Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections
Información
- DOI:
- https://doi.org/10.1002/14651858.CD007892.pub5Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 21 diciembre 2014see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Embarazo y parto
- Copyright:
-
- Copyright © 2014 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
All review authors helped develop the protocol, data extraction, and preparation of results and final report.
Sources of support
Internal sources
-
Indiana University School of Medicine, Indianapolis, USA.
External sources
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
There are no financial conflicts of interest to disclose. David Haas is the Principal Investigator for a randomized trial included in this review (Haas 2010). Sarah Morgan is also an investigator in the same trial. Trial authors were not involved in assessing trial quality or extracting data from the Haas 2010 study, this was carried out by the third review author, Karenrose Contreras and a third party (Dr Jon Hathaway, MD, PhD).
Acknowledgements
The authors thank Dr Jon Hathaway for his independent assessment of trial quality and data extraction for the Haas 2010 study and Erika Ota for preparing the 'Summary of findings' table.
Erika Ota's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors are responsible for the views expressed in this publication.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
We wish to thank Dr Ida Envall of Stockholm, who brought a trial to our attention that had been missed in our search methodology.
Version history
| Published | Title | Stage | Authors | Version |
| 2020 Apr 26 | Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections | Review | David M Haas, Sarah Morgan, Karenrose Contreras, Savannah Kimball | |
| 2018 Jul 17 | Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections | Review | David M Haas, Sarah Morgan, Karenrose Contreras, Savannah Enders | |
| 2014 Dec 21 | Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections | Review | David M Haas, Sarah Morgan, Karenrose Contreras | |
| 2014 Sep 09 | Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections | Review | David M Haas, Sarah Morgan, Karenrose Contreras | |
| 2013 Jan 31 | Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections | Review | David M Haas, Sarah Morgan, Karenrose Contreras | |
| 2010 Mar 17 | Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections | Review | David M Haas, Sarah Morgan Al Darei, Karenrose Contreras | |
| 2009 Jul 08 | Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections | Protocol | David M Haas, Sarah Al Darei, Karenrose Contreras | |
Differences between protocol and review
Three of the planned subgroup analyses were unable to be performed as they were not reported in the trials.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Administration, Intravaginal;
- Anti-Infective Agents, Local [*administration & dosage];
- Benzalkonium Compounds [administration & dosage];
- Cesarean Section [*adverse effects];
- Chlorhexidine [administration & dosage];
- Disinfection [*methods];
- Endometritis [*prevention & control];
- Fever [prevention & control];
- Povidone-Iodine [administration & dosage];
- Preoperative Care [*methods];
- Randomized Controlled Trials as Topic;
- Surgical Wound Infection [*prevention & control];
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICO
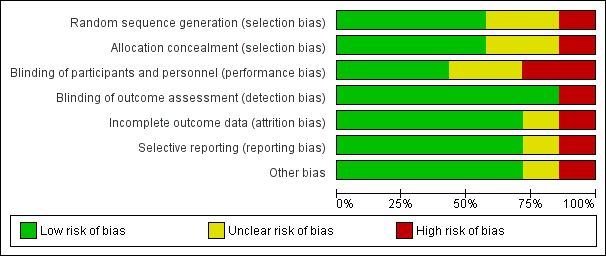
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Comparison 1 Vaginal preparation versus control, Outcome 1 Post‐cesarean endometritis.

Comparison 1 Vaginal preparation versus control, Outcome 2 Postoperative fever.
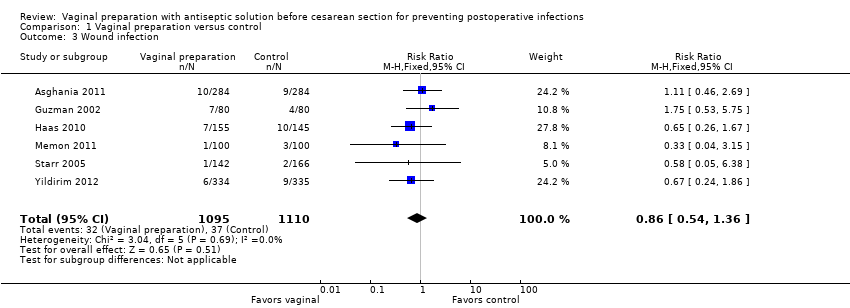
Comparison 1 Vaginal preparation versus control, Outcome 3 Wound infection.

Comparison 1 Vaginal preparation versus control, Outcome 4 Any wound complication.

Comparison 1 Vaginal preparation versus control, Outcome 5 Composite wound complication or endometritis.

Comparison 2 Vaginal preparation versus control ‐ stratified by presence of labor, Outcome 1 Post‐cesarean endometritis.

Comparison 2 Vaginal preparation versus control ‐ stratified by presence of labor, Outcome 2 Postoperative fever.

Comparison 2 Vaginal preparation versus control ‐ stratified by presence of labor, Outcome 3 Wound infection.
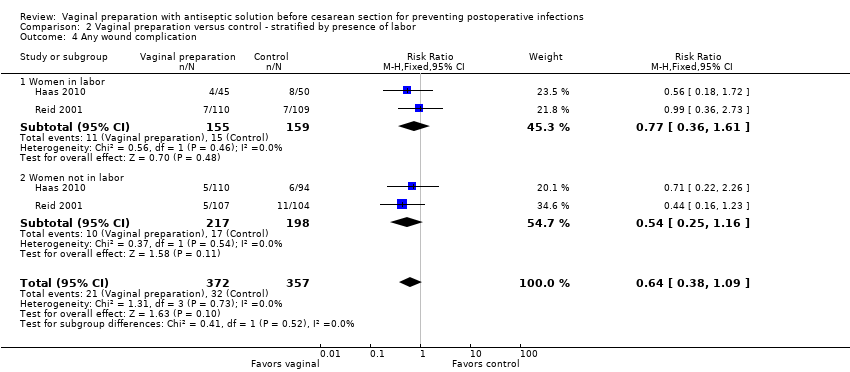
Comparison 2 Vaginal preparation versus control ‐ stratified by presence of labor, Outcome 4 Any wound complication.
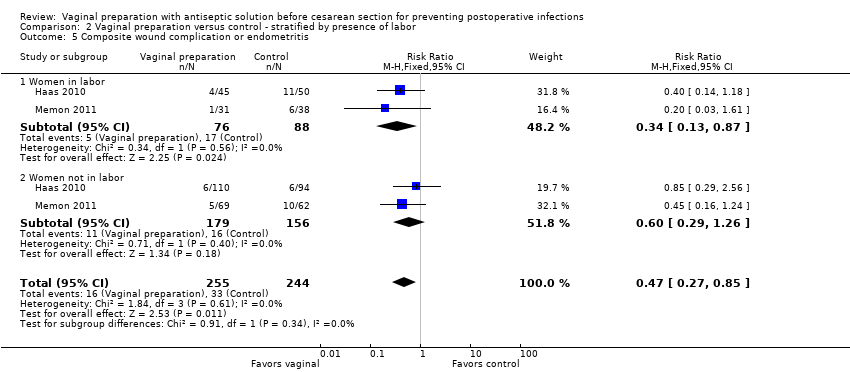
Comparison 2 Vaginal preparation versus control ‐ stratified by presence of labor, Outcome 5 Composite wound complication or endometritis.

Comparison 3 Vaginal preparation versus control ‐ stratified by presence of ruptured membranes, Outcome 1 Post‐cesarean endometritis.

Comparison 3 Vaginal preparation versus control ‐ stratified by presence of ruptured membranes, Outcome 2 Postoperative fever.

Comparison 3 Vaginal preparation versus control ‐ stratified by presence of ruptured membranes, Outcome 3 Wound infection.

Comparison 3 Vaginal preparation versus control ‐ stratified by presence of ruptured membranes, Outcome 4 Any wound complication.

Comparison 3 Vaginal preparation versus control ‐ stratified by presence of ruptured membranes, Outcome 5 Composite wound complication or endometritis.
| Vaginal preparation versus control for preventing postoperative infections | ||||||
| Population: Pregnant women who received a cesarean delivery | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Vaginal preparation versus control | |||||
| Post‐cesarean endometritis | Study population | RR 0.45 | 2635 | ⊕⊕⊝⊝ | ||
| 83 per 1000 | 37 per 1000 | |||||
| Moderate | ||||||
| 75 per 1000 | 34 per 1000 | |||||
| Postoperative fever | Study population | RR 0.9 | 2475 | ⊕⊕⊕⊝ | ||
| 141 per 1000 | 127 per 1000 | |||||
| Moderate | ||||||
| 117 per 1000 | 105 per 1000 | |||||
| Wound infection | Study population | RR 0.86 | 2205 | ⊕⊕⊝⊝ | ||
| 33 per 1000 | 29 per 1000 | |||||
| Moderate | ||||||
| 31 per 1000 | 27 per 1000 | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Most studies contributing data had design limitations. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Post‐cesarean endometritis Show forest plot | 7 | 2635 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.25, 0.81] |
| 2 Postoperative fever Show forest plot | 6 | 2475 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.74, 1.10] |
| 3 Wound infection Show forest plot | 6 | 2205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.54, 1.36] |
| 4 Any wound complication Show forest plot | 2 | 729 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.37, 1.07] |
| 5 Composite wound complication or endometritis Show forest plot | 2 | 499 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.26, 0.82] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Post‐cesarean endometritis Show forest plot | 3 | 1394 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.48, 1.02] |
| 1.1 Women in labor | 3 | 523 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.34, 0.95] |
| 1.2 Women not in labor | 3 | 871 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.52, 1.54] |
| 2 Postoperative fever Show forest plot | 2 | 965 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.59, 1.13] |
| 2.1 Women in labor | 2 | 307 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.42, 1.08] |
| 2.2 Women not in labor | 2 | 658 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.61, 1.49] |
| 3 Wound infection Show forest plot | 2 | 959 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.34, 1.34] |
| 3.1 Women in labor | 2 | 307 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.24, 2.21] |
| 3.2 Women not in labor | 2 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.27, 1.56] |
| 4 Any wound complication Show forest plot | 2 | 729 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.38, 1.09] |
| 4.1 Women in labor | 2 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.36, 1.61] |
| 4.2 Women not in labor | 2 | 415 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.25, 1.16] |
| 5 Composite wound complication or endometritis Show forest plot | 2 | 499 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.27, 0.85] |
| 5.1 Women in labor | 2 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.13, 0.87] |
| 5.2 Women not in labor | 2 | 335 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.29, 1.26] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Post‐cesarean endometritis Show forest plot | 3 | 1129 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.29, 0.70] |
| 1.1 Women with ruptured membranes | 3 | 272 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.10, 0.55] |
| 1.2 Women with intact membranes | 3 | 857 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.36, 1.06] |
| 2 Postoperative fever Show forest plot | 2 | 969 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.60, 1.14] |
| 2.1 Women with ruptured membranes | 2 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.34, 1.12] |
| 2.2 Women with intact membranes | 2 | 769 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.63, 1.36] |
| 3 Wound infection Show forest plot | 3 | 1129 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.49, 1.57] |
| 3.1 Women with ruptured membranes | 3 | 272 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.46, 3.20] |
| 3.2 Women with intact membranes | 3 | 857 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.35, 1.52] |
| 4 Any wound complication Show forest plot | 1 | 300 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.28, 1.44] |
| 4.1 Women with ruptured membranes | 1 | 76 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.15, 1.89] |
| 4.2 Women with intact membranes | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.25, 2.10] |
| 5 Composite wound complication or endometritis Show forest plot | 2 | 500 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.27, 0.85] |
| 5.1 Women with ruptured membranes | 2 | 134 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.13, 1.13] |
| 5.2 Women with intact membranes | 2 | 366 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.26, 1.04] |

