透過職業復健來幫助手指、手、手臂受傷的病人重返職場
Abstract
Background
Traumatic upper limb injury is a leading cause of work‐related disability. After return‐to‐work (RTW), many survivors of injuries are able to regain a quality of life (QoL) comparable with the normal population. Since RTW plays an important role in economic productivity and regaining health‐related QoL, enhancing RTW in workers with traumatic limb injuries is the primary goal of rehabilitation. Vocational rehabilitation has been commonly employed in the field of occupational safety and health to increase the number of injured people returning to the labour market, prevent illness, increase well‐being, and reduce disability.
Objectives
To assess the effects of vocational rehabilitation programmes for enhancing RTW in workers with traumatic upper limb injuries.
Search methods
This is an update of a Cochrane review previously published in 2013. We updated our searches of the following databases: the Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 9), MEDLINE (to 30 August 2017), EMBASE (to 3 September 2017), CINAHL (to 6 September 2017), and PsycINFO (to 6 September 2017), and we handsearched the references lists of relevant review articles.
Selection criteria
We aimed to include all randomised controlled trials (RCTs) comparing vocational rehabilitation with an alternative (control) intervention such as standard rehabilitation, a limited form of the vocational rehabilitation intervention (such as advice on RTW, referral information, or liaison with employer), or waiting‐list controls.
Data collection and analysis
Two authors independently inspected abstracts, and we obtained full papers when necessary. When the two authors disagreed about the inclusion of a study, we resolved disagreements by discussion. A third author arbitrated when necessary.
Main results
Our updated search identified 466 citations. Based on assessments of their titles and abstracts, we decided to evaluate the full texts of five records; however, none met our inclusion criteria.
Authors' conclusions
There is currently no high‐quality evidence to support or refute the efficacy of vocational rehabilitation for enhancing RTW in workers with traumatic upper limb injuries. Since injured people in occupational settings frequently receive vocational rehabilitation with the aim of decreasing work disability, enhancing RTW, increasing productivity, and containing the welfare cost, further high‐quality RCTs assessing the efficacy of vocational rehabilitation for workers with traumatic upper limb injury are needed to fill this gap in knowledge.
淺顯易懂的口語結論
透過職業復健來幫助手指、手、手臂受傷的病人重返職場
本篇文獻回顧的目的為何?
我們想知道,手指、手掌或上臂受傷的病人,在受傷後透過職業復健是否有助於他們重返職場。
關鍵訊息
並沒有任何隨機分派對照的試驗能證明上肢受傷的病人在透過職業復健以後,是否能順利回到職場。這類的研究有其必要性,而且,為了能產出高品質的研究結果,研究者應該要以大家有共識的標準來執行和報告這些研究。這些研究的內容應描述該職業復健的細節,以及在結束追踪後成功回到職場的個案數,或他們花了多少時間才回到職場。
本篇文獻回顧的研究內容為何?
本回顧所收錄的個案是因為手指、手掌或手臂受傷而無法持續正常工作的工人。當工人受傷程度已經影響他的工作能力時,許多國家的法律都強制要求需雇主對受傷的工人提供協助。而這類的協助通常是指的就是所謂的職業復健。職業復健所指的是,幫助因為受傷而導致殘障的員工能回到原工作崗位或是找到新的工作。「重返職場」的支持方式可包括調整工作內容或物理治療運動來讓病人更能適應重返職場的情境。雖然這些方法已在實際的情境中運用,但我們仍不太確定在特定情境下適合哪一些方式。這篇回顧是先前在 2013 年發表的考科藍回顧的更新版本。
本篇文獻回顧的主要結果為何?
我們查閱了2017年8月30日以前發表的研究,並僅納入透過隨機分派而接受了職業復健或其他治療方式的病人。以這種方法來執行的研究通常稱為隨機分派對照試驗,這是最能確認病患的進步確實是源於所採取的治療方式。我們沒有找到任何一篇隨機分派對照試驗能說明職業復健是否有助於上肢受傷的工人返回職場。
這篇回顧的時效性如何?
我們蒐尋了直到 2017 年 8 月 30 日以前的文獻。
Authors' conclusions
Background
Description of the condition
The World Health Organization (WHO) defines injury as "a bodily lesion at the organic level, resulting from acute exposure to energy in the work environment (mechanical, thermal, electrical, chemical or radiant) in amounts that exceed the threshold of physiological tolerance. In some cases (e.g. drowning, strangulation, freezing), the injury results from an insufficiency of a vital element" (Baker 1984). Among the various injuries, traumatic upper limb injuries frequently occur in mechanised industry when people interact with machines, at home, during transportation, and in recreation and sports activities (King 1992). Due to the complex physical arrangement, traumatic upper limb injuries often involve varying degrees of damage to, or even loss of, tissue such as the skin, tendons, nerves, blood vessels, bones, or the whole upper limb. Because traumatic upper limb injuries affect multiple systems (including the musculoskeletal, vascular, and nervous systems), the resulting impairment is often devastating (Cooper 2007). The disability caused by traumatic upper limb injuries significantly reduces physical (e.g. immobility), psychological (e.g. depression), and socioenvironmental well‐being (e.g. work and leisure activities) and can cause very severe health problems among workers (Hou 2013a). However, the ability to work after sick leave is strongly associated with improved health, self‐esteem, financial reward, connections with others in the community, and health‐related quality of life (Post 2006a).Therefore, a comprehensive return‐to‐work (RTW) rehabilitation programme following traumatic upper limb injuries aims to enable resumption of participation in work and leisure activities (Blackmore 1992).
In the UK, upper limb injuries were the most frequent type (47.3%) of non‐fatal injury to employees from 2010 to 2011 (HSE 2012). In Australia, there were 16,712 cases (32%) of work‐related hand and wrist injuries resulting in hospitalisations from 1 July 2002 to 30 June 2004; in Victoria alone, 12,491 (32.7%) of emergency department presentations were work‐related hand and wrist injuries (ASCC 2008). In the US, 25.1% of nonfatal occupational injuries and illnesses causing work absences per 10,000 full‐time workers were related to upper limb injuries in 2010 (BLS 2010). In Taiwan, traumatic upper limb injuries are the most frequent type of occupational injury and the major cause of functional impairment and work‐related disability (accounting for 45% of 14,261 occupational injuries and 55.8% of occupational permanent disability benefits in 2010) (CLA 2011). Many traditional factories in Taiwan are of medium to small scale and usually demand skilled manual labour. Factories commonly have inadequate occupational safety training programmes, or their staff is insufficiently knowledgeable and incapable of seeking adequate vocational rehabilitation (VR) programmes, which results in high hand injury‐related disability (Hou 2008). In addition to the inability to perform essential functions required at work, such as lifting and grasping, some injured workers also have great difficulties in daily activities such as bathing, dressing, and toileting independently.
Undoubtedly traumatic upper limb injuries cause considerable losses in working days and productivity (Ebel 2004). However, survivors of severe injuries can achieve a quality of life (QoL) comparable with the normal population after returning to their previous jobs (Post 2006). On the other hand, the permanent dysfunction of limb‐injured workers not only limits their daily activities but also directly affects their outcomes in their RTW. For a worker with traumatic upper limb injuries, RTW plays an important role in economic productivity and regaining meaningfulness in life. Therefore, the goals of rehabilitation for patients with traumatic upper limb injuries should be functional independence and RTW.
Description of the intervention
A person's ability to work can be profoundly affected by their disease, disability, and a range of contextual factors. Rehabilitation medicine is integral to the process that enables people to go back to working life following illness or injury, but other rehabilitation disciplines are also essential. It is important to clarify what rehabilitation physicians or trainees in rehabilitation medicine need to know about vocational rehabilitation (VR).
VR is defined as a process that enables persons with functional, psychological, developmental, cognitive and emotional impairments or health disabilities to overcome barriers to accessing, maintaining or returning to employment or other occupation (VRA 2013). On the other hand, general rehabilitation focuses on facilitating the functional recovery from injury, illness, or disease to its original state as possible. Therefore, VR consists of a range of techniques involving the provision of health advice and promotion, supporting self‐management of health conditions, making adjustments to the impact of a disability, case management, service coordination, job analysis, job development, career counselling, and functional or work capacity evaluations, which could effectively help disabled workers return to work or to find a new employment (VRA 2016).
VR is a process whereby those disadvantaged by illness or disability can access, maintain, or return to employment. This applies to those with temporary and permanent impairments. Miscellaneous VR programmes are involved, in parallel, during the process of returning to the labour market after an injury. Therefore, VR may be used synonymously with either clinical rehabilitation services or any other types of interventions involved in the community settings such as work disability prevention, prevention of job loss, or work reintegration. Furthermore, the personnel delivering VR include a range of practitioners such as rehabilitation specialists, occupational therapists, occupational physicians, and social security officers (Waddell 2008). According to the British Society of Rehabilitation Medicine, VR aims to maximise the ability of an individual to return to meaningful employment, improve work and activity tolerance, avoid illness behavior, prevent deconditioning, and reduce pain and the effects of illness or disability (BSRM 2000). In this review, we define VR as changes or interventions with the aim of facilitating a worker's employment after injury. These may include one or more of the following: education, follow‐up by a case manager, occupational therapy, worksite visits, on‐site management, vocational guidance, occupational health services, work hardening, work modification, job accommodation, work adjustments, work reintegration plans, and ergonomic interventions. VR deals mainly with rehabilitation on the basis of the International Classification of Functioning, Disability and Health (ICF)‐level of 'participation' (WHO 2001).
Workers who have not returned to work within 3 months after injury are at high risk of disability and dropping out of the work arena completely (Frank 1996). Therefore, encouraging early RTW by intervening at the workplace may be an efficient way to minimise socioeconomic and personal consequences (Elders 2004).
How the intervention might work
VR targets promoting employment opportunities for the disabled. When a defect due to trauma affects functional capacity for work or employment, VR may be necessary (Gobelet 2006). There are various factors influencing RTW. The chance of RTW is higher among younger people and men and among those with higher education, white collar work, less injury severity, less disability, more self‐efficacy, and better psychological or QoL condition (Chamberlain 2009). Factors may be personal or medical, and some are external influences, such as activity, participation, and environmental factors in the ICF, which are categorised in the ICF as environmental factors (WHO 2001).
Although VR interventions vary, their purpose is in general "to maximise the ability of an individual to return to meaningful employment" (BSRM 2000). In other words, the best rehabilitation practice in RTW enhances work and activity tolerance, prevents illness behavior, and reduces pain and the effects of illness or disability (Gobelet 2006). Therefore, VR helps the injured people in mitigating work disability, accelerating return to meaningful employment, minimising lost workdays, increasing the productivity of injured workers, reducing premature retirement, and containing the welfare cost (Disler 2001).
Alhough the Association of British Insurers has suggested that functional and vocational rehabilitation for severe injuries should be administered only after reaching a medical plateau, when the worker's medical condition has stabilised and further significant medical improvement is unlikely (ABI & TUC 2002). From that time on, early intervention and the patient's active involvement can decrease deconditioning, that is, the decrease of physiological adaptation to normal conditions due to immobility, and illness behavior, fostering higher RTW rates (ABI & TUC 2002). Early VR programmes are likely to increase both job and physical well‐being and to decrease the need for a disability pension and sick leave. According to a review on the general effects of rehabilitation on unspecified disability by Kuoppala 2008, VR and multimodal medical treatment combined with VR increase RTW. Moreover, VR delivered to people at risk of job loss (but still employed) can delay job loss (Allaire 2003). In this respect, VR can improve patients' QoL and well‐being as well as reduce workforce attrition.
Why it is important to do this review
Several VR programmes have been used for traumatic upper limb injuries without a critical appraisal of their benefits. Traditional rehabilitation has emphasised training to improve strength, endurance, sensory function, and range of motion. However, recent reviews have shown that various novel VR programmes are effective in enhancing RTW in workers with various diseases or conditions (Aas 2011; Arends 2012; De Boer 2011; Khan 2009; Schaafsma 2010; Van Vilsteren 2015; Vogel 2017). Yet only a few systematic reviews have examined the effectiveness of VR in enhancing early RTW. According to the systematic review by Franche 2005, there is moderate to strong evidence that five kinds of VR, including early contact by the workplace, work accommodation, contact between healthcare provider and workplace, an ergonomic worksite intervention, or the use of a RTW coordinator, can shorten the duration of work disability (Franche 2005). In addition, a recent Cochrane Review focused on the effectiveness of RTW coordination programmes for workers on sick leave compared with usual practice (Vogel 2017). The Van Vilsteren 2015 review, on the other hand, focused on people with low back pain, recurrent musculoskeletal disorders, mental health problems, chronic work‐related upper extremity disorders, or workers with cancer (Van Vilsteren 2015). Other published Cochrane Reviews have assessed the effectiveness of measures to improve RTW in a range of patient populations including those with brain injuries (Nair 2008), back pain (Schaafsma 2010), neck pain (Aas 2011), multiple sclerosis (Khan 2009), and cancer (De Boer 2011), which are all different from our target population of people with traumatic upper limb injuries. The first published version of this review found no randomised controlled trials (RCTs) on VR interventions for enhancing RTW in workers with traumatic upper limb injuries (Hou 2013).
Objectives
To assess the effects of vocational rehabilitation programmes for enhancing RTW in workers with traumatic upper limb injuries.
Methods
Criteria for considering studies for this review
Types of studies
We planned to include all RCTs that compared VR with an alternative (control) intervention such as standard rehabilitation, a more limited VR intervention (such as advice on RTW, referral information, or liaison with employer), or waiting‐list controls.
Types of participants
We planned to include trials where participants were working‐age adults (18 to 65 years) who had been in paid employment (employee or self‐employed) at the time of sustaining an acute episode of traumatic upper limb injury involving any parts of the fingers, hand, wrist, forearm, elbow, or arm, regardless of injury type and mechanism. We excluded participants with shoulder injuries. We excluded trials where participants had been suffering from a subacute or chronic upper limb injury for over three months.
When a study included workers with various kinds of injuries, we planned to include it if 50% or more of the participants had sustained upper limb injuries and the study authors reported separate analyses for them.
We excluded studies where participants had cumulative trauma disorders or repetitive strain injuries such as tendonitis or tendosynovitis, epicondylitis, carpal tunnel syndrome, or the like. We also excluded studies where participants had coexisting injuries to the central nervous system (that is brain or spinal cord), or to internal organs.
Types of interventions
We planned to include any type of intervention for enhancing RTW. Interventions may have been carried out either with an individual or in a group, and in a clinical setting or in the community. Interventions could primarily focus on different factors that influence RTW, for example on coping (in psychological interventions), workplace adjustments (in vocational interventions), or physical exercises (in physical interventions). Interventions are divided into the following.
-
Psychological: any type of psychological intervention such as counselling, education, training in coping skills, cognitive behavioral interventions, and problem‐solving therapy undertaken by any qualified professional (such as a psychologist, social worker, or nurse).
-
Vocational: any type of intervention focused on employment. Vocational interventions may be person‐directed or work‐directed. Person‐directed vocational interventions incorporate programmes that aim to encourage RTW, VR, or occupational rehabilitation in individuals. Work‐directed vocational interventions include workplace adjustments such as modified work hours, modified work tasks, modified workplace, and improved communication with or between managers, colleagues, and health professionals.
-
Physical: any type of physical training (such as functional capacity training, work hardening training), physical exercises (such as tendon exercises, nerve gliding exercises), or training of bodily functions (such as muscle strengthening, balance training, endurance training, sensory re‐education, range of motion).
-
Multifaceted: a combination of psychological, vocational, and physical interventions.
Where there were multiple intervention groups within a trial, we planned to conduct pairwise comparisons of an intervention versus no intervention, placebo, or another intervention.
Types of outcome measures
Primary outcomes
RTW included return to either full‐ or part‐time employment, to the same or a reduced role, and to either the previous job or any new employment (Clay 2010). We planned to consider two types of RTW data.
-
RTW measured as event data, such as RTW rates, or as (change in) disability pension rates (Arnetz 2003; Loisel 2003).
-
RTW measured as time‐to‐event data, such as number of days between reporting sick and any work resumption, or the number of days on sick leave during the follow‐up period (Ebel 2004; MacKenzie 1998; MacKenzie 2006).
Secondary outcomes
-
Functional status: measures related to job demands or activities of daily living expressed in terms of 'can perform the task' or 'cannot perform the task' (Burke 1994; Pransky 2005; Soberg 2010).
-
Quality of life (QoL), measures including overall QoL, physical QoL, emotional QoL, and pain (Bültmann 2007; Post 2006).
Search methods for identification of studies
Electronic searches
For this update, we searched the following electronic databases from the date of the last search in the previous version of the review.
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 9) in the Cochrane Library (searched 3 September 2017), using the search strategy in Appendix 1.
-
MEDLINE (15 November 2012 to 30 August 2017), using the search strategy in Appendix 2.
-
EMBASE (28 November 2012 to 3 September 2017), using the search strategy in Appendix 3.
-
CINAHL (5 May 2013 to 6 September 2017), using the search strategy in Appendix 4.
-
PsycINFO (7 December 2012 to 6 September 2017), using the search strategy in Appendix 5.
After discussion with the Editorial Base, we did not search the OSH UPDATE database for this update as it did not yield any relevant results for the previous version of this review (Hou 2013).
Searching other resources
In an effort to identify further published, unpublished, and ongoing studies, we:
-
scanned the reference lists of relevant review articles and planned to scan the reference lists of included studies;
-
contacted experts in the field of occupational health and safety;
-
planned to write to the authors of included studies to obtain additional references, unpublished trials, and ongoing trials, or to obtain missing data not reported in the original publication.
We set no limitations on publication language, publication status, or date of publication.
Data collection and analysis
Selection of studies
Two authors (WHH and CCC) independently selected suitable studies for inclusion in this review by screening the titles and abstracts of studies identified from the electronic databases. If the title and abstract provided sufficient information to determine that the inclusion criteria were not met, we excluded the study. We further checked the full text of the study if we could not confidently exclude it based on the abstract. When the two authors disagreed about the inclusion of a study, we resolved disagreements by discussion. A third author (HLL) arbitrated when necessary. We listed the studies we excluded after reading the full text and provided the reasons for exclusion in the 'Characteristics of excluded studies' table.
Data extraction and management
We planned to extract and summarise details of included studies using a standardised data extraction form. Where studies had been published more than once, we planned to extract data from all reports and consider the one with the greatest amount of data as the primary reference. Two authors (WHH and CCC) planned to independently extract the following data.
-
Author, title, source of reference, country, and publication year.
-
Number and description of participants.
-
Intervention and comparison.
-
Concomitant interventions.
-
Person(s) delivering the intervention.
-
Primary and secondary outcome data and methods of measurement.
-
Duration of follow‐up.
Assessment of risk of bias in included studies
Two authors (WHH and CCC) planned to independently assess each included study using the Cochrane tool for assessing risk of bias as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This tool addresses specific domains, namely random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of biases (for example extreme baseline imbalance); see Appendix 6 for details of the criteria. We planned to assess the blinding and completeness of the outcome data for each outcome separately and generate a 'Risk of bias' table for each included study. When the two authors disagreed about a particular judgment for the risk of bias, we planned to resolve disagreements by discussion and a third author (HLL) would arbitrate if necessary.
We planned to present the 'Risk of bias' assessments in a summary figure to illustrate all of the judgments in a cross‐tabulation of studies.
Measures of treatment effect
We planned to plot the results of each RCT as point estimates, such as RRs for dichotomous outcomes, means, and standard deviations (SDs) for continuous outcomes, or other types of data as reported by the authors of the studies. When we could not plot the results, we planned to describe them in the 'Characteristics of included studies' table or enter the data into 'Additional tables'.
We planned to plot time‐to‐event data as hazard ratios (HRs). If Kaplan‐Meier curves were presented, we planned to extract the data from the graphs and calculate HRs according to the methods given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Unit of analysis issues
All observed participants in the intervention and control groups were the planned primary unit of analysis. For studies that employed a cluster‐randomised design but did not make an allowance for the design effect, we planned to calculate the design effect based on a fairly large assumed intra‐cluster correlation of 0.10. We based this assumption, by analogy, on studies about implementation research (Campbell 2001). We planned to follow the methods stated in the Cochrane Handbook for Systematic Reviews of Interventions for the calculations (Higgins 2011).
Dealing with missing data
We planned to contact study authors to obtain missing data. Where we could not obtain missing data from study authors, we planned to judge the trials with incomplete outcome data according to the criteria recommended by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For example, if statistics were missing, such as SDs, we planned to calculate them from other available statistics such as P values.
Assessment of heterogeneity
We planned to assess clinical homogeneity based on similarity of population, intervention, outcomes, and follow‐up. We planned to categorise study participants into jobs with high hand load, such as typing or lifting small objects, and into jobs with low upper limb load, such as in monitoring or receptionist work. Otherwise we planned to consider study populations as similar if the participants had been in paid employment when 50% or more of them had sustained an acute episode of traumatic upper limb injury involving any parts of the fingers, hand, wrist, forearm, elbow, or arm, regardless of injury type and mechanism, and regardless of occupation or type of work. We planned to consider interventions as similar if they fell into one of the predefined categories of interventions (as stated in the paragraph on criteria for including studies). We planned to consider the RTW outcomes and sick leave duration outcomes as similar. We planned to regard follow‐up periods of less than 3 months, 3 months to 1 year, and more than 1 year as different. In addition, we planned to test for statistical heterogeneity by means of the Chi² test as implemented in the forest plots in Review Manager 5 (RevMan 5) software (RevMan 2014). This test examines the percentage of total variation across studies due to heterogeneity rather than to chance. We planned to use a significance level of P < 0.10 to indicate whether there was considerable heterogeneity. Moreover, we planned to quantify the degree of heterogeneity using the I² statistic, where an I² value of 25% to 50% indicates a low degree of heterogeneity; 50% to 75%, a moderate degree of heterogeneity; and more than 75%, a high degree of heterogeneity (Higgins 2003).
Assessment of reporting biases
We planned to reduce the effects of reporting bias by including studies and not publications to avoid the introduction of duplicate data. Following the Cho 2000 statement on redundant publications, we attempted to detect duplicate studies and, if more than one article reported on the same study, we planned to extract data only once. We prevented location bias by searching across multiple databases. We prevented language bias by not excluding any article based on language. If sufficient data, meaning at least ten studies with a similar comparison, are available in future updates of this review, we will assess publication bias with a funnel plot.
Data synthesis
We planned to pool data from studies judged to be clinically homogeneous using RevMan 2014. If sufficient data were available, we planned to perform meta‐analyses. When studies were statistically heterogeneous, we planned to use a random‐effects model; otherwise we planned to use a fixed‐effect model. When using the fixed‐effect model, we planned to conduct a sensitivity analysis by using the random‐effects model to test if there were differences in the results. We planned to include 95% CIs for all estimates. For the analysis of HRs, we planned to use the inverse variance method in RevMan 2014. For RTW outcomes we planned to deem time to RTW, the rate of RTW, and the number of days on sick leave sufficiently similar to be combined in a meta‐analysis. We planned to use effect sizes to combine continuous and dichotomous RTW outcome data. We planned to use the mean number of days off work to calculate the effect size for the days on sick leave with the following formula: mean change difference over SD (Håland 2002). For the HRs and rate ratios, we planned to take their natural logarithms and transform them into effect sizes as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Chinn 2000; Higgins 2011). We planned to use effect sizes and their standard errors as input in the meta‐analysis using the generic inverse variance method. After meta‐analysis, we planned to re‐calculate a mean difference in time‐to‐RTW from the pooled effect size using the median SD of the included studies in the formula: pooled mean difference = pooled effect size × median SD.
We planned to use the GRADE approach as described in Higgins 2011 and implemented in the GRADEPro 3.6 software to present the quality of evidence and 'Summary of findings' tables (GRADEpro).
The downgrading of the quality of a body of evidence for a specific outcome would be based on five factors.
-
Limitations of study.
-
Indirectness of evidence.
-
Inconsistency of results.
-
Imprecision of results.
-
Publication bias.
The GRADE approach specifies four levels of quality (high, moderate, low, and very low) (Van Tulder 2003).
Subgroup analysis and investigation of heterogeneity
If sufficient data are available in future updates of this review, we will perform subgroup analyses according to injury severity or body parts, setting, and quality of the study, because these variables could potentially affect the intervention effect estimates.
Similarly, if sufficient data are available in future updates of this review, we will also perform separate subgroup analyses of: return to the previous role (either under the same or a new employer), return to a reduced role (either under the same or a new employer), change from full‐time to part‐time employment, and change to a reduced pay employment.
Sensitivity analysis
If sufficient data are available in future updates of this review, we will conduct a sensitivity analysis to test the robustness of our meta‐analysis results by excluding studies judged to be at high risk of bias.
Results
Description of studies
Results of the search
In the previous version of our review (Hou 2013), we identified a total of 332 records. We identified a total of 466 records in this update. See Figure 1 for the PRISMA study flow diagram.
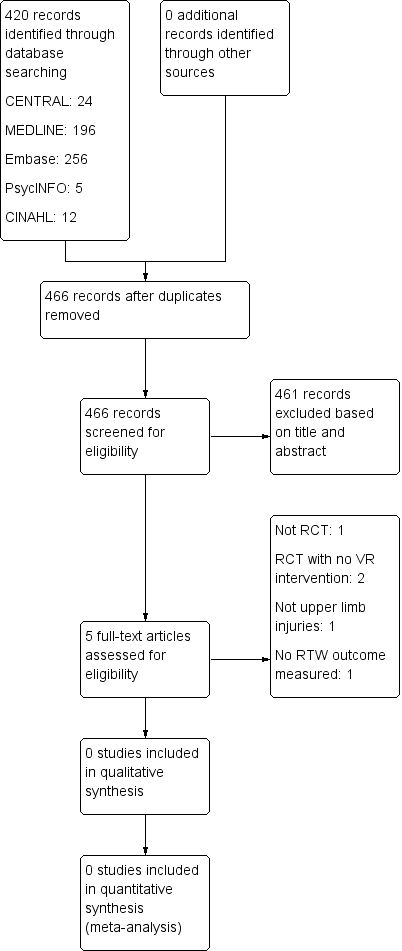
PRISMA study flow diagram.
Included studies
None of the studies identified met our inclusion criteria for this update.
Excluded studies
In the previous version of our review (Hou 2013), we considered 15 studies potentially eligible and retrieved their full texts. However, all of them failed to meet the inclusion criteria and therefore we excluded them. In this update, we considered five studies potentially eligible and retrieved their full texts. However, all five failed to meet our inclusion criteria. We present descriptions of all five studies with the reasons for exclusion in the Characteristics of excluded studies table.
Risk of bias in included studies
We did not include any RCTs, so there was no risk of bias to assess.
Effects of interventions
We did not include any RCTs, so we did not conduct any analyses.
Discussion
Summary of main results
In this update, we did not identify any RCTs addressing the efficacy of VR in enhancing RTW in workers with traumatic upper limb injuries. Most of the studies identified from the searches evaluated the effects of range of motion exercise and physical training to facilitate early RTW. A number of identified RCTs compared different policies of workplace accommodation, counselling, case management, or worksite visits for workers with chronic musculoskeletal problems of the upper extremities (Cheng 2007; Haahr 2005; Li 2006). There were also clinical trials comparing surgical intervention and medical rehabilitation (that is splinting, mobilising, or strengthening) for upper limb injuries during hospitalisation (Feehan 2004; Lubbert 2008; Unsworth‐White 1994). Various VR programmes have been developed to help workers who have sustained traumatic upper limb injury to return to the labour market. However, we found no high‐quality evidence to either support or refute the effects of VR for enhancing RTW in workers with traumatic upper limb injuries.
Overall completeness and applicability of evidence
The absence of randomised controlled trials eligible for inclusion in this review illustrates that the evidence on VR for enhancing RTW in workers with traumatic upper limb injuries is unclear and incomplete. All of the studies that we retrieved in the searches assessed the effects of different rehabilitation after immobilisation or enhancing range of motion strategies at acute medical stages, which we had pre‐specified as exclusion criteria for this review.
Potential biases in the review process
We made every attempt to limit bias in the review process by ensuring a comprehensive search for potentially eligible studies. The authors' independent assessments of eligibility of studies for inclusion in this review minimised the potential for additional bias.
Agreements and disagreements with other studies or reviews
We found a systematic review of early prognostic factors for RTW following orthopaedic trauma (Clay 2010). This review used prospective and retrospective cohort studies and explored prognostic factors either at pre‐injury or at the early postinjury phase. Two prospective studies that used survival analysis found that providing strong practical support and modified work increased the likelihood of RTW to 1.7 and 1.24 times, respectively (MacKenzie 1998; Seland 2006). However, none of the studies included in the Clay 2010 review assessed the effectiveness of VR interventions for acute orthopedic injuries.
There are several RCTs focusing on the effects of rehabilitation interventions for adults with distal radial fractures, and a previous Cochrane Review has pooled their results (Handoll 2006). The types of rehabilitation interventions examined in these studies are limited to hand therapy or medical rehabilitation, and do not include further VR programmes for patients with orthopaedic trauma.

PRISMA study flow diagram.

