomalacia

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 7: Necrotizing enterocolitis (NEC)

Comparison 6: Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention, Outcome 8: Oliguria (< 1 mL/kg/h)

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 1: Failure of PDA closure after first course of treatment

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 2: All‐cause mortality during initial hospital stay

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 3: Failure of PDA closure after two courses of treatment

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 4: Surgical closure of PDA

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 5: Intraventricular hemorrhage (IVH, Grade I‐IV)

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 6: Severe IVH (Grade III‐IV)

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 7: Necrotizing enterocolitis (NEC)

Comparison 7: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus ibuprofen (oral or IV), Outcome 8: Gastrointestinal bleed

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 1: Failure of PDA closure after first course of treatment

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 2: All‐cause mortality during initial hospital stay

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 3: Failure of PDA closure after two courses of treatment

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 4: Surgical closure of PDA

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 5: Intraventricular hemorrhage (IVH, Grade I‐IV)

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 6: Severe IVH (Grade III‐IV)

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 7: Necrotizing enterocolitis (NEC)

Comparison 8: Subgroup analysis (< 32 weeks' GA): paracetamol (oral or IV) versus indomethacin (oral or IV), Outcome 8: Gastrointestinal bleed
| Paracetamol (oral or IV) versus ibuprofen (oral or IV) for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Oral/IV ibuprofen | Oral/IV paracetamol | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | High‐risk study population | RR 1.02 | 1535 | ⊕⊕⊕⊝ |
| |
| 299 per 1000 | 308 per 1000 | |||||
| All‐cause mortality during initial hospital stay | High‐risk study population | RR 1.09 | 734 | ⊕⊕⊕⊝ |
| |
| 166 per 1000 | 181 per 1000 | |||||
| Necrotizing enterocolitisduring initial hospital stay (by radiological diagnosis) | 70 per 1000 | 91 per 1000 (61 to 136) | RR 1.30 | 1015 | ⊕⊕⊕⊝ |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aFor all three key critical outcomes, we downgraded the evidence by one level to moderate certainty, due to concerns regarding blinding of personnel and outcome assessment. | ||||||
| Paracetamol (oral or IV) versus indomethacin (IV) for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm infants with PDA Settings: neonatal intensive care unit in India, Egypt, and the USA Intervention: paracetamol Comparison: indomethacin | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Indomethacin | Paracetamol | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | High‐risk study population | RR 1.02 (0.78 to 1.33) | 380 | ⊕⊕⊝⊝ Lowa
|
| |
| 297 per 1000 | 303 per 1000 | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | 186 per 1000 | 160 per 1000 (73 to 358) | RR 0.86 (0.39 to 1.92) | 114 (2 studies) | ⊕⊕⊝⊝ Lowb |
|
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis) | 93 per 1000 | 39 per 1000 (18 to 89) | RR 0.42 (0.19 to 0.96) | 384 (4 studies) | ⊕⊕⊝⊝ |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded evidence by two levels to low certainty due to concerns regarding blinding of personnel and outcome assessment, and high heterogeneity. | ||||||
| Prophylactic administration of paracetamol (oral or IV) versus placebo (IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm infants with PDA Settings: neonatal intensive care units in Finland and Iran Intervention: paracetamol Comparison: placebo or no intervention | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Placebo or no intervention | Paracetamol | |||||
| Failure of PDA closure after first course (assessed by post‐treatment ECHO) | High‐risk study population | RR 0.27 (0.18 to 0.42) | 240 | ⊕⊕⊝⊝
|
| |
| 612 per 1000 | 165 per 1000 | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | High‐risk study population | RR 0.59 (0.24 to 1.44) | 240 | ⊕⊕⊝⊝
|
| |
| 91 per 1000 | 54 per 1000 | |||||
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis)
| High‐risk study population | Not reported | Not reported | Not reported | Not reported | |
| Data not available | Data not available | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence by two levels to low certainty due to concerns regarding selection bias, blinding of personnel, and high heterogeneity. | ||||||
| Early paracetamol (oral or IV, < 14 days postnatal age) versus placebo (oral or IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Placebo/no intervention | Oral/IV paracetamol | |||||
| Failure of PDA closure after first course of treatment (by post‐treatment ECHO) | High‐risk study population | RR 0.35 (0.23 TO 0.53) | 127 (2 studies) | ⊕⊕⊝⊝
|
| |
| 790 per 1000 | 277 per 1000 (182 to 419) | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence by two levels to low certainty due to concerns regarding selection bias, blinding of personnel and outcome assessors, and high heterogeneity. | ||||||
| Late paracetamol (oral or IV, ≥ 14 days postnatal age) versus placebo (oral or IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Placebo/no intervention | Oral/IV paracetamol | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | High‐risk study population | RR 0.85 (0.72 to 1.01) | 55 (1 study) | ⊕⊕⊝⊝ |
| |
| 1000 per 1000 | 850 per 1000 (720 to 1000) | |||||
| All‐cause mortality during initial hospital stay (by clinical assessment) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Necrotizing enterocolitis during initial hospital stay (by radiological diagnosis) | 36 per 1000 | 37 per 1000 (3 to 563) | RR 1.04 (0.07 to 15.76) | 55 (1 study) | ⊕⊕⊝⊝ |
|
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence for both failure of PDA closure after first course of treatment and NEC by two levels to low certainty due to concerns regarding indirectness and imprecision. | ||||||
| Paracetamol plus ibuprofen (oral or IV) versus ibuprofen plus placebo (oral or IV) or no intervention for PDA in preterm or low birth weight infants | ||||||
| Patient or population: preterm or low birth weight infants with PDA | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Ibuprofen plus placebo | Paracetamol plus ibuprofen | |||||
| Failure of PDA closure after first course of treatment (assessed by post‐treatment ECHO) | 313 per 1000 | 241 per 1000 (134 to 425) | RR 0.77 (0.43 to 1.36) | 111 (2 studies) | ⊕⊕⊝⊝ | |
| All‐cause mortality during initial hospital stay (by clinical assessment) | Not reported | Not reported | Not reported | Not reported | Not reported | Not reported |
| Necrotizing enterocolitis during initial hospital stay (radiological diagnosis) | 83 per 1000 | 28 per 1000 (1 to 621) | RR 0.33 (0.01 to 7.45)
| 24 (1 study) | ⊕⊕⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| aWe downgraded the evidence for both failure of PDA closure after first course of treatment and NEC by two levels to low certainty due to concerns regarding selection bias, blinding of personnel, outcome assessment, and imprecision. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Failure of PDA closure after first course of treatment Show forest plot | 18 | 1535 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.88, 1.18] |
| 1.2 Neurodevelopmental impairment Show forest plot | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.44, 1.96] |
| 1.3 All‐cause mortality during initial hospital stay Show forest plot | 8 | 734 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.80, 1.48] |
| 1.4 Neonatal mortality (deaths during the first 28 days of life) Show forest plot | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.43, 3.20] |
| 1.5 Re‐opening of the ductus arteriosus Show forest plot | 5 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [0.85, 2.12] |
| 1.6 Failure of PDA closure after second course of treatment Show forest plot | 13 | 393 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.78, 1.21] |
| 1.7 Surgical closure of the PDA Show forest plot | 6 | 603 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.34, 1.08] |
| 1.8 Duration of ventilator support (days) Show forest plot | 3 | 260 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐1.19, 0.08] |
| 1.9 Duration of need for supplementary oxygen (days) Show forest plot | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐12.40 [‐22.97, ‐1.83] |
| 1.10 Pulmonary hemorrhage Show forest plot | 5 | 442 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.36, 2.09] |
| 1.11 Pulmonary hypertension Show forest plot | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.97] |
| 1.12 Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA Show forest plot | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.45, 1.38] |
| 1.13 Moderate to severe BPD (according to the new criteria) Show forest plot | 1 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.22, 2.87] |
| 1.14 Severe BPD (according to the new criteria) Show forest plot | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.32, 1.23] |
| 1.15 Intraventricular hemorrhage (IVH, Grade I‐IV) Show forest plot | 8 | 800 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.77, 1.22] |
| 1.16 Severe IVH (Grade III‐IV) Show forest plot | 6 | 544 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.28, 1.43] |
| 1.17 Periventricular leukomalacia Show forest plot | 4 | 421 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.56, 3.50] |
| 1.18 Necrotizing enterocolitis (NEC) Show forest plot | 10 | 1015 | Risk Difference (M‐H, Fixed, 95% CI) | 0.02 [‐0.01, 0.05] |
| 1.19 Intestinal perforation Show forest plot | 2 | 191 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.83 [0.12, 67.87] |
| 1.20 Gastrointestinal bleed Show forest plot | 7 | 693 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.05 [‐0.09, ‐0.02] |
| 1.21 Retinopathy of prematurity stage ≥ 3 Show forest plot | 2 | 191 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.12, 1.55] |
| 1.22 Retinopathy of prematurity requiring treatment Show forest plot | 3 | 353 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.48, 1.85] |
| 1.23 Oliguria (< 1 mL/kg/h) Show forest plot | 5 | 608 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.30, 0.76] |
| 1.24 Sepsis Show forest plot | 7 | 844 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.72, 1.22] |
| 1.25 Post‐pre difference in serum or plasma levels of creatinine (mg/dL) Show forest plot | 6 | 557 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.13, ‐0.10] |
| 1.26 Serum levels of aspartate transaminase (AST) IU/L Show forest plot | 4 | 270 | Mean Difference (IV, Fixed, 95% CI) | 1.08 [‐0.16, 2.32] |
| 1.27 Post‐pre difference in serum levels of alanine aminotransferase (ALT) (IU/L) Show forest plot | 6 | 557 | Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.00, 1.05] |
| 1.28 Serum bilirubin following treatment (µmol/L) Show forest plot | 4 | 400 | Mean Difference (IV, Fixed, 95% CI) | ‐10.56 [‐13.16, ‐7.96] |
| 1.29 Hyperbilirubinemia (serum bilirubin level higher than the exchange level according to the postnatal age and BW) Show forest plot | 1 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.34, 0.97] |
| 1.30 Duration of hospitalization (days) Show forest plot | 4 | 361 | Mean Difference (IV, Fixed, 95% CI) | 2.79 [0.34, 5.24] |
| 1.31 Mental developmental index (MDI) < 70 Show forest plot | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.41, 2.59] |
| 1.32 Psychomotor developmental index (PDI) < 70 Show forest plot | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.33, 3.21] |
| 1.33 Moderate to severe cerebral palsy Show forest plot | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.07 [0.41, 10.46] |
| 1.34 Deafness Show forest plot | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.13] |
| 1.35 Blindness Show forest plot | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.13] |
| 1.36 Mental developmental index Show forest plot | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐8.19, 7.39] |
| 1.37 Psychomotor developmental index Show forest plot | 1 | 61 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐7.44, 7.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Failure of PDA closure after first course of treatment Show forest plot | 4 | 380 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.78, 1.33] |
| 2.2 All‐cause mortality during initial hospital stay Show forest plot | 2 | 114 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.39, 1.92] |
| 2.3 Failure of PDA closure after second course of treatment Show forest plot | 2 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.70, 1.50] |
| 2.4 Surgical closure of the PDA Show forest plot | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.72, 2.38] |
| 2.5 Pulmonary hemorrhage Show forest plot | 3 | 347 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.28, 2.10] |
| 2.6 Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA Show forest plot | 2 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.77, 1.75] |
| 2.7 Intraventricular hemorrhage (IVH, Grade I‐IV) Show forest plot | 2 | 275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.42, 1.63] |
| 2.8 IVH (Grade III‐IV) Show forest plot | 2 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.28, 4.31] |
| 2.9 Periventricular leukomalacia Show forest plot | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.14] |
| 2.10 Necrotizing enterocolitis (NEC) Show forest plot | 4 | 384 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.19, 0.96] |
| 2.11 Gastrointestinal bleed Show forest plot | 3 | 347 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.32, 1.25] |
| 2.12 Retinopathy of prematurity requiring treatment Show forest plot | 2 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.58, 2.99] |
| 2.13 Acute kidney injury Show forest plot | 1 | 77 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.08 [0.13, 73.26] |
| 2.14 Sepsis Show forest plot | 3 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.59, 1.82] |
| 2.15 Post‐pre difference in serum creatinine (mg/dL) Show forest plot | 2 | 270 | Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐0.40, ‐0.34] |
| 2.16 Serum bilirubin following treatment (µmol/L) Show forest plot | 1 | 200 | Mean Difference (IV, Fixed, 95% CI) | 1.03 [0.13, 1.93] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Failure of PDA closure after first course of prophylaxis Show forest plot | 3 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.18, 0.42] |
| 3.2 All‐cause mortality during initial hospital stay Show forest plot | 3 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.24, 1.44] |
| 3.3 Duration of need for supplementary oxygen (days) Show forest plot | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐2.40 [‐16.41, 11.61] |
| 3.4 Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA Show forest plot | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.02, 8.45] |
| 3.5 Intraventricular hemorrhage (IVH, Grade I‐IV) Show forest plot | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.28, 1.51] |
| 3.6 Severe IVH (Grade III‐IV) Show forest plot | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.07, 16.39] |
| 3.7 Intestinal perforation Show forest plot | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.02, 8.45] |
| 3.8 Retinopathy of prematurity requiring treatment Show forest plot | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.14, 76.01] |
| 3.9 Oliguria (< 1 mL/kg/h) Show forest plot | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.29, 2.11] |
| 3.10 Sepsis Show forest plot | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.36, 5.79] |
| 3.11 Cerebral palsy (5 years' follow‐up) Show forest plot | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.07, 15.66] |
| 3.12 Autism spectrum disorder (5 years' follow‐up) Show forest plot | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 3.13 Attention deficit hyperactivity disorder (5 years' follow‐up) Show forest plot | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.02, 8.10] |
| 3.14 Pervasive developmental disorder (5 years' follow‐up) Show forest plot | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.02, 8.10] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 4.1 Failure of PDA closure after first course of treatment Show forest plot | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.23, 0.53] |
| 4.2 Failure of PDA closure after two courses of treatment Show forest plot | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.02, 0.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 5.1 Failure of PDA closure after one course of treatment Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.72, 1.01] |
| 5.2 Surgical closure of PDA Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.11 [0.13, 73.11] |
| 5.3 Pulmonary hemorrhage Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.07 [0.20, 21.56] |
| 5.4 Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.61, 1.40] |
| 5.5 Necrotizing enterocolitis (NEC) Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.07, 15.76] |
| 5.6 Retinopathy of prematurity requiring treatment Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.11 [0.34, 28.09] |
| 5.7 Acute kidney injury Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.8 Failure of PDA closure/non‐significant PDA after treatment Show forest plot | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.29, 0.84] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 6.1 Failure of PDA closure after first course of treatment Show forest plot | 2 | 111 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.43, 1.36] |
| 6.2 Failure of PDA closure after two courses of treatment Show forest plot | 2 | 111 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.08, 0.99] |
| 6.3 Bronchopulmonary dysplasia (BPD) at 36 weeks' PMA Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.28, 2.27] |
| 6.4 Intraventricular hemorrhage (IVH, Grade I‐IV) Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.38, 4.72] |
| 6.5 Severe IVH (Grade III‐IV) Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.30, 7.43] |
| 6.6 Periventricular leukomalacia Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.45] |
| 6.7 Necrotizing enterocolitis (NEC) Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.45] |
| 6.8 Oliguria (< 1 mL/kg/h) Show forest plot | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.05, 4.81] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 7.1 Failure of PDA closure after first course of treatment Show forest plot | 6 | 584 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [1.00, 1.66] |
| 7.2 All‐cause mortality during initial hospital stay Show forest plot | 4 | 374 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.85, 1.91] |
| 7.3 Failure of PDA closure after two courses of treatment Show forest plot | 4 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.48, 1.01] |
| 7.4 Surgical closure of PDA Show forest plot | 5 | 543 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.36, 1.16] |
| 7.5 Intraventricular hemorrhage (IVH, Grade I‐IV) Show forest plot | 4 | 413 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.75, 1.19] |
| 7.6 Severe IVH (Grade III‐IV) Show forest plot | 4 | 354 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.14, 1.24] |
| 7.7 Necrotizing enterocolitis (NEC) Show forest plot | 5 | 552 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.71, 2.51] |
| 7.8 Gastrointestinal bleed Show forest plot | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 1.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 8.1 Failure of PDA closure after first course of treatment Show forest plot | 3 | 310 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.86, 1.87] |
| 8.2 All‐cause mortality during initial hospital stay Show forest plot | 2 | 114 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.39, 1.92] |
| 8.3 Failure of PDA closure after two courses of treatment Show forest plot | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.55, 1.40] |
| 8.4 Surgical closure of PDA Show forest plot | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.72, 2.38] |
| 8.5 Intraventricular hemorrhage (IVH, Grade I‐IV) Show forest plot | 2 | 275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.42, 1.63] |
| 8.6 Severe IVH (Grade III‐IV) Show forest plot | 2 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.28, 4.31] |
| 8.7 Necrotizing enterocolitis (NEC) Show forest plot | 3 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.20, 1.07] |
| 8.8 Gastrointestinal bleed Show forest plot | 2 | 277 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.33, 1.33] |

