Saline irrigation for the management of skin extravasation injury in neonates
Referencias
References to studies excluded from this review
Ir a:
Additional references
Ir a:
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Case series | |
| Case report | |
| Retrospective review of 31 cases | |
| Case report | |
| Retrospective review of 96 cases | |
| Retrospective review | |
| Case report | |
| Case report | |
| Case report | |
| Case report |
All 10 studies are either case reports or case series. Time to intervention from extravasation is highly variable. In all 10 studies, participants were neonates only. All 10 studies reported their outcomes as complete wound healing and no functional and cosmetic disability.
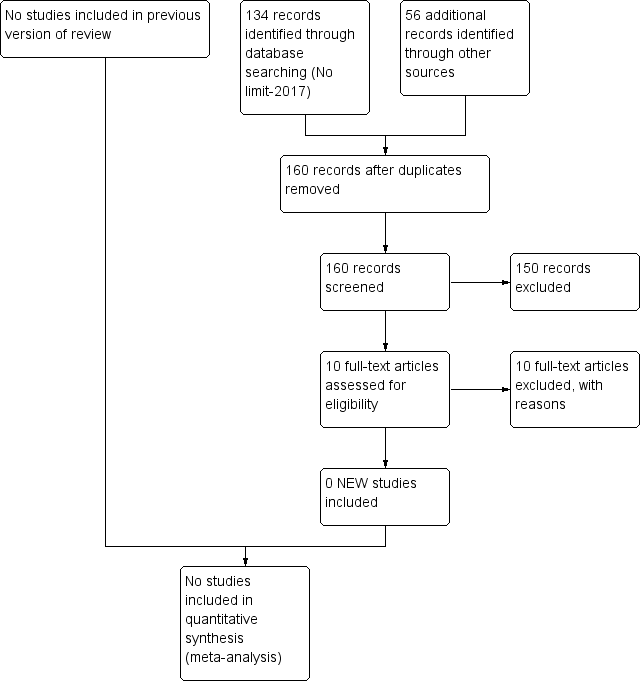
Study flow diagram: review update.
| Saline irrigation with or without prior infiltration of hyaluronidase vs standard wound care for management of extravasation injury in neonates | ||||||
| Patient or population: neonates requiring management of extravasation injury | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with standard wound care | Risk with saline irrigation with or without prior infiltration of hyaluronidase | |||||
| Complete wound healing after saline irrigation with or without prior hyaluronidase infiltration (wound healing): clinical assessment | Study population | Not estimable | 237 | ⊕⊝⊝⊝ | Pooled data for 237 neonates from 10 case report studies who underwent saline irrigation. Three neonates received further surgical intervention. For 234 neonates, complete wound healing was reported | |
| 0 per 1000 | 0 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| All 10 studies analysed in GRADE pro GDT are case reports, and the intervention methods mentioned are highly variable. In view of this, "relative effect (95% CI)" and "absolute effect (95% CI)" were not derived. | ||||||
| Study | Type of study | Number of neonates | Extravasation | Intervention | Outcome |
| Case series | 14 neonates | Dopamine ‐ 9 Caffeine ‐ 2 Calcium ‐ 2 Beta blocker ‐ 1 | Hyaluronidase infiltration and aspiration ‐ 12 Saline irrigation and aspiration ‐ 1 Hyaluronidase infiltration alone ‐ 1 | 3 cases developed skin necrosis but healed spontaneously | |
| Case report | 1 neonate | Total parenteral nutrition (TPN) | Infiltration with hyaluronidase with saline irrigation | Healing in 3 days | |
| Retrospective review of 31 cases | 31 neonates had 36 extravasations | TPN ‐ 13 Medications ‐ 10 Blood products ‐ 6 Crystalloids ‐ 5 Contrast ‐ 2 | Hyaluronidase infiltration and saline irrigation used for 24 extravasation injuries | No surgical graft required | |
| Case report | 2 preterm neonate less than 29 weeks gestation | TPN | Hyaluronidase infiltration and saline irrigation | Minimal or no scarring, no functional sequelae | |
| Retrospective review of 96 cases | Total 96 cases referred to a tertiary plastic surgical unit (age range ‐ preterm neonate to 72 years ‐ exact distribution not mentioned) 44 early referrals, i.e. within 24 hours 52 late referral, i.e. after 24 hours | TPN Inotrope Ca KCl Bicarbonate Dextrose: 10%‐20% Chemotherapeutics Contrast Antibiotics (exact numbers not mentioned) | Early referral group: 44 (saline irrigation alone ‐ 37, liposuction and saline irrigation ‐ 6, liposuction alone ‐ 1) Late referral group: wound and surgical management | Early referral group: 39 (88.5%) no soft tissue damage, 5 (11.5%) minor skin blistering Late referral group: 8 (15%) healed without tissue necrosis, 17 (33%) minor skin sloughing, 27 (52%) extensive damage to tissues ‐ 3 amputations | |
| Retrospective review | 56 neonates | TPN Inotrope Calcium Potassium chloride Sodium bicarbonate High concentration of dextrose (exact numbers not mentioned) | Saline irrigation alone | No skin loss. None required reconstructive surgery | |
| Case report | 34 neonates | TPN ‐ 28 10% dextrose ‐ 4 Second‐generation cephalosporin ‐ 2 | Saline irrigation followed by topical application of paraffin‐impregnated gauze and povidone‐iodine‐soaked gauze dressing | In 21 infants, no signs of soft tissue damage by 24 hours of treatment Minor findings still present for a few days in 7 patents after treatment Ischaemic signs present in 6 patients subsided within 25 days | |
| Case report | 1 neonate | Antibiotics | Infiltration with recombinant human hyaluronidase (rHuPH20) | Wound healed completely by 8 days | |
| Case report | 1 neonate | Dobutamine, adrenaline, 8.4% sodium bicarbonate, 10% calcium gluconate | Infiltration of hyaluronidase followed by liposuction and saline irrigation | No signs of soft tissue damage at 2 weeks | |
| Case report | 1 neonate | TPN | Hyaluronidase infiltration and saline irrigation | Healed fully by 5 days |
| Study | Stage of extravasation | Intervention | Outcome | Reason for exclusion |
| Skin necrosis (stage 3): n = 3 Swelling, oedema, discolouration (stage 1‐2): n = 11 | Hyaluronidase and aspiration ‐ 12 cases Hyaluronidase infiltration alone ‐ 1 Saline irrigation and aspiration ‐ 1 Treatment allocation not specified by stage of injury | No sequelae | Neither a randomised nor a quasi‐randomised study | |
| Swelling, erythema, and induration (stage 3): n = 1 | Hyaluronidase and saline irrigation | No sequelae | Neither a randomised nor a quasi‐randomised study | |
| Erythema and oedema (stage 1‐2): n = 12 Skin necrosis (stage 3): n = 24 | Stage 1‐2 ‐ standard wound management Stage 3 ‐ hyaluronidase and saline irrigation | No sequelae No sequelae | Neither a randomised nor a quasi‐randomised study | |
| Skin necrosis (stage 3): n = 2 | Hyaluronidase and saline irrigation | Minimal scarring, no sequelae | Neither a randomised nor a quasi‐randomised study | |
| Skin necrosis (stage 3): Early referral: n = 44 Delayed referral (stage 3‐4): n = 52 | Stage 3: Saline irrigation alone: n = 37 Liposuction and saline irrigation: n = 6 Liposuction alone: n = 1 Stage 3‐4: Wound debridement and surgical flap | No sequelae 8 (15%) healed without tissue necrosis, 17 (33%) minor skin sloughing, 27 (52%) extensive damage to tissues ‐ 3 amputations | Neither a randomised nor a quasi‐randomised study | |
| Exact stage of extravasation injury not specified: n = 56 | Saline irrigation | No sequelae | Neither a randomised nor a quasi‐randomised study | |
| Stage 3 and stage 4 extravasation | Saline irrigation within 30 minutes of extravasation injury | None of the wounds needed secondary skin coverage procedures | Neither a randomised nor a quasi‐randomised study | |
| Discolouration, oedema, cool, pulses not palpable (stage 4): n = 1 | Infiltration with recombinant human hyaluronidase (rHuPH20) | No sequelae | Neither a randomised nor a quasi‐randomised study | |
| Oedema, pallor, cold, and no capillary filling | Infiltration with hyaluronidase, liposuction, and saline irrigation | No sequelae | Neither a randomised nor a quasi‐randomised study | |
| Skin necrosis (stage 3): n = 1 | Hyaluronidase and saline irrigation | No sequelae | Neither a randomised nor a quasi‐randomised study |

