مقایسه درمان ترمیمی آتروماتیک در برابر درمانهای ترمیمی معمول برای مدیریت پوسیدگی دندان
چکیده
پیشینه
پوسیدگی دندان یک بیماری وابسته به قند است که به ساختار دندان آسیب میرساند و به دلیل از دست دادن اجزای معدنی ممکن است در نهایت منجر به کاویتاسیون یا حفرهزایی (cavitation) شود. پوسیدگی دندان شایعترین بیماری در سراسر جهان است و به عنوان مهمترین بار (burden) سلامت دهان در نظر گرفته شده است. روشهای متعارف درمان (سوراخ کردن و پر کردن) شامل استفاده از فرزهای چرخشی (rotary burs) تحت بیحسی موضعی است. نیاز به تامین برق، ابزارهای گرانقیمت و کارکنان سلامت بخش دندانپزشکی بسیار آموزش دیده ممکن است دسترسی به درمان دندانپزشکی را، به خصوص در مناطق توسعه نیافته محدود کند.
برای غلبه بر محدودیتهای درمان ترمیمی معمول (conventional restorative treatment)، درمان ترمیمی آتروماتیک (Atraumatic Restorative Treatment; ART) به طور عمده برای درمان پوسیدگی دندان در کودکان ساکن مناطق کمدرآمد دنیا که منابع و امکاناتی مانند برق و نیروی انسانی آموزش دیده در آنها محدود است، توسعه یافت. ART یک رویکرد تقریبا تهاجمی است که شامل حذف بافت پوسیده دندان با استفاده از ابزارهای دستی به تنهایی، و معمولا بدون استفاده از بیحسی و تجهیزات الکتریکی متحرک و ترمیم حفره دندان با مواد چسبنده (سمان گلاس اینومر (glass ionomer cement; GIC))، کامپوزیت رزینی، سمان گلاس اینومر رزینی اصلاح شده (resin‐modified glass‐ionomer cement; RM‐GIC) و کامپومرها (compomers) است.
اهداف
ارزیابی تاثیرات درمان ترمیمی آتروماتیک (ART) در مقایسه با درمان معمول برای مدیریت ضایعات پوسیده دندان در دندانهای شیری و دائمی کودکان و بزرگسالان.
روشهای جستوجو
متخصص اطلاعات گروه سلامت دهان در کاکرین بانکهای اطلاعاتی زیر را جستوجو کرد: پایگاه ثبت کارآزماییهای گروه سلامت دهان در کاکرین (تا 22 فوریه 2017)، پایگاه ثبت مرکزی کارآزماییهای کنترل شده کاکرین (CENTRAL)؛ کتابخانه کاکرین، شماره 1، 2017)؛ MEDLINE Ovid (از 1946 تا 22 فوریه 2017)؛ Embase Ovid (از 1980 تا 22 فوریه 2017)؛ LILACS BIREME Virtual Health Library (بانکهای اطلاعاتی علمی سلامت آمریکای لاتین و کارائیب؛ از 1982 تا 22 فوریه 2017)؛ و BBO BIREME Virtual Health Library (Bibliografia Brasileira de Odontologia؛ از 1986 تا 22 فوریه 2017). پایگاه ثبت کارآزماییهای موسسات ملی سلامت ایالات متحده (ClinicalTrail.gov) و پلتفرم بینالمللی پایگاه ثبت کارآزماییهای بالینی سازمان جهانی بهداشت برای شناسایی کارآزماییهای در حال انجام جستوجو شد. هنگام جستوجو در بانکهای اطلاعاتی الکترونیکی، هیچ محدودیتی از نظر زبان یا تاریخ انتشار اعمال نشد.
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترل شده (randomised controlled trials; RCTs) را با حداقل شش ماه پیگیری وارد کردیم که تاثیرات ART را با یک رویکرد ترمیمی معمول با استفاده از همان مواد یا مواد ترمیم کننده مختلف دندانپزشکی برای درمان ضایعات پوسیده دندان مقایسه کردند.
گردآوری و تجزیهوتحلیل دادهها
دو نویسنده مرور بهطور مستقل از هم نتایج جستوجو را غربالگری کردند، دادهها را از مطالعات وارد شده استخراج نموده و خطر سوگیری (bias) را در این مطالعات ارزیابی کردند. از روشهای استاندارد روششناسی مورد نظر کاکرین برای ارزیابی خطر سوگیری و سنتز دادهها استفاده کردیم. در جایی که تجمیع مناسب بود، با استفاده از مدل اثرات‐تصادفی، متاآنالیز (meta‐analysis) انجام دادیم. کیفیت شواهد را با استفاده از معیارهای درجهبندی توصیه، ارزیابی، توسعه و ارزشیابی (GRADE) ارزیابی کردیم.
نتایج اصلی
در مجموع 15 مطالعه واجد شرایط را با 3760 شرکتکننده تصادفیسازی شده برای این مرور وارد کردیم. سن شرکتکنندگان در این مطالعات بین 3 تا 101 سال بود که میانگین آنها 25.42 سال بود. %48 از شرکتکنندگان مرد بودند. تمام مطالعات وارد شده بین سالهای 2002 و 2016 منتشر شدند. دو مطالعه از 15 مطالعه اعلام کردند که حمایت مالی آنها از طرف شرکتهایی بود که مواد ترمیم کننده دندان تولید میکنند. پنج مطالعه منحصرا شامل مطالعات تصادفیسازی شده گروه موازی (randomised parallel‐group studies) بودند؛ شش مطالعه شامل مطالعات خوشهای‐تصادفیسازی شده گروه موازی (cluster‐randomised parallel‐group studies) بودند؛ و چهار مطالعه شامل مطالعات تصادفیسازی شدهای بودند که از طراحی اسپلیت دهان استفاده کردند. یازده مطالعه، تاثیرات ART را بر دندانهای شیری به تنهایی و چهار مطالعه تاثیرات آن را بر دندان دائمی بررسی کردند. دوره پیگیری مطالعات وارد شده از 6 ماه تا 36 ماه متغیر بود. تمام مطالعات را در معرض خطر بالای سوگیری قضاوت کردیم.
برای مقایسه اصلی ART در مقایسه با درمان متعارف با استفاده از ماده مشابه: تمام مطالعات به جز دو مطالعه، از گلاس اینومر با چسبندگی بالا (high‐viscosity glass ionomer; H‐GIC) به عنوان ماده ترمیمی استفاده کردند؛ یک مطالعه از مواد کامپوزیتی (composite material) استفاده کرد؛ و یک مطالعه از سمان گلاس اینومری رزینی اصلاح شده (resin‐modified glass ionomer cement; RM‐GIC) استفاده کرد.
در مقایسه با درمان معمول با استفاده از RM‐GIC؛ ART ممکن است خطر شکست ترمیم دندانهای اولیه را طی یک دوره پیگیری از 12 تا 24 ماه افزایش دهد (OR: 1.13؛ 95% CI؛ 1.60 تا 2.27؛ پنج مطالعه؛ 643 شرکتکننده تجزیهوتحلیل شدند؛ شواهد با کیفیت پائین). به دلیل نگرانیهای جدی در مورد خطر سوگیری عملکرد و ریزش نمونه (attrition bias)، اطمینان ما به تخمین اثرگذاری محدود است. در این مقایسه،ART ممکن است درد حین پروسیجر را در مقایسه با درمان معمول کاهش دهد (MD: ‐0.65؛ 95% CI؛ 1.38‐ تا 0.07؛ 40 شرکتکننده تجزیهوتحلیل شدند؛ شواهد با کیفیت پائین).
کیفیت مقایسه ART با درمان معمول با استفاده از کامپوزیت یا RM‐GIC، به علت غیر‐مستقیم بودن، عدم‐دقت و خطر بالای سوگیری عملکرد و ریزش نمونه به بسیار پائین کاهش یافت. با توجه به کیفیت بسیار پائین شواهد به دست آمده از مطالعات واحد، ما در مورد شکست ترمیم با ART در مقایسه با درمان معمول با استفاده از کامپوزیت طی یک دوره پیگیری 24 ماهه (OR: 1.11؛ 95% CI؛ 0.54 تا 2.29؛ یک مطالعه؛ 57 شرکتکننده) و ART با استفاده از RM‐GIC در دندانهای دائمی سالمندان مبتلا به آسیبهای ناشی از ضایعات پوسیده ریشه دندان طی یک دوره پیگیری شش ماهه (OR: 2.71؛ 95% CI؛ 0.94 تا 7.81؛ یک مطالعه؛ 64 شرکتکننده) نامطمئن بودیم.
هیچ مطالعهای حوادث جانبی یا هزینهها را گزارش نکرد.
نتیجهگیریهای نویسندگان
شواهد با کیفیت پائین نشان میدهند که ART با استفاده از H‐GIC ممکن است خطر شکست ترمیم بیشتری نسبت به درمان معمول آسیبهای ناشی از ضایعات پوسیده دندانهای شیری داشته باشد. تاثیرات ART با استفاده از کامپوزیت و RM‐GIC به دلیل کیفیت بسیار پائین شواهد نامطمئن هستند و ما نمیتوانیم بر این یافتهها متکی باشیم. بیشتر مطالعات، تاثیرات ART را بر دندانهای اولیه ارزیابی کردند.
RCTهای به خوبی طراحی شده مورد نیاز هستند تا شکست ترمیم را در نقاط زمانی مهم از لحاظ بالینی و همچنین پیامدهای گزارش شده را توسط شرکتکنندگان مانند درد و ناراحتی گزارش کنند. با توجه به تاثیرات مخدوششدگی بالقوه در استفاده از مواد مختلف دندانپزشکی، مجموعه شواهد قوی مربوط به تاثیرات ART در مقایسه با درمانهای معمول با استفاده از همان مواد ترمیم کننده ضروری است. ما چهار کارآزمایی در حال انجام را شناسایی کردیم که میتوانستند بینش بیشتری در این زمینه ارائه کنند.
PICO
خلاصه به زبان ساده
درمان ترمیمی آتروماتیک (ابزارهای دستی به تنهایی) در مقایسه با درمان معمول برای مدیریت پوسیدگی دندان
سوال مطالعه مروری
هدف از این مرور، ارزیابی تاثیرات یک رویکرد تقریبا تهاجمی، یعنی درمان ترمیمی آتروماتیک (Atraumatic Restorative Treatment; ART)، برای درمان پوسیدگی دندان در کودکان و بزرگسالان (دندانهای شیری و دائمی) است.
پیشینه
خرابی دندان (پوسیدگی دندان) به عنوان شایعترین بیماری جهانی شناخته شده است. روشهای متداول (سوراخ کردن و پر کردن) شامل استفاده از متههای الکتریکی برای برداشتن مناطق پوسیده شده دندان پیش از پر کردن است. مواد بیحسی موضعی (داروی مسکّن) به طور معمول برای پیشگیری از درد حین پروسیجر تزریق میشوند. درمانهای متعارف نیاز به پرسنل دندانپزشکی بخش سلامت بسیار مجرب، دسترسی به برق و ابزار مناسب دارند و گرانقیمت هستند. این عوامل ممکن است دسترسی به این خدمات را به ویژه در مناطق توسعه نیافته محدود کند.
درمان ترمیمی آتروماتیک (ART) یک رویکرد جایگزین برای مدیریت پوسیدگی دندان است که شامل حذف بافتهای پوسیده با استفاده از ابزارهای دستی به تنهایی است که معمولا بدون استفاده از بیحسی (تزریق داروی مسکّن) و تجهیزات الکتریکی انجام میشوند.
ویژگیهای مطالعه
این مرور، شواهد موجود را که تا 22 فوریه 2017 بهروز شده بودند، جستوجو کرد. ما 15 مطالعه مرتبط را یافتیم که شامل 3760 شرکتکننده با میانگین سنی 25 سال (از 3 تا 101 سال) بودند که 48% از آنها مرد بودند. دوره پیگیری در کارآزماییها از 6 تا 36 ماه متغیر بود. دو مورد از 15 مطالعه دریافت حمایت مالی را از شرکتهایی که مواد پر کننده دندان تولید میکردند، اعلام کردند. علاوه بر این، ما چهار مطالعه در حال انجام نیز یافتیم.
نتایج کلیدی
شواهد با کیفیت پائین وجود دارد که نشان میدهند دندانهای شیری که با روش ART با استفاده از سمان گلاس اینومر با چسبندگی بالا درمان میشوند، ممکن است بیشتر از افراد دریافت کننده درمان معمول با همان ماده، دچار شکست ترمیم شوند. در درمان دندانهای شیری، ART ممکن است تجربه درد را نسبت به درمان معمول کاهش دهد. کیفیت شواهد موجود برای ارزیابی تفاوت بین ART و درمانهای معمول با استفاده از سایر مواد ترمیم کننده یا در دندانهای دائمی بسیار پائین است، بنابراین ما نمیتوانیم در این زمینه نتیجهگیری کنیم. هیچ کدام از مطالعات وارد شده، عوارض جانبی منفی یا هزینهها را گزارش نکردند.
کیفیت شواهد
کیفیت شواهد موجود پائین تا بسیار پائین است. احتمال دارد پژوهشهای بیشتر و با کیفیت بالا بتوانند یافتههای ما را تغییر دهند. چهار مطالعه در حال انجام وجود دارد که ممکن است در آینده اطلاعات بیشتری ارائه دهند.
Authors' conclusions
Summary of findings
| Atraumatic restorative treatment (ART) using high‐viscosity glass ionomer cement (H‐GIC) compared with conventional restorative treatment using H‐GIC for dental caries | |||||
| Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using H‐GIC Comparison: conventional treatment using H‐GIC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment with H‐GIC | ART with H‐GIC | ||||
| Restoration failure (primary dentition) at 12 to 24 months | 471 per 1000 | 588 per 1000 | OR 1.60 | 643 participants/846 teeth | ⊕⊕⊝⊝ |
| Pain | Mean pain (primary teeth) was 1.38 (SD 1.21) | Mean pain (primary teeth) was 0.73 (SD 1.14) | MD 0.65 lower (1.38 lower to 0.07 higher) | 40 participants | ⊕⊕⊝⊝ |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1We downgraded the evidence by two levels because of very serious concerns regarding risk of bias: we judged all five studies as high risk of performance bias, three studies as high risk of attrition bias, and two studies as high risk of reporting bias. | |||||
| Atraumatic restorative treatment (ART) using composite resins compared with conventional restorative treatment using composite resins for dental caries | |||||
| Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using composite Comparison: conventional treatment using composite | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment | ART | ||||
| Restoration failure (primary dentition) | 362 per 1000 | 387 per 1000 | OR 1.11 | 57 participants/100 teeth | ⊕⊝⊝⊝ |
| Pain | ‐ | ‐ | ‐ | ‐ | Not measured |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1We downgraded the evidence by three levels: one level because it is a single study (indirectness) and two levels because of very serious concern regarding the risk of bias (high risk of performance bias and high risk of attrition bias). The result was also very imprecise. | |||||
| Atraumatic restorative treatment (ART) using resin‐modified glass ionomer cement (RM‐GIC) compared with conventional restorative treatment using RM‐GIC for dental caries | |||||
| Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using RM‐GIC Comparison: conventional treatment using RM‐GIC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment | ART | ||||
| Restoration failure (primary dentition) | ‐ | ‐ | ‐ | 0 studies | No studies included |
| Restoration failure (permanent teeth) | 75 per 1000 | 180 per 1000 | OR 2.71 | 64 participants/141 teeth | ⊕⊝⊝⊝ |
| Pain | ‐ | ‐ | ‐ | ‐ | Not measured |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1We downgraded the evidence by one level because it is a single study (indirectness), one level because of concern regarding high risk of performance bias, and one level because the result was imprecise. | |||||
Background
Description of the condition
Dental caries
Dental caries is a sugar‐dependent disease that damages tooth structure and may result in cavity formation in the hard tissues of the teeth (enamel, dentine and cementum) (Kidd 2005). Dental plaque is a biofilm formed on the tooth surface soon after tooth cleaning. It frequently contains caries‐producing bacteria such as Streptococcus mutans. Such micro‐organisms metabolise dietary sugars and produce acids on the tooth surfaces. The acid production could lead to the diffusion of calcium and phosphate ions and, consequently, demineralisation of enamel (Fejerskov 2004; Kidd 2004). If this process continues, loss of mineral components will eventually lead to cavitation.
Dental caries is the most prevalent disease worldwide (Marcenes 2013). Dental caries and its consequences are considered the most important burden of oral health. They are especially common in sociodemographically disadvantaged groups (Antoft 1999; Ekstrand 2007; Hannigan 2000; Martignon 2010; Petersen 2005; Schwendicke 2015; Sheiham 2010). It affects 60% to 90% of school‐aged children and up to 100% of adults in most countries (Petersen 2005).The resultant pain and discomfort can negatively affect people's quality of life. Furthermore, the management of this condition imposes huge financial burden on society and individuals (Leal 2012).
Description of the intervention
The treatment of dental caries lesions can be either by conventional drill and fill approach, using rotary instruments, or the atraumatic approach, using only hand instruments. Different restorative materials may be used for these two approaches.
Conventional treatments
Conventional methods involve the use of rotary burs, alone or in conjunction with metal hand instruments (Weerheijm 1999). Various dental restorative materials are used, ranging from metal‐based materials such as amalgam, the most popular dental restoration material, especially in the posterior teeth, to tooth‐coloured materials, such as resin composites.
The pain and discomfort associated with conventional cavity preparation methods have resulted in many patients being reluctant to seek dental treatment (Berggren 1984). Local anaesthesia is frequently needed to control the pain associated with cavity preparation. Factors potentially responsible for the discomfort and pain include: the sensitivity of vital dentine; the pressure on the tooth caused by mechanical stimulation of the tooth by rotary devices; bone‐conducted noise and vibration; the high‐pitched noise of the rotary device; and development of high temperatures at the cutting surface (thermal stimulation) (Banerjee 2000). In addition, an important limitation of conventional restorative methods is that they require an electricity supply, expensive handpieces and highly trained dental health personnel. This approach has been shown to have an increased risk of pulp exposure, postoperative pulpal symptoms and the weakening of the tooth as result of more invasive caries removal (Ricketts 2013). These factors limit the use of conventional restorative dentistry in many underdeveloped areas, where facilities and trained human resources are scarce.
Atraumatic treatments
To overcome the limitations of conventional restorative treatment, Atraumatic Restorative Treatment (ART) was developed around 1985, mainly for treating caries in children living in under‐served areas of the world where resources and facilities such as electricity and trained manpower are limited (Frencken 1996). ART is a minimally invasive approach, which involves removal of decayed tissue using hand instruments alone, usually without use of anaesthesia and electrically‐driven equipment, and restoration of the dental cavity with an adhesive material (glass ionomer cement (GIC), composite resins, resin‐modified glass‐ionomer cement (RM‐GICs) and compomers) (Tyas 2000).
Recently, modified ART approaches have been introduced, as opposed to 'true' ART as described above. These modified approaches involve opening the cavity with a drill, cleaning, restoring and finishing with hand instruments, or using alternative restorative materials including amalgam (Monse‐Schneider 2003). Also, some studies applied ART‐type GICs as pit and fissure sealants using different methods such as the press‐finger method (Yip 2002a). These modified ART approaches are not considered to be 'true' ART (Holmgren 2013).
Apart from these modified approaches, the American Academy of Pediatric Dentistry (AAPD) (AAPD 2008‐2009) introduced the Interim Therapeutic Restorations (ITR) approach, which uses almost the same technique as ART, although it may have different therapeutic goals. The ITR procedure involves removal of caries using hand or slow‐speed rotary instruments, as opposed to ART, which uses only hand instruments, followed by restoration with an adhesive restorative material such as self‐setting or resin‐modified glass ionomer cement (RM‐GIC). While ART is recognised as a permanent treatment, the AAPD regards ITR as a provisional technique. The ITR, according to AAPD, may be used "to restore and to prevent dental caries in young patients, uncooperative patients, patients with special health care needs, and situations in which traditional cavity preparation and/or placement of traditional dental restorations are not feasible; it may be used for caries control in children with multiple carious lesions prior to definitive restoration of the teeth" (AAPD 2008‐2009). Based on the AAPD definition, if ITR is applied using hand instruments, and not rotary instruments, it can then be considered as a 'true' ART.
The advantages of ART compared with conventional restorative techniques using dental handpiece and burs include: provision of restorative dental treatment outside the dental surgery setting; a biologically friendly approach; minimal cavity preparations; low costs (Frencken 1999; Mjör 1999; Yip 2001; Yip 2002a); reduced risk for subsequent endodontics and tooth extraction (Anusavice 1999); and lower dental anxiety in children and adults (more 'patient‐friendly') (Mickenautsch 2007; Schriks 2003). These advantages are particularly important in low‐income countries, where electricity supplies are intermittent and people have difficulties accessing dental care. In addition, people who are elderly, medically‐compromised (e.g. HIV infected) or dental phobic can have problems accessing dental care and could benefit from the ART approach (Cole 2000; Honkala 2002; Steele 2007).
Glass‐ionomer cements (GICs) are the predominant restorative materials used for ART (Yip 2001). GIC restorative materials have advantages such as the ability to bond chemically to enamel and dentine, biocompatibility with pulpal tissue and less potential to induce recurrent caries, inhibition of enamel demineralisation, good cavity seal, ease of use, and low costs (Frencken 1996; Van 't Hof 2006). As shown by a recent Cochrane Review, the sealing‐in effect of GICs apart from replacement of damaged tooth tissue, can help with the management of dental carious lesions (Dorri 2015). Although GICs have been the main material used, other adhesive materials include composite resins, RM‐GICs and compomers.
How the intervention might work
As described, ART approach relies on removal of dental caries using hand instruments only, followed by restoration with an adhesive material. The adhesive restorative material prevents diffusion of acids from biofilms into the lesion or mineral out of the lesion, thereby arresting the lesions or reducing their progression. Furthermore, using hand instruments only, minimises iatrogenic damage to the intact tooth substance whilst removing carious tissue.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important ones to maintain in the Cochrane Library (Worthington 2015). This review was identified as a priority title by the paediatric dentistry expert panel (Cochrane Oral Health priority review portfolio).
The ART approach seems to be an economic and effective method for improving the oral health not only of people in low‐income countries, but also of those in high‐income countries (Frencken 2004b). It may be considered as a minimally invasive alternative for conventional restorative dental treatment, particularly for Class I (occlusal) single‐surface dental cavities. Because of the advantages claimed for ART, it is important to systematically review the evidence available.
The available systematic reviews on studies comparing the ART approach with conventional approach have limitations including: restricting the search to only one electronic database (MEDLINE) and English language studies (Frencken 2004a; Van 't Hof 2006); not assessing the quality of included studies (Van 't Hof 2006); only including permanent teeth and class I cavities (Frencken 2004a); inconsistency with PRISMA guidelines (Moher 2009) in several areas, such as protocol and registration, risk of bias across studies, reporting of limitations and funding (Frencken 2004a; Mickenautsch 2010; Pettar 2011). We aimed to systematically review randomised controlled trials comparing 'true' ART with conventional restorative approaches.
Objectives
To assess the effects of true Atraumatic Restorative Treatment (ART) compared with conventional treatments for managing dental caries lesions in the primary and permanent teeth of children and adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) with at least six months' follow‐up that compared the effects of 'true' ART with a conventional restorative approach using the same or different restorative dental materials. Parallel‐group, split‐mouth and cluster‐study design were eligible for inclusion.
Types of participants
We included dentate participants, regardless of their age and sex, with a history of dental (coronal or root) primary caries lesions extended into enamel and dentine (but not the pulp) and who have undergone restorative treatment using either conventional restorative or true ART approaches. We also considered primary and permanent teeth with single or multiple surface lesions.
Types of interventions
We included adhesive restorative materials, such as GICs with different viscosities or resins, placed with the 'true' ART approach, including ITR with hand instruments, compared with the same or different restorative materials, such as GIC, placed with conventional cavity preparation methods. Only studies using the same restorative material in both arms were considered as key results and the other studies were included for completeness.
We excluded studies on modified ART techniques.
Types of outcome measures
Primary outcomes
-
Restoration failure, that is, a lost or deficient restoration in the 1) primary dentition, 2) permanent immature dentition, 3) permanent mature dentition
-
Pain (during and immediately after treatment expressed as intensity of pain or presence or absence of pain)
Secondary outcomes
-
Adverse events
-
Secondary caries
-
Participant experience, for example, satisfaction or quality of life measured by self report, and discomfort, anxiety or stress measured by physiological means or behavioural observation
-
Costs (direct) ‐ cost of treatment
-
Costs (indirect) ‐ time off school or work to attend dental visits
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials. There were no language, publication year or publication status restrictions:
-
Cochrane Oral Health’s Trials Register (searched 22 February 2017) (Appendix 1);
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 1) in the Cochrane Library (searched 22 February 2017) (Appendix 2);
-
MEDLINE Ovid (1946 to 22 February 2017) (Appendix 3);
-
Embase Ovid (1980 to 22 February 2017) (Appendix 4);
-
LILACS BIREME Virtual Health Library (Latin American and Caribbean Health Science Information database; 1982 to 22 February 2017) (Appendix 5);
-
BBO BIREME Virtual Health Library (Bibliografia Brasileira de Odontologia; 1986 to 22 February 2017) (Appendix 6).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying RCTs and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 (Lefebvre 2011).
Searching other resources
The following trials registries were searched for ongoing studies:
-
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 22 February 2017) (Appendix 7);
-
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 22 February 2017) (Appendix 8).
Reference lists
Two review authors independently examined the reference lists of relevant trials in order to identify studies not identified in the previous searches.
Correspondence
We contacted organisations, researchers and experts known to be involved in the field, either by phone, email or in person during scientific events, in an effort to trace unpublished or ongoing studies. We also contacted dental materials and equipment manufacturers to identify any ongoing or unpublished studies.
We did not perform a separate search for adverse effects of interventions used, we considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
We imported the downloaded set of records from each database to the bibliographic software package Endnote and merged them into one core database to remove duplicate records and to facilitate retrieval of relevant articles. We also obtained potentially relevant reports identified when searching other sources (reference lists of relevant trials, reviews, articles and textbooks). The records located from searching these (non‐electronic) sources were entered manually in Endnote. All records identified by the searches were checked on the basis of title first, then by abstract or keywords or both. Two review authors independently assessed the eligibility of the full text of relevant records (Figure 1).
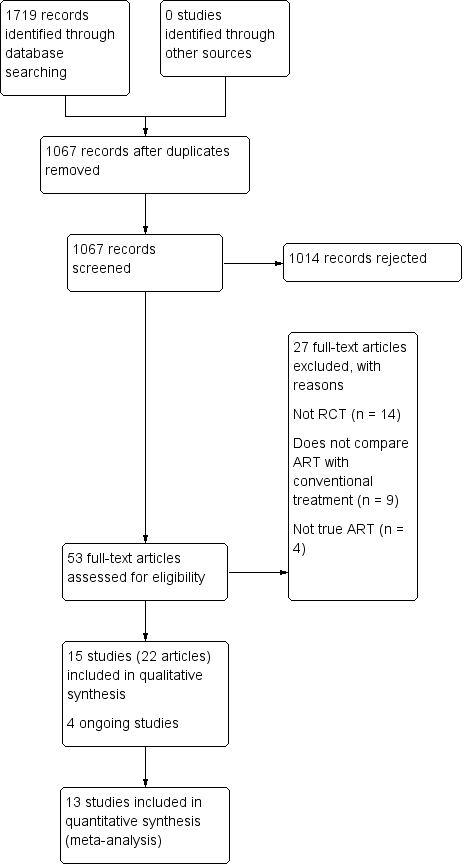
Study flow diagram
One review author (Mojtaba Dorri (MD)) assessed all the references. Two others researchers (Dominic Hurst (DH) and Carlos Zaror (CZ)) assessed the references to establish whether the studies met the inclusion criteria or not, using an inclusion criteria form, which had been prepared previously and pilot tested. We resolved disagreements by discussion. Had resolution not been possible, we would have consulted a third review author (Valeria Marinho (VM)).
The review authors could read reports in English, Persian, Arabic, Portuguese and Spanish. We identified two papers in Chinese and two papers in Dutch. The papers were translated by two translators who were native speakers and fluent in English. One of the authors (MD) compared two versions. The minor disagreements were resolved by discussion with the translators.
We contacted the authors of any articles we could not classify in order to ascertain if inclusion criteria were met. If we identified more than one publication of a trial, we listed the paper with the primary outcome as the primary reference. Where a trial report thought to be potentially relevant was in a language not known to the review authors, it was translated by a native speaker who was fluent in English.
From all studies meeting the inclusion criteria, we extracted the data and assessed risk of bias. We recorded studies rejected at this or subsequent stages in the ’Characteristics of excluded studies’ tables, along with reasons for exclusion.
Data extraction and management
Two review authors (CZ and MD) independently extracted data from the included studies using a pilot‐tested data‐extraction form. The data were then entered into the Characteristics of excluded studies table in Review Manager 5 (RevMan5) (RevMan 2014) and checked for differences. Any disagreements were resolved through discussion with another review author (Mª José Martínez Zapata (MMZ)) until we reached consensus. We contacted trial authors for clarification or missing information, where there was any uncertainty or data were missing. We treated studies with duplicate publications as a single source of data. Review authors were not blinded to the names of the authors, institutions, journal of publication, or results of the studies.
In the data extraction form, we recorded the following details for each trial: RCT design (e.g. parallel, split‐mouth, cluster); country where the trial took place; setting (e.g. primary or secondary care); funding source; inclusion criteria; exclusion criteria; number of participants randomised and evaluated; baseline number of decayed, missing and filled primary teeth (dmfts)/and permanent teeth (DMFTs); test and control interventions; type and number of operators; primary and secondary outcomes; sample size calculation; duration of follow‐up; any co‐interventions; risk of bias; and any other relevant data. We used the data for each specific time point or time interval separately, as reported in the original studies.
Assessment of risk of bias in included studies
Two review authors (CZ and MD) conducted 'Risk of bias' assessment independently and in duplicate for all the included trials, according to the criteria for assessing risk of bias described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreements were resolved through discussion with another review author (Mª José Martínez Zapata (MMZ)) until we reached a consensus. We contacted trial authors where necessary.
We assessed the risk of bias to be high, unclear or low for seven domains:
-
Sequence generation: was the method used to generate the allocation sequence appropriate to produce comparable groups? We graded this domain as having a low risk of bias if the authors described a random component in the sequence generation process (e.g. random number table, coin tossing, drawing of lots).
-
Allocation sequence concealment: was the method used to conceal the allocation sequence appropriate to prevent the allocation being known in advance of, or during, enrolment? We graded this domain as having a low risk of bias if the authors described adequate concealment (e.g. by means of central randomisation, sequentially numbered, opaque envelopes), and graded high risk of bias if inadequate concealment was documented (e.g. alternation, use of case record numbers, dates of birth or day of the week) or if allocation was not concealed.
-
Blinding of participants and personnel: was knowledge of the allocated intervention adequately prevented during the study? We graded this domain as having a high risk of bias if the study did not use any blinding of participants or operators.
-
Blinding of outcome assessors: was knowledge of the allocated intervention adequately prevented during the study? We graded this domain as having a high risk of bias if the study did not use any blinding of assessors.
-
Incomplete outcome data: how complete were the outcome data for the primary outcomes? Did authors report dropout rates and reasons for withdrawals? Did they impute missing data appropriately? We graded this domain as having a low risk of bias if the proportion of the missing outcome data was less than 25% and the groups were balanced in numbers and reasons for dropouts, or if investigators imputed missing data using appropriate methods. If dropout was above 25% and there was no information on reasons for dropouts across groups, but attrition was balanced, we graded the risk of bias as unclear. We graded it as high if the proportion of missing outcome data was over 25% and not balanced between groups.
-
Selective outcome reporting: did investigators report appropriate outcomes or were key outcomes missing? We graded this domain as having a low risk of bias if authors reported all pre‐specified outcomes. If they did not report prespecified or expected data, we assumed the risk of bias to be high.
-
Other sources of bias: was the study apparently free of other problems that could put it at a high risk of bias? These include information on the baseline characteristics of the intervention and control groups and the similarity in using co‐interventions between groups. We graded the trials as having a high risk of bias if there were important differences in demographic characteristics or if the groups received different co‐interventions during the trial, or if the statistical analysis was inadequate or inappropriate.
We developed a standardised 'Risk of bias' assessment form and entered data in the 'Risk of bias' tables in RevMan 5 (RevMan 2014).
We summarised the potential risk of bias for each study overall:
-
low risk of bias: plausible bias not likely to seriously alter the results (if low risk of bias for all items);
-
unclear risk of bias: plausible bias that raises some doubt about the results (if unclear risk of bias for one or more key items, but none at high risk of bias);
-
high risk of bias: plausible bias that seriously weakens confidence in the results (if high risk of bias for one or more key items), as described in Section 8.7 of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (updated March 2011) (Higgins 2011).
We completed a ’Risk of bias’ table for each included study (see Characteristics of included studies) and presented the results graphically by domain over all studies and by study (Figure 2; Figure 3).
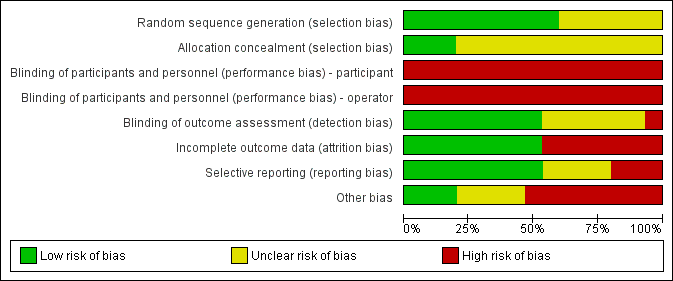
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
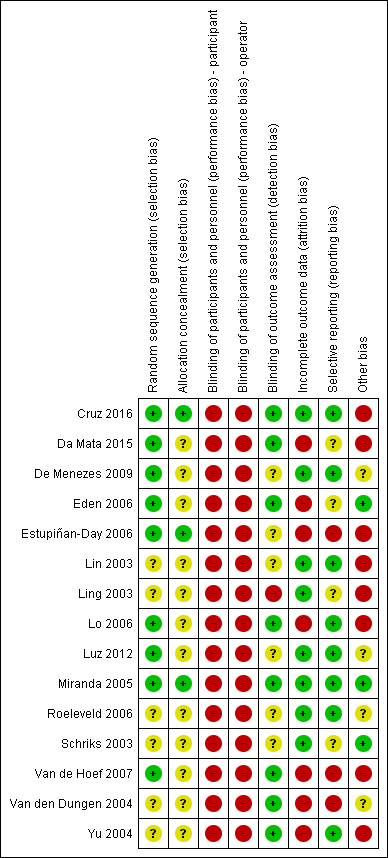
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Measures of treatment effect
We planned to convert data obtained from visual analogue scales and any categorical outcomes into dichotomous data prior to analysis. For continuous data, we planned to calculate mean difference with 95% confidence interval (CI). For each trial, we calculated odds ratios (OR) with 95% CIs for all prespecified dichotomous outcomes.
Unit of analysis issues
In parallel‐group studies, the unit of analysis was the individual. In studies where the unit of randomisation was the individual, but more than one tooth/surface was treated per individual (cluster‐randomised studies), we considered tooth/surface as the unit of analysis and standard errors of the estimates were adjusted taking into account the multiplicity or clustering (Deeks 2011). We considered an intracluster correlation coefficient (ICC) of 0.05, based on published data (Vas 2008).
In split‐mouth studies where two tooth/surfaces are randomised per individual, these pairs are not strictly independent (the unit of analysis is the pair) and therefore, were analysed as 'paired data' (Higgins 2003; Deeks 2011). In these cases, we computed design‐adjusted ORs and standard errors with the Becker‐Balagtas method outlined in Elbourne 2002, assuming a conservative correlation coefficient of 0.05 according to Dorri 2015. We planned to calculate the log odds ratio and standard error separately for each outcome.
In cluster split‐mouth studies, where more than two tooth/surfaces are randomised per individual, the unit of analysis is each pair. We considered these trials as split mouth, analysing the pairs independently, ignoring the clustering effect.
Dealing with missing data
We contacted the study authors where data were missing on the trial characteristics, methodology and/or outcomes. We did not consider missing data as a reason to exclude any of the trials from the review. We had planned to impute missing data, if appropriate. However, we did not carry out data imputation as we assumed all missing data to be at random.
Assessment of heterogeneity
We assessed statistical heterogeneity by examining the characteristics of the studies: the similarity between the types of participants, the interventions and the outcomes as described in Section 9.5 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
For this purpose we used the I² statistic (Higgins 2003), which examines the percentage of total variation across studies due to heterogeneity rather than to chance. According to the Cochrane Handbook for Systematic Reviews of Interventions the I2 values are interpreted as follows (Deeks 2011):
-
0% to 40% might not be important;
-
30% to 60% may represent moderate heterogeneity;
-
50% to 90% may represent substantial heterogeneity;
-
75% to 100% represents considerable heterogeneity.
Assessment of reporting biases
We had planned to assess whether the review was subject to publication bias (or small‐study effects) by using a funnel plot (plots of the effect estimates versus the inverse of their standard errors) (Egger 1997). Asymmetry of the funnel plot may indicate publication bias or other sources of asymmetry including poor methodological quality leading to spuriously inflated effects in smaller studies, true heterogeneity and chance (Sterne 2011). We did not include more than 10 trials in meta‐analysis and therefore, a funnel plot to explore possible publication biases was not indicated. For future updates, if more than 10 trials are included we plan to use a funnel plot to explore publication bias (Egger 1997).
Data synthesis
We pooled only studies that used the same restorative materials in both comparator groups, as different restorative materials require different cavity designs and have different properties that may affect the study outcomes. For example, whilst adhesive restorative materials (e.g. GIC, composite resins) rely on chemical bonding to the tooth for retention, the success of amalgam restoration depends on mechanical retention from the converged cavity walls. This would mean that for an amalgam restoration, following caries removal, the cavity may need to be extended in order to obtain mechanical retention. This may affect the length of procedure, and in turn the patient's experience, and also the restoration survival. In addition GIC releases fluoride that may affect restoration survival.
Our analysis includes data only of those whose results are known, using as a denominator the total number of participants for whom data were recorded for the particular outcome. We expected differences in effect estimates between studies in terms of the number of cavities or surfaces treated per participant and also the duration of follow‐up. Therefore, we applied a random‐effects model for any meta‐analyses (Deeks 2011).
We pooled parallel and split‐mouth data using the generic inverse variance (GIV) (Deeks 2011).
We did not pool data if heterogeneity was over 75%. This was mainly because indicating an average value for the intervention effect when there is a significant inconsistency in the direction of effect may be misleading (Deeks 2011).
We anticipated variation in the timing of endpoints across the studies, both in terms of participant‐reported pain and clinical restoration failure. We included in the meta‐analysis the longest follow‐up reported for each study.
Where studies had multiple intervention or comparator trial arms, we combined summary statistics from all groups where appropriate. We excluded any intervention arms without ART from the meta‐analysis.
The data was analysed using RevMan 5 software (RevMan 2014).
In the event that there were insufficient clinically homogeneous trials for any specific intervention or insufficient study data that could be pooled, a narrative synthesis was presented.
Subgroup analysis and investigation of heterogeneity
We had planned to perform subgroup analysis for dental caries type, as a source of clinical heterogeneity, if sufficient data were available. Therefore, we stratified the analyses in subgroups according to type of cavity surface:
-
studies reporting on single lesion;
-
studies reporting on multiple lesions;
-
studies reporting on single and multiple lesions;
-
studies where lesion type was not reported;
-
studies reporting on coronal and root lesion, or on root lesions only.
Sensitivity analysis
We had planned to conduct a sensitivity analysis of the primary outcomes by excluding studies with overall high risk of bias (that is high risk of bias in at least one domain). However, all the included studies were at high risk of bias for at least one domain and therefore, we did not carry out a sensitivity analysis.
Summary of findings
We used GRADEpro GDT software (GRADEpro GDT 2015) to assess the quality of the body of evidence for study outcomes (pain, restoration failure, adverse events) and to develop summary of findings Table for the main comparison, summary of findings Table 2 and summary of findings Table 3. The GRADE approach appraises the quality of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. The approach considers evidence from RCTs that do not have serious limitations as 'high' quality. The following factors can decrease the quality of evidence: within‐study limitations (risk of bias), indirectness of the evidence, heterogeneity (inconsistency) in the data, imprecision of effect estimates, and risk of publication bias (Schünemann 2011).
Results
Description of studies
Please see Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
The search strategy retrieved 1719 citations (Figure 1). After deleting duplicates and screening titles and abstracts, we evaluated 53 full texts of potentially eligible studies. We excluded 27 studies (Characteristics of excluded studies), and included 22 articles that corresponded to 15 completed RCTs (Cruz 2016; Da Mata 2015; De Menezes 2009; Eden 2006; Estupiñan‐Day 2006; Lin 2003; Ling 2003; Lo 2006; Luz 2012; Miranda 2005; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004) (Characteristics of included studies). We also retrieved four ongoing trials (CTRI007332; NCT02562456; NCT02568917; RBR‐4nwmk4) (Characteristics of ongoing studies).
Two studies were in Chinese (Lin 2003; Ling 2003) and two articles were in Dutch (Schriks 2003; Van den Dungen 2004). We contacted two authors in an effort to obtain additional information (Estupiñan‐Day 2006; Eden 2006). Both trial authors responded and answered our questions.
Included studies
We found 15 completed studies, reported in 22 articles, and 4 ongoing studies. Six studies were reported in multiple articles (Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Schriks 2003; Van de Hoef 2007; Yu 2004). Included studies were published between 2002 and 2016 with a follow‐up period that ranged from 6 to 36 months.
Design
Eleven studies used a parallel‐group design, with six of these using a parallel‐group, cluster‐randomised design. Four studies used a split‐mouth design (Eden 2006; Ling 2003; Miranda 2005; Yu 2004). Only five studies reported a sample size calculation (Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Lo 2006; Miranda 2005).
Funding for the studies was provided by government (Cruz 2016; Da Mata 2015; Lo 2006), foundations (De Menezes 2009; Eden 2006; Estupiñan‐Day 2006; Van de Hoef 2007; Van den Dungen 2004) and pharmaceutical sources or manfacturers(Eden 2006; Roeleveld 2006; Schriks 2003; Yu 2004). Funding was unclear in four studies (Lin 2003; Ling 2003; Luz 2012; Miranda 2005).
Setting
Studies were conducted in China (Lin 2003; Ling 2003; Lo 2006; Yu 2004), Brazil (De Menezes 2009; Luz 2012; Miranda 2005), Indonesia (Schriks 2003; Van den Dungen 2004), and Colombia, Ireland, Turkey, Tanzania and Surinam (Cruz 2016; Da Mata 2015; Eden 2006; Roeleveld 2006; Van de Hoef 2007). There was one international multicentre trial in Ecuador, Panamá and Uruguay (Estupiñan‐Day 2006).
The study setting was dental clinics or hospitals for seven studies (Da Mata 2015; De Menezes 2009; Eden 2006; Ling 2003; Luz 2012; Miranda 2005; Yu 2004); schools for two studies (Estupiñan‐Day 2006; Van den Dungen 2004), and nursing homes for two studies (Cruz 2016; Lo 2006). Four studies did not report the setting (Lin 2003; Roeleveld 2006; Schriks 2003; Van de Hoef 2007).
Participants
Overall, data on 3760 participants and 9944 teeth were included in the review. The studies examined 6347 teeth that were treated using ART and 3204 that received a conventional treatment. One study did not report the teeth treated by group (Van den Dungen 2004).
The mean age of the participants was 25.42 years (ranging from 3 to 101 years). Forty‐eight per cent of participants were male.
Only Eden 2006 reported the baseline dmft index (average number of decayed, missing and filled primary teeth) with a mean dmft of 6.9. Two studies reported a baseline DMFT (average number of decayed, missing and filled permanent teeth) index ranging between 1.0 to 28.54 (Da Mata 2015; Lo 2006).
Eleven trials included only primary teeth, with participants' age ranging from 3 to 13 years (De Menezes 2009; Eden 2006; Lin 2003; Ling 2003; Luz 2012; Miranda 2005; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). Four trials evaluated permanent teeth with participants aged between 7 to 101 years (Cruz 2016; Da Mata 2015; Estupiñan‐Day 2006; Lo 2006).
Interventions
The key results of this review are from the nine included studies that evaluated the effects of ART compared to conventional treatment using the same restorative material in both arms:
-
seven studies including a total of 1402 participants compared ART using H‐GIC (high viscosity glass ionomer cement) with conventional treatment using H‐GIC in primary teeth (De Menezes 2009; Lin 2003; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004);
-
one study with 160 participants compared ART using composite with conventional treatment using composite in primary teeth (Eden 2006);
-
one study with 75 participants compared ART using RM‐GIC (resin‐modified glass ionomer cement) with conventional treatment using RM‐GIC in permanent teeth (Cruz 2016).
Five included studies compared ART versus conventional treatment but used different restorative materials in each arm:
-
one study with 106 participants compared ART using H‐GIC versus conventional treatment using amalgam in primary teeth (Miranda 2005);
-
one study with 80 participants compared ART using GIC versus conventional treatment using amalgam in primary teeth (Ling 2003) and one study in permanent teeth (1629 participants) (Estupiñan‐Day 2006);
-
one study with 30 participants compared ART using H‐GIC versus conventional treatment using composite in primary teeth (Luz 2012);
-
two studies with 210 participants compared ART using H‐GIC versus conventional treatment using RM‐GIC in permanent teeth (Da Mata 2015; Lo 2006).
Only one study used local anaesthesia with an ART group (Van de Hoef 2007). This was a four‐armed study that used local anaesthesia in two of the four arms (one ART and one conventional treatment). Four other studies reported the use of local anaesthesia with conventional treatment (Da Mata 2015; De Menezes 2009; Lo 2006; Luz 2012); five studies reported that it was not used (Eden 2006; Miranda 2005; Roeleveld 2006; Schriks 2003; Yu 2004); and five studies did not report whether or not local anaesthesia was used (Cruz 2016; Estupiñan‐Day 2006; Lin 2003; Ling 2003; Van den Dungen 2004).
Six studies evaluated the effects of ART on multi‐surface caries lesions (Eden 2006; Luz 2012; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004). Four trials evaluated both single and multi‐surface lesions (Da Mata 2015; De Menezes 2009; Miranda 2005; Yu 2004). Two trials evaluated root lesions (Cruz 2016; Lo 2006). Three studies did not specify cavity type (Estupiñan‐Day 2006; Lin 2003; Ling 2003).
Most studies reported that the interventions were delivered by the dentist or by the dentist and dental students (Schriks 2003; Van de Hoef 2007; Van den Dungen 2004), or by dentists and dental hygienists (Estupiñan‐Day 2006).
Outcomes
Four studies measured pain (De Menezes 2009; Estupiñan‐Day 2006; Luz 2012; Miranda 2005); one study did not report whether anaesthesia was used (Estupiñan‐Day 2006); in two studies, local anaesthesia was given in the conventional treatment arm only (De Menezes 2009; Luz 2012); and the cavity preparation was different in the arms of one study (Miranda 2005).
Restoration failure was assessed in 13 studies (Cruz 2016; Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Lin 2003; Ling 2003; Lo 2006; Luz 2012; Miranda 2005; Roeleveld 2006; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). We pooled the results of the studies only if the same restorative material was used in the intervention and comparison arms.
None of the studies measured adverse effects.
Secondary/recurrent caries were measured in four studies (Cruz 2016; Miranda 2005; Roeleveld 2006; Yu 2004).
Other aspects of participant experience were measured in four studies: discomfort (Schriks 2003; Van de Hoef 2007); anxiety (Eden 2006); acceptability (Luz 2012); co‐operation (Estupiñan‐Day 2006; Ling 2003).
Two studies assessed cost‐effectiveness (Da Mata 2015; Estupiñan‐Day 2006).
We did not carry out meta‐analysis where different restorative materials were used in trial arms or local anaesthesia was used in only one study arm, as discussed above. In these cases, the data were narratively presented.
Excluded studies
We excluded 27 studies (see Characteristics of excluded studies). The reasons for exclusion were:
-
did not compare ART with conventional treatment (nine studies);
-
the ART technique was modified (14 studies);
-
not randomised (four studies).
Risk of bias in included studies
All studies were judged to be at overall high risk of bias (see Figure 2; Figure 3).
Allocation
Random sequence generation
Of 15 included studies, nine adequately reported the methods used to generate the randomisation sequence, which included computerised sequence generation (Da Mata 2015; De Menezes 2009; Eden 2006; Estupiñan‐Day 2006; Lo 2006; Van de Hoef 2007), ballot box (Luz 2012), or table of random numbers (Cruz 2016; Miranda 2005). We classified the other studies as 'unclear' as authors mentioned that the clinical trial was randomised but did not report further details.
Allocation concealment
Only three studies adequately reported allocation concealment using sealed envelopes (Cruz 2016; Miranda 2005) or centralised assignment (Estupiñan‐Day 2006). In the remaining studies this was not specified and therefore, we classified them as 'unclear'.
Blinding
Blinding of participants and personnel
Given the nature of the intervention, it is not feasible to blind participants and operators to the type of instruments (i.e. manual or rotary) used for restoration. Therefore, both participants and operators were aware of type of intervention.
Blinding of outcome assessors
It is, however, possible to blind outcome assessors to the type of intervention. The outcome assessors were blind in the eight studies that used the same restorative materials for both the intervention and comparison groups. We considered these studies to be at low risk of bias (Cruz 2016; Da Mata 2015; Eden 2006; Lo 2006; Miranda 2005; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). One study reported that assessors were not blind and therefore we rated it as 'high risk' (Ling 2003). Other studies did not report blinding of outcome assessor and were rated as 'unclear'.
Incomplete outcome data
All trials reported if there were any participants who were lost to follow‐up. However, only six studies reported the reasons for dropout (Cruz 2016; Da Mata 2015; Lo 2006; Luz 2012; Miranda 2005; Van de Hoef 2007). We assessed seven studies as 'high risk' of bias because they had losses to follow‐up over 20% (Da Mata 2015: Eden 2006; Estupiñan‐Day 2006; Lo 2006; Van de Hoef 2007; Van den Dungen 2004; Yu 2004), which was higher than had been estimated in the sample size calculation. We assessed the remaining studies as 'low' risk of attrition bias.
Selective reporting
We judged seven studies to be at 'high' or 'unclear' risk of selective reporting bias (Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Ling 2003; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004). Estupiñan‐Day 2006 did not report the results at three years' follow‐up and Van den Dungen 2004 did not report results at follow‐ups before three years. Other studies reported incomplete data for the follow‐ups.
Other potential sources of bias
We assessed three studies as having no other potential sources of bias (Eden 2006; Miranda 2005; Schriks 2003).
We judged four studies to be 'unclear' as they did not provide information about either important baseline characteristics of the included participants or co‐interventions, or both (De Menezes 2009; Luz 2012; Roeleveld 2006; Van den Dungen 2004).
We assessed eight studies as 'high risk' of other potential sources of bias. In addition to failing to provide information about baseline characteristics, Cruz 2016 did not consider the paired data in their analysis. Lin 2003 and Van de Hoef 2007 did not consider the intracluster coefficient. Ling 2003, Lo 2006 and Yu 2004 did not consider the paired data in their analysis. Da Mata 2015 had an imbalance in DMFT score between groups. Estupiñan‐Day 2006 did not report DMF scores or information about supply of water fluoridation between countries and their analysis did not consider the intracluster correlation coefficient.
Effects of interventions
See: Summary of findings for the main comparison Atraumatic restorative treatment (ART) using high‐viscosity glass ionomer cement (H‐GIC) compared with conventional restorative treatment using H‐GIC for dental caries; Summary of findings 2 Atraumatic restorative treatment (ART) using composite resins compared with conventional restorative treatment using composite resins for dental caries; Summary of findings 3 Atraumatic restorative treatment (ART) using resin‐modified glass ionomer cement (RM‐GIC) compared with conventional restorative treatment using RM‐GIC for dental caries
Comparison 1: ART using H‐GIC versus conventional treatment using H‐GIC
Seven studies reported data for this comparison in primary teeth: De Menezes 2009; Lin 2003; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004. Data from Schriks 2003 were not useable.
Restoration failure
Five studies, which randomised 959 participants, reported data for restoration failure in the primary dentition with follow‐ups of between 12 and 36 months (Lin 2003; Roeleveld 2006; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). The odd ratios (OR) of restoration failure were 1.60 times higher in the ART arm than in the conventional arm, over a follow‐up period of 12 to 24 months (OR 1.60, 95% CI 1.13 to 2.27; I2 = 0%, 643 participants analysed; Analysis 1.1). The quality of evidence was downgraded by two levels from 'high' to 'low' due to serious concerns regarding risk of performance bias in all five studies, attrition bias in three studies (Yu 2004; Van de Hoef 2007; Van den Dungen 2004), and reporting bias in two studies (Van de Hoef 2007; Van den Dungen 2004) (Analysis 1.1; Figure 4; summary of findings Table for the main comparison).
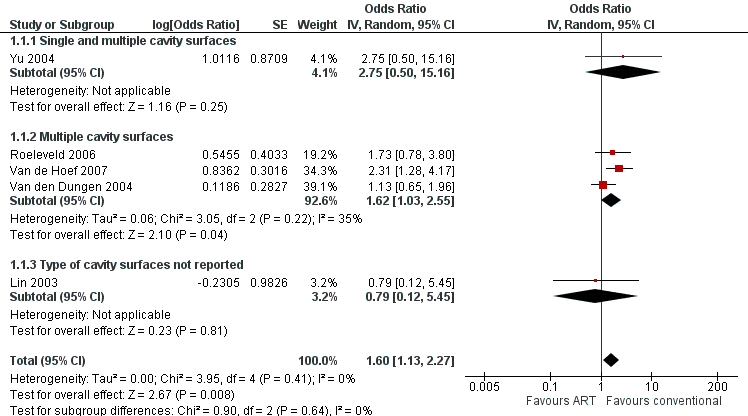
Forest plot of comparison 1. Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, outcome: 1.1 restoration failure (primary teeth) ‐ longest follow‐up
We carried out subgroup analysis to investigate the impact of cavity type on restoration failure. One study with 27 participants included single and multiple surfaces (Yu 2004). Three studies with 558 participants reported on multiple surfaces only (Roeleveld 2006; Van de Hoef 2007; Van den Dungen 2004). One study with 58 participants did not report the type of cavity treated (Lin 2003). The Chi2 test did not show any evidence of a difference according to cavity type (Chi2 = 0.90, df = 2, P = 0.64, I2 = 0%).
Pain
One study, which randomised 40 participants, reported data for pain in the primary dentition for children aged between four and seven years. ART may reduce the pain during procedure compared with control treatment (MD ‐0.65, 95% CI ‐1.38 to 0.07; 40 participants analysed; Analysis 1.2) (De Menezes 2009). The evidence was downgraded one level because it is a single study (indirectness) and one level because of serious concern regarding high risk of performance bias (summary of findings Table for the main comparison).
Secondary outcomes
Secondary caries
Two studies reported on secondary caries, but this outcome was not reported by trial arm (Yu 2004; Roeleveld 2006).
Participant experience (discomfort)
One study that reported the results of treating multiple lesions in primary dentition, found that the odds of discomfort were reduced with ART in children between six and eight years of age (OR 0.95, 95% CI 0.51 to 1.79; 220 participants analysed; Analysis 1.3) (Van de Hoef 2007). Local anaesthetic was administered in the intervention and comparison groups.
Other outcomes
No studies reported on restoration failure in permanent dentition, adverse events, or costs for this comparison.
Comparison 2: ART using composite versus conventional treatment using composite
Restoration failure
One study, which randomised 160 participants with a mean age of seven years, reported data for restoration failure in multi‐surface lesions of primary dentition with follow‐up at 24 months (Eden 2006). The odds of restoration failure were slightly greater with ART than conventional treatment, however the 95% CI included the possibility that ART both increased the risk of restoration failure and reduced restoration failure, so this result is inconclusive (OR 1.11, 95% CI 0.54 to 2.29, 57 participants analysed; Analysis 2.1). We downgraded the quality of evidence by three levels: one level because the information was based on a single study comprising participants of a very narrow age range (indirectness) and two levels because of very serious concerns regarding risk of bias (high risk of performance bias and attrition bias (103 children (64%) lost to follow‐up at 24 months)) (summary of findings Table 2).
Participant experience (dental anxiety)
Eden 2006 was the only study to report on participant experience (dental anxiety). The authors reported no observed difference in mean dental anxiety as measured by the Venham Picture test (MD 0.00, 95% CI ‐0.52 to 0.52; 57 participants analysed; Analysis 2.2).
Other outcomes
No studies reported on pain, restoration failure in the permanent dentition, adverse events, secondary caries, or costs for this comparison.
Comparison 3: ART using RM‐GIC versus conventional treatment using RM‐GIC
Restoration failure
One study, which randomised 75 participants with a mean age of 75 years (range 60 to 101 years), reported data for restoration failure in root surfaces of the mature permanent dentition (Cruz 2016). The odds of restoration failure at 24 months' follow‐up were not significantly greater with ART than conventional treatment (OR 2.71, 95% CI 0.94 to 7.81; 64 participants analysed; Analysis 3.1). We downgraded the quality of evidence by three levels: one level as the information was based on a single study comprising older adults only (indirectness), one level because of imprecision and one level because of serious concerns regarding risk of bias (high risk of performance bias (11 adults (15%) lost to follow‐up at six months)) (summary of findings Table 3).
Secondary caries
One study reported data on secondary caries for this comparison (Cruz 2016). The odds of secondary caries at six months were greater with ART than with conventional treatment (Analysis 3.2).
Other outcomes
No studies reported on pain, restoration failure in the primary dentition, adverse events, participant experience, or costs for this comparison.
Comparison 4: ART versus conventional treatment using different restorative materials
Restoration failure
Seven studies used different restorative materials for the intervention and comparator (Da Mata 2015; Estupiñan‐Day 2006; Ling 2003; Lo 2006; Luz 2012; Miranda 2005; Yu 2004) (see Table 1).
| ART with one material versus conventional treatment with another material | |||
| ART material | Conventional treatment material | Outcomes | Effect estimate OR (95% CI) |
| H‐GIC | Amalgam | Restoration failure ‐primary teeth – 2 studies (Miranda 2005; Yu 2004). Studies reporting on single + multiple lesions | 2.15 (0.73 to 6.35); I2 = 0% |
| Pain (primary dentition) – 1 study (Miranda 2005). Studies reporting on single + multiple lesions | 1.44 (0.45 to 4.60) | ||
| GIC | Amalgam | Restoration failure ‐ primary teeth – 1 study (Ling 2003). Studies reporting on lesion type: not reported | 0.78 (0.30 to 2.02) |
| Restoration failure ‐ permanent, immature teeth – 1 study (Estupiñan‐Day 2006). Studies reporting on lesion type: not reported | 1.71 (1.32 to 2.22) | ||
| Pain ‐ permanent, immature teeth (Estupiñan‐Day 2006) | 0.41 (0.35 to 0.47) | ||
| H‐GIC | Composite and local anaesthetic | Restoration failure ‐ primary teeth – 1 study (Luz 2012). Studies reporting on multiple lesions | 8.00 (1.24 to 51.48) |
| Pain (primary dentition) – 1 study (Luz 2012) | 2.22 (0.51 to 9.61) | ||
| H‐GIC | RM‐GIC and local anaesthetic | Restoration failure ‐ permanent, mature teeth – 2 studies (Da Mata 2015; Lo 2006). Studies reporting on coronal/root caries | 1.46 (0.74 to 2.88); I2 = 0% |
CI: confidence interval; OR: odds ratio
Studies comparing ART using H‐GIC may increase the risk of failure compared with conventional treatment using amalgam in primary teeth (Miranda 2005; Yu 2004).
One study comparing ART using GIC with conventional treatment using amalgam in primary teeth showed that ART may decrease the risk of restoration failure in the primary dentition (Ling 2003). However, in permanent immature teeth, ART resulted in a greater number of failures than conventional treatment (Estupiñan‐Day 2006).
When comparing ART using H‐GIC with conventional treatment using composite in primary teeth, the latter presented significantly fewer failures (Luz 2012).
In root caries of permanent mature teeth, ART with H‐GIC showed greater odds of restoration failure than conventional treatment with RM‐GIC (Da Mata 2015; Lo 2006).
Pain
Of the three studies reporting pain, two RCTs showed increased risk of pain during procedures for participants treated with ART compared with conventional treatment for primary dentition (Luz 2012; Miranda 2005).
One study on permanent immature teeth showed that participants treated with the ART approach presented significantly less pain than the control group (Estupiñan‐Day 2006).
Other outcomes
Ling 2003 assessed participant co‐operation during procedures, showing a co‐operation rate in the ART group significantly higher than in the control group.
No studies reported adverse events, secondary caries, or costs for this comparison.
Discussion
Summary of main results
In total, we included 15 eligible published RCTs in this review, with a total of 3760 participants of whom 48% were men. The mean age of the participants was 25.42 years. The median number of participants per RCT was 291 (range 30 to 2298). Eleven of the trials included primary teeth and four were carried out on permanent teeth. Six studies involved multi‐surface; four involved single and multiple surfaces; two were on root caries and in three trials cavity type was not specified. Most studies used H‐GIC as the restorative material in the ART group; one study used composite resins; and one study used RM‐CGIC. In three studies, the conventional group used amalgam; three studies used RM‐CGIC; two studies used composite resins; and the remaining studies used H‐GIC. We considered the key results to be from the three comparisons that used the same restorative material in both trial arms. The comparison between ART and conventional treatment using different restorative materials was narratively presented.
In primary teeth, there was low‐quality evidence that ART using H‐GIC may increase the risk of restoration failure compared with conventional treatment using H‐GIC. There was low‐quality evidence that ART may reduce pain during the procedure compared with control treatment.
Given the very low‐quality of the evidence from single studies, we are uncertain about the restoration failure of ART compared with conventional treatment using composite over a 24‐month follow‐up period and ART using RM‐GIC in the permanent teeth of older adults with root caries lesions over a six‐month follow‐up period.
None of the included studies reported on adverse effects.
Studies that compared ART with conventional treatment, using different restorative materials in trial arms, did not provide consistent results. The results of these studies for pain were also inconclusive.
Overall completeness and applicability of evidence
Although we included 15 studies in this review, there were only a small number of studies eligible for each comparison.
Only a few studies reported on any of the secondary outcomes.
Only one study that reported on pain was included in the analysis for the pain outcome.
Although the evidence showed that conventional treatment may be more effective than ART technique in primary teeth when the teeth are restored with H‐GIC, these findings should be considered with caution due to the low quality of the evidence. The findings were inconclusive when composite resins or RM‐GIC were used, and applicability to current clinical practice is uncertain due to only one study being included for these comparisons.
There were few available data for secondary caries and participants' experience. No studies reported on adverse events. Only one study reported on the cost of treatment (Da Mata 2015), and concluded that ART was more cost‐effective than conventional treatment for treating older adults. However, these results can only be applied to the healthcare system in Ireland.
In general, the findings of the review should be interpreted with caution because of the high risk of bias in the few studies included and low‐ to very‐low quality of evidence. Clinicians should inform patients of potential pros and cons of each treatment option to enable them to make an informed decision.
Quality of the evidence
We graded the evidence taking into account any limitations in the study design, risk of bias, inconsistency of results, indirectness of evidence, imprecision, presence of publication bias and magnitude of effect estimate.
Evidence on restoration failure was mainly assessed as low‐ to very low‐quality due to high risk of bias and imprecision. High risk of bias was due to performance, attrition, and selective reporting bias. Given that participants and personnel could not be blinded, it was not possible to avoid performance bias. Moreover, the low number of events (i.e. single study) led to additional downgrading for imprecision of the effect estimate.
For the pain outcome, the evidence was of very low quality due to high risk of performance bias and small sample size (i.e. single study).
Potential biases in the review process
We carried out this review according to Cochrane guidelines. We searched a wide range of major electronic databases, without any restriction of language or time. Apart from completed RCTs, we also identified ongoing clinical trials. Where there was uncertainty regarding the studies we contacted the study authors for clarification and further information.
It may be argued that the adjustments to the data made by authors to account for unit of analysis issues could have introduced a risk of bias. We endeavoured to minimise the risk of bias by ensuring that the screening of studies and data extraction were carried out by two authors independently. The data analyses were carried out by two authors and all authors examined the analysis and interpretation of results.
Agreements and disagreements with other studies or reviews
The present review included all available randomised trials comparing ART and conventional treatment in primary and permanent teeth of children and adults. We also identified other systematic reviews on the clinical effectiveness of the ART approach, most of which compared ART to conventional treatment using different restorative materials, mainly amalgam.
Frencken 2004a included only single‐surface ART restorations restored with GIC compared with conventional restorations with amalgam in permanent dentition. They did not show any differences between the two treatments. Mickenautsch 2012 also compared the failure rate in the ART approach versus amalgam fillings in permanent and primary teeth, leaving aside other filling materials. They found no difference between the approaches in both primary and permanent teeth.
Another important difference with some of the existing reviews, such as Frencken 2004a and Van 't Hof 2006 is that we did not introduce any language restrictions and searched a wide range of databases. In our review, we also assessed the quality of the evidence.
Most previous reviews considered survival rate as their only outcome (De Amorin 2012; Frencken 2004a; Van 't Hof 2006), whilst in our review we included a range of primary and secondary outcomes.
Van 't Hof 2006 and De Amorin 2012 assessed the survival of ART restoration using GIC in primary and permanent teeth. Both studies concluded that single‐surface ART restorations using GIC both in primary and permanent dentitions showed higher survival rate compared with multiple‐surface ART restorations.
Pettar 2011 carried out a more comprehensive review to assess the effect of ART on decayed primary and permanent teeth in children between four and 16 years old. It concluded that it was not possible to pool the results due to high clinical heterogeneity. Therefore, it was impossible to get a precise conclusion about the effect of treating childhood caries with ART versus a conventional approach.
Finally, a recent systematic review evaluated the effectiveness of ART in reducing dental anxiety in children with caries lesions in primary teeth compared to conventional treatment (Simon 2017). They concluded that ART was not more beneficial in reducing dental anxiety among paediatric dental patients. We reported a similar finding, although we only included one study for this outcome.

Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Forest plot of comparison 1. Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, outcome: 1.1 restoration failure (primary teeth) ‐ longest follow‐up

Comparison 1 Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, Outcome 1 Restoration failure ‐ primary teeth ‐ longest follow‐up.

Comparison 1 Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, Outcome 2 Pain ‐ primary teeth.

Comparison 1 Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, Outcome 3 Participant experience ‐ discomfort.

Comparison 2 Atraumatic restorative treatment using composite versus conventional treatment using composite, Outcome 1 Restoration failure ‐ primary teeth ‐ longest follow‐up.

Comparison 2 Atraumatic restorative treatment using composite versus conventional treatment using composite, Outcome 2 Participant experience ‐ dental anxiety.

Comparison 3 Atraumatic restorative treatment using resin‐modified glass ionomer cement (RM‐GIC) versus conventional treatment using RM‐GIC, Outcome 1 Restoration failure ‐ permanent teeth ‐ longest follow‐up.

Comparison 3 Atraumatic restorative treatment using resin‐modified glass ionomer cement (RM‐GIC) versus conventional treatment using RM‐GIC, Outcome 2 Secondary caries.
| Atraumatic restorative treatment (ART) using high‐viscosity glass ionomer cement (H‐GIC) compared with conventional restorative treatment using H‐GIC for dental caries | |||||
| Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using H‐GIC Comparison: conventional treatment using H‐GIC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment with H‐GIC | ART with H‐GIC | ||||
| Restoration failure (primary dentition) at 12 to 24 months | 471 per 1000 | 588 per 1000 | OR 1.60 | 643 participants/846 teeth | ⊕⊕⊝⊝ |
| Pain | Mean pain (primary teeth) was 1.38 (SD 1.21) | Mean pain (primary teeth) was 0.73 (SD 1.14) | MD 0.65 lower (1.38 lower to 0.07 higher) | 40 participants | ⊕⊕⊝⊝ |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1We downgraded the evidence by two levels because of very serious concerns regarding risk of bias: we judged all five studies as high risk of performance bias, three studies as high risk of attrition bias, and two studies as high risk of reporting bias. | |||||
| Atraumatic restorative treatment (ART) using composite resins compared with conventional restorative treatment using composite resins for dental caries | |||||
| Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using composite Comparison: conventional treatment using composite | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment | ART | ||||
| Restoration failure (primary dentition) | 362 per 1000 | 387 per 1000 | OR 1.11 | 57 participants/100 teeth | ⊕⊝⊝⊝ |
| Pain | ‐ | ‐ | ‐ | ‐ | Not measured |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1We downgraded the evidence by three levels: one level because it is a single study (indirectness) and two levels because of very serious concern regarding the risk of bias (high risk of performance bias and high risk of attrition bias). The result was also very imprecise. | |||||
| Atraumatic restorative treatment (ART) using resin‐modified glass ionomer cement (RM‐GIC) compared with conventional restorative treatment using RM‐GIC for dental caries | |||||
| Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using RM‐GIC Comparison: conventional treatment using RM‐GIC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment | ART | ||||
| Restoration failure (primary dentition) | ‐ | ‐ | ‐ | 0 studies | No studies included |
| Restoration failure (permanent teeth) | 75 per 1000 | 180 per 1000 | OR 2.71 | 64 participants/141 teeth | ⊕⊝⊝⊝ |
| Pain | ‐ | ‐ | ‐ | ‐ | Not measured |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1We downgraded the evidence by one level because it is a single study (indirectness), one level because of concern regarding high risk of performance bias, and one level because the result was imprecise. | |||||
| ART with one material versus conventional treatment with another material | |||
| ART material | Conventional treatment material | Outcomes | Effect estimate OR (95% CI) |
| H‐GIC | Amalgam | Restoration failure ‐primary teeth – 2 studies (Miranda 2005; Yu 2004). Studies reporting on single + multiple lesions | 2.15 (0.73 to 6.35); I2 = 0% |
| Pain (primary dentition) – 1 study (Miranda 2005). Studies reporting on single + multiple lesions | 1.44 (0.45 to 4.60) | ||
| GIC | Amalgam | Restoration failure ‐ primary teeth – 1 study (Ling 2003). Studies reporting on lesion type: not reported | 0.78 (0.30 to 2.02) |
| Restoration failure ‐ permanent, immature teeth – 1 study (Estupiñan‐Day 2006). Studies reporting on lesion type: not reported | 1.71 (1.32 to 2.22) | ||
| Pain ‐ permanent, immature teeth (Estupiñan‐Day 2006) | 0.41 (0.35 to 0.47) | ||
| H‐GIC | Composite and local anaesthetic | Restoration failure ‐ primary teeth – 1 study (Luz 2012). Studies reporting on multiple lesions | 8.00 (1.24 to 51.48) |
| Pain (primary dentition) – 1 study (Luz 2012) | 2.22 (0.51 to 9.61) | ||
| H‐GIC | RM‐GIC and local anaesthetic | Restoration failure ‐ permanent, mature teeth – 2 studies (Da Mata 2015; Lo 2006). Studies reporting on coronal/root caries | 1.46 (0.74 to 2.88); I2 = 0% |
| CI: confidence interval; OR: odds ratio | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Restoration failure ‐ primary teeth ‐ longest follow‐up Show forest plot | 5 | Odds Ratio (Random, 95% CI) | 1.60 [1.13, 2.27] | |
| 1.1 Single and multiple cavity surfaces | 1 | Odds Ratio (Random, 95% CI) | 2.75 [0.50, 15.16] | |
| 1.2 Multiple cavity surfaces | 3 | Odds Ratio (Random, 95% CI) | 1.62 [1.03, 2.55] | |
| 1.3 Type of cavity surfaces not reported | 1 | Odds Ratio (Random, 95% CI) | 0.79 [0.12, 5.45] | |
| 2 Pain ‐ primary teeth Show forest plot | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐1.38, 0.07] |
| 3 Participant experience ‐ discomfort Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Restoration failure ‐ primary teeth ‐ longest follow‐up Show forest plot | 1 | Odds Ratio (Random, 95% CI) | Totals not selected | |
| 2 Participant experience ‐ dental anxiety Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Restoration failure ‐ permanent teeth ‐ longest follow‐up Show forest plot | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Secondary caries Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |

