Intervenciones para la prevención o la reducción de la violencia doméstica contra la mujer embarazada
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Stratified RCT. Women were stratified by risk factor combination (1 of 15 possible combinations of 4 risk behaviours (IPV, alcohol, drugs, smoking)). | |
| Participants | Women attending 5 prenatal clinics in the San Francisco bay area (USA). Only women with risk factors were randomised. 37 women experiencing DV were randomised. Inclusion criteria: women less than 26 weeks’ gestation, English speaking, aged 18 years or older, not attending for first prenatal visit who screened positive for one (or more than one) of 4 risk factors (smoking, alcohol, drug use or DV). Exclusion criteria: women who had no risk factors were not randomised. | |
| Interventions | Experimental intervention: video doctor‐assessment with appropriate messages for risk factor (e.g. encouraging women to discuss problem) and healthcare staff were alerted and given a cueing sheet to discuss risk factor (DV). (20 women randomised to the intervention group.) Control/Comparison intervention: all women had video doctor‐assessment but healthcare staff did not receive cueing sheet. Women randomised to the control group received usual care and any discussion of risk was at the discretion of healthcare staff. (17 women randomised to control condition.) | |
| Outcomes | This study examined whether discussions re DV occurred and women’s views of the discussion (acceptability and helpfulness). No other outcome data were reported. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was by a computer programme, however, it was not clear how stratification affected the randomisation process as some women may have had several risk factors (it was not clear whether these women would then receive several intervention messages and several staff cueing forms). |
| Allocation concealment (selection bias) | Low risk | By computer programme. |
| Incomplete outcome data (attrition bias) | Unclear risk | 37 women experiencing DV were randomised and data appear available for all women at the immediate post‐intervention assessment. There were some missing data at follow‐up (32 were followed up at 2 months) but all women were included in a sensitivity analysis (those lost to follow‐up were assumed to have had no discussion of DV). |
| Selective reporting (reporting bias) | Unclear risk | Results for women assessed with a single risk factor were reported but it seems that women may have had multiple risk factors and multiple interventions and there may have been some interaction effect (it is possible that if a woman had multiple risk factors then she was more likely than those with a single risk factor to have discussions with healthcare staff). |
| Other bias | Low risk | Other bias not apparent. |
| Blinding of participants and personnel (performance bias) | High risk | Staff would have been aware of group assignment because the interview would have been conducted according to the intervention cue sheet for the intervention group. It is unclear whether women would have been aware of group assignment. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Staff would have been aware of group assignment because the interview would have been conducted according to the intervention cue sheet for the intervention group. It is unclear whether women would have been aware of group assignment. Outcomes are self‐reported, so it is unclear whether these would have been shaped by knowledge of group assignment. |
| Methods | RCT. 2‐arm trial with individual randomisation. | |
| Participants | Setting: public hospital in Lima, Peru, providing services to low‐income women living in Lima. Recruitment in 2007. Inclusion criteria: 220 pregnant women (gestational age between 12 and 26 weeks’ gestation) attending for care in the study hospital who screened positive for DV on the modified Abuse Assessment screen and able to speak and understand Spanish. (Women screened positive if they said yes to any of the following in the past year – been pushed, shoved, slapped, hit, kicked or otherwise physically hurt or been forced into sexual activity by a former or current partner.) | |
| Interventions | Experimental intervention: (110 randomised) empowerment intervention during pregnancy which included standard care (a card with information about agencies providing IPV support). Women in the empowerment intervention received supportive counselling and education, and advice in the areas of safety by a trained social worker lasting about 30 minutes. Interviewers listened empathetically to the women and acknowledged their perceptions and feelings. Interviewers also helped women understand the cycle of violence and reviewed components of the safety plan including behaviours indicated in the Safety Behavior Checklist. For example, women were asked how they might secure and hide money and important documents such as birth certificates. Interviewers helped women develop a code to use with family and trusted friends to signal the need for assistance and/or to mentally plan their escape when needed. Women were given a brochure with a 13‐item safety plan to reinforce safety behaviours. To make the safety plan brochure less conspicuous, other prenatal brochures on topics such as breastfeeding or nutrition were also offered to the women. Interviewers also provided a list of community resources, such as emergency shelter, legal aid, law enforcement, and counselling, and strategies for seeking help from these resources. As part of the intervention, interviewers also offered to assist women with telephone calls to social service agencies or women's groups who could act as advocates for abused women. At the conclusion of the empowerment intervention session, interviewers helped women determine if it was safe for her to keep the safety plan brochure and the referral card. Women were free to discuss the pros and cons of leaving the abuser, reporting the abuser to law enforcement, or applying for a protection order.
Control/Comparison intervention: (110 randomised) women randomised to receive standard care received a wallet‐size referral card listing agencies that provide DV services to abused women (e.g., legal, social services,and law enforcement). No counselling, advocacy, education, or other services were offered to women in this group during pregnancy. However, they were provided the empowerment intervention, specifically supportive counselling and education, and advice in the areas of safety by a trained social worker at the conclusion of the study during the 6th week postpartum visit. | |
| Outcomes | Physical, functional and emotional functioning at follow‐up as compared with baseline. Use of community resources and safety behaviours. Episodes of violence in the past year were reported at baseline but data on this outcome were not reported at follow‐up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Assignment was by a “randomised block design” but how the sequence was generated and block size were not stated. |
| Allocation concealment (selection bias) | Unclear risk | Methods used to allocate women to groups at the point of randomisation were not described. |
| Incomplete outcome data (attrition bias) | Low risk | Sixteen women (7.3%) were lost to follow‐up. 220 women were randomised and follow‐up data were available for 204. |
| Selective reporting (reporting bias) | Unclear risk | Episodes of violence at follow‐up were not reported in this paper (it may be that these outcomes will be addressed in future papers). |
| Other bias | Low risk | Groups were reported to be similar at baseline and there was no other bias apparent. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Women and staff would be aware of the purpose of the study and which group they were assigned to. Post‐intervention interviews were carried out by a different interviewer than those who carried out the pre‐intervention ones to reduce bias. It was not clear what impact lack of blinding would have on the outcomes reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Women and staff would be aware of the purpose of the study and which group they were assigned to. Post‐intervention interviews were carried out by a different interviewer than those who carried out the pre‐intervention ones to reduce bias. It was not clear what impact lack of blinding would have on the outcomes reported. |
| Methods | RCT, 2 arms with individual randomisation (2 sites). | |
| Participants | 1000 women who spoke English and were 13 to 23 weeks pregnant at the time of recruitment. At the completion of the first assessment, women were randomised to 1 of the 2 groups, 501 to the control group and 499 to the treatment group. Prenatal Psychosocial Profile test was used to estimate women's stress level. After women at risk of abuse with high level of stress were identified, 106 were in the intervention group and 101 in the control group. Study carried out in two prenatal clinics of a Health Maintenance Organisation in the USA (clinics both served what was described as a geographically, culturally and economically diverse group). Each clinic enrolled 500 women over the period 2001‐2003.
Exclusion criteria: adolescents for whom consent was not available. | |
| Interventions | Experimental intervention: standard care plus video about abuse (watched by < 30%), 24/7 access to Nurse Case Management. Women were contacted by phone by nurse who actively managed their care. The intervention was intended to provide support and was individually tailored to women’s needs. Control/Comparison intervention: standard care which involved written information on community and health services resources for abused women. (Women assessed as being in danger were provided with safety planning and the offer of referral to the clinic social worker.) | |
| Outcomes | Process outcomes (number of contacts, etc). The outcomes reported in this paper related to stress scores on Prenatal Psychosocial Profile measure (it was not clear what other outcome information was collected). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | High risk | 1000 women were enrolled on the study. 106 women in the intervention group and 101 women in the control group were assessed as being at high risk at the first study assessment and results were only provided for the high‐risk group (i.e. approximately 20% of those randomised). Of the high‐risk groups 99 of the high‐risk intervention group and 92 of the high‐risk control group provided follow‐up data. |
| Selective reporting (reporting bias) | Unclear risk | It was not clear what outcome data were collected. |
| Other bias | Unclear risk | There was very little information on methods and there may be further outcome data not published in this paper. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not described. It is likely that women and staff were aware of group assignment. |
| Blinding of outcome assessment (detection bias) | High risk | Blinding not described. It is likely that outcome assessors were aware of group assignment. |
| Methods | A complex RCT with several arms and 4 different interventions targeting women with risk factors (depression, smoking, passive smoking and IPV). Women may have had more than 1 risk factor and may have been randomised to receive more than 1 intervention. Women at risk of IPV were randomised into intervention and control arms. | |
| Participants | Setting: 6 community prenatal clinics serving mainly African‐American women in Washington DC. July 2001‐2003. Inclusion criteria: women from minority groups (mainly African‐American) aged at least 18 years, 28 weeks pregnant or less, English speaking and resident in the study area. Exclusion criteria: women who were identified as suicidal at baseline or follow‐up were excluded. | |
| Interventions | Experimental intervention: cognitive behavioural intervention focusing on 4 risk factors (smoking, passive smoking, depression and DV). Women received an intervention specifically focusing on their individual risk factors (most women had more than one risk factor and would receive more than 1 intervention component. 336 women reported DV and 169 were randomised to the DV intervention group. The intervention was delivered as part of routine prenatal visits by psychologists or social workers. The intervention was based on empowerment theory and emphasised safety planning and behaviours and a list of phone numbers for community resources was provided. The intervention took place over several sessions lasting about 30 minutes and women received a small incentive for attending sessions. There were 2 postpartum booster sessions to reinforce messages. 51% of women in the intervention group received 4 or more sessions and a quarter attended none. Comparison group: 167 of the women reporting DV received standard care according to protocols at each clinic. | |
| Outcomes | DV was identified by Abuse Assessment Screen at baseline. Follow‐up sessions used Conflict Tactics Scale to identify women at risk. Episodes of DV during pregnancy and in the early postpartum period (minor and severe and sexual violence). Low and very low birthweight, gestational age at delivery, preterm and very preterm birth. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation scheme with site and risk specific permuted block randomisation with investigators and staff blinded to block size. |
| Allocation concealment (selection bias) | Low risk | Allocation by external data co‐ordinating centre by telephone. |
| Incomplete outcome data (attrition bias) | High risk | More than 1000 women were recruited to this trial and randomised. Randomisation was stratified according to baseline risk and only those women with DV risk were randomised for the DV intervention. (In this review we have reported findings for those women identified at risk of DV and randomised to receive or not receive the DV intervention; If we carried out analysis using all women randomised any intervention effect would be diluted considerably). 336 with DV risk had baseline data but there were considerable amounts of missing data at follow‐up, although there were some outcome data for at least 1 of the follow‐up interviews for 306 women and outcome data for babies were available for 306 women. It was reported that women were analysed by randomisation group whether or not they received the planned intervention. |
| Selective reporting (reporting bias) | Unclear risk | Most women had more than 1 risk factor and were likely to receive different interventions – the interventions may have had some synergistic or interactive effect. But results are reported only by single risk factors – i.e. this paper only focuses on women reporting DV at baseline. |
| Other bias | Unclear risk | Intervention and control group characteristics appeared similar at baseline. It was no clear how many woman received multiple interventions or whether women in the control group received other interventions to address risk factors other than DV. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Women and staff delivering intervention would be aware of group assignment. Telephone interviewers were reported to be blind to allocation but it was not clear whether this was successful (women may have revealed their allocation during interviews). |
| Blinding of outcome assessment (detection bias) | Unclear risk | Women and staff delivering intervention would be aware of group assignment. Telephone interviewers were reported to be blind to allocation but it was not clear whether this was successful (women may have revealed their allocation during interviews). |
| Methods | 3‐arm trial. Quasi‐randomisation (clinics rotated through different interventions; “monthly sequential assignment. | |
| Participants | Setting: 2 prenatal clinics in SW USA. Each clinic served 2000‐3000 pregnant women each year and 97% were Hispanic. Inclusion criteria: women who reported abuse in the year prior to or during current pregnancy by current or former male partner (mean gestational age at recruitment 18 weeks). Exclusion criteria: not described. | |
| Interventions | 335 women agreed to participate. 96% women Hispanic – and only results for these 329 women are reported in this paper. 3 interventions:
| |
| Outcomes | Follow‐up at 2, 6, 12 and 18 months post‐intervention (i.e. after delivery). Outcomes were reported abuse and use of resources. Abuse on Severity of Violence against Women Scale (SVAWS) a 46 item scale; 19 items on threats of violence and 21 items on physical violence and 6 items on sexual violence with 4 point response re how often the behaviour occurred – never (1) to many times (4). Possible scores 19‐76 on threats and 27‐108 on violence. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Women were allocated by clinic. |
| Allocation concealment (selection bias) | High risk | Women were allocated by clinic; it is possible that women attending the different clinics were different and the order in which staff delivered the interventions may have had an effect. |
| Incomplete outcome data (attrition bias) | High risk | Results only reported for Hispanic women in the sample. Results by intervention group were available for 259/329 women (79%) (> 20% missing data). |
| Selective reporting (reporting bias) | Unclear risk | Results in this paper for Hispanic women only – while they were 96% of the population it is not clear why other women were excluded or whether they were balanced across groups. Results are reported by gestational age at recruitment and over time – so there were a large number of possible correlations. |
| Other bias | Low risk | Groups were described as similar at baseline. Other bias not apparent. |
| Blinding of participants and personnel (performance bias) | High risk | No mention of blinding; lack of blinding may have affected responses and other aspects of care. |
| Blinding of outcome assessment (detection bias) | High risk | No mention of blinding; lack of blinding may have affected responses and other aspects of care. |
| Methods | 3‐arm RCT. Individual women randomised. | |
| Participants | Setting: pregnant women attending state public health clinics in 3 parishes in Louisiana USA 1999‐2000. Inclusion criteria: pregnant women less than 28 weeks’ gestation with no previous live births and Medicaid eligible. | |
| Interventions | Experimental intervention: 2 intervention arms that were combined in the results.
Control/Comparison intervention: usual care (not clearly described). | |
| Outcomes | This thesis mainly reports on participation and adherence. Long‐term outcomes included child development, abuse and neglect, injury, subsequent pregnancy, mother‐child interaction and maternal employment. At follow‐up in the third trimester (28‐34 weeks) and at 6‐8 months postpartum results were described for depression (Beck Depression Inventory) and for partner violence (current and previous) (partner violence interview) with 13 items on physical violence (0 – never experienced, 1 – has experienced) (the time frame for reporting violence was not described). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out by an external agency. |
| Allocation concealment (selection bias) | Low risk | It was stated that the nurses carrying out recruitment had no influence over randomisation which was carried out by an external agency (allocations were obtained by telephone). |
| Incomplete outcome data (attrition bias) | High risk | 357 women consented to participation and were randomised (241 in intervention groups and 116 controls). There was considerable loss to follow‐up and deviations from protocol. 19.5% of intervention women received no intervention. 32.8% did not complete the first follow‐up interview at 28‐34 weeks, and an additional 9% of the women did not have this interview until after the birth of the baby and data were therefore not included in the analysis (206 followed up at interview one and 181 available at the postpartum follow‐up). Loss was balanced across groups but this loss to follow‐up and the large number of women not receiving the allocated intervention means that results are difficult to interpret. |
| Selective reporting (reporting bias) | Unclear risk | This thesis concentrated on only a limited part of the overall research project. The large number of analyses means that some significant results may have occurred by chance. |
| Other bias | Unclear risk | There was little information on some aspects of the trial design. We are not aware that other results from this trial have been published. Groups appeared similar at baseline. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and staff were aware of group assignment. |
| Blinding of outcome assessment (detection bias) | High risk | Participants and staff were aware of group assignment. Knowledge of treatment group may have affected reporting of outcomes. |
| Methods | RCT, 3‐arm trial, individual randomisation. | |
| Participants | Low‐income, pregnant women with no previous live births referred to antenatal clinic in Denver (n = 735) were included in this study. These women were either qualified for Medicaid or had no private insurance. Setting: 21 public and private healthcare settings in Denver, Colorado USA 1994‐5. Inclusion criteria: low‐income women with no previous live births and qualified for Medicaid or had no private medical insurance. | |
| Interventions | Home visits were provided from pregnancy through to child age 2 years. The home‐visiting program had 3 broad goals, (1) to improve maternal and fetal health during pregnancy by helping women improve their health‐related behaviours; (2) to improve children’s health and development by helping parents provide more competent care; and (3) to enhance mothers’ personal development by promoting planning of future pregnancies and helping women continue their education and find work. The visitors helped women accomplish these goals by promoting the adaptive behaviours specified above, by helping them improve their relationships with key family members and friends (especially their mothers and boyfriends), and by promoting women’s use of health and human services. Nurse home visitors were required to have a degree and experience in community or maternal and child health nursing, whereas para‐professionals were expected to have a high school education, no college preparation in the helping professions, and strong people skills. Women were randomised into 3 groups: Women in treatment 1 (n = 255) were provided with free developmental screening and referral for their children at 6, 12, 15, 21, and 24 months of age. Women in treatment 2 (n = 245) were provided with the screening offered in treatment 1 plus para‐professional home visiting during pregnancy and the child’s first 2 years of life. Women in treatment 3 (n = 235) were provided with the screening offered in treatment 1 plus nurse home visiting during pregnancy and the child's first 2 years. | |
| Outcomes | Outcomes consisted of maternal reports of subsequent pregnancies, participation in education and work, use of welfare, marriage, cohabitation, experience of domestic violence, mental health, substance use, and sense of mastery; observations of mother‐child interaction and the home environment; tests of children’s language and executive functioning; and mothers’ reports of children’s externalising behaviour problems. A large number of outcomes were reported in this study where follow‐up continued into late childhood. The paper relating to the follow‐up when the child was four years old collected data relating to child development, subsequent pregnancies, drug and alcohol use and episodes of DV during previous 6 months and since the child was 2 years (i.e. 3.5 years and 2‐4 years postpartum). | |
| Notes | The data reported in this review were from a paper reporting a follow‐up study of mothers and children in their homes near the child’s fourth birthday, 2 years after the end of the program. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation by computer by external operations office. |
| Allocation concealment (selection bias) | Low risk | External randomisation service. |
| Incomplete outcome data (attrition bias) | Unclear risk | 735 women randomised and 695 followed up at 4 years. There were missing data for some variables. |
| Selective reporting (reporting bias) | Unclear risk | It was not clear that all outcomes had been prespecified before the onset of the study. The study resulted in multiple publications. |
| Other bias | Unclear risk | Groups appeared comparable at baseline and follow‐up rates were relatively high. |
| Blinding of participants and personnel (performance bias) | High risk | Women and staff were aware of treatment group. |
| Blinding of outcome assessment (detection bias) | Unclear risk | It was reported that follow‐up data were collected by investigators who were blind to group assignments. |
| Methods | Study described as multi‐stage, longitudinal and randomised. Mixed‐methods trial. An urban sample of women was individually randomised to treatment groups (n = 92); 12 rural county health departments were randomised by site, 6 to treatment and 6 to placebo (cluster‐randomisation, n = 147). | |
| Participants | Participants were English speaking women, 31 weeks’ gestation and higher reporting abuse within the last 12 months, those registered in health department perinatal home visitation programs. | |
| Interventions | The usual care (UC) group received the standard home visitation (HV) and the Domestic Violence Enhanced Home Visitation Program (DOVE) was the intervention.DOVE intervention group received the standard HV in addition to the DOVE IPV intervention. Women in the DOVE intervention group received 3 prenatal and 3 postnatal DOVE sessions in addition to their HV protocols. | |
| Outcomes | Recruitment rate and retention rate. | |
| Notes | None of these outcomes are relevant to our review but future studies may report our primary and secondary outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised. Sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Unclear risk. Allocation concealment not described. |
| Incomplete outcome data (attrition bias) | Low risk | A total of 339 abused pregnant women were eligible for randomisation; 42 women refused, and 239 women were randomly assigned (124 DOVE; 115 usual care), resulting in a 71% recruitment rate. Retention rates from baseline included 93% at delivery, 80% at 3 months, 76% at 6 months, and 72% at 12 months. |
| Selective reporting (reporting bias) | High risk | No original outcome is reported in this publication. |
| Other bias | Unclear risk | Unknown. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not clear, blinding not mentioned. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not clear, blinding not mentioned. |
| Methods | RCT. 2‐arm trial with individual randomisation. | |
| Participants | Setting: public hospital in Hong Kong, May 2002–June 2003. Inclusion criteria: 110 women identified as abused by intimate partner. Pregnant women over 18 and less than 30 weeks’ gestation attending for first antenatal visit. Women had “answered ‘yes’ to being physically or emotionally abused by someone or forced to have sexual activities within the last year” (Abuse Assessment Screen). Exclusion criteria: no reported abuse or abused by someone other than their partner. | |
| Interventions | Experimental intervention: 55 women (51 followed up) Intervention based on empowerment and empathic understanding. The aim of the intervention was to enhance independence and control. In a 30‐minute interview with a midwife researcher women were advised on safety and problem solving (the intervention was tailored for use with Chinese women). Women were also given a brochure (it was not clear whether this intervention was in addition to standard care. Control/Comparison intervention: 55 women (all followed up). Standard care. Women were given written information about community resources to support abused women. | |
| Outcomes | Conflict Tactics scale (CTS) mean scores (with scores for minor and severe physical violence and psychological and sexual abuse); General Health scores; EPDS; and satisfaction with intervention. Women were followed up by telephone interview at 6 weeks postpartum. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The allocation schedule was generated by a computer. |
| Allocation concealment (selection bias) | Low risk | Allocation was “concealed in consecutively numbered sealed envelopes” by a researcher not involved in the study. |
| Incomplete outcome data (attrition bias) | Low risk | 110 women were randomised (55 in each group). 4 women were lost to follow‐up and it was stated that an intention‐to‐treat analysis was carried out although it was not clear what this meant. |
| Selective reporting (reporting bias) | Unclear risk | Assessment from published study report. |
| Other bias | Low risk | No other sources of bias identified. There did appear to be differences between groups at baseline but it is not clear whether or to what extent baseline differences influenced results. |
| Blinding of participants and personnel (performance bias) | High risk | Women and care providers would not be blind to randomisation group. |
| Blinding of outcome assessment (detection bias) | Low risk | It was stated that outcome assessment was carried out by researchers unaware of allocation and that women did not reveal their group until the end of the follow‐up interview. |
| Methods | RCT. 2 arms with individual randomisation. | |
| Participants | Women attending for prenatal care were recruited from 2 primary care clinics and a private clinic in Rhode Island (USA). Inclusion criteria: 54 pregnant women aged between 18 and 40 years who screened positive for recent (past year) DV on the Revised Conflict Tactics Scale. (Gestational age at recruitment not clear.) Exclusion criteria: women with a current affective disorder, post‐traumatic stress disorder or current substance abuse were excluded and referred for appropriate treatment. | |
| Interventions | Experimental intervention: (28 women randomised.) an intervention based on principles of interpersonal psychotherapy which aimed to enhance social support as a means of reducing depression, encouraging service use and reducing partner violence. The intervention also included empowerment and stabilisation components. The intervention involved four 60‐minute individual, scripted sessions during pregnancy and a booster session within 2 weeks of the birth; delivered by 2 trained staff. Control/Comparison intervention: (26 women randomised.) usual medical care which included educational material and list of resources for DV. Women in both groups received financial compensation for completing assessments. | |
| Outcomes | Assessed at baseline, 5‐6 weeks after recruitment, 2 weeks after the birth and 3 months postpartum. Physical, sexual and psychological attacks measured on Revised Conflict Tactic scale (at baseline and then since last assessment). Major depressive disorder (assessed on Longitudinal Interval Follow‐up Examination (LIFE)). Postnatal depression score on EPDS. Post traumatic stress (on Davidson Trauma scale). History of trauma. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated schedule. |
| Allocation concealment (selection bias) | Low risk | Allocations concealed in consecutively numbered, sealed envelopes; allocation was by an investigator blind to baseline assessments. |
| Incomplete outcome data (attrition bias) | Unclear risk | 54 women were randomised and there were outcome data for 46 (85%). Information on women lost to follow‐up was not provided. It was stated that analyses were by intention‐to‐treat. |
| Selective reporting (reporting bias) | Unclear risk | Assessment from published study reports. |
| Other bias | Low risk | No other bias is apparent. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding women, staff providing care and staff delivering the intervention to this type of intervention is not feasible. It is not clear how outcome data were collected |
| Blinding of outcome assessment (detection bias) | Unclear risk | It is not clear how outcome data were collected. |
DV: domestic violence
EPDS: Edinburgh Postnatal Depression Scale
IPV: intimate partner violence
RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| The population in this study were not pregnant women.This was a trial examining an intervention in the postnatal period. There was no intervention in pregnancy and women were not recruited until after the birth. The intervention was delivered by child health nurses who offered weekly visits to support mothers and enhance parenting confidence with advice on child development and behaviour and facilitate access to other services. Individually tailored to family circumstances. | |
| Women recruited to this study were not pregnant. The trial examined early childhood home visits to improve family functioning and reduce child maltreatment. Para‐professionals gave advice on child development and parenting and offered support. The first visit was scheduled within a week of the birth and visits were thereafter scheduled weekly at first then tapering off for up to 3 years (mean of 13 visits in first year). | |
| This study used samples from RCT study of Domestic Violence Enhanced Home Visitation (DOVE) to conduct a qualitative study. Reported depression scores are based on correlation with relationship with mother. This study does not fit with our review objectives. | |
| This study examined whether an antenatal health assessment form identified women with risk factors for postnatal depression (including DV). There was no intervention to prevent or reduce IPV. | |
| This study had an DV component but the objective did not meet this review criteria as it was looking into the effect of intervention on smoking cessation and DV reported as a part of secondary outcome. | |
| Target populations were not pregnant women. They were facilitators and trainers from various countries (n = 21). | |
| This is a descriptive population based study with important findings on the effect of DV on pregnancy outcome. However, it is not a RCT. | |
| This was a proposal for a study reported in a trial registration; the planned trial did not take place. | |
| This study did not examine interventions to prevent IPV rather it compared 2 different methods of increasing disclosure about DV. | |
| Women in this study were not pregnant. Participants included 399 English‐speaking women aged 16 years and older who referred to emergency department, | |
| This cohort study investigates the effect of police report on pregnancy outcome of women suffering DV. | |
| This was a longitudinal study with no randomisation and blinding. | |
| Intervention involved consultation pertaining to DV prevention but none of the our priori outcome of interest was reported. | |
| This study was not a RCT. | |
| The participants in this study were women attending family planning clinics; the women were not pregnant. The study was looking at reproductive coercion. | |
| This was not a RCT. | |
| Women were recruited to this study during pregnancy but were not randomised until after delivery and the intervention did not start until the postnatal period. The intervention was a postnatal home‐visiting service by nurse‐midwives aimed at “reducing adverse neonatal outcomes and in improving knowledge about contraception, vaccination schedules, and breastfeeding in teenage mothers younger than age 18 years” Structured home visits at 1, and 2 weeks and 1, 2, 4 and 6 months after the birth. Each visit lasted 1‐4 hours. Content of visits included infant feeding advice and support, information on vaccinations and to facilitate attendance for vaccinations, discussion of mood disorders and information on parenting. Follow‐up of any issues (which could include violence) raised at 2 months postpartum, discussion of issues re drugs and alcohol and advice on contraception. | |
| The women recruited to this study were not all pregnant. The sample included women who were pregnant, who had a child under 5 or who otherwise were at high risk of IPV. Women in the intervention arm received up to 12 months support from trained and supported non‐professional mentor mothers. Women in the intervention arm received up to 12 months support from a trained mentor. (No separate breakdown for pregnant women experiencing DV). |
DV: domestic violence
IPV: intimate partner violence
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT. |
| Participants | Participants were adolescent couples; women were pregnant at recruitment. |
| Interventions | A counselling intervention was compared with routine care. |
| Outcomes | Outcomes were episodes of violence within couples. It was not clear whether women or their partners were the victims of the violence; authors report that much of the violence was reciprocal. |
| Notes | We have contacted the authors to see if we can obtain data for women only. [email protected] (author contacted 20th June 2012). |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Enhanced Nurse Home Visitation Program To Prevent Intimate Partner Violence |
| Methods | RCT. |
| Participants | Women during pregnancy and postpartum. 250 women referred to the Multnomah County Health Department will be randomised to the experimental (NFP plus ECI) or control condition (NFP) and visited according to the regular NFP schedule during pregnancy and until the infant is 24 months old. |
| Interventions | Enhanced Nurse Home Visitation Program To Prevent Intimate Partner Violence. It is based on a choice or empowerment model whereby women can choose among interventions related to her goal for her current intimate relationship.The intervention concentrated on the prenatal and immediate (first 6 months) postpartum period with regular IPV, emotional abuse and controlling behaviour assessments throughout the study period. |
| Outcomes | Baseline and outcome measurement (CTS2, WEB, TPMI, depression ‐ Edinburgh, & parenting stress), screened at 3 months before delivery, 9 months and 21 months postpartum. |
| Starting date | January 2007 start date. End date October 2010. |
| Contact information | Principal Investigator: Lynette F Feder, PhD University of Central Florida, [email protected] |
| Notes | We have been unable to find any additional reports on this trial to confirm that the study has been completed. We emailed the author on 18/8/2014, but we have had no reply. |
| Trial name or title | The Dil Mil trial |
| Methods | RCT using a parallel comparison. |
| Participants | Young married pregnant women (18 to 30 years old) with a history of domestic violence in the first or second trimester of pregnancy (daughter‐in‐laws (DILs) and their mother‐in‐laws' (MILs). |
| Interventions | Intervention consists of 2 half‐day group sessions with DILs, 5 half‐day group sessions with MILs, and 1 joint half‐day session with DILs and MILs. |
| Outcomes | Domestic violence incidence, related health outcomes (perceived quality of life, psychosocial status, and maternal and infant health), knowledge of links between GBV and health, gender‐equitable attitudes, relationship with DILs (communication social support, support of freedom of movement), reduction in GBV perpetration, resistance to GBV inflicted by son, knowledge of safety and the links between GBV and health, gender‐equitable attitudes, decision‐making skills, freedom of movement, resistance to GBV by husband. |
| Starting date | Starting date unclear. |
| Contact information | Suneeta Krishnan, [email protected]. |
| Notes | This study is at recruitment stage. No results were available at the time of review update. |
| Trial name or title | Impact of Women's Empowerment Program for Abused Pregnant Women |
| Methods | RCT with parallel assignment. |
| Participants | Abused pregnant women aged 18 to 35 years of age with a history of suffering from physical abuse. |
| Interventions | Behavioural intervention aiming to empower women. The one‐our intervention, delivered over a 11‐week period, consisted of an empowerment and additional components adapted from freedom program run to support domestic abused women. The control arm received standard care, which was routine check ups with care provided by healthcare professionals. |
| Outcomes | Rate of episode of domestic violence, health status and safety behaviour. |
| Starting date | January 2013. Completion August 2013 with June 2013 final data collection date for primary outcome measure. |
| Contact information | Neha Sharma, PhD, Macmillan research group UK. (No email published on protocol.) |
| Notes | It is unclear whether this trial has been completed. |
| Trial name or title | MOVE, a cluster‐randomised trial of screening and referral in primary health care |
| Methods | A cluster‐randomised trial. |
| Participants | Nurses and pregnant mothers. |
| Interventions | IPV screening. |
| Outcomes | 1. For nurses: whether nurses inquire about IPV among their client population, referring women experiencing IPV to services, Inquire about the safety of women and children in the relationship. 2. For pregnant women:whether women are asked about IPV, disclose/discuss any abuse and are satisfied with the quality of care and support they receive. 3. Proportion of MCH clients who have ever, or who are currently, experiencing IPV and those abused when pregnant. |
| Starting date | Start and completion dates unclear. |
| Contact information | Angela J Taft ([email protected]) |
| Notes | This report is a protocol for the MOVE, a cluster‐randomised trial of screening and referral in primary health care. |
| Trial name or title | Intimate Partner Violence and Pregnancy, a Perinatal Care Intervention Study (MOM) |
| Methods | A single‐blind randomised controlled trial with parallel assignment. |
| Participants | Pregnant victims of partner violence (n = 150) |
| Interventions | Perinatal Care Intervention study that looks into the Impact of a resource card. The intervention group will receive an envelope with a gift voucher and a resource card (wallet size card with on the one side safety measures and on the other side contact details of resources for violence).The control group will receive the same envelope with a gift voucher and a letter of thanks. |
| Outcomes | Evolution of partner violence, help‐seeking behaviour of the pregnant victims of partner violence. |
| Starting date | June 2010. Estimated completion date March 2014. |
| Contact information | An‐Sofie Van Parys, Universiteit Gent, [email protected] |
| Notes | The contact author was emailed on 21/08/2014; data are not yet available because women are still being interviewed. Data may be available for next update. |
CTS: Conflict Tactics Scale
IPV: intimate partner violence
RCT: randomised controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Partner abuse: episodes during pregnancy Show forest plot | 1 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.25, 1.02] |
| Analysis 1.1 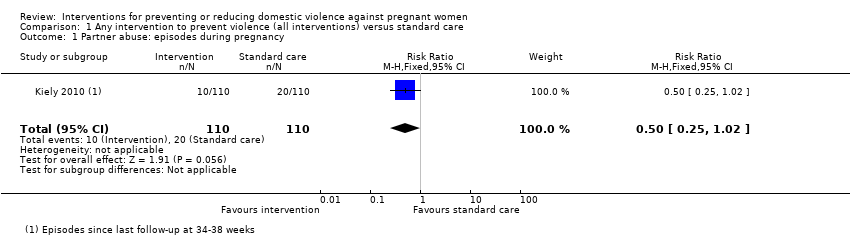 Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 1 Partner abuse: episodes during pregnancy. | ||||
| 2 Partner abuse: episodes during the first 3 months postpartum Show forest plot | 1 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.35, 1.04] |
| Analysis 1.2  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 2 Partner abuse: episodes during the first 3 months postpartum. | ||||
| 3 Partner abuse: abuse score first 3 months postpartum (Conflict Tactics Scale) Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 4.20 [‐10.74, 19.14] |
| Analysis 1.3  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 3 Partner abuse: abuse score first 3 months postpartum (Conflict Tactics Scale). | ||||
| 4 Partner abuse: abuse score in first 3 months postpartum (Conflict Tactics Scale) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.4 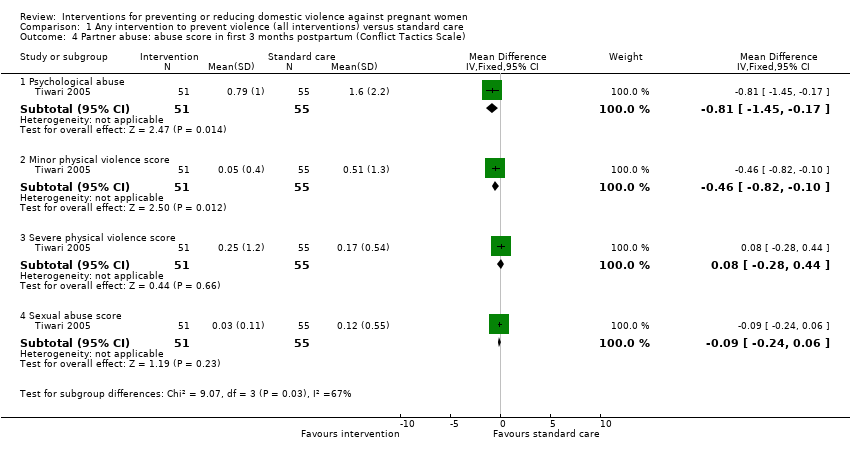 Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 4 Partner abuse: abuse score in first 3 months postpartum (Conflict Tactics Scale). | ||||
| 4.1 Psychological abuse | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.81 [‐1.45, ‐0.17] |
| 4.2 Minor physical violence score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.82, ‐0.10] |
| 4.3 Severe physical violence score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.28, 0.44] |
| 4.4 Sexual abuse score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.24, 0.06] |
| 5 Partner abuse in the first 3 months postpartum (Current abuse score) Show forest plot | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.31, 0.07] |
| Analysis 1.5  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 5 Partner abuse in the first 3 months postpartum (Current abuse score). | ||||
| 6 Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum) Show forest plot | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.43, 0.88] |
| Analysis 1.6  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 6 Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum). | ||||
| 7 Partner violence at 7‐8 months postpartum Show forest plot | 1 | 181 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.23, 1.21] |
| Analysis 1.7  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 7 Partner violence at 7‐8 months postpartum. | ||||
| 8 Women with depression (after the intervention) during pregnancy Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.31] |
| Analysis 1.8  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 8 Women with depression (after the intervention) during pregnancy. | ||||
| 9 Mean Depression Episodes, Psychiatric Status Rating) Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.97, 0.05] |
| Analysis 1.9 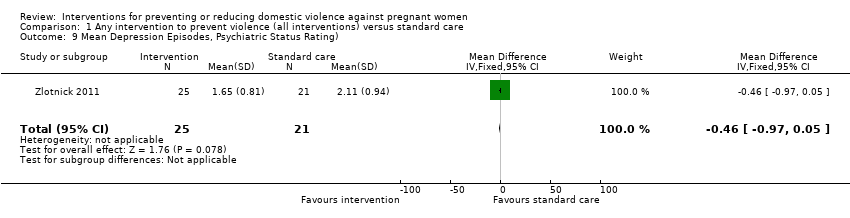 Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 9 Mean Depression Episodes, Psychiatric Status Rating). | ||||
| 10 Depression scores (after the intervention) during pregnancy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Women with depression up to 3 months postpartum Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.11 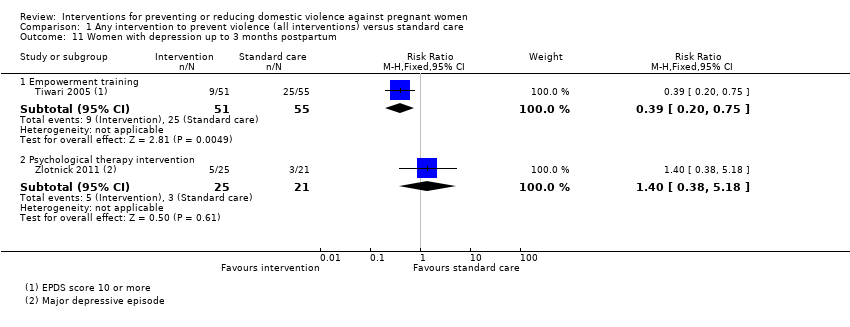 Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 11 Women with depression up to 3 months postpartum. | ||||
| 11.1 Empowerment training | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.20, 0.75] |
| 11.2 Psychological therapy intervention | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.38, 5.18] |
| 12 Depression scores up to 3 months postpartum Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐1.88 [‐5.24, 1.48] |
| Analysis 1.12  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 12 Depression scores up to 3 months postpartum. | ||||
| 13 Women with depression up to 1 year postpartum Show forest plot | 1 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.37, 1.98] |
| Analysis 1.13  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 13 Women with depression up to 1 year postpartum. | ||||
| 14 Depression scores up to 1 year postpartum Show forest plot | 1 | 182 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐2.41, 1.11] |
| Analysis 1.14  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 14 Depression scores up to 1 year postpartum. | ||||
| 15 Apgar score less than 7 at 1 minute | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Apgar score less than 7 at 5 minutes | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Stillbirth | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Neonatal death | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Miscarriage (up to 20 weeks) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Antepartum haemorrhage | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Placental abruption | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Mean infant birthweight (g) Show forest plot | 1 | 306 | Mean Difference (IV, Fixed, 95% CI) | 41.0 [‐106.19, 188.19] |
| Analysis 1.23 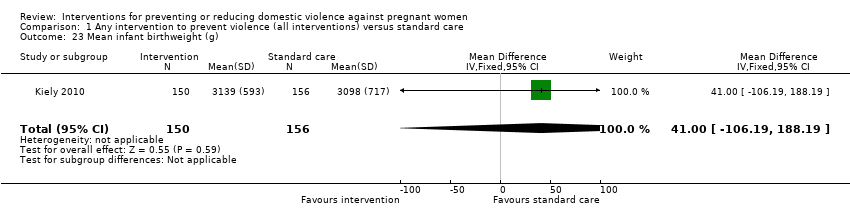 Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 23 Mean infant birthweight (g). | ||||
| 24 Number of low‐birthweight (< 2500 g) babies Show forest plot | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.41, 1.32] |
| Analysis 1.24 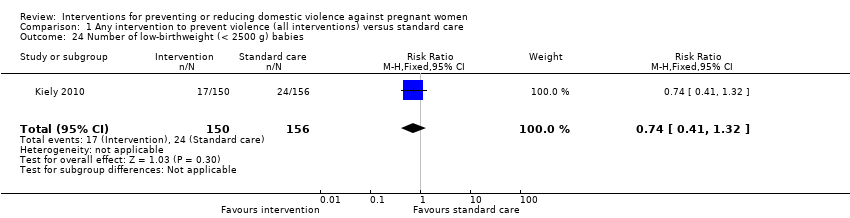 Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 24 Number of low‐birthweight (< 2500 g) babies. | ||||
| 25 Preterm labour (before 37 weeks' gestation) Show forest plot | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.40, 1.20] |
| Analysis 1.25  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 25 Preterm labour (before 37 weeks' gestation). | ||||
| 26 (Non‐prespecified outcome) Mean gestational age at birth (weeks) Show forest plot | 1 | 306 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.33, 2.47] |
| Analysis 1.26  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 26 (Non‐prespecified outcome) Mean gestational age at birth (weeks). | ||||
| 27 (Non‐prespecified outcome) Women adopting safety behaviours Show forest plot | 1 | 204 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.6 [1.41, 4.79] |
| Analysis 1.27  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 27 (Non‐prespecified outcome) Women adopting safety behaviours. | ||||
| 28 (Non‐prespecified outcome) stress score in late pregnancy Show forest plot | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐2.06 [‐3.34, ‐0.78] |
| Analysis 1.28  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 28 (Non‐prespecified outcome) stress score in late pregnancy. | ||||
| 29 (Non‐prespecified outcome) Did not discuss abuse with care providers Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.04, 0.66] |
| Analysis 1.29 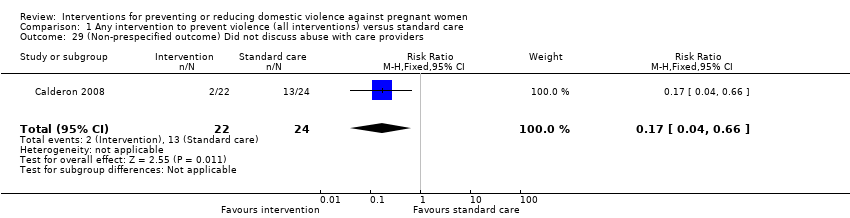 Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 29 (Non‐prespecified outcome) Did not discuss abuse with care providers. | ||||
| 30 (Non‐prespecified outcome) Women reporting any domestic violence 2‐4 years postpartum Show forest plot | 1 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.60, 1.08] |
| Analysis 1.30  Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 30 (Non‐prespecified outcome) Women reporting any domestic violence 2‐4 years postpartum. | ||||
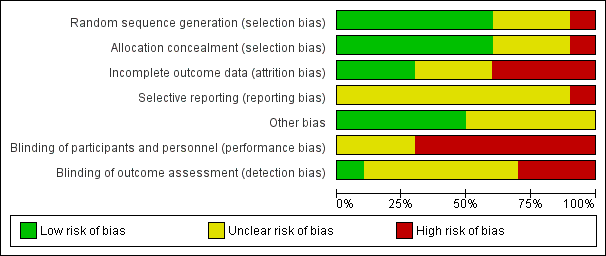
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
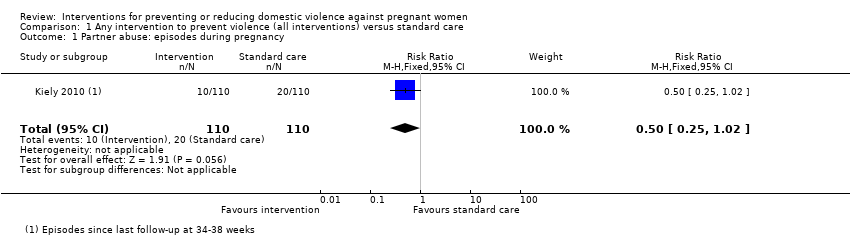
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 1 Partner abuse: episodes during pregnancy.
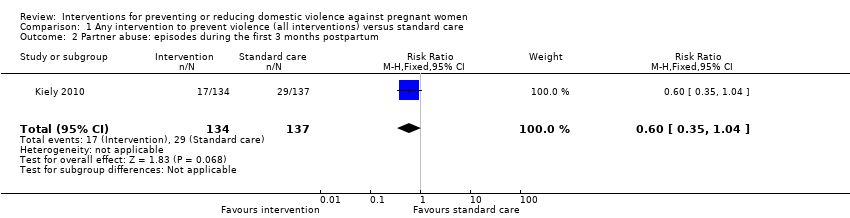
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 2 Partner abuse: episodes during the first 3 months postpartum.
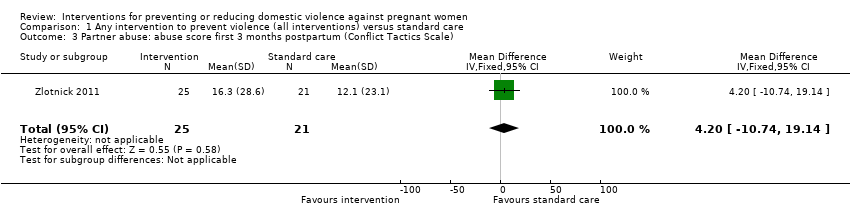
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 3 Partner abuse: abuse score first 3 months postpartum (Conflict Tactics Scale).

Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 4 Partner abuse: abuse score in first 3 months postpartum (Conflict Tactics Scale).
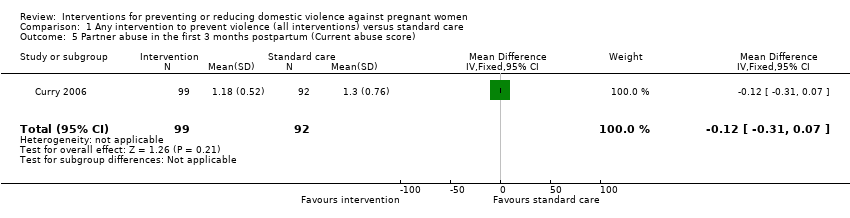
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 5 Partner abuse in the first 3 months postpartum (Current abuse score).
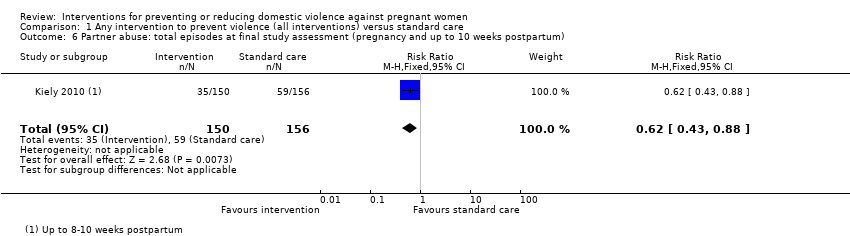
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 6 Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum).
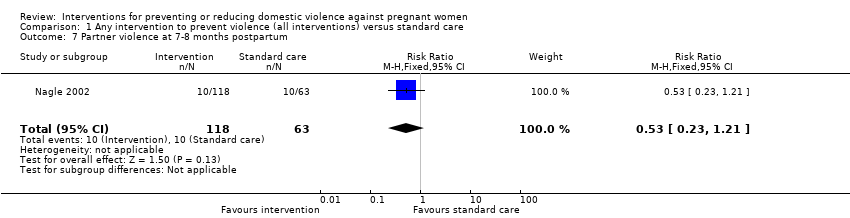
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 7 Partner violence at 7‐8 months postpartum.
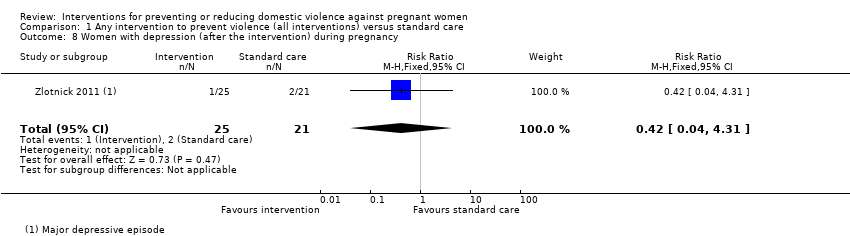
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 8 Women with depression (after the intervention) during pregnancy.
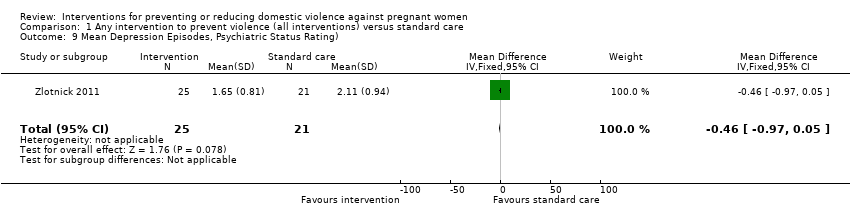
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 9 Mean Depression Episodes, Psychiatric Status Rating).
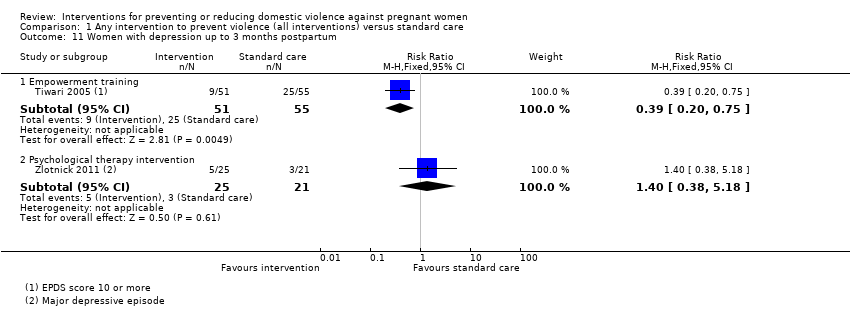
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 11 Women with depression up to 3 months postpartum.
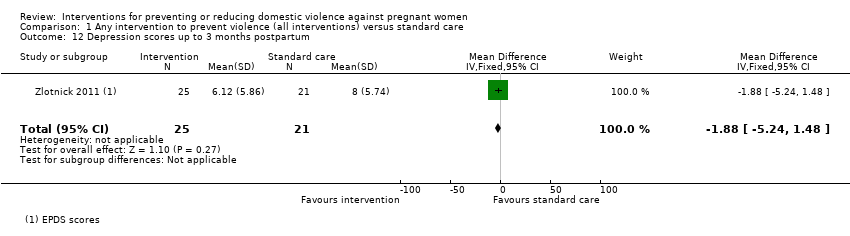
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 12 Depression scores up to 3 months postpartum.

Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 13 Women with depression up to 1 year postpartum.

Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 14 Depression scores up to 1 year postpartum.
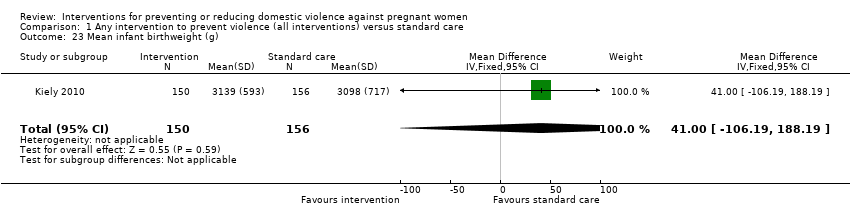
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 23 Mean infant birthweight (g).

Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 24 Number of low‐birthweight (< 2500 g) babies.

Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 25 Preterm labour (before 37 weeks' gestation).

Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 26 (Non‐prespecified outcome) Mean gestational age at birth (weeks).
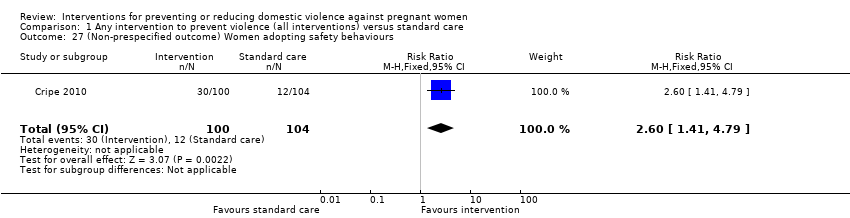
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 27 (Non‐prespecified outcome) Women adopting safety behaviours.
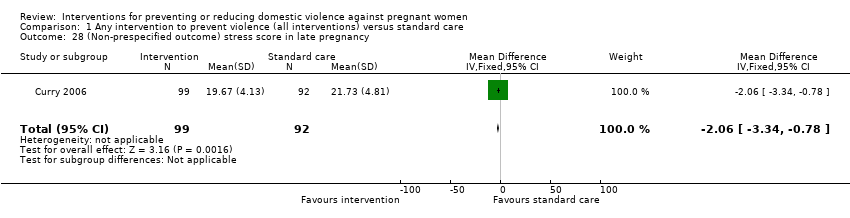
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 28 (Non‐prespecified outcome) stress score in late pregnancy.
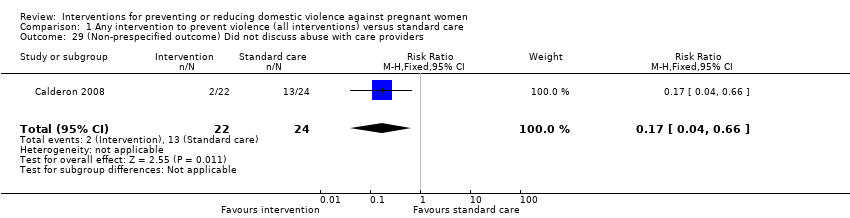
Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 29 (Non‐prespecified outcome) Did not discuss abuse with care providers.

Comparison 1 Any intervention to prevent violence (all interventions) versus standard care, Outcome 30 (Non‐prespecified outcome) Women reporting any domestic violence 2‐4 years postpartum.
| Any intervention to prevent violence (all interventions) versus standard care for preventing or reducing domestic violence against pregnant women | ||||||
| Patient or population: all pregnant women | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Any intervention to prevent violence (all interventions) versus standard care | |||||
| Partner abuse: episodes during pregnancy | Study population | RR 0.5 | 220 | ⊕⊝⊝⊝ | ||
| 182 per 1000 | 91 per 1000 | |||||
| Partner abuse: episodes during the first 3 months postpartum | Study population | RR 0.6 | 271 | ⊕⊝⊝⊝ | ||
| 212 per 1000 | 127 per 1000 | |||||
| Partner abuse: abuse score in the first 3 months postpartum (Conflict Tactics Score*) The CTS is a 19‐item self‐report scale listing behaviours that the respondent’s partner might use in conflicts. Women report the frequency of partner behaviours over the past year on a 7‐point scale where 0 = never and 6 = 20 or more times. | The mean partner abuse: abuse score in the first 3 months postpartum in the intervention groups was | 46 | ⊕⊝⊝⊝ | |||
| Partner abuse in the first 3 months postpartum (Current Abuse Score**) The Current abuse score consists of 2 scales: 1) Abuse Assessment Screen (AAS) and 2) Prenatal Psychosocial Profile (PPP). | The mean partner abuse in the first 3 months postpartum (current abuse score) in the intervention groups was | 191 | ⊕⊝⊝⊝ | |||
| Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum) | Study population | RR 0.62 | 306 | ⊕⊕⊕⊝ | ||
| 378 per 1000 | 234 per 1000 | |||||
| Number of low‐birthweight (< 2500 g) babies | Study population | RR 0.74 | 306 | ⊕⊕⊝⊝ | ||
| 154 per 1000 | 114 per 1000 | |||||
| *The Abuse Assessment Screen (AAS) tool was used to for screening. Respondents who answered ‘yes’ to being physically or emotionally hurt by someone or forced to have sexual activities within the last year were considered abused. These women, who responded "Yes" to AAS tool, were administered the Conflict Tactics Score (CTS). RR: risk ratio; CI: confidence interval | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 All studies contributing data had design limitations. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Partner abuse: episodes during pregnancy Show forest plot | 1 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.25, 1.02] |
| 2 Partner abuse: episodes during the first 3 months postpartum Show forest plot | 1 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.35, 1.04] |
| 3 Partner abuse: abuse score first 3 months postpartum (Conflict Tactics Scale) Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 4.20 [‐10.74, 19.14] |
| 4 Partner abuse: abuse score in first 3 months postpartum (Conflict Tactics Scale) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 Psychological abuse | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.81 [‐1.45, ‐0.17] |
| 4.2 Minor physical violence score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.82, ‐0.10] |
| 4.3 Severe physical violence score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.28, 0.44] |
| 4.4 Sexual abuse score | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.09 [‐0.24, 0.06] |
| 5 Partner abuse in the first 3 months postpartum (Current abuse score) Show forest plot | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.31, 0.07] |
| 6 Partner abuse: total episodes at final study assessment (pregnancy and up to 10 weeks postpartum) Show forest plot | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.43, 0.88] |
| 7 Partner violence at 7‐8 months postpartum Show forest plot | 1 | 181 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.23, 1.21] |
| 8 Women with depression (after the intervention) during pregnancy Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.31] |
| 9 Mean Depression Episodes, Psychiatric Status Rating) Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐0.46 [‐0.97, 0.05] |
| 10 Depression scores (after the intervention) during pregnancy | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Women with depression up to 3 months postpartum Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Empowerment training | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.20, 0.75] |
| 11.2 Psychological therapy intervention | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.38, 5.18] |
| 12 Depression scores up to 3 months postpartum Show forest plot | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | ‐1.88 [‐5.24, 1.48] |
| 13 Women with depression up to 1 year postpartum Show forest plot | 1 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.37, 1.98] |
| 14 Depression scores up to 1 year postpartum Show forest plot | 1 | 182 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐2.41, 1.11] |
| 15 Apgar score less than 7 at 1 minute | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Apgar score less than 7 at 5 minutes | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Stillbirth | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Neonatal death | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Miscarriage (up to 20 weeks) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Maternal mortality | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Antepartum haemorrhage | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Placental abruption | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Mean infant birthweight (g) Show forest plot | 1 | 306 | Mean Difference (IV, Fixed, 95% CI) | 41.0 [‐106.19, 188.19] |
| 24 Number of low‐birthweight (< 2500 g) babies Show forest plot | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.41, 1.32] |
| 25 Preterm labour (before 37 weeks' gestation) Show forest plot | 1 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.40, 1.20] |
| 26 (Non‐prespecified outcome) Mean gestational age at birth (weeks) Show forest plot | 1 | 306 | Mean Difference (IV, Fixed, 95% CI) | 1.40 [0.33, 2.47] |
| 27 (Non‐prespecified outcome) Women adopting safety behaviours Show forest plot | 1 | 204 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.6 [1.41, 4.79] |
| 28 (Non‐prespecified outcome) stress score in late pregnancy Show forest plot | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐2.06 [‐3.34, ‐0.78] |
| 29 (Non‐prespecified outcome) Did not discuss abuse with care providers Show forest plot | 1 | 46 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.04, 0.66] |
| 30 (Non‐prespecified outcome) Women reporting any domestic violence 2‐4 years postpartum Show forest plot | 1 | 735 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.60, 1.08] |

