Radioterapia estereotáctica para el schwannoma vestibular
Resumen
Antecedentes
Los schwannomas vestibulares (neurinomas acústicos) son tumores benignos comunes que surgen de las células de Schwann del nervio vestibular. Las opciones de tratamiento incluyen observación con seguimiento neurorradiológico, resección microquirúrgica y radioterapia estereotáctica.
Objetivos
Evaluar el efecto de la radioterapia estereotáctica comparada con observación, resección microquirúrgica, cualquier otra modalidad de tratamiento o una combinación de dos o más de los enfoques mencionados para el schwannoma vestibular.
Métodos de búsqueda
Se hicieron búsquedas en el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials); PubMed; EMBASE; CINAHL; Web of Science; CAB Abstracts; ISRCTN y en fuentes adicionales para encontrar ensayos publicados y no publicados. La fecha de la búsqueda fue el 24 de julio de 2014.
Criterios de selección
Ensayos controlados aleatorios (ECA) que exploran la eficacia de la radioterapia estereotáctica comparada con observación sola, resección microquirúrgica o cualquier otro tratamiento posible o una combinación de tratamientos en pacientes con un tumor del ángulo cerebelopontino de hasta 3 cm de diámetro, que se supone es un schwannoma vestibular.
Obtención y análisis de los datos
Se utilizaron los procedimientos metodológicos estándar previstos por la Colaboración Cochrane.
Resultados principales
Ningún estudio cumplió los criterios de inclusión para esta revisión.
Conclusiones de los autores
No existen pruebas de alta calidad en la bibliografía proveniente de ECA para determinar si la radioterapia estereotáctica es mejor que la resección microquirúrgica o la observación sola en pacientes con un schwannoma vestibular. Ante la falta de dichas pruebas, el método de tratamiento debe elegirse sobre una base individual, teniendo en cuenta las preferencias del paciente, la experiencia del médico y la disponibilidad de equipo radioterapéutico. Con la disponibilidad cada vez mayor de equipo radioterapéutico, deben emprenderse ensayos controlados aleatorios para evaluar la función de la radioterapia estereotáctica en comparación con otras opciones de tratamiento.
PICO
Resumen en términos sencillos
Radioterapia estereotáctica para el tratamiento del schwannoma vestibular (neuroma acústico)
Los schwannomas vestibulares, también conocidos como neurinomas acústicos, son tumores benignos del octavo nervio craneal (responsable de la audición y el equilibrio). Pueden ser tratados con cirugía o radioterapia estereotáctica (irradiación cerebral focalizada administrada con precisión), o sólo mantenerlos bajo observación debido a que pueden crecer muy lentamente o no crecer en absoluto.
Se realizaron búsquedas en la bibliografía para encontrar ensayos controlados aleatorios (ECA) que compararan radioterapia estereotáctica con otros métodos de tratamiento. Ninguno de los estudios identificados cumplió con los criterios para su inclusión en esta revisión.
Actualmente no hay pruebas de alta calidad provenientes de ECA para determinar si alguna de las opciones de tratamiento para los pacientes con un schwannoma vestibular presenta ventajas claras sobre las otras. Por lo tanto, el tratamiento debe seleccionarse sobre una base individual, teniendo en cuenta las propias preferencias del paciente, la experiencia del médico y la disponibilidad de equipo radioterapéutico. Se necesita más investigación para comparar la eficacia y seguridad de todas las diferentes opciones de tratamiento.
Authors' conclusions
Background
Description of the condition
Vestibular schwannomas, also known as acoustic neuromas, are benign tumours of Schwann cell origin that occur on the eighth cranial nerve. They represent 5% to 10% of all intracranial tumours (House 1974), and 80% to 90% of tumours of the cerebellopontine angle (Hart 1981).
The incidence of vestibular schwannoma is 2 per 100,000 person‐years (Stangerup 2012), and the prevalence is estimated at 2 in 10,000 people (Lin 2005). Several centres have reported an increasing incidence of diagnosed vestibular schwannoma over recent years (Stangerup 2012). These tumours occur with about equal frequency in adult males and females, most frequently in patients between the ages of 30 and 60 years (Stangerup 2012). A minority of patients have central neurofibromatosis, with bilateral tumours.
Commonly presenting symptoms include hearing loss, tinnitus and balance disturbance. Tumour progression can lead to brainstem compression, cranial neuropathies and hydrocephalus (Hansasuta 2011). The diagnosis is established with magnetic resonance imaging (MRI), which can demonstrate tumours as small as a few millimetres. As imaging technology has improved, more small tumours have been diagnosed.
Management options include observation, microsurgical resection and stereotactic radiotherapy (Hansasuta 2011; Varughese 2012).
Observation with neuroradiological follow‐up is a management option for vestibular schwannoma, since many of these tumours grow slowly over years, or may not grow at all (Stangerup 2012).
The surgical resection of vestibular schwannoma has been a central feature of neurosurgical practice for more than 100 years (Ramsden 1995), from the pioneering attempts to achieve simple decompression, to the contemporary era, where the function of the eighth and adjacent cranial nerves may be preserved (Sampath 1998). However, while total tumour removal is possible with microsurgical resection in about 95% of patients, normal or near‐normal facial nerve preservation is only possible in about 80% on average (Samii 1997), and hearing may be preserved in about 35% to 65% of patients (Battaglia 2006), although these numbers depend highly on tumour size, tumour localisation and the experience of the surgical team.
Stereotactic radiotherapy is a non‐invasive technique that delivers high‐dose irradiation to small, targeted tissue volumes. The use for vestibular schwannoma was first described by Leksell (Leksell 1971), and it represents an alternative to microsurgical resection in patients with small and moderate size tumours. It has been said that tumours up to 3 cm in diameter, when including the internal auditory canal in the measurement, can be successfully controlled in the majority of patients with this technique (Lederman 1997), although most studies reporting on the control of tumour growth include patients without documented tumour growth before the initiation of treatment.
There is no international consensus regarding the optimal treatment for vestibular schwannoma.
Description of the intervention
Brain radiotherapy is a procedure in which beams of radiation are converged and targeted at a volume of tissue within the brain. Stereotaxis is an accurate targeting technique for intracranial structures that uses an external reference frame fixed to the head. Stereotactic radiotherapy therefore refers to the non‐invasive destruction, by focused irradiation, of a particular intracranial target localised stereotactically.
In 1968, the first 'Leksell gamma unit', or 'gamma knife', was designed at the Karolinska Institute in Stockholm, Sweden. The unit evolved into the commercially available Leksell gamma unit, containing cobalt‐60 sources located in a hemispherical array around a common focal point. Stereotactic radiotherapy has become an important treatment option for many patients with intracranial and spinal disorders (Sheehan 2009), ranging from arterial venous malformations to benign and malignant neoplasms (Yu 1997). Targets up to 3 cm in diameter are usually considered suitable for stereotactic radiotherapy.
A typical stereotactic radiotherapeutic procedure begins with the application of the stereotactic head frame under local anaesthesia. A magnetic resonance imaging (MRI) scan is then performed and a radiotherapeutic protocol designed to deliver the radiation dose to the defined target volume. The procedure is usually performed as an outpatient procedure and is well tolerated by the patient, with few patients developing major acute effects (Chao 2012).
How the intervention might work
Stereotactic radiotherapy works by inducing radiation necrosis in the targeted tissue volume. The desired response is long‐term growth control of the tumour (Niranjan 2004).
An observational study by Breivik and colleagues followed 237 patients with vestibular schwannoma for almost five years. One‐hundred and thirteen patients received radiotherapy and 124 were managed conservatively. There was a significant reduction in tumour volume over time in the radiotherapy group and the need for additional treatment was reduced, compared to the observed patients, suggesting that vestibular schwannomas can be controlled by radiotherapy (Breivik 2013). As the technique has developed, cranial nerve complications following stereotactic radiotherapy have been significantly reduced by modifications in dose schedules (Noren 1993).
In comparison, a meta‐analysis of observation as a management option included 26 studies with 1340 patients in total. Growth of the tumour was observed in 46% of patients, with a mean growth rate of 1.2 mm/year. Subsequent active treatment was required by only 18% of all patients (Yoshimoto 2005).
Why it is important to do this review
We are unaware of any guidelines on the effectiveness and safety of stereotactic radiotherapy in comparison to observation or microsurgical resection as a management strategy. The best candidates for stereotactic radiotherapy are usually also ideal candidates for microsurgical resection (patients with easily resectable small to moderate size tumours). This dilemma is evident in everyday clinical practice, in centres which can offer stereotactic radiotherapy as an alternative treatment. Furthermore, it is still unclear whether some of these patients can be managed by observation alone. The limited availability of radiotherapeutic equipment makes decision‐making even more complex.
This review is important to facilitate decision‐making by clinicians and patients.
Objectives
To assess the effect of stereotactic radiotherapy compared to observation, microsurgical resection, any other treatment modality, or a combination of two or more of the above approaches for vestibular schwannoma.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) evaluating the efficacy of stereotactic radiotherapy for vestibular schwannoma. We considered for inclusion all studies, irrespective of publication status or language.
Types of participants
Patients, irrespective of gender, age or race, with a cerebellopontine angle tumour up to 3 cm in diameter, presumed to be vestibular schwannoma. We excluded patients who had previously been treated surgically for vestibular schwannoma.
Types of interventions
Stereotactic radiotherapy (any protocol, dose or hardware).
We looked for the following comparisons:
-
stereotactic radiotherapy versus microsurgical resection;
-
stereotactic radiotherapy versus observation;
-
stereotactic radiotherapy versus any other possible treatment or combination of treatments.
Types of outcome measures
Primary outcomes
-
Proportion of patients in whom the tumour has not grown and whose symptoms (hearing loss, facial function, tinnitus, balance disturbance) have not deteriorated a) at 12 months, b) at two years, c) in the long term.
Secondary outcomes
-
Tumour growth.
-
Changes in hearing.
-
Changes in facial function (assessed using a validated assessment instrument).
-
Changes in tinnitus.
-
Changes in balance disturbance.
-
Quality of life.
-
Reported side effects of stereotactic radiotherapy (early, intermediate and late), including the induction of secondary malignancies, peritumoral oedema, hydrocephalus and other cranial nerve neuropathies.
-
Reported side effects of microsurgical resection (mortality, postoperative cranial nerve neuropathies, meningitis, cerebrospinal fluid leaks).
-
Reported necessity for additional treatment in patients managed by observation.
Search methods for identification of studies
We conducted systematic searches for randomised controlled trials. There were no language, publication year or publication status restrictions. The date of the search was 24 July 2014.
Electronic searches
We searched the following databases from their inception for published, unpublished and ongoing trials: the Cochrane Central Register of Controlled Trials (CENTRAL 2014, Issue 6); PubMed; EMBASE; CINAHL; LILACS; KoreaMed; IndMed; PakMediNet; CAB Abstracts; Web of Science; ISRCTN; ClinicalTrials.gov; ICTRP, Google and Google Scholar.
We modelled subject strategies for databases on the search strategy designed for CENTRAL. Where appropriate, we combined subject strategies with adaptations of the highly sensitive search strategy designed by The Cochrane Collaboration for identifying randomised controlled trials and controlled clinical trials (as described in the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, Box 6.4.b. (Handbook 2011)). Search strategies for major databases including CENTRAL are provided in Appendix 1.
Searching other resources
We scanned the reference lists of identified publications for additional trials and contacted trial authors where necessary. In addition, we searched PubMed, TRIPdatabase, The Cochrane Library and Google to retrieve existing systematic reviews relevant to this systematic review, so that we could scan their reference lists for additional trials. We searched for conference abstracts using the Cochrane Ear, Nose and Throat Disorders Group Trials Register.
Data collection and analysis
Selection of studies
Two members of the review team independently selected papers and made decisions about eligibility, based on the analysis of the title, abstract or MeSH terms. We resolved all disagreements by discussion and consensus. We contacted the authors of the original papers to get additional data and clarify dubious issues.
Data extraction and management
We extracted the relevant data from the selected studies and recorded the data in customised forms. Two members of the review team performed the extraction, after determining the study eligibility. We discussed possible disagreements and if no consensus was reached, resolved them by the inclusion of the third author in the extraction process. We contacted authors of the original articles.
We extracted the following data:
-
study design, setting and duration;
-
participants;
-
sample size;
-
inclusion and exclusion criteria;
-
details of the experimental intervention (protocol);
-
details of the control intervention;
-
outcome (the effect of treatment, defined as tumour growth control at the six‐month to two‐year follow‐up);
-
presence of ethical approval;
-
funding sources;
-
conclusions as reported by the authors.
Assessment of risk of bias in included studies
No studies were included in the current version of the review. Should studies be included in future updates, will undertake assessment of the risk of bias of the included trials independently by with the following taken into consideration, as guided by theCochrane Handbook for Systematic Reviews of Interventions (Handbook 2011):
-
sequence generation;
-
allocation concealment;
-
blinding;
-
incomplete outcome data;
-
selective outcome reporting; and
-
other sources of bias.
We will use the Cochrane 'Risk of bias' tool in Review Manager (RevMan 5) (RevMan 2014), which involves describing each of these domains as reported in the trial and then assigning a judgement about the adequacy of each entry: 'low', 'high' or 'unclear' risk of bias.
Measures of treatment effect
If studies are included in future versions of review, we will analyse the data using RevMan 5. We will analyse binary data using odds ratio (with 95% confidence interval) and continuous outcomes by calculating means and standard deviations. We will pool scores as continuous variables either using weighted means or standardised means.
Unit of analysis issues
The unit of analysis will be the individual patient.
Dealing with missing data
Missing summary data will not be a reason to exclude a study from the review. If necessary, we will contact the authors of the original papers for more information on missing data.
Assessment of heterogeneity
We will test all included studies for clinical homogeneity. For studies considered to be clinically homogeneous, we will test the statistical heterogeneity using the Chi² test and the I² statistic. We will assume statistical significance of the Chi² test if the P value < 0.10. We will consider an I² statistic value greater than 50% to be substantial.
Assessment of reporting biases
Aside from within‐study biases tested as described in Assessment of risk of bias in included studies, we will assess between‐study biases by comparing outcomes stated in protocols to those reported or, where protocols are not available, by comparing outcomes listed in the methods section to those reported in the results section.
Data synthesis
We could not perform data synthesis, as no studies are included in present version of the review. If studies can be included in the future updates, we will use RevMan 5 to perform meta‐analysis, if we identify a sufficient number of studies (RevMan 2014). We will use a fixed‐effect model for dichotomous data.
Subgroup analysis and investigation of heterogeneity
No subgroup analysis is planned.
Sensitivity analysis
If necessary, we will perform sensitivity analysis by comparing the primary analysis with analysis of the subgroup of studies that excludes those with unclear or high risk of bias.
Results
Description of studies
Results of the search
Following a full search on 24 July 2014, we identified 760 studies. Other research sources provided no additional records. When we removed duplicates, 583 studies remained for further selection. Based on the title, abstract and keywords, we selected 36 studies as potentially relevant for the review and obtained them in full text (Figure 1). We discarded 33 of these studies, following review of the full text. We formally excluded three studies from the review (see Excluded studies). There are no studies awaiting assessment and we found no ongoing trials.
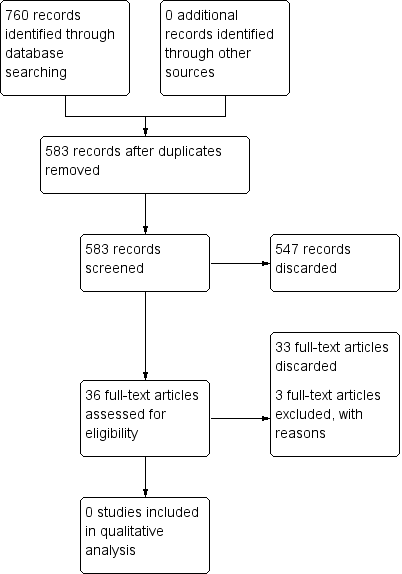
Study flow diagram.
Included studies
After we analysed the full‐text articles, we found that none of the studies met the inclusion criteria.
Excluded studies
See: Characteristics of excluded studies.
We excluded two prospective studies because of the lack of randomisation (Myrseth 2009; Pollock 2006). Both studies compared stereotactic radiotherapy with microsurgical resection. In the study by Myrseth et al, patients were allowed to choose treatment, after receiving information about all treatment alternatives (Myrseth 2009). Patients in the study by Pollock et al also chose the treatment after discussion of the options (Pollock 2006). One study was a prospective randomised controlled trial comparing two radiosurgical modalities. It did not report the treatment outcomes required for a study to be included in the review (Régis 2009). It evaluated irradiation time, treatment time, treatment room occupation time, dose‐planning parameters, dosimetry measurements on the patient's body, workflow, patient comfort and quality assurance procedures for patients with various intracranial pathologies, 79 of whom had acoustic neuromas. We contacted the authors of this study and they expect to publish data regarding the treatment outcome.
Risk of bias in included studies
No studies met the inclusion criteria.
Effects of interventions
No studies met the inclusion criteria.
Discussion
The wider availability of stereotactic radiotherapy has led to difficulty in choosing the optimal treatment for patients with vestibular schwannoma. While many papers and review articles report satisfactory tumour growth control and few side effects with this method (Arthurs 2011; Mendehall 2004), it is still unclear whether this treatment is superior to microsurgical resection. Furthermore, observation with neuroradiological follow‐up may be an equally valid option. Prospective randomised controlled trials comparing all three treatment options are therefore clearly needed.
Summary of main results
In the present version of the review, we were not able to include any studies, mainly due to lack of randomisation in otherwise well‐designed trials (Myrseth 2009; Pollock 2006). A randomised controlled trial comparing two stereotactic radiotherapy techniques has not yet reported any clinical outcome data, however the publication of these data is planned (Régis 2009).
Quality of the evidence
The main issue we identified with the studies considered for this review was the lack of randomisation. This may be because researchers consider it unethical to design such a trial, because individual patient considerations or preferences render randomisation very difficult or even impossible, because the treatment centres do not master the different treatment modalities equally well, or because the researchers themselves are biased towards one of the treatment options.
Furthermore, the studies we considered usually did not investigate the late side effects of stereotactic radiotherapy, such as the induction of secondary malignancies. This should be done in the assessment of all procedures using irradiation.
Potential biases in the review process
At present, the only possible bias in the review process could be related to accidentally missing relevant studies. However, we performed an extensive literature search for this review, covering 16 international databases, and our search is up to date to July 2014, so we consider this is highly unlikely.
Agreements and disagreements with other studies or reviews
There are three recent reviews of the literature on treatment modalities for vestibular schwannoma (Bassim 2010; Gauden 2011; Maniakas 2012). As in this review, no randomised controlled trials were identified. The main body of evidence comes from non‐randomised trials or observational studies. Bassim et al concluded that the lack of uniform reporting criteria for tumour control, facial function and hearing preservation, as well as the variability in follow‐up times, makes difficult to compare studies of radiation treatment for vestibular schwannoma; they recommend that consideration be given to using standardised reporting guidelines (such as those used in otology) for reporting vestibular schwannoma resection results (Bassim 2010). Gauden et al state that the most common quality of life measure used is the Short Form Questionnaire (SF‐36), although it has not been validated for patients with vestibular schwannomas (Gauden 2011). The problem of selecting uniform outcome measures is also evident in our review (Characteristics of excluded studies). All studies emphasise the need for well‐designed, randomised prospective research (Bassim 2010; Gauden 2011; Maniakas 2012), which is in concordance with our conclusions.
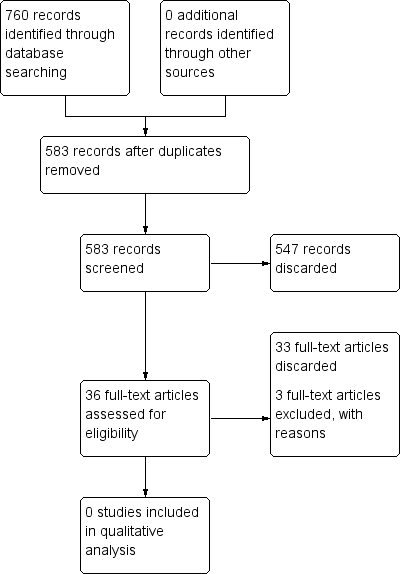
Study flow diagram.

