Interventionen zur Erhöhung des Konsums von Obst und Gemüse bei Kindern im Alter von 5 Jahren und jünger
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: Randomised controlled trial Funding: Not reported | |
| Participants | Description: Children aged 3 to 6 years attending an independent childcare facility in Central Pennsylvania, USA N (Randomised): 47 children Age: 3 to 6 years (mean = 4.7 years) % Female: 51% SES and ethnicity: Children: White = 83%, Asian = 10% Parents: “Most parents were well‐educated (median education = bachelor’s degree) and were currently employed. The majority of parents reported being married (88%), and the majority of the families reported annual combined family incomes greater than $60,000 (89%).” Inclusion/exclusion criteria: No explicit inclusion criteria stated for this trial Exclusion criteria: “Children were excluded if they had intolerance to study foods, a chronic illness affecting food intake, or if they were non‐English speaking. Additionally, individuals with extended absences were excluded from the results.” Recruitment: Not specified Recruitment rate: Unknown Region: Central Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): 41 (not specified by group) Description of intervention: “All children in each classroom received the same vegetable throughout the study”. “children were asked twice weekly over a period of 4 weeks to take of taste of a very small portion (˜4 g) of the vegetable in its assigned condition.” Repeated exposure: Vegetable intake without dip Flavor‐flavor associative conditioning: Vegetable intake with dip. “Dips served in this experiment included two savory dips (ketchup and ranch‐flavored) and one sweet‐tasting dip (cinnamon sugar)” Duration: 4 weeks Number of contacts: 8 exposure sessions (2 exposures/week) Setting: Preschool Modality: Face‐to‐face Interventionist: Research staff Integrity: No information provided Date of study: Unknown Description of control: NA | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of target vegetable (grams). “Children were served a bowl containing 60 g of the vegetable, and children in the AC condition were also served ˜60 g of dip in 3.25 oz soufflé cups, which accompanied the vegetable…. Instructions to children prior to the meal were to eat as much as they wanted, not to share food with others, and to remain in their seats…. When children finished snack, spilled or dropped foods were returned to the correct dish and snack trays were cleared. Vegetables were weighed before serving and were weighed after the intake session was complete, and the difference was recorded as vegetable intake.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 9 weeks Length of follow‐up post‐intervention: 2 weeks Subgroup analyses: None Loss to follow‐up: There was no loss to follow‐up Analysis: Unknown if sample size calculation was performed. | |
| Notes | Sensitivity analysis ‐ primary outcome: Primary outcome not stated. Child fruit and vegetable intake 2nd listed outcome measure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Participants were not blinded and it seems likely that children may have been influenced by those children around them and whether or not other children had a flavoured dip |
| Blinding of outcome assessment (detection bias) | Low risk | Food was weighed and it is unlikely to be influenced by whether the researchers were blinded to condition |
| Incomplete outcome data (attrition bias) | Low risk | There does not appear to be any attrition and therefore low risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol so it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: “This project was funded by Wageningen University and Research Centre.” | |
| Participants | Description: Healthy infants between 4 and 7 months (not being weaned yet) and their parent N (Randomised): 101 parent‐infant pairs Age: Child (mean): Green beans group = 162 days, Artichoke group = 160 days, Apple group = 165 days, Plum group = 162 days Mother (mean): Green beans group = 31 years, Artichoke group = 30 years, Apple group = 31 years, Plum group = 32 years % Female: Child: Green beans group = 54%, Artichoke group = 41%, Apple group = 56%, Plum group = 44% Parent: 96% SES and ethnicity: Parents education: Low = 17%, middle = 32%, high = 50% Inclusion/exclusion criteria: Inclusion criteria: “Only healthy Children between 4 and 7 months old, who were not being weaned yet, were included in the study.” Exclusion criteria: “Children with known food allergies, swallowing or digestion problems, or other medical problems that could influence the ability to eat, were excluded.” Recruitment: “The participants were recruited from the area of Wageningen and Almere in the Netherlands where both the research locations were. They were recruited via local newspapers, maternity or children welfare centers, postnatal care groups, and a mailing to subscribers of babyinfo.nl (a Dutch advertisement website that gives a box with free products for subscribers expecting a baby).” Recruitment rate: Unknown Region: Wageningen and Almere (The Netherlands) | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Green beans group = 24 Artichoke group = 27 Apple group = 24 Plum group = 24 Description of intervention: At the lab (days 1,2,17,18 and 19): “A bowl with two jars of vegetable purée was handed to the mother and the mother fed the infant at their usual rate until the end of the feeding was indicated by the infant (i.e. when it rejected the spoon more than three successive times).” At the home (days 3 ‐ 16): “At the end of the 2nd test‐day at the lab, the mothers received the jars of puréed vegetables or fruits for the home exposure period. Each jar was labelled with the date on which it had to be fed to the infant and numbered from 3 to 16 corresponding to the respective days of the intervention period. The feeding was carried out every day at about the same time and in the same way as during days 1 and 2 in the lab.” Duration: 19 days Number of contacts: 9 exposure sessions Setting: Lab and home Modality: Face‐to‐face Interventionist: Researchers trained parents to offer the target vegetable or fruit puree to their child Integrity: No information provided Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of target vegetable and fruit purees (grams). At the lab: “The pre‐ and post‐weight of the bowl including the spoon and bib was weighted to measure the actual intake.” At the home: “The mother was instructed to empty both jars completely on a plate and to put all what was left over after the feeding, including the vegetable purée that was spilled on the table, floor, bib, child’s face, etc., back in the jar and to seal the jar with the lid and put it in the refrigerator…. In order to have a standardized measure of home intake, the jars had been pre‐weighted in the lab before the home exposure period, and after they were collected and were post‐weighted again in the lab.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 19 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall = 2% (not specified by group) Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | There is no indication whether the mother who fed the child was blind to group allocation. Given the mother fed the child, at high risk of performance bias |
| Blinding of outcome assessment (detection bias) | Unclear risk | There is no indication whether the mother who fed the child and weighed the food was blinded to group allocation. Given the food was weighed by the mother the risk of detection bias is unclear |
| Incomplete outcome data (attrition bias) | Low risk | 94% retention and therefore risk of attrition bias is low |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol, therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Cluster‐randomised controlled trial Funding: “No external or intramural funding was received.” | |
| Participants | Description: Children 5 years of age in 12 nursery schools connected to the Izmir Provincial Directorate of National Education N (Randomised): 6 preschools, 238 children Age: Child: 5 years of age Mother (mean): Intervention = 33.4 years, Control = 33.4 years Father (mean): Intervention = 36.9 years, Control = 36.8 years % Female: Child: Intervention = 60%, Control = 48% SES and ethnicity: Education: Mother: Primary = 9%, Secondary school = 15%, High school = 38%, University = 38% Father: Primary = 10%, Secondary school = 14%, High school = 37%, University = 40% Family SES: Low = 16%, Medium = 73%, Upper = 11% Inclusion/exclusion criteria: Not specified Recruitment: Not specified Recruitment rate: Unknown Region: Izmir (Turkey) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 141, Control = 97 Description of intervention: “The content of the education guided by Piaget’s theory included play and visual materials. Thus, healthy food choices were created by means of play/games. Following age‐appropriate education carried out using Piaget’s theory, improvements are observed in food selection and consumption” Duration: Initial intervention = 6 weeks + at 1 year follow‐up a 3 week refresher intervention (20 ‐ 30 minutes per session) Number of contacts: 9 sessions (1 per week) Setting: Preschool Modality: Face‐to‐face Interventionist: “The researcher (H.B.), who is a nurse educator, was the interventionist for all sessions.” Integrity: No information provided Date of study: February 2007 to June 2008 Description of control: “The children in the control group had not received nutrition education but they had received a general program of education (the nutrition education prescribed by the Ministry of National Education preschool). The yearly syllabus of the Ministry includes subjects on nutrition every 2 months. This time frame, however, may be insufficient for nutrition education.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetables assessed using food frequency questionnaire (FFQ) completed by parents Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Post‐test: 4 months (pre‐test February 2007 – post‐test June 2007) Post‐test 2: 16 months (post‐test 2 June 2008) Length of follow‐up post‐intervention: Post‐test: 2 months Post‐test 2: 14 months Subgroup analyses: None Loss to follow‐up (at 2 and 14 months) Intervention: 1%, 52% Control: 9%, 51% Analysis: Unclear Sample size calculation was performed. | |
| Notes | Sensitivity analysis ‐ primary outcome: Primary outcome not stated, power calculation conducted on knowledge only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Nutrition knowledge & food frequency (self‐reported) There is no blinding to group allocation of participants or personnel described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Nutrition knowledge & food frequency There is no mention that participants were blinded to group allocation and therefore the risk of detection bias is high |
| Incomplete outcome data (attrition bias) | High risk | 67/141 (48%) in experimental group and 48/97 (49%) in control group completed post‐test 2 and therefore risk of attrition bias is high |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity do not appear to be an issue |
| Methods | Study design: Randomised controlled trial Funding: Not reported | |
| Participants | Description: Low‐income mother/toddler (12 ‐ 30 months) dyads N (Randomised): Unknown Age: Child: mean = 20 months Mother: mean = 27.4 years % Female: Child: 59% SES and ethnicity: “67.3% below poverty index, 34% married, 68% black” Inclusion/exclusion criteria: Low‐income mother (criteria not stated) with toddler 12 ‐ 30 months Recruitment: Recruited from WIC (Women, Infants and Children) Clinics Recruitment rate: Unknown Region: USA | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Preliminary = 151 Description of intervention: “Interventions (5 group & 3 individual sessions) used goal setting to promote: 1) parenting practices or 2) maternal diet and physical activity (PA)" Duration: Not specified Number of contacts: Not specified Setting: WIC Clinic Modality: Face‐to‐face Interventionist: Unclear Integrity: No information provided Date of study: Unknown Description of control: Placebo group, sessions provided on toddler safety. | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Change in vegetable and fruit intake (mypyramid equivalent per 1000 kcal) assessed using 24‐hour diet recall completed by parents Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 6 and 12 months Length of follow‐up post‐intervention: Unclear Subgroup analyses: None Loss to follow‐up: Unknown Analysis: Unknown if sample size calculation was performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | 24‐hour diet recall There is no blinding to group allocation of participants or personnel described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | 24‐hour diet recall There is no mention that participants were blinded to group allocation and therefore the risk of detection bias is high |
| Incomplete outcome data (attrition bias) | Unclear risk | There is no information provided about attrition rates at follow‐up |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | There is insufficient information to determine the risk of other bias |
| Methods | Study design: Randomised controlled trial Funding: “Funded by the Feeding For Life Foundation (grant reference number 11‐1170). ” | |
| Participants | Description: Children aged 2 to 4 years and their principle caregiver (parent) N (Randomised): 120 parent‐child dyads Age: Child (mean): Prompting no modelling = 27 months, Prompting and modelling = 29 months, Modelling ‘control’ group = 31 months Mothers (mean): Prompting no modelling = 34 years, Prompting and modelling = 26 years, Modelling ‘control’ group = 35 years % Female: Child: 45% Parent: 98% SES and ethnicity: Not specified Inclusion/exclusion criteria: “Inclusion criteria for children included the absence of known food allergies or disorders affecting eating, current or recent major illness or diagnosed intellectual disabilities.” Recruitment: “Caregivers and their children were recruited through the Children and Child Laboratory database, which contains information on families in which caregivers have indicated an interest in research participation at the University of Birmingham.” Recruitment rate: Unknown Region: UK | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Prompting no modelling = 35 dyads Prompting and modelling = 37 dyads Modelling ‘control’ group = 27 dyads Description of intervention: Prompting no modelling: “Caregivers were asked to use physical prompts to eat the novel fruit (NF) (including passing the food to the child, moving the food towards the child, holding the NF up to the child’s face, encouraging the child to touch the NF).” Prompting and modelling: As well as using physical prompts as in PNM, “The caregivers assigned to this condition were also asked to try the NF themselves.” Modelling ‘control’ group: “Caregivers in this condition were not given any information about prompting, but were simply asked to taste the NF themselves.” Duration: 1 day Number of contacts: 1 Setting: Lab Modality: Face‐to‐face Interventionist: Parents Integrity: Prompting no modelling: “Of an original sample of fifty, fifteen were classed as non‐compliant: ten caregivers failed to prompt a minimum of three times, and five caregivers were removed from the group because they ate the NF. This left a sample of thirty‐five parents who physically prompted but did not model eating the fruit.” Prompting and modelling: “Of an original sample of forty‐three dyads, six were non‐compliant because the parent failed to prompt three times or more, leaving a sample of thirty‐seven parents who prompted and modelled eating the fruit.” Modelling ‘control’ group: “There were twenty‐seven dyads in this condition, in which the parent modelled eating of the fruit; all were compliant with this request.” Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of novel fruit (grams): “All meal items were weighed on scientific scales before and after consumption.” “Owing to differences in weights of the different NF offered, it was not possible to compare conditions based on simple weight of consumption. Therefore, we calculated consumption of the NF based on the percentage consumed of the whole portion offered.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: < 1 day Length of follow‐up post‐intervention: Same day Subgroup analyses: None Loss to follow‐up: Prompting no modelling: 30% Prompting and modelling: 14% Modelling ‘control’ group: No loss to follow‐up Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure is unclear. The authors indicate that block randomisation was used to allocate to groups in blocks of 10 participants with conditions changing each week, allocated in order of recruitment |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Fruit intake is an objective measure of child’s fruit intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Fruit intake All meals were weighed on scientific scales before and after consumption therefore at low risk of detection bias |
| Incomplete outcome data (attrition bias) | High risk | Used a per‐protocol analysis rather than an intention‐to‐treat analysis and therefore at high risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | There was a significant difference in children’s ages and child’s age was controlled for in analyses. Therefore the risk of other bias is unclear |
| Methods | Study design: Cluster‐randomised controlled trial Funding: “National Health and Medical Research Council Grant No. 425801" | |
| Participants | Description: First‐time mothers and their infants N (Randomised): 62 parent groups, 542 parent‐child pairs Age: Child (mean): Intervention = 3.9 months, Control = 3.9 months Parent (mean): Intervention = 32.5 years, Control = 32.1 years % Female: Intervention = 48%, Control = 47% SES and ethnicity: Parent: Education level (Completed university degree or beyond): Intervention = 52%, Control = 57% Born in Australia: Intervention = 78%, Control = 78% Inclusion/exclusion criteria: Parent groups: Inclusion criteria: “Parent groups were eligible if ≥8 parents enrolled or ≥6 parents enrolled in areas of low socioeconomic position (SEP) because mothers in areas of low SEP are less likely to attend first‐time parent groups.” No explicit exclusion criteria stated for this trial Parents: Inclusion criteria: “Parents will be eligible to participate if they are able to freely give informed consent, are first‐time parents, members of a participating 'first‐time parents group' and are able to communicate in English.” Exclusion criteria: “Parents will be excluded from the study if they are unable to give informed consent or are unable to communicate in English. Infants with chronic health problems that are likely to influence height, weight, levels of physical activity or eating habits will be excluded from analyses but will be permitted to participate in the study.” Recruitment: “A two‐stage random sampling process will be used to select first‐time parent groups. At the first stage, twelve local government areas within a 60 km radius of the research centre (Deakin University in Burwood, Victoria, Australia) will be randomly selected.” “At the second stage, first‐time parent groups within selected local government areas will be randomly selected, proportional to the total number of first‐time parent groups within each area. The first‐time parents group currently underway will then be invited to participate.” Recruitment rate: Parent: 86% (542/630) Region: Melbourne (Australia) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 195, Control = 194 Description of intervention: “The dietitian‐delivered intervention comprised six 2‐hour sessions delivered quarterly during the first‐time parents’ group regular meeting.” The intervention “sought to build knowledge, skills, and social support regarding infant feeding, physical activity, and sedentary behaviors. Messages were anticipatory in nature, such that concepts were presented before the associated child developmental phase.” “Intervention materials incorporated 6 purpose‐designed key messages (for example, “Color Every Meal With Fruit and Veg,” “Eat Together, Play Together,” “Off and Running”) within a purpose‐designed DVD and written materials. A newsletter reinforcing key messages was sent to participants between sessions.” Duration: 15 months Number of contacts: 6 sessions at 3‐monthly intervals (2 hours per session) Setting: Parenting group Modality: Multiple (face‐to‐face, visual and written materials) Interventionist: Experienced Dietitian Integrity: “Program fidelity was audited via checklists by researchers attending but not delivering the intervention.” No further information reported Date of study: June 2008 to February 2010 Description of control: “Control parents received usual care from their MCH nurse, who may have provided lifestyle advice.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetable (grams) assessed using 3 x 24hr recalls (3 days, including 1 weekend day) conducted by trained nutritionists via telephone interview with parents Outcome relating to absolute costs/cost effectiveness of interventions: Intervention cost per family reported that adjusted “for the fact that a trial setting sees an artificially small number of families included relative to the workforce employed” Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 6 (mid‐intervention) and 15 months (post‐intervention) Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up (Immediately post‐intervention): Intervention = 28% Control = 28% Analysis: Adjusted for clustering. Sample size calculation was performed. | |
| Notes | First reported outcome (grams fruit/day) was extracted for inclusion in the meta‐analysis. Sample size per group was not reported and instead calculated based on assumption of equal loss to follow‐up per group, and reported baseline sample per group and total sample for diet outcomes at follow‐up. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, however power calculation was conducted on fruit or vegetable intake | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly allocated to condition using a computer‐generated random number schedule developed by a statistician with no contact with the centres |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | 24‐hour dietary recall (parent reported) Parents were not blinded to group allocation and therefore the risk of performance bias is high |
| Blinding of outcome assessment (detection bias) | High risk | 24‐hour dietary recall (parent reported) Parents were not blinded to group allocation and because this is a self‐reported measure the risk of detection bias is high, even though the dietary recalls were administered by telephone by staff blinded to participant’s group allocation |
| Incomplete outcome data (attrition bias) | Unclear risk | 389/542 (72%) completed the diet outcomes during this long‐term assessment. However the number and reasons for dropout is not reported by study group and so cannot establish if reasons for dropouts are similar across groups |
| Selective reporting (reporting bias) | High risk | There are physical activity outcomes referred to in the protocol that are not reported |
| Other bias | Low risk | There are no differences in baseline characteristics between trial arms & contamination and other bias unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: "This research has received funding from the European Community’s Seventh Framework Programme (FP7/2007‐3) under grant agreement no. 245012‐HabEat coordinated by Dr Sylvie Issanchou. (INRA, UMR 1324, Centre de Sciences du Gouˆt et de l’Alimentation, F‐21000 Dijon France)." | |
| Participants | Description: Children aged 6 to 36 months in private daycare nurseries in West and South Yorkshire, UK N (Randomised): Unclear “Of the 108 recruited, fourteen children were excluded due to food allergies (n 3) and for being older than 40 months (n 11). Of the ninety‐four children, six children refused to take part in the study, fifteen were excluded due to lack of attendance at nursery and one was removed for incomplete exposures. Table 2 provides characteristics of the children who took part in the intervention. Out of the potential sample, seventy‐two completed the Study.” Age: Mean: Repeated exposure = 24 months, Flavour‐flavour learning = 23 months, Flavour‐nutrient learning = 24 months % Female: Repeated exposure = 55%, Flavour‐flavour learning = 48%, Flavour‐nutrient learning = 68% SES and ethnicity: Unclear, “to ensure good representation of ethnic background and SES we selected nurseries in a variety of different locations in West and South Yorkshire, UK” Inclusion/exclusion criteria: No explicit inclusion criteria stated for this trial “All children reported to have any food allergies were excluded from taking part in the investigation.” Recruitment: “In the first instance, nursery managers were given details of the study to check their interest in the study. If the nursery managers expressed an interest, then the participant information sheets and consent forms were distributed to parents.” Recruitment rate: Unknown Region: West and South Yorkshire (UK) | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Repeated exposure = 22 Flavour‐flavour learning = 25 Flavour‐nutrient learning = 25 Description of intervention: “Around 2–4 d after the pre‐intervention period, each child was offered one pot (100 g) of artichoke for ten exposures.” Repeated exposure: “The RE recipe was a basic vegetable puree.” Flavour‐flavour learning: “For the FFL puree, the chosen unconditioned stimulus was sweetness. The selected sweet ingredient was sucrose.” Flavour‐nutrient learning: “For the FNL puree, the chosen unconditioned stimulus was a higher energy density. The selected energy‐dense ingredient was sunflower oil, because of its relatively neutral taste.” Duration: 10 days Number of contacts: 10 Setting: Preschool Modality: Face‐to‐face Interventionist: Nursery staff Integrity: No information provided Date of study: Recruitment took place February – May 2011 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of novel vegetable (artichoke) (grams) and changes in intake (grams) between a familiar (carrot) and novel vegetable (artichoke) “All pots were weighed before and after to determine intake (g) throughout the experiment. Any spillage on tables and bibs were collected after the session and were added back in to the pots before re‐weighing.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Unclear Length of follow‐up post‐intervention: 5 weeks Subgroup analyses: None Loss to follow‐up: Repeated exposure = 27% Flavour‐flavour learning = 40% Flavour‐nutrient learning = 46% Analysis: Unknown if sample size calculation was performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake (objective) Objective measure of child’s vegetable intake and staff were blinded to the target vegetable being offered to the children |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake (objective) Food was weighed to determine intake and staff were blinded to the target vegetable being offered to the children |
| Incomplete outcome data (attrition bias) | High risk | Of the 72 children taking part in the study 45 (63%) completed the follow‐up and so the risk of attrition bias is high |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: “Supported jointly by the Thrasher Research Fund; the World Health Organization; UNICEF/Honduras and the Institute for Reproductive Health (formerly the Institute for International Studies in Natural Family Planning), Georgetown University, under a Co‐operative Agreement with the U.S. Agency for International Development (A.I.D.) (DPE‐3040‐A‐00‐5064‐00 and DPE‐3061‐A‐00‐1029‐00).”s | |
| Participants | Description: Low income, first time mothers and their infants N (Randomised): 152 children Age: Infants: Infants were randomised at 16 weeks of age Mother (mean): 20.2 years % Female: 55% SES and ethnicity: “Subjects came from low income neighborhoods in which environmental sanitation was poor (only 60% of the households had indoor piped water). Mean household income was $120/mo.” Inclusion/exclusion criteria: Inclusion criteria: “Selection criteria were that mothers be primiparous, willing to exclusively breast‐feed for 26 wk, not employed outside the home prior to 6 mo postpartum, low income (less than $150/mo), at least 16 years old and healthy (not taking medication on a regular basis), and that infants be healthy, term, and weigh at least 2000g at birth.” Exclusion criteria: “Multiparous and working mothers were excluded because the intervention required a 3‐d stay in the La Leche League unit on three occasions to measure breast milk intake.” Recruitment: “Subjects were recruited from two public hospitals in San Pedro Sula, Honduras” Recruitment rate: 86% (152/176) Region: San Pedro Sula, Honduras | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Solid foods: 42 Solid foods + maintenance: 39 Exclusive breast‐feeding: 42 Description of intervention: Solid foods: introduction of solid foods at 4 months, with breast‐feeding as required 4‐6 months. Solids foods + maintenance: introduction of solid foods at 4 months, with mothers told to continue breast‐feeding as often as they had prior to the intervention. Exclusive breast‐feeding: exclusive breast‐feeding to 6 months; no other liquids (water, milk, formula) or solids In addition all mothers: 1. Stayed at the la Leche League unit at 16 weeks for 3‐days and returned to the unit at weeks 21 and 26 weeks for repeated measurements. 2. Received weekly home visits during the intervention period to collect data on breast‐feeding and infant morbidity. In the solid food groups these weekly visits also were used to monitor use of the foods provided and encourage mothers in the maintenance group to maintain their re‐intervention breast‐feeding frequency. Duration: 2 months Number of contacts: 13 (10 weekly home visits + 5 hospital visits) Setting: Home + hospital Modality: Face‐to‐face Interventionist: Mothers Integrity: “To encourage compliance with study procedures, mothers recorded the number of breastfeeds each day from 16 to 26 weeks on a simple form provided weekly. This was especially important for the SF‐M mothers, who were asked to maintain breastfeeding frequency. At 19 and 24 weeks, 12‐hour in‐home observations were conducted to record breastfeeding frequency and duration, and adherence to the feeding instructions.” Date of study: Recruited from October 1991‐January 1993 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of fruit (grams): “the amount of food offered and consumed at the midday meal was measured (using an electronic scale, to the nearest gram)” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 9 and 12 months Length of follow‐up post‐intervention: 2.5 and 5.5 months Subgroup analyses: None Loss to follow‐up (at 9 and 12 months): Unclear ‐ states “for a subsample of infants, n=60 at 9 months and n= 123 at 12 months” Analysis: Unknown if sample size calculation was performed | |
| Notes | First reported outcome (frequency of consuming fruit) at 9 months for the < 12 months was extracted for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: primary outcome not stated, fruit or vegetable consumption was not first reported outcome (first reported outcome was dairy). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "At 16 wk, subjects were randomly assigned, by week of infant's birth, to one of three groups: 1) Control: Exclusive breast‐feeding to 26 wk (EBF); 2) Solid Foods: Introduction of solid foods at 16 wk (SF), with ad libitum breast‐feeding; or 3) Solid Foods‐M: Introduction of solid foods at 16 wk (SF‐M), with mothers told to continue breast‐feeding as often as they had prior to the intervention.” Allocated to group by week of birth. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed from those conducting the research. |
| Blinding of participants and personnel (performance bias) | High risk | ”Subjects were not informed of their assignment until they had completed the first 16 wk of the study.” “All women were visited weekly during the first 4 mo postpartum to assist them in maintaining exclusive breast‐feeding.” Due to the nature of the intervention, both participants and personnel were aware of group allocation after 16 weeks. |
| Blinding of outcome assessment (detection bias) | High risk | “During the 9‐ and 12‐mo visits, the amount of food offered and consumed at the midday meal was measured (using an electronic scale, to the nearest gram) for a subsample of infants (n = 60 at 9 mo, n = 123 at 12 mo), and their mothers were interviewed regarding the infants' usual daily food intake and acceptance and frequency of consumption of a variety of common foods.” It is unclear whether outcome assessors visiting the home were aware of group allocation. Mothers self‐reported food intake and acceptance. |
| Incomplete outcome data (attrition bias) | Unclear risk | “Home visits were conducted for a subsample only (total n=141). 9mth n=60; 12 mth n=123.” Unclear if this is actual subsample or if this reflects attrition/non‐response It is unclear whether the n value for the subsample represents everyone who was eligible (i.e. had infants younger than 12 months prior to May 1993) with 100% consent rate, or if there were refusals. |
| Selective reporting (reporting bias) | Unclear risk | There is no trial registration or protocol. |
| Other bias | Unclear risk | It is unclear how the women were recruited, what the consent rate was, or how representative the sample was of the target population. |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "This research was supported by a grant from the Medical Research Council National Prevention Research Initiative." | |
| Participants | Description: 422 children in reception (4 to 5 years) and Year 1 (5 to 6 years) from 16 classes in 8 schools. N (Randomised): 16 classes, 472 children % Female: 47% female Age: Reception: 4 to 5 years (N = 216) Year 1: 5 to 6 years (N = 206) SES and ethnicity: “To ensure adequate representation of children from families of low socioeconomic status, we selected schools in which the proportions of pupils who were eligible for free school meals, who spoke English as a second language, and who came from minority ethnic backgrounds were above the national average." No individual child data on these variables were reported. Inclusion/exclusion criteria: Not stated Recruitment: Recruited from 16 classes in 8 schools (492 children, 472 consented) Recruitment rate: Children: 96% (472/492) Schools: unknown Region: United Kingdom | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Exposure + tangible non‐food reward (sticker) = 99 Exposure + social reward (praise) = 106 Exposure alone = 105 Control = 112 Description of interventions: “Children in the intervention conditions (ETR, EP, EA)* were seen individually from Day 3 to Day 14 and offered a small piece of their target vegetable.” Exposure + tangible non‐food reward: “Children in the ETR condition were told that if they tasted the vegetable, they could choose a sticker as a reward.” Exposure + social reward: “Children in the EP condition were praised if they tasted the vegetable (e.g. “Brilliant, you're a great taster”) Exposure alone: “Children in the EA condition were invited to taste the target vegetable but received minimal social interaction.” Duration: 3 weeks Number of contacts: 12 exposure sessions Setting: School Modality: Face‐to‐face, exposure Interventionist: Trained researchers Integrity: “Children in the three intervention groups agreed to taste their target vegetable in most sessions" Exposure + tangible non‐food reward (sticker): M = 11.34 sessions, SD = 1.45 Exposure + social reward (praise): M = 10.45 sessions, SD = 1.94; Exposure alone: M = 9.97 sessions,SD = 2.87. “Post hoc analyses showed higher compliance in the ETR condition than in the EP or EA conditions (p < 0.05), and compliance in the latter two conditions did not differ.” Date of study: Unknown Description of control: No‐treatment control: “Children in the control group did not receive taste exposure to the target vegetable during the intervention period.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: As‐desired consumption of target vegetable (grams). “The child was then invited to eat as much of the vegetable as he or she wanted, with intake (in grams) assessed by weighing the dish before and after consumption using a digital scale” (NB. “Care was taken to ensure that children in the ETR condition understood that the sticker reward was no longer available.”) Length of follow‐up from baseline: Acquisition data: day 15 Maintenance data: 1 month and 3 months later Subgroup analyses: None Loss to follow‐up (at 1 month and 3 months follow‐up): Exposure + tangible non‐food reward (sticker): 7%, 9% Exposure + social reward (praise): 8%, 5% Exposure alone: 8%, 8% Control: 11%, 6% Analysis: Analysis adjusted for clustering“Clustering by school was minimal; therefore, the final analyses adjusted only for clustering by class." Sample size calculation was performed "On the basis of evidence that 10 exposures are needed to alter preferences, we decided to repeat all analyses for a restricted subset of children who tasted their target vegetable on at least 10 days (n=365). Because there were no significant differences between the restricted and the full samples, results are reported for the full sample." | |
| Notes | Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit and vegetable intake 2nd listed outcome after liking | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Contact with the author indicated that the study used blocked randomisation performed using an online randomiser programme |
| Allocation concealment (selection bias) | Unclear risk | Randomisation occurred prior to consent. Head teachers were not aware of group allocation. It is unclear if study personnel knew of allocation. |
| Blinding of participants and personnel (performance bias) | Low risk | Contact with the author indicated that personnel were not blind to group allocations and that there was the potential that participants became aware of group allocation. However, given the objective outcome measure, review authors judged that the outcome would not be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Contact with the author indicated that some, but not all of the outcome assessors were blind to group allocation. The outcome measurement (grams of target vegetable consumed, as measured by a digital scale) was objective and unlikely to have been influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Low risk | Although reasons for missing data were not provided by group, rates of loss to follow‐up were low and similar across all experimental arms of the trial at both follow‐up points (Exposure+sticker = 6.5%, 8.8%; Exposure+praise = 8.2%, 5.0%; Exposure alone = 8.2%, 8.2%; Control = 10.9%, 5.7%, provided by the author). No reasons were reported for loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement Trial was registered, but not prospectively (ISRCTN42922680) |
| Other bias | Low risk | No further risks of bias identified |
| Methods | Study design: Randomised controlled trial – cross‐over Funding: "This project was part of a larger study funded by the Robert Wood Johnson Foundation Healthy Eating Research program." | |
| Participants | Description: Preschoolers enrolled in a Child and Adult Care Food Programme‐participating childcare centre N (Randomised): 57 children Age: Mean = 4.4 years % Female: 35% SES and ethnicity: “Among the children’s racial and ethnic backgrounds, 41.1% were non‐Hispanic black, 37.5% were non‐Hispanic white, 14.3% were Hispanic, and 7.1% were Asian. The median total family income was $33,600 (interquartile range, $19,337–$57,000).” Inclusion/exclusion criteria: “Preschool children enrolled full time were eligible for participation in the study." No explicit exclusion criteria stated for this trial Recruitment: “One large, racially diverse child care center in Connecticut was recruited for participation in the study in 2011.” Recruitment rate: 79% (57/72) Region: Connecticut (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Condition 1: the pairing of a vegetable with a familiar, well‐liked food (lunch) = 43 Condition 2: enhancing the visual appeal of a vegetable (snack) = 42 Description of intervention: “Classrooms were randomly assigned to first participate in either the intervention or control condition for lunch (condition 1) and snack (condition 2).” “The children participated in the second condition one week after the first condition for each meal.” Condition 1: “Steamed broccoli on top of the pizza” Condition 2: “Raw cucumbers arranged as a caterpillar with chive antennae and an olive eye.” Duration: 2 days (1 day per condition) Number of contacts: 2 (1 per condition) Setting: Preschool Modality: Face‐to‐face Interventionist: Teachers and researchers Integrity: No information provided Date of study: 2011 Description of control: Condition 1: “Steamed broccoli on the side of the pizza” Condition 2: “Raw cucumbers as semicircular half‐slices with chive and an olive on the side.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: The two primary outcome measures were: 1. Willingness to taste (defined as consumption of 3 grams or more of the test vegetable) and 2. Total consumption of the test vegetable (grams) “Researchers weighed the children’s meals in the center’s cafeteria in accordance with the CACFP‐recommended preschool serving sizes for all meal components before delivering them to the classrooms. After the meal was completed, researchers weighed the plate waste of meal components in the cafeteria. All weights were recorded to the nearest 0.1 g on a digital electronic balance.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: <1 day Length of follow‐up post‐intervention: Same day Subgroup analyses: None Loss to follow‐up: Condition 1 = 25% Condition 2 = 26% Analysis: Sample size calculation was performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake (objective) Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake (objective) Food was weighed to determine intake, but it is unlikely to be influenced by whether the researchers were blinded to condition |
| Incomplete outcome data (attrition bias) | High risk | Of the 57 participants 43 (75%) and 42 (74%) were present for both days of lunch and/or snack data collection respectively. Attrition > 20% for short‐term assessments |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: "College of Health and Human Development (Pennsylvania State University)" | |
| Participants | Description: Children aged 3 to 5 years with low vegetable intake N (Randomised): 24 children Age: Mean: Intervention = 3.8 years, Control = 4.0 years % Female: Intervention = 50%, Control = 50% SES and ethnicity: “The majority of the participants were white (92%) and 83.3% of mothers and 82.6% of fathers reported graduating from college and/or graduate school.” Inclusion/exclusion criteria: Inclusion criteria: children aged 3 ‐ 5 years, categorised as “at risk for obesity” based on family history, defined as having at least one parent with a body mass index > 25 and consuming 2 or fewer servings of vegetables per day (according to parent report) Exclusion criteria: pre‐existing medical conditions (including relevant food allergies) Recruitment: “recruited via flyers posted around the university community and in local newspapers and websites (e.g. Craigslist).” Recruitment rate: Unknown Region: Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 12, Control = 12 Description of intervention: “children in the treatment group (n=12) received vegetables packaged in containers decorated with their four favorite cartoon characters (selected on the first visit) and granola bars in generic packaging. All vegetable packages contained sticker incentives and children could collect stickers on a special game board and trade them for small prizes at the end of the study. This was done to simulate the concept of promotions that often come with packaged foods. Parents were in charge of deciding when children had eaten enough of a vegetable to be awarded the sticker for their game boards.” Duration: 2 weeks Number of contacts: Parents were instructed “to offer children a choice between either a vegetable or granola bar for at least three snacks and/or meals per day.” Setting: Home + lab Modality: Face‐to‐face Interventionist: Parents Integrity: “To assess compliance, parents completed daily checklists across the intervention to report when vegetables and granola bars were offered and record what children selected. In addition, parents could also report additional comments on these checklists to report other concerns or deviations. Parents were also responsible for keeping daily food diaries for children (data to be reported elsewhere). These logs were reviewed with parents during weekly home visits to assess progress.” Date of study: Recruitment August 2012 to June 2013 Description of control: “children in the control group (n=12) received weekly supplies of generic‐packaged vegetables and granola bars presented as part of a free choice at meals and snacks..” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Children’s intake of vegetables (grams), “Intake was measured as the difference between pre‐ and post‐weights of the foods provided.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 4 weeks Length of follow‐up post‐intervention: 1 week Subgroup analyses: None Loss to follow‐up: There was no loss to follow‐up Analysis: Sample size calculation was performed. | |
| Notes | First reported outcome (broccoli intake grams/day) at the longest follow‐up (4‐week follow‐up) was extracted for inclusion in meta‐analysis Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake is primary outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned to condition using a random‐number generator. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Outcome group: All/ Children’s vegetable and granola bar intake Families and researchers were not blinded to condition but it is unlikely that this influenced child consumption |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome group: All/ Children’s vegetable and granola bar intake Families and researchers were not blinded to condition and it is unclear if this had an impact on the weighing of food. The extent to which parents were compliant with instructions to return all leftovers is unknown |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: All/ 100% retention rate and so risk of attrition bias is low |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: "Research relating to this article was funded 2008‐2014 by two consecutive grants from the Australian National Health and Medical Research Council (426704, APP1021065); HJ Heinz (to KM); Meat and Livestock Australia; Department of Health South Australia; Food Standards Australia New Zealand; and Queensland University of Technology." | |
| Participants | Description: First‐time mothers with healthy term infants N (Randomised): 698 mother‐infant dyads Age: Child (mean): Intervention = 4.3 months, Control = 4.3 months Mother (mean): Intervention = 30.2 years, Control = 29.9 years % Female: Child: Intervention = 51%, Control = 50% SES and ethnicity: Mother: Education (university degree) = 59% Origin (born in Australia) = 79% SEIFA Index of Relative Advantage and Disadvantage (relative disadvantage ≤ 7th decile) = 33% Inclusion/exclusion criteria: Inclusion criteria: “Inclusion criteria were ≥18 years of age, infants >35 weeks gestation, and birth weight ≥2500 g, living in the study cities, facility with written and spoken English” Exclusion criteria: “Mother‐infant dyads will be excluded if the infant has any diagnosed congenital abnormality or chronic condition likely to influence normal development (including feeding behaviour) or the mother has a documented history of domestic violence or intravenous substance abuse or self‐reports eating, psychiatric disorders or mental health problems.” Recruitment: “A consecutive sample of first‐time mothers with healthy term infants was approached at seven maternity hospitals” “Consenting mothers were recontacted for full enrolment when their infant was four (range 2‐7) months old.” Recruitment rate: 16% (698/4376) Region: Brisbane and Adelaide (Australia) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 291, Control = 307 Description of intervention: “The first intervention module started immediately after baseline (children aged 4‐7 months) with the second module commencing 6 months after completion of the first (children aged 13‐16 months). Each module comprised six interactive group sessions (10‐15 mothers per group, total 40 groups) of 1‐1.5 hours duration, co‐facilitated by a dietitian (n=13) and psychologist (n=13). Developmentally appropriate content addressed: (i) repeated neutral exposure to unfamiliar foods combined with limiting exposure to unhealthy foods to promote healthy food preferences and (ii) responsive feeding that recognizes and responds appropriately to cues of hunger and satiety to promote self‐regulation of energy intake to need. A third theme was “feeding is parenting” and positive parenting (encouragement of autonomy, warmth, self‐efficacy).” Duration: 12 months (12 weeks duration for Modules 1 and 2 respectively, with 6‐month gap between Module 1 and 2) Number of contacts: 12 group sessions Setting: Child health clinics Modality: Face‐to‐face, group sessions Interventionist: Co‐facilitated by a dietitian and psychologists Integrity: No information provided Date of study: 2008 to 2011 Description of control: “The control group had access to universal community child health services, which, at the mother’s initiative, could include child weighing and web‐ or telephone‐based information. An important distinction was that controls did not receive anticipatory guidance but sought advice on a specific problem.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetables, “assessed using a three‐pass 24‐hour dietary recall conducted via telephone by a dietitian trained” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 20 months and 4.5 years Length of follow‐up post‐intervention: 6 months and 3.5 years Subgroup analyses: None Loss to follow‐up: Intervention = 26% Control = 19% Analysis: Sample size calculation was performed. | |
| Notes | First reported outcome (vegetable intake g/kg body weight) at the longest follow‐up < 12 months (6 months after intervention completion) and ≥ 12 months (3.5 years after intervention completion) was extracted for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, however power calculation was conducted on fruit or vegetable consumption | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned to condition using permuted‐blocks randomisation schedule generated by the Institute’s Research Methods Group, which includes this study’s statistician, all of whom will otherwise not be involved in data collection or intervention delivery |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All/ Food intake records, food preference, feeding behaviour (self‐reported) There is no blinding to group allocation of participants or personnel described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | There is no blinding to group allocation of participants described, and because self‐reported measures at high risk of detection bias |
| Incomplete outcome data (attrition bias) | High risk | There was 22% attrition at short‐term follow‐up and dropout was significantly higher in the intervention than the control group |
| Selective reporting (reporting bias) | Low risk | The measures reported in the protocol paper align with those reported in the outcome papers |
| Other bias | High risk | There were no differences according to group allocation at baseline. However at high risk of incorrect analysis as the protocol specifies that clustering within assessment clinics will be accounted for but this does not appear to have been done in any of the outcome papers |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "This work was supported by a grant from the Baden‐Württemberg Stiftung.” “F.D.B. is supported by the European Social Fund and by the Ministry of Science, Research and the Arts Baden‐Württemberg.” | |
| Participants | Description: Children aged 3 to 6 years in 18 preschools from 3 south German regions N (Randomised): 18 preschools, 377 children Age: Mean = 4.26 years % Female: 47% SES and ethnicity: Child: 32.4% came from an immigrant background Education levels (mother): Low = 16%, Middle = 56%, High = 21% Inclusion/exclusion criteria: “Pre‐schools were eligible to participate in the study if they were located in one of three predefined regions and had applied to participate in the nutritional intervention module of a state‐sponsored health promotion programme ‘Komm mit in das gesunde Boot’ (‘Come aboard the health boat’), with at least fifteen children participating.” “Children between 3 and 6 years of age attending one of the participating pre‐schools and participating in the programme were considered eligible for our study.” No explicit exclusion criteria stated for this trial Recruitment: Preschools: Selected from a group of preschools who had already “applied to participate in the nutritional intervention module of a state‐sponsored health promotion programme.” Recruitment rate: Preschool: 64% (18/28) Child: 80% (377/473) Region: 3 regions in Baden‐Württemberg (Germany) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): 202 children (not specified by group) Description of intervention: “Intervention activities consisted of familiarizing with different food types and preparation methods as well as cooking and eating meals together in groups of children, teachers and parents. One session additionally focused on healthy drinking behaviours.” Of the 15 sessions, five actively involved “parents by targeting them alone (discussions on parents’ modelling role and nutritional needs of children) or together with their children.” “Models for healthy eating within the intervention included: (i) use of nutrition experts; (ii) play acting with ‘pirate dolls’ used as props enjoying fruit and vegetables; (iii) active parental involvement; and (iv) involvement of other pre‐school peers. The exposure effect was taken into account by repeatedly offering healthy snacks like fruit and vegetables and water to the children every week.” Duration: 6 months Number of contacts: 15 sessions (1/week, 2hr per session) Setting: Preschool Modality: Face‐to‐face Interventionist: “The intervention was delivered by external nutrition experts” “Pre‐school group teachers assisted the external nutrition expert during each session to enable them to sustain intervention‐related activities after the study end.” Integrity: “Implementation rate was high with all modules delivered completely (5.0/5); no session was cancelled.” “Intervention fidelity was high with the majority of interventions delivered as planned.” Date of study: 2008 to 2009 Description of control: Waiting‐list control, “received the same intervention 6 months later than the intervention arm” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Change in child’s consumption of fruits and vegetables (portions/day) assessed using a questionnaire by parent self‐report Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 6 and 12 months Length of follow‐up post‐intervention: Immediately and 6 months Subgroup analyses: None Loss to follow‐up: “Of 348 pre‐school children, 29.6% completed all three measurements, 51.4% two measurements and 19% one measurement with 58% providing both pre‐ and post‐intervention measurements.” Individual loss to follow‐up data not reported. Analysis: Sample size calculation was performed. Analysis was not adjusted for clustering, but justification was provided. “As our data stemmed from natural pre‐school‐bound clusters of children, we first determined the extent of clustering. Intraclass correlation coefficients (ICC) on the level of pre‐schools were 0.016 and 0.014 for the primary outcomes of fruit intake and vegetable intake, respectively. With an average cluster size of 19.5 children per pre‐school, the design effect (d = 1 + (average cluster size ‐1) x ICC) did not exceed 2, allowing us to ignore the issue of clustering in our analyses.” | |
| Notes | Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake is primary outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Low risk | Preschool assignment was concealed through the use of sequentially‐numbered, sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All/ Fruit & vegetable intake (parent self‐reported survey) Due to the nature of the intervention, it was not possible to blind participants or intervention providers and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Fruit & vegetable intake (parent self‐reported survey) Parents were not blinded to group allocation and therefore the risk of detection bias is high |
| Incomplete outcome data (attrition bias) | High risk | Of 348 preschool children, 29.6% completed all 3 measurements, 51.4% 2 measurements and 19% 1 measurement, with 58% providing both pre‐ and post‐intervention measurements |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | The design effect did not exceed 2 and so the authors ignored clustering in the analyses. The impact of this on the analyses is unclear |
| Methods | Study design: Cluster‐randomised controlled trial Funding: “The study was commissioned, financed and steered by the Ministry of the Flemish Community (Department of Economics, Science and Innovation; Department of Welfare, Public Health and Family).” | |
| Participants | Description: Children attending pre‐primary and primary schools from 6 communities in Flanders, Belgium N (Randomised): 31 schools, 1589 children Age: Mean: Intervention = 4.86 years, Control = 5.04 years % Female: Intervention = 47%, Control = 55% SES and ethnicity: % Of lower SES children: Intervention = 34%, Control = 29% Inclusion/exclusion criteria: Not specified Recruitment: “All pre‐primary and primary schools in the six communities were invited to participate in the study.” Recruitment rate: Child: 49% (1589/3242) School: 64% (31/49) Region: Flanders (Belgium) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 396, Control = 298 Description of intervention: “The intervention was based on the ‘Nutrition and Physical Activity Health Targets’ of the Flemish Community clustered into: (i) increasing daily consumption of water and decreasing soft drinks consumption; (ii) increasing daily milk consumption; (iii) increasing daily consumption of vegetables and fruit; (iv) decreasing daily consumption of sweets and savoury snacks; and (v) increasing daily PA and decreasing screen‐time behaviour.” The community “Each intervention year, information brochures and posters regarding the five topics of the project were distributed through general practitioners, pharmacists, social services and at relevant community events by the regional health boards and the research team.” The schools “All intervention schools were requested to (i) implement five Healthy Weeks per intervention year (one for each cluster of topics) with a minimum 1 h of classroom time dedicated to the topic together with extracurricular activities (e.g. during the vegetables and fruits week only fruits could be brought to school as a snack; schools organized fruit and vegetable tastings), (ii) evaluate and improve their playground and snack and beverage policy, and (iii) communicate with the parents on the programme and distribute materials to the parents. The intervention started with a meeting with the teachers during which they received manuals and guidelines and an implementation plan was discussed.” The parents “The intervention materials for the parents were newly developed for the project. The parents received a poster visualizing the target messages and containing short tips regarding parenting practices and styles to encourage children to stick to the healthy eating and PA targets. Parents also received five letters, containing detailed information on the intervention topics and a website link with practical information such as tips and recipes. Based on the FFQ in the parental questionnaire, parents received a written, normative individual tailored advice on their child’s consumption of water, milk, fruits, vegetables, soft drinks and sweet and savoury snacks, and their PA and screen‐time behaviour.” The regional health boards “They contacted each school at least twice per year assisting them in selecting relevant intervention materials and supervising the implementation progress.” Duration: “The intervention was implemented over two school years (2008–2009 and 2009–2010) on different levels.” Number of contacts: Unclear (multi‐component) Setting: School Modality: Multiple (face‐to‐face, educational materials, resources (posters, brochures), letters) Interventionist: Multiple Integrity: “Process evaluation data revealed that all schools implemented the requested classroom hour. Regarding the snack and playground policy, it was clear that the requested adjustments asked for more time investment and at the time of observation, most schools did not yet meet up to the standard.” Date of study: 2008 to 2010 Description of control: No information provided | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetables (grams/day) assessed using a validated 24‐item semi‐quantitative food frequency questionnaire (FFQ) completed by parents Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 2 years Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall = 56% (not specified by group) Analysis: Did not adjust for clustering Sample size calculation was performed | |
| Notes | First reported outcome (fruit consumption grams/day) was extracted for inclusion in meta‐analysis. The reported estimate did not account for clustering, therefore we used post‐intervention data and calculated an effective sample size using ICC of 0.016 to enable inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake 2nd listed outcome after BMI | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All/ Fruit and vegetable intake (self‐reported) There is no blinding to group allocation of participants described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Fruit and vegetable intake (self‐reported) There is no mention that participants were blinded to group allocation and therefore the risk of detection bias is high |
| Incomplete outcome data (attrition bias) | High risk | 694/1589 (44%) completed 2‐year assessment. Long‐term attrition > 30% therefore at high risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | High risk | High risk of recruitment bias as communities were randomised and then schools within each community were invited to participate Unclear baseline imbalance as communities differed on nutrition and PA policy, raising awareness for these topics and health promotion expertise |
| Methods | Study design: Randomised controlled trial (as confirmed by the study author) Funding: "Grant from The Netherlands Organisation for Scientific Research (NWO)." | |
| Participants | Description: Children aged 4‐6 years from 6 primary schools in both urban and suburban districts in the Netherlands N (Randomised): 160 children Age: 4‐6 years (no mean provided) % Female: 49% SES and ethnicity: No explicit data: “The sample consisted of various socioeconomic and cultural backgrounds.” Inclusion/exclusion criteria: “Only schools without formal fruit and vegetable programs were selected.” Recruitment: Not specified Recruitment rate: Unknown Region: Urban and suburban districts of the Netherlands | |
| Interventions | Number of experimental conditions: 5 Number of participants (analysed): Interactive + congruent = 26 Interactive + incongruent = 26 Passive + congruent = 26 Passive + incongruent = 26 Baseline group = 56 Description of intervention: Children were read a picture book in a quiet room near their class. The picture book story described a main character rescuing his friend. The main character in this story is able to rescue his friend only after eating carrots to make him fit and strong. Passive vs interactive In the interactive sessions, the storyteller used a reading manual to ask children questions about the story and its characters before, during, and after the session. In the passive sessions, children were not asked any questions, but encouraged to sit quietly and listen. Congruent vs incongruent 1 book featured a product–congruent character (a rabbit), and the other featured a product–incongruent character (a turtle) Duration: 5 days Number of contacts: 5 sessions Setting: School Modality: Face‐to‐face Interventionist: Female daycare worker Integrity: No information provided Date of study: October‐December 2011 Description of control: Baseline ‘control’ group “not exposed to the book” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s proportional consumption of vegetables. “Children’s proportional product consumption was measured by dividing the number of pieces of each food eaten by the total number of pieces of foods eaten, for example: number of carrots eaten/total number of foods eaten.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 5 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: There was no loss to follow‐up Analysis: Unknown if sample size calculation was performed | |
| Notes | "Children in the experimental groups were randomly assigned to the four experimental conditions (n = 26 per cell)" whereas the children in the baseline control group were not randomised. Therefore the study was classified as a comparative effectiveness trial and we did not consider the data from the baseline control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake: Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake The experimenter counted the number of pieces of each snack eaten and therefore given it is an objective measure unlikely to be influenced by detection bias |
| Incomplete outcome data (attrition bias) | Unclear risk | There is no information about attrition provided |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: “This work was supported by a grant from the Dutch Ministry of Health, Welfare and Sport (grant number: 201400117.014.013). The Ministry's sole role was funding, and, thus, was not involved in the design, data collection, data analyses, data interpretation, and writing of the report. None of the authors had a potential conflict of interest.” | |
| Participants | Description: Children aged 2‐3 years in nursery schools in Rotterdam, the Netherlands N (Randomised): 163 children Age: Mean = 2.63 years % Female: 48% SES and ethnicity: “The sample consisted of toddlers from mostly low‐SES households with various cultural backgrounds.” Inclusion/exclusion criteria: “Only schools without formal fruit and vegetables programs were selected” Recruitment: Not specified Recruitment rate: 99% (197/199) Region: The Netherlands | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Passive with puppet: 36 Passive without puppet: 40 Interactive with puppet: 41 Interactive without puppet: 37 Description of intervention: Children were read a picture book “Rabbit’s brave rescue”. The embedded message in the book was that “eating carrots makes you strong”. Reading sessions were conducted in a quiet room within the nursery school during one workweek. The reading sessions were being held in small groups of 3‐5 toddlers, and took about 10 minutes. Reading was performed either with or without a hand puppet (hand puppets were developed that resembled the physical appearance of the main character in the picture book, ‘Rabbit’). Children allocated to the passive groups (with or without a puppet) were not asked questions during reading time and children allocated to the interactive groups (with or without a puppet) were asked questions during reading time. Duration: 4 days Number of contacts: 4 reading sessions (1 per day) Setting: Preschool Modality: Face‐to‐face Interventionist: Women with pedagogical education Integrity: The reading sessions were monitored. Date of study: Recruited in February and March 2015 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of carrots (proportion): “The proportion of consumed carrots was calculated by dividing the pieces of carrots the child had eaten by the total number of pieces of foods the child had eaten.” “Proportional scores were used, rather than absolute scores, because the proportional scores take into account the total amount of foods eaten.” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 4 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: “Children who were absent on the last reading day (n = 34), were excluded from the analyses.” “The total drop‐out was evenly spread across conditions.” Overall: 17% (not specified by group) Analysis: Unknown if sample size calculation was performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “On the first day, the storytellers picked up the children from class in order of the name list provided by the school, and randomly assigned them to one of the four reading conditions, ensuring balance in gender.” No mention of how the randomization sequence was generated. |
| Allocation concealment (selection bias) | High risk | The allocation was done by the person delivering the intervention. |
| Blinding of participants and personnel (performance bias) | Low risk | “For the reading sessions, four women with a pedagogical education were recruited and trained to perform all the different reading styles and puppetry conditions. These storytellers were teamed up with four female experimenters who observed the toddlers during the readings. With each team being allocated to a specific day of the week, all the toddlers in the study were exposed to all the storytellers and observers.” Those delivering the intervention were aware of group allocation, however this is unlikely to have impacted the outcomes. |
| Blinding of outcome assessment (detection bias) | Low risk | “The experimenter conducting the eating task was blinded to group assignment, because the reading sessions and eating tasks took place in different rooms.” |
| Incomplete outcome data (attrition bias) | High risk | Dropouts were 23% at short‐term follow‐up (in text). However in Consort flowchart, it appears that people were excluded prior to randomization. In the text it says that most were excluded due to not attending on the final measurement day. This sounds like the dropouts should be removed at the analysis/data collection stage. |
| Selective reporting (reporting bias) | Low risk | All outcomes are reported as pre‐specified in the trial registration. |
| Other bias | Low risk | No other sources of bias identified |
| Methods | Study design: Randomised controlled trial – cross‐over Funding: "European Community’s Seventh Framework Programme (FP7/2007‐2013) under the Grant agreement No. 245012‐HabEat." | |
| Participants | Description: Preschool‐aged children recruited from 3 daycare centres in Wageningen, the Netherland N (Randomised): 40 children Age: 21 to 46 months (mean = 36 months) % Female: 50% SES and ethnicity: Not specified Inclusion/exclusion criteria: Inclusion criteria: “Inclusion into the study required presence of the child at the day care‐centre for at least 2 days per week.” Exclusion criteria. “Participants were screened for food allergies and health problems (as reported by the parents)” Recruitment: “A total of 40 healthy children aged 2–4 years were recruited from 2 day care‐centres in Wageningen, The Netherlands. Participation was voluntary and parents and day care‐centres were thoroughly informed about the study. Written parental consent was given for the participating children.” Recruitment rate: Unknown Region: Wageningen (The Netherlands) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Spinach high‐energy/endive low‐energy = 15 Endive high‐energy/spinach low‐energy = 13 Description of intervention: “During the intervention period, half of the participants (n = 20) received vegetable soup flavour A low in energy content (LE) consistently paired with vegetable soup flavour B high in energy content (HE), whereas the other half of the participants received the reverse (i.e. flavour A HE + flavour B LE).” Duration: 7 weeks Number of contacts: 14 exposures (twice/week) Setting: Preschool Modality: Face‐to‐face Interventionist: Daycare leaders Integrity: No information provided Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: As‐desired consumption of vegetable soup (grams). “Consumption was measured by pre‐ and post‐weighing on a digital scale with a precision of 0.1 g.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 8 weeks and 4 and 8 months Length of follow‐up post‐intervention: 1 week and at 2 and 6 months Subgroup analyses: None Loss to follow‐up (at 2 and 6 months): Overall: 32%, 39% (not specified by group) Analysis: Sample size calculation was performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake (objective): The children and the daycare leaders were blinded to the treatment, i.e. they were unaware which product was high or low in energy and therefore low risk of performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake (objective): Outcome was pre‐post weight of soup bowl assessed by researcher. Researchers were not blinded to group allocation (as they served the soup (2 x green soups varying in energy intake)) and researcher was not present in room during consumption of soup |
| Incomplete outcome data (attrition bias) | High risk | Of 40 eligible children, 12 were excluded from data analysis due to low intake levels during the conditioning period. Of 28 children 17 (61%) completed the 6‐month follow‐up |
| Selective reporting (reporting bias) | Low risk | The primary outcomes reported in the paper align with those specified in the trial registration |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: "European Community’s Seventh Framework Programme (FP7/2007‐2013) under the Grant agreement No. 245012‐HabEat." | |
| Participants | Description: Preschool‐aged children recruited from 3 daycare centres in Wageningen, the Netherlands N (Randomised): 75 children Age: 1.9‐5.9 years (mean = 3.7 years) % Female: 50% SES and ethnicity: Not specified Inclusion/exclusion criteria: No explicit inclusion/exclusion criteria. “Participants were screened for food allergies and health problems (as reported by the parents)” Recruitment: “Parents with children in the targeted age range received an information letter and an invitation to register their child(ren) for participation via the day‐cares. Participation was voluntary and parents and day care‐centres were thoroughly informed about the study.” Recruitment rate: Unknown Region: Wageningen (The Netherlands) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Choice condition = 34 No‐choice condition = 36 Description of intervention: “Each child was exposed 12 times to six familiar target vegetables at home during dinner, which is the traditional hot meal including vegetables in The Netherlands….the choice group received two types of vegetables from which to choose, or they could choose to eat both vegetables during the meal.” Duration: 12 days Number of contacts: 12 Setting: Home Modality: Face‐to‐face Interventionist: Parents Integrity: No information provided Date of study: Unknown Description of control: “The no‐choice group received only one type of vegetable per dinner session” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: “The main outcome of the study was the children’s intake (in gram) of the vegetables. Vegetable intake was measured by weighing their plates before and after dinner (left overs).” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 12 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall = 6% (not specified by group) Analysis: Sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake (objective measure): Children’s vegetable intake was measured by weighing their plates before and after dinner (left‐overs). There is a low risk of performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake (objective measure): Children’s vegetable intake was measured by weighing their plates before and after dinner (left‐overs). There is a low risk of detection bias |
| Incomplete outcome data (attrition bias) | Low risk | 70/75 (93%) children completed the study and therefore risk of attrition bias is low |
| Selective reporting (reporting bias) | Unclear risk | The primary outcomes reported in the paper align with those specified in the trial registration. However in the trial registration the food diary is listed as a secondary outcome but the results are not reported in the outcome paper |
| Other bias | High risk | Despite random assignment, children in the no‐choice group on average liked vegetables better than children in the choice group (P < 0.01) and therefore baseline imbalance between groups |
| Methods | Study design: Randomised controlled trial – semi‐cross‐over Funding: "European Community’s Seventh Framework Programme (FP7/2007‐2013) under the Grant agreement No. 245012‐HabEat." | |
| Participants | Description: Preschool‐aged children recruited from 2 daycare centres in Wageningen, the Netherland N (Randomised): 45 children Age: 18‐45 months (mean = 32.6 months) % Female: 49% SES and ethnicity: Not specified Inclusion/exclusion criteria: No explicit inclusion/exclusion criteria. “Participants were screened for food allergies and health problems (as reported by the parents)” Recruitment: “recruited from two day‐care centres in Wageningen, the Netherlands. Parents signed an informed consent for their child’s participation.” Recruitment rate: Unknown Region: Wageningen (The Netherlands) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Parsnip crisps‐tomato ketchup/red beet crisps‐white sauce = 19 Red beets crisps‐tomato ketchup/parsnip crisps‐white sauce = 20 Description of intervention: “Half of the participants received red beet crisps combined with tomato ketchup (TK [C]) consistently paired with parsnip crisps combined with white sauce (WS [UC]). The other half of the participants received the reverse, i.e. red beet crisps + WS(UC) and parsnip crisps + TK(C).” Duration: 7 weeks Number of contacts: 14 exposures (twice/week) Setting: Preschool Modality: Face‐to‐face Interventionist: Daycare leaders Integrity: No information provided Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: As‐desired consumption of vegetable crisps (grams). “Consumption of crisps and dip sauces were measured by pre‐ and post‐weighing on a digital scale with a precision of 0.1 g.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Post‐test 1: 9 weeks Post‐test 2: 4 months (2 months after conditioning) Post‐test 3: 8 months (6 months after conditioning) Length of follow‐up post‐intervention: Post‐test 1: immediate Post‐test 2: 2 months Post‐test 3: 6 months after conditioning Subgroup analyses: None Loss to follow‐up (at 2 and 6 months): Overall: 5%, 33% (not specified by group) Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable crisps intake (objective): The children were not aware that their intake was measured or which condition they participated in and so the risk of performance bias is low |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable crisps intake (objective): The outcome was vegetable chip and dip intake (each assessed separately) by weighing amount before and after consumption. It is not clear who (i.e. researchers or daycare centre staff) weighed the chips & dip, and whether or not they were blinded. Blinding of outcome assessors unlikely to influence outcome |
| Incomplete outcome data (attrition bias) | High risk | Of the 45 children, 6 were excluded because they had no intake at all of the dip sauces. Of the remaining 39 children, 26 (67%) completed the 6‐month follow‐up. The risk of attrition bias is high |
| Selective reporting (reporting bias) | Unclear risk | The trial registration reports a secondary outcome that is not reported in the outcome paper |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: “The research leading to the results presented here received funding from the European Community’s Seventh Framework Programme (FP7/2007‐2013) under grant agreement no. 245012‐HabEat.” | |
| Participants | Description: Children aged 2‐4 years in 6 day‐care centres in Wageningen, the Netherlands N (Randomised): 103 children Age: Plain spinach (mean): 34.5 months Creamed spinach (mean): 36.1 months Spinach ravioli (mean): 35.4 months Green beans (mean): 35.8 months % Female: Plain spinach: 50% Creamed spinach: 52% Spinach ravioli: 46% Green beans: 42% SES and ethnicity: Not specified Inclusion/exclusion criteria: No explicit inclusion/exclusion criteria stated for this trial, “Participants were screened for food allergies and health problems (as reported by the parents).” Recruitment: Not specified, recruited from 6 child care centres Recruitment rate: 99% (103/104) Region: Wageningen (the Netherlands) | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Plain spinach: 26 Creamed spinach: 25 Spinach ravioli: 26 Green beans: 26 Description of intervention: “Families received a weekly vegetable parcel, including their vegetable product for one meal (main meal), cooking instructions, and a food diary. A standardized weighing scale with a precision of 1 g (Fiesta; Soehnle) was supplied to all participating families together with the first delivery of the vegetable parcel.” Duration: 6 weeks Number of contacts: 6 (once per week) Setting: Home Modality: Face‐to‐face Interventionist: Parents Integrity: No information provided Date of study: The study was conducted between September 2014 and January 2015 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: As‐desired intake of plain cooked spinach (grams): “Spinach intake was measured by weighing the bowls before and after lunch (leftovers) on a digital scale with a precision of 0.1 g.” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 7 weeks Length of follow‐up post‐intervention: 1 week Subgroup analyses: None Loss to follow‐up: “There were no lost to follow up or withdrawals” Analysis: Sample size calculations performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Children were randomly assigned to one of the four groups using a four‐block design: green beans (control), plain spinach (pure spinach), creamed spinach (diluted), and spinach ravioli (hidden). Randomization was done by a person who was not involved in study recruitment, enrollment, or assignment of participants.” No mention of how the randomisation sequence was generated |
| Allocation concealment (selection bias) | Unclear risk | There is no mention of allocation concealment. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group primary outcomes – preference and intake “Day‐care center staff members were instructed to behave as they usually did and not to alter their daily routine. The researchers were absent while children ate their spinach at lunch, to not disturb the normal daily lunch routine.” It is unclear whether the day‐care centre staff or researchers were blind to experimental group allocation. Outcome group: secondary outcomes – intake and liking "The products in the plain spinach, creamed spinach, and green beans groups were commercially available (frozen green beans [2.5 kg], frozen chopped spinach [2.5 kg], and frozen spinach a la crème [1 kg]) and were repacked in family portions and delivered frozen via the day‐care centers on a weekly basis.” It is likely parents knew their experimental group allocation and this could have affected the outcome. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group primary outcomes – preference and intake “Spinach intake was measured by weighing the bowls before and after lunch (leftovers) on a digital scale with a precision of 0.1 g (model S‐4001; Denver Instruments, and model Kern‐572; Kern & Sohn).” It is unclear whether the researchers were blind to group allocation, how the outcome assessment procedure is unlikely to have been impacted. Outcome group: secondary outcomes – intake and liking “Parents weighed the child’s vegetable portion before and after the meal to determine vegetable intake.” “After the main meal, parents completed a food diary, in which information was collected; for example, on deviations from the described procedures, dinnertime, consumption of other meal components, the child’s health status, and the child’s liking of the vegetables (parent’s perception and rated on a 9‐point scale (where 1= extremely disgusting and 9= extremely delicious).” All outcome data was collected by the parents themselves – self‐report |
| Incomplete outcome data (attrition bias) | Unclear risk | There were 10 children who had only 1 or 2 data points for intake of the 6 meals, with no reasons reported. Not enough information reported about the reasons for missing data. |
| Selective reporting (reporting bias) | Low risk | All outcomes are reported as pre‐specified in the trial registration. |
| Other bias | Low risk | No other sources of bias were identified. |
| Methods | Study design: Randomised controlled trial Funding: “C Collins is supported by a National Health and Medical Research Council Australian Career Development Research Fellowship (#6315005). K Duncanson is supported by a Clinical Education and Training Institute Rural Research Capacity Building Program Grant and New Staff Research Grant (University of Newcastle).” | |
| Participants | Description: Parents of children aged 2 to 5 years living in a rural area of New South Wales, Australia N (Randomised): 146 parents Age: Children (mean): Intervention = 4.0 years, Control = 4.0 years Parents: Younger than 30 years: Intervention = 34%, Control = 17% 30 years or older: Intervention = 66%, Control = 83% % Female: Child: Intervention = 47%, Control = 48% Parent: Intervention = 100%, Control = 99% SES and ethnicity: Parent education: Secondary = 46%, Tertiary = 55% Aboriginal: Child = 4%, Parent = 2% Inclusion/exclusion criteria: Inclusion criteria: “Inclusion criteria were eldest child in family ages 2 to 5 years, without a chronic health condition that affected dietary intake.” Exclusion criteria: “A child was excluded if he or she had a chronic disease, such as coeliac disease or a food allergy that has a significant effect on dietary intake. The eldest child within the eligible age range was selected as the study child for consistency and simplicity.” Kids were also excluded if they began primary school Recruitment: “parents of young children were recruited from child care facilities in 5 rural, low socioeconomic localities in NSW, Australia.” Recruitment rate: Parent: 81% (146/180) Region: New South Wales (Australia) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 45, Control = 43 Description of intervention: “The intervention involved dissemination of the Tummy Rumbles interactive CD (16) and the Raising Children DVD (17) at baseline in September 2009, accompanied by written instructions for optimal use. The only prompt provided to parents to use the resources was a reminder note delivered by post with the 3‐month follow‐up surveys. To simulate population‐level resource dissemination, further prompting of parents was not conducted.” “The tummy rumbles interactive nutrition education CD is a self‐directed resource for childcare staff and parents, Raising children is a guide to parenting from birth to 5” Duration: 12 months Number of contacts: DVD and CD played at parents' leisure, 1 contact from researchers at 3 months by phone Setting: Home Modality: DVD/CD Interventionist: N/A (provision of DVD) Integrity: “Intervention group participants were considered to have adhered to the study protocol if they reported using both Tummy Rumbles and Raising Children for at least 1 hour each during the intervention period.” Date of study: September 2009 to September 2010 Description of control: Wait‐list control,“ A generic nutrition brochure and the Active Alphabet physical activity resource were distributed to the control group to simulate real‐life exposure to control resources and facilitate retention and blinding of the control group. Tummy Rumbles and Raising Children were provided to the control group at trial completion.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetables (servings) assessed using a semi‐quantitative food frequency questionnaire (FFQ), the Australian Toddler Eating Survey (ATES) completed by parents Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 3 and 12 months Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up (at 3 and 12 months): Intervention = 17%, 40% Control = 24%, 39% Analysis: Sample size calculation was performed. | |
| Notes | First reported outcome (serves fruit/day) at 3‐month follow‐up was for inclusion in the short‐term meta‐analysis and 12 month follow‐up for the ≥ 12 months meta‐analysis. Additional data were provided by the author to allow pooling in meta‐analysis Sensitivity analysis ‐ primary outcome: Primary outcome not stated, power calculation conducted fruit or vegetable intake | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random sequence was created by computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed given that sequentially‐numbered unopened returned baseline survey envelopes were matched with computer‐generated random numbers |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were blinded to group allocation throughout the trial |
| Blinding of outcome assessment (detection bias) | Low risk | Participants were blinded to group allocation throughout the trial. The protocol indicates that assessors of the main outcome measures were blinded to participant group allocation |
| Incomplete outcome data (attrition bias) | High risk | Short‐term attrition was 21% and long‐term attrition was 40%. No imputation of missing data was carried out |
| Selective reporting (reporting bias) | Low risk | The primary outcomes published in the protocol align with the results reported in the outcomes paper |
| Other bias | High risk | There were no differences at baseline in parent and child characteristics except for % of parents older than 30 years. There is no mention that this was adjusted for in the analysis |
| Methods | Study design: Randomised controlled trial Funding: "The recruitment of the Gemini cohort was funded by a grant from Cancer Research UK (no. C1418/A7974), and the design and production of the packs used in this study was funded by Weight Concern (registered charity no. 1059686)." | |
| Participants | Description: Families with 3‐ to 4‐year‐old children from a larger cohort study (the Gemini study) N (Randomised): 1006 families Age: Child (mean): Intervention = 3.9 years, Control = 3.8 years Parent (mean): Intervention = 38.0 years, Control = 37.3 years % Female: Child: Intervention = 49%, Control = 50% Parent: not specified SES and ethnicity: Maternal education (below university level): intervention 49%, control = 49% Inclusion/exclusion criteria: Not specified Recruitment: “Participants were families with 3‐ to 4‐year‐old children from the Gemini study, a cohort of 2,402 families with twins born during 2007 in England and Wales. Currently active families (n=2,321) were sent information about a study to test a method of increasing children’s acceptance of vegetables” Recruitment rate: Families: 43% (1006/2321) Region: England and Wales | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 98, Control = 123 Description of intervention: “The intervention pack contained an exposure instruction leaflet, progress charts, and stickers. The exposure instructions asked parents to offer the child a single very small piece of their target vegetable every day for 14 days, allowing the child to choose a sticker as a reward if they tried it. They were asked to do this separately with each child and outside mealtimes.” Duration: 14 days Number of contacts: 14 Setting: Home Modality: Face‐to‐face Interventionist: Parents Integrity: “Among the 175 returned (89%), the mean number of exposure sessions was 13.8 (range=11 to 14), and children tasted their target vegetables a mean of 12.4 times (range=0 to 14). Children complied with the intervention by trying their target vegetable on an average of 90% (range 0% to 100%) of the exposure days during the experiment phase.” Date of study: Unknown Description of control: Received no intervention, “Control families were sent the intervention materials on completion of the study.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s intake of the target vegetable (number of pieces). Parents “recorded the number of pieces (including half‐pieces) of vegetable the child ate; this comprised the intake measure.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 14 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Intervention = 68% Control = 68% Analysis: Unknown if sample size calculation was performed | |
| Notes | Mean and SEM were estimated from a study figure using an online resource (Plot Digitizer: plotdigitizer.sourceforge.net) for intervention and control groups at the end of the experimental phase (T3). Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake is listed as primary outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Vegetable intake: There is no mention that the parents were blinded and they were cutting and offering the pieces to the child and this could have influenced performance |
| Blinding of outcome assessment (detection bias) | High risk | Vegetable intake: There is no mention that the parents were blinded and they were cutting and offering the pieces to the child and so at high risk of detection bias |
| Incomplete outcome data (attrition bias) | High risk | 472 (47%) out of the 1006 randomised returned the outcome data sheets and therefore high risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There are secondary outcomes reported in the trial registration that are not presented in the outcomes paper |
| Other bias | High risk | Children in the intervention group had significantly lower intake and liking than the control group at baseline (i.e. baseline imbalances) |
| Methods | Study design: Randomised controlled trial Funding: "This research is supported by European Community’s Seventh Framework Programme (FP7/2007‐2013) under the grant agreement no. 245012‐HabEat. The purees offered to participants in this study and the artichoke and peach purees used as a test food were donated by Danone Nutricia Research." | |
| Participants | Description: Mothers and their 4‐ to 6‐month‐old infants in the UK, Greece and Portugal N (Randomised): 146 parent‐infant dyads Age: Infant (mean): Intervention = 39.0 weeks, Control = 38.9 weeks Mother (mean, at child’s birth): Intervention = 33.0 years, Control = 32.7 years % Female: Infant: 52% SES and ethnicity: Education (below university) = 27% Inclusion/exclusion criteria: “Mothers were eligible to participate if they were over 18 years old at recruitment, they were sufficiently proficient in each country’s respective native language to understand the study materials and their infant was born after 37 weeks’ gestation, without diagnosed feeding problems.” Recruitment: “Women in the final trimester of their pregnancy and mothers of infants aged less than 6 months were recruited from antenatal clinics (n 327), primary care, paediatricians and hospitals in London (UK), Athens (Greece) and Porto (Portugal) to a larger study exploring children’s fruit and vegetable acceptance during weaning.” Recruitment rate: Mothers: 45% (146/327) Region: London (UK), Athens (Greece) and Porto (Portugal) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 71, Control = 68 Description of intervention: “In the intervention group, a researcher or health professional explained to the participant: (1) the importance of introducing vegetables early in the weaning process, (2) the beneficial effects of offering different single vegetables each day, (3) the techniques of exposure feeding, (4) interpreting infants’ facial reactions to food and (5) the need for persistence when an infant initially rejects a food. “five vegetables were selected as the first foods to be introduced. They were asked to offer the five vegetables in a sequence over 15 d as follows: A,B,C,D,E, A,B,C,D,E, A,B,C,D,E and to record progress on a chart provided. For a further 5 d, participants were told to continue to offer vegetables, but in addition, to start to introduce additional age‐appropriate foods.” Duration: 20 days (15 days exposure, 5 days veg plus other foods) Number of contacts: 20 (15 veg feeding exposures, 5 veg plus other food exposures) Setting: Home or health facility Modality: Face‐to‐face + leaflet Interventionist: Parent Integrity: “Completed intervention charts were returned by 86% of intervention families (UK; 100 % (28/28), Greece; 100 % (16/16), Portugal; 63% (17/27)). Completed charts revealed that over the 15‐d intervention period, parents recorded their infants consuming vegetables on 89% (mean 13·3 (SD 3·0)) of the fifteen possible eating occasions.” Date of study: February 2011 and July 2012 Description of control: Received no intervention, ‘usual care’ | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Infant consumption of fruits and vegetables (serves/day). “Mothers reported separately on the frequency of fruit and vegetable servings they had consumed in the past week and the data were recoded to provide an estimation of the total number each of fruit and vegetable portions consumed daily.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 1 month Length of follow‐up post‐intervention: 2 weeks Subgroup analyses: None Loss to follow‐up: Intervention = 5% Control = 4% Analysis: Sample size calculation was performed. | |
| Notes | First reported outcome (vegetable intake) was extracted for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit and vegetable intake 1st listed outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised to experimental group using a block randomisation matrix created by an independent statistician |
| Allocation concealment (selection bias) | Unclear risk | Allocation was revealed to the researcher, but unclear how or when |
| Blinding of participants and personnel (performance bias) | High risk | Infant’s consumption of novel vegetable: Mothers offered and fed the vegetable to infants. Given the nature of the intervention, parents in the intervention arm were not blinded and therefore this could have influenced performance |
| Blinding of outcome assessment (detection bias) | Unclear risk | Infant’s consumption of novel vegetable: The outcome was weighed, but it is not clear who weighed the food (mother who fed the child, or researcher who observed the mother feeding the child). The researcher who was present during outcome assessment was the same researcher who delivered the intervention to the mother. The impact on detection bias is unclear |
| Incomplete outcome data (attrition bias) | Low risk | 139/146 (95%) completed the follow‐up and therefore low risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Cluster‐randomised controlled trial Funding: “This work was funded by an investigator‐initiated grant to J.O.F. from the Clorox Company, which owns the Hidden Valley, The Original Ranch brand of dressing used in this research. The authors attest to having full scholarly authority over this work and responsibility for the research design and methods, the integrity of the data, the analyses, and the interpretation of the findings.” | |
| Participants | Description: Preschool‐aged children in Head Start classrooms and their parent N (Randomised): 155 parent‐child dyads Age: Child: 3 to 5 years (mean = 4 years) Parent: not specified % Female: Child: 48% Parent: not specified SES and ethnicity: “predominately Hispanic (88%) children” “Of participating parents, close to a majority (n=89) reported being married and slightly greater than one‐third (n=51) reported schooling beyond high school.” Inclusion/exclusion criteria: No explicit inclusion criteria stated for this trial Exclusion criteria: “Exclusion criteria included severe food allergies and/or other medical conditions (e.g., diabetes) that might influence the ability to participate in an as‐desired snack and absences at 75% or more of the vegetable exposure trials.” Recruitment: “To achieve a target sample size of 37 children per experimental dip condition, eight preschool classrooms within three Head Start Centers were approached to participate. Parents of 166 children were sent letters to request written consent for their own and their child’s participation in the study.” Recruitment rate: Parent‐child dyads = 93% (155/166) Region: Houston, TX (USA) | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Plain = 39, Regular = 39, Light = 36, Sauce = 38 142 parents (not specified by group) Description of intervention: “At each trial, raw broccoli was presented with 2% milk (8 oz [246 g]) to children in the condition to which they were assigned. Children were instructed to eat as much or as little as desired.” Plain: “broccoli was served without dressing.” Regular: “broccoli was served with 2.5 oz of a regular ranch‐flavored salad dressing.” Light: “broccoli was served with 2.5 oz of a reduced‐energy/fat ranch‐flavored salad dressing.” Sauce: “2.5 oz of the regular dressing was mixed together with broccoli as a sauce” Duration: 7 weeks Number of contacts: “Thirteen exposure trials (twice per week) took place in children’s classrooms across a 7‐week period.” Setting: Preschool Modality: Face‐to‐face Interventionist: Trained research staff Integrity: No information provided Date of study: 2008 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of target vegetables (broccoli) (grams) with/without dressing/sauce. “Weights of broccoli, milk, and the salad dressing (except in the plain condition) were recorded to the nearest 0.1 g once a stable reading was indicated using a calibrated, research grade digital electronic balance before and following the snacks. In the sauce condition, broccoli and the dressing intakes were estimated from the amount of the mixture consumed based on the proportionate contributions of each to the total pre‐weight.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 7 weeks Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall = 2% (not specified by group) Analysis: Adjusted for clustering Sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | (Authors describe as a quasi‐experimental design although appear to have randomised classrooms). Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | (Authors describe as a quasi‐experimental design although appear to have randomised classrooms). There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake (objective): Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake (objective): Objective measure of child’s vegetable intake and whether those who weighed the food were blinded is unlikely to have an impact on detection bias |
| Incomplete outcome data (attrition bias) | Low risk | 152/155 (98%) completed the study and therefore risk of attrition bias is low |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | There is insufficient information about baseline imbalances and whether clustering was adjusted for in the analyses |
| Methods | Study design: Randomised controlled trial Funding: “This work was supported by National Institutes of Health grant HD37119. Dr Forestell was the recipient of a Canadian Institutes of Health research postdoctoral fellowship.” | |
| Participants | Description: Children aged 4‐8 months and their mother N (randomised): 45 mother‐infant dyads Age: Infant (mean): green bean group = 5.6 months, green bean/peaches group = 5.9 months Mother (mean): green bean group = 32.2 years, green bean/peaches group = 31.6 years % Female: Infant: green bean group = 38%, green bean/peaches group = 52% SES and ethnicity: Years of schooling (mean): green bean group = 14.7 years, green bean/peaches group = 14.8 years Inclusion/exclusion criteria: Inclusion criteria: infants had to be born at term, healthy, currently aged between 4 and 8 months and had been weaned to cereal with very little experience with fruits and vegetables. Recruitment: “….recruited through advertisements in local newspapers, breastfeeding support groups, and the Supplemental Nutrition Program for Women, Infants, and Children in Philadelphia, Pennsylvania.” Recruitment rate: Unknown Region: Pennsylvania, USA | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Green bean group: 12 Green bean/peaches group: 26 Description of intervention: Green bean group: fed greens beans throughout the 8‐day home exposure period. Green bean/peaches group: fed greens beans and then within 1 h peaches throughout the 8‐day home exposure period. Both groups were fed green beans in the lab on days 1 and 2 and peaches on days 11 and 12. Duration: 12 days Number of contacts: 12 exposures (8‐day home exposure + 3 lab exposures/test days) Setting: Home + lab Modality: Face‐to‐face Interventionist: Mother Integrity: “To increase compliance, telephone contact was made with the mothers, who recorded the time of day and types and quantities of foods and liquids they fed their infants throughout the study. All of the mothers complied with these instructions.” Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of green beans and peaches (grams) assessed by weighing the amount of the food in the jar before and after consumption Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 12 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Green bean group: 25% Green bean/peaches group: 10% Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Infants were assigned randomly to 1 of 2 treatment groups.” It is unclear how randomisation occurred. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed from those conducting the research. |
| Blinding of participants and personnel (performance bias) | Unclear risk | “One group (group GB) was fed green beans, whereas the other (group GB‐P) was fed green beans and then (within 1 hour) peaches throughout the 8‐day home‐exposure period (days 3–10).” “To increase compliance, telephone contact was made with the mothers, who recorded the time of day and types and quantities of foods and liquids they fed their infants throughout the study.” |
| Blinding of outcome assessment (detection bias) | High risk | “Mothers fed at their customary pace until the child rejected the food ≥ 3 consecutive times or finished 2 jars of food.” Due to the nature of the intervention, mothers would have been aware of the infant’s group allocation, and this may have impacted the results. |
| Incomplete outcome data (attrition bias) | High risk | “Four infants were excluded from the analyses of green bean acceptance (4/16)and 3 from those of peach acceptance (3/29) because mothers were non‐compliant with test procedures (n=2), infants were sick during testings or exposure (n=2), or infants ate the maximum amount of food offered during their initial exposure (n=3)” |
| Selective reporting (reporting bias) | Unclear risk | There is no trial registration or protocol. |
| Other bias | Low risk | None identified |
| Methods | Study design: Randomised controlled trial Funding: “Supported by grants HD37119 and HD08428 from the National Institutes of Health and by a grant from the Gerber Companies Foundation. The Gerber Products Company supplied the baby foods used in this study.” | |
| Participants | Description: Mothers with healthy, term infants N (Randomised): 48 mother‐infant dyads Age: Infant (mean): carrot group = 4.6 months, potato group = 4.5 months, variety group = 4.8 months Mother (mean): carrot group = 27.4 years, potato group = 25.4 years, variety group = 29.9 years % Female: Infant: carrot group = 50%, potato group = 50%, variety group = 50% SES and ethnicity: “The racial background of the mothers and their infants was 45.8% African American, 39.6% white, 2.1% Hispanic, and 12.5% other ethnic groups.” Inclusion/exclusion criteria: Inclusion criteria: non‐smoking mothers, began feeding cereal to their infants in the past month and planned on introducing other solid foods during the next few weeks, and only mothers of formula‐fed infants. Recruitment: “recruited from advertisements in local newspapers and from Women, Infant and Children programs in Philadelphia.” Recruitment rate: Unknown Region: Philadelphia, USA | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Carrot group: 16 Potato group: 16 Variety group: 16 Description of intervention: Carrot group: during the home exposure period infants were fed pureed carrots only (the target vegetable). Potato group: during the home exposure period infants were fed pureed potatoes only. Variety group: during the home exposure period infants were fed a variety of vegetables that did not include carrots (potato, squash, peas). All groups were fed pureed carrots in the lab on days 1 and 11. Duration: 11 days Number of contacts: 11 exposures (9 day home exposure + 2 lab exposures/test days) Setting: Home + lab Modality: Face‐to‐face Interventionist: Mothers Integrity: “To encourage compliance, each mother kept a daily record of what they fed their infants, and daily phone contact was made with each mother during the exposure period.” Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of pureed carrots (grams): assessed by weighing the amount of the food in the jar before and after consumption using a top‐loading balance. Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 11 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: No loss to follow‐up Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Randomly assigned to one of 3 experimental groups” not enough information reported. Randomly allocated to experimental group but the random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | No information reported There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Mothers fed their infants and there is no mention of blinding and so high risk of performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake was determined by weighing vegetables and therefore low risk of detection bias. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up – 16 dyads per group All participants recruited completed the study and therefore at low risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol is available |
| Other bias | Low risk | Low risk of other bias |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "Funding for this work was provided by National Cancer Institute (R01 CA68398)." | |
| Participants | Description: Parents and their children participating in the 'Parents as Teachers' (PAT) programme sites in rural Missouri (USA) N (Randomised): 16 PAT sites, 1658 families Age: Children: 1 to 3 y: intervention = 67%, control = 61% 4 to 6 y: intervention = 33%, control = 40% Parents: < 25 y: intervention = 28%, control = 21% 25 to 29 y: intervention = 35%, control = 33% 30 to 34 y: intervention = 21%, control = 24% 35+ y: intervention = 17%, control = 23% % Female: Children: intervention = 47%, control = 49% Parents: intervention = 99%, control = 98% SES and ethnicity: Parent ‐ Not high school graduate: intervention = 16%, control = 11% Parent ‐ College graduate: intervention = 20%, control = 25% Household income: < USD 20K: intervention = 30%, control = 25% USD 20K to 35K: intervention = 30%, control = 25% USD 35K to 50K: intervention = 13%, control = 18% USD 50+K: intervention = 28%, control = 32% Ethnicity ‐ White: intervention = 86%, control = 80% Inclusion/exclusion criteria: Not specified Recruitment: "16 PAT programs from rural, southeast Missouri were recruited into the study. Within these sites 2012 families enrolled were assessed for eligibility and willingness to participate by parent educators." PAT is a "parenting and child development program with over 3000 sites across all 50 states and 8 US territories." PAT provides free services on "an annual basis to parents at the time of pregnancy until the youngest child is 3 years of age. However, PAT extends services until the youngest child is 5 years of age in the case of underserved families, defined as single or minority parent homes, those living in poverty or low parent education. In addition, underserved families may receive additional home visits as a means of ensuring complete delivery of the curriculum." Recruitment rate: Families: 79% families PAT sites: unknown Region: Rural southeast Missouri (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 605, Control = 701 Description of intervention: Intervention families received the standard PAT program plus the 'Hi 5 for Kids' (H5‐KIDS) protocol. "H5‐KIDS was comprised of three components: a tailored newsletter, a series of home visits, and materials for the parent and child, including storybooks." Computer‐tailored nutrition newsletter "To develop the tailored newsletter, parents were first formally enrolled in H5‐KIDS and completed a pretest interview. Relevant data was then imported into an in‐house computer‐based tailoring program. Scores were calculated based on FV knowledge and intake, frequency of parental modeling, style of parenting (coercive or non‐coercive), and quality of the home food environment (FV availability). Each newsletter began with a bulleted tailored statement that included the self reported servings of FVs the parent and the child consumed per day. Additional parent data (e.g. FV knowledge, parental role modeling, non‐coercive parenting skills, FV availability) were each uniquely used to individualize messages and describe the themes of each of the four storybook sets the family would receive at their home visits. For example, if participant data indicated a parent did not eat FV in front of their child very often (< 7/week), the tailored messages would emphasize the importance of modeling FV intake in front of the child as a means of improving consumption, and provide relevant examples of how this could be accomplished. The parent was then referred to H5‐KIDS storybooks that provided examples of modeling for the child. In contrast, parents who scored appropriately in each individual area received messages of praise encouraging them to continue their behaviors. Newsletters were mailed to the parent's home at the beginning of the program." Home visits "Parent educators delivered four H5‐KIDS home visits, each of which addressed the core program areas (knowledge, parental modeling of FV intake, non‐coercive feeding practices, FV availability). Parent educators then reinforced the core content in subsequent visits. Consistent with the philosophy of the PAT program, each visit provided examples of parent–child activities designed around healthy nutrition, that the parent could use to promote the child's language and cognitive ability, and fine and gross motor skill development (e.g. having the child learn the names and colors of various FV; child assists with selecting a variety of FV for breakfast). As part of each visit, parents also received materials and informational handouts with suggestions for improving feeding practices and the food environment in the home. Consistent with the standard PAT program, each home visit was designed to allow for 60 min of contact." Sing‐a‐long storybooks with audio cassette "At each home visit children received a H5‐KIDS sing‐a‐long storybook with audio cassette tape and a coloring book. Each storybook reinforced one of the core areas of the H5‐KIDS program through the use of child friendly characters and appealing storylines presented through songs." Duration: 60 minutes per home visit Number of contacts: 4 H5‐KIDS home visits plus 5 standard PAT home visits Setting: Home Modality: Face‐to‐face via home visits Interventionist: Parent educators who received 4 hours of training on nutrition content and overview of materials Integrity: "The H5‐KIDS program was delivered in its entirety to 78% of intervention families." Date of study: 2001 to 2006 Description of control: "Parent educators deliver a standardized curriculum via at least five home visits, on‐site group activities and newsletters." ("PAT ... empowers parents ... by encouraging positive parent‐child communication and increasing parents' knowledge of ways to stimulate children's social and physical development.") | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child's daily servings of fruits and of vegetables assessed using the Saint Louis University for Kids Food Frequency Questionnaire (SLU4Kids FFQ) administered by parent telephone survey Length of follow‐up from baseline: Average time to follow‐up was 7 months (range 6 to 11 months) Subgroup analyses: Normal weight vs overweight children Loss to follow‐up: Intervention: 15% (+ 5% missing or inconsistent data) Control: 17% (+ 5% missing or inconsistent data) Analysis: Analysis was not adjusted, but justification was provided. "There was minimal impact of grouping by site on the principle measures of impact in this study (ICC child fruit and vegetable servings = 0.00095 and ICC parent fruit and vegetable servings = 0.01). Therefore, the analyses did not adjust for group." Sample size calculation was performed. | |
| Notes | The proportion of normal weight vs overweight children not reported, making it difficult to interpret the subgroup analysis. First reported outcome (fruit intake) was extracted for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake only reported outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer generated number table was used for random assignment to intervention or control." |
| Allocation concealment (selection bias) | High risk | "Families enrolled in PAT were assessed for eligibility and willingness to participate by parent educators." Contact with the author indicated that parent educators were aware of site allocation when they were enrolling participants to the trial |
| Blinding of participants and personnel (performance bias) | High risk | Study personnel were aware of allocation ‐ "Sites were not blind to assignment." Contact with the author indicated that parent participants completed a consent form which described the activities of their experimental condition, and were therefore unlikely to be blind to allocation. Given the trial outcomes were based on parental report, the review authors judged there was potential for performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Contact with the author indicated that outcome assessors were blind to group allocation |
| Incomplete outcome data (attrition bias) | Low risk | Rates of loss to follow‐up (intervention = 15%, control = 17%) and missing/ inconsistent data (intervention = 5%, control = 5%) were similar across groups. No information was provided about reasons for loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | A subgroup analysis was conducted based on child's weight status (normal vs overweight). "A final limitation of the study is the limited power to definitely assess the impact of the intervention of children within weight status subgroups." It is unclear whether the subgroup analysis was pre‐specified. |
| Other bias | Low risk | Rationale provided for not adjusting analysis for clustering. "There was minimal impact of grouping by site on the principle measures of impact in this study (ICC child fruit and vegetable servings = 0.00095 and ICC parent fruit and vegetable servings = 0.01). Therefore, the analyses did not adjust for group." No further risks of bias identified. |
| Methods | Study design: Randomised controlled trial – cross‐over Funding: "Funded by a grant from the Robert Wood Johnson Foundation Healthy Eating Research program." | |
| Participants | Description: Preschool‐aged children attending a Head Start centre in Minneapolis, Minnesota, USA N (Randomised): 57 children Age: 2 to 3 years = 51% 4 to 5 years = 49% % Female: Not specified SES and ethnicity: Child: Non‐Hispanic African‐American = 76%, Hispanic or Latina/Latino = 6%, Multi‐racial = 13%, American Indian = 4%, Non‐Hispanic White = 2% Parent education: Less than high school = 9%, High school graduate = 42%, Some college = 49% Inclusion/exclusion criteria: Not specified Recruitment: “Children in three preschool classrooms were recruited. A consent form and letter explaining the study was sent to parents.” Recruitment rate: 98% (57/58) Region: Minneapolis, Minnesota (USA) | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Overall = 53 Description of intervention: Fruit and vegetable first: “During the fruit and vegetable first experimental weeks all fruits and non‐starchy vegetables on the lunch menu were served traditional family style five minutes in advance of other menu items. Children were allowed to begin eating the fruit and vegetable items served first, with the remaining menu items (e.g. milk, entrée, side dishes) placed on the tables for traditional family style meal service five minutes following distribution of the first course. All other usual meal service practices remained the same during the fruit and vegetable first experimental condition.” Provider portioned: “During the provider portioned experimental condition, a plate was prepared for each child that contained a specific quantity of each menu item.” Duration: “Each condition was implemented for two one‐week periods over the six week period, for a total of two weeks per condition” Number of contacts: Unclear, each day of the 6‐week period (dependent on how many days children attend) Setting: Preschool Modality: Face‐to‐face Interventionist: Classroom teachers Integrity: No information provided Date of study: Unknown Description of control: Usual ‘control’ meal service: “ "During each day of the control weeks, the usual traditional family style meal service approach to serving lunch meals at the center was followed. During usual lunch meals at the center children are seated around tables, and each food item on the menu is passed around the table from child to child in serving bowls for self‐service.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetable serves (1 cup equivalents). Study staff trained and certified in conducting lunch observations recorded food intake on a meal observation form. “The lunch observation data were entered into Nutrition Data System for Research (NDSR), a dietary analysis software program.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 6 weeks Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall = 7% Analysis: Unknown if sample size calculation was performed | |
| Notes | Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit and vegetable intake is the only outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | Intake: There is no mention if children were blinded and so it is unclear how this may impact children’s vegetable intake |
| Blinding of outcome assessment (detection bias) | Unclear risk | Intake: Observers made visual estimations of food amounts to determine the amount taken but it is unclear if observers were blinded to condition. Food amounts may not be accurately estimated by observers |
| Incomplete outcome data (attrition bias) | Low risk | 3/57 (93%) completed the study and therefore the risk of attrition bias is low |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "The research leading to these results has received funding from the European Community’s Seventh Framework Programme (FP7/2007‐2013) under the Grant Agreement No. FP7‐245012‐HabEat.” | |
| Participants | Description: Children aged 2 to 3 years from 5 nurseries in the Copenhagen area and suburbs N (Randomised): 104 children (“from 5 nurseries, involving 17 groups”) Age: Mean: Mere exposure group = 27.8 months, Flavour‐flavour learning group = 27.5 months, Flavour‐nutrient learning group = 30.8 months % Female: Mere exposure group = 63%, Flavour‐flavour learning group = 42%, Flavour‐nutrient learning group = 54% SES and ethnicity: Not specified Inclusion/exclusion criteria: Not specified Recruitment: “Children aged 2–3 years were recruited for the experiment from five nurseries, involving 17 groups, in the Copenhagen area and suburbs.” Recruitment rate: Unknown Region: Denmark | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Mere exposure group = 20 Flavour‐flavour learning group = 30 Flavour‐nutrient learning group = 21 Description of intervention: Mere exposure group, exposed to unmodified artichoke puree 10 times Flavour‐flavour learning group, exposed to a sweetened artichoke puree 10 times Flavour‐nutrient learning group, exposed 10 times to an energy dense artichoke puree with added fat Duration: 4 weeks Number of contacts: 10 exposures Setting: Preschool Modality: Face‐to‐face Interventionist: Nursery staff Integrity: No information provided Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of unmodified artichoke puree (grams). “Testing took part in group rooms. The children were seated at tables where they would normally eat their lunch to mimic the natural eating environment. The purées were served in preweighted plastic cups at room temperature. The standard serving size was 100 g for artichoke and 130 g carrot. Intake was measured individually and recorded for all sessions with a precision of 1 g.” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 5 and 8 months Length of follow‐up post‐intervention: 3 and 6 months Subgroup analyses: None Loss to follow‐up (at 3 and 6 months): Mere exposure group = 9%, 38% Flavour‐flavour learning group = 21%, 9% Flavour‐nutrient learning group = 23%, 46% Analysis: Adjusted for clustering (ANOVA proc mixed models). Unknown if sample size calculation was performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake: Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake: Intake was weighed and therefore it is unlikely that this would be influenced by detection bias |
| Incomplete outcome data (attrition bias) | High risk | Of 104 children, 71 (68%) completed the 6‐month follow‐up and therefore at high risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | The groups differed in age, but age was included as a covariate to correct for the possible influence on intake. Therefore the risk of other bias is unclear |
| Methods | Study design: Randomised controlled trial ‐ within subject Funding: “This work was supported by a University of Reading Life Sciences Studentship to the first author.” | |
| Participants | Description: Families with children aged between 20 and 24 months N (Randomised): 60 parent‐child dyad Age: Child (mean): 22 months (range 20‐24 months) Parent: NR % Female: Child = 48% Parent: NR SES and ethnicity: “78% came from a household where at least one parent was educated to graduate level.” “88% of families were white" Inclusion/exclusion criteria: Not specified Recruitment: “families with children aged between 20 and 24 months were recruited from the University of Reading’s Child Development Group database” “Parents were contacted by telephone and given a brief overview of the experiment. If a parent gave consent to their participation, the child was randomly allocated to one of three initial status” Recruitment rate: 100% Region: UK | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): 57 Description of intervention: Parents were asked whether their child liked, disliked or had not tried each vegetable listed in the Vegetable Liking and Familiarity Questionnaire. For each child, two vegetables were randomly selected from those for which the parent’s responses matched the initial status set to which the child had been assigned; these became the target (exposed) and control (non‐exposed) foods for that child. Parents were sent a picture book about their child’s target vegetable ‐ the books consisted of pictures and information about the target vegetable. Duration: 2 weeks Number of contacts: 14 readings (5 min/d, 2 weeks) Setting: Home + lab Modality: Face‐to‐face Interventionist: Parents Integrity: “the last page contained a tick‐sheet reading record upon which parents were asked to note how many times they looked at the book with their child.” “According to the reading records provided by parents, children saw their book an average of 14.9 times (SD = 9.9) during the exposure phase” Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of target vegetable they had seen in their book and a non‐exposed control vegetable of the same initial status (proportion): “Amount consumed” was coded as a proportion of the portion provided, again using a 5‐point scale (0 = none, 1 = nibble, 2 = less than ½ tsp, 3 = ½ tsp, 4 = whole portion).” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 14 days (unless rescheduled) Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: 5% Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | Low risk | The likelihood of performance bias in relation to vegetable consumption is low, given the children’s age. |
| Blinding of outcome assessment (detection bias) | High risk | No blinding. The coder was not blind to the liked/disliked or target/control food on each trial and so high risk of detection bias even though a second blind coder independently coded 20% of the recorded test sessions. |
| Incomplete outcome data (attrition bias) | Low risk | There were 57/60 infants who completed the study. Attrition rate < 20% and therefore low risk of attrition bias. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol |
| Other bias | Low risk | Low risk of other bias |
| Methods | Study design: Randomised controlled trial Funding: “Funding received through the EC Seventh Framework Programme (FP7/2007‐2013) under the IAPP 230637 “VIVA: V is for Vegetable – Applying Learning theory to increase liking and intake of vegetables” | |
| Participants | Description: Mothers with infants under 12 weeks old N (Randomised): 40 mother‐infant dyads (20 intervention, 20 control) Age: Infant (mean): Intervention = 4.78 months, Control = 4.88 months Mother (mean): Intervention = 33.7 years, Control = 30.9 years % Female: Infant: 57% SES and ethnicity: Not specified Inclusion/exclusion criteria: Not specified Recruitment: “Mothers were recruited from the local community using widespread advertising within mother and baby groups and a recruitment agency.” Recruitment rate: 83% (40/48) Region: UK | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 17, Control = 18 Description of intervention: “IG infants received 12 daily exposures to vegetable puree added to milk (days 1–12), then 12 x 2 daily exposures to vegetable puree added to baby rice at home (days 13–24). Then both groups received 11 daily exposures to vegetable puree (days 25‐35). They were each given a pack containing a 35 day diary and all of the equipment and foodstuffs they would need to complete the study. They were informed that breast or formula feeding should continue as normal.” Duration: 24 days Number of contacts: 24 exposures (daily) Setting: Home + lab Modality: Face‐to‐face Interventionist: Parents Integrity: “Another possible limitation of the study was that most of the intervention was conducted at home. It is then difficult to ensure that instructions were strictly followed.” Date of study: Recruitment took place between September 2011 and May 2012. Description of control: “Plain milk and cereal were given to the control group (days 1‐24)”. | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of vegetables (grams) measured by “a small set of portable digital pocket scales (MYCO MZ‐100, Dalman) to weigh accurately intakes (i.e. by weighing bottles or bowls before and after each feed) of all feeds consumed across the day.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 35 days, 6 months and 18 months Length of follow‐up post‐intervention: Immediate Subgroup analyses: None Loss to follow‐up (immediate, 6 months, 18 months): Intervention = 15%, 25%, 45% Control = 10%, 20%, 15% Analysis: Unknown if sample size calculation was performed. | |
| Notes | First reported outcome (vegetable intake grams during laboratory session) at immediate follow‐up was extracted for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit and vegetable intake 1st listed outcome in abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Mothers were randomised to either the intervention (n = 20) or control group (n = 20) after they had consented to the study and before they had completed any questionnaires.” No information provided about the randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | No information provided about allocation concealment |
| Blinding of participants and personnel (performance bias) | High risk | The participants were aware of whether or not they were adding vegetable puree to milk and rice cereal No blinding, and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) | Unclear risk | Food intake was weighed which would be low risk. However, "the researcher and mother made a joint decision on when 3 refusals were reached". This may have impacted on outcome assessment |
| Incomplete outcome data (attrition bias) | Low risk | “Forty parents provided informed consent for their infants to take part in the study; however, complete data were collected on 36 mother–infant dyads.” For outcome of vegetable intake grams during laboratory session 17 mothers in the intervention group and 18 mothers in the control group provided data. “At 6 months follow‐up, 15 mothers in the IG completed the two feeding sessions, while 16 mothers completed them in the CG (86% return rate).” |
| Selective reporting (reporting bias) | Unclear risk | No protocol listing prespecified outcomes |
| Other bias | Unclear risk | Recruitment bias may be an issue due to the method used. Baseline table showed that groups appeared similar, so there does not appear to be a high risk of bias. However there is not enough info to determine the level of risk. “Mothers were recruited from the local community using widespread advertising within mother and baby groups and a recruitment agency between September 2011 and May 2012.” “In total, the research team made contact with 48 mothers and from this initial contact 40 mothers were screened and accepted into the study.” |
| Methods | Study design: Randomised controlled trial Funding: Not reported | |
| Participants | Description: Children enrolled in the university‐based preschool during the 2013‐2014 academic year and their parents N (Randomised): 65 parent‐child dyads Age: Intervention (mean): 5 years Control (mean): 5 years % Female: Intervention: 38% Control: 64% SES and ethnicity: Monthly income (mean): Intervention = USD 6100, Control = USD 5336 Parent education High school: intervention = 0%, control = 3%; some college: intervention = 0%, control = 6%; Bachelor’s degree: intervention = 45%, control = 55%; Graduate degree: intervention = 45%, control 30% Ethnicity Non‐Hispanic white: intervention = 84%, control = 94%; Hispanic: intervention = 3%, control = 0%; Asian: intervention = 6%, control = 0%; Biracial: intervention = 6%, control = 6% Inclusion/exclusion criteria: No explicit inclusion/exclusion criteria stated for this trial, however the children had to be enrolled in the university‐based preschool during academic year 2013‐14 and were excluded if they participated in the 2012‐2013 academic year. Recruitment: “The parent who self‐identified as most responsible for preparing the child's meals was invited to complete the surveys. Preschool personnel sent an email inviting parents to consent to participate. Consent was obtained through an online survey.” Recruitment rate: 65% (65/100) Region: USA | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 32 parent‐child dyads, control = 33 parent‐child dyads Description of intervention: Parents received a health report describing their child’s average daily fruit and vegetable consumption along with the guidelines that children should consume 5 fruits and vegetables per day. Parents were also given a standardized set of recommendations for increasing fruit and vegetable intake as well as more comprehensive recommendations for how to increase their child’s fruit and vegetable intake (i.e. a more detailed list of parent behaviours to increase consumption). Duration: 4 weeks Number of contacts: Parents received one health report Setting: Home Modality: Written materials Interventionist: Preschool personnel provided the report Integrity: No information provided Date of study: 2013‐2014 academic year Description of control: “A delayed intervention group completed the initial baseline assessment but received no intervention until after the completion of the week 4 assessment.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Children’s consumption of fruit and vegetables (servings per day): “Parents of both groups completed the NCI Fruit and Vegetable Screener Questionnaire…. This measure was adapted to ascertain fruit and vegetable consumption over the previous week to allow for more frequent measurement of intake.” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 4 weeks Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: There was no loss to follow‐up Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Participants were randomly assigned to either an intervention (n=32) or a control (n=33) group using a random number generator.” Unclear how the sequence was generated |
| Allocation concealment (selection bias) | Unclear risk | There is no mention of allocation concealment. |
| Blinding of participants and personnel (performance bias) | Unclear risk | It is unclear whether those delivering the intervention, or the parents receiving the intervention were aware of their experimental group allocation. |
| Blinding of outcome assessment (detection bias) | High risk | “Parents completed the NCI Fruit and Vegetable Screener Questionnaire as an online survey.” Child fruit and vegetable consumption assessed via parent self‐report |
| Incomplete outcome data (attrition bias) | High risk | “In study 2, 22.6%, 44.4%, and 14% of combined fruit and vegetable data were missing at times 1, 2, and 3, respectively. Missing values analysis determined that data were missing at random; thus the researchers used full information maximum likelihood estimation.” Greater than 20% missing data at two time points, with over 40% of data missing at Time 2 |
| Selective reporting (reporting bias) | Unclear risk | There is no trial registration or protocol paper. |
| Other bias | Low risk | No other source of bias was identified. |
| Methods | Study design: Randomised controlled trial Funding: "Funding for this study came from NIH grant K01DK068008 and a St. Luke's Roosevelt Hospital Pilot Award. Additional support came from the Obesity Research Center Grant" | |
| Participants | Description: Healthy children aged 4 to 5 years from diverse ethnic backgrounds N (Randomised): 19 children Age: 4 to 5 years % Female: Not specified SES and ethnicity: “from diverse ethnic backgrounds.” Inclusion/exclusion criteria: “All the children were “at risk for obesity,” based on having at least one parent with a BMI≥25 kg/m2, and they had to consume fewer than two servings of F&V per day, based on parental report during a screening phone call.” Recruitment: Not specified Recruitment rate: Unknown Region: Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 7, Control = 9 Description of intervention: “Families in both groups attended weekly, small‐group sessions with the researchers where baseline measures were taken and family‐based nutrition education was delivered.” Children in the intervention group were “given F&V in containers decorated with their favorite cartoon characters. In addition, a sticker was included inside each decorated container to simulate the practice of premiums used by the food industry; children were allowed to collect these stickers on a game board to cash in for a prize the following week.” Duration: 7 weeks Number of contacts: Weekly group sessions and offered F&V containers 3 times a day Setting: Home + Lab Modality: Face‐to‐face Interventionist: Parents and researchers Integrity: No information provided Date of study: Unknown Description of control: “Children who were in the control group received F&V in plain plastic containers throughout the study” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetables (grams, servings per day). F&V containers were stored by parents throughout the study period and taken back to the lab to be weighed Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 7 weeks Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall = 16% (not specified by group) Analysis: Unknown if sample size calculations performed. | |
| Notes | First reported outcome (grams vegetables/week) was extracted for inclusion in the meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake only outcome reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | There is not enough information to determine the sequence generation |
| Allocation concealment (selection bias) | Unclear risk | There is not enough information to determine allocation concealment |
| Blinding of participants and personnel (performance bias) | Low risk | The outcome is objective consumption of fruit & veg which is unlikely to be influenced by lack of participant & personnel blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Objective assessment (weight) of fruit and vegetable consumption therefore low risk |
| Incomplete outcome data (attrition bias) | High risk | 16/19 (84%) children completed the 7‐week study, however 3 children were excluded from the analysis. Intention‐to‐treat analysis was not used, therefore high risk of bias |
| Selective reporting (reporting bias) | Unclear risk | There is not enough information to determine if there is any reporting bias |
| Other bias | Unclear risk | There is baseline imbalance between the study groups. Children in the intervention group consumed more servings of fruit & veg at baseline. Not clear of the impact this may have had on the results |
| Methods | Study design: Cluster‐randomised controlled trial – cross‐over Funding: “Supported by NIH Grant R01‐DK082580 and USDA National Institute for Food and Agriculture Grant 2011‐67001‐30117 Program A2121‐Childhood Obesity Prevention: Transdisciplinary Graduate Education and Training in Nutrition and Family Sciences” | |
| Participants | Description: Children aged 3‐6 years enrolled in 3 childcare centres near University Park, Pennsylvania N (Randomised): 11 classrooms, 31 children Age: Overall mean = 4.4 years % Female: 49% SES and ethnicity: “Based on the 106 parents (88%) who provided family information, household incomes and education levels were above average: 69% of households had an annual income of above $50,000 and 92% of mothers and 90% of fathers had a Bachelor's degree or higher.” “The sample of children was 69% white, 21% Asian, 3% black or African American, and 7% of mixed or another race; 4% were of Hispanic or Latino origin.” Inclusion/exclusion criteria: Inclusion criteria: children had to be enrolled in participating childcare centres Exclusion criteria: children with an allergy or intolerance to the foods or milk being served Recruitment: “Children were recruited by giving letters to parents with 3‐ to 6‐year‐old children enrolled at three childcare centers near University Park, PA.” Recruitment rate: Unknown Region: Pennsylvania, USA | |
| Interventions | Number of experimental conditions: 6 Number of participants (analysed): Overall = 120 Description of intervention: Across the 6 meals (groups), all foods and milk were served at 3 levels of portion size (100%, 150%, or 200% of reference amounts) and 2 levels of energy density (100% or 142%) and were consumed ad libitum” “The experimental meal consisted of chicken (grilled breast or breaded nuggets), macaroni and cheese, a green vegetable (broccoli or peas), applesauce, ketchup, and milk.” Duration: 6 weeks Number of contacts: 6 (1 meal/week) Setting: Preschool Modality: Face‐to‐face Interventionist: Teachers and undergraduate research assistants Integrity: No information provided Date of study: “enrolled in the study from May 2013 to July 2014.” Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of vegetables (grams): “To determine the amount consumed, all foods and beverages were weighed before and after the meal in a separate room out of the children's view. Food weights were recorded to the nearest 0.1 g using digital scales” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 6 weeks Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall: 8% (11/131) Analysis: Unknown if adjusted for clustering Sample size calculations performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The order of the six conditions was counterbalanced across classrooms using Latin squares, and classrooms were randomly assigned one of the condition sequences using a random number generator.” |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed from those conducting the research. |
| Blinding of participants and personnel (performance bias) | Low risk | “Neither parents nor children were informed about the purpose of the study.” “During each meal, adults, including teachers and undergraduate research assistants who did not know the purpose of the study, were instructed to redirect conversations about food‐related topics to minimize peer influence on children's lunch intake.” |
| Blinding of outcome assessment (detection bias) | Low risk | “During each meal, adults, including teachers and undergraduate research assistants who did not know the purpose of the study” low risk. Researchers who weighed all food and drink before and after the meal. Researchers were blinded to the purpose of the study. |
| Incomplete outcome data (attrition bias) | Low risk | ”A total of 131 children from 11 classrooms at the 3 childcare centers were enrolled in the study from May 2013 to July 2014. Eleven children were excluded from the analysis because they were absent for 3 or more of the 6 experimental meals. Thus, intake data was analyzed for 120 children (61 boys and 59 girls).” No attrition is reported. |
| Selective reporting (reporting bias) | Low risk | All proposed outcomes in trial registry are reported. |
| Other bias | Low risk | No other bias was identified |
| Methods | Study design: Cluster‐randomised controlled trial Funding: Not reported | |
| Participants | Description: Children aged 2 to 5 years at 4 primary care clinics and their parent N (Randomised): 4 primary care clinics, 306 children Age: Child (mean): Intervention = 40.1 months, Control = 41.1 months Parent (mean): Intervention = 29.3 years, Control = 29.5 years % Female: Child: 47% Parent: not specified SES and ethnicity: Education: no schooling = 0.3%, Primary school = 8.9%, Junior high = 33.7%, High school = 39.3%, Professional school – 12.5%, Postgraduate = 1.7% Inclusion/exclusion criteria: Inclusion criteria: “Participants comprised children aged 2 ‐ <5 years of age whose BMI (calculated as weight in kilograms divided by height in meters squared) was above the median for age and sex (BMI z‐score 0 ‐ 3); who attended one of the participating IMSS clinics during the recruitment period for pediatric care, vaccination, or accompanying a family member; and whose parent or caregiver gave written consent to participate.” Exclusion criteria: “Families were excluded if they planned to move residences or change primary care clinics during the study period; the child had motor limitations (e.g., physical disability or delay); or required a special diet by medical indication.” Recruitment: “The project manager approached the directors of the 6 primary care clinics in Mexico City with the greatest proportion of preschoolers (approximately 5% children <5 years) to request their support for the project.” Recruitment rate: Primary care clinic = 67% (4/6) Child = 10% (306/3095) (using number of participants approached as denominator) Region: Mexico City | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 168, control = 138 Description of intervention: Intervention participants received a 6‐week curriculum focused on obesity awareness and prevention. 5 aspects dealt with throughout the 6 sessions: 1) Dietary culture, risk‐benefit practices; 2) The process of feeding acquisition/preparation/service/eating behaviours; 3) Physical activity habits; 4) Importance of weighing/measuring oneself and its meaning; 5) feedback and evaluations Duration: 6 weeks Number of contacts: 6 sessions (2 hrs a session) Setting: Primary care clinics Modality: Face‐to‐face, group sessions Interventionist: Nutritionist, nurse and health educator Integrity: Delivery of intervention: “To ensure fidelity, a small group of study staff (nutritionist, nurse and health educator) administered all intervention sessions and completed all screening, baseline and follow‐up assessments. No quantitative measure of delivery of intervention components” Attendance: “Only 52% (88 of the 168 who agreed to participate) attended ≥ 1 educational session (405 sessions attended in total). The total number of expected attendances at educational sessions was 1008 (168 participants attending 6 sessions each). Thus, compliance in the intervention group was 40% (405/1008) of total expected attendances. However, of the 88 receiving any intervention content, 67% (59/88) attended 5‐6 of the intended 6 workshops” Date of study: March 2012 to April 2013 Description of control: Usual‐care control ‐ received no intervention | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetables (servings per week), “staff assisted parents in completing a child Food Frequency Questionnaire (FFQ) adapted from the FFQ used to assess dietary intake among 1‐4 year old children in the 2006 Mexican National Nutrition Survey.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 3 and 6 months Length of follow‐up post‐intervention: 1½ and 4½ months Subgroup analyses: None Loss to follow‐up (at 1 ½ and 4 ½ months): Intervention = 41%, 35% Control = 26%, 26% Analysis: Adjusted for clustering Unknown if sample size calculation was performed | |
| Notes | First reported outcome (fruit servings/week) at the longest follow‐up < 12 months (3 months after intervention completion ‐ as 6‐months follow‐up did not report retention values by group) was extracted for inclusion in meta‐analysis The reported estimate which adjusted for clustering assessed change from baseline, we therefore used post‐intervention data and calculated an effective sample size using ICC of 0.016 to enable inclusion in meta‐analysis Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake listed as primary outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated randomisation list designed by a statistician with no connection to the intervention was used for random allocation to experimental group |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Child dietary intake (parent‐reported): “Only after informed consent did participants learn of their treatment assignment”. There is no blinding to group allocation of participants at follow‐up described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Child dietary intake (parent reported): “Only after informed consent did participants learn of their treatment assignment”. There is no blinding to group allocation of participants at follow‐up described and because self‐reported measures were used this is likely to influence detection bias |
| Incomplete outcome data (attrition bias) | High risk | “Non‐participation was greater in the intervention (75 (45%) of 168 participants) than in the usual care (42 (30%) of 138 participants) arm (Figure 1).” Attrition rate was high with >35% of families not completing follow‐up at 3 months. Multiple imputations were performed to address missing data however non‐participation was greater in the intervention than in the usual care condition |
| Selective reporting (reporting bias) | Low risk | The primary outcomes reported in the paper align with those specified in the trial registration |
| Other bias | Unclear risk | There were baseline imbalances between the groups, but results were adjusted. Unclear risk of recruitment bias as individuals were recruited to the trial after clusters have been randomised |
| Methods | Study design: Randomised controlled trial Funding: Not reported | |
| Participants | Description: Children aged 4 to 9 months and their mother N (Randomised): 88 parent‐children dyads Age: Child (mean): Study 1 fruits = 6.7 months, Study 2 vegetables = 6.3 months Mother (mean): Study 1 fruits = 29 years, Study 2 vegetables = 28 years % Female: Child: Study 1 fruits = 49%, Study 2 vegetables = 43% Parent: 100% SES and ethnicity: Parent: “Their ethnic background was 55.4% (N =41) Black; 29.7% (N =22) White; 2.7% (N =2) Hispanic and 12.2% (N =9) Other/Mixed Ethnicity.” SES not specified Inclusion/exclusion criteria: “To qualify the Children had to have at least two weeks of experience eating cereal or fruit from a spoon and little experience with the target fruits and vegetables.” Recruitment: “Seventy‐four mothers whose Children were between the ages of 4 and 9 months were recruited from advertisements in local newspapers and from Women, Children and Children Programs in Philadelphia, PA.” Recruitment rate: Not specified Region: Philadelphia (USA) | |
| Interventions | Number of experimental conditions: 5 Number of participants (analysed): Study 1: fruits Pear group = 20 dyads, between‐meal (BM) group = 19 dyads Study 2: vegetables Green bean group = 11 dyads, between‐meal (BM) group = 12 dyads, between‐meal and within‐meal (BM‐WM) group = 12 dyads Description of intervention: Study 1: fruits “During the home exposure period, one group fed only pears at the target meal (Pear Group, N=20) whereas the other group fed a fruit which was different than the one experienced during the previous 2 days (Between‐Meal (BM) Fruit Variety Group, N=19).” Study 2: vegetables “The three groups differed in the type, amount and variety of foods that infants were fed during the target meal during the 8‐day home exposure period. The infants in the Green Bean Group (N=11) were fed only the target vegetable, green beans, whereas those in the Between‐Meal variety group (BM Vegetable Variety Group, N=12) and the Between‐Meal and Within‐Meal Variety Group (BM–WM Vegetable Variety Group, N=12) were fed a variety of vegetables. The BM Variety Group was fed only one vegetable each day and green and orange vegetables were alternated daily, whereas the BM–WM Variety Group was fed two vegetables each day (one green, one orange). In the latter group, the pair of vegetables varied from day‐to‐day but one of the pair was experienced the prior day.” Duration: 8 days Number of contacts: 8 exposures Setting: Home Modality: Face‐to‐face Interventionist: Mothers Integrity: “All of the mothers complied with these instructions.” Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetable purees (grams). Mother resealed jars and returned them after the exposure period to be weighed Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 12 days (4 days of test food(s)) Length of follow‐up post‐intervention: 2 days Subgroup analyses: None Loss to follow‐up: Condition 1: fruits Overall = 15% (no specified by group) Condition 2: vegetables Overall = 17% (no specified by group) Analysis: Unknown if sample size calculation was performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | Fruit & vegetable intake: The mother fed the child and there is no mention of blinding, therefore at unclear risk of performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | The mother fed the child and there is no mention of blinding. However, this is an objective measure of intake, and therefore low risk of detection bias |
| Incomplete outcome data (attrition bias) | High risk | Mother‐infant pairs were excluded from the study because they did not comply with experimental procedures or ate less than 5 grams on the testing days. An intention‐to‐treat approach was not adopted and therefore at high risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | High risk | The groups differed significantly in the fruit study (Study 1) in terms of approachability and there is no mention that this difference was adjusted for in the analysis |
| Methods | Study design: Cluster‐randomised controlled trial Funding: Not reported | |
| Participants | Description: Children and centre directors from 4 licensed childcare centres in North Carolina N (Randomised): 4 childcare centres Age: < 3 years = 27% 3 to 5 years = 73% % Female: Child: not specified Directors: 100% SES and ethnicity: “All centers had at least some subsidized children enrolled.” Directors: “75% were African American, and 50% had a college degree.” Inclusion/exclusion criteria: “To participate in the study, centers had to provide all foods and beverages to children in care (i.e., parents could not send food from home), not have an open case of abuse or neglect with the state licensing agency, and have at least three children between the ages of three and five years in care on a regular basis.” Recruitment: “We mailed a letter of invitation to every licensed center (n = 6) in the city limits of a small community near our research offices. The letter was followed by a telephone call from the study team. We enrolled the first four centers that agreed to participate. Center directors provided written informed consent to participate in the study; parents were provided a fact sheet describing the study and were asked to contact the project director if they did not want their children observed during the dietary assessment.” Recruitment rate: Region: Central North Carolina (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): 4 childcare centres, “An average of 19.0 (7.9) children were enrolled per center” Description of intervention: “The Watch Me Grow program is a garden‐based intervention aimed to increase the number of vegetables and fruits provided to and consumed by children in child care. The intervention took place in spring 2011. The program includes a “crop‐a‐month” structured curriculum for child‐care providers, consultation by a gardener, and technical assistance from a health educator. Over the course of the four‐month‐long intervention, providers and children in the intervention centers grew (1) lettuce, (2) strawberries, (3) spinach, and (4) broccoli. We designed the garden to yield one crop per month, and provided classrooms in the intervention centers with corresponding curriculum materials highlighting the target fruit or vegetable of the month.” Duration: 4 months Number of contacts: Health educators (technical assistance): monthly Visits from study gardener: at least monthly Centre staff provided curriculum activities: 1 activity per week Setting: Preschool Modality: Face‐to‐face Interventionist: Health educator/Gardener provided intervention to childcare centres Centre Staff provided curriculum/activities to children Integrity: No information provided Date of study: 2011 Description of control: Received no intervention | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetables (mean servings, consumed by 3 children in each centre). Registered dietitians observed all meals and snacks over 2 full days and recorded all foods consumed for each of the 3 target children Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: ˜ 5 months Length of follow‐up post‐intervention: 1 month Subgroup analyses: None Loss to follow‐up: N/A: “the same three children may not have been observed pre‐ to post‐intervention.” Analysis: Did not adjust for clustering Unknown if sample size calculation was performed | |
| Notes | First reported outcome (daily vegetable servings consumed) was extracted for inclusion in meta‐analysis. No adjustment was made for clustering; we therefore used post‐intervention data and calculated an effective sample size using ICC of 0.014 to enable inclusion in meta‐analysis Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake is primary outcome as in trial registry | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “either the intervention or control condition on a 1:1 ratio, using the Research Randomizer (www.randomizer.org/form.htm)” The research randomiser was used to generate the random sequence |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Dietary observation: A trained registered dietitian blinded to treatment group conducted the dietary assessments |
| Blinding of outcome assessment (detection bias) | High risk | Dietary observation: The outcome is observation of foods served and consumed at mealtimes at the childcare centre undertaken by blinded dietitians. However, there is no blinding of childcare centre staff, cooks, children etc., because they were provided with a garden at their centre, curriculum materials and lessons, and staff met with research team about the garden and how to incorporate it into all aspects of the centre |
| Incomplete outcome data (attrition bias) | Low risk | Randomly selected a classroom and then 3 children within classroom at centres to observe pre‐ and post‐intervention; it did not need to be the same 3 children observed pre‐ and post‐intervention |
| Selective reporting (reporting bias) | Low risk | The primary outcomes reported in the paper align with those specified in the trial registration |
| Other bias | Unclear risk | “Due to sample size limitations, we did not conduct formal statistical analysis beyond comparing crude differences in mean servings of vegetables and fruits.” Insufficient information was reported to determine whether childcare centres were similar at baseline or recruitment bias. No statistical method to account for clustering, but we calculated an effective sample size prior to inclusion in meta‐analysis to account for this |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "This research was funded by the Miami‐Dade County Children’s Trust (grant number 764‐287)." | |
| Participants | Description: Children aged 2 to 5 years enrolled in 8 subsidised childcare centres in Miami‐Dade County, Florida N (Randomised): 8 childcare centres, 307 children Age: “the average age for boys was 3.82 years, the average age for girls was 3.91 years” % Female: Intervention = 49%, Control = 48% SES and ethnicity: “Thirty‐six percent identified their child as black, 34% identified their child as white, 18% chose other, and 14% were unknown. The ethnicity of the sample mirrors that of Miami‐Dade County, with 32% of the parents identifying their child as Hispanic/other, 25% as Hispanic/Cuban, 22% as African American, and 2% as Caucasian. Thirty‐five percent of the sample were primarily Spanish speaking and completed the measures in Spanish, and 65% of the sample were primarily English speaking and completed the measures in English” Inclusion/exclusion criteria: “Center study inclusion criteria consisted of (a) serve >30 children, (b) serve low‐income children, and (c) ethnic makeup had to be reflective of the county as a whole (minority majority). Low income was determined based on whether or not the child received subsidized child care.” No inclusion/exclusion criteria specified for children. Recruitment: “All participants were recruited at the child care center. Parents were approached during drop‐off or pickup times. Consent forms were attached to the interview packets, and parent data were collected during the initial visit.” Recruitment rate: 98% Region: Miami‐Dade County, Florida (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 238, Control = 69 Description of intervention: Teacher curriculum: Modeled after a modified version of Hip‐Hop to Health Jr., included implementation of lessons and a low‐fat, high fibre diet that included more fruits and vegetables with an emphasis on cultural barriers. Parent curriculum: Modeled after a modified version of the Eating Right Is Basic and Hip‐Hop to Health Jr., included a monthly educational dinner (run by dietitians) in which nutrition and physical activity were discussed, monthly newsletters, and at‐home activities, also information on how to introduce new foods and how to encourage eating more fruits and vegetables. Parents were encouraged to reduce TV viewing, increase physical activity, and model healthy eating behaviours for their child at home. Centre‐based modifications: These included: the development of policies to increase physical activity and healthy eating; modifying menus to make them compliant with the policies and also to ensure that the U.S. Department of Agriculture (USDA) nutritional requirements were met; agreeing on a drink policy that included providing water as the primary beverage, not allowing juice or sweetened beverages more than one time per week; changing from whole milk to 1% milk; having a snack policy which consisted of substituting healthy snacks, such as fresh fruit and/or vegetables, for cookies and other high‐lipid snacks; having a physical activity policy to increase physical activity to more than one hour per day and to decrease TV viewing to less than 60 minutes two times a week. Duration: 6 months Number of contacts: Unclear, multiple contacts Setting: Preschool, home Modality: Multiple (face‐to‐face, newsletters) Interventionist: Teachers, Parents and Registered Dieticians Integrity: No information provided Date of study: Unknown Description of control: “The Attention control group centers received a visit from an injury prevention education mobile. The mobile provided parents and teachers with hands‐on safety education and information, as part of an ongoing injury prevention program at the University of Miami.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetables assessed using a 16‐item food frequency questionnaire (FFQ) completed by parents and teachers Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 3, 6 and 12 months Length of follow‐up post‐intervention: Immediately and 6 months Subgroup analyses: None Loss to follow‐up (Immediately post‐intervention and 12 months): Overall = 25%, 42% Analysis: Unclear if adjusted for clustering Unknown if sample size calculation performed | |
| Notes | Sensitivity analysis ‐ primary outcome: Primary outcome not stated, BMI 1st listed outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Food intake: There is no blinding to group allocation of participants or personnel described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Food intake (parent and teacher reported): There is no blinding to group allocation of participants or personnel described and this is likely to influence detection bias |
| Incomplete outcome data (attrition bias) | High risk | Of the 318 child‐parent dyads at baseline, there were 185 (58%) at the 1‐year follow‐up |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | Some evidence of baseline imbalance (e.g. ethnicity) Unclear recruitment bias Unclear whether potential clustering within childcare centres accounted for |
| Methods | Study design: Cluster‐randomised controlled trial Funding: “This study was sponsored by the National Institutes of Health (NIH)/National Institute of Child Health and Human Development through grant number R21‐HD073608. Partial support was received from the USDA Agriculture Research Service through specific cooperative agreement 58‐6250‐0‐008.” | |
| Participants | Description: Preschool‐aged children who were predominantly low‐income African‐American and Hispanics N (Randomised): 6 Head Start centres, 253 children Age: Mean: Intervention = 4.47 years, Control = 4.38 years % Female: Intervention = 49%, Control = 52% SES and ethnicity: Hispanics: Intervention = 46%, Control = 54% African‐American: Intervention = 59%, Control = 41% Inclusion/exclusion criteria: Not specified Recruitment: “Recruitment strategies included flyers that were sent to the home with the children, presentations at parent meetings, face‐to‐face recruitment during child drop‐off and pickup at Head Start, and active involvement of the Head Start manager and staff in the recruitment process” Recruitment rate: Children: 65% (253/391) Region: Houston, TX (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 128, Control = 125 Description of intervention: The intervention included 4 DVDs (videos) theatre‐based puppet shows that aimed at persuading children to increase vegetable consumption through encouragement, rationale/reason, reinforcement, and role modelling that were delivered over 4 consecutive weeks at preschools. Additionally, "each intervention child took home a bag including the DVD video for that week, a pamphlet, main ingredients to prepare a simple vegetable snack, crayons, and a disposable camera (if parents did not have a smart phone) to use as instructed in the booklets." The intervention was “based on the theoretical framework “transportation into a narrative world”, three professionally developed characters, unique storylines and an engaging, repetitious song were incorporated in four 20‐min videotaped puppet shows.” Duration: 4 weeks Number of contacts: 6 contacts per week Setting: Preschool, home Modality: Multiple (face‐to‐face, visual/audio – DVD) Interventionist: Teachers and parents Integrity: No information provided Date of study: Unknown Description of control: “During the 4‐week intervention period the control group did not receive any alternate intervention.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of vegetables assessed using digital photography and plate weight before and after consumption (grams). Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 4 weeks + 2 days Length of follow‐up post‐intervention: 2 days Subgroup analyses: None Loss to follow‐up: No loss to follow‐up Analysis: Adjusted for clustering. Unknown if sample size calculation performed. | |
| Notes | Reported estimates accounted for clustering, but confidence intervals or other measures of variance were not available. We therefore estimated means and SDs by groups at follow‐up from a study figure using an online resource (Plot Digitizer: plotdigitizer.sourceforge.net) and calculated an effective sample size using ICC of 0.014 to enable inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome was vegetable consumption | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation was not described |
| Allocation concealment (selection bias) | Unclear risk | No information about allocation concealment is provided and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and teachers in intervention preschools were not blinded to the intervention, as children viewed a DVD, and teachers were asked to identify the vegetable components served in the lunch. It is unclear whether this resulted in performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Children’s vegetable intake was assessed using the digital photography method and plates were weighed and therefore unlikely to be influenced by detection bias |
| Incomplete outcome data (attrition bias) | Low risk | 253 children were enrolled and all of them completed the follow‐up assessment, so risk of attrition bias is low |
| Selective reporting (reporting bias) | Low risk | The primary outcomes reported in the paper align with those specified in the trial registration |
| Other bias | Unclear risk | There is potential recruitment bias, as it is not clear when or how clusters were randomised, and whether recruitment occurred before or after |
| Methods | Study design: Cluster‐randomised controlled trial – cross over Funding: “Financial support was provided by the Rudd Foundation.” | |
| Participants | Description: Children aged 3 to 6 years attending 2 private preschools in a small north‐eastern city N (Randomised): 2 preschools (number of children not specified, 96 children recruited) Age: “Age ranged from 3 to 6 years old, but most (85%) children were 4 or 5 years old.” % Female: 44% SES and ethnicity: “These preschools primarily serve highly educated households; nearly all (93%) of the children had at least one parent with a bachelor’s degree and 75% had at least one parent with a graduate or professional degree.” “Race/ethnicity was white (69%), Asian (8%), African American (5%), Hispanic (6%), and other (12%).” Inclusion/exclusion criteria: Not specified Recruitment: Not specified Recruitment rate: Unknown Region: New Haven (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 43, control = 53 Description of intervention: “During the intervention, the children at Preschool A were served one of the new vegetables every day for 30 days in a 3‐day cycle (e.g., Monday, cauliflower; Tuesday, snow peas; Wednesday, green pepper) until they had received each vegetable a total of 10 times.” Duration: 6 weeks Number of contacts: 30 (1 per day for 30 days) Setting: Preschool Modality: Face‐to‐face Interventionist: Teachers Integrity: No information provided Date of study: 2007 Description of control: Control/delayed intervention (Preschool B). “ "Preschool B continued routine practices during the first 6 weeks of the study, and then switched conditions with Preschool A for the second 6 weeks” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of new vegetables (grams). “Researchers picked up the bags of vegetables later from the schools, weighed them, and calculated intake to the nearest gram.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 12 weeks Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: No loss to follow‐up Analysis: Adjusted for clustering (multilevel modelling) Sample size calculations performed | |
| Notes | Post‐intervention data were extracted following the first phase of the trial (Time 2) prior to cross‐over. As an estimate was not reported for the Time 2 follow‐up that adjusted for clustering, we used post‐intervention data and calculated an effective sample size using ICC of 0.014 to enable inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Fruit or vegetable only outcome reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable consumption: Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable consumption: Objective measure of child’s vegetable intake and unlikely to influence detection bias |
| Incomplete outcome data (attrition bias) | Low risk | There is no reported attrition. Data from 96 children were analysed |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | High risk | Baseline imbalances were reported. There were differences in vegetable consumption at baseline |
| Methods | Study design: Randomised controlled trial Funding: "Supported by Medical Research Council/National Preventive Research Initiative grant G0701864" | |
| Participants | Description: Children aged 3 to 4 years attending nursery school and their primary caregiver N (Randomised): 173 parent‐child dyads Age: Child (mean): tangible reward = 3.96 years, social reward = 3.99 years, control = 3.90 years Primary caregiver (mean): tangible reward = 37.44 years, social reward = 37.35 years, control = 37.52 years % Female: Child: tangible reward = 48%, social reward = 54%, control = 55% Primary caregiver (mother): tangible reward = 85%, social reward = 88%, control = 77% SES and ethnicity: Primary caregiver: Ethnicity: White = 66%, Black = 2.9%, South Asian = 6% Education level: Nongraduate = 24%, Degree level of higher = 62% Inclusion/exclusion criteria: Not specified Recruitment: “Children aged 3–4 years and their primary caregivers were recruited through nursery schools in North London, United Kingdom.” “Recruitment was done in 3 waves in 2010. At each wave, teachers distributed consent forms and information letters about the “Tiny Tastes” study, and families were asked to return their contact details in a prepaid envelope if they were interested in taking part. Potential participants were then contacted by telephone.” Recruitment rate: Parent‐child dyads: 82% (173/212) Region: North London (UK) | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Taste exposure + tangible reward = 47 Taste exposure + social reward = 46 No treatment control = 47 Description of intervention: Taste exposure + tangible reward: “The parents were asked to offer their child a small piece (˜2.5g) of their target vegetable every day for 12 weekdays and to tell them that they could choose a sticker if they tried it. No tastings were done over the weekends.” Taste exposure + social reward: “Parents were asked to offer the vegetable as described above and to praise their child with phrases such as “brilliant, you're a great vegetable taster” if they tasted it. The parents were to emphasize that the praise was being given for tasting the vegetable” Duration: 3 weeks Number of contacts: 12 taste exposures Setting: Home Modality: Face‐to‐face Interventionist: Primary caregiver Integrity: “The parents were also given a diary to record whether each day’s trial was performed, whether the child tried the vegetable, and whether the reward was given; space was allowed for comment.” “No differences in the number of days that the child was offered or tried the target vegetable were found between the intervention groups” Date of study: 2010 Description of control: “Families assigned to the control group did not perform any daily tastings and were given no instructions or materials for the intervention period, but were told that they would be taught a special technique to help their child to eat more vegetables after the last visit.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of target vegetable (grams). “Intake (in g) was recorded by weighing the bowl containing pieces of the target vegetable before and after consumption with a digital scale (Mettler Toledo).” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 3 weeks, ˜ 2 months and ˜ 4 months Length of follow‐up post‐intervention: Immediately and at 1 and 3 months Subgroup analyses: None Loss to follow‐up (Immediately post‐intervention, and at 1 and 3 months): Taste exposure + tangible reward = 0%, 0%, 3% Taste exposure + social reward = 0%, 3%, 2% No treatment control = 0%, 5%, 2% Analysis: Sample size calculations performed. | |
| Notes | Data from the longest follow‐up < 12 months (3 month follow‐up) were extracted for inclusion in meta‐analysis. Estimates were reported comparing the tangible reward and control conditions, but not social reward condition. We estimated mean and SEM from a study figure using an online resource (Plot Digitizer: plotdigitizer.sourceforge.net) for all 3 groups. The tangible reward and social reward conditions were combined into a single intervention group for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake is primary outcome as per trial registry. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Low risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Consumption of target vegetable: There is insufficient information to determine the likelihood of performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Consumption of target vegetable: There is insufficient information to determine the likelihood of detection bias |
| Incomplete outcome data (attrition bias) | Low risk | The proportion that completed the follow‐up assessments is not reported and therefore the risk of attrition bias is unclear |
| Selective reporting (reporting bias) | Unclear risk | The primary outcomes reported align with those specified in the trial registration. However the secondary outcomes specified on trial registry do not appear to be reported in the abstract |
| Other bias | Low risk | There is insufficient information to determine the risk of other bias |
| Methods | Study design: Randomised controlled trial Funding: Not reported | |
| Participants | Description: Children aged 4 to 8 months old and their parent N (Randomised): 100 parent‐child dyads Age: Mean: Repeated exposure = 6.3 months, Flavour‐flavour learning = 6.6 months, Flavour‐nutrient learning = 6.2 months Parent: not specified % Female: Child: Repeated exposure = 47%, Flavour‐flavour learning = 35%, Flavour‐nutrient learning = 38% Parent: mostly mothers (exact % not reported) SES and ethnicity: Not specified Inclusion/exclusion criteria: “The criteria for children inclusion were as follows: age between 4 and 8 mo, introduction of complementary foods was started at >2 wk and <2 mo before the start of the study, no health problems or food allergies at the beginning of the study, and gestational age ≥36 wk.” Recruitment: “Parents in the Dijon area of France were recruited using leaflets or posters distributed in health professionals consulting rooms, pharmacies, and day‐care centers.” Recruitment rate: Parent‐child dyads = 81% (100/123) Region: Dijon (France) | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Repeated exposure = 32 Flavour‐flavour learning = 30 Flavour‐nutrient learning = 30 Description of intervention: “During the exposure period, infants were exposed 10 times to a basic (RE group), a sweet (FFL group), or an energy‐dense (FNL group) artichoke puree according to their group.” Duration: Approx. 41 days Number of contacts: 2 ‐ 3 times per week Setting: Home Modality: Face‐to‐face Interventionist: Parents Integrity: “parents were given precise instructions, and data collected in the notebook revealed that they complied with the instructions.” Date of study: October 2010 and May 2011 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of varied artichoke purees (grams). “To measure intake, parents were asked to weigh each jar before and after consumption, using a digital kitchen scale (61 g, Soehnle) that we provided them with, and to record the weight in a notebook. After each observation, parents were required to reseal the jar(s) of food, freeze them, and bring the used jars back to the laboratory to check compliance with the study procedure and data accuracy.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Unclear Length of follow‐up post‐intervention: 2 weeks, 3 months and 6 months Subgroup analyses: None Loss to follow‐up (at 2 weeks, 3 and 6 months): Overall = 5%, 7%, 8% Analysis: Sample size calculations performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake: The interventions are all artichoke puree with different nutrient content. Parents would be unable to determine study group from feeding the child, and therefore this would be unlikely to influence the outcome |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake: This is objective assessment. Parents would be unable to determine study group from feeding the child, and therefore this would be unlikely to influence the outcome |
| Incomplete outcome data (attrition bias) | High risk | 5 families dropped out during the exposure period and were excluded. An intention‐to‐treat approach was not used and therefore at high risk of attrition bias |
| Selective reporting (reporting bias) | Low risk | The outcomes reported in the paper align with those specified in the trial registration |
| Other bias | Unclear risk | The groups differed significantly in relation to weaning, but this was adjusted for in analyses. Therefore the risk of other bias is unclear |
| Methods | Study design: Cluster‐randomised controlled trial – cross‐over Funding: "Supported by NIH grant R01 DK082580" | |
| Participants | Description: Children 3 to 5 years attending the Bennett Family Center on campus at The Pennsylvania State University Age: Mean: 4.4 years % Female: 52% SES and ethnicity: “The children were racially diverse: 56% were white, 29% Asian, 11% black or African American, and 4% Pacific Islander.” Inclusion/exclusion criteria: No explicit inclusion criteria stated for this trial Exclusion criteria: “Children who were allergic to any of the foods to be served at the snack were not included in the study.” Recruitment: “Participants in the study were recruited by distributing letters to parents of children in 4 classrooms of the childcare facility that included children aged 3–5 y; these classrooms had a total of ˜75 children present at snack time.” Recruitment rate: Unknown Region: Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 8 Number of participants (analysed): Overall = 61 Description of intervention: Variety type serve: 1 x occasion: a variety of all 3 vegetables offered (cucumber, sweet pepper, tomato) 1 x occasion: a variety of all 3 fruits offered (apple, peach, pineapple) Single‐type serve: 3 x occasions: a single type of vegetable offered (cucumber, sweet pepper, tomato) 3 x occasions: a single type of fruit offered (apple, peach, pineapple) Duration: 4 weeks Number of contacts: 8 Setting: Preschool Modality: Face‐to‐face Interventionist: Childcare helper Integrity: No information provided Date of study: February to April 2011 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetables (number of pieces). “The number of pieces of vegetables or fruit selected by each child in the study was recorded independently by 2 observers seated near each table.” “After the meal, the number of uneaten pieces on each child’s plate was recorded as well as any dropped pieces. All uneaten food and beverage items were weighed after the meal with digital scales (models PR5001 and XS4001S; Mettler‐Toledo Inc).” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Unclear Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: No loss to follow‐up Analysis: Unclear if adjusted for clustering Unclear if sample size calculations performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence created using a computerised random‐number generator. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable and fruit intake Child’s vegetable and fruit intake unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Unclear risk | Vegetable and fruit intake: 2 observers independently recorded the number of pieces of vegetables or fruit selected by each child. However it is unclear whether these observers were blinded to condition and whether this influenced detection bias. This was observation of the number of pieces of fruit or veg selected and eaten by each child, and weight of any uneaten pieces of fruit/veg on the plate at end of meal. It was assessed by 2 independent observers, but it is not clear if they were blinded or not. Childcare staff sat at table with children and passed around fruit & veg bowls but were unaware of the study hypotheses |
| Incomplete outcome data (attrition bias) | Low risk | 54 (89%) of the 61 children completed the liking ratings and therefore the risk of attrition bias is low |
| Selective reporting (reporting bias) | Low risk | The primary outcomes reported in the paper align with those specified in the trial registration |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "This work was supported by a grant for investigation in nursing from Collegi Oficial d’ Infermeria de Barcelona, 2009 (grant number PR‐5001/09); Primer Premio Nacional de Investigación en Enfermería, 2009, from Hospital Universitario Marqués de Valdecilla; and a grant for investigation in nursing from Acadèmia de Ciències Mèdiques de Catalunya i Balears, filial Maresme, 2010. The funders had no role in the design, analysis or writing of this article." | |
| Participants | Description: Children aged 1 to 2 years attending 12 daycare centres and their parent N (Randomised): 12 day‐care centres, 206 children, 195 parents Age: Child (mean): Intervention = 1.3 years, Control = 1.4 years Parent (mean): Intervention = 35 years, Control = 35 years % Female: Child: Intervention = 37%, Control = 49% Parent: Intervention = 93%, Control = 85% SES and ethnicity: Educational level: Primary = 10%, Secondary = 35%, University = 55% Inclusion/exclusion criteria: No explicit inclusion criteria stated for this trial Exclusion criteria: “Children still exclusively breast‐feeding at the time of the study, children whose parents were not responsible for their alimentation, children with special diets due to chronic diseases (such as coeliac disease, food intolerances or allergies, inflammatory bowel disease), parents with language difficulties, parents unable to attend the educational workshops and those who did not sign the informed consent.” Recruitment: “At the beginning of the school term, all parents of the children attending the participating day‐care centres were invited to informative meetings regarding the study with the use of pamphlets and posters.” Recruitment rate: Child: 35% (206/581) Region: The city of Mataró (north of Barcelona), Spain | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Child: Intervention = 75, Control = 67 Parent: Intervention = 74, Control 72 Description of intervention: “All parents from the day‐care centres in the intervention group (IG) were invited to attend four educational workshops on alimentation at the beginning of the study and one reminder at 4 months. A model of participatory‐active education was used, in order to achieve practical skills in addition to nutritional knowledge. Cognitive (teaching how to improve diet), emotional (addressing beliefs and attitudes of the participants through discussion and analysis techniques) and skill areas (developing dietary skills) were included. The aim was to incorporate new and better dietary knowledge and to change the habits of the participants.” Duration: 6 months (workshops in October ‐ November and a reminder in March) Number of contacts: 5 workshops Setting: Preschool Modality: Face‐to‐face Interventionist: Nurses trained in nutrition Integrity: No information provided Date of study: October 2010 to May 2011 Description of control: “The parents included in the control group (CG) did not receive any education related to nutrition. In order to avoid drop outs, the participants of the CG were invited to a workshop on a subject not related to the study or nutritional education (manipulation and conservation.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruits and vegetables (servings per day) assessed using a 78‐item food frequency questionnaire (FFQ) completed by parents Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 8 months Length of follow‐up post‐intervention: 2 months Subgroup analyses: None Loss to follow‐up: Child: Intervention = 32%, Control = 35% Parent: Intervention = 9%, Control = 8% Analysis: Did not adjust for clustering. Unknown if sample size calculation performed. | |
| Notes | First reported outcome (changes in vegetable and garden produce servings per day) was extracted for inclusion in the meta‐analysis. To enable inclusion in meta‐analysis, we calculated post‐intervention means by group by summing baseline and change from baseline means, assuming baseline SDs for post‐intervention SDs, and we calculated an effective sample size using ICC of 0.014 to account for clustering Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake 2nd listed outcome after adherence to Mediterranean diet | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Dietary intake (self‐reported): There is no blinding to group allocation of participants and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Dietary intake (self‐reported): There is no blinding to group allocation of participants and because this is a self‐reported measure this is likely to introduce detection bias |
| Incomplete outcome data (attrition bias) | High risk | “Of the parents randomized to the IG only sixty‐seven (65 %) attended three or more workshops, with the remaining parents considered drop outs. The reasons for not attending the workshops were mainly difficulties in family timetables and illness of the children”. 35% of the intervention group did not attend the minimum of 3 workshops and were considered dropouts. Therefore analysis was not undertaken according to intention‐to‐treat principles and risk of attrition bias is high |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | There were baseline imbalances for certain characteristics between the conditions (e.g. servings of legumes), although adjusted for in the analysis and so the impact of this is unclear. Analysis did not accounted for effect of clustering, but we calculated an effective sample size prior to pooling in meta‐analysis to account for this |
| Methods | Study design: Randomised controlled trial Funding: Not reported | |
| Participants | Description: Children aged 3 to 5 years attending full‐day childcare at the Child Development Laboratory located at The Pennsylvania State University N (Randomised): 21 children Age: Mean = 4.3 years % Female: 59% SES and ethnicity: “most of the families (60%) reported combined family incomes of US>$50,000.” Inclusion/exclusion criteria: “Exclusion criteria were the presence of food intolerance to study foods, chronic illness affecting food intake, consuming <22 g of the entree (<10% of the 220‐g entree portion), dislike of the main entree, uncooperative behavior during lunch, non‐English speaking, or extended absences.” Recruitment: Not specified Recruitment rate: Unknown Region: Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 6 Number of participants (analysed): Overall = 17 (not specified by group) Description of intervention: “Children were served a series of 6 lunches in a random order, once per week, which varied only in entrée portion size (entree portion size order: 100, 160, 220, 280, 320, and 400 g). Children were served lunch on the same day of the week at their regularly scheduled time in an eating laboratory dining room facility near their classroom.” “The menu at all lunches included the portion‐manipulated macaroni and cheese entree and fixed portions of 2% milk and other foods served with the entree (eg, green beans with butter, whole‐wheat roll, and unsweetened applesauce).” Duration: 6 days Number of contacts: 6 (1 lunch per day) Setting: Preschool Modality: Face‐to‐face Interventionist: Research staff Integrity: No information provided Date of study: 2007 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetable for different entree portion sizes (grams). “Food and milk weights were recorded before and after consumption to the nearest 0.1 g by using digital scales (Mettler‐Toledo PR5001 and Mettler‐Toledo XS4001S; Mettler‐Toledo Inc). The amount of each food item consumed (g) was determined by subtracting postmeal weights from premeal weights.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 6 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall = 19% (not specified by group) Analysis: Unknown if sample size calculations performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Food and milk intake: Objective measure of child’s food intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Food and milk intake (weighed before and after consumption): Objective measure of child’s food intake because food was weighed before and after consumption. Low risk of detection bias |
| Incomplete outcome data (attrition bias) | Low risk | There is no reported attrition. Data are reported for all of the 17 children who met predetermined inclusion criteria |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: “The project described was supported by grant numbers A1R21DK078239 (principal investigator [PI]: Sherwood), P30DK050456 (PI: Levine), and P30DK092924 (PI: Schmittdiel) from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).” | |
| Participants | Description: Parents with children aged 2‐4 years N (Randomised): 60 parent‐child dyads Age: Children (mean): Busy Bodies/Better Bites = 2.60 years, Healthy Tots/Safe Spots: 2.90 years Parent (mean): Bodies/Better Bites = 34.4 years, Healthy Totes/Safe Spots = 33.4 years % Female: Children: Busy Bodies/Better Bites = 50%, Healthy Totes/Safe Spots = 40% Parents: Busy Bodies/Better Bites = 97%, Healthy Totes/Safe Spots = 90% SES and ethnicity: Busy Bodies/Better Bites: white = 77%, Hispanic = 7%, Healthy Totes/Safe Spots: white = 83%, Hispanic = 7% Inclusion/exclusion criteria: Inclusion criteria: BMI between 85th and 95th percentile for age and gender OR BMI between 50th and 85th percentile and at least 1 overweight parent (BMI ≥ 25kg/m2) and receives care at a HealthPartners Clinic in the Twin Cities Metropolitan Area. Exclusion criteria: children with chronic disease, children who within the last 6 months or currently taking Prednisone, Prednisolone, Decadron, families who have limited English skills, and families who plan to move out of the Metropolitan area within the next 6 months Recruitment: “Parent‐child dyads were recruited through 20 clinics in the greater Minneapolis–St. Paul area” “…a study invitation letter was sent to parents. A subsequent phone call assessed interest and preliminary eligibility, confirmed in a home visit.” Recruitment rate: 94% (60/64) Region: USA | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Busy Bodies/Better Bites: 30 Healthy Totes/Safe Spots: 30 Description of intervention: All participants received pediatric primary care provider counselling during their well‐child visit to raise parental awareness of their child’s obesity risk and provide messaging regarding obesity and injury prevention behaviours. Busy Bodies/Better Bites: participants received an 8‐session phone‐coaching programme focused on healthy eating and PA and an associated workbook and busy bag, which included “a child focused book on television (TV) habits, activity and dinner table conversation idea cards, portion placement and plate, a kid‐friendly, healthy recipe pamphlet, small plastic cones, sidewalk chalk, stickers, a child‐focused dance music CD, and an inflatable beach ball.” Healthy Totes/Safe Spots: participants received an 8‐session phone‐coaching programme focused on safety and injury prevention and an associated workbook and safety tote, which included “a similar number of items [to the busy bag] relevant to the safety and injury prevention topics (e.g., travel‐size sunscreen or fire safety book).” Duration: 6 months Number of contacts: 9 (1 primary care component + 8 phone coaching sessions) Setting: Clinic + home Modality: Multiple (face‐to‐face, telephone, written materials) Interventionist: PCP (face‐to‐face) and experienced interventionists (telephone) Integrity: Provider adherence: “Well‐child visit protocol adherence was assessed by phone survey with parents 1–2 weeks post‐well‐child visit. Parents reported whether their provider talked about BMI percentile, whether they received the HHHK pamphlet, and whether the provider addressed specific PA, sedentary behavior, healthy eating, and safety/injury prevention issues.” Phone coaches: “Phone coaches completed a self‐assessment of session fidelity (e.g., use of behavioral adherence strategies and time spent discussing specific target areas) after each session. Phone sessions were audio recorded, and recordings were utilized during supervision sessions and subsequently coded by independent raters to provide a more in‐depth examination of fidelity.” Well‐child visit intervention component: “Parents reported that 78% of providers discussed BMI percentile. The majority of parents (87%) received the HHHK pamphlet, but less than half (44%) reported that their provider used the HHHK flipchart. The most frequently discussed obesity prevention topics included fruit and vegetable intake (27%), PA (24%), junk food, including sweetened beverages (11%), and media use (7%). Fewer parents reported that the provider discussed family meals (5%), eating breakfast (4%), and eating out at restaurants (0%).” “80% of participants in both arms completed the eight‐session intervention.” Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of fruits and vegetables (servings) using a multipass 24‐hour recall completed by parents. Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 6 months Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Busy Bodies/Better Bites: 13% Healthy Totes/Safe Spots: 3% Analysis: Unknown if sample size calculation was performed. | |
| Notes | Sensitivity analysis ‐ primary outcome: primary outcome as per trial registry included fruit and vegetable intake | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Sixty parent‐child dyads were randomized equally to the Busy Bodies/Better Bites Obesity Prevention and the Healthy Tots/Safe Spots Contact control arms.” It is unclear how the randomisation occurred |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed from those conducting the research. |
| Blinding of participants and personnel (performance bias) | High risk | “After the well‐child visit, parents received a randomized group assignment notification letter…” “Coaches worked with parents to address behavior change areas in order of parent preference, setting goals and discussing challenges and successes at subsequent sessions.” Participants were aware of their group allocation. Due to the nature of the intervention, staff would also have been aware of participant group allocation. |
| Blinding of outcome assessment (detection bias) | High risk | “A multipass 24‐hour dietary recall was administered by staff trained and certified to use the Nutrition Data System for Research software versions 2009, 2010, and 2011” It is unclear whether outcome assessors visiting the home were aware of group allocation. Parents self‐reported child dietary intake. |
| Incomplete outcome data (attrition bias) | Low risk | The number of parents who completed the follow‐up assessments is reported and there was only a small loss to follow‐up that was similar across experimental arms. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as per protocol, except for “Paediatrician participation and satisfaction at 6 months” This was reported after 3 HHHK visits, not at 6 months. |
| Other bias | Low risk | No other bias was identified. |
| Methods | Study design: Randomised controlled trial Funding: "Australian Research Council Linkage Grant (ARC LP100100049)" | |
| Participants | Description: Children aged 20 to 42 months and their parent N (Randomised): 201 parent‐child dyads Age: Child (mean): Intervention = 2.7 years, Control = 2.8 years Parent (mean): Intervention = 35 years, Control = 35 years % Female: Child: Intervention = 49%, Control = 37% Parent: not specified SES and ethnicity: Parent highest level of education (Bachelor degree or higher): Intervention = 57%, Control = 60% Annual family income (AUD): AUD < 450,000: Intervention = 14%, Control = 21% AUD 45,001 – 85,000: Intervention = 41%, Control = 33% AUD 85,001 – 125,000: Intervention = 27%, Control = 27% AUD > 125,000: Intervention = 17%, Control = 19% Location of parents' birth: Australia or New Zealand: Intervention = 77%, Control = 74% Europe: Intervention = 3%, Control = 4% Asia: Intervention = 11%, Control = 9% Inclusion/exclusion criteria: Inclusion criteria: “Families were eligible if their child was aged 20–42 months at baseline (waitlist children would still be ≤4 years when receiving the programme), and if parents were aged ≥ 18 years and could read and write English (with the assistance of an interpreter if required). There were no other qualifying or exclusion criteria.” Recruitment: “We sourced participants through community events, local newspaper and magazine advertisements, flyers distributed through kindergartens/pre‐schools/childcares, maternal and child health centres, and medical centres.” Recruitment rate: Parent‐child dyads = 97% (201/207) Region: Victoria (Australia) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Time 2: Intervention = 80, Control = 72 Time 3: Intervention = 74, Control = 69 Time 4: Intervention = 73, Control = 63 Description of intervention: MEND (Mind, Exercise, Nutrition…Do it! 2 – 4 intervention: “Each session included three sections: (i) 30 min of guided active play; (ii) 15 min of healthy snack time based on an evidence‐based, exposure technique to promote acceptance of fruit and vegetables and (iii) 45 min of supervised creative play activities for the children while parents attended an interactive education and skill development session. Guided active play involved games played with children and parents together that could be easily replicated at home. Healthy snack time centred on a role model (puppet called ‘Max Moon’) who encouraged children to sniff, touch, lick and taste fresh fruit and vegetables. Parents received weekly handouts.” Duration: 10 weeks Number of contacts: 10 (1 per week, 90 minutes a session) Setting: Community health centres Modality: Face‐to‐face Interventionist: Trained program leader Integrity: “Programme leaders were monitored regularly to ensure their practice was in accordance with guidelines.” Date of study: Between May 2010 and December 2012 Description of control: Wait‐list control: "The WLC group did not receive any intervention, but were offered the programme at study completion.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetables (usual servings) assessed by the Eating and Physical Activity Questionnaire completed by parents. Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Post‐intervention: 10 weeks Time 2: ˜ 8 ‐ 9 months Time 3: ˜ 15 months Length of follow‐up post‐intervention: Immediately Time 2: 6 months Time 3: 12 months Subgroup analyses: None Loss to follow‐up (Immediately post‐intervention and at 6 and 12 months): Intervention = 12%, 4%, 4% Control = 5%, 6%, 6% Analysis: Sample size calculations performed | |
| Notes | First reported outcome (usual servings a day of vegetables) at the longest follow‐up < 12 months (6 months) and ≥ 12 months (12 months) was extracted for inclusion in meta‐analysis Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake listed as primary outcome in trial registry. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ”conducted by a researcher not involved in data management using a randomized treatment allocation schedule produced by computer algorithm.” The random sequence was produced by computer algorithm |
| Allocation concealment (selection bias) | Unclear risk | Although the authors indicate that participants were informed of group allocation by opaque envelopes, there is no indication if these envelopes were sealed and sequentially numbered |
| Blinding of participants and personnel (performance bias) | High risk | Dietary intake (includes fruit and vegetables): There is no blinding to group allocation of participants described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Dietary intake (includes fruit and vegetables) (self‐report): There is no blinding to group allocation of participants described and because of the self‐report measure this is likely to influence detection bias |
| Incomplete outcome data (attrition bias) | Low risk | Attrition rate was < 20% at follow‐up T4 and missing values of baseline measurements were imputed using mean imputation |
| Selective reporting (reporting bias) | Unclear risk | “Outcomes not addressed here will be presented in future papers.” Insufficient evidence to determine, as it appears that future papers with additional outcomes are planned |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Cluster‐randomised controlled trial Funding: Not reported | |
| Participants | Description: Low socio‐economic children aged 3‐5 years attending Head Start preschools in Marion County, Ohio N (Randomised): 4 Head Start centres, 240 children Age: “All clusters combined had a total of 80 (38.3%) three year old children, 116 (55.5%) four year old children, and 13 (6.2%) five year old children in the study sample.” % Female: Access‐only cluster = 54%, access + education = 45%, control = 55% SES and ethnicity: Low socio‐economic “There were 9 (4.3%) Hispanic children, 152 (72.7%) white children, 36 (17.2%) multi‐racial, and 12 (5.7%) black children in the study sample” Inclusion/exclusion criteria: No explicit inclusion criteria Exclusion criteria: “Children or parents were excluded if a medical issue prohibited them from participating in the study. Children who were unable to eat solid foods were asked not to participate in this study. Children with chronic diseases, such as diabetes, were excluded from the study, as children with chronic diseases are known to have reduced carotenoid concentrations” Recruitment: “Purposive sampling was the method chosen for this study”. Parents were approached about consenting to the study at various meetings or when parents were dropping off or picking up their children. Recruitment rate: 83% (240/290) Region: Marion County, Ohio | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Access only: 61 Access + education: 82 Control: 66 Description of intervention: Access only: “received the take home weekly fruits and vegetables, without the educational intervention.” Access + education: “received weekly take home fruits and vegetables, education for the children, and supplemental materials, such as newsletters and recipes, for the families about the produce being provided.” The Supplemental Nutrition Assistance Program Education (SNAP‐Ed) was provided each week. “The Harvest for Healthy Kids curriculum was used and each week the focus was on a high carotenoid fruit or vegetable. Storybooks, activities such as making pumpkin pudding in a bag, and tastings were the foundation of the class sessions.” Duration: 8 weeks Number of contacts: 8 Setting: Preschool + home Modality: Access only: provision of fruit and vegetable Access + education: multiple (provision of fruit and vegetable, face‐to‐face education, written materials) Interventionist: Access only: unclear Access + education: Supplemental Nutrition Assistance Program Education (SNAP‐Ed) programme staff member delivered education Integrity: No information provided Date of study: October‐December 2016 Description of control: “the control group did not receive either the produce or education during the eight weeks.” “The group received education following the study.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of fruit and vegetable consumption measured by carotenoid levels in the skin Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 8 weeks Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Access only: 18% Access + education: 10% Control: 12% Analysis: Unclear if adjusted for clustering Sample size calculations performed | |
| Notes | We pooled the access + education intervention arm compared to the no‐intervention control group in meta‐analysis of multicomponent interventions. We described the access‐only intervention compared to the no‐intervention control group narratively. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Site clusters were randomly assigned to one of the treatment or control groups”. Randomly allocated to experimental group but the random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and study team were not blinded. Parent self‐reported survey on fruit and vegetable consumption and therefore at high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Parents were not blinded which may have affected how they responded to the survey. Parent self‐reported survey on fruit and vegetable consumption and therefore at high risk of detection bias. |
| Incomplete outcome data (attrition bias) | Low risk | There were 31/240 withdrawn (27 from intervention, 4 from control). |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol is available |
| Other bias | Unclear risk | There appears to be baseline imbalance between groups with differences between groups on child age and race. Analysis does not appear to account for clustering. |
| Methods | Study design: Cluster‐randomised controlled trial – cross‐over Funding: "Supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK082580) and the Robert Wood Johnson Foundation" | |
| Participants | Description: Children aged 3 to 6 years enrolled in daycare at the Bennett Family Center on campus at The Pennsylvania State University N (Randomised): 5 classrooms, 51 children Age: Mean = 4.4 years % Female: 57% SES and ethnicity: “Of the 51 children in the study, 46 parents provided demographic information for their children. Of these 46 children, 28 (61%) were white, 14 (30%) were Asian, 3 (7%) were black or African American, and 1 (2%) was American Indian or Alaska Native. Parents of the children had above‐average educational levels and household incomes; 90% of mothers and 85% of fathers had a college degree, and 79% of households had an annual income >$50,000.” Inclusion/exclusion criteria: Provided by study author: "Children with an allergy to the foods being served were not eligible to participate in the study. Parents and guardians provided informed written consent for both their own participation and that of their child." Recruitment: “Recruitment began in April 2008 by distributing letters to parents who had children aged 3–6 years enrolled in daycare at the Bennett Family Center at the University Park campus of The Pennsylvania State University.” Recruitment rate: Provided by study author: "100% of children whose parents signed consent form were included in the study" Region: Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Overall = 51 Description of intervention: One day a week for 4 weeks, children were provided with a first course and main course at lunch. Across the weeks the portion size of raw carrots and dip served as the first course of lunch was varied (30 g, 60 g, or 90 g) and during 1 week no first course was provided. Cooked broccoli was served as the vegetable with the main lunch course Duration: 4 weeks Number of contacts: 4 (1 day a week) Setting: Preschool Modality: Face‐to‐face Interventionist Preschool teacher Integrity: Provided by study author: "All children were served the food assigned in the experimental condition. There was no deviation from study protocol. No unplanned or unintended interventions." Date of study: Recruitment began in April 2008 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of vegetables for different first course portion sizes (grams). “Uneaten items were removed, and weights were recorded to the nearest 0.1 g with digital scales. Consumption of the foods and milk was determined by subtracting postmeal weights from premeal weights.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Unclear Length of follow‐up post‐intervention: Immediately Subgroup analyses: Provided by study author: "Differences between girls and boys in age, body weight, height, BMI percentile, and BMI z score were analyzed by using t tests. Analysis of covariance was used to assess the influence of continuous variables (age, body weight, height, BMI percentile, and BMI z score) on the relation between carrot portion size and the main study outcomes. Children who consumed all of the carrots (95% of the weight served) at any meal were identified, and data were analyzed both with and without these children to determine whether they influenced the results. The effect of individual children who were influential on the main study outcomes was assessed." Loss to follow‐up: There was no loss to follow‐up Analysis: Unclear if adjusted for clustering Sample size calculations performed. | |
| Notes | Sensitivity analysis ‐ primary outcome: Vegetable intake listed as primary outcome in trial registry. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Children were enrolled from 5 classrooms; the order of the experimental conditions across study weeks was assigned to classrooms by using a Latin square design.” Provided by study authors: "The orders of the experimental conditions across study weeks were created using Latin squares and then assigned to classrooms using a random number generator." |
| Allocation concealment (selection bias) | Unclear risk | It is not clear who undertook randomisation of classrooms. Provided by study authors: "Classrooms (and the associated condition order) were assigned a color coding so that participants and teachers were uninformed of the experimental condition." |
| Blinding of participants and personnel (performance bias) | Low risk | “Incidents of food and drink spillage were recorded by researchers. Teachers were instructed to redirect conversations pertaining to food to nonfood‐related topics to minimize the influence on lunch intake.” Objective outcome measurement. Children were not blinded and it seems unlikely that this would influence their intake. Staff present during the meal and staff who served the food to children were not blinded and it seems unlikely this would influence child intake |
| Blinding of outcome assessment (detection bias) | High risk | “Uneaten items were removed, and weights were recorded to the nearest 0.1 g with digital scales”. “Incidents of food and drink spillage were recorded by researchers.” Appears that researchers who weighed the food were the same researchers who recorded incidents of food and drink spillage. Researchers were not blinded and this may have had an impact on how the outcome was recorded in different classrooms |
| Incomplete outcome data (attrition bias) | Low risk | “A total of 51 children were enrolled, and all of them completed the study” There were no children who dropped out over the study |
| Selective reporting (reporting bias) | Low risk | There is no study protocol and unable to determine if all prespecified outcomes have been reported as described Provided by study authors: "All outcomes collected were reported in the paper (vegetable and food intake)" |
| Other bias | Low risk | There are no other sources of potential bias |
| Methods | Study design: Randomised controlled trial – cross‐over Funding: Provided by study author: "Supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK082580)." | |
| Participants | Description: Children aged 3‐6 years attending 2 daycare centres at the University Park campus of The Pennsylvania State University N (Randomised): 49 children Age: Mean = 4.7 years % Female: 54% SES and ethnicity: “Of the 39 children, 28 children (72%) were white, 9 children (23%) were Asian, and 2 children (5%) were black or African American. Parents of the children had above average education levels and household incomes; ˜90% of mothers and 80% of fathers had a college degree, and 76% of households had an annual income >$50,000.” Inclusion/exclusion criteria: Provided by study author: "Children with an allergy to the foods being served were not eligible to participate in the study. Parents and guardians provided informed written consent for both their own participation and that of their child." Recruitment: “Recruitment began by distributing letters to parents with children aged 3–6 years who were enrolled in daycare at the Bennett Family Center or the Child Development Laboratory at the University Park campus of The Pennsylvania State University.” Recruitment rate: Provided by study author: "100% of children whose parents signed consent form were included in the study" Region: Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Overall = 39 Description of intervention: “The 3 experimental entrees were manipulated by adding pureed vegetables to a standard recipe (100% energy dense (ED) condition) to reduce the ED by either 15% (85% ED condition) or 25% (75% ED condition). Manipulated entrees were zucchini bread at breakfast, pasta with tomato‐based sauce at lunch, and chicken noodle casserole at dinner and evening snack.” In addition unmanipulated side dishes and snacks were served, including fruit, vegetables, milk and cheese and crackers Duration: 3 weeks Number of contacts: 3 (1 day a week) Setting: Preschool Modality: Face‐to‐face Interventionist Provided by study author: "Preschool teacher" Integrity: Provided by study author: "All children were served the food assigned in the experimental condition. There was no deviation from study protocol. No unplanned or unintended interventions." Date of study: Between January and May 2010 Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of vegetable for difference energy density entrees (grams). “Food and beverage weights were recorded to the nearest 0.1 g with digital scales (PR5001 and XS4001S; Mettler‐Toledo Inc). The consumption of foods and beverages was determined by subtracting postmeal weights from premeal weights.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Effect of intervention on amount of meal consumed Length of follow‐up from baseline: Unclear Length of follow‐up post‐intervention: Immediately Subgroup analyses: Provided by study author: "ANCOVA was used to assess the influence of continuous subject variables (age, body weight, height, and BMI percentile) on the relation between entree energy dense (ED) and the main study outcomes. t tests were used to test differences between girls and boys in ages, body weights, heights, BMI percentiles, and BMI z scores." Loss to follow‐up: Overall = 18% Analysis: Sample size calculations performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random sequence was generated with computer software |
| Allocation concealment (selection bias) | Unclear risk | ”Random orders were generated with computer software and assigned to a list of participant identification numbers” The random sequence was assigned to a list of participant identification number, but it is unclear if allocation was concealed. Provided by study author: "Allocation was concealed to participants and teachers by assigning each child an ID number that was associated with their random order." |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake: Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake: Objective measure of child’s vegetable intake and unlikely to be influenced by detection bias |
| Incomplete outcome data (attrition bias) | High risk | 49 children were enrolled, but 9 were excluded because they had difficulty following the protocol. Given an intention‐to‐treat approach to analysis was not used, the risk of attrition bias is high |
| Selective reporting (reporting bias) | Low risk | The primary outcomes reported in the paper align with those specified in the trial registration |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Cluster‐randomised controlled trial – cross‐over Funding: Provided by study author: "Supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01 DK082580)." | |
| Participants | Description: Children aged 3‐5 years attending 2 daycare centres at the University Park campus of The Pennsylvania State University N (Randomised): 5 classrooms, 73 children Age: Range 3.3 to 5.7 years (mean = 4.7 years) % Female: 57% SES and ethnicity: “Parents of the children had above average education levels and household incomes; approximately 95% of mothers and 88% of fathers had a college degree and 70% of households had an annual income above $50,000.” “Parents provided demographic information for 66 of the 72 children; of these, 42 (67%) were white, 17 (27%) were Asian, and 4 (6%) were black or African American” Inclusion/exclusion criteria: Provided by study author: "Children with an allergy to the foods being served were not eligible to participate in the study. Parents and guardians provided informed written consent for both their own participation and that of their child." Recruitment: “Recruitment began by distributing letters to parents who had children within the age range of three to six years enrolled in two daycare centers on the University Park campus of The Pennsylvania State University.” Recruitment rate: Provided by study author: "100% of children whose parents signed consent form were included in the study" Region: Pennsylvania (USA) | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Overall = 72 Description of intervention: “On one day a week for four weeks, children in a daycare setting were provided with breakfast, lunch, and afternoon snack. Across the weeks, the portion size of soup (tomato soup) served in the first course of lunch was varied (150, 225, or 300 g) and during one week no first course was provided. The foods and beverages served in the main course of lunch, as well as the foods and beverages served at breakfast and snack, were not varied in portion size.” Duration: 4 weeks Number of contacts: 4 (1 day per week) Setting: Preschool Modality: Face‐to‐face Interventionist: Teachers Integrity: No information provided. Date of study: Provided by study author: "Data was collected from Dec. 2008 to Mar. 2009." Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of vegetable (grams): tomato consumed from soup + broccoli from main course, Broccoli only, Afternoon snack, Total (soup, broccoli and afternoon snack). Portion sizes of foods were provided and researchers recorded the amount consumed Outcome relating to absolute costs/cost effectiveness of interventions: Provided by study author: "Outside scope of this study; data not collected" Outcome relating to reported adverse events: Provided by study author: "Outside scope of this study; data not collected" Length of follow‐up from baseline: Unclear Length of follow‐up post‐intervention: Immediately Subgroup analyses: Provided by study author: "Analysis of covariance was used to assess the influence of continuous subject variables (age, body weight, height, and BMI percentile) on the relationship between soup portion size and the main study outcomes. T‐tests were used to test differences between girls and boys in age, body weight, height, and BMI percentile." Loss to follow‐up: Overall = 1% Analysis: Provided by study author: "Classroom was tested as a factor in the model, but it was not significant and was removed." Sample size calculations performed. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Provided by study author: "The orders of the experimental conditions across study weeks were created using Latin squares and then assigned to classrooms using a random number generator." |
| Allocation concealment (selection bias) | Unclear risk | Provided by study author: "Classrooms (and the associated condition order) were assigned a color coding so that participants and teachers were uninformed of the experimental condition." |
| Blinding of participants and personnel (performance bias) | Low risk | Vegetable intake: Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Vegetable intake: Researchers recorded the number of pieces of each food item taken by the child and it is unlikely that this would be influenced by detection bias |
| Incomplete outcome data (attrition bias) | Low risk | 72 out of 73 children were included in the vegetable intake analysis and therefore the risk of attrition bias is low |
| Selective reporting (reporting bias) | Low risk | Provided by study author: "All outcomes collected were reported in the paper (soup and food intake)" |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue |
| Methods | Study design: Randomised controlled trial Funding: “AES is supported, in part, by the 1 U54 GM104940 grant from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center (July, 2015 to June, 2017).” | |
| Participants | Description: Children aged 3 to 5 years attending at 2 full‐day preschools N (Randomised): 42 children Age: Mean: Food modelling DVD = 4.5 years, Non‐food DVD = 4.1 years, No DVD (Control) = 4.3 years % Female: 50% SES and ethnicity: Child: White = 74%, African American = 5%, Asian = 10%, Hispanic = 10% Inclusion/exclusion criteria: Not specified Recruitment: Not specified Recruitment rate: 39% (42/108) Region: LA (USA) | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Food modelling DVD = 14 Non‐food DVD = 14 No DVD (Control) = 14 Description of intervention: Food modelling group = Copy‐Kids Eat Fruits and Vegetables DVD Non‐food DVD group = Copy‐Kids Brush Teeth. Day 1: “Depending on the condition, on day 1 the child viewed 1 of 2 video clips or sat quietly for 7.5 minutes. Two plates of snacks (the modelled vegetable and a comparison food) were placed in front of the participant in a standardized format (green bell peppers on the right and dry cereal on the left) on separate, identical white Styrofoam plates. Children were instructed to eat as much or as little as they wished during this time. The video segments were played concurrently during the food presentation” Day 2 and 7: “food items were presented for 7.5 minutes without the concurrent video presentation”. Duration: 1 week ± 2 days Number of contacts: 3 Setting: Preschool Modality: Visual/audio ‐ DVD Interventionist: Unclear Integrity: No information provided Date of study: Unknown Description of control: No DVD Control: food items were presented the same way as in the intervention but no DVD was played on any of the 3 exposure days | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of vegetable (grams). “Study staff weighed 0.5 cups of the modeled vegetable (ie, approximately 80 g of raw, sliced green bell pepper) and 0.5 cups of the comparison food (ie, approximately 16 g of Multi Grain Cheerios; General Mills, Minneapolis, MN) using a transportable scale before and after snack presentation on days 1, 2, and 7.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 1 week ± 2 days Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: There was no loss to follow‐up Analysis: Unknown if sample size calculations performed. | |
| Notes | Outcome data from the longest follow‐up < 12 months (day 7). We estimated the mean and SEM from a study figure using an online resource (Plot Digitizer: plotdigitizer.sourceforge.net) for all 3 groups. We combined the control DVD and control conditions into a single control group for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake 1st listed outcome in abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “used block randomization to distribute age and sex evenly across conditions using a randomization schedule generated with SAS programming” The random sequence was generated using statistical software, SAS |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Unclear risk | Vegetable intake (weighed): Objective measure of child’s vegetable intake and unlikely to be influenced by performance bias Parent reported fruit and vegetable consumption: There is no blinding to group allocation of participants or personnel described and this is likely to influence performance. However, it does appear that parents were blinded to the food provided to their children. “Researchers did not inform parents regarding which foods were presented to the children.” |
| Blinding of outcome assessment (detection bias) | Unclear risk | Vegetable intake (weighed): Objective measure of child’s vegetable intake and unlikely to be influenced by detection bias Parent reported fruit and vegetable consumption: There is no blinding to group allocation of participants or personnel described and these are self‐reported measures. However, “Researchers did not inform parents regarding which foods were presented to the children.” |
| Incomplete outcome data (attrition bias) | Low risk | All participants randomised completed the study. Therefore low risk of attrition bias |
| Selective reporting (reporting bias) | Low risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | The authors state that limitations included potential for within‐school contamination across conditions. No other evidence presented about this potential bias |
| Methods | Study design: Randomised controlled trial Funding: Supported by the Gerber Products company and National Institutes of Health Grant 2RO0HD197S2‐07 | |
| Participants | Description: Mothers and their 4 to 6‐month old infants N (Randomised): 36 children Age: Child (mean): 22 weeks (17‐27 weeks) % Female: 56% SES and ethnicity: Not reported Inclusion/exclusion criteria: “The 36 infants and their mothers who participated met the following criteria: 1. Infants were between 4 and 6 months of age at the beginning of the study; 2. Parents had just begun feeding solid foods and had only given cereals or cereals and fruits; 3. Parents indicated readiness to begin or continue introducing solid foods to the infant; and 4. Absence of medical complications or physical problems.” Recruitment: “Subjects were solicited through birth records and advertisements in local newspapers.” “Parents were contacts and informed of the study before the time their infants would be expected to be introduced to solid foods and contact was reestablished when they were ready to participate.” Recruitment rate: Unknown Region: USA | |
| Interventions | Number of experimental conditions: 4 Number of participants (analysed): Peas salted: 9 Peas unsalted: 10 Green beans salted: 8 Green beans unsalted: 9 Description of intervention: “Foods used throughout the study, pureed peas and green beans, were prepared especially for the study by the Gerber Products Company. Salted and unsalted versions of the two vegetables were prepared. The salted version of each food contained 0.3g NaCI/100g. The foods were presented to the mothers in jars, containing 71g of food and labels did not indicate the presence or absence of salt.” Duration: 10 days Number of contacts: 10 (once per day) Setting: Home Modality: Face‐to‐face Interventionist: Parents Integrity: “On each feeding occasion, parents completed a brief form noting information on the number of the jar used (1through 10), date of feeding, time at the start and end of the feed, infant state of alertness at the beginning of the feed, health of the infant, and the overall quality of the interaction during the feeding.” Date of study: Unknown Description of control: N/A | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Children’s consumption of vegetable (grams): Weighed jars of off before feeding session, resealed and frozen once feeding was finished. Jars collected and weighed by research team to determine grams of intake. Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: No adverse reactions were observed Length of follow‐up from baseline: 25 days Length of follow‐up post‐intervention: Immediately and at 1 week Subgroup analyses: None Loss to follow‐up: There was no loss to follow‐up Analysis: Unknown if sample size calculation was performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “The 36 infants were randomly assigned to receive either salted or unsalted peas or green beans; thus forming a total of four treatment groups.” No mention of how the randomization sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | There is no mention of allocation concealment. |
| Blinding of participants and personnel (performance bias) | Low risk | “The foods were presented to the mothers in jars, containing 71 g of food, and labels did not indicate the presence or absence of salt.” |
| Blinding of outcome assessment (detection bias) | Low risk | “All ratings were made while mothers and the research assistant were blind to whether infants were fed peas or beans, whether the feedings observed occurred before or after the repeated exposures, and whether or not the infants were being fed salted or unsalted vegetables.” |
| Incomplete outcome data (attrition bias) | Low risk | There is no attrition reported. |
| Selective reporting (reporting bias) | Unclear risk | There is no trial registration or protocol paper. |
| Other bias | Low risk | No other sources of bias were identified. |
| Methods | Study design: Randomised controlled trial Funding: “Funding for this research was provided by an unrestricted grant from ‘‘Get Kids in Action,’’ a partnership between the Gatorade Corporation and the University of North Carolina.” | |
| Participants | Description: Children aged 2 to 5 years and their parent N (Randomised): 50 parent‐child dyads Age: Child (mean): Intervention = 3.9 years, Control = 3.3 years Parent (mean): Intervention = 36.6 years, Control = 36.2 years % Female: Child: Intervention = 59%, Control = 67% Parent: Intervention = 86%, Control 90% SES and ethnicity: Parent (non‐white): Intervention = 18%, Control = 10% Income (USD): < 50,000: Intervention = 18%, Control = 81% ≥ 50,000: Intervention = 77%, Control = 19% Education: College or less: Intervention = 36%, Control = 43% Inclusion/exclusion criteria: At least 1 child 2 ‐ 5 years old, “Additional eligibility criteria included having lived in their current residence and planning to stay in that residence for at least 6 months. If the family had more than 1 eligible child, the eldest was selected as the reference child” Recruitment: “A convenience sample of 50 parent‐child dyads, with at least 1 child 2‐5 years old, was recruited through child care centers, listservs, and community postings. Interested parents responded to recruitment materials and were screened by phone.” Recruitment rate: Unknown Region: USA | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 22, control = 21 Description of intervention: “addressed vegetable and food issues based on the baseline surveys, and the dietitian helped parents select 1 primary target area for improvement during the intervention from 4 possible options (vegetable availability; picky eating; modeling; family meals). These areas were selected based on Social Cognitive Theory, which posits that there is reciprocal interaction between an individual and his/her environment. This theory also highlights the importance of self‐efficacy, which was thus a target of the intervention as well.” Duration: 4 months Number of contacts: 6 (2 phone calls, 4 newsletters) Setting: Home Modality: Multiple (telephone, newsletters) Interventionist: A registered dietitian Integrity: No information provided Date of study: April and December 2009 Description of control: “Control group families received 4 non‐health/nutrition related children's books, 1 per month.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of vegetables (servings per day) assessed using a Block Kids food frequency questionnaire (FFQ) completed by parents. Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 5 months Length of follow‐up post‐intervention: Immediate Subgroup analyses: None Loss to follow‐up: Intervention = 12% Control = 16% Analysis: Unknown if sample size calculations performed | |
| Notes | To enable inclusion in meta‐analysis, we calculated post‐intervention means by group by summing baseline and change from baseline means, and assumed baseline SDs for post‐intervention SDs. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake 2nd listed outcome after height and weight | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Child vegetable intake (parent reported): There is no blinding to group allocation of participants or personnel described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Child vegetable intake (parent reported): There is no blinding to group allocation of participants or personnel described and because this is a parent‐reported measure at high risk of detection bias |
| Incomplete outcome data (attrition bias) | Low risk | 43 (86%) of the 50 parent‐child dyads recruited completed the study. Therefore at low risk of attrition bias |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | Participants differed on child age by condition. However although this was adjusted for in the analysis the impact of this imbalance is unclear |
| Methods | Study design: Cluster‐randomised controlled trial Funding: “Indian Council of Medical Research, India and the NIH/NICHD (5 R01 HD042219‐S1); additional funding from UNICEF, New York.” | |
| Participants | Description: Mothers and their infants from 60 villages in India N (Randomised): 60 villages (clusters), 607 mother‐infant dyads Age: Child: “The intervention began with infants are about 3 months old” Mother (mean): Complementary feeding group: 22.3 years, Responsive complementary feeding and play group: 22.3 years, Control group: 21.9 years % Female: Child: Complementary feeding group = 52%, Responsive complementary feeding and play group = 51%, Control group = 49% Parent: 100% SES and ethnicity: Percentage mothers finished secondary or high school: Complementary feeding group = 25%, Responsive complementary feeding and play group = 32%, Control group = 27%. Mean standard of living index score: Complementary feeding group = 25.6, Responsive complementary feeding and play group = 25.3, Control group = 26.3 Inclusion/exclusion criteria: Inclusion: had to be part of the ‘Integrated Child Development Services’ project areas, be pregnant in their third trimester No exclusion criteria mentioned in text but in figure states “excluded as per criteria: microcephaly, physical handicap, mother mentally handicapped, cerebral palsy, thalassemia, child passes away.” Recruitment: “We explained the study objectives to all the pregnant women in the villages and asked if they would like to participate in the study. There were no refusals.” Recruitment rate: 100% Region: India | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): Complementary feeding group = 170 Responsive complementary feeding and play group = 145 Control group = 168 Description of intervention: Complementary feeding group: “In addition to the ‘Integrated Child Development Services’, mothers in this group received 11 nutrition education messages on sustained breastfeeding and complementary feeding through twice‐a‐month or four times a month (depending on the age of the infant) home‐visits over 12 months by the trained village women using flip charts, other visual material, demonstrations and counselling sessions.” Responsive complementary feeding and play group: “In addition to the ‘Integrated Child Development Services’, mothers in this group received education on complementary feeding as in the complementary feeding group (11 messages), eight messages and skills on responsive feeding, and eight developmental stimulation messages using five simple toys. This group of mothers also received developmentally appropriate toys five times during the intervention with instructions on how to use them to engage and play with their children.” Duration: 12 months Number of contacts: 30 planned visits “The first visits were in the fourth month, after the baseline when infants were 3 months old. From 4 to 6 months, mothers were visited twice per month, or 6 visits; from 7 to 9 months, they were visited 4 times a month, or 12 visits; and from 10 to 14 months, they were visited twice a month, or 12 visits,” Setting: Home + centre‐based supplemental food Modality: Face‐to‐face Interventionist: The trained village women Integrity: “Trained graduates in nutrition supervised the village women, examined their records of visits and asked mothers independently what they were told in the village woman’s’ last visit. They also held periodic reinforcement training sessions with the village women.” Date of study: Unknown Description of control: “Control group (CG): Mothers and infants in this group received only the routine ‘Integrated Child Development Services’, which were operating across all study groups. These services consist mainly of centre‐based supplemental food provided to 1–6‐year‐olds, pregnant and nursing mothers, home‐visit counselling on breastfeeding and complementary feeding, monthly growth monitoring, and non‐formal preschool education for children 3–5 years of age.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of banana, spinach, pulses (legumes): “Dietary intake was evaluated by the 24‐h recall method using standard cups with specified volume to help recall the food serving amounts.” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 12 months Length of follow‐up post‐intervention: Immediately Subgroup analyses: None Loss to follow‐up: Overall: 15% Analysis: Adjusted for clustering Sample size calculations performed | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “The random allocation using a random number generator (facilitated through a tailor‐made syntax programme in the Statistical Package for the Social Sciences (SPSS), which uses the select cases function) was undertaken by a researcher who was not familiar with the villages or their characteristics other than what could be derived from the 2001 census data.” |
| Allocation concealment (selection bias) | Unclear risk | There is no mention of allocation concealment. |
| Blinding of participants and personnel (performance bias) | High risk | Both the village women (VW) delivering the intervention, and mothers receiving the intervention were likely to be aware of their experimental group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | “The assessment teams (psychologists and nutritionists) were blinded to the intervention and had no interaction with the VWs. They did not meet as they used different transport and timetable of activities. The villages had no identification mark to indicate the group to which they had been randomized.” |
| Incomplete outcome data (attrition bias) | Low risk | “After 12 months of intervention and consequent attrition (15%), the sample comprised 511 mothers and children with 182 in CG, 176 in CFG and 153 in the RCF&PG. All 60 clusters remained in the study. Loss to follow‐up was greater in the RCF&PG (22%) compared with the CG (9%) and CFG (16%) although this difference was not statistically significant.” “Reasons for follow‐up losses during the study were migration (9.2%), house found locked on repeated visits (4.7%) and death of the child (1%). The demographic characteristics of those lost to follow‐up and those who remained were not different.” Loss to follow‐up was uneven across the study arms (not stat significant), but were not due to the trial. No loss of clusters |
| Selective reporting (reporting bias) | Unclear risk | There is no trial registration or protocol paper. |
| Other bias | Low risk | Recruitment bias: (low) “We explained the study objectives to all the pregnant women in the villages and asked if they would like to participate in the study. There were no refusals.” Baseline imbalance: (low) “There were no significant differences among the three groups in any of the baseline characteristics" Loss of clusters: (low) “All 60 clusters remained in the study.” Incorrect analysis: (low) “Values presented in the text and tables are means & standard deviations at the individual level and ICCs are presented to quantify the clustering effects” |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "The work was supported by the Ministry of the Flemish Community (Department of Economics, Science and Innovation; Department of Welfare, Public Health and Family)." | |
| Participants | Description: Children aged 9 to 24 months enrolled at daycare centres in 6 different communities in Flanders (Belgium) N (Randomised): 70 day care centres, 203 children Age: Mean: Intervention = 15.8 months, Control = 14.9 months % Female: Intervention = 47%, Control = 44% SES and ethnicity: Low SES: Intervention = 13%, Control = 24% Inclusion/exclusion criteria: No explicit inclusion criteria stated for this trial Children were excluded if they were not present in daycare on the measurement day for objective height and weight at baseline (i.e. not fulfilling the minimum criteria to be included in the study) Recruitment: “Within each day‐care centre, parents of all children aged 9–24 months were invited to enrol their child in the study.” Recruitment rate: 50% (203/404) Region: Flanders (Belgium) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 100, control = 56 Description of intervention: “The intervention aimed at increasing daily consumption of water (instead of soft drinks), milk, fruit and vegetables, increasing daily physical activity and decreasing daily consumption of sweets and savoury snacks and daily screen‐time behaviour.” “programme that consisted of two components: (i) guidelines and tips presented on a poster and (ii) a tailored feedback form for parents about their children’s activity‐ and dietary related behaviours.” Duration: 12 months Number of contacts: Unclear Setting: Preschool Modality: Face‐to‐face Interventionist: Researchers Integrity: No information provided Date of study: 2008 to 2009 Description of control: No information provided | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetables assessed using a 24‐item semi‐quantitative food frequency questionnaire (FFQ) completed by parents. Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 12 months Length of follow‐up post‐intervention: Immediate Subgroup analyses: None Loss to follow‐up: Intervention = 21% Control = 14% Analysis: Did not adjust for clustering Unknown if sample size calculations performed | |
| Notes | First reported outcome (grams fruit/day) was extracted for inclusion in the meta‐analysis. The reported estimate that adjusted for clustering did not report 95% CI or SEM. Therefore we used final values and calculated an effective sample size using ICC of 0.016 to enable inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake 2nd listed outcome after BMI | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Fruit and vegetable intake (parent reported): Parents were not blinded to group allocation and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Fruit and vegetable intake (parent reported): Parents were not blinded to group allocation and this is likely to influence performance |
| Incomplete outcome data (attrition bias) | High risk | FT: Of 203 children, 156 (77%) were re‐examined 12 months later at follow‐up (this is the first follow‐up post‐intervention). If we define this as short‐term follow‐up, this is high risk of bias as > 20% dropout |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | High risk | Baseline imbalance: Baseline differences were observed between the control and intervention groups in sociodemographic characteristics and body composition. However although this was adjusted for in the analysis the impact of this imbalance is unclear. “The analyses were adjusted for SES, age of the child and BMI Z‐score at baseline to control for the observed baseline imbalance in these variables between intervention and control groups.” Recruitment bias: Appears that parents and childcare centres were recruited after communities had been matched and randomised ‐ high risk Incorrect analyses: Linear mixed models adjusted for clustering within daycare centres, but standard errors were not reported. Reported mean (SD) by group at follow‐up and calculation of effective sample sizes prior to inclusion in meta‐analyses accounted for this, therefore low risk. |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "The development of the intervention was funded by the PWO(Project‐related Scientific Research)‐funding of University College Arteveldehogeschool. Funds for the evaluation were provided by the Provincial Government East‐Flanders." | |
| Participants | Description: Children attending 16 preschools in East Flanders (Belgium) N (Randomised) 16 preschools, 1432 preschoolers Age: (DOB) < 2002: intervention = 41%, control = 51% 2002: intervention = 28%, control = 24% 2003: intervention = 31%, control = 26% % Female: Intervention = 53%, control = 44% SES and ethnicity: Predominantly low parental education Low education (mother): intervention = 49%, control = 49% Low education (father): intervention = 60%, control = 57% Ethnicity: No information provided Inclusion/exclusion criteria: Not specified Recruitment: Schools were approached by mail for consent. All parents of preschoolers attending the consenting schools were asked to fill in a food frequency questionnaire Recruitment rate: Parents: 54% Schools: 10% (40 out of 403 schools consented, although only 8 were selected in the end) Region: East Flanders (Belgium) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 308, Control = 168 Description of intervention: 8 preschools received a multi‐component intervention to assist schools to implement a healthy school food policy. "The main objectives were to increase the consumption of fruit, vegetables and water and to decrease the consumption of sugared milk drinks and fruit juice." The main strategies to influence the child and the different environmental factors included: "Child: Guided and self‐guided activities based on experiential education (e.g. tasting) and developmental education (e.g. explanation of concepts of food triangle); Role model, feed back and reinforcement by teachers; Educational role‐model story and characters; Availability of healthy foods; Availability of cooking equipment. Parents: Newsletters; Suggestions for the back and forth diary; Work sheets and creations by children; Parent evenings and other school activities with parents Teacher: Training sessions; Manual including didactic and policy aspects; Digital learning environment; Newsletters; Group discussions with teachers; Examples of good practices School environment: Newsletters; Training sessions for principals and cafeteria staff; Help on demand via e‐mail; Examples of good practices; Policy aspects in the teachers’ manual; Feedback to schools." Duration: 6 months Number of contacts: Unclear (multicomponent) Setting: Preschool Modality: Multiple (staff training, experiential education, newsletters, email support, resources) Interventionist: Not specified Integrity: No information provided Date of study: Sept 2006 ‐ April 2007 Description of control: 8 preschools received the control: no information provided | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Daily consumption of fresh fruit and vegetables (grams) as reported by parents in a written food frequency questionnaire Length of follow‐up from baseline: 6 months (March/April 2007) Subgroup analyses: None Loss to follow‐up Intervention: 47% Control: 45% Analysis: Contact with the author indicated that the analysis was adjusted for clustering by school Unknown if sample size calculation was performed | |
| Notes | Trial results are reported as change from baseline in mean daily consumption of fruit and vegetables and post‐intervention values. No standard deviations were reported for post‐intervention data to enable inclusion in meta‐analysis Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake is primary outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Contact with the author indicated that a computerised random‐number generator was used |
| Allocation concealment (selection bias) | Unclear risk | Contact with the author indicated that schools did not know their allocation prior to consenting to the study. It is unclear if study personnel responsible for recruitment were aware of group allocation |
| Blinding of participants and personnel (performance bias) | High risk | Contact with the author indicated that parents and school staff were not blind to group allocation and that parents could have attended information sessions organised by the researchers, or observed posters, newsletters or intervention materials in intervention schools. Given that the relevant trial outcomes were based on parental reports, the review authors judged that there was a risk of bias |
| Blinding of outcome assessment (detection bias) | High risk | Contact with the author indicated that parents and school staff were not blind to group allocation and that parents could have attended information sessions organised by the researchers, or observed posters newsletters or intervention materials in intervention schools. Given that the relevant trial outcomes were based on parental reports, the review authors judged that there was a risk of bias. (NB. There were no independent outcome assessors in this trial; the parents completed and returned a food frequency questionnaire about their child's food intake) |
| Incomplete outcome data (attrition bias) | Unclear risk | Although similar across groups (intervention = 47%, control = 45%), rates of loss to follow‐up were high. Contact with the author indicated that no information was collected on reasons for loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | Contact with the author indicated that analysis was adjusted for clustering No further risk of bias identified |
| Methods | Study design: Randomised controlled trial Funding: Not reported | |
| Participants | Description: Children aged 2 to 6 years and their principal caregiver (parent) who were recruited from a larger study N (Randomised): 156 children Age: Child: 34 to 82 months (mean = 53 months) Parent: mean = 36 years % female: Children (by group): Exposure = 34%, Nutrition Information = 58%, Control = 51% Parent (overall): 95% SES and ethnicity: "68% of parents had left full‐time education at the age of 21 or over" and "the majority of parents held further education qualifications." Ethnicity = 74% white Inclusion/exclusion criteria: No explicit inclusion/exclusion criteria stated for this trial, or for the trial from which participants were recruited. 13 children (1 girl, 12 boys) were excluded when they did not comply with the experimental procedures during the pre‐experimental taste test Recruitment: Participants were recruited from a larger study on the predictors of children's fruit and vegetable intake and expressed an interest in participating in further research to modify their children’s acceptance of vegetables Recruitment rate: Parents: 28% Region: United Kingdom | |
| Interventions | Number of experimental conditions: 3 Number of participants (analysed): i) Restricted to at least 10 out of 14 exposures: Exposure = 34, Nutrition Information = 48, Control = 44 ii) All available data: Exposure = 48, Nutrition Information = 48, Control = 44 Description of intervention: Exposure: Taste exposure intervention carried out in the home where parents were asked to offer their child a taste of a target vegetable daily for 14 consecutive days. Parents were given suggestions to encourage the child to taste the vegetable. Parents were given a vegetable diary to record their experiences, and children could record their liking for the vegetable after each session using 'face' stickers. Nutrition Information: Parents were informed about the ‘5 a day’ recommendations and given a leaflet with advice and suggestions for increasing children’s fruit and vegetable consumption Duration: 14 days Number of contacts: 14 (daily for 14 consecutive days) Setting: The home Modality: Face‐to‐face, exposure Interventionist: Researchers trained parents to offer the target vegetable to their child Integrity: 14 participants in the exposure group failed to complete a minimum of 10 out of 14 tasting sessions. ‐ 4 children completed 9 sessions, 2 completed 8 sessions, 2 completed 7 sessions, 1 completed 6 sessions, 4 completed 5 or less sessions Date of study: Not provided Description of control: "No treatment" control ‐ parents received no further intervention | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: As‐desired consumption of target vegetable (grams) assessed by weighing the amount of the vegetable on the plate before and after consumption using a professional digital scale (Tanita Corporation, Japan) Length of follow‐up from baseline: Approximately 2 weeks Subgroup analyses: Restricted sample to only those in the taste exposure group who received 10 or more exposures. This restricted the Exposure group from 48 to 34 children. Loss to follow‐up: 2% (140 provided follow‐up data of 143 who were eligible and provided data at baseline). Exposure: 4% (children withdrawn from their study by their parents following collection of baseline data). Nutrition Information: 0% Control: 2% (children withdrawn from their study by their parents following collection of baseline data). Analysis: Adjustment for clustering not applicable Unknown if sample size calculation was performed | |
| Notes | "Two sets of analyses were carried out: (a) on a restricted sample which excluded those in the Exposure group who completed less than 10 tasting sessions (n=126) and (b) on the whole sample (n=140). Results below refer to the reduced sample size ... results for the whole sample are only included where they differed from these." Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake 3rd listed outcome after rated and ranked liking. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were randomly assigned to one of three experimental treatment groups". No further information provided regarding sequence generation |
| Allocation concealment (selection bias) | Low risk | Contact with the author indicated that allocation was concealed in an opaque envelope opened at participant's homes after baseline data collection |
| Blinding of participants and personnel (performance bias) | Low risk | Contact with the author indicated that personnel delivering the intervention were not blind to group allocation and that parents may not have been blind to group allocation. However, given the objective assessment of outcome (electronic scales), the review authors judged that the study outcome was unlikely to be affected by lack of blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Contact with the author indicated that the outcome assessors were not blind to group allocation. Given the objective measure of outcome (electronic scales), assessment is unlikely to have been influenced by lack of blinding |
| Incomplete outcome data (attrition bias) | Low risk | Rates of loss to follow‐up were similar and low across the exposure (4%), nutrition information (0%) and the control conditions (2%). Reasons for loss to follow‐up were provided and were similar |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Low risk | No further risk of bias identified |
| Methods | Study design: Randomised controlled trial Funding: "This work was commissioned by the Food Standards Agency in 2009 and supported by the Department of Health (UK) from 2010." | |
| Participants | Description: New mothers attending baby clinics in disadvantaged London neighbourhoods N (Randomised): 312 mothers Age: Children: mean = 10 weeks Parents: mean = 30 years % Female: Children = not stated Parents = 100% SES and ethnicity: 28% lone parents 57% living in social housing 33% receiving income support/job seeker's allowance Ethnicity: 50% from an ethnic minority Inclusion/exclusion criteria: Inclusion criteria: "Women from Registrar General occupational classes II‐V (non‐professional); babies born >/= 37 weeks; babies' birth weight above 2500g; singletons; women able to understand written and spoken English; and resident in the study area." Exclusion criteria: "Women aged under 17 years; infants were diagnosed with a serious medical condition or were on special diets; infants aged over 12 weeks; women or their partners were from social class I (professional). Originally their intention was to restrict the sample to first‐time mothers over the initial 12 week recruitment period. The inclusion criteria was therefore changed to include all new‐mothers." Recruitment: "Women were recruited from December 2002 to February 2004 at baby clinics located in the more disadvantaged neighbourhoods across Camden and Islington where Surestart (a national social welfare initiative targeting families with young children) programmes existed. A standardised technique was used to approach new mothers attending the baby clinics. An overview of the study was given and randomisation explained. If the women were interested, a short screening questionnaire was then used to assess their eligibility." Recruitment rate: Mothers: 82% Region: London, UK | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 124, Control = 115 (12 months) Intervention = 108, Control = 104 (18 months) Description of intervention: A monthly home visiting programme (from 3 to 12 months) delivered by trained local mothers, providing practical support on infant‐feeding practices. Duration: 9 months (duration of each visit = 60 min) Number of contacts: Monthly from 3 to 12 months (maximum = 10 contacts) Setting: The home Modality: Face‐to‐face, via home‐visiting Interventionist: Trained local volunteers "A group of local mothers were recruited and trained to provide the support in a 12‐session programme delivered over a 4‐week period." Integrity: "On average each woman in the intervention group received five volunteer home visits (range 1‐10). A small number of women were also contacted by telephone when home visits were not possible." Date of study: Recruited from Dec 2002 to Feb 2004 Description of control: Usual care. "Women in the control group only received standard professional support from health visitors and GPs." | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Children's intake of vitamin C from fruit Secondary outcome: Proportion of children who consumed specific fruits and vegetables more than once a week Length of follow‐up from baseline: 9 months and 15 months (when children aged 12 months and 18 months, respectively) Subgroup analyses: None Loss to follow‐up: (at 9 and 15 months) Intervention: 27%, 34% Control: 20%, 30% Analysis: Adjustment for clustering not applicable Sample size calculation was performed | |
| Notes | Vitamin C (mg) from fruit at the longest follow‐up < 12 months (9 months ‐ children aged 12 months) and ≥ 12 months (15 months ‐ children aged 18 months old) was extracted for inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Vitamin C intake from fruit listed as primary outcome | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A random allocation schedule was prepared in advance using random digit computer tables." |
| Allocation concealment (selection bias) | Low risk | "Those responsible for recruiting ... were all masked to group assignment." |
| Blinding of participants and personnel (performance bias) | High risk | Contact with the author indicated that parent participants and intervention personnel were not blind to group allocation. Given that the trial outcome was based on parental reports of children's fruit intake, the review authors judged that there was a risk of performance bias in this study |
| Blinding of outcome assessment (detection bias) | Low risk | "Those responsible for ... assessing outcomes were all masked to group assignment." |
| Incomplete outcome data (attrition bias) | High risk | Rates of loss to follow‐up were similar across intervention (27%, 34%) and control (20%, 30%) groups at both time points and were moderate. There were no substantial differences in the reasons for loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All primary or secondary outcomes of interest were reported according to the information provided in the trial register (ISRCTN 55500035) |
| Other bias | Low risk | Small deviation in protocol: The original sample was restricted to first‐time mothers but after 12 weeks of the 14‐month recruit this was broadened to all new mothers No further risks of bias identified |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "This research was supported by US Department of Agriculture’s (USDA) Food and Nutrition Service (FNS)." | |
| Participants | Description: Children attending childcare centres participating in the Child and Adult Care Food Program and their parent N (Randomised): 24 childcare centres, 1143 parent‐child dyads Age: Child: mean = 4.4 years Parent: “Overall, 67% of respondents were between the ages of 18 and 34” % Female: Child = 48% Parent: not specified SES and ethnicity: Parent: “40% were Hispanic or Latino; 24% were white, non‐Hispanic; 27% were black, non‐Hispanic; and 9% were another race or more than one race” Inclusion/exclusion criteria: Not specified Recruitment: “The study sampled child‐care centers participating in the Child and Adult Care Food Program in New York” “Approximately 5 to 6 weeks before the start of the intervention in spring 2010, teachers sent children home with a study invitation and the baseline survey. Parents who agreed to participate in the study were asked to return a contact information card and the completed questionnaire in a separate envelope to preserve confidentiality.” Recruitment rate: Parent: 75% (1143/1518) Region: New York (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 440, control = 462 Description of intervention: Eat Well Play Hard in Child Care Settings program “is a Supplemental Nutrition Assistance Program (SNAP) Education program that allows states to receive funding for nutrition education to improve the likelihood that SNAP participants will make healthy food choices.” “The program includes multilevel messaging targeted to preschool children, their parents, and the childcare center staff who shape the policies and practices in their child‐care environment.” “Some of the most frequently taught modules used for this intervention included trying new foods (Food Mood); eating a variety of vegetables (Vary Your Veggies); eating a variety of fruits (Flavorful Fruit); incorporating more healthy dairy products into the diet (Dairylicious); eating healthier snacks (Smart Snacking); and engaging in physical activity (Fitness Is Fun).” Duration: 6 ‐ 10 weeks Number of contacts: 6 classes for children and parents separately (30‐60 minutes per session) 2 classes for centre’s staff “Finally, the RDN works with each centre director to identify areas of policy improvement that can enhance nutrition at the centre and teaches at least two classes to the centre’s staff to help them integrate the program’s messages into their classroom activities” Setting: Preschool Modality: Multiple (face‐to‐face, printed materials/resources) Interventionist: Registered dietitian nutritionist Integrity: No information provided Date of study: March and June 2010 Description of control: Wait‐list control: “control centers received the intervention after the evaluation was completed, but within the same calendar year.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetables (cups per day) by parent self‐report via mail or telephone survey using modified questions from the University of California Cooperative Extension Food and Behaviour Checklist. Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: Unclear, ˜ 7 to 10 weeks Length of follow‐up post‐intervention: 1 week Subgroup analyses: None Loss to follow‐up: Intervention = 20% Control = 22% Analysis: Adjusted for clustering Sample size calculations performed | |
| Notes | First reported outcome (cups of vegetables child consumed at home a day) was extracted for inclusion in the meta‐analysis. We selected post‐intervention values over change from baseline estimates, and calculated effective sample size at follow‐up using an ICC of 0.014 to enable inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: Primary outcome not stated, power calculation conducted on fruit or vegetable intake | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Child’s fruit and vegetable intake (parent survey): There is no blinding to group allocation of participants or personnel described and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Child’s fruit and vegetable intake (parent survey): There is no blinding to group allocation of participants or personnel described and because this is a parent‐reported survey this is likely to influence detection bias |
| Incomplete outcome data (attrition bias) | High risk | 902 (79%) out of 1143 parents completed the follow‐up. Given this was a short‐term follow‐up, the risk of attrition bias is high |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | At baseline, children in the intervention group were statistically significantly older than children in the control group, but unclear what impact this may have had. “At baseline, children in the intervention group were statistically significantly older than children in the control group (difference=0.2 years; 95% CI 0.1 to 0.3). Otherwise, there were no statistically significant differences in the characteristics of respondents and their households or in outcome measures between the intervention and control groups at baseline”. Analyses accounted for clustering |
| Methods | Study design: Cluster‐randomised controlled trial Funding: Not reported | |
| Participants | Description: Children aged 4 or 5 years at 17 childcare centres N (Randomised): 17 childcare centres, 263 children Age: “The researchers were not permitted to obtain specific ages of each child but were informed by the centers’ directors that the majority of the children were 4 or 5 years old.” % Female: 47% SES and ethnicity: Not specified Inclusion/exclusion criteria: Not specified Recruitment: Not specified Recruitment rate: Unknown Region: Boise Idaho (USA) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention: fruit = 83, vegetable = 70 Control: fruit = 70, vegetable = 52 Description of intervention: “Color Me Healthy comes in a ‘‘toolkit’’ that includes a teacher’s guide, 4 sets of picture cards, classroom posters, a music CD that contains 7 original songs, a hand stamp, and reproducible parent newsletters. Color Me Healthy is composed of 12 circle‐time lessons and 6 imaginary trips. The majority of the CMH circle‐time lessons focus on fruits and vegetables of different colors. Several of the lessons provide opportunities for children to try fruits and vegetables. The 6 imaginary trips included in CMH encourage children to use their imagination to explore places, be physically active, and eat fruits and vegetables. Six interactive take home activities were developed for the current evaluation. These interactive activities coincided with the circle‐time lessons.” Duration: 6 weeks Number of contacts: 24 (preschool = 2 circle‐time + 1 imaginary trip per week, each 15 ‐ 30 minutes, home = 6 interactive take home activities) Setting: Preschool + home Modality: Face‐to‐face Interventionist: Lead teachers Integrity: No information provided Date of study: Unknown Description of control: No treatment control: “During the study, comparison classrooms did not incorporate nutrition curriculum into their lesson plans.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetable snacks (grams). “To determine the amount of fruit and vegetable snack consumed, the fruit and vegetable snacks were weighed (in grams) before they were served to children and then weighed again after children had had an opportunity to consume the snack. Percentage of fruit and vegetable snack consumed was calculated for each child.” Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 7 weeks (1 week post‐intervention) and ˜ 5 months (3 months post‐intervention) Length of follow‐up post‐intervention: 1 week and 3 months Subgroup analyses: None Loss to follow‐up (at 3 months): Intervention: fruit = 50%, vegetable = 58% Control: fruit = 29%, vegetable = 47% Analysis: Adjusted for clustering Unknown sample size calculations performed | |
| Notes | First reported outcome (mean number of pineapple snacks remaining) at the longest follow‐up (3 month follow‐up) was extracted for inclusion in meta‐analysis. Insufficient data available to enable inclusion in meta‐analysis (standard deviation not reported, nor available from authors) Sensitivity analysis ‐ primary outcome: Primary outcome not stated, fruit or vegetable intake is only reported outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated to experimental group but the random sequence generation procedure is not described |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Fruit and vegetable snacks (weighed): Objective measure of child’s fruit and vegetable intake and unlikely to be influenced by performance bias |
| Blinding of outcome assessment (detection bias) | Low risk | Fruit and vegetable snacks (weighed): Objective measure of child’s fruit and vegetable intake and unlikely to be influenced by detection bias |
| Incomplete outcome data (attrition bias) | High risk | Attrition rate > 20% for short‐term follow‐up. Only 58% of consenting children received fruit snacks at all 3 time points |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting |
| Other bias | Unclear risk | Recruitment bias: it appears that parents were invited to participate after centres had been randomised, so unclear risk of bias Baseline imbalance: there are no baseline data comparing study groups, so we cannot tell if groups were balanced at baseline, so unclear risk of bias Incorrect analysis: “The current evaluation was a nested design; children were nested within classrooms. The classrooms were the units of assignment, but the outcome data were collected among the children.” HLM modelling accounted for clustering, therefore low risk of bias |
| Methods | Study design: Cluster‐randomised controlled trial Funding: "The trial is funded by the Cancer Institute New South Wales (Ref no. 08/ECF/1‐18)." | |
| Participants | Description: Children aged 3 to 5 years attending selected preschools, and their parent N (Randomised): 30 preschools, 394 parent‐child dyads Age: Child (mean): Intervention = 4.3 years, Control = 4.3 years Parent (mean): Intervention = 35.7 years, Control = 35.7 years % Female: Child: Intervention = 51%, Control = 46% Parent: Intervention = 95%, Control = 97% SES and ethnicity: Household income AUD ≥ 100K: Intervention = 42%, Control = 40% University education: Intervention = 45%, Control = 50% Aboriginal and/or Torres Strait Islander: Child: Intervention = 1%, Control = 5% Parent: Intervention = 1%, Control = 3% Inclusion/exclusion criteria: Preschool: Inclusion criteria: licensed in NSW Exclusion criteria: “Preschools will be excluded from the trial if they provide meals to children in their care (as this limits parents' capacity to influence the foods their children consume), cater exclusively for children with special needs (given the specialist care required for such children), are Government preschools (as conduct of the research has not been approved by the New South Wales Government Department of Education and Training) or have participated child healthy eating research projects within six months of the commencement of recruitment.” Parent: Inclusion criteria: “participant must be a parent of a child aged 3 to 5 years attending a participating preschool, must reside with that child for at least four days a week (in order for the child to be sufficiently exposed to the intervention strategies that the parent may implement), must have some responsibility for providing meals and snacks to that child, and must be able to understand spoken and written English.” Exclusion criteria: “Parents will be excluded from the trial if their children have special dietary requirements or allergies that would necessitate specialised tailoring of the intervention or that may be adversely affected by the intervention. Such exclusions will be determined by an Accredited Practising Dietitian who is independent of the research team.” Recruitment: Preschools randomly selected “The supervisors of the selected preschools will be sent letters and consent forms informing them of the study and requesting permission to recruit parents through their services.” Recruitment packs will be delivered to each participating preschool Distribution of these packs to parents will occur via methods considered by the preschool supervisor to be most effective and appropriate in engaging parents Where possible, research staff will attend the preschool, hand out recruitment packs to parents and be available to answer parent questions Recruitment rate: Preschool = 51% (30/59) Region: New South Wales (Australia) | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention = 174, Control = 169 Description of intervention: The intervention group will receive a resource kit and weekly scripted telephone contacts. “The kit comprises a participant workbook containing information and activities, a pad of meal planners, and a cookbook including recipes high in fruit and vegetables.” “Each telephone contact aims to provide parents with appropriate knowledge and skills to modify three key domains within the home food environment: availability and accessibility of fruit and vegetables; supportive family eating routines, and parental role‐modelling.” Duration: 4 weeks Number of contacts: 4 (one a week) Setting: Home Modality: Telephone and mailed resources Interventionist: Trained telephone interviewers Integrity: “During each four‐week batch of telephone calls, members of the research team will monitor at least two completed calls made by each interviewer to assess adherence with the intervention protocol.” “In total, 44 intervention calls were monitored, representing 6% of all completed calls and an average of 9 calls per interventionist. Across all monitored calls, interventionists covered 97% of key content areas, and in .80% of calls they “rarely” deviated from the script. In instances in which calls deviated from the script, interventionists were provided with feedback immediately after the call, and the issue was raised during biweekly supervision.” Date of study: April to December 2010 Description of control: “Parents allocated to the control group were mailed the Australian Guide to Healthy Eating—a 22‐page booklet outlining the dietary guidelines and ways to meet them.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Child’s consumption of fruit and vegetables assessed by parent self‐report by telephone survey using items from the Children’s Dietary Questionnaire. Outcome relating to absolute costs/cost effectiveness of interventions: Not reported Outcome relating to reported adverse events: Effect of intervention on family food expenditure Length of follow‐up from baseline: 2 and 6 months Length of follow‐up post‐intervention: 1 and 5 months Subgroup analyses: None Loss to follow‐up (at 1 and 5 months): Intervention = 14%, 16% Control = 4%, 9% Analysis: Adjusted for clustering Sample size calculations performed | |
| Notes | The fruit and vegetable score outcome at the longest follow‐up < 12 months (6 months) was extracted for inclusion in meta‐analysis. The reported estimate and 95% CI which adjusted for baseline and clustering were included in meta‐analysis Sensitivity analysis ‐ primary outcome: Fruit or vegetable intake listed as primary outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random sequence was generated using a random‐number function in Microsoft Excel |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Fruit and vegetable intake (self‐reported): Participants were unblinded and this is likely to influence performance |
| Blinding of outcome assessment (detection bias) | High risk | Fruit and vegetable intake (self‐reported): Participants were unblinded and because self‐reported measure this is likely to influence detection bias |
| Incomplete outcome data (attrition bias) | Low risk | Of 394 parents, 343 (87%) completed the 6‐month follow‐up. Sensitivity analyses were also conducted where missing follow‐up data were imputed by using baseline observation carried forward |
| Selective reporting (reporting bias) | Low risk | The primary outcomes reported in the outcomes paper align with those specified in the protocol. The 12‐ and 18‐month fruit and vegetable outcomes are reported in Wolfenden 2014 |
| Other bias | Low risk | Contamination, baseline imbalance, & other bias that could threaten the internal validity are unlikely to be an issue. Analyses adjusted for clustering |
| Methods | Study design: Cluster‐randomised controlled trial Funding: “This project received financial support from the Fresh Produce Centre and the Ministry of Economic Affairs (grant number TU 1310‐086). Neither organization had any role in the design, analyses, or writing of this article.” | |
| Participants | Description: Infants aged 0‐4 years in 4 childcare centres in Utrecht, Netherlands N (Randomised): 4 childcare centres Age: Mean: intervention = 25.6 months, control = 25.0 months % Female: Intervention = 44%, control = 42% SES and ethnicity: Parent education level* ‐ intervention: low (0%), middle (5%), high (95%), control: low (0%), middle (10%), high (90%) *low = primary and/or secondary school, middle = vocational education, high = higher vocational education and/or university degree Inclusion/exclusion criteria: “Healthy children without any allergies to the study products could participate.” Recruitment: Recruited via 4 childcare centres in Utrecht, Netherlands “Information packs were distributed to 526 parents to inform them about the study aims and procedures.” Recruitment rate: Unknown Region: The Netherlands | |
| Interventions | Number of experimental conditions: 2 Number of participants (analysed): Intervention (2 centres): 101 children Control (2 centres): 91 children Description of intervention: “To prevent boredom and encourage tasting, each vegetable was presented in two different preparations: pumpkin blanched and as a cracker spread; courgette blanched and as soup; white radish raw and as a cracker spread.” “The study vegetables were offered during the habitual vegetable snack moment in the afternoon, between 15h00 and16h00.” “A vegetable song ‐ developed specifically for this study was played to make the vegetable eating occasion recognizable and fun for the children.” Duration: 21 weeks Number of contacts: Unclear, 21 weeks “was chosen to ensure that each child was exposed to each vegetable at least 10 times” Setting: Preschool Modality: Face‐to‐face Interventionist: Childcare employees Integrity: “Intervention children received on average six exposures to each vegetable product” Date of study: Unknown Description of control: “The control group kept their regular eating routines during this period.” | |
| Outcomes | Outcome relating to children's fruit and vegetable consumption: Consumption of vegetables (grams) as desired, assessed by weighing the vegetable cups before and after consumption. “Vegetable intake was calculated by subtracting the leftovers from the pre‐weight.” Outcome relating to absolute costs/cost‐effectiveness of interventions: Not reported Outcome relating to reported adverse events: Not reported Length of follow‐up from baseline: 21 weeks Length of follow‐up post‐intervention: 4 weeks Subgroup analyses: None Loss to follow‐up: Unclear Analysis: Unclear if adjusted for clustering Sample size calculations performed | |
| Notes | We extracted first reported outcome (mean g of pumpkin intake) for inclusion in meta‐analysis. We estimated mean and SD from a study figure using an online resource (Plot Digitizer: plotdigitizer.sourceforge.net) for intervention and control groups at post‐test. As an estimate at that adjusted for clustering was not reported, we used post‐intervention data and calculated an effective sample size using ICC of 0.014 to enable inclusion in meta‐analysis. Sensitivity analysis ‐ primary outcome: primary outcome not stated, sample size was based on vegetable intake outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Two childcare centres were randomly assigned to the intervention condition” Randomly allocated to experimental group but the random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | Low risk | Parents and child care staff were blinded to the aims of the study. The likelihood of performance bias in relation to vegetable consumption is low, given the children’s age. |
| Blinding of outcome assessment (detection bias) | Low risk | Research assistants present to observe process of weighing food and eating – however this seems unlikely to impact child consumption. Vegetable cups were weighed before and after consumption and therefore low risk of detection bias. |
| Incomplete outcome data (attrition bias) | High risk | Attrition rate > 20% (see Table 3) |
| Selective reporting (reporting bias) | Unclear risk | Trial protocol is not available |
| Other bias | Unclear risk | There may be potential recruitment bias as intervention and control parents were told different aims of the study (pg 318), which meant that researchers were aware of study group allocation before recruiting parents to study. Also unclear if clustering was accounted for during the analysis |
BMI: body mass index
EA: exposure alone
EP: exposure plus praise
ETR: exposure plus tangible non‐food reward
DOB: date of birth
FV: fruit and vegetables
ICC: intra‐class correlation
N/A: not applicable
PA: physical activity
SD: standard deviation
SEM: standard error of the mean
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This responsive feeding trial was ineligible as its primary outcome was not to increase fruit and vegetable consumption and the study only assessed children's fruit and vegetable consumption post‐hoc in order to describe the mechanism behind a change in weight status among participants in the sample | |
| No fruit or vegetable intake outcome | |
| Not RCT: editorial | |
| No fruit or vegetable intake outcome | |
| Not RCT | |
| Not RCT | |
| Study design: not RCT | |
| No fruit or vegetable intake outcome | |
| Children aged 6‐17 years | |
| Participants were Grade 3‐5 children | |
| Mean age of children 5.3 years | |
| Participant mean age 5.01 years | |
| Participants were 2nd and 3rd grade children | |
| Children aged 14‐17 years | |
| Not RCT: Editorial | |
| Not RCT: editorial | |
| Not RCT: editorial | |
| Not RCT: editorial | |
| Children aged 5‐9 years | |
| Participants were 4th grade children | |
| Participants were adult, no participants aged 0‐5 years | |
| Not RCT | |
| Primary outcome was not fruit or vegetable intake; primary outcome was dental caries incidence and prevalence of obesity | |
| No fruit or vegetable intake outcome, only assessed intake of fruit juice | |
| No fruit or vegetable intake outcome | |
| Mean age of participants was 9.8 years | |
| Participants were elementary school children | |
| Outcome is food choice (apple or crackers) | |
| Not RCT | |
| Children aged 9‐18 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome was weight and BMI | |
| Not RCT: Editorial | |
| Child mean age 6 years | |
| Children aged 8‐12 years | |
| Participants were aged 6‐12 years | |
| Intervention was not designed to increase fruit and/or vegetable consumption, intervention aimed to explore individual, family and environmental factors and their relationship to child weight status | |
| Outcome is quality of meals | |
| No fruit or vegetable intake outcome, only amount served | |
| Quasi‐experiemental design | |
| Participants were 6th and 7th grade children | |
| Not RCT: book review | |
| Participants were 3rd, 4th and 5th grade children | |
| No comparison group | |
| No fruit or vegetable intake outcome | |
| Children aged 12‐14 years | |
| Children aged 7‐12 years | |
| Study design: allocation to conditions not random | |
| Not randomised | |
| No control group | |
| Not RCT | |
| Child mean age of subgroups ranged from 5.8‐11 years | |
| No comparison group | |
| Child mean age 6.2 years | |
| Children aged 7‐9 years | |
| Outcome is vitamins and minerals, not fruit and vegetable consumption | |
| Participants were primary school children | |
| Participants were aged 6‐8 years | |
| Allocation of groups to condition was not randomised | |
| No fruit or vegetable intake outcome, outcome is preference | |
| No fruit and vegetable consumption outcome | |
| Children aged 8‐11 years | |
| No comparison group | |
| Children aged 6‐18 years | |
| No comparison group | |
| No comparison group | |
| Not RCT: Editorial | |
| Primary outcome was not fruit or vegetable intake; primary outcome was observed servings in packed lunch | |
| Not RCT ‐ review of resource | |
| No fruit and vegetable consumption outcome | |
| Non‐equivalent control group design | |
| Participants were 4th grade school children | |
| Primary outcome not F&V consumption, primary outcomes was parent engagement | |
| Participants were 5th grade students | |
| Child mean age 5.2 years | |
| Not RCT: descriptive review | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI and audits of home environment characteristics/lifestyle practice | |
| Outcome was willingness to taste kohlrabi | |
| Participants were children aged 6‐13 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome was body weight and waist circumference | |
| Primary outcomes were length for age score and rates of stunting | |
| No fruit and vegetable consumption outcome reported | |
| No fruit or vegetable intake outcome | |
| Allocation of groups to condition was not randomised | |
| Not RCT | |
| Children aged 9‐12 years | |
| No comparison group | |
| Child mean age 6 years | |
| Not RCT | |
| Study design: results are not reported by study group. Additionally the paper reports data from 3 other included studies: Caton 2013; Hausner 2012; Remy 2013 | |
| Participants mean age 6.15 years | |
| Participants were aged 5‐8 years old | |
| No comparison group | |
| No fruit or vegetable intake outcome, only number of days per week child consumes | |
| Children aged 8‐12 years | |
| Child mean age 8.6 years | |
| No fruit and vegetable outcomes | |
| Child mean age 8 years | |
| Quasi‐experimental: intervention sample randomly selected from 1 church. Control randomly selected from a separate church | |
| Children aged 5‐11 years | |
| No fruit or vegetable intake outcome | |
| Child mean age 9 years | |
| Children aged 5‐11 years | |
| Participants were children with mean age 5.16 years | |
| No comparison group | |
| No comparison group ‐ pretest‐post‐test design | |
| No fruit and vegetable consumption outcome | |
| No participants, these are guidelines, not research trial | |
| Child mean age 5.9 years | |
| Child mean age 8.3 years | |
| As per trial registry, fruit and vegetable consumption was not the primary outcome | |
| Participants were kindergarten‐grade 5 and grade 6‐8 children | |
| Participants were kindergarten‐grade 5 | |
| No child fruit or vegetable intake outcome | |
| Primary outcome was not fruit or vegetable intake; primary outcome was knowledge, attitudes and physical activity habits | |
| Child mean age 6 years | |
| No child fruit or vegetable intake outcome | |
| Related to Daniels 2014 ‐ No fruit and vegetable consumption outcome | |
| Not RCT | |
| Primary outcome was not fruit or vegetable intake as per trial registry | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Child mean age 9‐10 years | |
| No fruit or vegetable intake outcome, only assessed foods touched and tasted | |
| Child mean age in intervention group 6.05 year and in control group 5.98 years | |
| No fruit or vegetable intake outcome, only assessed liking and purchase request intent | |
| No fruit and vegetable consumption outcome | |
| No comparison group | |
| Quasi‐experimental, repeat cross‐sectional design | |
| Intervention was not designed to increase fruit and/or vegetable consumption | |
| Not RCT: Editorial | |
| No child fruit or vegetable intake outcome | |
| Children aged 9‐10 years | |
| Participants were 4, 5 and 6 grade children | |
| Not RCT: descriptive review | |
| Related to Duncanson 2013 ‐ does not report RCT results | |
| No fruit and vegetable consumption outcome | |
| Outcome no consumption measure | |
| Child mean age 6.6 years | |
| Children aged 6‐12 years | |
| Children aged 6‐11 years | |
| Children aged 7 years | |
| Not RCT | |
| Children aged 8‐12 years | |
| Children in 4th, 5th grade school | |
| No child fruit or vegetable intake outcome | |
| Participants were 3rd grade children | |
| No fruit and vegetable consumption outcome | |
| Cross‐sectional survey | |
| The intervention programme was not specifically designed to increase consumption of fruit and vegetables; instead primary aim is to illustrate a methodological concept. “This methodological note illustrates the use of co‐twin design for testing substitution, phenomenon, a prominent behavioural economics concept. We test whether fruits and vegetables can substitute for high‐fat snack foods in young children in a single meal laboratory setting.” | |
| Primary outcome as reported in trial registry was not fruit or vegetable intake | |
| Not RCT: measurement tool | |
| Child mean age 11 years | |
| Intervention was not designed to increase fruit and/or vegetable consumption | |
| No fruit and vegetable consumption outcome | |
| No fruit and vegetable consumption outcome | |
| No child fruit or vegetable intake outcome | |
| Not RCT: Editorial | |
| Outcome is weight change | |
| Not RCT | |
| Children aged 13‐19 years | |
| Children in 4th, 5th grade school | |
| Children in grades 1‐3 school | |
| Children aged 6‐13 years | |
| Outcome is child feeding attitudes and practices | |
| Intervention was not designed to increase fruit and/or vegetable consumption | |
| Participants were 5th, 7th and 8th grade students | |
| Not RCT: task force report | |
| Participants were parents of 8‐12 year‐old children | |
| No fruit and vegetable consumption outcome reported | |
| Participants were 1st and 2nd grade children | |
| Participants were aged 6‐11 years | |
| Children aged 8‐11 years | |
| Participants were aged 9‐12 years | |
| Participants were at least 18 years of age | |
| No comparison group | |
| Child mean age 7.5 years | |
| Children in 3rd, 4th, 5th grade school | |
| Children aged 8‐12 years | |
| No child fruit or vegetable intake outcome | |
| Not RCT: Editorial | |
| Participants were parents of primary school‐aged children | |
| Not RCT | |
| Child mean age 8.3 years | |
| Fruit and vegetable intake not primary outcome as per contact with author very low food security is primary outcome | |
| No comparison group | |
| Quasi‐experimental: childcare centres in existing study matched to other childcare centres, then randomised | |
| No child fruit or vegetable intake outcome | |
| No participants, not research trial | |
| Outcome not fruit and vegetable consumption | |
| Children aged 11‐16 years | |
| No comparison group | |
| Intervention was not designed to increase fruit and/or vegetable consumption | |
| Primary outcome was not fruit or vegetable intake; primary outcome was obesity | |
| No participants aged 0‐5 years | |
| Not RCT | |
| Participants were 3rd to 5th grade students | |
| No child fruit or vegetable intake outcome | |
| Children aged 9‐10 years | |
| Primary outcome not fruit and vegetable intake, primary outcome is BMI | |
| Children aged 5‐13 years | |
| Not RCT: Editorial | |
| No fruit and vegetable consumption outcome | |
| Participants were children aged 6‐14 years | |
| Not a randomised study design | |
| No fruit or vegetable intake outcome, only assessed lunchbox contents | |
| No child fruit or vegetable intake outcome | |
| Child mean age 6.3 years | |
| Participants were primary school children ‐ aged 4‐12 years old | |
| Children aged 5‐12 years | |
| No child fruit or vegetable intake outcome | |
| No fruit and vegetable consumption outcome | |
| No assessments of children included in study | |
| Participants had mean age of 5.2 years | |
| No fruit and vegetable consumption outcome | |
| Children in 4th and 6th grade school | |
| Primary outcome was not fruit or vegetable intake; primary outcome was food neophobia and staff feeding practices | |
| Primary outcome was not fruit or vegetable intake; primary outcome was food neophobia and staff feeding practices | |
| No comparison group | |
| No comparison group | |
| Participants were 1st, 2nd and 4th grade children | |
| Participants were 1st and 6th grade children | |
| Not RCT: Editorial | |
| No comparison group | |
| Primary outcome not fruit and vegetable intake as per trial registry | |
| Child mean age 6.2 years | |
| Participants were 6th‐12th grade children | |
| F&V intake not primary outcome as per trial registry BMI is primary outcome | |
| Participants were Kindergarten‐5th Grade children | |
| Not RCT ‐ allocation was not randomised | |
| No child fruit or vegetable intake outcome | |
| Child mean age 7 years | |
| Non‐equivalent control group study design | |
| Intervention was not designed to increase fruit and/or vegetable consumption, intervention aimed to increase the consumption of orange sweet potato over consumption of white and yellow sweet potato | |
| Intervention was not designed to increase fruit and/or vegetable consumption, intervention aimed to increase the consumption of orange sweet potato over consumption of white and yellow sweet potato | |
| No comparison group | |
| Outcome is eating behaviours and weight, not fruit and vegetables | |
| Outcome is feeding styles and behaviour | |
| No fruit and vegetable consumption outcome | |
| Fruit and vegetable intake not primary outcome, primary outcome combined health behaviour score | |
| Children aged 9‐12 years | |
| No fruit and vegetable consumption outcome | |
| Not RCT | |
| No child fruit or vegetable intake outcome | |
| No comparison group | |
| No child fruit or vegetable intake outcome | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Participants were children with mean age 5.8 years | |
| Fruit and vegetable intake not primary outcome | |
| Outcome is food choice | |
| This study was excluded as fruit and vegetable consumption was measured in terms of dietitian‐classified 'appropriate' versus 'inappropriate' consumption levels, and as such, it failed to meet the inclusion criteria relating to the primary outcome | |
| Outcome is food preference and ranking | |
| No child fruit or vegetable intake outcome | |
| No child fruit or vegetable intake outcome | |
| No comparison group | |
| Participants were elementary school children | |
| No child fruit or vegetable intake outcome | |
| Participants aged 6‐12 years | |
| No participants, not research trial | |
| Fruit and vegetable intake not primary outcome | |
| Not RCT | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Child mean age 10 years | |
| Participants mean age 5.28 years | |
| Children in 6th grade school | |
| Not RCT: Editorial | |
| Participants were adults | |
| Not RCT: review | |
| Dietary outcomes are not reported for the control group and no comparison is made between experimental conditions | |
| Quasi‐experimental: 2 areas, 1 intervention, 1 control, not randomly selected | |
| Outcome is proportion being fed bananas | |
| Child mean age 9.3 years | |
| Primary outcome was exclusive breastfeeding | |
| Participants aged 8‐9 years | |
| Primary outcome was not fruit or vegetable intake | |
| No fruit and vegetable consumption outcome | |
| Child mean age 5.18 years | |
| No participants aged < 5 | |
| No fruit and vegetable consumption outcome | |
| No comparison group | |
| No outcome data reported ‐ related to ongoing study Seguin 2017 | |
| Quasi‐experimental: 8 intervention schools; 8 matched control schools | |
| No fruit or vegetable intake outcome, only number of pieces of food consumed | |
| Not RCT: Editorial | |
| Participants were children with mean age 5.9 years | |
| Not RCT: review | |
| No comparison group | |
| No comparison group | |
| No child fruit or vegetable intake outcome | |
| Child mean age 7.9 years | |
| No fruit and vegetable outcome | |
| No fruit and vegetable consumption outcome | |
| Fruit and vegetable consumption was secondary outcome | |
| No comparison group ‐ pretest‐posttest design | |
| Participants were adolescents | |
| No fruit and vegetable outcome | |
| No child fruit or vegetable intake outcome | |
| Not RCT | |
| No fruit and vegetable consumption outcome | |
| Not RCT | |
| Child mean age 6 years | |
| Participants were fathers of children aged 5‐12 years | |
| No comparison group | |
| Not RCT ‐ Editorial | |
| No child fruit or vegetable intake outcome | |
| Not RCT: Editorial | |
| Quasi‐experimental, 2 intervention areas, and 1 control area selected, in prospective longitudinal study | |
| Child mean age 8.8 years | |
| Intervention was not designed to increase fruit and/or vegetable consumption, intervention aimed to improve children's emotional and behavioural self regulation on preventing obesity | |
| Not RCT ‐ treatment group not randomised | |
| Not RCT | |
| Not RCT | |
| Not RCT | |
| No fruit and vegetable consumption data | |
| Related to Daniels 2014 ‐ only reports data from the control group | |
| Child mean age 5.7 years | |
| Not RCT | |
| No comparison group | |
| No outcome data ‐ related to ongoing study Østbye 2015 | |
| Not RCT ‐ resource review | |
| Child mean age 9 years | |
| No child fruit or vegetable intake outcome | |
| Children aged 12‐14 years | |
| Participants were children with mean age 5.4 years | |
| No comparison group | |
| Primary outcome was not fruit or vegetable intake; primary outcome was parental habit strength | |
| Child mean age 6.3‐6.8 years | |
| F&V not primary outcome, primary outcomes were related to feasibility | |
| No comparison group | |
| Child mean age 9.9 years | |
| No fruit and vegetable consumption outcome | |
| Participants were children aged 8‐13 years | |
| Participants aged 8‐14 years | |
| Fruit and vegetable not primary outcome, primary outcome Vitamin D plasma concentrations | |
| No comparison group ‐ cross‐sectional study | |
| Not RCT ‐ quasi‐experimental | |
| Not RCT | |
| Participants were aged 5‐12 years old | |
| Participants were Grade 1‐5 students | |
| No fruit and vegetable outcome | |
| Participants mean age 6.12 years | |
| Participants aged 8.0‐16.9 years | |
| Guidelines not trial, so no participants | |
| Primary outcome was not fruit or vegetable intake as per trial registry | |
| Mean age of participants 5.85 years | |
| Child mean age 5.5 years | |
| Children aged 8‐11 years | |
| No fruit and vegetable consumption outcome | |
| No fruit and vegetable intake outcome | |
| Not fruit and vegetable intake outcome reported, only preference. | |
| No child fruit or vegetable intake outcome | |
| Not RCT | |
| Primary outcome is frequency of exclusive and total breastfeeding as per trial registry | |
| Fruit and vegetable not primary outcome, primary outcome was BMI | |
| No comparison group | |
| Fruit and vegetable not primary outcome ‐ primary outcomes relate‐school readiness, physical health etc | |
| Participants aged 6‐9 years | |
| Children aged 7‐13 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Participants were children in 2nd and 3rd grade | |
| Children in 4th grade school | |
| Children in 3rd, 4th grade school | |
| Outcome is process evaluation | |
| No fruit and vegetable consumption outcome | |
| Children in 3rd, 4th grade school | |
| Primary outcomes are children's body mass index and waist circumference at four years | |
| No child fruit or vegetable intake outcome | |
| The average age was 5.1 years (SD 0.8, range 4‐6.8 years) | |
| The average age was 5.1 years (SD 0.8, range 4‐6.8 years) | |
| No fruit and vegetable consumption outcome | |
| Participants were 3rd‐5th grade children | |
| Participants aged 5‐11 years | |
| Child mean age 11.7 years | |
| Participants aged 5‐15 years | |
| No child fruit or vegetable intake outcome | |
| Participants were primary school children | |
| Not RCT ‐ resource review | |
| Outcome asks if vegetables eaten today (Yes/No). No amount provided | |
| Non‐RCT. 1 intervention sample and 1 matched control sample | |
| Child mean age 6.7 years | |
| Children aged 9‐12 years | |
| No child fruit or vegetable intake outcome | |
| Quasi‐experimental: consenting schools paired then randomised to 1 of 2 interventions. Control schools in different area identified and then matched | |
| Primary aim (as per trial registry) is mean height for age z‐scores | |
| Primary outcome was not fruit or vegetable intake, primary outcome was weight | |
| Children aged 8‐10 years | |
| Participants were 4th grade children | |
| No fruit or vegetable intake outcome, only assessed diet quality | |
| Children aged 6‐11 years | |
| No fruit and vegetable intake outcome | |
| Children aged 9‐10 years | |
| Child mean age 8.6 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome was waist circumference and self‐esteem | |
| Not RCT ‐ quasi‐experimental non‐randomized study | |
| Child mean age 11 years | |
| As per trial registry, fruit and vegetable not primary outcome, anthropometry is primary outcome | |
| Not RCT | |
| No comparison group | |
| No fruit or vegetable intake outcome, only assessed child‐feeding practices | |
| The intervention programme was not specifically designed to increase consumption of fruit and vegetables. The aim of intervention, as reported in a separate paper (Lapinleimu 1995) is“to investigate the effects of an individually supervised, eucaloric, diet with low content of fat, saturated fat and cholesterol in healthy children” | |
| Children aged 6‐17 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Child mean age 8 years | |
| No fruit and vegetable outcome | |
| Intervention was not designed to increase fruit and/or vegetable consumption, intervention focused on dietary fat quality | |
| Comparison between treatment groups not reported for fruit and vegetable consumption | |
| Participants were 4th grade students | |
| Participants were parents of children with mean age of 10 years | |
| Child participants had median age of 12.9 years | |
| Study design used convenience sample | |
| Quasi‐experimental ‐ 2 elementary schools randomly allocated to 1 intervention and 1 control | |
| Not RCT | |
| Intervention did not aim to increase consumption of fruit or vegetables | |
| Participants were 1st grade children | |
| Participants were children aged 6‐11 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Not RCT as confirmed by author | |
| No child fruit or vegetable intake outcome | |
| Participants were 4th‐6th grade children | |
| No comparison group | |
| Not RCT | |
| No child fruit or vegetable intake outcome | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| No fruit and vegetable intake outcome | |
| No comparison group | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Not RCT | |
| No comparison group | |
| Review, not trial, no participants | |
| Participants were 4th and 5th grade students | |
| Primary outcome was not fruit or vegetable intake; primary outcome was change in overall knowledge, attitudes and habits | |
| Participants were parents of elementary school children | |
| No fruit and vegetable consumption outcome | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Not RCT ‐ allocation not randomised | |
| Participants were parents of children aged 5‐13 years | |
| Participants mean age 5.84 years | |
| Participants were Kindergarten and 1st grade children | |
| No fruit and vegetable intake outcome | |
| Primary outcome was not fruit or vegetable intake; primary outcome was observed servings in packed lunch | |
| No comparison group | |
| Child mean age 7.7 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Participants were primary school‐aged children 4‐11 years old | |
| No child fruit or vegetable intake outcome | |
| Primary outcome, as per trial registry, was not fruit or vegetable intake | |
| Not RCT: review | |
| Participants' mean age 6.5 years | |
| Fruit and vegetable intake not primary outcome, primary outcome was anthropometric measures as per trial registry | |
| Children aged 10‐13 years | |
| Primary outcome was not fruit and vegetable intake | |
| Fruit and vegetable intake not primary outcome, primary outcome was weight‐for‐length | |
| Not RCT: Editorial | |
| Not RCT ‐ allocation not random | |
| Fruit and vegetable intake not primary outcome, primary outcome was BMI | |
| Not RCT ‐ allocation not random | |
| Not RCT ‐ uses baseline data from an ongoing study ‐ Østbye 2015 | |
| Not RCT | |
| No comparison group ‐ cross‐sectional survey | |
| Participants were 4th and 5th grade school children | |
| Participants were aged 8‐12 years | |
| Outcome was eating habits | |
| Participants were primary school children aged 4‐11 years | |
| Not RCT | |
| Not RCT | |
| Not a RCT | |
| Children aged 8‐10 years | |
| Not RCT: Editorial | |
| Not RCT: commentary | |
| No fruit and vegetable intake outcome | |
| No fruit and vegetable outcome | |
| Children school‐aged | |
| Outcome was weight, not fruit and vegetable consumption | |
| Children aged 9‐19 years | |
| Not RCT | |
| Primary outcome was not fruit or vegetable intake; primary outcome was Healthy Eating Index | |
| Fruit and vegetable intake not primary outcome, as per trial registry primary outcome was exclusive breastfeeding | |
| Participants had mean age of 5.5 years (intervention) or 5.4 years (control) | |
| Primary outcome, as per trial registry, was not fruit or vegetable intake; primary outcome was BMI | |
| Participants were middle school children | |
| Participants were middle school children | |
| Primary outcome was not fruit or vegetable intake; primary outcome was percent body fat | |
| Primary outcome is change in centre's nutrition environments | |
| Child mean age 6 years | |
| Participants were children aged 8‐16 years | |
| Not RCT ‐ cross‐sectional | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Primary outcome: duration of breastfeeding and timing of introduction of solids, as described in the published research protocol | |
| Primary outcome was not fruit or vegetable intake; primary outcome was good eating behaviour | |
| Fruit and vegetable intake was secondary outcome | |
| Participants were elementary school children | |
| Study design in intervention and matched control site | |
| No fruit and vegetable intake outcome | |
| Children aged 6‐12 years | |
| Participants were primary school children | |
| No fruit and vegetable consumption outcome | |
| Children aged 9‐10 years | |
| No child fruit or vegetable intake outcome | |
| No fruit and vegetable intake outcome | |
| Intervention was not designed to increase fruit and/or vegetable consumption | |
| Fruit and vegetable intake was not primary outcome, primary outcome was children's service compliance with dietary guidelines | |
| No fruit and vegetable intake outcome | |
| Primary outcome was not fruit or vegetable intake; primary outcome was BMI | |
| Participants were children with mean age 5.1‐5.2 years | |
| Participants were young adults | |
| Not RCT | |
| Child mean age as reported by author 8.6 years | |
| Children aged 11‐15 years | |
| Primary outcome was not fruit or vegetable intake; primary outcome as per trial registry was BMI |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | No full text available to determine eligibility. Contact with author reported chapter describing study currently underway |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Full text only available in Persian. Translation has been sought. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Healthy start‐Départ santé |
| Methods | Cluster‐randomised controlled trial |
| Participants | Approximately 735 children aged 3‐5 years from 62 Early Childcare Centres |
| Interventions | Intervention: “The intervention is composed of six interlinked components which are presented in more detail in Fig. 1. These components include: 1) intersectoral partnerships conducive to participatory action that leads to promoting healthy weights in communities and ECC; 2) the Healthy Start‐Départ Santé implementation manual for educators on how to integrate healthy eating and physical activity in their centre; 3) customized training, role modelling and monitoring of Healthy Start‐Départ Santé in ECC; 4) the evidence‐based resource, LEAP‐GRANDIR [16], which contains material for both families and educators; 5) supplementary resources from governmental partners; and 6) a knowledge development and exchange (KDE), and communication strategy involving social media and web‐resources to raise awareness and mobilize grassroots organizations and communities. Healthy Start‐Départ Santé is delivered over 6‐8 months and includes a partnership agreement, an initial training session which orients ECC staff to the concepts, the implementation manual and the use of resources, on‐going support and monitoring over time, one tailored booster session, and a family day to celebrate the ECC’ success at the end of the intervention.” Control: “Usual practice controls” “Control sites are given the option of receiving the intervention once their participation in the evaluation has been completed” |
| Outcomes | Usual intake of fruits and vegetables assessed via parent‐reported semi‐quantitative food frequency questionnaire |
| Starting date | Participant recruitment began in Autumn 2013 |
| Contact information | Anne Leis: [email protected] |
| Notes |
| Trial name or title | Simply Dinner Study |
| Methods | Multiphase Optimization Strategy (MOST), where the main, additive and interactive effects of 6 support strategies are first tested in a screening phase to identify the intervention components most robustly associated with increased family meals and improvements in dietary quality. The MOST factorial design includes 6 intervention components with a Usual Head Start Exposure condition (usual‐care control); thus, individual participants are randomised to one of 64 experimental conditions. The 64 experimental conditions result from the crossing of 6 Simply Dinner intervention components, each of which has 2 conditions (present vs. not), and reflect all possible pairings of the intervention components, including a no‐intervention condition. These components are then tested in the confirming phase via RCT. |
| Participants | Families from Head Start preschools (disadvantaged families) |
| Interventions | 6 intervention components ranging from the most to least intense forms of support
|
| Outcomes | Children’s diet quality over the previous week assessed using the Block Dietary Data Systems Kids Food Screener—Last Week (Version 2) |
| Starting date | Screening design: "planned completion is Dec 2017” Confirming RCT planned to commence in September 2018 |
| Contact information | Holly‐E Brophy‐Herb: [email protected] |
| Notes | Clincaltrials.gov Identifier NCT02487251; Registered 26 June 2015 |
| Trial name or title | Early food for future health: a randomized controlled trial evaluating the effect of an eHealth intervention aiming to promote healthy food habits from early childhood |
| Methods | Randomised controlled trial of parents with children aged between 3 and 5 months recruited through Norwegian child health centres and announcements on Facebook Baseline questionnaires assessed eating behaviour and feeding practices, food variety and diet quality. All participants will be followed up at ages 12 and possibly 24 and 48 months, with questionnaires relating to eating behaviour and feeding practices, food variety and diet quality. |
| Participants | Parents of children aged between 3 and 5 months |
| Interventions | The intervention group received monthly emails with links to an age‐appropriate website when their child was between 6 and 12 months |
| Outcomes | Eating behaviour and feeding practices, food variety and diet quality |
| Starting date | Participant recruitment began in March 2016 |
| Contact information | Christine Helle: |
| Notes | ISRCTN13601567 |
| Trial name or title | Healthy Me, Healthy We (HMHW) trial |
| Methods | 2‐arm, cluster‐randomised controlled trial, where childcare centres are randomly assigned to an intervention or waitlist control group |
| Participants | 96 childcare centres located in central North Carolina (NC), USA Classroom teachers of children aged 3‐4 years 768 parents and children dyads (aged 3‐4 years) |
| Interventions | 8‐month social marketing campaign delivered over the year targeting childcare teachers and parents Childcare component involves a kick‐off event including hanging of study (HMHW) banner, inviting parents to attend, hanging of classroom poster, signing the Fit Family Promise and engaging in classroom activity. Kick‐off event followed by four 6‐week classroom units targeting healthy eating and physical activity goals through both classroom and home components. Home components include a family guide (targeted at achieving unit goals) and activity tracker (to track completion of at‐home activities), and aim to help parents partner with the childcare centre. Control: waitlist control group |
| Outcomes | Primary: children's dietary intakes will be assessed using a combination of direct observation of foods and beverages consumed while at the centre and parent‐completed food diaries. Dietary intake at child care (outside of parent's supervision) will be assessed by trained data collectors during observations of participating children during breakfast/morning snack, lunch, and afternoon snack using the Diet Observation in Child Care protocol. Children’s diet quality will be assessed with Healthy Eating Index (HEI) scores |
| Starting date | October (year unclear) |
| Contact information | Heidi Hennink‐Kaminski: [email protected] |
| Notes | Registered at ClinicalTrials.gov (NCT0233‐345, 23 December 2014) |
| Trial name or title | The healthy toddlers trial |
| Methods | Randomised controlled trial |
| Participants | Approximately 600 children aged 12 to 26 months recruited from community programmes, immunisation clinics and food pantries |
| Interventions | Intervention: “HT addresses core nutrition concepts but moves well beyond basic nutrition to address maternal self‐efficacy during feeding, appropriate feeding styles, and practices, including skill development to increase success in making these behavioural changes.” “The HT intervention consists of eight in‐home visits by a specially trained paraprofessional instructor plus four weekly telephone follow‐up reinforcement contacts. Particularly for high‐risk families with young children, providing services within the context of the family’s home environment appears to be a useful and effective strategy to provide parents with information, emotional support, access to other services and direct education [19]. The home‐visitation model also engages families who lack transportation or child care, a challenge frequently reported by families with low incomes. Paraprofessional instructors are peer educators who can relate to the target audience. Research shows that people learn best from their peers (people like themselves). Eight home visit sessions have been found to produce behavioral change [20]. At each visit, the paraprofessional spends approximately 1 hour with the mother and toddler dyad. The HT lessons use a variety of techniques and materials to enhance each mother’s learning experience and help reinforce knowledge. Each lesson includes opportunities for discussion, hands‐on activities, and an opportunity for mothers to practice skills covered in the lesson. The eight lessons include a lesson plan, handouts, and recipes. Mothers receive a notebook binder at the beginning of Lesson 1.” Control: “The control group families receive the usual services provided by Building strong families (BSF) or Expanded Food and Nutrition Education Program (EFNEP) in respective states. These families are newly enrolled into BSF or EFNEP as part of the HT study and have not received home visitation previously. The control lessons are similarly delivered as the HT lessons, such that, a paraprofessional instructor provides eight lessons during an in‐home visit, which last approximately 60 minutes. However, the control lessons focus on parenting (BSF) or nutrition (EFNEP) and do not include extensive content on feeding toddlers. Paraprofessionals who provide the lessons for the control group families are different to prevent cross contamination between the two groups.” |
| Outcomes | Child fruit and vegetable intake will be assessed via 3‐day dietary record of child’s intake |
| Starting date | Unknown |
| Contact information | Mildred Horodynski: [email protected] |
| Notes |
| Trial name or title | First food for infants (Randomized controlled trial evaluating a cooking intervention to improve parental cooking skills and thereby improve dietary intake in infants aged 6‐12 months) |
| Methods | Randomised controlled trial |
| Participants | Approximately 160 children aged 5‐6 months attending selected public health clinics and their parent(s) |
| Interventions | Intervention: the intervention group is invited to a 2‐day course including some theory of infant nutrition, and a main focus on increasing practical food cooking skills (i.e. how to prepare and cook the first food for infants). They are also taught how to store food and how to be confident in making infants’ food themselves. 5 groups of participants attend the course on two different days. Each of the 2 course days lasts 4 hours, and parents are given theoretical knowledge about the infant's first food as well as practical knowledge on how to make nutritious and varied food. Control: parents receive a booklet containing recipes for homemade foods for infants. |
| Outcomes | Food intake, measured using food frequency questionnaire |
| Starting date | The trial started in June 2012 |
| Contact information | Nina Cecilie Øverby: [email protected] |
| Notes | ISRCTN45864056 |
| Trial name or title | A cluster randomized web‐based intervention trial among one‐year‐old‐children in kindergarten to reduce food neophobia and promote healthy diets |
| Methods | Cluster‐randomised controlled trial |
| Participants | Approximately 306 children born in 2016, attending kindergartens in the counties of Oppland and Telemark in Norway |
| Interventions | Intervention group 1: kindergartens will be asked to serve a warm lunch meal with a variety of vegetables 3 days a week during the intervention period which will last for 3 months. Intervention group 2: kindergartens will be asked to use given pedagogical tools including sensory lessons (the Sapere method) and advice on meal practice and feeding styles, in addition to serving the same meals as intervention group 1. Control: control kindergartens will continue their usual practices. |
| Outcomes | Child vegetable intake, dietary habits and food variety using detailed questionnaires developed for this specific study |
| Starting date | The trial started in August 2017 |
| Contact information | Nina Cecilie Øverby: [email protected] |
| Notes | ISRCTN98064772 |
| Trial name or title | Happy child study |
| Methods | Two‐arm, cluster‐randomised controlled trial with outcomes assessed at baseline and after 9 months, via a self‐constructed questionnaire |
| Participants | Male and female children aged 3‐6 years attending kindergartens |
| Interventions | Programme in kindergarten setting that aims for the development of a healthy lifestyle of kindergartners, offering alternatives for their diet, exercise behaviour and leisure‐time activities delivered by the child‐care workers. The programme is carried out in the course of a kindergarten year supported by especially developed pre‐structured lessons to be integrated into the daily routine as well as the involvement of parents. The programme’s goal is the increase of physical activity of kindergartners, the reduction of consumption of sweetened drinks as well as the reduction of time spent in front of computers and TVs. |
| Outcomes | Changes in dietary intake of fruit and vegetables |
| Starting date | September/October 2016 |
| Contact information | Susanne Kobel: susanne.kobel at uni‐ulm.de |
| Notes | DRKS00010089 |
| Trial name or title | Learning to like vegetables during breastfeeding |
| Methods | Dyads were randomly assigned into the following groups who differed in the timing and duration of when lactating mothers drank vegetable juices during their infants’ first 4 months postpartum as follows: exposure from 0.5‐1.5 months (1M0.5), exposure from 1.5‐2.5 months (1M1.5), exposure from 2.5‐3.5 months (1M2.5), exposure from 0.5‐3.5 months, or no exposure (control group) |
| Participants | 97 mother‐infant dyads |
| Interventions | Lactating mothers drank vegetable, beet, celery, and carrot juices for 1 month beginning at 0.5, 1.5, or 2.5 months postpartum or for 3 months beginning at 0.5 months postpartum. Mothers in all groups were given 118‐mL cups from which to drink the juice (exposure group) or water (control group). Women in the experimental groups were provided with monthly supplies of the juices gratis at the beginning of the exposure month (i.e. 0.5, 1.5, or 2.5 months) or months (0.5–2.5 months). The women were instructed to drink a cupful (118 mL) of the vegetable juices per occasion during their particular month or months of exposure (resulting in 24 total exposures/month; 8 carrot juice exposures; and 8 vegetable juice exposures, 4 beet juice exposures, and 4 celery juice exposures). Control group drank equal volumes of water and avoided drinking the juices |
| Outcomes | The number of minutes that elapsed from the start to end of feeding was the duration of the feed, and the amount consumed was determined by weighing the bowl immediately before and after each feed on a Mettler balance (model SG1600; Mettler‐Toledo). All food that was spilled onto the tray or bib during the feed was placed in the bowl before weighing |
| Starting date | Unclear |
| Contact information | Julie A Mennella: [email protected] |
| Notes | This trial was registered at clinicaltrials.gov as NCT01667549 |
| Trial name or title | A randomised control trial of an educational and taste‐exposure intervention to promote vegetable intake in preschool aged children |
| Methods | Cluster‐randomised control trial |
| Participants | 160 children aged 2‐5 years |
| Interventions | Taste exposure: children will be repeatedly offered the single vegetable, which is unfamiliar to them over the 12‐week period. Children will be offered 40 g of the vegetable by their usual nursery staff. Nutritional education: nursery staff will be trained by the PhunkyFoods team to deliver the nutritional education programme. Children will be taught Eat Well (learning about different food groups) and Strive for Five (learning about eating fruits and vegetables) components of the PhunkyFoods education programme by their usual nursery staff. Nurseries will be advised to deliver as much as possible of the two components over the 12‐week period. Taste exposure and nutritional education: children will be repeatedly offered a single unfamiliar vegetable over the 12‐week period as well as receive the PhunkyFoods educational programme (Eat Well and Strive for Five components). Children will be offered the vegetable and nutritional education by their usual nursery staff. No intervention control: children will be offered a single unfamiliar vegetable at the beginning, end and at the follow‐up. They will be offered the nutritional education after the completion of the study. |
| Outcomes | Intake of an unfamiliar vegetable measured using weight in grams |
| Starting date | The trial started in September 2016 |
| Contact information | Chandani Nekitsing: [email protected] |
| Notes | NCT03003923 |
| Trial name or title | What promotes healthy eating? |
| Methods | Factorial, randomised controlled trial |
| Participants | 7200 mother‐father‐child pairs |
| Interventions | Group 1: weekly maternal nutrition behaviour‐change communication (BCC) sessions for 4 months Group 2: weekly maternal nutrition BCC sessions for 4 months and weekly paternal nutrition BCC sessions for 3 months Group 3: receipt of a food voucher for 6 months (randomly select 1 parent) Group 4: weekly maternal nutrition BCC sessions for 4 months and receipt of a food voucher for 6 months Group 5 weekly maternal nutrition BCC sessions for 4 months and weekly paternal nutrition BCC sessions for 3 months and receipt of a food voucher for 6 months Control group: unspecified |
| Outcomes | Child dietary diversity score Mean difference in child dietary diversity score defined by consumption of number of food group consumed by a child Food consumption score Mean difference in food consumption score calculated using the frequency of consumption of different food groups consumed by a child. |
| Starting date | Registration date: 25 July 2017 – status was recruiting |
| Contact information | Hyuncheol Kim : [email protected] |
| Notes | This trial was registered at clinicaltrials.gov as NCT03229629 |
| Trial name or title | Baby's first bites (The what and how in weaning: a randomised controlled trial to assess the effects of vegetable‐exposure and responsive feeding on vegetable acceptance in infants and toddlers) |
| Methods | Randomised controlled trial |
| Participants | 240 first‐time mothers of healthy term infants |
| Interventions | Intervention A: this intervention repeatedly exposed infants and toddlers to vegetables and involved 2 days of pre‐test, a 15‐day feeding schedule and 2 days of post‐test. During 15 consecutive days, children are exposed to one of two target vegetables according to a set scheme where one target vegetable is offered to the infant every other day. On the days in between, infants receive other vegetables for variety. During the feeding‐schedule on day 5 and 12 mothers will receive a phone call to motivate them to continue exposing their infant to vegetables. When the children are 8, 13 and 16 months of age, mothers will receive a booster phone call to reinforce daily vegetable intake. Intervention B: receives an intervention on how to feed their infant, in addition to a 15‐day feeding schedule consisting of mostly fruit. The intervention mothers receive purely focuses on the promotion of responsive feeding practices. The intervention mothers will receive the Video‐feedback Intervention to promote Positive Parenting ‐Feeding Infants (VIPP‐FI) and will be delivered during home visits. VIPP‐FI focuses on improving responsive feeding and sensitive ways of dealing with unwilling infants during the feeding process. Mothers are shown videotapes of their own feeding‐interaction with their infant, and receive feedback on these tapes by a trained intervener. Intervention C: will receive a combination of Intervention A and Intervention B. Mothers will be asked to feed the infant according to the schedule for the vegetable‐exposure intervention and will also receive feedback on how they should go about feeding their infant according to the VIPP‐FI intervention. Attention‐Control Condition D: receive the same feeding schedule as Intervention B and receive phone calls at the same time‐points as the intervention groups in which they will not receive any specific advice, but will be asked about topics such as the general development of the child. If mothers have questions about weaning or feeding, they are referred to “Het Voedingscentrum” or their infant welfare centre. |
| Outcomes | Infants' and toddlers' vegetable consumption |
| Starting date | The trial started in April 2016 |
| Contact information | Judi Mesman: [email protected] |
| Notes | NTR6572 and NCT03348176 |
| Trial name or title | Farm Fresh Foods for Healthy Kids (F3HK) |
| Methods | The Farm Fresh Foods for Healthy Kids community‐based, randomised intervention trial will build on formative and longitudinal research to examine the impact of cost‐offset community supported agriculture on diet and other health behaviours as well as the economic impacts on local economies. In each program, families will be recruited to join existing community supported agriculture programs in New York, North Carolina, Vermont, and Washington, and families will be randomised 1:1 to intervention or delayed intervention groups. Data will be collected at baseline, and in the fall and spring for 3 years. |
| Participants | Low‐income families with at least 1 child aged 2‐12 years. Target is 240 families (120 per arm) |
| Interventions | The intervention will involve reduced‐price community supported agriculture shares, which can be paid for on a weekly basis, nine skill‐based and seasonally tailored healthy eating classes, and the provision of basic kitchen tools. |
| Outcomes | Children’s intake of fruits and vegetables |
| Starting date | Unknown |
| Contact information | |
| Notes | NCT02770196 |
| Trial name or title | Play and grow |
| Methods | Randomised controlled trial |
| Participants | Approximately 240 families with children aged 2‐4 years |
| Interventions | Intervention: “Play & Grow is a 10‐week family‐based, multi‐component healthy lifestyle programme” "The Play & Grow will have educational strategies including instructions, parental peer support and group discussions, and homework tasks, in accordance with the elements developed in our Play & Grow pilot study. Each session will comprise: (i) 15 min of guided active play involving both children and parents; (ii) 15 min of interactive education and skill development for parents; simultaneous supervised active play with foods for children, to promote acceptance of vegetables, and (iii) 15 min of guided active nature games outdoors, involving both children and parents. The sessions will incorporate a lifestyle component, for example: eating, active play and connectedness to nature). These will target the parents’ knowledge and skills on how to introduce and maintain their child’s correct lifestyle routines. A group leader and co‐leader with healthcare backgrounds (and trained by the PI during the Play & Grow pilot study) will facilitate the sessions involving 4 to 5 parent‐child dyads. The proposed intervention, we will employ environmental education and nature‐related activities to help participating families develop skills conducive to improving playtime and eating habits in children." Control: “The (waiting list or control group) WLCG children will be offered the Play & Grow programme at study completion” |
| Outcomes | Child fruit and vegetable intake will be assessed using the Eating and Physical Activity Questionnaire (EPAQ) and The Children’s Eating Behaviour Questionnaire (CEBQ) |
| Starting date | Unknown |
| Contact information | Tanja Sobko: [email protected] |
| Notes |
| Trial name or title | Choosing Healthy Eating when Really Young (CHERRY) |
| Methods | Randomised controlled trial |
| Participants | Approximately 288 parents of children aged 18 months to 5 years from children's centres |
| Interventions | Intervention: “The intervention group participants attended four sessions (one each week) over 4 weeks. Each session lasted 2 h. The first hour of each session involved parents discussing and learning about a variety of aspects of healthy eating while the children attended a free crèche in the adjacent room (the crèche activities were not considered part of CHERRY and were not monitored). The second hour involved parents. and children together for a more practical, ‘hands on’ cook and eat session involving basic food preparation and tasting. Each session began with a recap from the previous week and finished with parents being given a ‘CHERRY at home’ activity to complete before the following week’s session; these were both designed to consolidate parents’ learning. The intervention group also received SMS reminders via mobile phones between sessions; SMSs included the main messages of the CHERRY programme, as well as reminders to attend each session. The intervention comprised not only individually focused nutrition support, but also encompassed activities directed at developing the capacity of the children’s centre to promote and maintain healthy nutritional practices. In the intervention centres, a staff training session was offered to all staff working in the centres. The training session covered various aspects of healthy eating and nutrition for early years and included an introduction and overview of the CHERRY programme. Each training session was tailored to the needs of the staff, as identified by heads of each intervention centre. Intervention centres were also given support and advice to revise and develop their centre’s food policies in order to support healthy eating practices and procedures.” Control: “The children’s centres randomised to the control group did not receive any of the components of the CHERRY programme. During the study period, the control centres agreed not to implement any new nutritional interventions but continued with existing support. On final completion of the study, the CHERRY resources were disseminated to control centres and other early years settings interested in nutrition.” |
| Outcomes | "Child’s fruit and vegetable consumption at home (portions per day). This was defined as the total weight (grams) of fruit and vegetables consumed the number of different types of fruit and vegetables consumed, and the actual types of fruit and vegetables consumed. The child’s diet was assessed using the multiple‐pass 24‐h recall method. As the children concerned were under 5 years of age, the parents completed the interviews on their behalf.” |
| Starting date | Parents were recruited into the study over 5 recruitment waves between September 2010 and November 2011 |
| Contact information | Richard Geddie Watt: [email protected] |
| Notes |
| Trial name or title | Keys to Healthy Family Child Care Homes (KEYS) |
| Methods | Cluster‐randomised controlled trial |
| Participants | Approximately 450 children aged 18 months to 4 years from 150 Family Child Care Homes |
| Interventions | Intervention: “The Keys intervention is delivered over nine months, spending approximately three months on each of three modules. These modules are designed to help providers (1). Modify their own weight‐related behaviors so that they can become role models for children (Module 1: Healthy You), (2) create environments that encourage and support children’s physical activity and healthy eating habits (Module 2: Healthy Home), and (3) adopt sound business practices that will help them sustain the changes introduced (Module 3: Healthy Business). "The intervention is delivered through workshops, home visits, tailored coaching calls, and educational toolkits." Control: “Participants in the control arm receive the Healthy Business" only |
| Outcomes | Child intake collected using direct observation at the Family Child Care Homes |
| Starting date | Unknown |
| Contact information | Courtney Mann: [email protected] |
| Notes |
LGA: Local Government Area
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vegetable intake Show forest plot | 13 | 1741 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| Analysis 1.1  Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 1 Vegetable intake. | ||||
| 2 Vegetable intake ‐ sensitivity analysis ‐ risk of bias Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| Analysis 1.2  Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 2 Vegetable intake ‐ sensitivity analysis ‐ risk of bias. | ||||
| 2.1 Low/unclear risk of bias | 5 | 487 | Std. Mean Difference (Random, 95% CI) | 0.23 [0.03, 0.44] |
| 2.2 High risk of bias | 8 | 1183 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.06, 0.68] |
| 3 Vegetable intake ‐ sensitivity analysis ‐ primary outcome Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| Analysis 1.3  Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 3 Vegetable intake ‐ sensitivity analysis ‐ primary outcome. | ||||
| 3.1 Primary outcome of child fruit or vegetable intake | 10 | 1331 | Std. Mean Difference (Random, 95% CI) | 0.45 [0.19, 0.70] |
| 3.2 Primary outcome unclear | 3 | 339 | Std. Mean Difference (Random, 95% CI) | 0.03 [‐0.19, 0.24] |
| 4 Vegetable intake ‐ sensitivity analysis ‐ missing data Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| Analysis 1.4  Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 4 Vegetable intake ‐ sensitivity analysis ‐ missing data. | ||||
| 4.1 Low attrition or high attrition with ITT analysis | 8 | 757 | Std. Mean Difference (Random, 95% CI) | 0.29 [0.10, 0.48] |
| 4.2 High attrition and no ITT analysis | 5 | 913 | Std. Mean Difference (Random, 95% CI) | 0.35 [‐0.10, 0.79] |
| 5 Vegetable intake ‐ subgroup analysis ‐ modality Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| Analysis 1.5 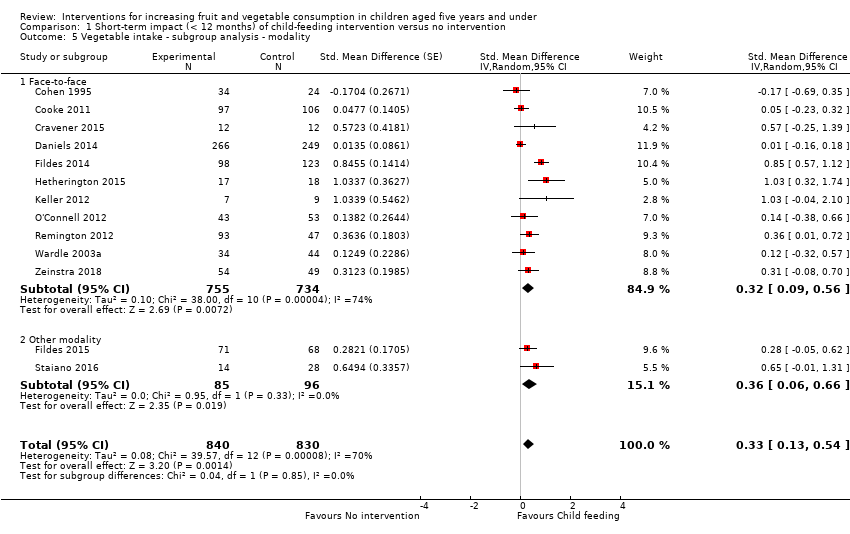 Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 5 Vegetable intake ‐ subgroup analysis ‐ modality. | ||||
| 5.1 Face‐to‐face | 11 | 1489 | Std. Mean Difference (Random, 95% CI) | 0.32 [0.09, 0.56] |
| 5.2 Other modality | 2 | 181 | Std. Mean Difference (Random, 95% CI) | 0.36 [0.06, 0.66] |
| 6 Vegetable intake ‐ subgroup analysis ‐ setting Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| Analysis 1.6  Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 6 Vegetable intake ‐ subgroup analysis ‐ setting. | ||||
| 6.1 School or preschool | 4 | 444 | Std. Mean Difference (Random, 95% CI) | 0.19 [‐0.02, 0.40] |
| 6.2 Home | 4 | 474 | Std. Mean Difference (Random, 95% CI) | 0.56 [0.18, 0.95] |
| 6.3 Home + Lab | 2 | 40 | Std. Mean Difference (Random, 95% CI) | 0.74 [0.09, 1.39] |
| 6.4 Other settings | 3 | 712 | Std. Mean Difference (Random, 95% CI) | 0.06 [‐0.14, 0.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fruit and vegetable intake Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| Analysis 2.1  Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 1 Fruit and vegetable intake. | ||||
| 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| Analysis 2.2  Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome. | ||||
| 2.1 Primary outcome of child fruit or vegetable intake | 8 | 2792 | Std. Mean Difference (Random, 95% CI) | 0.04 [‐0.08, 0.16] |
| 2.2 Primary outcome unclear | 3 | 286 | Std. Mean Difference (Random, 95% CI) | 0.52 [0.03, 1.00] |
| 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| Analysis 2.3 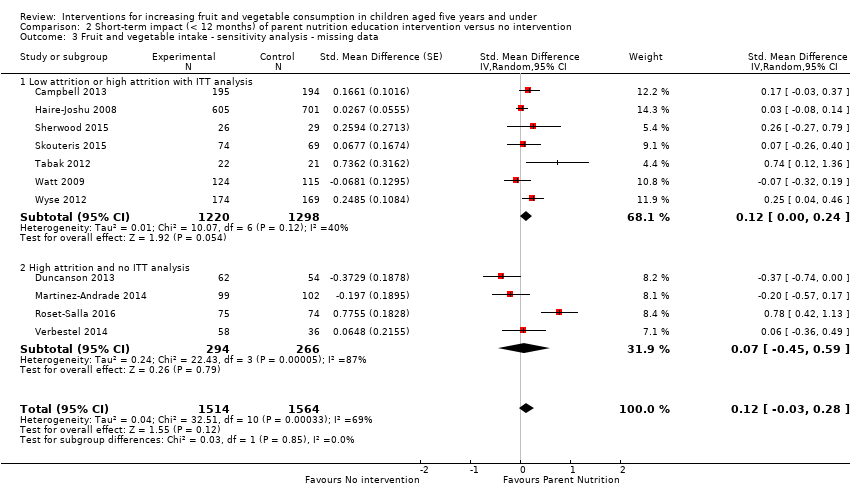 Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data. | ||||
| 3.1 Low attrition or high attrition with ITT analysis | 7 | 2518 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.00, 0.24] |
| 3.2 High attrition and no ITT analysis | 4 | 560 | Std. Mean Difference (Random, 95% CI) | 0.07 [‐0.45, 0.59] |
| 4 Fruit and vegetable intake ‐ subgroup analysis ‐ modality Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| Analysis 2.4  Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 4 Fruit and vegetable intake ‐ subgroup analysis ‐ modality. | ||||
| 4.1 Face‐to‐face only | 5 | 826 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.20, 0.45] |
| 4.2 Audio visual only | 2 | 386 | Std. Mean Difference (Random, 95% CI) | 0.40 [‐0.04, 0.85] |
| 4.3 Other modality | 4 | 1866 | Std. Mean Difference (Random, 95% CI) | 0.03 [‐0.16, 0.21] |
| 5 Fruit and vegetable intake ‐ subgroup analysis ‐ setting Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| Analysis 2.5  Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 5 Fruit and vegetable intake ‐ subgroup analysis ‐ setting. | ||||
| 5.1 Home | 5 | 2047 | Std. Mean Difference (Random, 95% CI) | 0.06 [‐0.16, 0.27] |
| 5.2 Preschool | 2 | 243 | Std. Mean Difference (Random, 95% CI) | 0.43 [‐0.27, 1.13] |
| 5.3 Other settings | 4 | 788 | Std. Mean Difference (Random, 95% CI) | 0.09 [‐0.07, 0.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fruit and vegetable intake Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| Analysis 3.1  Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 1 Fruit and vegetable intake. | ||||
| 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| Analysis 3.2  Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome. | ||||
| 2.1 Primary outcome of child fruit or vegetable intake | 4 | 1315 | Std. Mean Difference (Random, 95% CI) | 0.44 [‐0.00, 0.87] |
| 2.2 Primary outcome unclear | 1 | 694 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.13, 0.38] |
| 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| Analysis 3.3  Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data. | ||||
| 3.1 Low attrition or high attrition with ITT analysis | 3 | 413 | Std. Mean Difference (Random, 95% CI) | 0.65 [0.43, 0.88] |
| 3.2 High attrition and no ITT analysis | 2 | 1596 | Std. Mean Difference (Random, 95% CI) | 0.06 [‐0.08, 0.20] |
| 4 Fruit and vegetable intake ‐ subgroup analysis ‐ setting Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| Analysis 3.4  Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 4 Fruit and vegetable intake ‐ subgroup analysis ‐ setting. | ||||
| 4.1 School or preschool | 3 | 1608 | Std. Mean Difference (Random, 95% CI) | 0.07 [‐0.07, 0.20] |
| 4.2 Other settings | 2 | 401 | Std. Mean Difference (Random, 95% CI) | 0.66 [0.43, 0.89] |

Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Funnel plot of comparison 1. Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention on child consumption of target fruit or vegetable, outcome 1.1, fruit and/or vegetable intake

Funnel plot of comparison 3. Short‐term impact (< 12 months) of parent nutrition education intervention versus usual care, outcome 3.1, fruit and/or vegetable intake

Funnel plot of comparison 4. Short‐term impact (< 12 months) of multicomponent intervention versus usual care, outcome 4.1, fruit and/or vegetable intake

Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 1 Vegetable intake.

Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 2 Vegetable intake ‐ sensitivity analysis ‐ risk of bias.

Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 3 Vegetable intake ‐ sensitivity analysis ‐ primary outcome.

Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 4 Vegetable intake ‐ sensitivity analysis ‐ missing data.

Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 5 Vegetable intake ‐ subgroup analysis ‐ modality.

Comparison 1 Short‐term impact (< 12 months) of child‐feeding intervention versus no intervention, Outcome 6 Vegetable intake ‐ subgroup analysis ‐ setting.

Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 1 Fruit and vegetable intake.

Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome.

Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data.

Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 4 Fruit and vegetable intake ‐ subgroup analysis ‐ modality.

Comparison 2 Short‐term impact (< 12 months) of parent nutrition education intervention versus no intervention, Outcome 5 Fruit and vegetable intake ‐ subgroup analysis ‐ setting.
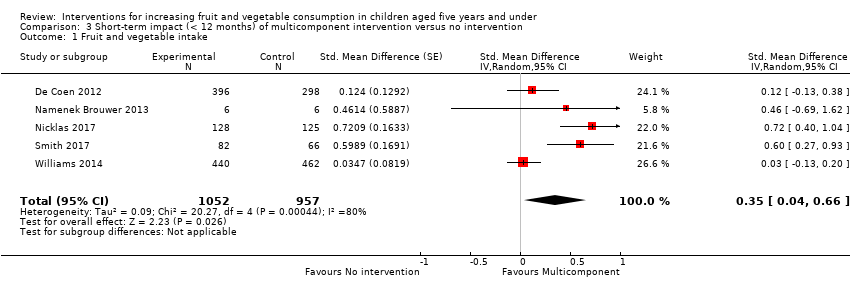
Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 1 Fruit and vegetable intake.

Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome.

Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data.

Comparison 3 Short‐term impact (< 12 months) of multicomponent intervention versus no intervention, Outcome 4 Fruit and vegetable intake ‐ subgroup analysis ‐ setting.
| Child feeding interventions compared to no intervention for children aged five years and under | ||||||
| Patient or population: children aged five years and under | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with child‐feeding interventions | |||||
| Short‐term impact (< 12 months) child vegetable intake | The mean as‐desired vegetable intake was 7.7 grams1 | The mean as‐desired vegetable intake (grams) in the intervention group was 3.50 higher (1.38 higher to 5.73 higher) | ‐ | 1741 | ⊕⊝⊝⊝ | Scores estimated using a standardised mean difference of 0.33 (0.13 to 0.54) and a standard deviation of 10.61.1 The mean duration of follow‐up post‐intervention for studies included in the meta‐analysis was 6.2 weeks. Harnack 2012 compared ≥ 1 child‐feeding practice interventions to a no‐treatment control and reported a significant increase in intake of fruit but could not be synthesised in meta‐analysis. |
| Short‐term impact (< 12 months) cost effectiveness ‐ not reported | No child‐feeding interventions reported this outcome | ‐ | ‐ | ‐ | ‐ | |
| Short‐term impact (< 12 months) unintended adverse events | One trial (Spill 2011a) reported no adverse effects on amount of meals consumed | ‐ | 39 | ⊕⊝⊝⊝ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1We used the post‐intervention mean and standard deviation of the control group from Wardle 2003a for the risk with no intervention and to re‐express the SMD in terms of grams of intake. | ||||||
| Parent nutrition education interventions compared to no intervention for children aged 5 years and under | ||||||
| Patient or population: children aged 5 years and under | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with parent nutrition education interventions | |||||
| Short‐term impact (< 12 months) child fruit and vegetable intake | The mean servings of vegetables per day was 1.61 | The mean servings of vegetables per day in the intervention group was 0.12 higher (0.03 lower to 0.28 higher) | ‐ | 3078 | ⊕⊝⊝⊝ | Scores estimated using a standardised mean difference of 0.12 (‐0.03 to 0.28) and a standard deviation of 1.01 The mean duration of follow‐up post‐intervention for studies included in the meta‐analysis was 8.8 weeks. We were unable to pool results of three trials that reported mixed results in the meta‐analysis. One study found a parent‐responsivity and behaviour‐management intervention to be effective in increasing total fruit intake compared to control (Black 2011); one study found a parent health report on fruit and vegetable consumption to be effective in increasing total vegetable intake compared to control, but not fruit (Hunsaker 2017); and the other study found both a parent‐complementary feeding intervention and a parent‐complementary feeding and home‐visit intervention to be effective in increasing both fruit and vegetable intake compared to control (Vazir 2013). |
| Short‐term impact (< 12 months) cost effectiveness | Information regarding intervention costs was reported in 1 trial (Campbell 2013) | ‐ | 389 | ⊕⊝⊝⊝ | ‐ | |
| Short‐term impact (< 12 months) unintended adverse events | One trial (Wyse 2012) reported no adverse effect on family food expenditure | ‐ | 343 | ⊕⊝⊝⊝ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1We used the post‐intervention mean and standard deviation of the control group from Skouteris 2015 for the risk with no intervention and to re‐express the SMD in terms of servings of vegetables per day. | ||||||
| Multicomponent interventions compared to no intervention for children aged 5 years and under | ||||||
| Patient or population: children aged 5 years and under | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with multicomponent interventions | |||||
| Short‐term impact (< 12 months) child fruit and vegetable intake | The mean cups of vegetables per day was 1.081 | The mean cups of vegetables per day in the intervention group was 0.37 higher (0.04 higher to 0.69 higher) | ‐ | 2009 | ⊕⊕⊝⊝ | Scores estimated using a standardised mean difference of 0.35 (0.04 to 0.66) and a standard deviation of 1.051 The mean duration of follow‐up post‐intervention for studies included in the meta‐analysis was 1.1 weeks 4 studies could not be pooled in meta‐analysis. 3 reported significant increases in both fruit and vegetable consumption, and 1 significantly increased fruit but not vegetable consumption |
| Short‐term impact (< 12 months) cost effectiveness ‐ not reported | No studies reported this outcome | ‐ | ‐ | ‐ | ‐ | |
| Short‐term impact (< 12 months) unintended adverse events ‐ not reported | No studies reported this outcome | ‐ | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1We used the post‐intervention mean and standard deviation of the control group from Williams 2014 for the risk with no intervention and to re‐express the SMD in terms of cups vegetables per day. | ||||||
| Child nutrition education interventions compared to no intervention for children aged 5 years and under | ||||||
| Patient or population: children aged 5 years and under | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with child nutrition education interventions | |||||
| Short‐term impact (< 12 months) child fruit and vegetable intake | The mean short‐term impact (< 12 months) child vegetable intake frequency score was 4 (a score of 4 corresponds to consumption of vegetables 3 ‐ 4 times per week) | MD 0 | ‐ | 238 | ⊕⊕⊝⊝ | The only study (Baskale 2011) reported an increase in some of the fruits and vegetables assessed in the intervention group and no significant differences in the control group The duration of follow‐up post‐intervention was 8 weeks |
| Cost or cost effectiveness ‐ not reported | No studies reported this outcome | ‐ | ‐ | ‐ | ‐ | |
| Unintended adverse events ‐ not reported | No studies reported this outcome | ‐ | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded one level for risk of bias: high risk of bias due to lack of blinding and loss to follow‐up. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Vegetable intake Show forest plot | 13 | 1741 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| 2 Vegetable intake ‐ sensitivity analysis ‐ risk of bias Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| 2.1 Low/unclear risk of bias | 5 | 487 | Std. Mean Difference (Random, 95% CI) | 0.23 [0.03, 0.44] |
| 2.2 High risk of bias | 8 | 1183 | Std. Mean Difference (Random, 95% CI) | 0.37 [0.06, 0.68] |
| 3 Vegetable intake ‐ sensitivity analysis ‐ primary outcome Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| 3.1 Primary outcome of child fruit or vegetable intake | 10 | 1331 | Std. Mean Difference (Random, 95% CI) | 0.45 [0.19, 0.70] |
| 3.2 Primary outcome unclear | 3 | 339 | Std. Mean Difference (Random, 95% CI) | 0.03 [‐0.19, 0.24] |
| 4 Vegetable intake ‐ sensitivity analysis ‐ missing data Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| 4.1 Low attrition or high attrition with ITT analysis | 8 | 757 | Std. Mean Difference (Random, 95% CI) | 0.29 [0.10, 0.48] |
| 4.2 High attrition and no ITT analysis | 5 | 913 | Std. Mean Difference (Random, 95% CI) | 0.35 [‐0.10, 0.79] |
| 5 Vegetable intake ‐ subgroup analysis ‐ modality Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| 5.1 Face‐to‐face | 11 | 1489 | Std. Mean Difference (Random, 95% CI) | 0.32 [0.09, 0.56] |
| 5.2 Other modality | 2 | 181 | Std. Mean Difference (Random, 95% CI) | 0.36 [0.06, 0.66] |
| 6 Vegetable intake ‐ subgroup analysis ‐ setting Show forest plot | 13 | 1670 | Std. Mean Difference (Random, 95% CI) | 0.33 [0.13, 0.54] |
| 6.1 School or preschool | 4 | 444 | Std. Mean Difference (Random, 95% CI) | 0.19 [‐0.02, 0.40] |
| 6.2 Home | 4 | 474 | Std. Mean Difference (Random, 95% CI) | 0.56 [0.18, 0.95] |
| 6.3 Home + Lab | 2 | 40 | Std. Mean Difference (Random, 95% CI) | 0.74 [0.09, 1.39] |
| 6.4 Other settings | 3 | 712 | Std. Mean Difference (Random, 95% CI) | 0.06 [‐0.14, 0.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fruit and vegetable intake Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| 2.1 Primary outcome of child fruit or vegetable intake | 8 | 2792 | Std. Mean Difference (Random, 95% CI) | 0.04 [‐0.08, 0.16] |
| 2.2 Primary outcome unclear | 3 | 286 | Std. Mean Difference (Random, 95% CI) | 0.52 [0.03, 1.00] |
| 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| 3.1 Low attrition or high attrition with ITT analysis | 7 | 2518 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.00, 0.24] |
| 3.2 High attrition and no ITT analysis | 4 | 560 | Std. Mean Difference (Random, 95% CI) | 0.07 [‐0.45, 0.59] |
| 4 Fruit and vegetable intake ‐ subgroup analysis ‐ modality Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| 4.1 Face‐to‐face only | 5 | 826 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.20, 0.45] |
| 4.2 Audio visual only | 2 | 386 | Std. Mean Difference (Random, 95% CI) | 0.40 [‐0.04, 0.85] |
| 4.3 Other modality | 4 | 1866 | Std. Mean Difference (Random, 95% CI) | 0.03 [‐0.16, 0.21] |
| 5 Fruit and vegetable intake ‐ subgroup analysis ‐ setting Show forest plot | 11 | 3078 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.03, 0.28] |
| 5.1 Home | 5 | 2047 | Std. Mean Difference (Random, 95% CI) | 0.06 [‐0.16, 0.27] |
| 5.2 Preschool | 2 | 243 | Std. Mean Difference (Random, 95% CI) | 0.43 [‐0.27, 1.13] |
| 5.3 Other settings | 4 | 788 | Std. Mean Difference (Random, 95% CI) | 0.09 [‐0.07, 0.25] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Fruit and vegetable intake Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| 2 Fruit and vegetable intake ‐ sensitivity analysis ‐ primary outcome Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| 2.1 Primary outcome of child fruit or vegetable intake | 4 | 1315 | Std. Mean Difference (Random, 95% CI) | 0.44 [‐0.00, 0.87] |
| 2.2 Primary outcome unclear | 1 | 694 | Std. Mean Difference (Random, 95% CI) | 0.12 [‐0.13, 0.38] |
| 3 Fruit and vegetable intake ‐ sensitivity analysis ‐ missing data Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| 3.1 Low attrition or high attrition with ITT analysis | 3 | 413 | Std. Mean Difference (Random, 95% CI) | 0.65 [0.43, 0.88] |
| 3.2 High attrition and no ITT analysis | 2 | 1596 | Std. Mean Difference (Random, 95% CI) | 0.06 [‐0.08, 0.20] |
| 4 Fruit and vegetable intake ‐ subgroup analysis ‐ setting Show forest plot | 5 | 2009 | Std. Mean Difference (Random, 95% CI) | 0.35 [0.04, 0.66] |
| 4.1 School or preschool | 3 | 1608 | Std. Mean Difference (Random, 95% CI) | 0.07 [‐0.07, 0.20] |
| 4.2 Other settings | 2 | 401 | Std. Mean Difference (Random, 95% CI) | 0.66 [0.43, 0.89] |

