Analgesia para el parto con fórceps
Información
- DOI:
- https://doi.org/10.1002/14651858.CD008878.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 30 septiembre 2013see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Embarazo y parto
- Copyright:
-
- Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Emily Bain and Payam Nikpoor independently assessed trials for inclusion, extracted data and assessed the risk of bias for the included studies. Emily Bain wrote the first draft of the review, and Payam Nikpoor contributed to the subsequent drafts and the final version of the review.
Sources of support
Internal sources
-
ARCH, Robinson Institute, The University of Adelaide, Australia.
External sources
-
Australian Department of Health and Ageing, Australia.
-
National Health and Medical Research Council, Australia.
Declarations of interest
None known.
Acknowledgements
The review authors would like to acknowledge the expert guidance and support of Philippa Middleton and Caroline Crowther, Australian Research Centre for Health of Women and Babies, Robinson Institute, The University of Adelaide. The review authors would also like to thank Rae Watson‐Jones for her contribution in reviewing the literature and developing the protocol.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team) and the Group's Statistical Adviser.
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Pregnancy and Childbirth Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2013 Sep 30 | Analgesia for forceps delivery | Review | Payam Nikpoor, Emily Bain | |
| 2010 Dec 08 | Analgesia for forceps delivery | Protocol | Payam Nikpoor, Rae Watson‐Jones | |
Differences between protocol and review
We have reported data on the following outcomes in this review that were not anticipated and thus not pre‐specified in the protocol, but we believed that they were clinically relevant and important.
-
Good anaesthesia (as judged by the obstetrician considering the restlessness of the woman)
-
Maternal awareness or sensation of the operation
-
Comfortable/pleasant recovery
We have re‐ordered and re‐grouped the review's outcomes according to a number of subheadings for clarity and ease of reading (we have not changed the individual outcomes).
PICO

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
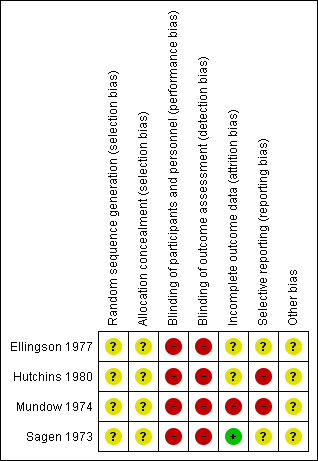
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
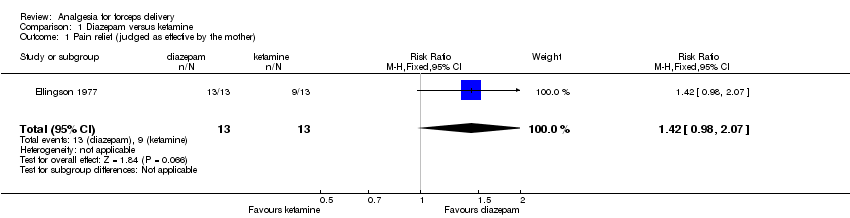
Comparison 1 Diazepam versus ketamine, Outcome 1 Pain relief (judged as effective by the mother).
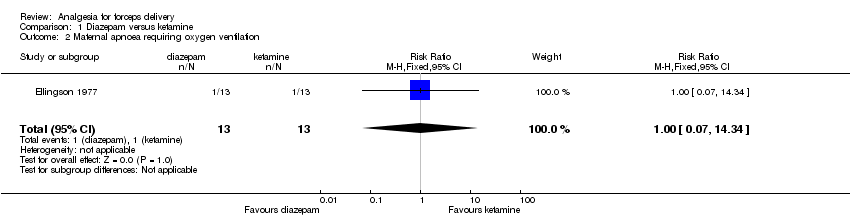
Comparison 1 Diazepam versus ketamine, Outcome 2 Maternal apnoea requiring oxygen ventilation.

Comparison 1 Diazepam versus ketamine, Outcome 3 Apgar score of less than seven at five minutes.
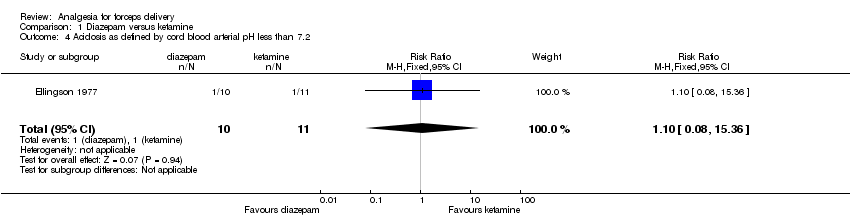
Comparison 1 Diazepam versus ketamine, Outcome 4 Acidosis as defined by cord blood arterial pH less than 7.2.

Comparison 1 Diazepam versus ketamine, Outcome 5 Good anaesthesia (judged by the obstetrician).

Comparison 1 Diazepam versus ketamine, Outcome 6 Pleasant recovery (judged by the mother).

Comparison 1 Diazepam versus ketamine, Outcome 7 Awareness (mother sensed the operation).
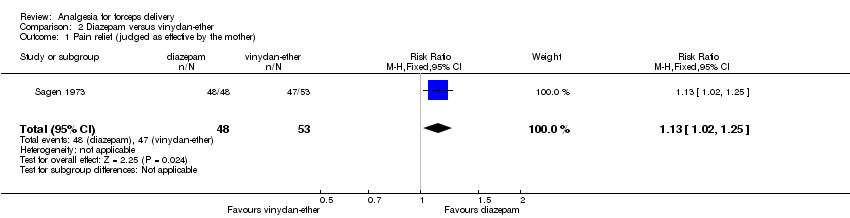
Comparison 2 Diazepam versus vinydan‐ether, Outcome 1 Pain relief (judged as effective by the mother).

Comparison 2 Diazepam versus vinydan‐ether, Outcome 2 Vomiting.

Comparison 2 Diazepam versus vinydan‐ether, Outcome 3 Apgar score of less than seven at five minutes.

Comparison 2 Diazepam versus vinydan‐ether, Outcome 4 Good anaesthesia (judged by the obstetrician).

Comparison 2 Diazepam versus vinydan‐ether, Outcome 5 Comfortable induction and recovery (judged by the mother).

Comparison 3 Diazepam versus other (general, local, other anaesthetic), Outcome 1 Apgar score of less than eight at two minutes.

Comparison 4 Spinal analgesia versus pudendal block anaesthesia, Outcome 1 Pain relief (analgesia achieved).

Comparison 4 Spinal analgesia versus pudendal block anaesthesia, Outcome 2 Severe pain during delivery.
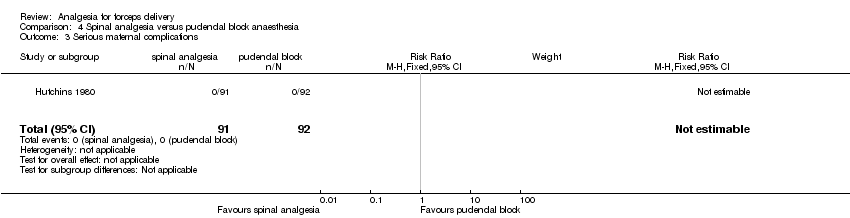
Comparison 4 Spinal analgesia versus pudendal block anaesthesia, Outcome 3 Serious maternal complications.

Comparison 4 Spinal analgesia versus pudendal block anaesthesia, Outcome 4 Request for additional anaesthesia.

Comparison 4 Spinal analgesia versus pudendal block anaesthesia, Outcome 5 Maternal hypotension (defined as a decrease in diastolic or systolic blood pressure of more than 10 mmHg).

Comparison 4 Spinal analgesia versus pudendal block anaesthesia, Outcome 6 Headache (mild or moderate).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain relief (judged as effective by the mother) Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.98, 2.07] |
| 2 Maternal apnoea requiring oxygen ventilation Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 14.34] |
| 3 Apgar score of less than seven at five minutes Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Acidosis as defined by cord blood arterial pH less than 7.2 Show forest plot | 1 | 21 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.1 [0.08, 15.36] |
| 5 Good anaesthesia (judged by the obstetrician) Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.41, 0.97] |
| 6 Pleasant recovery (judged by the mother) Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.08 [1.17, 3.68] |
| 7 Awareness (mother sensed the operation) Show forest plot | 1 | 26 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.01, 1.88] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain relief (judged as effective by the mother) Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [1.02, 1.25] |
| 2 Vomiting Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.04 [0.00, 0.62] |
| 3 Apgar score of less than seven at five minutes Show forest plot | 1 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.45, 3.50] |
| 4 Good anaesthesia (judged by the obstetrician) Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.56 [1.11, 2.21] |
| 5 Comfortable induction and recovery (judged by the mother) Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.45 [2.26, 5.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Apgar score of less than eight at two minutes Show forest plot | 1 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.1 [0.51, 2.38] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain relief (analgesia achieved) Show forest plot | 1 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.36 [2.46, 4.60] |
| 2 Severe pain during delivery Show forest plot | 1 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.02 [0.00, 0.27] |
| 3 Serious maternal complications Show forest plot | 1 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Request for additional anaesthesia Show forest plot | 1 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Maternal hypotension (defined as a decrease in diastolic or systolic blood pressure of more than 10 mmHg) Show forest plot | 1 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Headache (mild or moderate) Show forest plot | 1 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.53, 1.58] |

