Tipos de trócar en la laparoscopia
Información
- DOI:
- https://doi.org/10.1002/14651858.CD009814.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 16 diciembre 2015see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Ginecología y fertilidad
- Copyright:
-
- Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
CC contributed to the conception of the review, co‐ordinated the review, wrote to authors of papers for additional information and worked on the data management.
CC and HS together designed and drafted the review, collected data for the review, organised retrieval of papers, screened the retrieved papers, appraised the quality of the papers, extracted the data of the papers, obtained and screened data on unpublished studies, entered data into Review Manager 5, analysed and interpreted the data and wrote the review.
SMR contributed to the conception and designing of the review, helped in providing a methodological perspective, helped with the interpretation of data and critically revised the draft review.
MW and CC together designed search strategies.
MW undertook the searches (in consultation with the Trials Search Co‐ordinator of the Cochrane Gynaecology and Fertility Group, Marian Showell).
FWJ contributed to the conception and design of the review, helped interpreting the data, provided a clinical and consumer perspective and critically reviewed the draft review.
BWM contributed to the conception of the review and critically reviewed the draft review.
All authors approved the final version of the review.
Sources of support
Internal sources
-
None, Other.
External sources
-
None, Other.
Declarations of interest
The authors do not have any potential conflicts of interest.
Acknowledgements
The review authors thank the members and reviewers of the Editorial Board of the Cochrane Gynaecology and Fertility Group (formerly Menstrual Disorders and Subfertility Group) for constructive comments on the protocol of this review, Ms Marian Showell for her assistance with the development of search strategies and Ms Helen Nagels for her assistance in managing the review process.
Version history
| Published | Title | Stage | Authors | Version |
| 2015 Dec 16 | Trocar types in laparoscopy | Review | Claire F la Chapelle, Hilko A Swank, Monique E Wessels, Ben Willem J Mol, Sidney M Rubinstein, Frank Willem Jansen | |
| 2012 Apr 18 | Trocar types in laparoscopy | Protocol | Claire F la Chapelle, Hilko A. Swank, Monique E Wessels, Ben Willem J Mol, Sidney M Rubinstein, Frank Willem Jansen | |
Differences between protocol and review
We used a fixed‐effect model for meta‐analysis of dichotomous data.
We have added three subgroups: primary entry technique, secondary entry technique and differing trocar diameter.
We removed the planned sensitivity analysis where eligibility would be restricted to studies on bariatric surgery.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Patient Safety;
- Abdominal Injuries [etiology];
- Equipment Design [adverse effects];
- Hernia, Abdominal [etiology];
- Laparoscopy [adverse effects, *instrumentation];
- Pain, Postoperative [prevention & control];
- Randomized Controlled Trials as Topic;
- Surgical Instruments [*adverse effects];
- Vascular System Injuries [*etiology];
- Viscera [*injuries];
Medical Subject Headings Check Words
Humans;
PICO
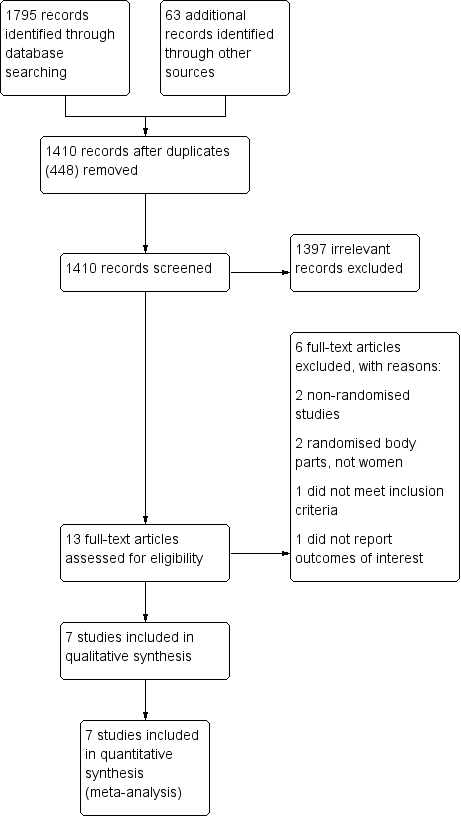
Study flow diagram.

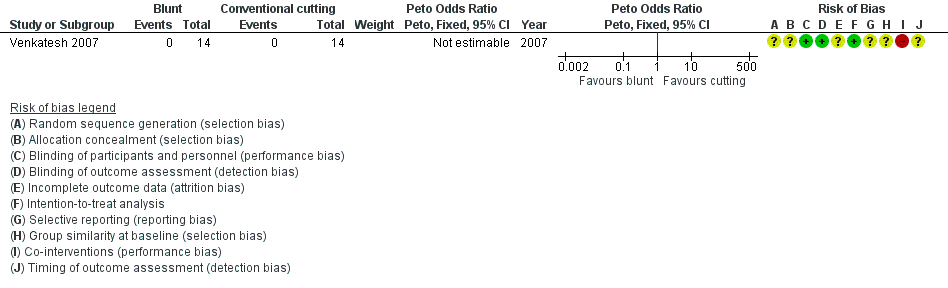
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

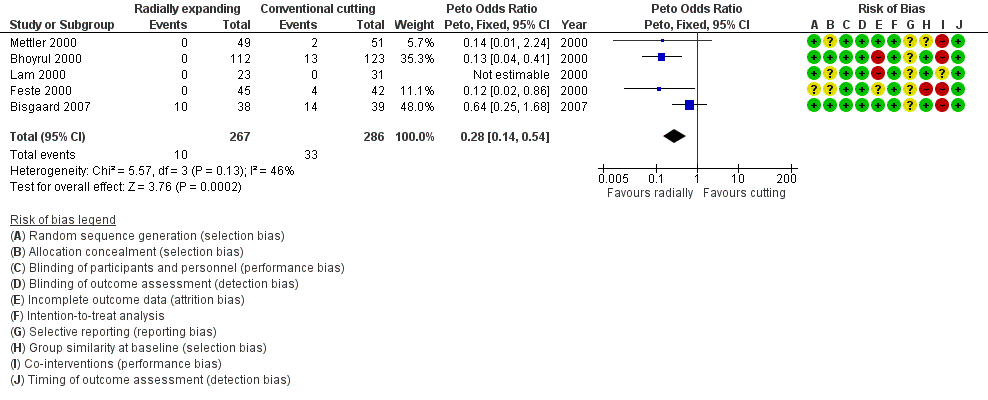
Forest plot of comparison: 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, outcome: 1.3 Trocar site herniation.
Forest plot of comparison: 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, outcome: 1.4 Trocar site bleeding.

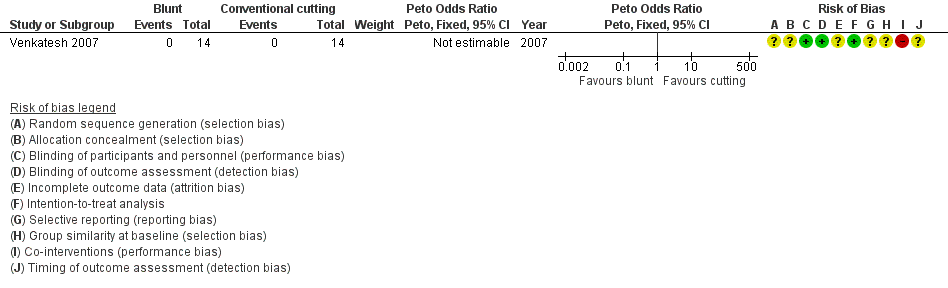
Forest plot of comparison: 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, outcome: 1.5 Trocar site haematoma.

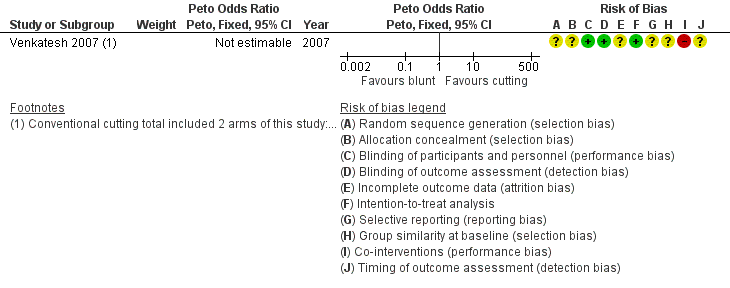
Forest plot of comparison: 2 Conical blunt‐tipped trocar versus cutting trocar for secondary port entry, outcome: 2.1 Visceral injury.

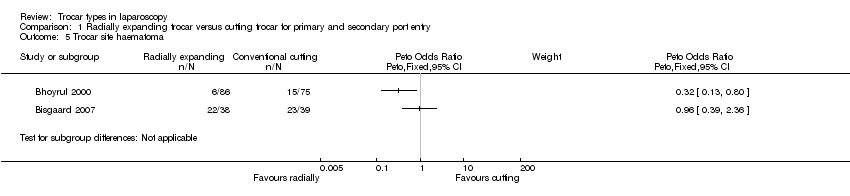
Forest plot of comparison: 2 Conical blunt‐tipped trocar versus cutting trocar for secondary port entry, outcome: 2.2 Vascular injury.
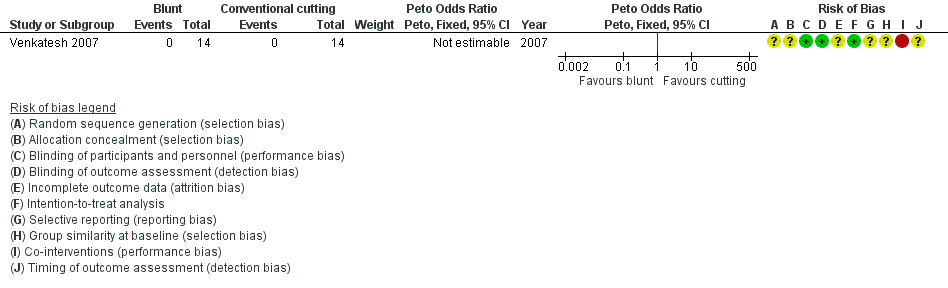
Forest plot of comparison: 2 Conical blunt‐tipped trocar versus cutting trocar for secondary port entry, outcome: 2.3 Trocar site herniation.
Forest plot of comparison: 3 Radially expanding trocar versus conical blunt‐tipped trocar for secondary port entry, outcome: 3.1 Visceral injury.

Forest plot of comparison: 3 Radially expanding trocar versus conical blunt‐tipped trocar for secondary port entry, outcome: 3.2 Vascular injury.
Forest plot of comparison: 4 Single‐bladed trocar versus pyramidal‐bladed trocar, outcome: 4.1 Visceral injury.
Forest plot of comparison: 4 Single‐bladed trocar versus pyramidal‐bladed trocar, outcome: 4.2 Vascular injury.

Comparison 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, Outcome 1 Visceral injury.

Comparison 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, Outcome 2 Vascular injury.

Comparison 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, Outcome 3 Trocar site herniation.

Comparison 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, Outcome 4 Trocar site bleeding.
Comparison 1 Radially expanding trocar versus cutting trocar for primary and secondary port entry, Outcome 5 Trocar site haematoma.

Comparison 2 Conical blunt‐tipped trocar versus cutting trocar for secondary port entry, Outcome 1 Visceral injury.
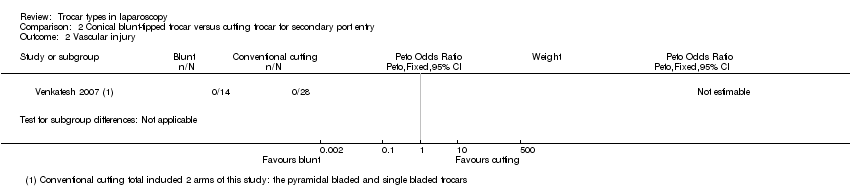
Comparison 2 Conical blunt‐tipped trocar versus cutting trocar for secondary port entry, Outcome 2 Vascular injury.
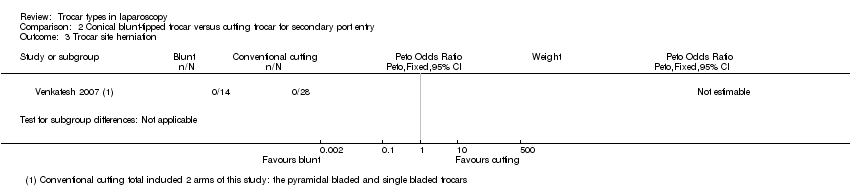
Comparison 2 Conical blunt‐tipped trocar versus cutting trocar for secondary port entry, Outcome 3 Trocar site herniation.
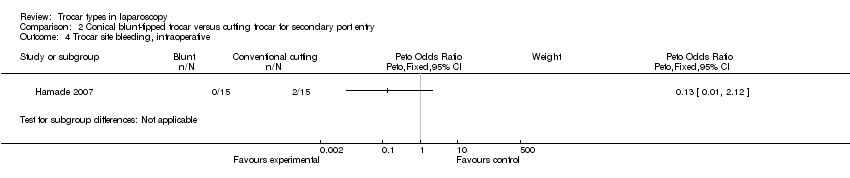
Comparison 2 Conical blunt‐tipped trocar versus cutting trocar for secondary port entry, Outcome 4 Trocar site bleeding, intraoperative.

Comparison 3 Radially expanding trocar versus conical blunt‐tipped trocar for secondary port entry, Outcome 1 Visceral injury.

Comparison 3 Radially expanding trocar versus conical blunt‐tipped trocar for secondary port entry, Outcome 2 Vascular injury.
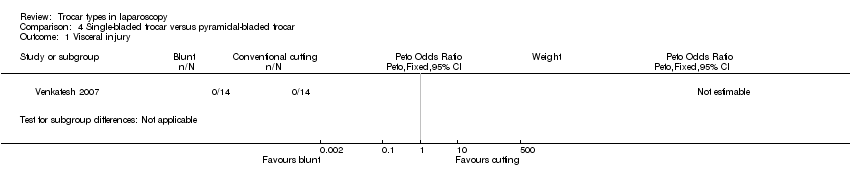
Comparison 4 Single‐bladed trocar versus pyramidal‐bladed trocar, Outcome 1 Visceral injury.
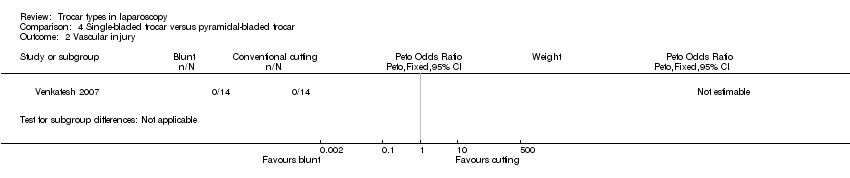
Comparison 4 Single‐bladed trocar versus pyramidal‐bladed trocar, Outcome 2 Vascular injury.
| Radially expanding trocars compared to cutting trocars for laparoscopy | ||||||
| Patient or population: people undergoing laparoscopy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Cutting trocars | Radially expanding trocars | |||||
| Visceral injury | 4 per 1000 | 4 per 1000 | OR 0.95 | 473 | ⊕⊝⊝⊝ | ‐ |
| Vascular injury | 4 per 1000 | 1 per 1000 | OR 0.14 | 473 | ⊕⊝⊝⊝ | ‐ |
| Trocar site herniation | No events reported | No events reported | Not estimable3 | 463 | ⊕⊝⊝⊝ | ‐ |
| Trocar site bleeding | 115 per 1000 | 35 per 1000 | OR 0.28 | 553 | ⊕⊝⊝⊝ | ‐ |
| Trocar site haematoma5 | See comment5 | See comment5 | Not estimable5 | 238 | ⊕⊝⊝⊝ | ‐ |
| Postoperative pain6 | See comment6 | See comment6 | Not estimable6 | 306 | See comment6 | ‐ |
| *The basis for the assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to high risk of attrition bias. | ||||||
| Conical blunt‐tipped trocar compared to cutting trocar for laparoscopy | ||||||
| Patient or population: people undergoing laparoscopy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Cutting trocar | Conical blunt‐tipped trocar | |||||
| Visceral injury | No events reported | No events reported | Not estimable1 | 42 | ⊕⊝⊝⊝ | ‐ |
| Vascular injury | No events reported | No events reported | Not estimable1 | 42 | ⊕⊝⊝⊝ | ‐ |
| Trocar site bleeding | 133 per 1000 | 20 per 1000 | OR 0.13 | 30 | ⊕⊝⊝⊝ | ‐ |
| Postoperative pain5 | See comment5 | See comment5 | Not estimable5 | 42 | ⊕⊝⊝⊝ | ‐ |
| *The basis for the assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 No events reported. | ||||||
| Radially expanding trocar compared to conical blunt‐tipped trocar for laparoscopy | ||||||
| Patient or population: people undergoing laparoscopy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Conical blunt‐tipped trocar | Radially expanding trocar | |||||
| Visceral injury | No events reported | No events reported | Not estimable1 | 28 | ⊕⊝⊝⊝ | ‐ |
| Vascular injury | No events reported | No events reported | Not estimable1 | 28 | ⊕⊝⊝⊝ | ‐ |
| Trocar site herniation | No events reported | No events reported | Not estimable1 | 28 | ⊕⊝⊝⊝ | ‐ |
| *The basis for the assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 No events reported. | ||||||
| Single‐bladed trocar compared to pyramidal‐bladed trocar for laparoscopy | ||||||
| Patient or population: people undergoing laparoscopy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Pyramidal‐bladed trocar | Single‐bladed trocar | |||||
| Visceral injury | No events reported | No events reported | Not estimable1 | 28 | ⊕⊝⊝⊝ | ‐ |
| Vascular injury | No events reported | No events reported | Not estimable1 | 28 | ⊕⊝⊝⊝ | ‐ |
| Trocar site herniation | No events reported | No events reported | Not estimable1 | 28 | ⊕⊝⊝⊝ | ‐ |
| *The basis for the assumed risk is the mean control group risk across studies. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 No events reported. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Visceral injury Show forest plot | 4 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2 Vascular injury Show forest plot | 4 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 3 Trocar site herniation Show forest plot | 4 | 463 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Trocar site bleeding Show forest plot | 5 | 553 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.28 [0.14, 0.54] |
| 5 Trocar site haematoma Show forest plot | 2 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Visceral injury Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2 Vascular injury Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 3 Trocar site herniation Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 4 Trocar site bleeding, intraoperative Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Visceral injury Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2 Vascular injury Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Visceral injury Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2 Vascular injury Show forest plot | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |

