Cirugía de transección subpial para la epilepsia
Resumen
Antecedentes
Alrededor del 30% de los pacientes con epilepsia siguen teniendo crisis convulsivas a pesar de la administración de varios fármacos antiepilépticos (FAE). Se considera que estos pacientes presentan epilepsia refractaria o no controlada. Aunque no existe una definición universalmente aceptada de epilepsia no controlada o refractaria a los fármacos, para los objetivos de esta revisión se considerará que las convulsiones son resistentes a los fármacos si no han respondido a un mínimo de dos FAE. Los especialistas consideran que la intervención quirúrgica precoz puede prevenir las convulsiones a una edad más temprana, lo que a su vez puede mejorar la condición intelectual y social de los niños. Existen muchos tipos de cirugía para el tratamiento de la epilepsia refractaria; uno de esos procedimientos se conoce como transección subpial.
Objetivos
Evaluar los efectos de la transección subpial para las convulsiones de inicio focal y las convulsiones tónico‐clónicas generalizadas en niños y adultos.
Métodos de búsqueda
Para la última actualización se hicieron búsquedas en las siguientes bases de datos el 7 de agosto de 2018: el Registro Cochrane de Estudios (CRS Web), que incluye el Registro Especializado del Grupo Cochrane de Epilepsia (Cochrane Epilepsy Group) y el Registro Cochrane Central de Ensayos Controlados (CENTRAL), MEDLINE (Ovid, 1946 al 6 de agosto de 2018), ClinicalTrials.gov y la WHO International Clinical Trials Registry Platform(ICTRP). No se impuso restricciones de idioma.
Criterios de selección
Se consideraron todos los estudios aleatorizados y cuasialeatorizados de grupos paralelos, con o sin cegamiento.
Obtención y análisis de los datos
Dos autores de la revisión (BK y SR), de forma independiente, examinaron los ensayos identificados mediante la búsqueda. Los mismos dos autores de la revisión planificaron evaluar de forma independiente la calidad metodológica de los estudios. Si se hubieran identificado estudios para inclusión, un autor de la revisión habría extraído los datos y el otro los habría verificado.
Resultados principales
No se encontraron estudios relevantes.
Conclusiones de los autores
No se encontró evidencia que apoye o rechace el uso de la cirugía de transección subpial en pacientes con epilepsia refractaria a los fármacos. Se necesitan ensayos controlados aleatorizados bien diseñados para guiar la práctica clínica.
PICO
Resumen en términos sencillos
Cirugía de transección subpial para la epilepsia
Antecedentes
Casi el 30% de los pacientes con epilepsia siguen teniendo crisis convulsivas a pesar de la administración de varios fármacos antiepilépticos (FAE). Se considera que esos pacientes presentan epilepsia que no responde a los fármacos (refractaria) o no controlada, lo que afecta directamente a la función intelectual y a la condición social de los niños. También causa morbilidad y mortalidad considerables que afectan la calidad de vida del paciente. Algunos pacientes con epilepsia resistente al tratamiento se benefician con los tratamientos quirúrgicos.
La transección subpial múltiple (TSM) es una técnica quirúrgica en la cual se cortan parcialmente las conexiones del foco epiléptico sin resección del mismo. La MST es un tipo de cirugía que se puede realizar a los pacientes con epilepsia que no responde a los fármacos, en los que no se puede resecar la zona epileptogénica debido al alto riesgo de déficit neurológico.
Objetivo de la revisión
En esta revisión, se planificó evaluar los efectos beneficiosos y los efectos adversos de la transección subpial múltiple en pacientes con epilepsia resistente al tratamiento.
Resultados
No se encontraron ensayos controlados aleatorizados que compararan la transección subpial con el tratamiento con fármacos antiepilépticos u otro tipo de cirugía de la epilepsia.
Conclusiones
No hay evidencia suficiente para determinar si la transección subpial es eficaz o segura; se necesitan estudios adicionales. La evidencia está actualizada hasta agosto de 2018.
Authors' conclusions
Background
Description of the condition
Epilepsy is a neurological condition with an estimated incidence of 50 per 100,000 people overall, and a prevalence of 5 to 10 per 1000 in the developed world (Sander 1996). Nearly 70% of people with epilepsy have a good prognosis, and their seizures can be well controlled with antiepileptic drugs (AEDs). Up to 30% of patients with epilepsy will continue to have seizures despite using several antiepileptic drug regimens (Walker 1997). Most of the healthcare costs of epilepsy are due to medically refractory seizures (Murray 1994). While there is no universally accepted definition of medically refractory epilepsy (French 2006), for the purposes of this review we will consider seizures to be drug‐resistant if patients have failed to respond to a minimum of two AEDs that are appropriate to their type of epilepsy and given in adequate doses as monotherapy or in combination.
Description of the intervention
Despite using newer AEDs, many people with epilepsy do not achieve seizure freedom, and some could benefit from surgery. In the early years, epilepsy surgery focused on removal of gross structural lesions of the brain. With the addition of electroencephalography (EEG) data from preoperative and intraoperative recordings, areas of removal were expanded to include tissue that was grossly normal in appearance but was known to give rise to epileptiform activity. Partial lobectomies and more extensive cortical resection soon took the place of small areas of resection. Surgical procedures performed for epilepsy can be resective or non‐resective. Resection techniques generally yield the best surgical results, and they include lesionectomy (removal of the abnormal area of the brain), lobectomy (removal of diseased lobe), hemispherectomy (removal of diseased hemisphere) and corticectomy (removal of the cortex of the cerebrum). Non‐resective techniques comprise callosotomy (division of the corpus callosum), subpial transection (a series of shallow cuts into the brain's cerebral cortex), and vagus nerve and deep brain stimulation (Tellez‐Zenteno 2005). Temporal lobe resection is the surgical procedure most commonly performed in adults with refractory epilepsy, and extratemporal cortical resection, hemispherectomy, corpus callosotomy and temporal resection are performed for refractory childhood epilepsy.
Multiple subpial transection (MST) is a novel technique that was conceived and first described by Dogali 1993, Morrell 1989 and Shimizu 1991; this approach is useful in patients for whom the epileptogenic lesion cannot be resected because it lies in an eloquent cortical area, or in regions where excision may produce major deficits. The surgical technique consists of severing horizontal intracortical fibres at intervals of 5 mm, while preserving both vertical fibres and penetrating blood vessels. This results in reduction of synchronised discharge from the epileptic focus and limitation of its spread, without jeopardised function of the cerebral cortex. The procedure may control seizures without producing major postoperative neurological deficits. Brain resection may be performed in addition to MST in some patients. Hence, if epileptiform activity involves vital cortical areas or an inoperable site, subpial transection may be a preferred option in patients with medically refractory epilepsy.
How the intervention might work
Subpial transection may prevent the spread of epileptic discharges without altering the normal function of the cortex, thus preventing seizures. Sometimes the area of seizure onset is one in which resection may produce neurological deficits; in these people, subpial transection may be beneficial. Specialists believe that early surgical intervention may prevent seizures at a younger age, which in turn may improve the intellectual and social status of children (Dlugos 2001). The minimum volume essential for sustaining synchronous spiking has been empirically determined to be 12.5 mm. Cortical islands greater than 5 mm can support paroxysmal discharge (Sawhney 1995). This is the reason why in subpial transection, multiple controlled lesions are placed 5 mm apart at the mid‐level of cortical gyri – to prevent the spread of epileptic discharges without altering the normal function of the cortex (Kaufmann 1996).
Risk for surgery‐related mortality may be present, although no clear data are available. Morbidity such as aphasia or dysphasia, limb paralysis or postoperative infection such as meningitis may also be present in some cases.
Why it is important to do this review
Despite using new AEDs, nearly 30% of people with epilepsy do not achieve seizure reduction or seizure freedom, affecting quality of life and increasing healthcare costs. As subpial transection is one of the surgeries performed for medically refractory epilepsy, an urgent need exists to precisely establish its efficacy and harm through a systematic review of randomised trials. Studies done previously (Orbach 2001; Sawhney 1995; Schramm 2002) have reported good postoperative outcomes after subpial transection; two‐year follow‐up has shown good results. Even in people with Landau Kleffner syndrome, subpial transection has resulted in improved communication skills among previously mute patients. This procedure is particularly useful for terminating prolonged medically refractory seizures and seizures involving eloquent areas of the cortex. It does not lead to postoperative deficits. A meta‐analysis of 211 patients undergoing multiple subpial transection (MST) at six centres (non‐randomised trials) found that 62% to 71% had greater than 95% seizure reduction (Spencer 2002). An analysis of individual patient data extracted from 34 non‐randomised studies reported a seizure freedom rate of 55.2% when MST is combined with resection and 23.9% when used alone; authors concluded that MST is a viable option for treating eloquent foci, provided that a careful risk‐benefit analysis is conducted (Rolston 2018).
Objectives
To assess the effects of subpial transection for focal‐onset seizures and generalised tonic‐clonic seizures in children and adults.
Methods
Criteria for considering studies for this review
Types of studies
-
Randomised or quasi‐randomised parallel‐group studies
-
Studies may be blinded or non‐blinded
Types of participants
Children or adults with refractory focal‐onset seizures (simple focal, complex focal or secondary generalised tonic‐clonic seizures) or generalised‐onset tonic‐clonic seizures (with or without other generalised seizure types).
Types of interventions
-
Subpial transection versus antiepileptic drug therapy (monotherapy or multi‐drug therapy)
-
Subpial transection versus another type of epilepsy surgery or vagal nerve stimulation
-
Subpial transection versus sham surgery
Types of outcome measures
-
Seizure outcomes at one year, two years and five years after surgery: free of disabling seizures, completely seizure‐free, improved, not improved
-
Time to achieve one‐ or two‐year seizure remission
-
Quality of life outcomes, assessed by generic and disease‐specific validated scales
-
Employment outcomes: postoperative unemployment, underemployment, employment
-
Activities of daily living and driving
-
Medication ‐ postsurgical requirement of antiepileptic medication: increased, decreased, stopped, monotherapy or polytherapy
-
Changes in cognitive function and behaviour following surgery (assessed by validated scales)
-
Mortality
-
Morbidity: infection, new neurological deficits and other surgical complications
Search methods for identification of studies
Electronic searches
We ran searches for the original review in April 2012 and subsequent searches in August 2013, June 2015 and January 2017. For the latest update we searched the following databases on 7 August 2018.
-
Cochrane Register of Studies (CRS Web), which includes the Cochrane Epilepsy Group Specialised Register and the Cochrane Central Register of Controlled Trials (CENTRAL), using the search strategy outlined in Appendix 1.
-
MEDLINE (Ovid; 1946 to August 06, 2018), using the search strategy outlined in Appendix 2.
-
ClinicalTrials.gov, using the search strategy outlined in Appendix 3.
-
WHO International Clinical Trials Registry Platform (ICTRP), using the search strategy outlined in Appendix 4.
We applied no language restrictions.
Data collection and analysis
Selection of studies
Two review authors (BK and SR) assessed trials yielded by the search strategy to determine eligibility. We compared results and resolved disagreements by discussion.
Data extraction and management
We could not extract the data in the present review, as no study met the inclusion criteria. We planned to conduct the data extraction process as follows.
Two review authors planned to extract data independently using a data extraction form, which we had previously piloted, and to compare results and resolve disagreements by discussion. In future updates of this review, we plan to obtain the following information for each trial that meets our inclusion criteria.
Methodological data
-
Method of randomisation
-
Method of concealment of randomisation
-
Stratification factors
-
Methods of blinding, if used
-
Description of withdrawals and losses to follow‐up
-
Duration of baseline period
-
Duration of follow‐up
Participant factors
-
Seizure type(s)
-
Age
-
Sex
-
Presence of neurological deficits/signs at baseline
-
Number of seizures or seizure frequency before randomisation
-
Duration of epilepsy
-
EEG results at baseline
-
Aetiology of epilepsy and imaging data
-
Number of antiepileptic drugs and dosages
-
Side on which surgery was performed
Treatment issues
-
Setting (neurosurgical or specialised epilepsy centre)
-
Country
-
Differences in technique, if any
Outcomes
-
Outcome data as listed above
Quality assessment
Had we identified any studies, we would have evaluated their methodological quality according to guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Data analysis
Our primary analysis would have been an intention‐to‐treat analysis of participants according to treatment allocation, regardless of the final treatment given.
We planned to use risk ratio (RRs) and 95% confidence intervals (CIs) for binary outcomes, and mean differences (MDs) and 95% CIs for continuous outcomes. We would have compared participant characteristics, methodological diversities, outcomes across trials and treatment regimens to assess clinical heterogeneity and to compare patient populations. We would have checked for statistical heterogeneity by using the I2 test for heterogeneity. We would have synthesised data by using a fixed‐effect or a random‐effects model as appropriate. We planned to carry out a sensitivity analysis by excluding the study with the largest or smallest effect, or by excluding studies of poor quality to test the robustness of the meta‐analysis.
We intended to describe data on neurological examinations, computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, EEG results and adverse effects. For psychological, cognitive and behavioural outcomes, we would have narratively summarised the results and, only if appropriate, combined the results in a meta‐analysis.
If we had identified sufficient studies, we would have undertaken a subgroup analysis according to seizure type, neuroimaging data and age groups (children younger than 17 years versus adults).
Results
Description of studies
In total, we identified 426 references through database searching. We considered none of them to be relevant, as no study met the inclusion criteria. See Figure 1 for further details.

Study flow diagram.
Risk of bias in included studies
We included no studies in the review.
Effects of interventions
No studies met the inclusion criteria.
Discussion
Summary of main results
Despite an exhaustive literature search, we were not able to find any study that fulfilled our inclusion criteria.
Overall completeness and applicability of evidence
No study met the inclusion criteria. Hence at present, no reliable evidence supports the efficacy of subpial transection surgery for epilepsy.
Quality of the evidence
No studies met the inclusion criteria.
Potential biases in the review process
Some unpublished trials may have been conducted, or some trials might not have been retrieved, despite our exhaustive search strategy.
Agreements and disagreements with other studies or reviews
A meta‐analysis of 211 participants undergoing multiple subpial transection (MST) at six centres (non‐randomised trials) found that 62% to 71% had greater than 95% seizure reduction. MST plus cortical resection did not improve outcomes further (Spencer 2002). However, the pooled proportion of long‐term seizure‐free participants after subpial transection (2 non‐randomised studies; 74 participants) was 16% (95% CI 8 to 24) (Orbach 2001; Schramm 2002; Tellez‐Zenteno 2005). Non‐randomised trials may overestimate the effects of treatments compared with randomised trials (Dasheiff 1994; Devinsky 2003; Kuzniecky 2007).
This review has highlighted our knowledge gap regarding the efficacy of subpial transection as a treatment modality for people with medically refractory epilepsy.
The Cochrane Epilepsy group has published a Cochrane Review of all types of surgery (including subpial transections) for epilepsy, incorporating non‐randomised as well as randomised controlled trials. Please refer to this review for more information (West 2015).
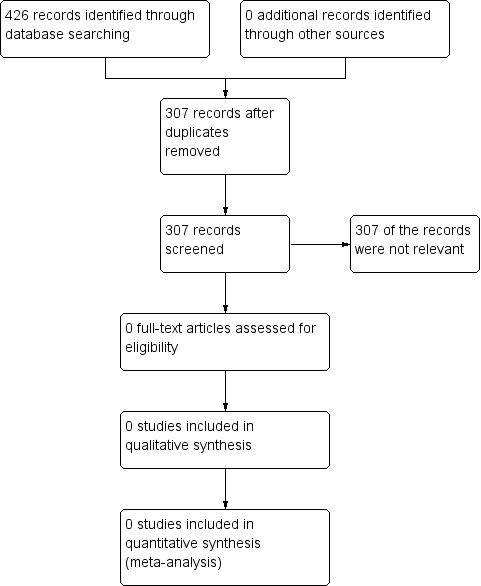
Study flow diagram.

