Intervenciones para optimizar la prescripción para personas de edad avanzada en residencias geriátricas
Información
- DOI:
- https://doi.org/10.1002/14651858.CD009095.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 12 febrero 2016see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Práctica y organización sanitaria efectivas
- Copyright:
-
- Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
David Alldred conceived and co‐ordinated the review and is the guarantor of the review. David Alldred prepared the original protocol with support and advice from Carmel Hughes, Nick Barber, David Raynor, Pat Spoor and Tim Chen. Paul Miller adapted the original search strategy (previously developed by Ms Pat Spoor with input from David Alldred) and ran the searches. All authors were involved in the retrieval of papers. David Alldred and Mary‐Claire Kennedy screened the search results, assessed retrieved papers against the eligibility criteria, assessed risk of bias and extracted data from the papers. David Alldred was responsible for entering data into RevMan and drafting the review with input from all authors.
Sources of support
Internal sources
-
School of Healthcare, University of Leeds, UK.
Funding was provided for the services of Ms Pat Spoor to develop the original search strategy and run the searches.
External sources
-
No sources of support supplied
Declarations of interest
David Alldred is an author on a study that was included in this review (Zermansky 2006).David Alldred ‐ none other than as indicated above. Mary‐Claire Kennedy ‐ no declarations of interest. Carmel Hughes ‐ no declarations of interest. Timothy F Chen ‐ no declarations of interest. Paul Miller ‐ no declarations of interest.
Acknowledgements
We would like to thank Gerd Flodgren, Julia Worswick (Managing Editors EPOC Oxford, UK) and Pierre Durieux (EPOC Paris, France) for their assistance in updating the review.
We would like to acknowledge the previous authors of the review, Professor DK (Theo) Raynor, Professor Nick Barber and Ms Pat Spoor. We would also like to acknowledge the previous contributors to the review: Michelle Fiander (Trials Search Coordinator, EPOC group) in refining the original search strategy with Pat Spoor and Sally Dalton (Faculty Team Librarian, University of Leeds) for helping to run the original searches, as well as the helpful comments of peer reviewers on the protocol, Luciana Ballini, Kirby Lee, Aaron Tejani, Craig Ramsay, and the support of Lisa Bero. We would like to thank the members of the EPOC group in Canada and the UK for their help and advice. We would also like to acknowledge Mrs Julie Sowter (School of Healthcare, University of Leeds) and Noortje Arts (Institute for Linguistics, University of Utrecht) for translating the Strikwerda paper from Dutch to English and Ms Rachel Payne (School of Healthcare, University of Leeds) for secretarial support.
Version history
| Published | Title | Stage | Authors | Version |
| 2016 Feb 12 | Interventions to optimise prescribing for older people in care homes | Review | David P Alldred, Mary‐Claire Kennedy, Carmel Hughes, Timothy F Chen, Paul Miller | |
| 2013 Feb 28 | Interventions to optimise prescribing for older people in care homes | Review | David P Alldred, David K Raynor, Carmel Hughes, Nick Barber, Timothy F Chen, Pat Spoor | |
| 2011 Apr 13 | Interventions to optimise prescribing for older people in care homes | Protocol | David P Alldred, D K (Theo) Raynor, Carmel Hughes, Nick Barber, Timothy F Chen, Pat Spoor | |
Differences between protocol and review
We intended to pool results and conduct meta‐analyses if studies were homogeneous. However, as studies were heterogeneous, this was not undertaken. Following identification of unit of analysis errors, we intended to attempt to reanalyse the data and report the intra‐cluster correlation coefficient and adjust for clustering if possible. However, instead, we commented on unit of analysis errors where appropriate within the results and discussion. Similarly, subgroup analyses were not possible. We used a revised search strategy for the update (see Search methods for identification of studies). New authors for this review were Mary‐Claire Kennedy and Paul Miller. Previous authors were Professor DK (Theo) Raynor, Professor Nick Barber and Ms Pat Spoor.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Aged; Humans;
PICO

Study flow diagram.
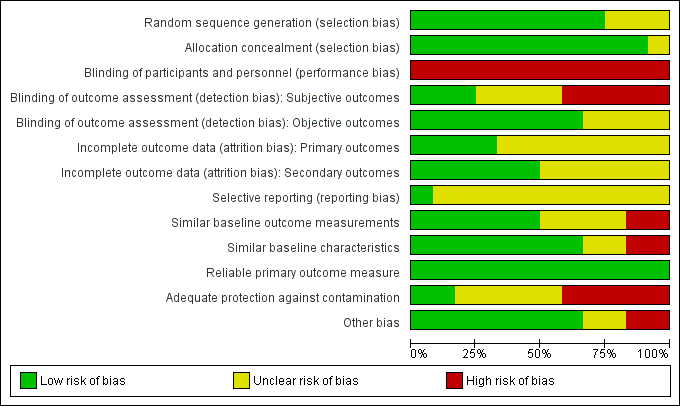
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Interventions to optimise prescribing compared with usual GP care for care home residents | |||
| Patient or population: older people (aged 65 years or older) living in care homes Settings: Institutionalised care facilities in Australia, Finland, Israel, Netherlands, New Zealand, Spain, Sweden, United Kingdom, and USA and Canada Intervention: Intervention to optimise prescribing (single or multicomponent intervention) Comparison: Usual care by general practitioner | |||
| Outcomes | Impact | No of Participants | Quality of the evidence |
| Adverse drug events | There was no evidence of an effect on adverse drug events | 1228 in 87 care homes (2 studies) | ⊕⊕⊝⊝ |
| Hospital admissions | It is uncertain whether medication review reduces hospital admissions | 7606 in 309 care homes (8 studies) | ⊕⊕⊝⊝ |
| Mortality | There was no evidence of an effect on mortality | 6805 in 188 care homes (6 studies) | ⊕⊕⊝⊝ |
| Quality of life | It is uncertain whether medication review improves quality of life | 586 in 21 care homes (2 studies) | ⊕⊕⊝⊝ |
| Medication‐related problems | Medication review may lead to the identification and resolution of medication‐related problems | 6640 in 251 care homes (7 studies) | ⊕⊕⊝⊝ |
| Medication appropriateness | Medication review may lead to an improvement in medication appropriateness | 1566 in 152 care homes (5 studies) | ⊕⊕⊝⊝ |
| Medicine costs | It is uncertain whether medication review decreases medication costs | 4734 in 142 care homes (5 studies) | ⊕⊝⊝⊝ |
| GRADE Working Group grades of evidence | |||
| Quality assessment of evidence for each outcome was based on study design, risk of bias, inconsistency, indirectness and imprecision. The evidence was downgraded from high to low for adverse drug events (Crotty 2004b; Gurwitz 2008) due to a serious risk of bias and imprecision. The evidence was downgraded from high to low for hospital admissions (Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014; Connolly 2015), mortality (Furniss 2000; Roberts 2001; Zermansky 2006; Frankenthal 2014; Pitkala 2014; Connolly 2015), quality of life (Frankenthal 2014; Pitkala 2014) and medication appropriateness (Crotty 2004a; Crotty 2004b; Frankenthal 2014; Garcia‐Gollarte 2014; Pitkala 2014) due to a serious risk of bias and inconsistency. The evidence for medicines costs (Furniss 2000; Roberts 2001; Crotty 2004a; Zermansky 2006; Frankenthal 2014 was downgraded from high to very low due to a serious risk of bias, inconsistency and imprecision. The evidence for medicine‐related problems (Strikwerda 1994; Claesson 1998; Furniss 2000; Roberts 2001; Crotty 2004b; Zermansky 2006; Frankenthal 2014 was reduced from high to low due to design, risk of bias and imprecision. | |||
| Study,Country, Design | Participants | Intervention | Outcome measures | Duration |
| Sweden Cluster‐RCT | 1854 residents in 33 nursing homes | Multidisciplinary meetings with physician, pharmacist and nurse(s) | Medication‐related problems | 14 months |
| Australia Cluster‐RCT | 1998 residents in 36 nursing homes | Multidisciplinary meetings with study geriatrician, a GP, a pharmacist and a nurse manager. Education of nurses and care‐givers | Hospital admissions Mortality | 14 months |
| Australia Cluster‐RCT | 154 residents in 10 nursing homes | Multidisciplinary case conferencing with GP, a geriatrician, a pharmacist, residential care staff and an Alzheimer's Association representative | Medication Appropriateness Index | 3 months |
| Australia Patient‐RCT | 110 patients discharged to 85 long‐term care facilities | Pharmacist transition co‐ordinator. Transfer of medicines information to nursing staff, family physician and community pharmacist plus medication review and case conferencing | Adverse drug events Hospital admissions Medication‐related problems Medication Appropriateness Index | 8 weeks |
| Israel Patient‐RCT | 359 residents in 1 chronic care geriatric facility | Medication review by the study pharmacist | Hospital admissions Mortality Quality of life Medication appropriateness (STOPP‐START) Medication‐related problems Medicine costs | 12 months |
| UK Cluster‐RCT | 330 residents in 14 nursing homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 8 months |
| Spain Cluster‐RCT | 716 residents in 36 nursing homes | Physician educational programme followed by on‐demand support (prescription advice) by phone | Hospital admissions (total number of days spent in hospital) Medication appropriateness (STOPP‐START) | 6 months |
| USA/Canada Cluster‐RCT | 1118 residents in 29 units in 2 long‐term care facilities | Computerised provider order entry with clinical decision support | Adverse drug events | 12 months |
| Finland Cluster‐RCT | 227 residents in 20 assisted living facilities | Nurse training and education | Hospital admissions Mortality Health‐related Quality of Life Medication appropriateness (Beer's criteria plus others) | 12 months |
| Australia Cluster‐RCT | 3230 residents in 52 nursing homes | Introduction of new professional role, nurse education and medication review by pharmacists | Hospital admissions Mortality Medication‐related problems Medicine costs | 24 months |
| Netherlands Cluster‐RCT | 196 residents in 1 nursing home | Feedback on GP prescribing from community pharmacist | Medication‐related problems | 6 weeks |
| UK Patient‐RCT | 661 residents in 65 care homes | Medication review by a single pharmacist | Hospital admissions Mortality Medication‐related problems Medicine costs | 6 months |

