نقش جراحیهای اسلینگ تکبرش در درمان بیاختیاری ادراری در زنان
چکیده
پیشینه
بیاختیاری ادراری (urinary incontinence) تا 50% از زنان را مبتلا کرده است. مطالعات در ایالات متحده آمریکا بیانگر آن است که 80% از این زنان، دارای نشانهای از بیاختیاری ادراری استرسی هستند. این موضوع، بار (burden) سلامتی و اقتصادی چشمگیری را بر جامعه و زنان مبتلا تحمیل میکند. کولپوساسپنشن (colposuspension) و اکنون اسلینگهای میدیورترال (mid‐urethral) در درمان بیماران مبتلا به بیاختیاری استرسی موثر هستند. با این حال حوادث جانبی همراه با آنها عبارتنداز: آسیب به مثانه و روده، درد کشاله ران و تشکیل هماتوم. این امر منجر به ایجاد اسلینگهای تکبرش نسل سوم شد که تحت عنوان مینی‐اسلینگها (mini‐slings) نیز نامیده میشوند.
لازم به ذکر است که TVT‐Secur (Gynecare, Bridgewater, NJ, USA)، یکی از انواع اسلینگ تکبرش است که به دلیل نتایج ضعیف، از بازار خارج شد. با این حال، این شیوه یکی از گستردهترین اسلینگهای تکبرش است که مورد بررسی قرار گرفته و در چند کارآزمایی وارد شده در این مرور نیز از آن استفاده شده بود. با وجود منع استفاده بالینی، تصمیم گرفته شد که دادههای مربوط به این اسلینگ در نخستین تکرار از این مرور گنجانده شود، به طوری که دادههای سطح a1 در این منابع علمی در دسترس هستند تا فقدان اثربخشی آن تایید شود.
اهداف
هدف این مرور، ارزیابی اثربخشی پروسیجرهای مینی‐اسلینگ در زنان مبتلا به بیاختیاری ادراری استرسی یورودینامیک (urodynamic) بالینی یا مخلوط، از نظر وضعیت توانایی نگه داشتن ادرار، کیفیت زندگی یا حوادث جانبی است.
روشهای جستوجو
ما این موارد را جستوجو کردیم: پایگاه ثبت تخصصی گروه بیاختیاری در کاکرین (شامل: CENTRAL؛ MEDLINE؛ MEDLINE in process) (جستوجو در 6 فوریه 2013)؛ ClinicalTrials.gov؛ WHO ICTRP (جستوجو در 20 سپتامبر 2012) و فهرست منابع.
معیارهای انتخاب
همه کارآزماییهای تصادفیسازی یا شبه‐تصادفیسازی و کنترل شده را در نظر گرفتیم، که در آنها زنان مبتلا به بیاختیاری استرسی یورودینامیک، یا زنان مبتلا به نشانههای بیاختیاری استرسی یا بیاختیاری ادراری مخلوط با غلبه استرس بررسی شده بودند و در حداقل یک بازوی کارآزمایی تحت درمان با اسلینگهای تکبرش جدید قرار گرفته بودند. تعریف اسلینگ تکبرش عبارت است از «اسلینگی که دربرگیرنده مسیر ترانس اوبتوراتور یا رتروپوبیک تروکار (Trocar) یا نوار نباشد و فقط شامل یک تکبرش واژینال باشد (یعنی بدون زخمهای خارجی در کشاله ران یا قسمت تحتانی شکم).»
گردآوری و تجزیهوتحلیل دادهها
سه نویسنده این مرور، کیفیت روششناسی کارآزماییهای بالقوه واجد شرایط را ارزیابی کرده و بهطور مستقل از هم دادهها را از هر کارآزمایی استخراج کردند.
نتایج اصلی
ما 31 کارآزمایی را شامل 3290 زن شناسایی کردیم. تعدادی نقص روششناسی در برخی کارآزماییها مشاهده شد، خلاصهای از آنها در بخش «خطر سوگیری (bias) در مطالعات وارد شده» آورده شده است.
هیچ مطالعهای اسلینگهای تکبرش را در برابر عدم درمان، درمان محافظهکارانه (conservative)، کولپوساسپنشن، پروسیجرهای لاپاروسکوپیک یا اسلینگهای سابیورترال (sub‐urethral) مرسوم مقایسه نکرده بود. هیچ دادهای درباره مقایسه اسلینگهای تکبرش با اسلینگهای میدیورترال رتروپوبیک (رویکرد بالا به پائین (top‐down)) موجود نبود؛ اما نویسندگان این مرور اعتقاد دارند این موضوع، مقایسه کلی را در برابر اسلینگهای میدیورترال رتروپوبیک تحت تاثیر قرار نمیدهد.
انواع اسلینگهای تکبرش در این مرور عبارتند از: TVT‐Secur (Gynecare)؛ MiniArc (American Medical Systems, Minnetonka, USA)؛ Ajust (CR Bard Inc., Covington, USA)؛ Needleless (Mayumana Healthcare, Lisse, The Netherlands)؛ Ophira (Promedon, Cordoba, Argentina)؛ Tissue Fixation (TFS PTY Ltd, Sydney, Australia) و CureMesh (DMed Co. Inc., Seoul, Korea).
زنان با احتمال بیشتری بعد از جراحی با اسلینگهای تکبرش نسبت به اسلینگهای رتروپوبیک مانند نوار واژینال بدون کشش (TVTTM) بیاختیار باقی مانده بودند (121/292؛ 41% در برابر 72/281؛ 26%؛ خطر نسبی (RR): 2.08؛ 95% فاصله اطمینان (CI): 1.04 تا 4.14). مدت زمان جراحی برای اسلینگهای تکبرش، اندکی کوتاهتر بود، اما احتمال de novo urgency بالاتر بود (RR: 2.39؛ 95% CI؛ 1.25 تا 4.56). چهار مورد از پنج مطالعه در این مقایسه، شامل TVT‐Secur به عنوان اسلینگ تکبرش بودند.
اسلینگهای تکبرش باعث نرخ بیاختیاری ادراری بیشتری در قیاس با اسلینگهای ترانس اوبتوراتور شده بود (30% در برابر 11%؛ RR: 2.55؛ 95% CI؛ 1.93 تا 3.36). پروفایل حوادث جانبی به طور چشمگیری بدتر بود، به ویژه در زمینه خطرات بیشتر مواجهه با مش (mesh) واژینال (RR: 3.75؛ 95% CI؛ 1.42 تا 9.86)، اروزیون مثانه/مجرا (RR: 17.79؛ 95% CI؛ 1.06 تا 298.88) و خونریزی حین جراحی (تفاوت میانگین (MD): 3.70؛ 95% CI؛ 18.79 تا 33.88). درد پس از جراحی شیوع کمتری با اسلینگهای تکبرش داشت (RR: 0.29؛ 95% CI؛ 0.20 تا 0.43) و نرخ درد و رنج بلندمدت به صورت نامحسوسی کمتر بود، اما اهمیت بالینی این تفاوتها جای تردید دارد. اغلب این یافتهها از کارآزماییهایی کسب شده بود که مشتمل بر TVT‐Secur بودند: مستثنا کردن کارآزماییهای دیگر نشان داد که خطر بالای بیاختیاری اساسا با استفاده از این وسیله مرتبط بوده است (RR: 2.65؛ 95% CI؛ 1.98 تا 3.54). TVT‐Secur از مصرف بالینی کنار گذاشته شده است.
شواهد برای آنکه نشان دهنده تفاوت در نرخ بیاختیاری با سایر اسلینگهای تکبرش در مقایسه با اسلینگهای ترانس اوبتوراتور Inside‐out یا Outside‐in باشند، ناکافی هستند. مدت زمان جراحی به طور نامحسوسی برای اسلینگهای تکبرش در قیاس با اسلینگهای ترانس اوبتوراتور کوتاهتر بود، اما فقط حدود دو دقیقه و همراه با ناهمگونی زیاد در این مقایسه. خطر درد کشاله ران/ران پس از جراحی و طولانیمدت، اندکی با اسلینگهای تکبرش کمتر بود، اما شواهد کلی برای نشان دادن یک تفاوت چشمگیر در حوادث جانبی اسلینگهای تکبرش در قیاس با اسلینگهای ترانس اوبتوراتور ناکافی بود. همچنین شواهد برای اجازه انجام یک تجزیهوتحلیل حساسیت معنادار از سایر اسلینگهای تکبرش در مقایسه با اسلینگهای ترانساوبتوراتور ناقص بود، زیرا همه فواصل اطمینان گسترده بود. تنها تفاوتهای عمده در نرخهای درد پس از جراحی و بلندمدت و مدت زمان جراحی بود که اندکی به نفع اسلینگهای تکبرش بود.
نتایج کلی نشان میدهد که TVT‐Secur بهطور قابل توجهی پائینتر از اسلینگهای رتروپوبیک و ترانساوبتوراتور Inside‐out قرار دارد، اما شواهد بیشتری برای پذیرفتن هرگونه مقایسه معقول اسلینگهای تکبرش در برابر اسلینگهای ترانس اوبتوراتور مورد نیاز است.
هنگامی که یک اسلینگ تکبرش با دیگری مقایسه شد، شواهد برای نشان دادن یک تفاوت معنادار میان هریک از اسلینگها در هرکدام از مقایسههای انجام شده ناکافی بود.
نتیجهگیریهای نویسندگان
TVT‐Secur نسبت به اسلینگهای میدیورترال استاندارد برای درمان زنان مبتلا به بیاختیاری استرسی، پائینتر قرار میگیرد و در حال حاضر از استفاده بالینی کنار گذاشته شده است. شواهد کافی درباره سایر اسلینگهای تکبرش در مقایسه با اسلینگهای رتروپوبیک یا ترانساوبتوراتور برای انجام مقایسههای قابل اعتماد وجود نداشت. یک تفسیر اقتصادی مختصر (brief economic commentary‐BEC) دو مطالعه را شناسایی کرد که هیچ تفاوتی را در پیامدهای بالینی بین اسلینگهای تکبرش و اسلینگهای میدیورترال ترانساوبتوراتور گزارش نکرده بود، اما اسلینگهای تکبرش ممکن است بر مینای پیگیری یکساله، هزینه‐اثربخشتر از اسلینگهای میدیورترال ترانس اوبتوراتور باشد. نیاز به کارآزماییهای بیشتری با قدرت کافی و کیفیت بالا با پیگیری طولانی‐مدت وجود دارد. کارآزماییها باید به وضوح مکانیسم تثبیت این اسلینگهای تکبرش را تشریح کنند: واضح است که اگرچه آنها به عنوان یک گروه مجزا گرد هم میآیند، یک تفاوت قابل ملاحظه در مکانیسمهای تثبیت میتواند پیامدها را تحت تاثیر قرار دهد.
PICO
خلاصه به زبان ساده
نقش جراحیهای اسلینگ تکبرش در درمان بیاختیاری ادراری در زنان
بیاختیاری ادراری استرسی (نشت ادرار به هنگام تمرین و ورزش، سرفه، عطسه یا خنده) یک بیماری شایع است که یک نفر از هر سه زن را در سراسر جهان مبتلا میکند. این بیماری معمولا نتیجه تضعیف حمایت عضلانی لوله هدایت کننده ادرار (حالب) است، یا به علت تضعیف عضله اسفنکتر (حلقوی) در قاعده مثانه رخ میدهد، چون این عضله توانایی نگهداری ادرار را حفظ میکند. این عارضه در زنانی که کودکشان از طریق زایمان واژینال متولد شدهاند و کسانی که دچار ضعف در عضلات کف لگن به دلایل دیگر هستند، شایعتر است. مقدار قابل توجهی از درآمد این زنان و خانواده آنها میتواند صرف مدیریت این نشانهها شود.
از گذشته انواع زیادی از جراحیها برای درمان زنان مبتلا به بیاختیاری ادراری استرسی انجام میشده است. روش استاندارد پذیرفته شده طی 10 سال اخیر، جراحی اسلینگ میدیورترال بوده که در آن یک نوار یا مش مصنوعی را به صورت مستقیم در پائین حالب قرار داده و در بخشهای مجاور کشاله ران یا دقیقا زیر استخوان پوبیس (Pubic) به بافتها محکم میکنند. نمونههای این اسلینگها که به صورت شایع استفاده میشوند، نوار واژینال بدون کشش (TVTTM) و نوار ترانس اوبتوراتور (transobturator tape; TOT) هستند. این جراحیها معمولا بسیار موفق بوده و نرخ موفقیت در آنها نزدیک به 80% یا 90% است. با این حال این جراحیها باعث عوارض جانبی چشمگیری میشوند که میتوانند آزار دهنده و گاهی خطرناک، مانند آسیب به مثانه ناشی از قرار دادن نوار، اروزیون نوار در حالب در حین دوره بهبود یا درد مزمن کشاله ران/ران (thigh/groin) باشند.
در تلاش برای حفظ اثربخشی در عین حذف برخی از عوارض جانبی، نسل جدیدی از اسلینگها ایجاد شد که «اسلینگهای تکبرش» یا «مینی‐اسلینگها (mini‐slings)» نام داشتند؛ این اسلینگها، موضوع این مرور هستند. آنها طراحی شده بودند تا نسبت به اسلینگهای میدیورترال استاندارد، کوتاهتر (در طول) باشند و با عمق کمتری از اسلینگهای استاندارد در بافتها نفوذ کنند. بنابراین تصور می شد که در عین حال که تاثیر کمتری ندارند، عوارض جانبی کمتری ایجاد میکنند. مثالهایی از اسلینگهای تکبرش عبارتند از TVT‐Secur؛ MiniArc؛ Ajust و اسلینگهای بدون سوزن.
ما به دنبال تمام کارآزماییهایی بودیم که شرکتکنندگان را به صورت تصادفی به اسلینگهای تکبرش در برابر هرگونه درمان دیگر برای بیاختیاری استرسی در زنان، به ویژه مقایسه با اسلینگهای میدیورترال اختصاص داده باشند. در مجموع 31 کارآزمایی را شامل 3290 زن شناسایی کردیم که همگی آنها نوعی از اسلینگهای تکبرش را در برابر یکی از انواع اسلینگهای میدیورترال یا گونههای مختلفی را از اسلینگهای تکبرش در برابر یکدیگر مقایسه کرده بودند. کیفیت کلی این کارآزماییها، متوسط بود.
ما دریافتیم که تفاوتهای مبهم در شیوهای که هر مینی‐اسلینگ عمل میکند، گاهی موجب دشواری مقایسه کردن میشود. TVT‐Secur نوع خاصی از مینی‐اسلینگ است که به طور همسو و سازگار نشان داده شده که در قیاس با اسلینگهای میدیورترال استاندارد، کنترل ضعیفتری بر بیاختیاری دارد و نرخ عوارض جانبی آن نیز بیشتر است. اکنون این وسیله از مصرف بالینی کنار گذاشته شده است.
از لحاظ هزینه، یک مرور غیر‐سیستماتیک از مطالعات اقتصادی حاکی از آن بود که اسلینگهای تکبرش، ارزانتر از اسلینگهای میدیورترال هستند. با وجود این، هیچ شواهد روشنی درباره تفاوتها در هزینهها و تاثیرات ارائه نشده بود.
از آنجایی که اکثر کارآزماییهایی که در حال حاضر برای ورود به این مرور در دسترس هستند، TVT‐Secur را ارزیابی کردهاند، کارآزماییهایی که دیگر اسلینگهای تکبرش را با اسلینگهای میدیورترال مقایسه کرده باشند، برای انجام مقایسههای معنادار بسیار کم هستند. بعضی شواهد نشان میدهند که اسلینگهای تکبرش سریعتر انجام میشوند و ممکن است باعث درد پس از جراحی کمتری شوند، اما برای ارزیابی مناسب اینکه سایر انواع مینی‐اسلینگها در حقیقت به اندازه اسلینگهای میدیورترال استاندارد یا بیشتر از آنها ایمن هستند یا خیر، نیاز به کارآزماییهایی بیشتری وجود دارد.
Authors' conclusions
Background
Urinary incontinence (UI) is an extremely common yet under‐reported, under‐diagnosed, under‐treated and potentially manageable condition that is prevalent throughout the world. It can cause a great deal of distress and embarrassment to individuals, as well as significant financial costs to those individuals and to societies. Estimates of prevalence vary from 10% to 40% depending on the definition and type of incontinence studied, with annual incidence ranging from 2% to 11% (Hunskaar 2002; Milsom 2009). Studies in the USA have shown that up to 80% of women with incontinence have an element of stress urinary incontinence (Hampel 1997). At the turn of the century, Turner estimated that the total annual cost to the United Kingdom National Health Service of treating clinically significant urinary incontinence was GBP 233 million (1999/2000 GDP), with the cost to individuals estimated at an additional GBP 178 million (Turner 2004). In the USA the annual direct costs of urinary incontinence in both men and women is over USD 16 billion (1995 USD) (Chong 2011), with a societal cost of USD 26.2 billion (1995 USD) (Wagner 1998). Approximately USD 13.12 billion (1995 USD) of the total direct costs of urinary incontinence are spent on SUI (Chong 2011; Kunkle 2015). About 70% of this USD 13.12 billion is borne by the patients, mainly through routine care (purchasing pads and disposable underwear (diapers), laundry and dry cleaning). This constitute a significant individual financial burden. Of the remaining 30%, 14% is spent on nursing home admissions, 9% on treatment, 6% on addressing complications and 1% on diagnosis (Chong 2011). Subak 2008 reported that about 1% of the median annual household income (USD 50,000 to USD 59,999) was spent by women on incontinence management. This study estimated that women spent an annual mean cost of USD 751 to USD 1277(2006 USD) on incontinence. This cost increases based on the severity of the symptoms (Subak 2008).The indirect cost associated exerts social and psychological burdens which are unquantifiable. (Chong 2011; Kilonzo 2004). Nevertheless, Birnbaum 2004 estimated that the annual average direct medical costs of SUI for one year (1998 USD) was USD 5642, and USD 4208 for indirect workplace costs.The cost of management and treatment of SUI appears to have increased over time, due to increasing prevalence and increased desire for improved quality of life. This in turn has resulted from improved recognition of the condition, as well as increased use of surgical and non‐surgical managements.
The surgical approach to stress urinary incontinence has progressed rapidly over the past one and a half decades. In the mid‐1990s, a prospective randomised study confirmed the superiority of the colposuspension over the Kelly plication and modified Pereyra needle suspension techniques, with five‐year cure rates in excess of 80% (Bergman 1995). This established the colposuspension as the standard approach to stress incontinence surgery. A colposuspension, however, entails major surgery with substantial operating time and lengthy hospital stay, as well as significant potential for morbidity (Lapitan 2012). The pubovaginal sling, which employs a fascial strip for support, is an effective alternative to the colposuspension, with similar efficacy (Rehman 2011). The incidence of severe adverse events following these procedures is high, for example, 10% after colposuspension (Lapitan 2012) and 13% after pubovaginal slings (Bezerra 2005).
Description of the condition
Classically, UI is subdivided into three main types.
-
Stress urinary incontinence (SUI) is characterised by leakage that occurs mainly during 'stress,' which can be brought about by coughing, sneezing, exercise or any manoeuvre that increases intra‐abdominal pressure. SUI is generally due to an anatomical/mechanical abnormality or weakness in the urethra/sphincter/pelvic floor support, and it is commonly treated with an anatomical/mechanical solution (i.e. surgery).
-
Urgency urinary incontinence (UUI) is characterised by leakage associated with a sense of urgency (defined as a sudden compelling desire to pass urine that cannot be postponed for fear of leakage). UUI is thought to be caused by involuntary detrusor contractions, which may be neurogenic or idiopathic, and it is treated with medication (most commonly anti‐muscarinic drugs), intra‐vesical botulinum toxin injections or, in extreme cases, surgery.
-
Mixed urinary incontinence (MUI) is a combination of stress and urgency incontinence.
Surgical management of SUI or stress‐predominant MUI is most commonly achieved these days by using a mid‐urethral support in the form of a tape or mesh. A great deal of research continues to be conducted to find the best balance of efficacy and minimal adverse events in choosing the right kind of tape.
Women with SUI or stress‐predominant MUI, diagnosed clinically or on urodynamics, have been included in this review.
Description of the intervention
In 1993 Ulmsten and Petros proposed the integral theory, a new concept in the maintenance of female urinary continence (Petros 1993). This is considered to be one of the drivers for the development of “tension‐free vaginal tape” (TVT), which was the first effective minimally invasive procedure for stress incontinence in women (Ulmsten 1998). The five‐year efficacy of TVT has been shown to be comparable with that of the Burch colposuspension, with the added benefits of shorter operating time and decreased hospital stay (Ward 2008).
The major disadvantage of the TVT procedure is that it involves the “blind” passage of a retropubic needle, which poses a significant risk for bladder, bowel and major vessel damage. The incidence of bladder injury is approximately 6% (Ogah 2009). This led to the development of the next generation of sub‐urethral sling procedures with the launch of transobturator tape (TOT) (Delorme 2001). Objective and subjective cure rates for both types of mid‐urethral tape have been shown to be equivalent (Nambiar 2012), but the transobturator passage resulted in fewer injuries to the bladder and other organs. A recent Cochrane review (Ogah 2009) describes lower complication rates with TOT, including less bladder perforation and shorter operating time. The transobturator approach is not without complications, and it has been shown to be associated with significant risk of groin and hip pain following surgery. A meta‐analysis (Latthe 2007) reported an incidence of 12% for groin and hip pain following an obturator‐type sling compared with only 1% for the retropubic approach.
The significant risk of visceral injury associated with the retropubic tape and the high incidence of groin pain following the transobturator route have led to the development of a new generation of stress incontinence devices. Popularly known as the “mini‐slings” (Moore 2009), these third‐generation devices differ from previous sling procedures in that a single incision is made within the vagina with no tape exit incisions. They have also been called single‐incision slings (Molden 2008). The tape used in these devices is significantly shorter (eight to 14 cm) in length than first‐ and second‐generation slings. The insertion pass stops short of the obturator membrane or pelvic floor. This less invasive approach is thought to reduce complications, including bladder/bowel and vascular injury and groin and thigh pain, with a shorter hospital stay and less postoperative pain. Interest is gradually increasing regarding the efficacy and safety of the mini‐slings, but at present, clinical data on these procedures are lacking.
How the intervention might work
Single‐incision slings have been developed that are based on the same mechanistic principles as minimally invasive slings, that is, to restore or enhance the woman's urethral support during a sudden rise in intra‐abdominal pressure, such as during a cough or sneeze, thus preventing involuntary loss of urine. At the same time, they aim to minimise the risk of major side effects associated with minimally invasive slings, such as bladder/vaginal/urethral/vascular perforations or erosions and chronic pain. To try to achieve this, these slings have shorter tape lengths and different fixation systems compared with minimally invasive slings. The main difference in these fixation systems is that they do not penetrate the obturator fossa (hence potentially minimising the risk of groin pain) or the retropubic space (minimising the risk of major vessel or visceral injury).
Currently six minimally invasive sling devices are available, including TVT Secur, MiniArc, Ajust, Needleless, Tissue Fixation System and Ophira. Differences between the various devices include the following.
-
The TVT‐Secur is inserted with a metal introducer that anchors the device in the obturator membrane. It is placed snugly against the urethra.
-
The MiniArc has a curved introducer that clips into two plastic anchoring hooks on the ends of the sling; this is used to insert the sling and secure it into the obturator membrane.
-
The Ajust also has a curved introducer with plastic anchoring hooks, but it differs from the other devices in that it has a pulley‐like system that allows adjustment following insertion.
-
The Needleless device is 60% longer than the other mini‐slings. It has a pocket‐like fold on each end, and an artery forceps is placed onto the end of the sling in this pouch. The sling is pushed laterally and through the obturator membrane at insertion.
-
The Ophira mini‐sling is a type 1 polypropylene monofilament mesh with two fixation arms that penetrate the obturator internus muscle on either side with the help of a retractile insertion guide.
-
The TFS consists of non‐stretch multi‐filament polypropylene tape with two polypropylene soft tissue anchors at either end. The tape is passed in the same direction as standard TVT, but the anchors are embedded into the pubourethral ligament inferior to the pubic symphysis.
-
CureMesh is a 14‐cm polypropylene mesh similar to the MiniArc sling but manufactured domestically in South Korea.
Why it is important to do this review
Various observational trials have reported cure rates of 77% (Debodinance 2008) and 81% (Meschia 2009) for the TVT‐Secur and 77% for the MiniArc (Gauruder‐Burmester 2009). Preliminary data also suggest lower rates of bladder injury and groin or hip pain following insertion of these devices.
With the introduction of new devices, clinicians have to decide whether they are going to adopt the new technique. Studies of surgical devices can be notoriously difficult to conduct and to report and interpret. It is therefore imperative that a high‐quality review is conducted to pool relevant data from randomised controlled trials to try to answer the question of whether these new single‐incision slings are capable of providing adequate treatment for stress incontinence with a lower rate of side effects compared with currently available standard methods of treatment. This is even more important in the current clinical climate in 2014, when implantable meshes and tapes are under intense scrutiny, both in the media and in clinical circles.
Objectives
To assess the effectiveness of mini‐sling procedures in women with urodynamic clinical stress or mixed urinary incontinence in terms of improved continence status, quality of life or adverse events.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials in which at least one trial arm involves one of the new single‐incision slings.
Types of participants
Adult women with stress urinary incontinence due to urethral hypermobility or intrinsic sphincter deficiency diagnosed urodynamically (urodynamic stress incontinence (USI)) or clinically (stress urinary incontinence (SUI)). Trials involving women with mixed urinary incontinence (MUI) were also included, if these women were shown to have stress‐predominant symptoms.
Types of interventions
At least one arm of the trial included a single‐incision sling (as defined above) to treat stress or mixed urinary incontinence. The comparison intervention included other surgical techniques and non‐surgical interventions. The definition of a single‐incision sling was “a sling that does not involve either a retropubic or transobturator passage of the tape or trocar and involves only a single vaginal incision (i.e. no exit wounds in the groin or lower abdomen).”
The following comparisons were made.
-
Single‐incision slings versus no treatment.
-
Single‐incision slings versus conservative treatment.
-
Single‐incision slings versus colposuspension.
-
Single‐incision slings versus laparoscopic procedures.
-
Single‐incision slings versus traditional sub‐urethral slings.
-
Single‐incision slings versus retropubic minimally invasive slings (subgrouped: 'bottom‐up' and 'top‐down' approach).
-
Single‐incision slings versus obturator minimally invasive slings (subgrouped: medial‐to‐lateral 'inside out' approach and lateral‐to‐medial 'outside‐in' approach).
-
One single‐incision sling versus another.
Comparisons were made on the basis of brand of sling, as significant differences between these products have been noted.
Types of outcome measures
The primary outcome measure was the proportion of women who still had urinary incontinence following surgery.
Primary outcomes
Primary effectiveness outcome: number of women with urinary incontinence.
Secondary outcomes
Women’s observations
-
Number of women with no improvement in urinary incontinence.
Quantification of symptoms
-
Number of pad changes.
-
Incontinence episodes.
-
Pad tests (weights).
Clinicians’ observations
-
Objective measurement of incontinence (such as observation, leakage observed at urodynamics).
Quality of life
-
General health status measures (e.g. Short Form 36).
-
Condition‐specific health measures (specific instruments designed to assess incontinence).
Surgical outcome measures
-
Duration of the operation.
-
Operative blood loss.
-
Duration of inpatient stay.
-
Time to return to normal activity level.
Adverse events
-
Major vascular or visceral injury.
-
Bladder or urethral perforation.
-
Inadvertent vaginal wall perforation (“button‐holing”).
-
Urinary retention and need for catheterisation in the short or long term.
-
Nerve damage.
-
Other perioperative surgical complications.
-
Wound dehiscence.
-
Infection related to use of synthetic mesh.
-
Erosion to vagina.
-
Erosion to bladder or urethra.
-
Long‐term pain/discomfort including pain/discomfort when sitting.
-
Dyspareunia.
-
De novo urgency symptoms or urgency incontinence.
-
(New) detrusor overactivity (urodynamic diagnosis).
-
Repeat incontinence surgery.
-
New prolapse surgery.
-
Need for additional or repeat treatment for incontinence.
Other outcomes
-
Non‐prespecified outcomes judged important when the review was performed.
Search methods for identification of studies
We imposed no language or other limits on the searches.
Electronic searches
This review drew on the search strategy developed for the Cochrane Incontinence Group. We identified relevant trials from the Cochrane Incontinence Group Specialised Trials Register. For more details on the search methods used to build the Specialised Register, please see the Group's module in The Cochrane Library. This register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and MEDLINE in process, and by handsearching of journals and conference proceedings. Most of the trials in the Cochrane Incontinence Group Specialised Register are also contained in CENTRAL. The date of the last search was 6 February 2013.
The terms used to search the Incontinence Group Specialised Register are given below.
(({DESIGN.CCT*} OR {DESIGN.RCT*}) AND {INTVENT.SURG.SLINGS.MINISLING*} AND {TOPIC.URINE.INCON*})
(All searches were of the keyword field of Reference Manager 2012.)
Other specific searches in a trials register and a trial portal were performed for this review.
-
ClinicalTrials.gov (searched 20 September 2012).
-
World Health Organization (WHO) Internatonal Clinical Trials Registry Platform (ICTRP) (searched 20 September 2012).
The search terms used are given in Appendix 1.
We performed additional searches for the Brief Economic Commentary (BECs). We conducted them in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). We ran all searches on 6 April 2017. Details of the searches run and the search terms used can be found in Appendix 2.
Searching other resources
Reference lists of all relevant reviews and trial reports were searched to identify further relevant studies.
Data collection and analysis
All data abstraction, synthesis and analysis for this review were conducted in accordance with standard guidelines and criteria of The Cochrane Collaboration. Data abstraction was carried out independently by two review authors and was checked by a third. All three review authors contributed towards the analysis.
Selection of studies
Randomised and quasi‐randomised trials were identified using the above search strategy. Studies were excluded if they were not randomised or quasi‐randomised controlled trials for women with stress incontinence or stress‐predominant mixed incontinence. All eligible trials were evaluated for appropriateness for inclusion before the results were considered by the three review authors. Excluded studies are listed in the Characteristics of excluded studies table, along with the reasons for their exclusion.
Data extraction and management
Trials were assessed independently by two review authors starting with the titles and gaining further clarity from the abstracts when necessary. Reports of potentially eligible trials were retrieved in full, assessed independently by two review authors and checked by a third. When data may have been collected but not reported, clarification was sought from the trialists when possible. Disagreements were resolved by discussion. Data extraction was performed independently by all three review authors; this approach served as a robust cross‐check for errors.
We extracted data independently using a standard form containing prespecified outcomes. Included trial data were processed as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Differences of opinion related to study inclusion, methodological quality or data extraction were resolved by discussion among review authors and, when necessary, were referred to a third party for arbitration.
Assessment of risk of bias in included studies
The Cochrane Collaboration risk of bias tool was used to examine the following features: sequence generation, allocation sequence concealment, blinding and incomplete outcome data. Two review authors assessed risk of bias independently. These assessments are presented in the risk of bias tables, graphs and summary figures.
Measures of treatment effect
We used RevMan software version 5.2.3 to conduct a meta‐analysis when two or more eligible trials were identified. A combined estimate of treatment effect across trials was calculated for each specified outcome. For categorical outcomes, the numbers reporting an outcome were related to the numbers at risk in each group to derive a risk ratio (RR). For continuous variables, means and standard deviations were used to derive a mean difference (MD). When feasible, intention‐to‐treat data were used. If similar outcomes were reported on different scales, we calculated the standard mean difference (SMD). We reversed the direction of effect, if necessary, to ensure consistency across trials.
Data synthesis
We used a fixed‐effect approach to the analysis unless evidence of heterogeneity was noted across trials, in which case a random‐effects model was used.
Subgroup analysis and investigation of heterogeneity
Differences between trials were investigated when apparent from visual inspection of the results, or when statistically significant heterogeneity was demonstrated by using the Chi2 test at the 10% probability level or assessment of the I2 statistic (Higgins 2003). When no obvious reason was noted for heterogeneity to exist (after consideration of populations, interventions, outcomes and settings of the individual trials), or when it persisted despite the removal of trials that were clearly different from the others, we used a random‐effects model.
No subgroup analyses were preplanned, but clinical factors such as symptoms of stress urinary incontinence, urodynamic stress incontinence, mixed urinary incontinence, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used or experience of the surgeon might all influence the outcomes of surgery and may be taken into account in future reviews.
Sensitivity analysis
Concomitant stress incontinence with prolapse is a common problem that is frequently corrected simultaneously at surgery; therefore we believed it was important to assess single‐incision slings in this clinically relevant scenario. When appropriate, sensitivity analyses have been conducted, with exclusion of trials in which concomitant surgery was performed.
Timing of outcome measures can vary between trials, and this can serve as a potential source of bias. When comparisons have been made between trials with significantly different mean duration of follow‐up, sensitivity analyses have been performed to assess whether this could be a source of bias.
Results
Description of studies
Trials included in this review have been named in such a way as to make identification and comparisons in tables more intuitive. Trials have been named in the format of <First author surname><Year of publication><Abbreviation of single‐incision sling(s) included in the study>. Abbreviations of single‐incision slings used in this review are as follows.
-
TVT‐Secur (SEC).
-
MiniArc (ARC).
-
Ajust (AJS).
-
Contasure Needleless (NDL).
-
Tissue Fixation System (TFS).
-
Ophira (OPH).
-
CureMesh (CUR).
For example, Abdelwahab 2010 SEC is a trial report published by Abdelwahab in 2010 including TVT‐Secur as the single‐incision sling intervention; Pardo 2010 SEC ARC included both TVT‐Secur and MiniArc as interventions. This naming system allows easy identification of the types of single‐incision slings used in each study for evaluation of the figures and tables in this review.
Characteristics of the different single‐incision slings
One of the important differences between the different types of single‐incision slings is whether a fixation system, or hook, holds them in place.
Slings that include a fixation system or hook are MiniArc (ARC), CureMesh (CUR), Ajust (AJS), Contasure Needleless (NDL) and Tissue Fixation System (TFS).
Slings that do not include a fixation system or hook are TVT‐Secur (SEC) and Ophira (OPH).
These divisions, however, are subject to further scrutiny because it is difficult to define what is meant by a good 'fixation system.' For example, the Contasure Needleless (NDL) system uses fascial pockets at both ends, in which normal artery forceps are placed to guide the ends of the sling to the obturator tunnel. Technically these pockets act as anchors once the forceps have been removed, but the strength and pull‐out forces could be quite different from those of the tissue fixation system (TFS), which anchors into the pubourethral ligament/muscle complex. Nevertheless, they are regarded as third‐generation sub‐urethral slings, as they do share several common characteristics. The review authors decided that for this iteration of the review, they would be assessed as one group, in line with the protocol.
Results of the search
We identified 81 reports of studies from the literature search (Figure 1). We excluded 13, and ongoing studies will be taken into account for future updates (Characteristics of ongoing studies). As the result of overlap between abstracts and published papers, and through separation of single‐centre reports from multi‐centre trials, we finally identified 31 trials that met the inclusion criteria.

PRISMA study flow diagram.
-
19 full published papers (Abdelwahab 2010 SEC; Amat 2011 NDL; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Enzelsberger 2010 ARC; Hinoul 2011 SEC; Hota 2012 SEC; Lee 2010 SEC; Liapis 2010 SEC; Martan 2012 ARC AJS; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Sivaslioglu 2012 TFS; Sottner 2012 ARC AJS; Tommaselli 2010 SEC; Wang 2011 SEC).
-
One thesis (Mackintosh 2010 AJS).
-
11 abstracts (Bianchi 2012 SEC; Djehdian 2010 OPH; Friedman 2009 SEC; Kim 2010 SEC; Lee 2010 CUR/SEC; Lee 2012 ARC; Pardo 2010 SEC ARC; Schweitzer 2012 AJS; Seo 2011 SEC; Smith 2011 ARC; Yoon 2011 NDL).
Four ongoing trials were identified (Foote 2012; Maslow 2011; Robert 2012; Rosamilia 2012; Characteristics of ongoing studies). One paper, in Russian, that we are still trying to obtain is listed in Studies awaiting classification (Pushkar 2011).
Included studies
In all, 31 trials met the inclusion criteria. These include 19 fully published papers, one thesis and 11 abstracts. The characteristics of included trials varied considerably and have been described in detail in Characteristics of included studies. A brief descriptive summary follows.
No trials were identified that compared single‐incision slings versus no treatment, conservative treatment, colposuspension, laparoscopic procedures or traditional sub‐urethral slings.
Single‐incision slings versus retropubic mid‐urethral slings
Five trials were identified. These were further sub‐divided on the basis of comparisons with top‐to‐bottom or bottom‐to‐top approaches of retropubic slings; however no trials compared single‐incision slings versus top‐to‐bottom retropubic slings. All five trials were fully published papers and compared single‐incision slings versus bottom‐to‐top retropubic slings (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC).
Women with prolapse
One study included women with concomitant prolapse (Barber 2012 SEC) but did not present separate data for participants who underwent sling surgery alone. Two trials were unclear about inclusion of women with associated prolapse (Andrada Hamer 2012 SEC; Wang 2011 SEC). No other significant difference was noted between participant groups. Methodology was not well described in Abdelwahab 2010 SEC but was adequate in the four other trials.
Single‐incision slings versus transobturator mid‐urethral slings
These trials were further sub‐divided by type of trans‐obturator sling into inside‐out (TVT‐O) and outside‐in (TOT).
Inside‐out slings
Thirteen trials compared single‐incision slings versus inside‐out transobturator slings. Eight were fully published papers (Amat 2011 NDL; Hinoul 2011 SEC; Hota 2012 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC), four were abstracts (Bianchi 2012 SEC; Friedman 2009 SEC; Schweitzer 2012 AJS; Seo 2011 SEC) and one was a thesis (Mackintosh 2010 AJS). Reporting and adequacy of methodology were variable—methodological information in all abstracts was minimal, as it was in Oliveira 2011 ARC SEC, but in Amat 2011 NDL, the randomisation method used was considered inadequate. The other full papers described methodology well.
Women with prolapse
Amat 2011 NDL; Friedman 2009 SEC; and Hota 2012 SEC included participants with associated prolapse who may have had concomitant prolapse surgery. Bianchi 2012 SEC; Hinoul 2011 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; and Tommaselli 2010 SEC excluded patients with associated prolapse. Mackintosh 2010 AJS; Schweitzer 2012 AJS; and Seo 2011 SEC did not specify this in their exclusion criteria.
Outside‐in slings
Seven trials compared single‐incision slings versus outside‐in transobturator slings (TOTs). Only one is a fully published paper (Sivaslioglu 2012 TFS); the others were abstracts (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Smith 2011 ARC; Yoon 2011 NDL). Enzelsberger 2010 ARC is a German paper that contains an English language abstract with minimal information. A full translation was not obtained, but we will try to request this for future updates. Methodological quality of these trials was variable. In Lee 2012 ARC; Sivaslioglu 2012 TFS; and Smith 2011 ARC,randomisation methods were adequately described, but allocation and blinding were not described. Randomisation was unequal, and the method was not described in Djehdian 2010 OPH, was inadequately performed in Yoon 2011 NDL, and was not clearly described in Kim 2010 SEC.
Prolapse and overactive bladder symptoms
Djehdian 2010 OPH excluded patients with significant genitourinary prolapse, and Sivaslioglu 2012 TFS excluded patients with predominant overactive bladder symptoms, but Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Smith 2011 ARC; and Yoon 2011 NDL were unclear about inclusion/exclusion of these patient groups.
One type of single‐incision sling versus another
Nine trials were identified: five full papers (Lee 2010 SEC; Liapis 2010 SEC; Masata 2012 SEC; Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC) and four abstracts (Lee 2010 CUR/SEC; Martan 2012 ARC AJS; Pardo 2010 SEC ARC; Sottner 2012 ARC AJS). Methodological quality was variable even among fully published papers, ranging from inadequate randomisation methods used in Liapis 2010 SEC to overall very robust and well‐reported methodology used in Palomba 2012 AJS ARC SEC. Methodology as reported in the abstracts was generally unclear. Comparisons varied in these trials and have been grouped into three owing to the difference in fixation systems of the different types of single‐incision slings: TVT‐SECUR versus MiniArc, U‐type versus H‐type of TVT‐Secur and MiniArc versus Ajust. The Sottner 2012 ARC AJS paper was published in Czech with an English abstract, but no useful data were available, and no translation was obtained; however, this will be requested for future updates.
Excluded studies
Seven studies were excluded because they were not randomised control trials or because they did not include single‐incision slings as one of the comparators. Four trials were ongoing at the time of writing of this review and therefore were not included in the analysis but may be considered in future updates. One trial is awaiting classification because currently available information is lacking; however, it will be considered in future updates. The details of these studies are given under Characteristics of excluded studies.
Five other studies are awaiting assessment or are ongoing trials; details are given in the Characteristics of studies awaiting classification and Characteristics of ongoing studies sections.
Risk of bias in included studies
The risk of bias in included trials was variable, with about half of the trials using adequate methods of randomisation and allocation concealment, while in the other half, methods used were inadequate or were not described. Attempts to double‐blind were even less rigorous, with only five trials carrying out some kind of blinding of participants. Although blinding can be notoriously difficult to achieve in surgical trials, it is nonetheless possible to a reasonable degree; therefore the review authors believed it was warranted to utilise this as a criterion in the risk of bias section. The findings of the risk of bias assessment are summarised in Figure 2 and Figure 3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
The risk of bias was considered to be low for random sequence generation for 14 trials, in which the sequence was generated most often by using a computer (Barber 2012 SEC; Basu 2010 ARC; Hinoul 2011 SEC; Lee 2010 SEC; Lee 2012 ARC; Mackintosh 2010 AJS; Martan 2012 ARC AJS; Masata 2012 SEC; Mostafa 2012 AJS; Palomba 2012 AJS ARC SEC; Sivaslioglu 2012 TFS; Smith 2011 ARC; Tommaselli 2010 SEC; Wang 2011 SEC).
The risk of bias was considered high for three trials, in which allocation was based on medical record number (Amat 2011 NDL), participants were allocated alternately (Liapis 2010 SEC) or the method of randomisation was inadequately described (Pardo 2010 SEC ARC).
The risk of bias was considered unclear in the remaining 14 trials, in which no description was given in the report (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Bianchi 2012 SEC; Djehdian 2010 OPH; Enzelsberger 2010 ARC; Friedman 2009 SEC; Hota 2012 SEC; Kim 2010 SEC; Kim 2010 SEC; Lee 2010 CUR/SEC; Oliveira 2011 ARC SEC; Schweitzer 2012 AJS; Seo 2011 SEC; Sottner 2012 ARC AJS; Yoon 2011 NDL).
Allocation concealment
Eleven trials used an adequate allocation concealment method (most often opaque envelopes) (Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Hota 2012 SEC; Lee 2012 ARC; Mackintosh 2010 AJS; Martan 2012 ARC AJS; Masata 2012 SEC; Mostafa 2012 AJS; Palomba 2012 AJS ARC SEC; Wang 2011 SEC).
The other 20 trials failed to describe any method of allocation concealment.
Blinding
Blinding of participants or personnel
Only five trials carried out some kind of blinding of participants. The Barber trial (Barber 2012 SEC) used sham incisions in the mini‐sling arm to facilitate blinding. In the Basu trial (Basu 2010 ARC), participants were blinded but researchers could not be blinded because of differences in devices. The Palomba trial (Palomba 2012 AJS ARC SEC) stated that participants and data assessors were masked to the procedure. The Schweitzer trial (Schweitzer 2012 AJS) reported that women were blinded to the type of procedure by use of a sham incision in the Ajust group. Tommaselli et al (Tommaselli 2010 SEC) reported that participants "were left blinded to the devices used until the end of the procedure." The other trials made no mention of blinding or stated that it was not possible.
Blinding of outcome assessors
Six trials mentioned methods of reducing risk of bias through blinded outcome assessment (Andrada Hamer 2012 SEC; Barber 2012 SEC; Mackintosh 2010 AJS; Mostafa 2012 AJS; Palomba 2012 AJS ARC SEC; Sivaslioglu 2012 TFS). Three were considered to be at high risk of bias owing to unblinded outcome assessment or inadequate information for assessment (Pardo 2010 SEC ARC; Schweitzer 2012 AJS; Smith 2011 ARC).
Incomplete outcome data
The risk of bias was considered high for eight trials (Amat 2011 NDL; Andrada Hamer 2012 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Liapis 2010 SEC; Schweitzer 2012 AJS; Smith 2011 ARC; Tommaselli 2010 SEC) as the result of high dropout rates. Of these, differential dropout rates were observed in Andrada Hamer 2012 SEC and Hinoul 2011 SEC. Hota 2012 SEC failed to recruit the required number of participants and was stopped at interim analysis.
Effects of interventions
Single‐incision slings versus no treatment
No trials that compared single‐incision slings versus no treatment were found.
Single‐incision slings versus conservative treatment
No trials that compared single‐incision slings versus conservative treatment were found.
Single‐incision slings versus colposuspension
No trials that compared single‐incision slings versus colposuspension were found.
Single‐incision slings versus laparoscopic procedures
No trials that compared single‐incision slings versus laparoscopic procedures were found.
Single‐incision slings versus traditional sub‐urethral slings
No trials that compared single‐incision slings versus traditional sub‐urethral slings were found.
Single‐incision slings versus retropubic minimally invasive slings (subgrouped: 'bottom‐up' and 'top‐down' approach)
Five trials met the inclusion criteria (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC). All single‐incision slings were compared with 'bottom‐up' retropubic minimally invasive slings. All but one trial (Basu 2010 ARC) involved one type of mini‐sling: TVT‐Secur. The study authors note that the Andrada Hamer 2012 SEC study was stopped at interim analysis (two months) because of poor efficacy and complication rates with the TVT‐Secur.
No trials that compared a single‐incision sling versus a 'top‐down' retropubic sling were identified. These types of slings are no longer used in clinical practice, but if we had identified such trials, they would have been included for completeness.
Number of women with urinary incontinence (primary outcome)
All five trials were included in this meta‐analysis. The overall result showed that more women had persistent urinary incontinence after the single‐incision surgery (121/292, 41% vs 72/281, 26%; RR 2.08, 95% CI 1.04 to 4.14; Analysis 6.1), and this was statistically significant in favour of retropubic slings. One trial (Basu 2010 ARC) compared the MiniArc sling against TVT; the other four compared TVT‐Secur against TVT.
Statistical heterogeneity is apparent in this meta‐analysis, possibly as a result of the inconclusive results of the small Abdelwahab trial and the larger Barber trial. Clinical heterogeneity may also be a factor: One trial (Barber 2012 SEC) did include women with concomitant prolapse, and almost half of the study population underwent some form of concomitant surgery. Two of the other trials (Andrada Hamer 2012 SEC; Wang 2011 SEC) were not clear about whether women with concomitant prolapse were included. However, the result remained statistically significant in favour of retropubic tape when a more conservative random‐effects model was used.
Follow‐up ranged from nine months (Abdelwahab 2010 SEC) to three years (Basu 2010 ARC) but was one year for the other three trials (Andrada Hamer 2012 SEC; Barber 2012 SEC; Wang 2011 SEC). Most trials used a composite measure of cure consisting of subjective and objective measures of incontinence. Although one‐year follow‐up data are reported for the Andrada Hamer 2012 SEC study, it must be noted that only half of the planned number of subjects were recruited because the trial was stopped at interim analysis. Nevertheless, the review authors believed that the reported data should be included in the meta‐analysis.
Number of women with no improvement
Three trials were included in the meta‐analysis (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Wang 2011 SEC). The overall result showed that almost all women had improved, but no statistically significant difference was observed between the two treatments, and the confidence interval was wide (Analysis 6.2).
Objective measurement of incontinence
Two trials were included in the meta‐analysis (Andrada Hamer 2012 SEC; Basu 2010 ARC). The Andrada Hamer trial compared TVT‐Secur against TVT with follow‐up at one year. Investigators performed both cough test and pad test for objective measurement of SUI; we have used the results of the cough test in this analysis. The Basu trial compared the MiniArc against TVT with follow‐up of three years; however urodynamic evaluation of incontinence (the objective measurement criterion used in the trial) was done at six‐month follow‐up, and these data were used in this comparison. The overall result reflected the individual results of the separate trials and was statistically significant favouring retropubic slings (RR 4.44, 95% CI 2.06 to 9.56) (Analysis 6.3).
Quality of life
The Barber trial (Barber 2012 SEC) measured condition‐specific quality of life at one year using the Incontinence Severity Index score. Quality of life was statistically significantly better in the retropubic group (Analysis 6.4).
Surgical outcome measures
Duration of operation
Three trials were included in the meta‐analysis (Abdelwahab 2010 SEC; Barber 2012 SEC; Wang 2011 SEC). Andrada Hamer 2012 SEC also provided data for mean duration of operation, but the standard deviation was not given; therefore it could not be included in the meta‐analysis. The duration of the operation was significantly shorter for the single‐incision sling (17 minutes, 95% CI 3 to 32 minutes) (Analysis 6.5). However, statistical heterogeneity may be explained clinically by differences in the definition of what constitutes "duration of operation." Statistical significance persisted when the more conservative random‐effects model was used, and all three trials favoured the single‐incision arm.
Operative blood loss
Only one study was included in this analysis (Abdelwahab 2010 SEC), but lower blood loss with a single‐incision sling was not statistically significant (Analysis 6.6).
Length of in‐patient stay
One study was included in the analysis (Abdelwahab 2010 SEC), but the results were not statistically significant and the confidence interval was wide (Analysis 6.7).
Adverse events
Major vascular or visceral injury; vaginal wall perforation
The small Andrada Hamer trial (Andrada Hamer 2012 SEC) reported that one woman had major vascular or visceral injury (Analysis 6.8), and one in each group had vaginal wall perforation (Analysis 6.9); however, the results were not statistically significant because wide confidence intervals implied lack of evidence in favour of either procedure.
Bladder or urethral perforation
Bladder or urethral perforation was reported in four trials (Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC) and was not common (<4%). The overall result was not statistically significant and the confidence interval was wide (Analysis 6.10). Apart from the Basu trial (Basu 2010 ARC), which compared the MiniArc with TVT, all other trials used TVT‐Secur as the experimental intervention, but no statistical heterogeneity was evident.
Urinary retention and the need for catheterisation
Five trials reported on this outcome (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC). Less than 4% of women experienced difficulty voiding; the difference between groups was not statistically significant and the confidence interval was wide (Analysis 6.11).
Infection due to synthetic mesh; dyspareunia
Infection related to the use of synthetic mesh and dyspareunia were reported in one small study (Abdelwahab 2010 SEC), but no evidence showed a difference between the procedures (Analysis 6.12; Analysis 6.16).
Vaginal mesh exposure
Vaginal exposure (erosion) of mesh was reported in three women in two trials (Barber 2012 SEC; Basu 2010 ARC); this result was not statistically significant and the confidence interval was wide (Analysis 6.13).
Mesh extrusion into bladder or urethra
Mesh extrusion into the bladder or urethra was reported in five women in three trials (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC); the combined result showed no evidence of a difference between the two procedures and the confidence interval was wide (Analysis 6.14).
Long‐term pain or discomfort
Two trials reported this outcome (Barber 2012 SEC; Wang 2011 SEC). None of the 329 women reported this adverse effect.
De novo urgency; new‐onset detrusor overactivity
De novo urgency was reported in three trials (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Wang 2011 SEC), all of which compared TVT‐Secur versus TVT. It was more common in the single‐incision group, and the meta analysis showed a statistically significant difference favouring the retropubic TVT procedure (27/125, 22% vs 11/123, 9% after TVT; RR 2.39, 95% CI 1.25 to 4.56) (Analysis 6.17).
One small trial (Basu 2010 ARC) reported that two women in each group developed new‐onset detrusor overactivity (Analysis 6.18).
Repeat stress incontinence surgery
Repeat stress incontinence surgery was reported in only two trials (Barber 2012 SEC; Basu 2010 ARC), which used different single‐incision slings. In the Basu trial (Basu 2010 ARC), nine women required further incontinence surgery after a single‐incision sling compared with none in the retropubic sling group—a result that was statistically significant in favour of retropubic slings versus the MiniArc. Although the Barber trial (Barber 2012 SEC) showed no statistically significant difference in the comparison between retropubic slings versus TVT‐Secur, only six women required further surgery and the confidence interval was wide (Analysis 6.19).
Need for any other additional or new surgical procedure to treat complications
This outcome was reported in Barber 2012 SEC and Basu 2010 ARC. No significant difference was noted in the number of women who required additional procedures to treat complications of the index surgery (Analysis 6.20).
Single‐incision slings versus obturator minimally invasive slings (subgrouped: medial‐to‐lateral 'inside out' approach and lateral‐to‐medial 'outside‐in' approach)
Twenty trials met the inclusion criteria.
Thirteen trials compared single‐incision slings versus inside‐out transobturator slings (Amat 2011 NDL; Bianchi 2012 SEC; Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Schweitzer 2012 AJS; Seo 2011 SEC; Tommaselli 2010 SEC; Wang 2011 SEC).
Seven trials compared single‐incision slings versus outside‐in transobturator slings (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC; Yoon 2011 NDL).
The combined overall results for single‐incision slings versus any types of transobturator slings are stated when available.
Number of women with urinary incontinence (primary outcome)
Ten trials that compared a single‐incision sling (eight TVT‐Secur, two AJS and one ARC) against inside‐out transobturator slings were included in the meta‐analysis (Bianchi 2012 SEC; Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Seo 2011 SEC; Wang 2011 SEC). Both Masata 2012 SEC and Oliveira 2011 ARC SEC were three‐arm trials with two types of single‐incision devices. For purposes of this analysis, the data from the single‐incision arms have been combined for each trial. More women had urinary incontinence in the single‐incision sling arms (172/572, 30%), and the overall result was statistically significant in favour of inside‐out transobturator slings (incontinence in 55/481, 11% of women; RR 2.55, 95% CI 1.94 to 3.36) (Analysis 7.1.1). A sensitivity analysis excluding the two trials that did not use TVT‐Secur (Mackintosh 2010 AJS; Mostafa 2012 AJS) made no difference in the results (RR 2.65, 95% CI 1.98 to 3.54) (Analysis 7.1.1). This device has been withdrawn from clinical use.
Follow‐up for all trials was 12 months, apart from Bianchi 2012 SEC; Friedman 2009 SEC; and Masata 2012 SEC, which reported two‐year follow‐up, and Mackintosh 2010 AJS, which reported three‐month follow‐up. Exclusion of the Mackintosh 2010 AJS study made no difference in the results.
Seven trials compared five different types of single‐incision slings against outside‐in transobturator slings (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC; Yoon 2011 NDL). The overall result was not statistically significant (36/306, 12% vs 38/296, 13%; RR 0.91, 95% CI 0.60 to 1.39; Analysis 7.1), nor was individual comparison by subtype of single‐incision sling. Considerable variation in the range of follow‐up was seen, from four weeks (Yoon 2011 NDL) to five years (Sivaslioglu 2012 TFS). Djehdian 2010 OPH is an ongoing trial with unequal randomisation reported at six‐month follow‐up.
When results for transobturator slings were combined as a single group, the result was still statistically significant in favour of transobturator slings (RR 1.91, 95% CI 1.53 to 2.39) (Analysis 7.1), but this introduces a degree of heterogeneity, with an I2 statistic of 49%.
Number of women with no improvement
Four trials that compared TVT‐Secur against inside‐out transobturator slings were included in the meta‐analysis (Masata 2012 SEC; Oliveira 2011 ARC SEC; Seo 2011 SEC; Wang 2011 SEC). Oliveira 2011 ARC SEC was a three‐arm trial; for purposes of analysis, the two single‐incision arms were combined, but a sensitivity analysis showed that this had little impact on the combined result. Masata 2012 SEC had the longest follow‐up, at two years. Similar to the analysis of participant‐reported incontinence rates, the overall result was statistically significant in favour of inside‐out transobturator slings (RR 4.80, 95% CI 2.00 to 11.55; Analysis 7.2).
One small trial (Lee 2012 ARC) compared MiniArc against an outside‐in transobturator tape, but the result was not statistically significant.
The combined result was still statistically significant in favour of transobturator slings (RR 2.29, 95% CI 1.29 to 4.06) but with a degree of heterogeneity (I2 = 59%).
Objective measurement of incontinence
Seven trials that compared TVT‐Secur against inside‐out transobturator slings were included in the meta‐analysis (Bianchi 2012 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Mostafa 2012 AJS; Tommaselli 2010 SEC). Women were nearly three times more likely to be incontinent with a single‐incision sling, and the overall result was statistically significant in favour of inside‐out transobturator slings (RR 2.91, 95% CI 2.00 to 4.25) (Analysis 7.3.1). Evidence of some statistical heterogeneity was seen in this result, but the direction of effect was the same in all trials.
Five trials that compared different types of single‐incision slings against outside‐in transobturator slings were included in the meta‐analysis (Djehdian 2010 OPH; Lee 2010 CUR/SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC). The result was not statistically significant, but confidence intervals were too wide to ensure no differences between the groups.
Overall, the results obtained when both types of transobturator tapes were combined still favoured the latter (RR 1.88, 95% CI 1.49 to 2.36) (Analysis 7.3).
Incontinence episodes
One study (Smith 2011 ARC) compared MiniArc against outside‐in transobturator slings but was too small to show a difference in the number of incontinence episodes at a mean follow up of 33 months (Analysis 7.4).
Pad test (weight of urine lost)
Two trials (Djehdian 2010 OPH; Lee 2012 ARC) performed pad tests at six months. However, it must be noted that Djehdian 2010 OPH reported one‐hour pad weights and Lee reported 24‐hour pad weights. Although no statistically significant difference was observed between the groups, the confidence interval was wide (Analysis 7.5).
Quality of life
Two trials (Hinoul 2011 SEC; Mostafa 2012 AJS) of single‐incision versus inside‐out transobturator slings are included in this meta‐analysis. Different condition‐specific health questionnaires were used (Urinary Distress Inventory (UDI)‐6 and International Consultation on Incontinence Modular Questionnaire, Short Form (ICIQ‐SF)); therefore results were combined by using standardised mean differences. The result was not statistically significant (Analysis 7.6.1) and the confidence interval was wide.
One small trial compared a single‐incision sling versus an outside‐in transobturator sling (Djehdian 2010 OPH) and favoured the TOT, but a large discrepancy was noted in recruitment for this study, with the single‐incision group almost double the TOT group; therefore the results must be interpreted with caution (Analysis 7.6.2).
Surgical outcome measures
Duration of operation
Six trials (Hinoul 2011 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Schweitzer 2012 AJS; Tommaselli 2010 SEC; Wang 2011 SEC) compared single‐incision slings versus inside‐out transobturator slings, and three trials (Enzelsberger 2010 ARC; Lee 2012 ARC; Yoon 2011 NDL) compared single‐incision slings versus outside‐in transobturator slings.
The overall duration of the operation was one minute less for single‐incision slings (MD ‐1.17 minutes, 95% CI ‐1.60 to ‐0.75) (Analysis 7.7), but the clinical and economic advantages of a one‐minute reduction in theatre time are likely to be negligible. Significant statistical heterogeneity may be explained by differences in the definition of what constitutes "duration of operation."
Operative blood loss
Two trials (Hinoul 2011 SEC; Masata 2012 SEC) comparing TVT‐Secur against inside‐out TVT‐O showed that women lost 19 mL less blood with the TVT‐O; this is a statistically significant result favouring TVT‐O (MD 19, 95% CI 4 to 34 mL; Analysis 7.8.1).
Length of in‐patient stay
One study (Hinoul 2011 SEC) reported this outcome, but the result was not statistically significant.
Adverse events
Major vascular or visceral injury
This outcome was reported in three trials (Hinoul 2011 SEC; Masata 2012 SEC; Tommaselli 2010 SEC), all of which compared TVT‐Secur against inside‐out transobturator slings. Very few events were reported, and no evidence suggested superiority of either procedure (Analysis 7.10.1)
Bladder or urethral perforation
This rare outcome (four women in all) was reported in five trials (Amat 2011 NDL; Hinoul 2011 SEC; Masata 2012 SEC; Schweitzer 2012 AJS; Wang 2011 SEC) that compared single‐incision slings versus inside‐out transobturator slings, and in four versus outside‐in TOT (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Lee 2010 CUR/SEC; Sivaslioglu 2012 TFS). The overall results were not statistically significant (Analysis 7.11), but the confidence intervals were wide.
Vaginal wall perforation
Six women had vaginal wall perforation, as reported in five trials (Friedman 2009 SEC; Hinoul 2011 SEC; Masata 2012 SEC; Oliveira 2011 ARC SEC; Schweitzer 2012 AJS) that compared single‐incision slings against inside‐out transobturator slings, and in one trial versus an outside‐in transobturator sling (Djehdian 2010 OPH). The overall result was not statistically significant, and the confidence interval was wide (Analysis 7.12).
Urinary retention and the need for catheterisation
Ten trials reported this outcome by comparing single‐incision slings against inside‐out transobturator slings (Amat 2011 NDL; Bianchi 2012 SEC; Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC). Few women had this complication (2% to 3%), and the overall result was not statistically significant, with a wide confidence interval (RR 0.72, 95% CI 0.34 to 1.52) (Analysis 7.13.1).
Five trials compared single‐incision slings against outside‐in transobturator slings (Djehdian 2010 OPH; Lee 2010 CUR/SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC). Three times as many women required catheterisation after an outside‐in transobturator sling as after a single‐incision sling (2.5%) or an inside‐out transobturator sling (3.2%); this is difficult to explain. The overall result was statistically significant in favour of single‐incision slings, but the trials were not consistent in this respect. This result was driven mainly by the larger Lee 2012 ARC study, which was given the highest weight in the meta‐analysis. Statistical heterogeneity was apparent, and when a random‐effects model was used, the overall result was no longer statistically significant (Analysis 7.13.2).
The combined result was not statistically significant either and had a wide confidence interval, implying that evidence was insufficient to suggest any difference (RR 0.57, 95% CI 0.28 to 1.15) (Analysis 7.13).
Infection related to the use of synthetic mesh
One study reported this outcome in comparing single‐incision slings against inside‐out transobturator slings (Hinoul 2011 SEC), but the overall result was not statistically significant and the confidence interval was wide (Analysis 7.14.1).
Another study also reported this outcome in comparing single‐incision slings against outside‐in transobturator slings (Lee 2012 ARC), but again the overall result was not statistically significant and the confidence interval was wide (Analysis 7.14.2).
Vaginal exposure of mesh
Vaginal exposure (erosion) of mesh was reported in five trials (Bianchi 2012 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mostafa 2012 AJS; Tommaselli 2010 SEC) that compared single‐incision slings (all TVT‐Secur) against inside‐out transobturator slings. More women in the single‐incision groups had exposure (18/284, 6% vs 4/278, 1%), and the overall result was statistically significant, favouring inside‐out transobturator slings (RR 3.75, 95% CI 1.42 to 9.86) (Analysis 7.15.1). Four trials (Djehdian 2010 OPH; Lee 2010 CUR/SEC; Sivaslioglu 2012 TFS; Smith 2011 ARC) compared single‐incision slings against outside‐in transobturator slings. The number of cases was fewer, and the overall result was not statistically significant, with a wide confidence interval (Analysis 7.15.1).
The combined overall result was still significant in favour of transobturator slings (RR 2.59, 95% CI 1.21 to 5.56) (Analysis 7.15).
Mesh extrusion into bladder or urethra
Only two small trials reported on this outcome (Hota 2012 SEC; Lee 2010 CUR/SEC). Only eight women were reported to have this complication, all in the single‐incision sling group in one of the trials: A statistically significant result favouring transobturator slings was of dubious reliability because of the small numbers (Analysis 7.16).
Post‐operative pain or discomfort
Pain was reported in eight trials (Amat 2011 NDL; Bianchi 2012 SEC; Friedman 2009 SEC; Lee 2012 ARC; Mackintosh 2010 AJS; Mostafa 2012 AJS; Seo 2011 SEC; Tommaselli 2010 SEC). The overall result was statistically significant favouring single‐incision slings: Fewer women (27/415, 7%) had pain versus 90/391 (23%) after an inside‐out transobturator sling (RR 0.29, 95% 0.20 to 0.43) (Analysis 7.17.1). Most of the trials used TVT‐Secur as the experimental intervention, apart from Amat 2011 NDL; Lee 2012 ARC; and Mackintosh 2010 AJS, but a sensitivity analysis excluding these trials made little difference in the results for individual single‐incision sling subtypes. Two trials (Lee 2012 ARC; Sivaslioglu 2012 TFS) compared single‐incision slings against outside‐in transobturator slings, and the result was similar, with statistical significance in favour of single‐incision slings (Analysis 7.17.2).
The combined overall result showed that women had less short‐term pain or discomfort after a single‐incision sling (34/563, 6% vs 129/539, 23.9% after a TOT; RR 0.26, 95% CI 0.19 to 0.37) (Analysis 7.17), but the relevance of this difference may not be clinically important to women.
Long‐term pain or discomfort
This was rare and was reported in only three trials comparing TVT‐Secur against inside‐out transobturator slings (Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC) and in two trials comparing single‐incision slings against outside‐in transobturator slings (Djehdian 2010 OPH; Sivaslioglu 2012 TFS). A statistically significant difference favoured single‐incision slings in the latter case only (RR 0.12, 95% CI 0.02 to 0.82) (Analysis 7.18.2).
Although uncommon, women were significantly less likely to have long‐term pain after a single‐incision sling than after a transobturator sling, and the overall result favoured single‐incision slings (1/196, 0.5% vs 11/155, 7.1%; RR 0.14, 95% CI 0.04 to 0.54) (Analysis 7.18).
De novo urgency
Eight trials were included in the meta‐analysis comparing TVT‐Secur versus inside‐out transobturator tapes (Abdelwahab 2010 SEC; Bianchi 2012 SEC; Friedman 2009 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC). Overall no statistically significant difference between the groups was observed (Analysis 7.19.1). Two trials compared single‐incision slings versus outside‐in transobturator tapes (Djehdian 2010 OPH; Smith 2011 ARC) and again found no statistically significant difference between the groups (Analysis 7.19.2).
Around 10% of women reported this symptom. The overall result was not quite statistically significant in favour of transobturator slings but the confidence intervals were wide (RR 1.41, 95% CI 0.98 to 2.03) (Analysis 7.19).
Repeat stress incontinence surgery
Three trials compared TVT‐Secur against inside‐out transobturator slings (Hota 2012 SEC; Masata 2012 SEC; Mostafa 2012 AJS); the pooled analysis showed that women were nearly six times more likely to need further stress incontinence surgery after a single‐incision sling—a significant difference in favour of transobturator slings (28/240, 12% vs 3/180, 2%; RR 5.86, 95% CI 2.0 to 17.21) (Analysis 7.20.1). Two trials compared MiniArc versus outside‐in transobturator tapes (Lee 2012 ARC; Smith 2011 ARC) but found no difference between the groups, as did one study (Sivaslioglu 2012 TFS) that compared the tissue fixation system single‐incision sling (TFS) versus outside‐in transobturator tapes (Analysis 7.20.2).
The overall result was still statistically significant in favour of transobturator slings: Women are three times more likely to need repeat incontinence surgery after a single‐incision sling (33/412, 8.0% vs 8/352, 2.3%; RR 3.09, 95% CI 1.48 to 6.49) (Analysis 7.20). However, this result was driven by the two trials that used TVT‐Secur (Hota 2012 SEC; Masata 2012 SEC). Without these two trials, no significant difference in repeat surgery rates would be reported.
Need for any other additional or new surgical procedure to treat complications
For this outcome, we assessed any subsequent procedures required to treat complications of the index surgery (e.g. cutting for voiding difficulty, removing tape for mesh exposure or extrusion).
Five trials were included in the meta‐analysis comparing TVT‐Secur against inside‐out transobturator slings (Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Masata 2012 SEC; Oliveira 2011 ARC SEC). The results were statistically significant in favour of transobturator slings (Analysis 7.21.1). Three trials compared single‐incision slings against outside‐in transobturator slings but found no difference between the groups (Analysis 7.21.2).
The overall result was still statistically significant in favour of transobturator slings: Twice as many women required surgery for complications after a single‐incision sling (28/541, 5.2% vs 11/448, 2.5%; RR 2.03, 95% CI 1.09 to 3.78) (Analysis 7.21).
One single‐incision sling versus another
Comparisons were made on the basis of brand of sling because significant differences between various products were possible.
Nine trials met the inclusion criteria (Lee 2010 SEC; Lee 2010 CUR/SEC; Liapis 2010 SEC; Martan 2012 ARC AJS; Masata 2012 SEC; Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC; Sottner 2012 ARC AJS). The only one of these trials that was methodologically robust on every dimension of risk of bias was Palomba 2012 AJS ARC SEC. Follow‐up varied among trials, ranging from 30 days (Palomba 2012 AJS ARC SEC) to two years (Martan 2012 ARC AJS; Masata 2012 SEC).
Because of the numerous types of slings compared, very few data could be combined in meta‐analysis and evidence was insufficient to allow the review authors to confidently identify any differences between any of the different types of single‐incision sling.
Number of women with urinary incontinence (primary outcome)
TVT‐Secur versus MiniArc
Two trials were included in this analysis (Oliveira 2011 ARC SEC; Pardo 2010 SEC ARC) and data were too few to allow inferences of any difference between the groups (Analysis 8.1.1).
U‐type versus H‐type TVT‐Secur
Three trials were included in this analysis (Kim 2010 SEC; Liapis 2010 SEC; Masata 2012 SEC) and showed no significant differences between groups, but the confidence interval was wide (Analysis 8.1.2).
MiniArc versus Ajust
Only one study was included in this analysis (Martan 2012 ARC AJS); it showed no significant differences between groups and the confidence interval was wide (Analysis 8.1.3).
Number of women with no improvement
TVT‐Secur versus MiniArc
Two trials were included in this analysis (Oliveira 2011 ARC SEC; Pardo 2010 SEC ARC); although the trials seem to favour the MiniArc procedure, no statistically significant differences between groups were reported (Analysis 8.2.1).
U‐type versus H‐type TVT‐Secur
Only one study was included in this analysis (Masata 2012 SEC) and data were too few to allow inferences about any differences between groups (Analysis 8.2.2).
MiniArc versus Ajust
Only one study was included in this analysis (Martan 2012 ARC AJS) and the data were too few to allow inferences about any differences between groups (Analysis 8.2.3).
Objective measurement of incontinence
MiniArc versus Ajust
Only one study was included in this analysis (Martan 2012 ARC AJS) and data were too few to allow inferences about any differences between groups (Analysis 8.3.1).
U‐type versus H‐type TVT‐Secur
Three trials were included in this analysis (Lee 2010 SEC; Liapis 2010 SEC; Masata 2012 SEC); although the results favoured the U‐type procedure, the result was not statistically significant. (Analysis 8.3.2).
Quality of life
MiniArc versus Ajust
Only one study was included in this analysis, which measured condition‐specific health (Martan 2012 ARC AJS). No significant differences between groups were reported and the confidence interval was wide (Analysis 8.4.1).
U‐type versus H‐type TVT‐Secur
Two trials were included in this analysis and measured condition‐specific health (Lee 2010 SEC; Masata 2012 SEC). No significant differences between groups were reported and the confidence interval was wide (Analysis 8.4.2).
Surgical outcome measures
Duration of operation
TVT‐Secur versus MiniArc
Two trials were included in this analysis (Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC). No significant differences between groups were reported (Analysis 8.5.1).
Ajust versus MiniArc
Only one study, which was methodologically robust, was included in this analysis (Palomba 2012 AJS ARC SEC); it showed no significant differences between groups (Analysis 8.5.2).
Operative blood loss
U‐type versus H‐type TVT‐Secur
Two trials (Lee 2010 SEC; Masata 2012 SEC) compared U‐ versus H‐type TVT‐Secur. The trialists did not provide standard deviations (SDs), so the data could not be analysed (Analysis 8.6.1).
Ajust versus MiniArc
One trial compared Ajust versus MiniArc (Palomba 2012 AJS ARC SEC); the data were too few to allow inferences of any differences between groups (Analysis 8.6.2).
TVT‐Secur versus MiniArc
One trial compared TVT‐Secur versus MiniArc (Palomba 2012 AJS ARC SEC); no significant differences between groups were noted in any of these comparisons (Analysis 8.6.3).
Adverse events
U‐type versus H‐type TVT‐Secur
Major vascular or visceral injury was reported in two trials (Lee 2010 SEC; Masata 2012 SEC), but no significant differences between groups were noted and the confidence interval was wide (Analysis 8.7.1).
Bladder or urethral perforation was reported in two trials (Lee 2010 SEC; Masata 2012 SEC); no differences between groups were noted and the confidence interval was very wide (Analysis 8.8.1).
Vaginal erosion was reported in two trials (Lee 2010 SEC; Masata 2012 SEC), which showed no significant differences between groups (Analysis 8.11.1).
Vaginal wall perforation was reported in one study that compared U‐ and H‐type TVT‐Secur (Lee 2010 SEC). No significant difference between either of the groups was noted, and the confidence interval was wide (Analysis 8.9.2).
Urinary retention and need for catheterisation were reported in one trial comparing U‐ and H‐type TVT‐Secur (Lee 2010 SEC). No significant differences between groups were observed in any of these comparisons (Analysis 8.10.2).
TVT‐Secur versus MiniArc
Bladder or urethral perforation was recorded in one study (Pardo 2010 SEC ARC). No significant differences were noted in either of the groups and the confidence interval was very wide (Analysis 8.8.2).
Vaginal wall perforation was reported in one study comparing TVT‐Secur and MiniArc (Oliveira 2011 ARC SEC). No significant differences were noted between either of the groups (Analysis 8.9.1).
Urinary retention and need for catheterisation were reported in three trials comparing TVT‐Secur versus MiniArc (Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC), No significant differences between groups were reported in any of these comparisons (Analysis 8.10.1).
Postoperative pain or discomfort was reported in one three‐arm study that compared TVT‐Secur versus MiniArc (Palomba 2012 AJS ARC SEC). No significant differences between groups were reported (Analysis 8.12.2).
Ajust versus MiniArc
Urinary retention and need for catheterisation were reported in one study (Palomba 2012 AJS ARC SEC). No significant differences between groups were reported (Analysis 8.10.3).
Postoperative pain or discomfort was reported in one three‐arm study (Palomba 2012 AJS ARC SEC); no significant differences between groups were reported in either comparison (Analysis 8.12.1).
De novo urgency
TVT‐Secur versus MiniArc
Three trials were included in the comparison (Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC) and showed no significant differences between groups (Analysis 8.13.1).
U‐type versus H‐type TVT‐Secur
Two trials were included in the comparison (Lee 2010 SEC; Liapis 2010 SEC) and showed no significant differences between groups (Analysis 8.13.2).
Ajust versus MiniArc
One study was included in this comparison (Palomba 2012 AJS ARC SEC) and showed no significant differences between groups (Analysis 8.13.3).
Repeat stress incontinence surgery
Two trials were included in this analysis, which compared U‐ and H‐type TVT‐Secur (Lee 2010 SEC; Masata 2012 SEC). About 5% of women required repeat incontinence surgery. The data were too few to allow inferences about any differences between groups (Analysis 8.14.1).
Need for any other additional or new surgical procedure to treat complications
Two trials were included in the analysis, which compared U‐ and H‐type TVT‐Secur (Lee 2010 SEC; Masata 2012 SEC). No differences between groups were reported and confidence intervals were wide (Analysis 8.15.1). One study compared TVT‐Secur versus Mini‐Arc (Pardo 2010 SEC ARC) but again showed no differences between groups (Analysis 8.15.2).
Subgroup analyses
No subgroup analyses were preplanned, but clinical factors such as symptoms of urinary stress incontinence, urodynamic stress incontinence, mixed urinary incontinence, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used or experience of the surgeon have been noted and might influence the outcome of surgery. This may be taken into account in future reviews.
Discussion
Summary of main results
We found no trials that compared single‐incision slings versus conservative treatment, colposuspension, laparoscopic surgery or traditional sub‐urethral slings. To supplement the main systematic review of effects, we sought economic evaluations which have compared single‐incision slings with any of the other main categories of surgical procedures listed under the 'Types of interventions' in the Methods section. A supplementary search in MEDLINE and Embase identified two economic evaluations which compared single‐incision slings with transobturator slings. We found no economic evaluation for the other types of interventions.The search strategies used are given in Appendix 2.
Single‐incision slings versus retropubic minimally invasive slings
Four of the five trials in this comparison compared TVT‐Secur against bottom‐up retropubic slings. The overall rate of cure of incontinence for single‐incision slings was worse (RR 2.08, 95% CI 1.04 to 4.14) (Analysis 6.1), as was the objective rate of cure of incontinence (RR 4.44, 95% CI 2.06 to 9.56). Women were more likely to have de novo urgency after single‐incision slings (RR 2.39, 95% CI 1.25 to 4.56) (Analysis 6.17) but evidence was insufficient to confirm a difference between the slings in terms of rates of other adverse events or need for repeat incontinence surgery. Single‐incision slings require less time to perform (mean difference ‐17.33 minutes, 95% CI ‐32.09 to ‐2.57) (Analysis 6.5), but the confidence interval for this comparison is quite wide and may not be clinically important.
No comparisons of singe‐incisions slings versus top‐down retropubic slings were performed, but the review authors believe this did not have an impact on the overall comparison.
A supplementary search carried out to identify economic evaluations for the brief economic commentary yielded no result.
Single‐incision slings versus obturator minimally invasive slings (subgrouped: medial‐to‐lateral 'inside out' approach and lateral‐to‐medial 'outside‐in' approach)
These results were subgrouped on the basis of whether the comparator was an inside‐out transobturator sling or an outside‐in transobturator sling.
Comparison with inside‐out transobturator slings
Generally TVT‐Secur was compared with inside‐out slings, and other types of mini‐slings were compared with outside‐in slings. Single‐incision slings resulted in higher incontinence rates compared with inside‐out transobturator slings (30% vs 11%, RR 2.55, 95% CI 1.93 to 3.36) (Analysis 7.1.1). Participants were also more likely to require repeat procedures to cure their persistent incontinence (RR 5.86, 95% CI 2.00 to 17.21) (Analysis 7.20.1). The adverse event profile was significantly worse, specifically, higher risk of vaginal mesh exposure, bladder/urethral erosion and operative blood loss. Participants were also more likely to require additional procedures to treat complications of the index surgery (RR 2.15, 95% CI 1.04 to 4.43) (Analysis 7.21.1). Postoperative pain was less common with single‐incision slings, and rates of long‐term pain or discomfort were marginally lower, but few trials reported these outcomes and the clinical significance of these differences is questionable. On the other hand, duration of the operation was marginally shorter for single‐incision slings.
However, most of these findings were due to the trials involving TVT‐Secur: Excluding the other trials showed that the high risk of incontinence was principally due to this device (RR 2.65, 95% CI 1.98 to 3.54). This sling has now been withdrawn from clinical use.
Overall these results show that TVT‐Secur is considerably inferior to inside‐out transobturator slings. Evidence of a difference in adverse event profiles for other single‐incision slings compared with inside‐out transobturator slings was insufficient to allow any further conclusions.
Economic evidence
The two cost‐effectiveness analyses compared single‐incision slings with inside‐out transobturator mid‐urethral slings.These adopted the perspective of the Spanish (Castañeda 2014) and UK (Boyers 2013) healthcare systems respectively. Boyers 2013 used clinical evidence from a prospective RCT (Mostafa 2012), while Castañeda 2014 used evidence from a retrospective observational study, to one‐year follow‐up in both cases. Both studies reported no statistically significant differences in the clinical outcomes: 6.7% difference, 95% Cl ‐6.6 to 20.0, P = 0.527 (Castañeda 2014); 5% difference, 95% Cl 0.38 to 2.26, P = 1.00 (Boyers 2013). Boyers 2013 reported no significant difference in peri‐operative complications (data and P value not reported). Castañeda 2014 also reported no statistically significant differences in intraoperative complication (P = 0.55). Boyers 2013 also reported the impact on health‐related quality of life, expressed as quality‐adjusted life years (QALYs). There was no significant difference in QALYs (mean difference ‐0.003, 95% Cl ‐0.008 to 0.002) (Boyers 2013). However, in the single‐incision sling arm, there were statistically significant improved postoperative pain scores up to four weeks with a pain score of zero compared with mid‐urethral slings with a total pain score of two (P < 0.001, 95% Cl 1.245 to 1.853). There was also a statistically significant one day earlier return to normal activities with single‐incision slings (P = 0.025, 95% Cl 6.1 to 9.4 days) (Boyers 2013), and fewer repeated urinary tract infections (Castañeda 2014). Single‐incision sling was less costly in both studies. The mean total direct cost of single‐incision sling in Boyers 2013 was GBP 1277 (2011 GBP), while that of transobturator slings was GBP 1462 (2011 GBP), with a 94% probability (95% Cl GBP ‐316.99 to GBP 32.17) of being cost‐saving compared to transobturator slings, irrespective of whether single‐incision sling was performed under local or general anaesthesia. In Castañeda 2014, the average cost of single‐incision sling (2013 euros) was EUR 2059 (95% Cl EUR 1914 to 2285) while transobturator slings were EUR 2821(95% Cl EUR 2661 to 2997), with a 100% probability of single‐incision sling being cost‐saving. Castañeda 2014 suggested that the mini‐sling might be more cost‐effective compared with transobturator slings, based on the relative effectiveness of both intervention and the lower cost associated with a single‐incision sling. Boyers 2013 also concluded that the single‐incision sling procedure, especially when performed under local anaesthesia, was likely to be more cost‐effective than transobturator slings over a one‐year follow‐up, but said that a longer follow‐up was required.
Comparison with outside‐in transobturator slings
Too little information was provided on other single‐incision slings for a reliable comparison of efficacy and adverse event profiles versus outside‐in transobturator slings. However, the duration of surgery and risks of postoperative and chronic pain were less with single‐incision slings. Comparisons between other single‐incision slings and inside‐out transobturator slings were too few to allow further conclusions.
Comparison with any transobturator sling
The combined results show that transobturator slings have lower incontinence rates than single‐incision slings overall but with significant heterogeneity in the comparisons due to differences in the trials. Women who have transobturator slings have a lower risk of vaginal erosion (RR 2.59, 95% CI 1.21 to 5.56) (Analysis 7.15) and a lesser chance of requiring repeat incontinence surgery (RR 3.09, 95% CI 1.48 to 6.49) (Analysis 7.20) or repeat surgery to treat complications (RR 2.03, 95% CI 1.09 to 3.78) (Analysis 7.21). Risks of postoperative pain and long‐term pain are slightly higher with transobturator slings. Evidence was insufficient to reveal any differences in the rates of other adverse events.
Sensitivity analysis excluding TVT‐Secur trials
Not enough evidence was obtained in a sensitivity analyses comparing all other single‐incision slings (excluding TVT‐Secur) versus transobturator slings to allow any conclusions regarding continence rates or most adverse events. Differences in the rates of postoperative pain (favouring single‐incisions slings; RR 0.23, 95% CI 0.14 to 0.38) (Analysis 7.17) and long‐term pain (favouring single incision slings; RR 0.15, 95% CI 0.03 to 0.67) (Analysis 7.18) were noted, but the magnitude of these differences was small. Single‐incision slings remained quicker to perform in this analysis (RR ‐1.98, 95% CI ‐2.68 to ‐1.2), but again the margin of difference (less than two minutes) is too small to be clinically important.
One single‐incision sling versus another
Seven trials compared one type of single‐incision sling versus another, but too few data were obtained for the review authors to infer any significant differences between the slings in any of the comparisons made. It is interesting that direct comparison of TVT‐Secur versus other single‐incision slings showed no significant difference, but it must be noted that very few trials made this comparison.
A supplementary search carried out to identify economic evaluations for the brief economic commentary yielded no result.
Overall completeness and applicability of evidence
We identified no studies that compared single‐incision slings versus conservative management, laparoscopic surgery or open colposuspension. For economic evidence, we did not subject the two economic evaluations to critical appraisal, and we do not attempt to draw any firm or general conclusions about the relative costs or efficiency of single‐incision slings in treatment of SUI. Taking into account the limitation of the need for a longer time horizon to explore the downstream costs associated with these interventions, the economic evidence from both studies were consistent, and suggested that single‐incision slings were likely to be cost‐effective up to one‐year follow‐up when compared with transobturator mid‐urethral slings.. Also,given that retropubic and transobturator mid‐urethral slings have become the gold standard treatment for stress urinary incontinence in women, it is reasonable for single‐incision slings to be routinely compared with these mid‐urethral slings in clinical trials.
Differences in fixation systems
The review authors believe it is important to note that although single‐incision slings have been clubbed together as a single group, a significant difference in the fixation systems between some of these slings has been noted. Whereas some simply rely on tissue in‐growth into the porous mesh to hold them in place, others use anchors or other fixation mechanisms to anchor them to tissue. These differences make comparisons difficult. TVT‐Secur is the single‐incision sling that has been studied most widely, and the evidence clearly shows it to be inferior to both retropubic slings and inside‐out transobturator slings in achieving cure of stress incontinence while leading to higher risk of adverse events. It does not have a fixation system, and this may have contributed to its poor performance. Undoubtedly the results of these trials have contributed to withdrawal of this particular sling from the market.
The data are less consistent for other single‐incision slings. Fewer trials of variable quality make interpretation difficult, and again, grouping these slings together is not always intuitive because of the different fixation mechanisms involved. At present evidence is insufficient to suggest that these slings are inferior to outside‐in transobturator slings, and comparisons versus inside‐out transobturator slings are too few to allow any meaningful conclusions. However in the current clinical climate, where implantable meshes and tapes are under intense scrutiny, evidence suggests that these slings must be used with caution.
Trials including TVT‐Secur
The inclusion of such a large number of trials including TVT‐Secur as a comparator inevitably has had a major influence on the overall results. Given that this sling has subsequently been removed from the market, it could be questioned why it was included in this review at all. The review authors came to the unanimous conclusion that it should be included in the first iteration of this review, so that level 1 evidence is available to demonstrate its lack of efficacy. Currently lack of available evidence on other single‐incision slings prevents any meaningful conclusions. However, we are aware of a number of ongoing trials and therefore plan to update the review towards the end of 2014, at which stage all TVT‐Secur data will be excluded.
Choice of outcomes
Objective cure is relatively easily assessed, and various methods, such as cough stress tests, pad tests and urodynamic assessment, are used to measure it. But subjective cure can be more difficult to assess and is greatly dependant on the patient's perceptions of success. We have defined subjective cure or patient‐reported success as the most important outcome for this type of surgery, and indeed many trials use subjective success or cure rate as the primary outcome measure. It is therefore critical to establish before surgery what a patient's expectations of success are, so that postoperative evaluations can be based on these definitions. Without this, there is a real danger of introducing significant clinical heterogeneity into a meta‐analysis of these outcomes. However, the included trials differed markedly in their definitions of incontinence and cure, and we have used an inclusive approach to interpretation to maximise the available data.
Quality of the evidence
As stated in the Risk of bias in included studies section, the quality of included trials varied widely. Thirty‐two trials (19 fully published papers, one thesis and 12 abstracts) were included in this review, including overall 3427 women.
The trials included in the comparison of single‐incision slings versus retropubic mid‐urethral slings were of moderate and consistent quality, with no major differences apart from inclusion of some women with concomitant prolapse in up to three of the trials. Results are also consistent across the trials, and hence the results of the meta‐analysis can be considered robust.
Trials comparing single‐incision slings versus inside‐out transobturator slings were more heterogenous in terms of methodology and consistency of results. Fourteen trials (eight fully published papers, five abstracts and one thesis) comprising a total of 1542 women were included. Despite these general inconsistencies, efficacy outcomes were consistently better for inside‐out transobturator slings across the trials, and results of the pooled meta‐analysis give a statistically significant result, even though results in some individual trials may not have reached significance.
Seven trials comprising a total of 658 women compared single‐incision slings versus outside‐in transobturator slings; only one was a fully published paper, and the rest were abstracts. This made evaluation of methodology difficult because of the limited information provided in some of the abstracts. Efficacy outcomes were not statistically significant, but it must be noted that this comparison is a composite of different types of single‐incision slings (MiniArc, CureMesh, Ajust, TFS and Contasure Needleless). The difference in fixation systems between these slings makes the value of a pooled analysis debatable. However none of the individual trials reported a statistically significant difference in efficacy. Duration of the operation was found to be significantly shorter for single‐incision slings, but for the same reasons as were stated for the previous comparison, a high degree of statistical and clinical heterogeneity is present here.
Nine trials comprising a total of 1007 women (five fully published papers and four abstracts) compared one type of single‐incision sling versus another. Methdological quality was variable, and comparisons were made mainly between three different types of single‐incision slings (MiniArc vs TVT‐Secur, U‐ vs H‐type TVT‐Secur and MiniArc vs Ajust). None of the overall comparisons reached statistical significance; neither did any of the individual comparisons in individual trials. Therefore the only possible conclusion is that currently not enough evidence is available to suggest whether any differences between single‐incision slings can be found based on direct comparisons.
Potential biases in the review process
Data were independently checked by three review authors. No restrictions were placed on language of included papers, and two full papers are included that were written in languages other than English (one German, one Czech). These papers included English abstracts in the text and data were extracted from these as far as possible. However, translations could not be obtained; therefore some data may not have been identified.
Ranges of follow‐up varied considerably between trials, and sometimes trials with significantly different mean durations of follow‐up were included in the same comparison. However, when this was the case, sensitivity analyses could be performed to assess whether this could represent a source of bias.
The review authors decided not to include selective outcome reporting for assessment of risk of bias, as considerable variation was found in the availability of this information. This might introduce a potential source of bias.
Agreements and disagreements with other studies or reviews
Other relevant systematic reviews include Abdel‐Fattah 2011; Jeffery 2010; Tommaselli 2011; and Walsh 2011.
Abdel‐Fattah 2011 (literature search up to January 2011) included nine studies of 758 women (six studies of TVT‐Secur) and concluded that single‐incision slings were associated with inferior patient‐reported and objective cure rates on short‐term follow‐up, as well as higher reoperation rates for SUI, while having a significantly shorter operative time, lower day one pain scores and less postoperative groin pain.
Jeffery 2010 included 57 studies, of which only 32 provided information about the type of study conducted (three RCTs, nine retrospective studies and 20 prospective studies). Overall cure rates were reported to range between 70% and 81%, with less than 1% risk of bladder injury and groin or hip pain.
Tommaselli 2011 was a systematic review similar in design to Jeffery 2010 but limited to studies involving TVT‐Secur. It included 54 studies (35 prospective studies, seven RCTs and 12 retrospective studies) and concluded that the objective cure rate for TVT‐Secur did not reach 80% (significantly lower than that of standard mid‐urethral slings), while subjective cure rates were somewhat higher. Complication rates were lower than 10%, and complications were limited to vaginal erosion, bladder injury, de novo urgency and reoperation for SUI.
Walsh 2011 reported 12‐month outcomes after TVT‐Secur in 10 studies including 1178 women and reported objective and subjective cure rates of 76%, a 10% incidence of de novo urgency and 2.4% of mesh exposure. Rates of other complications were low.
Overall the results of these reviews are in keeping with ours, bearing in mind the lower number of randomised studies included in the above reviews. The conclusion of poor performance of TVT‐Secur has been reiterated in this review, which only strengthens this conclusion.
It is generally thought that there is no difference in efficacy between retropubic and transobturator slings for cure of stress incontinence (Nambiar 2012; Ogah 2009), but a difference in the adverse event profile has been reported (Nambiar 2012). It is therefore still relevant to compare single‐incision slings versus both types of synthetic mid‐urethral slings. However descriptions of the types of slings being studied, along with descriptions of the fixation systems and clear documentation of the common adverse events, are important.
An adverse event that is commonly used to define differences between all types of slings is the occurrence of groin/thigh pain. It should be clearly documented in trial reports whether this is postoperative pain (short‐term) or long‐term chronic pain. By convention, short‐term pain is generally taken to be any pain lasting up to six to eight weeks postoperatively, and long‐term or chronic pain lasts beyond six months. Some effort should also be made to document the nature of the pain to try to identify those patients whose pain could reasonably have been caused by sling insertion.
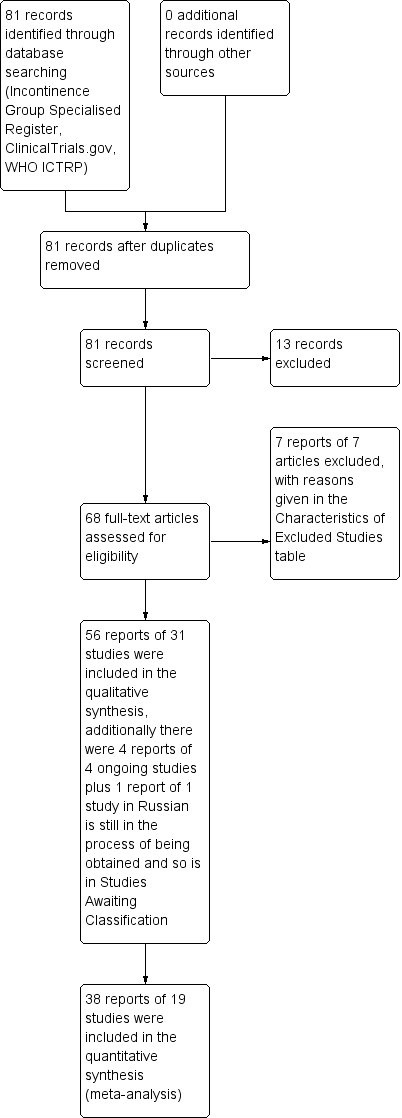
PRISMA study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
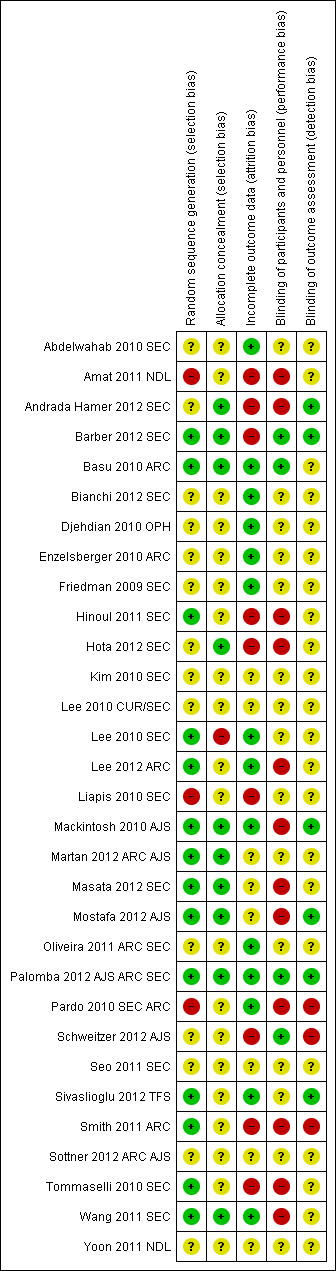
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
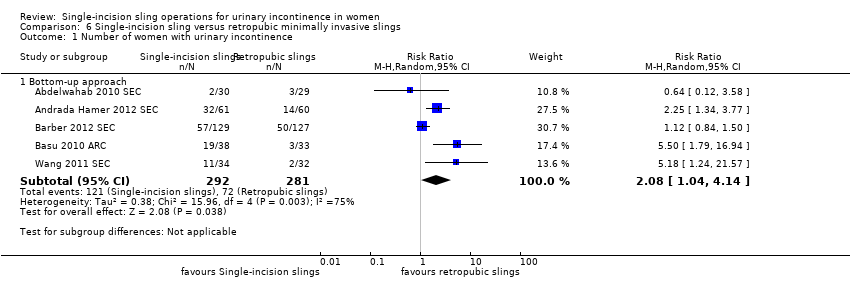
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 1 Number of women with urinary incontinence.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 2 Number of women with no improvement.
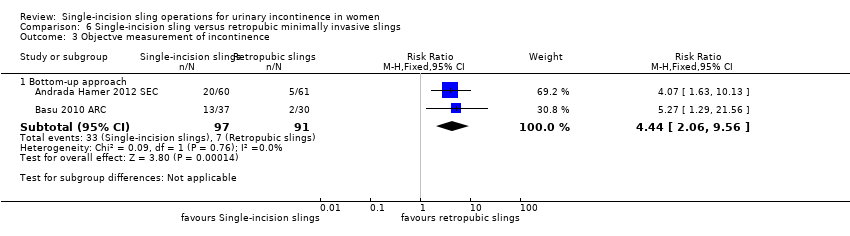
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 3 Objectve measurement of incontinence.
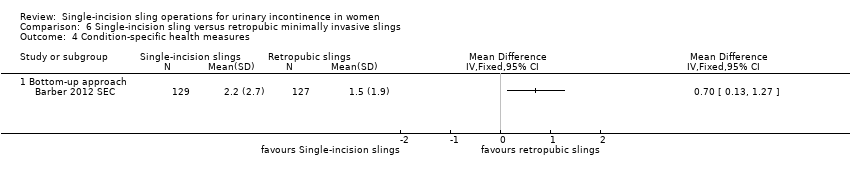
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 4 Condition‐specific health measures.
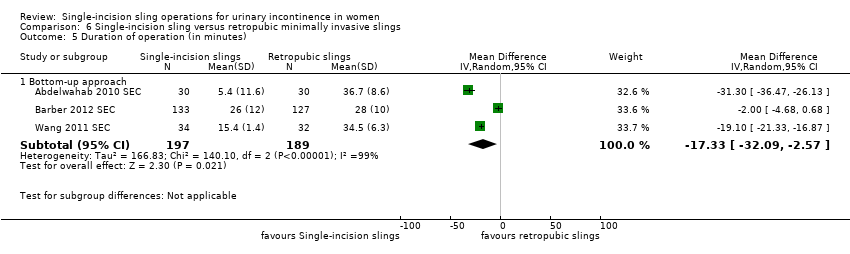
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 5 Duration of operation (in minutes).
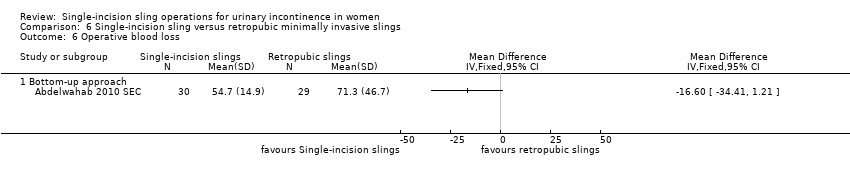
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 6 Operative blood loss.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 7 Length of in‐patient stay.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 8 Major vascular or visceral injury.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 9 Vaginal wall perforation.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 10 Bladder or urethral perforation.
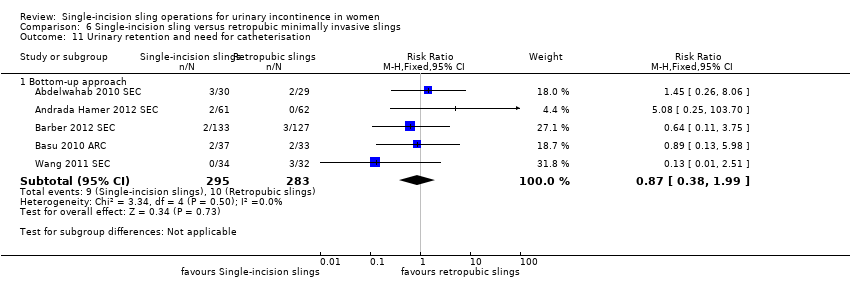
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 11 Urinary retention and need for catheterisation.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 12 Infection related to use of synthetic mesh.
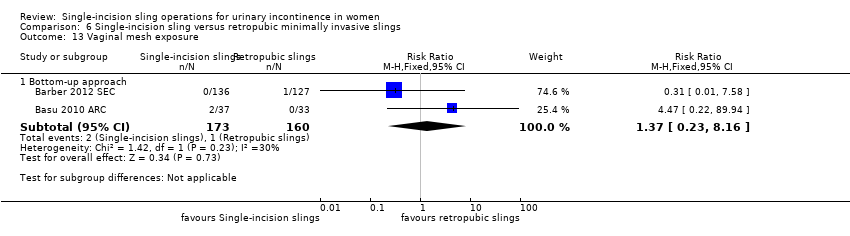
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 13 Vaginal mesh exposure.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 14 Mesh extrusion into the bladder or urethra.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 15 Long‐term pain or discomfort.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 16 Dyspareunia.
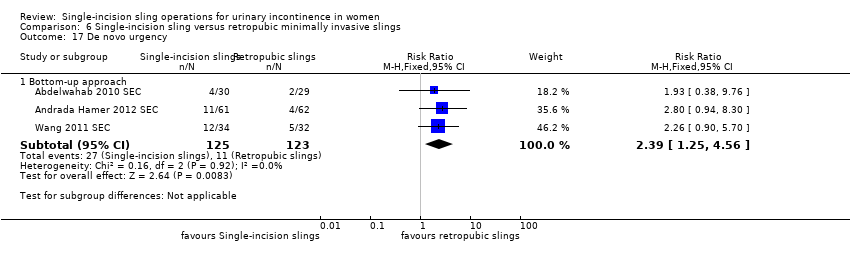
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 17 De novo urgency.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 18 New‐onset detrusor overactivity.

Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 19 Repeat stress incontinence surgery.
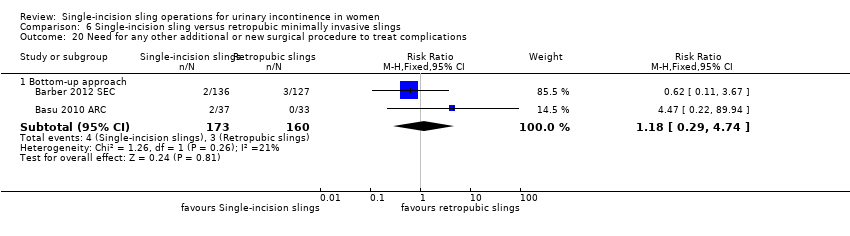
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 20 Need for any other additional or new surgical procedure to treat complications.
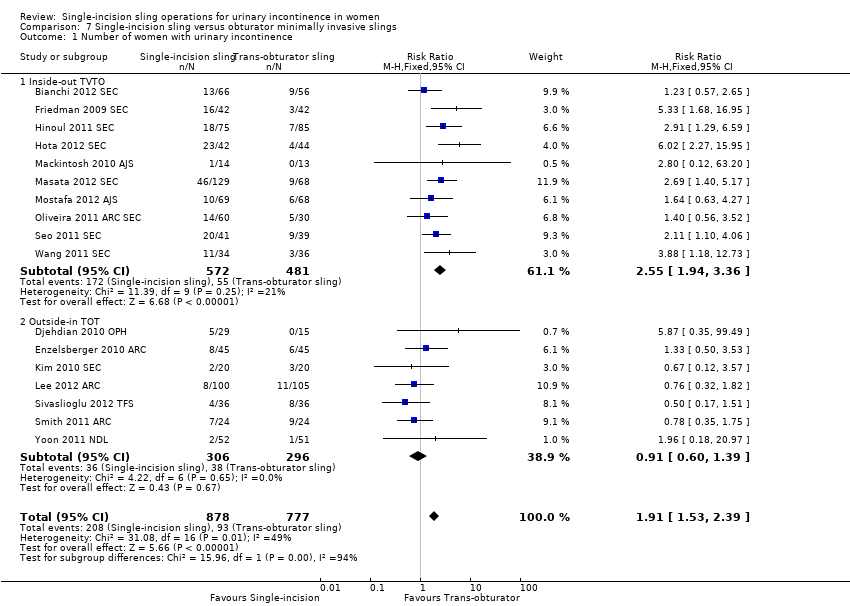
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 1 Number of women with urinary incontinence.
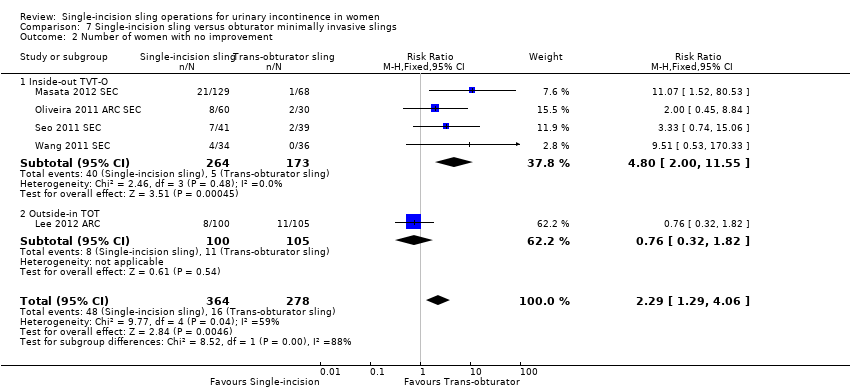
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 2 Number of women with no improvement.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 3 Objective measurement of incontinence.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 4 Incontinence episodes.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 5 Pad test (weights).
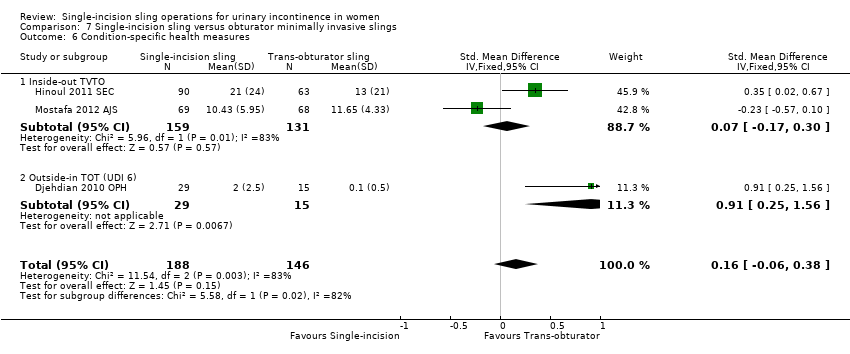
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 6 Condition‐specific health measures.
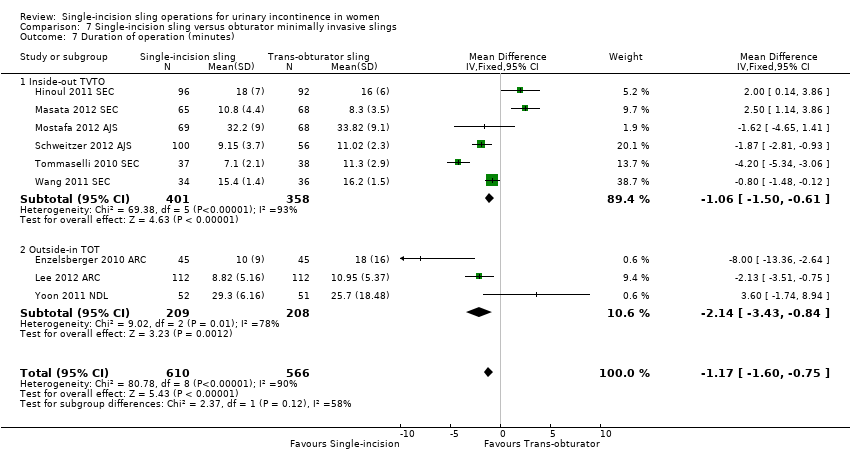
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 7 Duration of operation (minutes).

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 8 Operative blood loss (mL).
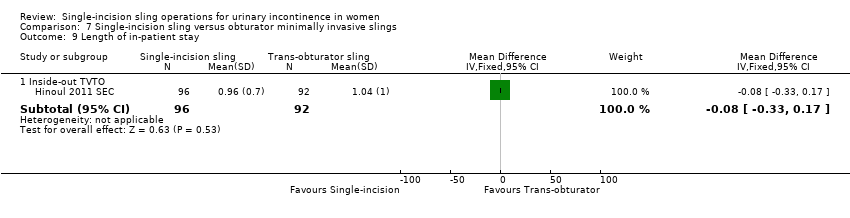
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 9 Length of in‐patient stay.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 10 Major vascular or visceral injury.
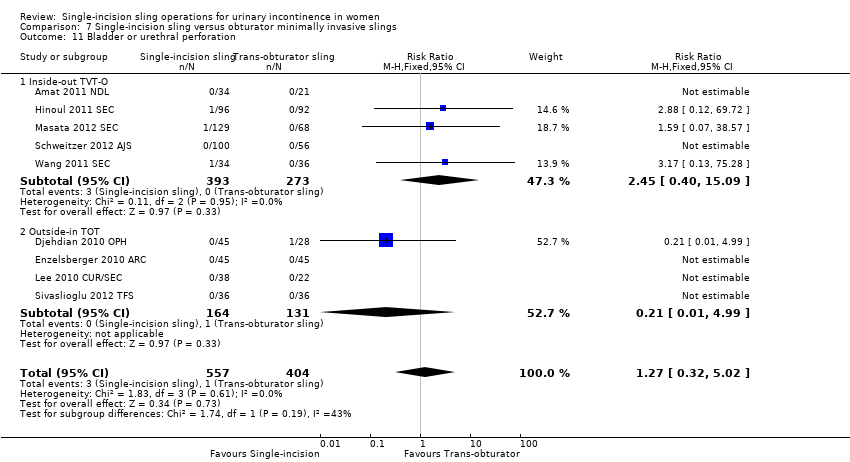
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 11 Bladder or urethral perforation.
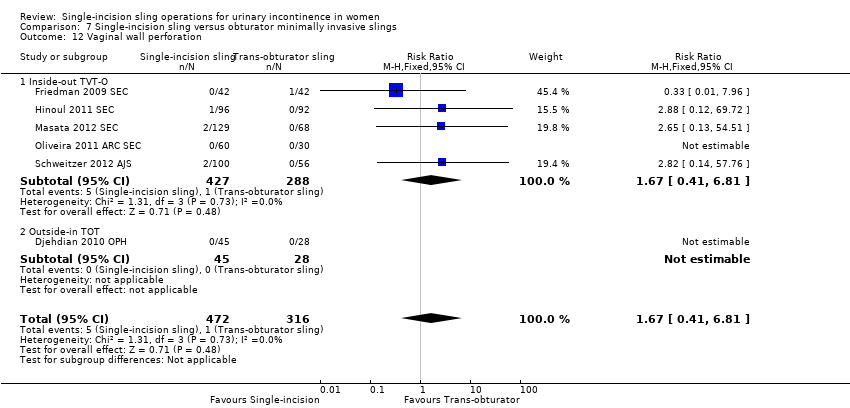
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 12 Vaginal wall perforation.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 13 Urinary retention and need for catheterisation.
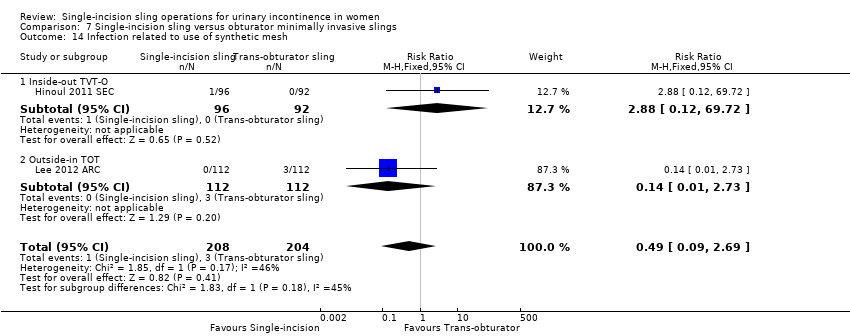
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 14 Infection related to use of synthetic mesh.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 15 Vaginal mesh exposure.
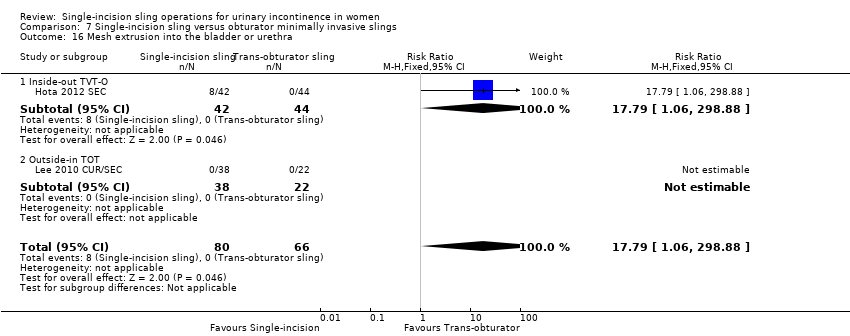
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 16 Mesh extrusion into the bladder or urethra.
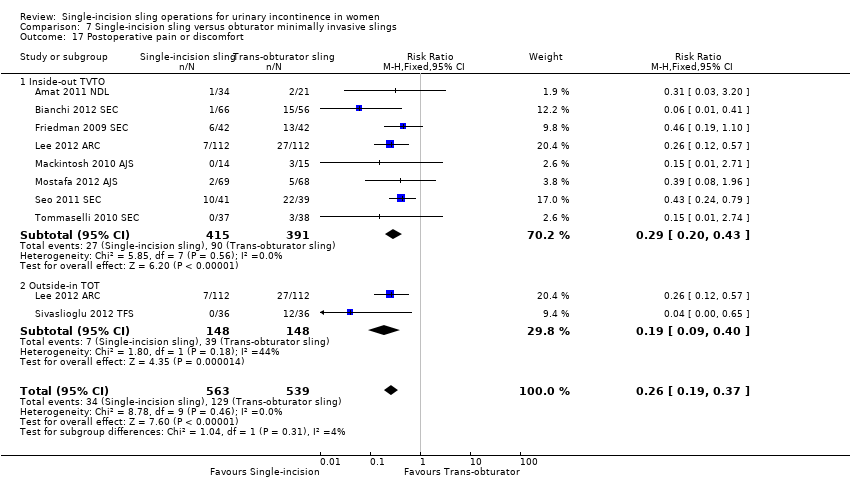
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 17 Postoperative pain or discomfort.
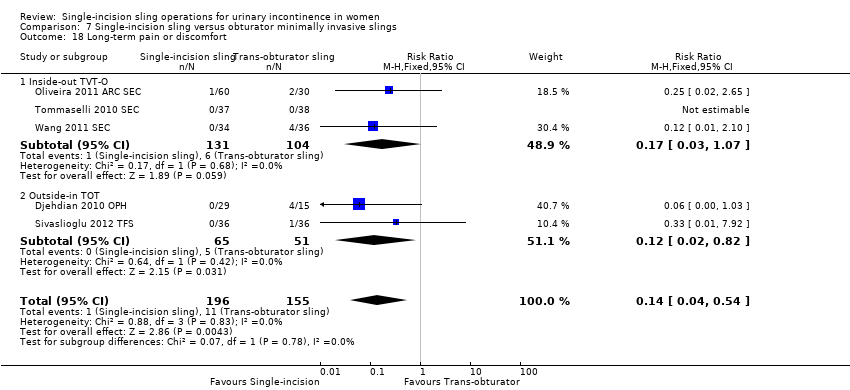
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 18 Long‐term pain or discomfort.
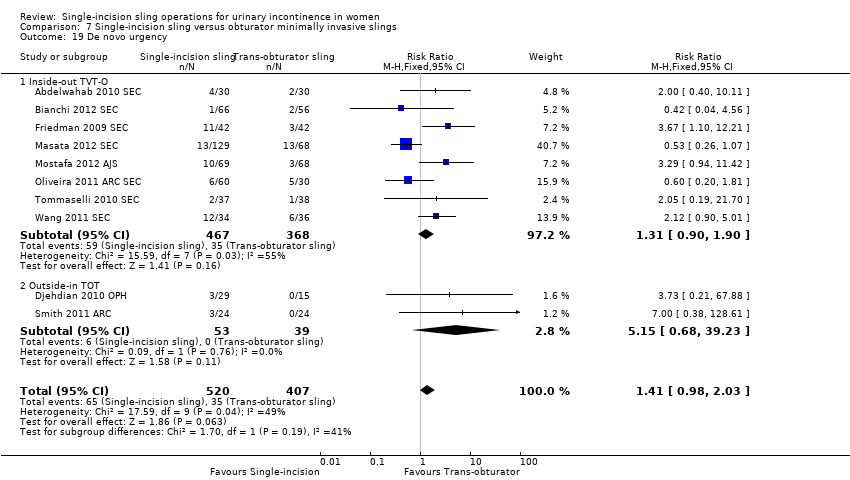
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 19 De novo urgency.

Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 20 Repeat stress incontinence surgery.
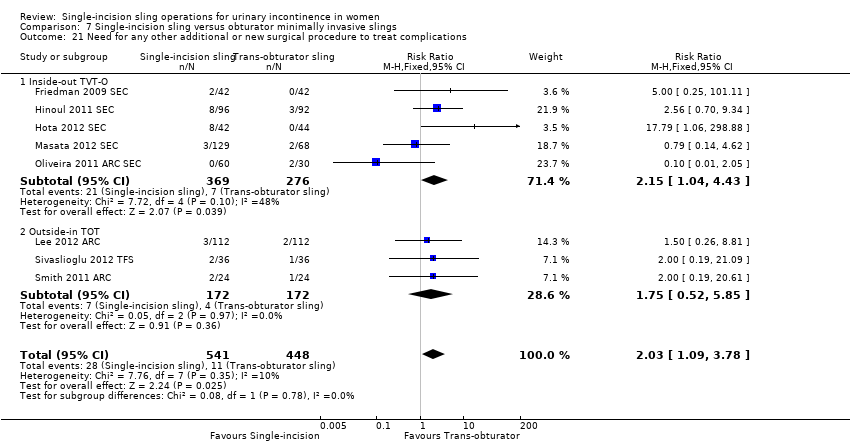
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 21 Need for any other additional or new surgical procedure to treat complications.

Comparison 8 One single‐incision sling versus another, Outcome 1 Number of women with urinary incontinence.
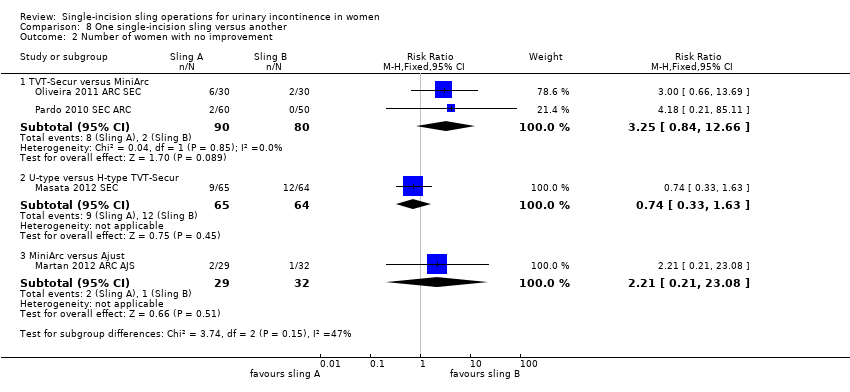
Comparison 8 One single‐incision sling versus another, Outcome 2 Number of women with no improvement.
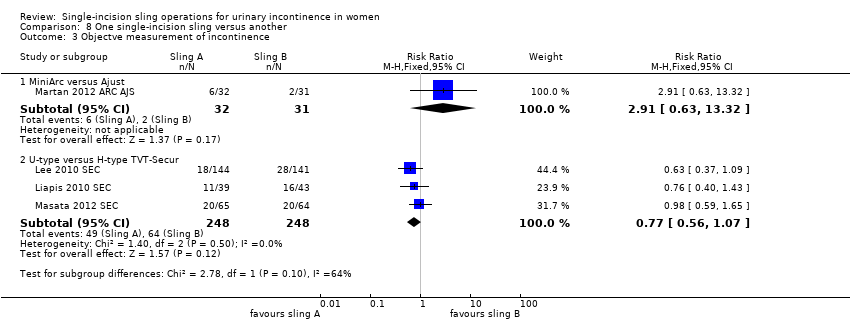
Comparison 8 One single‐incision sling versus another, Outcome 3 Objectve measurement of incontinence.
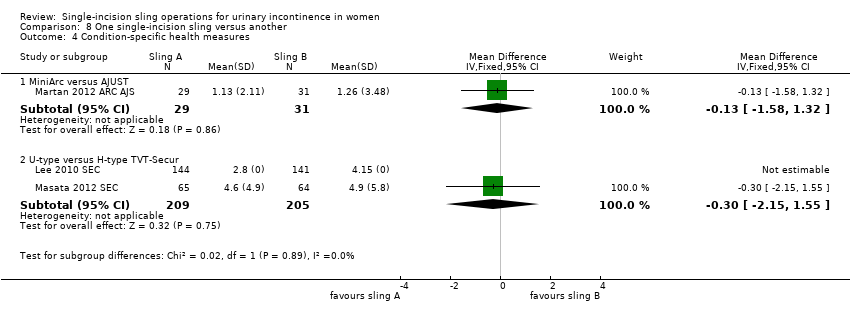
Comparison 8 One single‐incision sling versus another, Outcome 4 Condition‐specific health measures.

Comparison 8 One single‐incision sling versus another, Outcome 5 Duration of operation (minutes).
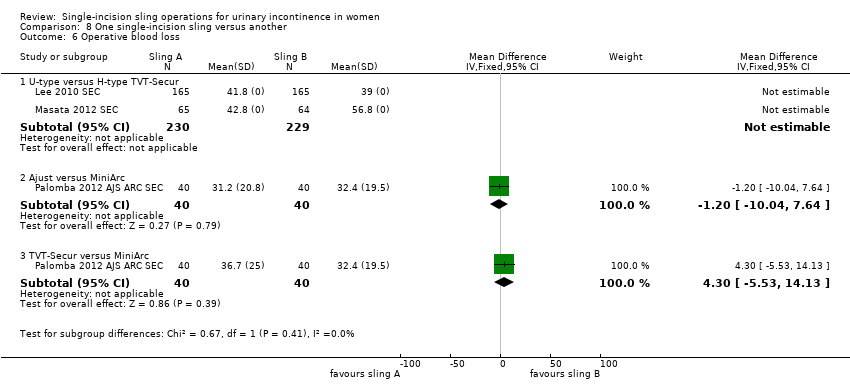
Comparison 8 One single‐incision sling versus another, Outcome 6 Operative blood loss.

Comparison 8 One single‐incision sling versus another, Outcome 7 Major vascular or visceral injury.

Comparison 8 One single‐incision sling versus another, Outcome 8 Bladder or urethral perforation.

Comparison 8 One single‐incision sling versus another, Outcome 9 Vaginal wall perforation.

Comparison 8 One single‐incision sling versus another, Outcome 10 Urinary retention and need for catheterisation.
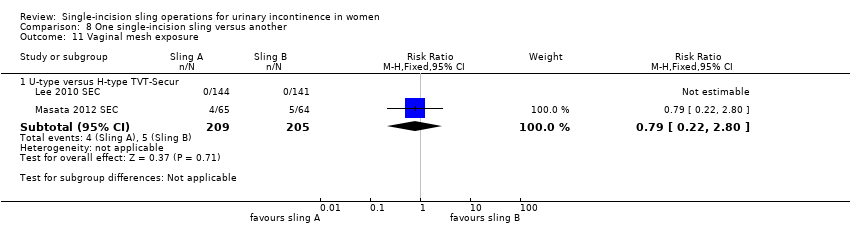
Comparison 8 One single‐incision sling versus another, Outcome 11 Vaginal mesh exposure.

Comparison 8 One single‐incision sling versus another, Outcome 12 Postoperative pain or discomfort.
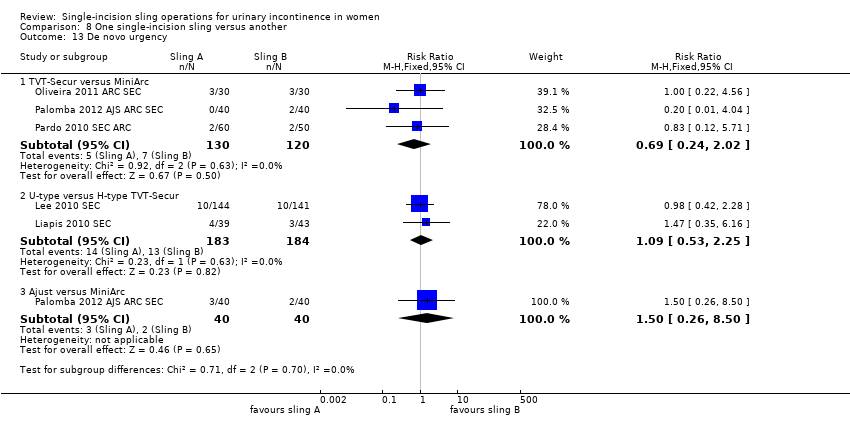
Comparison 8 One single‐incision sling versus another, Outcome 13 De novo urgency.
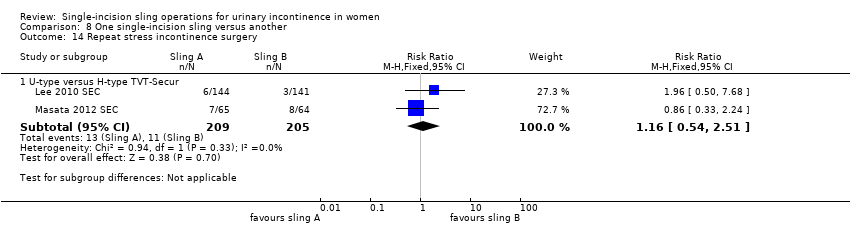
Comparison 8 One single‐incision sling versus another, Outcome 14 Repeat stress incontinence surgery.

Comparison 8 One single‐incision sling versus another, Outcome 15 Need for any other additional or new surgical procedure to treat complications.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Bottom‐up approach | 5 | 573 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [1.04, 4.14] |
| 2 Number of women with no improvement Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Bottom‐up approach | 3 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.55, 3.46] |
| 3 Objectve measurement of incontinence Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Bottom‐up approach | 2 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.44 [2.06, 9.56] |
| 4 Condition‐specific health measures Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Duration of operation (in minutes) Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Bottom‐up approach | 3 | 386 | Mean Difference (IV, Random, 95% CI) | ‐17.33 [‐32.09, ‐2.57] |
| 6 Operative blood loss Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Length of in‐patient stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Major vascular or visceral injury Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Bottom‐up approach | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Vaginal wall perforation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Bottom‐up approach | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Bladder or urethral perforation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Bottom‐up approach | 4 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.15, 1.38] |
| 11 Urinary retention and need for catheterisation Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Bottom‐up approach | 5 | 578 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.38, 1.99] |
| 12 Infection related to use of synthetic mesh Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Bottom‐up approach | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.22, 17.89] |
| 13 Vaginal mesh exposure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.23, 8.16] |
| 14 Mesh extrusion into the bladder or urethra Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Bottom‐up approach | 3 | 445 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.19, 3.01] |
| 15 Long‐term pain or discomfort Show forest plot | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Bottom‐up approach | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Dyspareunia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Bottom‐up approach | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.9 [0.32, 26.30] |
| 17 De novo urgency Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Bottom‐up approach | 3 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [1.25, 4.56] |
| 18 New‐onset detrusor overactivity Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Bottom‐up approach | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.13, 5.98] |
| 19 Repeat stress incontinence surgery Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.34 [0.79, 6.92] |
| 20 Need for any other additional or new surgical procedure to treat complications Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.29, 4.74] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 17 | 1655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.91 [1.53, 2.39] |
| 1.1 Inside‐out TVTO | 10 | 1053 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.55 [1.94, 3.36] |
| 1.2 Outside‐in TOT | 7 | 602 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.60, 1.39] |
| 2 Number of women with no improvement Show forest plot | 5 | 642 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [1.29, 4.06] |
| 2.1 Inside‐out TVT‐O | 4 | 437 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.80 [2.00, 11.55] |
| 2.2 Outside‐in TOT | 1 | 205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.32, 1.82] |
| 3 Objective measurement of incontinence Show forest plot | 12 | 1198 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [1.49, 2.36] |
| 3.1 Inside‐out TVT‐O | 7 | 804 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [2.00, 4.25] |
| 3.2 Outside‐in TOT | 5 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.90, 1.55] |
| 4 Incontinence episodes Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Outside‐in TOT | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pad test (weights) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Outside‐in TOT | 2 | 268 | Mean Difference (IV, Fixed, 95% CI) | ‐1.64 [‐6.24, 2.96] |
| 6 Condition‐specific health measures Show forest plot | 3 | 334 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐0.06, 0.38] |
| 6.1 Inside‐out TVTO | 2 | 290 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.17, 0.30] |
| 6.2 Outside‐in TOT (UDI 6) | 1 | 44 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.91 [0.25, 1.56] |
| 7 Duration of operation (minutes) Show forest plot | 9 | 1176 | Mean Difference (IV, Fixed, 95% CI) | ‐1.17 [‐1.60, ‐0.75] |
| 7.1 Inside‐out TVTO | 6 | 759 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.50, ‐0.61] |
| 7.2 Outside‐in TOT | 3 | 417 | Mean Difference (IV, Fixed, 95% CI) | ‐2.14 [‐3.43, ‐0.84] |
| 8 Operative blood loss (mL) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Inside‐out TVTO | 2 | 320 | Mean Difference (IV, Fixed, 95% CI) | 18.79 [3.70, 33.88] |
| 9 Length of in‐patient stay Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Inside‐out TVTO | 1 | 188 | Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.33, 0.17] |
| 10 Major vascular or visceral injury Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Inside‐out TVT‐O | 3 | 460 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.28, 6.89] |
| 11 Bladder or urethral perforation Show forest plot | 9 | 961 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.32, 5.02] |
| 11.1 Inside‐out TVT‐O | 5 | 666 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.40, 15.09] |
| 11.2 Outside‐in TOT | 4 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.99] |
| 12 Vaginal wall perforation Show forest plot | 6 | 788 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| 12.1 Inside‐out TVT‐O | 5 | 715 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| 12.2 Outside‐in TOT | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Urinary retention and need for catheterisation Show forest plot | 15 | 1477 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.28, 1.15] |
| 13.1 Inside‐out TVTO | 10 | 996 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.34, 1.52] |
| 13.2 Outside‐in TOT | 5 | 481 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.08, 3.44] |
| 14 Infection related to use of synthetic mesh Show forest plot | 2 | 412 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.09, 2.69] |
| 14.1 Inside‐out TVT‐O | 1 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.88 [0.12, 69.72] |
| 14.2 Outside‐in TOT | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.73] |
| 15 Vaginal mesh exposure Show forest plot | 9 | 819 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.59 [1.21, 5.56] |
| 15.1 Inside‐out TVT‐O | 5 | 562 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.75 [1.42, 9.86] |
| 15.2 Outside‐in TOT | 4 | 257 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.27, 4.28] |
| 16 Mesh extrusion into the bladder or urethra Show forest plot | 2 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| 16.1 Inside‐out TVT‐O | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| 16.2 Outside‐in TOT | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Postoperative pain or discomfort Show forest plot | 9 | 1102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.19, 0.37] |
| 17.1 Inside‐out TVTO | 8 | 806 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.20, 0.43] |
| 17.2 Outside‐in TOT | 2 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.40] |
| 18 Long‐term pain or discomfort Show forest plot | 5 | 351 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.04, 0.54] |
| 18.1 Inside‐out TVT‐O | 3 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.03, 1.07] |
| 18.2 Outside‐in TOT | 2 | 116 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.82] |
| 19 De novo urgency Show forest plot | 10 | 927 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.98, 2.03] |
| 19.1 Inside‐out TVT‐O | 8 | 835 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.90, 1.90] |
| 19.2 Outside‐in TOT | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.15 [0.68, 39.23] |
| 20 Repeat stress incontinence surgery Show forest plot | 6 | 764 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.09 [1.48, 6.49] |
| 20.1 Inside‐out TVT‐O | 3 | 420 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.86 [2.00, 17.21] |
| 20.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.18] |
| 21 Need for any other additional or new surgical procedure to treat complications Show forest plot | 8 | 989 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [1.09, 3.78] |
| 21.1 Inside‐out TVT‐O | 5 | 645 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.15 [1.04, 4.43] |
| 21.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.52, 5.85] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Number of women with urinary incontinence Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 TVT‐SECUR versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.95, 1.29] |
| 1.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.78, 1.40] |
| 1.3 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 2 Number of women with no improvement Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 TVT‐Secur versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.84, 12.66] |
| 2.2 U‐type versus H‐type TVT‐Secur | 1 | 129 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.33, 1.63] |
| 2.3 MiniArc versus Ajust | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.21, 23.08] |
| 3 Objectve measurement of incontinence Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 3.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.07] |
| 4 Condition‐specific health measures Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 MiniArc versus AJUST | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐1.58, 1.32] |
| 4.2 U‐type versus H‐type TVT‐Secur | 2 | 414 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐2.15, 1.55] |
| 5 Duration of operation (minutes) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 TVT‐Secur versus MiniArc | 2 | 190 | Mean Difference (IV, Fixed, 95% CI) | 1.70 [‐4.11, 7.51] |
| 5.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐4.67, 7.07] |
| 6 Operative blood loss Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐10.04, 7.64] |
| 6.3 TVT‐Secur versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 4.30 [‐5.53, 14.13] |
| 7 Major vascular or visceral injury Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.19] |
| 8 Bladder or urethral perforation Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 8.2 TVT‐Secur versus MiniArc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.18 [0.21, 85.11] |
| 9 Vaginal wall perforation Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 TVT‐S versus MiniArc | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 U‐type versus H‐type TVT‐Secur | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Urinary retention and need for catheterisation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.47, 8.95] |
| 10.2 U‐type versus H‐type TVT‐Secur | 1 | 330 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.11, 3.94] |
| 10.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 100.97] |
| 11 Vaginal mesh exposure Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.22, 2.80] |
| 12 Postoperative pain or discomfort Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Ajust versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 TVT‐Secur versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 De novo urgency Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.24, 2.02] |
| 13.2 U‐type versus H‐type TVT‐Secur | 2 | 367 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.53, 2.25] |
| 13.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.50] |
| 14 Repeat stress incontinence surgery Show forest plot | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.54, 2.51] |
| 15 Need for any other additional or new surgical procedure to treat complications Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.04, 1.61] |
| 15.2 TVT‐Secur vs Mini‐Arc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.16, 17.85] |

