治疗外伤性强直恒门牙的干预措施
摘要
研究背景
遭受创伤的牙齿可能会与周围的骨骼融合,这一过程称为牙齿强直。强直的恒门牙在面部生长过程中无法萌出,并且可能移位,从而导致功能和美观问题。牙齿强直还与牙根吸收有关,这最终可能导致受影响的牙齿脱落。临床上已经有了治疗强直恒门牙的不同干预措施,但尚不清楚哪种干预措施最有效。
研究目的
评估可用于治疗强直恒门牙的干预措施的效果。
检索策略
检索了以下电子数据库:Cochrane口腔健康组试验注册库(截至2015年8月3日)、Cochrane对照试验中心注册库(Cochrane Central Register of Controlled Trials, CENTRAL)( Cochrane图书馆 ,2015年,第7期)、MEDLINE(通过OVID,1946年至8月3日)2015)、EMBASE(通过OVID,1980年至2015年8月3日)和LILACS(通过BIREME,1982年至2015年8月3日)。我们检索了美国国立卫生研究院试验注册中心( http://clinicaltrials.gov )和世卫生组织临床试验注册平台,了解正在进行的试验。我们检索电子数据库时,未对语言或出版日期进行任何限制。
纳入排除标准
我们纳入了随机对照试验(randomised controlled trials, RCT),比较了治疗任一年龄个体的强直性恒门牙移位的所有干预。其中一种治疗方案与其它方案或安慰剂进行比较。
资料收集与分析
两位综述作者独立筛选并选择纳入研究。我们获得了可能相关试验的论文全文。尽管没有纳入任何研究,但作者计划独立提取资料并根据 《Cochrane干预性系统综述手册》 分析数据。
主要结果
没有发现符合纳入标准的随机对照试验。
作者结论
我们无法确认任何关于强直恒门牙不同治疗方案疗效的随机对照试验报告。由于缺乏管理这一健康问题的高质量证据,急需针对这一主题进行精心设计的临床试验,并要符合CONSORT声明( www.consort-statement.org/ )。
PICO
简语概要
治疗受损并与骨头融合的恒门牙的干预措施
系统综述问题
本综述的目的是评估不同的治疗方法对于治疗受损并融合到骨头上的恒门牙(强直前牙)的效果如何。
研究背景
有时,牙齿受伤后,例如当牙齿被撞击并推入颌骨时,牙齿会融合到颌骨上。这种融合称为“强直”。通常,融合(“强直”)牙齿的根部会被身体吸收并被周围的骨头所取代。对于某些人来说,这可能会导致融合的牙齿脱落。这些牙齿不会随着颌骨的正常生长而生长,因此如果在儿童时期受伤,这些牙齿可能会逐渐移动。目前尚不清楚哪种治疗方法最适合治疗这些融合牙齿,这是我们进行本综述的原因。
研究特征
来自Cochrane口腔健康组(Cochrane Oral Health Group)的综述作者对本综述现有的研究进行评估,证据截至2015年10月3日。没有发现符合本综述纳入标准的研究。
主要研究结果和证据质量
该综述发现,目前没有高质量的证据来比较不同治疗研究方法对融合前牙的效果。需要进一步的研究为不同的治疗方法及其相对有效性和安全性提供证据。
Authors' conclusions
Background
Teeth that have suffered severe trauma can fuse to the surrounding bone during recovery, a process termed ankylosis (Kawanami 1999). These severe traumatic injuries include intrusion, where the tooth is pushed up into the jawbone, or avulsion and replantation, where the tooth is knocked out and replanted (Andreasen 1995; Andreasen 2006). The five‐year survival rate of ankylosed teeth is poor. Where this occurs the root is resorbed and replaced by the adjacent bone, which is termed replacement resorption. The speed of replacement resorption and loss of the tooth is related to the age of the patient (Barrett 1997). When dental ankylosis occurs in a growing child, the ankylosed tooth fails to erupt compared to adjacent teeth during vertical growth which alters alveolar development (Campbell 2005b; Kofod 2005; Malmgren 2002). Severe infraocclusion causes functional and aesthetic problems and can lead to tilting of the adjacent teeth if left untreated (Takahashi 2005).
Prevalence
The upper front teeth are the most frequently affected by trauma. Soriano 2007 found prevalence of 10.5% of traumatic dental injuries to the permanent anterior teeth among a group of Brazilian schoolchildren. Simiarly, the 2013 Children's Dental Health Survey in England, Wales and Northern Ireland found around 10% of children had experienced trauma to their incisors (Children's Dental Health Survey 2013).
Diagnosis
Clinically, 'ankylosis' is defined as a pathological fusion of the external root surface of the tooth with the surrounding bone and presents typical clinical signs. Lack of mobility and different percussion sound when compared with adjacent unaffected teeth are typical features (Campbell 2005a; Campbell 2005b). Radiographic examination is considered to be of limited value in the early detection of ankylosis because of the two‐dimensional nature of the image (Campbell 2005b). The observation of progressive infraocclusion during adolescent growth is another indicator (Andreasen 1995). Diagnostic data can be complemented by electronic devices (Periotest and digital sound wave) (Campbell 2005a).
Treatment options
Different interventions have been proposed for treating ankylosed permanent front teeth but there is uncertainty as to which intervention is most effective. This systematic review seeks to provide reliable evidence for the different treatment options available for ankylosed permanent front teeth.
The choice of treatment for displaced ankylosed teeth depends on the severity of infraocclusion and replacement resorption, the preference and experience of the clinician, and patient age (facial growth and dental development) and expectations (Campbell 2005b). Considering these factors, treatments can be summarised as follows.
1) Periodical follow‐up
Periodical follow‐up of the ankylosed teeth with possible composite build‐up for any minor infraocclusion.
2) Repositioning of the ankylosed teeth
Interventions for ankylosis that preserve the crown include surgical dislodgement and repositioning. It involves the mechanical breakage of the bridge between the tooth and the surrounding bone and is said to permit the tooth to resume eruption. The tooth can be placed a few millimetres from its original position and a flexible splint is inserted for a few days (Moffat 2002). Another option is to insert an orthodontic appliance immediately after surgery instead of a splint (Takahashi 2005). Another treatment option is bone sectioning (osteotomy) around the root with immediate repositioning (Medeiros 1997).
Distraction osteogenesis has also been used to reposition displaced teeth. The ankylosed tooth and a bone segment are separated from the surrounding bone through osteotomy and a device is placed to perform slow movement, thereby correcting the tissue and positional deficiencies (Nocini 2004).
3) Autotransplantation
Autotransplantation of a premolar to the ankylosed tooth position may provide a long‐lasting physiological and aesthetic solution (Andreasen 1990a; Andreasen 1990b; Kinzinger 2003; Kofod 2005; Kristerson 1991). It is recommended when the premolar root is less than three quarters developed (the first lower premolar is the preferred choice). In adolescents over 12 to 14 years, tooth transplantation may be no longer recommended (Isaacson 2001; Sapir 2008; Small 2002), due to a higher chance of complications associated with transplanted teeth with complete formed roots (Andreasen 1990a; Andreasen 1990b).
4) Conventional prosthodontics and dental implants
Another option is to remove the ankylosed teeth and to insert dental prostheses or implants, which is more recommended for adults. Height of jawbones should be maintained for adequate aesthetics and function, so decoronation (crown removal beneath surrounding bone) is proposed as an alternative to conventional tooth extraction. Decoronation is justified by the following reasons: an implant will be planned in the future, jaw growth is not yet complete, tooth transplantation is orthodontically contraindicated, and heavily discoloured or malpositioned teeth are not aesthetically acceptable (Sapir 2008). This is usually indicated if transplant or orthodontic space closure is not feasible in a growing child (Malmgren 2000).
5) Extraction and orthodontic space closure
Orthodontic space closure after the early loss of the traumatised tooth may provide an aesthetic solution as well as rehabilitation of the alveolar bone ridge. Unfortunately, limitations such as the underlying malocclusion, dental and skeletal age, teeth involved (systemic health, periodontal status, tooth shape and size), the need for compensatory extractions or reshaping of teeth as well as cost and compliance limit this option to well selected cases (Sapir 2008).
Objectives
To evaluate the effectiveness of any intervention that can be used in the treatment of ankylosed permanent front teeth.
Methods
Criteria for considering studies for this review
Types of studies
Only randomised controlled trials (RCTs) were considered in this review.
Types of participants
Any patient with ankylosis and displacement of permanent front teeth diagnosed by clinical and radiographic assessment. Both teeth with or without previous endodontic treatment were considered.
Types of interventions
All interventions for treating displaced ankylosed teeth were considered, including.
-
Implant‐supported crowns after extraction or decoronation of the ankylosed teeth.
-
Fixed prostheses cemented to prepared teeth after extraction or decoronation of the ankylosed teeth.
-
Transplantation of other teeth after extraction of the ankylosed teeth.
-
Repositioning of ankylosed teeth after osteotomy followed or not by distraction osteogenesis, or after luxation.
Interventions would also be compared with attempt for conventional orthodontic treatment or follow‐up with no specific treatment for ankylosis.
Types of outcome measures
Primary outcomes
-
Tooth survival, expressed as the ratio between extracted and non‐extracted teeth at specific time intervals. Regarding implant‐supported crowns, failure can be defined as mobile implants, removal of stable implants dictated by progressive marginal bone loss or infection, implant fractures, or implants which were left 'sleeping' due to wrong alignment (Esposito 2005).
-
Pain, discomfort or aesthetic complaints.
-
Participant satisfaction.
Secondary outcomes
-
Prevention and control of the resorption process.
-
Degree of mobility and percussion sound, as assessed by conventional clinical exam or electronic devices.
-
Complications during the therapy or thereafter. If possible, the severity of these complications would also be recorded.
-
Direct costs for the use of different treatment interventions and dentist time.
Search methods for identification of studies
Electronic searches
For the identification of studies included or considered for this review, detailed search strategies were developed for each searched database. These were based on the search strategy developed for MEDLINE (see Appendix 1) but revised appropriately for each database.The search strategy used a combination of controlled vocabulary and free text terms and was linked with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials (RCTs) in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) (Higgins 2011). As the yield of references from EMBASE and LILACS was already small, no search filter for identifying randomised controlled trials was used for these two databases.
The following databases were searched:
-
The Cochrane Oral Health Group Trials Register (to 3 August 2015) (Appendix 2);
-
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2015, Issue 7) (Appendix 3);
-
MEDLINE via OVID (1946 to 3 August 2015) (Appendix 1);
-
EMBASE via OVID (1980 to 3 August 2015) (Appendix 4);
-
LILACS via BIREME (1982 to 3 August 2015) (Appendix 5).
No restrictions were placed on the language or date of publication when searching the electronic databases.
Searching other resources
We searched the following databases for ongoing trials:
-
US National Institutes of Health Trials Register (http://clinicaltrials.gov) (to 3 August 2015) (see Appendix 6);
-
The WHO Clinical Trials Registry Platform (http://apps.who.int/trialsearch/default.aspx) (to 3 August 2015) (see Appendix 7).
Only handsearching done as part of the Cochrane Worldwide Handsearching Programme and uploaded to CENTRAL was included (see the Cochrane Masterlist for details of journal issues searched to date).
We planned to cross check the reference lists of any clinical trials identified for additional trials published outside the handsearched journals. A search for existing meta‐analyses and non‐Cochrane systematic reviews was performed and their reference lists scanned for additional trials. We searched the reference lists of relevant articles and the review authors' personal database of trial reports. In future updates if eligible trials are found, we will contact investigators of included studies by electronic mail to ask for details of additional published and unpublished trials.
In order to enhance the sensitivity of the search methods, we also attempted to contact the corresponding authors of the other studies found by electronic mail to ask about additional published and unpublished trials. In that case, we considered the studies by using the 'types of participants', 'types of interventions' and 'types of outcome measures' criteria.
Data collection and analysis
Selection of studies
Two review authors (Raphael Freitas de Souza (RFS) and Tim Newton (TN)) independently assessed the abstracts of studies resulting from the searches. Full copies of all relevant and potentially relevant studies (i.e. those appearing to meet the inclusion criteria, or for which there were insufficient data in the title and abstract to make a clear decision) were obtained. The full‐text papers were assessed independently and in duplicate by two review authors and any disagreement on the eligibility of included studies would have been resolved through discussion and consensus or if necessary through a third party (Melissa Marchesan (MM)). All non‐eligible studies were excluded; reasons for their exclusion were noted in the Characteristics of excluded studies table in Review Manager (RevMan) 5.1 (RevMan 2011).
Data extraction and management
We had planned to enter study details into the Characteristics of included studies table in RevMan 5.1. In future updates if studies are available, the review authors (RFS and TN) will collect outcome data independently and in duplicate using a pre‐determined form designed for this purpose. The review authors will only include data if there is an independently reached consensus, any disagreements will be resolved by consulting with a third review author (Helen Travess (HT)).
The following details were planned for extraction from included studies:
(1) Trial methods
(a) Method of allocation
(b) Masking of participants and outcomes
(c) Exclusion of participants after sequence generation and proportion of losses at follow‐up.
(2) Participants
(a) Demographic characteristics such as household income, education, ethnicity, and regional/rural origin, when available
(b) Source of recruitment
(c) Country of origin
(d) Sample size
(e) Age
(f) Gender
(g) Inclusion and exclusion criteria as described in the Criteria for considering studies for this review section
(h) Previous endodontic treatment of ankylosed teeth
(i) Periodontal ligament/root surface treatment before ankylosis and at the moment of the intervention.
(3) Intervention
(a) Type of intervention
(b) Duration and length of time in follow‐up.
(4) Control
(a) Type of control ‐ no specific treatment or sham procedure
(b) Duration and length of time in follow‐up in the control group.
(5) Outcomes
(a) Primary and secondary outcomes as described in the outcome measures section of this review.
We had also planned to record any sources of funding reported in the included trials. We had intended to use this information for assessing heterogeneity and the external validity of the trials.
Assessment of risk of bias in included studies
An assessment of the risk of bias in included studies would have been undertaken independently and in duplicate by two review authors (HT and MM) following the recommendations as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011). In future updates, any inconsistencies between the review authors will be discussed and resolved and if necessary a third review author will be consulted. Where uncertainty cannot be resolved, effort will be made to contact authors directly for clarification.
A specific tool for assessing risk of bias in each included study would have been adopted. This comprises a description and a judgement for each entry in a risk of bias table, where each entry addresses a specific feature of the study:
(1) Random sequence generation (selection bias)
(2) Allocation concealment (selection bias)
(3) Blinding (performance bias and detection bias). In some instances it will not be possible to blind participants and researchers but we would expect that the outcome assessors and data analysts would be blinded
(4) Incomplete outcome data (attrition bias)
(5) Selective reporting (reporting bias)
(6) Other bias
Each entry would have been assessed as at low risk of bias, high risk of bias, or unclear risk of bias (lack of information or uncertainty over the potential for bias). We had planned to summarise an assessment of the overall risk of bias involving the consideration of the relative importance of different domains.
Measures of treatment effect
The following procedures will be conducted if we found eligible trials in future updates.
For dichotomous data, the estimates of effect of an intervention will be expressed as risk ratios together with 95% confidence intervals. For continuous outcomes, mean differences and 95% confidence intervals will be used to summarise the data for each group where they are calculable from the data presented.
Assessment of heterogeneity
The review authors planned to assess clinical heterogeneity by examining the characteristics of the included studies: the differences between the types of participants, the interventions and the outcomes within and across the trials. We had planned to assess statistical homogeneity using a χ2 test in addition to the I2 statistic, where I2 values over 50% indicate moderate to high heterogeneity (Higgins 2003) but no studies were included in this review.
Assessment of reporting biases
Reporting bias was not assessed due to insufficient studies. If we identify a sufficient number of included studies in future updates, we will attempt to assess publication bias using a funnel plot (Egger 1997).
Data synthesis
In future updates, if we include sufficient studies, we will use the fixed‐effect and random‐effects models as appropriate, for the synthesis and meta‐analysis of any quantitative data. If we establish that there is heterogeneity between the studies, we may undertake a random‐effects model as appropriate, but if the heterogeneity between the studies is significant, we may not undertake a meta‐analysis. If there are too few clinically homogenous trials or insufficient data for pooling, we will present the results of the individual trials and perform a descriptive analysis only.
Subgroup analysis and investigation of heterogeneity
In future updates if data are available, we will conduct analyses based on separate age groups ((1) less than 12 years, (2) 12 to 18 years, and (3) 18 or more years), gender and mature versus immature open apex teeth.
Sensitivity analysis
If data are available in future updates, the review authors plan to conduct sensitivity analyses to assess the robustness of their review results by repeating the analysis after exclusion of trials with unclear or inadequate allocation concealment and unclear or lack of blinding.
Results
Description of studies
No studies were included in this review. We present the study selection process as a flow chart in Figure 1.
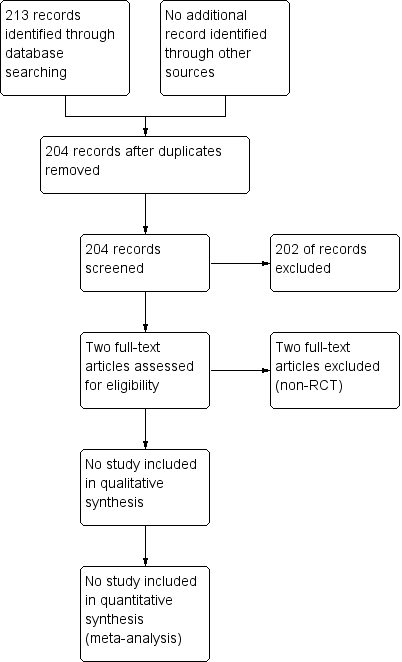
Study flow diagram.
Results of the search
The search strategy retrieved 213 references to studies, which after de‐duplication resulted in 204 potentially eligible studies. After examination of the titles and abstracts of these references, all but two were eliminated and excluded from further review. Those studies (Akhare 2011; Filippi 2006) were excluded after examination of the full text copy.
Included studies
No study was eligible for inclusion in this review.
Excluded studies
We excluded the Akhare 2011 and Filippi 2006 studies because they did not match our inclusion criteria. The reasons for the exclusion were noted in the Characteristics of excluded studies table.
Risk of bias in included studies
No trials were included.
Effects of interventions
None of the studies retrieved in our searches met our inclusion criteria and therefore no data were available for analysis.
Discussion
Several articles report interventions for the management of displaced ankylosed anterior teeth (Filippi 2006; Kinzinger 2003; Kofod 2005; Medeiros 1997; Moffat 2002; Sapir 2008; Takahashi 2005). There are some case reports and case series, as previously stated by Campbell 2005b. However, we found no clinical trial to support clinical decision making for this oral health problem. The absence of clinical trials means that we cannot be confident about which intervention is more effective or safer. Traumatic injuries to the anterior teeth are relatively common and can result in ankylosis (Soriano 2007). Thus, it is disappointing to acknowledge that even trials for possible exclusion by reasons associated with quality assessment were rare. We hypothesise that difficulties regarding the enrolment of participants might be one of the reasons for the absence of trials.
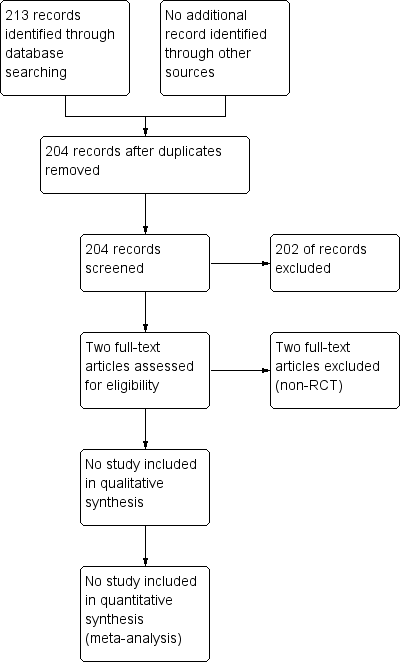
Study flow diagram.

