Środki motywujące w profilaktyce palenia tytoniu wśród dzieci i młodzieży
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Controlled cluster trial, no randomization reported. Public schools assigned to intervention in 2 communities, with the third community acting as control | |
| Participants | Country: USA (3 communities in Iowa). 7th graders in participating schools. 1187 students completed baseline surveys. Authors reported majority were white (> 90%), working or middle class students | |
| Interventions | 2 intervention communities received an education programme (6 sessions) plus competitions. 2 competitions ran concurrently: 1 which aimed to improve knowledge and the other to reward non‐smoking. Competition 1: A t‐shirt with the project logo was given to all students in the class at each school with most improved knowledge Competition 2. Non‐smoking competition between 7th graders in the 2 intervention communities. Students in the community with lower smoking rates at end of the project rewarded with a movie pass and voucher for free ice‐cream Control community received only education programme | |
| Outcomes | Baseline (Fall 1984) – survey of tobacco use (self‐reported description using 5 categories, frequency measured using 5 categories, quantity measured using 6 categories), smoking beliefs, subjective norms, knowledge, saliva TCN
18‐month follow‐up (Spring 1986) – 18‐month follow‐up survey of tobacco use (self‐reported description measured using 5 categories, smoking frequency using 10 categories (never smoked (1) to smoke more than half a packet a day (10)), smoking beliefs, subjective norms, saliva TCN
TCN results only used to justify the use of self‐report except at baseline when 39 self‐reported never‐smokers were reclassified as occasional smokers | |
| Notes | Theoretical basis: Intervention based on Fishbein & Ajzen’s theory of reasoned action which posits that preventing behaviour depends on altering relevant beliefs and norms | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized. No data on breakdown of demographics (age, sex, SES) provided between intervention and control groups. Authors reported no significant pre‐intervention differences found between the 2 groups on self‐report/biochemical assessment of smoking status, knowledge, beliefs and smoking intentions |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding of participants and personnel (performance bias) | Low risk | Not reported but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) | High risk | Not reported. Students’ self‐reporting of smoking status may have been influenced by knowledge that they were in a competition for prizes |
| Incomplete outcome data (attrition bias) | Low risk | 1187 participants surveyed at baseline (Fall 1984), 964 followed up 18 months later (81%). More participants lost in control (22.6%) than intervention (16.7%) group. The authors reported “No significant interaction was found for 3 of the 4 pre‐intervention measures of smoking, we concluded that the validity of the study was not jeopardized by differential attrition.” |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to make a judgement on prespecified outcomes |
| Methods | Randomized controlled cluster trial | |
| Participants | Country: Netherlands. 26 schools providing lower secondary education. Schools recruited through community health services. 14 of 54 health services provided names of schools. 26 schools were recruited but unclear about number of schools approached
'First grade students' from 154 classes participated (mean age 13 years). 1444 in intervention, 1118 in control at baseline. Minority of the sample were of non‐Dutch ethnicity | |
| Interventions | As well as usual drug prevention/education programme, the intervention classes received 3 lessons on knowledge, attitude and social influence, followed by class agreement not to start smoking or stop smoking for 5 months. Admission to competition to win a prize dependent on classes completing registration, having < 10% smokers after 5 months and producing a photo expressing the idea of a non‐smoking class. Competition prizes (monetary prizes EUR 220 – EUR 450) available to 6 classes with < 10% smoking and ‘a photo best expressing a non‐smoking class’.
Control classes received the usual drug prevention/education programme; in 7 schools this was the national drug education programme | |
| Outcomes | Baseline (October 1998) 8 months follow‐up (June 1999) 20 months follow‐up (June 2000)
Self‐reported smoking behaviour, intentions and attitudes measured at each time point. Smoking defined as including ‘experimenting’, weekly and daily smoking. No biochemical verification of smoking | |
| Notes | Theoretical basis: Intervention based on ‘social influence model’, which was not described in detail | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Schools recruited, then randomized. Coin tossing by independent person. Intervention group had a significantly lower proportion of boys, older participants, and non‐Dutch participants at baseline. These were adjusted for in the reported analyses. No significant difference in smoking prevalence between groups at baseline |
| Allocation concealment (selection bias) | Low risk | Allocation by independent person |
| Blinding of participants and personnel (performance bias) | Low risk | Not blinded but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) | Low risk | Students told that the jury of the competition were not informed of the results of the study and that registration for the competition was conducted independently of the study evaluation |
| Incomplete outcome data (attrition bias) | High risk | High number lost to follow‐up: in intervention group, 907 participants were lost to follow‐up (1444 at baseline to 537 at 20 months). In control group, 714 participants were lost to follow‐up (1118 at baseline to 404 at 20 months). 1 school dropped out in intervention; 2 schools dropped out in control
Statistically significantly different distribution of baseline measures of SES, ethnicity, religion, age and smoking among those who were followed up at 8 months and were lost to follow‐up. Non‐response was higher among smokers, especially in the control group. Similar comparisons were not made at 20 months |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to make a judgement on prespecified outcomes |
| Methods | Randomized controlled cluster trial | |
| Participants | Country: Germany (1 rural region). 7th grades of 212 eligible ‘Gymnasium’ (for high academic‐achieving students) and ‘Sekundarschule’ schools invited to participate. Schools stratified by type of school. Exclusion criteria: (a) foreseen closure of school in next 2 years; (b) school engaged in tobacco control programme; (c) participated in the intervention before. 50% girls. Mean age 12.65 years. SES measured using type of school as a proxy (Sekundarschule schools = lower SES). SES not reported. > 95% students were of German nationality | |
| Interventions | Intervention: SFC competition: classes agree and sign a contract to remain smoke‐free for 6 months to enter a lottery to win a number of prizes, the grand prize including a class trip. Requirements to participate: at least 90% of class must agree to participate; classes monitor smoking on a weekly basis; classes report whether > 90% non‐smokers to the organisers on a monthly basis. If the class is smoke‐free (> 90% non‐smokers) they remain in the competition for prizes, with the main prize being a class trip; if not they drop out. The intervention group consisted of 2 subgroups: the classes who agreed to participate (IG‐participation) and the classes who were randomized to intervention group but declined to participate (IG‐no participation). Participating classes also received material including the contract, feedback cards, parent leaflet, CD‐ROM, and access to web page
Control group classes received ‘usual curriculum’ | |
| Outcomes | Baseline (October 2008) 1st follow‐up at 7 months post‐baseline 2nd follow‐up at 12 months post‐baseline 3rd follow‐up at 19 months post‐baseline
At baseline and follow‐ups participants completed a questionnaire asking about self‐reported ‘current smoking’ (non‐smoker, occasional use or regular use) and ‘lifetime smoking’ (never, experimenters, established smoking) | |
| Notes | Theoretical basis: Intervention based on principles of correcting social norms (i.e. correcting the common overestimation of smokers by adolescents) and fostering commitment to a social contract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Schools stratified by type of school, consented to participate and then assigned to groups by drawing lots. Lifetime and current smoking more frequent in IG‐no participation group compared with the other 2 groups (IG‐participation and control). Baseline group differences in outcome and confounding variables adjusted for in reported analyses. In our reanalysis of data we only compared IG‐participation and control groups (IG‐no participation excluded) |
| Allocation concealment (selection bias) | Low risk | Allocating person was blinded to purpose of the study |
| Blinding of participants and personnel (performance bias) | Low risk | Not reported but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) | Low risk | Students not informed that outcome assessments were linked to the SFC. Authors noted that they did not observe a difference between groups regarding inconsistent response patterns over time (e.g. backward transitions for lifetime use) |
| Incomplete outcome data (attrition bias) | Low risk | 3490 participants at baseline, 3123 at 7 months, 2595 at 12 months, 2420 at 19 months. 2159 completed all assessments (61%). 6 schools lost from intervention; 2 from control. Attrition analyses performed. Authors report, "Since attrition effects are especially problematic when study dropout is related to one of the outcome variables, we also checked interactions between covariates and intervention status with respect to attrition. However, we found significant interaction effects only for the variables age (interaction age×IG‐no participation (ref. CG): OR=1.37 (1.08 to 1.74), p=0.009) and school type." |
| Selective reporting (reporting bias) | Unclear risk | Primary outcomes specified in study protocol (ISRCTN27091233) were (i) knowledge about smoking; (ii) attitudes towards smoking; (iii) intention to use tobacco; and (iv) smoking status. Only smoking status reported in this paper |
| Methods | Controlled cluster trial, no randomization reported. Public schools assigned to intervention in 2 communities, with the third community acting as control | |
| Participants | Country: Canada (3 city health regions). All elementary schools in these regions invited to participate in the intervention arm (number of schools not reported), 27 agreed, 1262 completed baseline measures. Control schools from 2 different health regions matched to intervention regions in terms of location, urbanization and sociodemographic characteristics. 2 control schools matched to each intervention school according to location and school deprivation indicator. 57 control schools invited to participate, 1657 completed baseline measures. Sample was grade 6 students. Ethnicity not stated and SES described using a measure of school deprivation | |
| Interventions | Intervention: SFC competition (variant): To participate in intervention programme each class was required to have at least 90% of students sign a confidential contract not to smoke for 6 months. Intervention participants received the ‘Mission TNT.06’ programme; a 6‐month programme consisting of didactic material, teacher’s guide and resources to improve knowledge about the health and social effects of smoking. Dose and frequency of education programme unclear. Teachers and students received participation incentives and classes were eligible for half‐day surprise activities
Control group: unclear as to what they received. Authors were contacted to provide further information but this was not forthcoming | |
| Outcomes | Baseline (Oct ‐ Dec 2002) Follow‐up at 10 ‐ 14 months (Oct 2003 ‐ April 2004)
At both baseline and follow‐up participants asked about self‐reported ‘ever smoking’ status defined as ever smoking a cigarette in their life, even a puff. Also questions on knowledge, attitudes and beliefs about tobacco. No biochemical verification of smoking status | |
| Notes | Theoretical basis: The premise for the intervention rested on positive reinforcement for not smoking to stimulate the desired behaviour, but did not reference a specific social theory | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized. Matched allocation of control schools. No breakdown of demographics (age, sex, SES) provided between intervention and control baseline participants. Comparison of baseline characteristics of those who completed follow‐up reported, with significant differences by age, school location and social deprivation index (adjusted for in reported analyses) |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding of participants and personnel (performance bias) | Low risk | Not reported but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) | High risk | Students’ self‐reporting of smoking status may have been influenced by knowledge that they were in a competition for prizes. Note large numbers of ever‐smokers at baseline denying ever smoking at follow‐up. Statistically significantly more in intervention vs control (24% vs 16%) |
| Incomplete outcome data (attrition bias) | Unclear risk | 1262 participants in intervention arm completed baseline, 843 completed follow‐up (33% loss to follow‐up); 1657 participants in control arm completed baseline, 1213 completed follow‐up (27% loss to follow‐up). Analytic sample were those that completed baseline and follow‐up. Reasons for attrition not reported. No detail on comparison between those followed up and those lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to make a judgement on prespecified outcomes |
| Methods | Randomized controlled cluster trial | |
| Participants | Country: Germany (3 counties). 7th grades of all Heidelberg schools and a random sample of schools in Mannheim and Rhine‐Neckar counties. Schools stratified by type of school (unclear what the differences were between schools). 172 classes from 68 schools participated. Approximately 50% girls. > 90% 12 ‐ 13 years. SES and ethnicity not reported | |
| Interventions | Intervention: SFC competition. Classes agree and sign a contract to remain smoke‐free for 6 months to enter a lottery to win a number of prizes, the grand prize including a class trip. Requirements to participate: school classes decide to be a non‐smoking class for 6 months; classes monitor smoking and report it regularly to competition organizers. If the class is smoke‐free (≥ 90% non‐smokers) they remain in the competition for prizes. If > 10% of the class is smoking, the class drops out of the competition. The intervention included weekly curricula consisting of health information about smoking and strategies for how to quit smoking and resist peer pressure to smoke
Unclear exactly what the control group received | |
| Outcomes | Baseline (October 2008) Follow‐up at 24 months post‐baseline
At both baseline and follow‐up participants completed a questionnaire asking about self‐reported smoking. Note additional response options added in follow‐up survey | |
| Notes | Theoretical basis: None reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation process not reported but authors stated schools were "randomly assigned." Active recruitment whereby schools randomized and then classes recruited. 3 classes in control refused to forego intervention and were included in intervention. Some systematic differences between 2 groups relating to age and smoking status as baseline. Significantly more smokers in control group. Adjusted for age in final reported analysis |
| Allocation concealment (selection bias) | Unclear risk | Process for allocation concealment not reported. See above |
| Blinding of participants and personnel (performance bias) | Low risk | Not reported but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) | Low risk | Students not informed that outcome assessments were linked to the SFC |
| Incomplete outcome data (attrition bias) | High risk | High level of attrition: 4043 participants at baseline, 1852 followed‐up at 24 months Overall attrition rate 54%. No association between intervention group and attrition Reasons for attrition not reported in detail. Association between smoking status and attrition not explored |
| Selective reporting (reporting bias) | Unclear risk | Prespecified outcomes unclear |
| Methods | Controlled cluster trial, no randomization reported. Schools assigned to intervention based on agreement to participate, with non‐participating classes acting as controls and matched with participating classes based on region and age group | |
| Participants | Country: Switzerland. Canton of Berne, German‐ and French‐speaking classes, urban and rural areas. Total of 1035 participants from 71 classes ‐ 34 in participation (intervention) group, 37 in control group. All participants were in 7th or 8th grade. Mean age 13.3 years, 53.2% girls | |
| Interventions | SFC competition. Entire classes were required to commit to a contract to be smoke‐free for 6 months to win a prize | |
| Outcomes | Smoking status at baseline (Oct/Nov 2010), and follow up about 7 months later (May/Jun 2011). Self‐reported smoking status in the past 6 months, and also in past month. Smoking‐related knowledge was assessed at baseline and follow‐up. Peer smoking was also recorded at baseline | |
| Notes | Theoretical basis: Intervention based on principles of correcting social norms (i.e. correcting the common overestimation of smokers by adolescents) and fostering commitment to a social contract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomization was not possible, as classes registered of their own accord. Analysis was undertaken for a randomly selected subsample of participating and non‐participating classes. Some differences between participating classes that participated and completed the competition compared to control, and participating classes that dropped out compared to control. (Age, class atmosphere, peers who smoked) |
| Allocation concealment (selection bias) | High risk | No process for allocation concealment reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Overall low attrition |
| Selective reporting (reporting bias) | Unclear risk | Insufficient reporting to make a judgement on prespecified outcomes |
| Methods | Controlled cluster trial | |
| Participants | Country: Finland. Intervention: All 600 junior high schools in Finland were invited to be in SFC competition each year. In 1991‐2, 1219 8th Grade classes (from 368 schools) entered the competition (⅓ of age cohort) and 65 of these classes were randomly selected to take part in this study Control group: randomly selected from classes that did not register for the competition Age of participants not provided but reported they were 8th graders (approx. 14 year olds). Sex, SES and ethnicity not reported | |
| Interventions | Intervention: SFC competition (here known as ‘no smoking class competition’): classes agree and must remain 100% smoke‐free for 6 months to enter a lottery to win 4 main prizes of USD 2000 and 10 second prizes of USD 200; the grand prize including a class trip. Prize money can be used in any way the class chooses. Requirements to participate: All of class must agree to participate; classes monitor smoking on a weekly basis; if anyone starts smoking and does not quit the class must drop out of the competition. The contact teacher for each class organizes health education sessions about smoking during school hours – no other details provided about this education
Unclear what control group classes received | |
| Outcomes | Baseline (Fall 1991) 1st follow‐up at 6 months post‐baseline (Spring 1992) 2nd follow‐up at 18 months post‐baseline (Spring 1993)
At both baseline and follow‐up participants completed a questionnaire asking about self‐reported daily smoking (Do you now smoke?: not at all/less than once a month/1 ‐ 2 times a month/1 ‐ 2 times a week/daily). Daily smokers were reported as smokers) | |
| Notes | Theoretical basis: not provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized. No baseline comparisons except smoking status. A higher proportion of control group reported daily smoking at baseline compared with the intervention group. This was adjusted for in final reported analysis. Control group chose not to register for the competition, so increased likelihood of systematic differences between groups |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding of participants and personnel (performance bias) | Low risk | Not reported but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) | Low risk | Authors state pupils were not aware that survey was related to the competition |
| Incomplete outcome data (attrition bias) | Unclear risk | 1284 intervention and 551 control participants at baseline; 976 intervention (76%) and 443 control (80%) participants completed all 3 surveys (analyzed sample). Reasons for attrition were not reported and no detail on comparison between those followed up and those lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Prespecified outcomes unclear |
| Methods | Controlled cluster trial | |
| Participants | Country: Germany (3 cities). Intervention: multiple secondary school classes from schools who registered for the SFC competition (all schools were invited) from Hamburg and Berlin. The intervention group consisted of classes that decided to participate in the competition. | |
| Interventions | Intervention: SFC competition: classes agree and sign a contract to remain smoke‐free for 6 months to enter a lottery to win a number of prizes, the grand prize including a class trip. Requirements to participate: At least 90% of class must agree to participate, classes monitor smoking on a weekly basis, classes report whether > 90% non‐smokers to the organisers on a monthly basis. If the class is smoke‐free ( > 90% non‐smokers) they remain in the competition for prizes, with the main prize being a class trip; if not they drop out. The intervention group consisted of 2 subgroups: the classes who successfully completed the competition and the classes who dropped out of the competition (but continued in the study). Participating classes also received 2 newsletters with information about competition, teachers received a brochure
The control group (CG) classes did not receive a specific intervention | |
| Outcomes | Baseline (October/November 1998) 1st follow‐up at 6 months post‐baseline (May 1999) 2nd follow‐up at 12 months post‐baseline (November 1999) At both baseline and follow‐up participants completed a questionnaire asking about self‐reported ‘four week smoking prevalence’ (‘Have you smoked during the last four weeks?’) and ‘daily smoking prevalence’ (‘Have you smoked daily during the last seven days?’) | |
| Notes | Theoretical basis: Reference to learning theory that asserts that positive reinforcement enhances the probability of producing a desired behaviour | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomized. Classes who volunteered to take part in the competition made up the intervention group versus classes from another town, that were not invited to take part in the competition (control group). No SES or ethnicity reported or compared. Smoking prevalence at baseline was higher in the control group than in the intervention group, although not statistically significantly so. No baseline differences in age or sex |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding of participants and personnel (performance bias) | Low risk | Not reported but unlikely to affect outcome |
| Blinding of outcome assessment (detection bias) | Low risk | Authors note that students' knowledge that they were in a competition should not have had an influence on their answers in the follow‐up, since the competition had been completed at that point |
| Incomplete outcome data (attrition bias) | High risk | High level of attrition: 4372 participants at baseline, 2142 (49%) completed all 3 surveys (1495 intervention and 647 control) At baseline, those lost to follow‐up were significantly more likely to be smokers or in the intervention group; percentage of smokers in retention group under‐represented. No significant interaction for smoking status and group condition among attrition and retention sample. No differences in age or sex |
| Selective reporting (reporting bias) | Unclear risk | Prespecified outcomes unclear |
SES: socioeconomic status; SFC: Smokefree Class Competition
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Incentive(s) not used to reward participants for not starting to smoke | |
| Incentive(s) not used to reward participants for not starting to smoke | |
| No incentive used as part of the intervention | |
| A review, not a controlled trial | |
| No incentive used as part of the intervention | |
| Incentives/competitions not a central component of this smoke‐free programme | |
| A review, not a controlled trial | |
| Repeated cross‐sectional surveys of participants for not starting to smoke | |
| A review, not a controlled trial and response letters, does not present additional data | |
| Does not report original data on evaluation, but gives an overview on participation rates in SFC competition and summarizes all evaluation findings | |
| Does not report original data on evaluation, but gives an overview on participation rates in SFC competition and summarizes all evaluation findings | |
| A review, not a controlled trial | |
| Incentive(s) not used to reward participants for not starting to smoke | |
| Not a controlled trial | |
| Not a controlled trial | |
| Study discontinued | |
| Incentive(s) not used to reward participants for not starting to smoke | |
| Follow‐up less than 6 months | |
| Not a controlled trial. No incentive used | |
| Re‐analyses of previous studies. | |
| The only trial (out of 3 described in this record) that used incentives employed a repeated cross‐sectional design | |
| Incentive(s) not used to reward participants for not starting to smoke | |
| Not a controlled trial | |
| Not a controlled trial | |
| Incentive(s) not used to reward participants for not starting to smoke | |
| Not the relevant target population. Incentives used to reward persistent abstinence after quitting | |
| Not a controlled trial | |
| Not a controlled trial | |
| Not a controlled trial | |
| Not a controlled trial | |
| Introduces the concept behind the SFC competition and presents results of process evaluation | |
| Focused on smoking cessation, not smoking initiation |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking uptake at longest follow‐up (RR) Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.1 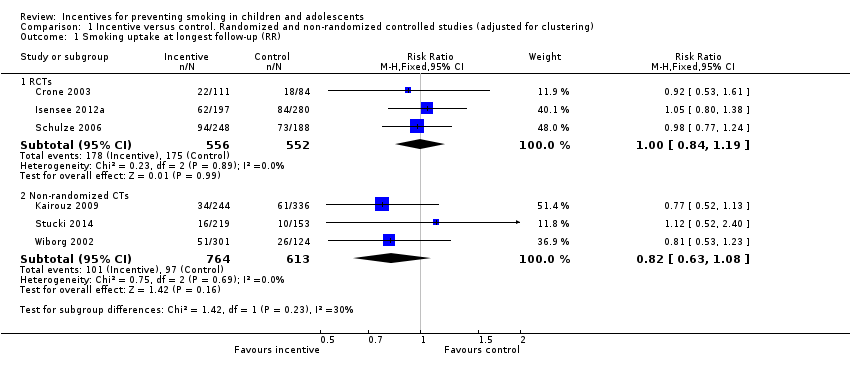 Comparison 1 Incentive versus control. Randomized and non‐randomized controlled studies (adjusted for clustering), Outcome 1 Smoking uptake at longest follow‐up (RR). | ||||
| 1.1 RCTs | 3 | 1108 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.84, 1.19] |
| 1.2 Non‐randomized CTs | 3 | 1377 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.63, 1.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 Results table: RCTs Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.1
Comparison 2 Results of included studies, Outcome 1 Results table: RCTs. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 Results table: non‐randomized CTs Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 2.2
Comparison 2 Results of included studies, Outcome 2 Results table: non‐randomized CTs. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

PRISMA study flow diagram of search results
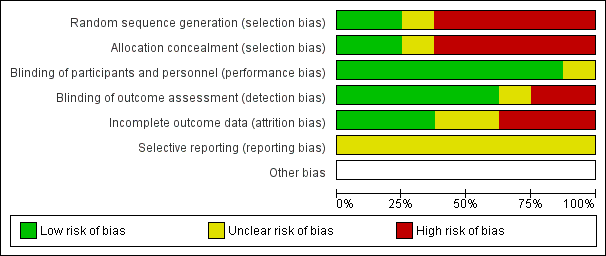
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
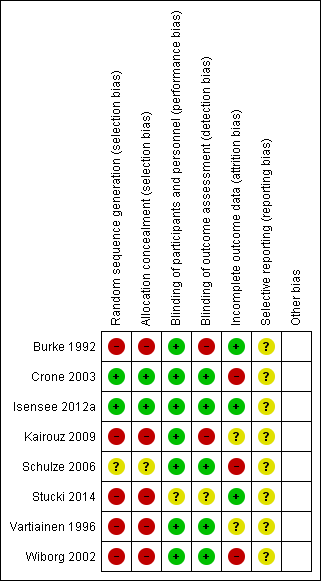
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
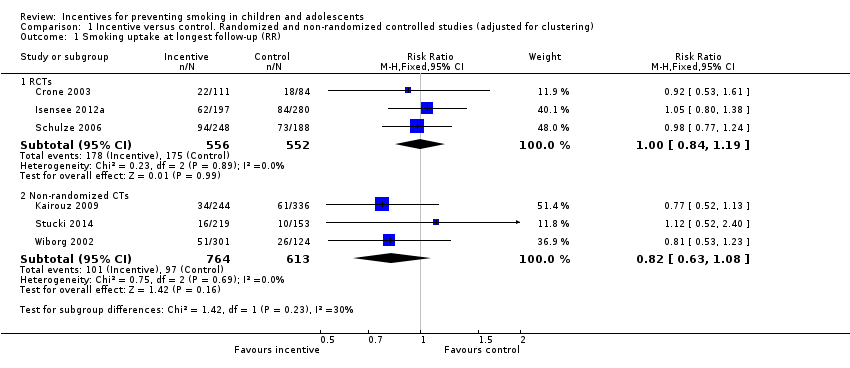
Comparison 1 Incentive versus control. Randomized and non‐randomized controlled studies (adjusted for clustering), Outcome 1 Smoking uptake at longest follow‐up (RR).
| Study | Number of non‐smokers at baseline | Number of smokers at endpoint who reported not smoking at baseline | Time point | Outcome | Biological criterion | Results | Secondary outcomes (dose response, cost, harms) |
| Crone 2003 | 556 intervention; 420 control (data from authors) | 112 intervention; 88 control
| 19 months | Smoking = current smoking, including daily/weekly/experimental | Not biochemically verified | Not reported at 19 months in published paper. Our reanalysis: RR 0.92 (95% CI 0.53 to 1.61) | Not reported |
| Isensee 2012a | 430 never‐ smokers in intervention; 610 never‐smokers in control (data from authors) | 136 intervention; 184 control | 19 months | Smoking = ever smoking, even just a puff | Not biochemically verified | From published paper: Authors reported that no group differences were found in the frequency of smoking initiation but data not presented in paper. Our reanalysis: RR 1.05 (95% CI 0.80 to 1.38) | Bullying (Hanewinkel 2010): "When compared with control classrooms on all three dependent variables – being victimised, active bullying or being isolated – the adjusted ORs indicated no significant differences at post‐test for any of the IGs [Intervention Groups]". |
| Schulze 2006 | 591 never‐smokers in intervention; 449 never‐smokers in control | 224 intervention; 173 control | 24 months | Smoking = current smoking, including irregular (less than weekly) smoking | Not biochemically verified | From published paper: 62.1% remained ‘never smoker’ in intervention group at follow‐up versus 61.4% in control group: OR 1.02 (0.83 to 1.24) adjusted for age, sex and school type.
Our reanalysis: RR 0.98 (95% CI 0.77 to 1.24) | Not reported |
Comparison 2 Results of included studies, Outcome 1 Results table: RCTs.
| Study | Number of non‐smokers at baseline | Number of smokers at endpoint who reported not smoking at baseline | Time point | Outcome | Biological criterion | Results | Secondary outcomes (dose response, cost, harms) | Comment |
| Burke 1992 | Not reported | Not reported | 18 months | Mean (SD) score of 5‐category self‐definition of smoking and 10‐category self‐reported frequency | Salivary thiocyanate (TCN) | From published paper: Mean TCN at follow‐up of pre‐intervention never‐smokers higher (560 mcg/mL, SD 403) versus control (514 mcg/mL, SD 424). Primary outcome for this review not available. | Not reported | |
| Kairouz 2009 | 664 intervention; 915 control | 93 intervention; 165 control | 10 ‐ 18 months | Smoking = ever smoking, even just a puff | Not biochemically verified | From published paper: OR 0.8 (0.5 to 1.1), adjusted for age, gender, school location, social deprivation index. Our reanalysis: RR 0.81 (95% CI 0.55 to1.20) | Intervention participants more likely than control participants to report that people “should not hang out with smokers” (14% versus 11%) and that they, themselves would “not want to be friends with a classmate who smokes” (28% versus 25%) | Concerns about misreporting of smoking status. Note large numbers of ever‐smokers at baseline then denying ever smoking at follow‐up. Stat sig more in intervention vs control (24% vs 16%) |
| Stucki 2014 | 544 intervention, 378 control | 39 intervention, 24 control | About 7 months | Smoking = any smoking in last 6 months, even just a puff and smoking during the previous month | Not biochemically verified | From published and additional data from authors. OR for decreased smoking prevalence 0.7, CI 0.5 to 1.0 | Increased smoking‐related knowledge b ‐1.0, P < 0.01 | |
| Vartiainen 1996 | Not reported and not available from authors | Not reported and not available from authors | 18 months | Smoking = daily smoking | Not biochemically verified | Reports only on the increase in prevalence of smoking from baseline to follow‐up. From baseline to longest follow‐up, increase by 10.8% points in Intervention group vs 11.2% points in control group: OR 1.25 (P = 0.15). Primary outcome for this review not available. | Not reported. Except in discussion – authors report "The social pressure created by the competition process was not greatly criticised in the pupils’ answers." | |
| Wiborg 2002 | 1215 intervention group; 502 control (data from authors) | 207 intervention; 107 control | 12 months | Smoking = 4 week prevalence of smoking | Not biochemically verified | From published paper: OR 1.36 (1.04 to 1.76), adjusted for age, sex, smoking status at baseline Our reanalysis: RR 0.81 (95% CI 0.53 to 1.23) | Cost benefit (Hoeflymayr 2008). Cost benefit ratio: economic modelling based on estimates of reduced smoking prevalence in Intervention group and models of assumed future smoking behaviour and cessation. Not based on prevention of initiation | |
Comparison 2 Results of included studies, Outcome 2 Results table: non‐randomized CTs.
| Smokefree Class Competitions (SFC) for preventing smoking uptake | |||||
| Patient or population: Children and adolescents aged 5 ‐ 18 years who were non‐smokers at baseline Settings: Schools in Germany, the Netherlands, Finland, Switzerland, Canada and the United States Intervention: Participation in SFC Comparison: No participation in SFC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants Actual number/ effective number2 | Quality of the evidence | |
| Assumed risk1 | Corresponding risk | ||||
| Smoking uptake at longest follow‐up (RCTS) | 317 per 1000 | 320 per 1000 | RR 1.00 (0.84 to 1.19) | 3056/1108 (3) | Low3, 4 |
| Smoking uptake at longest follow‐up (Non‐RCTs) | 158 per 1000 | 132 per 1000 | RR 0.82 (0.63 to 1.08) | 4219/1377 (3) | Very low3, 5, 6 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1'Assumed risk' calculated as risk in control groups. | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking uptake at longest follow‐up (RR) Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 RCTs | 3 | 1108 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.84, 1.19] |
| 1.2 Non‐randomized CTs | 3 | 1377 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.63, 1.08] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Results table: RCTs Show forest plot | Other data | No numeric data | ||
| 2 Results table: non‐randomized CTs Show forest plot | Other data | No numeric data | ||

