Usporedba umjetnih rožnica i donorskih rožnica u slučajevima ponovljenih presađivanja rožnice
Abstract
Background
Individuals who have failed one or more full thickness penetrating keratoplasties (PKs) may be offered repeat corneal surgery using an artificial or donor cornea. An artificial or prosthetic cornea is known as a keratoprosthesis. Both donor and artificial corneal transplantations involve removal of the diseased and opaque recipient cornea (or the previously failed cornea) and replacement with another donor or prosthetic cornea.
Objectives
To assess the effectiveness of artificial versus donor corneas in individuals who have had one or more failed donor corneal transplantations.
Search methods
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (2013, Issue 10), Ovid MEDLINE, Ovid MEDLINE In‐Process and Other Non‐Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE (January 1946 to November 2013), EMBASE (January 1980 to November 2013), Latin American and Caribbean Health Sciences Literature Database (LILACS) (January 1982 to November 2013), the metaRegister of Controlled Trials (mRCT) (www.controlled‐trials.com), ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). We did not use any date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 27 November 2013.
Selection criteria
Two review authors independently assessed reports from the electronic searches to identify randomized controlled trials (RCTs) or controlled clinical trials (CCTs). We resolved discrepancies by discussion or consultation with a third review author.
Data collection and analysis
For discussion purposes, we assessed findings from observational cohort studies and non‐comparative case series. No data synthesis was performed.
Main results
We did not identify any RCTs or CCTs comparing artificial corneas with donor corneas for repeat corneal transplantations.
Authors' conclusions
The optimal management for those individuals who have failed a conventional corneal transplantation is not known. Currently, in some centers, artificial corneal devices routinely are recommended after just one graft failure, and in others, not until after multiple graft failures, or not at all. To date, there have been no controlled trials comparing the visual outcomes and complications of artificial corneal devices (particularly the Boston type 1 keratoprosthesis which is the most commonly implanted artificial corneal device) with repeat donor corneal transplantation, in order to guide surgeons and their patients. It is apparent that such a trial is needed and would offer significant benefit to an ever‐increasing pool of people with visual disability due to corneal opacification, most of whom are still in productive stages of their lives.
PICO
Laički sažetak
Usporedba umjetnih rožnica i ljudskih donorskih rožnica u slučajevima ponovljenih presađivanja rožnice
Istraživačko pitanje
Cilj autora je bio usporediti uspješnost presađivanja umjetnih rožnica (prednjeg dijela oka) i ljudskih donorskih rožnica u ljudi kojima je već neuspješno presađena barem jedna donirana rožnica.
Dosadašnje spoznaje
Postoji više načina presađivanja rožnice. Način presađivanja ovisi o tome koliki je dio rožnice uklonjen i zamijenjen. Uklanjanje i zamjena cijele rožnice zove se na engleskom jeziku „full thickness penetrating keratoplasty“ (PK). Ako se samo dio rožnice uklanja i zamjenjuje istim dijelom rožnice donora, operacija se imenuje prema dijelovima rožnice koji se presađuju (npr. endotelna keratoplastika (EK) se odnosi na presađivanje unutarnjih ili endotelnih slojeva rožnice).
Presađivanje rožnice jedno je od najuspješnijih presađivanja tkiva ili organa. Međutim, ponekad presađivanje ne bude uspješno i tkivo davatelja postane neprozirno (zamućeno). U ovom sustavnom pregledu analizirana su istraživanja u kojima su proučavane samo osobe koje su imale barem jednu neuspješnu PK i kojima je bila potrebna dodatna operacija rožnice.
U nekim zdravstvenim ustanovama umjetne rožnice se preporučuju nakon što je bolesnik imao samo jedan neuspjeh pri donorskoj PK; u drugim ustanovama umjetna rožnica se ne preporučuje prije nego što je bolesnik imao nekoliko neuspješnih donorskih PK. U nekim ustanovama umjetna rožnica se ni ne nudi. Trenutačno ne postoje smjernice po pitanju broja donorskih presađivanja rožnice koje se mogu izvoditi na oku na kojem je presađivanje rožnice bilo neuspješno.
Presađivanje rožnice donorskom ili umjetnom rožnicom (poznato kao keratoprostetika) obuhvaća uklanjanje zamućene rožnice i zamjenu prozirnom rožnicom ili rožničnom napravom. Neki primjeri keratoprostetike (KPros) su Boston KPro (vrste I i II), AlphaCor, osteoodontokeratoprostetika (OOKP) i Fyodorov‐Zuevov KPro. Boston KPro je najčešća umjetna rožnična naprava koja se usađuje.
Glavni rezultati i zaključci
Nisu pronađena kontrolirana istraživanja koja bi usporedila uspješnost, uključujući vid i popratne pojave, presađivanja umjetnih rožnica i donorskih rožnica u ljudi kojima su prethodna presađivanja donorske rožnice bila neuspješna. Najbolje liječenje za pacijente s neuspjelim PK nije poznato. Ne postoje dokazi visoke kakvoće koji bi uputili kirurge i bolesnike na najbolje liječenje nakon što donorsko presađivanje ne uspije. Dakle, potrebna su dodatna istraživanja koja uspoređuju uporabu umjetnih i ljudskih donorskih rožnica nakon neuspjele PK. Usporedna klinička istraživanja su potrebna da ponude činjenice koje nedostaju. Ta bi istraživanja bila vrlo korisna za liječenje sve većeg broja osoba s oštećenjem vida uzrokovanim zamućenom rožnicom, od kojih je većina u radnoj ili školskoj dobi.
Authors' conclusions
Background
Description of the condition
The cornea is the transparent layer of the anterior surface of the eye and functions to transmit light and provide most of the refractive power of the eye. Diseases affecting the cornea are a major cause of blindness worldwide. Globally, corneal opacity is the fourth leading cause of bilateral blindness after cataract, glaucoma, and age‐related macular degeneration, affecting some four to eight million people, 90% of whom live in the developing world (Murthy 2012; Whitcher 2001). Furthermore, unilateral corneal blindness, which also creates much disability, is not reflected in these statistics. Additionally, children and young adults are affected by corneal blindness proportionately more than by other major blinding diseases, such as macular degeneration and glaucoma, which are associated with aging.
Unfortunately, there are currently no proven medical treatments available to restore clarity in diseased corneas. Surgery with donor corneal transplantation (keratoplasty) is the definitive treatment for corneal blindness. Although the majority of these transplants are successful, if the transplantation fails the first time for any reason, a repeat transplantation using an artificial or donor cornea may be considered.
Description of the intervention
Corneal transplantation is one of the most commonly performed transplant procedures in the developed world. A total of 46,892 corneal transplantations were performed in the United States in 2013 (EBAA 2013). Successful transplantation occurs when the corneal graft is not rejected and it retains clarity and integrity. Several recently published studies documented that the single most important factor affecting the success of corneal transplantation is the pre‐operative indication for the surgery (Thompson 2003; Wagoner 2009). Donor corneal transplantation achieves remarkable overall success rates with approximately 90% of "low risk" patients having successful transplants (ACGR 1993; Thompson 2003; Wagoner 2009). Patients at "low risk" of corneal graft failure typically suffer vision loss from corneal shape problems (such as keratoconus) or from loss of clarity due to genetic problems of the endothelial layer of the cornea (such as Fuchs endothelial dystrophy), trauma or infection. For example, although the five‐year survival probability is usually over 90% for keratoconus, this rate is less than 50% when the indication is corneal edema due to endothelial failure from intraocular surgery, and even lower when the eye is aphakic (without the natural lens) (ACGR 1993; Thompson 2003).
The likelihood of corneal graft survival drops markedly in the setting of previous corneal graft failure. Re‐graft (repeat donor corneal transplantation), presence of significant neovascularization of the host bed, history of glaucoma and previous herpetic infection also decrease the likelihood of graft survival (ACGR 1993; Siganos 2010; Thompson 2003; Wagoner 2009). Overall risk of failure for re‐grafts is about 50% at five years (Thompson 2003; Yildiz 2010), although this percentage is probably an underestimate as most surgeons tend to limit re‐grafting only to patients in whom they believe there is a reasonable chance of success for subsequent graft survival and improvement in visual acuity. Of note, about 10% to 16% of all corneal transplants around the world are re‐grafts (EBAA 2013; Thompson 2003; Yildiz 2010).
In the United States, patients who have failed multiple corneal grafts may be offered an artificial cornea. An artificial or prosthetic cornea, known as a keratoprosthesis (KPro), is a corneal implant made of synthetic material, the most common of which is the Boston keratoprosthesis (Boston KPro). The Boston KPro is a two piece, collar‐button device made of polymethylmethacrylate (PMMA), a transparent thermoplastic, with a titanium locking ring. Although it is associated with some complications, such as infection, extrusion, glaucoma, and retinal detachment, because it is made of artificial material it will not opacify (become cloudy). The AlphaCor device, made from poly‐2‐hydroxyethyl methacrylate, is made of a one‐piece flexible implant with a peripheral skirt and a transparent central region connected on a molecular level by an interpenetrating polymer network. It is implanted in the recipient eye via a two‐stage surgical procedure. Osteo‐odonto‐keratoprosthesis, reserved for individuals with severe ocular surface disorders, requires a complex multi‐step surgical procedure and, therefore, is performed very infrequently. A lamina of the patient's tooth is grafted into the eye after having been transplanted elsewhere for biointegration and vascularization purposes. An artificial optic made of PMMA is then installed in the unit to allow vision. The Fyodorov–Zuev keratoprosthesis, commonly used in the former Soviet Union, is made of a titanium supporting plate with two large openings to allow aqueous humor to flow anteriorly. An optical cylinder is screwed into the center of the supporting plate, then the assembled device is implanted.
In general, artificial corneal implantation requires long‐term topical and sometimes oral treatment to prevent or treat complications such as infections and glaucoma. Close postoperative follow‐up is required due to risk of complications, which can sometimes lead to permanent blindness, particularly due to retinal detachment and endophthalmitis. These complication rates have been well monitored by surveillance studies (Boston Type 1 KPro Study; Hicks 2006). The rates of vision‐threatening complications and visual outcomes on the other hand are less well studied in repeat donor corneal transplantation cases. However, the rates of corneal melting and infection certainly are expected to be lower with donor transplantation than with artificial devices.
How the intervention might work
Both donor and artificial corneal transplantations involve removal of the diseased and opaque portion of the recipient cornea, and replacement with clear cornea or corneal device. The surgical procedure using an artificial cornea is similar to full thickness corneal transplantation using a donor cornea (penetrating keratoplasty, PK) once the device has been assembled.
The Boston KPro, the most commonly implanted artificial corneal device, comes in two main types (Aquavella 2005; Ilhan‐Sarac 2005; Ma 2005). Type I is the most commonly used style in the United States. It consists of two plastic parts: an anterior part which houses the refractive portion, and a removable perforated back plate. The device requires donor corneal tissue to be sandwiched between the two plates. The holes in the back plate are thought to enhance nutrition and rehydration of the clamped corneal stroma adjacent to the stem, which may help to prevent necrosis of the surrounding tissue. In addition, the device has a titanium locking c‐ring to secure the unit after its assembly and prevent unscrewing of the back plate. After assembly, the whole device is then sutured into the recipient eye in the same manner as with donor corneal transplantation. A newer generation type I KPro with a back plate made of titanium recently has been approved by the United States Food and Drug Administration (MEEI 2013). This model does not require a locking c‐ring (Todani 2011).
The type I Boston KPro is indicated in eyes with sufficient tear secretion and normal blinking. The longer type II device is similar to type I, except for an additional 2 mm long anterior nub for through‐the‐lid implantation. The front plate is usually 5 mm in diameter and the back plate is 8.5 mm in diameter. The back plate also has two rows of eight holes, each 1.5 mm in diameter. The type II Boston KPro is reserved for extreme dry eye conditions and end‐stage ocular surface diseases with significant cicatricial conjunctival changes, such as mucous membrane pemphigoid (MMP) and Stevens Johnson syndrome (SJS), in which there is a lack of fornices to support a contact lens as recommended for the type I device. Both types are custom made to have a range of dioptric powers to match the axial length of the patient’s eye when aphakic (the natural lens, if present, is removed during surgery and no additional intraocular lens needs to be implanted).
Other artifical corneas such as AlphaCor, osteo‐odonto‐keratoprosthesis, and Fyodorov–Zuev keratoprosthesis, work in the same general manner, as substitutes for donor corneas.
Why it is important to do this review
There has been a renewed interest in artificial corneal implantation following the approval of AlphaCor device in 2002 by US Food and Drug Administration (FDA). Although the Boston type I device was cleared by US FDA in 1992, prior to 2004, fewer than 100 had been implanted, most of which were performed at the Massachusetts Eye and Ear Infirmary (the distributor of the device) (Zerbe 2006). This renewed interest resulted in a wealth of studies evaluating artificial corneal devices. However, due to high complication rates associated with the AlphaCor, the device has been removed from the market, leaving the artificial corneal device arena mostly to the Boston KPro. Once considered a last resort, the Boston KPro is now frequently a viable alternative for eyes with prior failure of traditional donor penetrating keratoplasty. Furthermore, there has been interest in expanding indications for KPro implantation as a primary procedure in patients with limbal stem cell failure from various causes (Michael 2008; Utine 2011).
As surgeons and centers have gained more experience with keratoprosthesis, it has become apparent that artificial corneal devices may be an alternative to repeat PK in a broader subset of patients than previously considered. It also has been suggested that artificial corneal transplant surgery is comparable to PK surgery using donor corneas in terms of cost‐effectiveness (Ament 2010). The purpose of this review was to compare systematically the clinical performance of artificial corneas with the current standard of care, transplantation with donor corneas, as the use of keratoprostheses is becoming more popular for repeat corneal replacement procedures.
Objectives
To assess the effectiveness of artificial versus donor corneas in individuals who have had one or more failed donor corneal transplantations.
Methods
Criteria for considering studies for this review
Types of studies
We planned to include randomized controlled trials (RCTs) and quasi‐randomized controlled clinical trials (CCTs). We also stated a priori that we would discuss findings from non‐RCTs, prospective and retrospective cohort studies, and interventional case series (Akpek 2012). We excluded from our discussion of the latter group of studies those that reported on fewer than 10 individuals/cases. We grouped multiple reports from the same study when authors reported only information on the same group of participants (e.g. results from longer follow‐up, data for subsets of participants).
Types of participants
We included studies of participants with corneal opacity who had failed one or more full thickness PKs. We excluded reports of primary keratoprosthesis cases only. We included studies with adults (ages 18 years and older), but did not exclude studies that also included some participants less than 18 years of age. However, we excluded the studies that reported results exclusively or mostly from pediatric patients. There was no restriction regarding whether participants were phakic, aphakic, or pseudophakic.
Types of interventions
We included artificial corneas (keratoprostheses) of any type and full thickness, and penetrating human donor corneal transplantations. We excluded studies of anterior or posterior (endothelial) lamellar corneal transplantations for previous graft failures. We also reported each type of artificial cornea (e.g. Boston KPro, AlphaCor, osteo‐odonto‐keratoprosthesis, and Fyodorov‐Zuev KPro) individually.
Types of outcome measures
Primary outcomes
The primary outcome for comparison of corneal transplant procedures was the proportion of participants with best‐corrected visual acuity (BCVA) of 20/100 or better, measured as Snellen equivalent, at two years after corneal replacement.
Secondary outcomes
Secondary outcomes for comparison of corneal transplant procedures included:
-
the proportion of participants with BCVA of 20/100 or better at one and five years after corneal replacement;
-
the proportion of participants with worse vision than pre‐operative vision at one, two and five years after corneal replacement;
-
the mean change in BCVA at one, two and five years after corneal replacement;
-
the proportion of participants with corneal graft failure at one, two and five years after corneal replacement;
-
PK group: the proportion of participants with corneal allograft rejection or failure leading to opacity of the graft at one, two and five years after corneal replacement;
-
KPro group: the proportion of participants with removal of KPro due to any cause at one, two and five years after corneal replacement;
-
-
the proportion of participants with enucleation of the eyeball due to any cause at one, two and five years after corneal replacement.
When data were available, we reported the proportion of participants with failure who required another corneal surgery with a donor or artificial cornea, and the proportion of participants who had complications requiring other surgery, such as glaucoma and retinal detachment.
We also summarized adverse events reported by the individual studies, including glaucoma, infection, retinal detachment, retroprosthetic membrane formation and further extrusion of the device. We planned to compare quality of life outcomes and economic outcomes; however, these outcomes were not reported by eligible studies.
Search methods for identification of studies
Electronic searches
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (2013, Issue 10), Ovid MEDLINE, Ovid MEDLINE In‐Process and Other Non‐Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE (January 1946 to November 2013), EMBASE (January 1980 to November 2013), Latin American and Caribbean Health Sciences Literature Database (LILACS) (January 1982 to November 2013), the metaRegister of Controlled Trials (mRCT) (www.controlled‐trials.com), ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). We did not use any date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 27 November 2013.
See: Appendices for details of search strategies for CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), LILACS (Appendix 4), mRCT (Appendix 5), ClinicalTrials.gov (Appendix 6) and the ICTRP (Appendix 7).
Searching other resources
We searched the reference lists of relevant studies for any additional studies not identified by the electronic searches. We planned to use the Science Citation Index to identify potentially relevant studies that cited included studies; however, since no RCTs or CCTs were included, we did not use this database. We contacted experts in the field for information on current, past or unpublished trials, but no RCTs or CCTs were identified (KPro Study Group Bibliography 2013).
Data collection and analysis
Selection of studies
Two pairs of review authors (SN and FH; KL and MA) assessed the search results independently. Authors classified each record based on title and abstract as: (1) definitely relevant, (2) possibly relevant, or (3) definitely not relevant according to the 'Criteria for considering studies for this review'. No relevant RCTs or CCTs were identified; thus, we classified no records as (1) definitely relevant. We resolved discrepancies by consensus for non‐randomized studies assessed as (2) possibly relevant. For consideration of non‐randomized studies to include in discussion, we obtained full text copies of reports and two authors working independently assessed each as (a) include for discussion, (b) exclude from discussion, or (c) exclude, not relevant. Studies assessed as (a) include for discussion are listed in the review as Excluded studies. Studies assessed as (b) exclude from discussion or (c) exclude, not relevant are summarized, but not listed individually in the Results section under 'Excluded studies'. We resolved discrepancies by consensus. No study was classified as unclear after review of the full text and there were no study reports in languages that we required to be translated.
Data extraction and management
Two pairs of review authors (SN and FH; KL and MA) extracted data independently onto data extraction forms adapted from Cochrane Eyes and Vision Group forms. Study characteristics extracted for each relevant study included methods, participants, interventions, outcomes, and funding sources. One review author entered the data into Review Manager (RevMan 2014) and a second review author verified the data entered. We resolved discrepancies by discussion. We did not contact primary investigators of observational studies to request missing data; instead we used the information as available in the published reports.
Assessment of risk of bias in included studies
Two review authors assessed independently the sources of systematic bias in studies according to the methods described in Chapter 8 (Higgins 2011) and Chapter 13 (Reeves 2011) of the Cochrane Handbook for Systematic Reviews of Interventions. We resolved discrepancies through discussion.
We planned to consider the following parameters when assessing risk of bias in RCTs and CCTs: (a) selection bias (random sequence generation, quality of allocation concealment); (b) detection bias (masking of outcome assessors and data analyzers); (c) attrition bias (completeness of follow‐up, intention‐to‐treat (ITT) analysis); (d) reporting bias; and (e) other potential sources of bias (such as funding source). We did not plan to assess masking (blinding) of study participants and personnel (performance bias) due to the differences in interventions and surgical procedures. Each risk of bias parameter was to be assessed as having a "low risk of bias", a "high risk of bias" or an "unclear risk of bias" (insufficient information to permit judgment of low or high risk).
Although a formal assessment of risk of bias was not done for observational studies, we considered the following parameters when discussing cohort studies: (a) selection bias (similarity between groups, reporting of baseline characteristics and potential confounders); (b) performance bias (objective measurements of exposures); (c) detection bias (masking of outcome assessors, objective measurements of outcomes, equal likelihood of detecting outcome for both groups); (d) attrition bias (low attrition rates, similar follow‐up between groups); (e) reporting bias; and (f) other potential sources of bias (such as funding source).
Risk of bias considerations for non‐comparative studies included: (a) selection bias (consecutive versus preferential selection of participants); (b) performance bias and detection bias (objective measurements of exposures and outcomes); (c) attrition bias (rate of loss to follow‐up); (d) reporting bias; and (e) other potential sources of bias (such as funding source).
Measures of treatment effect
The primary outcome for this review was a dichotomous outcome. We planned to report the measure of effect as a risk ratio with 95% confidence intervals. We planned to report dichotomous secondary outcomes in the same manner.
We planned to report mean changes in BCVA as mean differences between groups with 95% confidence intervals. We also planned to report continuous data for quality of life outcomes or economic outcomes as mean differences with 95% confidence intervals.
Unit of analysis issues
The unit of analysis was the eye. For studies in which both eyes of a single participant were included, we reported whether or not adjustments for inter‐person correlation of outcomes were made.
Dealing with missing data
No RCTs or CCTs were included in the review and we did not contact study authors of non‐randomized studies for additional information.
Assessment of heterogeneity
We planned to use the I² statistic to examine heterogeneity. An I² value greater than 60% would have been interpreted as indicating substantial statistical heterogeneity. If substantial statistical heterogeneity was present, we did not plan to conduct meta‐analysis and instead would have reported the study results independently. We also planned to assess clinical heterogeneity based on the characteristics of participants in the included studies, including type of artificial cornea, lens status (phakic, aphakic, or pseudophakic), age, and underlying co‐morbidities (such as retinal detachment, glaucoma, and ocular surface disease).
Assessment of reporting biases
We planned to examine the symmetry of funnel plots to assess reporting biases when more than 10 studies were included in a meta‐analysis.
Data synthesis
We did not perform quantitative data synthesis.
Subgroup analysis and investigation of heterogeneity
We did not perform subgroup analysis.
Sensitivity analysis
We did not perform sensitivity analysis.
Results
Description of studies
Results of the search
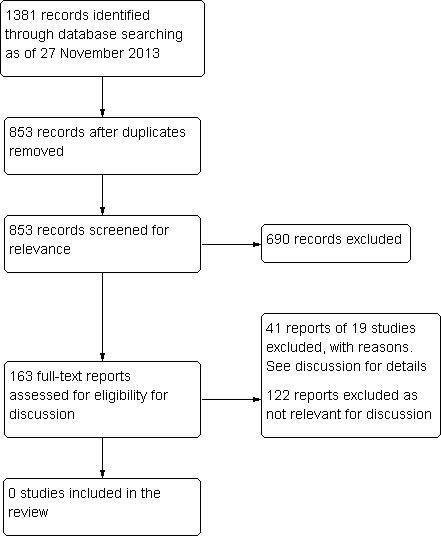
We identified a total of 853 unique records by the electronic searches as of 27 November 2013 (Figure 1). After screening of titles and abstracts, we did not identify any relevant RCTs or CCTs comparing artificial versus donor corneas in people undergoing repeat corneal transplantation. Of the 853 records from the search, we excluded 690 records and reviewed full‐text reports for 163 potentially relevant records. From the 163 potentially relevant records, we identified 41 reports of 19 non‐randomized studies that evaluated keratoprosthesis in people undergoing repeat corneal transplantation, which we assessed as relevant for discussion.

Results for searching for studies for inclusion in the review.
Non‐randomized studies
Of the 19 studies of keratoprosthesis we identified, 14 evaluated the Boston KPro (previously known as the Dohlman‐Doane KPro), three AlphaCor (previously known as the Chirila KPro); and one each of osteo‐odonto‐keratoprosthesis (OOKP) and Fyodorov‐Zuev keratoprosthesis (see Characteristics of excluded studies).
Boston KPro
The Boston Type 1 KPro Study Group consisted of 19 surgeons at 18 medical centers who volunteered clinical data of Boston keratoprosthesis type 1 surgeries they performed in 300 eyes of 300 patients between January 2003 and July 2008 (Boston Type 1 KPro Study). Some of these surgeons also have published separate reports of outcomes from their own patients, which made it difficult to assess study cohorts independently. In addition to the Boston Type 1 KPro Study, we identified case series reports from 12 individual institutions (combined total of 638 patients; 687 eyes) and one international case series (100 patients; 107 eyes) (Table 1).
| Study | Study design | Study dates | Country | Follow‐up | Number of participants | Number with repeat PK | Funding source and declarations of interest |
| Multicenter retrospective and prospective case | 2003‐2008 | 18 sites in the USA | Mean 17 (range 1 week to 6.1 years) | 300 (300 eyes) | 244/300 (81.3%) | "No surgeons in the study group have any proprietary interest in the Boston Type 1 keratoprosthesis." | |
| Retrospective case series | 2004‐2011 | USA (Jules Stein Eye Institute) | Mean 24 months (range 0 to 84 months) | 94 (98 eyes, 110 devices) | 82/98 (83.7%) eyes | "The author(s) have no proprietary or commercial interest in any materials discussed in this article." | |
| Retrospective case series | 2004‐2011 | Armenia, India, Indonesia, Nepal, Philippines, Russia, and Saudi Arabia | Mean 14.2 months (range 0 to 48 months) | 100 (107 eyes, 113 devices) | 74/107 (69.2%) eyes | "The author(s) have no proprietary or commercial interest in any materials discussed in this article." | |
| Retrospective case series | 2005‐2007 | USA (Wills Eye Institute) | Mean 16 months (range 6 to 28 months) | 37 (37 eyes) | 29/37 (78.4%) | "Dr. H. F. Chew was supported by the E. A. Baker Fellowship Fund Grant from the Canadian National Institute for the Blind." | |
| Retrospective case series | 2004‐2008 | USA (Wilmer Eye Institute and University of Rochester Eye Institute) | 6 months | 122 (126 eyes) | 112/126 (88.9%) eyes | "The authors have no proprietary or commercial interest in any of the materials discussed in this article." | |
| Retrospective case series | 2004‐2008 | USA (University of California, Davis) | Mean 19 months (range 1 to 48 months) | 28 (30 eyes) | 26/30 (86.7%) eyes | "The author(s) have no proprietary or commercial interest in any materials discussed in this article." | |
| Retrospective case series | 2006‐2011 | Spain (Instituto Microcirugia Ocular of Barcelona) | Mean 20 months (range 1 to 56 months) | 53 (54 eyes) | 49/54 (90.7%) eyes | "This work has been done with the help of the Ophthalmological Society of the Valencian Community, Valencia, Spain. The first author of the work has been awarded a fellowship for further study of residents at the Ocular Microsurgery Institute of Barcelona, sponsored by Pfizer."; "The authors have no financial or proprietary interest in the materials presented herein." | |
| Retrospective case series | 2003‐2009 | USA (Kellogg Eye Center, University of Michigan) | Mean 17 months (range 3 to 67 months) | 29 (30 eyes) | 23/30 (76.7%) eyes | "Supported in part by a departmental grant from the Research to Prevent Blindness (RPB), the RPB Lew R.Wasserman Merit Award, and the National Eye Institute K23 Mentored Clinician Scientist Award." | |
| Retrospective case series | 2009‐2011 | Germany (Neuhann & Colleagues) | Mean 9.1 months (range 1 to 21 months) | 14 (14 eyes) | 13/14 (92.9%) | "The corresponding author indicates no conflict of interests." | |
| Retrospective case series | 2006‐2010 | USA (New York Eye and Ear Infirmary) | Mean 21.5 months (range 3 to 47 months) | 51 (58 eyes) | 47/58 (81.0%) eyes | "The authors declare no conflict of interest." | |
| Retrospective case series | 2007‐2010 | Jordan (King Abdullah University Hospital) | Mean 18 months (range 3 to 36 months) | 19 (20 eyes) | 19/20 (95%) eyes | "Source of Support: Nil, Conflict of Interest: None declared." | |
| Retrospective case series | 2008‐2009 | Canada (Centre Hospitalier de l’Université de Montréal, Hôpital Notre‐Dame), | Mean 16.5 months | 38 (38 eyes) | 25/38 (65.8%) eyes | "Supported by a research grant from the Fonds de Recherche en Ophthalmologie de l’Université de Montréal, Montreal, Canada; and a Resident Research Grant from Pfizer Canada (Kirkland, Canada)"; "The authors indicate no financial conflict of interest." | |
| Early model of Boston keratoprosthesis (known as Dohlman‐Doane keratoprosthesis) | |||||||
| Retrospective case series | 2003‐2005 | USA (University of Rochester Eye Institute) | 12 months | 25 (25 eyes) | 22/25 (88%) | "The authors have no proprietary interest in any products mentioned in this article." | |
| Retrospective case series | 1990‐2004 | USA (Massachusetts Eye and Ear Infirmary) | Mean 35 months (range 1 to 108 months) | 128 (157 eyes) | 157/157 (100%) eyes | "Supported by a Massachusetts Eye and Ear Infirmary fund and the Alcon Research Institute award." | |
PK: penetrating keratoplasty
Visual acuity and graft failure outcomes were reported in many of the Boston KPro studies. However, few studies reported outcomes at specified follow‐up times (e.g. one year, two years, five years) (Table 2). These studies also had large amounts of missing data, particularly beyond one year of follow‐up.
| Study | Number with BCVA ≥ 20/100 | Other visual acuity outcomes | Proportion of graft failures* | Number of device extrusions | ||||
| 1 year | 2 years | 5 years | 1 year | 2 years | 5 years | |||
| 29 of 62 (46.8%) | NR | NR | "The number of patients with best‐corrected VA (BCVA) 20/200 or better went from 3.6% preoperatively to 57% postoperatively. Nineteen percent had postoperative vision of 20/40 or better." | 21/300 (7.0%) (12/244, 4.9% in participants with previous failed graft); failure rate 6% (n = 161 eyes) | NR; failure rate 11% (n = 91 eyes) | NR | 4/300 (1.3%) | |
| 42 of 77 (54.5%) | 22 of 47 (46.8%) | 5 of 7 (71.4%) | NR | 22/110 (20.0%) devices failed at final follow‐up; failure rate 8.3% (n = 74) | NR; failure rate 21.6% (n = 45) | NR; failure rate 38.4% (n = 5) | NR | |
| 33 of 65 (50.8%) | 18 of 34 (52.9%) | 0 of 1 (0%) | "In 82.2% (74/90) of the eyes in the international series in which the keratoprosthesis was retained at the final follow‐up visit, the final postoperative CDVA was better than the preoperative CDVA, and in 13.3% (12/90) of eyes, the preoperative and postoperative CDVAs were the same." | 22/113 (19.5%) devices failed at final follow‐up; failure rate 20.8% (n = 58) | NR; failure rate 25.4% (n = 18) | NA | NR | |
| NR | NR | NA | The mean BCVA at any point postoperatively and at last follow‐up were 20/50 (range: 20/400 to 20/20; P < 0.001) and 20/90 (range: light perception to 20/25; P < 0.001), respectively. The mean BCVA over time at 6 ,12, and 18 months showed significant visual improvement (P < 0.001) compared with BCVA preoperatively.16 patients (43%) achieved a BCVA better than or equal to 20/50 at last follow‐up (time not specified); 23 of 30 patients (76.7%) with minimum follow‐up of 12 months had a BCVA better than or equal to 20/200) | 1/30 (3%) (the type 2 model) | NA | NA | 1/30 (3%) (the type 2 model) | |
| NA | NA | NA | "Of 126 eyes, 104 (82.5%) achieved improved vision within the first 6 months postoperatively."; "At the 3‐month follow‐up, 54% of eyes had 20/200 vision or better, and 18% were 20/40 or better. Twenty‐two of the eyes (22/126; 17.4%) did not have improved vision. Eight eyes lost vision" | NA | NA | NA | 3/126 (2.4%) extrusion/corneal melt at 6 months | |
| NR | NR | NA | In the subgroup of 16 eyes followed for at least 1 year after keratoprosthesis implantation (mean follow‐up, 28 months; range 12 to 48 months; SD 12.8 months; median 24 months), vision was ≥ 20/200 in 75% of eyes and ≥ 20/40 in 25% of eyes | 5/30 (16.7%) at mean of 19 months follow‐up | NR | NR | NR | |
| 12/54 eyes at final follow‐up | NR | NR | "The postoperative BCVA was 0.097 (SD 0.18). Thirty‐three (33%) achieved a BCVA ≥ 0.1 (18 eyes) and 7.4% achieved ≥ 0.4 (4 eyes). Rapid improvement in the BCVA was observed. The measurements obtained 3 months after the operation do not differ significantly from the final BCVA." | 2/54 (3.7%); failure rate 4% | NR | NR | NR | |
| NR | NR | NR | Mean postoperative BCVA 20/390 (range 20/40 to LP; n = 16) at one year; "When comparing preoperative BCVA with final BCVA, vision improved in 19 of 30 eyes (63%) and was unchanged in 7 eyes (23%). Vision worsened in 4 eyes (13%) because of glaucoma in 3 eyes, 2 of which became no light perception, and retinal detachment occurred in 1 eye” | 6/20 (30%) | NR | NR | NR | |
| 2 of 4 (50%) | NA | NA | 10 of 14 had BCVA ≥ 0.03, 1 had CF, and 3 had HM at the last follow‐up (mean 9; range 1 to 21 months) | failure rate 0% (n = 4) | NA | NA | None | |
| NR | NR | NA | "At the last follow‐up, 43.1% of eyes attained BCVA ≥ 20/200. By follow‐up, the percentage of eyes with BCVA ≥ 20/200 showed a decreasing trend with 74.5% (35/47) at 1 year, 50.0% (16/32) at 2 years, and 36.3% (4/11) at 3 years"; "At the last follow‐up, BCVA improved in 55.2% of eyes (32/58), remained the same in 27.6% of eyes (16/58), and worsened in 17.2% of eyes (10/58) because of postoperative complications." | 7/58 (12.1%) | None | NA | 4/58 (6.9%) | |
| NR | NR | NA | "In the subgroup of 15 eyes followed for at least 1 year (median follow‐up: 20 months; range: 12–36 months) after KPro implantation, vision improved in 86.7% of eyes; it was 20/200 in 66.7% of eyes and 20/50 in 26.7% of eyes." | 0/15; failure rate 0% (n = 15) | 2 had extrusion (12 and 15 months) | NA | 2/20 (10%) | |
| 11 of 32 (34.4%) | NR | NA | Thirty‐one eyes (82%) that underwent KPro surgery displayed postoperative BCVA improvement. | 0/32; failure rate 0% (n = 32) with a mean follow‐up time of 16.5 (SD 4.7) months | NR | NA | None | |
| Early model of Boston keratoprosthesis (known as Dohlman‐Doane keratoprosthesis) | ||||||||
| NR | NA | NA | 12/25 with 20/200 or better; 3/25 with 20/40 or better | NR | NA | NA | None at one year | |
| NR | NR | NR | NR | NR | NR | NR | NR | |
*graft failure as reported by individual studies
BCVA: best‐corrected visual acuity
CDVA: corrected‐distance visual acuity
CF: counting fingers
HM: hand motions
LP: light perception
NA: not applicable
NR: not reported
SD: standard deviation
AlphaCor
Similar to the Boston Type 1 KPro Study Group, Hicks and colleagues compiled clinical data of AlphaCor surgeries between 1998 to 2006 from surgeons who voluntarily contributed their patient data (Hicks 2006). This case series included data reported by 84 surgeons from 11 countries who implanted 322 AlphaCor devices in 302 patients. We identified two additional case series of AlphaCor (Table 3).
| Study | Study design | Study dates | Country | Follow‐up | Number of participants | Number with repeat PK | Funding source and declarations of interest | |||
| Multicenter surveillance data | 1998‐2006 | 11 countries, including Australia, Singapore, and USA | Mean 15.5 months (range 0.5 to 7.4 years) | 302 (304 eyes, 322 devices implanted) | 302 (304 eyes, 322 devices implanted) | "Hicks and Crawford have a financial interest with the manufacturer of AlphaCor, CooperVision Surgical, through support of departmental funding, travel and research." | ||||
| Retrospective case series | NR | Germany/Czech Republic | Mean 38 months (range 12 to 67 months) | 15 (15 eyes) | 12/15 (80%) | "Supported in part by research project MZO 00179906 "The authors declare no conflict of interest." | ||||
| Retrospective case series | 2009‐2011 | France | Mean 16 months (range 2 to 24 months) | 14 (14 eyes) | 10/14 (71%) | "Conference invitations as a speaker for Addition Technology, Inc." | ||||
| Study | Number with BCVA ≥ 20/100 | Other visual acuity outcomes | Number of graft failures | Number of device extrusions | ||||||
| 1 year | 2 years | 5 years | 1 year | 2 years | 5 years | |||||
| "41.4% of all post–stage 2 cases achieved 20/200 or better", timing not specified by year | VA achieved postoperatively was LP to 20/20, mean 20/200; "mean improvement of 2 lines"; "6 eyes permanently lost vision over a summed 416 years of follow‐up. This finding equates to an annual risk per eye of 0.014." | NR; failure rate 20% for on‐label use | NR; failure rate 38% for on‐label use | 110/322 devices at final follow‐up; failure rate 34.2% | NR | |||||
| 2 of 13 (15%) | 2 of 7 (29%) | NR | NR | NR | NR | NR | NR | |||
| NR | NR | NA | "Postoperative mean visual acuity gain was 2.5 +/‐ 3.1 lines (from 0 to +11 lines). Visual acuity was superior or equal to 20/200 in 21% of cases." | NR; failure rate 28.6% with mean follow‐up of 15.6 months | NR | NA | 1/14 (7%) | |||
BCVA: best‐corrected visual acuity
LP: light perception
NR: not reported
PK: penetrating keratoplasty
VA: visual acuity
Visual acuity data were reported in all of the three AlphaCor studies; however only one study reported outcomes at specified follow‐up times (Table 3). Two studies reported graft failure or retention outcomes.
Other types of artificial corneas
We identified case series reports of two other types of artificial corneal devices, one each of Fyodorov‐Zuev keratoprosthesis (10 patients) and osteo‐odonto‐keratoprosthesis (OOKP) (25 patients). Both studies reported visual acuity outcomes and number of device extrusions (Table 4).
| Study | Study design | Study dates | Country | Follow‐up | Number of participants | Number with repeat PK | Funding source and declarations of interest | |||
| Retrospective case series of the Fyodorov‐Zuev KPro | 2003‐2007 | Iran (Dr. Khodadoust Eye Hospital) | Mean 52 months (range 28 to 84 months) | 10 (10 eyes) | 10/10 (100%) | "None of the authors have any financial or proprietary interest in any material or method mentioned." | ||||
| Retrospective case series the OOKP | 1993‐2004 | Germany (University of Saarland) | Median 2.9 years | 25 (25 eyes) | 18/25 (72%) | NR | ||||
| Study | Number with BCVA ≥ 20/100 | Other visual acuity outcomes | Number of graft failures | Number of device extrusions | ||||||
| 1 year | 2 years | 5 years | 1 year | 2 years | 5 years | |||||
| 8/10 | 8/10 | 2/4 | "Patients retained BUVA of 20/200–20/50 in 50%, 20/60‐20/ 100 in 30%, 20/200 in 10% and 20/400 in 10% of cases. Overall, 90% had 1 year postoperative vision of 20/200 or better. Eyes had 20/200 or better in 70% of cases at the last follow‐up (average 52 months)." | 1/10 (10%) | 2/10 (20%) | 3/10 (30%) at 3 years; failure rate 30% during follow‐up | 3/10 (30%) during follow‐up | |||
| 11/20 (55%) | 7/14 (50%) | 2/5 (40%) | 79% achieved ambulatory vision of 20/400 at last follow up | NR | NR | NR | None reported | |||
BCVA: best‐corrected visual acuity
BUVA: best‐uncorrected visual acuity
OOKP: osteo‐odonto‐keratoprosthesis
NR: not reported
PK: penetrating keratoplasty
Excluded studies
We further excluded 122 reports after review of the full‐text for the following reasons: 47 reports were of primary KPro procedures or did not specify how many patients had previous PK procedures; 31 reports included fewer than 10 patients undergoing repeat corneal transplantation; 34 reports did not include original data (e.g. editorials, descriptions of surgical procedures, reviews); and 10 reports dealt with postoperative management of corneal transplantation (e.g. use of soft contact lenses, how to image eyes with implanted KPros, treatment of endophthalmitis).
Risk of bias in included studies
We could not assess risk of bias since no RCTs were included in the review.
Effects of interventions
We did not identify any evidence comparing the effectiveness of artificial versus donor corneas for repeat corneal transplantation.
Discussion
Summary of main results
No relevant randomized or quasi‐randomized controlled trials were identified for inclusion in this review. We identified 19 studies of KPro surgery in patients undergoing repeat corneal transplantation, none of which compared implantation of KPro devices with human donor corneal transplantation.
The majority of non‐randomized studies we identified were reports of case series of KPro implantations from medical centers in the USA. One study compared results of Boston KPros implanted at a medical center in the USA with a case series of Boston KPros implanted internationally (Aldave 2012a; Aldave 2012b). The authors of the report concluded that visual acuity outcomes, retention rates, and adverse events were comparable between the two groups of patients. It is important to note, however, that the average follow‐up times differed in the two cohorts, with the US‐based cohort having a mean follow‐up of 24 months (up to 84 months) and the non‐US‐based group having a mean follow‐up of 14 months (up to 48 months).
When data could be abstracted from the non‐randomized studies, the failure rates at one year after implantation ranged from 0% to 30%. However, these rates are very uncertain due to the high amount of loss to follow‐up in the studies and the variability in patient risk factors (e.g. indication for surgery, number of previous graft failures).
Overall completeness and applicability of evidence
This review aimed to gain information regarding the visual outcomes and complication rates of artificial corneal transplantation surgeries in comparison with repeat donor corneal transplantation in individuals with prior failed full thickness penetrating keratoplasty. No such studies directly comparing the results were noted from extensive literature searches. Given the increasing popularity of Boston type I KPro and a trend to expanding the indications even to patients who have not yet received donor transplantations, a head‐to‐head comparison is needed. The inclusion criteria to enroll participants in such a study should be carefully considered. For instance, a non‐vascularized cornea in a phakic eye after a single episode of rejection may do very well with repeat donor grafting and probably would not be considered for KPro surgery. The situation is entirely different when there are additional risk factors for failure such as neovascularization, ocular surface diseases, or glaucoma. Future studies comparing these methods should take into consideration the cause of prior graft failure, preoperative diagnosis, and presence of high risk characteristics for rejection when enrolling participants.
In addition, the currently available studies reporting outcomes of both repeat donor PK as well as KPro surgeries are limited in regards to the length of follow‐up. It is conceivable that the lifetime risks of complications and the possibility of permanent vision loss after either procedure may differ significantly. This fact could not be addressed in this review due to the very limited follow‐up of the available reports. A careful review of literature of repeat PK outcomes might perhaps help determine the best outcomes to assess in a head‐to‐head comparison. For example, incidence of endophthalmitis and vision loss due to glaucoma, which have been reported to be higher after implantation of Boston type 1 KPro compared with PK, would be important outcomes to study.
Quality of the evidence
The literature we found on this topic consisted primarily of clinical studies evaluating only one type of procedure (KPro or PK), i.e. non‐comparative case series and case reports. We also found that few of these studies reported visual acuity or graft survival outcomes up to one year of follow‐up for all study participants. The most common method of reporting outcomes was to combine participant data at 'final follow‐up', rather than at specific follow‐up time points. Since graft survival is associated with the duration of the implantation (i.e. the longer a person has the device), it is inappropriate to combine findings from different follow‐up times. When outcomes were reported at specific time points (e.g. six months, one year, two years), data often were not reported for all study participants and reported only for those with available data.
Potential biases in the review process
We conducted a highly sensitive search to identify trials comparing artificial corneal implants with human donor corneas for people needing repeat corneal transplantation. As we anticipated finding few or no randomized controlled trials on this topic, we also searched for any observational or clinical study evaluating KPro for repeat corneal transplantation. Clinicians and methodologists on the review team were paired to duplicate tasks in order to minimize selection bias and errors during the study selection and data abstraction processes.
Not all of the studies included only eyes undergoing repeat corneal surgery. Many studies also included keratoprosthesis as a primary procedure in eyes at high risk of failure with donor corneal transplantation (e.g. people with chemical injury, SJS, or MMP). We limited our review of non‐randomized studies to those in which more than 60% of participants had at least one failed PK. We allowed a mix of cases based on clinical experience, knowing these cases were likely to be grouped together in study cohorts.
Agreements and disagreements with other studies or reviews
We are unaware of any other systematic review comparing artificial versus donor corneas in people needing repeat corneal transplantation following a failed full thickness PK. Based on non‐randomized studies identified from our searches, different types of KPros are being used for individuals undergoing repeat corneal transplantation procedures. Historically, artificial corneas have been considered for 'salvage' procedures when no alternative exists. Therefore, the majority of the patients in the published reports had been deemed "ineligible" to receive another donor corneal transplantation and hence were likely to have worse vision prior to the surgery as well as worse co‐morbidity than the patients who were considered for repeat corneal transplantation with donor corneas. Despite this trend, the high retention rates reported with Boston type 1 KPro have made this device an attractive alternative to repeat donor corneal transplantations (AAO PPP 2013; Boston Type 1 KPro Study). As surgeons and centers have gained more experience with KPro, particularly following advances in design and materials, the utilization of KPros has shown a substantial increase in the most recent few years including in a wider subset of patients than previously considered (MEEI 2013).
Importantly, the number of repeat corneal transplantations in the US has been steadily increasing. According to the Eye Bank Association of America, repeat corneal transplantation for a previously failed graft is the second most common indication for full thickness donor PK in the US, after keratoconus, comprising about 17% of all those undergoing a full thickness donor PK during the last decade (EBAA 2013). This percentage is in line with rates from other countries as well (Bersudsky 2001; Wagoner 2009; Williams 1995). Of all transplant procedures, corneal transplantation has a good success rate: however, the risk of graft failure increases with the number of repeat procedures and time. The graft survival rate at one year was reported to be 80.5% (95% CI 75.4% to 85.0%) for the first repeat PK, 76.9% (95% CI 64.9% to 85.6%) for the second repeat PK, and 51.9% (95% CI 33.4% to 73.4%) for the third or more repeat PKs based on national data from Australia (ACGR 1993). A more recent study of repeat PK in the USA showed better overall survival rates for the second or more repeat PKs than the Austrailian study, but also supported findings that graft survival at one year was higher for eyes having their second repeat PK (89%, 95% CI 76% to 96%) versus their third repeat PK (73%, 95% CI 39% to 94%) (Yildiz 2010).
Results for searching for studies for inclusion in the review.
| Study | Study design | Study dates | Country | Follow‐up | Number of participants | Number with repeat PK | Funding source and declarations of interest |
| Multicenter retrospective and prospective case | 2003‐2008 | 18 sites in the USA | Mean 17 (range 1 week to 6.1 years) | 300 (300 eyes) | 244/300 (81.3%) | "No surgeons in the study group have any proprietary interest in the Boston Type 1 keratoprosthesis." | |
| Retrospective case series | 2004‐2011 | USA (Jules Stein Eye Institute) | Mean 24 months (range 0 to 84 months) | 94 (98 eyes, 110 devices) | 82/98 (83.7%) eyes | "The author(s) have no proprietary or commercial interest in any materials discussed in this article." | |
| Retrospective case series | 2004‐2011 | Armenia, India, Indonesia, Nepal, Philippines, Russia, and Saudi Arabia | Mean 14.2 months (range 0 to 48 months) | 100 (107 eyes, 113 devices) | 74/107 (69.2%) eyes | "The author(s) have no proprietary or commercial interest in any materials discussed in this article." | |
| Retrospective case series | 2005‐2007 | USA (Wills Eye Institute) | Mean 16 months (range 6 to 28 months) | 37 (37 eyes) | 29/37 (78.4%) | "Dr. H. F. Chew was supported by the E. A. Baker Fellowship Fund Grant from the Canadian National Institute for the Blind." | |
| Retrospective case series | 2004‐2008 | USA (Wilmer Eye Institute and University of Rochester Eye Institute) | 6 months | 122 (126 eyes) | 112/126 (88.9%) eyes | "The authors have no proprietary or commercial interest in any of the materials discussed in this article." | |
| Retrospective case series | 2004‐2008 | USA (University of California, Davis) | Mean 19 months (range 1 to 48 months) | 28 (30 eyes) | 26/30 (86.7%) eyes | "The author(s) have no proprietary or commercial interest in any materials discussed in this article." | |
| Retrospective case series | 2006‐2011 | Spain (Instituto Microcirugia Ocular of Barcelona) | Mean 20 months (range 1 to 56 months) | 53 (54 eyes) | 49/54 (90.7%) eyes | "This work has been done with the help of the Ophthalmological Society of the Valencian Community, Valencia, Spain. The first author of the work has been awarded a fellowship for further study of residents at the Ocular Microsurgery Institute of Barcelona, sponsored by Pfizer."; "The authors have no financial or proprietary interest in the materials presented herein." | |
| Retrospective case series | 2003‐2009 | USA (Kellogg Eye Center, University of Michigan) | Mean 17 months (range 3 to 67 months) | 29 (30 eyes) | 23/30 (76.7%) eyes | "Supported in part by a departmental grant from the Research to Prevent Blindness (RPB), the RPB Lew R.Wasserman Merit Award, and the National Eye Institute K23 Mentored Clinician Scientist Award." | |
| Retrospective case series | 2009‐2011 | Germany (Neuhann & Colleagues) | Mean 9.1 months (range 1 to 21 months) | 14 (14 eyes) | 13/14 (92.9%) | "The corresponding author indicates no conflict of interests." | |
| Retrospective case series | 2006‐2010 | USA (New York Eye and Ear Infirmary) | Mean 21.5 months (range 3 to 47 months) | 51 (58 eyes) | 47/58 (81.0%) eyes | "The authors declare no conflict of interest." | |
| Retrospective case series | 2007‐2010 | Jordan (King Abdullah University Hospital) | Mean 18 months (range 3 to 36 months) | 19 (20 eyes) | 19/20 (95%) eyes | "Source of Support: Nil, Conflict of Interest: None declared." | |
| Retrospective case series | 2008‐2009 | Canada (Centre Hospitalier de l’Université de Montréal, Hôpital Notre‐Dame), | Mean 16.5 months | 38 (38 eyes) | 25/38 (65.8%) eyes | "Supported by a research grant from the Fonds de Recherche en Ophthalmologie de l’Université de Montréal, Montreal, Canada; and a Resident Research Grant from Pfizer Canada (Kirkland, Canada)"; "The authors indicate no financial conflict of interest." | |
| Early model of Boston keratoprosthesis (known as Dohlman‐Doane keratoprosthesis) | |||||||
| Retrospective case series | 2003‐2005 | USA (University of Rochester Eye Institute) | 12 months | 25 (25 eyes) | 22/25 (88%) | "The authors have no proprietary interest in any products mentioned in this article." | |
| Retrospective case series | 1990‐2004 | USA (Massachusetts Eye and Ear Infirmary) | Mean 35 months (range 1 to 108 months) | 128 (157 eyes) | 157/157 (100%) eyes | "Supported by a Massachusetts Eye and Ear Infirmary fund and the Alcon Research Institute award." | |
| PK: penetrating keratoplasty | |||||||
| Study | Number with BCVA ≥ 20/100 | Other visual acuity outcomes | Proportion of graft failures* | Number of device extrusions | ||||
| 1 year | 2 years | 5 years | 1 year | 2 years | 5 years | |||
| 29 of 62 (46.8%) | NR | NR | "The number of patients with best‐corrected VA (BCVA) 20/200 or better went from 3.6% preoperatively to 57% postoperatively. Nineteen percent had postoperative vision of 20/40 or better." | 21/300 (7.0%) (12/244, 4.9% in participants with previous failed graft); failure rate 6% (n = 161 eyes) | NR; failure rate 11% (n = 91 eyes) | NR | 4/300 (1.3%) | |
| 42 of 77 (54.5%) | 22 of 47 (46.8%) | 5 of 7 (71.4%) | NR | 22/110 (20.0%) devices failed at final follow‐up; failure rate 8.3% (n = 74) | NR; failure rate 21.6% (n = 45) | NR; failure rate 38.4% (n = 5) | NR | |
| 33 of 65 (50.8%) | 18 of 34 (52.9%) | 0 of 1 (0%) | "In 82.2% (74/90) of the eyes in the international series in which the keratoprosthesis was retained at the final follow‐up visit, the final postoperative CDVA was better than the preoperative CDVA, and in 13.3% (12/90) of eyes, the preoperative and postoperative CDVAs were the same." | 22/113 (19.5%) devices failed at final follow‐up; failure rate 20.8% (n = 58) | NR; failure rate 25.4% (n = 18) | NA | NR | |
| NR | NR | NA | The mean BCVA at any point postoperatively and at last follow‐up were 20/50 (range: 20/400 to 20/20; P < 0.001) and 20/90 (range: light perception to 20/25; P < 0.001), respectively. The mean BCVA over time at 6 ,12, and 18 months showed significant visual improvement (P < 0.001) compared with BCVA preoperatively.16 patients (43%) achieved a BCVA better than or equal to 20/50 at last follow‐up (time not specified); 23 of 30 patients (76.7%) with minimum follow‐up of 12 months had a BCVA better than or equal to 20/200) | 1/30 (3%) (the type 2 model) | NA | NA | 1/30 (3%) (the type 2 model) | |
| NA | NA | NA | "Of 126 eyes, 104 (82.5%) achieved improved vision within the first 6 months postoperatively."; "At the 3‐month follow‐up, 54% of eyes had 20/200 vision or better, and 18% were 20/40 or better. Twenty‐two of the eyes (22/126; 17.4%) did not have improved vision. Eight eyes lost vision" | NA | NA | NA | 3/126 (2.4%) extrusion/corneal melt at 6 months | |
| NR | NR | NA | In the subgroup of 16 eyes followed for at least 1 year after keratoprosthesis implantation (mean follow‐up, 28 months; range 12 to 48 months; SD 12.8 months; median 24 months), vision was ≥ 20/200 in 75% of eyes and ≥ 20/40 in 25% of eyes | 5/30 (16.7%) at mean of 19 months follow‐up | NR | NR | NR | |
| 12/54 eyes at final follow‐up | NR | NR | "The postoperative BCVA was 0.097 (SD 0.18). Thirty‐three (33%) achieved a BCVA ≥ 0.1 (18 eyes) and 7.4% achieved ≥ 0.4 (4 eyes). Rapid improvement in the BCVA was observed. The measurements obtained 3 months after the operation do not differ significantly from the final BCVA." | 2/54 (3.7%); failure rate 4% | NR | NR | NR | |
| NR | NR | NR | Mean postoperative BCVA 20/390 (range 20/40 to LP; n = 16) at one year; "When comparing preoperative BCVA with final BCVA, vision improved in 19 of 30 eyes (63%) and was unchanged in 7 eyes (23%). Vision worsened in 4 eyes (13%) because of glaucoma in 3 eyes, 2 of which became no light perception, and retinal detachment occurred in 1 eye” | 6/20 (30%) | NR | NR | NR | |
| 2 of 4 (50%) | NA | NA | 10 of 14 had BCVA ≥ 0.03, 1 had CF, and 3 had HM at the last follow‐up (mean 9; range 1 to 21 months) | failure rate 0% (n = 4) | NA | NA | None | |
| NR | NR | NA | "At the last follow‐up, 43.1% of eyes attained BCVA ≥ 20/200. By follow‐up, the percentage of eyes with BCVA ≥ 20/200 showed a decreasing trend with 74.5% (35/47) at 1 year, 50.0% (16/32) at 2 years, and 36.3% (4/11) at 3 years"; "At the last follow‐up, BCVA improved in 55.2% of eyes (32/58), remained the same in 27.6% of eyes (16/58), and worsened in 17.2% of eyes (10/58) because of postoperative complications." | 7/58 (12.1%) | None | NA | 4/58 (6.9%) | |
| NR | NR | NA | "In the subgroup of 15 eyes followed for at least 1 year (median follow‐up: 20 months; range: 12–36 months) after KPro implantation, vision improved in 86.7% of eyes; it was 20/200 in 66.7% of eyes and 20/50 in 26.7% of eyes." | 0/15; failure rate 0% (n = 15) | 2 had extrusion (12 and 15 months) | NA | 2/20 (10%) | |
| 11 of 32 (34.4%) | NR | NA | Thirty‐one eyes (82%) that underwent KPro surgery displayed postoperative BCVA improvement. | 0/32; failure rate 0% (n = 32) with a mean follow‐up time of 16.5 (SD 4.7) months | NR | NA | None | |
| Early model of Boston keratoprosthesis (known as Dohlman‐Doane keratoprosthesis) | ||||||||
| NR | NA | NA | 12/25 with 20/200 or better; 3/25 with 20/40 or better | NR | NA | NA | None at one year | |
| NR | NR | NR | NR | NR | NR | NR | NR | |
| *graft failure as reported by individual studies BCVA: best‐corrected visual acuity | ||||||||
| Study | Study design | Study dates | Country | Follow‐up | Number of participants | Number with repeat PK | Funding source and declarations of interest | |||
| Multicenter surveillance data | 1998‐2006 | 11 countries, including Australia, Singapore, and USA | Mean 15.5 months (range 0.5 to 7.4 years) | 302 (304 eyes, 322 devices implanted) | 302 (304 eyes, 322 devices implanted) | "Hicks and Crawford have a financial interest with the manufacturer of AlphaCor, CooperVision Surgical, through support of departmental funding, travel and research." | ||||
| Retrospective case series | NR | Germany/Czech Republic | Mean 38 months (range 12 to 67 months) | 15 (15 eyes) | 12/15 (80%) | "Supported in part by research project MZO 00179906 "The authors declare no conflict of interest." | ||||
| Retrospective case series | 2009‐2011 | France | Mean 16 months (range 2 to 24 months) | 14 (14 eyes) | 10/14 (71%) | "Conference invitations as a speaker for Addition Technology, Inc." | ||||
| Study | Number with BCVA ≥ 20/100 | Other visual acuity outcomes | Number of graft failures | Number of device extrusions | ||||||
| 1 year | 2 years | 5 years | 1 year | 2 years | 5 years | |||||
| "41.4% of all post–stage 2 cases achieved 20/200 or better", timing not specified by year | VA achieved postoperatively was LP to 20/20, mean 20/200; "mean improvement of 2 lines"; "6 eyes permanently lost vision over a summed 416 years of follow‐up. This finding equates to an annual risk per eye of 0.014." | NR; failure rate 20% for on‐label use | NR; failure rate 38% for on‐label use | 110/322 devices at final follow‐up; failure rate 34.2% | NR | |||||
| 2 of 13 (15%) | 2 of 7 (29%) | NR | NR | NR | NR | NR | NR | |||
| NR | NR | NA | "Postoperative mean visual acuity gain was 2.5 +/‐ 3.1 lines (from 0 to +11 lines). Visual acuity was superior or equal to 20/200 in 21% of cases." | NR; failure rate 28.6% with mean follow‐up of 15.6 months | NR | NA | 1/14 (7%) | |||
| BCVA: best‐corrected visual acuity | ||||||||||
| Study | Study design | Study dates | Country | Follow‐up | Number of participants | Number with repeat PK | Funding source and declarations of interest | |||
| Retrospective case series of the Fyodorov‐Zuev KPro | 2003‐2007 | Iran (Dr. Khodadoust Eye Hospital) | Mean 52 months (range 28 to 84 months) | 10 (10 eyes) | 10/10 (100%) | "None of the authors have any financial or proprietary interest in any material or method mentioned." | ||||
| Retrospective case series the OOKP | 1993‐2004 | Germany (University of Saarland) | Median 2.9 years | 25 (25 eyes) | 18/25 (72%) | NR | ||||
| Study | Number with BCVA ≥ 20/100 | Other visual acuity outcomes | Number of graft failures | Number of device extrusions | ||||||
| 1 year | 2 years | 5 years | 1 year | 2 years | 5 years | |||||
| 8/10 | 8/10 | 2/4 | "Patients retained BUVA of 20/200–20/50 in 50%, 20/60‐20/ 100 in 30%, 20/200 in 10% and 20/400 in 10% of cases. Overall, 90% had 1 year postoperative vision of 20/200 or better. Eyes had 20/200 or better in 70% of cases at the last follow‐up (average 52 months)." | 1/10 (10%) | 2/10 (20%) | 3/10 (30%) at 3 years; failure rate 30% during follow‐up | 3/10 (30%) during follow‐up | |||
| 11/20 (55%) | 7/14 (50%) | 2/5 (40%) | 79% achieved ambulatory vision of 20/400 at last follow up | NR | NR | NR | None reported | |||
| BCVA: best‐corrected visual acuity | ||||||||||

