آسپیراسیون و اسکلروتراپی در مقابل هیدروسلکتومی در درمان هیدروسل
چکیده
پیشینه
هیدروسلها (hydrocoele) ناهنجاریهای شایع کیستیک کیسه بیضه یا اسکروتوم (scrotum) هستند، که به صورت تجمع پر از مایع میان لایههای احشایی و جداری تونیکا واژینالیس (tunica vaginalis) اسکروتوم توصیف میشود. دو روش برای درمان هیدروسل وجود دارد: هیدروسلکتومی (hydrocoelectomy) با جراحی باز و آسپیراسیون و به دنبال آن اسکلروتراپی (sclerotherapy).
اهداف
فواید و مضرات آسپیراسیون و اسکلروتراپی را در مقابل هیدروسلکتومی برای مدیریت درمانی هیدروسل مقایسه کردیم.
روشهای جستوجو
از طریق برقراری ارتباط با هماهنگکننده جستوجوی کارآزماییها و با استفاده از واژگان و اصطلاحات جستوجوی مرتبط با این مرور، پایگاه ثبت تخصصی گروه کلیه و پیوند در کاکرین را تا تاریخ 2 آگوست 2014 جستوجو کردیم.
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترلشده (randomised controlled trials; RCTs) و شبه‐RCTهایی که آسپیراسیون و اسکلروتراپی را در مقابل هیدروسلکتومی برای مدیریت درمانی هیدروسلها مقایسه کردند.
گردآوری و تجزیهوتحلیل دادهها
دو نویسنده بهطور مستقل از هم دادهها را استخراج کرده و خطر سوگیری (bias) را در مطالعات واردشده ارزیابی کردند. متاآنالیز اثرات تصادفی (random effects) با استفاده از نسبت خطر (relative risk; RR) برای پیامدهای دو حالتی (dichotomous outcome) و تفاوتهای میانگین (MD) برای پیامدهای پیوسته (continuous outcome)، با 95% فواصل اطمینان (CI)، اجرا شدند.
نتایج اصلی
چهار مطالعه کوچک را پیدا کردیم که معیارهای ورود را داشتند. این مطالعات 275 بیمار را با 282 هیدروسل مورد بررسی قرار دادند. شرکتکنندگان برای دریافت آسپیراسیون و اسکلروتراپی (155 بیمار با 159 هیدروسل) و جراحی (120 بیمار با 123 هیدروسل) تصادفیسازی شدند. همه مطالعات با خطر پائین یا نامشخص برای سوگیری انتخاب (selection bias)، سوگیری تشخیص (detection bias)، سوگیری ریزش نمونه (attrition bias) و سوگیری گزارشدهی انتخابی (selective reporting) ارزیابی شدند. کورسازی (blinding) برای شرکتکنندگان و محققین بر اساس نوع مداخلات امکانپذیر نبود. کورسازی متخصصان آمار در هیچ یک از مطالعات واردشده گزارش نشد.
تفاوت معنیداری در درمان بالینی بین دو گروه وجود نداشت (3 مطالعه، 215 شرکتکننده: RR: 0.45؛ 95% CI؛ 0.18 تا 1.10)، با این حال ناهمگونی (heterogeneity) قابل توجهی وجود داشت (I² = 95%). در بررسی بیشتر، یک مطالعه ایجادکننده همه ناهمگونیها بود. این مساله میتواند به دلیل عامل مورد استفاده یا شاید به این دلیل باشد که این مطالعه بسیار قدیمیتر از دو مطالعه دیگر موجود در این آنالیز است. هنگامی که مطالعه مذکور از آنالیز حذف شد، ناهمگونی 0% شد و نتیجه قابل توجه بود (به نفع جراحی) (2 مطالعه، 136 شرکتکننده: RR: 0.74؛ 95% CI؛ 0.64 تا 0.85). در افرادی که اسکلروتراپی دریافت کردند، در مقایسه با جراحی، افزایش قابل توجهی در عود دیده شد (3 مطالعه، 196 شرکتکننده: RR: 9.37؛ 95% CI؛ 1.83 تا 48.4). یک مطالعه، کاهش غیرقابل توجهی را در تب در گروه اسکلروتراپی گزارش کرد (60 شرکتکننده: RR: 0.25؛ 95% CI؛ 0.06 تا 1.08). تعداد عفونتها در گروه جراحی افزایش یافت، اما این افزایش از نظر آماری معنیدار نبود (4 مطالعه، 275 شرکتکننده: RR: 0.31؛ 95% CI؛ 0.09 تا 1.05؛ I² = 0%). سه مطالعه گزارش کردند که فراوانی درد در گروه جراحی بیشتر از گروه آسپیراسیون و اسکلروتراپی بود، اما به دلیل استفاده از ابزارهای اندازهگیری متفاوت در این مطالعات، نتوانستیم نتایج را با هم ترکیب کنیم. بهبودی بیمار از نظر رادیولوژیکی در هیچ یک از مطالعات واردشده گزارش نشد. تفاوت معنیداری در تشکیل هماتوم میان دو گروه وجود نداشت (3 مطالعه، 189 شرکتکننده: RR: 0.57؛ 95% CI؛ 0.17 تا 1.90؛ I² = 0%). فقط یک مطالعه رضایت بیمار را در سه و شش ماه گزارش کرد؛ تفاوت معنیداری میان دو گروه دیده نشد.
نتیجهگیریهای نویسندگان
عوارض پس از جراحی و همچنین هزینه و زمان لازم برای از سرگیری کار در گروه آسپیراسیون و اسکلروتراپی کمتر بود؛ اما به بهای میزان عود بیشتر. نرخ بهبودی در پیگیری کوتاهمدت میان گروهها مشابه بود، با این حال، به دلیل ناهمگونی بالا، عدم قطعیت قابلتوجهی در این نتیجه وجود دارد. نیاز زیادی به انجام RCTهای دقیق از نظر روششناسی (methodology) وجود دارد که اثربخشی انواع مختلف عوامل اسکلروز کننده، غلظت محلول اسکلروز کننده و حجم تزریق را برای درمان هیدروسلها ارزیابی کنند. مهم است که RCTها حجم نمونه به اندازه کافی بزرگ و دوره پیگیری طولانی داشته باشند. مطالعات میبایست پیامدهای بالینی را مانند درد، عود، رضایت از درمان، عوارض و درمان را با استفاده از ابزارهای معتبر ارزیابی کنند. پروتکلهای همه مطالعات میبایست در پایگاههای ثبت کارآزمایی بالینی ثبت شده و گزارشهای این مطالعات با دستورالعملهای بالینی بینالمللی گزارشدهی از کارآزمایی مانند CONSORT مطابقت داشته باشند. مطالعات میبایست به مقرون به صرفه بودن روشها نیز بپردازند.
خلاصه به زبان ساده
آسپیراسیون و اسکلروتراپی در مقابل هیدروسلکتومی در درمان هیدروسل
هیدروسلها ناهنجاریهای شایع کیستیک کیسه بیضه یا اسکروتوم هستند، که به صورت تجمع پر از مایع در اطراف بیضهها توصیف میشوند. هیدروسل را میتوان با تخلیه مایع همراه با تزریق یک ماده شیمیایی در اطراف بیضه، به منظور پیشگیری از عود، یا با جراحی باز درمان کرد. هدف این مرور مقایسه این دو روش درمان است. پس از جستوجوی گسترده در متون علمی، چهار مطالعه کوچک شناسایی شدند. با توجه به اطلاعات محدود موجود در مورد طراحی مطالعات، و تعداد اندک بیماران، نتایج باید با احتیاط تفسیر شوند. متاآنالیز، نرخ کمتری را از عود در گروه جراحی نشان داد، با این حال، شواهد کافی برای نتیجهگیری قوی وجود نداشت. عوارض پس از جراحی مانند عفونت و تب، همچنین هزینه درمان و زمان شروع مجدد کار، در گروه آسپیراسیون و اسکلروتراپی کمتر بودند، اما به بهای نرخ عود بیشتر. نرخ درمان در پیگیری کوتاهمدت میان گروهها مشابه بود، اما عدم قطعیت قابل توجهی در این نتیجه وجود دارد که ممکن است به دلیل قدیمی بودن یکی از مطالعات و عامل استفادهشده متفاوت در آن در مقایسه با دیگر مطالعات، باشد.
Authors' conclusions
Background
Description of the condition
Hydrocoeles are common cystic scrotal abnormalities, described as a fluid‐filled collection between the visceral and parietal layers of the tunica vaginalis of the scrotum. Hydrocoeles are responsible for most painless scrotal swellings (Micallef 2000). These masses are either congenital or acquired, and can present in any age group, from neonates to the elderly (Epstein 1988). Accumulation of fluid resulting from communication between the tunica vaginalis and the peritoneal cavity leads to formation of congenital hydrocoeles. Acquired hydrocoeles are most commonly idiopathic, although they can occur secondary to intrascrotal infections, regional or systemic diseases, inguinal or scrotal surgery, or neoplasms (Rubenstein 2004). The prevalence of idiopathic hydrocoele in adult male population is unclear but some experts reported the incidence of hydrocoele to be 1% in adult male population in USA (Rudkin 2012).
Description of the intervention
Although most hydroceles do not require therapeutic intervention, two approaches are common in practice. Surgical open hydrocoelectomy is considered to be the current therapeutic standard (Beiko 2003; Epstein 1988). An alternative approach is percutaneous aspiration followed by sclerotherapy. Aspiration without sclerotherapy carries a significant risk of hydrocoele recurrence (Roosen 1991).
How the intervention might work
Aspiration and sclerotherapy for the management of hydrocoeles involves aspirating the hydrocoele and then injecting a sclerosing solution into the hydrocoele sac. This solution fuses the visceral and parietal layers of the tunica vaginalis, obliterating the potential space for reformation of the hydrocoele (Moloney 1975; Shan 2003).
Why it is important to do this review
When treating hydrocoeles, physicians should consider issues such as success rate, morbidity, costs to patient, health care system, community and patient satisfaction. Although surgical open hydrocoelectomy has been done successfully since the 1970s and is considered as standard treatment, few published studies have reported absolute cure rates and complications following this procedure (Shan 2003).
Sclerotherapy, a minimally invasive approach used to treat hydrocoeles, evolved from demand and need for less aggressive surgical approaches. Successful sclerotherapy may avoid the need for surgery to treat hydrocoeles. Various sclerosing agents have been used in the management of hydrocoeles, including antazoline (Roosen 1991), tetracycline (Levin 1988), ethanolamine oleate (Tammela 1992), adhesive fibrin glue (Sirpa 1998), talc (Yilmaz 1998), blood, rifampin (Yilmaz 2000), polidocanol (Sigurdsson 1994), OK‐432 (Yamamoto 1994), phenol (Savion 1989), and sodium tetradecyl sulphate (Beiko 2003; Fracchia 1998; Stattin 1996). A number of sclerotherapy techniques have been used, and a variety of definitions of success applied in studies. The results of studies on sclerotherapy are therefore inconsistent and variable success rates from 33% to 100% have been reported for the same sclerosing agent (Fracchia 1998; Hu 1984; Levin 1988; Ozkan 1990).
Objectives
We compared the benefits and harms of aspiration and sclerotherapy versus hydrocoelectomy for the management of hydrocoeles.
Methods
Criteria for considering studies for this review
Types of studies
We included all reports of randomised controlled trials (RCTs) and quasi‐RCTs (studies in which allocation to treatment was obtained by alternation, use of date of birth, alternate medical records, or other predictable methods). There was no limitation in terms of language of publication or the date of the study.
Types of participants
We included men and boys over 14 years of age with primary hydrocoele. The diagnosis of hydrocoele was based on physical examination or ultrasonography. We excluded studies that included men and boys with recurrent hydrocoele, congenital hydrocoele, communicating hydrocoele (associated with inguinal hernia) and secondary hydrocoele due to scrotal pathologies (infections and malignancies), varicocoele surgery, scrotal surgery and scrotal trauma. We excluded patients who underwent sclerotherapy after hydrocoelectomy and vice‐versa.
Types of interventions
We included reports of studies that compared the effects of aspiration and sclerotherapy with any type of sclerosants (e.g. antazoline, tetracycline, rifampin, sodium tetradecyl sulphate) versus hydrocoelectomy.
Types of outcome measures
-
Single surgery versus single sclerotherapy
-
Single surgery versus two rounds of sclerotherapy and
-
Single surgery versus three rounds of sclerotherapy.
Primary outcomes
-
Clinical cure: absence of hydrocoele on postoperative clinical assessment
-
Radiological cure: absence of hydrocoele on postoperative ultrasound
-
Recurrence: the accumulation of hydrocoele on postoperative ultrasound or clinical assessment, or both, that required re‐intervention after three months of surgery or sclerotherapy
-
Postoperative complications
-
Fever: oral temperature more than 38°C
-
Acute pain: scrotal pain 48 h after intervention (pain should be assessed using the visual analogue scale (VAS; 0 = no pain; 10 = worst pain imaginable)
-
Chronic pain: scrotal pain at follow‐up more than two days after intervention (pain should be assessed using the visual analogue scale (VAS; 0 = no pain; 10 = worst pain imaginable)
-
Infection: the presence of either positive microbial culture from wound discharge, or a combination of fever, pain, local redness and discharge at the incision site
-
Other complications including haematocoele, oedema, haematoma: based on physician reports in studies.
-
Secondary outcomes
-
Length of hospital stay
-
Return to normal activities
-
Total cost: addition of all intervention costs, cost of hospitalisation, drugs and materials. Loss of working days was not be including in the total cost. If possible, we provided a cost‐effectiveness analysis
-
Patient satisfaction in terms of: decrease in hydrocoele size, relief from any hydrocoele‐related disability, and satisfaction with the overall experience and results of the procedure
-
Spermogram result: semen volume (mL), concentration (million/mL), motility and morphology.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Renal Group's Specialised Register (to 2 August 2014) through contact with the Trials' Search Co‐ordinator using search terms relevant to this review. The Cochrane Renal Group’s Specialised Register contains studies identified from the following sources.
-
Quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL)
-
Weekly searches of MEDLINE OVID SP
-
Handsearching of renal‐related journals and the proceedings of major renal conferences
-
Searching of the current year of EMBASE OVID SP
-
Weekly current awareness alerts for selected renal journals
-
Searches of the International WHO ICTRP search portal and ClinicalTrials.gov.
Studies contained in the Specialised Register are identified through search strategies for CENTRAL, MEDLINE, and EMBASE based on the scope of the Cochrane Renal Group. Details of these strategies, as well as a list of handsearched journals, conference proceedings and current awareness alerts, are available in the specialised register section of information about the Cochrane Renal Group.
See Appendix 1 for search terms used in strategies for this review.
Searching other resources
-
Reference lists of nephrology textbooks, clinical practice guidelines, review articles and relevant studies
-
Citation tracking of identified RCTs and reviews using Science Citation Index
-
Letters seeking information about unpublished or incomplete studies to investigators known to be involved in previous studies.
Data collection and analysis
Selection of studies
The search strategy was applied to identify all studies relevant to the review. Two authors independently screened titles and if necessary reviewed the full text and provided detailed descriptions of the included and excluded articles. Disagreement was resolved by discussion, and a third author arbitrated if necessary.
Data extraction and management
Data were extracted independently by two authors using a self‐developed data extraction form. Studies reported in non‐English language journals were translated before assessment. If more than one publication on each study were identified, reports were grouped together and the most recent or most complete report was included in the meta‐analyses. Where data from a study was conflicted or insufficient, authors were contacted to request further information. Relevant information obtained in this manner was included in the analysis. Disagreement was resolved by discussion, or consulting a third author if necessary.
Assessment of risk of bias in included studies
Two authors independently assessed the risk of bias in the selected studies based on articles’ full text. Disagreements was resolved with a third author (Higgins 2011) (see Appendix 2).
-
Was there adequate sequence generation (selection bias)?
-
Was allocation adequately concealed (selection bias)?
-
Was knowledge of the allocated interventions adequately prevented during the study (detection bias)?
-
Participants and personnel
-
Outcome assessors
-
-
Were incomplete outcome data adequately addressed (attrition bias)?
-
Are reports of the study free of suggestion of selective outcome reporting (reporting bias)?
-
Was the study apparently free of other problems that could put it at a risk of bias?
Measures of treatment effect
For dichotomous outcomes (e.g. cure, fever, patient satisfaction) results were expressed as risk ratio (RR) with 95% confidence intervals (CI). Where continuous scales of measurement are used to assess the effects of treatment (e.g. pain, length hospital stay, cost) the mean difference (MD) was used, or the standardised mean difference (SMD) if different scales were used.
Unit of analysis issues
Cross‐over studies were not included because this study design was not consistent with outcomes related to the treatment of hydrocoeles.
Dealing with missing data
Any further information required from the original author was requested by written correspondence and any relevant information obtained in this manner was included in the review. Evaluation of important numerical data such as screened, randomised patients as well as intention‐to‐treat (ITT), as‐treated and per‐protocol (PP) population were carefully performed. Attrition rates, for example drop‐outs, losses to follow‐up and withdrawals were investigated. Issues of missing data and imputation methods (for example, last‐observation‐carried‐forward (LOCF)) were critically appraised (Higgins 2011).
Assessment of heterogeneity
Heterogeneity was analysed using a Chi² test on N‐1 degrees of freedom, with an alpha of 0.05 used for statistical significance and with the I² test (Higgins 2003). I² values of 25%, 50% and 75% correspond to low, medium and high levels of heterogeneity. We assessed the potential sources of clinical heterogeneity by exploring clinical and methodological characteristics of these studies (e.g. differences in study quality, participants, intervention, or outcome assessment).
Assessment of reporting biases
We planned to construct funnel plots to assess for the potential existence of small study bias (Higgins 2011). This was not possible due to the small number of studies identified.
Data synthesis
We pooled all primary and secondary outcomes data using the random‐effects model. The fixed‐effect model was also to be used to ensure robustness of the model chosen and susceptibility to outliers, however due to the small number of studies identified this was not done.
Subgroup analysis and investigation of heterogeneity
We planned to perform the following subgroup analyses.
-
Intervention: e.g. different kinds of sclerosant agents
-
Study quality: e.g. RCTs and quasi‐RCTs.
If possible, the risk difference with 95% CI was to be calculated for each adverse effect, either compared with no treatment or another agent; this was not done.
Sensitivity analysis
We planned to perform the following sensitivity analyses in order to explore the influence of the following factors on effect size, however due to the small number of studies identified this was not done.
-
Repeating the analysis excluding unpublished studies
-
Repeating the analysis taking into account the risk of bias, as specified above
-
Repeating the analysis excluding in large studies to establish the degree of their impact on the results
-
Repeating the analysis excluding studies using the following filters: diagnostic criteria; language of publication; source of funding (industry versus other); and country.
Results
Description of studies
Results of the search
After searching the Cochrane Renal Group's Specialised Register we identified seven potentially relevant studies. Reference and citation tracking identified seven additional studies. We identified two additional potentially relevant studies after contact with experts and investigators in order to seek published and unpublished studies. After reviewing titles and abstracts, we excluded four studies. The full text of the remaining 12 studies were retrieved, and eight were excluded. These selection process resulted in four small studies that met our inclusion criteria (Agrawal 2009a; Khaniya 2009; Latif 2008; Osman 1994) (Figure 1).

Study selection flow diagram.
Included studies
Authors of the four included studies were contacted for clarification regarding methodology and some missing data, however no further information was received. These studies included 275 patients with 282 hydroceles. The patients were randomised to aspiration and sclerotherapy (155 patients; 159 hydroceles) and surgery (120 patients; 123 hydroceles). The types of sclerosant agent, dose and frequency of treatments varied among the studies. Khaniya 2009 and Latif 2008 used sodium tetradecyl sulphate, Osman 1994 used tetracycline, and Agrawal 2009a used phenol and polidocanol as sclerosant agents in two separate groups. The characteristics of the methods, populations, interventions and outcomes in the included studies are reported in the Characteristics of included studies.
Excluded studies
We excluded four studies based on titles and abstracts. Eight studies were excluded after review of the full text. The reasons for exclusion were that the studies were not randomised (5); they enrolled the wrong population (1), or they investigated the wrong intervention (2) (see Characteristics of excluded studies).
Risk of bias in included studies
Details are available for each study in Characteristics of included studies, Figure 2 and Figure 3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Randomisation was by computer random number generator in Khaniya 2009. The method of randomisation was unclear in other three studies. Allocation concealment was unclear in all included studies.
Blinding
Blinding was not possible for participants and investigators based on the type of interventions. Blinding for statisticians was not reported in any of the included studies.
Incomplete outcome data
Included studies had short follow‐up time, therefore the loss to follow‐up was not a significant problem in two included studies (Agrawal 2009a; Latif 2008). In Khaniya 2009 there were some missing data regarding patient satisfaction. The risk of attrition bias was unclear in Osman 1994.
Selective reporting
The protocols of the included studies were not available, therefore judgement was not possible.
Other potential sources of bias
There were insufficient data to permit judgment.
Effects of interventions
Primary outcomes
Clinical cure
Three studies (Agrawal 2009a; Latif 2008; Osman 1994) reported clinical cure after single sclerotherapy versus surgery. There was no significant difference in clinical cure between the two treatment groups (Analysis 1.1.1 (3 studies, 215 participants): RR 0.45, 95% CI 0.18 to 1.10). Significant heterogeneity was seen between the studies (Chi² = 38.12, P < 0.00001, I² = 95%). On further investigation Osman 1994 contributed all of the heterogeneity ‐ this could be due to the agent used or perhaps due to the fact that this is a much older study than the other two studies included in this analysis. When this study was removed from the analysis the heterogeneity was 0% and the result was significant (in favour of surgery) (Analysis 1.1.3 (2 studies, 136 participants): RR 0.74; 95% CI 0.64 to 0.85).
Recurrence
Three studies (Khaniya 2009; Latif 2008; Osman 1994) reported recurrence as an outcome. Osman 1994 assessed recurrence at the sixth month follow‐up, and in Khaniya 2009 and Latif 2008 recurrence was evaluated at three months after the intervention. Ignoring these assessment times, pooling results there was a significant increase in recurrence in the sclerotherapy group compared with surgical group (Analysis 1.2 (3 studies, 189 participants): RR 9.43, 95% CI 1.82 to 48.77). Heterogeneity was moderate (Chi² = 4.60, P = 0.10, I² = 56%). The two studies assessing recurrence at three months also showed a significant increase in the rate of recurrence with sclerotherapy compared with surgery (Analysis 1.2.1 (2 studies, 110 participants): RR 5.26, 95% CI 1.04 to 26.75). There was no significant heterogeneity (Chi² = 1.48, P = 0.22, I² = 33%).
Fever
Khaniya 2009 reported a non‐significant decrease in fever in the sclerotherapy group (Analysis 1.3 (1 study, 60 participants): RR 0.25, 95% CI 0.06 to 1.08).
Infection
All four studies reported post intervention infection rates. There was an increased number of infections in the surgery group however this increase was not statistically significant (Analysis 1.4 (4 studies, 275 participants): RR 0.31, 95% CI 0.09 to 1.05; I² = 0%).
Haematoma
Three studies (Khaniya 2009; Latif 2008; Osman 1994) compared haematoma formation as an adverse event. There was no significant difference between the two groups (Analysis 1.5 (3 studies, 189 participants): RR 0.57, 95% CI 0.17 to 1.90; I² = 0%).
Radiological cure
This outcome was not reported in any of the included studies.
Postoperative pain
This outcome was not assessed using the VAS in the included studies. Latif 2008 and Khaniya 2009 reported postoperative pain as dichotomous data, while Osman 1994 reported this outcome in three grades (mild, moderate and severe) but did not define these categories. These studies reported the frequency of pain in the surgery group was higher than aspiration and sclerotherapy group but because of different measurement tools applied in these studies, we did not pool the results.
Secondary outcomes
Time to resumption of work
Khaniya 2009 reported a significantly shorter work absence among those who underwent sclerotherapy (Analysis 1.6 (60 participants): MD ‐5.94 days, 95% CI ‐7.15 to ‐4.73).
Cost
Two studies (Khaniya 2009; Latif 2008) considered cost of treatment for patients. In both studies, cost of sclerotherapy was significantly lower. Khaniya 2009 summarized total cost in groups with median cost: "The cost of treatment (median) of hydrocele was NC Rs 300 (US$4.3) and NC Rs 1527 (US$ 21.8) in the group 1 and 2 respectively (p< 0.001) (1US$ = 70NC Rs)"; while Latif 2008 reported this as an average cost: "Average cost of sclerotherapy was 224 Rupees (125‐350 Rs. Including cost of repeat procedures). The average cost of surgery was Rs. 1663 (Rs.1375 to 1950).". Due to variety of the settings, different cost currency and diversity of reported summary measures, we could not meta‐analyse these studies.
Satisfaction
Khaniya 2009 reported no significant difference in patient satisfaction assessed at three months (Analysis 1.7.1 (48 participants): RR 0.90, 95% CI 0.66 to 1.24) and six months (Analysis 1.7.2 (41 participants): RR 0.72 95% CI 0.51 to 1.02) between the two groups.
Length of hospital stay
Agrawal 2009a, Latif 2008 and Osman 1994 reported that length of hospital stay was significantly lower in the sclerotherapy group compared to the surgery group. These studies did not provide data for this comparison and we could not pool the results.
Spermogram result
This outcome was not reported in any of the included studies.
Fixed‐effect analyses
Due to small number of studies and moderate to high heterogeneity for our primary outcomes, fixed‐effect analyses were not performed.
Subgroup analysis
There were not enough studies to properly investigate planned subgroup analyses.
Sensitivity analysis
No unpublished studies were included, and all studies were published in English. Since the included studies had similar risk of bias and numbers of participants, sensitivity analysis was not performed. All studies used similar diagnostic criteria for detecting patients; there was little variation, and hence, sensitivity analysis was not feasible.
Discussion
Summary of main results
We identified four small studies enrolling 275 patients (282 hydroceles) that met our inclusion criteria (Agrawal 2009a; Khaniya 2009; Latif 2008; Osman 1994). Our results suggest that the short‐term cure rate was not significantly different between surgery and aspiration and sclerotherapy. However recurrence after sclerotherapy was significantly higher than surgical treatment. The included studies did not adequately report their methods, which in turn limits our ability to draw strong conclusions.
Some complications (hematoma and infection) were not significantly different between the two groups. Pain was not assessed using the VAS in the included studies. The variability of measurement tools for pain assessment in the included studies made meta‐analysis impossible. Nevertheless three studies (Khaniya 2009; Latif 2008; Osman 1994) reported the frequency of pain in the surgery group was higher than the aspiration and sclerotherapy group.
Only one study assessed the time to work resumption and two studies considered cost of treatment for patients. Because of diverse settings, different currencies and a variety of reported summary measures, pooling of the results could not be performed, however these studies reported lower absence from work and cost in the sclerotherapy group. Notably, the difference in the cost and absence from work was reported in comparison of single sclerotherapy versus surgery. The recurrence rate after sclerotherapy is higher than surgery and patients needed to repeat the aspiration and sclerotherapy. The necessity of repeating the procedure may lead to an increase in the absence from work and cost, however, these studies did not assess these outcomes.
In one study satisfaction of the patients were assessed and the satisfaction rate was lower in sclerotherapy group. The reason for dissatisfaction in aspiration and sclerotherapy was the high recurrence rate.
Overall completeness and applicability of evidence
The included studies provided data about different type of sclerosant agents, sclerosing solution concentration and injection volume. This may have caused some degree of heterogeneity but we still believe there are still similar enough that could be combined. The results of present review may be generally applicable for similar kinds of sclerosant agents represented in this review.
Quality of the evidence
Our review was based on the results of four small studies. There are three limitations that must be acknowledged and addressed regarding our included studies. First, the relatively small sample size of identified studies and variability in aspiration and sclerotherapy procedure. Included studies used different type of sclerosant agents, sclerosing solution concentration and injection volume. This in turn may have caused some of the heterogeneity seen in this review. Nevertheless we still believe there are still similar enough that could be combined. Second, the included studies had short‐term follow‐up period and did not assess the long term effects of interventions. Thirdly, the methodological aspects of the identified studies were not clear. Our efforts to obtain more information from the authors were not successful; no responses were received. This lack of clarity may affect the reliability of findings.
Potential biases in the review process
The strength of this review is that it is the first systematic review of aspiration and sclerotherapy versus hydrocoelectomy for treating hydrocoeles. Our search strategy was comprehensive and broad and we did not have any restriction in time and language.
Agreements and disagreements with other studies or reviews
Three other studies have compared aspiration and sclerotherapy versus hydrocoelectomy for treating hydrocoeles; one study was not randomised (Beiko 2003) and two studies included patients with recurrent (Roosen 1991) or secondary (Shan 2003) hydrocoeles.
Shan 2003 reported the results of a RCT comparing the safety and effectiveness of sclerotherapy with phenol and surgical treatment for hydrocoele. Of the 33 subjects in sclerotherapy group, 47.5%, 30%, 12.5%, 5% and 2.5% of the hydroceles were cured with one to five injections, respectively. Of the 34 patients in the hydrocelectomy group 97.5% and 2.5% of hydroceles were cured with one and two operations, respectively. They concluded that sclerotherapy with phenol is as efficacious as hydrocelectomy. Also, they noted that the efficacy of a single hydrocelectomy was higher than single round sclerotherapy and it avoided the need for several follow‐up visits. They reported that when follow‐up is difficult, hydrocelectomy was the intervention of choice.
Roosen 1991 reported a RCT comparing aspiration and sclerotherapy versus hydrocoelectomy in men with recurring hydrocoele after single round of aspiration. A total of 76 patients were randomly divided into two groups. One group underwent antazoline sclerotherapy and the other underwent hydrocelectomy. Of the 40 patients treated with antazoline sclerotherapy, 11 were cured after a single round sclerotherapy and 14 patients underwent second round sclerotherapy and 13 were cured. In the surgery group, only 16 patients from 36 patients completed the study and the cure rate was 100%.
Beiko 2003 compared the effects of aspiration and sclerotherapy using sodium tetradecyl sulphate and hydrocoelectomy as first‐line treatment in patients with hydrocoeles; 27 patients with 28 symptomatic hydrocoeles were prospectively enrolled in an aspiration and sclerotherapy protocol. This group was compared with a group of patients who underwent hydrocoelectomy two years before starting of this study. At the end of the study the patient satisfaction was 75% for aspiration and sclerotherapy and 88% for hydrocoelectomy. The overall success rate for aspiration and sclerotherapy was 76% compared with 84% for hydrocelectomy. The complications included oedema, haematoma, wound infection and cellulitis were seen only 8% in the aspiration and sclerotherapy group, but 40% in the surgery group. Comparative costs per procedure showed that surgery was more expensive than aspiration and sclerotherapy ($905 versus $104).
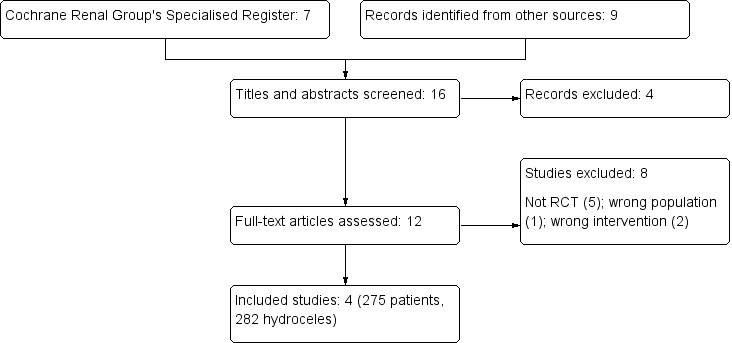
Study selection flow diagram.
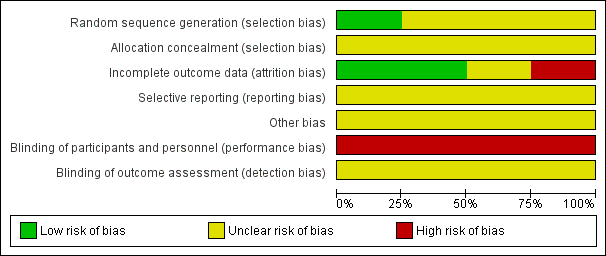
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
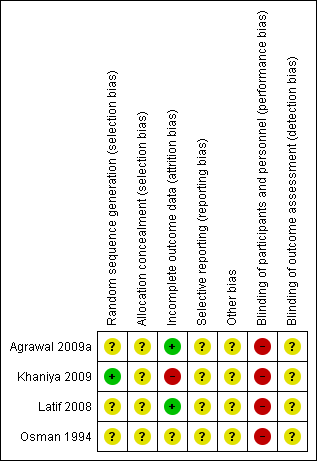
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Aspiration and sclerotherapy versus hydrocoelectomy, Outcome 1 Clinical cure.
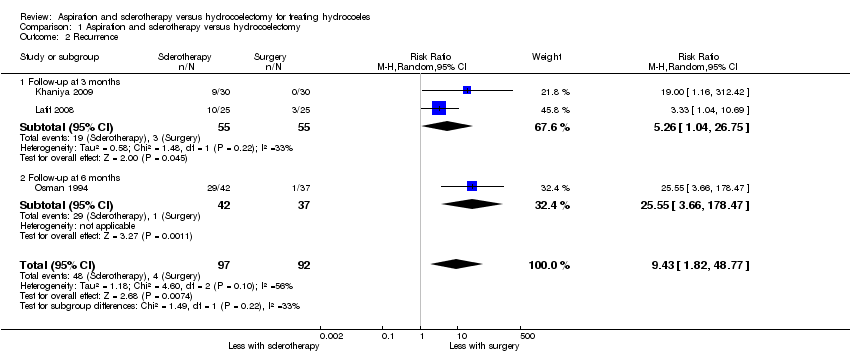
Comparison 1 Aspiration and sclerotherapy versus hydrocoelectomy, Outcome 2 Recurrence.

Comparison 1 Aspiration and sclerotherapy versus hydrocoelectomy, Outcome 3 Fever.

Comparison 1 Aspiration and sclerotherapy versus hydrocoelectomy, Outcome 4 Infection.
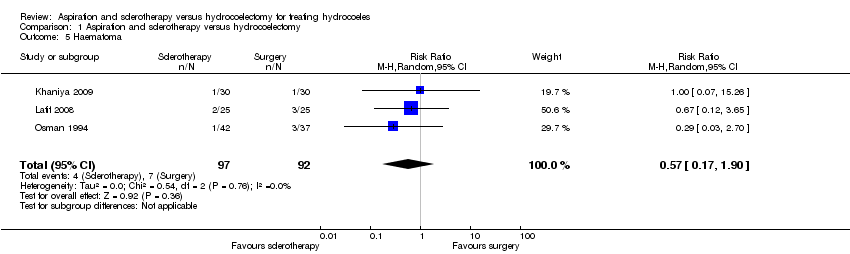
Comparison 1 Aspiration and sclerotherapy versus hydrocoelectomy, Outcome 5 Haematoma.
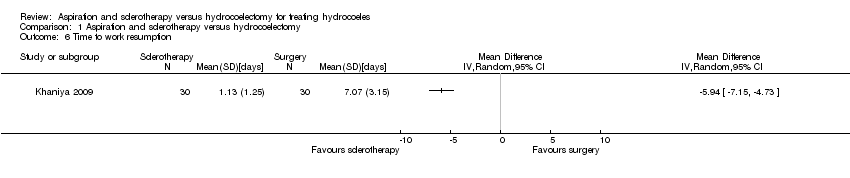
Comparison 1 Aspiration and sclerotherapy versus hydrocoelectomy, Outcome 6 Time to work resumption.
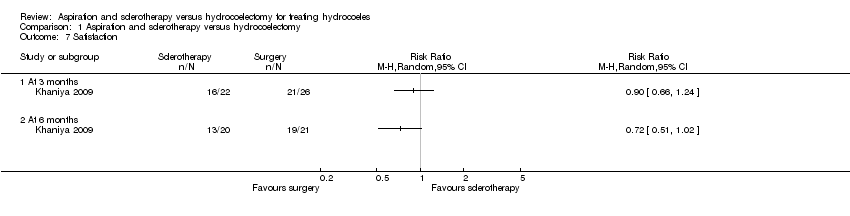
Comparison 1 Aspiration and sclerotherapy versus hydrocoelectomy, Outcome 7 Satisfaction.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical cure Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 One round of sclerotherapy | 3 | 215 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.18, 1.10] |
| 1.2 Two rounds of sclerotherapy | 2 | 129 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.21, 1.65] |
| 1.3 Osman 1994 removed (one round of sclerotherapy) | 2 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.64, 0.85] |
| 2 Recurrence Show forest plot | 3 | 189 | Risk Ratio (M‐H, Random, 95% CI) | 9.43 [1.82, 48.77] |
| 2.1 Follow‐up at 3 months | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 5.26 [1.04, 26.75] |
| 2.2 Follow‐up at 6 months | 1 | 79 | Risk Ratio (M‐H, Random, 95% CI) | 25.55 [3.66, 178.47] |
| 3 Fever Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4 Infection Show forest plot | 4 | 275 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.09, 1.06] |
| 5 Haematoma Show forest plot | 3 | 189 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.17, 1.90] |
| 6 Time to work resumption Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 Satisfaction Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.1 At 3 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 At 6 months | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |

