Pomagala za položaj spavanja za djecu s cerebralnom paralizom
Appendices
Appendix 1. Electronic search strategies
Cochrane Library databases
Cochrane Central Register of Controlled Trials (CENTRAL)
Cochrane Database of Systematic Reviews (CDSR)
Database of Abstracts of Reviews of Effects (DARE)
Cochrane Methodology Register (CMR)
Health Technology Assessment (HTA) Database
NHS Economic Evaluation Database (EED)
#1 MeSH descriptor Cerebral Palsy explode all trees
#2 (cerebral NEXT palsy):ti,ab
#3 CP:ti,ab
#4 spastic*:ti,ab
#5 quadriplegi*:ti,ab
#6 tetrapleg*:ti,ab
#7 dipleg*:ti,ab
#8 MeSH descriptor Quadriplegia explode all trees
#9 (disab* NEAR/7 child*):ti,ab
#10 (handicap* NEAR/3 child*):ti,ab
#11 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10)
#12 positioning:ti,ab
#13 (sleep* NEXT position*):ti,ab
#14 (sleep* NEXT system*):ti,ab
#15 (sleep NEXT management):ti,ab
#16 (sleep* NEXT support*):ti,ab
#17 (postural NEXT support*):ti,ab
#18 (postural NEXT position*):ti,ab
#19 (postural NEXT management):ti,ab
#20 (postural NEXT system*):ti,ab
#21 (night NEXT time NEXT support*):ti,ab
#22 (night NEXT time NEXT position*):ti,ab
#23 (lying NEXT support*):ti,ab
#24 (lying NEXT position*):ti,ab
#25 (supine NEXT position*):ti,ab
#26 chailey:ti,ab
#27 dreama:ti,ab
#28 sleepform:ti,ab
#29 moonlight:ti,ab
#30 symmetrisleep:ti,ab
#31 snoooo*:ti,ab
#32 "simple stuff works":ti,ab
#33 (#12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #32)
#34 (#11 AND #33)
Ovid MEDLINE
1 Cerebral Palsy/
2 cerebral palsy.ti,ab.
3 CP.ti,ab.
4 spastic*.ti,ab.
5 quadriplegi*.ti,ab.
6 Quadriplegia/
7 tetraplegi*.ti,ab.
8 diplegi*.ti,ab.
9 disabled children/
10 (disab* adj7 child*).ti,ab.
11 (handicap* adj3 child*).ti,ab.
12 or/1‐11
13 positioning.ti,ab.
14 sleep* position*.ti,ab.
15 sleep system*.ti,ab.
16 sleep management.ti,ab.
17 sleep* support*.ti,ab.
18 postural support*.ti,ab.
19 postural position*.ti,ab.
20 postural management.ti,ab.
21 postural system*.ti,ab.
22 night time support*.ti,ab.
23 night time position*.ti,ab.
24 lying support*.ti,ab.
25 lying position*.ti,ab.
26 supine position*.ti,ab.
27 chailey.ti,ab.
28 dreama.ti,ab.
29 sleepform.ti,ab.
30 moonlight.ti,ab.
31 moonlite.ti,ab.
32 symmetrisleep.ti,ab.
33 snoooo*.ti,ab.
34 simple stuff works.ti,ab.
35 or/13‐34
36 12 and 35
Ovid EMBASE
1 Cerebral Palsy/
2 cerebral palsy.ti,ab.
3 CP.ti,ab.
4 spastic*.ti,ab.
5 quadriplegi*.ti,ab.
6 Quadriplegia/
7 tetraplegi*.ti,ab.
8 diplegi*.ti,ab.
9 disabled children/
10 (disab* adj7 child*).ti,ab.
11 (handicap* adj3 child*).ti,ab.
12 or/1‐11
13 positioning.ti,ab.
14 sleep* position*.ti,ab.
15 sleep system*.ti,ab.
16 sleep management.ti,ab.
17 sleep* support*.ti,ab.
18 postural support*.ti,ab.
19 postural position*.ti,ab.
20 postural management.ti,ab.
21 postural system*.ti,ab.
22 night time support*.ti,ab.
23 night time position*.ti,ab.
24 lying support*.ti,ab.
25 lying position*.ti,ab.
26 supine position*.ti,ab.
27 chailey.ti,ab.
28 dreama.ti,ab.
29 sleepform.ti,ab.
30 moonlight.ti,ab.
31 moonlite.ti,ab.
32 symmetrisleep.ti,ab.
33 snoooo*.ti,ab.
34 simple stuff works.ti,ab.
35 or/13‐34
36 12 and 35
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCOhost)
S32 (S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30) AND (S9 and S31)
S31 S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30
S30 TI "simple stuff works" OR AB "simple stuff works"
S29 TI snoooo* OR AB snoooo*
S28 TI symmetrisleep OR AB symmetrisleep
S27 TI moonlight OR AB moonlight OR TI moonlite OR AB moonlite
S26 TI sleepform OR AB sleepform
S25 TI dreama OR AB dreama
S24 TI chailey OR AB chailey
S23 TI "supine position*" OR AB "supine position*"
S22 TI "lying position*" OR AB "lying position*"
S21 TI "lying support*" OR AB "lying support*"
S20 TI "night time position*" OR AB "night time position*"
S19 TI "night time support*" OR AB "night time support*"
S18 TI "postural system*" OR AB "postural system*"
S17 TI "postural management" OR AB "postural management"
S16 TI "postural position*" OR AB "postural position*"
S15 TI "postural support*" OR AB "postural support*"
S14 TI "sleep support*" OR AB "sleep support*"
S13 TI "sleep management" OR AB "sleep management"
S12 TI "sleep system*" OR AB "sleep system*"
S11 TI "sleep position*" OR AB "sleep position*"
S10 TI Positioning OR AB Positioning
S9 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8
S8 TI handicap* N7 child* OR AB handicap* N7 child*
S7 TI disab* N7 child* OR AB disab* N7 child*
S6 TI dipleg* OR AB dipleg*
S5 TI tetraplegi* OR AB tetraplegi*
S4 TI quadriplegi* OR AB quadripleg*
S3 TI spastic* OR AB spastic*
S2 TI CP OR AB CP
S1 TI "cerebral palsy" OR AB "cerebral palsy"
British Nursing Index (ProQuest)
S33 S9 and S32
S32 TI,AB(positioning) OR TI,AB("sleep position*") OR TI,AB("sleep system*") OR TI,AB("sleep management*") OR TI,AB("sleep management") OR TI,AB("sleep* support*") OR TI,AB("postural support*") OR TI,AB("postural position*") OR TI,AB("postural management") OR TI,AB("postural system*") OR TI,AB("night time support") OR TI,AB("night time position*") OR TI,AB("lying support*") OR TI,AB("lying position*") OR TI,AB("supine position*") OR TI,AB(chailey) OR TI,AB(dreama) OR TI,AB(sleepform) OR TI,AB(moonlight) OR TI,AB(symmetrisleep) OR TI,AB(snoooo*) OR TI,AB("simple stuff works")
S31 TI,AB("simple stuff works")
S30 TI,AB(snoooo*)
S29 TI,AB(symmetrisleep)
S28 TI,AB(moonlight)
S27 TI,AB(sleepform)
S26 TI,AB(drama)
S25 TI,AB(chailey)
S24 TI,AB("supine position*")
S23 TI,AB("lying position*")
S22 TI,AB("lying support*")
S21 TI,AB("night time position*")
S20 TI,AB("night time support")
S19 TI,AB("postural system*")
S18 TI,AB("postural management")
S17 TI,AB("postural position*")
S16 TI,AB("postural support*")
S15 TI,AB("sleep* support*")
S14 TI,AB("sleep management")
S13 TI,AB("sleep management*")
S12 TI,AB("sleep system*")
S11 TI,AB("sleep position*")
S10 TI,AB(positioning)
S9 TI,AB("cerebral palsy") OR TI,AB(CP) OR TI,AB(spastic*) OR TI,AB(quadriplegi*) OR TI,AB(tetraplegi*) OR TI,AB(diplegi*) OR TI,AB(disabled NEAR/7 child*) OR TI,AB(handicap* NEAR/3 child*)
S8 TI,AB(handicap* NEAR/3 child*)
S7 TI,AB(disabled NEAR/7 child*)
S6 TI,AB(diplegi*)
S5 TI,AB(tetraplegi*)
S4 TI,AB(quadriplegi*)
S3 TI,AB(spastic*)
S2 TI,AB(CP)
S1 TI,AB("cerebral palsy")
Health Management Information System (Ovid)
1 Cerebral Palsy/
2 cerebral palsy.ti,ab.
3 CP.ti,ab.
4 spastic*.ti,ab.
5 quadriplegi*.ti,ab.
6 Quadriplegia/
7 tetraplegi*.ti,ab.
8 diplegi*.ti,ab.
9 disabled children/
10 (disab* adj7 child*).ti,ab.
11 (handicap* adj3 child*).ti,ab.
12 or/1‐11
13 positioning.ti,ab.
14 sleep* position*.ti,ab.
15 sleep system*.ti,ab.
16 sleep management.ti,ab.
17 sleep* support*.ti,ab.
18 postural support*.ti,ab.
19 postural position*.ti,ab.
20 postural management.ti,ab.
21 postural system*.ti,ab.
22 night time support*.ti,ab.
23 night time position*.ti,ab.
24 lying support*.ti,ab.
25 lying position*.ti,ab.
26 supine position*.ti,ab.
27 chailey.ti,ab.
28 dreama.ti,ab.
29 sleepform.ti,ab.
30 moonlight.ti,ab.
31 moonlite.ti,ab.
32 symmetrisleep.ti,ab.
33 snoooo*.ti,ab.
34 simple stuff works.ti,ab.
35 or/13‐34
36 12 and 35
Conference Proceedings Citation Index ‐ Science; and Conference Proceedings Citation Index ‐ Social Sciences and Humanities (Web of Science)
# 32 #31 AND #9
# 31 #30 OR #29 OR #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10
# 30 TS=("simple stuff works")
# 29 TS=(snoooo*)
# 28 TS=(symmetrisleep)
# 27 TS=(moonlight or moonlite)
# 26 TS=(sleepform)
# 25 TS=(dreama)
# 24 TS=(chailey)
# 23 TS=("supine position*")
# 22 TS=("lying position*")
# 21 TS=("lying support*")
# 20 TS=("night time position*")
# 19 TS=("night time support*")
# 18 TS=("postural system*")
# 17 TS=("postural management")
# 16 TS=("postural position")
# 15 TS=("postural support")
# 14 TS=("sleep* support")
# 13 TS=("sleep* management")
# 12 TS=("sleep* system*")
# 11 TS=("sleep* position*")
# 10 TS=(positioning)
# 9 #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1
# 8 TS=(handicap* Near/3 child*)
# 7 TS=(disabled Near/7 child*)
# 6 TS=("disabled children")
# 5 TS=((quadriplegi* or tetraplegi* or diplegi*))
# 4 TS=(spastic*)
# 3 TS=(CP.ti,ab)
# 2 TS=(cerebral palsy)
# 1 TS=(cerebral palsy)
PEDro (Physiotherapy Evidence Database)
Cerebral palsy AND sleep*
OTSeeker (Occupational Therapy Systematic Evaluation of Evidence)
Cerebral palsy AND sleep*
Clinical trials
Cerebral palsy AND sleep
World Health Organisation (WHO) International Clinical Trials Registry Platform (ICTRP)
Cerebral palsy AND sleep
WorldCat
kw:cerebral palsy kw:sleep
Appendix 2. Additional methods table
| Measures of treatment effect | Where continuous data are presented but measured in different ways across studies (e.g. physical functioning scores), we plan to calculate standardised mean differences (SMD) with 95% confidence intervals (CIs). We plan to use the same techniques where outcomes are ordinal. We plan to use the relative risk (RR) with 95% CIs as the measures of effect for each dichotomous outcome. If there is only one study for a particular outcome, or if the outcome is measured in the same way across studies, we plan to use the mean difference (MD) with 95% confidence intervals. |
| Unit of analysis issues | We anticipate that future studies could use a cross‐over design. If so, we will attempt to obtain standard errors based on paired data. If this information is not provided we will attempt to infer it (see 'Dealing with missing data' section). If we cannot obtain data for a paired analysis, we will treat the cross‐over trial as a parallel group trial with information from the first period only. |
| Dealing with missing data | We will approach the authors directly for information:
If it is not possible to obtain the data from the original investigators, we will analyse the available data separately, and explore the potential impact of missing data on the findings of the review in the 'Discussion' section. We will collect the proportions of participants for whom no outcome data are obtained and report this in the 'Risk of bias' assessment. If cross‐over designs are reported in studies without information on the standard error of within‐individual differences, we will attempt to obtain it using one of the following (in priority order):
|
| Assessment of heterogeneity | Where there are sufficient data, we will calculate a summary statistic for each outcome using both fixed‐effect and random‐effects models. We will combine outcomes only if it is sensible to do so, and we will interpret results cautiously. We will consider methodological heterogeneity (differences in study design) and clinical heterogeneity (differences in participants, interventions or outcome measures). We will assess heterogeneity by examining the scatter in the data points and the overlap of the confidence intervals, as well as by performing Chi². Any result with a P value greater than 0.05 will be considered to be heterogeneous. We will cautiously explore reasons for heterogeneity and, data permitting, assess it further with subgroup analysis or meta‐regression. |
| Assessment of reporting bias | Publication and other reporting bias We will examine included studies to check for duplication of results (i.e. whether the same data have been analysed and presented more than once). In these cases, we will contact the authors and request further details and individual participant data. If sufficient data are available, we will produce a funnel plot from the outcome data and and explore the reasons for asymmetry such as poor methodological quality or heterogeneity. |
| Subgroup analysis and investigation of heterogeneity | If sufficient trials are available in the future, and statistical heterogeneity is evident, we will examine the following subgroups to explore clinical heterogeneity:
|
| Sensitivity analysis | If sufficient trials are available in the future, we will conduct sensitivity analyses by repeating the analysis with the following exclusions:
|
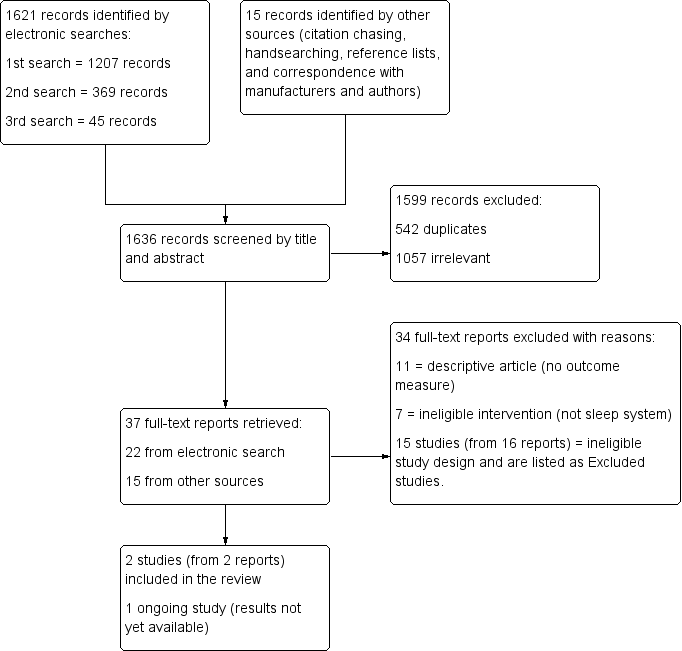
Study flow diagram

Risk of bias summary: Review authors' judgements about each risk of bias item for each included study.
| Sleeping in a sleep positioning system compared with not sleeping in a sleep positioning system for children with cerebral palsy | |||
| Population: Children with cerebral palsy Settings: United Kingdom (at home or in paediatric research laboratory) Intervention: Sleeping in sleep positioning system Comparison: Not sleeping in sleep positioning system | |||
| Outcomes | Impact | Number of participants | Quality of the evidence |
| Reduce hip migration/hip problems | No RCTs measured effect of sleep positioning systems on hip migration/hip problems | ‐ | ‐ |
| Effect on sleep patterns and quality | Limited data. A small number of established users of sleep positioning systems showed no significant difference in sleep quality indicators | 21 | ⊕⊝⊝⊝ |
| Effect on quality of life of child and family | No RCTs measured effect of sleep positioning systems on child and family quality of life | ‐ | ‐ |
| Effect on pain | Limited data. A small number of established users of sleep positioning systems showed no significant difference in levels of pain | 10 (1 study) | ⊕⊝⊝⊝ |
| Effect on physical functioning | No RCTs measured effect of sleep positioning systems on physical functioning | ‐ | ‐ |
| Adverse effects | No RCTs measured harms or reported adverse events | ‐ | ‐ |
| GRADE Working Group grades of evidence | |||
| GRADE: Grades of Recommendation, Assessment, Development and Evaluation. | |||
| Outcome | Variable | Definition | Study ID | Number of participants | Sleeping in sleep positioning system Mean (SD) | Sleeping out of sleep positioning system Mean (SD) | Mean difference (95% CI) | Paired t‐test | |
| t value | P value | ||||||||
| Sleep patterns/sleep quality | Sleep latency | Time (in minutes) to fall asleep | 9* | 69.1† (52.6) | 32.9 (26.0) | 36.2 (‐1.12 to 73.45) | 2.24 | 0.06 | |
| 8£ | 64.1 (54.0) | 37.0 (24.5) | 27.1 (‐8.76 to 62.89) | 1.79 | 0.12 | ||||
| 9 | 68.8 (49.8) | 80.1 (48.1) | ‐11.3 (‐30.70 to 8.03) | ‐1.35 | 0.21 | ||||
| Sleep efficiency | % of time in bed actually asleep | 9 | 80.7 (15.4) | 83.1 (12.0) | ‐2.4 (‐11.77 to 7.04) | ‐0.58 | 0.58 | ||
| 10 | 76.2 (8.3) | 73.8 (11.1) | 2.4 (‐2.98 to 7.73) | 1.00 | 0.34 | ||||
| Pain | Pain | Paediatric Pain Profile (PPP) scale (parent‐reported scores) | 10 | 11.3 (12.1) | 13.0 (14.6) | ‐1.7 (‐4.88 to 0.15) | ‐1.68 | 0.13 | |
| CI: Confidence intervals; ID: Identifier; SD: Standard Deviation | |||||||||
| * Includes one participant who fell asleep before recording started (recorded as zero), as reported by Hill 2009. | |||||||||
| Study | Variable of sleep quality | Number of participants | Sleeping in sleep positioning systems Mean (SD) | Sleeping out of sleep positioning system Mean (SD) | Sleeping in sleep positioning system Median (IQR) | Sleeping out of sleep positioning system Median (IQR) |
| Total sleep time (in minutes)¹ | 10 | 517.1 (54.4) | 509.1 (72.5) | 511.5 (52.5) | 527.5 (117.5) | |
| Total sleep time (in minutes) | 9 | 349.9 (101.1) | 427.7 (55.0) | 412.5 (143.5)* | 421.0 (89.0)* | |
| Total sleep time that was S1^ (%) | 9 | 2.4 (2.2) | 3.2 (2.4) | 1.7 (1.1)* | 3.6 (3.5)* | |
| Total sleep time that was S4^ (%) | 9 | 33.3 (10.6) | 29.0 (10.6) | 29.2 (11.3) | 28.0 (7.5) | |
| Total sleep time that was S3^ (%) | 9 | 6.4 (1.7) | 6.2 (2.4) | 6.3 (2.2) | 5.5 (3.8) | |
| Total sleep time that was S2^ (%) | 9 | 46.4 (10.0) | 50.5 (11.0) | 48.7 (11.3) | 49.7 (10.8) | |
| REM onset latency (in minutes) | 9 | 159.0 (99.4) | 204.3 (122.4) | 190.0 (18.0) | 187.0 (65.0) | |
| Number of REM cycles | 9 | 3.3 (0.9) | 2.9 (1.1) | 4.0 (1.0)* | 2.0 (2.0) | |
| Total sleep time that was REM^ (%) | 9 | 11.5 (5.1) | 11.0 (4.6) | 10.7 (1.4) | 11.1 (3.9) | |
| Total arousal index | 9 | 11.5 (6.5) | 11.4 (5.0) | 8.5 (6.0)* | 10.8 (8.2)* | |
| Central Apnoea Index (CAI) | 9 | 3.0 (8.0) | 4.0 (9.9) | 0.4 (0.4)* | 0.6 (0.9)* | |
| Respiratory Arousal Index (RAI) | 9 | 2.2 (3.7) | 1.5 (2.5) | 1.4 (1.9)* | 0.6 (1.4)* | |
| Apnoea ‐ Hypopnoea Index (AHI) | 9 | 1.9 (1.8) | 0.9 (1.2) | 2.6 (3.0) | 0.4 (1.5)* | |
| Obstructive Apnoea Index (OAI) | 9 | 0.5 (0.6) | 0.4 (0.9) | 0.3 (0.8)* | 0.1 (0.3)* | |
| % total sleep time with SpO₂ > 95% | 9 | 80.5 (29.0) | 77.2 (28.1) | 98.0 (19.9)* | 87.8 (12.6)* | |
| Average (mean) SpO₂ over total time | 9 | 95.7 (0.9) | 96.2 (1.9) | 95.0 (1.0)* | 97.0 (2.0)* | |
| Minimum SpO₂ (Nidus value) | 9 | 92.7 (1.7) | 90.6 (3.0) | 92.0 (1.0)* | 91.0 (3.0)* | |
| IQR: Interquartile range; REM: Rapid eye movement; SD: Standard deviation; SpO₂: Peripheral capillary oxygen saturation | ||||||
| ¹ Originally reported in hours and minutes, here given as minutes to be comparable. ^S1, S2, S3, S4 refer to the different stages of sleep; stages one to four. All values in this table are calculated from data supplied by study authors. For results from Hill 2009, some discrepancies were found between our calculations and the original publication. These are highlighted with an asterisk (*). | ||||||

