Manipulative Interventionen, um einen Kindermädchen‐Ellbogen bei jungen Kindern wieder einzurenken
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Quasi‐randomised clinical trial (according to date of birth). | |
| Participants | Orthopaedic emergency centre, Poorsina Hospital, Rasht, Iran. 2004 to 2009. Inclusion criteria: children less than 7 years old presenting with history and signs or symptoms of 'elbow strain' (clinical diagnosis of radial head subluxation). Exclusion criteria: patients with doubtful or unknown history, history of direct trauma to elbow, specific deformity, local oedema or swelling, ecchymosis on elbow, polytrauma, congenital bone disease. 110 children enrolled. 69 boys and 41 girls. Mean age 4.05 years (SD 1.51). | |
| Interventions | Hyperpronation (figure provided showed elbow held at 90° before hyperpronation at the wrist) (n = 52) versus Supination‐flexion (figure provided showed elbow held at 90° before supination at the wrist followed by flexion at the elbow) (n = 58). If first attempt unsuccessful (extremity function had not returned), same method used for second attempt 15 minutes later. If this failed, the alternative method was used 15 minutes later. If unsuccessful, this was repeated after 15 minutes. If both methods failed, elbow radiography to rule out other injury. | |
| Outcomes | Success after first attempt and second attempt (same method, 15 minutes later). | |
| Notes | Article in Persian Arabic with English abstract. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised (assignment according to odd and even birth date). |
| Allocation concealment (selection bias) | High risk | Not concealed. |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Low risk | All 110 allocated children were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Unclear, no trial registration or protocol available. |
| Other bias | Unclear risk | No information regarding baseline comparability. Care providers and provision of treatment seem comparable.. |
| Methods | Quasi‐randomised trial (according to date of birth). | |
| Participants | Accident and emergency department, Gülhane Military Medical Academy, Ankara, Turkey. Inclusion criteria: aged younger than 5 years of age with a clinical presentation and history suggestive of pulled elbow. 66 children enrolled. 26 boys and 40 girls. | |
| Interventions | Hyperpronation: flexing the elbow to 90° and rotating the forearm into hyperpronation (n = 34) If first attempt failed (child did not start to use injured arm), same method used for second attempt. If this failed, the alternative method was used. | |
| Outcomes | Success rate during first attempt, second attempt (same method, 15 minutes later), and third method (alternative method). | |
| Notes | All reductions carried out by one of three final‐year residents, who received briefing about reduction methods before they started the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised (assignment according to odd and even birth date). |
| Allocation concealment (selection bias) | High risk | Not concealed. |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Low risk | All 66 participants were included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | Unclear, no trial registration or protocol available. |
| Other bias | Unclear risk | Mean age in hyperpronation group was 4 months older, but the reported difference was not statistically significant (P = 0.1). Care providers and provision of treatment seemed comparable. |
| Methods | Quasi‐randomised trial (odd or even days of hospital admission). | |
| Participants | Tertiary paediatric orthopaedic unit, Pamplona, Spain. January 1996 to June 2012. Inclusion criteria: symptoms compatible with pulled elbow (causal mechanism, pseudoparalysis, position of forearm). Exclusion criteria: underlying musculoskeletal disorder or condition, history of upper extremity injury, or other systemic diagnosis. 115 children enrolled. Mean age: 27 months, range 20 to 64 months. 30 children (26%) reported a previous episode. | |
| Interventions | Hyperpronation: to 70° to 90° of flexion, without forcing flexion or extension of the elbow (n = 65) Supination‐flexion: complete flexion of the elbow simultaneous with forced supination of the forearm, while the thumb of the examiner was placed over the area of the radial head to detect a pop or click that confirmed diagnosis and reduction (n = 50). If first attempt failed, the alternative manoeuvre was performed (waiting time unknown), if second attempt failed, first manoeuvre was repeated. | |
| Outcomes | Success at first attempt, at second attempt, and at third attempt. | |
| Notes | 17 (8 hyperpronation versus 9 supination‐flexion) children had had attempts at reduction (11 had > 3 attempts) using the supination‐flexion method before entering the study. These were not included in the meta‐analysis. Response from Serafín García‐Mata on 6th April 2017 to queries from Helen Handoll; shared with authors:: "1. The method of randomization: we choose HP or SF method depending on the number of the day: even or odd number of the day, that the child attended. 2. The method was the same throughout the 16 years. 3. The 30 recurrent cases: we do not assess how many of them were of the HP or the SF groups." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Vaguely described: "randomly choosing individuals and dividing patients into 2 groups" in paper. Personal communication revealed assignment according to day of admission (April 2017). |
| Allocation concealment (selection bias) | High risk | Not described in paper. Personal communication revealed assignment according to day of admission (April 2017). |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol available. |
| Other bias | Unclear risk | No baseline imbalances. Mean age in hyperpronation group was 4 months younger, but the reported difference was not statistically significant (P = 0.68). No data on distribution of children with a previous episode of pulled elbow. Care providers and provision of treatment seemed comparable. |
| Methods | Randomised trial. | |
| Participants | Emergency department, Miami Children’s Hospital, Miami, Florida, USA. Inclusion criteria: aged between 6 months and 7 years with clinical findings suggestive of radial head subluxation. 75 children enrolled, of whom 3 (allocated group not stated) were excluded due to nonadherence to protocol (1 data form was lost; and 2 were excluded because their study packets were completed by residents and not by the attending physician). 29 boys and 41 girls. (As well as the 3 exclusions, Table 1 of the article had 2 missing; see Notes). | |
| Interventions | Forced pronation without flexion (n = 35) versus Supination‐flexion (n = 37). If primary attempt was unsuccessful, the alternative method was used for the second attempt 10 minutes later. If still unsuccessful, the participant received care at discretion of the attending physician. | |
| Outcomes | Success rate during first attempt and second attempt (with the alternative method), which was done 10 minutes later. Pain before, during and 1 minute after successful repositioning using visual analogue scale (10 cm) by parents, nurse and physician. (For pain measurement, 9 additional children were excluded due to unsuccessful first attempt of reduction). | |
| Notes | Number of participants in flow chart and text did not match with table of baseline characteristics in the paper. The former were assumed to be correct. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly assigned using a consecutive case allocation" (p.235). |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Unclear risk | Table 1 was not clear (data discrepancies in the article); 3 excluded participants (non adherence to study protocol) with no data. |
| Selective reporting (reporting bias) | High risk | No trial registration or protocol available. Pain perception reported for successful reduction only. |
| Other bias | High risk | Considerable baseline imbalance with respect to time since injury (mean time of injury: 6.58 versus 13.47 hours) probably due to outlier(s) (high SD). Care providers and provision of treatment seemed comparable. |
| Methods | Quasi‐randomised (according to day of admission). | |
| Participants | Tertiary care emergency department, Ankara, Turkey. October 2009 to October 2010. Inclusion criteria: age 0 to 6 years, written consent, 'nursemaid's elbow'. Exclusion criteria: localised elbow oedema, ecchymosis, deformity, fracture findings on x‐ray. 150 children enrolled. Mean age 27.5 months, range 6 to 72 months. | |
| Interventions | Hyperpronation: child's elbow held at 90° in one hand and then firmly pronating wrist (n = 68) Supination‐flexion: performed by holding the child's elbow at 90° with one hand, then firmly supinating the wrist, and by flexing the elbow so that the wrist was directed to the ipsilateral shoulder (n = 82). If first attempt unsuccessful (child did not reach for a toy or piece of candy within 10 minutes), after another 10 minutes a second attempt was made with same technique. If second attempt unsuccessful, the other technique was used. | |
| Outcomes | Success after first attempt, second attempt, third attempt, total. Pain (in 113 children who were older than 1 year and had a successful first attempt) using the mCHEOPS (modified Children's Hospital of Eastern Ontario Pain Scale). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "pseudorandomized ... according to date of admission to ED": |
| Allocation concealment (selection bias) | High risk | No concealment. |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol available. |
| Other bias | Unclear risk | The sex data in Table 1 in the article were incorrect; they reported data for 91 and 59 participants in the two groups. Care providers and provision of treatment seemed comparable. |
| Methods | Randomised trial. | |
| Participants | Emergency department of Samsun Training and Research Hospital, Turkey. Inclusion criteria: previously healthy children younger than 6 years, presenting with clinical findings suggestive of radial head subluxation (difficulty in moving elbow and painful pronation). Exclusion criteria: fracture, point tenderness, local ecchymosis (bruising) or oedema (swelling), deformity and persistent pain. 78 children enrolled (40 to hyperpronation, 38 to supination) (but see Notes below). (Of 78) 31 boys and 47 girls. | |
| Interventions | Hyperpronation (picture provided showed elbow held in slight flexion before hyperpronation at the wrist) (n = 40) Supination‐flexion (picture provided showed elbow held in slight flexion before supination at wrist and flexion) (n = 38). If first attempt unsuccessful after 20 minutes, a second attempt was made with same technique. If failure after 10 minutes from the second attempt, the other technique was used for the third attempt 15 minutes later. | |
| Outcomes | Success rate during first attempt (success was return to baseline function of the arm after 20 minutes), second attempt (same method, 10 minutes later), and third attempt (alternative method, 15 minutes later); need for latter was considered a 'failed reduction'. (However, two complete failures were excluded from the results). Pain before and after reduction: if child was able to communicate: faces rating scale (WBFPRS); if not: Face, Legs, Activity, Cry, Consolability Scale (FLACCS) scored by research assistant. | |
| Notes | Badly edited paper with multiple errors and typos. Number of participants unclear: 88 mentioned under study design and sum of people with different mechanism of injuries at end of results, but Tables 1 and 3 gave n = 78, and start of results paragraph was confusing. Table 1 gave baseline characteristics and also study results. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "via a randomizations table". |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Unclear risk | No loss to follow‐up but postrandomisation exclusions may have affected results. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol available. |
| Other bias | High risk | Median age in supination group 4 months older, no statistical testing done or possible. Poor reporting was likely to indicate other problems with this trial. Care providers and provision of treatment seemed comparable. |
| Methods | Randomised trial. | |
| Participants | Two urban paediatric emergency departments and two suburban paediatric ambulatory care centres in the USA (Texas and Colorado). Inclusion criteria: previously healthy, younger than 6 years with clinical findings suggestive of radial head subluxation. 90 episodes (in 85 participants) were included in randomisation, five were excluded because of a fracture, and one participant failed protocol. 34 boys and 51 girls. 28 (33%) reported a previous episode. | |
| Interventions | Hyperpronation: the child's elbow was gripped while held at 90° in one hand while forcefully pronating the wrist with the other hand (picture provided) (n = 41) versus Supination‐flexion: child's elbow gripped in one hand while the elbow was held at 90° and the wrist forcefully supinated with the other hand (picture provided) (n = 44). Participants were reexamined every 5 minutes throughout protocol for return of elbow function. Initial procedure repeated if no return of baseline function at 15 minutes. If failure of second attempt after 15 minutes, third attempt using alternative technique (cross‐over); fourth attempt also used alternative technique. Continued failure was followed by radiography of the elbow and treatment at discretion of emergency medicine physician. | |
| Outcomes | Success rate (success was return to baseline function of the arm after 15 minutes) at first attempt, second attempt with same procedure or third (and fourth) attempt with the other procedure. | |
| Notes | Five participants enrolled twice (in 4 participants, the episodes were more than 2 months apart and 1 participant presented after several days of normal usage of the arm), not accounted for clustering in analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Enrollees were randomly assigned to begin the protocol with either the hyperpronation technique or the supination technique via a randomizations table." |
| Allocation concealment (selection bias) | Low risk | "Technique assignment was unknown to the attending physician at the time of enrolment". |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Low risk | Data for all 90 participants were reported. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol available. |
| Other bias | Unclear risk | No baseline imbalance but data only reported for 85, not 90 participants. Care providers and provision of treatment seemed comparable. |
| Methods | Randomised trial. | |
| Participants | Emergency department of a tertiary care children’s hospital in Louisville, USA. Inclusion criteria: children younger than 7 years presenting with a complaint of an upper extremity injury and with refusal to use their arm. 148 participants enrolled, of whom 13 were excluded: 6 had a fracture; 2 spontaneously reduced; in 2 cases, the study protocol was not followed; and in 3 cases data were missing. 58 boys and 77 girls. Age range: 3 months to 6 years. | |
| Interventions | Rapid hyperpronation and flexion (n = 67) versus Rapid supination and flexion (n = 68). If failure (child unable to use his/her arm to reach for a toy or piece of candy within 30 minutes after manipulation) after first attempt, second attempt used same procedure and third attempt used the other procedure. | |
| Outcomes | Success rate (success was defined as using the arm to reach for a toy or piece of candy within 30 minutes after manipulation) after first attempt. If failed, second attempt used same procedure and third attempt used the other procedure. Pain during manipulation measured by the physician and the parent on an ordinal scale (0 = no pain, 1 = little pain, 2 = quite a lot of pain, 3 = very bad pain). Parents' scoring sheets were illustrated with descriptive drawings of facial expressions. | |
| Notes | Prior to the start of the study, physicians received a brief in‐service training on performing both reduction techniques. Printed instructions given on enrolment forms. Reductions were performed by students or residents (trainees). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | ".. blocked randomisation list generated by computer... trial was balanced after every 10 patients". |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Low risk | Low risk for primary outcome. Unclear for pain assessments: three participants missing in pronation group. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol available. |
| Other bias | Low risk | No important baseline imbalance. Care providers and provision of treatment seemed comparable. |
| Methods | Quasi‐randomised trial (odd or even days of hospital admission). | |
| Participants | Emergency department of a children’s hospital in Los Angeles, USA. Inclusion criteria: "all children who were diagnosed as having a radial head subluxation at discharge". 83 children with 87 episodes, 1 child with both arms affected. 36 boys and 51 girls (based on 87 episodes). Mean age 27 months, range 4.5 to 73 months. 26.7% reported a previous episode; however, this did not tally with the number of children with recurrent episodes; stated to be 19. | |
| Interventions | Supination of wrist, then elbow extended (n = 25) versus If first attempt failed (child failed to regain use of his or her arm) after 15 minutes, the other manoeuvre was tried. Obtaining radiographs or orthopaedic consultation were optional. Radiographs recommended if two reduction attempts failed or there was diagnostic uncertainty. | |
| Outcomes | Success after first maneuver and after second maneuver (waiting time 15 minutes). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised: allocation according to odd and even days of admission. |
| Allocation concealment (selection bias) | High risk | No concealment. |
| Blinding (performance bias and detection bias) | High risk | Participants: not possible. |
| Incomplete outcome data (attrition bias) | Unclear risk | For episodes treated according to protocol, but data for second attempts not provided. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or protocol available. |
| Other bias | High risk | Unknown number of cases not treated according to protocol, due to physician preference for supination‐flexion, resulting in skewed distribution (25 extension versus 51 flexion). Additionally,11/87 episodes could not be evaluated because another method was used or cases resolved spontaneously. |
SD: standard deviation
HP: hyperpronation
SF: supination‐flexion
ED: emergency department
mCHEOPS: modified Children's Hospital of Eastern Ontario Pain Scale
WBFPRS: Wong‐Baker Faces Pain Rating Scale
FLACCS: Faces, Legs, Activities, Cry Consolability Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Randomised trial which compared trained nurses performing hyperpronation to physicians performing their favourite technique. This was not a comparison of manipulative interventions. | |
| Neither randomised nor quasi‐randomised. Unclear how choice between treatments was made. | |
| Not comparing methods, but participant series (n = 41) of one method, a modified pronation technique. | |
| Not investigating methods to reduce the pulled elbow, but about subsequent management, including splinting. Not in scope of review. |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | An eligible comparison but unclear if actually "randomized" as claimed. |
| Participants | Emergency department of University Children's Hospital of Belgrade, Serbia. 54 children less than 4 years old with pulled elbow. |
| Interventions | Hyperpronation versus supination‐flexion. |
| Outcomes | Success evaluated by time to return to function, duration of child crying and palpable confirmation of successful reduction. Failure was another attempt using the other method because of non‐return of full function after 30 minutes. |
| Notes | This trial was only reported as a conference abstract. The trial authors referred to "preliminary results". A request for further information has been sent. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A clinical trial of pronation versus supination maneuvers for the reduction of the pulled elbow. |
| Methods | Randomised, single‐blind, trial. |
| Participants | Target: 90 children aged 6 months to 6 years. Inclusion criteria: Pulled elbow suspected in any child presenting one of the following:
Exclusion criteria:
|
| Interventions | Pronation versus supination. |
| Outcomes | Successful reduction (10 to 20 minutes). Pain of the procedure (1 to 5 minutes). |
| Starting date | June 2012 (see Notes). |
| Contact information | Carlos A Cuello‐Garcia, Instituto Tecnologico y de Estudios Superiores de Monterey, Mexico, email: [email protected]. |
| Notes | Email contact with Cuello‐Garcia (September 2014): study not started yet. Cuelle‐Garcia moved to Canada, former colleague plans to continue. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure: second attempt required Show forest plot | 8 | 811 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.25, 0.50] |
| Analysis 1.1 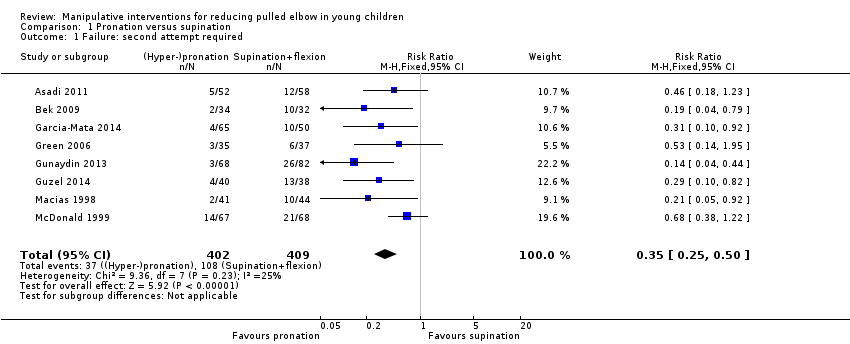 Comparison 1 Pronation versus supination, Outcome 1 Failure: second attempt required. | ||||
| 2 Failure: continued failure after second attempt with same procedure Show forest plot | 6 | 624 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.09, 0.32] |
| Analysis 1.2  Comparison 1 Pronation versus supination, Outcome 2 Failure: continued failure after second attempt with same procedure. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure: second attempt required Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Supination and extension versus supination then flexion, Outcome 1 Failure: second attempt required. | ||||
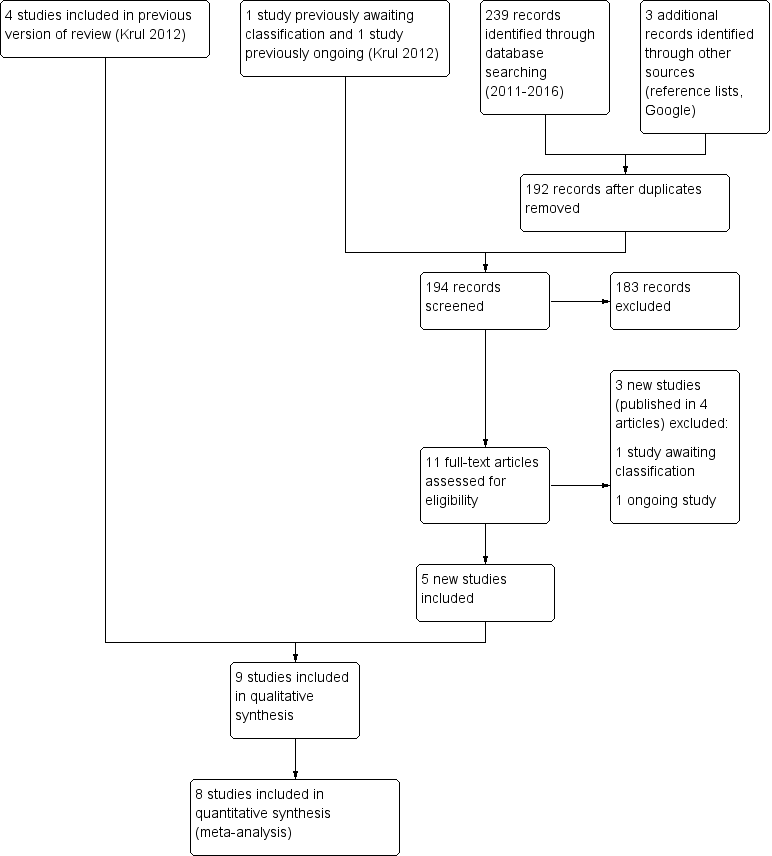
Study flow diagram
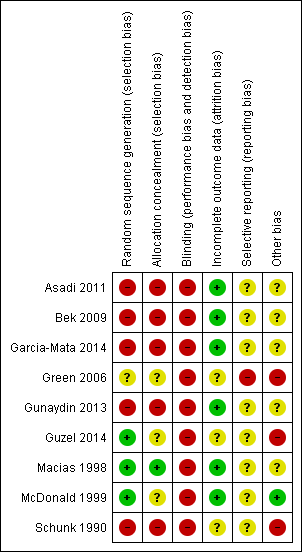
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
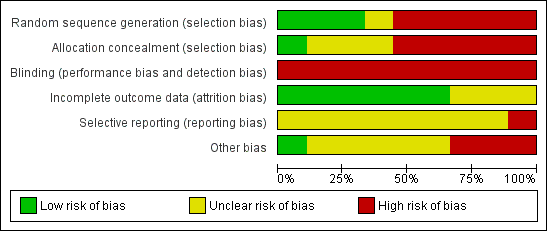
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Forest plot of comparison: 1 Pronation versus supination, outcome: 1.1 Failure: second attempt required.

Comparison 1 Pronation versus supination, Outcome 1 Failure: second attempt required.

Comparison 1 Pronation versus supination, Outcome 2 Failure: continued failure after second attempt with same procedure.

Comparison 2 Supination and extension versus supination then flexion, Outcome 1 Failure: second attempt required.
| Pronation compared with supination reduction techniques for pulled elbow in young children | ||||||
| Patient or population: Children with pulled elbow1 Settings: Emergency departments, ambulatory care centres or orthopaedic units Intervention: Pronation (all were hyperpronation) for first manipulation Comparison: Supination (all included flexion) for first manipulation | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Supination‐flexion | Hyperpronation | |||||
| Failure: second attempt required | 268 per 10002 | 94 per 1000 (67 to 134) | RR 0.35 (0.25 to 0.50) | 811 | ⊕⊕⊝⊝ | |
| Pain (preferably during the procedure) | see Comments | see Comments | see Comments | ⊕⊝⊝⊝ | Data for this outcome are incomplete and were measured in very different ways in four studies. | |
| Adverse effects (e.g. bruising) | see Comments | see Comments | None of the trials reported this outcome. | |||
| Failure: continued failure after second attempt using same procedure as before | 147 per 10002 | 24 per 1000 | RR 0.16 (0.09 to 0.32) | 624 | ⊕⊝⊝⊝ | This outcome represented the cumulative effect of two manipulations using hyperpronation versus cumulative effect of two manipulations using supination‐flexion. Reassuringly, both procedures when used again resulted in further successful reductions; these were proportionally greater with hyperpronation (64% versus 28%). However, the second attempt should not be considered independently of the first attempt and the characteristics of the children requiring a second attempt may have differed in important ways between the two groups. |
| Ultimate failure | see Comments | see Comments | Although potentially influenced by the initial (allocated) method of manipulation, this outcome reflected various manipulation protocols that stipulated the choice of method used for subsequent attempts. Overall failure at the end of the protocol ranged from 0 to 6 (4.1% of 148 episodes). | |||
| Recurrence (within one month) | see Comments | see Comments | None of the trials reported this outcome. | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1. Young children: typically aged under 7 years; mean age around 2 years. 2. Median control group (supination‐flexion) risk across studies 3. Evidence downgraded two levels for very serious risk of bias (selection and detection biases). 4. Evidence downgraded two levels for very serious risk of bias (selection, detection and incomplete outcome biases) and one level for inconsistency (two of the studies reported in favour of pronation, whereas two studies reported no difference between the procedures) 5. Evidence downgraded two levels for very serious risk of bias (and one level for imprecision (there were just 9 events in the hyperpronation group) | ||||||
| Radial head subluxation |
| Partial dislocation of the radial head peculiar to children |
| Dislocation of the head of the radius by elongation |
| Annular ligament displacement |
| Partial epiphyseal separation of the radial head |
| Anterior isolated subluxation of the radial head |
| Internal derangement of the elbow |
| Slipped elbow of young children |
| Painful elongation of young children |
| Painful paralysis in young children |
| Rotation syndrome |
| Painful pronation |
| Tamper tantrum elbow |
| Elbow sprain |
| Goyrands’s injury |
| Malaigne’s luxation |
| Gromeyer’s injury |
| Pronatio dolorosa infantum (Chassaignac) |
| Curbstone fracture |
| Supermarket elbow |
| Sunday (afternoon) arm |
| Housemaid’s elbow |
| Nursemaid’s elbow |
| Babysitter’s elbow |
| Sensitivity analysis | Results | NNT |
| Removal of quasi‐RCTs | RR 0.47, 95% CI 0.30 to 0.73; 370 participants; I2 = 13% | 8, 95% CI 5 to 17 |
| Removal of Green 2006 (baseline imbalance) | RR 0.34, 95% CI 0.24 to 0.49; 739 participants; I2 = 35% | 6, 95% CI 5 to 8 |
| Removal of 17 participants with prior manipulation in Garcia‐Mata 2014) | RR 0.35, 95% CI 0.24 to 0.50; 794 participants; I2 = 28% | 7, 95% CI 5 to 10 |
| Study | Outcome definition | Overall no. of failures / no. episodes | Protocol |
| Failure after 4 attempts | Not reported | 4 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | 0 / 66 (0%) | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | 3 / 115 (2.6%) | 3 attempts, cross‐over on 2rd attempt original method for 3rd attempt | |
| Failure after 2 attempts | 2 / 75 (2.7%) | 2 attempts, cross‐over on 2nd attempt | |
| Failure after 3 attempts | 0 / 150 (0%) | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 3 attempts | Not reported | 3 attempts, cross‐over on 3rd attempt | |
| Failure after 4 attempts | 1 / 90 (1.1%) | 4 attempts, cross‐over on 3rd attempt order same for 4th attempt | |
| Failure after 3 attempts | 6 / 148 (4.1%) | 3 attempts, cross‐over on 3rd attempt |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure: second attempt required Show forest plot | 8 | 811 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.25, 0.50] |
| 2 Failure: continued failure after second attempt with same procedure Show forest plot | 6 | 624 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.09, 0.32] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Failure: second attempt required Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |

