Atención domiciliaria o en hogar de acogida versus atención residencial a largo plazo para pacientes mayores con dependencia funcional
Información
- DOI:
- https://doi.org/10.1002/14651858.CD009844.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 03 abril 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Práctica y organización sanitaria efectivas
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Two review authors (CY and DS) independently selected studies, assessed the methodological quality of the studies and extracted data.CY, AH, DGB, and DS drafted the review, and all authors read and commented on drafts and approved the final version. All authors made substantial contributions to the conception and design of the work.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Supported by an unrestricted grant from the Age‐related Diseases Trust, TJQ is supported by a joint Stroke Association/Chief Scientist Office Senior Clinical Lecturer Fellowship, UK.
-
NIHR Cochrane Programme grant, UK.
Declarations of interest
CY: the Age Related Diseases Trust provided grant support to the University of Glasgow for this review
AMH: none known
DGB: none known
TJQ: none known
LH: none known
BVM: none known
DS: the Age Related Diseases Trust provided grant support to the University of Glasgow for this review
Acknowledgements
Supported by an unrestricted grant from the Age‐related Diseases Trust, and the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding and a Cochrane programme grant to the EPOC Group; the views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS, or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Apr 03 | Home or foster home care versus institutional long‐term care for functionally dependent older people | Review | Camilla Young, Amanda M Hall, Daniela C Gonçalves‐Bradley, Terry J Quinn, Lotty Hooft, Barbara C van Munster, David J Stott | |
| 2012 Jun 13 | At‐home versus institutional long‐term‐care for chronic functionally dependent older people | Protocol | Camilla Young, Esther MM van de Glind, Terry J Quinn, Lotty Hooft, Lynn A Legg, Barbara C van Munster, David J Stott | |
Differences between protocol and review
We amended the title of the review to reflect the interventions identified for inclusion. We introduced other changes to comply with Cochrane standards for conducting and reporting a review, namely introduced a Summary of findings table. Two authors left the review team (EMMvdG and LH) and two authors joined the review team (AMH and DCGB).
Notes
This review was first published in the Cochrane Library in 2002 (Mottram 2002), but in 2007 it was withdrawn, as it was determined to be out‐of‐date at that time and contained possibly misleading evidence. A revised protocol was published in 2012 (Young 2012).
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Aged; Humans;
PICO

Study flow diagram.
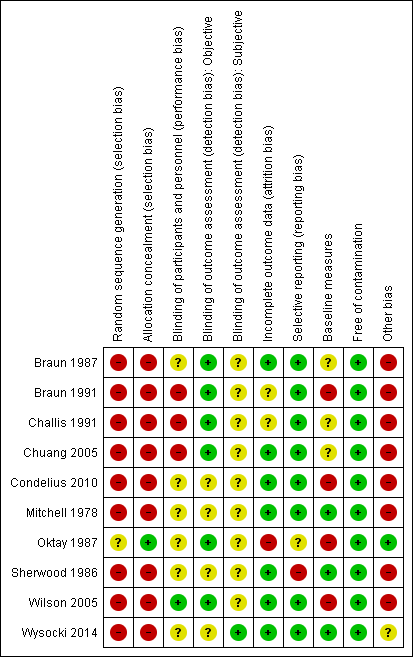
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
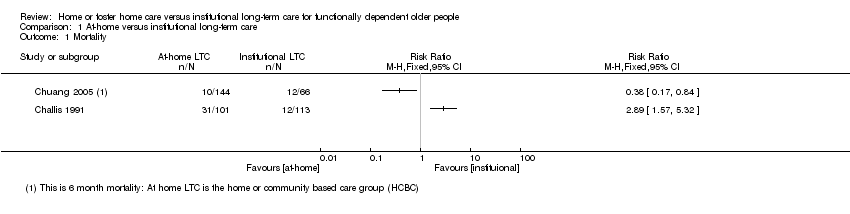
Comparison 1 At‐home versus institutional long‐term care, Outcome 1 Mortality.
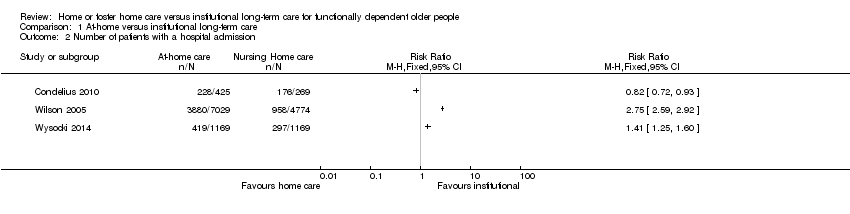
Comparison 1 At‐home versus institutional long‐term care, Outcome 2 Number of patients with a hospital admission.
| Home or foster home versus institutional long‐term care for functionally dependent older people | ||||
| Patient or population: older adults with functional dependence Settings: long‐term care Intervention: long‐term home care Comparison: long‐term institutional care | ||||
| Outcomes | Relative effect | No of participants | Certainty of evidence | Comments |
| Mortality (6 months) | It is uncertain whether long‐term home care compared to nursing home care decreases mortality risk Estimates ranged from a relative increase in risk of mortality of RR 2.89 (95% CI 1.57 to 5.32) to a relative reduction in risk of RR 0.38 (95% CI 0.17 to 0.61). | 314* | ⊕⊝⊝⊝ | Data were not pooled due to the high degree of statistical heterogeneity for this outcome (I2 = 94%) |
| Physical function (3‐6 months) | It is uncertain whether long‐term home care compared to nursing home care improves physical function Estimates ranged from and improvement in activities of daily living of MD −0.25 points (95% CI −0.44 to −0.06) to MD −1.90 (95% CI −2.18 to −1.62) | 1295* | ⊕⊝⊝⊝ | 3 studies reporting data used the Katz Index of ADLs or a variation of this measure 2 studies did not provide usable post or change‐score data. 1 study reported no between‐group difference in change in ADLs. 2 studies reported improvements in ADLs for participants receiving home LTC compared to nursing home LTC |
| Quality of life (3‐6 months) | It is uncertain whether long‐term home care compared to nursing home care improves happiness (RR 1.97, 95% CI 1.27 to 3.04) or general satisfaction | 114 | ⊕⊝⊝⊝ | Both studies used proxy items for this outcome. While both variables were assessed using continuous measures, authors further dichotomised the outcome for reporting, precluding meta‐analysis. |
| Hospital admissions | It is uncertain whether long‐term home care compared to nursing home care decreases hospital admissions Estimates ranged from a relative increase in risk of a hospitalisation of RR 2.75 (95% CI 2.59 to 2.92) to a relative reduction in risk of RR 0.82 (95% CI 0.72 to 0.93). | 14,853 (3 studies) | ⊕⊝⊝⊝ | This outcome described the number of participants having at least one hospital admission. Data were not pooled due to the high degree of statistical heterogeneity for this outcome (I2 = 99%) |
| Number of adverse health outcomes | The extent to which long‐term home care was associated to more or fewer adverse health outcomes than nursing home care was not reported. | ‐‐‐ | ‐‐‐ | ‐‐‐ |
| ADL: activities of daily living; CI: confidence interval; LTC: long‐term care; RR: risk ratio. | ||||
| GRADE Working Group grades of evidence | ||||
| aDowngraded due to study design. * For Chuang 2005, only participants receiving institutional or home/community‐based care were included; participants receiving family care were not included. | ||||
| Study | Service Location (home / community) | Type of services | Dose (how many services and their frequency of provision) | Provider |
| Home | Help with laundry, shopping, cleaning, and personal care. Excluded meals on wheels or transport services | ≥ 4 home visits per month | Not reported | |
| Home | Medical care and ancillary services in participant's own home. A potential caregiver (friend, relative, or hired caretaker) must be living in the patient's home and able to assume responsibility for care. | Not reported | Home care team (physician, nurse, dietician, social worker) | |
| Home | Darlington Care Project: case management service, which could include any number of medical services based on client needs (speech therapy, stoma care, catheter care, change of dressing). Personal care (bathing, dressing, toileting, feeding, hand/nail care), physical care, (assist with walking, lifting/transferring). Social and recreational activities and therapeutic exercises | Not reported | Case manager likely a nurse? Other HCPs as needed | |
| Home | Not reported | Not reported | Not reported | |
| Home or community | Not reported | Not reported | Not reported | |
| Home or community | Not reported | Not reported | Not reported | |
| Home or community | Nursing Home Without Walls (NHWW) provides an array of services including case management, skilled nursing, personal care, adult day health, home delivered meals, nutritional counselling, transportation, respite, emergency alarms, moving assistance, rehabilitation, home maintenance, environmental modifications, homemakers | Not reported | Nurse | |
| Community | Counselling, transportation, meals, recreational activities, information/referral, and monitoring services. Based on a patient assessment, the programme could provide medication monitoring, and/or arrange for various types of therapies | Not reported | Social worker/nurse |
| Study | Service Location | Type of services | Provider |
| Room in a foster home | Caregivers provided the patient with meals, laundry, assistance with personal and instrumental ADLS, 24‐hour supervision and nursing tasks as needed (e.g. monitoring medication, injections and behavioural modification) | Caregivers were trained by the Johns Hopkins Hospital | |
| Foster home care | Caregivers provided personal care services, 24‐hour supervision, and meal, laundry and household services | Caregivers were a part of a certification and monitoring programme | |
| Foster care home | Community Care Program: families provide 24‐hour supervision, room and board, homemaker services, personal care including assistance with ADLs, medication, range of motion and other exercises, and in some cases, tube feeding, dressing changes, insulin injections, catheter irrigations, transportation to medical and social outings | Families are trained and supervised by social worker/nurse teams to adopt and care for 1‐2 patients |
| Study | Time‐point | Type of long‐term care | Sample size | Results | Relative effect RR (95% CI) | |
| Home care | Nursing home | |||||
| 6 months | Blended | 352 | 8% (18/221) | 16% (21/131) | 0.51 (0.28 to 0.92) | |
| 6 months | Home care | 214 | 34% (31/101) | 11% (12/113) | 2.89 (1.57 to 5.32) | |
| 6 months | Home care | 474 poststroke | 6% (24/408) | 18% (12/66) | 0.38 (0.17 to 0.61) | |
| 12 months | Home care | 214 | 40% (40/101) | 31% (35/113) | 1.28 (0.89 to 1.84) | |
| 12 months | Foster care | 112 | 29% (17/59) | 32% (17/53) | 0.90 (0.51 to 1.57) | |
| CI: confidence interval; RR: risk ratio. | ||||||
| RR: risk ratio. | ||||||
| Study | Time point | Sample size | Measure | D/Ca | Results | Relative effectb (95% CI) | |
| Home care | Nursing home | ||||||
| Home care | |||||||
| 3 months | 195 | ADLd (change) | — | — | — | — | |
| 3 months | 98 | ADLe | C | Post: 13.02 | Post: 13.16 | — | |
| 3 months | 98 | ADL (mobility)e | C | −1.02 | −1.05 | — | |
| 6 months | 210 | ADLe | — | — | — | — | |
| 9 months | 98 | ADL performance assessment | ? | — | — | −0.25 (−0.44 to −0.06) | |
| Unclear | 694 | ADLg | C | 3.0 (1.2) | 3.9 (0.4) | −0.9 (−1.02 to −0.78) | |
| Unclear | 694 | ADLh | C | 1.4 (1.7) | 3.4 (1.9) | −1.90 (−2.18 to −1.62) | |
| Foster care | |||||||
| 12 months | 53 | ADLd (improved/maintained) | D | 79% (22/28) | 60% (15/25) | 0.19 (−0.07 to 0.43) | |
| 12 months | 53 | ADLg (improved/maintained) | D | 75% (21/28) | 68% (17/25) | 0.07 (−0.17 to 0.31) | |
| 9 months | 62 | ADL performance assessment | — | — | — | — | |
| Unclear | — | — | — | — | — | — | |
| Blended | |||||||
| 6 months | 352 | ADLe (pre‐post) | C | Pre: 12.87 Post: 12.16 | Pre: 14.43 Post: 13.78 | — | |
| 6 months | 352 | ADLe (change) | 0.71 | 0.65 | — | ||
| ADL: activities of daily living; CI: confidence interval; RR: risk ratio. | |||||||
| aD: dichotomous outcome; C: continuous outcome. | |||||||
| Study | Time point | Type of long‐term care | Sample Size | Measure | D/Ca | Results | Relative effectb (95% CI) | Favours | |
| Home care | Nursing home | ||||||||
| Home care | |||||||||
| 3 months | Community care | 132 | Reported level of happinessc | D | 67% (59/88) | 34% (15/44) | 1.97 (1.27 to 3.04) | Home care | |
| 6 months | Community care | 214 | General satisfactiond (change) | C | 0.79 | 0.08 | — | Home care | |
| 6 months | Community care | 214 | Well‐being – moraled (change) | C | 0.79 | 0.21 | — | Home care | |
| 6 months | Community care | 214 | Well‐being – depressiond (change) | C | 0.33 | −1.05 | — | Home care | |
| Foster care | |||||||||
| 12 months | Foster care | 53 | Life satisfaction (improved/maintained) | D | 46% (13/28) | 72% (18/25) | RR: 0.64 (0.40 to 1.03) | Nursing | |
| 12 months | Foster care | 53 | Perceived health (improved/maintained) | D | 68% (19/28) | 84% (21/25) | RR: 0.81 (0.59 to 1.10) | Nursing | |
| 12 months | Foster care | 53 | Mental status (improved/maintained) | D | 64% (18/28) | 60% (15/25) | RR: 1.07 (0.70 to 1.64) | ||
| CI: confidence interval; RR: risk ratio. | |||||||||
| aD: dichotomous outcome; C: continuous outcome. | |||||||||
| Study | Time‐point | Type of long‐term care | Sample Size | Measure | Results | Relative effect: RR (95% CI) | Favours | |
| Home care | Nursing home | |||||||
| Observational (data set) | Home care | 11,803 | Hospital admissiona | 55% (3880/7029) | 20% (958/4774) | 2.75 (2.59 to 2.92) | Nursing home? | |
| Observational (dataset) | Home care | 11,803 | Emergency room visitsb | 70.1% (4992/70290 | 34.8% (1662/4774) | — | Nursing home? | |
| Observational (dataset) | Home/community care | 2338 | Preventable hospitalisationc | 11.4% (133/1169) | 9.7% (113/1169) | — | Nursing home? | |
| Observational (dataset) | Home/community care | 2338 | Any hospitalisationd | 35.8% (419/1169) | 25.4% (297/1169) | 1.41 (1.25, 1.60) | Nursing home? | |
| unclear | Home care | 694 | Hospital staysf | 53.6% (228/425) | 65.4% (176/269) | 0.82 (0.72, 0.93) | Home care? | |
| CI: confidence interval; RR: risk ratio. | ||||||||
| aNumber admitted to hospital at least once. | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Number of patients with a hospital admission Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

