De‐escalation of antimicrobial treatment for adults with sepsis, severe sepsis or septic shock
Referencias
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Intervention not of interest: single large iv dose (10 mg/kg) of gentamicin with a standard multiple dose regimen of gentamicin. | |
| Intervention not of interest, patients were randomized to:
The patients were not randomized to have an initial empirical and broad‐spectrum antimicrobial therapy, adjusted according to the culture results or clinical condition. | |
| Intervention not of interest: patients randomized to be monitored by inflammatory marker (procalcitonin) or control group. The patients were not randomized to have their antimicrobial therapy adjusted according to the culture results or clinical condition. Clinical condition out of area of interest: ICU patients with no obvious site of Infection. | |
| Interventions not of interest: routine sepsis work up versus intervention strategy with additional cytokine measurements. Clinical condition not of interest: paediatric patients. | |
| Interventions not of interest: procalcitonin measurements. Clinical condition out of area of interest: ICU patients. | |
| Intervention out of area of interest: participants with septic shock were randomized to have renally adjusted dosage of antibiotics. | |
| Interventions out of area of interest: intravenous immunoglobulin in combination therapy with antibiotics versus antibiotics monotherapy. | |
| Intervention out of area of interest: different daily doses of piperacillin‐tazobactam by bolus dosing or continuous infusion. | |
| Intervention out of area of interest, patients were randomized to:
| |
| Intervention not of interest (once‐daily versus twice‐daily administration of ceftazidime), clinical condition not of interest (preterm infants). | |
| Interventions out of area of interest: procaine penicillin intramuscularly (narrow‐spectrum antimicrobial) versus cefuroxime intravenously (broad‐spectrum antimicrobial) for 4 to 7 days. Clinical condition out of area of interest: common infections of childhood. |
ICU ‐ intensive care unit
iv ‐ intravenous
Characteristics of ongoing studies [ordered by study ID]
Ir a:
| Trial name or title | De‐escalation of Empirical Antimicrobial Therapy Study in Severe Sepsis |
| Methods | Open label randomized controlled trial |
| Participants |
|
| Interventions | 1. Experimental: a strategy based on de‐escalation intervention. Procedure: streamlining of the empirical antimicrobial therapy 2. Active comparator: a conservative strategy intervention. Procedure: continuation of the empirical antimicrobial therapy |
| Outcomes | |
| Starting date | October 2011 |
| Contact information | Marc Leone marc.leone@ap‐hm.fr |
| Notes |
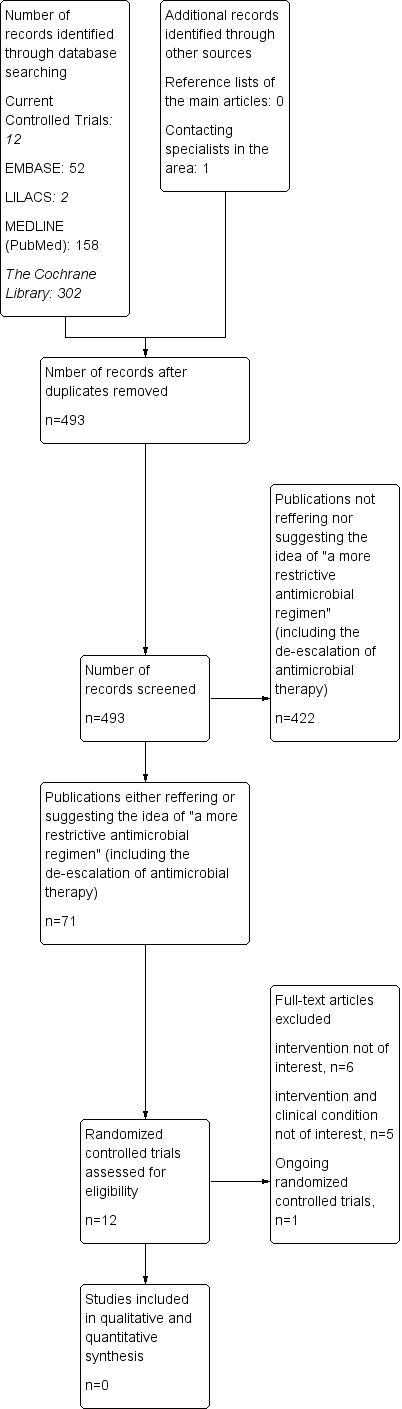
Study flow diagram.

A simplified patients' flow for future randomized controlled trials testing the de‐escalation of antimicrobial therapy for septic patients. Adapted with kind permission of David Moher from the figure in Moher 2005.

