دمیدن هوای گرم شده با یا بدون مرطوب کردن آن در جراحی لاپاروسکوپی شکمی
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع مطالعات در انتظار ارزیابی
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Double‐blinded RCT | |
| Participants | n = 110, laparoscopic cholecystectomy; n = 40, laparoscopic fundoplication | |
| Interventions | Warmed, humidified CO2 vs standard CO2 | |
| Outcomes | Core temperature, postoperative pain, analgesic requirements, lens fogging, postoperative pain and the need for anaesthesia. In addition , OR time, hospitalisation, complications | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were assigned to 2 groups using a computer model post‐anaesthesia but the groups were 84 in standard CO2 and 66 in heated, humidified CO2 Comment: with computer‐generated randomisation, it would be unlikely for the groups to be this uneven |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was not clearly stated |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Only the surgical nurse knew the temperature of the CO2 feed." Comment: adequate blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Only the surgical nurse knew the temperature of the CO2 feed." Comment: adequate blinding |
| Incomplete outcome data (attrition bias) | Unclear risk | Outcome data was unclear, number of participants included in analysis was not reported |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Unclear risk | Originally published in Russian, the study authors had a certified translator translate it into English. However, the translation and the qualification certificate of the translator were provided voluntarily by a research scientist from a surgical humidification device company |
| Methods | RCT | |
| Participants | n = 26, prolonged (> 120 min) fundoplication, hernioplasty, resection of the sigmoid colon and rectopexy | |
| Interventions | Warmed, humidified CO2 vs standard CO2 | |
| Outcomes | Core temperature, cardiac index, urine output, recovery room opioid usage and pain score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) | Unclear risk | No description |
| Blinding of outcome assessment (detection bias) | Unclear risk | Only stated that the pain score was recorded by a trained nurse unaware of the temperature of the pneumoperitoneum |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry provided heating device |
| Methods | RCT | |
| Participants | n = 50, consecutive, morbidly obese, laparoscopic antecolic proximal Roux‐en‐Y gastric bypass surgery | |
| Interventions | Heated and humidified CO2 vs cold and dry CO2 | |
| Outcomes | Intraoperative core temperature, room temperature, litres of CO2 insufflation, operating time, number of lens cleanings, recovery room temperature, narcotics usage, length of hospitalisation, high‐sensitivity CRP at 24 h, abdominal and shoulder pain scores | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A blind draw by an impartial third party |
| Allocation concealment (selection bias) | Low risk | A draw was held to determine which type of insufflation was to be used on the first case, after which the insufflation method was alternated for the next 49 cases consecutively, with no interruption or exclusions. |
| Blinding of participants and personnel (performance bias) | Low risk | Single‐blind study where participants were blinded as they were anaesthetized but personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The nursing personnel, who were unaware of the study, recorded the subjective pain score." Comment: adequate blinding of outcome assessment |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | Blinded RCT | |
| Participants | n = 44, laparoscopic gastric bypass | |
| Interventions | Cold CO2 vs cold humidified CO2 vs heated CO2 vs heated humidified CO2 | |
| Outcomes | Core temperature, humidity, intraoperative urine output, lens fogging, recovery room time, length of hospital stay, postoperative pain, total morphine sulphate equivalent | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block fashion randomisation |
| Allocation concealment (selection bias) | Low risk | Results in sealed envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Single‐blind study where participants were blinded as they were anaesthetised but study personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Intraoperative outcomes were not blinded but they are objective measurements. Participants recorded postoperative pain and they remained blinded to their intervention. |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry funded research grant. |
| Methods | Double‐blinded RCT | |
| Participants | n = 40 women, diagnostic laparoscopy | |
| Interventions | Heated, humidified vs cold CO2 | |
| Outcomes | Shoulder pain, fentanyl use, percent requiring general anaesthetic, percent requiring intravenous sedation, amount of gas instilled before experiencing pain, operating time, recovery room time, time to recovery of shoulder pain | |
| Notes | This study presented outcomes as percentages of participants in each group (e.g. for operative time, percentage of participants in groups 0‐10 min, 10‐20 min, 20‐30 min, and 30‐40 min) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Low risk | Sealed envelope: "The circulating nurse opened a sealed envelope directing her to have the unit turned on or off during the procedure." |
| Blinding of participants and personnel (performance bias) | Low risk | Only the circulating nurse was not blinded: "To blind the surgeon further, the light on the unit could not be seen, and the plastic tubing was taped so the surgeon could not see condensation there." |
| Blinding of outcome assessment (detection bias) | Low risk | Only the circulating nurse was not blinded: "To blind the surgeon further, the light on the unit could not be seen, and the plastic tubing was taped so the surgeon could not see condensation there." |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Unclear risk | This study did not report any temperatures. |
| Other bias | Unclear risk | This study did not report any baseline demographics. |
| Methods | Double‐blinded RCT | |
| Participants | n = 117, laparoscopic cholecystectomy (16 excluded) | |
| Interventions | Heated, humidified CO2 vs cold CO2 | |
| Outcomes | Core temperature, lens fogging, postoperative pain, total morphine equivalents, hospital stay, return to baseline activity level | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer model randomisation |
| Allocation concealment (selection bias) | Low risk | Randomisation was done by surgical scrub nurse at the time of anaesthetic induction |
| Blinding of participants and personnel (performance bias) | Low risk | Participants, surgeons, operative and floor nurses, study co‐ordinators were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded when measuring intraoperative outcomes. Participants remained blinded when completing their pain scores. |
| Incomplete outcome data (attrition bias) | Low risk | 16 participants excluded from analysis due to 11 conversions to open, 3 requiring additional operations and 2 had the insufflation removed for technical reasons Comment: all excluded participants properly reported and not included in the analysis |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry provided heating device. |
| Methods | Double‐blinded RCT | |
| Participants | n = 50, laparoscopic gastric bypass (6 excluded) | |
| Interventions | Heated and humidified CO2 vs cold CO2 | |
| Outcomes | Core temperature, postoperatively tympanic temperature, pain score, shivering, morphine, nausea score, Aldrete recovery assessment score, hospital stay, lens fogging | |
| Notes | Warm blankets were used to cover the upper chest and arms in all control group participants for ethical considerations | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | An OR nurse was responsible for connecting the device |
| Blinding of participants and personnel (performance bias) | Low risk | Participants, surgeons, anaesthesiologist, data‐collecting personnel, recovery nurses were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Personnel collecting data were blinded and participants remained blinded when completing their verbal rating scales |
| Incomplete outcome data (attrition bias) | Low risk | 6 participants excluded from analysis (4 converted to open, 2 required rescuing with active warming for temperature < 34 °C) Comment: all excluded participants properly reported and not included in analysis |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry funded research grant. |
| Methods | Double‐blinded RCT | |
| Participants | n = 90 women, gynaecologic laparoscopic surgery (53 with data) | |
| Interventions | Humidified heated CO2 vs heated dry CO2 vs cold dry CO2 | |
| Outcomes | Analgesic requirements and postoperative pain | |
| Notes | The trial was stopped following enrolment of 53 participants because of a tendency toward less pain and higher postoperative satisfaction in control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants, data analyst and interviewer were blinded to randomisation. However, no description of blinding of other participants (surgeon and nurses) |
| Blinding of outcome assessment (detection bias) | Unclear risk | No description of blinding of outcomes assessors |
| Incomplete outcome data (attrition bias) | Unclear risk | Trial was stopped early for there was a tendency toward less pain and higher postoperative satisfaction in participants in the control group |
| Selective reporting (reporting bias) | Unclear risk | Out of 90 participants, data only available on 53 participants |
| Other bias | Low risk | Industry provided heating device. |
| Methods | Double‐blinded RCT | |
| Participants | n = 148, laparoscopic cholecystectomy | |
| Interventions | Warmed, humidified CO2 vs standard CO2 | |
| Outcomes | Core temperature, postoperative pain, time of first bowel movement after surgery | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was unclear and treatment groups were uneven (67 received heated, humidified CO2 and 81 received standard CO2) Comment: randomisation likely not properly done |
| Allocation concealment (selection bias) | Low risk | Quote: "The secretary was privy to which method of gas was being used. The secretary opened a sealed opaque envelope to randomly allocate the procedure." |
| Blinding of participants and personnel (performance bias) | Low risk | The participants, surgeons, nurses, and study co‐ordinator were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | The nurses recording intraoperative outcomes were blinded. Participants remained blinded when recording their visual analogue pain scales. |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | RCT | |
| Participants | n = 30, gastrectomy, colectomy or low‐anterior resection | |
| Interventions | Heated CO2 vs room temperature CO2 | |
| Outcomes | Acid‐base parameters, ETCO2, and core temperature | |
| Notes | An upper body blanket was applied to all participants and if their temperature fell below 35 °C, a Bair Hugger forced air warmer and a warming mattress with circulating water at 38 °C were applied | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | No description in the article. Contacted study authors and they indicated that a random number table was used |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes were used |
| Blinding of participants and personnel (performance bias) | Low risk | No description but contacted study authors and they indicated that this was a blinded study |
| Blinding of outcome assessment (detection bias) | Low risk | No description but contacted study authors and they indicated that this was a blinded study |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | RCT | |
| Participants | n = 60 women, gynaecologic laparoscopic surgery | |
| Interventions | Heated humidified CO2 vs cold dry CO2 | |
| Outcomes | Core temperature, analgesic usage, postoperative pain, postoperative nausea and recovery room time | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator |
| Allocation concealment (selection bias) | Low risk | Sealed in sequential opaque envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | All nursing staff were blinded and patient was blinded as they were anaesthetised |
| Blinding of outcome assessment (detection bias) | Low risk | Nurses recording outcome data were blinded. Participants remained blinded when nurses administered visual analogue scales. |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry provided heating device. |
| Methods | RCT | |
| Participants | n = 40, laparoscopic cholecystectomy (8 excluded) | |
| Interventions | Heated, humidified CO2 vs cold CO2 | |
| Outcomes | Core temperature change, postoperative pain score, morphine usage | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) | Unclear risk | No description |
| Blinding of outcome assessment (detection bias) | Unclear risk | No description |
| Incomplete outcome data (attrition bias) | Low risk | 8 participants excluded due to conversion to open, pancreatitis or postoperative haematoma Comment: all excluded participants properly reported and not included in the analysis |
| Selective reporting (reporting bias) | Low risk | Data were available on 32 out of 40 participants and the reason was given by the study author. |
| Other bias | Low risk | Industry offered assistance for research. |
| Methods | Double‐blinded RCT | |
| Participants | n = 40 women, laparoscopic hysterectomy (3 excluded) | |
| Interventions | Heated CO2 vs cold CO2 | |
| Outcomes | Tympanic temperature, heart rate variability | |
| Notes | Data on 37 women were analysed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) | Unclear risk | No description on which personnel were blinded during operation |
| Blinding of outcome assessment (detection bias) | Low risk | Participants and staff in the postoperation care unit and ward were blinded. Intraoperative outcomes are objective so non‐blinding likely has less effect |
| Incomplete outcome data (attrition bias) | Unclear risk | 3 excluded participants, 2 "did not fulfil the study protocol" and 1 "because of surgical problems." Comment: unclear reasons for exclusion |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry provided heating device. |
| Methods | RCT | |
| Participants | n = 20, laparoscopic Nissen fundoplication | |
| Interventions | Heated and humidified CO2 vs cold CO2 | |
| Outcomes | Core temperature, pain score, morphine consumption, urine output, lens fogging | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Intraoperative randomisation |
| Blinding of participants and personnel (performance bias) | Low risk | Single‐blinded study where the participants were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Intraoperative outcomes were not blinded but they are objective measurements. Participants recorded postoperative pain and they remained blinded to their intervention |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | Multi‐centre RCT | |
| Participants | n = 72 women, laparoscopic gynaecologic surgery (50 with data) | |
| Interventions | Heated and humidified CO2 vs cold CO2 | |
| Outcomes | Postoperative pain and recovery room length of stay | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) | Unclear risk | No description |
| Blinding of outcome assessment (detection bias) | Unclear risk | No description |
| Incomplete outcome data (attrition bias) | High risk | Data were only available on 50 out of 72 participants and no reason was given. Some data was extracted from a different systematic review (Sammour 2008) as the original trial did not present all data. |
| Selective reporting (reporting bias) | Unclear risk | Data were only available on 50 out of 72 participants and no reason was given. |
| Other bias | Unclear risk | This study did not separate baseline demographics between groups. Industry provided heating device. |
| Methods | RCT | |
| Participants | n = 30, laparoscopic cholecystectomy | |
| Interventions | Warmed CO2 vs cold CO2 | |
| Outcomes | Core temperature, intraperitoneal cytokines, pain score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) | Unclear risk | No description |
| Blinding of outcome assessment (detection bias) | Unclear risk | No description |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | RCT | |
| Participants | n = 20, laparoscopic cholecystectomy | |
| Interventions | Heated CO2 vs cold CO2 | |
| Outcomes | Core temperature, intra‐abdominal temperature, postoperative pain, analgesics consumption | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and ward nurses were blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Participants remained blinded when assessing postoperative pain. Unclear if operating room nurses were blinded during measurement of outcomes |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry provided heating device. |
| Methods | Multi‐centre RCT | |
| Participants | n = 82, laparoscopic colonic surgery (8 excluded) | |
| Interventions | Heated humidified CO2 vs cold CO2 | |
| Outcomes | Postoperative pain, intraoperative core temperature, camera fogging, morphine‐equivalent usage, postoperative parameters | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Low risk | Allocations were concealed in opaque numbered envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Participants, investigators, surgeon and medical care staff were all blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Participants, investigators, surgeon and medical care staff were all blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Eight excluded after randomisation with clearly stated rationale Comment: all excluded participants properly reported and not included in the analysis |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | Blinded RCT | |
| Participants | n = 30, laparoscopic gastric bypass | |
| Interventions | Heated humidified CO2 vs cold CO2 | |
| Outcomes | Postoperative pain score, morphine consumption, OR time, core temperature, hospital stay | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | Participants randomised at the time of enrolment |
| Blinding of participants and personnel (performance bias) | Low risk | All clinicians except 1 author were blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | All clinicians except 1 author were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the study and there were no treatment withdrawals, no trial group changes and no major adverse events. |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | Double‐blinded RCT | |
| Participants | n = 108, laparoscopic cholecystectomy, fundoplication or Heller's myotomy (8 excluded) | |
| Interventions | Heated CO2 vs unheated CO2 | |
| Outcomes | Postoperative pain, core temperature, morphine consumption, nausea and vomiting, hospital stay, length of postoperative Ileus | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table in sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes opened in the operating room |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and nurses were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Nurses were blinded when collecting outcome data. Participants remained blinded when assessing postoperative pain. |
| Incomplete outcome data (attrition bias) | Low risk | 8 participants excluded (4 conversion to open, 2 postoperative biliary collections, 1 technical problems with insufflator, 1 refused) Comment: all excluded participants properly reported and not included in the analysis |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
| Methods | Blinded RCT | |
| Participants | n = 41, laparoscopic fundoplication (1 excluded) | |
| Interventions | Heated CO2 vs cold CO2 | |
| Outcomes | Core temperature, postoperative pain, analgesic requirement, postoperative recovery | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Surgeons, anaesthetist, data analyst, participants and ward nurses were blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Surgeons, anaesthetist, data analyst, participants and ward nurses were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | One participant excluded for missing postoperative pain scores and one underwent repeat laparotomy. Comment: all excluded participants properly reported and not included in the analysis |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | Industry provided heating device. |
| Methods | Double‐blinded RCT | |
| Participants | n = 195 adolescents, laparoscopic appendectomy (5 excluded) | |
| Interventions | Warm, humidified CO2 vs standard CO2 | |
| Outcomes | Opioid usage, pain score, core temperature, postoperative recovery and return to normal activities | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Online random number programme |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque, numbered envelopes were used |
| Blinding of participants and personnel (performance bias) | Low risk | Only one rotating scrub nurse assisted with randomisation. All other participants were blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Only one rotating scrub nurse assisted with randomisation. All other participants were blinded |
| Incomplete outcome data (attrition bias) | Low risk | 5 participants excluded after randomisation for major protocol violation Comment: all excluded participants properly reported and not included in the analysis |
| Selective reporting (reporting bias) | Low risk | We judged this trial free of selective reporting. |
| Other bias | Low risk | We did not detect any other potential bias. |
CO2: carbon dioxide
ETCO2: end tidal carbon dioxide
VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not a RCT | |
| Intervention was heated dry CO2 vs heated humidified CO2 | |
| Intervention was heated dry CO2 vs heated humidified CO2 | |
| Not primarily a laparoscopic abdominal surgery (laparoscopic‐assisted vaginal hysterectomy) | |
| Not a RCT | |
| Not a laparoscopic abdominal procedure (thoracoscopic) | |
| Not a RCT | |
| Different intervention: underbody warming system | |
| This study was only presented as a poster and no published paper was found | |
| Published as an abstract only, study authors contacted for data. No response | |
| Published as an abstract only, authors contacted for data. No response | |
| Not a RCT |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | n = 101, minimally‐invasive colon resection |
| Interventions | Warmed, humidified CO2 vs standard CO2 |
| Outcomes | Core temperature, postoperative pain, analgesic requirements, length of stay, time to first flatus, and tolerance of solids |
| Notes | Recently published abstract awaiting classification |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in core temperature Show forest plot | 19 | 1100 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.06, 0.36] |
| Analysis 1.1  Comparison 1 Core temperature (ºC), Outcome 1 Change in core temperature. | ||||
| 1.1 Heated, humidified vs cold | 14 | 885 | Mean Difference (IV, Random, 95% CI) | 0.31 [0.09, 0.53] |
| 1.2 Heated only vs cold | 7 | 215 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.16, 0.20] |
| 2 Change in core temperature for low risk of bias studies Show forest plot | 10 | 653 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.01, 0.33] |
| Analysis 1.2 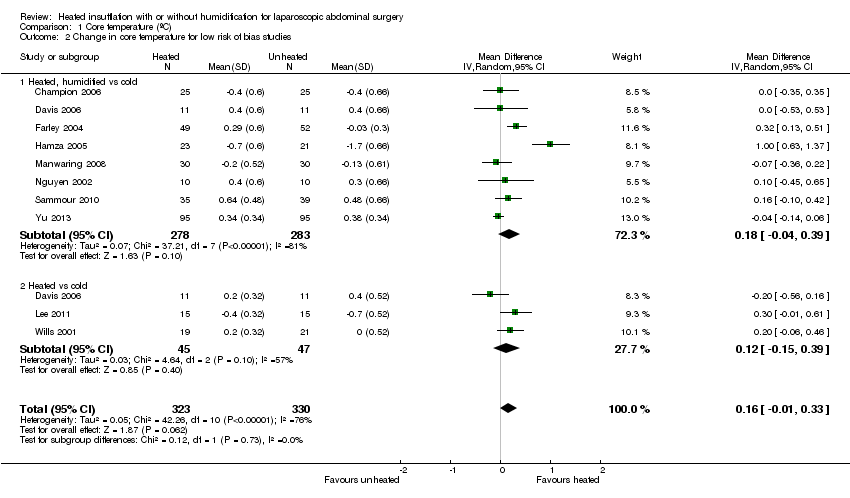 Comparison 1 Core temperature (ºC), Outcome 2 Change in core temperature for low risk of bias studies. | ||||
| 2.1 Heated, humidified vs cold | 8 | 561 | Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.04, 0.39] |
| 2.2 Heated vs cold | 3 | 92 | Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.15, 0.39] |
| 3 Change in core temperature for operations > 120 Minutes Show forest plot | 4 | 194 | Mean Difference (IV, Random, 95% CI) | 0.70 [0.10, 1.30] |
| Analysis 1.3 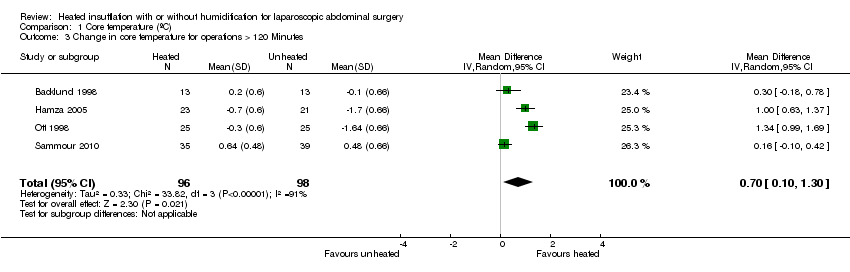 Comparison 1 Core temperature (ºC), Outcome 3 Change in core temperature for operations > 120 Minutes. | ||||
| 4 Change in core temperature with external warming Show forest plot | 8 | 545 | Mean Difference (IV, Random, 95% CI) | 0.29 [0.05, 0.52] |
| Analysis 1.4  Comparison 1 Core temperature (ºC), Outcome 4 Change in core temperature with external warming. | ||||
| 5 Change in temperature without external warming Show forest plot | 6 | 340 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.11, 0.75] |
| Analysis 1.5  Comparison 1 Core temperature (ºC), Outcome 5 Change in temperature without external warming. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Day 1 pain score Show forest plot | 14 | 991 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.42, 0.34] |
| Analysis 2.1  Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 1 Day 1 pain score. | ||||
| 1.1 Heated, humidified vs cold (abdominal) | 10 | 670 | Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.60, 0.33] |
| 1.2 Heated, humidified vs cold (shoulder) | 3 | 171 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.75, 1.05] |
| 1.3 Heated vs cold | 3 | 150 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐0.11, 1.12] |
| 2 Day 1 pain score for low risk of bias studies Show forest plot | 7 | 570 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.21, 0.55] |
| Analysis 2.2  Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 2 Day 1 pain score for low risk of bias studies. | ||||
| 2.1 Heated, humidified vs cold (abdominal) | 7 | 460 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.29, 0.63] |
| 2.2 Heated, humidified vs cold (shoulder) | 2 | 110 | Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.81, 1.31] |
| 3 Day 2 pain score Show forest plot | 10 | 695 | Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.78, 0.21] |
| Analysis 2.3 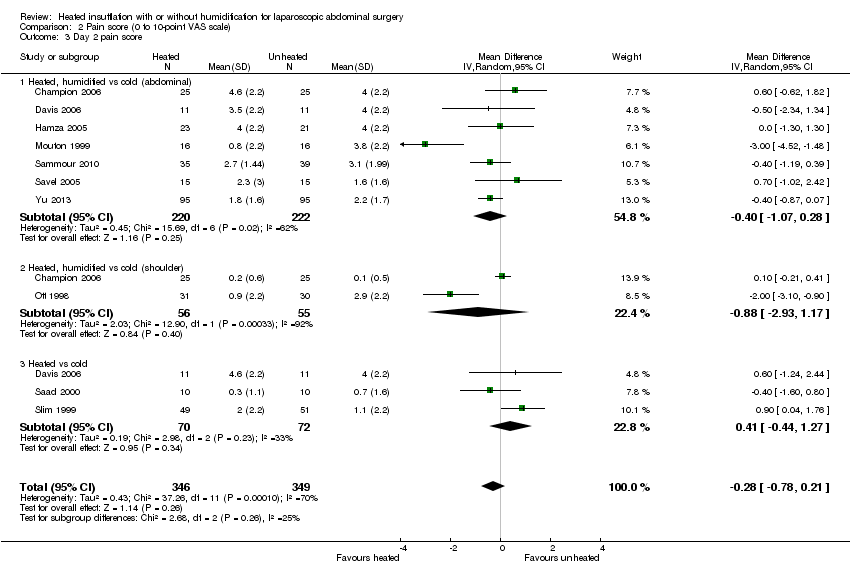 Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 3 Day 2 pain score. | ||||
| 3.1 Heated, humidified vs cold (abdominal) | 7 | 442 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.07, 0.28] |
| 3.2 Heated, humidified vs cold (shoulder) | 2 | 111 | Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐2.93, 1.17] |
| 3.3 Heated vs cold | 3 | 142 | Mean Difference (IV, Random, 95% CI) | 0.41 [‐0.44, 1.27] |
| 4 Day 2 pain score of low risk of bias studies Show forest plot | 5 | 380 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.65, 0.07] |
| Analysis 2.4  Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 4 Day 2 pain score of low risk of bias studies. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
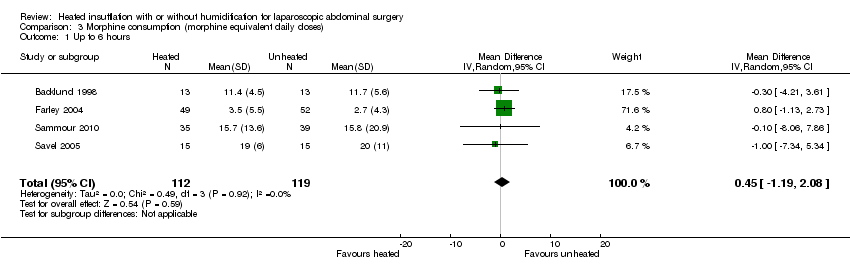
| 1 Up to 6 hours Show forest plot | 4 | 231 | Mean Difference (IV, Random, 95% CI) | 0.45 [‐1.19, 2.08] |
| Analysis 3.1 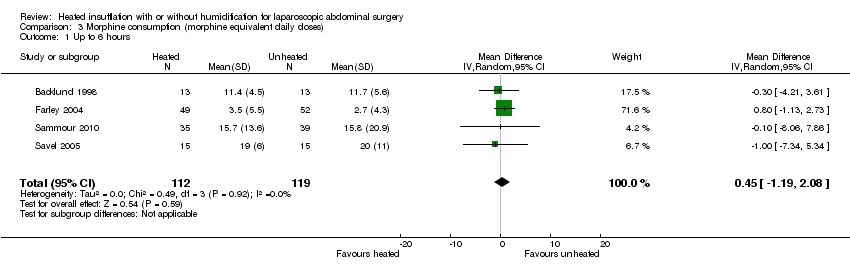 Comparison 3 Morphine consumption (morphine equivalent daily doses), Outcome 1 Up to 6 hours. | ||||
| 2 Day 1 morphine Show forest plot | 9 | 573 | Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐4.48, 3.20] |
| Analysis 3.2 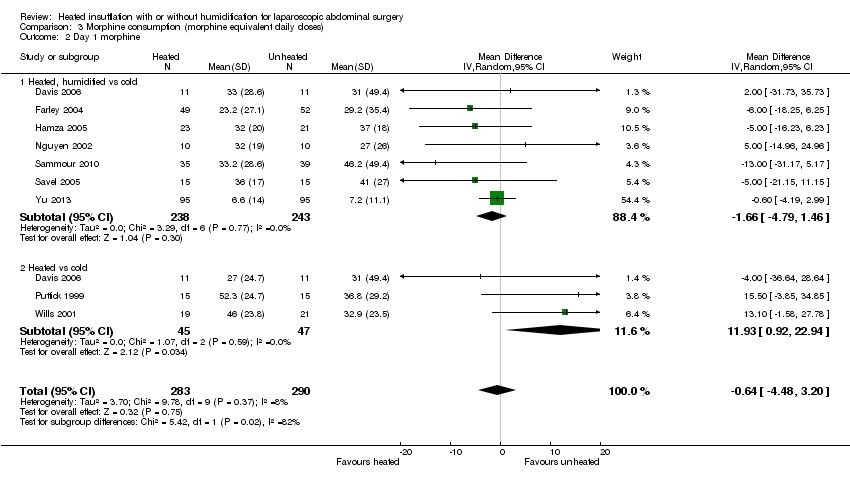 Comparison 3 Morphine consumption (morphine equivalent daily doses), Outcome 2 Day 1 morphine. | ||||
| 2.1 Heated, humidified vs cold | 7 | 481 | Mean Difference (IV, Random, 95% CI) | ‐1.66 [‐4.79, 1.46] |
| 2.2 Heated vs cold | 3 | 92 | Mean Difference (IV, Random, 95% CI) | 11.93 [0.92, 22.94] |
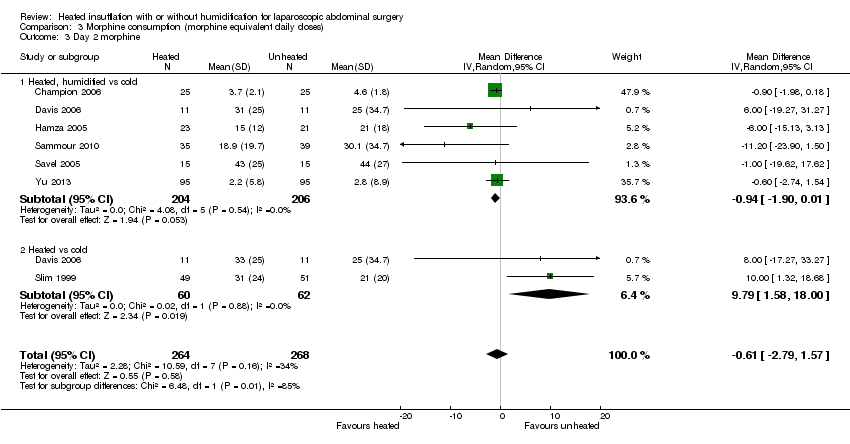
| 3 Day 2 morphine Show forest plot | 7 | 532 | Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐2.79, 1.57] |
| Analysis 3.3  Comparison 3 Morphine consumption (morphine equivalent daily doses), Outcome 3 Day 2 morphine. | ||||
| 3.1 Heated, humidified vs cold | 6 | 410 | Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.90, 0.01] |
| 3.2 Heated vs cold | 2 | 122 | Mean Difference (IV, Random, 95% CI) | 9.79 [1.58, 18.00] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
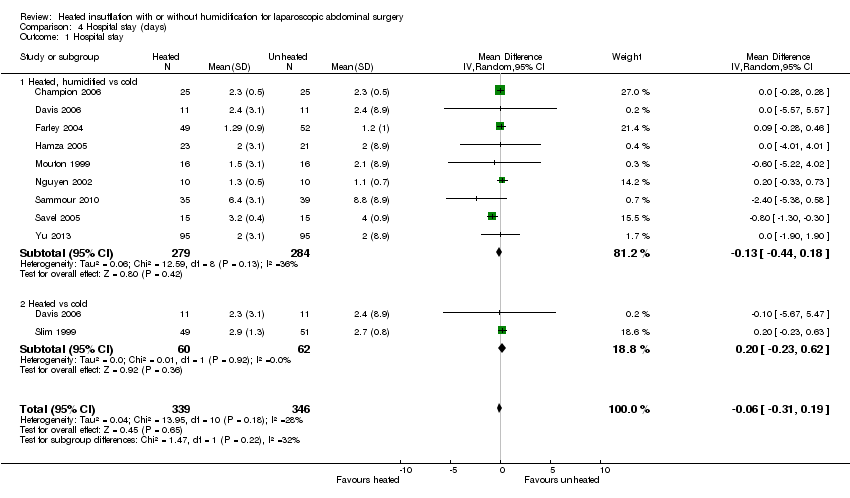
| 1 Hospital stay Show forest plot | 10 | 685 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.31, 0.19] |
| Analysis 4.1  Comparison 4 Hospital stay (days), Outcome 1 Hospital stay. | ||||
| 1.1 Heated, humidified vs cold | 9 | 563 | Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.44, 0.18] |
| 1.2 Heated vs cold | 2 | 122 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.23, 0.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recovery time Show forest plot | 6 | 327 | Mean Difference (IV, Random, 95% CI) | ‐26.79 [‐51.34, ‐2.25] |
| Analysis 5.1  Comparison 5 Recovery room stay (minutes), Outcome 1 Recovery time. | ||||
| 2 Recovery time for low risk of bias studies Show forest plot | 5 | 277 | Mean Difference (IV, Random, 95% CI) | ‐1.22 [‐6.62, 4.17] |
| Analysis 5.2  Comparison 5 Recovery room stay (minutes), Outcome 2 Recovery time for low risk of bias studies. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Times cleaned Show forest plot | 7 | 341 | Mean Difference (IV, Random, 95% CI) | 0.73 [‐0.32, 1.77] |
| Analysis 6.1 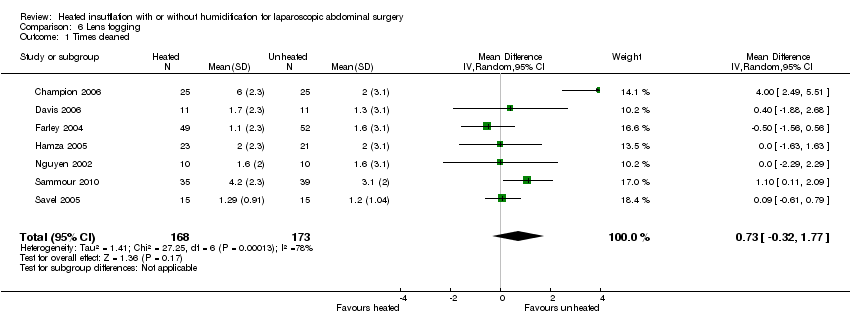 Comparison 6 Lens fogging, Outcome 1 Times cleaned. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative time Show forest plot | 20 | 1318 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐3.91, 3.04] |
| Analysis 7.1 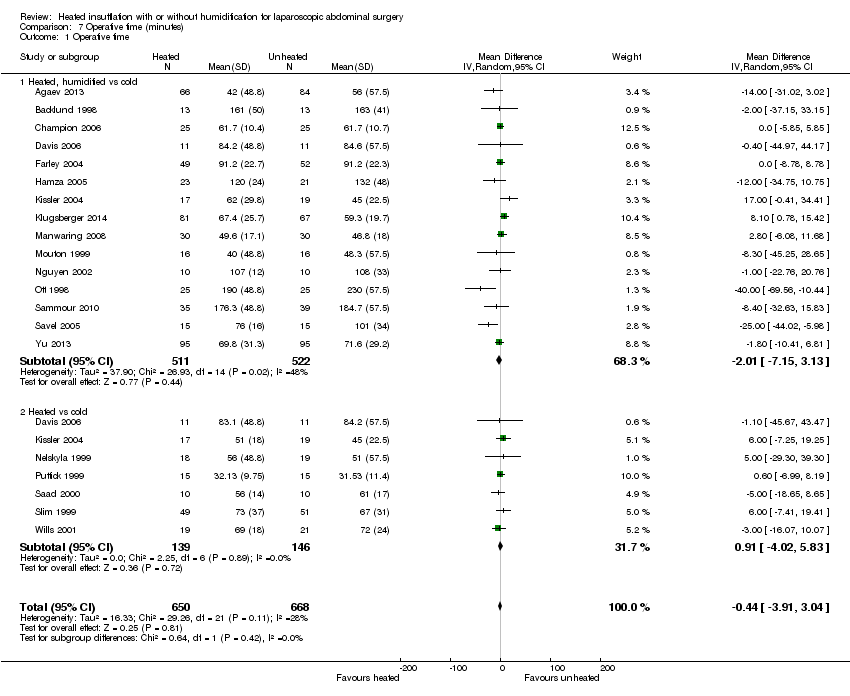 Comparison 7 Operative time (minutes), Outcome 1 Operative time. | ||||
| 1.1 Heated, humidified vs cold | 15 | 1033 | Mean Difference (IV, Random, 95% CI) | ‐2.01 [‐7.15, 3.13] |
| 1.2 Heated vs cold | 7 | 285 | Mean Difference (IV, Random, 95% CI) | 0.91 [‐4.02, 5.83] |
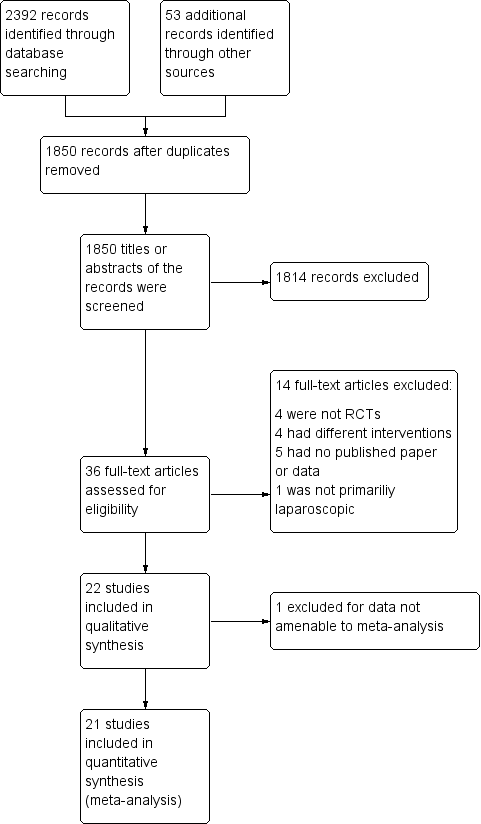
Study flow diagram

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study

Forest plot of comparison: 2 Core temperature, outcome: 2.1 Change in core temperature

Forest plot of comparison: 2 Core temperature, outcome: 2.2 Change in core temperature for low risk of bias studies
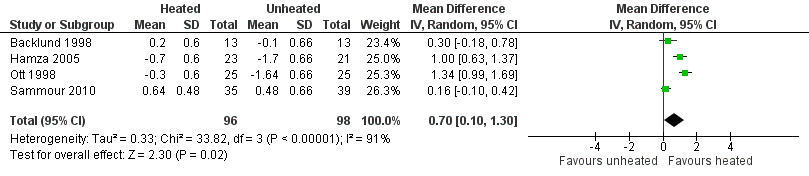
Forest plot of comparison: 1 Core temperature, outcome: 1.5 Change in core temperature in heated, humidified vs cold groups with OR > 120 Minutes

Forest plot of comparison: 2 Core temperature, outcome: 2.3 Change in core temperature in heated, humidified vs cold groups with external warming

Forest plot of comparison: 1 Core temperature, outcome: 1.4 Change in temperature in heated, humidified vs cold groups without external warming

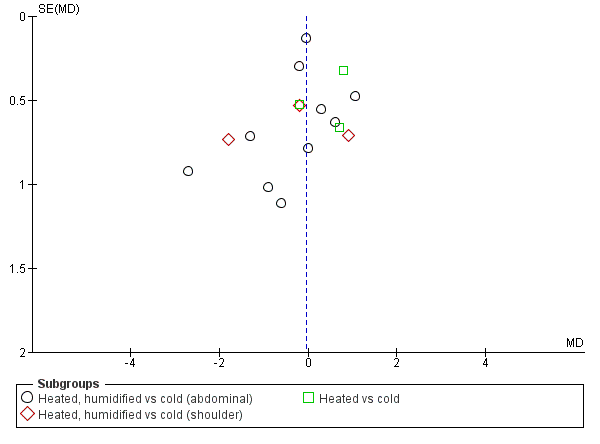
Forest plot of comparison: 1 Pain score, outcome: 1.1 Day 1 pain score

Forest plot of comparison: 1 Pain score, outcome: 1.3 Day 1 pain score for low risk of bias study
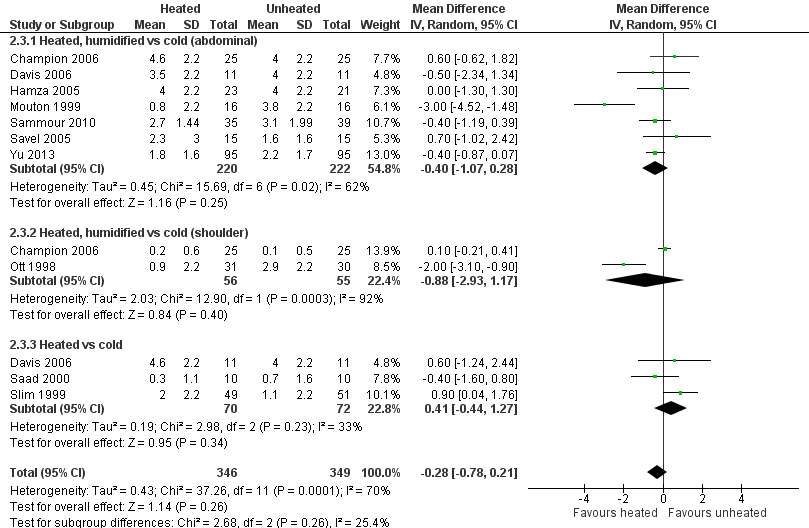
Forest plot of comparison: 1 Pain score, outcome: 1.2 Day 2 pain score

Forest plot of comparison: 1 Pain score, outcome: 1.4 Day 2 pain score of low risk of bias studies

Forest plot of comparison: 3 Morphine consumption, outcome: 3.1 Up to 6 hours
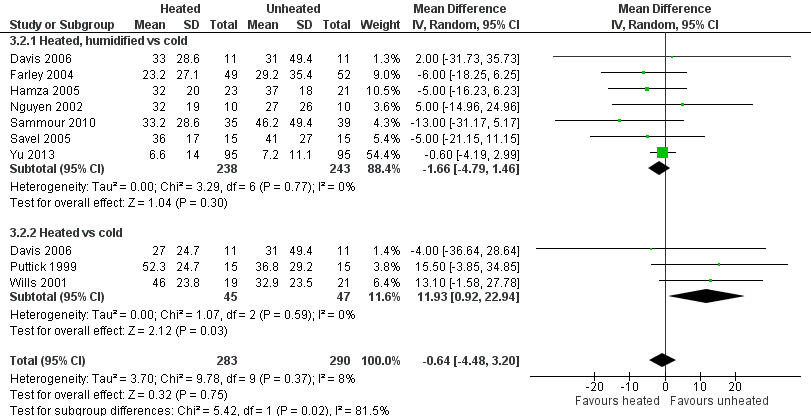
Forest plot of comparison: 3 Morphine consumption, outcome: 3.2 Day 1 morphine

Forest plot of comparison: 3 Morphine consumption, outcome: 3.3 Day 2 morphine
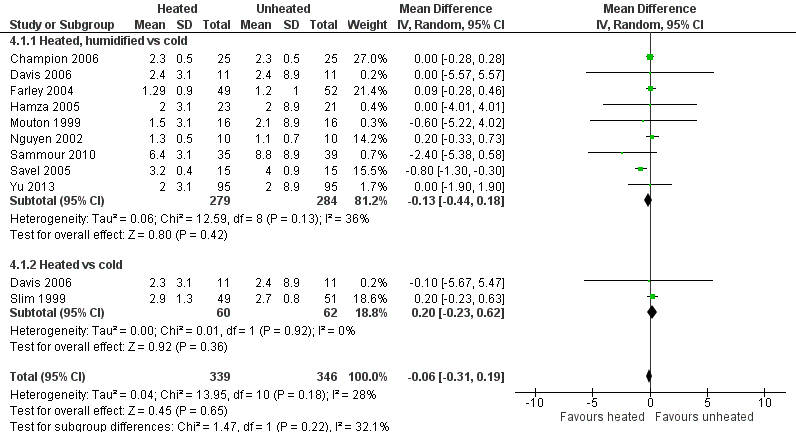
Forest plot of comparison: 4 Hospital stay, outcome: 4.1 Hospital stay

Forest plot of comparison: 7 Recovery room stay, outcome: 7.1 Recovery time

Forest plot of comparison: 7 Recovery room stay, outcome: 7.2 Recovery time for low risk of bias studies

Forest plot of comparison: 5 Lens fogging, outcome: 5.1 Lens fogging

Forest plot of comparison: 6 Operative time, outcome: 6.1 Operative time

Funnel plot of comparison: 2 Core temperature, outcome: 2.1 Change in core temperature
Funnel plot of comparison: 1 Pain Score, outcome: 1.1 Day 1 pain score

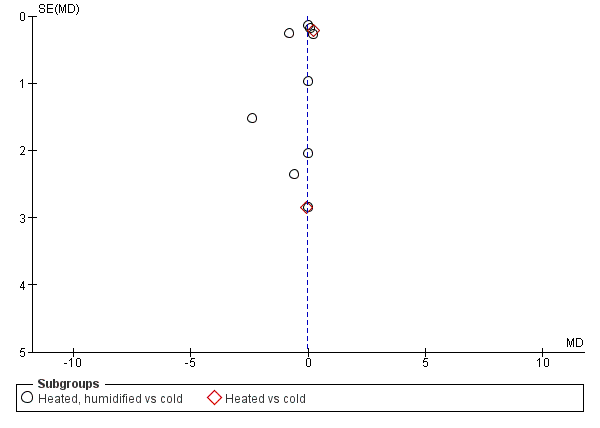
Funnel plot of comparison: 3 Morphine consumption, outcome: 3.2 Day 1 morphine
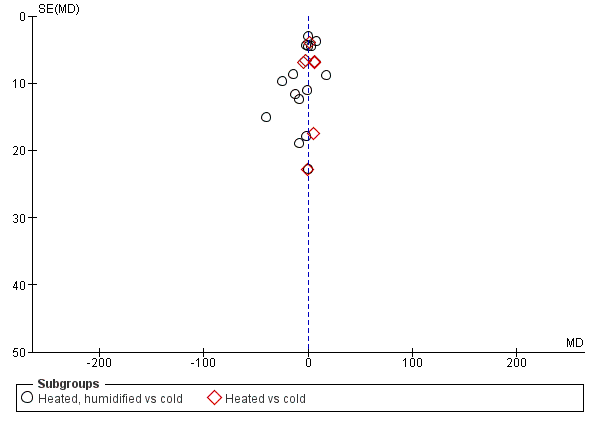
Funnel plot of comparison: 4 Hospital stay, outcome: 4.1 Hospital stay
Funnel plot of comparison: 6 Operative time, outcome: 6.1 Operative time
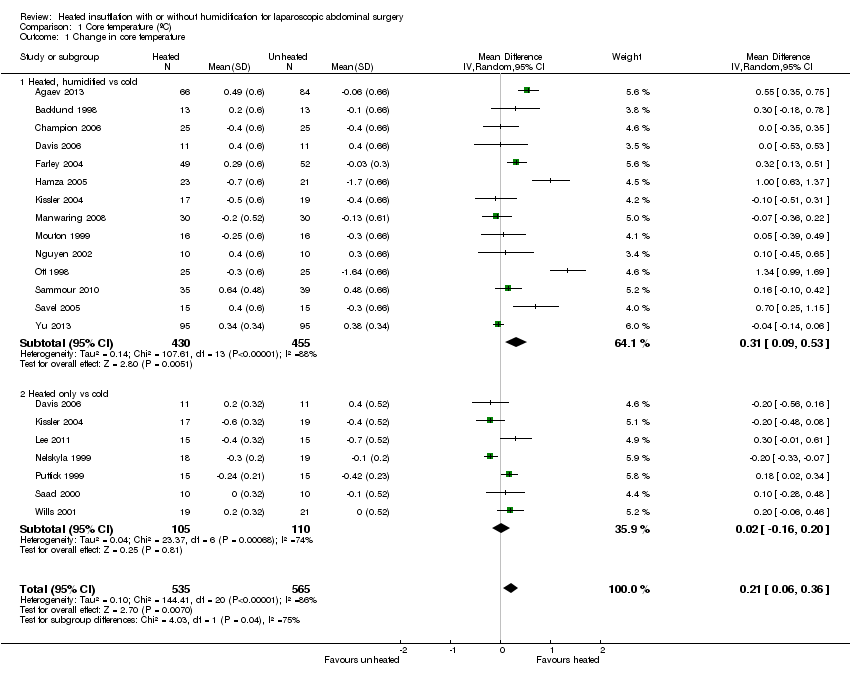
Comparison 1 Core temperature (ºC), Outcome 1 Change in core temperature.

Comparison 1 Core temperature (ºC), Outcome 2 Change in core temperature for low risk of bias studies.
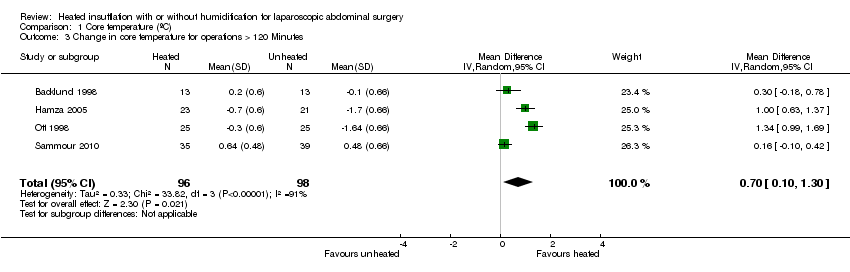
Comparison 1 Core temperature (ºC), Outcome 3 Change in core temperature for operations > 120 Minutes.

Comparison 1 Core temperature (ºC), Outcome 4 Change in core temperature with external warming.
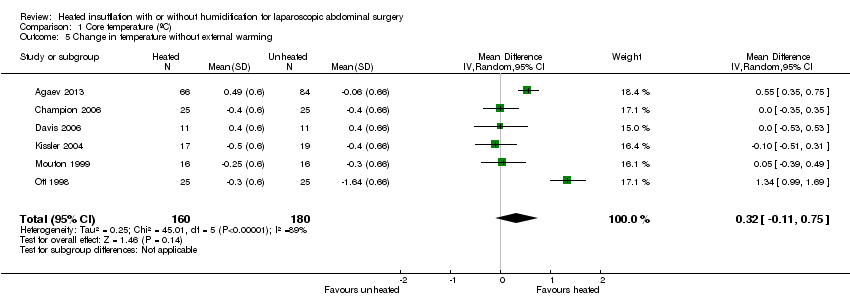
Comparison 1 Core temperature (ºC), Outcome 5 Change in temperature without external warming.

Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 1 Day 1 pain score.
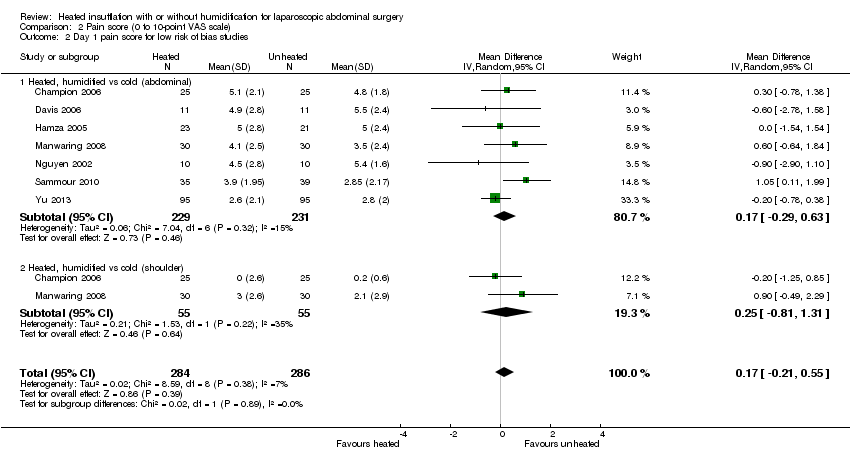
Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 2 Day 1 pain score for low risk of bias studies.

Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 3 Day 2 pain score.
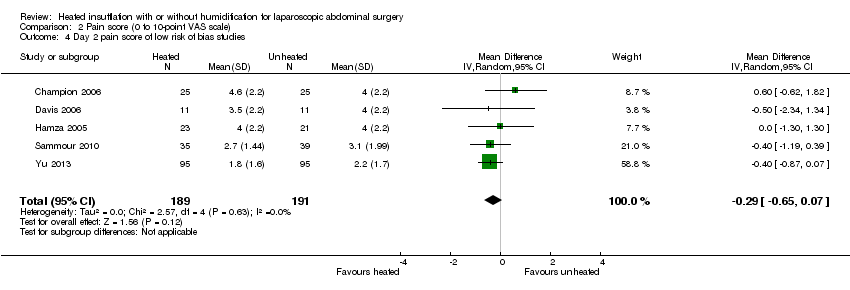
Comparison 2 Pain score (0 to 10‐point VAS scale), Outcome 4 Day 2 pain score of low risk of bias studies.
Comparison 3 Morphine consumption (morphine equivalent daily doses), Outcome 1 Up to 6 hours.

Comparison 3 Morphine consumption (morphine equivalent daily doses), Outcome 2 Day 1 morphine.
Comparison 3 Morphine consumption (morphine equivalent daily doses), Outcome 3 Day 2 morphine.
Comparison 4 Hospital stay (days), Outcome 1 Hospital stay.

Comparison 5 Recovery room stay (minutes), Outcome 1 Recovery time.

Comparison 5 Recovery room stay (minutes), Outcome 2 Recovery time for low risk of bias studies.

Comparison 6 Lens fogging, Outcome 1 Times cleaned.

Comparison 7 Operative time (minutes), Outcome 1 Operative time.
| Heated CO2 with or without humidification for laparoscopic abdominal surgery | |||||
| Patient or population: Laparoscopic abdominal surgery (core temperature) | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Quality of the evidence | Comments | |
| Risk with cold gas | Risk with heated gas | ||||
| Change in core temperature (ºC) | The mean change in core temperature was ‐0.22 °C | The mean change in core temperature in the intervention group was 0.21 °C higher (0.06 to 0.36) | 1100 | ⨁⨁◯◯ | Negative temperature indicates core temperature dropped during surgery |
| Change in core temperature: heated, humidified vs cold | The mean change in core temperature: heated, humidified vs cold was ‐0.25 °C | The mean change in core temperature: heated, humidified vs cold in the intervention group was 0.31 °C higher (0.09 to 0.53) | 885 | ⨁⨁◯◯ | |
| Change in core temperature: heated only vs cold | The mean change in core temperature: heated vs cold was ‐0.19 °C | The mean change in core temperature: heated vs cold in the intervention group was 0.02 °C higher (‐0.16 to 0.20) | 215 | ⨁⨁◯◯ | |
| Change in core temperature for known low risk of bias studies | The mean change in core temperature for low risk of bias studies was ‐0.10 °C | The mean change in core temperature for low risk of bias studies in the intervention group was 0.16 °C higher (‐0.01 to 0.33) | 653 | ⨁⨁⨁◯ | |
| Change in core temperature for known low risk of bias studies: heated, humidified vs cold | The mean change in core temperature for low risk of bias studies: heated, humidified vs cold was ‐0.09 °C | The mean change in core temperature for low risk of bias studies: heated, humidified vs cold in the intervention group was 0.18 °C higher (‐0.04 to 0.39) | 561 | ⨁⨁⨁◯ | |
| Change in core temperature for low risk of bias studies: heated only vs cold | The mean change in core temperature for low risk of bias studies: heated vs cold was ‐0.10 °C | The mean change in core temperature for low risk of bias studies: heated vs cold in the intervention group was 0.12 °C higher (‐0.15 to 0.39) | 92 | ⨁⨁⨁◯ | |
| Change in core temperature with external warming | The mean change in core temperature with external warming was ‐0.14 °C | The mean change in core temperature with external warming in the intervention group was 0.29 °C higher (0.05 to 0.52) | 545 | ⨁⨁⨁◯ | |
| Change in core temperature without external warming | The mean change in core temperature without external warming was ‐0.40 °C | The mean change in core temperature without external warming in the intervention group was 0.32 °C higher (‐0.11 to 0.75) | 340 | ⨁⨁⨁◯ | |
| Change in core temperature for operations > 120 min | The mean change in core temperature for operations > 120 min was ‐0.74 °C | The mean change in core temperature for operations > 120 min in the intervention group was 0.70 °C higher (0.10 to 1.30) | 194 | ⨁⨁⨁◯ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
|
| |||||
| Heated CO2 with or without humidification for laparoscopic abdominal surgery | |||||
| Patient or population: Laparoscopic abdominal surgery (pain score) | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Quality of the evidence | Comments | |
| Risk with cold gas | Risk with heated gas | ||||
| Day 1 pain score (0 to 10‐point VAS) | The mean day 1 pain score was 2.8 | The mean day 1 pain score in the intervention group was 0.04 fewer (‐0.42 to 0.34) | 991 | ⨁⨁◯◯ | Higher score indicates more pain for participants |
| Day 1 pain score: heated, humidified vs cold (abdominal) | The mean day 1 pain score: heated, humidified vs cold (abdominal) was 4 | The mean day 1 pain score: heated, humidified vs cold (abdominal) in the intervention group was 0.14 fewer (‐0.6 to 0.33) | 670 | ⨁⨁◯◯ | |
| Day 1 pain score: heated, humidified vs cold (shoulder) | The mean day 1 pain score: heated, humidified vs cold (shoulder) was 2 | The mean day 1 pain score: heated, humidified vs cold (shoulder) in the intervention group was 0.35 fewer (‐1.75 to 1.05) | 171 | ⨁◯◯◯ | |
| Day 1 pain score: heated only vs cold | The mean day 1 pain score: heated vs cold was 2.8 | The mean day 1 pain score: heated vs cold in the intervention group was 0.5 more (‐0.11 to 1.12) | 150 | ⨁⨁⨁◯ | |
| Day 2 pain score | The mean day 2 pain score was 2.2 | The mean day 2 pain score in the intervention group was 0.28 fewer (‐0.78 to 0.21) | 695 | ⨁⨁◯◯ | |
| Day 2 pain score: heated, humidified vs cold (abdominal) | The mean day 2 pain score: heated, humidified vs cold (abdominal) was 3.2 | The mean day 2 pain score: heated, humidified vs cold (abdominal) in the intervention group was 0.4 fewer (‐1.07 to 0.28) | 442 | ⨁⨁◯◯ | |
| Day 2 pain score: heated, humidified vs cold (shoulder) | The mean day 2 pain score: heated, humidified vs cold (shoulder) was 1.5 | The mean day 2 pain score: heated, humidified vs cold (shoulder) in the intervention group was 0.88 fewer (‐2.93 to 1.17) | 111 | ⨁◯◯◯ | |
| Day 2 pain score: heated only vs cold | The mean day 2 pain score: heated vs cold was 1.9 | The mean day 2 pain score: heated vs cold in the intervention group was 0.41 more (‐0.44 to 1.27) | 142 | ⨁⨁◯◯ | |
| Day 1 pain score for low risk of bias studies | The mean day 1 pain score for low risk of bias studies was 2.7 | The mean day 1 pain score for low risk of bias studies in the intervention group was 0.17 more (‐0.21 to 0.55) | 570 | ⨁⨁⨁⨁ | |
| Day 1 pain score for low risk of bias studies: heated, humidified vs cold (abdominal) | The mean day 1 pain score for low risk of bias studies: heated, humidified vs cold (abdominal) was 4.3 | The mean day 1 pain score for low risk of bias studies: heated, humidified vs cold (abdominal) in the intervention group was 0.17 more (‐0.29 to 0.63) | 460 | ⨁⨁⨁⨁ | |
| Day 1 pain score for low risk of bias studies: heated, humidified vs cold (shoulder) | The mean day 1 pain score for low risk of bias studies: heated, humidified vs cold (shoulder) was 1.2 | The mean day 1 pain score for low risk of bias studies: heated, humidified vs cold (shoulder) in the intervention group was 0.25 more (‐0.81 to 1.31) | 110 | ⨁⨁⨁◯ | |
| Day 2 pain score for low risk of bias studies | The mean day 2 pain score for low risk of bias studies was 3.5 | The mean day 2 pain score for low risk of bias studies in the intervention group was 0.29 fewer (‐0.65 to 0.07) | 380 | ⨁⨁⨁⨁ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
|
| |||||
| Heated CO2 with or without humidification for laparoscopic abdominal surgery | |||||
| Patient or population: Laparoscopic abdominal surgery (morphine consumption) | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Quality of the evidence | Comments | |
| Risk with cold gas | Risk with heated gas | ||||
| Up to 6 h | The mean up to 6 h morphine consumption was 12.6 mg | The mean up to 6 h in the intervention group was 0.45 mg more (‐1.19 to 2.08) | 231 | ⨁⨁⨁◯ | Morphine consumption was presented as equivalent daily dose |
| Day 1 morphine | The mean day 1 morphine consumption was 32.4 mg | The mean day 1 morphine consumption in the intervention group was 0.64 mg less (‐4.48 to 3.20) | 573 | ⨁⨁⨁◯ | |
| Day 1 morphine: heated, humidified vs cold | The mean day 1 morphine consumption: heated, humidified vs cold was 31.2 mg | The mean day 1 morphine consumption: heated, humidified vs cold in the intervention group was 1.66 mg less (‐4.79 to 1.46) | 481 | ⨁⨁◯◯ | |
| Day 1 morphine: heated only vs cold | The mean day 1 morphine consumption: heated vs cold was 33.6 mg | The mean day 1 morphine consumption: heated vs cold in the intervention group was 11.93 mg more (0.92 to 22.94) | 92 | ⨁⨁◯◯ | |
| Day 2 morphine | The mean day 2 morphine consumption was 22.1 mg | The mean day 2 morphine consumption in the intervention group was 0.61 mg less (‐2.79 to 1.57) | 532 | ⨁⨁⨁◯ | |
| Day 2 morphine: heated, humidified vs cold | The mean day 2 morphine consumption ‐ Heated, humidified vs cold was 21.3 mg | The mean day 2 morphine consumption: heated, humidified vs cold in the intervention group was 0.94 mg less (‐1.9 to 0.01) | 410 | ⨁⨁⨁◯ | |
| Day 2 morphine: heated only vs cold | The mean day 2 morphine consumption: heated vs cold was 23 mg | The mean day 2 morphine consumption: heated vs cold in the intervention group was 9.79 mg more (1.58 to 18.00) | 122 | ⨁⨁◯◯ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1. Risk of bias not clear | |||||
| Heated CO2 with or without humidification for laparoscopic abdominal surgery | |||||
| Patient or population: Laparoscopic abdominal surgery (hospital stay) | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Quality of the evidence | Comments | |
| Risk with cold gas | Risk with heated gas | ||||
| Hospital stay (days) | The mean hospital stay was 2.7 days | The mean hospital stay in the intervention group was 0.06 days less (‐0.31 to 0.19) | 685 | ⨁⨁⨁◯ | |
| Hospital stay: heated, humidified vs cold | The mean hospital stay: heated, humidified vs cold was 2.9 days | The mean hospital stay: heated, humidified vs cold in the intervention group was 0.13 days less (‐0.44 to 0.18) | 563 | ⨁⨁⨁◯ | |
| Hospital stay: heated only vs cold | The mean hospital stay: heated vs cold was 2.6 days | The mean hospital stay: heated vs cold in the intervention group was 0.20 days more (‐0.23 to 0.62) | 122 | ⨁⨁⨁◯ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1. Risk of bias not clear | |||||
| Heated CO2 with or without humidification for laparoscopic abdominal surgery | |||||
| Patient or population: Laparoscopic abdominal surgery (recovery time) | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Quality of the evidence | Comments | |
| Risk with cold gas | Risk with heated gas | ||||
| Recovery time (minutes) | The mean recovery time was 106.8 min | The mean recovery time in the intervention group was 26.79 min less (‐51.34 to ‐2.25) | 327 | ⨁⨁◯◯ | |
| Recovery time for low risk of bias studies | The mean recovery time for low risk of bias studies was 90.1 min | The mean recovery time for low risk of bias studies in the intervention group was 1.22 min less (‐6.62 to 4.17) | 277 | ⨁⨁⨁◯ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1. Risk of bias not clear | |||||
| Heated CO2 with or without humidification for laparoscopic abdominal surgery | |||||
| Patient or population: Laparscopic abdominal surgery (lens fogging) | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Quality of the evidence | Comments | |
| Risk with cold gas | Risk with heated gas | ||||
| Times cleaned | The mean frequency of cleaning was 1.8 times | The mean times cleaned in the intervention group was 0.73 times more (‐0.32 to 1.77) | 341 | ⨁⨁◯◯ | The frequency of lens cleaning during surgery |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1. Risk of bias not clear | |||||
| Heated CO2 with or without humidification for laparoscopic abdominal surgery | |||||
| Patient or population: Laparoscopic abdominal surgery (operative time) | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants | Quality of the evidence | Comments | |
| Risk with cold gas | Risk with heated gas | ||||
| Operative time (minutes) | The mean operative time was 76.6 min | The mean operative time in the intervention group was 0.44 min less (‐3.91 to 3.04) | 1318 | ⨁◯◯◯ | |
| Operative time: heated, humidified vs cold | The mean operative time: heated, humidified vs cold was 94.3 min | The mean operative time: heated, humidified vs cold in the intervention group was 2.01 min less (‐7.15 to 3.13) | 1033 | ⨁◯◯◯ | |
| Operative time: heated only vs cold | The mean operative time: heated vs cold was 58.8 min | The mean operative time: heated vs cold in the intervention group was 0.91 min more (‐4.02 to 5.83) | 285 | ⨁⨁◯◯ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1. Risk of bias not clear | |||||
| Study | Number of participants | Mean age (years) | % Female | Mean BMI (kg/m2) or weight (kg) |
| 150 | 52 | 72.7 | ||
| 26 | 49W/53C | 42.3 | 25W/25C (BMI) | |
| 50 | 41.5WH/44C | 86 | 50W/52.9C (BMI) | |
| 44 | 42.3WH/40.6W/44.8H/42.5C | 47.2WH/49.1W/48.5H/52.4C (BMI) | ||
| 40 | 100 | |||
| 117 (16 excluded) | 52 | 68.3 | 29.5W/29.7C (BMI) | |
| 50 (6 excluded) | 44WH/45C | 89.1 | 125W/128C (weight) | |
| 90 (53 with data) | 37WH/33W/36C | 100 | 63WH/63W/65C (weight) | |
| 148 | 55.7 | 69.6 | 28.56 (BMI) | |
| 30 | 60.1W/55.1C | 36.7 | ||
| 60 | 30WH/30C | 100 | 25W/24C (BMI) | |
| 32 | 23‐89 (range) | |||
| 37 | 46W/47C | 100 | 63W/66C (weight) | |
| 20 | 43WH/45C | 45 | ||
| 72 (50 with data) | 100 | |||
| 30 | 46.2W/53.7C | |||
| 20 | 62W/51C | 60 | 75W/83C (weight) | |
| 82 (8 excluded) | 71WH/69C | 57.1W/59C | 26.5W/25.5C (BMI) | |
| 30 | 41WH/39C | 80 | 50.6W/52.3C (BMI) | |
| 108 (8 excluded) | 52W/53C | 58 | 26.9W/25.7C (BMI) | |
| 41 (1 excluded) | 47.5W/52.2C | 45 | 27W/29.2C (BMI) | |
| 195 (5 excluded) | 12 | 36.8 | 49.6W/50.3C (weight) | |
| W = warmed cohort, C = cold cohort, H = humidified cohort, WH = warmed and humidified cohort | ||||
| Study | Procedures | Method of temperature measurement | Insufflation gas | Gas temperature (°C) | Heating device | Humidification (%) | Duration of surgery (minutes) | External warming |
| 110 laparoscopic cholecystectomy, 40 laparoscopic fundoplication | Carbon dioxide | WISAP Flow Thermo | Not specified | 42WH/56C | None | |||
| Laparoscopic fundoplication, hernioplasty, sigmoid colon resection, rectopexy | Pulmonary artery catheter | Carbon dioxide | 37 | WISAP Flow Thermo | None | 161W/163C | Warm blanket/ warm waterbath mattress | |
| Laparoscopic Roux‐en‐Y gastric bypass | Rectal thermometer | Carbon dioxide | 35 | Lexion Insuflow | 95 | 61.7WH/61.7C | None | |
| Laparoscopic Roux‐en‐Y gastric bypass | Foley catheter for bladder temperature | Carbon dioxide | 37 | Lexion Insuflow | 95 | 78‐84 (range) | None | |
| Awake laparoscopy | Carbon dioxide | 35 | Lexion Insuflow | 95 | None | |||
| Laparoscopic cholecystectomy | Oesophageal probe | Carbon dioxide | 35 | Lexion Insuflow | 95 | 91.2 | Bair Hugger forced air warmer (32 °CW/34 °C C) | |
| Laparoscopic Roux‐en‐Y gastric bypass | Oesophageal/ tympanic membrane | Carbon dioxide | 37 | Lexion Insuflow | 95 | 120WH/132C | Warm cotton blankets | |
| Laparoscopic gynaecologic surgery | Intravesical temperature | Carbon dioxide | 38 | Laparo‐CO2‐Pneu2232 | 95‐100 | 62WH/51W/45C | None | |
| Laparoscopic cholecystectomy | Rectal probe | Carbon dioxide | 35 | Storz Optitherm | 95 | 63.88 | None | |
| Laparoscopic low anterior resection, colectomy, gastrectomy | Oesophageal temperature probe | Carbon dioxide | 37 | WISAP Flow Thermo | None | 212W/230C | Bair Hugger forced air warmer/ warming mattress with circulating water at 38 °C | |
| 49 laparoscopy for endometriosis, 16 laparoscopy for adhesions | Carbon dioxide | 37 | Fisher & Paykel | 100 | 49.6WH/46.8C | Upper body warming blanket | ||
| Laparoscopic cholecystectomy | Oesophageal thermoresistor | Carbon dioxide | 34‐37 | LINS‐1000 | 88‐90 | 40WH/48.3WH | None | |
| Laparoscopic hysterectomy | Tympanic and nasopharyngeal infrared technique | Carbon dioxide | 37 | None | 56W/51C | None | ||
| Laparoscopic Nissen fundoplication | Oesophageal probe | Carbon dioxide | 37 | Georgia BioMedical Insuflow | 95 | 35.6WH/35.6C | Bair Hugger forced air warmer | |
| Laparoscopic gynaecologic surgery | Endotracheal temperature probe | Carbon dioxide | 36.2 | Insuflow | 95 | 38‐262 (range) | None | |
| Laparoscopic cholecystectomy | Oesophageal probe | Carbon dioxide | 37 | WISAP Flow Thermo | None | 31.5W/32.1C | None | |
| Laparoscopic cholecystectomy | Oesophageal probe | Carbon dioxide | 37 | WISAP Flow Thermo | None | 56W/61C | None | |
| Laparoscopic colon resection | Oesophageal probe | Carbon dioxide | 37 | Fisher & Paykel | 98 | 176.3WH/184.7C | Bair Hugger forced air warmer | |
| Laparoscopic Roux‐en‐Y gastric bypass | Oesophageal probe | Carbon dioxide | 35 | Lexion Insuflow | 95 | 76WH/101C | Bair Hugger forced air warmer at discretion of blinded anaesthesiologist | |
| Laparoscopic cholecystectomy, fundoplication, myotomy | Subdiaphragmatic thermometric probe | Carbon dioxide | 37 | ThermoFlator | None | 73W/67C | None | |
| Laparoscopic fundoplication | Nasopharyngeal thermistor | Carbon dioxide | 37 | Cook LINS‐2000 | None | 69W/72C | Bair Hugger forced air warmer | |
| Laparoscopic appendectomy | Naso‐oesophageal probe | Carbon dioxide | 37 | Fisher & Paykel | 98 | 69.8WH/71.6C | Forced‐air warming blanket | |
| W = warmed cohort, C = cold cohort, H = humidified cohort, WH = warmed and humidified cohort | ||||||||
| Study | Mean change in core temperature (°C) | Adverse events (Clavien‐Dindo ≥ III) | ||||
| Heated and humidified | Heated only | Cold | Heated and humidified | Heated only | Cold | |
| 0.49 | ‐0.06 | Not reported | Not reported | |||
| 0.2 | ‐0.1 | Not reported | Not reported | |||
| ‐0.4 | ‐0.4 | Not reported | Not reported | |||
| 0.4 | 0.2 | 0.4 | Not reported | Not reported | Not reported | |
| Not reported | Not reported | Not reported | Not reported | |||
| 0.29 | ‐0.03 | Not reported | Not reported | |||
| ‐0.7 | ‐1.7 | Not reported | Not reported | |||
| ‐0.5 | ‐0.6 | ‐0.4 | Not reported | Not reported | Not reported | |
| Not reported | Not reported | 0 | 0 | |||
| ‐0.4 | ‐0.7 | Not reported | Not reported | |||
| ‐0.2 | ‐0.13 | Not reported | Not reported | |||
| ‐0.25 | ‐0.3 | 0 | 0 | |||
| ‐0.2 | 0 | Not reported | Not reported | |||
| 0.4 | 0.3 | 0 | 0 | |||
| ‐0.3 | ‐1.64 | 0 | 0 | |||
| ‐0.24 | ‐0.42 | Not reported | Not reported | |||
| 0 | ‐0.1 | Not reported | Not reported | |||
| 0.64 | 0.48 | 3 (8.6%) | 5 (12.8%) | |||
| 0.4 | ‐0.3 | Not reported | Not reported | |||
| Not reported | Not reported | 0 | 0 | |||
| 0.2 | 0 | 0 | 1 (4.8%) | |||
| 0.1 | 0.1 | 3 (10.3%) | 0 | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Change in core temperature Show forest plot | 19 | 1100 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.06, 0.36] |
| 1.1 Heated, humidified vs cold | 14 | 885 | Mean Difference (IV, Random, 95% CI) | 0.31 [0.09, 0.53] |
| 1.2 Heated only vs cold | 7 | 215 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.16, 0.20] |
| 2 Change in core temperature for low risk of bias studies Show forest plot | 10 | 653 | Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.01, 0.33] |
| 2.1 Heated, humidified vs cold | 8 | 561 | Mean Difference (IV, Random, 95% CI) | 0.18 [‐0.04, 0.39] |
| 2.2 Heated vs cold | 3 | 92 | Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.15, 0.39] |
| 3 Change in core temperature for operations > 120 Minutes Show forest plot | 4 | 194 | Mean Difference (IV, Random, 95% CI) | 0.70 [0.10, 1.30] |
| 4 Change in core temperature with external warming Show forest plot | 8 | 545 | Mean Difference (IV, Random, 95% CI) | 0.29 [0.05, 0.52] |
| 5 Change in temperature without external warming Show forest plot | 6 | 340 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.11, 0.75] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Day 1 pain score Show forest plot | 14 | 991 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.42, 0.34] |
| 1.1 Heated, humidified vs cold (abdominal) | 10 | 670 | Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.60, 0.33] |
| 1.2 Heated, humidified vs cold (shoulder) | 3 | 171 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.75, 1.05] |
| 1.3 Heated vs cold | 3 | 150 | Mean Difference (IV, Random, 95% CI) | 0.50 [‐0.11, 1.12] |
| 2 Day 1 pain score for low risk of bias studies Show forest plot | 7 | 570 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.21, 0.55] |
| 2.1 Heated, humidified vs cold (abdominal) | 7 | 460 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.29, 0.63] |
| 2.2 Heated, humidified vs cold (shoulder) | 2 | 110 | Mean Difference (IV, Random, 95% CI) | 0.25 [‐0.81, 1.31] |
| 3 Day 2 pain score Show forest plot | 10 | 695 | Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.78, 0.21] |
| 3.1 Heated, humidified vs cold (abdominal) | 7 | 442 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.07, 0.28] |
| 3.2 Heated, humidified vs cold (shoulder) | 2 | 111 | Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐2.93, 1.17] |
| 3.3 Heated vs cold | 3 | 142 | Mean Difference (IV, Random, 95% CI) | 0.41 [‐0.44, 1.27] |
| 4 Day 2 pain score of low risk of bias studies Show forest plot | 5 | 380 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.65, 0.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Up to 6 hours Show forest plot | 4 | 231 | Mean Difference (IV, Random, 95% CI) | 0.45 [‐1.19, 2.08] |
| 2 Day 1 morphine Show forest plot | 9 | 573 | Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐4.48, 3.20] |
| 2.1 Heated, humidified vs cold | 7 | 481 | Mean Difference (IV, Random, 95% CI) | ‐1.66 [‐4.79, 1.46] |
| 2.2 Heated vs cold | 3 | 92 | Mean Difference (IV, Random, 95% CI) | 11.93 [0.92, 22.94] |
| 3 Day 2 morphine Show forest plot | 7 | 532 | Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐2.79, 1.57] |
| 3.1 Heated, humidified vs cold | 6 | 410 | Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.90, 0.01] |
| 3.2 Heated vs cold | 2 | 122 | Mean Difference (IV, Random, 95% CI) | 9.79 [1.58, 18.00] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospital stay Show forest plot | 10 | 685 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.31, 0.19] |
| 1.1 Heated, humidified vs cold | 9 | 563 | Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.44, 0.18] |
| 1.2 Heated vs cold | 2 | 122 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.23, 0.62] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Recovery time Show forest plot | 6 | 327 | Mean Difference (IV, Random, 95% CI) | ‐26.79 [‐51.34, ‐2.25] |
| 2 Recovery time for low risk of bias studies Show forest plot | 5 | 277 | Mean Difference (IV, Random, 95% CI) | ‐1.22 [‐6.62, 4.17] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Times cleaned Show forest plot | 7 | 341 | Mean Difference (IV, Random, 95% CI) | 0.73 [‐0.32, 1.77] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Operative time Show forest plot | 20 | 1318 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐3.91, 3.04] |
| 1.1 Heated, humidified vs cold | 15 | 1033 | Mean Difference (IV, Random, 95% CI) | ‐2.01 [‐7.15, 3.13] |
| 1.2 Heated vs cold | 7 | 285 | Mean Difference (IV, Random, 95% CI) | 0.91 [‐4.02, 5.83] |

