Contenido relacionado
Revisiones y protocolos relacionados
Xudong Yang, Yao Cheng, Nansheng Cheng, Jianping Gong, Lian Bai, Longshuan Zhao, Yilei Deng | 15 marzo 2022
Daniel W Birch, Jerry T Dang, Noah J Switzer, Namdar Manouchehri, Xinzhe Shi, Ghassan Hadi, Shahzeer Karmali | 19 octubre 2016
Rashmi Verma, Richard L Nelson | 18 julio 2007
Iosief Abraha, Gian A Binda, Alessandro Montedori, Alberto Arezzo, Roberto Cirocchi | 25 noviembre 2017
Bobby VM Dasari, Damian McKay, Keith Gardiner | 19 enero 2011
Stefan Sauerland, Maren Walgenbach, Brigitte Habermalz, Christoph M Seiler, Marc Miserez | 16 marzo 2011
Wolfgang Schwenk, Oliver Haase, Jens J. Neudecker, Joachim M Müller | 20 abril 2005
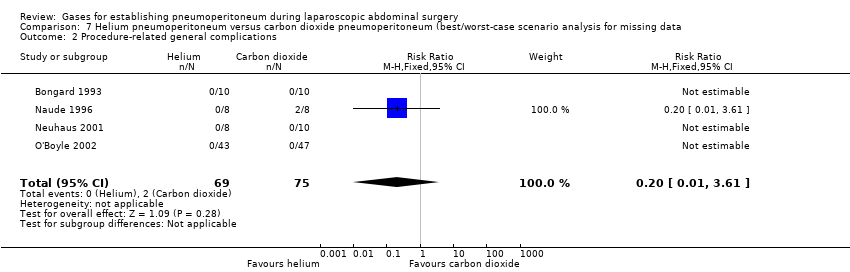
Kurinchi Selvan Gurusamy, Jessica Vaughan, Brian R Davidson | 18 marzo 2014
Senthil Kumar, Peng F Wong, David J Leaper | 21 enero 2009
Kirsty McCormack, Neil Scott, Peter M.N.Y.H Go, Sue J Ross, Adrian Grant, Collaboration the EU Hernia Trialists | 20 enero 2003