Administración de suplementos de vitamina D para la prevención de la mortalidad en adultos
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 208 healthy calcium‐replete, black postmenopausal African American women, 50 to 75 (mean 60) years of age. African American ancestry of the participants was assessed by self‐declaration that both parents and at least three of four grandparents were African American. Inclusion criteria: ambulatory postmenopausal African American women not receiving hormone therapy. Exclusion criteria: previous treatment with bone active agents and any medication or illness that affects skeletal metabolism. | |
| Interventions | Participants were randomly assigned to receive: Intervention group: vitamin D3 (800 IU) plus calcium (1200 to 1500 mg) daily, (n = 104); Control group: matched placebo plus calcium (1200 to 1500 mg) daily, (n = 104); for a two‐year period. After two years, the vitamin D3 dose was increased to 2000 IU daily in the intervention group, and the trial continued for an additional year. The calcium supplements were provided as calcium carbonate. | |
| Outcomes | The primary outcome measure was the bone mineral density of the total hip. | |
| Stated aim of study | "To examine the effect of vitamin D3 supplementation on bone loss in African American women." | |
| Notes | "81 participants from the intervention group and 78 participants form the control group completed two years in the trial. 81 participants from the intervention group switched to vitamin D3 2000 IU daily plus 1200 to 1500 mg of calcium daily after two years. 78 participants from the control group switched to matched placebo plus 1200 to 1500 mg of calcium daily after two years. 74 participants from the intervention group completed 36 months of trial. 74 participants from the control group completed 36 months of the trial. A total of 222 adverse events were reported in the trial over three years. There were 15 serious adverse events, eight in the intervention group and seven in the control group. Mean pill count compliance was 87% ± 8% of vitamin D3 pills consumed after the randomisation visit." Vitamin D3 capsules and matched placebo capsules were custom manufactured for the trial (Tishcon Corp, Westbury, NY). Vitamin D3 content was also analysed in an independent laboratory (Vitamin D, Skin, and Bone Research Laboratory, Department of Medicine, Boston University School of Medicine, Boston, Mass). The calcium supplements were provided as calcium carbonate." Additional information on the risk of bias domains was received through personal communication with Dr John F Aloia (30.01.2009; 03.02.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Vitamin D3 capsules and matched placebo capsules were custom manufactured for the trial (Tishcon Corp, Westbury, NY). |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised clinical trial using 2 x 2 factorial design. | |
| Participants | Country: United Kingdom. Number of participants randomised: 134, aged 70 years or over (mean age 77), 83% women. Inclusion criteria: people aged 70 years or over with an osteoporotic fracture within the last 10 years. Exclusion criteria: daily oral treatment with more than 200 IU (5 µg) vitamin D or more than 500 mg calcium or other bone active medications. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (800 IU) daily (n = 35); Intervention group 2: calcium (1000 mg) daily (n = 29); Intervention group 3: vitamin D3 (800 IU) plus calcium (1000 mg) daily (n = 35); Intervention group 4 (Control group): no tablets daily (n = 35); for a one‐year period. The calcium supplements were provided as calcium carbonate. | |
| Outcomes | Primary outcomes were recruitment, compliance, and retention within a randomised trial. | |
| Stated aim of study | "To assess the effects of an open trial design (without placebo and participants knowing what tablets they were given) when compared with a blinded, placebo‐controlled design on recruitment, compliance, and retention within a randomised trial of secondary osteoporotic fracture prevention." | |
| Notes | "All participants were asked to return unconsumed tablets for a tablet count compliance. Compliance amongst those who returned their tablet containers was similar (overall 85% versus 84.5% of tablet takers took their tablets on more than 80% of days). The same pattern was observed for self‐reported tablet consumption at four, eight or 12 months during the trial." "Shire Pharmaceuticals funded the capsules, which were co‐funded and manufactured by Nycomed." Additional information on mortality was received through personal communication with Dr Alison Avenell (28.01.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | High risk | Participants were told to which compound they had been allocated. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Participants were told to which compound they had been allocated. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | "Shire Pharmaceuticals funded the capsules, which were co‐funded and manufactured by Nycomed." |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised Evaluation of Calcium Or vitamin D (RECORD). Multicentre, randomised, double‐blind, placebo‐controlled trial using 2 x 2 factorial design. | |
| Participants | Country: United Kingdom. Number of participants randomised: 5292 people (85% women) aged 70 and over (mean 77 years) with low‐trauma, osteoporotic fracture in the previous 10 years. Inclusion criteria: elderly people aged 70 years or older, who were mobile before developing a low‐trauma fracture. Exclusion criteria: bed or chair bound before fracture; cognitive impairment indicated by an abbreviated mental test score of less than seven; cancer in the past 10 years that was likely to metastasise to bone; fracture associated with pre‐existing local bone abnormality; those known to have hypercalcaemia; renal stone in the past 10 years; life expectancy of less than 6 months; individuals known to be leaving the United Kingdom; daily intake of more than 200 IU vitamin D or more than 500 mg calcium supplements; intake in the past 5 years of fluoride, bisphosphonates, calcitonin, tibolone, hormone‐replacement therapy, selective oestrogen‐receptor modulators, or any vitamin D metabolite (e.g., calcitriol); and vitamin D by injection in the past year. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (800 IU) daily (n = 1343); Intervention group 2: calcium (500 mg) daily (n = 1311); Intervention group 3: vitamin D3 (800 IU) plus calcium (500 mg) daily (n = 1306); Intervention group 4 (Control group): matched placebo tablets (n = 1332); for a 45 month period. Participants were followed for a period of 6.2 years. Tablets varied in size and taste, and thus each had matching placebos. | |
| Outcomes | The primary outcome measure was all‐new low‐energy fractures including clinical, radiologically confirmed vertebral fractures, but not those of the face or skull. | |
| Stated aim of study | "To assess whether vitamin D3 and calcium, either alone or in combination, were effective in prevention of secondary fractures." | |
| Notes | "Compliance was measured by a postal questionnaire sent every four months, in which participants were asked how many days of the past seven days they had taken tablets. A randomly selected 10% sample was asked to return unused tablets for pill counting. Based on questionnaire responses at 24 months, 2886 (54,5%) of 5292 were still taking tablets. Throughout the trial about 80% of those taking tablets did so on more than 80% of days, which is consistent with pill counts in the subsample (data not shown). However, the number who were taking any tablets fell over time. At 24 months, 2268 of 4841 (46,8%), who returned questionnaires, had taken pills on more than 80% of days." Shire Pharmaceuticals co‐funded the drugs, with Nycomed, who also manufactured the drugs. Additional information received through personal communication with Dr Alison Avenell (02.02.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. "Allocation was controlled by a central and independent randomisation unit. The allocation programme was written by the trial programmer and the allocation remained concealed until the final analyses (other than for confidential reports to the data monitoring committee)." |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Shire Pharmaceuticals co‐funded the drugs, with Nycomed, who also manufactured the drugs. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (three intervention groups). | |
| Participants | Country: Denmark. Number of participants randomised: 240 healthy postmenopausal women, 58 to 67 (mean 62.5) years of age. Inclusion criteria: Caucasian background, age 58 to 67 years, good general health and postmenopausal status defined as cessation of menstrual bleeding for at least six months. Exclusion criteria: treatment with oestrogen or calcitonin during the previous 12 months or with bisphosphonates in the previous 24 months, presence of diseases known to affect bone metabolism, renal disease with serum creatinine above 120 mmol/L, and hepatic disease with increased alanine aminotransferase and/or decreased extrinsic coagulation factors II, VII and X. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (560 IU) plus calcium 1000 mg daily, (n = 80); Intervention group 2: vitamin D3 (560 IU) plus calcium (1000 mg) plus multivitamin containing retinol 800 μg; thiamine 1.4 mg; riboflavine 1.6 mg; pyridoxine 2 mg; cyanocobalamin 1 μg; folic acid 100 μg; niacin 18 mg; pantothenic acid 6 mg; biotin 150 μg; ascorbic acid 60 mg; D‐alpha tocopherol 10 mg; and phylloquinone 70 μg; daily, (n = 80); Intervention group 3 (Control group): matched placebo in a similar combination daily (n = 80); for a two‐year period. Participants were asked to take no calcium or vitamin D supplement other than the supplement supplied for the trial. Calcium was in the form of calcium carbonate. | |
| Outcomes | The primary outcome was changes from baseline in the bone mineral density (BMD) in the lumbar spine (L2–4). Secondary outcome measures were hip BMD, forearm BMD, serum calcium, serum phosphate and serum intact parathyroid hormone. | |
| Stated aim of study | "To evaluate the effect of vitamin D supplement and a calcium supplement plus or minus multivitamins on bone loss at the hip, spine, and forearm." | |
| Notes | "For all variables measured, authors observed no significant differences between the two experimental intervention groups. In presenting the results, authors, therefore, considered the two groups as one group. During the trial, 41 of the 240 women dropped out. No significant difference in drop‐out rate was found between the groups. One hundred and ninety‐nine women completed all visits. In the analysis, an additional two women were excluded due to development of radiologically verified vertebral fractures in the lumbar spine. No formal assessment of compliance, such as tablet counting, was made. At each visit, the participants were questioned about their compliance with the trial medication and encouraged to comply." All placebo and active treatment tablets were provided by Lube Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described |
| Selective reporting (reporting bias) | Unclear risk | Not all pre‐defined or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | All placebo and active treatment tablets were provided by Lube Ltd. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Switzerland. Number of participants randomised: 122 elderly women in long‐stay geriatric care, aged 60 years or older (mean age 85.3 years). Inclusion criteria: age 60 or older and the ability to walk three meters with or without a walking aid. Exclusion criteria: primary hyperparathyroidism, hypocalcaemia, hypercalciuria, renal insufficiency, and fracture or stroke within the last three months, any treatment with hormone replacement therapy, calcitonin, fluoride, or bisphosphonates during the previous 24 months. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (800 IU) plus calcium 1200 mg daily (n = 62); Intervention group 2 (Control group): calcium 1200 mg daily (n = 60); for a three‐month period. | |
| Outcomes | The primary outcome measure was number of falls per person. Secondary outcome measures were musculoskeletal function and bone remodeling. | |
| Stated aim of study | "To evaluate hypothesis that higher vitamin D serum levels may increase muscle strength and reduce the number of falls." | |
| Notes | "Tablets containing vitamin D and calcium or calcium alone were taken in the presence of the trial nurse to ensure compliance." The trial was supported by Strathmann AG, Germany. Authors reported deaths but not according to intervention group of the trial. All‐cause mortality data was taken from a Cochrane systematic review prepared by Avenell et al (Avenell 2009) who obtained mortality data by personal communication with Bischoff trial authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by sealed envelopes so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. "Tablets in both groups had an identical appearance. Participants, nurses, and all investigators were blinded to the intervention assignment throughout the trial." |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial was supported by Strathmann AG, Germany. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (three intervention groups). | |
| Participants | Country: Finland. Number of participants randomised: 218 chronically bedridden patients (81.7 % women), 65 to 104 (mean 84.5) years of age. Inclusion criteria: age over 65 years, chronically impaired mobility, stable general condition, and no known present disease (except osteoporosis) or medication (vitamin D supplements, glucocorticoids, antiepileptics, etc.) affecting calcium or bone metabolism. Exclusion criteria: markedly elevated creatinine levels (> 125 µmol/L) hypercalcaemia (ionised calcium > 1.32 mmol/L), hypothyroidism (thyrotropin > 5.3 mU/L) or hyperthyroidism (thyrotropin < 0.2 mU/L). | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (1200 IU) daily, (n = 73); 17 participants from this group received calcium 500 mg daily; Intervention group 2: vitamin D3 (400 IU) daily, (n = 77); 11 participants from this group received calcium 500 mg daily; Intervention group 3 (Control group): matched placebo vitamin D3 (0 IU) daily (n = 68), 15 participants from this group received calcium 500 mg daily; for a six‐month period. "Participants received vitamin D3 (Vigantol, Merck KGaA, Darmstadt, Germany 20,000 IU/ml in Migliol oil) in doses of 0 µg, 140 µg, or 420 µg (groups 1, 2, 3) every 2 weeks, equivalent with average daily intakes of 0 IU, 400 IU, or 1200 IU. To ensure that all three groups received identical volumes (26 drops = 0.84 ml), medication oil was diluted three‐fold with Migliol oil in group 2, and group 1 received plain Migliol oil. Furthermore, the oil was swallowed entirely in the presence of the nurse and given with a small amount of food or drink, if necessary." "Before the start of the intervention, the use of dairy products was roughly evaluated to be insufficient among 40 patients, who received a daily calcium carbonate substitution of 500 mg during the intervention. Three other patients also received a previous daily medication of 500 mg calcium carbonate at entry, which they continued to receive through the intervention." | |
| Outcomes | The primary outcome measures were parathyroid function and bone turnover. | |
| Stated aim of study | "To evaluate the effects of vitamin D supplementation on parathyroid function and bone turnover in aged, chronically immobile patients." | |
| Notes | "Vitamin D supplementation was well tolerated. One patient, however, developed a mild hypercalcaemia (ionised calcium from 1.24 to 1.40 mmol/L) in group 3." Treatment agents were produced by Vigantol, Merck KGaA, Darmstadt, Germany. Authors did not provide data about compliance. Additional information on the risk of bias domains was received through personal communication with Dr Mikko Björkman (31.01.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | "Allocation was controlled by coded bottles. Each bottle was individually coded to blind the participants and the ward nurses of not only the content of the bottles but also of the group labels (1, 2, 3)." |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Treatment agents were produced by Vigantol, Merck KGaA, Darmstadt, Germany. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo controlled trial using 2 x 2 factorial design. | |
| Participants | Country: United Kingdom. Number of participants randomised: 244 healthy, non‐osteoporotic women, aged 60 years or over (mean 68). Inclusion criteria: healthy, non‐osteoporotic women, aged 60 years or over. Exclusion criteria: clinical osteoporosis or chronic disease (e.g., diabetes mellitus, cardiovascular disease, cancer, fat malabsorption syndromes), routine medication that interferes with vitamin K, vitamin D, or bone metabolism (notably warfarin and steroids), and consumption of nutrient supplements that provided in excess of 30 µg vitamin K, 400 IU vitamin D, or 500 mg calcium daily. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (400 IU) plus calcium 1000 mg daily, (n = 62); Intervention group 2: vitamin D3 (400 IU) plus calcium 1000 mg plus vitamin K1 200 μg daily, (n = 61); Intervention group 3: vitamin K1 200 μg daily (n = 60); Intervention group 4 (Control group): matched placebo daily (n = 61); for a two‐year period. | |
| Outcomes | The primary outcome measure was bone mineral density. Secondary outcome measure was possible interaction with vitamin K, of vitamin D and calcium. | |
| Stated aim of study | "The putative beneficial role of high dietary vitamin K1 (phylloquinone) on bone mineral density and the possibility of interactive benefits with vitamin D were studied." | |
| Notes | "Of the 244 eligible women randomised in the trial, 209 (85.6%) completed the two‐year trial. Compliance with the trial intervention was good based on pill count (median, 99; interquartile range, 97.3 to 99.8%)." Hoffmann‐La Roche (Basel, Switzerland) provided the supplementation tablets. Additional information on mortality, adverse events, and risk of bias domains was received through personal communication with Dr Martin J Shearer (03.02.2009; 05.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. "An independent statistician at Hoffmann‐La Roche, who had no other connection to the trial, provided a randomisation list to the researchers." |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Hoffmann‐La Roche (Basel, Switzerland) provided the supplementation tablets. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Multicentre, randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: France. Number of participants randomised: 192 women with a 25‐hydroxyvitamin D level ≤ 12 ng/mL, mean age 74.6 years. Inclusion criteria: community‐dwelling ambulatory women aged > 65 years who spontaneously consulted a practitioner and presented with vitamin D insufficiency (i.e., serum 25‐hydroxy vitamin D ≤ 12 ng/mL). Exclusion criteria: hypercalcaemia (serum calcium > 2.62 mmol/L), primary hyperparathyroidism, renal insufficiency (serum creatinine >130 pmol/L), hepatic insufficiency, treatment with a bisphosphonate, calcitonin, vitamin D or its metabolites, oestrogen, raloxifene, fluoride, anticonvulsives, or any other drug acting on bone metabolism (e.g., glucocorticoids) in the past six months. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (800 IU) plus calcium (1000 mg) daily (n = 95); Intervention group 2 (Control group): matched placebo tablets (n = 97); for a one‐year period. | |
| Outcomes | The primary outcome was to assess the effects of vitamin D3 plus calcium on bone mineral density and biochemical markers of bone formation and resorption. Secondary outcome was to evaluate the clinical and laboratory safety of treatment. | |
| Stated aim of study | "An evaluation of the clinical and laboratory safety of a one‐year course of treatment with a combination vitamin D and calcium tablets in ambulatory women aged > 65 years with vitamin D insufficiency." | |
| Notes | Fifty women (21/95 vitamin D plus calcium, 29/97 placebo) were prematurely withdrawn from the trial for various reasons. Treatment‐related adverse events were reported in 21 and 23 women in the respective intervention groups. These events consisted mainly of metabolic disorders (9 and 10), particularly hypercalcaemia (6 and 8) and gastrointestinal disorders (9 and 8). "Treatment compliance was assessed at each visit based on counts of the number of tablets taken compared with the number that was to be taken. Compliance at each visit ranged from a median of 93% to 94% in the vitamin D plus calcium group and from 93% to 96.5% in the placebo group. Global compliance was 92% in the vitamin D plus calcium group and 92.5% in the placebo group. No significant difference in compliance was observed between the two groups at any visit." This trial was supported by Innothera Laboratories, Arcueil, France. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | This trial was supported by Innothera Laboratories, Arcueil, France. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (five intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 124 nursing home residents (73% women), mean 89 years of age. Inclusion criteria: a life expectancy of at least six months, the ability to swallow medication, and three months residency at Hebrew Rehabilitation Center for the Aged. Exclusion criteria: use of glucocorticoids, anti‐seizure medication, or pharmacological doses of vitamin D; calcium metabolism disorders; severe mobility limitations; or fracture within the previous six months. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 (800 IU) daily (n = 23); Intervention group 2: vitamin D2 (600 IU) daily (n = 25); Intervention group 3: vitamin D2 (400 IU) daily (n = 25); Intervention group 4: vitamin D2 (200 IU) daily (n = 26); Intervention group 5 (Control group): matched placebo tablets daily (n = 25); for a five‐month period. | |
| Outcomes | The primary outcome measure was effect of the vitamin D doses on falls over the trial period. | |
| Stated aim of study | "To determine the effect of four vitamin D supplement doses on the risk of falls in elderly nursing home residents." | |
| Notes | "Over the 5‐month trial period, 114 completed the trial. Of the 10 participants who did not complete the trial, seven died and three withdrew. There were no significant differences between the intervention groups in the number who did not complete the 5‐month trial period with a loss of one to three participants from each intervention group." "Compliance was calculated as the number of pills taken, as determined according to blister pack counts after the completion of the trial divided by the total days a participant was actively participating (alive, living at Hebrew Rehabilitation Center for Aged, not withdrawn from the trial)." "Average compliance was 97.6%, with only two participants having a compliance level of less than 50%. Compliance did not differ between the intervention groups." The vitamin D2 tablets were purchased from Tishcon Corporation (Westbury, NY). Vitamin D content of the supplements was verified at the BU Vitamin D Laboratory. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. "The pharmacy of The Hebrew Rehabilitation Center for the Aged randomised participants in blocks of 15 to one of the five intervention groups." |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. "The pharmacy labelled pill blister packs with names and patient identification numbers only. Blister packs and tablets from all five groups were identical in appearance and taste, so nursing staff, participants, and the trial team were unaware of the group assignment." |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The vitamin D2 tablets were purchased from Tishcon Corporation (Westbury, NY). |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Sweden. Number of participants randomised: 100 (68 % women), aged 18 to 69 years (mean age 52). Inclusion criteria: ambulatory patients with rheumatoid arthritis of at least two years duration. Exclusion criteria: patients with steroid, gold, or antimalaria therapy. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (100,000 IU) daily (n = 25); Intervention group 2 (Control group): placebo daily (n = 25); for a one year period. | |
| Outcomes | The primary outcomes were subjective an objective improvement. | |
| Stated aim of study | To determine the effect of vitamin D supplementation on objective and subjective improvement of patients with rheumatoid arthritis. | |
| Notes | The trial was supported financially by a grant from Ekhagastiftelsen. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised, but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised, but the method used to conceal the allocation was not described so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | There is insufficient information to assess whether the type of blinding used is likely to induce bias on the estimate of effect. |
| Incomplete outcome data (attrition bias) | Low risk | The underlying reasons for missing data are unlikely to make treatment effects depart from plausible values. |
| Selective reporting (reporting bias) | Unclear risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial was supported financially by a grant from Ekhagastiftelsen. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 205 (59 % women), aged 65 years or over (mean age 83), acute admissions to a geriatric medical unit. Inclusion criteria: patients newly transferred or admitted into the general assessment and rehabilitation wards in an acute geriatric unit aged 65 years or over. Exclusion criteria: known hypercalcaemia, urolithiasis or renal dialysis therapy, terminal or bed‐bound patients with a reduced Glasgow Coma Scale, those already prescribed vitamin D supplements and calcium, and those who were deemed 'nil by mouth'. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (800 IU) plus calcium (1200 mg) daily (n = 101); Intervention group 2 (Control group): calcium (1200 mg) daily (n = 104); for a 30‐day period. | |
| Outcomes | The primary outcomes were numbers of fallers and falls. | |
| Stated aim of study | "To determine whether routine supplementation with vitamin D plus calcium reduces numbers of fallers and falls in a cohort of hospital admissions while they are inpatients." | |
| Notes | "Vitamin D and calcium were well tolerated in the total trial cohort with a median compliance level of 88%." Strakan Pharmaceuticals supplied all trial drugs free of charge. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using a random number table. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. Randomisation was known only to the statistician and pharmacist. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. "Statistician and pharmacist subsequently issued an appropriate uniquely numbered drug blister pack to each patient's ward. Thereafter, trained staff nurses administered trial drugs as part of routine drug rounds. The researchers, therapists, and patients remained blinded to trial drug allocation." |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Strakan Pharmaceuticals supplied all trial drugs free of charge. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised controlled trial using 2 x 2 factorial design. The VIP (visual impairment) trial. | |
| Participants | Country: New Zealand. Number of participants randomised: 391 elderly people (68 % women) aged 75 to 96 (mean 83.6) years, with visual acuity of 6/24 or worse, who were living in the community. Inclusion criteria: elderly people aged 75 years or over with visual acuity of 6/24 or worse who were living in the community. Exclusion criteria: those who could not walk around their own residence, who were receiving physiotherapy at the time of recruitment, or could not understand the trial requirements. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: home safety assessment and modification programme delivered by an occupational therapist (n = 100); Intervention group 2: an exercise programme prescribed at home by a physiotherapist plus vitamin D3 100,000 IU initially and then 50,000 IU monthly (n = 97); Intervention group 3: both interventions (intervention 1 plus intervention 2) (n = 98); Intervention group 4 (Control group): social visits (n = 96); for a one‐year period. The one‐year exercise intervention consisted of the specific muscle strengthening and balance retraining exercises that progress in difficulty and a walking plan, modified for those with severe visual acuity loss, with vitamin D supplementation. The home safety assessment and modification programme was specifically designed for people with severe visual impairments. The occupational therapist visited the person at home and used a home safety assessment checklist to identify hazards and to initiate discussion with the participant about any items, behaviour, or lack of equipment that could lead to falls. Research staff made two home visits lasting an hour each during the first six months of the trial to participants in intervention group four. | |
| Outcomes | The primary outcome measures were number of falls and number of injuries resulting from falls. Secondary outcome measure was costs of implementing the home safety programme. | |
| Stated aim of study | "To assess the efficacy and cost effectiveness of a home safety programme and a home exercise programme to reduce falls and injuries in older people with poor vision." | |
| Notes | Additional information received through personal communication with Professor John Campbell (19.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using a random number table. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. "The schedule was held by an independent person at a separate site and was accessed by a research administrator for the trial, who telephoned after each baseline assessment was completed. The administrator then informed the occupational therapist, physiotherapist, or social visitor, who delivered the assigned intervention to that participant where possible within the next two weeks." |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Low risk | The trial is not funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Vitamin D, Calcium, Lyon Study I (DECALYOS I). Randomised, double‐blind, placebo controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: France. Number of participants randomised: 3270, 69 to 106 (mean 84) years of age, healthy ambulatory women. Inclusion criteria: ambulatory woman (with activity levels ranging from going outdoors easily to walk indoors with a cane or a walker), with no serious medical conditions, and with a life expectancy of at least 18 months. Exclusion criteria: receiving drugs known to alter bone metabolism, such as corticosteroids, thyroxine, or anticonvulsant drugs within the past year, women who had been treated with fluoride salts for more than three months, or with vitamin D or calcium during the previous six months or for more than one year within the past five years. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (800 IU) plus calcium (1200 mg) daily (n = 1634); Intervention group 2 (Control group): double placebo daily (n = 1636); for a 18 month period. Participants were followed for four years. Calcium was in a form of tricalcium phosphate powder in an aqueous suspension. Placebo pills contained lactose and suspension of lactose, kaolin, and starch. The supplements were taken in the presence of a nurse to ensure compliance. | |
| Outcomes | The primary outcome was frequency of hip fractures and other nonvertebral fractures, identified radiologically. | |
| Stated aim of study | "To evaluate if vitamin D and calcium supplements reduce the risk of hip fractures and other nonvertebral fractures identified radiologically." | |
| Notes | Duphar and Company Laboratories provided the vitamin D3 (Devaron), and Merck‐Clevenot Laboratories provided the tricalcium phosphate (Ostram). Additional information on mortality was received through personal communication with Professor Pierre Meunier (27.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Duphar and Company Laboratories provided the vitamin D3 (Devaron), and Merck‐Clevenot Laboratories provided the tricalcium phosphate (Ostram). |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Vitamin D, Calcium, Lyon Study II (DECALYOS II). Multicenter, randomised, double‐blind, placebo controlled trial using parallel group design (three intervention groups). | |
| Participants | Country: France. Number of participants randomised: 610, 64 to 99 (mean 85) years of age, healthy ambulatory women. Inclusion criteria: ambulatory woman (able to walk indoors with a cane or a walker) and life expectancy of at least 24 months. Exclusion criteria: intestinal malabsorption, hypercalcaemia (serum calcium 42.63 mmol/L) or chronic renal failure (serum creatinine 4150 mmol/L), receiving drugs known to alter bone metabolism, such as corticosteroids, anticonvulsants, or a high dose of thyroxine within the past year, treatments with fluoride salts (43 months), bisphosphonates, calcitonin (41 month), calcium (4500 mg/day), and vitamin D (4100 IU/day) during the last 12 months. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (800 IU) plus calcium (1200 mg) daily (fixed combination) (n = 199); Intervention group 2: vitamin D3 (800 IU) plus calcium (1200 mg) daily (separate combination) (n = 194); Intervention group 3 (Control group): double placebo daily (n = 190); for a two‐year period. "The sachet of the calcium–vitamin D3 fixed combination (Ostram–vitamin D3, Merck KGaA) contains a fixed combination of 1200 mg elemental calcium in the form of tricalcium phosphate and 800 IU of vitamin D3. The calcium (Ostram, Merck KGaA) contains 1200 mg of elemental calcium in the form of tricalcium phosphate. Vitamin D3 (Devaron, i.e., cholecalciferol, Duphar Solvay) was given in two pills of 400 IU each. Each day women in intervention groups one and two received 1200 mg of elemental calcium and 800 IU of vitamin D3 given either by a sachet of calcium–vitamin D3 fixed combination (Ca–D3 group) or as a sachet of calcium and two tablets of vitamin D3 (Ca+D3 group). The other women received a placebo of vitamin D3 and calcium (one sachet containing lactose, microcrystalline cellulose and the same excipient as the active treatment and two tablets of vitamin D3 placebo)." | |
| Outcomes | The primary outcomes were biochemical variables of calcium homeostasis, femoral neck bone mineral density, and hip fracture risk. | |
| Stated aim of study | "To confirm the effects of combined vitamin D supplementation and calcium on biochemical variables of calcium homeostasis, femoral neck bone mineral density, and hip fracture risk." | |
| Notes | "The supplements were taken in the presence of a nurse to ensure compliance. The mean compliance was more than 95% for both sachets and tablets in each treatment group." The trial was sponsored by MERCK KGaA, Darmstadt, Germany. Additional information on mortality was received through personal communication with Professor Pierre Meunier (27.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial was sponsored by MERCK KGaA, Darmstadt, Germany. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (six intervention groups). | |
| Participants | Country: the Netherlands. Number of participants randomised: 338 (77% women), aged 70 years or over (mean age 84), nursing home residents. Inclusion criteria: nursing home residents aged 70 years or over. Exclusion criteria: going outside in the sunshine more than once a week, the use of vitamin D or calcium supplementation, the use of more than one vitamin D fortified food or drink per day, complete immobilisation and a very poor life expectancy. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (600 IU) daily (n = 55); Intervention group 2 (control group): matched placebo tablet daily (n = 57); Intervention group 3: vitamin D3 (4200 IU) weekly (n = 54); Intervention group 4 (Control group): matched placebo tablets weekly (n = 58); Intervention group 5: vitamin D3 (18,000 IU) powder monthly (n = 57); Intervention group 6 (Control group): matched placebo powder monthly (n = 57); for a four and a half month period. The treatment period of four and a half months was completed by 276 out of 338 participants. The 276 participants who completed the vitamin D intervention trial were randomly assigned to receive: Intervention group: calcium 800 mg or 1600 mg daily (n = 138); Control group: matched placebo tablet daily (n = 138); for the period of 4 months. The treatment was completed by 269 participants. The first 156 randomised participants received 800 mg calcium carbonate or placebo; the subsequent 120 participants received 1600 mg calcium carbonate or placebo. | |
| Outcomes | The primary outcome was to assess efficacy of different doses and intervals of oral vitamin D3 supplementation with the same total dose. Secondary outcome measure was to assess the additional effect of calcium supplementation following vitamin D supplementation on serum parathyroid hormone and markers of bone turnover. | |
| Stated aim of study | "To investigate, in a Dutch nursing home population, whether there is a difference in efficacy of different doses and intervals of oral vitamin D3 supplementation with the same total dose compared with placebo. A second aim was to assess the additional effect of calcium supplementation following vitamin D supplementation on serum parathyroid hormone and markers of bone turnover." | |
| Notes | "The trial medication was centrally distributed to ensure compliance. Random samples of the returned medication were counted in order to verify compliance." "The compliance assessed within 96 random samples of the returned medication was good. In the daily administration group, all 33 participants were compliant, used at least 80% of the tablets. For weekly administration, 80% of the 35 participants were compliant, used at least 80% of the tablets. For monthly administration, 93% of the 28 participants were compliant, used at least four out of five powders." Solvay Pharmaceuticals supplied the research medication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Solvay Pharmaceuticals supplied the research medication. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 46 (2% women), aged 70 years an older (mean age 80). Inclusion criteria: community‐dwelling elderly veterans living in south Florida who were aged 70 and older. Exclusion criteria: current users of vitamin D or corticosteroids; or had hypo‐ or hypercalcaemia, hypercalciuria, hyperparathyroidism, chronic serum creatinine greater than 2.0 mg/dL, or cholestatic liver disease; or were unable to take medication daily. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (2000 IU) daily (n = 23); Intervention group 2 (Control group): placebo daily (n = 23); for a one year period. The 41 participants found to have inadequate calcium intake (< 1200 mg/d) according to dietary questionnaire were also dispensed a calcium supplement to provide adequate daily intake. | |
| Outcomes | The primary outcomes were serum calcium, 25‐hydroxyvitamin D, parathyroid hormone, and 24‐hour urinary calcium. | |
| Stated aim of study | "To determine the prevalence of hypovitaminosis D (serum 25‐hydroxyvitamin D < 32 ng/mL; HVD) in a population of elderly veterans and conduct a preliminary assessment of the efficacy of supplementation with cholecalciferol in correcting HVD". | |
| Notes | Carlson Laboratories donated the cholecalciferol and placebo capsules. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) | Low risk | There is insufficient information to assess whether the missing data mechanism in combination with the method used to handle missing data are likely to induce bias on the estimate of effect. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Carlson Laboratories donated the cholecalciferol and placebo capsules. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Australia. Number of participants randomised: 187 healthy, white, postmenopausal women, mean age 56 years. Inclusion criteria: healthy, white women who were postmenopausal for one to ten years, and who were not receiving hormone replacement therapy. Exclusion criteria: malignant disease, renal, hepatic, endocrine, or gastrointestinal disorder associated with abnormal calcium metabolism, use of oestrogen, progesterone, glucocorticoids, anticonvulsants, thiazide diuretics, vitamin D supplements, or other medications known to affect calcium or bone metabolism in the previous 12 months. Participants with laboratory evidence of renal, hepatic, or endocrine disorder; a serum follicle‐stimulating hormone concentration < 40 mIU/mL, or bone mineral density at any site ± two standard deviation from the mean for potential participant matched for age were also excluded. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 (10,000 IU) weekly plus calcium (1000 mg) daily (n = 93); Intervention group 2 (Control group): calcium (1000 mg) daily (n = 94); for a two‐year period. Calcium was in a form of tricalcium phosphate powder in an aqueous suspension. | |
| Outcomes | The primary outcome was bone mineral density. | |
| Stated aim of study | "To examine the effects of vitamin D2 supplementation on changes in bone mineral density in younger (age: 56 years) postmenopausal women who were also given 1000 mg calcium daily and to compare those changes with the changes in bone mineral density in women given 1000 mg calcium daily only." | |
| Notes | "Compliance was assessed by tablet counts and diary review. Compliance with treatment was 98.2 ± 6.1% for the calcium plus vitamin D group and 97.7 ± 5.4% for the calcium group." Vitamin D2 was provided by Ostelin; Boots Healthcare Pharmaceuticals, Sydney, Australia. Calcium carbonate was provided by Cal‐Sup; 3M Pharmaceutical, Sydney, Australia. Additional information on mortality and risk of bias domains was received through personal communication with Professor Philip Clifton‐Bligh (12.11.2007; 08.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Vitamin D2 was provided by Ostelin; Boots Healthcare Pharmaceuticals, Sydney, Australia. Calcium carbonate was provided by Cal‐Sup; 3M Pharmaceutical, Sydney, Australia. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised double‐blind placebo controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 82, elderly hospital patients (78% women), mean age 82.4 years. Inclusion criteria: elderly hospital patients. Exclusion criteria: overt clinical osteomalacia, either plasma calcium less than 1.95 mmol/L or Looser's zones, or on calciferol therapy; a judgement that he or she was unlikely to be able to co‐operate in the trial; plasma creatinine more than 150/mmol/L, potassium less than 3.3 mmol/L; plasma 25(OH)D more than 40nmol/L (16ng/ml); refused consent or unable to give informed consent. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 (9000 IU) daily (n = 32); Intervention group 2 (Control group): matching placebo tablets daily (n = 33); for a nine‐month period. Placebo tablets were identical in appearance to the vitamin D2 tablets containing lactose. | |
| Outcomes | The primary outcome measure was abilities of elderly hospital patients to carry out basic activities of daily life. | |
| Stated aim of study | "To evaluate the effect of oral vitamin D supplements on the ability of elderly hospital patients with low or low normal plasma 25(OH)D to perform basic activities of daily living." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The source of funding is not clear. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Australia. Number of participants randomised: 167 ambulatory community living men 50 to 87 (mean 61.9) years of age. Inclusion criteria: ambulatory community living men aged 50 years or over. Exclusion criteria: taking calcium and/or vitamin D supplements in the preceding 12 months, participating in regular high‐intensity resistance training in the previous six months or more, then 150 minutes a week of moderate‐ to high‐impact weight‐bearing exercise, had a body mass index > 35 kg/m2, lactose intolerance, consuming more than four alcoholic beverages per day, a history of osteoporotic fracture or medical disease, or medication use that is known to affect metabolism of bones. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: calcium‐vitamin D3‐fortified milk containing vitamin D3 (800 IU) plus calcium (1000 mg) daily (n = 85); Intervention group 2 (Control group): usual diet (n = 82); for a two‐year period. Participants were followed for additional a year and a half. | |
| Outcomes | The primary outcome measure was bone mineral density. | |
| Stated aim of study | "To assess the effects of calcium and vitamin D3 fortified milk on bone mineral density in community living men > 50 years of age." | |
| Notes | "To monitor milk compliance, participants were asked to record the number of tetra packs consumed per day on a compliance calendar, which was collected and checked every three months. Compliance proportion (expressed as a percentage) was calculated as the actual number of tetra packs consumed, divided by the expected consumption each month. The overall mean reported milk compliance, calculated as the percentage of the tetra packs consumed and based on daily diaries was 85.1%. Milk was specifically formulated by Murray Goulburn Cooperative Co. (Brunswick, Australia). The added milk calcium salt (Natra‐Cal) was prepared by Murray Goulburn Cooperative Co. The vitamin D (Vitamin D3) used to fortify the milk was obtained from DSM Nutritional Products Pty (NSW, Australia)." Additional information on mortality was received through personal communication with Professor Robin Daly (04.02.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using a random number table. |
| Allocation concealment (selection bias) | High risk | The allocation sequence was known to the investigators who assigned participants. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The vitamin D (Vitamin D3) used to fortify the milk was obtained from DSM Nutritional Products Pty (NSW, Australia). |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Boston STOP IT (Sites Testing Osteoporosis Prevention Intervention Treatment). Randomised, double‐blind, placebo controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 389, healthy, ambulatory participants (55% women), aged 65 years or older (mean 71). Inclusion criteria: healthy, ambulatory men and women 65 years of age or older. Exclusion criteria: current cancer or hyperparathyroidism; a kidney stone in the past five years; renal disease; bilateral hip surgery; therapy with a bisphosphonate, calcitonin, oestrogen, tamoxifen, or testosterone in the past six months or fluoride in the past two years; femoral‐neck bone mineral density more than 2 SD below the mean for participants of the same age and sex; dietary calcium intake exceeding 1500 mg per day; and laboratory evidence of kidney or liver disease. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (700 IU) plus calcium (500 mg) daily (n = 187); Intervention group 2 (Control group): matched placebo tablets daily (n = 202); for a three‐year period. Calcium was in the form of calcium citrate malate. Placebo pills contained microcrystalline cellulose. | |
| Outcomes | The primary outcome measures were bone mineral density, biochemical measures of bone metabolism, and the incidence of nonvertebral fractures. | |
| Stated aim of study | "To examine the effects of combined vitamin D supplementation and calcium on bone loss, biochemical measures of bone metabolism, and the incidence of nonvertebral fractures in men and women 65 years of age or older who were living in the community." | |
| Notes | Procter & Gamble, Cincinnati manufactured calcium tablets. Additional information on mortality was received through personal communication with Professor Bess Dawson‐Hughes (04.02.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Procter & Gamble, Cincinnati manufactured calcium tablets. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Switzerland. Number of participants randomised: 378 (51% women), mean age 71 years, community‐dwelling elderly people. Inclusion criteria: community‐dwelling elderly people who are mobile and have an independent life style. Exclusion criteria: primary hyperparathyroidism, polyarthritis or inability to walk, calcium intake by supplement of more than 500 mg daily, vitamin D intake of more than 200 IU daily, active kidney stone disease, history of hypercalcuria or cancer or other incurable diseases, dementia, elective surgery within the next three months, severe renal insufficiency (creatinine clearance < 20 mL/min, and fracture or stroke within the last 3 months. Calcium supplementation of 500 mg/d or less was accepted. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: 1 α(OH)D3 (alfacalcidol), (1 μg) daily (n = 192); Intervention group 2 (Control group): placebo (n = 186); for a nine‐month period. | |
| Outcomes | The primary outcome measure was number of fallers. Secondary outcome measures were muscle strength, balance, blood pressure, and bone quality. | |
| Stated aim of study | "To evaluate whether treatment with alfacalcidol, a precursor of the D hormone calcitriol, reduces the number of fallers and falls in community‐dwelling men and women." | |
| Notes | Trial medication was provided by TEVA Pharmaceuticals Industries Ltd, Israel. Additional information on the risk of bias domains was received through personal communication with Dr Laurent C Dukas (28.01.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. "An independent statistical group performed the blinding and randomisation. All investigators and staff conducting the trial remained blinded throughout the intervention period." |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Trial medication was provided by TEVA Pharmaceuticals Industries Ltd, Israel. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Australia. Number of participants randomised: 625, older residents (mean age 83.4), 95% females, with serum 25‐hydroxyvitamin D levels between 25 and 90 nmol/L. Inclusion criteria: older people resident in hostels and nursing homes with serum 25‐hydroxyvitamin D levels between 25 and 90 nmol/L. Exclusion criteria: use of agents that could affect bone and mineral metabolism, such as warfarin, chronic heparin therapy, vitamin D therapy within the previous three months, glucocorticoids at an average daily dose of greater than 5 mg prednisolone (or equivalent) for more than one month within the preceding year, current use of bisphosphonates, and hormone replacement therapy, thyrotoxicosis within the previous three years, primary hyperparathyroidism treated within the previous three years, multiple myeloma, Paget’s disease of bone, history of malabsorption, intercurrent active malignancy, and other disorders affecting bone and mineral metabolism. | |
| Interventions | Participants were randomly assigned to receive: Intervention group: vitamin D3 (10000 IU) weekly until November 1998 and thereafter vitamin D31000 IU daily plus calcium (600 mg) daily (n = 313); Control group: calcium (600 mg) (n = 312); for a two‐year period. | |
| Outcomes | The primary outcomes were falls and fractures. | |
| Stated aim of study | "To test whether administration of vitamin D could reduce the incidence of falls and fractures in nursing home residents." | |
| Notes | "Supplements and placebos were purchased commercially, and the suppliers played no role in the trial design or in the collection, analysis, or interpretation of data." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. An individual who was not involved in contact with the participants or the residential care institutions performed randomisation. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. "Participants were randomised to receive sequentially numbered bottles containing vitamin D or placebo. Both interventions had matching placebo preparations given in identical fashion, and residents, institutional staff, and trial staff were blinded to treatment allocation." |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Low risk | The trial is not funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Sites Testing Osteoporosis Prevention / Intervention Treatment (STOP IT). Randomised, double‐blind, placebo‐controlled trial using 2 x 2 factorial design. | |
| Participants | Country: United States. Number of participants randomised: 489 healthy elderly women 65 to 77 (mean 71.5) years of age. Inclusion criteria: healthy elderly women 65 to 77 years of age and femoral neck density within the normal range for their age. Exclusion criteria: severe chronic illness, primary hyperparathyroidism or active renal stone disease, and were on certain medications, such as bisphosphonates, anticonvulsants, oestrogen, fluoride, or thiazide diuretics in the previous 6 months. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: calcitriol (0.5 μg) daily (n = 123); Intervention group 2: conjugated oestrogens (Premarin) 0.625 mg/daily plus medroxyprogesterone acetate (Provera) 2.5 mg daily (n = 121); Intervention group 3: calcitriol (0.5 μg) plus conjugated oestrogens daily; (Premarin) 0.625 mg/daily plus medroxyprogesterone acetate (Provera) 2.5 mg daily (n = 122); Intervention group 4 (Control group): matched placebo daily (n = 123); for a three‐year period. | |
| Outcomes | The primary outcome measure was the change in bone mineral density of the femoral neck and spine. Secondary outcome measure was incidence of nonvertebral fractures. | |
| Stated aim of study | "To examine the effect of oestrogen and 1,25‐dihydroxyvitamin D therapy given individually or in combination on bone loss in elderly women." | |
| Notes | "Compliance to trial medication was evaluated by pill counts. At 36 months, treatment group differences in adherence to assigned therapy were evident, with 78% of those assigned to placebo, 70% of those assigned to calcitriol, 65% of those assigned to HRT/ERT and 62% of those assigned to HRT/ERT calcitriol still adherent to their assigned medication. Among those still on medication the compliance for the groups calculated at six months and compared with 36 months, respectively, was: conjugated estrogens, 86% and 92%; medroxyprogesterone acetate, 91% and 94%; calcitriol, 87% and 93%; placebos, 94% and 92%." The active trial drug and placebo were supplied by Wyeth‐Ayerst Laboratories, Inc Pharm, Hoffman‐LaRoche Inc and Pharmacia & Upjohn, Inc. Additional information on mortality and risk of bias domains was received through personal communication with Dr John Gallagher (09.02.2009; 11.03.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. An independent statistical group performed the blinding and randomisation. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The active trial drug and placebo were supplied by Wyeth‐Ayerst Laboratories, Inc Pharm, Hoffman‐LaRoche Inc and Pharmacia & Upjohn, Inc. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Australia. Number of participants randomised: 686 community‐dwelling ambulant women aged over 70 years (mean 76.7). Inclusion criteria: age over 70 years, registration with a general practitioner, and likelihood, in the investigators’ opinion, of attending four study visits over 9 months. Exclusion criteria: consumption of vitamin D supplementation either in isolation or as part of a combination treatment; e.g., Actonel combi +D or Fosamax plus, cognitive impairment (Mini Mental State Score < 24), and individuals who in the investigators’ opinion would not be | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: cholecalciferol 150,000 three‐monthly (n = 353); Intervention group 2 (Control group): placebo vitamin D three‐monthly (n = 333); for a nine‐month period. | |
| Outcomes | The primary outcome measures were falls, muscle strength, and mobility. Secondary outcome measures were serum 25‐hidrohyvitamin D levels, and adverse events. | |
| Stated aim of study | "to evaluate the effects of cholecalciferol treatment and lifestyle advice compared to lifestyle advice alone on falls, serum 25OHD levels, physical function, and adverse events in 686 women aged over 70 years" | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) | Low risk | The underlying reasons for missing data are unlikely to make treatment effects depart from plausible values. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The source of funding is not clear. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 98 elderly ambulatory men and women (54%) women, aged 70 to 97 (mean 79.1) years of age. Inclusion criteria: elderly ambulatory men and women. Exclusion criteria: serum calcium levels of 2.57 mmol/L or more, urinary calcium levels of 7.28 mmol/day or more, creatinine clearance less than 0.42 mmol/s, history of hypercalcaemia, nephrolithiasis, seizure disorder, hyperparathyroidism, treatment with calcium, vitamin D or thiazide diuretics, and average calcium intake greater than 1000 mg/day. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: calcitriol (0.5 μg) daily (n = 50); Intervention group 2 (Control group): placebo vitamin D (n = 48); for a six‐month period. | |
| Outcomes | The primary outcome measure was muscle strength. | |
| Stated aim of study | "To test the hypothesis that the weakness associated with aging is in part due to inadequate serum concentrations of 1,25‐(OH2)D3." | |
| Notes | "Participants were evaluated at 1, 2, 4, 8, 12, 18, and 24 weeks of intervention regimen to maintain compliance. Participants in both groups took more than 95% of the assigned medication." Calcitriol and placebo capsules were provided by Hoffman‐LaRoche (Nutley, NJ). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Calcitriol and placebo capsules were provided by Hoffman‐LaRoche (Nutley, NJ). |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Norway. Number of participants randomised: 104 (45% women), mean age 51.5 years. Inclusion criteria: participants with low serum 25‐hydroxyvitamin D levels. Exclusion criteria: diabetes, acute myocardial infarction or stroke during the past 12 months, cancer during the past 5 years, steroid use, serum creatinine ≥130 μmol/L (males) ≥ 110 μmol/L (females), possible primary hyperparathyroidism (plasma parathyroid hormone [PTH] > 5.0 pmol/L combined with serum calcium > 2.50 mmol/L), sarcoidosis, systolic blood pressure > 175 mmHg or diastolic blood pressure > 105 mmHg, and specifically for women, pregnancy, lactation, or fertile age and no contraception use. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (20,000 IU) twice weekly (n = 51); Intervention group 2 (Control group): placebo twice weekly (n = 53); for a six months period. | |
| Outcomes | The primary outcomes were insulin sensitivity and secretion. Secondary outcome measure was blood lipid level. | |
| Stated aim of study | "to compare insulin sensitivity (the primary end point) and secretion and lipids in subjects with low and high serum 25(OH)D (25‐hydroxyvitamin D) levels and to assess the effect of vitamin D supplementation on the same outcomes among the participants with low serum 25(OH)D levels." | |
| Notes | Vitamin D3 was manufactured by Dekristol; Mibe, Brehna, Germany. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) | Low risk | The underlying reasons for missing data are unlikely to make treatment effects depart from plausible values. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Vitamin D3 was manufactured by Dekristol; Mibe, Brehna, Germany. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | The Nottingham Neck of Femur Study (NONOF). Randomised controlled trial, using parallel group design (four intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 150 previously independent elderly women, 67 to 92 (mean 81.2) years of age, recruited following surgery for hip fracture. Inclusion criteria: elderly women post‐hip fracture, previous community residence, independence in activities of daily living. Exclusion criteria: institutionalised patients, diseases or medication known to affect bone metabolism, and those with a 10‐point abbreviated mental test score less than seven at the time of recruitment. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: single injection of 300,000 IU of vitamin D2 (n = 38); Intervention group 2: single injection of 300,000 IU of vitamin D2 plus oral calcium (1000 mg) daily (n = 36); Intervention group 3: oral vitamin D3 (800 IU) plus calcium (1000 mg) daily (n = 39); Intervention group 4 (Control group): no treatment (n = 37); for a one‐year period. | |
| Outcomes | The primary outcomes were bone biochemical markers, bone mineral density, and rate of falls and new fractures. | |
| Stated aim of study | "To compare the effects of different calcium and vitamin D supplementation regimens on bone biochemical markers, bone mineral density, and rate of falls in elderly women post‐hip fracture." | |
| Notes | "There were no cases of hypercalcaemia, and no participants were withdrawn because of adverse effects of trial medication." The trial was supported by Provalis Healthcare Ltd. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a opaque and sealed envelopes. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial was supported by Provalis Healthcare Ltd. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Women’s Health Initiative (WHI). Multicentre, randomised, double‐blind, placebo controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 36,282 50 to 79 (mean 62) years of age, healthy postmenopausal women. Inclusion criteria: postmenopausal women 50 to 79 years of age at the initial screening without evidence of a medical condition associated with a predicted survival of less than three years and no safety, adherence, or retention risks. Exclusion criteria: hypercalcaemia, renal calculi, corticosteroid use, and calcitriol use. Personal supplemental calcium (up to 1000 mg per day) and vitamin D (up to 600 IU per day) were allowed. In 1999, the upper limit of personal vitamin D intake was raised to 1000 IU. The calcium with vitamin D trial permitted the use of bisphosphonates and calcitonin. Use of oestrogen (with or without a progestin) was according to randomisation among women in the Hormone Therapy trial. Independent use of hormone therapy or selective oestrogen‐receptor modulators was permitted for women in the Dietary Modification trial. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (400 IU) plus calcium (1000 mg) daily (n = 18176); Intervention group 2 (Control group): matched placebo daily (n = 18106); for a seven‐year period. | |
| Outcomes | The primary outcome measure was hip fracture. The secondary outcomes were other fractures and colorectal cancer. | |
| Stated aim of study | "To test the primary hypothesis that postmenopausal women randomly assigned to vitamin D supplementation plus calcium would have a lower risk of hip fracture, and, secondarily, of all fractures than women assigned to placebo. Another secondary hypothesis was that women receiving calcium with vitamin D supplementation would have a lower rate of colorectal cancer than those receiving placebo." | |
| Notes | "The Women’s Health Initiative was clinical investigation of strategies for the prevention of some of the most common causes of morbidity and mortality among postmenopausal women. It consisted of two components, the randomised controlled clinical trial and observational study. Randomised controlled trial tested two interventions (hormone therapy and dietary modification. Women who were ineligible or unwilling to enrol in randomised trial were invited to participate in the observational study. One year later participants enrolled in the dietary modification trial, hormone therapy trials, or both were invited to join the Women Health Initiative calcium‐vitamin D trial." "Adherence to the trial medication was established by weighing returned pill bottles during clinic visits. The rate of adherence (defined as use of 80% or more of the assigned trial medication) ranged from 60% to 63% during the first three years of follow‐up, with an additional 13% to 21% of the participants taking at least half of their trial pills. At the end of the trial, 76% were still taking the trial medication, and 59% were taking 80% or more of it." The active trial drug and placebo were supplied by GlaxoSmithKline Consumer Healthcare (Pittsburgh). We extracted data about cancer occurrence and cancer mortality from the article: Brunner RL, Wactawski‐Wende J, Caan BJ, Cochrane BB, Chlebowski RT, Gass ML, et al. The effect of calcium plus vitamin D on risk for invasive cancer: results of the Women's Health Initiative (WHI) calcium plus vitamin D randomised clinical trial. Nutrition an Cancer 2011;63(6):827‐41. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The active trial drug and placebo were supplied by GlaxoSmithKline Consumer Healthcare (Pittsburgh). |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Netherlands. Number of participants randomised: 70 female geriatric patients older than 65 years with serum 25 hydroxyvitamin D concentrations between 20 and 50 nmol/L. Inclusion criteria: vitamin D insufficient geriatric patients able to walk and follow simple instructions. Exclusion criteria: treatment with vitamin D or steroids in the previous six months, a history of hypercalcaemia or renal stones, liver cirrhosis, serum creatinine > 200 μmol/L, malabsorptive bowel syndrome, primary hyperparathyroidism, uncontrolled thyroid disease, anticonvulsant drug therapy, and/or presence of any other condition that would probably interfere with the patients compliance (i.e., surgery planned). | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (400 IU) plus calcium (500 mg) daily (n = 36); Intervention group 2 (Control group): placebo vitamin D3 plus calcium (500 mg) daily (n = 34); for a six months period. | |
| Outcomes | The primary outcomes were muscle strength, power and functional mobility. | |
| Stated aim of study | "To test the hypothesis that vitamin D plus calcium supplementation improves muscle strength and mobility, compared with calcium monotherapy in vitamin D insufficient female geriatric patients." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit. |
| Blinding (performance bias and detection bias) | Low risk | The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) | Low risk | The underlying reasons for missing data are unlikely to make treatment effects depart from plausible values. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Low risk | The trial is not funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using 2 x 2 factorial design. | |
| Participants | Country: Finland. Number of participants randomised: 464, recently postmenopausal women without contraindications to hormone replacement therapy 47 to 56 (mean 52.7) years of age. Inclusion criteria: nonosteoporotic, early postmenopausal women (6 to 24 months had elapsed since their last menstruation). Exclusion criteria: history of breast or endometrial cancer, thromboembolic diseases, and medication‐resistant hypertension. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: sequential combination of 2 mg estradiol valerate (E2Val; days 1 to 21) and 1 mg cyproterone acetate (days 12 to 21) and a treatment‐free interval (days 22 to 28) (n = 116); Intervention group 2: vitamin D3 (300 IU) plus calcium (500 mg) daily, intervention‐free interval June‐August, the Vit D3 dosage was lowered to 100 IU/day after 4 years of treatment because of adverse lipid changes noticed during the first years of the trial (N = 116); Intervention group 3: sequential combination of 2 mg estradiol valerate (E2Val; days 1 to 21) and 1 mg cyproterone acetate (days 12 to 21) and a intervention‐free interval (days 22 to 28) plus vitamin D3 (300 IU) and calcium (500 mg) daily (n = 116); Intervention group 4 (Control group): placebo daily (n = 116); for a five‐year period. | |
| Outcomes | The primary outcome was bone mineral density. | |
| Stated aim of study | "To examine the long term effects of a sequential oestrogen‐progestin combination therapy (estradiol valerate and cyproterone acetate) and low dose vitamin D3 supplementation on bone mineral density in nonosteoporotic, early postmenopausal women and to determine whether vitamin D3 supplementation can give additional benefit to hormone replacement therapy." | |
| Notes | "Of the 464 women enrolled in the trial, 435 (94%) eligible women completed it. Among the 29 drop‐outs were 20 women who could not be contacted in the end of the trial and 3 who died from unrelated causes during the trial period. In addition, 6 osteoporotic women were withdrawn from the trial after enrolment when participant eligibility data were available (baseline lumbar or femoral BMD above ‐2 SD of the mean of the whole trial population)." The trial was supported by Leiras Oy, Finland and Schering AG, Germany. Hormone replacement therapy provided by Climen, Schering AG, Germany; Vitamin D3 by D‐Calsor, Orion Ltd, Finland, and calcium by Rohto Ltd, Tampere, Finland. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit, so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial was supported by Leiras Oy, Finland and Schering AG, Germany. Hormone replacement therapy provided by Climen, Schering AG, Germany; Vitamin D3 by D‐Calsor, Orion Ltd, Finland, and calcium by Rohto Ltd, Tampere, Finland. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised clinical trial using parallel group design (two intervention groups). | |
| Participants | Country: Switzerland. Number of participants randomised: 248 elderly institutionalised women 62 to 98 (mean 84.5) years of age. Inclusion criteria: elderly institutionalised women. Exclusion criteria: not reported. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (880 IU) plus calcium (1000 mg) daily (n = 124); Intervention group 2 (Control group): no treatment (n = 124); for a two‐year period. | |
| Outcomes | The primary outcomes were quantitative ultrasound parameters of bones and metabolic disturbances. | |
| Stated aim of study | "To assess the effect of supplementation with vitamin D and calcium on quantitative ultrasound parameters and metabolic disturbances in elderly institutionalised women." | |
| Notes | "The drugs were given by the nursing staff to avoid lack of compliance." Trial agents were provided by Novartis Pharma, Basle, Switzerland. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | High risk | The allocation sequence was known to the investigators who assigned participants. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Trial agents were provided by Novartis Pharma, Basle, Switzerland. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Osteoporosis Risk Factor and Prevention Study‐Fracture Prevention Study (OSTPRE‐FPS). Randomised controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Finland. Number of participants randomised: 3139 ambulatory postmenopausal women, aged 65 to 71 (mean 67) years. Inclusion criteria: ambulatory women aged 65 years or more at the end of November 2002, living in Kuopio province area at the onset of the trial, and not belonging to the former OSTPRE bone densitometry sample. Exclusion criteria: none stated. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 800 IU plus calcium (calcium carbonate) 1000 mg daily (n = 1718); Intervention group 2 (Control group): no intervention (n = 1714); for a three‐year period. | |
| Outcomes | The primary outcome measure was the occurrence of falls. | |
| Stated aim of study | "To test the hypothesis that the calcium and vitamin D supplementation prevents falls at the population level." | |
| Notes | This trial was based on the OSTPRE‐FPS (Osteoporosis Risk Factor and Prevention Study‐Fracture Prevention Study) which began in 2003 in Kuopio, Finland. "The compliance was calculated as the dispensed tablets on prescriptions and not on exact number of tablets consumed. The mean compliance in the entire trial population was 78%. The values for 70%, 80% and 90% compliance were 77.4%, 74.2% and 69.1% of the intervention group (entire trial population), respectively." Supported by Leiras‐Nycomed Ltd with calcium and vitamin D supplementation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | High risk | The trial was not blinded, so that the allocation was known during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The trial was supported by Leiras‐Nycomed Ltd with calcium and vitamin D supplementation. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (three intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 1179 healthy postmenopausal white women, 55 years of age and older (mean 66.7). Inclusion criteria: age > 55 years, at least four years past last menses; in generally good health, living independently in the community, and weighing less than 300 pounds. Exclusion criteria: a medical diagnosis of any chronic kidney disease, Paget's or other metabolic bone disease, and history of cancer except for superficial basal or squamous cell carcinoma of the skin and other malignancies treated curatively more than 10 years prior to entry into the trial. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (1000 IU) plus calcium (1400 to 1500 mg) daily (n = 446); Intervention group 2: vitamin D3 placebo plus calcium (1400 to 1500 mg) daily (n = 445); Intervention group 3 (Control group): placebo, consisting of both vitamin D3 placebo and a brand‐specific calcium placebo daily (n = 288); for a four‐year period. | |
| Outcomes | The primary outcome was fracture incidence, and the principal secondary outcome was cancer occurrence. | |
| Stated aim of study | "To determine the efficacy of calcium alone and calcium plus vitamin D in reducing incident cancer risk of all types." | |
| Notes | "Compliance with trial medication was assessed at six months intervals by bottle weight. Mean adherence (defined as taking 80% of assigned doses) was 85.7% for the vitamin D component of the combined regimen and 74.4% for the calcium component." The calcium supplements were provided by Mission Pharmacal (San Antonio, TX) and GlaxoSmithKline (Parsippany, NJ). The vitamin D3 was obtained from Tishcon Corporation (Westbury, NY). Additional information on mortality was received through personal communication with Professor Joan M Lappe (21.11.2007). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | High risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were not described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The calcium supplements were provided by Mission Pharmacal (San Antonio, TX) and GlaxoSmithKline (Parsippany, NJ). The vitamin D3 was obtained from Tishcon Corporation (Westbury, NY). |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Cluster‐randomised clinical trial using 2 x 2 factorial design. | |
| Participants | Country: Denmark. Number of participants randomised: 9605, (60 % women), 66 to 103 (mean 75) years or over community‐dwelling residents. Inclusion criteria: community‐dwelling residents, aged 66 years or over. Exclusion criteria: elderly, who were living in nursing homes, severely impaired persons living in sheltered homes for the elderly, as well as elderly with mental retardation who were unable to give informed consent. | |
| Interventions | Municipality of Randers, Denmark was divided into four comparable blocks. The four blocks were allocated at random to three different fracture prevention programs or no intervention. Intervention group 1: home safety inspection by a community nurse to identify and remedy possible hazards and identify and correct potential health or dietary problems. The nurse evaluated the resident’s prescribed medication to identify possible errors or necessary dose adjustments. Those who accepted a home visit in this area were given leaflets with information of different ways to avoid falling (n = 2532); Intervention group 2: vitamin D3 (400 IU) plus calcium (1000 mg) daily. Furthermore, these participants were offered an evaluation of their prescribed medication. This revision also ensured that the elderly took no other types of vitamin D products and calcium. If the participants used cardiovascular medicine (digoxin or calcium antagonists) that may interact with calcium, they were referred to their general practitioner. Those who accepted a home visit were given leaflets with information of different ways to avoid osteoporosis (n = 2426); Intervention group 3: a combination of the intervention 1 and intervention 2 (n = 2531); Intervention group 4 (Control group): no intervention (n = 2116); for a three and a half year period. | |
| Outcomes | The primary outcome was osteoporotic fractures leading to acute hospital admission. | |
| Stated aim of study | "To evaluate the effect of two programmes for the prevention of fractures leading to acute hospital admission in a population of elderly community‐dwelling Danish residents. One programme included the provision of vitamin D and calcium, whereas the other programme offered an evaluation of and suggestions for the improvement of the domestic environment. Both programmes included revision of the resident’s current pharmaceutical treatment." | |
| Notes | The trial was supported by Nycomed DAK. Nycomed DAK supplied the free vitamin D tablets and calcium (Calcichew). Additional information on mortality was received through personal communication with Dr Leif Mosekilde and Dr Lars Rejnmark (06.02.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised, but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | High risk | The allocation sequence was known to the investigators who assigned participants. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | High risk | The number or reasons for dropouts and withdrawals were not described. |
| Selective reporting (reporting bias) | Unclear risk | Not all pre‐defined, or clinically relevant and reasonably expected outcomes are reported on or are not reported fully, or it is unclear whether data on these outcomes were recorded or not. |
| Industry bias | Unclear risk | The trial was supported by Nycomed DAK. Nycomed DAK supplied the free vitamin D tablets and calcium (Calcichew). |
| Other bias | Unclear risk | There are other factors in the trial that could put it at risk of bias. Recruitment bias was judged as probably adequate. |
| Methods | The Frailty Interventions Trial in Elderly Subjects (FITNESS). Multicentre, randomised, placebo controlled trial using 2 x 2 factorial design. | |
| Participants | Country: New Zealand. Number of participants randomised: 243, 64 to 99 (mean 85) years of age, healthy ambulatory women. Inclusion criteria: aged 65 and older, considered frail according to simple clinical measures of frailty and no clear indication or contraindication to either of the trial interventions (i.e., the clinician had substantial uncertainty about the benefits or harms of either interventions for a specific patient). Exclusion criteria: if patients were considered not frail (i.e., fit and independent or fully dependent in activity of daily living) or if, in the opinion of the responsible clinician, that treatment was considered to be potentially hazardous or definitely indicated for a patient; had a poor prognosis and were unlikely to survive six months; severe cognitive impairment that would compromise adherence to the exercise programme (generally people with scores < 20 on a 30‐point Mini‐Mental State Examination); physical limitations that could limit adherence to the exercise programme (e.g., poor upper limb function that limited application of the weights); unstable cardiac status, or large ulcers about the ankles that would preclude safe application of the ankle weights. In addition, because of difficulties that would arise with their follow‐up assessments, people who lived outside the hospitals' normal geographical zones and patients who were not fluent in English were excluded. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: resistance exercise to the quadriceps muscles with frequency‐matched social home visits (ten week programme) (n = 120); Intervention group 2: vitamin D3 (300,000 IU) (n = 121); Intervention group 3: attention control (n = 123); Intervention group 4 (Control group): placebo vitamin D3 (n = 122); for a six‐month period. The vitamin D intervention was given in a single oral dose. Patients received either six vitamin D3 (300,000 IU) or matching placebo tablets. A trial nurse administered the tablets. Overall, vitamin D received 121 participant and placebo 122 participants. | |
| Outcomes | The primary outcomes were self‐rated physical health at three months and falls over the sixth‐month period. Secondary outcomes were physical performance and self‐rated function. | |
| Stated aim of study | "To determine whether a simple home‐based programme of resistance exercise to the quadriceps muscles or a single high dose of vitamin D could improve self‐reported physical health and reduce the risk of falls in frail older people who had recently been discharged from hospital." | |
| Notes | "Compliance was monitored using a participants diary. Compliance with the single high dose of calciferol or placebo was 100%. No participants were lost to follow‐up." Additional information on mortality and form of vitamin D used in the trial was received through personal communication with Professor Nancy K Latham (01.02.2009) and Professor Ian Cameron (24.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The trial biostatistician generated the randomisation sequence using a computerised central randomisation scheme. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | It was specified that there were no dropouts or withdrawals. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The trial is supported by grants from the Health Research Council of New Zealand, the Auckland University of Technology Research Fund, and a bequest from the Lenore Wilson Estate. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Cluster‐randomised clinical trial using parallel group design (two intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 3717 participating residents (76% women), average age 85 years. Inclusion criteria: elderly people aged 60 years or over. Exclusion criteria: temporary residents admitted for respite care, residents who were already taking calcium/vitamin D or drugs that increase bone density (such as bisphosphonates), and residents who had sarcoidosis or malignancy, or other life‐threatening illness. | |
| Interventions | Participants (30‐bedded units) were randomly assigned to receive: Intervention group 1: vitamin D2 (1100 IU) daily (n = 1762); Intervention group 2 (Control group): no intervention (n = 1955); for a ten‐month period. Vitamin D was given as tablets containing vitamin D2 (ergocalciferol) 100,000 IU (Norton Healthcare (now Ivax Pharmaceuticals)) every three months; Residents in the control group took no vitamin D (there was no placebo). | |
| Outcomes | The primary outcomes were non‐vertebral fractures and falls. | |
| Stated aim of study | "To determine whether vitamin D supplementation reduces the risk of fracture or falls in elderly people in care home accommodation." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using cluster randomisation by computer. |
| Allocation concealment (selection bias) | High risk | The allocation sequence was known to the investigators who assigned participants. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The source of funding is not clear. |
| Other bias | Unclear risk | The trial may or may not be free of other components that could put it at risk of bias. There was potential selection bias as no data given on non‐participants. Recruitment bias judged as unknown. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Belgium. Number of participants randomised: 182 patients with chronic obstructive pulmonary disease (COPD), (20% women), mean age 68 years. Inclusion criteria: current or former smokers, older than 50 years, diagnosis of COPD according to the Global Initiative for Chronic Obstructive Lung Disease definition (postbronchodilator FEV1– FVC ratio < 0.7), and had an FEV1 less than 80% predicted. Exclusion criteria: a history of hypercalcaemia, sarcoidosis, or active cancer. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 100,000 IU monthly (n = 91); Intervention group 2 (Control group): matched placebo monthly (n = 91); for one year. | |
| Outcomes | The primary outcome was time to first exacerbation. Secondary outcomes were exacerbation rate, time to first hospitalisation, time to second exacerbation, FEV1, quality of life, and death. | |
| Stated aim of study | "To explore the effect of adequate vitamin D supplementation on exacerbations in patients with moderate to very severe COPD." | |
| Notes | Laboratoires SMB Brussels, Belgium, provided the study medication free of charge. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The outcome measurement is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) | Low risk | The underlying reasons for missing data are unlikely to make treatment effects depart from plausible values. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Laboratoires SMB Brussels, Belgium, provided the study medication free of charge. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: the Netherlands. Number of participants randomised: 2578 independently living elderly persons (74% women), 70 to 97 (mean 80) years of age. Inclusion criteria: elderly people, aged 70 years or over, reasonable healthy and able to give informed consent. Exclusion criteria: history of hip fracture or total hip arthroplasty, known hypercalcaemia, sarcoidosis, or recent urolithiasis (< 5 years earlier), diseases or medications that influence bone metabolism (such as thyroid disease or glucocorticoid medication). | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 400 IU daily (n = 1291); Intervention group 2 (Control group): matched placebo daily (n = 1287); for a three and a half year period. | |
| Outcomes | The primary outcomes were hip fractures and other peripheral bone fractures. | |
| Stated aim of study | "To determine whether vitamin D supplementation decreases the incidence of hip fractures and other peripheral bone fractures." | |
| Notes | "Compliance was checked when the tablet containers were replaced (every 6 months), by questionnaire (every year), and by measurement of the serum 25(OH)D concentration. Compliance was considered to be adequate if the participants reported on the questionnaire that they took the tablets five or more days per week. This occurred in 85% of the participants and was similar in both groups." Vitamin D and placebo tablets were provided by Solvay‐Duphar, Inc, Weesp, the Netherlands. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation or a random number table. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Vitamin D and placebo tablets were provided by Solvay‐Duphar, Inc, Weesp, the Netherlands. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled multicenter trial using parallel group design (two intervention groups). | |
| Participants | Country: the Netherlands. Number of participants randomised: 226 men and women aged ≥ 70 (mean 78) years who were vitamin D insufficient (serum 25‐hydroxyvitamin D concentrations ≤ 20 but ≥ 6 ng/mL). Inclusion criteria: ambulatory elderly people who were vitamin D insufficient, aged 70 years or over, able to walk 10 feet without a walking aid) and mentally competent. If patients had serum 25‐hydroxyvitamin D concentrations ≥ 6 but ≤ 9 ng/mL, they needed to have 24‐h urine calcium concentrations ≥ 50 mg/d and bone‐specific alkaline phosphatase concentrations not higher than the upper limit of normal. Exclusion criteria: primary hyperparathyroidism, active thyroid disease, impaired renal function, osteomalacia, neurologic impairment, peripheral neuropathy, myocardial infarction within 6 months of screening, uncontrolled hypertension, postural hypotension, malabsorption syndrome, alcohol abuse (i.e., > 2 drinks/day), cancer, treatment with oral glucocorticoids, anabolic steroids, or a growth hormone within 12 months of screening; treatment with > 800 IU vitamin D a day or with active metabolites of vitamin D within 6 months of screening; or treatment with any drug that might affect vitamin D metabolism or interfere with postural stability at screening. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 8400 IU weekly (n = 114); Intervention group 2 (Control group): matched placebo weekly (n = 112); for a 16 weeks period. "For participants with a daily dietary calcium intake <1000 mg (as assessed by a questionnaire at screening), daily calcium carbonate containing 500 mg elemental calcium was also prescribed." | |
| Outcomes | The primary outcome measure was mediolateral sway with eyes open. Secondary outcome measures were change in functional status assessed with the short physical performance battery, mean serum 25‐hydroxyvitamin D, calcium, and phosphate concentrations, and adverse events. | |
| Stated aim of study | "To assess whether a once‐weekly treatment with 8400 IU vitamin D3 would improve body postural stability and lower‐extremity function in elderly people with low vitamin D status (serum 25‐hydroxyvitamin D concentrations ≤ 20 ng/mL)." | |
| Notes | "All patients who completed the trial were adherent to treatment, which was defined as taking ≥ 13 of the 16 total doses prescribed." Supported by Merck & Co Inc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit. Participants were stratified (2:1) at randomisation according to baseline serum 25‐hydroxyvitamin D concentration. Patients were assigned a unique allocation number according to their appropriate stratification block. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. Investigators were blinded to serum 25‐hydroxyvitamin D concentrations and to stratum definitions. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described or if it was specified that there were no dropouts or withdrawals. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial is funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 3440 older people living in institutional care (76% women), 62 to 107 (mean 84) years of age. Inclusion criteria: elderly people, including those with mobility, cognitive, visual, hearing or communication impairments living in nursing homes, residential homes, and sheltered housing. Exclusion criteria: people already receiving ≥ 400 IU of vitamin D/day and those already known to have contraindications to vitamin D supplementation. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 100,000 IU three times a year (four‐monthly) (n = 1725); Intervention group 2 (Control group): matched placebo tablet three times a year (four‐monthly) (n = 1715); for a three‐year period. | |
| Outcomes | The primary outcome measure was the incidence of first fracture. Secondary outcome measures were the incidence of hip fractures, fractures at common osteoporotic sites (hip/wrist/forearm/vertebrae), and mortality rates. | |
| Stated aim of study | "To examine the effect of vitamin D supplementation on fracture rate in people living in sheltered accommodation." | |
| Notes | "Dosing was supervised by the research nurse to ensure adherence, but nurse, participant, and analysts were blinded to the allocation. Adherence among participants in the trial was 80% overall (percentage of occasions observed to take tablets whilst in the trial)." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Low risk | The trial is not funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Germany. Number of participants randomised: 55 healthy volunteers (65% postmenopausal women), 33 to 78 (mean 55,8) years of age. Inclusion criteria: healthy volunteers. Exclusion criteria: history or clinical evidence of significant skeletal or nonskeletal disease, taking any medication known to affect bone metabolism, including vitamin D and mineral supplements. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 500 IU daily plus calcium 500 mg daily (n = 30); Intervention group 2 (Control group): no intervention (n = 25); for a six‐month period. Participants were followed an additional six‐month period. The first year of the trial after randomisation was designed as an observation period only, during which the participants followed their usual daily routine with no intervention per protocol. During the winter of the second year, from October to March, the participants assigned to the intervention group received a daily supplement of oral vitamin D3 (500 IU) and calcium (500 mg), whereas the participants in the control group received no supplements and were asked to remain off such agents. The trial medication was open label. | |
| Outcomes | The primary outcomes were circannual changes in bone turnover, and bone mineral density and rates of bone turnover and bone loss during the winter months. | |
| Stated aim of study | "To evaluate the circannual changes in bone turnover, and bone mineral density and to determine the effect of oral calcium and vitamin D3 supplementation on rates of bone turnover and bone loss during the winter months." | |
| Notes | "Adherence to intervention was checked in monthly intervals through personal interviews." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Low risk | The trial is not funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Postmenopausal Health Study (PMHS). Randomised controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Greece. Number of participants randomised: 112 postmenopausal women, aged 55 to 65 (mean 60.3) years. Inclusion criteria: postmenopausal non‐osteoporotic women. Exclusion criteria: a T‐score lower than 22.5, taking medications (i.e., thiazide diuretics, glucocorticoids) and/or dietary supplements (calcium, magnesium, phosphate or vitamin D) that affect bone metabolism, having any kind of degenerative chronic disease (i.e., diabetes, nephrolithiasis, heart disease, cancer, hyper‐ and hypothyroidism, hyperparathyroidism, impaired renal and liver function), smoking and being postmenopausal for less than 1 year | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 300 IU plus calcium 1200 mg daily (n = 42); Intervention group 2: calcium 1200 mg (n = 30); Intervention group 3 (Control group): no intervention (n = 40); for a one‐year period. | |
| Outcomes | The primary outcome measure was bone mineral density. | |
| Stated aim of study | "To examine whether the use of calcium supplementation could prevent bone loss in healthy postmenopausal women or more favourable outcomes could be obtained using a holistic approach combining dietary intervention and consumption of dairy products fortified with calcium and vitamin D3." | |
| Notes | "To ensure compliance with the intervention scheme, ‘Health and Nutrition Education’ sessions were held biweekly within the settings of the university and the required quantities of fortified dairy products for the next two weeks were provided at the end of the sessions. Adherence of the participants in the calcium group was assessed by checking for remaining calcium tablets in the returned packages but also via weekly phone calls. Compliance to the intervention scheme was reaching a rate of 93% (range 89 to 100 %). Compliance rate in calcium group was approximately 95% (range 91 to 100 %)." The trial was supported by a research grant from Friesland Foods Hellas. Additional information on mortality was received through personal communication with Dr George Moschonis (23.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using a random number table. |
| Allocation concealment (selection bias) | High risk | The allocation sequence was known to the investigators who assigned participants. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial was supported by a research grant from Friesland Foods Hellas. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: The Netherlands. Number of participants randomised: 348 women, aged 70 years or older, who were reasonably mobile. Inclusion criteria: elderly mobile women aged 70 years or older. Exclusion criteria: hip fracture in the past, total hip prosthesis, and recent history of urolithiasis, hypercalcaemia, or sarcoidosis. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 400 IU daily (n = 177); Intervention group 2 (Control group): matched placebo daily (n = 171); for a two‐year period. | |
| Outcomes | The primary outcome measures were bone mineral density of both hips (femoral neck and trochanter) and the distal radius, as well as biochemical markers of bone turnover. | |
| Stated aim of study | "To determine the effect of vitamin D supplementation on bone turnover and bone loss in elderly women." | |
| Notes | "Compliance was established by questionnaire, by pill counting, and by measuring serum 250HD levels in blood. If participants were suspected of poor compliance resulting from memory problems, the nursing staff were asked to supervise the taking of the trial intervention or to administer it." "The compliance was good in both groups. According to the yearly questionnaire, 85% used one tablet daily, and 14% used between three and six tablets weekly. The analysis of the remaining tablets showed a slightly better compliance in the second trial year. In the first year, 63% had used between six and seven tablets weekly, and 4% had used less than three weekly; in the second year, these compliance rates were 78% and 1%, respectively. Of the women receiving the vitamin D supplement, only 5 participants (3%) did not achieve a serum 25 hydroxyvitamin D level higher than 30 nmol/L, whereas 68.4% of the participants in the placebo group had serum levels below 30 nmol/L." The trial medication was provided by Duphar Nederland BV, Amsterdam, the Netherlands. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. Randomisation was performed by the hospital pharmacy, and double‐blinding was assured. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The trial medication was provided by Duphar Nederland BV, Amsterdam, the Netherlands. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United States. Number of participants randomised: 86 postmenopausal women, 50 to 80 (mean 67.5) years of age. Inclusion criteria: postmenopausal women with at least two compression fractures (> 15% reduction in anterior height) without history of serious trauma. Exclusion criteria: history of corticosteroid use, malnutrition, sarcoidosis, liver disease, rheumatoid arthritis, nephrolithiasis, renal disease, or recent malignancy. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: calcitriol 0.25 to 2 μg plus calcium 1000 mg (n = 43); Intervention group 2 (Control group): placebo vitamin D plus calcium 1000 mg daily (n = 43); for a two‐year period. | |
| Outcomes | The primary outcome measure was bone mass. Secondary outcome measure was adverse effects of calcitriol. | |
| Stated aim of study | "To determine if calcitriol is an effective treatment in postmenopausal osteoporosis." | |
| Notes | Hoffman‐La Roche (Nutley, New Jersey) supplied the vitamin D supplements. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Hoffman‐La Roche (Nutley, New Jersey) supplied the vitamin D supplements. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 3314 women, aged 70 and over (mean 76.8) years, with one or more risk factors for hip fracture. Inclusion criteria: elderly women, aged 70 years or older, who had at least one self reported risk factor for hip fracture: low bodyweight (< 58 kg), any previous fracture, maternal history of hip fracture, smoker, and poor or fair health. Exclusion criteria: unable to give written consent, receiving of any calcium supplementation of more than 500 mg a day, a history of kidney or bladder stones, renal failure, or hypercalcaemia. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 800 IU plus calcium 1000 mg daily (n = 1321); Intervention group 2 (Control group): information leaflet on dietary calcium intake and prevention of falls, or leaflet only (n = 1993); for a 25‐month period. | |
| Outcomes | The primary outcome measure was fracture, excluding those of the digits, rib, face, and skull. Secondary outcomes included hip fracture; quality of life as measured by the 12 item short‐form health survey questionnaire, and the European quality of life instrument, death, visits to the doctor and hospital admissions, falls and fear of falling. | |
| Stated aim of study | "To assess whether supplementation with calcium and vitamin D3 reduces the risk of fracture in women with one or more risk factors for fracture of the hip." | |
| Notes | "Adherence was measured through self report every six months. Rates for adherence at 12 months were about 63%." The trial was supported by Shire and Nycomed. Shire supplied the vitamin D supplements and calcium. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | High risk | Trial was not blinded, so that the allocation was known during the trial. Placebo was not used. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Unclear risk | Not all clinically relevant and reasonably expected outcomes are reported on. Adverse events were not reported. |
| Industry bias | High risk | The trial was supported by Shire and Nycomed. Shire supplied the vitamin D supplements and calcium. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Australia. Number of participants randomised: 302 community‐dwelling ambulant older women aged 70 to 90 (mean 77.2) years with a history of falling and vitamin D insufficiency. Inclusion criteria: community‐dwelling ambulant older women with a history of falling in the past 12 months and a plasma 25 hydroxyvitamin D concentration of less than 24.0 ng/mL. Exclusion criteria: current vitamin D consumption; current consumption of bone or mineral active agents apart from calcium; a bone mineral density z score at the total hip site of less than ‐2.0; medical conditions or disorders that influence bone mineral metabolism, including laboratory evidence of renal insufficiency (a creatinine level more than two‐fold above the reference range); a fracture in the past 6 months; a Mini‐Mental State Examination score of less than 24; or the presence of marked neurological conditions likely to substantially impair balance or physical activity, such as stroke and Parkinson's disease. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 1000 IU plus calcium 1000 mg daily (n = 151); Intervention group 2 (Control group): matched placebo tablet of vitamin D plus calcium 1000 mg daily (n = 151); for a one‐year period. | |
| Outcomes | The primary outcome measure was risk of falls in older women at high risk of falling. | |
| Stated aim of study | "To evaluate the effect of vitamin D2 and calcium supplementation compared with calcium alone on the risk of falls in older women at high risk of falling." | |
| Notes | "Adherence to the trial medications was established by counting tablets returned at the clinic visits at 6 and 12 months. The rate of compliance with trial medication in participants who continued to receive the medication, as determined from tablet counting, was 86% in both groups." Vitamin D2 (ergocalciferol) or identical placebo was provided by Ostelin; Boots Healthcare, North Ryde, Australia. Calcium as calcium citrate was provided by Citracal; Mission Pharmacal, Key Pharmaceutical Pty Ltd, Rhodes, Australia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. Randomisation schedule was kept in the pharmacy department, where the bottles were labelled and dispensed to the participants.The trial participants and the trial staff remained blinded to the treatment code until all the data had been entered, evaluated for accuracy, and the a priori hypotheses reviewed. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Vitamin D2 (ergocalciferol) or identical placebo was provided by Ostelin; Boots Healthcare, North Ryde, Australia. Calcium as calcium citrate was provided by Citracal; Mission Pharmacal, Key Pharmaceutical Pty Ltd, Rhodes, Australia. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Single centre, randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). The Vital D study. | |
| Participants | Country: Australia. Number of participants randomised: 2258 community‐dwelling women, 70 years or older (mean age 76 years) considered to be at high risk of fracture. Inclusion criteria: community‐dwelling women at higher risk of hip fracture, defined by criteria such as maternal hip fracture, past fracture, or self‐reported faller. Exclusion criteria: unable to provide informed consent or information about falls or fractures; permanently resided at a high‐level care facility; had an albumin‐corrected calcium level higher than 2.65 mmol/L; or had a creatinine level higher than 150 μmol/L, or currently took vitamin D doses of 400 IU or more, calcitriol, or antifracture therapy. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 500,000 IU yearly (n = 1131); Intervention group 2 (Control group): matched placebo tablet of vitamin D yearly (n = 1127); for a three to five years (in autumn or winter), median 2.96 years. "Ten tablets were mailed to participants annually (March‐August, determined by recruitment date) with instructions to take all tablets on a single day. Study staff confirmed by telephone the ingestion of study medication within 2 weeks. Subsequent dosing occurred within 2 weeks of the anniversary of the first dose." | |
| Outcomes | The primary outcome measures were falls and fractures. Secondary outcome measures were serum 25‐hydroxycholecalciferol and intact parathyroid hormone levels. | |
| Stated aim of study | "To determine whether a single annual dose of 500 000 IU of cholecalciferol administered orally to older women in autumn or winter would improve adherence and reduce the risk of falls and fracture." | |
| Notes | "Study staff confirmed by telephone the ingestion of study medication." Study medication was supplied by PSM Healthcare, Auckland, New Zealand. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | "Allocation was performed by an independent statistician. Treatment allocation status was e‐mailed directly to the hospital clinical trials pharmacist responsible for dispensing study medication." |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. The participants and study staff were blinded to intervention group. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Study medication was supplied by PSM Healthcare, Auckland, New Zealand. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Japan. Number of participants randomised: 64 (45% women) mean age 68.5 years) outpatients with hemiplegia after stroke. Inclusion criteria: patients with hemiplegia after stroke. Exclusion criteria: shoulder‐hand syndrome, multiple strokes, history of hip fracture, a stroke duration of less than 1 month, or the use of medication known to affect bone metabolism, including oestrogen, calcium, vitamin D, corticosteroids, thyroxine, or anticonvulsants. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D in the form of 1(OH)D3 (alfacalcidol) 1 μg plus calcium 300 mg daily (n = 45); Intervention group 2 (Control group): matched placebo tablet of vitamin D plus calcium 300 mg daily (n = 39); for a six‐month period. | |
| Outcomes | The primary outcome measures were bone mineral density and hip fractures. | |
| Stated aim of study | "To evaluate the efficacy of 1(OH)D3and supplemental elemental calcium in reducing the severity of osteopenia in the second metacarpals and decreasing the risk of hip fractures in chronically ill stroke patients with hemiplegia." | |
| Notes | Additional information on mortality was received through personal communication with Dr Yoshiro Sato (05.02.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Unclear risk | Not all pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. Adverse events were not reported. |
| Industry bias | Unclear risk | The source of funding is not clear. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Japan. Number of participants randomised: 86 elderly patients (78% women) aged 65 to 88 (mean 70.6) with Parkinson's disease. Inclusion criteria: elderly patients with Parkinson's disease and low serum 1,25‐dihydroxyvitamin D concentrations. Exclusion criteria: other known causes of osteoporosis, such as hyperparathyroidism or renal osteodystrophy; impairment of renal, cardiac, or thyroid function; a history of therapy with corticosteroids, estrogens, calcitonin, etidronate, calcium, or vitamin D for three months or longer during the 18 months preceding the trial; or even brief treatment of this nature during the two months immediately preceding the trial. Patients at Hoehn and Yahr stage 5 were excluded because their poor ambulation status largely precluded any chance of fracture. Patients with a history of non‐vertebral fracture were also excluded. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D in a form of 1‐α hydroxyvitamin D3 (alfacalcidol) (1 μg) daily (n = 43); Intervention group 2 (Control group): matched placebo tablet daily (n = 43); for a 18‐month period. | |
| Outcomes | The primary outcome measure was non‐vertebral fractures. Secondary outcome was progression of osteopenia in the second metacarpal bone. | |
| Stated aim of study | "To evaluate the efficacy of 1‐α hydroxyvitamin D3 (alfacalcidol) in reducing progression of osteopenia in the second metacarpal and in decreasing non‐vertebral fractures in elderly patients with Parkinson's disease with low serum 1,25‐dihydroxyvitamin D concentrations." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Unclear risk | The trial was described as randomised but the method used to conceal the allocation was not described, so that intervention allocations may have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Unclear risk | The trial was described as double blind, but the method of blinding was not described, so that knowledge of allocation was possible during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The source of funding is not clear. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised controlled trial using parallel group design (three intervention groups). | |
| Participants | Country: Japan. Number of participants randomised: 103 patients (56% women), mean age 70.7 with hemiplegia after stroke. Inclusion criteria: outpatients with post‐stroke hemiplegia of more than one year duration. Exclusion criteria: congestive heart failure or obstructive pulmonary disease, other known causes of osteoporosis, such as hyperparathyroidism or renal osteodystrophy; impairment of renal, cardiac, or thyroid function; a history of therapy with corticosteroids, estrogens, calcitonin, etidronate, calcium, or vitamin D for 3 months or longer during the 12 months preceding the trial; or even brief treatment of this nature during the 2 months immediately preceding the trial. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D in a form of 1‐α hydroxyvitamin D3 (alfacalcidol) (1 μg) daily (n = 34); Intervention group 2: ipriflavone 600 mg daily (n = 34); Intervention group 2 (Control group): no treatment (n = 35); for a one‐year period. | |
| Outcomes | The primary outcome measures was bone mineral density. | |
| Stated aim of study | "To evaluate the effect of ipriflavone and 1 alpha‐hydroxyvitamin D3 administration on bone mineral density preservation." | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial is described as randomised but the method of sequence generation was not specified. |
| Allocation concealment (selection bias) | High risk | The allocation sequence was known to the investigators who assigned participants. |
| Blinding (performance bias and detection bias) | High risk | The trial was not blinded, so that the allocation was known during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The source of funding is not clear. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Japan. Number of participants randomised: 96 hospitalised elderly women with post stroke hemiplegia mean age 74.1 years. Inclusion criteria: hospitalised elderly women with post stroke hemiplegia who had first‐ever cerebral infarction or haemorrhage more than two years before and were in a convalescent stage with post‐stroke hemiplegia. Exclusion criteria: dementia, total disability, or hospitalisation of less than two years' duration, receiving any drugs known to alter vitamin D metabolism, such as anticonvulsants, calcium, or vitamin D, during the 12 months preceding the trial. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 (1000 IU) daily (n = 48); Intervention group 2 (Control group): matched placebo tablet daily (n = 48); for a two‐year period. | |
| Outcomes | The primary outcome measure was number of falls. Secondary outcome measures were muscular strength and morphological changes of muscle. | |
| Stated aim of study | "To evaluate the efficacy of vitamin D2 therapy in reducing the risk of falls in elderly women with stroke. Histochemical examination of skeletal muscles was performed to assess the effect of the therapy." | |
| Notes | Additional information on mortality was received through personal communication with Dr Yoshiro Sato (05.02.2009). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation or a random number table. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | The source of funding is not clear. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: Germany. Number of participants randomised: 123 patients (17% women) aged 50 to 63 (mean 51) years with congestive heart failure. Inclusion criteria: patients with congestive heart failure and New York Heart Association functional class II. Exclusion criteria: hypercalcaemia, serum creatinine concentration > 2 mg/dL, nephrolithiasis, sarcoidosis, use of a biventricular pacemaker, acute heart insufficiency, and an actual intake of supplements containing vitamin D and calcium. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (2000 IU) plus calcium (500 mg) daily (n = 61); Intervention group 2 (Control group): matched placebo tablet of vitamin D plus calcium 500 mg daily (n = 62); for a nine‐month period. Participants were followed‐up for a 15‐month period. | |
| Outcomes | The primary outcome measures were survival rates, and biochemical variables such as natriuretic peptides and cytokines. Secondary outcomes were those haemodynamic variables, which were assessed routinely during the ambulatory visits, such as left ventricular ejection fraction, left ventricular end‐diastolic diameter, the cardiothoracic ratio, maximal oxygen intake (spiroergometry; O2max), and blood pressure. | |
| Stated aim of study | "To evaluate the effect of vitamin D supplementation on the survival rate and different biochemical variables in patients with congestive heart failure." | |
| Notes | "Compliance was measured by controlling the trial medication at each visit (bottle counts) and by the analysis of serum 25 hydroxyvitamin D concentrations." Vitamin D3 was provided by Vigantol Oel; Merck, Darmstadt, Germany, and placebo by Migliol‐Oel; Merck, Darmstadt, Germany. Additional information received thorough personal communication with Professor Armin Zittermann (10.02.2010). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Vitamin D3 was provided by Vigantol Oel; Merck, Darmstadt, Germany, and placebo by Migliol‐Oel; Merck, Darmstadt, Germany. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Wessex Fracture Prevention Trial (WFPT). | |
| Participants | Country: United Kingdom. Number of participants randomised: 9440 elderly people (54% women) aged 75 years and over. Inclusion criteria: elderly people aged 75 years and over. Exclusion criteria: current cancer or any history of treated osteoporosis, taking 400 IU or more vitamin D daily, bilateral total hip replacement, renal failure, renal stones, hypercalcaemia or sarcoidosis. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 (300,000 IU) intramuscular injection yearly (n = 4727); Intervention group 2 (Control group): matched placebo intramuscular injection of vitamin D yearly (n = 4713); for a three‐year period. Active or placebo injections were administered every autumn at annual intervals and concealed in the same way as the first injection. | |
| Outcomes | The primary outcome measure was all non‐vertebral fracture. Secondary outcome measures were hip and wrist fractures, and all falls. | |
| Stated aim of study | "To evaluate if vitamin D2 is effective in preventing non‐vertebral fractures among elderly men and women resident in the general population." | |
| Notes | The trial was supported by Celltech UK plc. Additional information on mortality was received through personal communication with Professor Cyrus Cooper and Dr Sarah Crozier (16.11.2007). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. Packing and labelling were carried out by an external contractor; allocation was concealed from investigators, practice nurses, and participants. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. Each participating practice was sent mixed boxes containing previously randomised, numbered ampoules of either vitamin D or placebo, which were identical in visual appearance and consistency. As each participant consented to participate in the trial, they were allocated consecutive ampoules. The number of the ampoule was then linked to the participant's name and phoned to a central location. This trial number remained with the participant for the duration of the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | High risk | The trial was supported by Celltech UK plc. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised double‐blind placebo‐controlled trial with parallel group design (two intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 2686 elderly people (24% women) aged 65 to 85 (mean 74.7) years. Inclusion criteria: elderly people living in the general community. Exclusion criteria: already taking vitamin D supplements and conditions that were contraindications to vitamin D supplementation (a history of renal stones, sarcoidosis, or malignancy). | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D3 (100,000 IU) every four months orally (n = 1345); Intervention group 2 (Control group): matched placebo every four months orally (n = 1341); for a five‐year period. | |
| Outcomes | The primary outcome measures were fracture incidence and total mortality by cause. | |
| Stated aim of study | "To determine the effect of four monthly vitamin D supplementation on the rate of fractures in men and women aged 65 years and over living in the community." | |
| Notes | "Seventy six percent of participants had at least 80% compliance (12/15 doses). Compliance for the final dose was 66%; excluding participants who had died, compliance was estimated to be 80%. The 100,000 IU vitamin D supplement or placebo used in this trial was specially prepared by the Ipswich Hospital Pharmacy." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. Participants and investigators were blinded to the treatment until the trial ended, when Ipswich Pharmacy revealed the coding. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Low risk | The trial is not funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (two intervention groups). | |
| Participants | Country: United Kingdom. Number of participants randomised: 105 patients with systolic heart failure aged 70 or over (mean 79.7) years, 34% females with 25‐hydroxyvitamin D levels < 50nmol/L (20 ng/ml). Inclusion criteria: aged 70 years or over with a previously recorded clinical diagnosis of chronic heart failure, previously documented left ventricular systolic dysfunction by echocardiography, radionuclide ventriculography or angiography as part of their usual clinical care, a New York Heart Association class II or III symptoms, and a 25‐hydroxyvitamin D level of < 50nmol/L (20 ng/ml). Exclusion criteria: a clinical diagnosis of osteomalacia, under investigation for recurrent falls, already taking vitamin D supplements, moderate to severe cognitive impairment, defined as a Folstein mini‐mental state examination < 15/30), serum creatinine > 200umol/L, liver function tests (bilirubin, alanine aminotransferase, alkaline phosphatase) > 3 times the upper limit of the local reference range, systolic blood pressure < 90mmHg, albumin adjusted calcium > 2.55 mmol/L or < 2.20 mmol/L), metastatic malignancy, and wheelchair bound patients unable to perform the primary outcome, and excluded patients unwilling or unable to give informed consent. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 (10,000 IU) tablet at baseline and 10 weeks (n = 53); Intervention group 2 (Control group): matched placebo tablet at baseline and 10 weeks (n = 52). Participants were followed for 20 weeks. | |
| Outcomes | The primary outcome measure was the six‐minute walk test, a measure of submaximal exercise capacity. Secondary outcomes were muscle function, daily physical activity levels, health status/health‐related quality of life, cardiovascular and inflammatory markers. | |
| Stated aim of study | "To examine whether vitamin D supplementation could improve parameters that are directly relevant to older people with heart failure – i.e., exercise capacity, physical function and quality of life." | |
| Notes | "Administration of vitamin D2 was supervised in the participant’s own home by the research nurse to ensure 100% adherence." | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was performed using computer generated random number tables by DHP Pharmaceuticals (Gwent, UK). |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit. Code allocation was concealed from the research nurse and investigators until after data analysis was complete. |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. DHP Pharmaceuticals (Gwent, UK) encapsulated the trial medication to render it identical to placebo. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Low risk | The trial is not funded by a manufacturer of vitamin D. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel group design (three intervention groups). | |
| Participants | Country: Australia. Number of participants randomised: 120 community‐dwelling women aged 70 to 80 (mean 75) years. Inclusion criteria: aged over 70 year old, likely to survive a five year trial, and not receiving bone active agent. Exclusion criteria: none stated. | |
| Interventions | Participants were randomly assigned to receive: Intervention group 1: vitamin D2 (1000 IU) plus calcium (1200 mg) daily (n = 39); Intervention group 2: calcium 1200 mg plus placebo vitamin D daily (n = 40); Intervention group 3 (Control group): matched placebo vitamin D and placebo calcium daily (n = 41); for a five year period. | |
| Outcomes | The primary outcome measures were bone mineral density, plasma 25‐hydroxyvitamin D, biomarkers of bone turnover, parathyroid hormone, and intestinal calcium absorption. | |
| Stated aim of study | "To evaluate the relative benefits of 5 year of calcium supplementation of 1200 mg with or without 1000 IU vitamin D2, compared with placebo, on hip BMD and bone‐related biochemistry in ambulant elderly women aged 70 to 80 year living in a sunny climate." | |
| Notes | "This trial was nested within the larger Calcium Intake Fracture Outcome Study, a five year double‐blinded, randomised, controlled calcium supplementation trial, in which 1500 community‐living ambulant women over the age of 70 years old were randomised to received either 1200 mg calcium per day or identical placebo. The first 120 sequential participants presenting in September 1998 (end of winter in Western Australia) enrolled in this substudy and were randomised." "Adherence to the trial interventions was established by counting tablets returned every 12 months. There were no significant differences among the three groups in the compliance rates determined by tablet counting for calcium or placebo in the intervention groups 1, 2, and 3 (80.7, 80.9, and 86.9%, respectively) or for vitamin D or placebo (84.2, 86.9, and 89.8%, respectively)." Vitamin D2 (ergocalciferol) or identical placebo was provided by Ostelin; Boots Healthcare, North Ryde, New South Wales, Australia. Calcium as calcium citrate was provided by Caltrate; Wyeth Consumer Healthcare, Baulkham Hills, New South Wales, Australia. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation was achieved using computer random number generation. |
| Allocation concealment (selection bias) | Low risk | Allocation was controlled by a central and independent randomisation unit so that intervention allocations could not have been foreseen in advance of, or during, enrolment. "Randomisation was undertaken by an independent research fellow and was kept in the Pharmacy Department of the Sir Charles Gairdner Hospital, in which the bottles were labelled and dispensed to participants. The trial participants and trial staff remained blinded to the treatment code until all the data had been entered, evaluated for accuracy, and the a priori hypotheses reviewed." |
| Blinding (performance bias and detection bias) | Low risk | The trial was described as blinded, the parties that were blinded, and the method of blinding was described, so that knowledge of allocation was adequately prevented during the trial. |
| Incomplete outcome data (attrition bias) | Low risk | The numbers and reasons for dropouts and withdrawals in all intervention groups were described. |
| Selective reporting (reporting bias) | Low risk | Pre‐defined, or clinically relevant and reasonably expected outcomes are reported on. |
| Industry bias | Unclear risk | Vitamin D2 (ergocalciferol) or identical placebo was provided by Ostelin; Boots Healthcare, North Ryde, New South Wales, Australia. Calcium as calcium citrate was provided by Caltrate; Wyeth Consumer Healthcare, Baulkham Hills, New South Wales, Australia. |
| Other bias | Low risk | The trial appears to be free of other components that could put it at risk of bias. |
Abbreviations:
BMD: bone mineral density; HRT: hormone replacement therapy; ERT: oestrogen replacement therapy; FEV: Forced expiratory volume; FEV: forced vital capacity
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Randomised controlled trial. This trial included patients receiving corticosteroids (diagnosed with polymyalgia rheumatica, temporal arteritis, asthma, vasculitis, or systemic lupus erythematosus). | |
| Randomised controlled trial. This trial included participants younger than 18 years (adolescent girls median age 12.2 years). | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. This trial included patients receiving corticosteroids (diagnosed with inflammatory bowel disease). | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. This trial included participants younger than 18 years. | |
| Randomised controlled trial. This trial included patients receiving corticosteroids (diagnosed with rheumatoid arthritis). | |
| This is not a randomised controlled trial. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. All women received hormone replacement therapy. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial in patients with glucocorticoid‐induced osteopenia. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received 400 IU of vitamin D2. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial comparing the effect of nandrolone decanoate, 1‐alphahydroxyvitamin D3 and intermittent calcium infusions. Vitamin D group was not supplemented with calcium. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. All participants received vitamin D. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. Vitamin D group also received anabolic steroids. | |
| This is not a randomised controlled trial. Participants were divided into treatment groups according to month of birth. | |
| Randomised controlled trial. All participants received vitamin D. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. This trial did not fulfil our inclusion criteria. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Quasi‐randomised trial. Participants randomised by date of birth. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. Participants in the control group supplemented with calcium. Participants in the vitamin D group were not supplemented with calcium. | |
| Randomised controlled trial. This trial included participants younger than 18 years. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. Participants in a control group supplemented with small dose of vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. This trial included patients receiving corticosteroids (diagnosed with systemic lupus erythematodes, multiple sclerosis, rheumatoid arthritis or asthma bronchiale). | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. This trial included participants with primary hyperparathyroidism. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. All participants received vitamin D or vitamin D analogs. | |
| Quasi‐randomised trial. Before the trial started, the days of the month (1–31 days) were divided randomly into group A and group B, and based on the day of birth, a participant was placed automatically in group A or group B when registered in the trial database. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. Participants received 25‐hydroxyvitamin D3. | |
| Randomised controlled trial. All participants received vitamin D. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. This trial included patients receiving high doses of corticosteroids (cardiac transplant, severe inflammatory syndrome, etc). | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. Participants received a combination of vitamin D, vitamin C, vitamin B1, vitamin B12, and folate. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial. This trial included patients on a long‐term corticosteroid therapy. | |
| Randomised controlled trial in patients after cardiac or lung transplantation. | |
| Randomised controlled trial. All participants received vitamin D2 plus calcium, vitamin D3 or alendronate plus calcium. There is no control group of the trial. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. Participants received a combination of menatrenone, vitamin D2, and calcium. | |
| Randomised controlled trial. Participants were randomised to a combination of alendronate and vitamin D2. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| This is not a randomised controlled trial. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial in children. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. Participants younger than 18 years were included. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. Participants in active treatment group treated with vitamin D and participants in the control group treated with calcium. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial. All participants received vitamin D. | |
| Randomised controlled trial in adolescent girls. | |
| This is not a randomised controlled trial. | |
| Randomised controlled trial in patients with tuberculosis starting antituberculosis treatment. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | The interaction between calcium and vitamin D Intake |
| Methods | Randomised, double‐blind, placebo‐controlled trial using 2 × 2 factorial design |
| Participants | Country: United States Estimated number of participants: 120 Inclusion criteria: healthy women aged 45 and above who have been menopausal for at least one year (absence of menstrual period for a period of 12 months or longer) Exclusion criteria: any chronic medical illness including uncontrolled diabetes mellitus, recent history of myocardial infarction or heart failure, malignancy, uncontrolled hypertension, obesity (BMI > 35 kg/m2), history of anaemia, leukaemia or other hematological abnormalities, lupus, rheumatoid arthritis, or other rheumatological disease, or kidney disease of any kind as determined by history and physical examination; participants with osteoporosis of the hip (total hip T‐score equal to or less than ‐2.5) or taking medications for osteoporosis such as bisphosphonate, pregnancy, use of medication that influences bone metabolism (i.e. anticonvulsant medications, long‐term use of steroids and high‐dose diuretics), significant deviation from normal in medical history, physical examination or laboratory tests as evaluated by the primary investigator, history of hypercalciuria, hypercalcaemia, nephrolithiasis and active sarcoidosis, participation in another investigational trial in the past 30 days before the screening evaluation, unexplained weight loss of > 15% during the previous year or history of anorexia nervosa, medications that interfere with vitamin D metabolism; patients with a habitual dietary calcium intake that exceeds 800 mg/day; smokers greater than one pack per day, patients reporting alcohol intake greater than two drinks daily and serum 25‐hydroxyvitamin D level > 75 nmol/L |
| Interventions | Participants will be randomly assigned to receive: Intervention 1: vitamin D3 (4000 IU) daily; Intervention 2: calcium (1200 mg) daily; Intervention 3: vitamin D3 (4000 IU) plus calcium (1200 mg) daily; or Intervention group 4 (control group): placebo daily for a period of six months |
| Outcomes | Primary outcome measures will be the influence of calcium supplementation alone on serum parathyroid hormone levels and bone markers in healthy adult women. Secondary outcome measures will be the interaction between calcium and vitamin D supplementation and their combined effect on serum parathyroid hormone levels and bone markers in healthy adult women |
| Starting date | November 2008. Expected completion: 2009 |
| Contact information | John F Aloia, MD; [email protected] |
| Notes |
| Trial name or title | Vitamin D/calcium polyp prevention study |
| Methods | Randomised, double‐blind, placebo‐controlled trial using 2 × 2 factorial design |
| Participants | Country: United States Estimated number of participants: 2200 Inclusion criteria: aged 45 to 75 years; one or more histologically verified neoplastic polyp (adenoma) that measures at least 2 mm removed from the large bowel, with the entire large bowel examined by colonoscopy and documented to be free of further polyps or areas suspicious for neoplasia within 120 days of trial entry; anticipated colonoscopic follow‐up three years or five years after the qualifying colonoscopy; agreement to avoid pregnancy (i.e. use of standard contraception); willingness to forego calcium supplementation (including multivitamins containing calcium) or, for women only, option of taking calcium supplementation of 1200 mg daily (contained in the trial pills); willingness to forego vitamin D supplementation (including multivitamins containing vitamin D); agreement to daily dietary intake of the equivalent of not more than 1200 mg calcium; agreement to daily dietary intake of the equivalent of not more than 400 IU vitamin D; blood calcium level within normal range; blood creatinine level not to exceed 20% above upper limit of normal; serum 25‐hydroxyvitamin D within lower limit of normal to 70 ng/mL; ability and willingness to follow the trial protocol, as indicated by provision of informed consent to participate; good general health, with no severely debilitating diseases or active malignancy that might compromise the participant's ability to complete the trial Exclusion criteria: participation in another colorectal (bowel) trial in the past five years; current participation in any other clinical trial (intervention trial); pregnancy or lactation; a diagnosis of narcotic or alcohol dependence in the past five years; a diagnosis of dementia (e.g. Alzheimer's) in the past five years; a diagnosis of a significant psychiatric disability (e.g. schizophrenia, refractory bipolar disorder, current severe depression) in the past five years; any diagnosis of kidney stones; a diagnosis of granulomatous diseases (e.g. sarcoidosis), active chronic fungal or mycobacterial infection (tuberculosis, histoplasmosis, coccidioidomycosis, blastomycosis), berylliosis, Wegener's granulomatosis in the past five years; hyperparathyroidism or other serious disturbance of calcium metabolism in the past five years; a diagnosis of severe kidney disease (e.g. chronic renal failure) in the past five years; unexplained hypercalcaemia in the past five years; osteoporosis with physician recommendation for treatment of low bone mass; two or more low trauma fractures in the past five years; medical condition requiring treatment with vitamin D (e.g. osteomalacia) in the past five years; invasive carcinoma of the large bowel (even if confined to a polyp); familial colorectal cancer syndromes (e.g. familial adenomatous polyposis (FAP), including Gardner syndrome, Turcot's syndrome), hereditary nonpolyposis colorectal cancer (HNPCC), hamartomatous polyposis syndromes (including Peutz‐Jeghers or familial juvenile polyposis); inflammatory bowel disease (e.g. Crohn's disease, ulcerative colitis); a diagnosis of chronic intestinal malabsorption syndromes (e.g. celiac sprue, bacterial overgrowth, chronic pancreatitis, pancreatic insufficiency) in the past five years; large bowel resection; a diagnosis of malignancy other than non‐melanoma skin cancer in the past five years; severe lung disease class three or four (e.g. COPD or emphysema requiring oxygen) in the past five years; severe heart disease: cardiovascular disease functional class three or four in the past five years; severe liver disease (e.g. cirrhosis); any HIV‐positive diagnosis; active hepatitis B, defined as Hep B surface antigen positive; active hepatitis C, defined as measurable HCV RNA; use of long‐term oral corticosteroid therapy in the past five years; use of lithium in the past five years; use of phenytoin in the past five years; use of quinidine in the past five years; use of therapeutic vitamin D in the past five years |
| Interventions | Participants will be randomly assigned to receive: Intervention group 1: vitamin D3 (1000 IU) daily; Intervention group 2: calcium (1200 mg) daily; Intervention group 3: vitamin D3 (1000 IU) plus calcium (1200 mg) daily; or Intervention group 4 (control group): placebo daily for a period of five years. Women who decline to forego calcium supplementation will be randomly assigned only to calcium alone or to calcium plus vitamin D intervention |
| Outcomes | Primary outcome measure will be new adenomas detected on follow‐up colonoscopy |
| Starting date | July 2004. Expected completion: December 2017 |
| Contact information | John A Baron, MD, Principal Investigator, Dartmouth‐Hitchcock Medical Center |
| Notes |
| Trial name or title | Vitamin D supplementation in younger women |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (five intervention groups) |
| Participants | Country: United States Estimated number of participants: 200 Inclusion criteria: premenopausal Caucasian or African American women, aged 25 to 45 years (women with hysterectomy and/or oophorectomy must have a premenopausal follicle‐stimulating hormone level); serum 25‐hydroxyvitamin D level 5 to 20 ng/mL; BMI < 45 kg/m2; willing to discontinue vitamin D supplements after entering the trial; negative pregnancy test before BMD and calcium absorption tests; willing to give signed informed consent form Exclusion criteria: cancer (exceptions: basal cell carcinoma or cancer that occurred more than 10 years ago) or terminal illness; previous hip fracture; hemiplegia; uncontrolled type I diabetes ± significant proteinuria or fasting blood sugar > 140 mg in type II diabetes; kidney stones more than two in a lifetime; chronic renal failure (serum creatinine > 1.4 mg/dL); evidence of chronic liver disease, including alcoholism; physical conditions such as severe osteoarthritis, rheumatoid arthritis, heart failure severe enough to prevent reasonable physical activity; previous treatment with bisphosphonates (longer than three months), parathyroid hormone (PTH) or PTH derivatives (e.g. teriparatide or fluoride) in the past six months; previous treatment within the past six months with calcitonin or oestrogen (except birth control pills); long‐term high‐dose corticosteroid therapy (> 10 mg/day) for over six months and not within the past six months; anticonvulsant therapy (Dilantin, phenobarbital); high‐dose thiazide therapy (> 37.5 mg); 24‐hour urine calcium > 290 mg on two baseline tests; serum calcium exceeding upper normal limit on two baseline tests; bone mineral density; T‐score less than ‐3.0 for spine or hip |
| Interventions | Participants will be randomly assigned to receive: Intervention group 1: vitamin D3 (400 IU) daily; Intervention group 2: vitamin D3 (800 IU) daily; Intervention group 3: vitamin D3 (1600 IU) daily; Intervention group 4: vitamin D3 (2400 IU) daily; or Intervention group 5 (control group): placebo daily for a period of one year |
| Outcomes | Primary outcome measures will be serum 25‐hydroxyvitamin D and parathyroid hormone. Secondary outcome measures will be serum and urine calcium levels |
| Starting date | October 2007; Expected completion: January 2012 |
| Contact information | JC Gallagher, MD; tel: 402‐280‐4518; [email protected] |
| Notes |
| Trial name or title | Vitamin D for chemoprevention |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (four intervention groups) |
| Participants | Country: United States Estimated number of participants: 320 Inclusion criteria: healthy black participants 30 to 80 years of age; comfortable communicating in English; currently with a primary care physician; willing to discontinue vitamin D or calcium supplements; willing to have all protocol specific tests run Exclusion criteria: plans on taking a vacation or travelling to a sunny region within three months of vitamin supplementation period except for a short period (i.e. one weekend); pregnant or breast feeding or planning on becoming pregnant in the following year; pre‐existing calcium (including hypercalcaemia), parathyroid conditions (including hyperparathyroidism), sarcoidosis; no concurrent active malignancies (other than non‐melanoma skin cancer) or previous diagnosis of prostate cancer; cognitively impaired; active thyroid disease (e.g. Graves', Hashimoto's or thyroiditis); history of nephrolithiasis, chronic liver disease, chronic renal disease or renal dialysis |
| Interventions | Participants will be randomly assigned to receive: Intervention group 1: vitamin D3 (1000 IU) daily; Intervention group 2: vitamin D3 (2000 IU) daily; Intervention group 3: vitamin D3 (4000 IU) daily; or Intervention group 4 (control group): placebo daily for a period of three months. Participants will be followed six months |
| Outcomes | Primary outcome measures will include to identify among blacks a dose of oral vitamin D supplementation that will result in levels of plasma 25‐hydroxyvitamin D that would be predicted to reduce colorectal cancer occurrence. Secondary outcome measures will be to determine the influence of oral vitamin D supplementation on inflammatory markers and to compare germline polymorphic variation in vitamin D pathway genes between blacks and a cohort of whites |
| Starting date | October 2007; Expected completion: October 2009 |
| Contact information | Charles Fuchs, MD; tel: (617) 632‐5840; [email protected] |
| Notes |
| Trial name or title | Vitamin D, glucose control and insulin sensitivity in African‐Americans |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (two intervention groups) |
| Participants | Country: United States Estimated number of participants: 96 Inclusion criteria: African‐American by self designation aged 40 and older; glucose intolerance; body mass index 25.0 to 39.9 Exclusion criteria: diabetes potentially requiring pharmacotherapy, defined as A1c > 7%; uncontrolled thyroid disease; current parathyroid, liver or kidney disease; renal stone within five years; sarcoidosis, current pancreatitis, active tuberculosis, hemiplegia, gout; inflammatory bowel disease, colostomy, malabsorption; cancer other than basal cell skin cancer within five years; uncontrolled arrhythmia in past year; albinism or other condition associated with reduced skin pigmentation; pregnancy over the past year; intent to become pregnant; menopause onset within one year; any other unstable medical condition laboratory tests; fasting plasma glucose < 100; haemoglobin A1c > 7%; laboratory evidence of liver disease (e.g. AST > 70 U/L or ALT > 72 IU/L); laboratory evidence of kidney disease (e.g. estimated glomerular filtration rate < 60 mL/min/1.73 m2); elevated spot urine calcium‐to‐creatinine ratio > 0.38 mg/dL; abnormal serum calcium (serum calcium > 10.5 mg/dL); anaemia (hematocrit < 36% in men, < 33% in women); medications (use in past three months; oestrogen or testosterone); prescription vitamin D, lithium; oral corticosteroids; antiseizure medications; unstable doses of psychotropics or phenothiazines; cholestyramine supplements (current use may discontinue after screening); vitamin D supplements, cod liver oil, calcium supplements; body mass index < 25 or > 39.9; consumption of more than 14 alcoholic drinks per week; inability to attend all three trial visits as scheduled; inability to provide written informed consent; age < 40 years; not African‐American (by self designation); participation in another research intervention trial; corresponds to a 24‐hour urinary calcium excretion > 400 mg |
| Interventions | Participants will be randomly assigned to receive: Intervention group 1: vitamin D3 (4000 IU) daily; or Intervention group 2 (control group): placebo daily for a period of 12 weeks |
| Outcomes | Primary outcome measure will be insulin secretion, insulin sensitivity and glucose control |
| Starting date | July 2008; Expected completion: February 2011 |
| Contact information | Nancy Palermo, BS; tel: 617‐556‐3073; [email protected] |
| Notes |
| Trial name or title | Vitamin D and omega‐3 trial (VITAL) |
| Methods | Randomised, double‐blind, placebo‐controlled trial using 2 × 2 factorial design |
| Participants | Country: United States Estimated number of participants: 20,000 Inclusion criteria: men aged 50 or older or women aged 55 or older who have at least a high school education Exclusion criteria: history of cancer (except non‐melanoma skin cancer), heart attack, stroke, transient ischaemic attack, angina pectoris, coronary artery bypass graft or percutaneous coronary intervention; history of renal failure or dialysis, hypercalcaemia, hypoparathyroidism or hyperparathyroidism, severe liver disease (cirrhosis) or sarcoidosis or other granulomatous diseases such as active chronic tuberculosis or Wegener's granulomatosis; allergy to fish or soy; other serious illness that would preclude participation; consuming no more than 800 IU of vitamin D from all supplemental sources combined (individual vitamin D supplements, calcium + vitamin D supplements, medications with vitamin D [e.g. Fosamax Plus D] and multivitamins), or, if taking, willing to decrease or forego such use during the trial; consuming no more than 1200 mg/d of calcium from all supplemental sources combined, or, if taking, willing to decrease or forego such use during the trial; taking fish oil supplements, or, if taking, willing to forego their use during the trial |
| Interventions | Intervention group 1: vitamin D3 and omega‐3; Intervention group 2: vitamin D3 and omega‐3 placebo; Intervention group 3: vitamin D placebo and omega‐3; or Intervention group 4 (control group): vitamin D placebo and omega‐3 placebo orally, daily for a two‐year period |
| Outcomes | Cancer and cardiovascular disease |
| Starting date | July 2010 |
| Contact information | Project manager; 1‐800‐388‐3963; [email protected] www.vitalstudy.org |
| Notes |
| Trial name or title | A trial to study the effect of vitamin D supplementation on glucose and insulin metabolism in centrally obese men |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (two intervention groups) |
| Participants | Country: India Estimated number of participants: 100 Inclusion criteria: male, aged 35 years or older, waist circumference ≥ 78 cm Exclusion criteria: diabetic (fasting blood sugar > 126 mg/dL or on anti‐diabetic medication; blood pressure > 140/90 mmHg or on antihypertensive medication; receiving Vitamin D or calcium supplementation; chronic disease renal/hepatic/malignancy/gastrointestinal; on any medication within the last month that could potentially influence insulin secretion, insulin sensitivity, vitamin D or calcium metabolism; febrile illness or infective morbidity in the past 10 days; past history of nephrolithiasis |
| Interventions | Paraticipants will be randomly assigned to receive: Intervention group 1: vitamin D weekly; or Intervention group 2 (control group): placebo weekly for a period of six weeks |
| Outcomes | Primary outcome measure will be oral glucose insulin sensitivity (OGIS). Secondary outcome measures will be lipid profile, CRP, ApoA1, ApoB and blood pressure |
| Starting date | July 2006; Expected completion: September 2006 |
| Contact information | Jitendra N Pande, MD; Sitaram Bhartia Institute of Science and Research, New Delhi 110016 India |
| Notes |
| Trial name or title | Effects of vitamin D on lipids |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (three intervention groups) |
| Participants | Country: United States Estimated number of participants: 90 Inclusion criteria: any medically stable person with hypercholesterolaemia able to swallow pills Exclusion criteria: clinical instability of underlying disease process (e.g. recent hospitalisation, change of dosages of medications within the prior two weeks, or new medications within one month); recent transfusion; severe renal failure or dialysis; hypercalcaemia; malignancy under active treatment; feeding tube; intestinal bypass surgery; inability to swallow tablets |
| Interventions | Paraticipants will be randomly assigned to receive: Intervention group 1: vitamin D2 (1000 IU) daily; Intervention group 2: vitamin D3 (1000 IU) daily; or Intervention group 3 (control group): placebo daily for a period of 12 weeks |
| Outcomes | Primary outcome measure will be low‐density lipoprotein‐cholesterol. Secondary outcome measures will be vitamin D and metabolite concentrations with supplementation and time course of repletion in deficient or insufficient participants, measures of inflammatory markers |
| Starting date | July 2008; Expected completion: April 2010 |
| Contact information | Janice B Schwartz, MD; Jewish Home, University of California, San Francisco |
| Notes |
| Trial name or title | ViDA (vitamin D assessment) trial |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (two intervention groups) |
| Participants | Country: New Zealand Estimated number of participants: 5100 Inclusion criteria: age 50 to 84 years; ability to give informed consent; resident in Auckland at recruitment; anticipated residence in New Zealand for the four‐year study period Exclusion criteria: current use of vitamin D supplements (> 600 IU per day if aged 50 to 70 years; > 800 IU per day if aged 71 to 84 years); diagnosis of psychiatric disorders that would limit ability to comply with study protocol (i.e. history of regular exacerbation of major psychosis (schizophrenia, bipolar disorder) in past two years); history of hypercalcaemia, nephrolithiasis, sarcoidosis, parathyroid disease or gastric bypass surgery; enrolled in another study, which could affect participation in the vitamin D study; serum calcium from baseline blood sample > 2.50 mmol/L |
| Interventions | Intervention group 1: vitamin D3 200,000 IU oral capsule at baseline, then 100,000 IU oral capsule monthly (aside from 200,000 IU oral capsule in each June); or Intervention group 2 (control group): placebo (sunflower lecithin) for four years |
| Outcomes | Incidence rate of fatal and non‐fatal cardiovascular disease, as assessed by mortality, hospital discharges and family doctors |
| Starting date | 7/04/2011 |
| Contact information | |
| Notes |
| Trial name or title | The effect of vitamin D supplementation during caloric restriction on intestinal calcium absorption |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (two intervention groups) |
| Participants | Country: United Kingdom Estimated number of participants: 60 Inclusion criteria: postmenopausal women aged 50 to 70 years who are more than two years since last menses; obese or overweight; living in the geographic vicinity of Rutgers University Exclusion criteria: currently taking any medication known to influence calcium or bone metabolism, including hormone replacement therapy, or with evidence of diseases known to influence calcium metabolism (i.e. metabolic bone disease), hyperparathyroidism, untreated thyroid disease, significant immune, hepatic, or renal disease, significant cardiac disease (i.e. heart attack or stroke in the past six months, abnormal electrocardiogram), active malignancy or cancer therapy within the past year; history of kidney stones; weight gain or weight loss (5% of body weight) within three months before recruitment; participation in other investigational studies during the 12‐month trial period; travel for longer than two consecutive weeks during the trial period; usually have a very high or low intake of calcium (more than 1500 mg or less than 500 mg per day) |
| Interventions | Paraticipants will be randomly assigned to receive: Intervention group 1: vitamin D3 (1200 IU) daily plus weight loss; Intervention group 2: (control group): placebo daily plus weight loss; Intervention group 3: vitamin D3 (1200 IU) daily plus weight maintenance; or Intervention group 4 (control group): vitamin D3 (1200 IU) daily plus weight maintenance for a period of five weeks |
| Outcomes | Primary outcome measure will be changes in calcium absorption. Secondary outcome measures will be changes in serum and urine bone markers, hormones, proteins and genes |
| Starting date | March 2007; Expected completion: May 2011 |
| Contact information | Sue Shapses, PhD, RD; [email protected] |
| Notes |
| Trial name or title | The impact of vitamin D supplementation in chronic heart failure |
| Methods | Randomised, double‐blind, placebo‐controlled trial using parallel‐group design (two intervention groups) |
| Participants | Country: United Kingdom Estimated number of participants: 100 Inclusion criteria: patients aged 18 years or over with class II and III heart failure due to left ventricular systolic dysfunction (left ventricular ejection fraction less than or equal to 40%); stable symptoms for three months on maximally tolerated medical therapy with no recent change in medication; able to give informed written consent Exclusion criteria: currently taking (or have taken in the previous three months) calcium or other vitamin supplements; currently prescribed amlodipine or other calcium channel antagonists (intake of spironolactone will be recorded); chronic heart failure due to untreated valvular heart disease; history of primary hyperparathyroidism, sarcoidosis, tuberculosis or lymphoma; vitamin D levels greater than 50 nmol/L |
| Interventions | Patients will be randomly assigned to receive: Intervention group 1: vitamin D3 (4000 IU) daily; or Intervention group 2 (control group): placebo daily for a period of one year |
| Outcomes | Primary outcome measures will be left ventricular function assessed at baseline and 12 months, measured by cardiac magnetic resonance. Secondary outcome measures will be symptom status (New York Heart Association status), measured at baseline, one month, four months, eight months, 12 months; exercise tolerance, measured at baseline and 12 months; quality of life (Minnesota Living With Heart Failure questionnaire, European Quality of Life instrument and a 19‐item Likert scale index), measured at baseline, one month, four months, eight months, 12 months; flow‐mediated dilatation, measured at baseline and 12 months; immune status, measured at baseline and 12 months; insulin resistance, measured at baseline and 12 months; autonomic activation (measured by heart rate variability), measured at baseline and 12 months; renal function, measured at baseline and 1, 4, 8 and 12 months; B‐type natriuretic peptide, measured at baseline and 1, 4, 8 and 12 months |
| Starting date | 01.01.2009; Expected completion: 31.12.2012 |
| Contact information | Klaus Witte Division of Cardiovascular and Diabetes Research |
| Notes |
AST: aspartate aminotransferase; ALT: alanine aminotransferase; BMI: body mass index; CRP: C‐reactive protein; DMSO: dimethyl sulphoxide; DNA: deoxyribonucleic acid; MSM: methylsulfonylmethane
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All‐cause mortality in trials with low or high risk of bias Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| Analysis 1.1  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 1 All‐cause mortality in trials with low or high risk of bias. | ||||
| 1.1 Trials with low risk of bias | 30 | 67516 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.92, 0.99] |
| 1.2 Trials with high risk of bias | 26 | 27770 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.92, 1.06] |
| 2 All‐cause mortality in individually randomised and cluster‐randomised trials Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| Analysis 1.2  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 2 All‐cause mortality in individually randomised and cluster‐randomised trials. | ||||
| 2.1 Individually randomised trials | 54 | 81964 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.93, 0.99] |
| 2.2 Cluster‐randomised trials | 2 | 13322 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.82, 1.34] |
| 3 All‐cause mortality in placebo‐controlled and no intervention trials Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| Analysis 1.3  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 3 All‐cause mortality in placebo‐controlled and no intervention trials. | ||||
| 3.1 Placebo in the control group | 44 | 73892 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.93, 0.99] |
| 3.2 No intervention in the control group | 12 | 21394 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.91, 1.21] |
| 4 All‐cause mortality and risk of industry bias Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| Analysis 1.4  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 4 All‐cause mortality and risk of industry bias. | ||||
| 4.1 Trials without risk of industry bias | 7 | 7372 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.92, 1.03] |
| 4.2 Trials with risk of industry bias | 49 | 87914 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.93, 1.00] |
| 5 All‐cause mortality in primary and secondary prevention trials Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| Analysis 1.5  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 5 All‐cause mortality in primary and secondary prevention trials. | ||||
| 5.1 Primary prevention trials | 48 | 94491 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 5.2 Secondary prevention trials | 8 | 795 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.73, 2.35] |
| 6 All‐cause mortality and vitamin D status Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| Analysis 1.6  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 6 All‐cause mortality and vitamin D status. | ||||
| 6.1 Vitamin D insufficiency | 26 | 56697 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 0.99] |
| 6.2 Vitamin D adequacy | 19 | 16283 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.05] |
| 6.3 Unknown vitamin D status | 11 | 22306 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.92, 1.13] |
| 7 All‐cause mortality in ambulatory and institutionalised participants Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| Analysis 1.7  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 7 All‐cause mortality in ambulatory and institutionalised participants. | ||||
| 7.1 Ambulatory participants | 45 | 86071 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.92, 0.98] |
| 7.2 Institutionalised participants | 11 | 9215 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.92, 1.13] |
| 8 All‐cause mortality ('best‐worst case' and 'worst‐best case' scenario) Show forest plot | 53 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 8 All‐cause mortality ('best‐worst case' and 'worst‐best case' scenario). | ||||
| 8.1 'Best‐worst' case scenario | 53 | 84418 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.32, 0.51] |
| 8.2 'Worst‐best' case scenario | 53 | 84418 | Risk Ratio (M‐H, Random, 95% CI) | 2.78 [2.13, 3.63] |
| 9 All‐cause mortality in trials using vitamin D3 (cholecalciferol) Show forest plot | 38 | 75927 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.91, 0.98] |
| Analysis 1.9  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 9 All‐cause mortality in trials using vitamin D3 (cholecalciferol). | ||||
| 9.1 Vitamin D3 trials with low risk of bias | 20 | 52645 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.89, 0.98] |
| 9.2 Vitamin D3 trials with high risk of bias | 18 | 23282 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 1.00] |
| 10 All‐cause mortality in trials using vitamin D3 singly or combined with calcium Show forest plot | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.10  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 10 All‐cause mortality in trials using vitamin D3 singly or combined with calcium. | ||||
| 10.1 Vitamin D3 singly | 13 | 12609 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.85, 1.00] |
| 10.2 Vitamin D3 combined with calcium | 27 | 63051 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.92, 0.99] |
| 11 All‐cause mortality in trials using low or high dose of vitamin D3 Show forest plot | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.11  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 11 All‐cause mortality in trials using low or high dose of vitamin D3. | ||||
| 11.1 Low dose of vitamin D3 (< 800 IU a day) | 13 | 50437 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.87, 0.97] |
| 11.2 High dose of vitamin D3 (≥ 800 IU a day) | 26 | 25558 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.92, 1.00] |
| 12 All‐cause mortality in trials applying vitamin D3 daily or intermittently Show forest plot | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.12  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 12 All‐cause mortality in trials applying vitamin D3 daily or intermittently. | ||||
| 12.1 Vitamin D3 daily | 31 | 69168 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 0.98] |
| 12.2 Vitamin D3 intermittently | 8 | 6871 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.77, 1.03] |
| 13 All‐cause mortality in trials using vitamin D3 and vitamin D status Show forest plot | 38 | 75927 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.91, 0.98] |
| Analysis 1.13  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 13 All‐cause mortality in trials using vitamin D3 and vitamin D status. | ||||
| 13.1 Vitamin D insufficiency | 20 | 55883 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 0.99] |
| 13.2 Vitamin D adequacy | 10 | 4979 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.80, 1.07] |
| 13.3 Unknown vitamin D status | 8 | 15065 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.78, 1.16] |
| 14 All‐cause mortality in trials using vitamin D3 according to the participant's sex Show forest plot | 38 | 75927 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.91, 0.98] |
| Analysis 1.14  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 14 All‐cause mortality in trials using vitamin D3 according to the participant's sex. | ||||
| 14.1 Vitamin D3 trialsincluding only women | 19 | 53062 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 14.2 Vitamin D3 trials including men and women | 19 | 22865 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.89, 0.98] |
| 15 All‐cause mortality in trials using vitamin D2 (ergocalciferol) Show forest plot | 12 | 18349 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.96, 1.08] |
| Analysis 1.15  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 15 All‐cause mortality in trials using vitamin D2 (ergocalciferol). | ||||
| 15.1 Vitamin D2 trials with low risk of bias | 9 | 14439 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.04] |
| 15.2 Vitamin D2 trials with high risk of bias | 3 | 3910 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.05, 1.37] |
| 16 All‐cause mortality in trials using vitamin D2 singly or combined with calcium Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.16  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 16 All‐cause mortality in trials using vitamin D2 singly or combined with calcium. | ||||
| 16.1 Vitamin D2 singly | 8 | 17079 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.96, 1.12] |
| 16.2 Vitamin D2 combined with calcium | 5 | 1307 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.64, 1.57] |
| 17 All‐cause mortality in trials using low or high dose of vitamin D2 Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.17  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 17 All‐cause mortality in trials using low or high dose of vitamin D2. | ||||
| 17.1 Low dose of vitamin D2 | 1 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.17, 3.98] |
| 17.2 High dose of vitamin D2 | 12 | 18273 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.95, 1.10] |
| 18 All‐cause mortality in trials applying vitamin D2 daily or intermittently Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.18  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 18 All‐cause mortality in trials applying vitamin D2 daily or intermittently. | ||||
| 18.1 Vitamin D2 daily | 6 | 1349 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.68, 1.12] |
| 18.2 Vitamin D2 intermittently | 6 | 17000 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.95, 1.18] |
| 19 All‐cause mortality in trials using vitamin D2 and vitamin D status Show forest plot | 12 | 18349 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.96, 1.08] |
| Analysis 1.19  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 19 All‐cause mortality in trials using vitamin D2 and vitamin D status. | ||||
| 19.1 Vitamin D insufficiency | 6 | 4413 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.05, 1.37] |
| 19.2 Vitamin D adequacy | 5 | 10496 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.10] |
| 19.3 Unknown vitamin D status | 1 | 3440 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.05] |
| 20 All‐cause mortality in trials using alfacalcidol (1α‐hydroxyvitamin D) Show forest plot | 4 | 617 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.22, 4.15] |
| Analysis 1.20  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 20 All‐cause mortality in trials using alfacalcidol (1α‐hydroxyvitamin D). | ||||
| 21 All‐cause mortality in trials using alfacalcidol and vitamin D status Show forest plot | 4 | 617 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.22, 4.15] |
| Analysis 1.21  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 21 All‐cause mortality in trials using alfacalcidol and vitamin D status. | ||||
| 21.1 Vitamin D insufficiency | 2 | 155 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.11, 9.52] |
| 21.2 Vitamin D adequacy | 1 | 378 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.06, 15.37] |
| 21.3 Unknown vitamin D status | 1 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.06, 13.40] |
| 22 All‐cause mortality in trials using calcitriol (1,25‐dihydroxyvitamin D) Show forest plot | 3 | 430 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.27, 7.03] |
| Analysis 1.22  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 22 All‐cause mortality in trials using calcitriol (1,25‐dihydroxyvitamin D). | ||||
| 23 All‐cause mortality in trials using calcitriol and vitamin D status Show forest plot | 3 | 430 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.27, 7.03] |
| Analysis 1.23  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 23 All‐cause mortality in trials using calcitriol and vitamin D status. | ||||
| 23.1 Vitamin D insufficiency | 1 | 86 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.96] |
| 23.2 Vitamin D adequacy | 2 | 344 | Risk Ratio (M‐H, Random, 95% CI) | 2.28 [0.34, 15.39] |
| 24 Cancer mortality Show forest plot | 4 | 44492 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 0.98] |
| Analysis 1.24  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 24 Cancer mortality. | ||||
| 25 Cardiovascular mortality Show forest plot | 10 | 47267 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.90, 1.07] |
| Analysis 1.25  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 25 Cardiovascular mortality. | ||||
| 26 Adverse events Show forest plot | 35 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.26  Comparison 1 Vitamin D versus placebo or no intervention, Outcome 26 Adverse events. | ||||
| 26.1 Hypercalcemia in trials using supplemental forms of vitamin D | 15 | 11323 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.85, 2.18] |
| 26.2 Hypercalcemia in trials using active forms of vitamin D | 3 | 710 | Risk Ratio (M‐H, Random, 95% CI) | 3.18 [1.17, 8.68] |
| 26.3 Nephrolithiasis in trials using vitamin D3 combined with calcium | 4 | 42876 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.02, 1.34] |
| 26.4 Nephrolithiasis in trials using calcitriol | 1 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 8.10] |
| 26.5 Hypercalciuria | 3 | 695 | Risk Ratio (M‐H, Random, 95% CI) | 4.64 [0.99, 21.76] |
| 26.6 Renal insufficiency | 3 | 5495 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [0.27, 10.70] |
| 26.7 Cardiovascular disorders | 8 | 4495 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.86, 1.05] |
| 26.8 Gastrointestinal disorders | 16 | 9702 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.87, 2.13] |
| 26.9 Psychiatric disorders | 3 | 580 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.56, 3.73] |
| 26.10 Skin disorders | 2 | 3810 | Risk Ratio (M‐H, Random, 95% CI) | 3.27 [0.17, 62.47] |
| 26.11 Cancer | 14 | 49707 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.06] |

Study flow diagram.
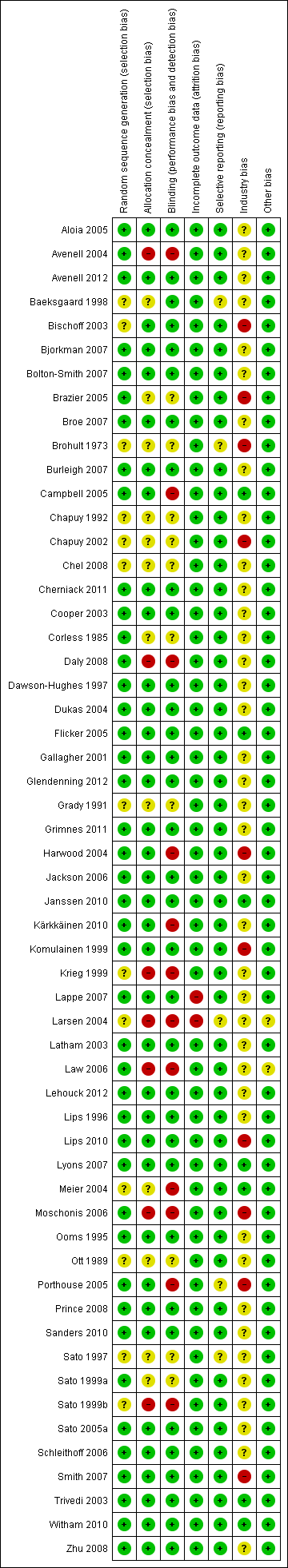
Risk of bias according to bias domains in the 56 randomised clinical trials on vitamin D and mortality.
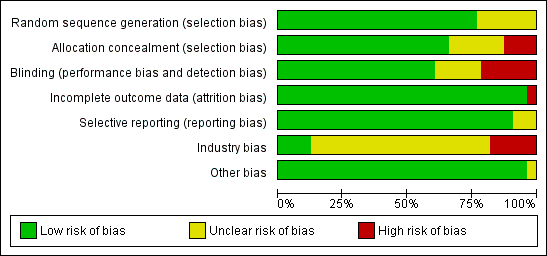
Risk of bias in the included 56 randomised clinical trials on vitamin D and mortality.
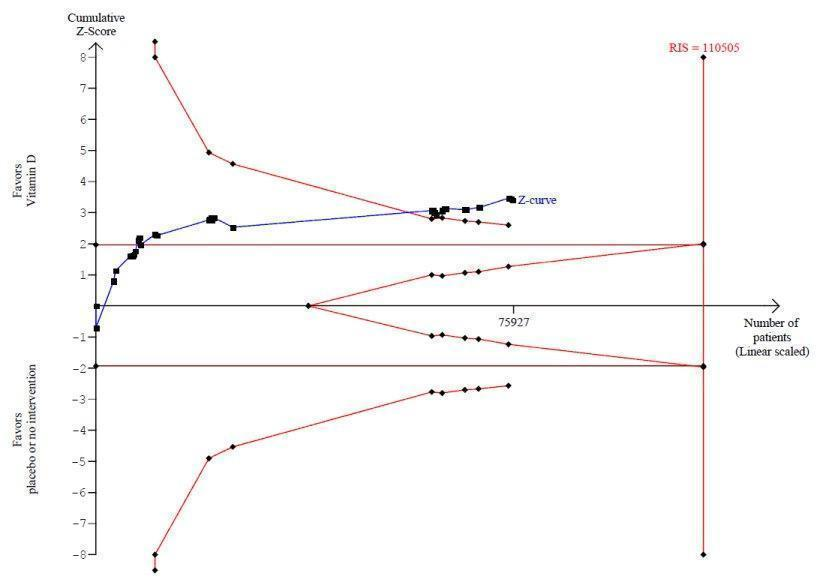
Trial sequential analysis on mortality in 38 vitamin D3 trials
The diversity‐adjusted required information size (RIS) was calculated based on mortality in the control group of 10%; relative risk reduction of 5% in the experimental group; type I error of 5%; and type II error of 20% (80% power). No diversity was noted. The required information size was 110,505 participants. The cumulative Z‐curve (blue line) crossed the trial sequential monitoring boundaries for benefit (red inward sloping line) after the 22nd trial. Accordingly, the risk of random error in the finding seems acceptable according to the O'Brien Fleming stopping rule for an individual trial interim analysis. Subsequently, 16 trials have been published.

Trial sequential analysis on mortality in the 13 trials that administered low dose of vitamin D3 (i.e. a dose less than 800 IU per day)
The diversity‐adjusted required information size (RIS) was calculated based on mortality in the control group of 10%; relative risk reduction of 5% in the experimental group; type I error of 5%; and type II error of 20% (80% power). No diversity was noted. The required information size was 110,505 participants. The cumulative Z‐curve (blue line) did not cross the trial sequential monitoring boundaries for benefit (red line) at any time. Accordingly, the crossing of the conventional statistical 5% boundary (the horizontal brown line) may be due to random errors.

Trial sequential analysis of mortality in 12 vitamin D2 trials
The diversity‐adjusted required information size (RIS) was conducted based on 10% mortality in the control group; relative risk reduction of 10% in the experimental group; type I error of 5%; and type II error of 20% (80% power). No diversity was noted. The required information size was 27,585 participants. The cumulative Z‐curve (blue line) crossed the trial sequential monitoring boundaries for futility (red outward sloping line) after the eighth trial.
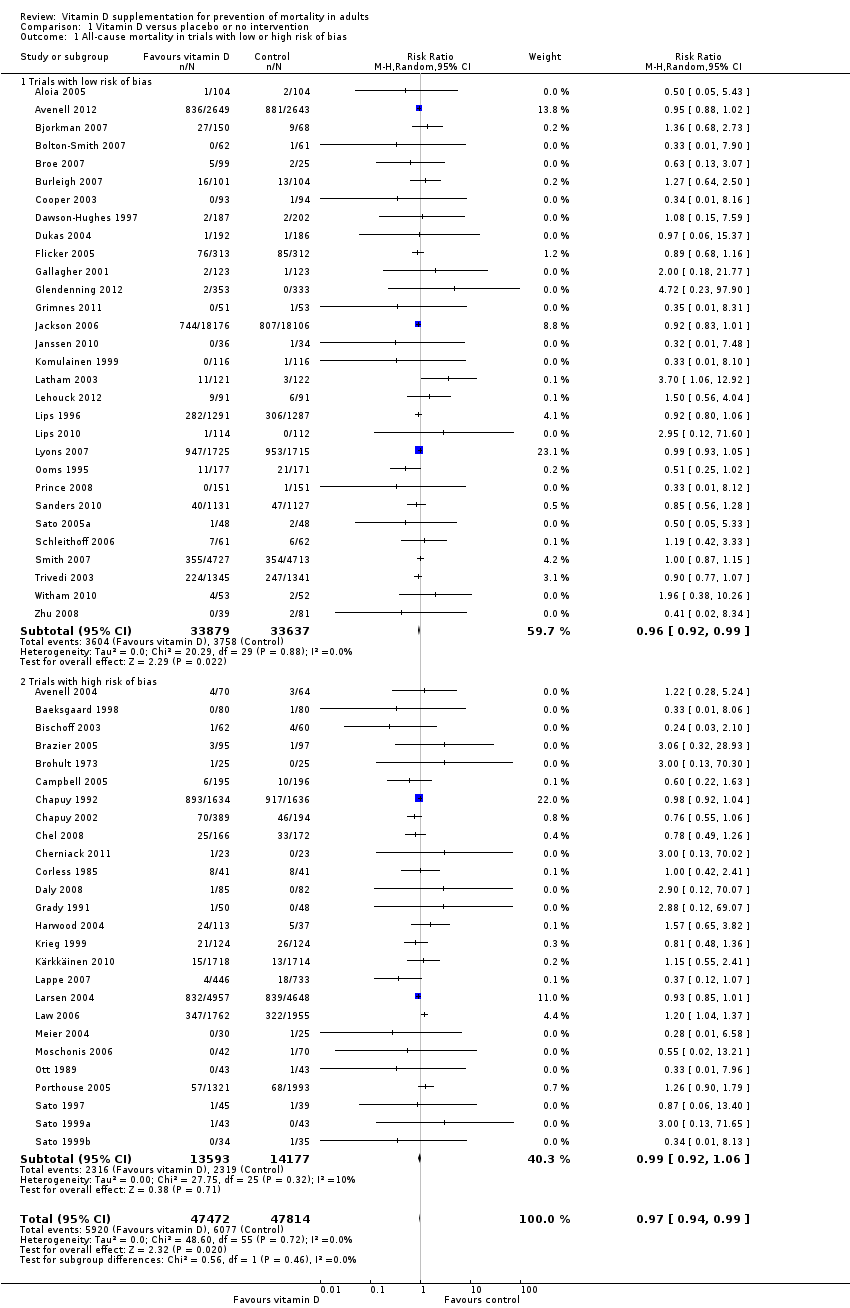
Comparison 1 Vitamin D versus placebo or no intervention, Outcome 1 All‐cause mortality in trials with low or high risk of bias.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 2 All‐cause mortality in individually randomised and cluster‐randomised trials.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 3 All‐cause mortality in placebo‐controlled and no intervention trials.
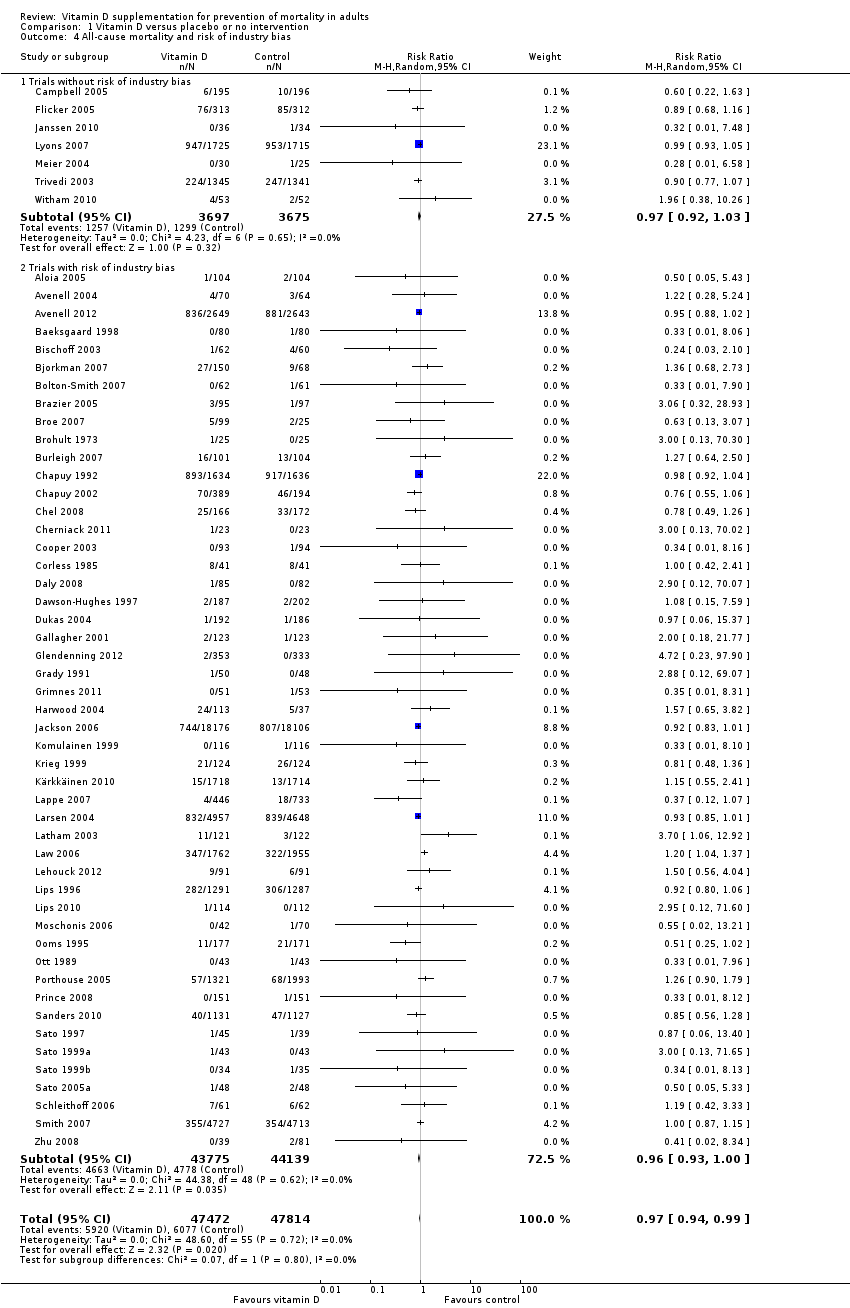
Comparison 1 Vitamin D versus placebo or no intervention, Outcome 4 All‐cause mortality and risk of industry bias.
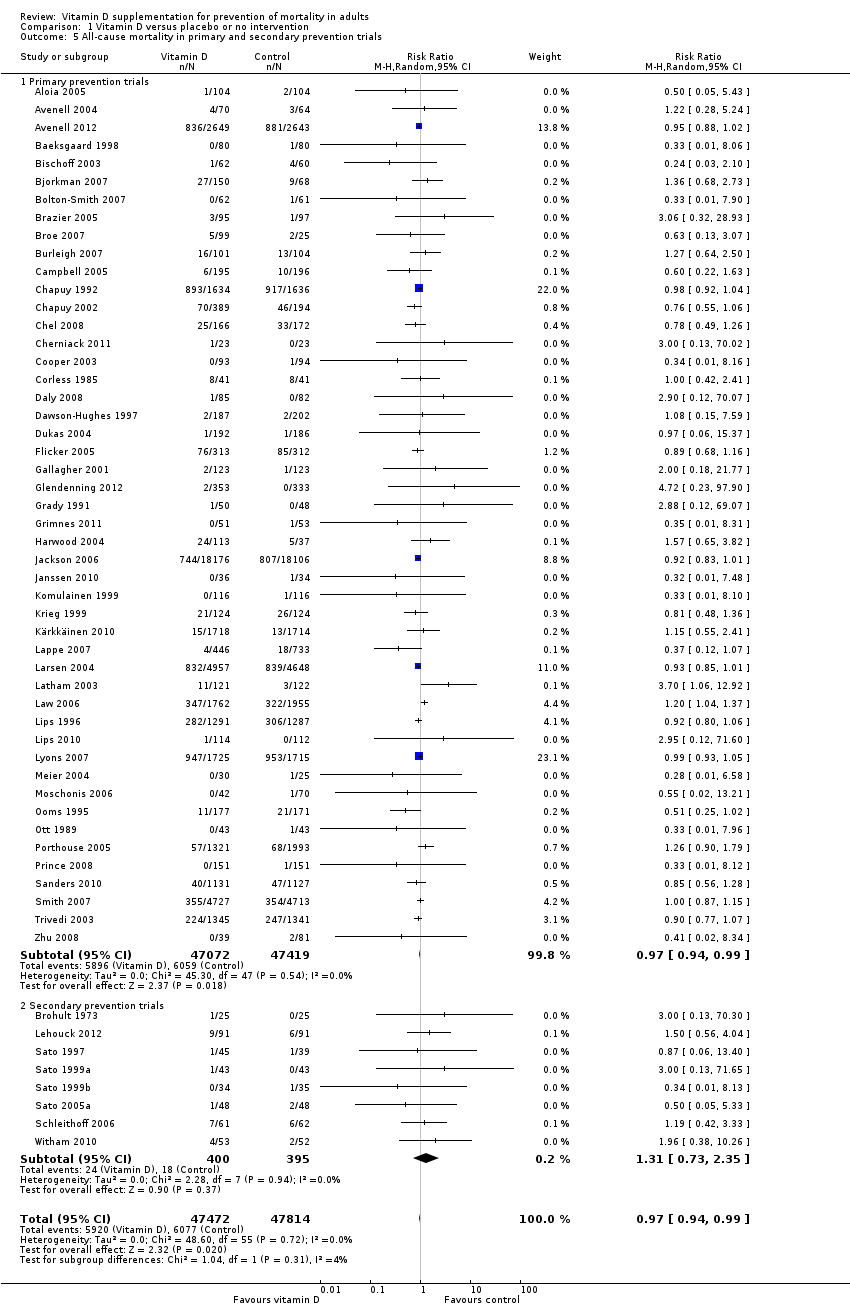
Comparison 1 Vitamin D versus placebo or no intervention, Outcome 5 All‐cause mortality in primary and secondary prevention trials.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 6 All‐cause mortality and vitamin D status.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 7 All‐cause mortality in ambulatory and institutionalised participants.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 8 All‐cause mortality ('best‐worst case' and 'worst‐best case' scenario).

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 9 All‐cause mortality in trials using vitamin D3 (cholecalciferol).

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 10 All‐cause mortality in trials using vitamin D3 singly or combined with calcium.
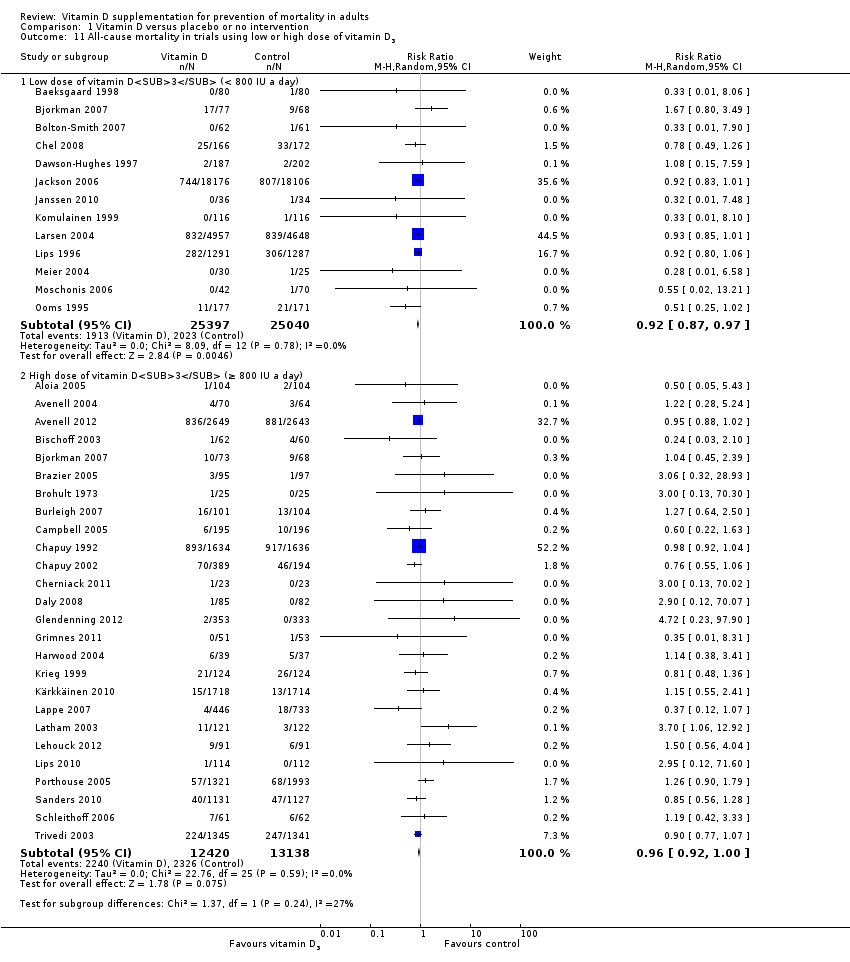
Comparison 1 Vitamin D versus placebo or no intervention, Outcome 11 All‐cause mortality in trials using low or high dose of vitamin D3.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 12 All‐cause mortality in trials applying vitamin D3 daily or intermittently.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 13 All‐cause mortality in trials using vitamin D3 and vitamin D status.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 14 All‐cause mortality in trials using vitamin D3 according to the participant's sex.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 15 All‐cause mortality in trials using vitamin D2 (ergocalciferol).
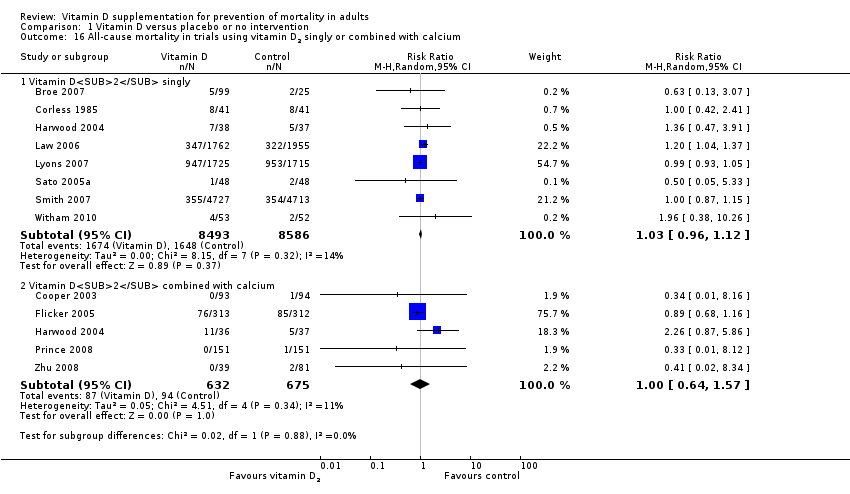
Comparison 1 Vitamin D versus placebo or no intervention, Outcome 16 All‐cause mortality in trials using vitamin D2 singly or combined with calcium.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 17 All‐cause mortality in trials using low or high dose of vitamin D2.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 18 All‐cause mortality in trials applying vitamin D2 daily or intermittently.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 19 All‐cause mortality in trials using vitamin D2 and vitamin D status.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 20 All‐cause mortality in trials using alfacalcidol (1α‐hydroxyvitamin D).

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 21 All‐cause mortality in trials using alfacalcidol and vitamin D status.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 22 All‐cause mortality in trials using calcitriol (1,25‐dihydroxyvitamin D).
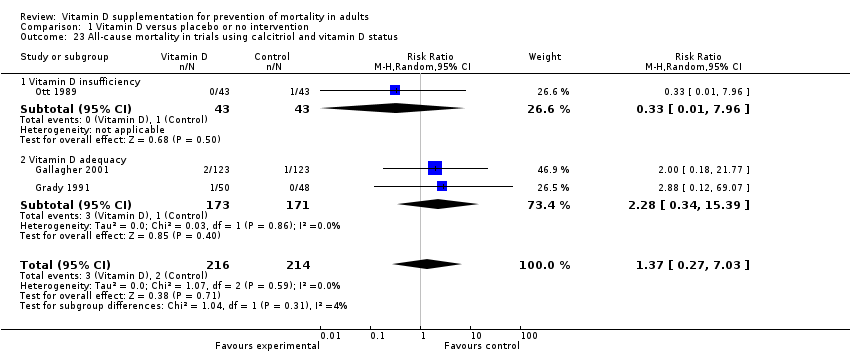
Comparison 1 Vitamin D versus placebo or no intervention, Outcome 23 All‐cause mortality in trials using calcitriol and vitamin D status.
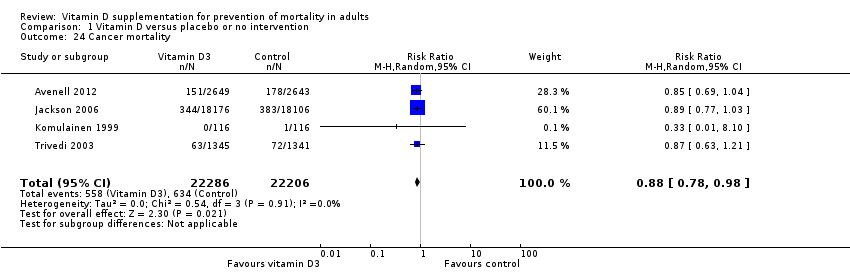
Comparison 1 Vitamin D versus placebo or no intervention, Outcome 24 Cancer mortality.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 25 Cardiovascular mortality.

Comparison 1 Vitamin D versus placebo or no intervention, Outcome 26 Adverse events.
| Vitamin D supplementation for prevention of mortality in adults | ||||||
| Population: adults | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo or no intervention | Vitamin D | |||||
| All‐cause mortality in trials using vitamin D3 (Follow‐up: 0.08 to 7 years) | Study population | RR 0.94 | 75,927 | ⊕⊕⊕⊝ moderatea | Trial sequential analysis of all trials irrespective of bias risks showed that the required information size had not yet been reached and that the cumulative Z‐curve crossed the trial sequential monitoring boundary for benefit. If this is correct, the intervention effect corresponds to a number needed to treat for a beneficial outcome (NNTB) of 150 participants over five years to save one additional life | |
| 114 per 1000 | 107 per 1000 | |||||
| Moderate risk | ||||||
| 46 per 1000 | 43 per 1000 | |||||
| Cardiovascular mortality in trials using vitamin D3 (cholecalciferol) (Follow‐up: 0.31 to 6.2 years) | Study population | RR 0.98 | 47,267 | ⊕⊕⊝⊝ lowb | Trial sequential analysis showed that the cumulative Z‐curve did not cross the conventional monitoring boundary for benefit. The required information size was 2,539,845 participants | |
| 42 per 1000 | 41 per 1000 | |||||
| Moderate risk | ||||||
| 13 per 1000 | 11 per 1000 | |||||
| Cancer mortality in trials using vitamin D3 (cholecalciferol) (Follow‐up: 5 to 7 years) | Study population | RR 0.88 | 44,492 | ⊕⊕⊕⊝ moderatea | Trial sequential analysis showed that the cumulative Z‐curve did not cross the conventional monitoring boundary for benefit. The required information size was 66,724 participants | |
| 29 per 1000 | 25 per 1000 | |||||
| Moderate risk | ||||||
| 21 per 1000 | 19 per 1000 | |||||
| Adverse events: nephrolithiasis in trials using vitamin D3 combined with calcium (Follow‐up: 1.25 to 7 years) | Study population | RR 1.17 | 42,876 | ⊕⊕⊕⊝ | ||
| 18 per 1000 | 21 per 1000 | |||||
| Moderate risk | ||||||
| 9 per 1000 | 11 per 1000 | |||||
| Adverse events: hypercalcaemia in trials using the active forms of vitamin D (alfacalcidol and calcitriol) (Follow‐up: 0.75 to 3 years) | Study population | RR 3.18 | 710 | ⊕⊕⊝⊝ | ||
| 23 per 1000 | 72 per 1000 | |||||
| Moderate risk | ||||||
| 11 per 1000 | 15 per 1000 | |||||
| Health‐related quality of life (Follow‐up: 0.38 years) | See comment | See comment | Not estimable | 105 (1) | See comment | Insufficient information: significant worsening in disease‐specific quality of life in the vitamin D2 group compared with the placebo group was reported. The between‐group difference at 20 weeks was 5.3 (0.5 to 10.2), and the minimally important difference (MID) is estimated to be 5 points in either direction |
| Health economics (Follow‐up: 4 years) | See comment | See comment | Not estimable | 3270 (1) | See comment | Insufficient information: authors reported that vitamin D3 and calcium supplementation prevented 46 hip fractures in every 1000 women treated |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded by one level because of risk of attrition bias | ||||||
| Characteristic Study ID | Design | Arms | Bias | Blinding | Participants | Women | Mean |
| Aloia 2005 | Parallel | 2 | Low | PL | 208 | 100 | 60 |
| Avenell 2004 | 2 × 2 | 4 | High | NI | 134 | 83 | 77 |
| Avenell 2012 | 2 × 2 | 4 | Low | PL | 5292 | 85 | 77 |
| Baeksgaard 1998 | Parallel | 3 | High | PL | 240 | 100 | 62.5 |
| Bischoff 2003 | Parallel | 2 | High | PL | 122 | 100 | 85.3 |
| Bjorkman 2007 | Parallel | 3 | Low | PL | 218 | 82 | 84.5 |
| Bolton‐Smith 2007 | 2 × 2 | 4 | Low | PL | 244 | 100 | 68 |
| Brazier 2005 | Parallel | 2 | High | PL | 192 | 100 | 74.6 |
| Broe 2007 | Parallel | 5 | Low | PL | 124 | 73 | 89 |
| Brohult 1973 | Parallel | 2 | High | PL | 50 | 68 | 52 |
| Burleigh 2007 | Parallel | 2 | Low | PL | 205 | 59 | 83 |
| Campbell 2005 | 2 × 2 | 4 | High | NI | 391 | 68 | 83.6 |
| Chapuy 1992 | Parallel | 2 | High | PL | 3270 | 100 | 84 |
| Chapuy 2002 | Parallel | 3 | High | PL | 610 | 100 | 85 |
| Chel 2008 | Parallel | 6 | High | PL | 338 | 77 | 84 |
| Cherniack 2011 | Parallel | 2 | High | PL | 46 | 2 | 80 |
| Cooper 2003 | Parallel | 2 | Low | PL | 187 | 100 | 56 |
| Corless 1985 | Parallel | 2 | High | PL | 65 | 78 | 82.4 |
| Daly 2008 | Parallel | 2 | High | NI | 167 | 0 | 61.9 |
| Dawson‐Hughes 1997 | Parallel | 2 | Low | PL | 389 | 55 | 71 |
| Dukas 2004 | Parallel | 2 | Low | PL | 378 | 51 | 71 |
| Flicker 2005 | Parallel | 2 | Low | PL | 625 | 95 | 83.4 |
| Gallagher 2001 | 2 × 2 | 4 | Low | PL | 489 | 100 | 71.5 |
| Glendenning 2012 | Parallel | 2 | Low | PL | 686 | 100 | 76.7 |
| Grady 1991 | Parallel | 2 | High | PL | 98 | 54 | 79.1 |
| Grimnes 2011 | Parallel | 2 | Low | PL | 104 | 49 | 52 |
| Harwood 2004 | Parallel | 4 | High | NI | 150 | 100 | 81.2 |
| Jackson 2006 | Parallel | 2 | Low | PL | 36,282 | 100 | 62.4 |
| Janssen 2010 | Parallel | 2 | Low | PL | 70 | 100 | 80.8 |
| Komulainen 1999 | 2 × 2 | 4 | Low | PL | 464 | 100 | 52.7 |
| Krieg 1999 | Parallel | 2 | High | NI | 248 | 100 | 84.5 |
| Kärkkäinen 2010 | Parallel | 2 | High | NI | 3139 | 100 | 67 |
| Lappe 2007 | Parallel | 3 | High | PL | 1179 | 100 | 66.7 |
| Larsen 2004 | 2 × 2 | 4 | High | NI | 9605 | 60 | 75 |
| Latham 2003 | 2 × 2 | 4 | Low | PL | 243 | 53 | 79.5 |
| Law 2006 | Parallel | 2 | High | NI | 3717 | 76 | 85 |
| Lehouck 2012 | Parallel | 2 | Low | PL | 181 | 20 | 68 |
| Lips 1996 | Parallel | 2 | Low | PL | 2578 | 74 | 80 |
| Lips 2010 | Parallel | 2 | Low | PL | 226 | NR | 78 |
| Lyons 2007 | Parallel | 2 | Low | PL | 3440 | 76 | 84 |
| Meier 2004 | Parallel | 2 | High | NI | 55 | 65 | 56.5 |
| Mochonis 2006 | Parallel | 3 | High | NI | 112 | 100 | 60.3 |
| Ooms 1995 | Parallel | 2 | Low | PL | 348 | 100 | 80.3 |
| Ott 1989 | Parallel | 2 | High | PL | 86 | 100 | 67.5 |
| Porthouse 2005 | Parallel | 2 | High | NI | 3314 | 100 | 76.8 |
| Prince 2008 | Parallel | 2 | Low | PL | 302 | 100 | 77.2 |
| Sanders 2010 | Parallel | 2 | Low | PL | 2258 | 100 | 76.0 |
| Sato 1997 | Parallel | 2 | High | PL | 64 | 45 | 68.5 |
| Sato 1999a | Parallel | 2 | High | PL | 86 | 78 | 70.6 |
| Sato 1999b | Parallel | 3 | High | NI | 103 | 56 | 70.7 |
| Sato 2005a | Parallel | 2 | Low | PL | 96 | 100 | 74.1 |
| Schleithoff 2006 | Parallel | 2 | Low | PL | 123 | 17 | 51 |
| Smith 2007 | Parallel | 2 | Low | PL | 9440 | 54 | 79.1 |
| Trivedi 2003 | Parallel | 2 | Low | PL | 2686 | 24 | 74.7 |
| Witham 2010 | Parallel | 2 | Low | PL | 105 | 34 | 79.7 |
| Zhu 2008 | Parallel | 3 | Low | PL | 120 | 100 | 75 |
| NI: no intervention; NR: not reported; PL: placebo | |||||||
| Characteristic Study ID | Participants | Outcome Measures | Country | Sponsor |
| Aloia 2005 | Black postmenopausal African‐American women | Bone mineral density | USA | No |
| Avenell 2004 | Elderly people with an osteoporotic fracture within the past 10 years | Recruitment, compliance and retention within a randomised trial | UK | Yes |
| Avenell 2012 | Elderly people with low‐trauma osteoporotic fracture in the previous 10 years | Fractures | UK | Yes |
| Baeksgaard 1998 | Postmenopausal women | Bone mineral density | Denmark | Yes |
| Bischoff 2003 | Elderly women living in institutional care | Falls | Switzerland | Yes |
| Bjorkman 2007 | Chronically bedridden patients | Parathyroid function and bone mineral density | Finland | Yes |
| Bolton‐Smith 2007 | Elderly non‐osteoporotic women | Bone mineral density | UK | Yes |
| Brazier 2005 | Elderly vitamin D–insufficient women | Bone mineral density | France | Yes |
| Broe 2007 | Nursing home residents | Falls | USA | Yes |
| Brohult 1973 | Patients with rheumatoid arthritis | Objective and subjective improvement | Sweden | Yes |
| Burleigh 2007 | Older geriatric inpatients | Falls | UK | Yes |
| Campbell 2005 | Elderly people with visual impairment | Numbers of falls and injuries resulting from falls | New Zealand | No |
| Chapuy 1992 | Healthy ambulatory women | Fractures | France | Yes |
| Chapuy 2002 | Elderly people living in institutional care | Biochemical variables of calcium homeostasis, femoral neck bone mineral density and hip | France | Yes |
| Chel 2008 | Nursing home residents | Vitamin D status | Netherlands | Yes |
| Cherniack 2011 | Elderly people | Vitamin D status | USA | Yes |
| Cooper 2003 | Postmenopausal women | Bone mineral density | Australia | Yes |
| Corless 1985 | Elderly patients from the geriatric wards | Abilities to carry out basic activities of daily life | UK | Yes |
| Daly 2008 | Healthy ambulatory men | Bone mineral density | Australia | Yes |
| Dawson‐Hughes 1997 | Healthy ambulatory participants | Bone mineral density | USA | Yes |
| Dukas 2004 | Elderly people | Falls | Switzerland | Yes |
| Flicker 2005 | Elderly people living in institutional care | Falls and fractures | Australia | No |
| Gallagher 2001 | Elderly women | Bone mineral density | USA | No |
| Glendenning 2012 | Elderly community‐dwelling ambulatory women | Falls, muscular strength and mobility | Australia | No |
| Grady 1991 | Elderly people | Muscle strength | USA | Yes |
| Grimnes 2011 | Healthy people with a low vitamin D status | Insulin sensitivity and secretion | Norway | No |
| Harwood 2004 | Elderly women following surgery for hip fracture | Bone mineral density, falls and fractures | UK | Yes |
| Jackson 2006 | Postmenopausal women | Fractures | USA | Yes |
| Janssen 2010 | Elderly vitamin D–insufficient women | Muscle strength, power and functional mobility | Netherlands | Yes |
| Komulainen 1999 | Postmenopausal women | Bone mineral density | Finland | Yes |
| Krieg 1999 | Elderly institutionalised women | Bone mineral density | Switzerland | Yes |
| Kärkkäinen 2010 | Postmenopausal women | Falls | Finland | Yes |
| Lappe 2007 | Healthy postmenopausal white women | Fractures | USA | Yes |
| Larsen 2004 | Older community‐dwelling residents | Falls | Denmark | Yes |
| Latham 2003 | Frail elderly people | Self‐rated physical health and falls | New Zealand | No |
| Law 2006 | Nursing home residents | Falls and fractures | UK | No |
| Lehouck 2012 | Patients with chronic obstructive pulmonary disease | Time to first exacerbation | Belgium | Yes |
| Lips 1996 | Elderly people | Fractures | Netherlands | Yes |
| Lips 2010 | Elderly people with vitamin D insufficiency | Postural stability, muscle strength and safety | Netherlands | No |
| Lyons 2007 | Older people living in institutional care | Fractures | UK | No |
| Meier 2004 | Healthy volunteers | Bone mineral density | Germany | No |
| Mochonis 2006 | Postmenopausal women | Bone mineral density | Greece | Yes |
| Ooms 1995 | Elderly people | Bone mineral density | Netherlands | Yes |
| Ott 1989 | Postmenopausal women | Bone mass | USA | Yes |
| Porthouse 2005 | Elderly women with one or more risk factors for hip fracture | Fractures | UK | Yes |
| Prince 2008 | Elderly women with a history of falling and vitamin D insufficiency | Falls | Australia | Yes |
| Sanders 2010 | Elderly women at high risk of fracture | Falls and fractures | Australia | Yes |
| Sato 1997 | Outpatients with hemiplegia after stroke | Bone mineral density and fractures | Japan | No |
| Sato 1999a | Elderly patients with Parkinson's disease | Fractures | Japan | No |
| Sato 1999b | Outpatients with hemiplegia after stroke | Bone mineral density | Japan | Yes |
| Sato 2005a | Hospitalised elderly women with post‐stroke hemiplegia | Falls | Japan | No |
| Schleithoff 2006 | Patients with congestive heart failure | Mortality | Germany | Yes |
| Smith 2007 | Elderly people | Fractures | UK | No |
| Trivedi 2003 | Elderly people | Mortality, fractures | UK | No |
| Witham 2010 | Patients with systolic heart failure | Exercise capacity | UK | No |
| Zhu 2008 | Elderly women | Bone mineral density | Australia | No |
| Characteristic Study ID | D3 | D2 | 1α(OH)D | 1,25(OH)2D | Ca | Regimen | Route | Treatment | Follow‐up |
| Aloia 2005 | 800 |
|
|
| 1200‐1500a | Daily | Oral | 3 | 3 |
| Avenell 2004 | 800 |
|
|
| 1000b | Daily | Oral | 1 | 1 |
| Avenell 2012 | 800 |
|
|
| 500b | Daily | Oral | 3.75 | 6.2 |
| Baeksgaard 1998 | 560 |
|
|
| 1000 | Daily | Oral | 2 | 2 |
| Bischoff 2003 | 800 |
|
|
| 1200a | Daily | Oral | 0.25 | 0.25 |
| Bjorkman 2007 | 400 |
|
|
| 500a | Daily | Oral | 0.5 | 0.5 |
| Bolton‐Smith 2007 | 400 |
|
|
| 1000 | Daily | Oral | 2 | 2 |
| Brazier 2005 | 800 |
|
|
| 1000 | Daily | Oral | 1 | 1 |
| Broe 2007 |
| 200 |
|
|
| Daily | Oral | 0.42 | 0.42 |
| Brohult 1973 | 100,000 | Daily | Oral | 1 | 1 | ||||
| Burleigh 2007 | 800 |
|
|
| 1200a | Daily | Oral | 0.08 | 0.08 |
| Campbell 2005 | 50,000 100,000 |
|
|
|
| Monthly | Oral | 1 | 1 |
| Chapuy 1992 | 800 |
|
|
| 1200 | Daily | Oral | 1.5 | 4 |
| Chapuy 2002 | 800 |
|
|
| 1200 | Daily | Oral | 2 | 2 |
| Chel 2008 | 600 |
|
|
| 800 | Daily | Oral | 0.33 | 0.33 |
| Cherniack 2011 | 2000 | 1200a | Daily | Oral | 0.5 | 0.5 | |||
| Cooper 2003 |
| 10,000 |
|
| 1000a | Weekly | Oral | 2 | 2 |
| Corless 1985 |
| 9000 |
|
|
| Daily | Oral | 0.75 | 0.75 |
| Daly 2008 | 800 |
|
|
| 1000 | Daily | Oral | 2 | 3.5 |
| Dawson‐Hughes 1997 | 700 |
|
|
| 500 | Daily | Oral | 3 | 3 |
| Dukas 2004 |
|
| 1 |
|
| Daily | Oral | 0.75 | 0.75 |
| Flicker 2005 |
| 1000 |
|
| 600a | Daily | Oral | 2 | 2 |
| Gallagher 2001 |
|
|
| 0.5 |
| Daily | Oral | 3 | 5 |
| Glendenning 2012 | 150,000 | Three‐monthly | Oral | 0.5 | 0.75 | ||||
| Grady 1991 |
|
|
| 0.5 |
| Daily | Oral | 0.5 | 0.5 |
| Grimnes 2011 | 20,000 | Twice weekly | Oral | 0.5 | 0.5 | ||||
| Harwood 2004 | 800 | 300,000 |
|
| 1000 | Single dose | Intramuscular Oral | 1 | 1 |
| Jackson 2006 | 400 |
|
|
| 1000 | Daily | Oral | 7 | 7 |
| Janssen 2010 | 400 | 500a | Daily | Oral | 0.5 | 0.5 | |||
| Komulainen 1999 | 300 |
|
|
| 500 | Daily | Oral | 5 | 5 |
| Krieg 1999 | 880 |
|
|
| 1000 | Daily | Oral | 2 | 2 |
| Kärkkäinen 2010 | 800 |
|
|
| 1000 | Daily | Oral | 3 | 3 |
| Lappe 2007 | 1000 |
|
|
| 1400‐1500b | Daily | Oral | 4 | 4 |
| Larsen 2004 | 400 |
|
|
| 1000 | Daily | Oral | 3.5 | 3.5 |
| Latham 2003 | 300,000 |
|
|
|
| Single dose | Oral | 0.003 | 0.5 |
| Law 2006 |
| 100,000 |
|
|
| Four‐monthly | Oral | 0.83 | 0.83 |
| Lehouck 2012 | 100,000 | Monthly | Oral | 1 | 1 | ||||
| Lips 1996 | 400 |
|
|
|
| Daily | Oral | 3.5 | 3.5 |
| Lips 2010 | 8400 | 500a | weekly | Oral | 0.31 | 0.31 | |||
| Lyons 2007 |
| 100,000 |
|
|
| Four‐monthly | Oral | 3 | 3 |
| Meier 2004 | 500 |
|
|
| 500 | Daily | Oral | 0.5 | 1 |
| Mochonis 2006 | 300 |
|
|
| 1200b | Daily | Oral | 1 | 1 |
| Ooms 1995 | 400 |
|
|
|
| Daily | Oral | 2 | 2 |
| Ott 1989 |
|
|
| 0.5 | 1000a | Daily | Oral | 2 | 2 |
| Porthouse 2005 | 800 |
|
|
| 1000 | Daily | Oral | 2 | 2 |
| Prince 2008 |
| 1000 |
|
| 1000a | Daily | Oral | 1 | 1 |
| Sanders 2010 | 500,000 | Yearly | Oral | 2.96 | 2.96 | ||||
| Sato 1997 |
|
| 1 |
| 300a | Daily | Oral | 0.5 | 0.5 |
| Sato 1999a |
|
| 1 |
|
| Daily | Oral | 1.5 | 1.5 |
| Sato 1999b |
|
| 1 |
|
| Daily | Oral | 1 | 1 |
| Sato 2005a |
| 1000 |
|
|
| Daily | Oral | 2 | 2 |
| Schleithoff 2006 | 2000 |
|
|
| 500a | Daily | Oral | 0.75 | 1.25 |
| Smith 2007 |
| 300,000 |
|
|
| Yearly | Intramuscular | 3 | 3 |
| Trivedi 2003 | 100,000 |
|
|
|
| Four‐monthly | Oral | 5 | 5 |
| Witham 2010 | 100,000 |
|
|
| 10‐weekly | Oral | 0.38 | 0.38 | |
| Zhu 2008 |
| 1000 |
|
| 1200b | Daily | Oral | 5 | 5 |
| aEqual dose of calcium was administered to a control group | |||||||||
| Characteristic Study ID | Intervention(s) and control(s) | [N] screened / eligible | [N] randomised | [N] ITT | [N] finishing study | [%] of randomised participants |
| 1. Aloia 2005 | I: vitamin D3 plus calcium | 322 | 104 | 104 | 74 | 71 |
| C: placebo | 104 | 104 | 74 | 71 | ||
| total: | 208 | 208 | 148 | 71 | ||
| 2. Avenell 2004 | I: vitamin D3 | 180 | 70 | 70 | ‐ | ‐ |
| C: no intervention | 64 | 64 | ‐ | ‐ | ||
| total: | 134 | 134 | ‐ | ‐ | ||
| 3. Avenell 2012 | I: vitamin D3 | 15,024 | 2649 | 2649 | 1813 | 68 |
| C: matched placebo tablets | 2643 | 2643 | 1762 | 67 | ||
| total: | 5292 | 5292 | 3575 | 68 | ||
| 4. Baeksgaard 1998 | I: vitamin D3 plus calcium | ‐ | 80 | 80 | 65 | 81 |
| C: matched placebo tablets | 80 | 80 | 64 | 80 | ||
| total: | 160 | 160 | 129 | 80 | ||
| 5. Bischoff 2003 | I: vitamin D3 plus calcium | 130 | 62 | 62 | ‐ | ‐ |
| C: calcium | 60 | 60 | ‐ | ‐ | ||
| total: | 122 | 122 | 89 | 73 | ||
| 6. Bjorkman 2007 | I: vitamin D3 plus calcium | 1215 | 150 | 150 | 123 | 82 |
| C: calcium | 68 | 68 | 59 | 87 | ||
| total: | 218 | 218 | 182 | 83 | ||
| 7. Bolton‐Smith 2007 | I: vitamin D3 plus calcium | ‐ | 62 | 62 | 50 | 81 |
| C: matched placebo | 61 | 61 | 56 | 92 | ||
| total: | 123 | 123 | 106 | 86 | ||
| 8. Brazier 2005 | I: vitamin D3 plus calcium | 360 | 95 | 95 | 74 | 78 |
| C: matched placebo tablets | 97 | 97 | 68 | 70 | ||
| total: | 192 | 192 | 142 | 74 | ||
| 9. Broe 2007 | I: vitamin D2 | 126 | 99 | 99 | 96 | 97 |
| C: matched placebo tablets | 25 | 25 | 25 | 100 | ||
| total: | 124 | 124 | 121 | 98 | ||
| 10. Brohult 1973 | I: vitamin D3 | ‐ | 25 | 25 | 24 | 96 |
| C: placebo | 25 | 25 | 25 | 100 | ||
| total: | 50 | 50 | 49 | 98 | ||
| 11. Burleigh 2007 | I: vitamin D3 plus calcium | 515 | 101 | 101 | 98 | 97 |
| C: placebo | 104 | 104 | 101 | 97 | ||
| total: | 205 | 205 | 199 | 97 | ||
| 12. Campbell 2005 | I: home safety assessment and modification programme | 391 | 195 | 195 | 177 | 91 |
| C: social visits | 196 | 196 | 184 | 94 | ||
| total: | 391 | 391 | 361 | 92 | ||
| 13. Chapuy 1992 | I: vitamin D3 plus calcium | ‐ | 1634 | 1634 | 1590 | 97 |
| C: double placebo | 1636 | 1636 | 1573 | 96 | ||
| total: | 3270 | 3270 | 3163 | 96 | ||
| 14. Chapuy 2002 | I: vitamin D3 plus calcium | 639 | 393 | 393 | ‐ | ‐ |
| C: double placebo | 190 | 190 | ‐ | ‐ | ||
| total: | 583 | 583 | ‐ | ‐ | ||
| 15. Chel 2008 | I: vitamin D3 | 1006 | 166 | 166 | 139 | 84 |
| C: matched placebo tablets | 172 | 172 | 137 | 80 | ||
| total: | 338 | 338 | 276 | 82 | ||
| 16. Cherniack 2011 | I: vitamin D3 plus calcium | 52 | 23 | 23 | 17 | 74 |
| C: matched placebo plus calcium | 23 | 23 | 17 | 74 | ||
| total: | 46 | 46 | 34 | 74 | ||
| 17. Cooper 2003 | I: vitamin D2 plus calcium | ‐ | 93 | 93 | 73 | 78 |
| C: calcium | 94 | 94 | 80 | 85 | ||
| total: | 187 | 187 | 153 | 82 | ||
| 18. Coreless 1985 | I: vitamin D2 | 320 | 32 | 32 | 8 | 25 |
| C: placebo | 33 | 33 | 17 | 51 | ||
| total: | 65 | 65 | 25 | 38 | ||
| 19. Daly 2006 | I: calcium‐vitamin D3–fortified milk plus calcium | 422 | 85 | 85 | 76 | 89 |
| C: no intervention | 82 | 82 | 73 | 89 | ||
| total: | 167 | 167 | 149 | 89 | ||
| 20. Dawson‐Hughes 1997 | I: vitamin D3 plus calcium | 545 | 187 | 187 | 148 | 79 |
| C: placebo | 202 | 202 | 170 | 84 | ||
| total: | 389 | 389 | 318 | 82 | ||
| 21. Dukas 2004 | I: alfacalcidol | 410 | 192 | 192 | ‐ | ‐ |
| C: placebo | 186 | 186 | ‐ | ‐ | ||
| total: | 378 | 378 | ‐ | ‐ | ||
| 22. Flicker 2005 | I: vitamin D3 plus calcium | 1767 | 313 | 313 | 269 | 86 |
| C: calcium | 312 | 312 | 271 | 87 | ||
| total: | 625 | 625 | 540 | 86 | ||
| 23. Gallagher 2001 | I: calcitriol | 1905 | 123 | 123 | 101 | 82 |
| C: matched placebo | 123 | 123 | 112 | 91 | ||
| total: | 246 | 246 | 213 | 87 | ||
| 24. Glendenning 2012 | I: cholecalciferol 150,000 three‐monthly | 2110 | 353 | 353 | 331 | 94 |
| C: placebo vitamin D | 333 | 333 | 307 | 92 | ||
| total: | 686 | 686 | 638 | 93 | ||
| 25. Grady 1991 | I: calcitriol | 98 | 50 | 50 | 49 | 98 |
| C: placebo vitamin D | 48 | 48 | 47 | 98 | ||
| total: | 98 | 98 | 96 | 98 | ||
| 26. Grimnes 2011 | I: vitamin D3 | 108 | 51 | 51 | 49 | 96 |
| C: placebo | 53 | 53 | 45 | 85 | ||
| total: | 104 | 104 | 94 | 90 | ||
| 27. Harwood 004 | I: vitamin D plus calcium | 208 | 113 | 113 | ‐ | ‐ |
| C: no intervention | 37 | 37 | ‐ | ‐ | ||
| total: | 150 | 150 | ‐ | ‐ | ||
| 28. Jackson 2006 | I: vitamin D3 plus calcium | 68,132 | 18,176 | 18,176 | 16,936 | 93 |
| C: matched placebo | 18,106 | 18,106 | 16,815 | 93 | ||
| total: | 36,282 | 36,282 | 33,751 | 93 | ||
| 29. Janssen 2010 | I: vitamin D3 plus calcium | 91 | 36 | 36 | 18 | 50 |
| C: matched placebo vitamin D3 plus calcium | 34 | 34 | 31 | 91 | ||
| total: | 70 | 70 | 49 | 70 | ||
| 30. Komulainen 1999 | I: oestradiol valerate and cyproterone acetate | 13,100 | 116 | 116 | ‐ | ‐ |
| C: placebo | 116 | 116 | ‐ | ‐ | ||
| total: | 232 | 232 | ‐ | ‐ | ||
| 31. Krieg 1999 | I: vitamin D3 plus calcium | ‐ | 124 | 124 | 50 | 40 |
| C: no treatment | 124 | 124 | 53 | 43 | ||
| total: | 248 | 248 | 103 | 41 | ||
| 32. Kärkkäinen 2010 | I: vitamin D3 plus calcium | 5407 | 1718 | 1718 | 1566 | 91 |
| C: no treatment | 1714 | 1714 | 1573 | 92 | ||
| total: | 3432 | 3432 | 3139 | 91 | ||
| 33. Lappe 2007 | I: vitamin D3 plus calcium | 1180 | 446 | 446 | ‐ | ‐ |
| C: calcium plus placebo tablets | 733 | 733 | ‐ | ‐ | ||
| total: | 1179 | 1179 | ‐ | ‐ | ||
| 34. Larsen 2004 | I: home safety inspection, vitamin D3 plus calcium | 62,000 | 4957 | 4957 | ‐ | ‐ |
| C: no intervention | 4648 | 4648 | ‐ | ‐ | ||
| total: | 9605 | 9605 | ‐ | ‐ | ||
| 35. Latham 2003 | I: vitamin D3 | 3,028 | 121 | 121 | 108 | 89 |
| C: matched placebo tablets | 122 | 122 | 114 | 93 | ||
| total: | 243 | 243 | 222 | 91 | ||
| 36. Law 2006 | I: vitamin D2 | ‐ | 1762 | 1762 | 1366 | 77 |
| C: no intervention | 1955 | 1955 | 1569 | 80 | ||
| total: | 3717 | 3717 | 2935 | 79 | ||
| 37. Lehouck 2012 | I: vitamin D3 | 419 | 91 | 91 | 72 | 79 |
| C: matched placebo | 91 | 91 | 78 | 86 | ||
| total: | 182 | 182 | 150 | 82 | ||
| 38. Lips 1996 | I: vitamin D3 | ‐ | 1291 | 1291 | 1061 | 82 |
| C: matched placebo | 1287 | 1287 | 1029 | 80 | ||
| total: | 2578 | 2578 | 2090 | 81 | ||
| 39. Lips 2010 | I: vitamin D3 | 593 | 114 | 114 | 105 | 92 |
| C: matched placebo | 112 | 112 | 97 | 87 | ||
| total: | 226 | 226 | 202 | 89 | ||
| 40. Lyons 2007 | I: vitamin D2 | 5745 | 1725 | 1725 | 778 | 45 |
| C: matched placebo tablets | 1715 | 1715 | 762 | 44 | ||
| total: | 3440 | 3440 | 1540 | 44 | ||
| 41. Meier 2004 | I: vitamin D3 | ‐ | 30 | 30 | 27 | 90 |
| C: no intervention | 25 | 25 | 16 | 64 | ||
| total: | 55 | 55 | 43 | 78 | ||
| 42. Mochonis 2006 | I: vitamin D3 plus calcium | ‐ | 72 | 72 | 65 | 90 |
| C: no intervention | 40 | 40 | 36 | 90 | ||
| total: | 112 | 112 | 101 | 90 | ||
| 43. Ooms 1995 | I: vitamin D3 | ‐ | 177 | 177 | 126 | 71 |
| C: matched placebo | 171 | 171 | 118 | 69 | ||
| total: | 348 | 348 | 244 | 70 | ||
| 44. Ott 1989 | I: vitamin D3 plus calcium | ‐ | 43 | 43 | 39 | 91 |
| C: matched placebo vitamin D plus calcium | 43 | 43 | 37 | 86 | ||
| total: | 86 | 86 | 76 | 88 | ||
| 45. Porthouse 2005 | I: vitamin D3 plus calcium | 11,022 | 1321 | 1321 | 1212 | 92 |
| C: no intervention | 1993 | 1993 | 1862 | 93 | ||
| total: | 3454 | 3454 | 3074 | 92 | ||
| 46. Prince 2008 | I: vitamin D2 plus calcium | 827 | 151 | 151 | 144 | 95 |
| C: matched placebo tablets of vitamin D plus calcium | 151 | 151 | 145 | 96 | ||
| total: | 302 | 302 | 289 | 95 | ||
| 47. Sanders 2010 | I: vitamin D3 | 7204 | 1131 | 1131 | 1015 | 90 |
| C: matched placebo tablets | 1127 | 1127 | 1017 | 90 | ||
| total: | 2258 | 2258 | 1032 | 90 | ||
| 48. Sato 1997 | I: vitamin D (alfacalcidol) plus calcium | ‐ | 45 | 45 | 30 | 67 |
| C: matched placebo tablets of vitamin D and calcium | 39 | 39 | 34 | 87 | ||
| total: | 84 | 84 | 64 | 76 | ||
| 49. Sato 1999a | I: vitamin D (alfacalcidol) | ‐ | 43 | 43 | 40 | 93 |
| C: matched placebo tablets of vitamin D | 43 | 43 | 40 | 93 | ||
| total: | 86 | 86 | 80 | 93 | ||
| 50. Sato 1999b | I: vitamin D (alfacalcidol) | ‐ | 34 | 34 | 32 | 94 |
| C: matched placebo tablet of vitamin D | 35 | 35 | 32 | 91 | ||
| total: | 69 | 69 | 64 | 93 | ||
| 51. Sato 2005a | I: vitamin D2 | ‐ | 48 | 48 | 43 | 90 |
| C: matched placebo tablets of vitamin D | 48 | 48 | 42 | 87 | ||
| total: | 96 | 96 | 85 | 88 | ||
| 52. Schleithoff 2006 | I: vitamin D3 plus calcium | ‐ | 61 | 61 | 42 | 69 |
| C: matched placebo vitamin D plus calcium | 62 | 62 | 51 | 82 | ||
| total: | 103 | 103 | 93 | 90 | ||
| 53. Smith 2007 | I: vitamin D2 | 13,487 | 4727 | 4727 | 2304 | 49 |
| C: matched placebo intramuscular injection | 4713 | 4713 | 2266 | 48 | ||
| total: | 9440 | 9440 | 4570 | 48 | ||
| 54. Trivedi 2003 | I: vitamin D3 | ‐ | 1345 | 1345 | 1262 | 94 |
| C: matched placebo vitamin D | 1341 | 1341 | 1264 | 94 | ||
| total: | 2696 | 2696 | 2526 | 94 | ||
| 55. Witham 2010 | I: vitamin D2 | 173 | 53 | 53 | 48 | 91 |
| C: matched placebo tablets | 52 | 52 | 48 | 91 | ||
| total: | 105 | 105 | 96 | 91 | ||
| 56. Zhu 2008 | I: vitamin D2 plus calcium | ‐ | 39 | 39 | 33 | 85 |
| C: matched placebo vitamin D and calcium | 81 | 81 | 74 | 91 | ||
| total: | 120 | 120 | 107 | 89 | ||
| Grand total | All interventions | 47,472 | 45,351 | |||
| All controls | 47,814 | 45,278 | ||||
| All interventions and controls | 95,286 | 90,629a | ||||
| "‐" denotes not reported aNumbers not available for all studies C: control; I: intervention; ITT: intention‐to‐treat | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All‐cause mortality in trials with low or high risk of bias Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 1.1 Trials with low risk of bias | 30 | 67516 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.92, 0.99] |
| 1.2 Trials with high risk of bias | 26 | 27770 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.92, 1.06] |
| 2 All‐cause mortality in individually randomised and cluster‐randomised trials Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 2.1 Individually randomised trials | 54 | 81964 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.93, 0.99] |
| 2.2 Cluster‐randomised trials | 2 | 13322 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.82, 1.34] |
| 3 All‐cause mortality in placebo‐controlled and no intervention trials Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 3.1 Placebo in the control group | 44 | 73892 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.93, 0.99] |
| 3.2 No intervention in the control group | 12 | 21394 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.91, 1.21] |
| 4 All‐cause mortality and risk of industry bias Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 4.1 Trials without risk of industry bias | 7 | 7372 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.92, 1.03] |
| 4.2 Trials with risk of industry bias | 49 | 87914 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.93, 1.00] |
| 5 All‐cause mortality in primary and secondary prevention trials Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 5.1 Primary prevention trials | 48 | 94491 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 5.2 Secondary prevention trials | 8 | 795 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.73, 2.35] |
| 6 All‐cause mortality and vitamin D status Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 6.1 Vitamin D insufficiency | 26 | 56697 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 0.99] |
| 6.2 Vitamin D adequacy | 19 | 16283 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.87, 1.05] |
| 6.3 Unknown vitamin D status | 11 | 22306 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.92, 1.13] |
| 7 All‐cause mortality in ambulatory and institutionalised participants Show forest plot | 56 | 95286 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.94, 0.99] |
| 7.1 Ambulatory participants | 45 | 86071 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.92, 0.98] |
| 7.2 Institutionalised participants | 11 | 9215 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.92, 1.13] |
| 8 All‐cause mortality ('best‐worst case' and 'worst‐best case' scenario) Show forest plot | 53 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 'Best‐worst' case scenario | 53 | 84418 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.32, 0.51] |
| 8.2 'Worst‐best' case scenario | 53 | 84418 | Risk Ratio (M‐H, Random, 95% CI) | 2.78 [2.13, 3.63] |
| 9 All‐cause mortality in trials using vitamin D3 (cholecalciferol) Show forest plot | 38 | 75927 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.91, 0.98] |
| 9.1 Vitamin D3 trials with low risk of bias | 20 | 52645 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.89, 0.98] |
| 9.2 Vitamin D3 trials with high risk of bias | 18 | 23282 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 1.00] |
| 10 All‐cause mortality in trials using vitamin D3 singly or combined with calcium Show forest plot | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 10.1 Vitamin D3 singly | 13 | 12609 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.85, 1.00] |
| 10.2 Vitamin D3 combined with calcium | 27 | 63051 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.92, 0.99] |
| 11 All‐cause mortality in trials using low or high dose of vitamin D3 Show forest plot | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Low dose of vitamin D3 (< 800 IU a day) | 13 | 50437 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.87, 0.97] |
| 11.2 High dose of vitamin D3 (≥ 800 IU a day) | 26 | 25558 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.92, 1.00] |
| 12 All‐cause mortality in trials applying vitamin D3 daily or intermittently Show forest plot | 38 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Vitamin D3 daily | 31 | 69168 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 0.98] |
| 12.2 Vitamin D3 intermittently | 8 | 6871 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.77, 1.03] |
| 13 All‐cause mortality in trials using vitamin D3 and vitamin D status Show forest plot | 38 | 75927 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.91, 0.98] |
| 13.1 Vitamin D insufficiency | 20 | 55883 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.91, 0.99] |
| 13.2 Vitamin D adequacy | 10 | 4979 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.80, 1.07] |
| 13.3 Unknown vitamin D status | 8 | 15065 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.78, 1.16] |
| 14 All‐cause mortality in trials using vitamin D3 according to the participant's sex Show forest plot | 38 | 75927 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.91, 0.98] |
| 14.1 Vitamin D3 trialsincluding only women | 19 | 53062 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.84, 1.03] |
| 14.2 Vitamin D3 trials including men and women | 19 | 22865 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.89, 0.98] |
| 15 All‐cause mortality in trials using vitamin D2 (ergocalciferol) Show forest plot | 12 | 18349 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.96, 1.08] |
| 15.1 Vitamin D2 trials with low risk of bias | 9 | 14439 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.93, 1.04] |
| 15.2 Vitamin D2 trials with high risk of bias | 3 | 3910 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.05, 1.37] |
| 16 All‐cause mortality in trials using vitamin D2 singly or combined with calcium Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 16.1 Vitamin D2 singly | 8 | 17079 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.96, 1.12] |
| 16.2 Vitamin D2 combined with calcium | 5 | 1307 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.64, 1.57] |
| 17 All‐cause mortality in trials using low or high dose of vitamin D2 Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 17.1 Low dose of vitamin D2 | 1 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.17, 3.98] |
| 17.2 High dose of vitamin D2 | 12 | 18273 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.95, 1.10] |
| 18 All‐cause mortality in trials applying vitamin D2 daily or intermittently Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 18.1 Vitamin D2 daily | 6 | 1349 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.68, 1.12] |
| 18.2 Vitamin D2 intermittently | 6 | 17000 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.95, 1.18] |
| 19 All‐cause mortality in trials using vitamin D2 and vitamin D status Show forest plot | 12 | 18349 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.96, 1.08] |
| 19.1 Vitamin D insufficiency | 6 | 4413 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.05, 1.37] |
| 19.2 Vitamin D adequacy | 5 | 10496 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.10] |
| 19.3 Unknown vitamin D status | 1 | 3440 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.93, 1.05] |
| 20 All‐cause mortality in trials using alfacalcidol (1α‐hydroxyvitamin D) Show forest plot | 4 | 617 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.22, 4.15] |
| 21 All‐cause mortality in trials using alfacalcidol and vitamin D status Show forest plot | 4 | 617 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.22, 4.15] |
| 21.1 Vitamin D insufficiency | 2 | 155 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.11, 9.52] |
| 21.2 Vitamin D adequacy | 1 | 378 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.06, 15.37] |
| 21.3 Unknown vitamin D status | 1 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.06, 13.40] |
| 22 All‐cause mortality in trials using calcitriol (1,25‐dihydroxyvitamin D) Show forest plot | 3 | 430 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.27, 7.03] |
| 23 All‐cause mortality in trials using calcitriol and vitamin D status Show forest plot | 3 | 430 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.27, 7.03] |
| 23.1 Vitamin D insufficiency | 1 | 86 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.96] |
| 23.2 Vitamin D adequacy | 2 | 344 | Risk Ratio (M‐H, Random, 95% CI) | 2.28 [0.34, 15.39] |
| 24 Cancer mortality Show forest plot | 4 | 44492 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 0.98] |
| 25 Cardiovascular mortality Show forest plot | 10 | 47267 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.90, 1.07] |
| 26 Adverse events Show forest plot | 35 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 26.1 Hypercalcemia in trials using supplemental forms of vitamin D | 15 | 11323 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.85, 2.18] |
| 26.2 Hypercalcemia in trials using active forms of vitamin D | 3 | 710 | Risk Ratio (M‐H, Random, 95% CI) | 3.18 [1.17, 8.68] |
| 26.3 Nephrolithiasis in trials using vitamin D3 combined with calcium | 4 | 42876 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.02, 1.34] |
| 26.4 Nephrolithiasis in trials using calcitriol | 1 | 246 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 8.10] |
| 26.5 Hypercalciuria | 3 | 695 | Risk Ratio (M‐H, Random, 95% CI) | 4.64 [0.99, 21.76] |
| 26.6 Renal insufficiency | 3 | 5495 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [0.27, 10.70] |
| 26.7 Cardiovascular disorders | 8 | 4495 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.86, 1.05] |
| 26.8 Gastrointestinal disorders | 16 | 9702 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.87, 2.13] |
| 26.9 Psychiatric disorders | 3 | 580 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.56, 3.73] |
| 26.10 Skin disorders | 2 | 3810 | Risk Ratio (M‐H, Random, 95% CI) | 3.27 [0.17, 62.47] |
| 26.11 Cancer | 14 | 49707 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.94, 1.06] |

