Fármacos anti‐factor de crecimiento endotelial vascular (FCEV) para el tratamiento de la retinopatía del prematuro
Resumen
Antecedentes
El factor de crecimiento endotelial vascular (FCEV) tiene una influencia clave en la angiogénesis en la vida fetal. Recientemente los investigadores han intentado utilizar los agentes anti‐FCEV para el tratamiento de la retinopatía del prematuro (RP), un trastorno vasoproliferativo. Actualmente existe incertidumbre con respecto a la seguridad y la eficacia de estos agentes en los lactantes prematuros con RP.
Objetivos
Evaluar la eficacia y la seguridad de los fármacos anti‐FCEV cuando se administran como monoterapia, es decir, sin crioterapia o tratamiento con láser concomitantes o en combinación con crioterapia / tratamiento con láser planificados en los lactantes prematuros con RP tipo 1 (definida como zona I cualquier estadio con enfermedad plus, zona I estadio 3 con o sin enfermedad plus o zona II estadio 2 ó 3 con enfermedad plus).
Métodos de búsqueda
Se hicieron búsquedas en el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL 2016, número 1), MEDLINE (1966 hasta 1 enero 2016), EMBASE (1980 hasta 1 enero 2016), CINAHL (1982 hasta 1 enero 2016), en actas de congresos y revisiones anteriores.
Criterios de selección
Ensayos controlados aleatorios o cuasialeatorios que evaluaron la eficacia y la seguridad de la administración, o ambas, de los agentes anti‐FCEV en comparación con tratamiento convencional en los lactantes prematuros con RP.
Obtención y análisis de los datos
Se utilizaron los métodos estándar Cochrane y del Grupo Cochrane de Neonatología para la obtención y el análisis de los datos.
Resultados principales
Tres ensayos con 239 lactantes cumplieron los criterios de inclusión. Dos ensayos compararon bevacizumab intravitreal con tratamiento convencional con láser (monoterapia), mientras que el tercer ensayo comparó pegaptanib intravitreal más tratamiento con láser con láser y crioterapia (tratamiento de combinación) en lactantes con RP tipo 1.
De los dos estudios que evaluaron bevacizumab intravitreal, uno asignó al azar a los lactantes mientras el otro asignó al azar los ojos de los lactantes a los grupos de intervención y control. El primero no informó diferencias en la incidencia de desprendimiento completo o parcial de la retina entre los grupos (143 lactantes; CR 1,04; IC del 95%: 0,21 a 5,13; DR 0,00; IC del 95%: ‐0,06 a 0,07; pruebas de calidad muy baja), pero informó una reducción significativa en el riesgo de defectos de la refracción (miopía muy alta) a los 30 meses de vida (211 ojos; CR 0,06; IC del 95%: 0,02 a 0,20; DR ‐0,40; IC del 95%: ‐0,50 a 0,30; pruebas de calidad baja) y en la recurrencia de la RP a las 54 semanas de edad posmenstrual (143 lactantes; CR 0,22; IC del 95%: 0,08 a 0,62; DR ‐0,20; IC del 95%: ‐0,31 a 0,09; pruebas de calidad moderada) en el grupo bevacizumab. El estudio no encontró diferencias en el riesgo de mortalidad antes del alta hospitalaria (150 lactantes; CR 1,50; IC del 95%: 0,26 a 8,75; DR 0,01; IC del 95%: ‐0,04 a 0,07; pruebas de calidad baja), mortalidad a los 30 meses de vida (150 lactantes; CR 0,86; IC del 95%: 0,30 a 2,45; DR ‐0,01, IC del 95%: ‐0,10 a 0,08; pruebas de calidad baja), opacidad de la córnea que requirió trasplante corneal (286 ojos; CR 0,34; IC del 95%: 0,01 a 8,26; DR ‐0,01, IC del 95%: ‐0,03 a 0,02; pruebas de calidad muy baja), u opacidad de la lente que requirió extirpación de cataratas (286 ojos; CR 0,15; IC del 95%: 0,01 a 2,79; DR ‐0,02; IC del 95%: ‐0,05 a 0,01; pruebas de muy baja calidad). El segundo ensayo que asignó al azar los ojos de los lactantes no encontró diferencias en el riesgo de desprendimiento completo de la retina entre los ojos asignados al azar a bevacizumab y los asignados al azar a tratamiento con láser (13 ojos; CR 0,33; IC del 95%: 0,01 a 7,50; DR ‐0,08; IC del 95%: ‐0,27 a 0,11).
Cuando se utilizó en combinación con tratamiento con láser, se encontró que pegaptanib intravitreal redujo el riesgo de desprendimiento de la retina en comparación con láser / crioterapia solo (152 ojos; CR 0,26; IC del 95%: 0,12 a 0,55; DR ‐0,29; IC del 95%: ‐0,42 a 0,16; pruebas de baja calidad). La incidencia de recurrencia de la RP a las 55 semanas de edad posmenstrual también fue inferior en el grupo de pegaptanib + tratamiento con láser (76 lactantes; CR 0,29; IC del 95%: 0,12 a 0,7; DR ‐0,35; IC del 95%: ‐0,55 a 0,16; pruebas de baja calidad). No hubo diferencias en el riesgo de hemorragias retinianas perioperatorias entre los dos grupos (152 ojos; CR 0,62; IC del 95%: 0,24 a 1,56; DR ‐0,05; IC del 95%: ‐0,16 a 0,05; pruebas de muy baja calidad). Sin embargo, no se conoce el riesgo de efectos adversos sistémicos retardados con ninguno de los fármacos.
Conclusiones de los autores
Implicaciones para la práctica: El bevacizumab intravitreal reduce el riesgo de defectos de la refracción durante la niñez cuando se administra como monoterapia, mientras que el pegaptanib intravitreal reduce el riesgo de desprendimiento de la retina cuando se administra conjuntamente con tratamiento con láser en los lactantes con RP tipo 1. Sin embargo, la calidad de las pruebas para ambos resultados fue baja debido al riesgo de sesgo de detección y otros sesgos. No se conoce el efecto sobre otros resultados fundamentales y, lo que es más importante, los efectos adversos sistémicos a largo plazo de los fármacos. La falta de datos suficientes impide establecer conclusiones sólidas que favorezcan el uso sistemático de los agentes anti‐FCEV intravitreal en los lactantes prematuros con RP tipo 1.
Implicaciones para la investigación: Se necesitan estudios adicionales para evaluar el efecto de los agentes anti‐FCEV sobre resultados estructurales y funcionales en la niñez y los efectos adversos sistémicos retardados como la disfunción miocárdica y resultados adversos del desarrollo nervioso.
PICO
Resumen en términos sencillos
Fármacos anti‐factor de crecimiento endotelial vascular (FCEV) para el tratamiento de la retinopatía del prematuro
Antecedentes
La retinopatía del prematuro (RP) es un trastorno vascular de la retina inmadura que puede provocar deterioro visual e incluso ceguera en los lactantes prematuros. Se trata principalmente mediante la extracción de la parte de la retina sin vasos sanguíneos (retina "avascular") por crioterapia o tratamiento con láser. Aunque estos tratamientos dan lugar a una mejoría significativa en los resultados a largo plazo, los resultados están lejos de ser perfectos. Además, provocan una pérdida permanente del campo visual periférico. Recientemente se han realizado estudios para evaluar la administración de los agentes anti‐FCEV para tratar la RP. Estos agentes inhiben la acción del factor de crecimiento endotelial vascular (FCEV), un regulador clave de la formación de nuevos vasos en la vida fetal. Los estudios en animales han mostrado una reducción significativa en la respuesta neovascular posterior a la inyección de anticuerpos anti‐FCEV en la cavidad vítrea de los ojos (tratamiento "intravitreal").
Características de los estudios
En enero de 2016 se efectuaron búsquedas en las bases de datos científicas en busca de estudios que evaluaran la eficacia y la seguridad del tratamiento intravitreal con agentes anti‐FCEV en los lactantes prematuros con RP. Se encontraron tres ensayos controlados aleatorios con 239 lactantes. Dos ensayos compararon bevacizumab intravitreal con tratamiento convencional con láser. El tercer ensayo comparó el tratamiento con láser más pegaptanib intravitreal con láser / crioterapia solo.
Resultados clave
Los resultados indican que el bevacizumab intravitreal reduce el riesgo de defectos de la refracción (miopía alta) durante la infancia, mientras que pegaptanib intravitreal administrado conjuntamente con el tratamiento con láser reduce el riesgo de desprendimiento de la retina. No se conocen los efectos sobre otros resultados fundamentales que incluyen los efectos secundarios retardados como el accidente cerebrovascular. Se necesitan más estudios para evaluar estos resultados.
Calidad de la evidencia
La calidad de las pruebas se calificó como muy baja o baja para la mayoría de los resultados clave.
Authors' conclusions
Summary of findings
| Intravitreal anti‐VEGF therapy compared to conventional laser/cryotherapy in preterm infants with type 1 ROP | |||||
| Patient or population: preterm infants with type 1 ROP | |||||
| Outcomes* | Illustrative comparative risks# (95% CI) | Relative effect | No of Participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| conventional laser/cryotherapy | intravitreal anti‐VEGF therapy | ||||
| Structural outcome ‐ retinal detachment | Study population | RR 1.04 | 143 | ⊕⊝⊝⊝ | |
| 27 per 1000 | 28 per 1000 | ||||
| Refractive error ‐ very high myopia ‐ at 30 months of age (unit of analysis: eyes) | Study population | RR 0.06 | 211 | ⊕⊕⊝⊝ | |
| 416 per 1000 | 25 per 1000 | ||||
| Mortality before discharge from primary hospital | Study population | RR 1.5 | 150 | ⊕⊕⊝⊝ | |
| 27 per 1000 | 40 per 1000 | ||||
| Mortality at 30 months of age | Study population | RR 0.86 | 150 | ⊕⊕⊝⊝ | |
| 93 per 1000 | 80 per 1000 | ||||
| Local adverse effects ‐ corneal opacity requiring corneal transplant (unit of analysis: eyes) | Study population | RR 0.34 | 286 | ⊕⊝⊝⊝ | |
| 7 per 1000 | 2 per 1000 | ||||
| Local adverse effects ‐ lens opacity requiring cataract removal (unit of analysis: eyes) | Study population | RR 0.15 | 286 | ⊕⊝⊝⊝ | |
| 21 per 1000 | 3 per 1000 | ||||
| Recurrence of ROP by 54 weeks PMA | Study population | RR 0.22 | 143 | ⊕⊕⊕⊝ | |
| 260 per 1000 | 57 per 1000 | ||||
| *Only the outcomes for which data are available are reported here; #The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Outcome assessment not blinded 295% CI around the pooled estimate includes both 1) no effect and 2) appreciable benefit or appreciable harm 3Number of events too small 4Serious risk of bias in analysis (unit of analysis error) 5Outcome assessment not blinded but outcome is objective | |||||
| Anti‐VEGF combined with laser/cryotherapy compared to laser/cryotherapy in preterm infants with type 1 ROP | |||||
| Patient or population: preterm infants with type 1 ROP | |||||
| Outcomes* | Illustrative comparative risks# (95% CI) | Relative effect | No of Participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| laser/cryotherapy | anti‐VEGF combined with laser/cryotherapy | ||||
| Structural outcome ‐ retinal detachment (unit of analysis: eyes) | Study population | RR 0.26 | 152 | ⊕⊕⊝⊝ | |
| 393 per 1000 | 102 per 1000 | ||||
| Local adverse effects ‐ perioperative retinal haemorrhages (unit of analysis: eyes) | Study population | RR 0.62 | 152 | ⊕⊝⊝⊝ | |
| 143 per 1000 | 89 per 1000 | ||||
| Recurrence of ROP by 55 weeks' PMA | Study population | RR 0.29 | 76 | ⊕⊕⊝⊝ | |
| 500 per 1000 | 145 per 1000 | ||||
| *Only the outcomes for which data are available are reported here; #The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Outcome assessment not blinded 2Serious risk of bias in analysis (unit of analysis error) 3Unclear risk of selection bias 495% CI around the pooled estimate includes both 1) no effect and 2) appreciable benefit or appreciable harm | |||||
Background
Description of the condition
Retinopathy of prematurity (ROP) is one of the major avoidable causes of childhood blindness in both developed and developing countries (Gilbert 2008). Essentially a neovascularising disease of the retina, ROP occurs almost exclusively in preterm very low birth weight (VLBW) infants. With improved survival of the VLBW infants, the absolute number of children with visual impairment secondary to ROP has increased in recent years (Gilbert 2005; Mantagos 2009).
The incidence of ROP varies inversely with gestation and weight at birth. A multicenter study of infants born between 1986 and 1987 reported that 81.6% of infants weighing less than 1000 grams (g) developed ROP while only 46.9% of those weighing 1000 g to 1250 g had ROP (Palmer 1997).
The other risk factors of ROP include exposure to varying oxygen concentrations, hypercapnia, anaemia, acidosis, chronic lung disease and intraventricular haemorrhage (IVH) (Ashton 1953; Smith 2003; Tasman 2006).
The predisposition of preterm infants to development of ROP relates to their immature retinal vasculature. In humans, retinal vascularisation begins at about 12 weeks and is completed by 36 weeks to 40 weeks of gestation. Normally, the blood vessels develop from the optic disc and then progress outwards towards the ora serrata. Infants born before this period will, therefore, have an immature retina with a peripheral avascular zone. ROP develops if there is a disruption in the new vessel formation ‐ angiogenesis ‐ in this zone. The disruption of angiogenesis has been found to occur in two sequential phases: a vaso‐obliterative phase followed by a vaso‐proliferative phase (Ashton 1954). In the vaso‐obliterative phase (phase 1), the normally high arterial oxygen saturation in the postnatal life coupled with hyperoxia secondary to oxygen supplementation leads to involution and loss of formed blood vessels. In the second phase (phase 2), the relatively hypoxic environment due to ischaemia caused by vessel loss coupled with the high metabolic demands of the avascular retina leads to up regulation of various angiogenic factors resulting in abnormal neovascularisation. In most infants, the new vessels formed regress without leaving any sequelae. However, in some infants the neovascularisation goes unchecked leading to retinal scarring, traction and finally detachment.
The extent and severity of ROP are traditionally described in terms of location (zones; I to III), severity (stages; 1 to 5), extent (clock hours; 1 to 12), and vascular dilatation and tortuosity (plus disease) according to the International Classification of ROP definitions (Committee for Classification of ROP 1984). In addition to defining the progression of the disease, this classification also serves as a guide for surgical intervention. In 2005, the classification was revised to include aggressive posterior ROP (AP‐ROP), pre‐plus disease, and a practical way to estimate the extent of zone I with the indirect ophthalmoscope. Concomitantly, the recommendations for treatment were also revised based on the results of the Early Treatment for Retinopathy of Prematurity trial (ET‐ROP Group 2003). The new recommendations place more emphasis on the presence of plus disease, rather than the number of clock hours, to decide upon the need for treatment (American Academy of Pediatrics 2006). Accordingly, treatment is initiated for the following retinal findings (type 1 ROP):
-
Zone I ROP: any stage with plus disease
-
Zone I ROP: stage 3 ‐ no plus disease
-
Zone II ROP: stage 2 or stage 3 with plus disease
The current treatment strategy for infants with type 1 ROP involves peripheral retinal ablation by either cryotherapy or laser therapy. Both techniques result in significant improvement in the structural and functional outcomes ‐ a Cochrane review reported significant reduction in the risk of early unfavourable retinal structure from 47.9% to 28.1% and unfavourable visual acuity in early childhood from 63% to 50.6% following peripheral retinal ablation (Andersen 1999). However, in a small but significant proportion of preterm infants, the disease progresses despite treatment. Also, visual fields are slightly smaller in eyes subjected to peripheral retinal ablation as compared to 'control' eyes (Andersen 1999). Moreover, the ablation techniques are cumbersome and require sedation, general anaesthesia, or both. This has led to the quest for simpler and more effective treatment strategies.
Description of the intervention
Vascular endothelial growth factor (VEGF) is a key regulator of angiogenesis in fetal life. In the normally developing retina, VEGF is released in response to the higher oxygen demand of the retinal tissue which leads to the development of blood vessels from the optic nerve to the periphery. In preterm infants with disrupted angiogenesis, however, the expression and levels of VEGF differ markedly in the two different phases. While the levels are suppressed in the vaso‐obliterative phase, there is an over production/expression of VEGF leading to abnormal vascular proliferation in the vaso‐proliferative phase. Hugely elevated levels of VEGF have been documented in the vitreous cavity of eyes with stage 4 ROP (Lashkari 2000).
The key role played by VEGF in inducing retinal neovascularisation prompted researchers to explore the role of anti‐VEGF drugs in the management of ROP. Intravitreal injection of neutralizing anti‐VEGF antibodies had demonstrated significant reduction in the neovascular response in animal studies (Aiello 1995). Two anti‐VEGF drugs namely, pegaptanib sodium and ranibizumab, had been approved by the United States Food and Drug Administration (FDA) for intraocular use in adults in neovascular and age‐related macular degeneration (AMD). The third inhibitor ‐ bevacizumab ‐ is being used off‐label for intraocular injection in adults with similar results. Unfortunately, none of these drugs have been approved for intraocular use in children to date (Mantagos 2009). However, given the limitations of existing treatment strategies (see above), many investigators have evaluated the off‐label use of these agents in infants with ROP (Shah 2007; Kong 2008; Mintz‐Hittner 2008). These studies ‐ predominantly case‐series and retrospective studies ‐ used one or more of the following approaches to evaluate the efficacy of VEGF inhibitors:
-
monotherapy ‐ using an anti‐VEGF drug instead of cryo/laser therapy;
-
combination therapy ‐ using anti‐VEGF simultaneously with cryo/laser therapy;
-
rescue therapy ‐ using anti‐VEGF in infants with progression of the disease despite adequate treatment and in the rare instances where the infant presents with advanced ROP (stage 4 or more).
While the efficacy of anti‐VEGF drugs in ROP was demonstrated in most of the studies, their safety is yet to be established. Though no significant adverse events have been reported so far (except for tractional retinal attachment in an occasional infant with advanced ROP), concerns still remain regarding their potential local and systemic adverse effects. By inhibiting VEGF, a key factor in regulation of angiogenesis in the developing retina as well as the central nervous system, these drugs could result in significant local and systemic adverse effects. Indeed, there have been concerns regarding the risk of cerebrovascular accidents following intravitreal ranibizumab injections in adults with AMD (Ueta 2009). Though bevacizumab, the most frequently tested drug in ROP, has a lower risk of systemic absorption following intravitreal injections, the distinct possibility of its systemic effects cannot be ruled out in preterm infants with immature, and often impaired, blood‐retinal barrier (Law 2010).
The risk of systemic absorption, though small, brings its own complexity in the methods of randomisation and analysis in trials involving a locally administered drug. For a drug with truly local action, one can randomise either the study subject or a local body part of the subject to intervention and control groups. In the former, infants would be randomized ‐ both eyes of the infants (if needed) would receive the intervention or control therapy as per the group allocation. In the latter, eyes of the infants would be randomized ‐ one eye would receive the intervention while the other eye would receive 'control' therapy. However, if the drug is likely to have systemic effects (like most anti‐VEGF agents), randomising the body part is not an ideal method of randomisation.
Why it is important to do this review
Treatment of ROP, to date, is largely surgical ‐ by cryotherapy or by laser therapy. Although these treatments result in a significant improvement in long‐term visual outcomes, the results are far from perfect. Despite appropriate treatment, progression to tractional retinal detachment occurs in 10% to 15% of infants with threshold disease (ET‐ROP Group 2003). In addition, the ablation procedures invariably cause permanent loss of the peripheral visual field. Simple, effective, and less destructive treatment strategies would definitely be preferable to these procedures.
The recent reports of success following bevacizumab use have stimulated various investigators to conduct clinical studies on the efficacy of this intervention. However, many of these studies are not powered to detect any serious adverse events ‐ local or systemic ‐ in the enrolled infants. Also, most have not systematically documented the risk of recurrence of ROP at a later age or examined the duration of follow‐up required to detect recurrence following intravitreal therapy. Given the protracted course of the disease and the short half‐life of anti‐VEGF drugs, the potential risk of recurrence is high (Wong 2015).
An earlier systematic review on the use of bevacizumab for severe ROP that included only case reports/case‐series and retrospective studies found considerable variability in how bevacizumab is used for the treatment of ROP (Micieli 2009). It concluded that 'further randomized control trials are warranted'. The purpose of this review is to identify all the available randomized controlled trials (RCT) on intravitreal anti‐VEGF therapy and to systematically analyse their results.
Objectives
To evaluate the efficacy and safety of anti‐VEGF drugs when used either as monotherapy, i.e. without concomitant cryotherapy or laser therapy or in combination with planned cryo/laser therapy in preterm infants with type 1 ROP (defined as zone I any stage with plus disease, zone I stage 3 with or without plus disease or zone II stage 2 or 3 with plus disease).
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials that evaluated the efficacy or safety of administration, or both, of anti‐VEGF agents in human preterm infants were considered for inclusion in this review. We included only those trials that used VEGF inhibitors either alone (i.e. monotherapy) or in combination with cryo/laser therapy (i.e. combination therapy). We excluded those studies that used these drugs when other treatments such as cryo/laser therapy or vitrectomy had failed ('rescue therapy').
Types of participants
Studies that enrolled preterm (< 37 weeks' gestation at birth) infants with type 1 ROP at enrolment were considered for inclusion. Type 1 ROP was defined as zone I any stage with plus disease, zone I stage 3 ROP with or without plus or zone II stage 2 or 3 ROP with plus disease (ET‐ROP Group 2003). For the purpose of this review, we excluded those studies that enrolled infants with more advanced ROP ‐ stage 4 or more ‐ at the time of enrolment (irrespective of the treatment strategy employed).
Types of interventions
Objective 1
Intervention: Administration of any anti‐VEGF agent by intravitreal route.
Control: Cryotherapy/laser therapy.
Objective 2
Intervention: Intravitreal administration of VEGF inhibitors within seven days (before or after) of a planned laser or cryotherapy.
Control: Cryotherapy/laser therapy alone.
Types of outcome measures
Primary outcomes
-
Functional outcome ‐ blindness or severe visual impairment (acuity ≤ 20/200) at 6 months to 12 months of corrected age.
-
Structural outcome ‐ progression to retinal detachment involving the macula.
Secondary outcomes
-
Functional outcome(s) at 6 months to 12 months of corrected age:
-
amblyopia;
-
nystagmus and/or;
-
refractive error in either eye.
-
-
Unfavourable structural outcomes, assessed at 6 months to 12 months of corrected age, and defined as:
-
retinal fold involving the macula or;
-
retinal detachment involving zone 1 of the posterior pole and/or;
-
retrolental tissue or 'mass' obscuring the view of the posterior pole.
-
-
Childhood unfavourable visual acuity, assessed at four years to six years, and defined as absence of vision or Snellen visual acuity of 20/200 or worse.
-
Mortality measured as:
-
death before discharge from the primary hospital;
-
death before two years corrected age.
-
-
Adverse neurodevelopmental outcomes at 18 months to 24 months of corrected age:
-
cerebral palsy and/or;
-
moderate to severe developmental delay as assessed on performance in formal neurodevelopmental testing such as Bayley scale.
-
-
Local adverse effects such as conjunctival haemorrhage, vitreous haemorrhage, and endophthalmitis after the procedure.
-
Acute systemic effects such as apnoea requiring respiratory support and cardiorespiratory arrest during or immediately after the treatment procedure.
-
Delayed systemic effects such as cerebrovascular accidents (stroke) and myocardial dysfunction (based on echocardiographic parameters such as ejection fraction and fractional shortening) diagnosed in the first 24 months of life.
-
Parental satisfaction regarding the treatment procedure employed (in Likert or other such scales).
-
Recurrence of ROP requiring re‐treatment by 54 weeks to 55 weeks PMA.
Search methods for identification of studies
Electronic searches
We used the criteria and standard methods of the Cochrane Collaboration and the Cochrane Neonatal Review Group (see the Cochrane Neonatal Group search strategy for specialized register). We conducted a comprehensive search including: Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (Issue 1, 2016), MEDLINE (1966 to January 1, 2016) via PubMed, EMBASE (1980 to January 1, 2016) and CINAHL (1982 to January 1, 2016) using the following search terms: (bevacizumab OR Avastin OR ranibizumab OR pegaptanib sodium OR anti‐angio* OR angiogenesis inhibitors), plus database‐specific limiters for RCTs and neonates (see Appendix 1 for the full search strategies for each database). We limited the searches to human studies. We did not apply any language restrictions. We searched clinical trials registries for ongoing or recently completed trials (clinicaltrials.gov; the World Health Organization’s International Trials Registry and Platform www.whoint/ictrp/search/en/, and the ISRCTN Registry).
Searching other resources
We searched for unpublished studies by handsearching the conference proceedings of the Society for Pediatric Research (2002‐2013) and American Academy of Ophthalmology Annual Meeting (1999‐2013). We also searched the reference lists of all studies identified by the above methods.
Data collection and analysis
Selection of studies
Three review authors (MJS, JS and MM) independently searched and identified the eligible trials based on the following characteristics: study population (preterm infants with type 1 ROP ), study intervention (administration of anti‐VEGF drugs with or without laser/cryotherapy), and study design (RCTs).
The authors screened the titles and abstracts to identify potentially relevant citations. The full text of the article was retrieved and reviewed if relevance could not be ascertained by screening the title and the abstract. The review authors independently assessed the eligibility of the studies by filling out eligibility forms designed in accordance with the specified inclusion criteria. We resolved any disagreement by discussion.
We contacted the study investigators for additional information or clarification of the method of randomisation, patient characteristics, details of interventions, definitions of events, additional relevant outcomes and losses to follow‐up, as necessary.
Data extraction and management
Data extraction was done using a data extraction form that was designed and pilot tested by the review authors. We extracted information regarding:
-
study setting (for example, country and settings);
-
study intervention;
-
sample size;
-
length of follow‐up;
-
randomisation procedure;
-
risk of different biases (see Assessment of risk of bias in included studies below);
-
outcomes as listed above.
For dichotomous outcomes, we extracted the total number of participants for each group and the number of participants experiencing an event. For continuous outcomes, we extracted mean, standard deviation (or data required to calculate this) and the total number of participants for each group.
Assessment of risk of bias in included studies
Three review authors (MJS, JS and MM) independently assessed the methodological quality of all the included studies using The Cochrane 'Risk of bias' tool (Higgins 2011; Higgins 2011a). The items in the tool included the following:
-
sequence generation (allocation sequence adequately generated);
-
allocation sequence concealment (allocation adequately concealed);
-
blinding (knowledge of the allocated intervention adequately prevented during the study);
-
incomplete outcome data (incomplete outcome data adequately addressed);
-
selective outcome reporting (reports of the study free of suggestion of selective outcome reporting);
-
other potential sources of bias (study apparently free of other problems that could put it at a high risk of bias).
A judgement of 'Yes' indicates low risk of bias, 'No' indicates high risk of bias, and 'Unclear' indicates unclear or unknown risk of bias. We contacted the study authors when insufficient information was provided to determine the risk of bias. Risk of bias was summarised for the primary outcomes.
In addition to assessing the risk of bias, we also applied the GRADE system to assess the quality of the body of the evidence (Schünemann 2011). According to GRADE, the domains that may decrease the quality of the evidence include:
-
study design;
-
risk of bias;
-
inconsistency of results;
-
indirectness (non‐generalisability);
-
imprecision (insufficient data);
-
other factors (e.g. reporting bias).
The quality of the evidence was reduced by one level for each of the domains that was encountered. The following levels of evidence were defined.
-
High quality evidence: Further research is very unlikely to change our confidence in the estimate of effect. There are consistent findings among 75% of RCTs with low risk of bias that are generalisable to the population in question. There are sufficient data, with narrow confidence intervals. There are no known or suspected reporting biases (all of the domains are met).
-
Moderate quality evidence: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate (one of the domains is not met).
-
Low quality evidence: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate (two of the domains are not met).
-
Very low quality evidence: We are very uncertain about the estimate (three of the domains are not met).
We used the GRADE profiler(GRADEpro GDT) to import data from Review Manager 5.3 (RevMan) (RevMan 2014) to create the 'Summary of findings' tables. These tables provide outcome‐specific information concerning the overall quality of evidence from studies included in the comparison, the magnitude of effect of the interventions examined, and the sum of available data on the outcomes we considered.
Measures of treatment effect
We used the standard methods of the Neonatal Review Group to synthesise the data. We expressed effects as risk ratio (RR), risk difference (RD) and 95% confidence intervals (CI) for categorical data, and mean difference (MD) and 95% CI for continuous data. For significant differences, we also calculated the number needed to treat for an additional beneficial outcome (NNTB) based on 1/RD. We used the fixed‐effect model for pooling the results of individual studies.
Unit of analysis issues
We anticipated that the units of randomisation and analysis in the included trials would be individual infants and not eyes (it is difficult to randomise eyes because intravitreal anti‐VEGF can be absorbed into the systemic circulation). However, if a given study had randomized eyes and not infants, we intended to use the study data but refrained from pooling it with data of studies that had randomized infants. We a priori decided to use the eye‐level data (and not infant‐level data) in these studies, i.e. incidence of outcomes in eyes randomized to anti‐VEGF vs. incidence of outcomes in eyes randomized to the control group; consequently, individual‐level outcomes such as mortality were not considered in these studies. We a priori assumed that the beneficial effect, if any, would be diluted in them, i.e. the effect size would be closer to the null effect, if systemic absorption of anti‐VEGF agents were to occur (because the eye randomized to control group would be exposed to both anti‐VEGF agents and 'control' treatment).
If a given study had randomized infants but provided the outcome data for eyes, we planned to contact the authors to obtain infant‐level data so as to avoid unit of analysis error ‐ using eyes as the denominator without adjusting for non‐independence between the eyes may result in spuriously precise results, i.e. narrow confidence intervals similar to that seen in cluster randomized trials when the clusters are randomized but the outcomes are analysed at the individual level without adjusting for 'cluster' effect (Higgins 2011b). If that information could not be obtained, we used the data for eyes but mentioned up‐front that the analysis referred to eyes and not infants.
Dealing with missing data
At the outcome level, if the data were measured but not reported, we planned to request such data from study authors. If there was a discrepancy in the number randomized and the number analysed in each treatment group, we calculated and reported the percentage lost to follow‐up in each group.
Assessment of heterogeneity
We intended to examine for heterogeneity between trial results by inspecting the forest plots and quantifying the impact of heterogeneity in any meta‐analysis using a measure of the degree of inconsistency in the studies’ results (Deeks 2011).
We estimated the proportion of total statistical heterogeneity not explained by chance using the I2 statistic (Higgins 2003). I2 (calculated as I2 = 100% x (Q ‐ df )/Q; where Q is Cochrane’s heterogeneity statistic and df is the degrees of freedom) lies between 0% and 100%.
Data synthesis
Quantitative data was entered into RevMan (RevMan 2014) and analysed using the standard methods of Cochrane and Cochrane Neonatal. We used the Mantel‐Haenszel method for estimates of typical RR and RD. We analysed continuous outcomes using the inverse variance method.
Subgroup analysis and investigation of heterogeneity
Considerations of clinical diversity included assessment of differences in nature of the surgical intervention, type and extent of disease and the number and route of administration of VEGF inhibitors. Accordingly, we planned to analyse the studies based on differences in the following pre‐planned subgroups.
-
Nature of retinal ablation procedure (cryotherapy versus laser therapy)
-
Location of ROP at enrolment (zone I versus zone II)
-
Severity of ROP at enrolment (AP‐ROP versus others)
-
Specific anti‐VEGF agent administered
-
Number of doses of anti‐VEGF drug (single versus multiple)
-
Birth weights of the enrolled infants (< 1250 g versus ≥ 1250 g)
Sensitivity analysis
We intended to conduct a sensitivity analysis to investigate the robustness of the results for the primary outcome by excluding trials at high risk of bias or with drop‐out rates of more than 10% (overall).
Results
Description of studies
See:Characteristics of included studies
Results of the search
A total of 1518 records were retrieved from the literature, of which 1513 were excluded after scanning the title or abstract, or both (Figure 1). Three randomized trials fulfilled the eligibility criteria (BEAT‐ROP Trial 2011; Autrata 2012; Lepore 2014) and were included in the review. Two articles remain in studies awaiting classification. No article was excluded after full‐text assessment.

Study flow diagram.
Included studies
Of the three included studies, two compared intravitreal bevacizumab monotherapy with conventional laser therapy (BEAT‐ROP Trial 2011; Lepore 2014) while the third compared intravitreal pegaptanib plus conventional laser therapy with laser and cryotherapy (Autrata 2012). Two trials (BEAT‐ROP Trial 2011; Autrata 2012) randomized infants whereas the third randomized eyes of the infants to the two groups (Lepore 2014).
BEAT‐ROP Trial 2011 was a multi‐centre randomized trial conducted at 15 hospitals in the United States of America (BEAT‐ROP Trial 2011). It enrolled 150 preterm infants with zone I or zone II posterior stage 3+ ROP and randomly assigned them to receive intravitreal bevacizumab (0.625 mg in 0.025 ml of solution) or conventional laser therapy, bilaterally. The primary outcome was treatment failure, defined as the recurrence of neovascularisation in one or both eyes requiring re‐treatment, by 54 weeks’ postmenstrual age (PMA). RetCam (retinal imaging) photographs taken at different time points were evaluated to document recurrence of ROP. The study investigators reported the refractive outcomes at 30 months of age in a separate publication in 2014 by Geloneck (see BEAT‐ROP Trial 2011). Of the originally enrolled 150 infants, 131 infants underwent cycloplegic retinoscopic refraction to assess refractive outcomes at this age.
Autrata 2012 enrolled 76 preterm infants with zone I or zone II posterior stage 3+ ROP, admitted in a University Hospital in the Czech Republic. Enrolled infants were randomly assigned to receive intravitreal pegaptanib (0.3 mg in 0.02 ml of solution) plus conventional diode laser therapy or laser therapy combined with cryotherapy, bilaterally. The primary outcome was treatment success defined as absence of recurrence of stage 3+ ROP in one or both eyes by 55 weeks' PMA. RetCam photographs taken at different time points were evaluated to document recurrence of ROP. Infants who were randomized to the intervention group and had recurrence were given an additional intravitreal pegaptanib injection; those in the laser‐plus‐cryotherapy group did not receive pegaptanib for recurrence.
Lepore 2014 conducted a single‐centre randomized trial and enrolled 13 infants with type 1 ROP in zone I in both eyes who required treatment according to ET‐ROP criteria (ET‐ROP Group 2003). One eye of the enrolled infants was randomized to receive an intravitreal injection of 0.5 mg bevacizumab while the fellow eye received conventional laser photoablation. The eye assigned to conventional laser peripheral ablation was treated first. The primary outcome was presence of retinal and choroidal abnormalities on fluorescein angiography (FA) at nine months of age. After treatment, binocular indirect ophthalmoscopy and RetCam imaging were performed every three days, and FA was performed every two weeks until discharge. FA was done again at nine months of age under general anaesthesia.
Further details of the three studies are provided in the Characteristics of included studies table.
Excluded studies
No study was excluded following full‐text assessment.
The studies of Kong 2015 and Moran 2014 are awaiting further assessment.
Risk of bias in included studies
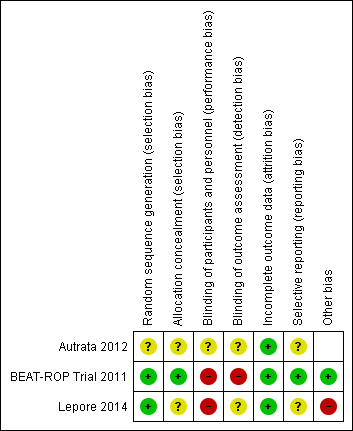
Quality assessments are detailed in Characteristics of included studies table and are also summarised in Figure 2.
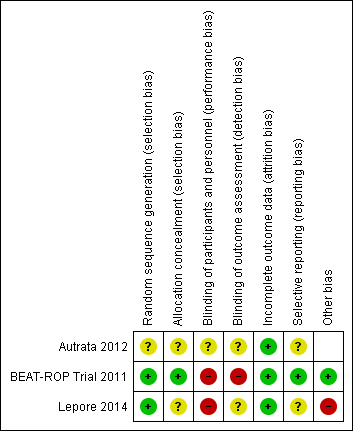
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
BEAT‐ROP Trial 2011 reported an adequate allocation concealment method whereas the other two trials (Autrata 2012; Lepore 2014) did not report details of allocation concealment.
Blinding
Given the nature of the intervention, blinding of the intervention was not possible in any of the studies.
BEAT‐ROP Trial 2011 constituted a panel of six independent experts to examine the photographs taken at 54 weeks' PMA, and masked them to the treatment assignments by cropping the photographs to include only the optic disk and macula without laser marks. This enabled the study investigators to perform blinded assessment of some of the secondary outcomes (e.g. macular dragging) but not the primary outcome of the study. Paediatric ophthalmologists who performed the cycloplegic retinoscopic refractions to assess the refractive errors at 30 months of age were not masked to the treatment assignments.
It is not clear if the outcome assessors were masked to the group allocation in the other two trials (Autrata 2012; Lepore 2014).
Incomplete outcome data
Two trials reported no loss to follow‐up until 54 weeks' PMA (BEAT‐ROP Trial 2011; Autrata 2012). About 17% of eligible infants were lost to follow‐up at 30 months of age in BEAT‐ROP Trial 2011. There was no loss to follow‐up at nine months of age in Lepore 2014.
Selective reporting
BEAT‐ROP Trial 2011 reported all the outcomes listed in the protocol (see NCT00622726 in BEAT‐ROP Trial 2011). The other two trials had unclear risk of reporting bias. We could not refer to the study protocol in Autrata 2012; secondary outcomes were not provided in the study protocol of Lepore 2014.
Other potential sources of bias
In Lepore 2014, eyes of enrolled infants were randomized. If there was significant systemic absorption of bevacizumab, the eye randomized to control group would have been exposed to both anti‐VEGF agents and control treatment resulting in better outcomes in that eye.
We intended to assess the likelihood of potential publication bias using funnel plots, provided there were at least 8 to10 trials (Sterne 2011).
Effects of interventions
See: Summary of findings for the main comparison Intravitreal anti‐VEGF therapy compared to conventional laser/cryotherapy in preterm infants with type 1 ROP; Summary of findings 2 Anti‐VEGF combined with laser/cryotherapy compared to laser/cryotherapy in preterm infants with type 1 ROP
Comparison 1: Anti‐VEGF vs cryo/laser therapy ('monotherapy')
Two trials (BEAT‐ROP Trial 2011; Lepore 2014) compared intravitreal bevacizumab with conventional laser therapy. While BEAT‐ROP Trial 2011 randomized preterm infants with stage 3+ ROP in zone I or zone II posterior, Lepore 2014 randomized eyes of infants with type 1 ROP in zone I. Because the unit of randomisation was different in the two studies (infants versus eyes), we did not attempt to pool their results.
Primary outcomes
Functional outcome ‐ blindness or severe visual impairment at 6 to 12 months of corrected age
Neither of the studies reported this outcome.
Structural outcome ‐ progression to retinal detachment involving the macula (Outcome 1.1)
BEAT‐ROP Trial 2011 did not report any difference in the incidence of complete or partial retinal detachment between the two groups (RR 1.04, 95% CI 0.21 to 5.13; RD 0.00, 95% CI ‐0.06 to 0.07; Analysis 1.1). Only a small number of infants ‐ two infants each in the two groups ‐ had retinal detachment. The quality of evidence was graded very low because of the small number of events and the risk of detection bias (summary of findings Table for the main comparison). No separate data was available for the risk of retinal detachment involving only the macula.
In the other trial (Lepore 2014), one eye (8.5%) treated with conventional laser progressed to complete retinal detachment four weeks after treatment while none of the eyes randomized to intravitreal bevacizumab had complete detachment (RR 0.33, 95% CI 0.01 to 7.50; RD ‐0.08, 95% CI ‐0.27 to 0.11; Analysis 1.2).
Secondary outcomes
Functional outcome(s) ‐ refractive error at 30 months of age (Outcomes 1.2 to 1.3)
One study (BEAT‐ROP Trial 2011) reported the outcome using eyes as the denominator. The risk of very high myopia, defined as ‐8 diopters (D) or more, was significantly lower in the eyes of infants randomized to intravitreal bevacizumab (RR 0.06, 95% CI 0.02 to 0.20; RD ‐0.40, 95% CI ‐0.50 to ‐0.30)(Analysis 1.3). The magnitude of benefit was almost the same in both zone I and zone II posterior ROP. The quality of evidence was graded low because of the unit of analysis error and the risk of detection bias (summary of findings Table for the main comparison).
The mean spherical equivalent refractive error was also significantly less in eyes of infants who received intravitreal bevacizumab (mean difference [MD] 5.68 Diopter, 95% CI 4.33 to 7.02). The magnitude of difference was almost the same in both zone I (MD 6.93 Diopter, 95% CI 4.26 to 9.60) and zone II posterior ROP (MD 5.25 Diopter, 95% CI 3.69 to 6.81)(Analysis 1.4).
Unfavourable structural outcomes, assessed at 6 to 12 months of corrected age
Neither of the studies reported this outcome.
Childhood unfavourable visual acuity, assessed at four to six years
Neither of the studies reported this outcome.
Mortality before discharge from the primary hospital and at 30 months of age (Outcomes 1.4 to 1.5)
BEAT‐ROP Trial 2011 reported no difference in the risk of mortality between the two groups ‐ either before discharge from the primary hospital (RR, 1.50; 95% CI 0.26 to 8.75)(Analysis 1.5) or at a mean age of 30 months (RR 0.86, 95% CI 0.30 to 2.45)(Analysis 1.6). The number of events was, however, very small.
Adverse neurodevelopmental outcomes at 18 to 24 months of corrected age
Neither of the studies reported this outcome.
Local adverse effects (Outcomes 1.6 to 1.7)
One study (BEAT‐ROP Trial 2011) reported the outcome using eyes as the denominator. There was no significant difference in the incidence of corneal opacity requiring corneal transplant (RR 0.34, 95% CI 0.01 to 8.26) (Analysis 1.7) or lens opacity requiring cataract removal (RR 0.15, 95% CI 0.01 to 2.79) (Analysis 1.8) between the two groups. The study did not report the risk of conjunctival haemorrhage, vitreous haemorrhage, or endophthalmitis in the two groups.
Acute systemic effects during or immediately after the treatment procedure
Neither of the studies reported this outcome.
Delayed systemic effects
Neither of the studies reported this outcome.
Parental satisfaction regarding the treatment (in Likert or other such scales)
Neither of the studies reported this outcome.
Additional outcomes
Recurrence of ROP by 54 weeks' postmenstrual age
One study (BEAT‐ROP Trial 2011) reported this outcome. Infants randomized to intravitreal bevacizumab therapy had significantly lower risk of recurrence of ROP requiring retreatment by 54 weeks' PMA when compared to infants who received conventional laser therapy (RR 0.22, 95% CI 0.08 to 0.62; RD ‐0.20, 95% CI ‐0.31 to ‐0.09; NNTB 5; 95% CI 3 to 11) (Analysis 1.9). The quality of evidence for this outcome was graded moderate (summary of findings Table for the main comparison). On subgroup analysis, the difference was found to be significant only in infants with Zone I ROP.
Comparison 2: Anti‐VEGF plus cryo/laser therapy ('combination therapy') vs cryo/laser therapy alone
Autrata 2012 compared intravitreal pegaptanib plus conventional laser therapy with laser and cryotherapy in preterm infants with stage 3+ ROP.
Primary outcomes
Functional outcome ‐ blindness or severe visual impairment at 6 to 12 months of corrected age
The study did not report this outcome.
Structural outcome ‐ progression to retinal detachment involving the macula (Outcome 2.1)
The study reported the outcome using eyes as the denominator. The risk of complete or partial retinal detachment was significantly lower in the eyes of infants randomized to intravitreal pegaptanib plus laser therapy (RR 0.26, 95% CI 0.12 to 0.55; RD ‐0.29, 95% CI ‐0.42 to ‐0.16; one study, 152 infants) (Analysis 2.1). The quality of evidence was graded low because of the unit of analysis error and the risk of detection bias (summary of findings Table 2).
No separate data was available for the risk of retinal detachment involving only the macula in the two groups.
Secondary outcomes
Functional outcome(s) ‐ refractive error at 6 to 12 months of age or later
The study did not report this outcome.
Unfavourable structural outcomes at 6 to 12 months of age
The study did not report this outcome.
Childhood unfavourable visual acuity
The study did not report this outcome.
Mortality before discharge from the primary hospital and at 30 months of age
The study did not report this outcome.
Adverse neurodevelopmental outcomes at 18 to 24 months of corrected age
The study did not report this outcome.
Local adverse effects (Outcomes 2.2)
The study reported the outcome using eyes as the denominator. There was no significant difference in the risk of perioperative retinal haemorrhages after laser therapy between the two groups (RR 0.62, 95% CI 0.24 to 1.56; one study, 152 infants) (Analysis 2.2). The study did not report the risk of conjunctival haemorrhage or vitreous haemorrhage in the two groups.
The study reported that "no systemic or significant ocular complications of intravitreal pegaptanib injections, such as endophthalmitis or RD were found during the follow‐up period after treatment" but did not provide the corresponding data for the other group.
Acute systemic effects during or immediately after the treatment procedure
The study did not report this outcome (see 'Local adverse effects' above).
Delayed systemic effects
The study did not report this outcome.
Parental satisfaction regarding the treatment (in Likert or other such scales)
The study did not report this outcome.
Additional outcomes
Recurrence of ROP by 55 weeks' postmenstrual age (Outcome 2.3)
Infants randomized to intravitreal pegaptanib plus laser therapy had significantly lower risk of recurrence of ROP by 55 weeks' PMA when compared to those randomized to laser therapy with cryotherapy (RR 0.29, 95% CI 0.12 to 0.70; RD ‐0.35, 95% CI ‐0.55 to ‐0.16; NNTB 3; 95% CI 2 to 6; one study, 76 infants) (Analysis 2.3). The quality of evidence for this outcome was graded low because of the risk of detection bias and the unclear risk of selection bias (summary of findings Table 2).
Discussion
Summary of main results
The systematic review included three studies, of which two evaluated the effects of bevacizumab monotherapy while the third examined the effects of intravitreal pegaptanib plus laser therapy. When used as monotherapy, intravitreal bevacizumab did not improve short‐term structural outcomes (partial or complete retinal detachment) but significantly reduced the risk of refractive errors at 30 months of age. When used in conjunction with laser therapy, intravitreal pegaptanib reduced the risk of retinal detachment in infants with stage 3+ ROP. Both the agents reduced the risk of recurrence of ROP requiring re‐treatment in the first few weeks of life. No significant difference was noted in the incidence of local adverse events with either of the drugs. On subgroup analysis, the risk of all the outcomes ‐ except for recurrence of ROP requiring re‐treatment ‐ was found to be similar in infants with zone I ROP and those with zone II posterior ROP receiving intravitreal bevacizumab monotherapy. However, the numbers were too small to draw any meaningful conclusion on the subgroup analysis.
Overall completeness and applicability of evidence
The currently available evidence is 'incomplete' for three major reasons. Firstly, the limited number of studies included in the review. Despite the well established pathophysiological rationale for using anti‐VEGF agents and the short‐term benefits observed in numerous case reports and case series (Shah 2007; Kong 2008; Mintz‐Hittner 2008), only three RCTs have been published so far. Secondly, the long‐term beneficial effects, if any, in terms of favourable structural and functional outcomes are not known. Both the agents were found to reduce the risk of recurrent ROP requiring re‐treatment in the first few weeks of life but it is not clear if this benefit would translate into lesser risk of blindness, severe visual impairment or unfavourable structural outcomes at a later age. Also, the risk of recurrence of ROP beyond the first few weeks of life in the intervention group is not known. Thirdly, the safety concerns of anti‐VEGF drugs are yet to be addressed. One trial (BEAT‐ROP Trial 2011) reported no difference in the risk of mortality between the intervention and control groups at a mean age of 30 months but the number of events was very small. Given the potential risk of systemic absorption and consequent adverse effects like cerebrovascular accidents following intravitreal anti‐VEGF therapy, the lack of evidence on safety outcomes is a major concern.
The incomplete evidence is indeed a serious dampener in the quest to identify a simple, safe, and effective therapy for ROP. Unlike the current standard of therapy, laser or cryotherapy, anti‐VEGF administration is technically simple and does not require general anaesthesia or the services of a skilled retinal surgeon. This could be a great boon, particularly in settings with limited resources from low‐ and middle‐income countries. There is an urgent need to generate more evidence on the long‐term structural outcomes as well as the adverse effects following intravitreal therapy with anti‐VEGF agents before they can be considered for routine clinical use in infants with ROP. Future studies should also examine how these drugs affect the natural history of the disease, the focus being late recurrence that might warrant long‐term follow‐up and the risk of local complications like infections following therapy, especially in resource‐restricted settings.
Quality of the evidence
We intended to include all the outcomes ‐ primary and secondary ‐ of the review in the 'Summary of findings' tables. However, many of the outcomes were not reported in the included studies. Therefore, only seven outcomes for the comparison of 'Anti‐VEGF vs cryo/laser therapy' and three outcomes for the comparison of 'Anti‐VEGF plus cryo/laser therapy vs cryo/laser therapy alone' were reported in the 'Summary of findings' tables.
The quality of evidence was graded as very low to low for almost all outcomes of the review (summary of findings Table for the main comparison; summary of findings Table 2). The risk of detection bias was high in all the studies because the outcome assessors were not blinded to the group allocation. The risk of other biases including selection bias and reporting bias was low in BEAT‐ROP Trial 2011; the risk of these biases is not clear in the other two studies (Autrata 2012; Lepore 2014).
Potential biases in the review process
Most outcomes of the review were not reported in the included studies. The authors of the studies were contacted to collect additional information on these outcomes but no response was obtained.
Agreements and disagreements with other studies or reviews
The earlier systematic review Off‐label use of bevacizumab for severe retinopathy of prematurity, was published in 2009 (Micieli 2009). It included nine articles, of which six were case reports, two were retrospective studies, and one was a prospective case series. It found considerable variability in how bevacizumab is used for the treatment of ROP, and concluded that "further randomized control trials are warranted". The current review included three randomized trials ‐ two on intravitreal bevacizumab monotherapy and one on intravitreal pegaptanib combination therapy.
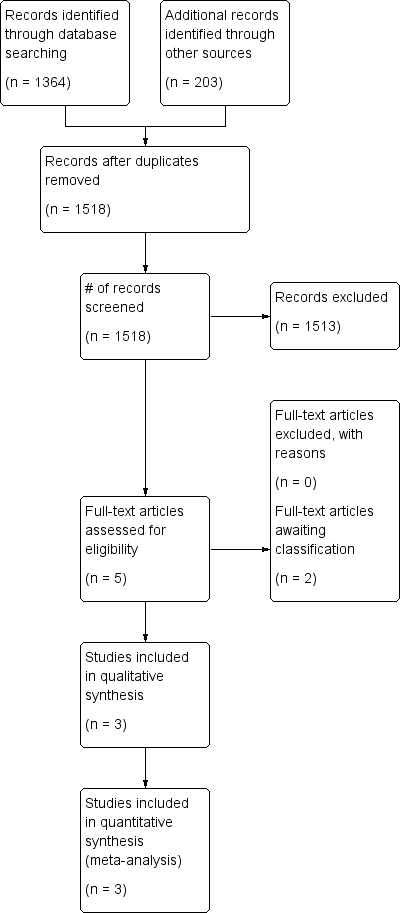
Study flow diagram.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 1 Structural outcome ‐ partial or complete retinal detachment.

Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 2 Structural outcome ‐ complete retinal detachment (unit of analysis: eyes).

Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 3 Refractive error ‐ very high myopia ‐ at 30 months of age (unit of analysis: eyes).
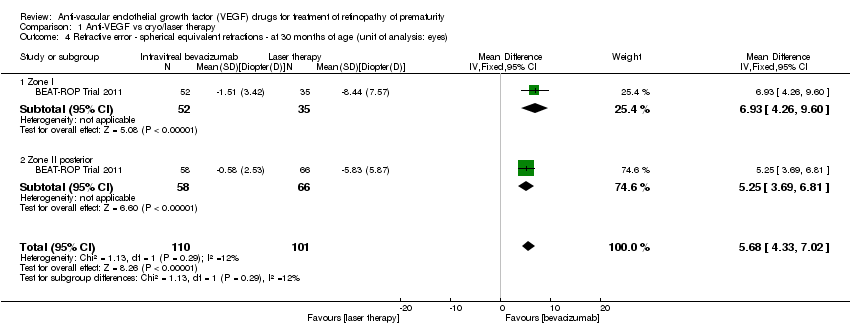
Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 4 Refractive error ‐ spherical equivalent refractions ‐ at 30 months of age (unit of analysis: eyes).

Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 5 Mortality before discharge from primary hospital.

Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 6 Mortality at 30 months of age.

Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 7 Local adverse effects ‐ corneal opacity requiring corneal transplant (unit of analysis: eyes).

Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 8 Local adverse effects ‐ lens opacity requiring cataract removal (unit of analysis: eyes).
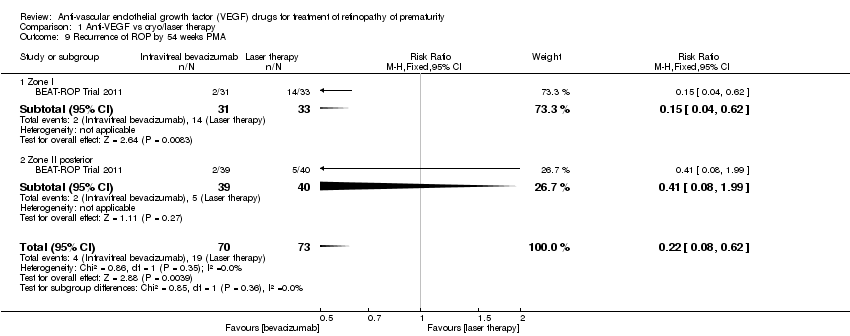
Comparison 1 Anti‐VEGF vs cryo/laser therapy, Outcome 9 Recurrence of ROP by 54 weeks PMA.
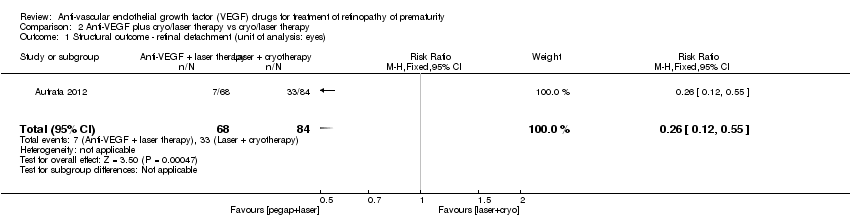
Comparison 2 Anti‐VEGF plus cryo/laser therapy vs cryo/laser therapy, Outcome 1 Structural outcome ‐ retinal detachment (unit of analysis: eyes).
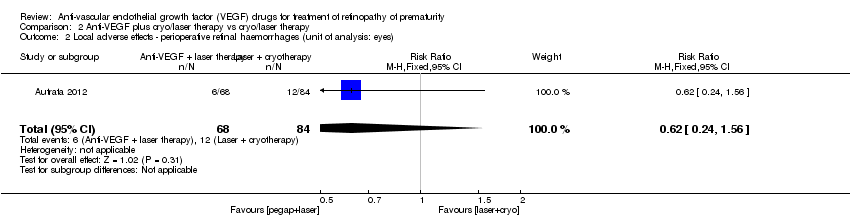
Comparison 2 Anti‐VEGF plus cryo/laser therapy vs cryo/laser therapy, Outcome 2 Local adverse effects ‐ perioperative retinal haemorrhages (unit of analysis: eyes).
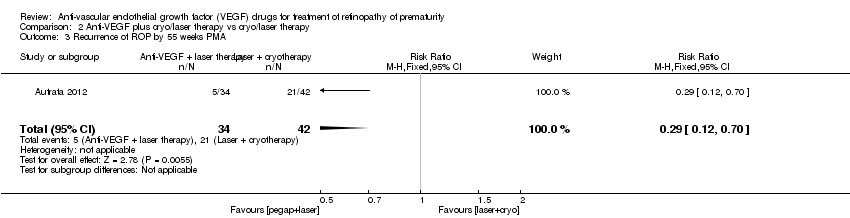
Comparison 2 Anti‐VEGF plus cryo/laser therapy vs cryo/laser therapy, Outcome 3 Recurrence of ROP by 55 weeks PMA.
| Intravitreal anti‐VEGF therapy compared to conventional laser/cryotherapy in preterm infants with type 1 ROP | |||||
| Patient or population: preterm infants with type 1 ROP | |||||
| Outcomes* | Illustrative comparative risks# (95% CI) | Relative effect | No of Participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| conventional laser/cryotherapy | intravitreal anti‐VEGF therapy | ||||
| Structural outcome ‐ retinal detachment | Study population | RR 1.04 | 143 | ⊕⊝⊝⊝ | |
| 27 per 1000 | 28 per 1000 | ||||
| Refractive error ‐ very high myopia ‐ at 30 months of age (unit of analysis: eyes) | Study population | RR 0.06 | 211 | ⊕⊕⊝⊝ | |
| 416 per 1000 | 25 per 1000 | ||||
| Mortality before discharge from primary hospital | Study population | RR 1.5 | 150 | ⊕⊕⊝⊝ | |
| 27 per 1000 | 40 per 1000 | ||||
| Mortality at 30 months of age | Study population | RR 0.86 | 150 | ⊕⊕⊝⊝ | |
| 93 per 1000 | 80 per 1000 | ||||
| Local adverse effects ‐ corneal opacity requiring corneal transplant (unit of analysis: eyes) | Study population | RR 0.34 | 286 | ⊕⊝⊝⊝ | |
| 7 per 1000 | 2 per 1000 | ||||
| Local adverse effects ‐ lens opacity requiring cataract removal (unit of analysis: eyes) | Study population | RR 0.15 | 286 | ⊕⊝⊝⊝ | |
| 21 per 1000 | 3 per 1000 | ||||
| Recurrence of ROP by 54 weeks PMA | Study population | RR 0.22 | 143 | ⊕⊕⊕⊝ | |
| 260 per 1000 | 57 per 1000 | ||||
| *Only the outcomes for which data are available are reported here; #The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Outcome assessment not blinded 295% CI around the pooled estimate includes both 1) no effect and 2) appreciable benefit or appreciable harm 3Number of events too small 4Serious risk of bias in analysis (unit of analysis error) 5Outcome assessment not blinded but outcome is objective | |||||
| Anti‐VEGF combined with laser/cryotherapy compared to laser/cryotherapy in preterm infants with type 1 ROP | |||||
| Patient or population: preterm infants with type 1 ROP | |||||
| Outcomes* | Illustrative comparative risks# (95% CI) | Relative effect | No of Participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| laser/cryotherapy | anti‐VEGF combined with laser/cryotherapy | ||||
| Structural outcome ‐ retinal detachment (unit of analysis: eyes) | Study population | RR 0.26 | 152 | ⊕⊕⊝⊝ | |
| 393 per 1000 | 102 per 1000 | ||||
| Local adverse effects ‐ perioperative retinal haemorrhages (unit of analysis: eyes) | Study population | RR 0.62 | 152 | ⊕⊝⊝⊝ | |
| 143 per 1000 | 89 per 1000 | ||||
| Recurrence of ROP by 55 weeks' PMA | Study population | RR 0.29 | 76 | ⊕⊕⊝⊝ | |
| 500 per 1000 | 145 per 1000 | ||||
| *Only the outcomes for which data are available are reported here; #The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Outcome assessment not blinded 2Serious risk of bias in analysis (unit of analysis error) 3Unclear risk of selection bias 495% CI around the pooled estimate includes both 1) no effect and 2) appreciable benefit or appreciable harm | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Structural outcome ‐ partial or complete retinal detachment Show forest plot | 1 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.21, 5.13] |
| 1.1 Zone I | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.26] |
| 1.2 Zone II posterior | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.13 [0.25, 103.45] |
| 2 Structural outcome ‐ complete retinal detachment (unit of analysis: eyes) Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.50] |
| 3 Refractive error ‐ very high myopia ‐ at 30 months of age (unit of analysis: eyes) Show forest plot | 1 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.02, 0.20] |
| 3.1 Zone I | 1 | 87 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.02, 0.30] |
| 3.2 Zone II posterior | 1 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.05 [0.01, 0.34] |
| 4 Refractive error ‐ spherical equivalent refractions ‐ at 30 months of age (unit of analysis: eyes) Show forest plot | 1 | 211 | Mean Difference (IV, Fixed, 95% CI) | 5.68 [4.33, 7.02] |
| 4.1 Zone I | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | 6.93 [4.26, 9.60] |
| 4.2 Zone II posterior | 1 | 124 | Mean Difference (IV, Fixed, 95% CI) | 5.25 [3.69, 6.81] |
| 5 Mortality before discharge from primary hospital Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.50 [0.26, 8.75] |
| 5.1 Zone I | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.07, 15.80] |
| 5.2 Zone II posterior | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [0.18, 20.71] |
| 6 Mortality at 30 months of age Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.30, 2.45] |
| 6.1 Zone I | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.16, 2.38] |
| 6.2 Zone II posterior | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.26, 8.31] |
| 7 Local adverse effects ‐ corneal opacity requiring corneal transplant (unit of analysis: eyes) Show forest plot | 1 | 286 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.26] |
| 7.1 Zone I | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Zone II posterior | 1 | 158 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.26] |
| 8 Local adverse effects ‐ lens opacity requiring cataract removal (unit of analysis: eyes) Show forest plot | 1 | 286 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.79] |
| 8.1 Zone I | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Zone II posterior | 1 | 158 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.79] |
| 9 Recurrence of ROP by 54 weeks PMA Show forest plot | 1 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.08, 0.62] |
| 9.1 Zone I | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.04, 0.62] |
| 9.2 Zone II posterior | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.08, 1.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Structural outcome ‐ retinal detachment (unit of analysis: eyes) Show forest plot | 1 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.12, 0.55] |
| 2 Local adverse effects ‐ perioperative retinal haemorrhages (unit of analysis: eyes) Show forest plot | 1 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.24, 1.56] |
| 3 Recurrence of ROP by 55 weeks PMA Show forest plot | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.12, 0.70] |

