Konservative Maßnahmen zur Behandlung belastungsbedingter muskulotendinöser, ligamentärer und knöcherner Leistenschmerzen
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: single‐blinded randomized controlled trial Setting: Clinic of Sports Medicine, Department of Orthopaedic Surgery, Amager University Hospital, Copenhagen, Denmark | |
| Participants |
| |
| Interventions | 1. Exercise therapy (AT): 8 to 12 weeks; 3 times a week Module 1: first 2 weeks ‐ Static adduction against soccer ball placed between feet when lying supine (10 rep. of 30s, each) ‐ Static adduction against soccer ball placed between knees when lying supine (10 rep. of 30s, each) ‐ Abdominal sit‐ups both in straightforward direction and in oblique direction (5 series of 10 rep.) ‐ Combined abdominal sit‐ups and hip flexion, starting from supine position and with soccer ball between knees (5 series of 10 rep.) ‐ Balance training on wobble board (5 min) ‐ One‐foot exercises on sliding board, with parallel feet as well as with 90 angle between feet (5 sets of 1 min continuous work with each leg and in both positions)
Module 2: 2 to 6 weeks ‐ Leg abduction and adduction exercises performed in side lying (5 series of 10 rep. of each exercise ‐ twice) ‐ Low‐back extension exercises prone over end of couch (5 series of 10 rep. – twice) ‐ One‐leg weight pulling abduction/adduction standing (5 series of 10 rep. for each leg – twice) ‐ Abdominal sit‐ups both in straightforward direction and in oblique direction (5 series of 10 rep. – twice) ‐ One‐leg coordination exercise with flexing and extending knee and swinging arms in same rhythm (5 series of 10 rep. for each leg – twice) ‐ Training in sideways motion on mini‐skateboard (5 min) ‐ Balance training on wobble board (5 min) ‐ Skating movements on sliding board (5 sets of 1 min continuous work) 2. Conventional physiotherapy (PT): 8 to 12 weeks; twice a week ‐ Laser treatment with a gallium aluminium arsen laser. All painful points of the adductor‐tendon insertion at the pubic bone received treatment for 1 min, receiving 0·9 mJ per treated point. The probe was in contact with the skin at 90° angle. The laser was fitted with an 830 nm (±0·5 nm) 30 mW, diode beam divergence was 4° and area of probe head was 2·5 mm2 ‐ Transverse friction massage for 10 min on painful area of adductor‐tendon insertion into pubic bone ‐ Stretching of adductor muscles, hamstring muscles, and hip flexors. The contract‐relax technique was used. The stretching was repeated three times and the duration of each stretch was 30 s ‐ Transcutaneous electrical nerve stimulation was given for 30 min at painful area. The apparatus used was a Biometer, Elpha 500, frequency 100 Hz and a pulse width of one and a maximum of 15 mA (100% effect) Treatment was given or instructed by physiotherapists and in both groups a return to running program was done after 6 weeks. | |
| Outcomes |
‐ No pain at palpation of the adductors tendon or during resisted adduction ‐ No pain in connection with or after athletic activity in the same sport and at the same level of competition ‐ Return to sports at the same level without groin pain If all three measures above were reached, the result was labelled excellent, if two measures were reached, the result was good, if one measure was reached, the result was fair and if no measures were reached, the result was poor.
Outcomes were evaluated at 16 weeks and long‐term (8 to 12 years) follow‐up. | |
| Notes | ‐ The participants from AT group were treated in groups with two to four patients, while in PT group the treatment was individual ‐ A longer‐ term follow‐up of Hölmich 1999 (8 to 12 years from the original study) was included (Hölmich 2011) ‐ Percentage of lost participants (follow‐up of 16 weeks): 13% (9/68); 5 losses from AT group and 4 from PT group ‐ Reasons for withdrawn (follow‐up of 16 weeks): knee injury (one patient); immigration to Australia (one); loss to follow‐up at 4 months (two); did not want the treatment they were assigned (two patients assigned AT); could not get sufficient time off from work to complete the study (three) ‐ Percentage of lost participants (follow‐up of 8 to 12 years): 31% (21/68); 10 losses from AT group and 11 from PT group ‐ Reasons for withdrawal (follow‐up of 8 to 12 years): 5 individuals could not be located; 4 because of lack of current address 1 because of emigration; 5 were not interested primarily because they would have to take time off work to attend the examination, and 2 could not participate because they had suffered serious disability due to an accident not related to their groin problem | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly allocated by sealed, opaque, and serially numbered envelope to AT or PT group by means of block randomisation (block size four)" |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomly allocated by sealed, opaque, and serially numbered envelope to AT or PT group by means of block randomisation (block size four)" Quote: "The examining physician was not involved in the randomisation procedure and remained unaware of the treatment allocation" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and physiotherapists could not be blinded to allocation treatment |
| Blinding of outcome assessment (detection bias) | Unclear risk | While the examining physician was not involved in the randomization procedure and remained unaware of the treatment allocation, there were subjective outcomes (successful treatment and patients' subjective global assessment) assessed by the trial participants, who were not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | While the study participant flow was clear and the missing data were balanced across groups, with reasons for missing data provided, the characteristics of lost participants were not described. The analyses were not entirely 'intention to treat', nor were sensitivity analyses to address decisions regarding handling missing data. Quote: "The subjective global assessment of the effect of treatment in the two groups based solely on results from patients completing the study (per‐protocol analysis)" |
| Selective reporting (reporting bias) | Unclear risk | Function (an important primary outcome) was not evaluated. No protocol available. |
| Other bias | High risk | There was no explicit information about supplementary treatment and physical activity of participants during the follow‐up period (8 to 12 years). |
| Methods | Study design: single‐blinded randomized controlled trial Setting: The Hague Medical Centre, Antoniushove hospital, Department of Sports Medicine. Leidschendam, the Netherlands | |
| Participants |
| |
| Interventions | 1. Multi‐modal treatment group (MMT): heat + manual therapy + stretching. ‐ Maximum two sessions of manual therapy and heat, and 15 days of stretching (the stretches were done after a 5 min warming‐up using jogging or cycling). Before the manual therapy the adductor muscle group is warmed using paraffin packs for 10 min ‐ The manual therapy technique consists of: with the patient in a supine position, the contralateral hand is used to control the tension in the adductor muscles while the ipsilateral hand is used to move the hip from a neutral position into flexion, external rotation and abduction while keeping the knee in extension. The treating physician controls the tension subjectively and applies the maximum tolerable stretch to the adductor muscles. After the movement has been performed the adductor muscle group is compressed with one hand while the other hand moves the hip into adduction and slight flexion. This circular motion followed by compressions lasts about 25 s and is repeated three times in one treatment session 2. Exercise therapy group (ET): 8 to 12 weeks; 3 times a week. Module 1: first 2 weeks ‐ Static adduction against soccer ball placed between feet when lying supine (10 rep. of 30s, each) ‐ Static adduction against soccer ball placed between knees when lying supine (10 rep. of 30s, each) ‐ Abdominal sit‐ups both in straightforward direction and in oblique direction (5 series of 10 rep.) ‐ Combined abdominal sit‐ups and hip flexion, starting from supine position and with soccer ball between knees (5 series of 10 rep.) ‐ Balance training on wobble board (5 min) ‐ One‐foot exercises on sliding board, with parallel feet as well as with 90 angle between feet (5 sets of 1 min continuous work with each leg and in both positions)
Module 2: 2 to 6 weeks ‐ Leg abduction and adduction exercises performed in side lying (5 series of 10 rep. of each exercise‐ twice) ‐ Low‐back extension exercises prone over end of couch (5 series of 10 rep. – twice) ‐ One‐leg weight pulling abduction/adduction standing (5 series of 10 rep. for each leg – twice) ‐ Abdominal sit‐ups both in straightforward direction and in oblique direction (5 series of 10 rep. – twice) ‐ One‐leg coordination exercise with flexing and extending knee and swinging arms in same rhythm(5 series of 10 rep. for each leg – twice) ‐ Training in sideways motion on mini‐skateboard (5 min) ‐ Balance training on wobble board (5 min) ‐ Skating movements on sliding board (5 sets of 1 min continuous work) In both groups a return to running program was done after treatment. | |
| Outcomes |
‐ No pain in connection with or after athletic activity in the same sport and at the same level of competition ‐ No pain during resisted adduction or on palpation of the adductors tendon at the pubic bone insertion ‐ Return to sports at the same level without groin pain If all three measures above were reached, the result was labelled excellent, if two measures were reached, the result was good, if one measure was reached, the result was fair and if no measures were reached, the result was poor.
Outcomes were evaluated at 16 weeks follow‐up. | |
| Notes | The participants from exercise therapy (ET) were not supervised while performed the exercises. They were only instructed on how to perform it. Percentage of participants lost to follow‐up: 11% (6/59); 3 losses from ET group and 3 from MMT group Reasons for withdrawal: did not want the treatment they were assigned (three patients); ankle injury (one patient); low‐back pain (one patients); and lost to follow‐up (one patient) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After informed consent and inclusion the athletes were randomised using sealed envelopes.The athlete chose one of 100 opaque envelopes in the presence of the department’s secretary" |
| Allocation concealment (selection bias) | Low risk | Quote: "After informed consent and inclusion the athletes were randomised using sealed envelopes.The athlete chose one of 100 opaque envelopes in the presence of the department’s secretary" Quote: "The examining physician was not involved in the randomisation process and remained unaware of the treatment allocation" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and physiotherapists could not be blinded to allocation treatment |
| Blinding of outcome assessment (detection bias) | Unclear risk | While the examining physician was not involved in the randomization procedure and remained unaware of the treatment allocation, there were subjective outcomes (Successful treatment) assessed by the trial participants, who were not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Although missing data were balanced across groups and reasons for missing data were provided, the characteristics of the lost participants were not described. Furthermore, a per protocol analysis was done |
| Selective reporting (reporting bias) | Unclear risk | Function (an important primary outcome) was not evaluated. No protocol available |
| Other bias | Low risk | No other source of bias was detected |
rep. = repetitions
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Conservative treatment versus surgical treatment; not in review scope | |
| Conservative treatment versus surgical treatment; not in review scope |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Randomized controlled, parallel group trial |
| Participants | Male athletes, 18 to 45 years old, hip adduction‐related complaints, for a period of at least six weeks, strong desire to compete in sports |
| Interventions | Two different kinds of physiotherapeutic treatments are given for the population. Both treatment strategies are already in use in daily practice. |
| Outcomes | 1. Severity of the pain over the last three days (11‐point visual analogue scale (VAS)) 2. Participation in sports (11‐point VAS) 4. Global change (six‐point Likert scale) |
| Notes | The author of this study was contacted via email and reported that the trial was not completed as a randomized clinical trial and therefore the results have not been published. |
VAS = visual analogue scale
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 'Successful treatment' Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 1 'Successful treatment'. | ||||
| 1.1 Follow‐up 16 weeks, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up 8 to 12 years, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Follow‐up 8 to 12 years, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Patients' subjective global assessment (better or much better) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 2 Patients' subjective global assessment (better or much better). | ||||
| 2.1 Follow‐up 16 weeks, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Follow‐up 16 weeks, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Follow‐up 8 to 12 years, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Follow‐up 8 to 12 years, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Return to sports Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3 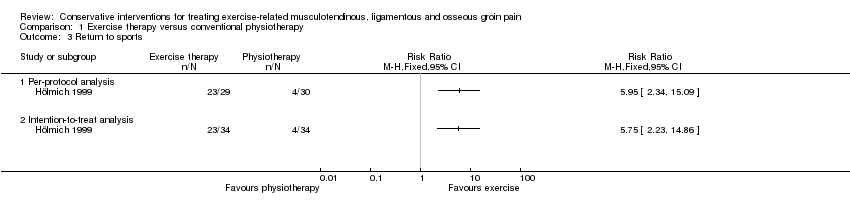 Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 3 Return to sports. | ||||
| 3.1 Per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 'Successful treatment' Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 1 'Successful treatment'. | ||||
| 1.1 Per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Maximum pain during sports Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 2 Maximum pain during sports. | ||||
| 3 Return to sports Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 3 Return to sports. | ||||
| 3.1 Per protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Time to return to sports (weeks) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.4 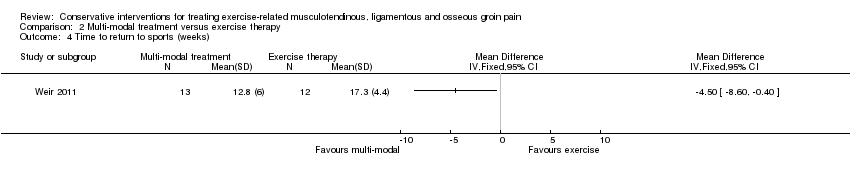 Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 4 Time to return to sports (weeks). | ||||

Flow diagram showing the reference screening and study selection.
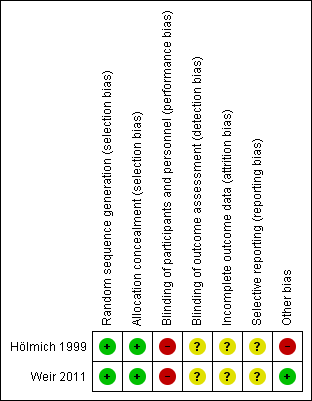
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
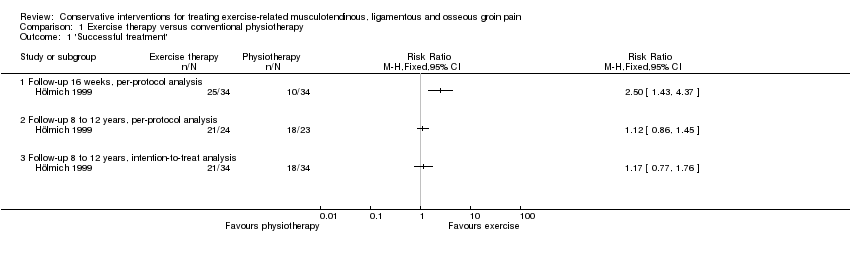
Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 1 'Successful treatment'.

Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 2 Patients' subjective global assessment (better or much better).

Comparison 1 Exercise therapy versus conventional physiotherapy, Outcome 3 Return to sports.
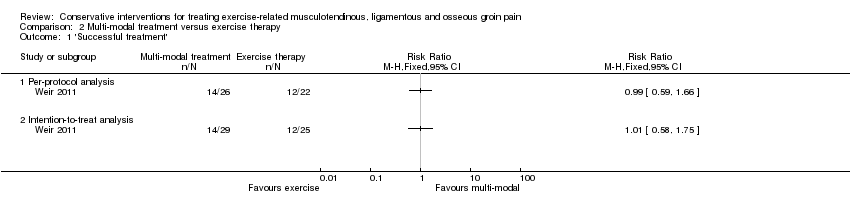
Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 1 'Successful treatment'.
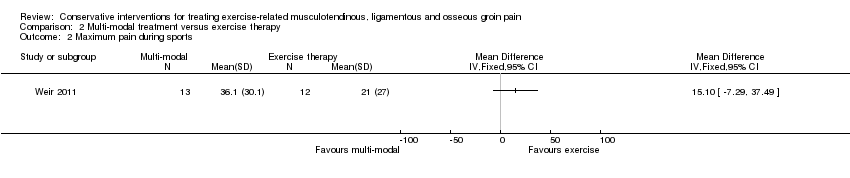
Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 2 Maximum pain during sports.

Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 3 Return to sports.

Comparison 2 Multi‐modal treatment versus exercise therapy, Outcome 4 Time to return to sports (weeks).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 'Successful treatment' Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Follow‐up 16 weeks, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Follow‐up 8 to 12 years, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Follow‐up 8 to 12 years, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Patients' subjective global assessment (better or much better) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Follow‐up 16 weeks, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Follow‐up 16 weeks, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Follow‐up 8 to 12 years, per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 Follow‐up 8 to 12 years, intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Return to sports Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 'Successful treatment' Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Per‐protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Maximum pain during sports Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Return to sports Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 Per protocol analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intention‐to‐treat analysis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Time to return to sports (weeks) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |

